Chronic Renal Failure Internal Medicine Xu Xiaoqi Shanghai

- Slides: 60
Chronic Renal Failure Internal Medicine Xu Xiaoqi Shanghai Second Medical Uni. 2005. 10. 6
Content Ì Ì Ì Ì Definition Etiology Pathogenesis of CRF Pathogenesis of uremic syndrome Clinical presentations Diagnosis Treatment
Definition(定义) ü CRF is a permanent, usually progressive, diminution in renal function to a degree that has damaging consequences for the patient. ü It is characterized by an increasing inability of the kidney(肾脏) to maintain normal low levels of the products of protein metabolism(such as urea), normal blood pressure and hematocrit, and sodium, water, potassium, and acid-base(酸碱) balance.
ü This occurs when glomerular(肾小球) filtration rate (GFR) is reduced by at least 50 m. L/min. It can be mild, moderate, or servere. ü End-stage renal disease (ESRD,终末期肾病) is the degree of renal failure that would cause the death of the patient unless some form of RRT is initiated.
n The progression of CRF leads, in the majority of instances, to end stage renal disease (ESRD) at which point renal replacement required. therapy is
§ The rate of progression of CRF varies according to the underlying nephropathy and between individual patients. § Age, gender, race, proteinuria(蛋 白尿), lipids, hypertension, smoking.
n It has been suggested that it is faster in CGN (慢性肾小球肾炎)compared with chronic interstitial nephropathies (CIN, 慢 性 间 质 性 肾 炎 ) or hypertensive nephrosclerosis(HNS,高血压肾硬化).
Proteinuria is the only continuous variable identified as an independent risk factor.
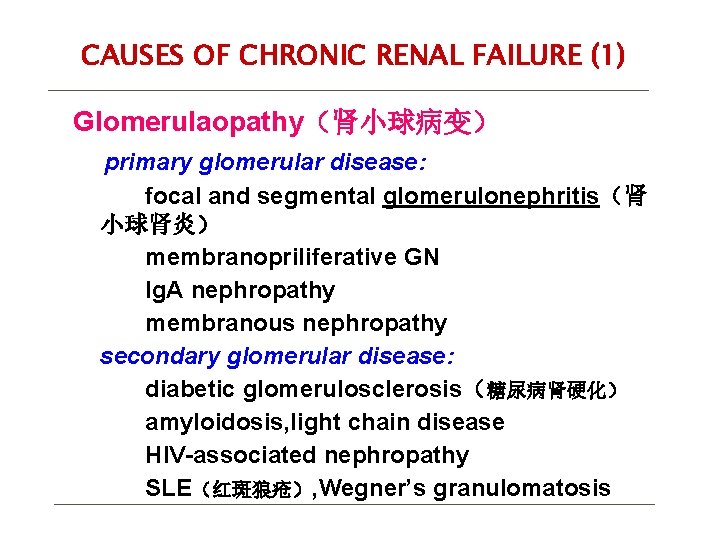
