Circulatory System Most animals have a circulatory system
- Slides: 28
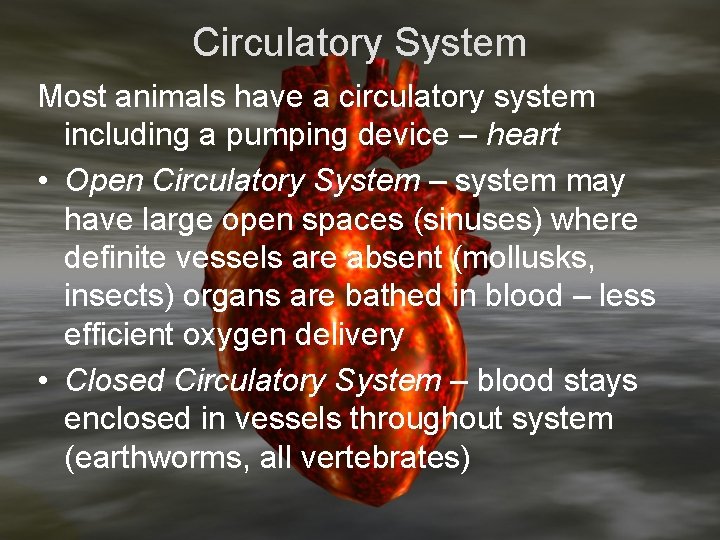
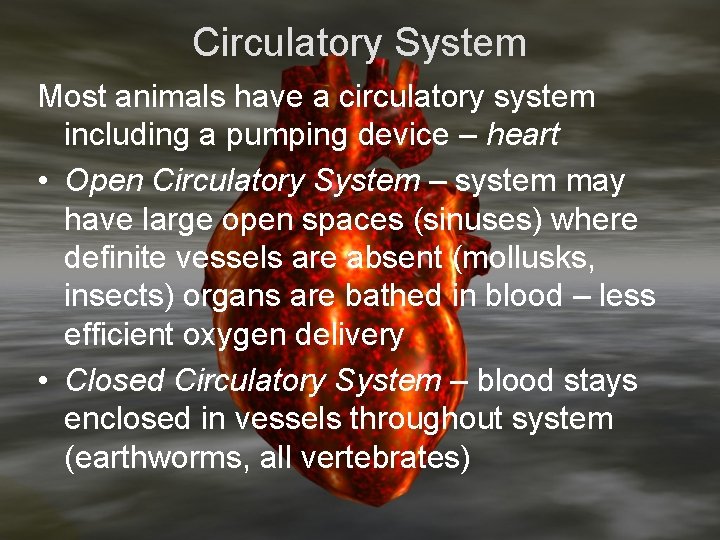
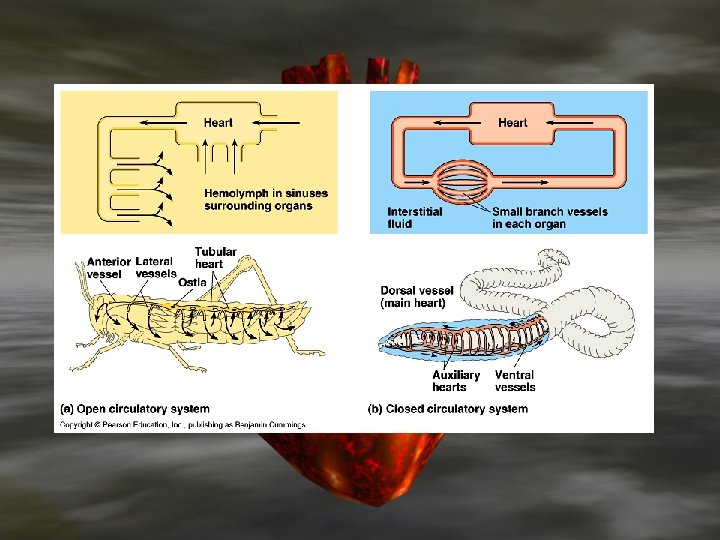
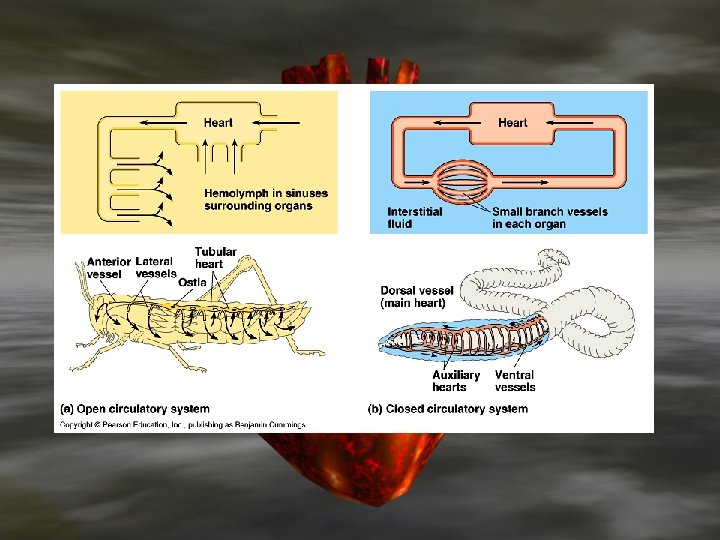
Circulatory System Most animals have a circulatory system including a pumping device – heart • Open Circulatory System – system may have large open spaces (sinuses) where definite vessels are absent (mollusks, insects) organs are bathed in blood – less efficient oxygen delivery • Closed Circulatory System – blood stays enclosed in vessels throughout system (earthworms, all vertebrates)
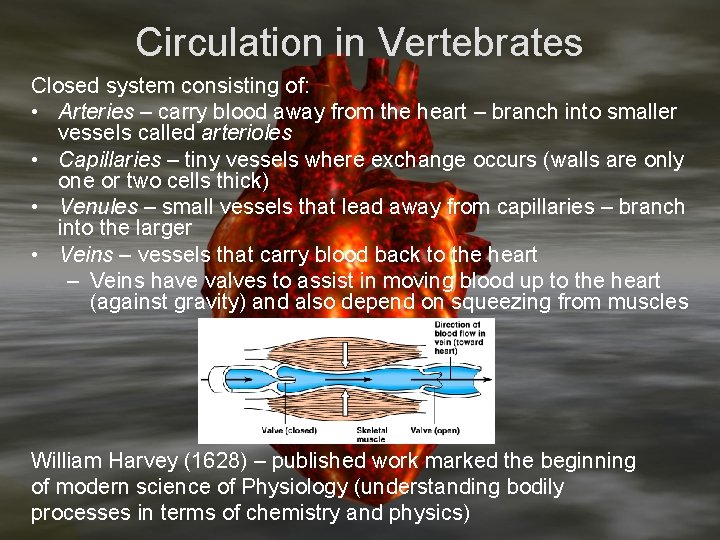
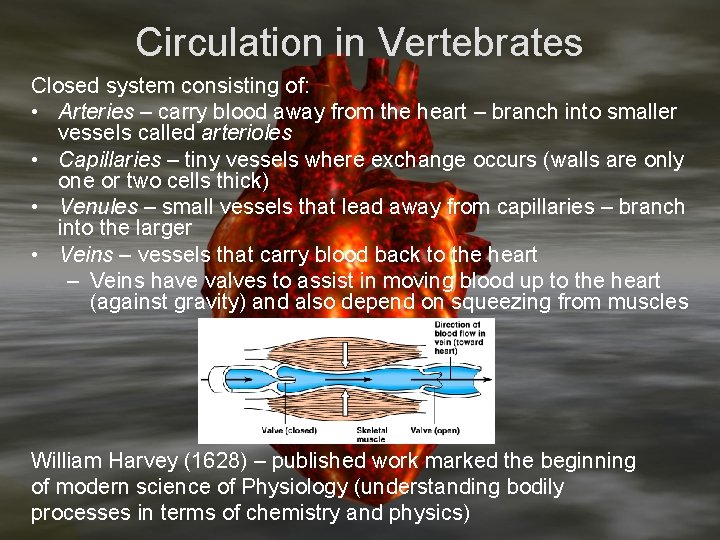
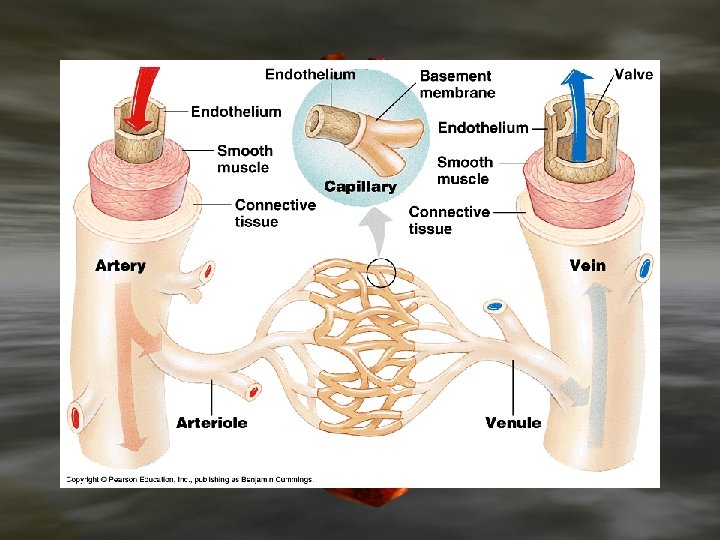
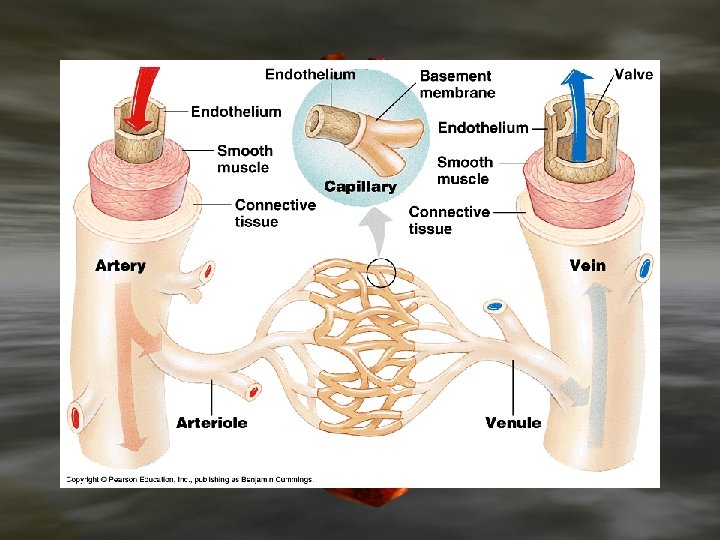
Circulation in Vertebrates Closed system consisting of: • Arteries – carry blood away from the heart – branch into smaller vessels called arterioles • Capillaries – tiny vessels where exchange occurs (walls are only one or two cells thick) • Venules – small vessels that lead away from capillaries – branch into the larger • Veins – vessels that carry blood back to the heart – Veins have valves to assist in moving blood up to the heart (against gravity) and also depend on squeezing from muscles William Harvey (1628) – published work marked the beginning of modern science of Physiology (understanding bodily processes in terms of chemistry and physics)
