Circulatory Arrest Cooper University Hospital School of Perfusion
- Slides: 28
Circulatory Arrest Cooper University Hospital School of Perfusion 2015 Michael F. Hancock, CCP
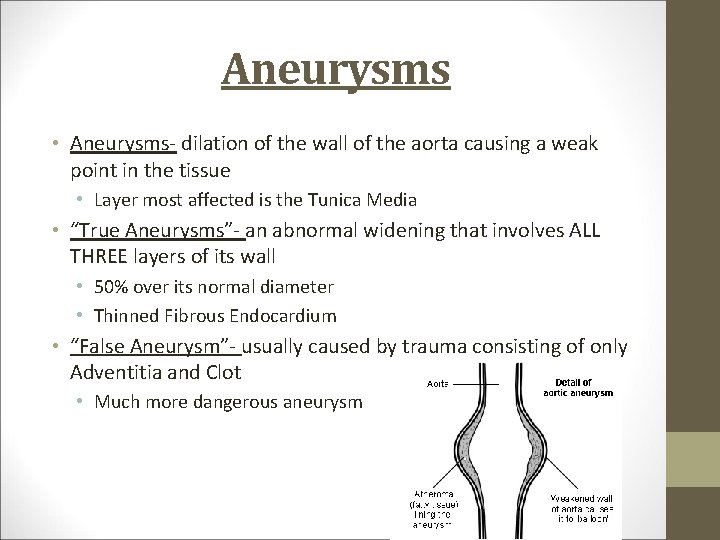
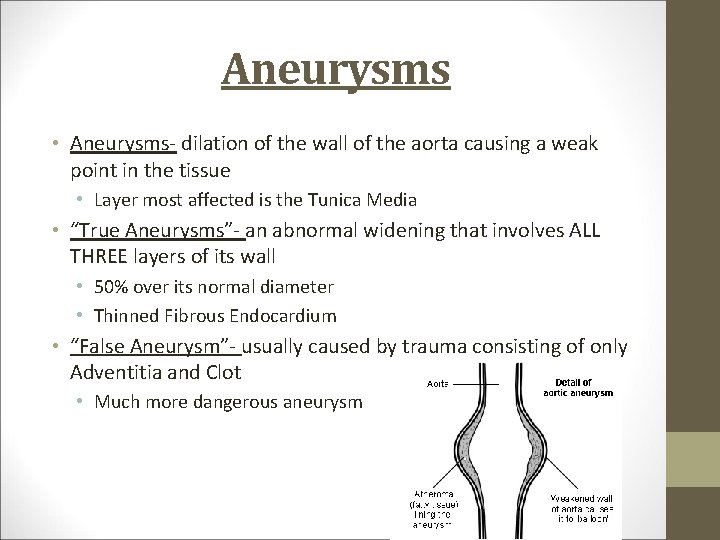
Aneurysms • Aneurysms- dilation of the wall of the aorta causing a weak point in the tissue • Layer most affected is the Tunica Media • “True Aneurysms”- an abnormal widening that involves ALL THREE layers of its wall • 50% over its normal diameter • Thinned Fibrous Endocardium • “False Aneurysm”- usually caused by trauma consisting of only Adventitia and Clot • Much more dangerous aneurysm
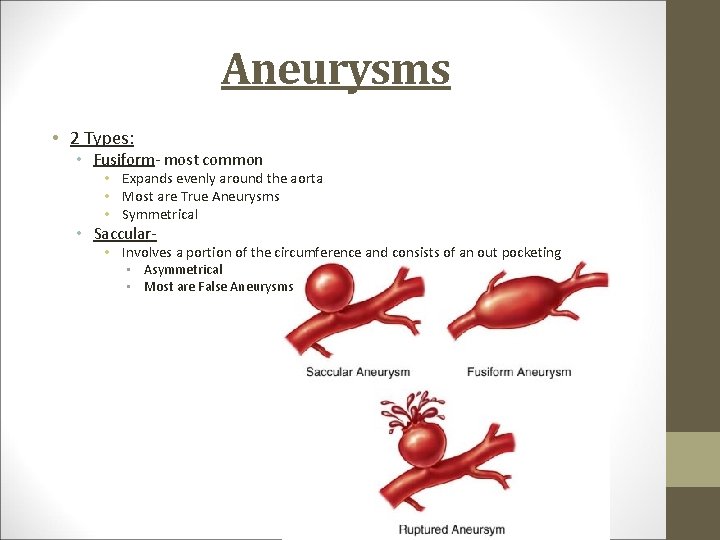
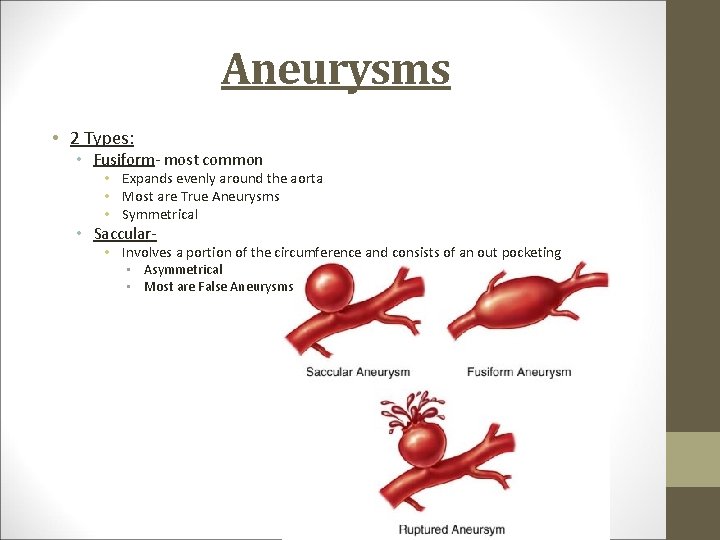
Aneurysms • 2 Types: • Fusiform- most common • Expands evenly around the aorta • Most are True Aneurysms • Symmetrical • Saccular- • Involves a portion of the circumference and consists of an out pocketing • Asymmetrical • Most are False Aneurysms
Causes of Aneurysms • Atherosclerosis- most common • Cystic Medial Degeneration • Ie. Marfan’s Syndrome • Degeneration of the elastic and smooth muscle fibers of the tunica media • Trauma • HTN • Infections
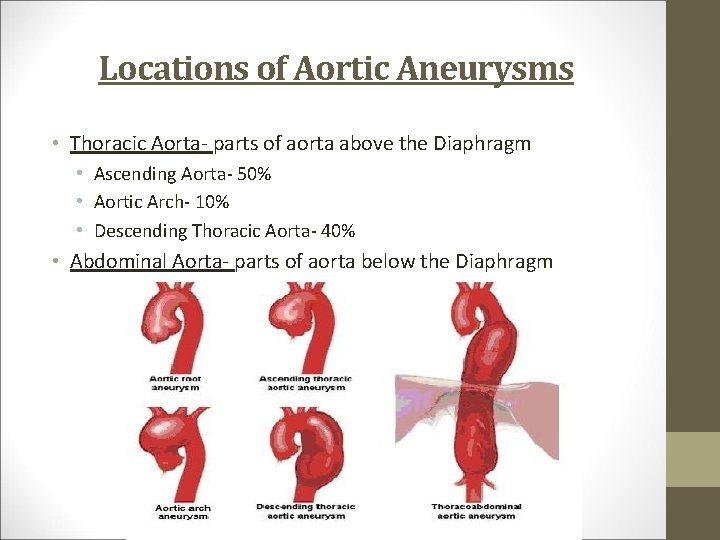
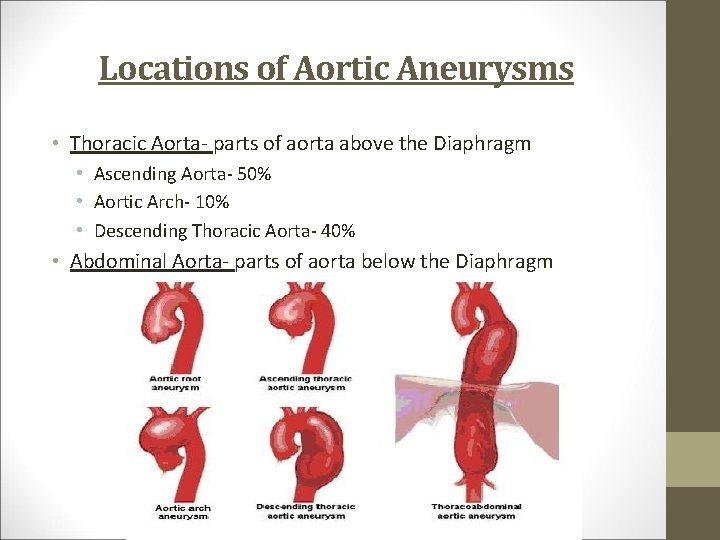
Locations of Aortic Aneurysms • Thoracic Aorta- parts of aorta above the Diaphragm • Ascending Aorta- 50% • Aortic Arch- 10% • Descending Thoracic Aorta- 40% • Abdominal Aorta- parts of aorta below the Diaphragm
Thoracic Aortic Aneurysms • Thoracic Aorta • Account for 25% of aortic aneurysms • Cause • Atherosclerosis • Marfan’s Syndrome • HTN- leads to growth of aneurysm size • Symptoms • Back or Neck Pain • Coughing, Edema • 50% Asymptomatic • Detection- CAT Scan or MRI • Rupture- leads to hypovolemic shock and death
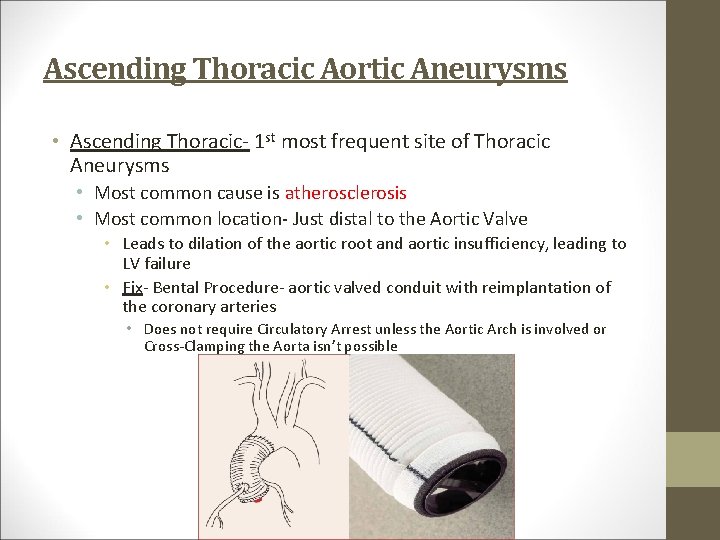
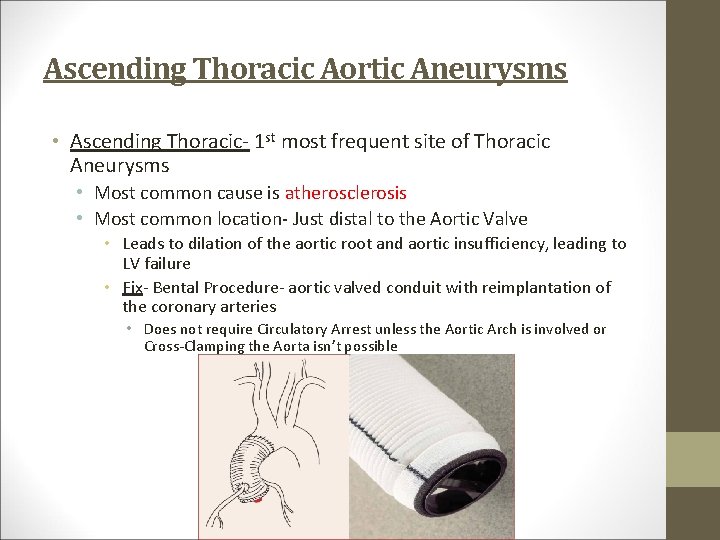
