Chronic Obstructive Pulmonary Disease COPD Dr K V
Chronic Obstructive Pulmonary Disease (COPD) Dr. K. V. CHALAPATHI RAO PROFESSOR DEARTMENT OF GENERAL HOSPITAL ASRAM MEDICAL COLLEGE
Overview • • • Definition Burden of COPD Types Pathology & Pathogenesis Risk factors Clinical features Diagnosis Treatment Complications
Definition • The GOLD document states that “COPD is a common, preventable and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities, usually caused by significant exposure to noxious particles or gases. ”
Burden of COPD • COPD is the leading cause of morbidity & mortality worldwide that includes both economic and social burden. • Prevalance of COPD is increasing every year. • Mortality associated with COPD is around 3 million deaths every year and this is projected to increase significantly in the time to come. • COPD causes significant morbidity.
Types of COPD • • Chronic bronchitis predominant COPD Emphysema predominant COPD These terminologies are not used frequently these days. Phenotyping of COPD is also done. Phenotype guided treatment of COPD will be the future.
Pathology • Pathology of COPD is seen in airways, lung parenchyma & pulmonary vasculature. • Pathological changes in COPD include chronic inflammation with different types of inflammatory cells and damage of airways that is proportional to duration of COPD.
Pathogenesis • Inflammation observed in the respiratory tract of COPD patients is modification of normal inflammatory response to smoke, noxious gasses. • Mechanisms of this exaggerated inflammatory response are poorly understood. However, the following mechanisms may contribute – 1. Oxidative stress 2. Protease-Antiprotease imbalance 3. Inflammatory cells 4. Inflammatory mediators 5. Peri bronchiolar and Interstitial fibrosis.
Risk factors • • • Smoking of cigarettes or beedi or hookah Biomass fuel smoke exposure Exposure to noxious gasses and fumes Exposure to air pollution Occupational exposure to dusts or gasses Host factors such as alpha 1 anti-trypsin deficiency
Clinical features • Presence of cough, usually productive. • Breathlessness (m. MRC staging) • Weakness and fatigue • • Exacerbation of COPD – Presence of severe breathing difficulty Cough Expectoration
Key indicators for considering diagnosis of COPD 1. Dyspnea that is. Progressive over time * Characteristically worse with exercise * Persistent 2. Chronic cough – * Usually productive * May be intermittent and may be unproductive * Recurrent wheeze 3. Chronic Sputum production Any pattern of chronic sputum production may indicate COPD 4. Recurrent lower respiratory tract infections 5. History of risk factors -* Host factors* Tobacco smoke and other smoke 6. Family history of COPD and/or childhood factors -* low birthweight * Childhood respiratory tract infections
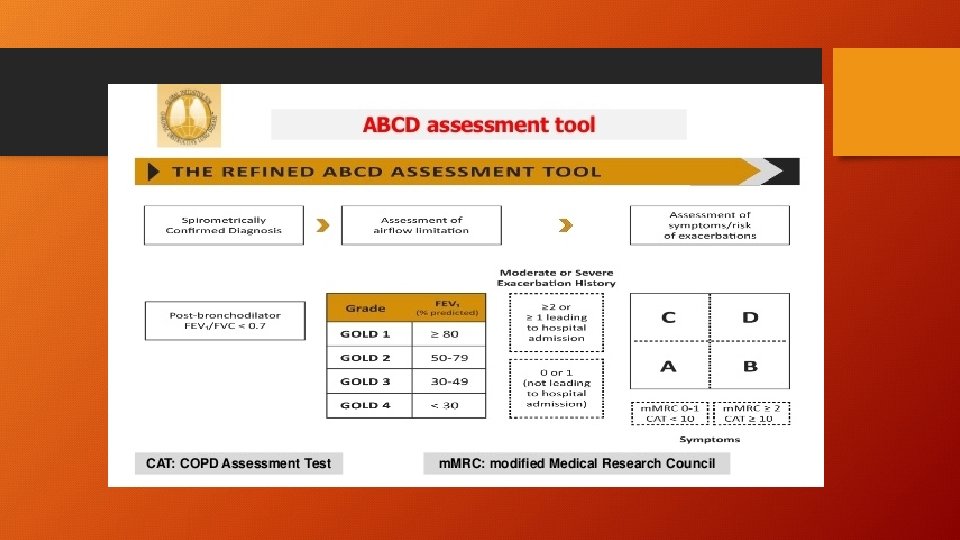
Diagnosis and staging of COPD 1. Spirometry Role – • Diagnosis • Severity of airflow limitation (Prognosis) • Followup assessment 2. m. MRC grading dyspnea and score that are included in refined ABCD assesment tool.