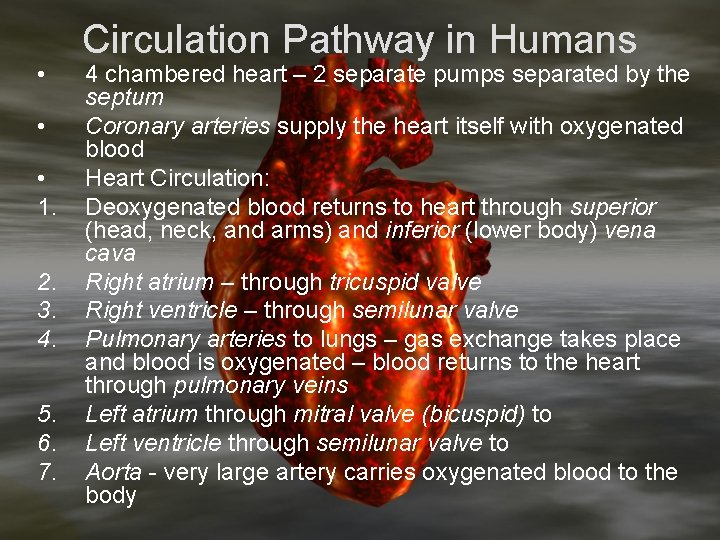
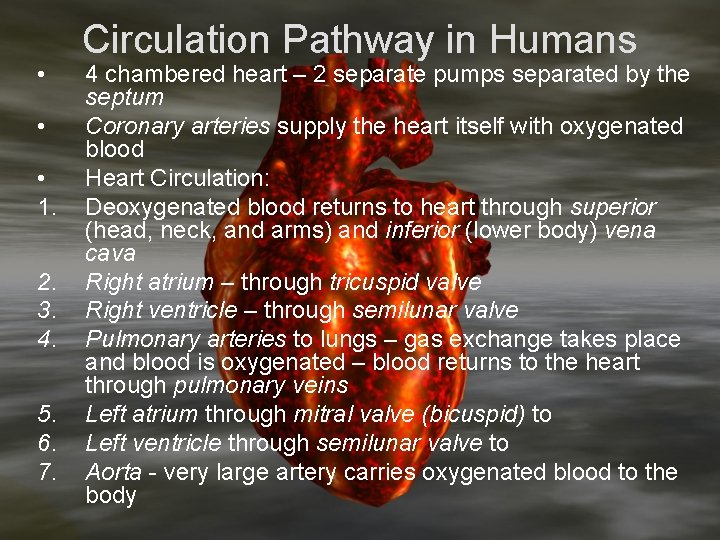
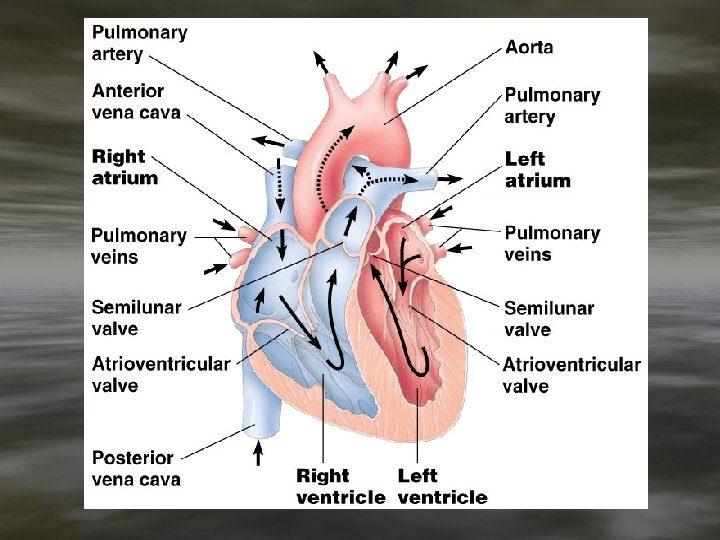
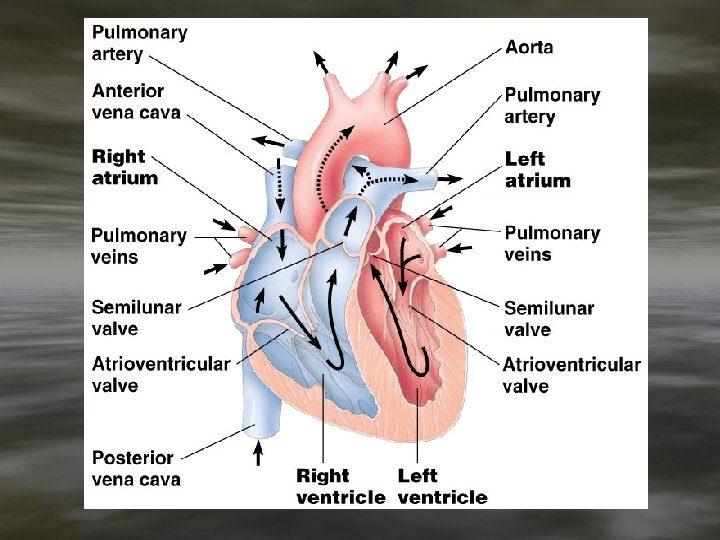
• • • 1. 2. 3. 4. 5. 6. 7. Circulation Pathway in Humans 4 chambered heart – 2 separate pumps separated by the septum Coronary arteries supply the heart itself with oxygenated blood Heart Circulation: Deoxygenated blood returns to heart through superior (head, neck, and arms) and inferior (lower body) vena cava Right atrium – through tricuspid valve Right ventricle – through semilunar valve Pulmonary arteries to lungs – gas exchange takes place and blood is oxygenated – blood returns to the heart through pulmonary veins Left atrium through mitral valve (bicuspid) to Left ventricle through semilunar valve to Aorta - very large artery carries oxygenated blood to the body
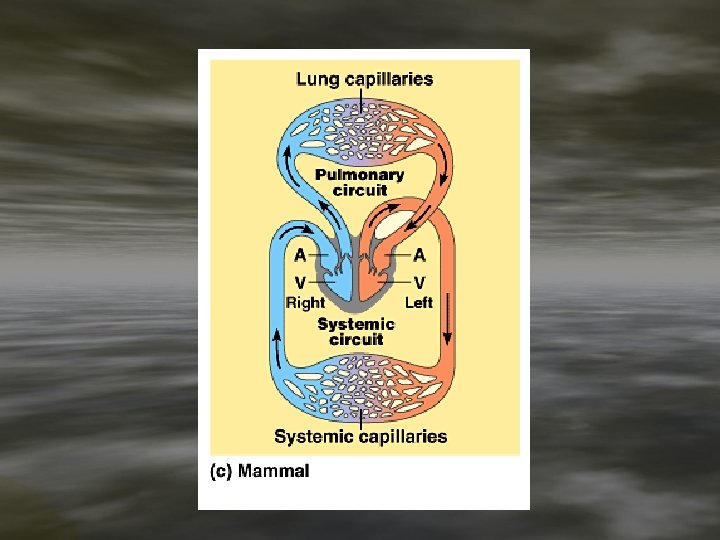
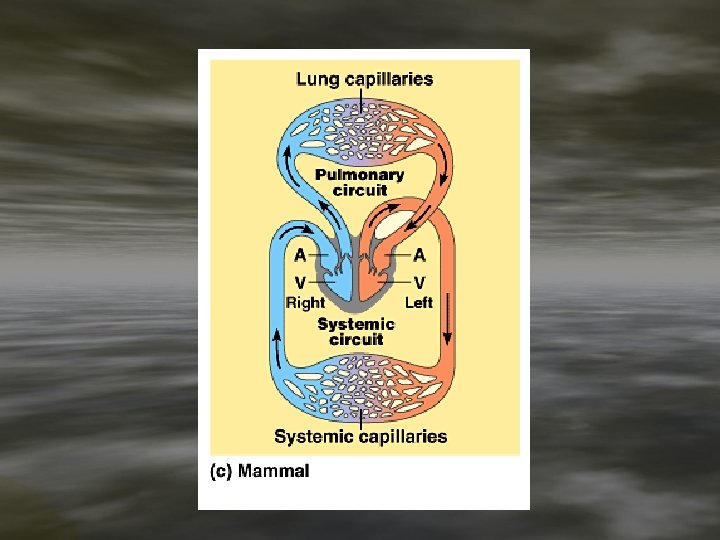
Circulation outside of the heart is divided into: • Pulmonary circulation – pulmonary arteries carry deoxy. blood to lungs and pulmonary veins carry oxy. blood to heart • Systemic circulation – aorta, arteries and arterioles carry oxg. blood to cells – venules and veins carry deoxy. blood back to heart
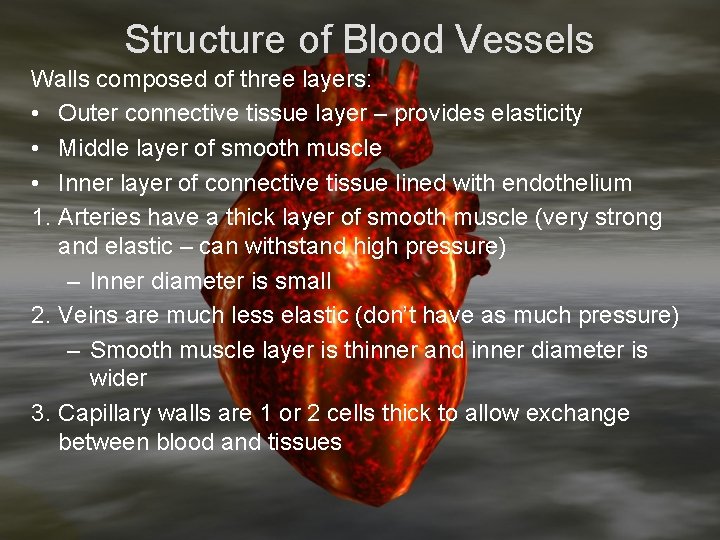
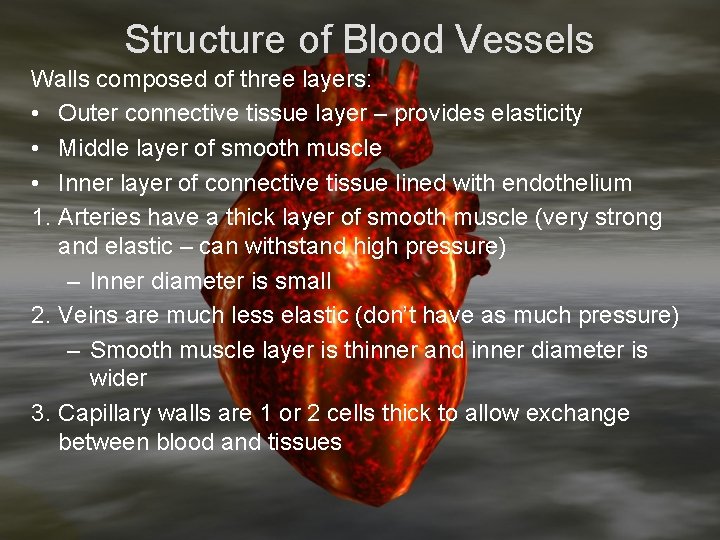
