Chronic Scapulothoracic Pain or Chronic Shoulder Pain Steve

- Slides: 43
Chronic Scapulothoracic Pain or Chronic Shoulder Pain Steve Moll, DO Senior Medical Officer USS SAIPAN (LHA-2)
Chronic Scapulothoracic Pain At the conclusion of this activity, you should: Appreciate the degree to which myofascial pain syndromes from the scapulothoracic region cause shoulder pain. Understand the importance of treating predisposing factors in myofascial pain syndromes. Know that successful treatment requires a multifactorial approach.
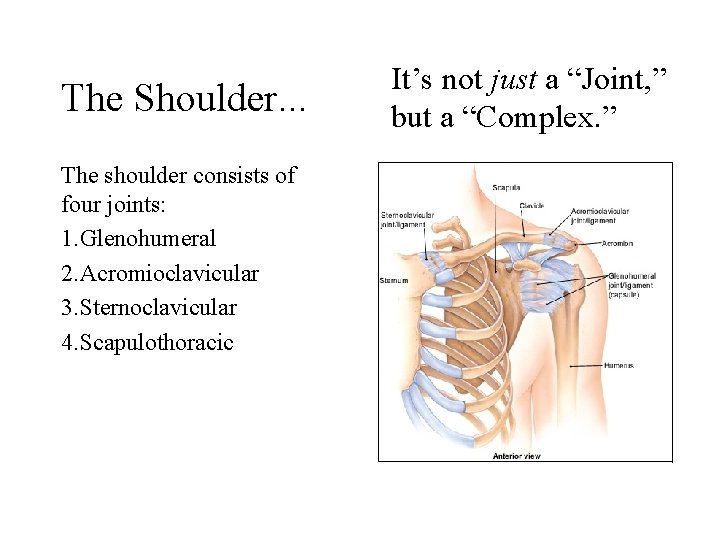
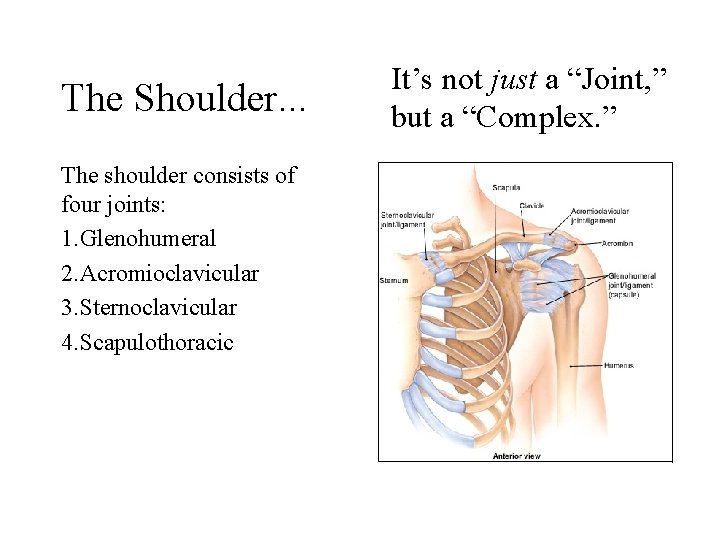
The Shoulder. . . The shoulder consists of four joints: 1. Glenohumeral 2. Acromioclavicular 3. Sternoclavicular 4. Scapulothoracic It’s not just a “Joint, ” but a “Complex. ”
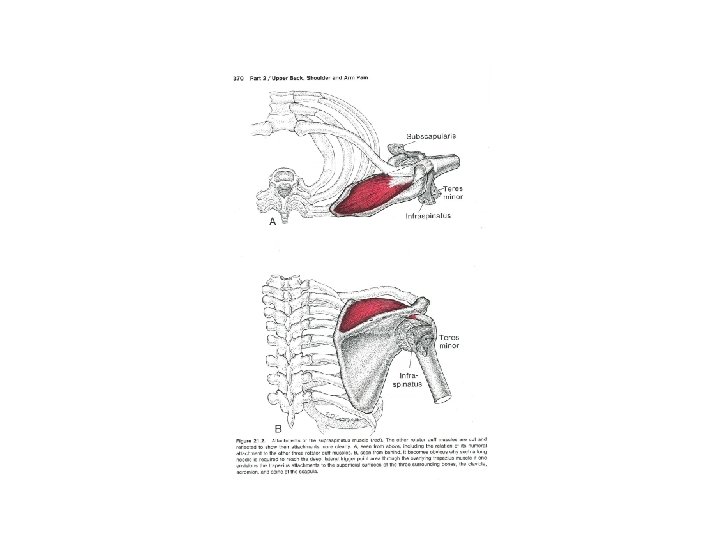
