Chronic Obstructive Pulmonary Disease Philip Kiely pcdk 1

Chronic Obstructive Pulmonary Disease Philip Kiely pcdk 1 e 08@soton. ac. uk
Outline § Go through COPD using DAPSICAMP § Focus on understanding pathophysiology and clinical features § Obstructive vs. Restrictive Lung Disease § Respiratory Failure 2
DAPSICAMP Definition Aetiology Pathophysiology Signs and symptoms Investigations Complications Alternative diagnoses Management Prognosis 3
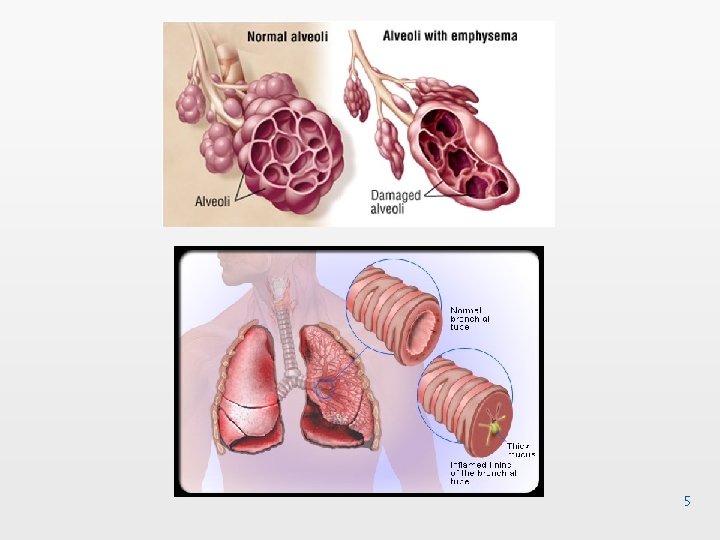
§ Definition: COPD is an umbrella term for a spectrum of diseases that result in non-reversible airflow limitation § Typically a combination of chronic bronchitis and emphysema § Chronic bronchitis = a productive cough on most days for 3 months in 2 consecutive years § Emphysema = destruction of airspaces distal to the terminal bronchiole 4
5
Facts and stats § COPD represents long-term damage caused by inhaled irritants § Cigarette smoking is the predominant risk factor § Prevalence of 1. 5 million; mortality 23, 000 per year in the UK § By 2020, it is predicted to become third leading cause of death worldwide § Currently causes 1 in 8 hospital admissions 6