Ascending Thoracic Aortic Aneurysms • Ascending Thoracic- 1 st most frequent site of Thoracic Aneurysms • Most common cause is atherosclerosis • Most common location- Just distal to the Aortic Valve • Leads to dilation of the aortic root and aortic insufficiency, leading to LV failure • Fix- Bental Procedure- aortic valved conduit with reimplantation of the coronary arteries • Does not require Circulatory Arrest unless the Aortic Arch is involved or Cross-Clamping the Aorta isn’t possible
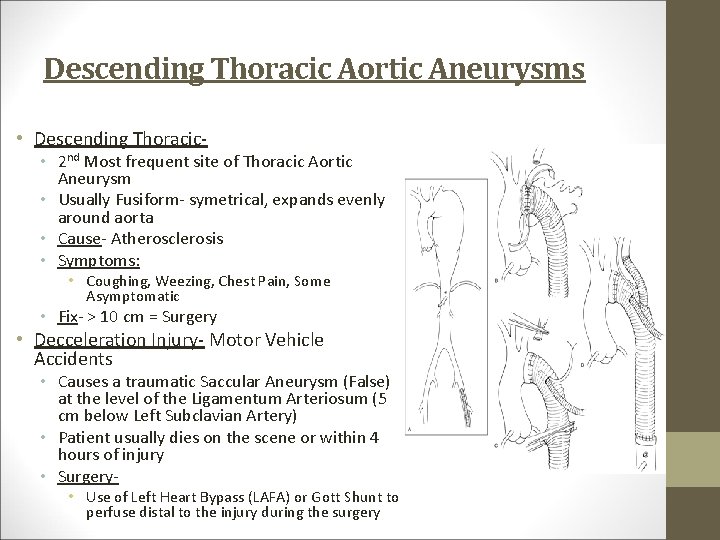
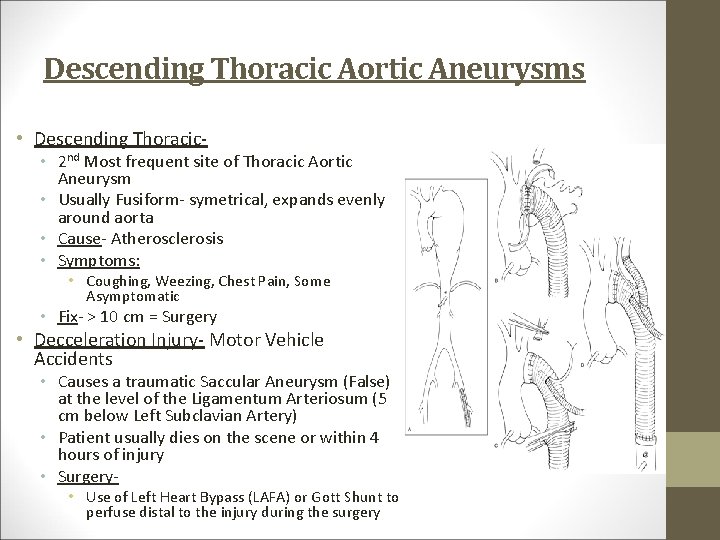
Descending Thoracic Aortic Aneurysms • Descending Thoracic- • 2 nd Most frequent site of Thoracic Aortic Aneurysm • Usually Fusiform- symetrical, expands evenly around aorta • Cause- Atherosclerosis • Symptoms: • Coughing, Weezing, Chest Pain, Some Asymptomatic • Fix- > 10 cm = Surgery • Decceleration Injury- Motor Vehicle Accidents • Causes a traumatic Saccular Aneurysm (False) at the level of the Ligamentum Arteriosum (5 cm below Left Subclavian Artery) • Patient usually dies on the scene or within 4 hours of injury • Surgery- • Use of Left Heart Bypass (LAFA) or Gott Shunt to perfuse distal to the injury during the surgery
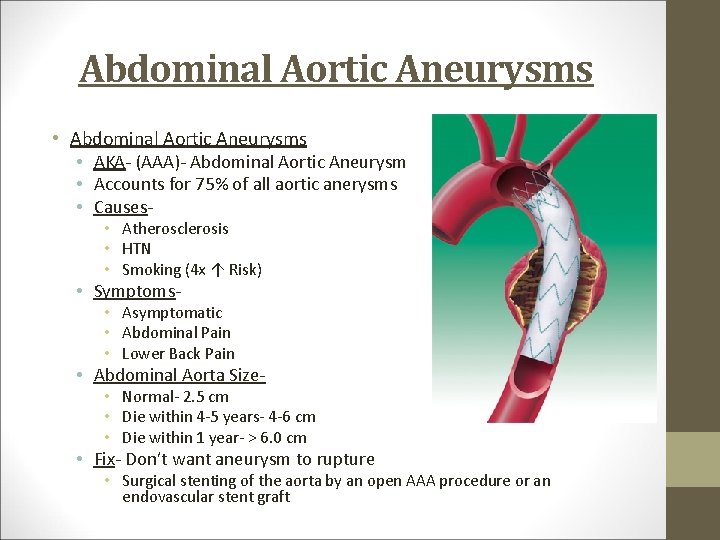
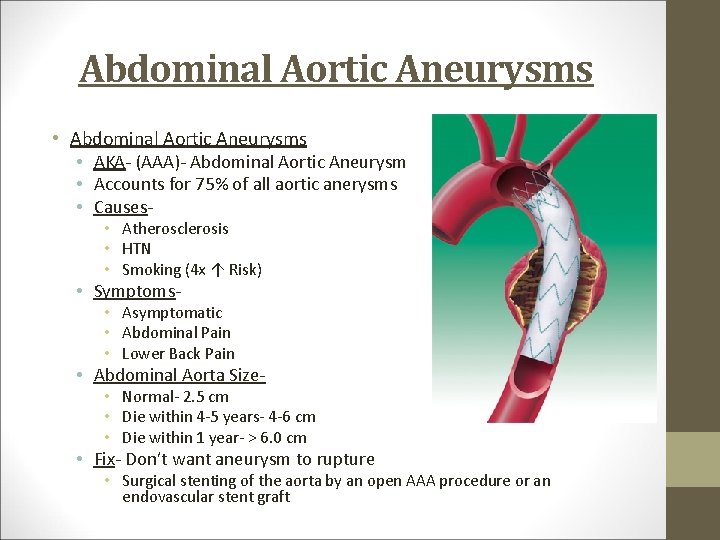
Abdominal Aortic Aneurysms • AKA- (AAA)- Abdominal Aortic Aneurysm • Accounts for 75% of all aortic anerysms • Causes • Atherosclerosis • HTN • Smoking (4 x ↑ Risk) • Symptoms- • Asymptomatic • Abdominal Pain • Lower Back Pain • Abdominal Aorta Size- • Normal- 2. 5 cm • Die within 4 -5 years- 4 -6 cm • Die within 1 year- > 6. 0 cm • Fix- Don’t want aneurysm to rupture • Surgical stenting of the aorta by an open AAA procedure or an endovascular stent graft
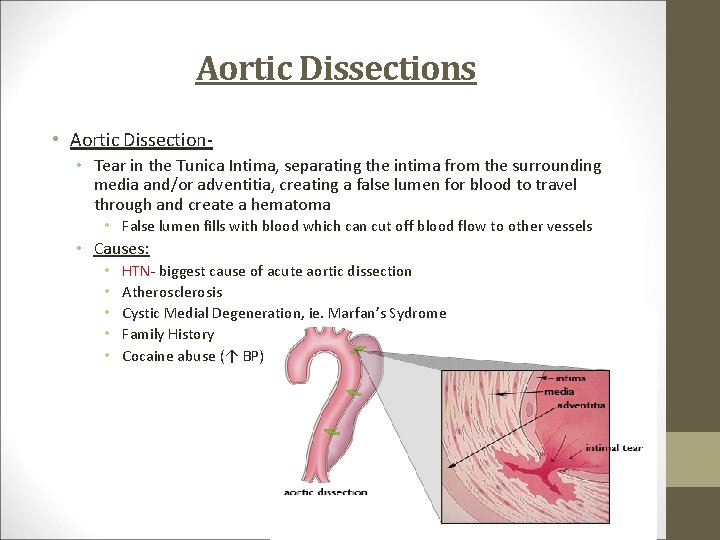
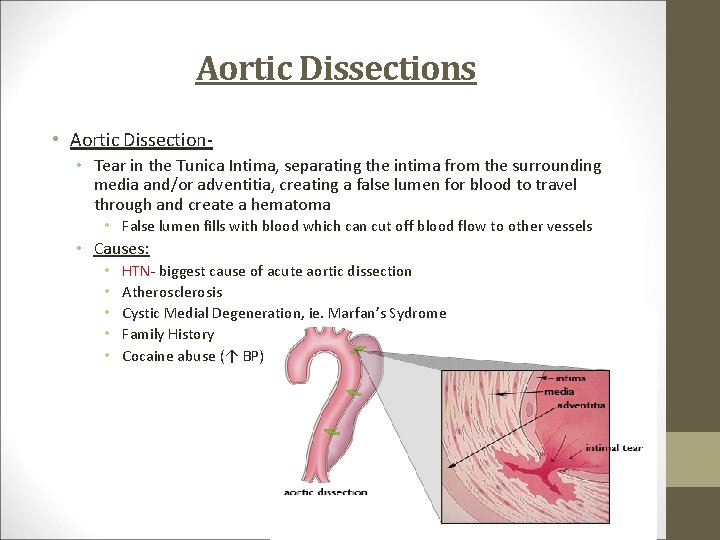