CAUSES OF CHRONIC RENAL FAILURE (1) Glomerulaopathy(肾小球病变) primary glomerular disease: focal and segmental glomerulonephritis(肾 小球肾炎) membranopriliferative GN Ig. A nephropathy membranous nephropathy secondary glomerular disease: diabetic glomerulosclerosis(糖尿病肾硬化) amyloidosis, light chain disease HIV-associated nephropathy SLE(红斑狼疮), Wegner’s granulomatosis
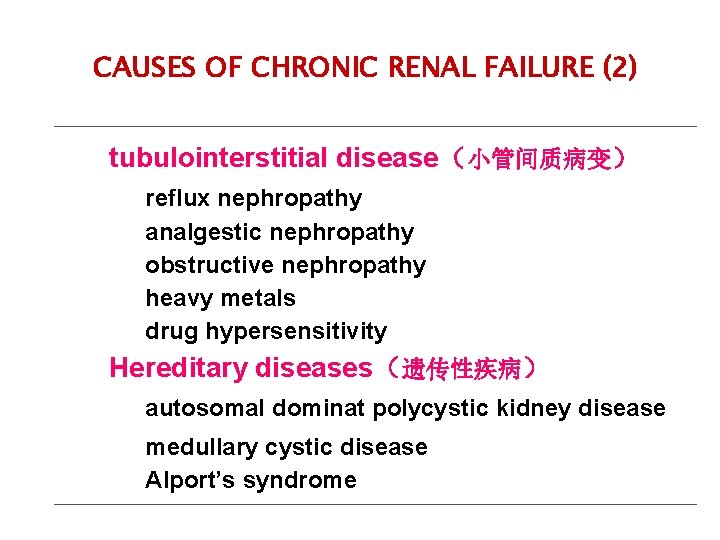
CAUSES OF CHRONIC RENAL FAILURE (2) tubulointerstitial disease(小管间质病变) reflux nephropathy analgestic nephropathy obstructive nephropathy heavy metals drug hypersensitivity Hereditary diseases(遗传性疾病) autosomal dominat polycystic kidney disease medullary cystic disease Alport’s syndrome
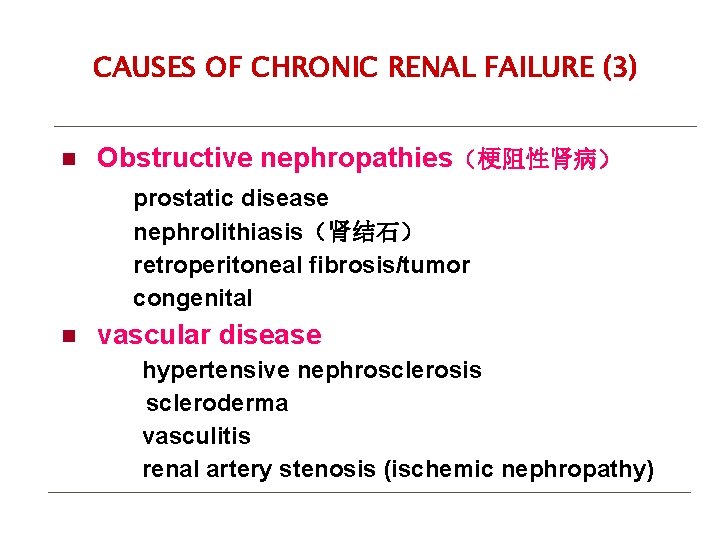
CAUSES OF CHRONIC RENAL FAILURE (3) n Obstructive nephropathies(梗阻性肾病) prostatic disease nephrolithiasis(肾结石) retroperitoneal fibrosis/tumor congenital n vascular disease hypertensive nephrosclerosis scleroderma vasculitis renal artery stenosis (ischemic nephropathy)
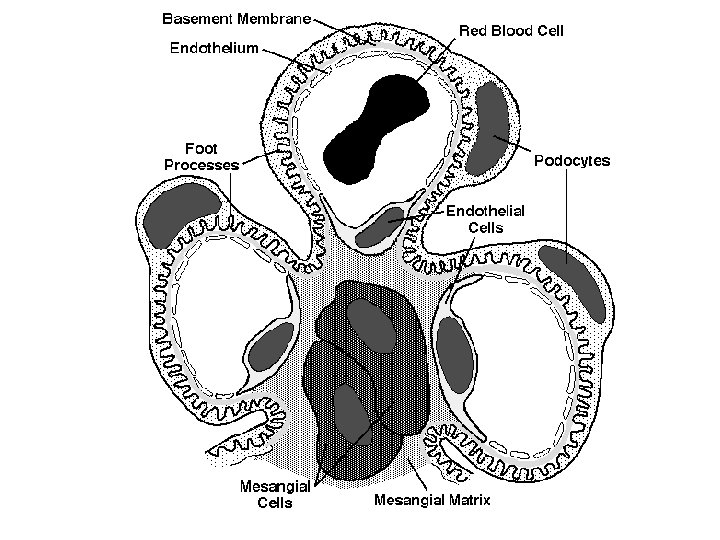
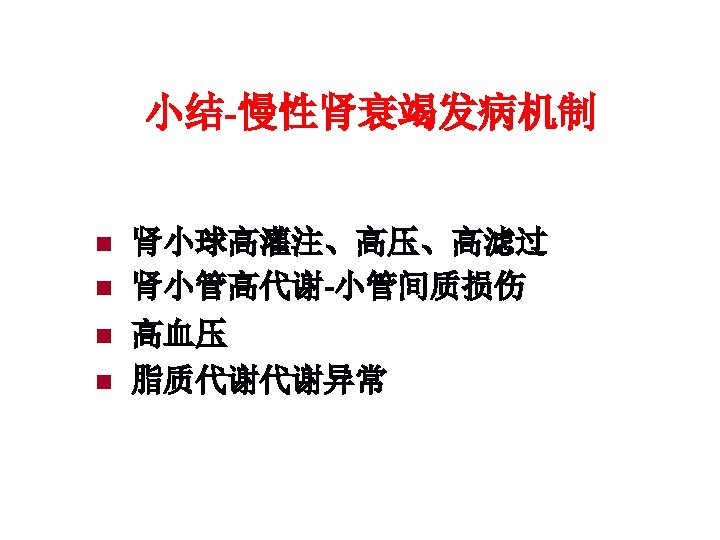
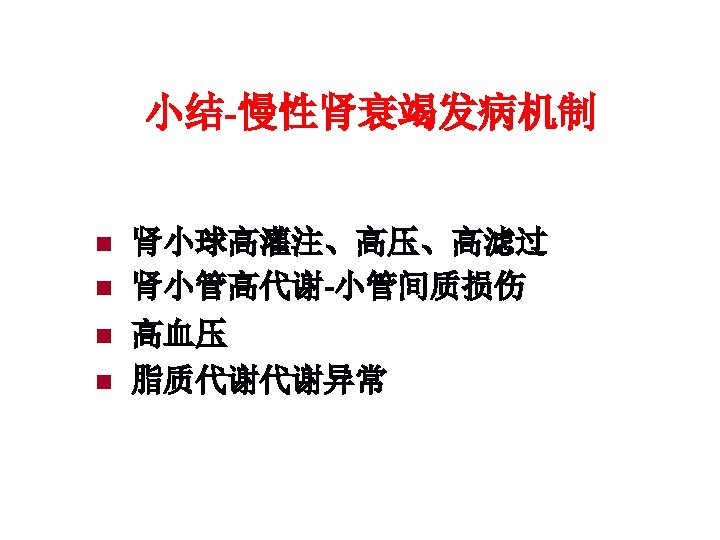
Pathogenesis of chronic renal failure
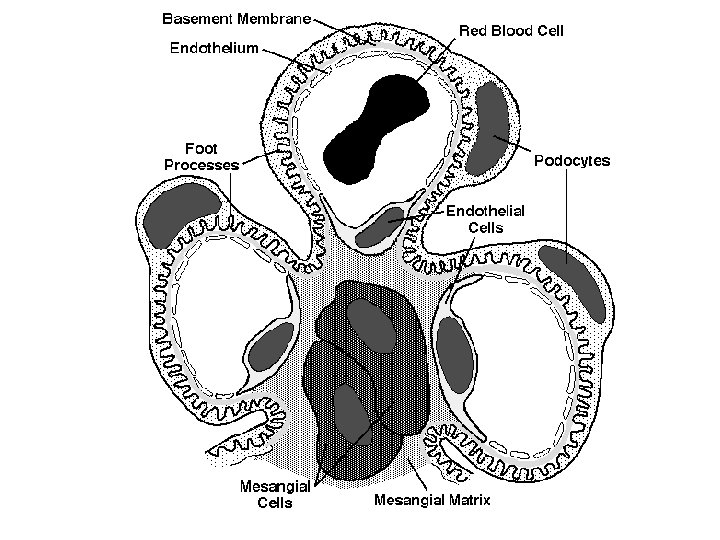
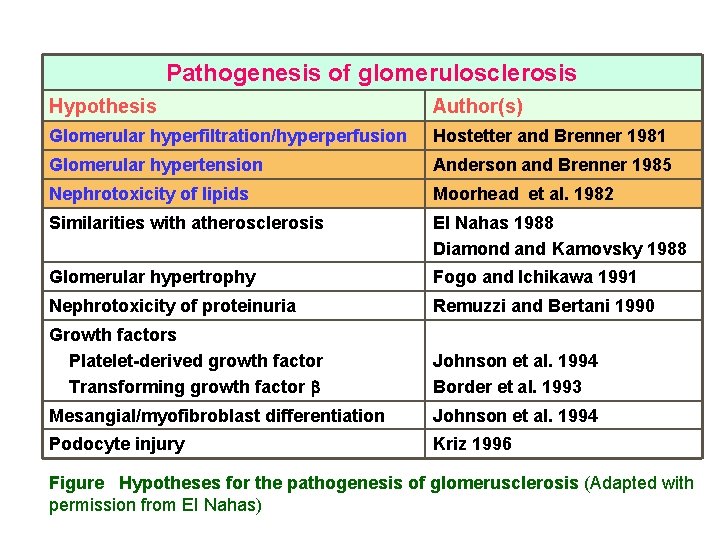
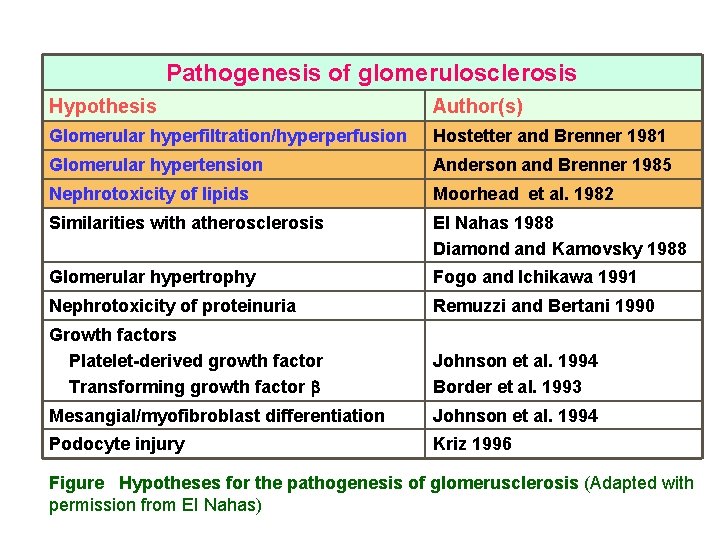
Pathogenesis of glomerulosclerosis Hypothesis Author(s) Glomerular hyperfiltration/hyperperfusion Hostetter and Brenner 1981 Glomerular hypertension Anderson and Brenner 1985 Nephrotoxicity of lipids Moorhead et al. 1982 Similarities with atherosclerosis EI Nahas 1988 Diamond and Kamovsky 1988 Glomerular hypertrophy Fogo and Ichikawa 1991 Nephrotoxicity of proteinuria Remuzzi and Bertani 1990 Growth factors Platelet-derived growth factor Transforming growth factor Johnson et al. 1994 Border et al. 1993 Mesangial/myofibroblast differentiation Johnson et al. 1994 Podocyte injury Kriz 1996 Figure Hypotheses for the pathogenesis of glomerusclerosis (Adapted with permission from EI Nahas)