Pathophysiology § Damage to the airways results in mucus gland hypertrophy and goblet cell hyperplasia § Inflammation which over time progresses to fibrosis and scarring § Air becomes trapped in the lungs due to mucus plugging of small airways and loss of connective tissue 7
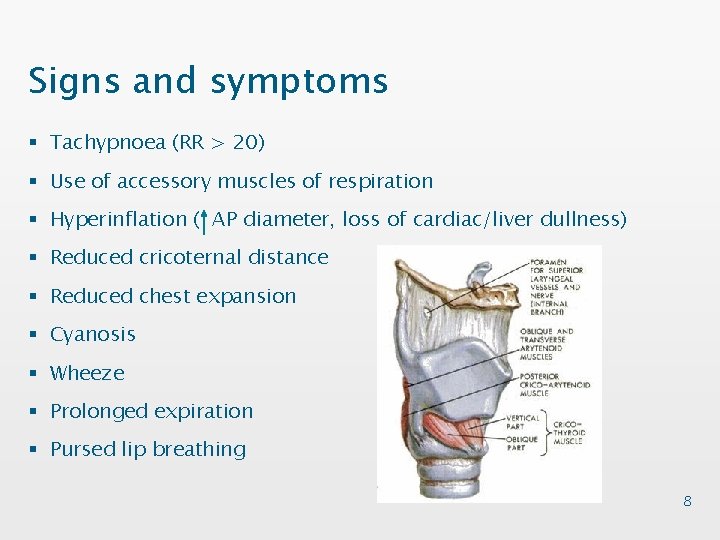
Signs and symptoms § Tachypnoea (RR > 20) § Use of accessory muscles of respiration § Hyperinflation ( AP diameter, loss of cardiac/liver dullness) § Reduced cricoternal distance § Reduced chest expansion § Cyanosis § Wheeze § Prolonged expiration § Pursed lip breathing 8
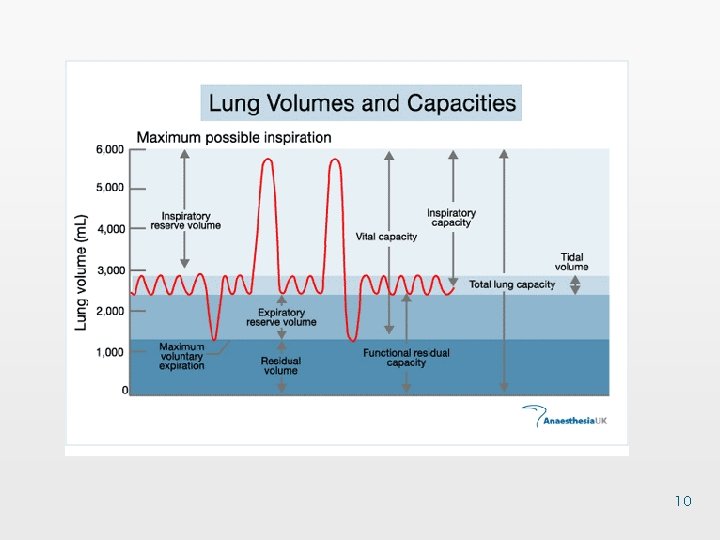
Investigations § Bedside - Spirometry - (FVC < 80% predicted, FEV 1: FVC < 70%) § Bloods - normocytic normchromic anaemia (low Hb, normal MCV), raised PCV (> 45%) § Imaging - CXR - hyperinflation, spherical heart, decreased peripheral vascular markings 9
10

11
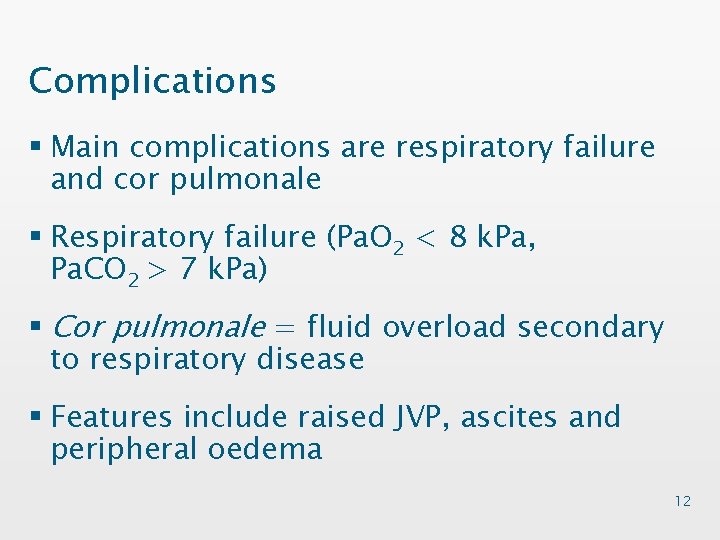
Complications § Main complications are respiratory failure and cor pulmonale § Respiratory failure (Pa. O 2 < 8 k. Pa, Pa. CO 2 > 7 k. Pa) § Cor pulmonale = fluid overload secondary to respiratory disease § Features include raised JVP, ascites and peripheral oedema 12
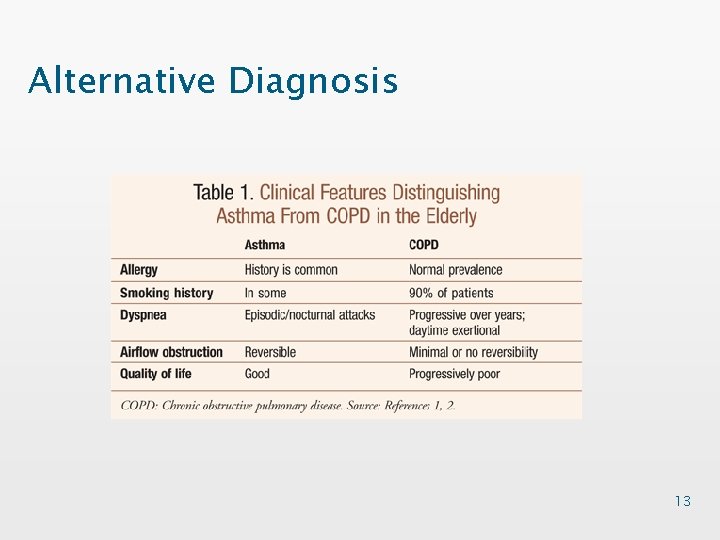
Alternative Diagnosis 13