Differential Diagnosis Shoulder pain arising from problems: • Intrinsic to the A-C / glenohumeral joints, or • Extrinsic “ “ (“referred pain” patterns) – Somatic – Visceral
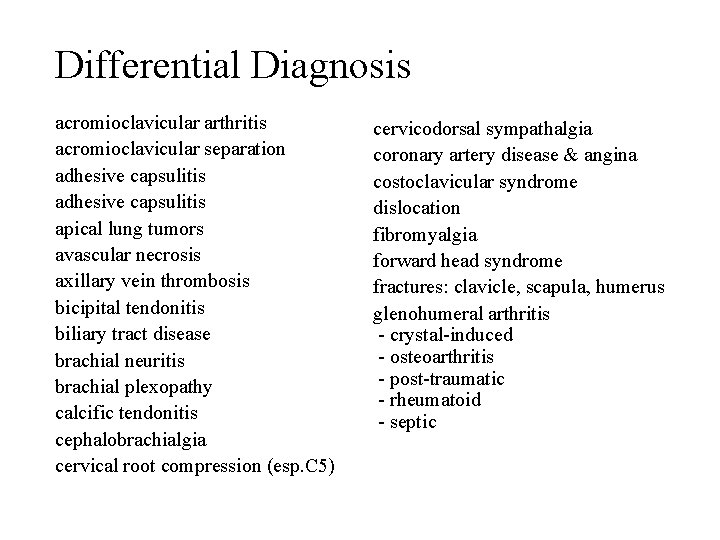
Differential Diagnosis acromioclavicular arthritis acromioclavicular separation adhesive capsulitis apical lung tumors avascular necrosis axillary vein thrombosis bicipital tendonitis biliary tract disease brachial neuritis brachial plexopathy calcific tendonitis cephalobrachialgia cervical root compression (esp. C 5) cervicodorsal sympathalgia coronary artery disease & angina costoclavicular syndrome dislocation fibromyalgia forward head syndrome fractures: clavicle, scapula, humerus glenohumeral arthritis - crystal-induced - osteoarthritis - post-traumatic - rheumatoid - septic
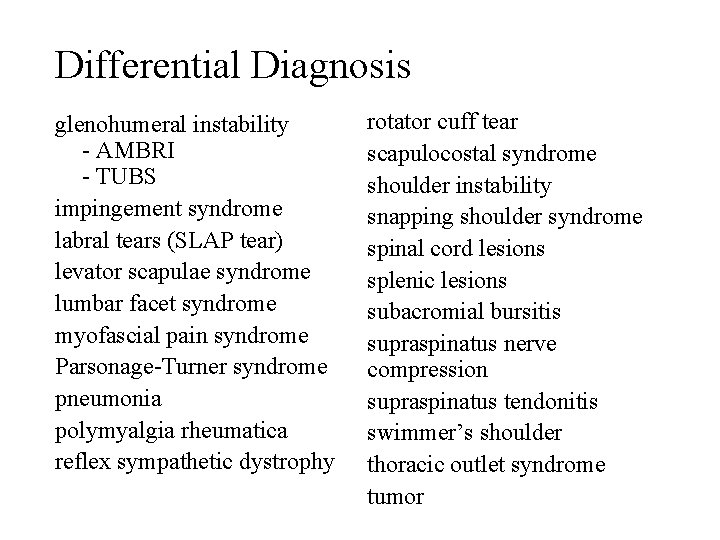