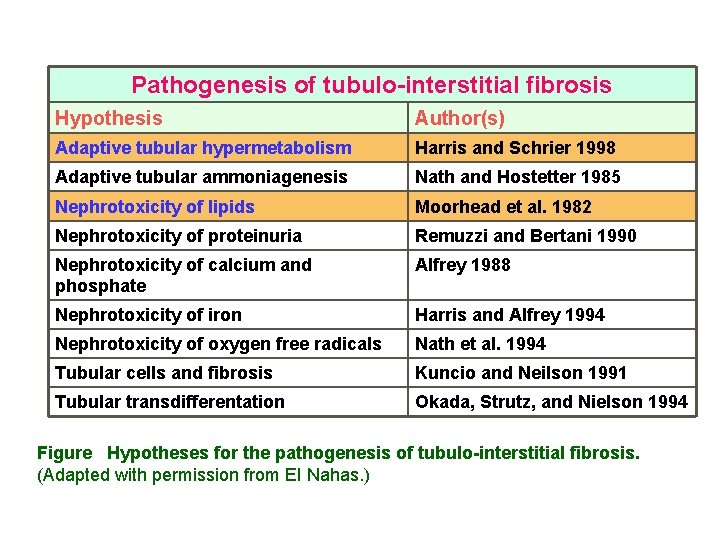
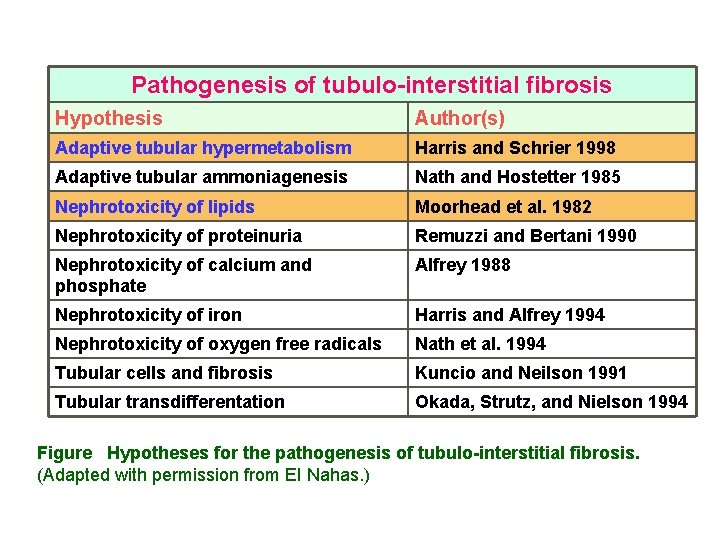
Pathogenesis of tubulo-interstitial fibrosis Hypothesis Author(s) Adaptive tubular hypermetabolism Harris and Schrier 1998 Adaptive tubular ammoniagenesis Nath and Hostetter 1985 Nephrotoxicity of lipids Moorhead et al. 1982 Nephrotoxicity of proteinuria Remuzzi and Bertani 1990 Nephrotoxicity of calcium and phosphate Alfrey 1988 Nephrotoxicity of iron Harris and Alfrey 1994 Nephrotoxicity of oxygen free radicals Nath et al. 1994 Tubular cells and fibrosis Kuncio and Neilson 1991 Tubular transdifferentation Okada, Strutz, and Nielson 1994 Figure Hypotheses for the pathogenesis of tubulo-interstitial fibrosis. (Adapted with permission from EI Nahas. )
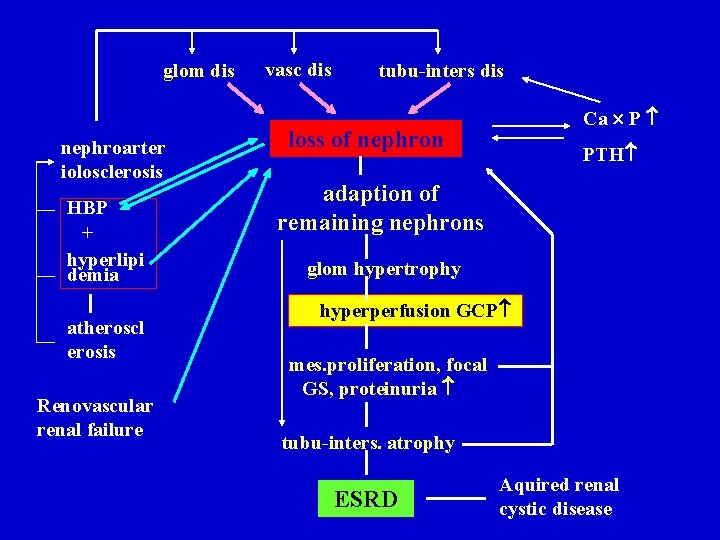
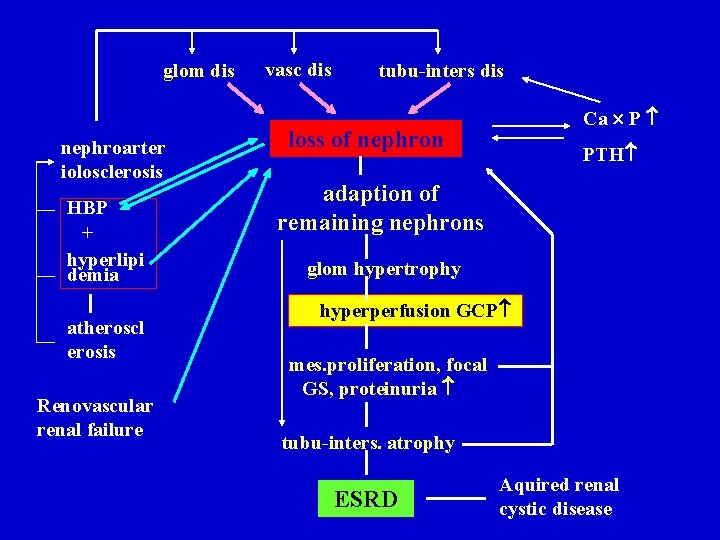
glom dis nephroarter iolosclerosis HBP + hyperlipi demia atheroscl erosis Renovascular renal failure vasc dis tubu-inters dis Ca P loss of nephron PTH adaption of remaining nephrons glom hypertrophy hyperperfusion GCP mes. proliferation, focal GS, proteinuria tubu-inters. atrophy ESRD Aquired renal cystic disease
Pathogenesis of the uremic syndrome
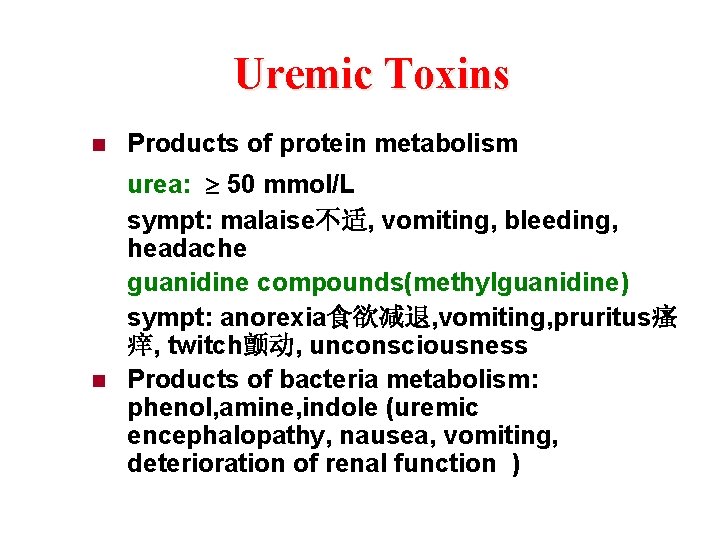
Uremic Toxins n n Products of protein metabolism urea: 50 mmol/L sympt: malaise不适, vomiting, bleeding, headache guanidine compounds(methylguanidine) sympt: anorexia食欲减退, vomiting, pruritus瘙 痒, twitch颤动, unconsciousness Products of bacteria metabolism: phenol, amine, indole (uremic encephalopathy, nausea, vomiting, deterioration of renal function )
