Chronic Myeloid Leukemia Amer Rassam M D Learning

- Slides: 61
Chronic Myeloid Leukemia Amer Rassam, M. D.
Learning Objectives v Myeloproliferative v Molecular disorders (MPDs) genetics of chronic myeloid leukemia v Clinical manifestations and diagnosis of chronic myeloid leukemia v Overview of the treatment of chronic myeloid leukemia v Initial treatment of chronic myeloid leukemia in chronic phase
Learning Objectives v Explain how to define and identify a relapse v Treatment of CML in chronic phase after failure of initial therapy v Clinical use of tyrosine kinase inhibitors for chronic myeloid leukemia v Treatment blast crisis v Prognosis of CML in accelerated phase and
Myeloproliferative Disorders v Chronic Myeloid Leukemia (CML) v Polycythemia Vera (PCV) v Essential Thrombocythemia (ET) v Primary Myelofibrosis (PMF)
Myeloproliferative Disorders v Clonal disorders of hematopoiesis that arise in hematopoietic stem or early progenitor cell. v Characterized by the dysregulated production of particular lineage of mature myeloid cells with fairly normal maturation. v Exhibit a variable tendency to progress to acute leukemia v Share abnormalities of hemostasis and thrombosis v Overlap between the clinical features
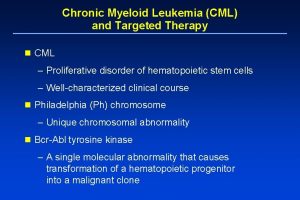
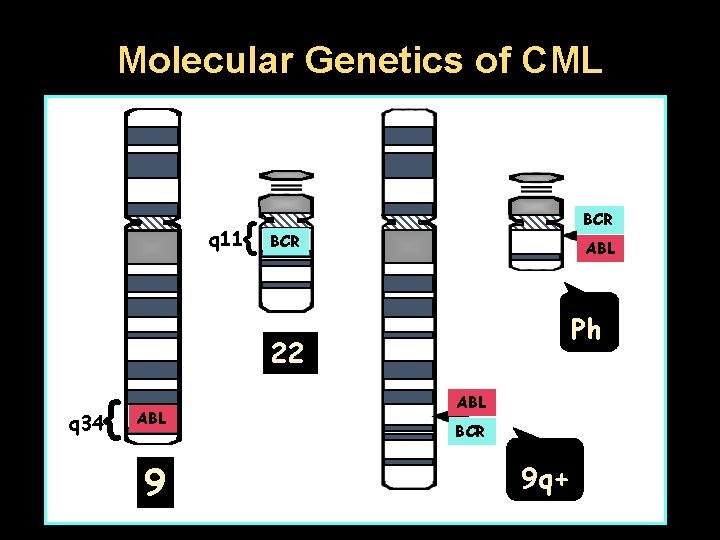
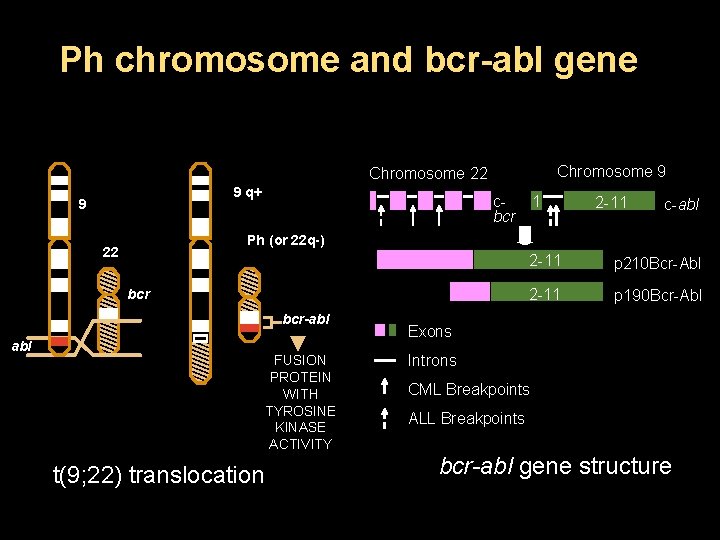
Introduction v CML is a clonal myeloproliferative neoplasm v Dysregulated production and uncontrolled proliferation of mature and maturing granulocyte with fairly normal differentiation v Fusion of 2 genes: BCR (or chromosome 22) and ABL 1 (on chromosome 9), resulting in BCR-ABL 1 fusion gene v Final result: Abnormal chromosome 22 called Philadelphia (Ph) chromosome v Final product: BCR-ABL 1 fusion protein, a dysregulated tyrosine kinase
