CHRONIC RENAL FAILURE OUTLINE INTRODUCTION DEFINITION EPIDEMIOLOGY AETIOLOGY
- Slides: 57
CHRONIC RENAL FAILURE
OUTLINE INTRODUCTION DEFINITION EPIDEMIOLOGY AETIOLOGY PATHOPHYSIOLOGY CLINICAL SIGNS/SYMPTOMS MANAGEMENT ◦ MEDICAL ◦ RENAL REPLACEMENT THERAPY
INTRODUCTION Chronic Kidney Disease or CRF encompasses all degrees of decreased in Renal function It’s a worldwide problem and there is a rising in incidence and prevalence of kidney failure with poor outcomes and high cost of management
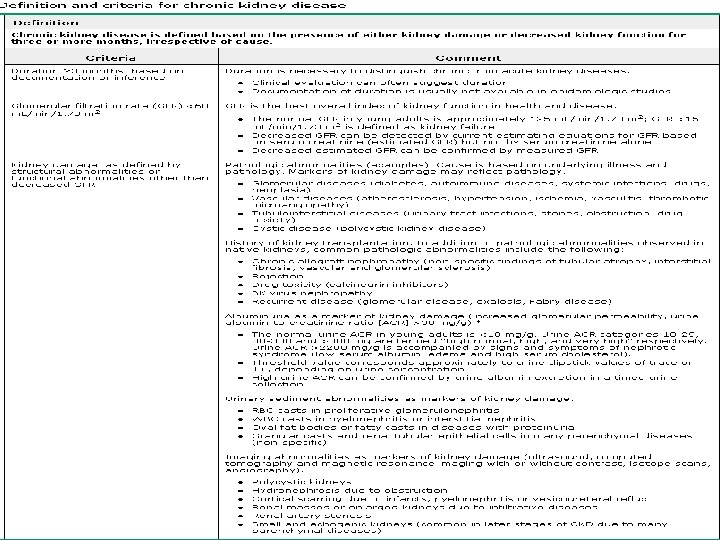
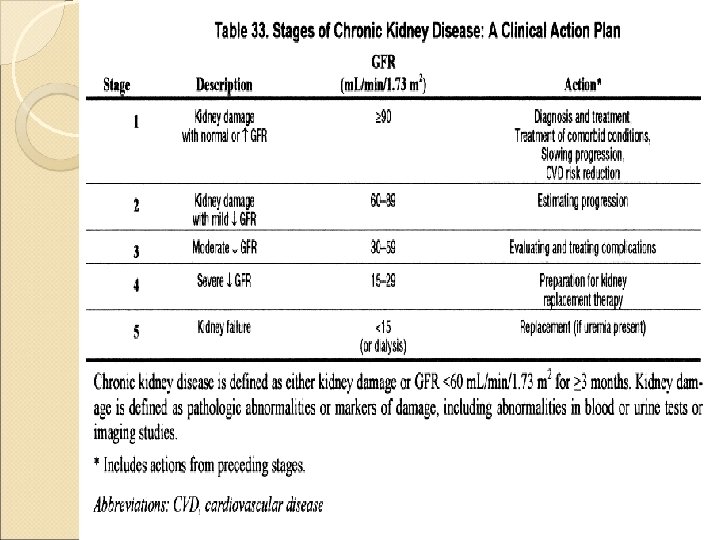
Definition 3 Criteria are involved ◦ Evidence of kidney damage or reduction in function ◦ Duration>3 months ◦ Irrespective of the aetiology
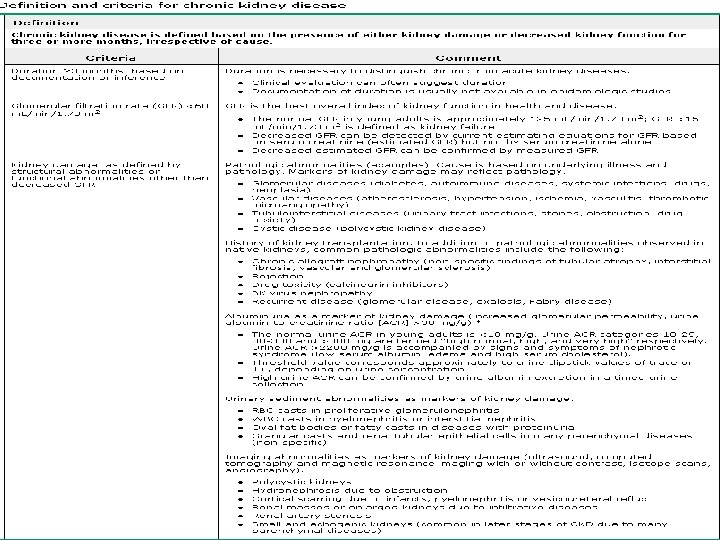
It is characterized by a progressive deterioration in renal function ultimately leading to irreversible structural damage to existing nephrons. A substantial decline in function leading to azotemia. renal
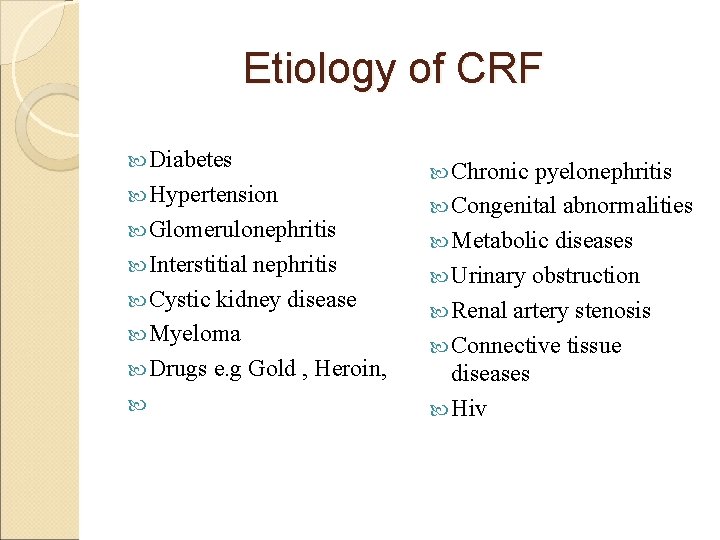
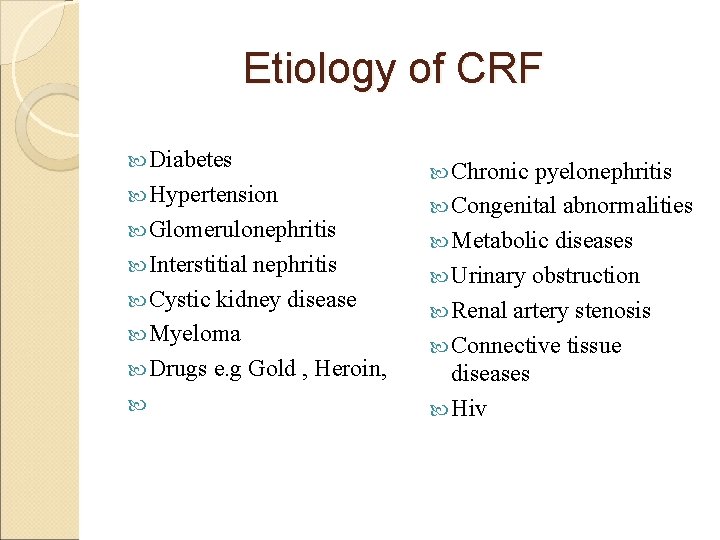
Etiology of CRF Diabetes Hypertension Glomerulonephritis Interstitial nephritis Cystic kidney disease Myeloma Drugs e. g Gold , Heroin, Chronic pyelonephritis Congenital abnormalities Metabolic diseases Urinary obstruction Renal artery stenosis Connective tissue diseases Hiv
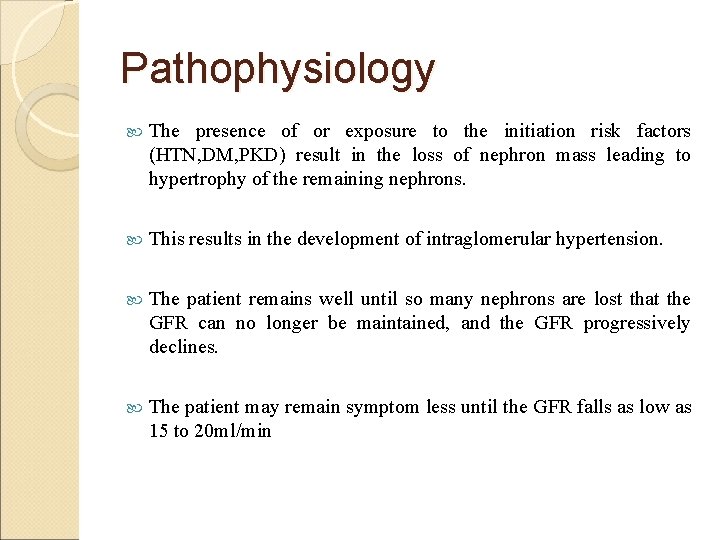
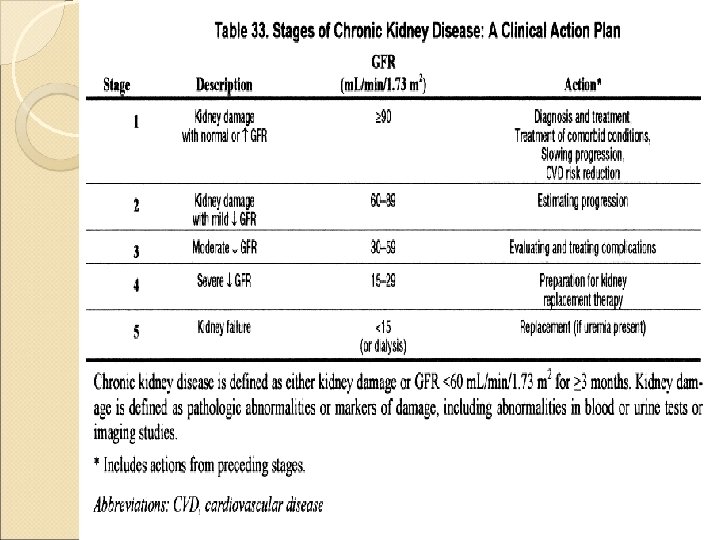