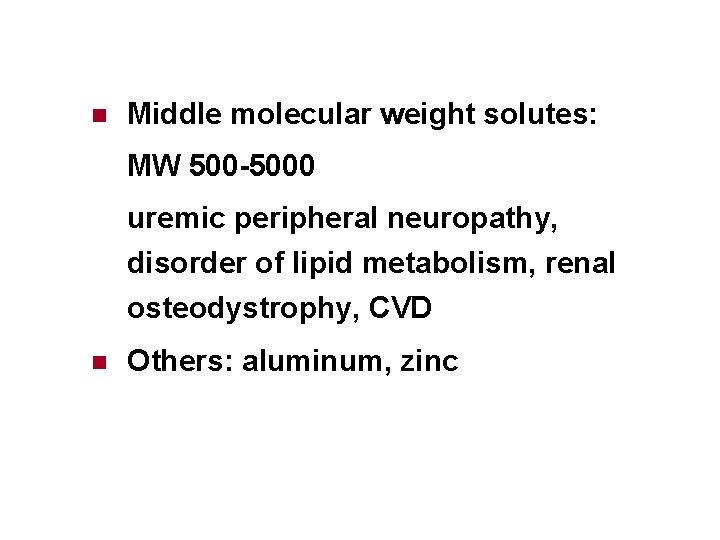
n Middle molecular weight solutes: MW 500 -5000 uremic peripheral neuropathy, disorder of lipid metabolism, renal osteodystrophy, CVD n Others: aluminum, zinc
Disorder of nutrition & metabolism n Catabolic metabolism分解代谢: n Anabolic metabolism合成代谢: n Intake:
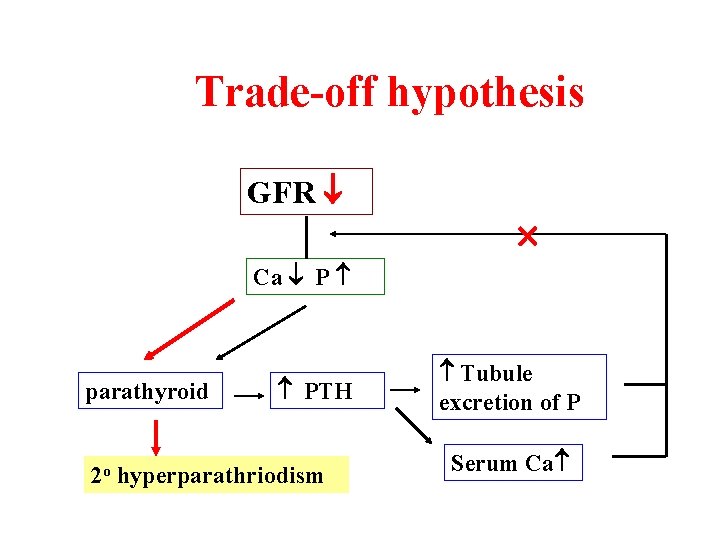
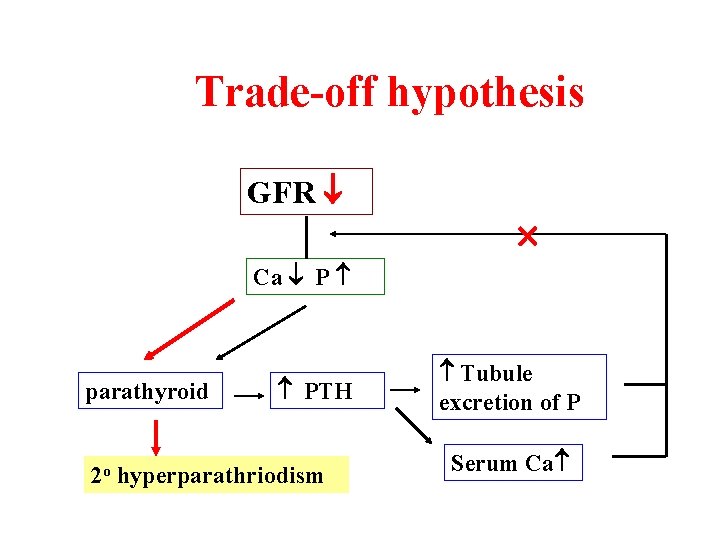
Trade-off hypothesis GFR Ca P parathyroid PTH 2 o hyperparathriodism Tubule excretion of P Serum Ca
Endocrine – metabolic disorder n Erythropoietin n 1, 25(OH)2 D 3 PTH n Insulin resistance
Clinical Presentations
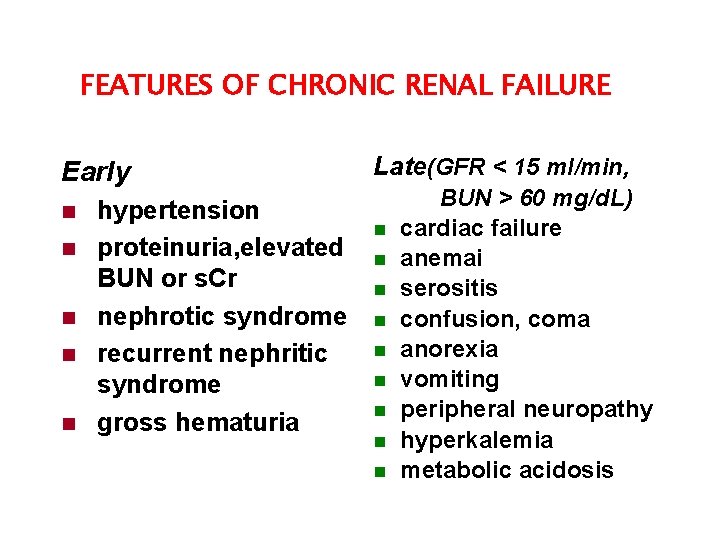
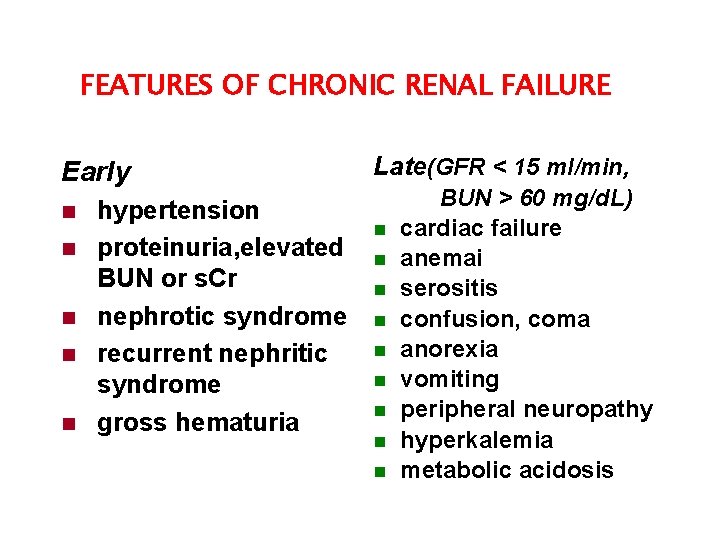
FEATURES OF CHRONIC RENAL FAILURE Early n n n hypertension proteinuria, elevated BUN or s. Cr nephrotic syndrome recurrent nephritic syndrome gross hematuria Late(GFR < 15 ml/min, n n n n n BUN > 60 mg/d. L) cardiac failure anemai serositis confusion, coma anorexia vomiting peripheral neuropathy hyperkalemia metabolic acidosis

l Gastroenterologic (胃肠道) manifestations prominent and frequently encountered ö anorexia ö nausea, vomiting, diarrhea ö uremic gastroenteritis ö peptic ulcer, bleeding ö unpleasant , metallic taste (uremic fetor)
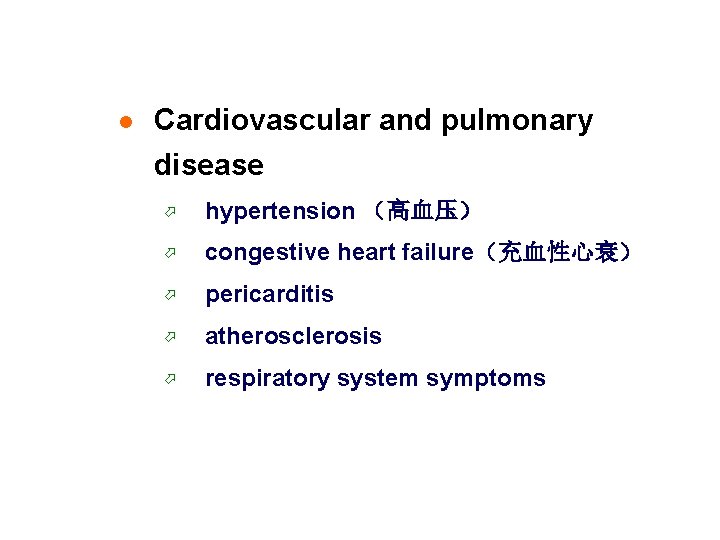
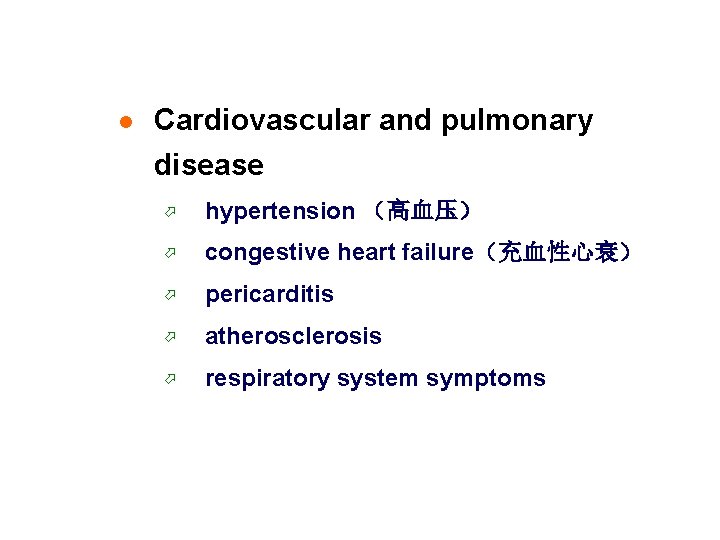
l Cardiovascular and pulmonary disease ö hypertension (高血压) ö congestive heart failure(充血性心衰) ö pericarditis ö atherosclerosis ö respiratory system symptoms
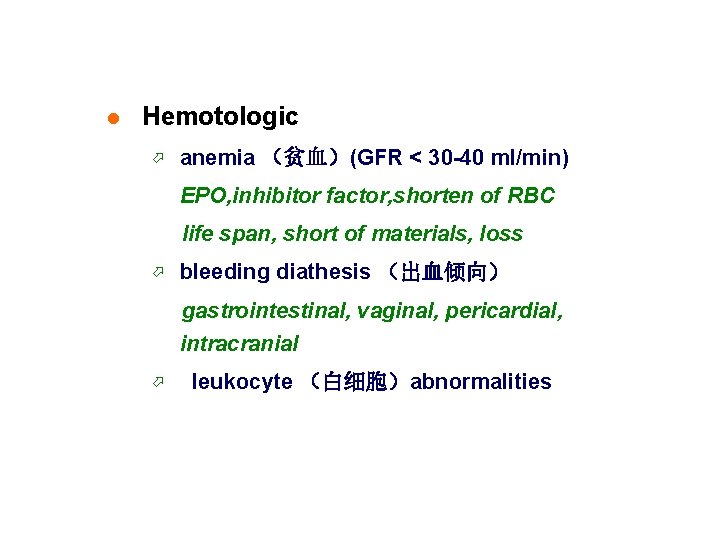
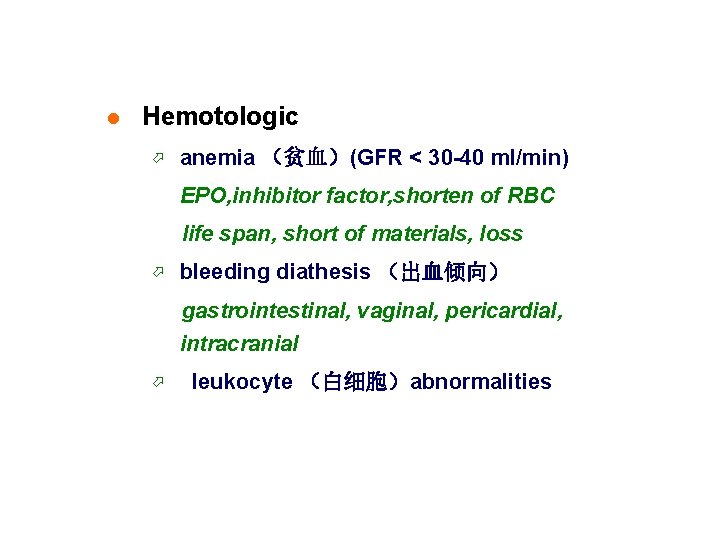
l Hemotologic ö anemia (贫血)(GFR < 30 -40 ml/min) EPO, inhibitor factor, shorten of RBC life span, short of materials, loss ö bleeding diathesis (出血倾向) gastrointestinal, vaginal, pericardial, intracranial ö leukocyte (白细胞)abnormalities