Differential Diagnosis glenohumeral instability - AMBRI - TUBS impingement syndrome labral tears (SLAP tear) levator scapulae syndrome lumbar facet syndrome myofascial pain syndrome Parsonage-Turner syndrome pneumonia polymyalgia rheumatica reflex sympathetic dystrophy rotator cuff tear scapulocostal syndrome shoulder instability snapping shoulder syndrome spinal cord lesions splenic lesions subacromial bursitis supraspinatus nerve compression supraspinatus tendonitis swimmer’s shoulder thoracic outlet syndrome tumor

History & Physical Exam
History What’s new or different in the 6 months prior to the onset of pain?
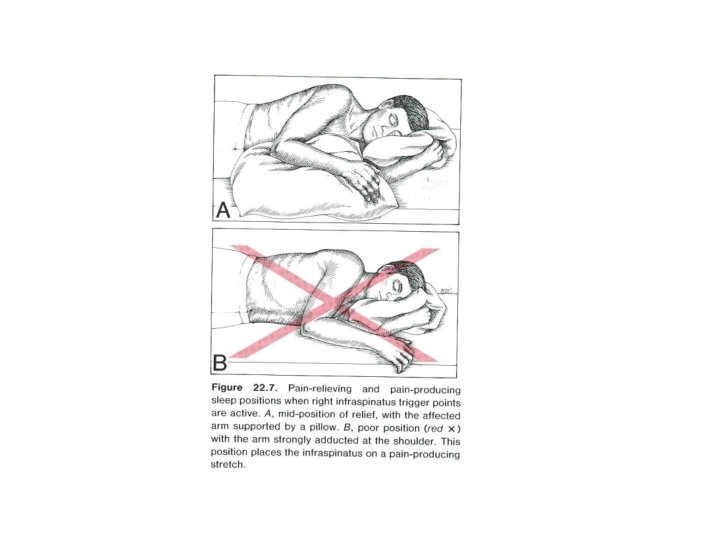
History What’s new or different in the 6 months prior to the onset of pain? - New job? Longer hours in front of the computer? - New car? Longer commute? - New duty station (shipboard)? Running shoes? - Raked leaves? - More stress? Less/poorer sleep? - Marital conflict? - Different pillow? - Pregnancy?
History What occupies the majority of your day? How much time do you spend - sitting? - talking on the phone? - driving? , or - being ‘driven nuts’?
History • Is there a time of the day when your is pain better? Worse? • How well do you sleep?
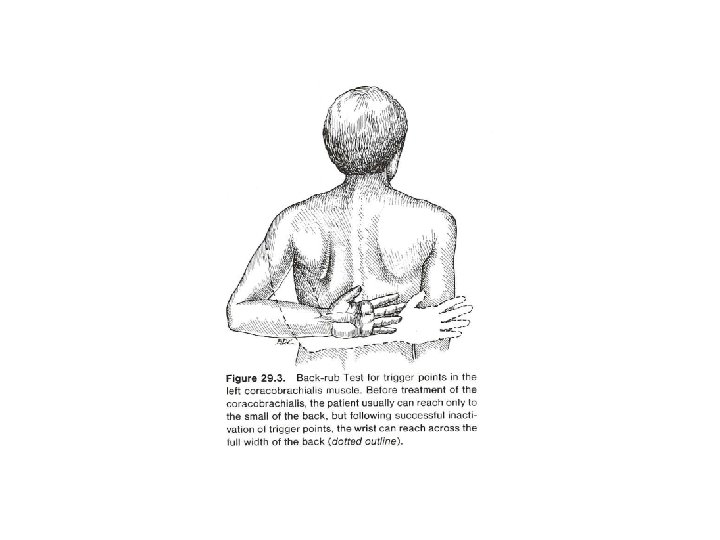
Physical Exam - ROM (active & passive) - Strength - Special tests (lift off; Neer; Hawkins; cross -body adduction; “empty can”)
Physical Exam - ROM (active & passive) - Strength - Special tests (e. g. lift off; Neer; Hawkins; cross-body adduction; “empty can”) - Palpate - Posture
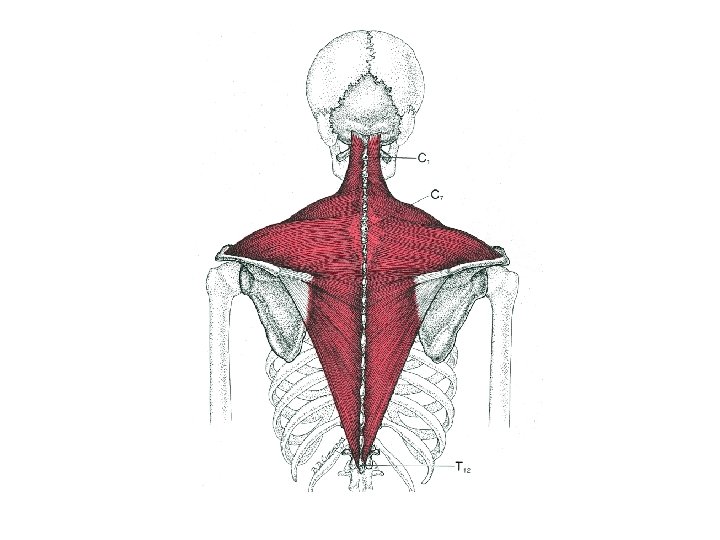
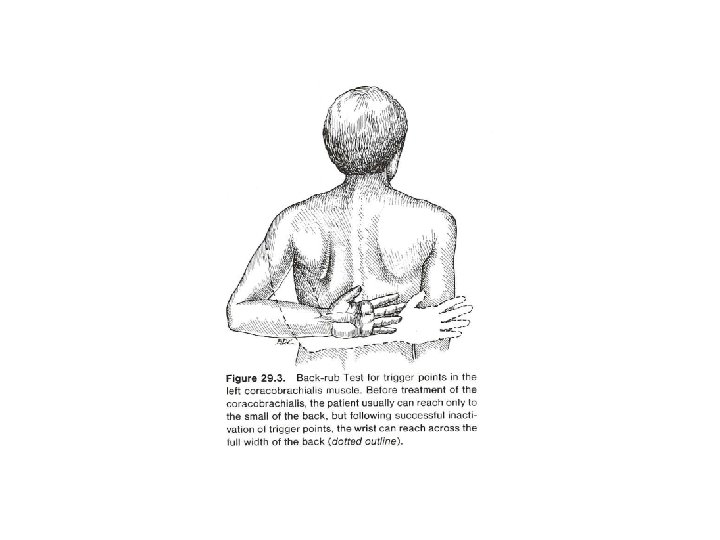
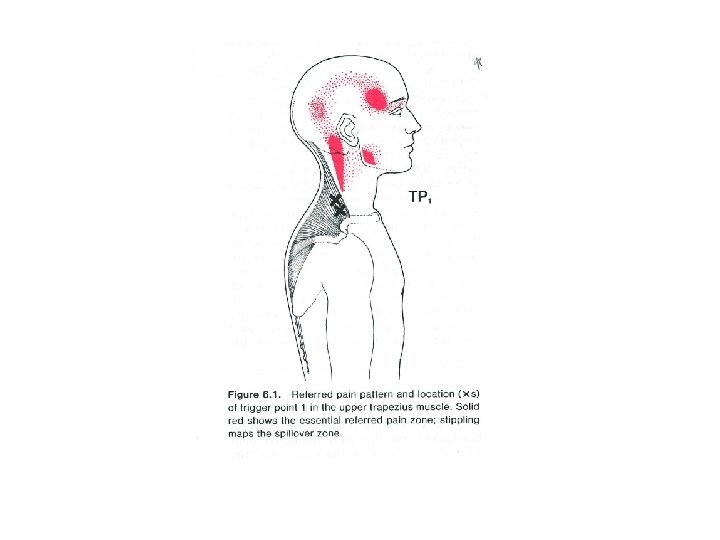