Pathophysiology The presence of or exposure to the initiation risk factors (HTN, DM, PKD) result in the loss of nephron mass leading to hypertrophy of the remaining nephrons. This results in the development of intraglomerular hypertension. The patient remains well until so many nephrons are lost that the GFR can no longer be maintained, and the GFR progressively declines. The patient may remain symptom less until the GFR falls as low as 15 to 20 ml/min
Hypertension & Diabetes Common cause of ESRD Diabetes –nephropathy Hypertension is both a cause and result of CKD HT promote renal impairment through elevated systemic pressure to glomeruli. The result is glomerular capillary hyper perfusion and hypertension leading to progressive renal damage. Glomerular Ischemia induced by damage preglomerular arteries and arterioles may also occur to
Chronic Glomerulonephritis Common cause in adults &children Idiopathic and Systemic disease Trapping of immune complexes in the glomerulus and leads to inflammatory response Responsible antigens include certain strains of Streptococci, malaria, endogenous antigens (neoplastic lesions), SLE and drugs
Chronic Glomerulonephritis Proteinuria Haematuria Oliguria edema Hypertension High Proteinuria is referred to as nephrotic syndrome, which is characterized by: 1. Pitting edema 2. Proteinuria > 3. 5 gm/day 3. Hypoalbuminaemia
Interstitial Nephritis Inflammation of the interstitium of the kidney Drugs and toxins Nocturia Anemia Renal osteodystrophy
Polycystic Kidney Disease Characterized by many bilateral renal cysts that increase renal size but reduce functioning of renal tissue PKD is of three types 1. Autosomal dominant (adult) PKD 2. Autosomal recessive Childhood PKD 3. Congenital Polycystic kidney disease