Introduction v Uncontrolled production of mature and maturing granulocytes v Predominantly neutrophils, but also basophils and eosinophils v Triphasic or biphasic clinical course v Chronic phase, accelerated phase, blast crisis
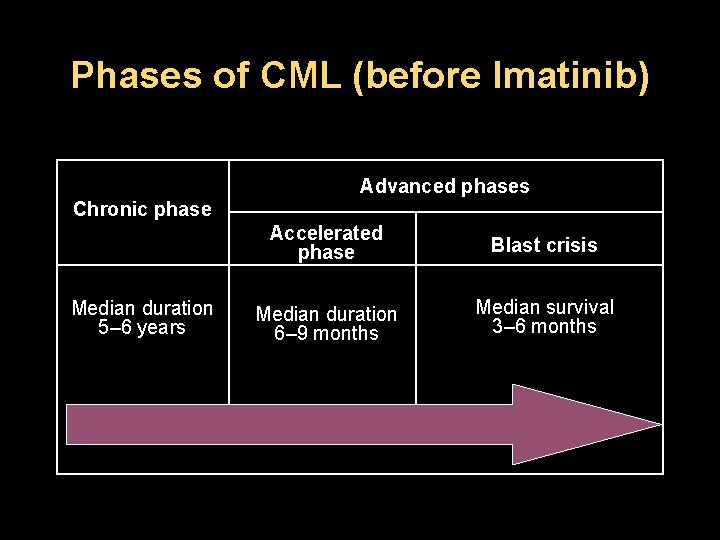
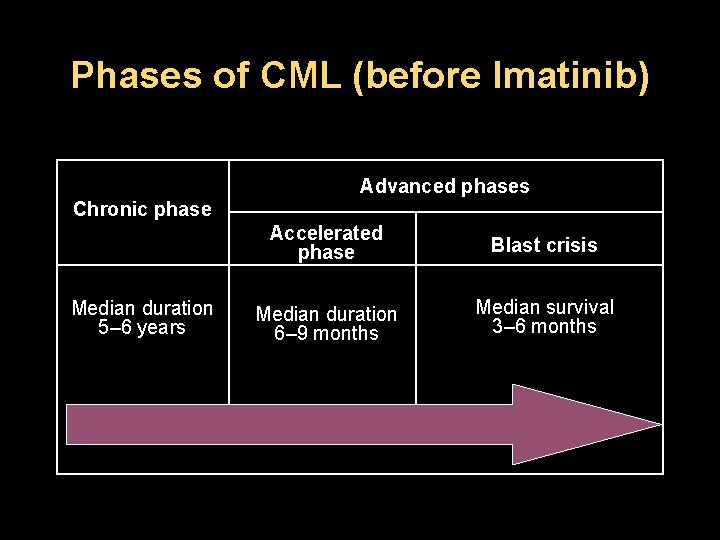
Phases of CML (before Imatinib) Advanced phases Chronic phase Median duration 5– 6 years Accelerated phase Blast crisis Median duration 6– 9 months Median survival 3– 6 months
Epidemiology v Annual v 15% incidence: 1 to 2 cases per 100, 000 – 20% of all adult leukemias v Incidence increases significantly with age – Median age: ~ 55 years – Prevalence increasing due to current therapy – Most patients present in CP, 85% • Majority of CML-related deaths due to progression to AP/BC – 50% of CML patients are asymptomatic at diagnosis v Risk factors – Exposure to ionizing radiation, the only known
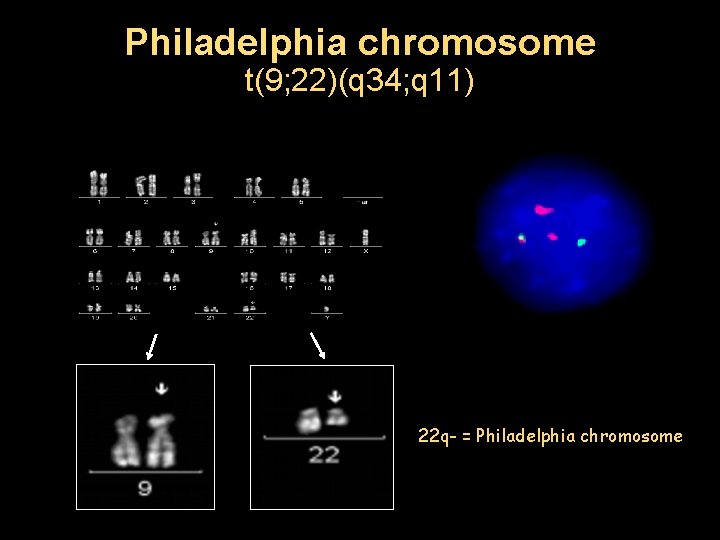
Molecular Genetics of CML v The Philadelphia chromosome was originally detected by workers in Philadelphia. v The first genetic abnormality to be associated with a human cancer. v The result of a balanced translocation between chromosomes 9 and 22. v Derivative chromosome 22 is significantly smaller v Ph chromosome is present in hematopoietic cells from patients with CML. v Therefore, the Ph chromosome is acquired and NOT inherited through the germline.