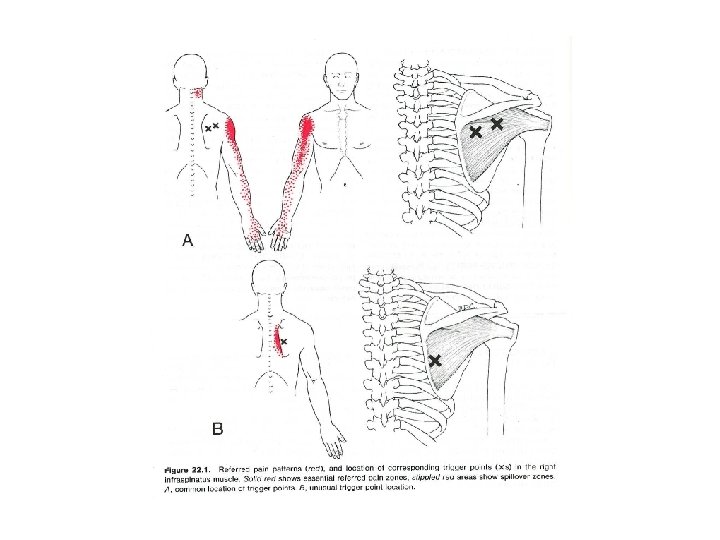
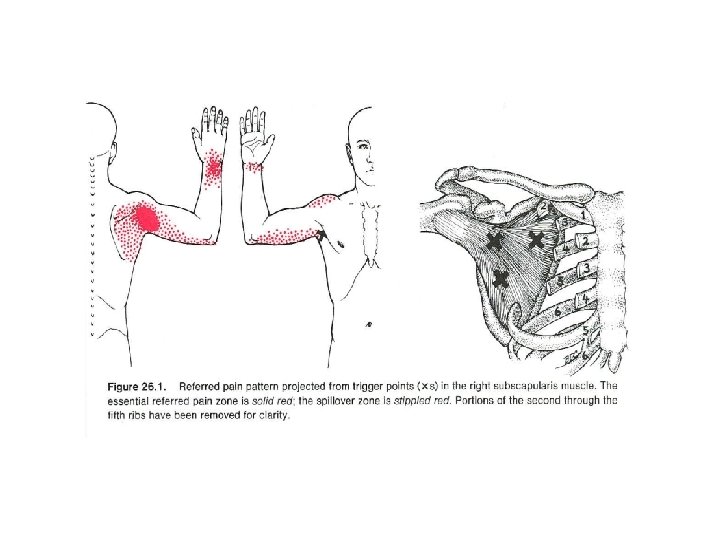
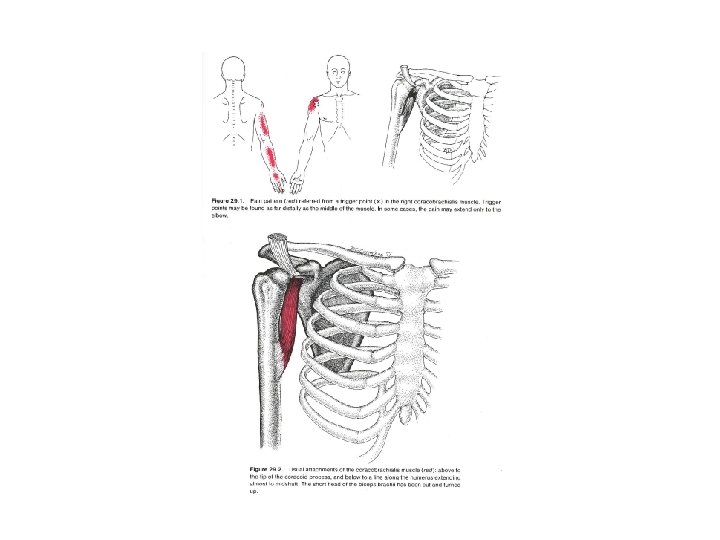
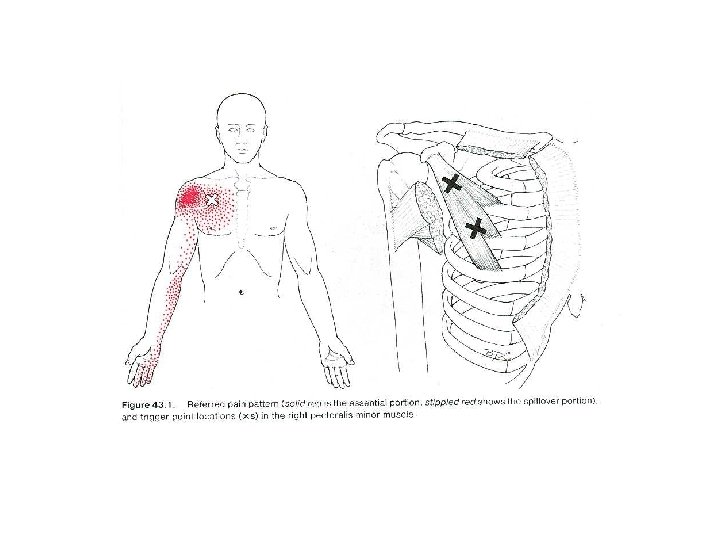
Travell Trigger Points (Tr. Ps) & Myofascial Pain Syndrome • Tr. P: "a hyperirritable spot in skeletal muscle that is associated with a hypersensitive palpable nodule in a taut band. The spot is tender when pressed and can give rise to characteristic referred pain, motor dysfunction, and autonomic phenomena. • Palpation is a reliable diagnostic criterion for locating Tr. Ps.
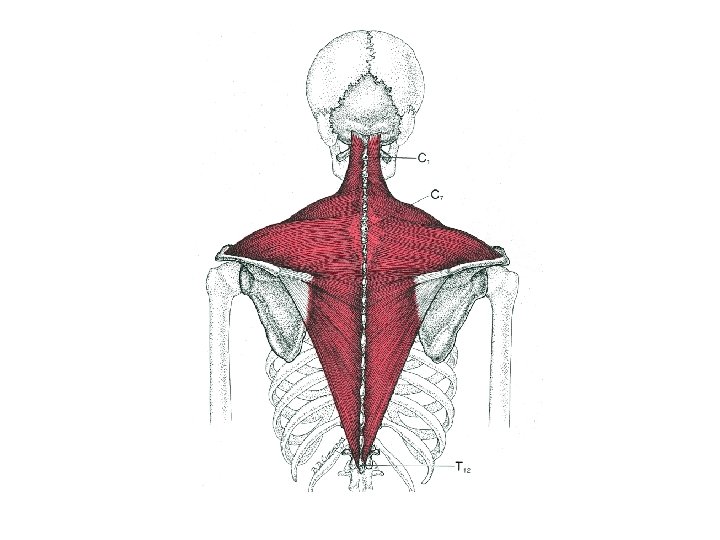
Travell Trigger Points (Tr. Ps) & Myofascial Pain Syndrome Etiology of Tr. Ps: 1. Local myofascial tissues - Motor end plate dysfunction cascade 5 - from genetic defects, or - acquired defects (nicotine, caffeine, psychological & physiological stress 2. CNS factors (central sensitization)4, 5 3. Biomechanical factors