Aortic Dissections • Aortic Dissection • Tear in the Tunica Intima, separating the intima from the surrounding media and/or adventitia, creating a false lumen for blood to travel through and create a hematoma • False lumen fills with blood which can cut off blood flow to other vessels • Causes: • • • HTN- biggest cause of acute aortic dissection Atherosclerosis Cystic Medial Degeneration, ie. Marfan’s Sydrome Family History Cocaine abuse (↑ BP)
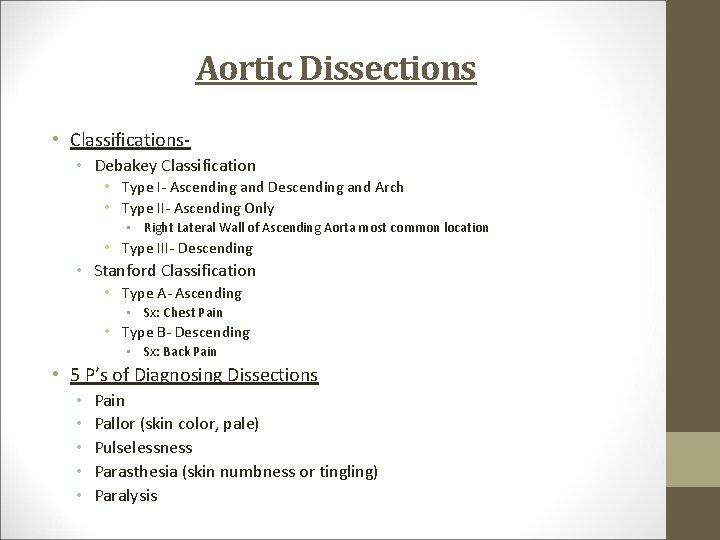
Aortic Dissections • Classifications • Debakey Classification • Type I- Ascending and Descending and Arch • Type II- Ascending Only • Right Lateral Wall of Ascending Aorta most common location • Type III- Descending • Stanford Classification • Type A- Ascending • Sx: Chest Pain • Type B- Descending • Sx: Back Pain • 5 P’s of Diagnosing Dissections • • • Pain Pallor (skin color, pale) Pulselessness Parasthesia (skin numbness or tingling) Paralysis
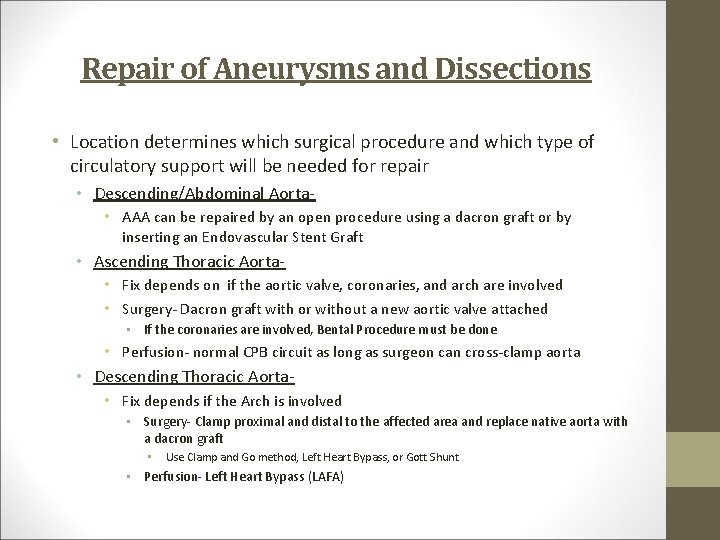
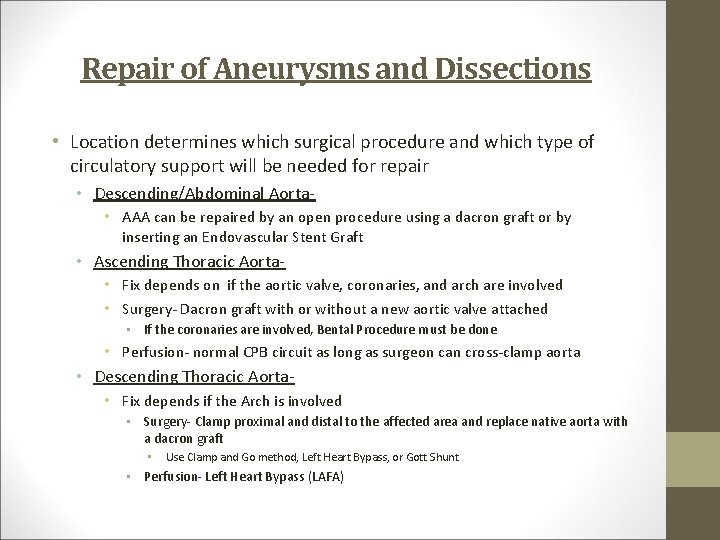
Repair of Aneurysms and Dissections • Location determines which surgical procedure and which type of circulatory support will be needed for repair • Descending/Abdominal Aorta • AAA can be repaired by an open procedure using a dacron graft or by inserting an Endovascular Stent Graft • Ascending Thoracic Aorta • Fix depends on if the aortic valve, coronaries, and arch are involved • Surgery- Dacron graft with or without a new aortic valve attached • If the coronaries are involved, Bental Procedure must be done • Perfusion- normal CPB circuit as long as surgeon can cross-clamp aorta • Descending Thoracic Aorta • Fix depends if the Arch is involved • Surgery- Clamp proximal and distal to the affected area and replace native aorta with a dacron graft • Use Clamp and Go method, Left Heart Bypass, or Gott Shunt • Perfusion- Left Heart Bypass (LAFA)
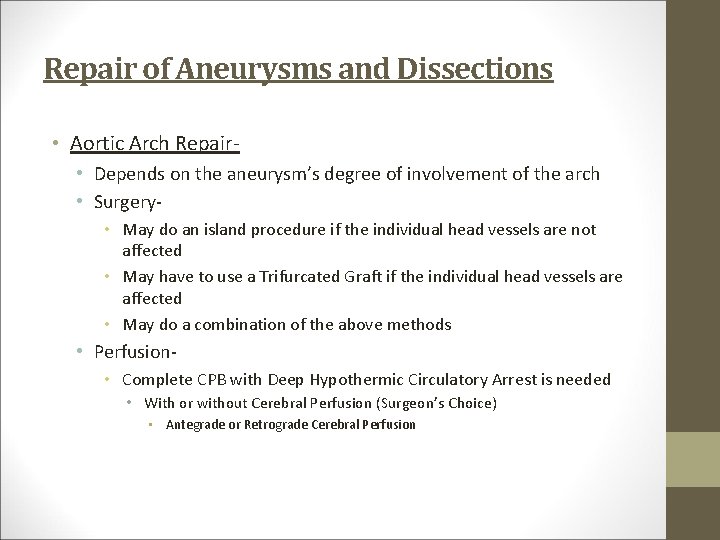
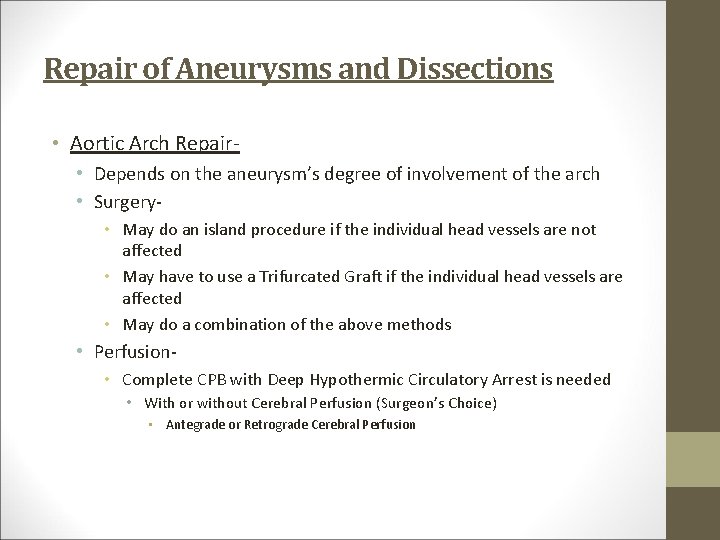