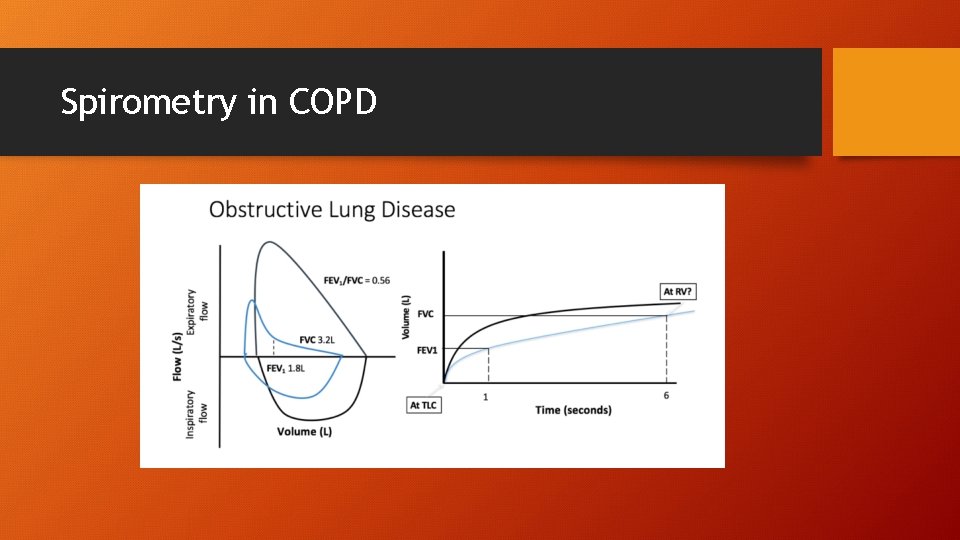
Spirometry in COPD
Additional investigations 1. 2. 3. 4. 5. 6. Imaging – CXR and CT Lung volumes & Diffusing capacity Pulse oximetry & ABG Exercise testing & Assessment if physical activity Composite scores- BODE index Biomarkers
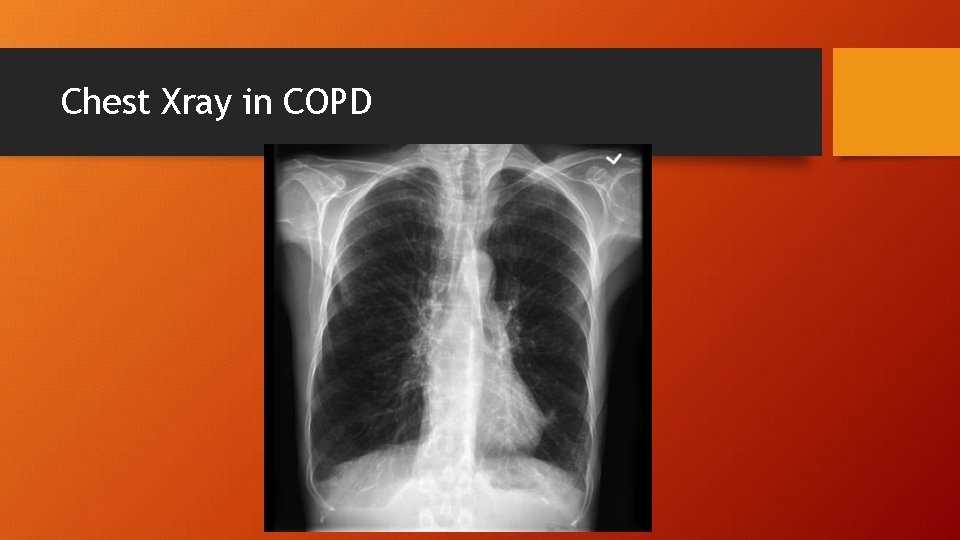
Chest Xray in COPD
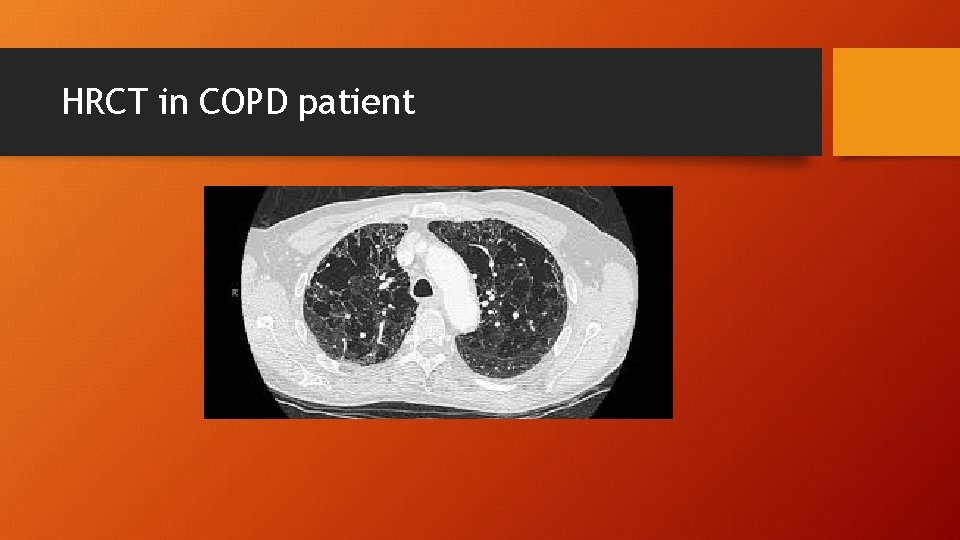
HRCT in COPD patient
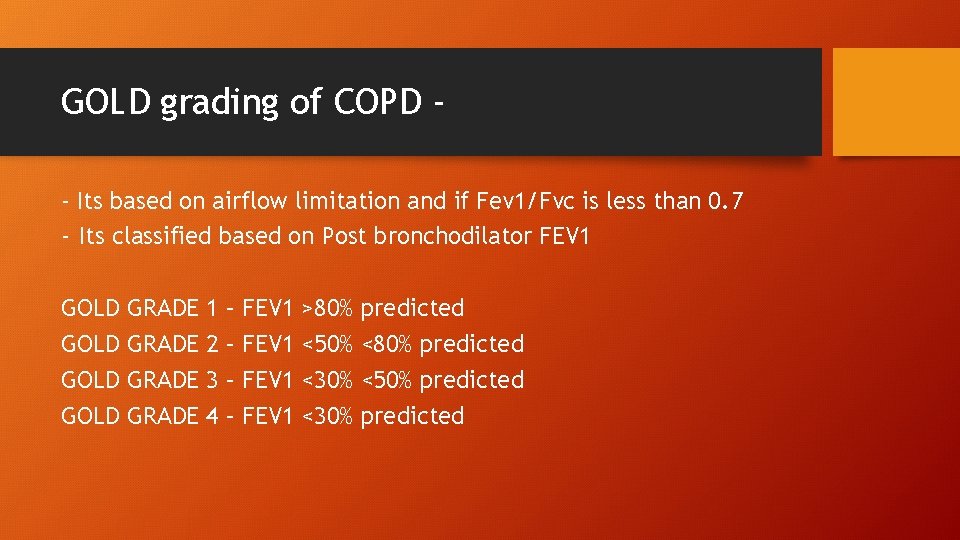
GOLD grading of COPD - Its based on airflow limitation and if Fev 1/Fvc is less than 0. 7 - Its classified based on Post bronchodilator FEV 1 GOLD GRADE 1 2 3 4 – – FEV 1 >80% <50% <30% predicted <80% predicted <50% predicted
Differential diagnosis of COPD • • • Asthma Congestive Heart Failure Bronchiectasis Tuberculosis Obliterative bronchiolitis Diffuse panbronchiolitis
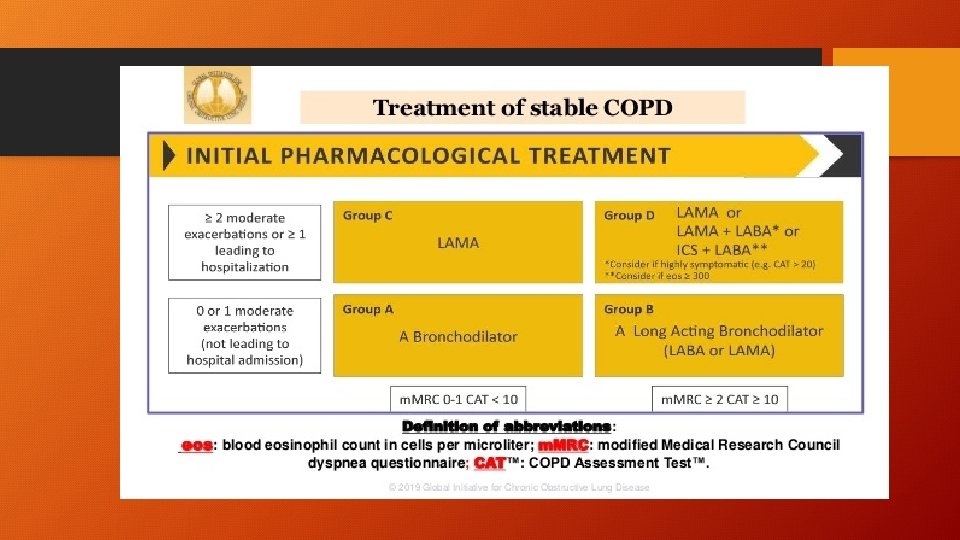
Treatment • Bronchodilators – Beta 2 agonists – LABA, SABA Anti muscarinic agents – LAMA, SAMA • Anti inflammatory medications – 1. Inhalational corticosteroids 2. Oral glucocorticoids 3. PDE 4 inhibitors – Roflumilast 4. Antibiotics such as Azithromycin, Erythromycin 5. Mucoregulators and other Antioxidants – NAC 6. Other anti inflammatory medications