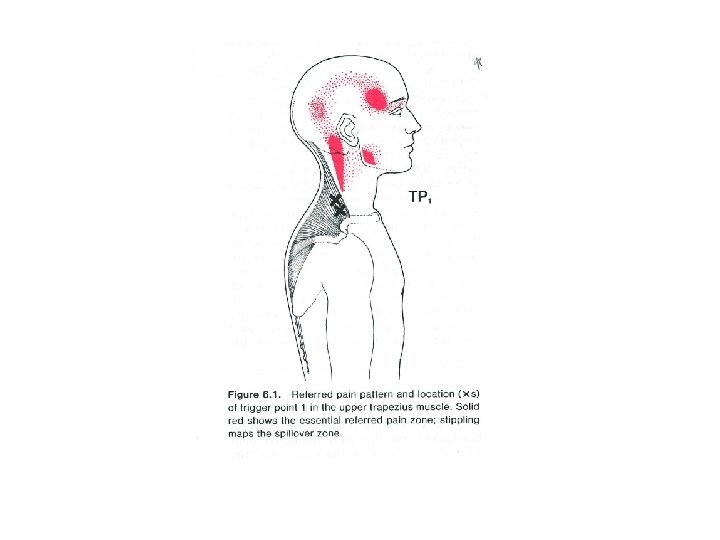
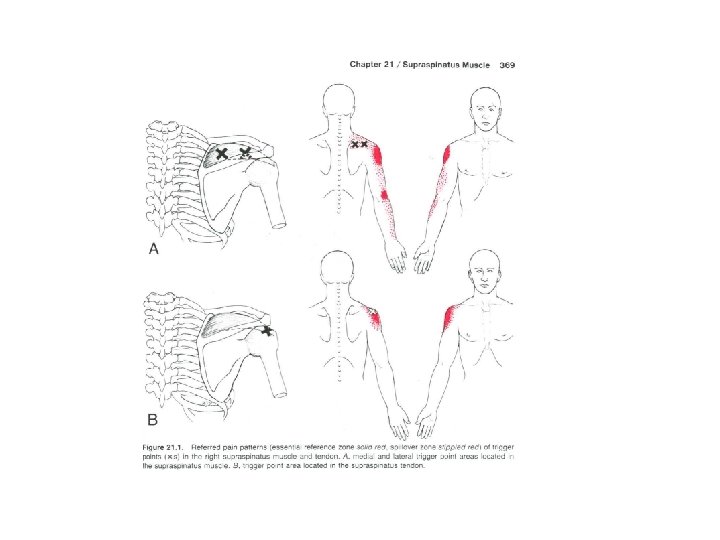
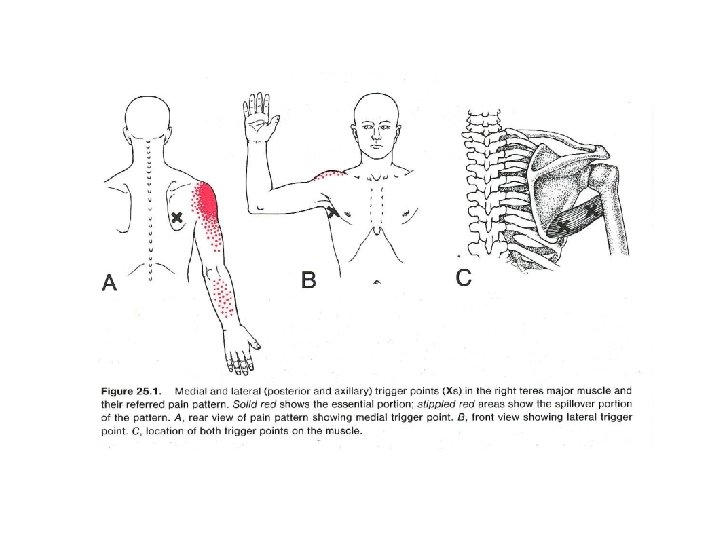
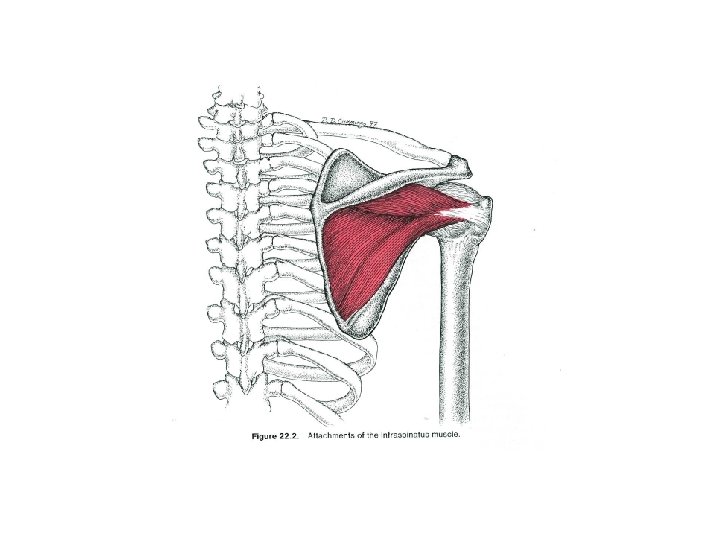
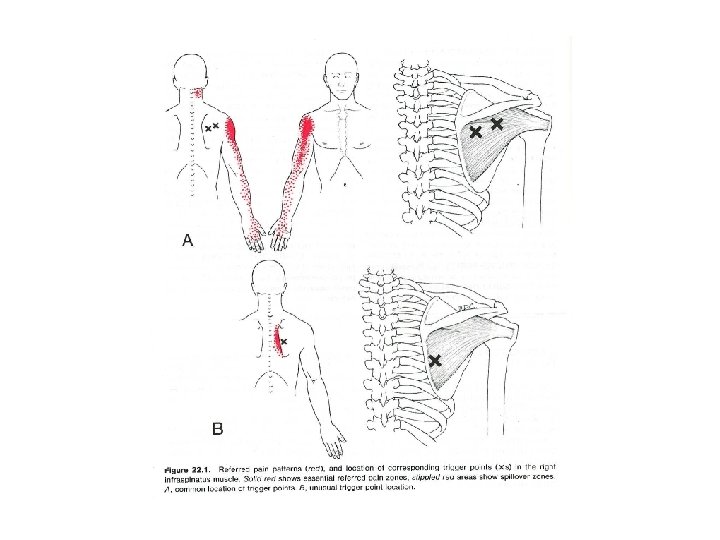
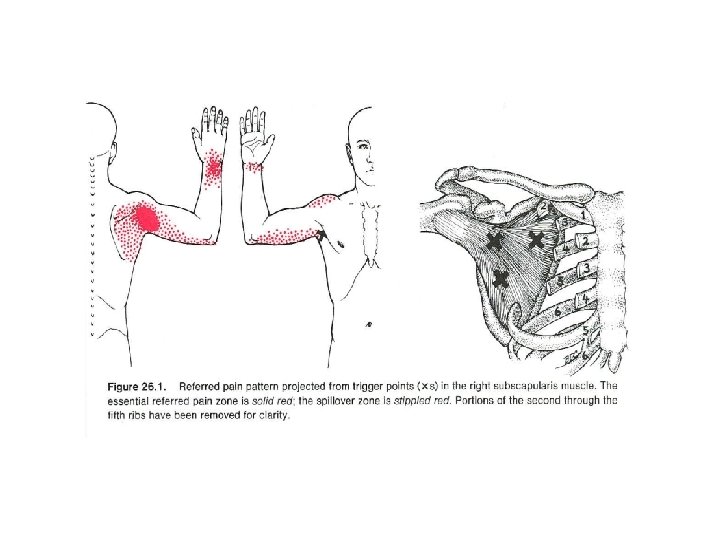
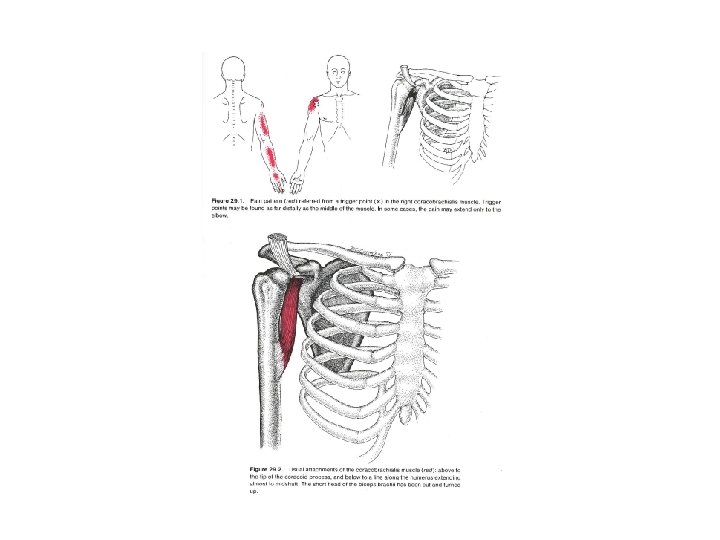
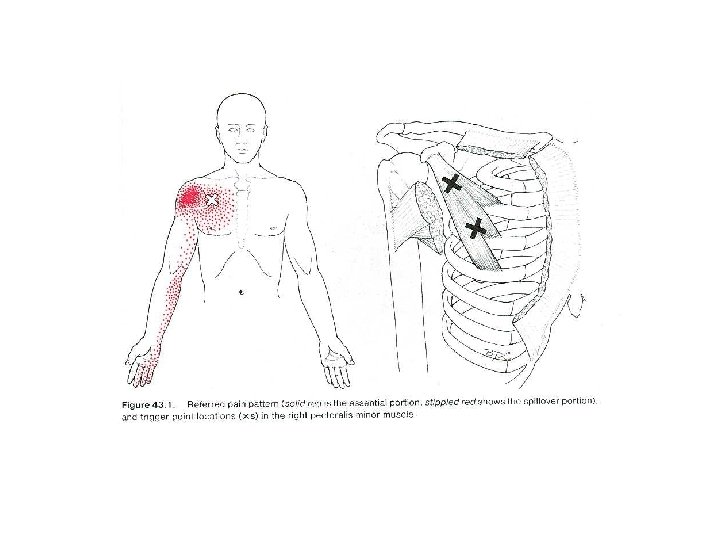
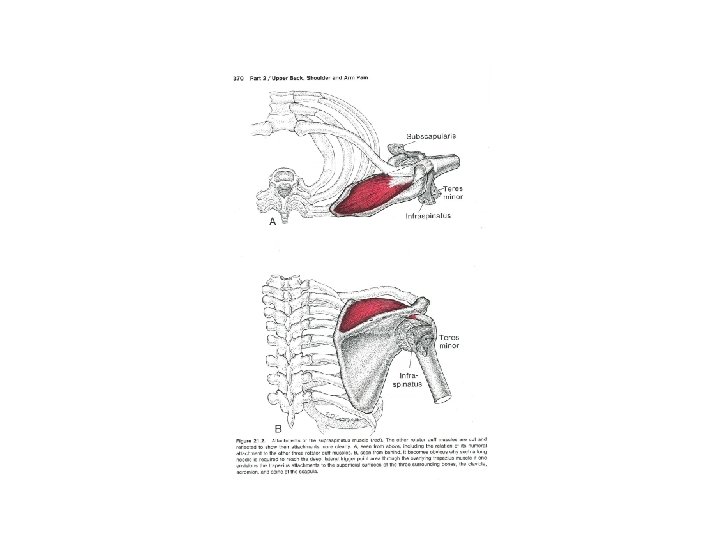
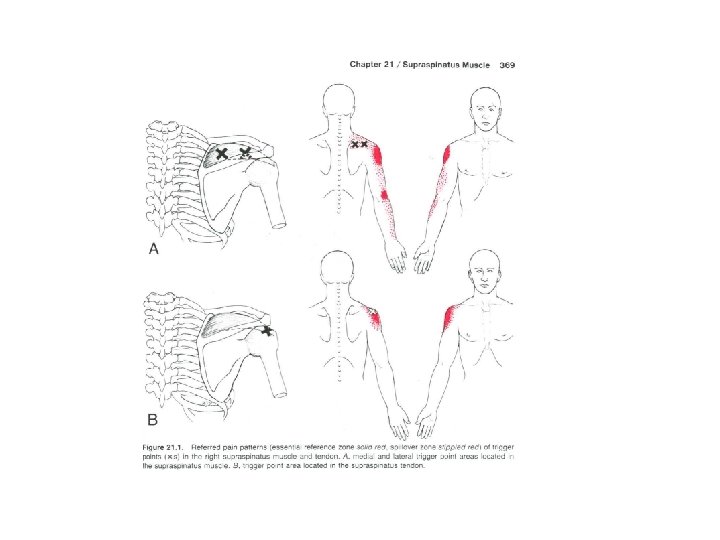
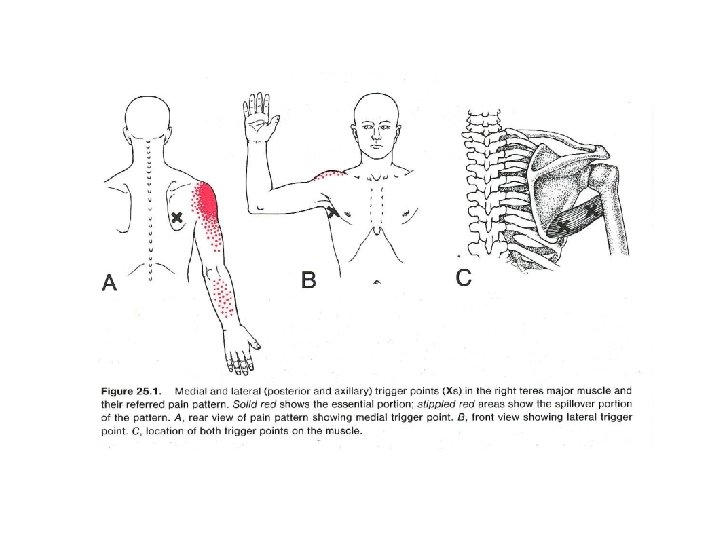
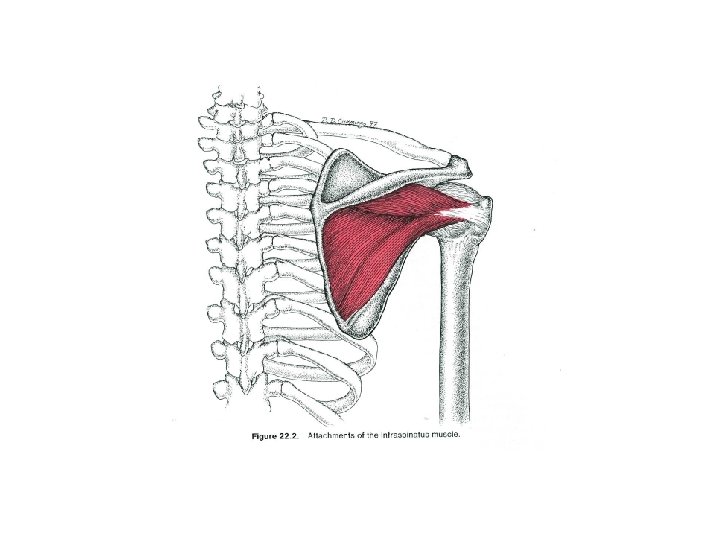
Referred pain patterns
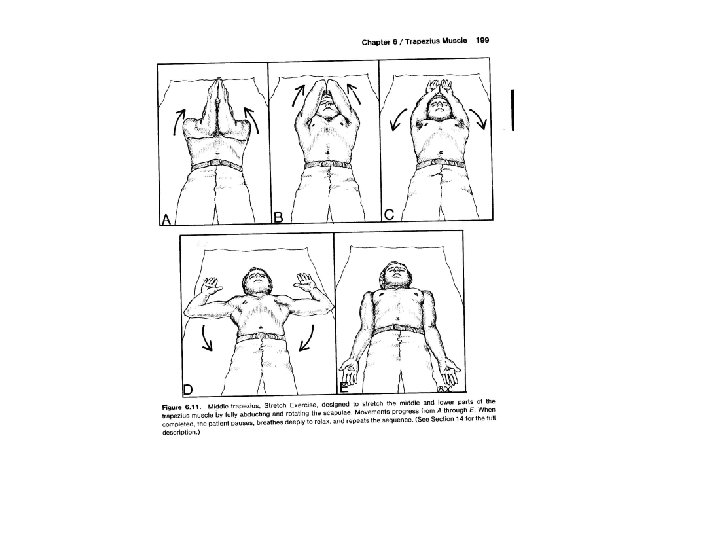
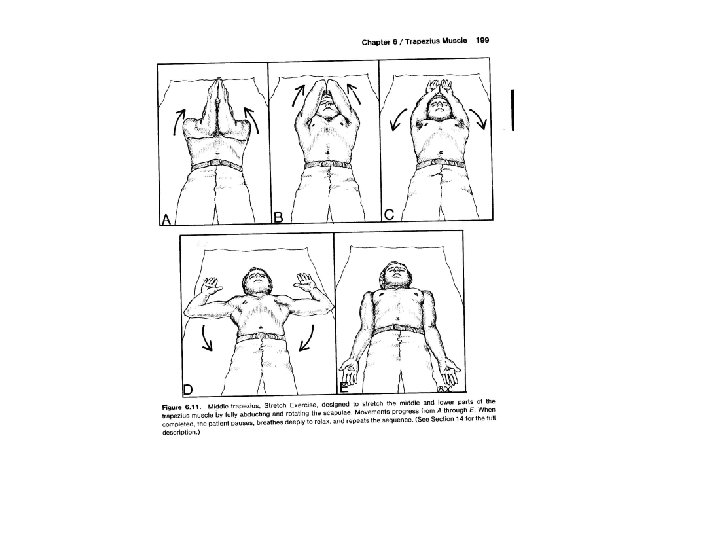
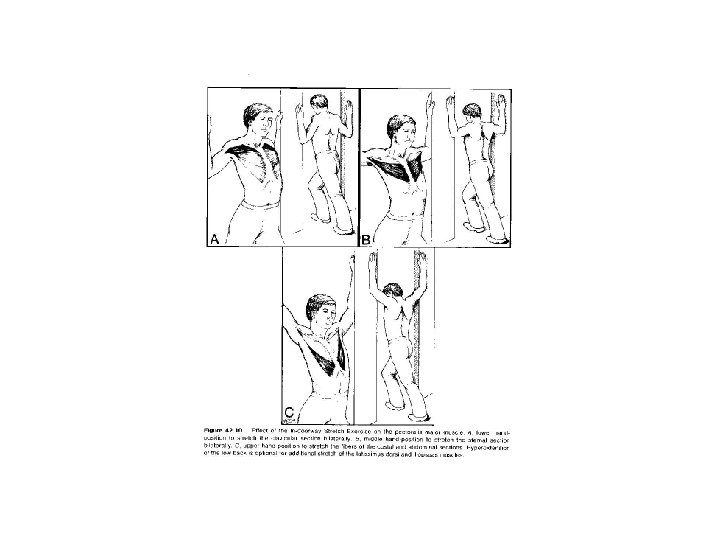
Treatment Direct Tx of TPs - pressure - injection - dry needling - massage Treatment of Perpetuating Factors