Repair of Aneurysms and Dissections • Aortic Arch Repair • Depends on the aneurysm’s degree of involvement of the arch • Surgery • May do an island procedure if the individual head vessels are not affected • May have to use a Trifurcated Graft if the individual head vessels are affected • May do a combination of the above methods • Perfusion • Complete CPB with Deep Hypothermic Circulatory Arrest is needed • With or without Cerebral Perfusion (Surgeon’s Choice) • Antegrade or Retrograde Cerebral Perfusion
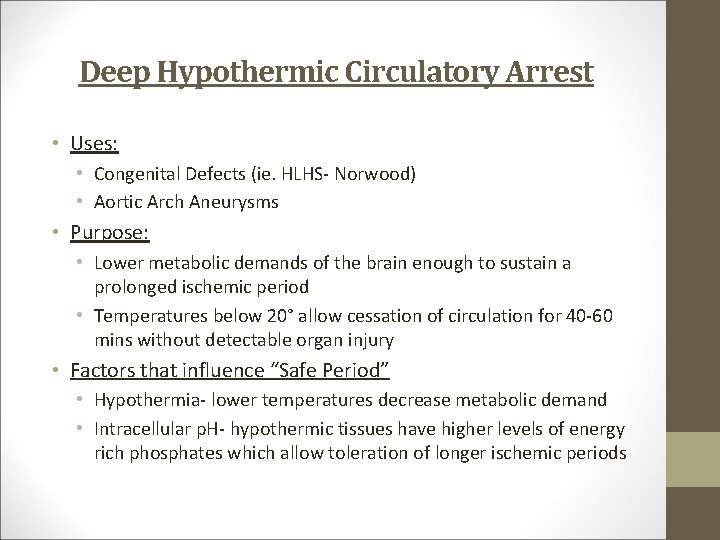
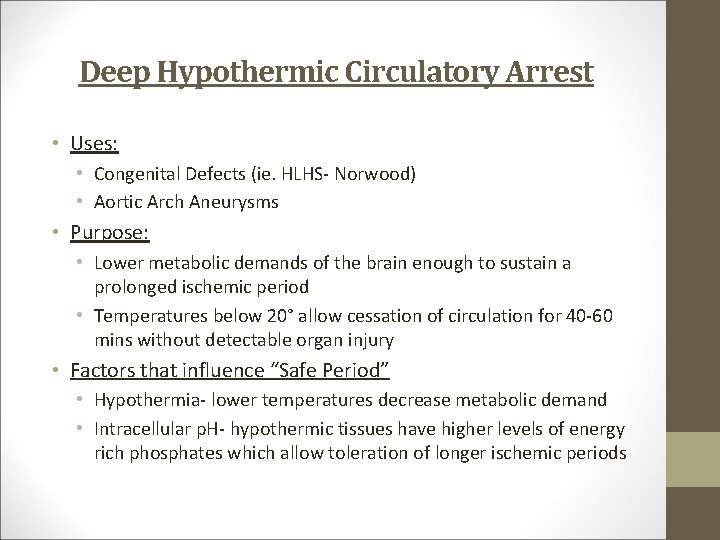
Deep Hypothermic Circulatory Arrest • Uses: • Congenital Defects (ie. HLHS- Norwood) • Aortic Arch Aneurysms • Purpose: • Lower metabolic demands of the brain enough to sustain a prolonged ischemic period • Temperatures below 20° allow cessation of circulation for 40 -60 mins without detectable organ injury • Factors that influence “Safe Period” • Hypothermia- lower temperatures decrease metabolic demand • Intracellular p. H- hypothermic tissues have higher levels of energy rich phosphates which allow toleration of longer ischemic periods
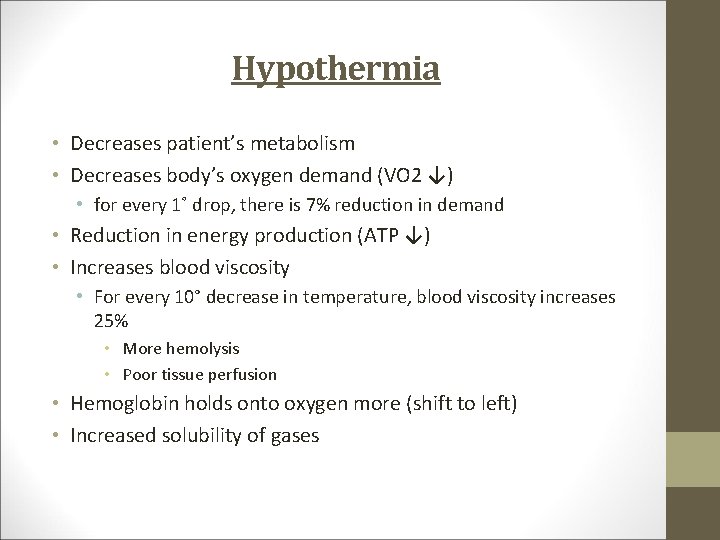
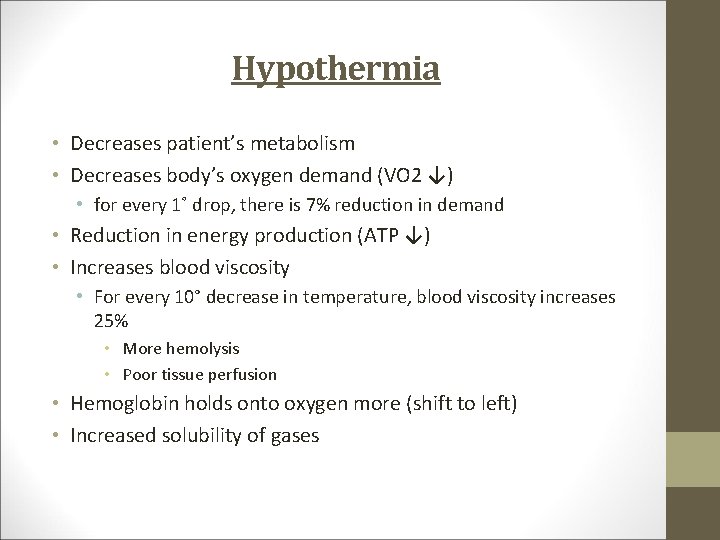
Hypothermia • Decreases patient’s metabolism • Decreases body’s oxygen demand (VO 2 ↓) • for every 1˚ drop, there is 7% reduction in demand • Reduction in energy production (ATP ↓) • Increases blood viscosity • For every 10° decrease in temperature, blood viscosity increases 25% • More hemolysis • Poor tissue perfusion • Hemoglobin holds onto oxygen more (shift to left) • Increased solubility of gases
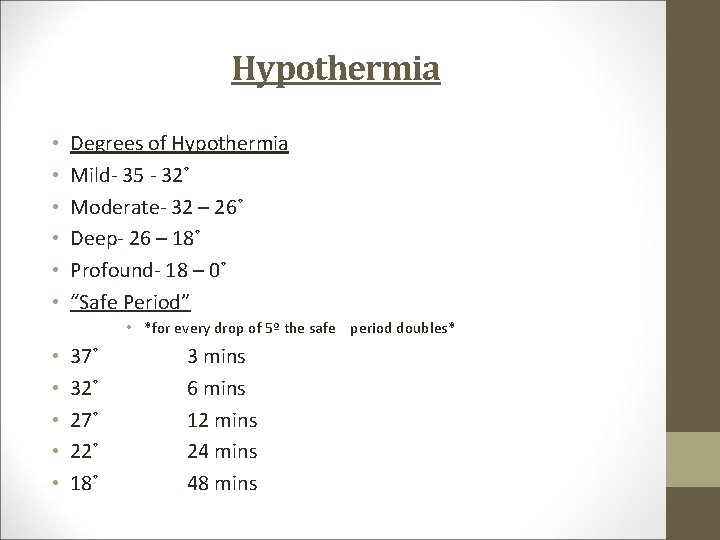
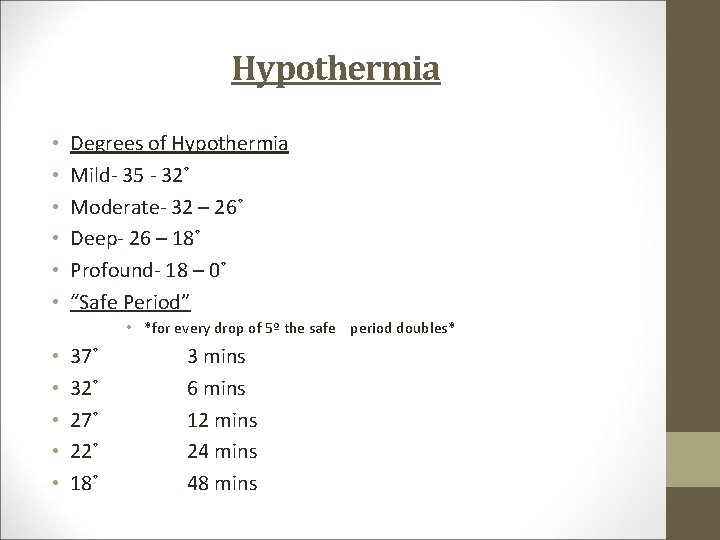
Hypothermia • • • Degrees of Hypothermia Mild- 35 - 32˚ Moderate- 32 – 26˚ Deep- 26 – 18˚ Profound- 18 – 0˚ “Safe Period” • *for every drop of 5º the safe period doubles* • • • 37˚ 32˚ 27˚ 22˚ 18˚ 3 mins 6 mins 12 mins 24 mins 48 mins