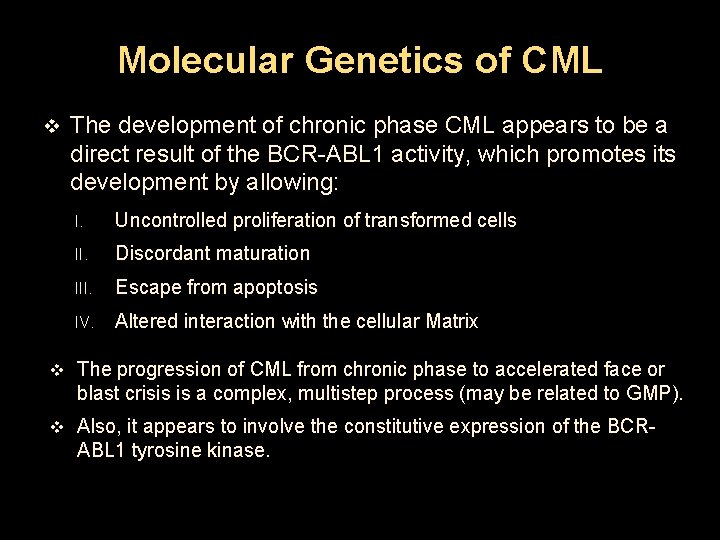
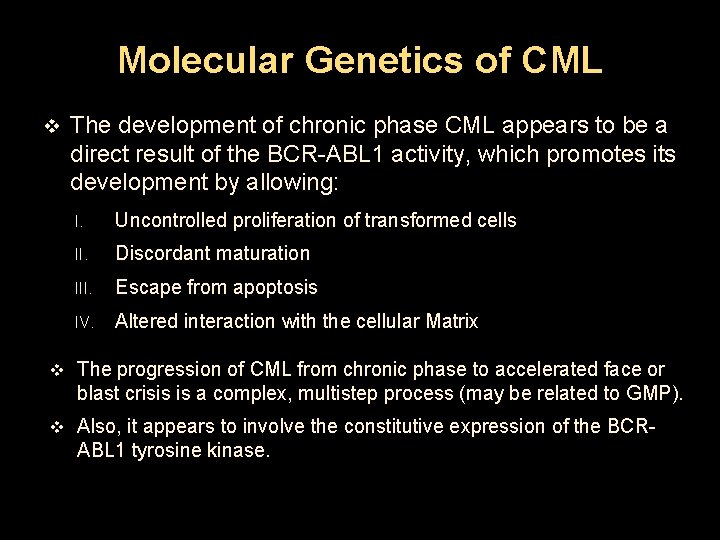
Molecular Genetics of CML v The development of chronic phase CML appears to be a direct result of the BCR-ABL 1 activity, which promotes its development by allowing: I. Uncontrolled proliferation of transformed cells II. Discordant maturation III. Escape from apoptosis IV. Altered interaction with the cellular Matrix v The progression of CML from chronic phase to accelerated face or blast crisis is a complex, multistep process (may be related to GMP). v Also, it appears to involve the constitutive expression of the BCRABL 1 tyrosine kinase.