Structure of Blood Vessels Walls composed of three layers: • Outer connective tissue layer – provides elasticity • Middle layer of smooth muscle • Inner layer of connective tissue lined with endothelium 1. Arteries have a thick layer of smooth muscle (very strong and elastic – can withstand high pressure) – Inner diameter is small 2. Veins are much less elastic (don’t have as much pressure) – Smooth muscle layer is thinner and inner diameter is wider 3. Capillary walls are 1 or 2 cells thick to allow exchange between blood and tissues
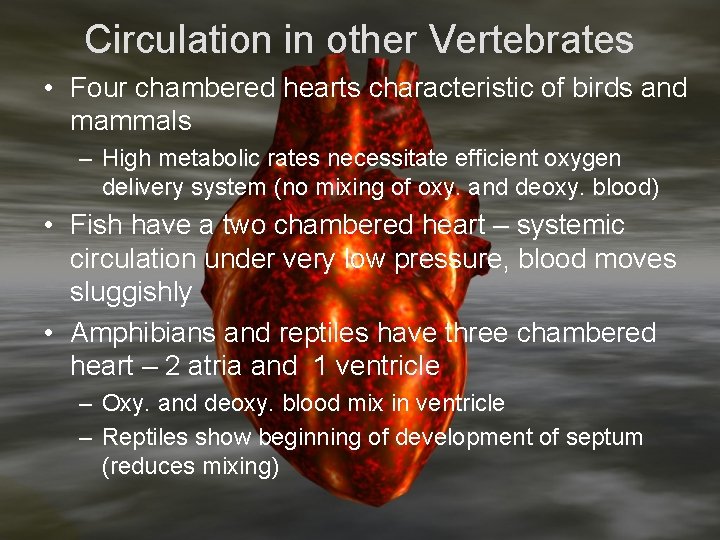
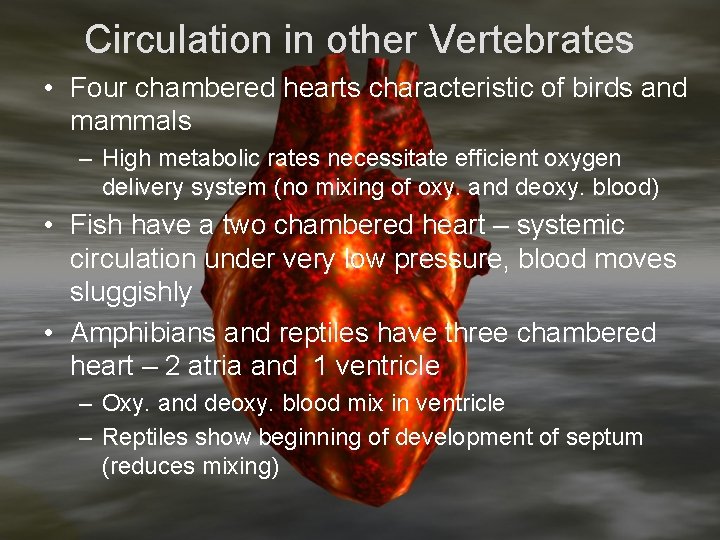
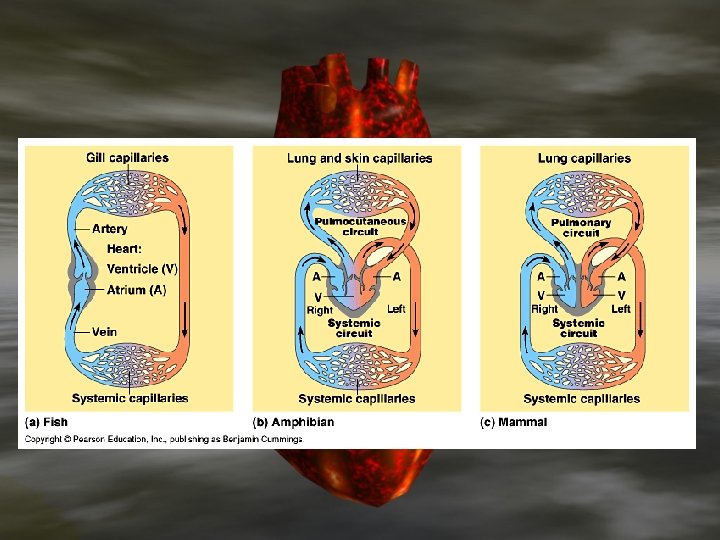
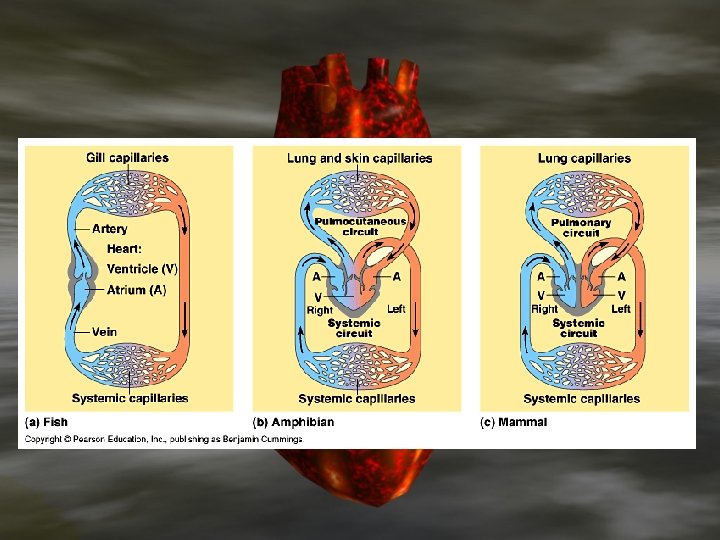
Circulation in other Vertebrates • Four chambered hearts characteristic of birds and mammals – High metabolic rates necessitate efficient oxygen delivery system (no mixing of oxy. and deoxy. blood) • Fish have a two chambered heart – systemic circulation under very low pressure, blood moves sluggishly • Amphibians and reptiles have three chambered heart – 2 atria and 1 ventricle – Oxy. and deoxy. blood mix in ventricle – Reptiles show beginning of development of septum (reduces mixing)
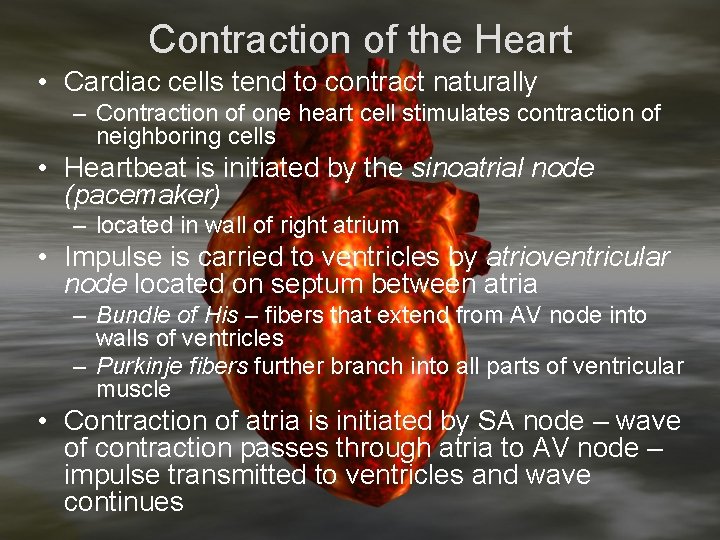
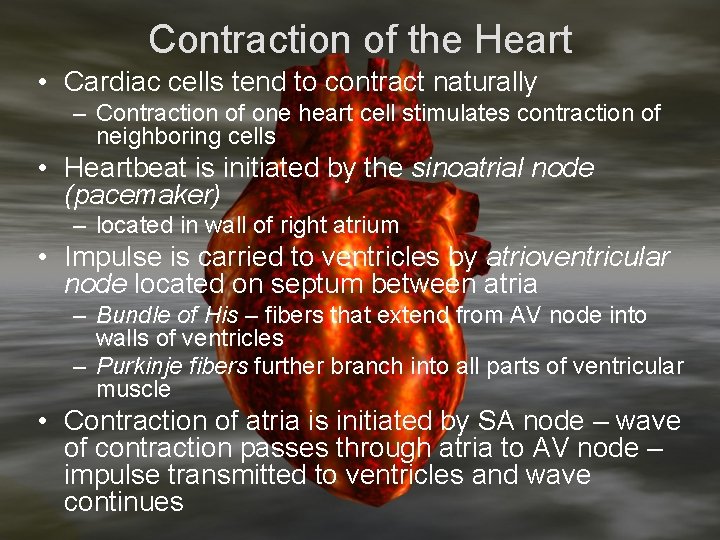
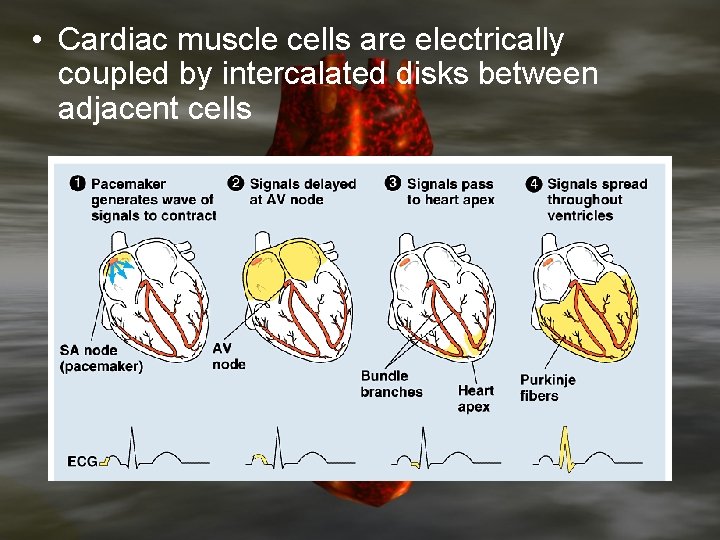
Contraction of the Heart • Cardiac cells tend to contract naturally – Contraction of one heart cell stimulates contraction of neighboring cells • Heartbeat is initiated by the sinoatrial node (pacemaker) – located in wall of right atrium • Impulse is carried to ventricles by