Hypothermia and Cerebral Blood Flow • During hypothermia, less cerebral oxygen consumption takes place so less cerebral blood flow is acceptable • CBF decreases linearly as temp drops • CMRO 2 (cerebral metabolic rate of O 2) decreases exponentially as temp reach deep hypothermic temperatures • Normothermia CBF: CMRO 2 = 20: 1 • Deep Hypothermia CBF: CMRO 2 = 75: 1 • CBF of 10 cc/kg/min is acceptable flow
Cooling • Rate of Cooling- wide gradiants between body and perfusate temperature correlate with cell necrosis • We do not use any specific guidelines for cooling, we cool down fast, and warm up slow • Brain Temperature Monitoring Sites • Nasopharyngeal- most used • Tympanic • EEG (Electroencephalographic) Monitoring • Used to determine cessation of brain activity which determines the ideal endpoint of the cooling process • No peripheral body temperature will consistently predict this point • If no EEG is available, cooling for at least 25 -40 minutes to a temp of 1820° is ideal • ~25° if using Antegrade/Retrograde Cerebral Perfusion • Surgeon dependant • Once desired end-point temperature is reached, pump is turned off, cannula removed, and systemic circulation ceases
Monitoring during Circ. Arrest • Cerebral ice-packs are optional, not often used. • Cerebral Oximetry measurements are recommended. • Continuous Pump Sv. O 2 measurements is considered a perfusion standard with DHCA • EEG, optional • BIS • Core Temperature • Brain Temperature- Nasopharyngeal • Arterial Temperature • Venous Temperature
CPB Circ Arrest Timeline • Routine cardiopulmonary bypass is established with or without Bicaval cannulation. • Cooling is initiated to reach desired end-point cooling temp. , ~25° for Dr. Bowen due to him using ACP • If we are able to apply Cross-Clamp: • Cardioplegia is given every 15 -20 min or when activity is noted until endpoint cooling temp. is reached, usally a dose of plegia will be given right before circ. arrest • Deliberate