Chronic Pyelonephritis Chronic inflammation of the renal parenchyma with scarring of the kidney. Recurrent urine infection. Important cause of kidney destruction in children with severe lower urinary tract infections
Urinary Obstruction This may be sudden or insidious, partial or complete, unilateral or bilateral. Symptoms –oliguria and pain Causes include: Prostate hypertrophy Renal calculi (stone Vesicoureteric reflux formation) indwelling urinary catheters
Metabolic Diseases Diabetes mellitus and Amyloidosis ( accumulation of glycoprotein in tissues(kidney)) are probably the most common metabolic diseases that may lead to chronic glomerular nephritis
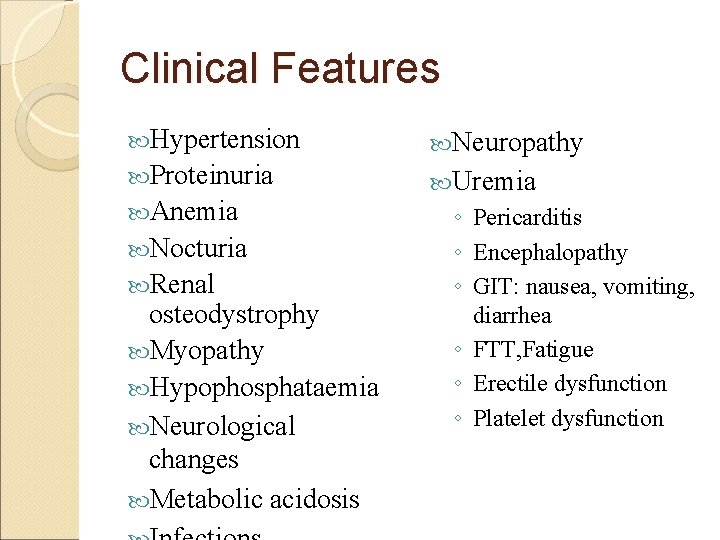
Clinical Features Hypertension Neuropathy Proteinuria Uremia Anemia Nocturia Renal osteodystrophy Myopathy Hypophosphataemia Neurological changes Metabolic acidosis ◦ Pericarditis ◦ Encephalopathy ◦ GIT: nausea, vomiting, diarrhea ◦ FTT, Fatigue ◦ Erectile dysfunction ◦ Platelet dysfunction
Clinical Features Patients with CKD stage 1 -3 are frequently asymptomatic. Generally, the symptoms become more evident at stage 4 -5.
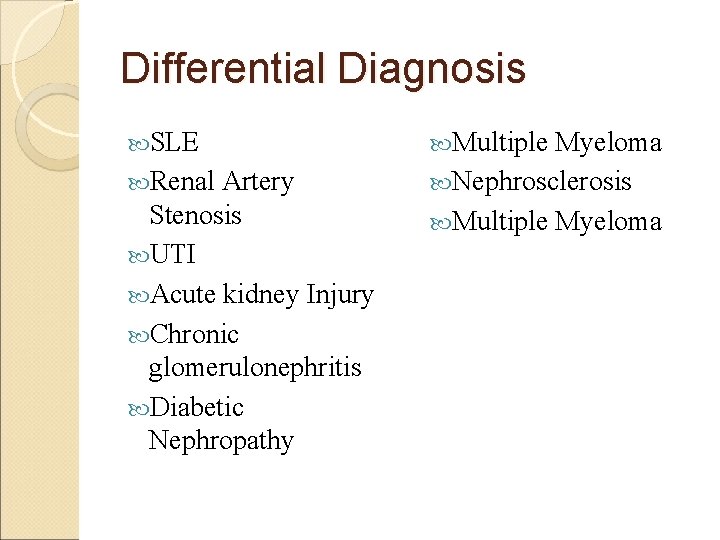
Differential Diagnosis SLE Renal Artery Stenosis UTI Acute kidney Injury Chronic glomerulonephritis Diabetic Nephropathy Multiple Myeloma Nephrosclerosis Multiple Myeloma
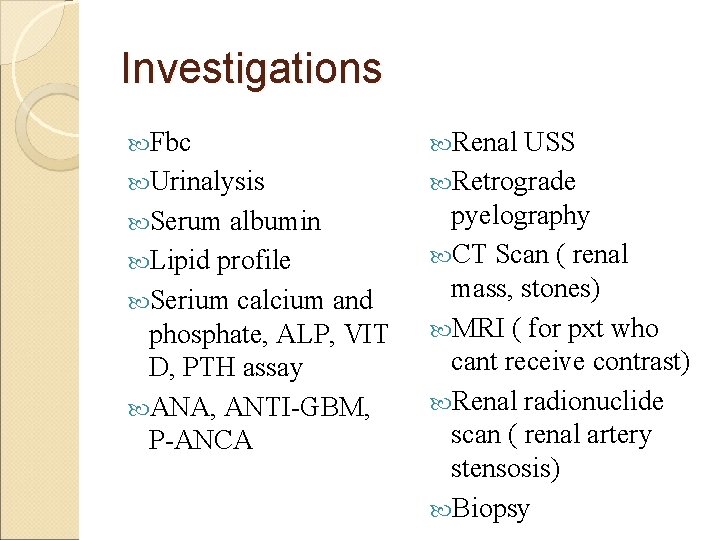
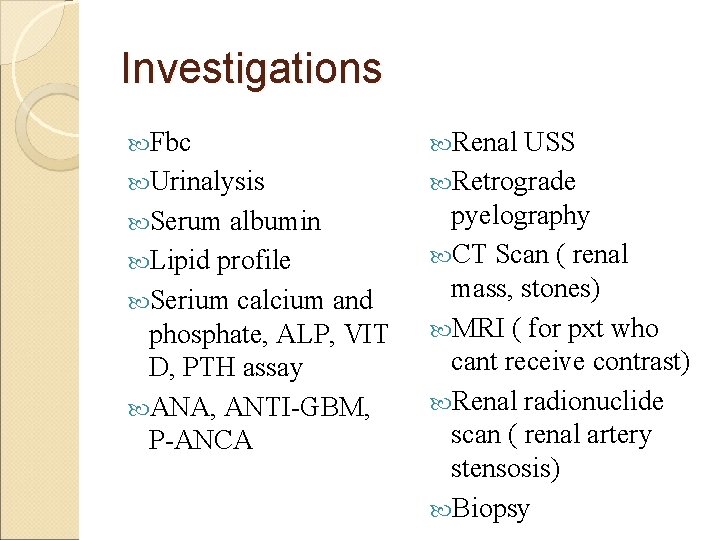
Investigations Fbc Urinalysis Serum albumin Lipid profile Serium calcium and phosphate, ALP, VIT D, PTH assay ANA, ANTI-GBM, P-ANCA Renal USS Retrograde pyelography CT Scan ( renal mass, stones) MRI ( for pxt who cant receive contrast) Renal radionuclide scan ( renal artery stensosis) Biopsy