atrioventricular node located on septum between atria – Bundle of His – fibers that extend from AV node into walls of ventricles – Purkinje fibers further branch into all parts of ventricular muscle • Contraction of atria is initiated by SA node – wave of contraction passes through atria to AV node – impulse transmitted to ventricles and wave continues
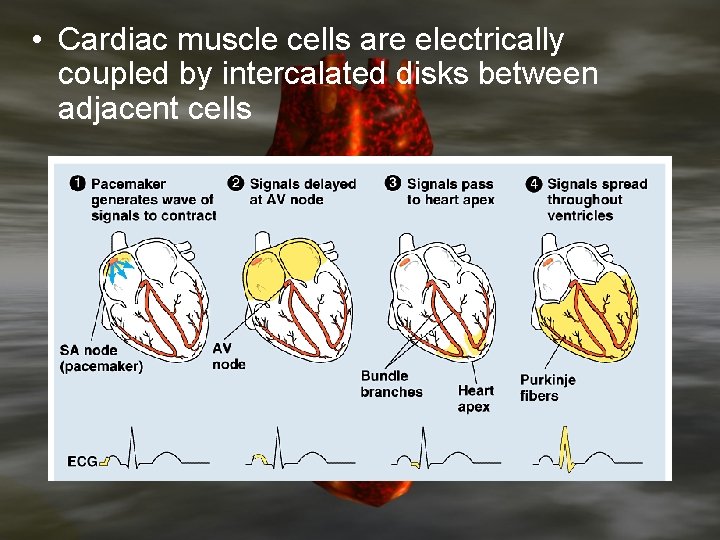
• Cardiac muscle cells are electrically coupled by intercalated disks between adjacent cells
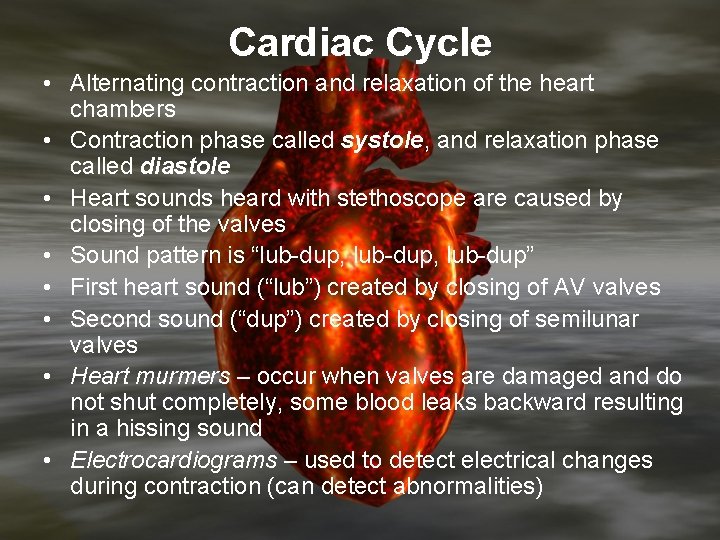
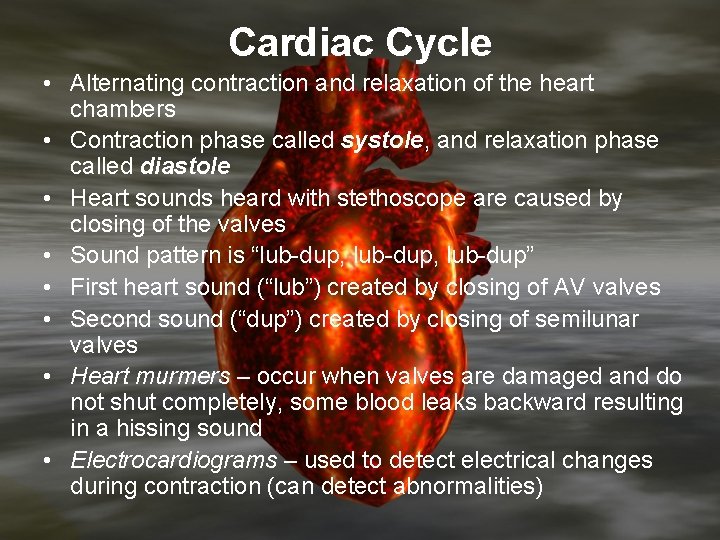
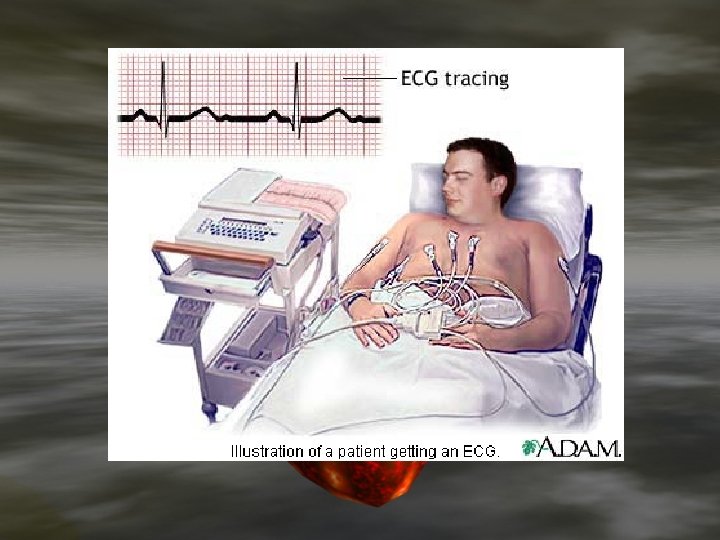
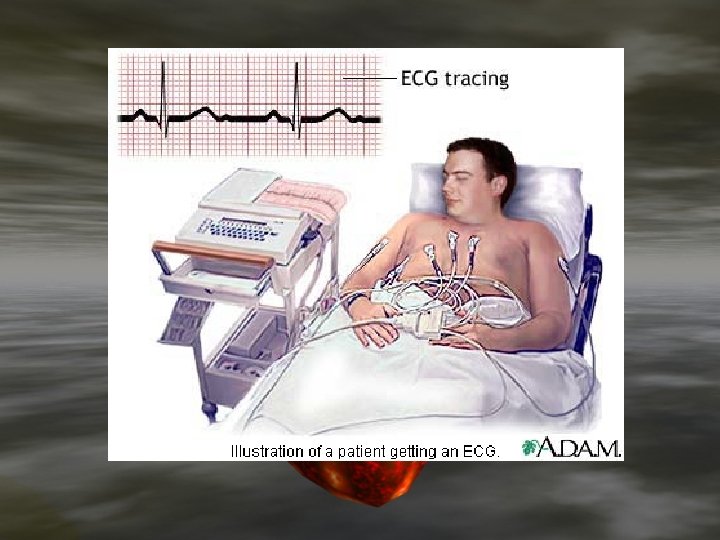
Cardiac Cycle • Alternating contraction and relaxation of the heart chambers • Contraction phase called systole, and relaxation phase called diastole • Heart sounds heard with stethoscope are caused by closing of the valves • Sound pattern is “lub-dup, lub-dup” • First heart sound (“lub”) created by closing of AV valves • Second sound (“dup”) created by closing of semilunar valves • Heart murmers – occur when valves are damaged and do not shut completely, some blood leaks backward resulting in a hissing sound • Electrocardiograms – used to detect electrical changes during contraction (can detect abnormalities)
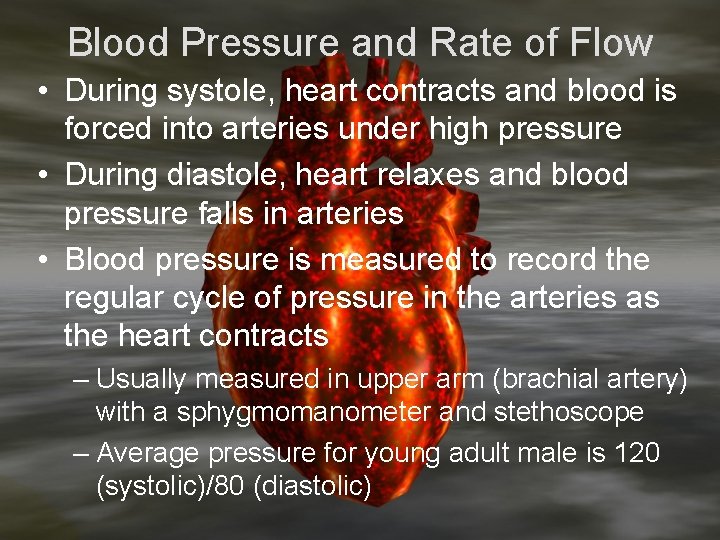