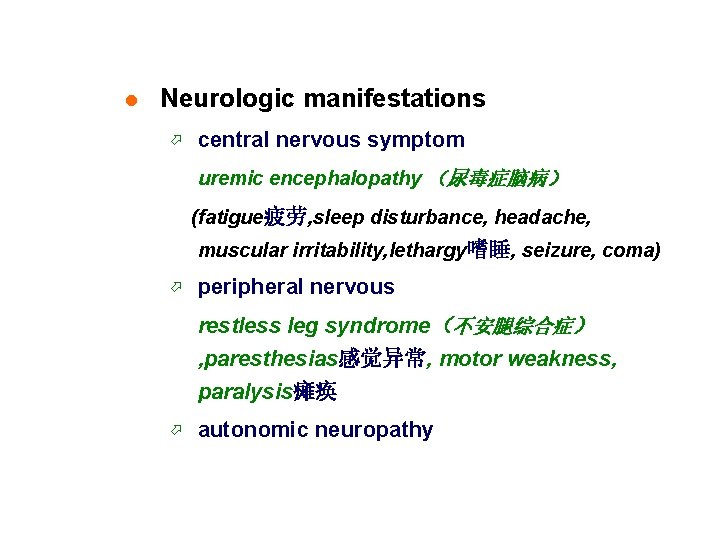
l Neurologic manifestations ö central nervous symptom uremic encephalopathy (尿毒症脑病) (fatigue疲劳, sleep disturbance, headache, muscular irritability, lethargy嗜睡, seizure, coma) ö peripheral nervous restless leg syndrome(不安腿综合症) , paresthesias感觉异常, motor weakness, paralysis瘫痪 ö autonomic neuropathy
l Dermatologic manifestations(皮肤表现) pallor苍白, hyperpigmentation, pruritus l Renal osteodystrophy(肾性骨营养不良) high-bone turnover dis: osteitis fibrosa cystica, osteoporosis, osteosclerosis low-bone turnover dis: osteomalacia骨软化, osteopenia骨量减少 mixed l Endocrine abnormalities l Infection cellular immune function is depressed
l Metabolic disturbance ö carbohydrate (碳水化合物)metabolism ö glucose tolerance (葡萄糖耐量) is reduced ö insulin(胰岛素)resistance ö hyperlipidemia: triglyceride(甘油三酯)
l Fluid, electrolyte(电解质) and acidbase disturbance ö sodium (钠)and water ö potassium(钾) ö metabolic acidosis(代谢性酸中毒) ö abnormalities of calcium, phosphate (钙、 磷) and vitamin D metabolism
Diagnosis & Differential diagnosis § History § Physical examination § Lab (urinalalysis, renal function, biochemical analysis of blood) § X-ray, ultrasound, radiorenogram
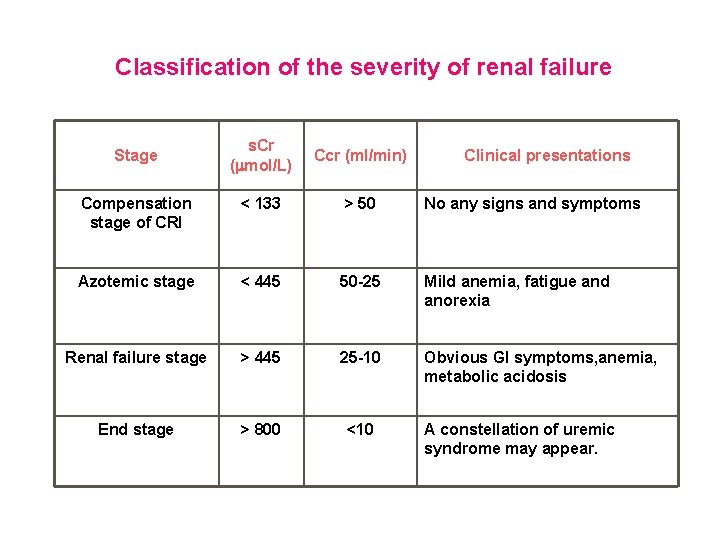
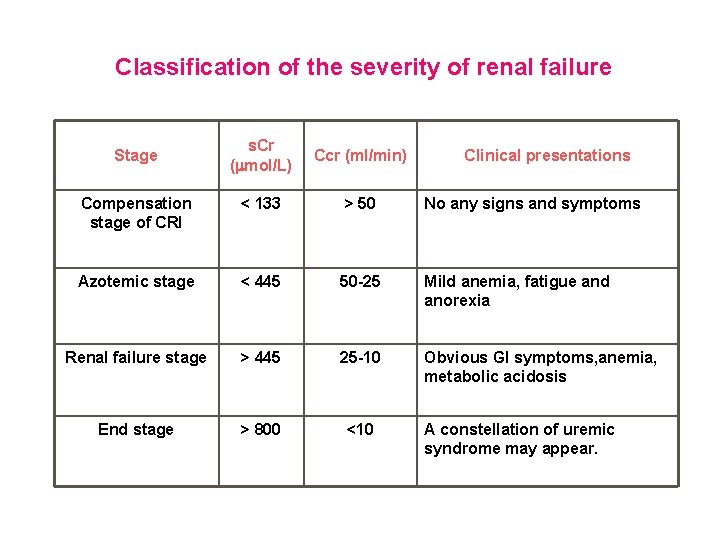
Classification of the severity of renal failure s. Cr ( mol/L) Ccr (ml/min) Compensation stage of CRI < 133 > 50 No any signs and symptoms Azotemic stage < 445 50 -25 Mild anemia, fatigue and anorexia Renal failure stage > 445 25 -10 Obvious GI symptoms, anemia, metabolic acidosis End stage > 800 <10 Stage Clinical presentations A constellation of uremic syndrome may appear.