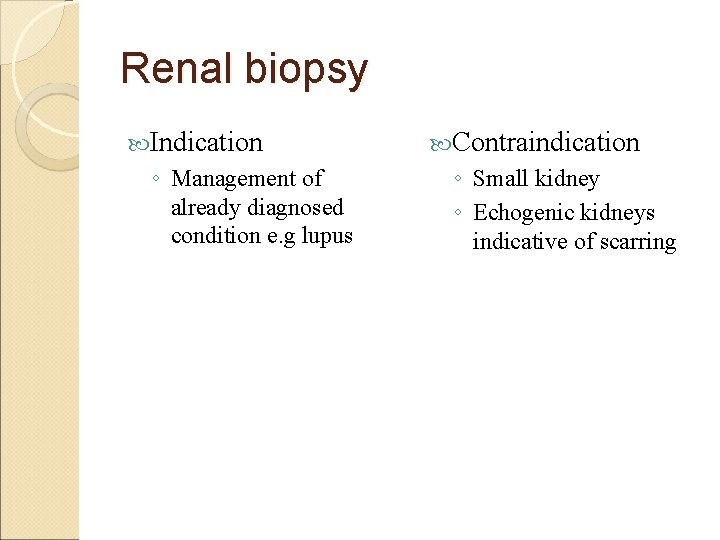
Renal biopsy Indication ◦ Management of already diagnosed condition e. g lupus Contraindication ◦ Small kidney ◦ Echogenic kidneys indicative of scarring
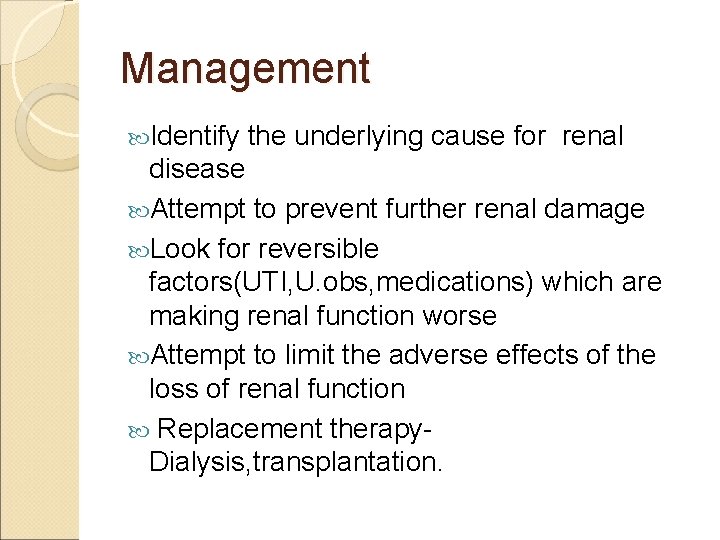
Management Identify the underlying cause for renal disease Attempt to prevent further renal damage Look for reversible factors(UTI, U. obs, medications) which are making renal function worse Attempt to limit the adverse effects of the loss of renal function Replacement therapy. Dialysis, transplantation.
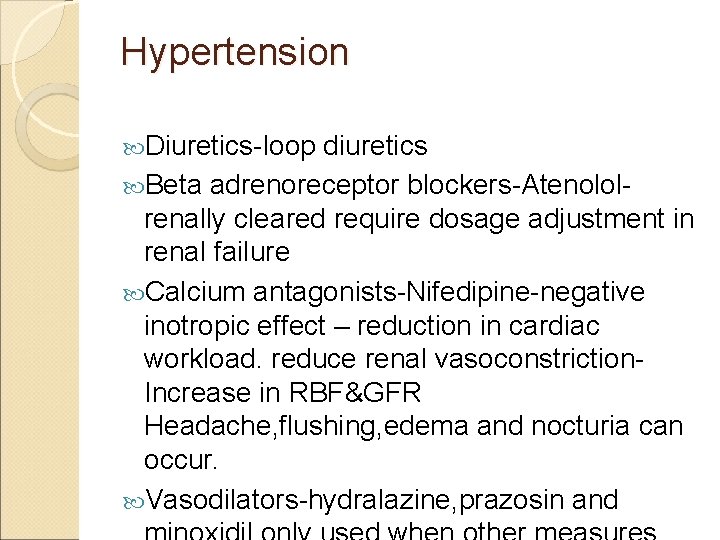
Hypertension Diuretics-loop diuretics Beta adrenoreceptor blockers-Atenololrenally cleared require dosage adjustment in renal failure Calcium antagonists-Nifedipine-negative inotropic effect – reduction in cardiac workload. reduce renal vasoconstriction. Increase in RBF&GFR Headache, flushing, edema and nocturia can occur. Vasodilators-hydralazine, prazosin and
Uremia Urea is one of the toxin -Symptomatic relief when the dietary protein intake is reduced. Nausea, vomiting and pruritis are some of the uremic symptoms Vomiting, nausea- Ondansetron, domperidone Pruritis-chlorpheniramine, Loratadine
Anemia Relative deficiency of erythropoietin (regulator of red cell production) Shortened red cell survival and marrow suppression due to uremic toxins Treatment-Recombinant human erythropoietin Target hemoglobin between 10&12 g/dl Complication of treatment-Increased blood pressure, and Increased blood coaguility, Increased incidence of thrombosis of AV fistulae used in hemodialysis.