hemodilution should be used to reduce the hematocrit to match the end-point cooling temp. to prevent sludging in the cerebral microcirculation. • Ie. Cooling temp = 25°, HCT = <25 • When temperatures are reached or we notice cessation of brain activity, circ. Arrest drugs are added • 1 g Methylprednisone, 20 -40 mg Lasix, 25 g Mannitol, 2 g Magnesium • Sodium Pentothal used to be given by anesthesia, now they will give Fentanyl or let us give it
CPB Circ Arrest Timeline • Once drugs have recirculated, the surgeon will give the command to “Circ. Arrest” or “Pump Off” • Arterial line clamped, and controlled exsanguination is allowed via the venous line. • Send excess volume up to your spike bags and venous sequester bag • Leave your venous line unclamped to allow drainage throughout the circ. Arrest period, especially if you are using ACP • Start your Circ. Arrest clock to keep track of ischemic time • At this point, you will begin your cerebral perfusion, usually by ACP using the 18/20 fr. Optisite cannula sitting in the Innominate Artery • He will snare the proximal part of the Innominate Artery preventing your flow from reaching the systemic circulation, forcing blood into the Right Common Carotid Artery and Right Subclavian, he may snare the sublcavian as well • He will say to start ACP or “Flow to the brain” • Reduce RPMs to about 1500 and open arterial line clamp, come up to flow slowly • He wants flow of 10 cc/kg/min usually coming out to be 600 -1000 cc of flow • Watch your arterial line pressure and don’t let it get too high, that will dictate your flow • Watch your cerebral SATs, right should be higher, and notice if you have a Right Radial Line, you will get a BP during this time if he did not snare the subclavian