Blood Pressure and Rate of Flow • During systole, heart contracts and blood is forced into arteries under high pressure • During diastole, heart relaxes and blood pressure falls in arteries • Blood pressure is measured to record the regular cycle of pressure in the arteries as the heart contracts – Usually measured in upper arm (brachial artery) with a sphygmomanometer and stethoscope – Average pressure for young adult male is 120 (systolic)/80 (diastolic)
Blood pressure varies by location in body and decreases with distance from the heart • Resulting gradient of pressure causes continuing flow of blood – fluids move from regions of high pressure to regions of low pressure • Differences in systolic and diastolic pressures diminish with distance from heart • By the time blood reaches capillaries the flow is constant (rather than surging as in the arteries) • Pressure continually drops through arterioles and capillaries, lowest in veins closest to heart • Rate of flow highest in arteries • Rate of flow lowest in capillaries • Increases again in veins
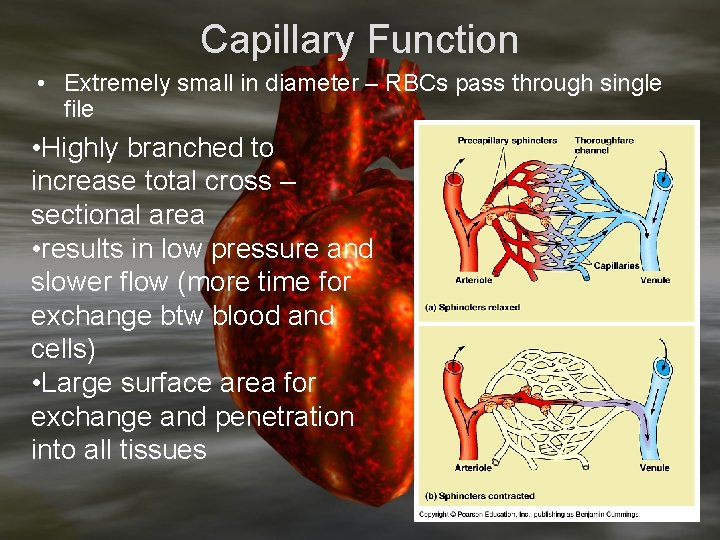
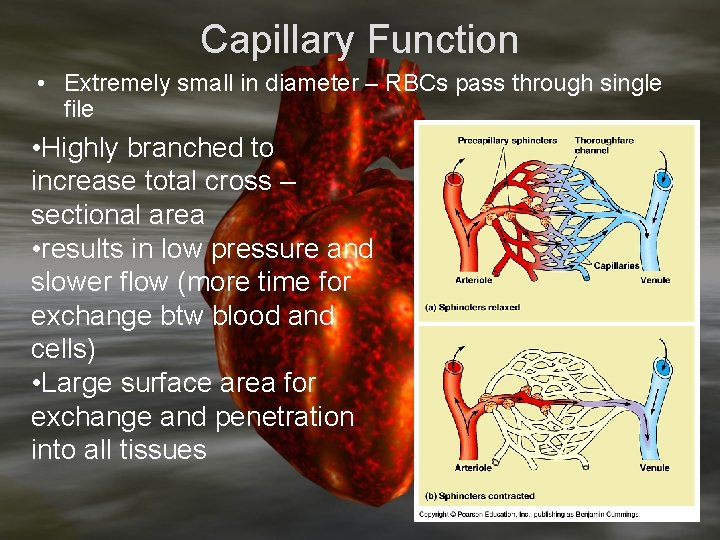
Capillary Function • Extremely small in diameter – RBCs pass through single file • Highly branched to increase total cross – sectional area • results in low pressure and slower flow (more time for exchange btw blood and cells) • Large surface area for exchange and penetration into all tissues