Renal Osteodystrophy Cholecalciferol is the precursor of active vitamin D is both absorbed in the GIT and produced in the skin Production of 1, 25 dihydroxycholecalciferol(calcitriol) requires the hydroxylation of the Cholecalciferol molecule at 1 and the 25 position. 1 -position hydroxylation occurs in the kidney (impaired in CRF)& 25 position in the liver. Defective mineraliation of bone and
Renal Osteodystrophy Hyperphosphataemia phosphate excretion due to reduced Hypocalcaemia and a reduction in the direct suppressive action of 1, 25 dihydroxycholecalciferol on the parathyroid gland results in increased secretion of PTH Failed kidney unable to respond to PTH by increasing renal calcium absorption- the serum PTH levels remain persistently elevated, and hyperplasia of the parathyroid gland occurs-resulting in secondary hyperparathyroidism.
Renal Osteodystrophy Hyperphosphataemia-dietary foods with high phosphate (milk, cheese, egg) restriction of Phosphate binding agents-aluminium hydroxide cap 300 -600 mg before each meal. Calcium VIT carbonate 500 mg with each meal D deficiency-alfacalcidol at 0. 25 microgram/day or 1, 25 dihydroxycholecalciferol(calcitriol)1 -
Neurological changes Inability to concentrate, memory impairment, irritability Peripheral neuropathy- demyelination of medullated fibres. (paresthesia) Improve-once dialysis is initiated
Muscle function Muscle cramps & restless legs (legs are jumpy during the night) Due to nutritional deficiency &electrolyte disturbances, vitamin D deficiency Treatment- Clonazepam Muscle cramps-quinine sulphate
Edema Result of Sodium and water retention Hypoalbuminaemia-due to renal loss Pulmonary and peripheral edema are best controlled with dialysis but diuretics can be useful Salt restriction
Hyperkalaemia Potassium restricted diet Fruits , tender coconut, Vegetables, chocolate, Beer, instant coffee Emergency treatment of hyperkalemia
Acidosis Reduction in serum bicarbonate Sodium bicarbonate 1 -6 g/day
Infection Cellular and humoral immunity is impaired with increased susceptibility to infection Infections are the second common death in dialysis patients after the cardiovascular deaths