Circ. Arrest Timeline • You will flow ACP the entire time • He may give some doses of plegia, let him know at 20 mins or so • Once he is done his distal anastomosis and/or Arch work is complete, he will clamp the proximal end of the dacron graft (the new ascending aorta) and de-air the graft • He will then re-establish full bypass perfusing the entire systemic circulation by removing his Innominate snares • You will work your way up to full flow, dropping the volume that you sequestered as needed and start to warm watching your temp. gradients • You will give a dose of plegia, take a blood gas and treat any issues, usually some acidosis
Circ. Arrest Timeline • From this point on it is a normal case, giving plegia every 1520 minutes and warming • Once his proximal anastamosis is complete, he will ask you to “Fill the root” at which point you will turn on your ANTEGRADE cardioplegia and run it very hard to pressure the new root • He is doing this to de-air his graft and test the suture lines • At this point he can take off the cross-clamp if he wishes, which he will do even if you are still cold • Proceed from here as if it were a normal case • Ask if he wants blood products which he usually will • These cases bleed a lot due to all of the suture lines • Usually order 2 Platelets, 4 FFP, 20 Cryo
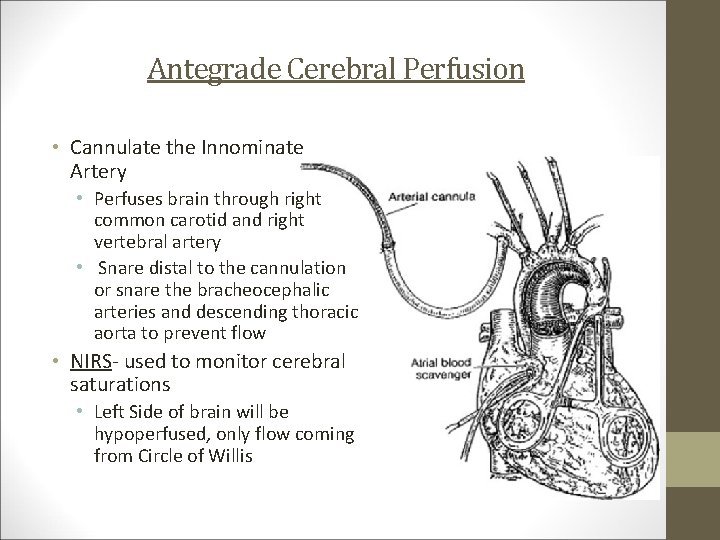
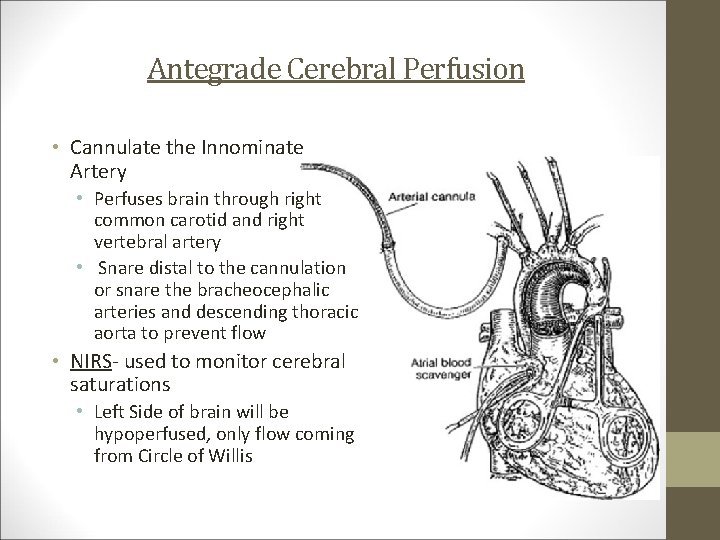
Antegrade Cerebral Perfusion • Cannulate the Innominate Artery • Perfuses brain through right common carotid and right vertebral artery • Snare distal to the cannulation or snare the bracheocephalic arteries and descending thoracic aorta to prevent flow • NIRS- used to monitor cerebral saturations • Left Side of brain will be hypoperfused, only flow coming from Circle of Willis
Retrograde Cerebral Perfusion • Started as a treatment for massive air embolism • Can extend safe periods up to 60 minutes • Washes out metabolic waste products, embolic debris, air bubbles and delivery of O 2 and nutrients to the ischemic brain during HCA • Optimal pressure for RCP is 20 -25 mm Hg • Flows of 10 -30 cc/kg/min • Infusion temperature should match the desired core temperature • Cannula placed in SVC and blood return from aortic root is retrieved by suckers