Mechanisms for Exchange between Blood and Tissue • Diffusion • Materials are picked up by vesicles in cell membrane of capillary endothelial cell (endocytosis) travel across cell and are expelled by exocytosis • Water and dissolved molecules (not proteins) filter through clefts between adjacent endothelial cells
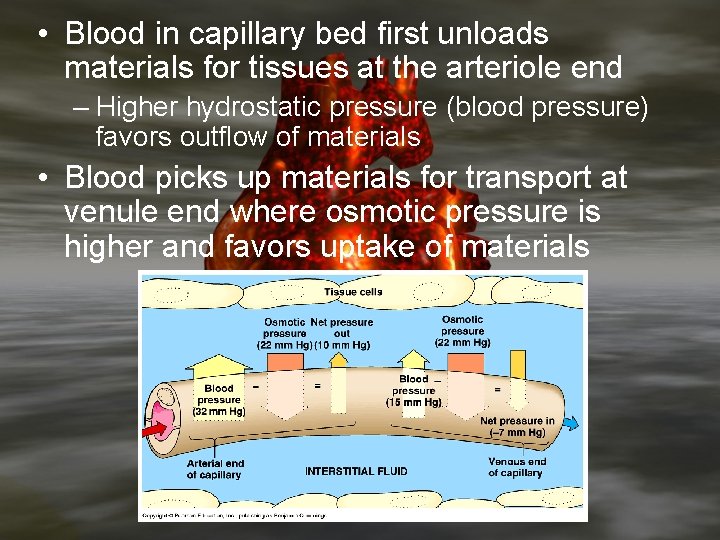
Capillary exchange occurs as a result of two opposing forces: 1. Hydrostatic pressure of blood higher at arteriole end than at venule end – tends to force materials out of capillary into tissues 2. Osmotic pressure is higher in blood than in surrounding tissues (because of concentration of proteins in blood) so water tends to diffuse back into capillaries
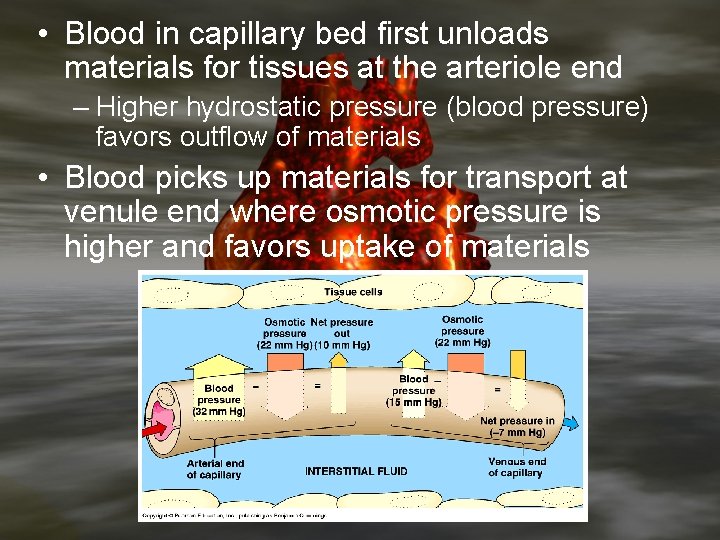
• Blood in capillary bed first unloads materials for tissues at the arteriole end – Higher hydrostatic pressure (blood pressure) favors outflow of materials • Blood picks up materials for transport at venule end where osmotic pressure is higher and favors uptake of materials
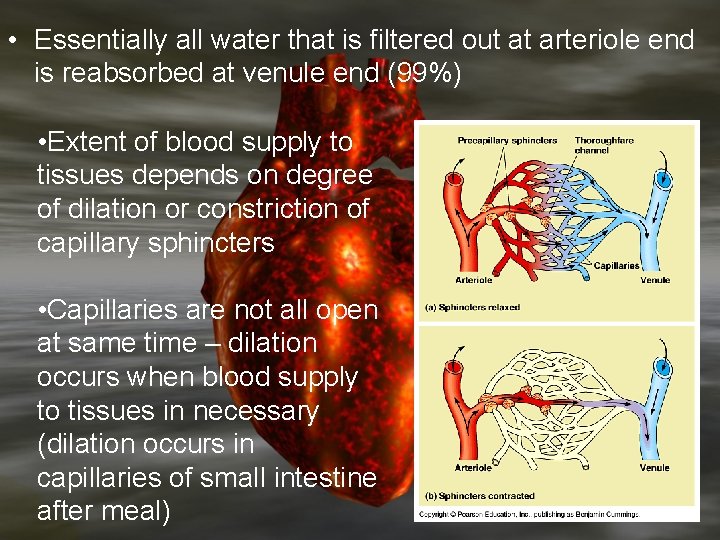
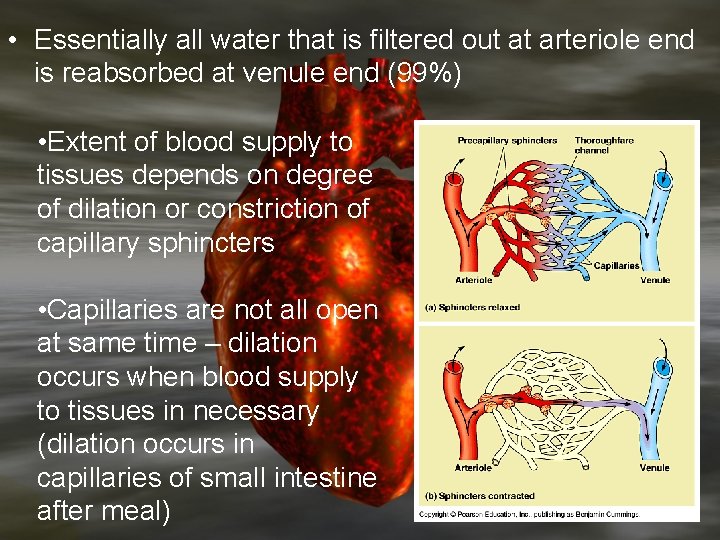
• Essentially all water that is filtered out at arteriole end is reabsorbed at venule end (99%) • Extent of blood supply to tissues depends on degree of dilation or constriction of capillary sphincters • Capillaries are not all open at same time – dilation occurs when blood supply to tissues in necessary (dilation occurs in capillaries of small intestine after meal)
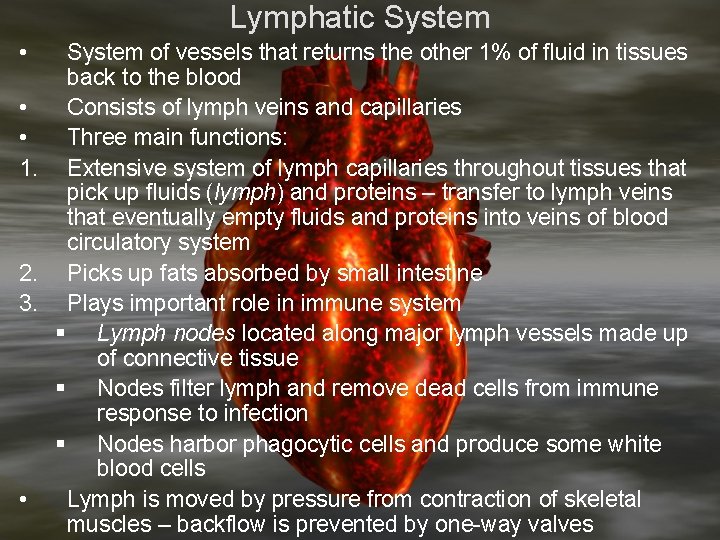