Treatment § Primary disease and reversible factors treatment § § Conservative treatment Treatment of complications of uremia Blood purification Renal transplantation
General Recommendations (1) n The following general recommendations can be made for the management of patients with progressive CRF. l Frequent clinic follow-up is required with particular attention to the detction, monitoring, and treatment of hypertension. Emphasis should also be on a simultaneous reduction of proteinuria (evidence-based statement). l It is reasonable to advise patients with progressive CRF to avoid a high-protein diet, but caution should be exerted when recommending dietary protein restriction with its inherent risk of undernutrition. It may be better to start dialysis a few months earlier and be well nourished than risk malnutrition with its associated increased morbidity and mortality on dialysis.
General Recommendations (2) n Attention should be paid to the management of the complications of CRF including metabolic acidosis, hypocalcemia, and hyperphosphatemia with the associated renal osteodystrophy (evidence-based statement). n Potential nephrotoxins should be avoided including nonsteroidal anti-inflammatory agents; ACE inhibitors should also be used with careful monitoring.
General Recommendations (3) § Nephrologists should refrain from imposing unnecessary and unproven interventions on their patients with CRF. Such interventions should first undergo the rigors of clinical trials. Clinical trials in progressive CRF remain, however, very difficult to conduct in view of the heterogeneity of the population studied, which necessitates very large number of patients and lengthy followup to reach definitive conclusions.
Potentially reversible factors in CRF § Volume depletion; Intravenous radiographic contrast; § Selected antimicrobial agents (for example, § aminoglycosides and amphotericin B); § Nonsteroidal anti-inflammatory agents; including cyclo-oxygenase type 2 inhibitors; § Angiotensin-converting enzyme inhibition and angiotensin-2 receptor blockers; § Cyclosporine and tacrolimus; § Obstruction of the urinary tract.