Beta 2 agonists • Salbutamol – acts on beta 2 receptors, acts for 4 -6 hours with a good bronchodilator action. • Levo salbutamol – better than salbutamol, it is efficacious and has less side effects such as tremors, tachycardia, acts for 4 -8 hours • Salmeterol – acts for upto 12 hours on beta 2 receptors, long acting beta 2 agonist. • Formeterol – acts for 12 hours on beta 2 receptors. • Indacetrol & Vilanterol – acts for upto 24 hours
Muscarinic antagonists • Ipratropium – Short acting muscarinic antagonist – acts for 4 -8 hours • Tiotropium – Long acting – upto 24 hours – side effects – dry mouth and urinary retention in few. • Glycopyrronium – acts for 24 hours • Ultra long acting – Umeclidinium – acts for more than 24 hours- yet to reach india.
Inhalational corticosteroids • • Budesonide – most commonly used Fluticasone propionate – most potent ICS Beclamethasone – smallest diameter of less than 2 microns Cyclosenide- pre drug, gets activated in lungs, therefore cannot cause oral candidiasis
Add on medications • PDE 4 inhibitor – Roflumilast • Theophyllines – Acerebrophylline – multiple mechanisms of action • Mucolytics - N-acetyl cysteine
Additional management • Education, Self management • Pulmonary Rehabilitation • Supportive, palliative care ---Other Therapies – • Oxygen therapy – LTOT • Ventilator support • Interventional therapy such as lung volume reduction surgery (LVRS), Bullectomy, Lung transplantation.
Prevention & Maintenance Therapy • • • Smoking cessation Vaccination Maintenance inhalers Additional therapy with medications Nutritional rehabilitation
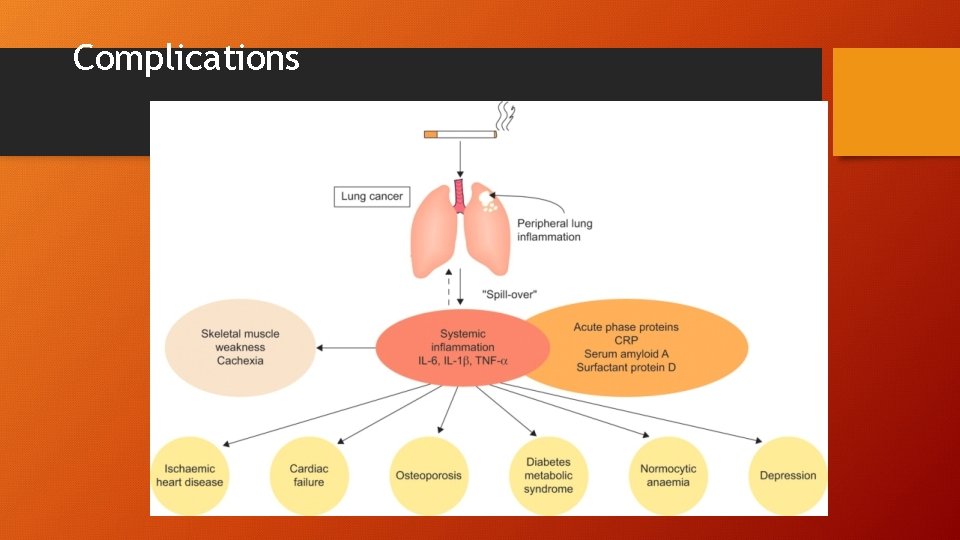
Complications
Treatment of complications • It is important to address complications in COPD 1. Skeletal muscle wasting – High protein diet and pulmonary rehabilitation 2. Depression – Anti depressants 3. IHD & Heart failure – supportive cardiac care 4. Lung cancer – screen annually to look for any lung nodules or mass 5. Osteoporosis – Calcium and vit D 3 supplements 6. Diabetes and metabolic syndrome – control of diabetes, anti oxidants etc.
Treat from all aspects – Holistic approach • • Cessation of smoking or exposure to smoke Pharmacotherapy & vaccines Rehabilitation – Pulmonary, Physical, Nutritional & psychological Emotional support
Thank you
- Slides: 30