Lymphatic System • System of vessels that returns the other 1% of fluid in tissues back to the blood • Consists of lymph veins and capillaries • Three main functions: 1. Extensive system of lymph capillaries throughout tissues that pick up fluids (lymph) and proteins – transfer to lymph veins that eventually empty fluids and proteins into veins of blood circulatory system 2. Picks up fats absorbed by small intestine 3. Plays important role in immune system § Lymph nodes located along major lymph vessels made up of connective tissue § Nodes filter lymph and remove dead cells from immune response to infection § Nodes harbor phagocytic cells and produce some white blood cells • Lymph is moved by pressure from contraction of skeletal muscles – backflow is prevented by one-way valves
1. 2. 3. 4. 5. 6. Composition of Blood Plasma – liquid matrix constituting 50 – 60% of whole blood plasma is 90% water with a variety of dissolved substances: • 0. 9% - inorganic cations (Na+, Ca+2, K+, Mg+2) and organic anions (Cl-, HCO 3 -) § concentrations are kept relatively stable to maintain homeostasis (even slight shifts in concentration cause dysfunction or cell death) 7 – 9% - plasma proteins (fibrinogen, albumins, and globulins – important for osmotic pressure in plasma, help to transport substances, blood clotting) Organic nutrients (glucose, fats, phospholipids, amino acids, lactic acid, cholesterol) Nitrogenous wastes – urea, ammonia and uric acid Hormones – regulatory chemicals 3 gases found in small amounts – nitrogen, oxygen and carbon dioxide