Left Heart Bypass • Uses: • Descending Thoracic Aneurysms/Dissections • Thoracoabdominal Aneurysms/Dissections • Goal: • To perfuse the body distal to the clamp placed near the aneurysm/dissection • Circuit: • • • Inflow and Outflow cannula 3/8” tubing Centrifugal Pump NO heat exchanger or oxygenator needed NO heparin needed, some places will give 100 u/kg to maintain patency of small intercostal arteries and spinal arteries • Heparin administration causes excessive bleeding around suture sites and in pre-existing traumatic locations
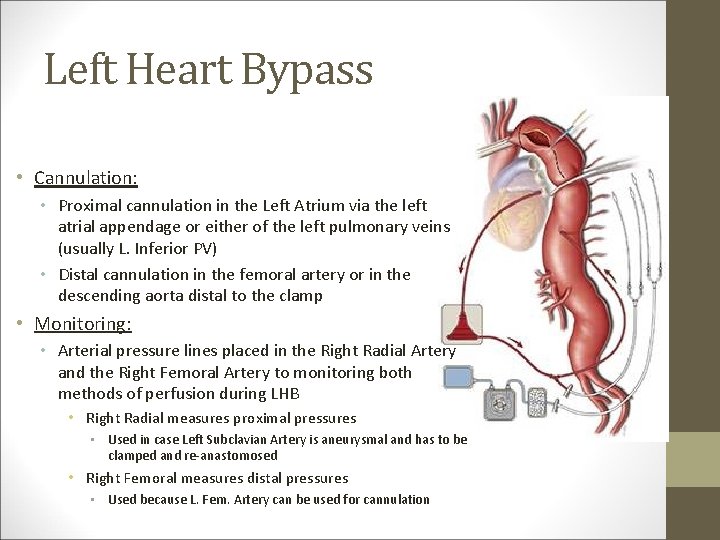
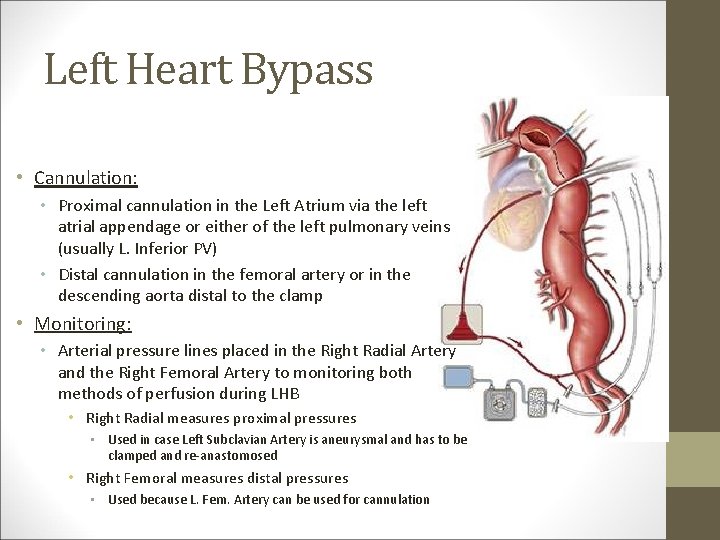
Left Heart Bypass • Cannulation: • Proximal cannulation in the Left Atrium via the left atrial appendage or either of the left pulmonary veins (usually L. Inferior PV) • Distal cannulation in the femoral artery or in the descending aorta distal to the clamp • Monitoring: • Arterial pressure lines placed in the Right Radial Artery and the Right Femoral Artery to monitoring both methods of perfusion during LHB • Right Radial measures proximal pressures • Used in case Left Subclavian Artery is aneurysmal and has to be clamped and re-anastomosed • Right Femoral measures distal pressures • Used because L. Fem. Artery can be used for cannulation
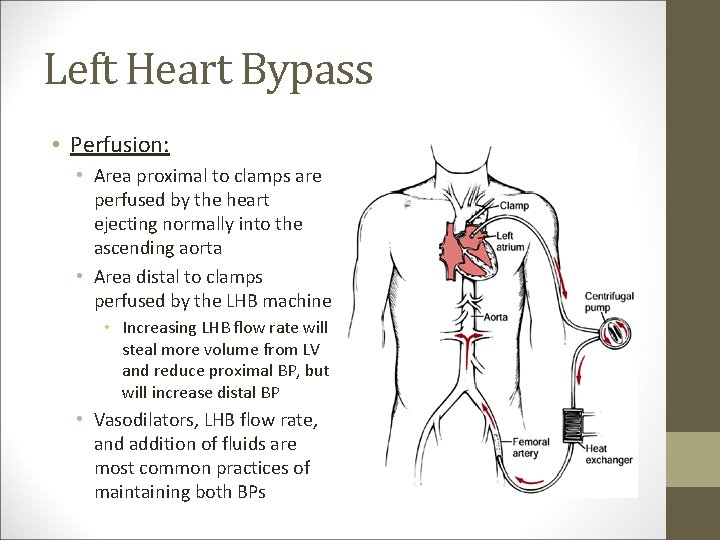
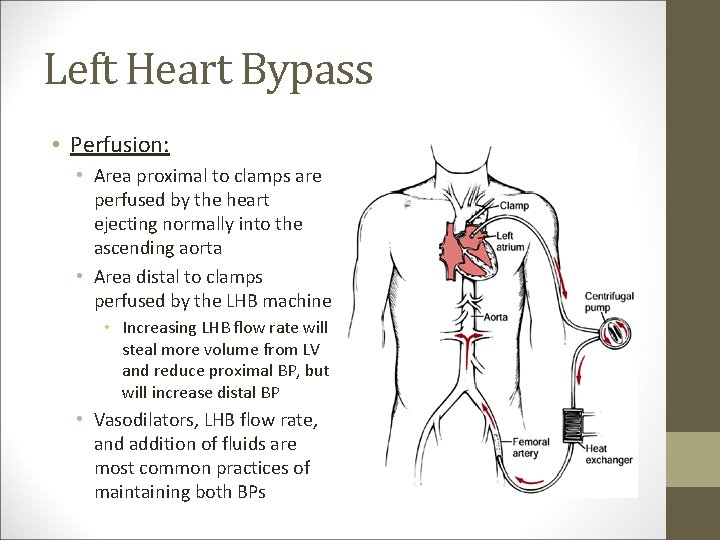
Left Heart Bypass • Perfusion: • Area proximal to clamps are perfused by the heart ejecting normally into the ascending aorta • Area distal to clamps perfused by the LHB machine • Increasing LHB flow rate will steal more volume from LV and reduce proximal BP, but will increase distal BP • Vasodilators, LHB flow rate, and addition of fluids are most common practices of maintaining both BPs