Treatment Dialysis ◦ Hemodialysis ◦ Peritoneal dialysis ◦ Haemofiltration Transplantation with immunosuppressive agents
Dialysis The movement of fluid and molecules across a semi permeable membrane from one compartment to another. Dialysis does not correct renal dysfunction Dialysis helps to replace renal function when kidneys have failed ◦ Correct fluid/electrolyte imbalances ◦ Remove waste products 10/20/2021 36
Dialysis When initiated? ◦ When uremia can no longer be managed conservatively. ◦ Immediately when: Unresponsive to diuretics (fluid overload) Pericarditis present Uncontrolled hypertension Neurologic manifestations Unresponsive hyperkalemia GFR less than 15 ml/minute 10/20/2021 37
Dialysate A balanced mix of electrolytes and water Closely resembles human plasma Need not be sterile in hemodialysis, but sterile with peritoneal dailysis 10/20/2021 38
Dialysate Solutions Common electrolytes included: ◦ Potassium ◦ Sodium chloride ◦ Magnesium ◦ Calcium ◦ Glucose: added to increase filtration of fluid ◦ Bicarbonate or acetate added to buffer (stabilize any existing metabolic acidosis) 10/20/2021 39
Dialysis: General Principles Diffusion ◦ Movement of solutes from an area of greater concentration to lesser concentration Osmosis ◦ Movement of fluid from an area of lesser to an area of greater concentration of solutes. 10/20/2021 40
Dialysis: General Principles Ultrafiltration (water & fluid removal) ◦ Movement of fluid across a semi permeable membrane as a result of an artificially created pressure gradient. 10/20/2021 41
Types of Dialysis Hemodialysis Peritoneal Dialysis Hemofiltration/Continuous Renal Replacement Therapy (CRRT) 10/20/2021 42
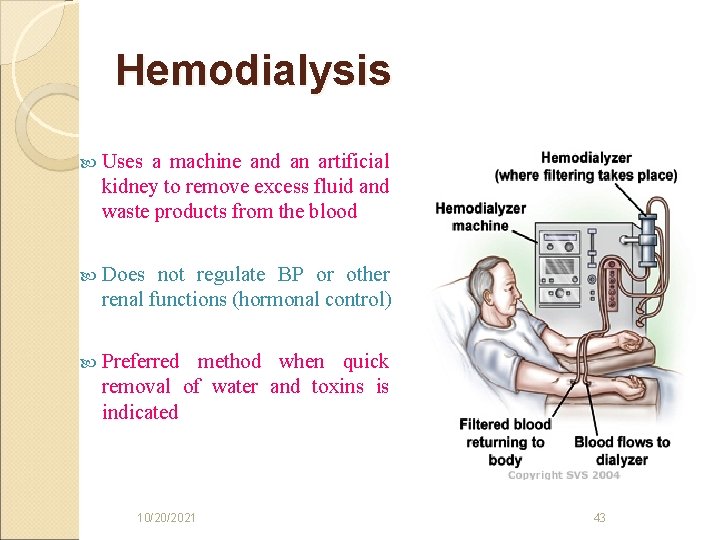
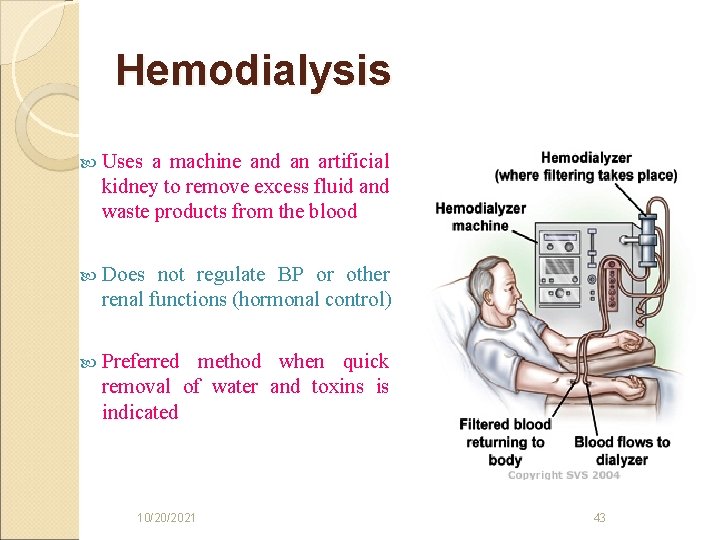
Hemodialysis Uses a machine and an artificial kidney to remove excess fluid and waste products from the blood Does not regulate BP or other renal functions (hormonal control) Preferred method when quick removal of water and toxins is indicated 10/20/2021 43