Treatment of Perpetuating Factors Postural stresses • Psychological stress • Mechanical factors • Constriction of muscles • Social habits
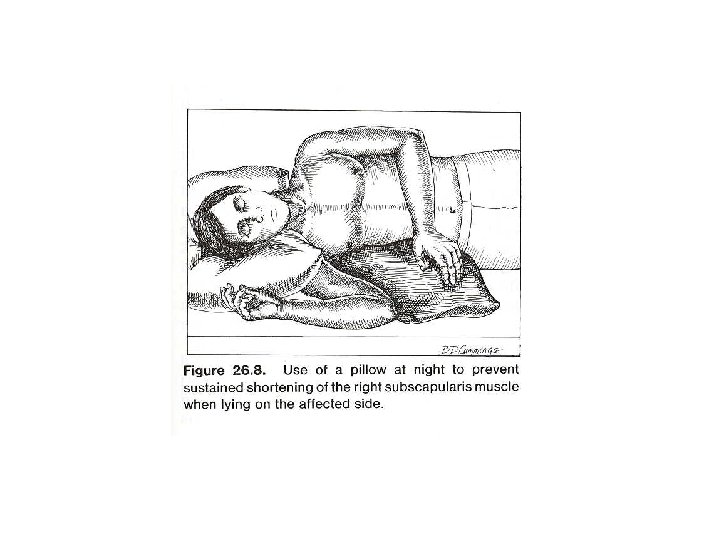
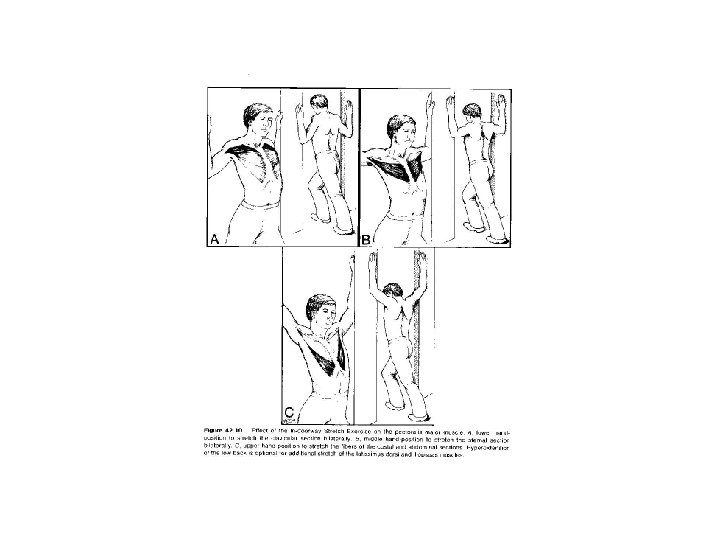
Treatment of Perpetuating Factors Postural stresses - poor posture - misfitting furniture - immobility - frequent repetitive movements
Treatment of Perpetuating Factors Psychological stress - hopelessness - depression - anxiety & tension
Treatment of Perpetuating Factors Mechanical factors - SI dysfunctions - hemipelvic disparities - limb length discrepancy - Morton's foot (long second metatarsal)
Treatment of Perpetuating Factors Social habits - nicotine - caffeine - alcohol abuse
Conclusion The Family Practice Physician is eminently qualified to successfully manage the multifactorial problems which plague the chronic pain patient.