Prevention additional injury ü 在 碘 造 影 剂 使 用 前 应 给 予 足 够 水 分 ( Patients should be adequately hydrated before receiving iodinated radiocontrast material) ü 在手术前应适当补充血容量(Adequate hydration is necessary before certain surgical procedures) ü 化疗前化疗中应补充血容量(Adequate hydration is essential before and during chemotherapy) ü 肾 病 患 者 中 避 免 NSAID( NSAID should be avoided in patients with renal diseases) ü 肾损药物应避免或加强监测(Nephrotoxic drugs should be avoided or carefully monitored)
Diet therapy n Enough calorie intake: 126 -147 KJ n Low protein diet: 0. 6 -0. 8 g/kg/d, 60% high quality protein n Essential amino acid supplement n -ketoacid supplement n Vitamin supplement: folic acid, Vit C, Vit B 6, Vit D
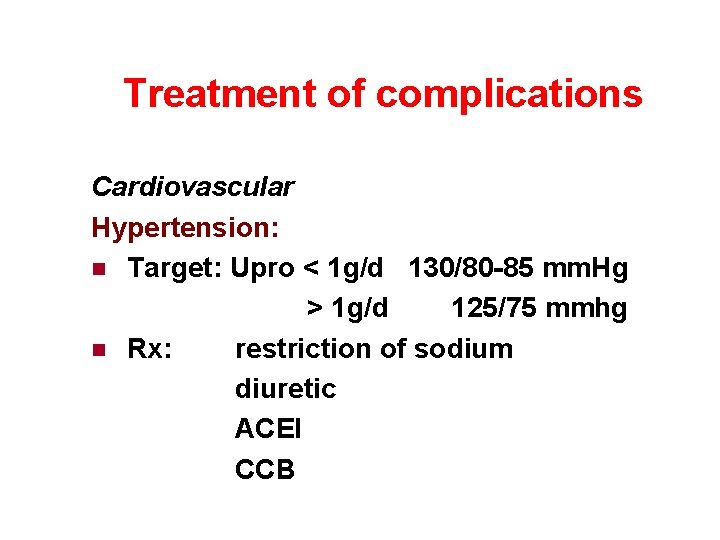
Treatment of complications Cardiovascular Hypertension: n Target: Upro < 1 g/d 130/80 -85 mm. Hg > 1 g/d 125/75 mmhg n Rx: restriction of sodium diuretic ACEI CCB
Heart failure n Restriction of water and sodium n Large dose of furosemide n Vascular dilation n Digoxins n Blood purification n Correction of electrolytes and acid-base disturbance n Improvement of anemia
Pericarditis n Increase dialysis frequency or time n corticosteroids n surgery
Anemia n Recombinant human erythropoietin 50 u/kg tiw, i. H target: Hb 100 -120 g/L, Hct 30 -35% n Iron n Folic acid
Renal osteodystrophy n Recover the imbalance of Ca, P restriction of intake phosphate binding n Vitamin D supplement n Partial parathyroidectomy
fluid, electrolytes and acid-base disturbance § Fluid and electrolytes water intake = urinary output + 500 ml Na intake: 3 g/d § § Hyperkalemia Metabolic acidosis biocarbonate < 13. 5 mmol/L i. V
§ § Control infection § Traditional Chinese medicine Remove uremic toxins from gastrointestinal
Blood purification n Hemodialysis n Peritoneal dialysis
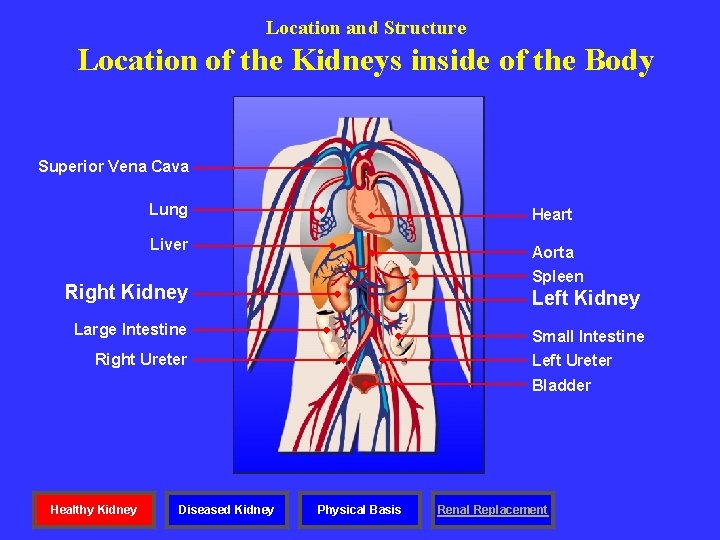
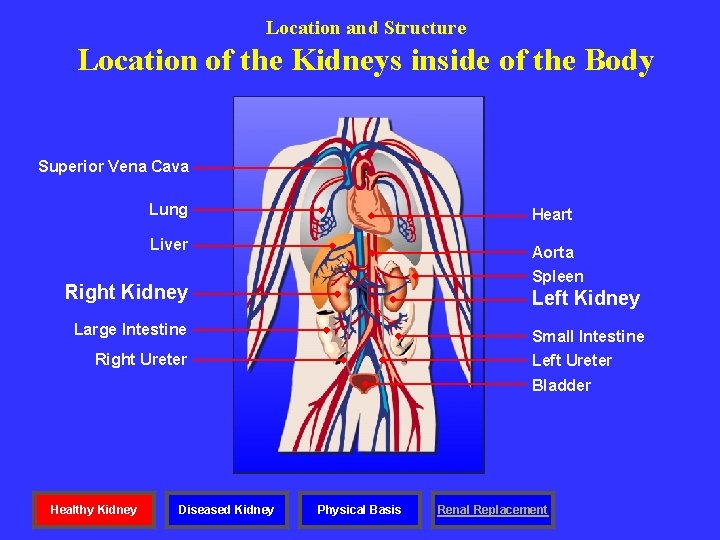
Location and Structure Location of the Kidneys inside of the Body Superior Vena Cava Lung Heart Liver Aorta Spleen Right Kidney Left Kidney Large Intestine Small Intestine Right Ureter Left Ureter Bladder Healthy Kidney Diseased Kidney Physical Basis Renal Replacement