Hemodialysis Blood pumped out of client via the vascular access Passes through a filter (dialyzer) Semi-permeable pores allows small substances to pass through (creatinine, urea, water) does not allow passage of blood, protein, bacteria Blood returned to client once filtered 10/20/2021 44
Duration & Frequency Dependent on: ◦ Amount of metabolic waste to be cleared ◦ Clearance capacity of dialysis machine ◦ The amount of fluid to be removed 12 hours per week, divided into three 4 hour treatments Restricts activity level of client 10/20/2021 45
Anticoagulation Heparin used to inhibit tendency of blood to clot when in contact with foreign surfaces (dialyzer membrane) Clients receiving erythropoietin may need more heparin Risk for hemorrhage during and immediately after treatment 10/20/2021 46
Hemodialysis Complications Hypotension-100 -200 ml of NS Headache-Paracetamol Nausea/vomiting-ondansetron Malaise Dizziness Muscle cramps Blood Loss Sepsis Disequilibrium syndrome Dialysis encephalopathy Itching –Diphenhydramine 25 -50 mg 10/20/2021 47
Hemodialysis Complications Disequilibrium syndrome ◦ Due to rapid changes in the composition of the extracellular fluid. ◦ Solutes (BUN) removed more rapidly from the blood than from the CSF and brain ◦ Creates a high osmotic gradient in the brain resulting in a shift of fluid into the brain = Cerebral edema Confusion Decreased level of consciousness Restlessness Headache seizures 10/20/2021 48
Hemodialysis Advantages maximum solute clearance best tx for severe hyper-K+ ready availability limited anti-coagulation time bedside vascular access Disadvantages hemodynamic instability hypoxemia rapid fluid + solute shifts complex equipment specialized personnel Costly 10/20/2021 49
Peritoneal Dialysis After placement of peritoneal dialysis catheter-usually PD is not initiated until 7 -14 days to allow for proper sealing of the catheter. Three phases are present in peritoneal dialysis ◦ Inflow(fill)-a prescribed amount of dialysate solution is inserted usually 2 liters in an adult over about 10 -15 minutes(based on client comfort) ◦ Dwell(equilibration)-diffusion and osmosis occur between the patients blood and the peritoneal cavity. The duration of the dwell time can last 20 -30 minutes to 8 hours or more. ◦ Drain-draining of the peritoneal fluid takes approximately 20 -30 minutes and may be facilitated by gently massaging the abdomen 10/20/2021 50