Common Concomitants ØForward Head Syndrome ØMyofascial Pain (Scapulothoracic) Syndrome ØRotator Cuff Syndrome ØThoracic facet syndrome (somatic dysfunction)
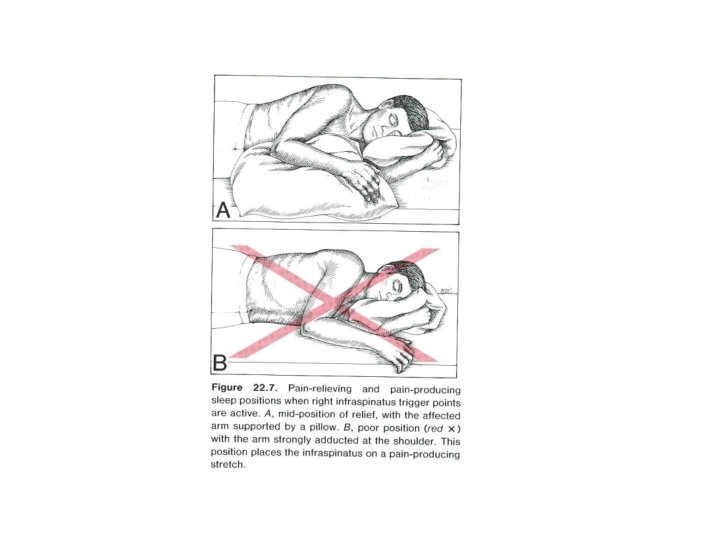
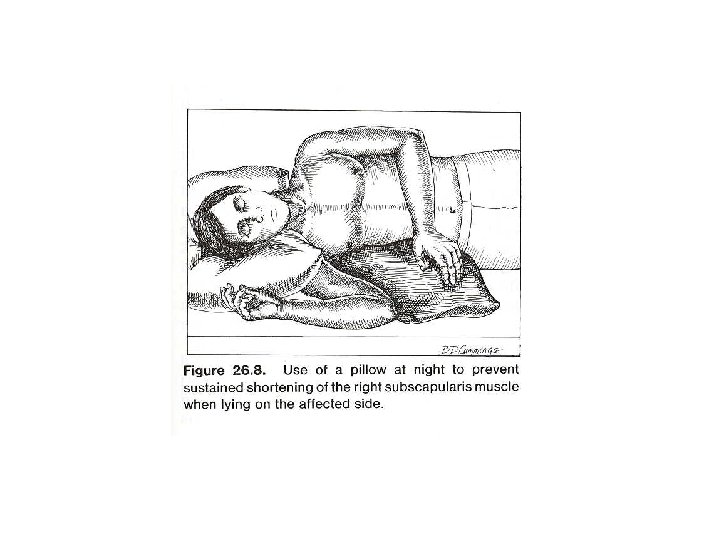
Treatment (cont’d) • Fix the SLEEP problem! No sleep. No relief. No hope. • Raise SEROTONIN levels. • Treat the depression &/or anxiety.
Treating Insomnia • R/O Obstructive Sleep Apnea • Trazodone (Desyrel) • • – Allow self-titration – Explicit verbal & written instructions – Treatment failures? … Bipolar until proven otherwise. TCAs (nortriptylene; amitriptyline) Gabapentin (Neurontin) Zolpidem (Ambien) SSRIs
Boosting Serotonin Levels • SSRIs – Start early – Escalate doses, as tolerated • “Yes… this is an ‘anti-depressant’. ” “No… I don’t think you’re depressed. ” “I am giving this to you as an adjunct…”