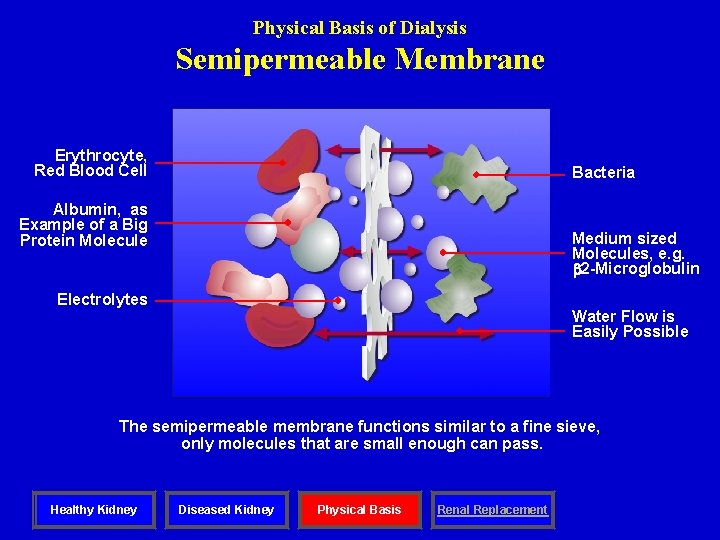
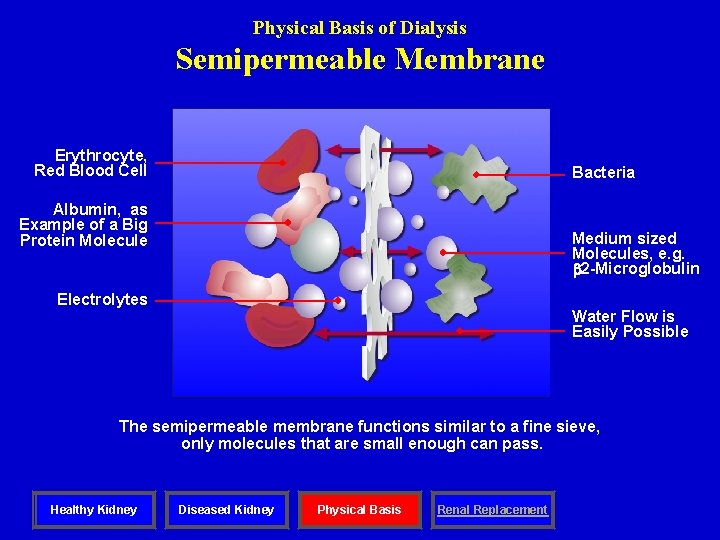
Physical Basis of Dialysis Semipermeable Membrane Erythrocyte, Red Blood Cell Bacteria Albumin, as Example of a Big Protein Molecule Medium sized Molecules, e. g. 2 -Microglobulin Electrolytes Water Flow is Easily Possible The semipermeable membrane functions similar to a fine sieve, only molecules that are small enough can pass. Healthy Kidney Diseased Kidney Physical Basis Renal Replacement
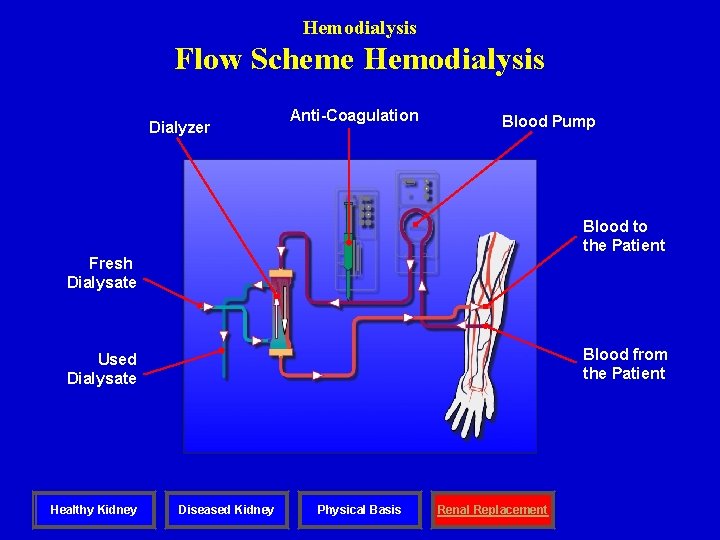
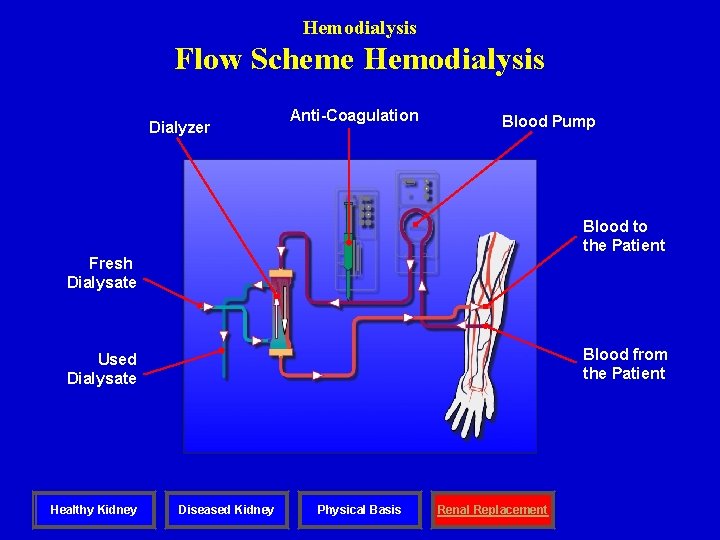
Hemodialysis Flow Scheme Hemodialysis Dialyzer Anti-Coagulation Blood Pump Blood to the Patient Fresh Dialysate Blood from the Patient Used Dialysate Healthy Kidney Diseased Kidney Physical Basis Renal Replacement
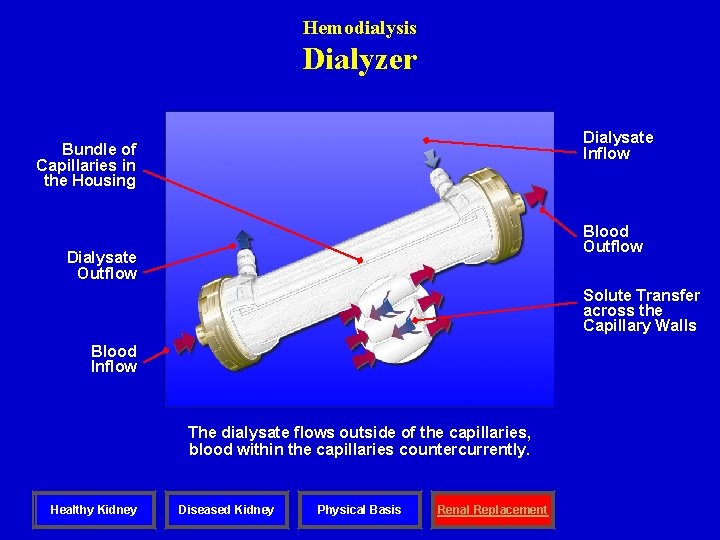
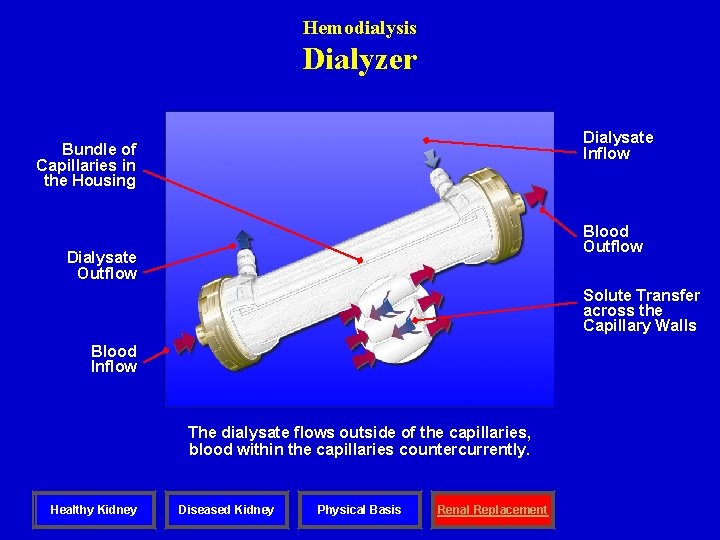
Hemodialysis Dialyzer Dialysate Inflow Bundle of Capillaries in the Housing Blood Outflow Dialysate Outflow Solute Transfer across the Capillary Walls Blood Inflow The dialysate flows outside of the capillaries, blood within the capillaries countercurrently. Healthy Kidney Diseased Kidney Physical Basis Renal Replacement
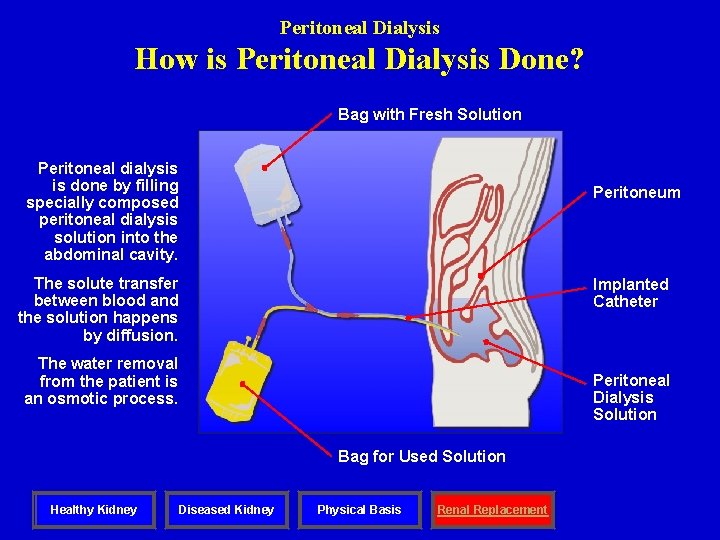
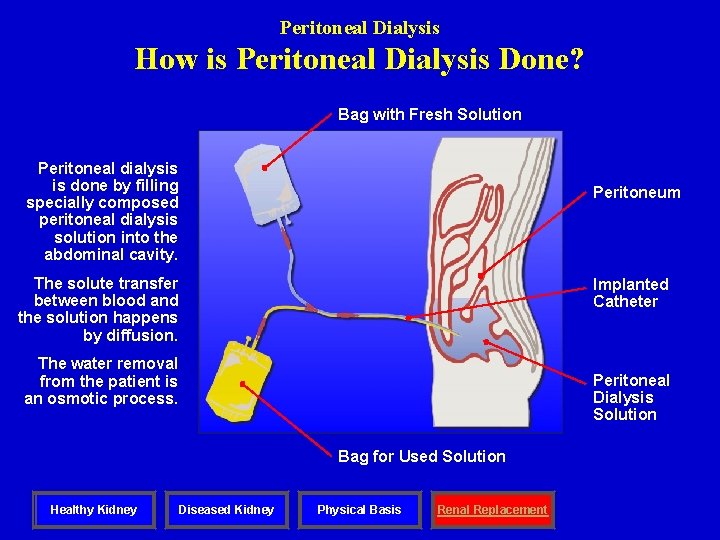
Peritoneal Dialysis How is Peritoneal Dialysis Done? Bag with Fresh Solution Peritoneal dialysis is done by filling specially composed peritoneal dialysis solution into the abdominal cavity. Peritoneum The solute transfer between blood and the solution happens by diffusion. Implanted Catheter The water removal from the patient is an osmotic process. Peritoneal Dialysis Solution Bag for Used Solution Healthy Kidney Diseased Kidney Physical Basis Renal Replacement
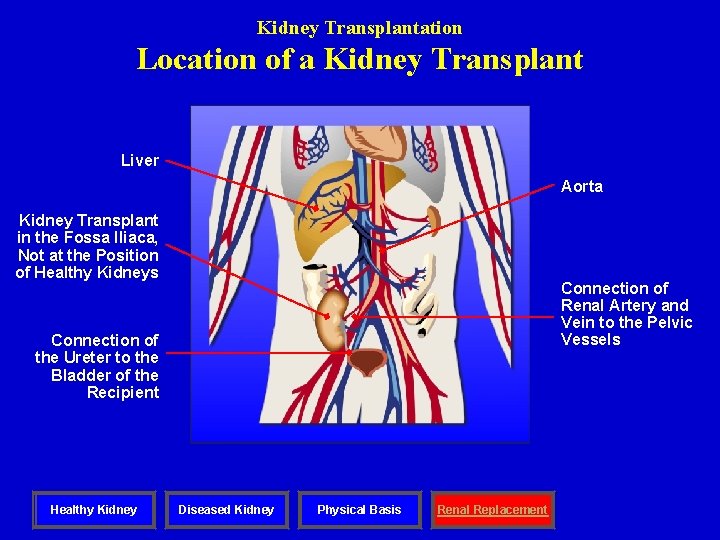
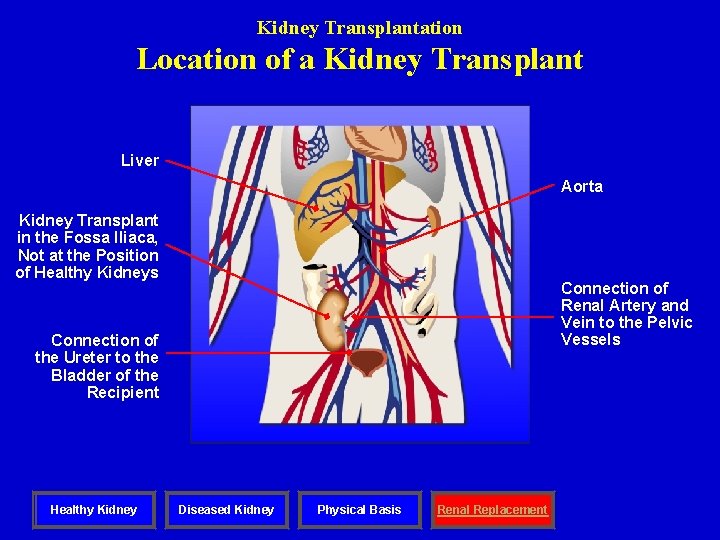
Kidney Transplantation Location of a Kidney Transplant Liver Aorta Kidney Transplant in the Fossa Iliaca, Not at the Position of Healthy Kidneys Connection of Renal Artery and Vein to the Pelvic Vessels Connection of the Ureter to the Bladder of the Recipient Healthy Kidney Diseased Kidney Physical Basis Renal Replacement