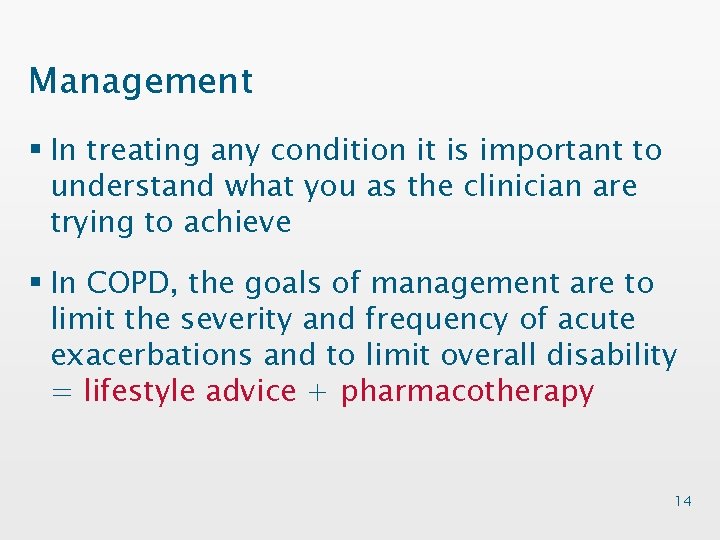
Management § In treating any condition it is important to understand what you as the clinician are trying to achieve § In COPD, the goals of management are to limit the severity and frequency of acute exacerbations and to limit overall disability = lifestyle advice + pharmacotherapy 14
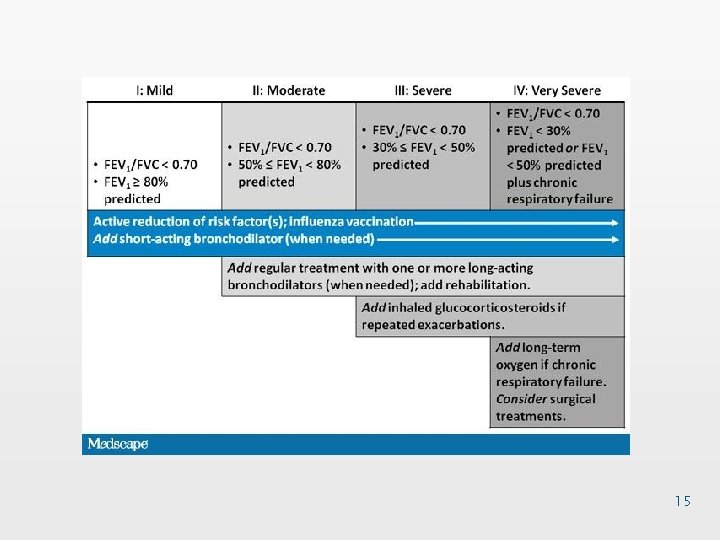
15
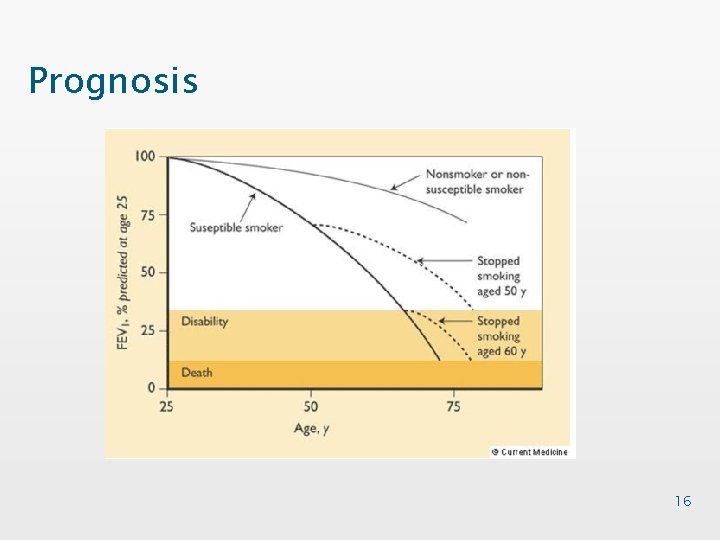
Prognosis 16

Obstructive vs. Restrictive Lung Disease § Obstructive = inability to get air out § Restrictive = inability to get air in § Obstructive lung disease: COPD, Asthma, Bronchiectasis, CF PEFR, FVC, FEV 1: FVC § Restrictive Lung Disease: Fibrosis (2º to radiation, medication, asbestos exposure) FEV 1, FVC, but normal FEV 1: FVC ratio 17
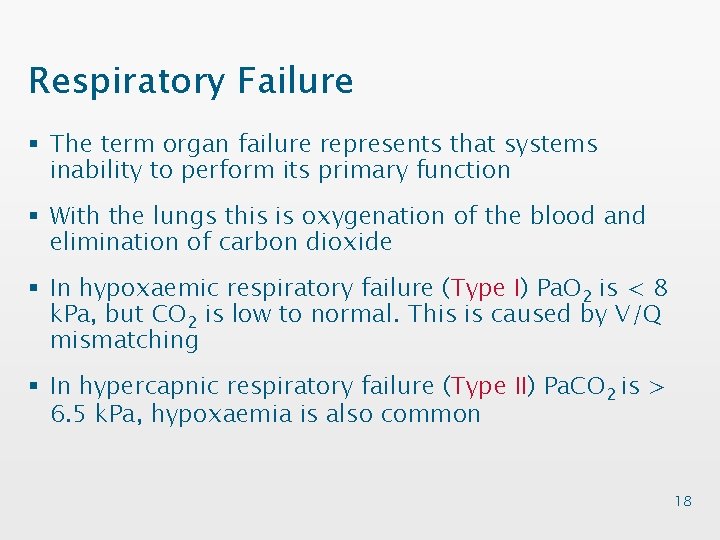
Respiratory Failure § The term organ failure represents that systems inability to perform its primary function § With the lungs this is oxygenation of the blood and elimination of carbon dioxide § In hypoxaemic respiratory failure (Type I) Pa. O 2 is < 8 k. Pa, but CO 2 is low to normal. This is caused by V/Q mismatching § In hypercapnic respiratory failure (Type II) Pa. CO 2 is > 6. 5 k. Pa, hypoxaemia is also common 18
- Slides: 18