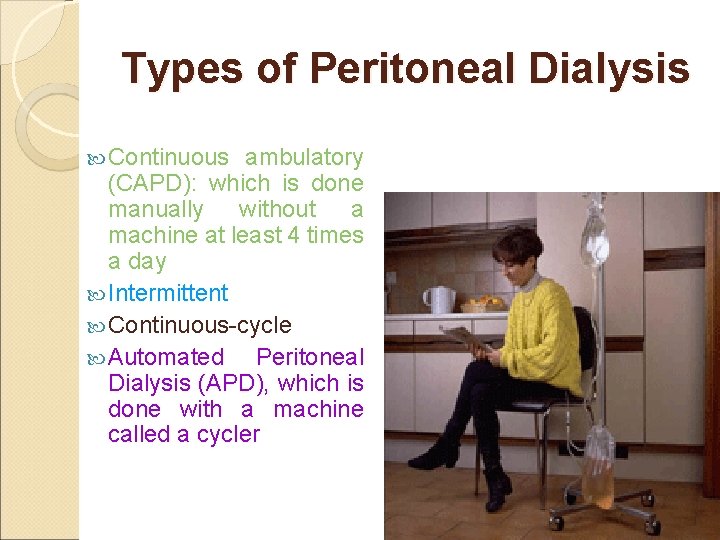
Types of Peritoneal Dialysis Continuous ambulatory (CAPD): which is done manually without a machine at least 4 times a day Intermittent Continuous-cycle Automated Peritoneal Dialysis (APD), which is done with a machine called a cycler 10/20/2021 51
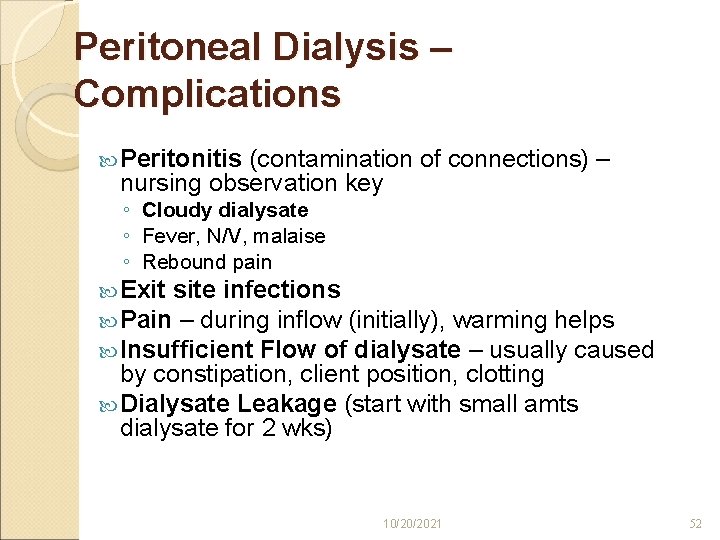
Peritoneal Dialysis – Complications Peritonitis (contamination of connections) – nursing observation key ◦ Cloudy dialysate ◦ Fever, N/V, malaise ◦ Rebound pain Exit site infections Pain – during inflow (initially), warming helps Insufficient Flow of dialysate – usually caused by constipation, client position, clotting Dialysate Leakage (start with small amts dialysate for 2 wks) 10/20/2021 52
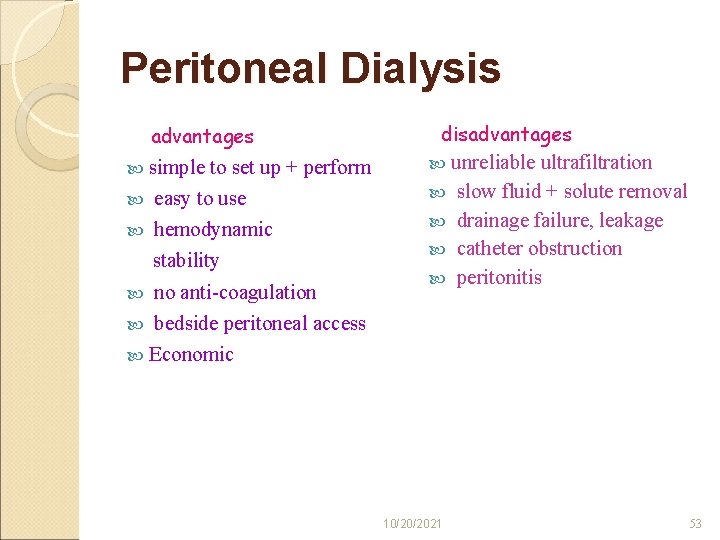
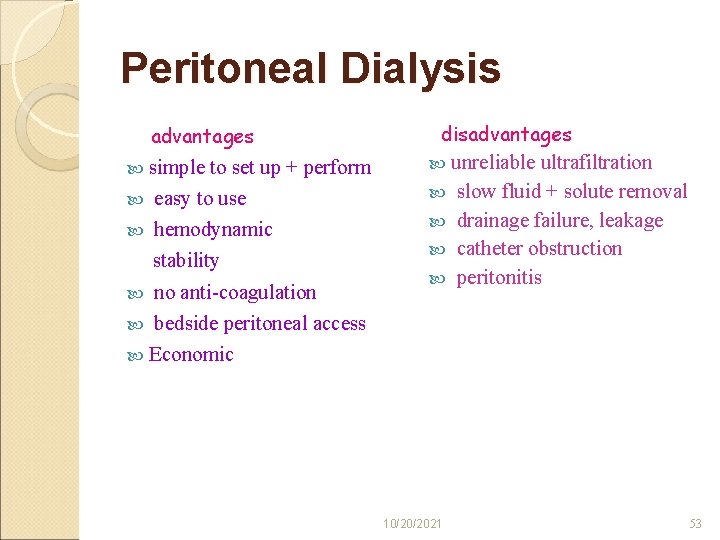
Peritoneal Dialysis advantages simple to set up + perform easy to use hemodynamic stability no anti-coagulation bedside peritoneal access Economic disadvantages unreliable 10/20/2021 ultrafiltration slow fluid + solute removal drainage failure, leakage catheter obstruction peritonitis 53
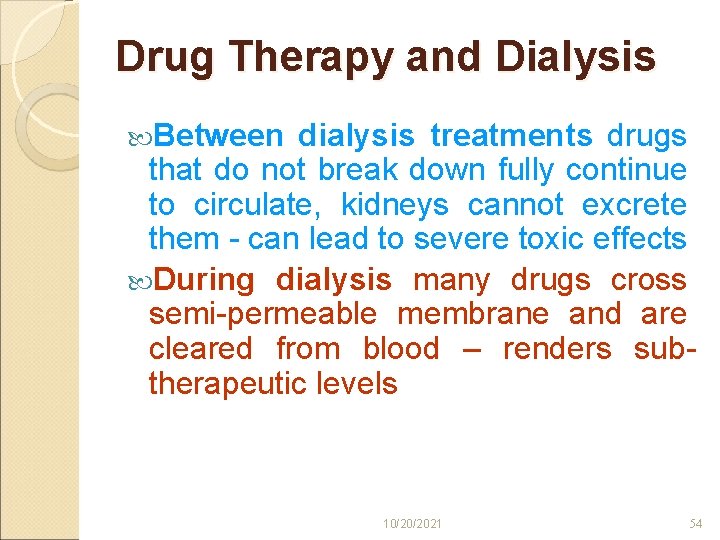
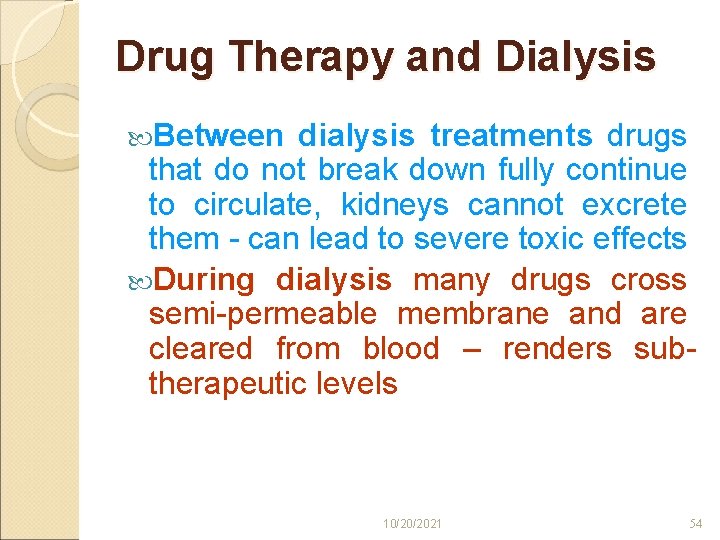
Drug Therapy and Dialysis Between dialysis treatments drugs that do not break down fully continue to circulate, kidneys cannot excrete them - can lead to severe toxic effects During dialysis many drugs cross semi-permeable membrane and are cleared from blood – renders subtherapeutic levels 10/20/2021 54
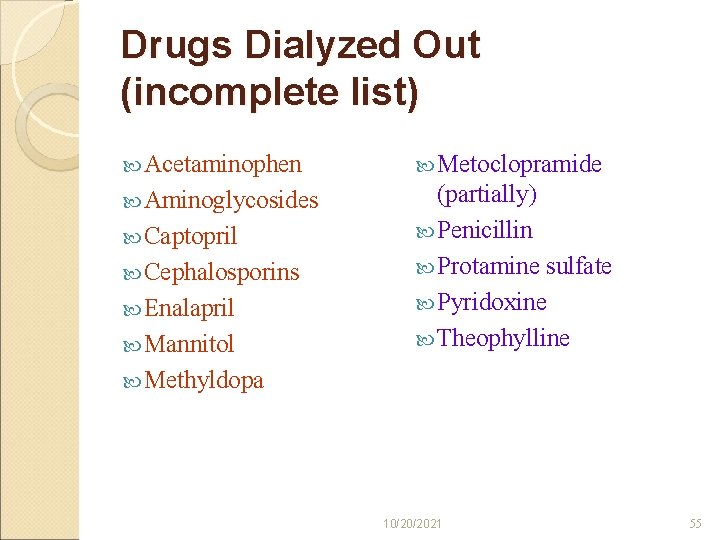
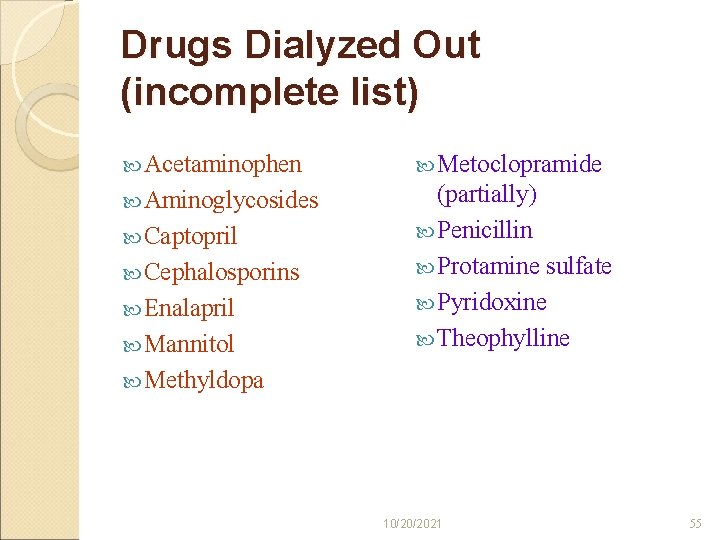
Drugs Dialyzed Out (incomplete list) Acetaminophen Metoclopramide Aminoglycosides (partially) Penicillin Protamine sulfate Pyridoxine Theophylline Captopril Cephalosporins Enalapril Mannitol Methyldopa 10/20/2021 55
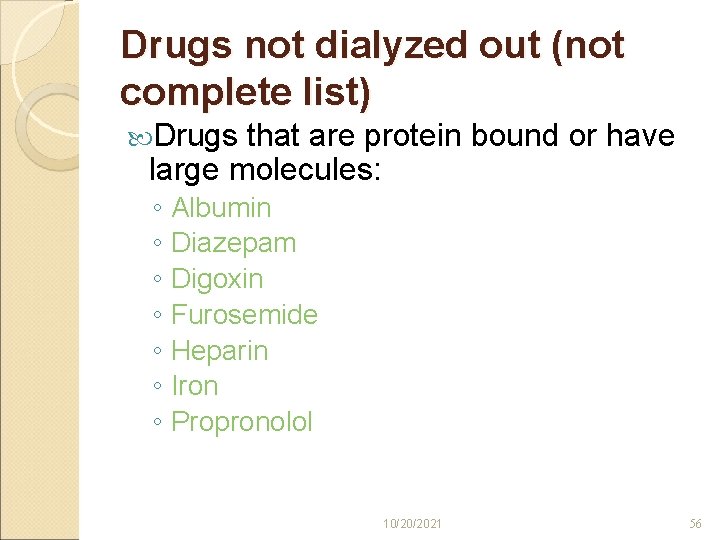
Drugs not dialyzed out (not complete list) Drugs that are protein bound or have large molecules: ◦ Albumin ◦ Diazepam ◦ Digoxin ◦ Furosemide ◦ Heparin ◦ Iron ◦ Propronolol 10/20/2021 56
THANK YOU