Composition of Blood Cells found in blood: 1. White blood cells – leukocytes • Five major types: monocytes, neutrophils, basophils, eosinophils, and lymphocytes • Fight infections • Monocytes and neutrophils are phagocytes • Eosinophils fight infection against parasites • Basophils release histamine – causes vasodilation (increases blood flow to injured site) – part of inflammatory response • Lymphocytes – B cells and T cells – part of specific immune response resulting from exposure to an antigen (foreign substance in body) § B cells produce antibodies (globulin proteins) to destroy antigen – specifically fight antigen that stimulates production
Composition of Blood 2. Red Blood Cells – erythrocytes • • • Biconcave, disc-shaped, lack nuclei Approx 5 million/mm 3 of blood Live approx 120 days – destroyed by liver and spleen Formed in red bone marrow (in long bones, skull, ribs, and pelvis) Filled with hemoglobin (carries oxygen, gives red color) • Some animals (mollusks and arthropods) have hemocyanin – contains Cu instead of Fe – dissolved in plasma not in cells
• Whole blood – blood as it is in the circulatory system • Blood plasma – whole blood without formed elements • Blood serum – plasma without fibrinogen
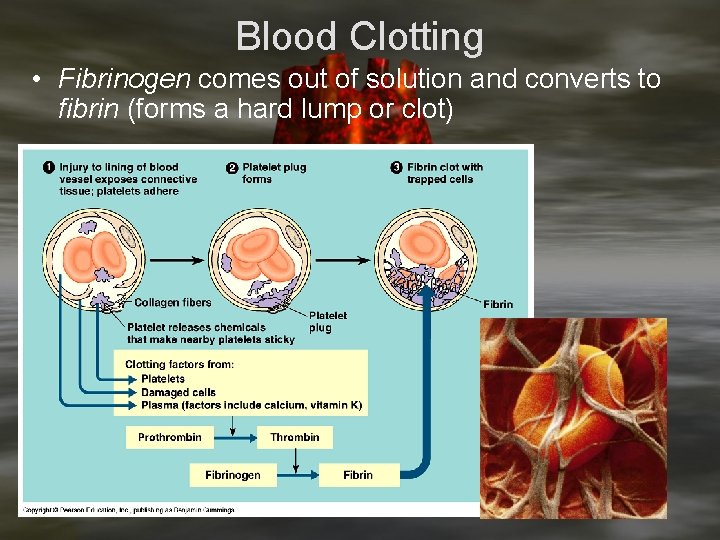
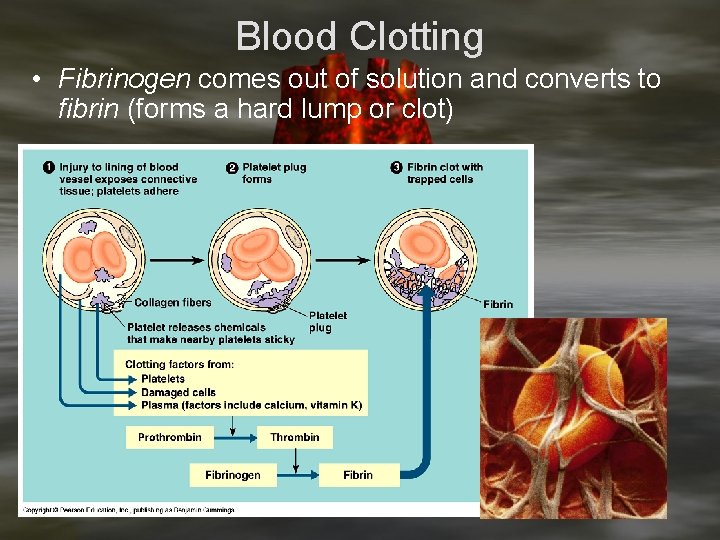
Blood Clotting • Fibrinogen comes out of solution and converts to fibrin (forms a hard lump or clot)