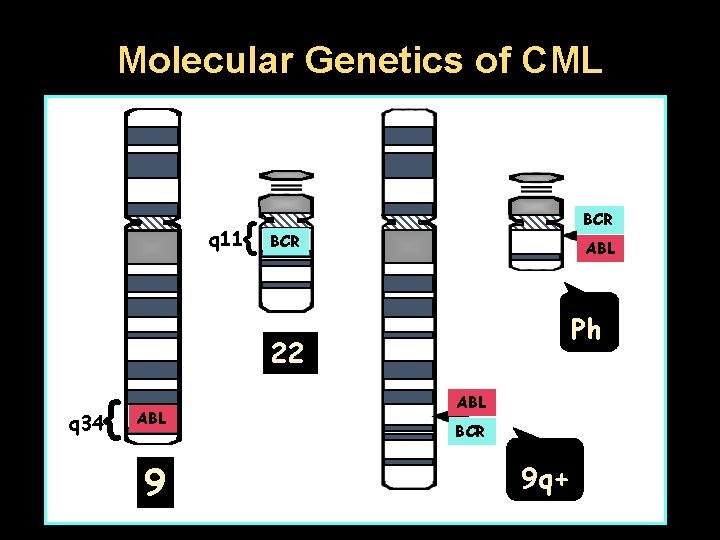
Molecular Genetics of CML { q 11 BCR ABL Ph 22 { q 34 ABL 9 ABL BCR 9 q+
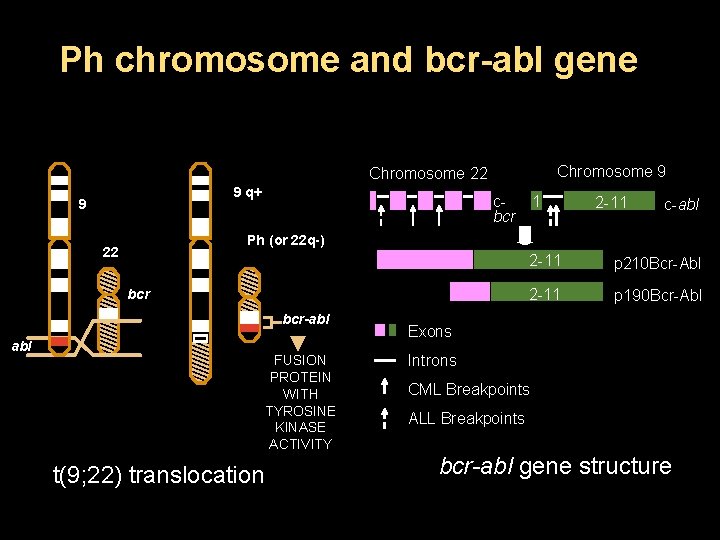
Ph chromosome and bcr-abl gene Chromosome 9 Chromosome 22 9 q+ 9 cbcr 1 2 -11 c-abl Ph (or 22 q-) 22 bcr-abl FUSION PROTEIN WITH TYROSINE KINASE ACTIVITY t(9; 22) translocation 2 -11 p 210 Bcr-Abl 2 -11 p 190 Bcr-Abl Exons Introns CML Breakpoints ALL Breakpoints bcr-abl gene structure
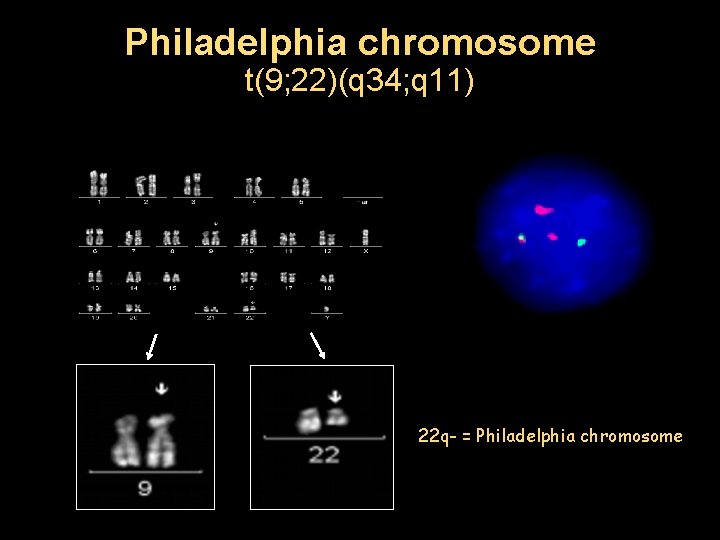
Philadelphia chromosome t(9; 22)(q 34; q 11) 22 q- = Philadelphia chromosome
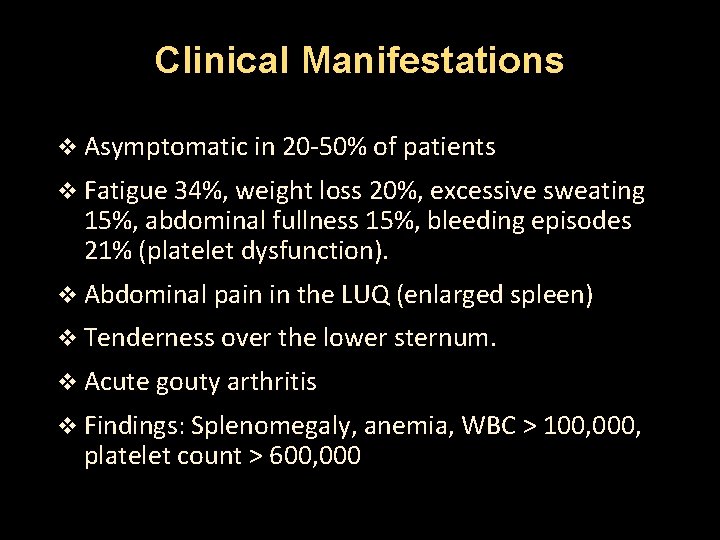
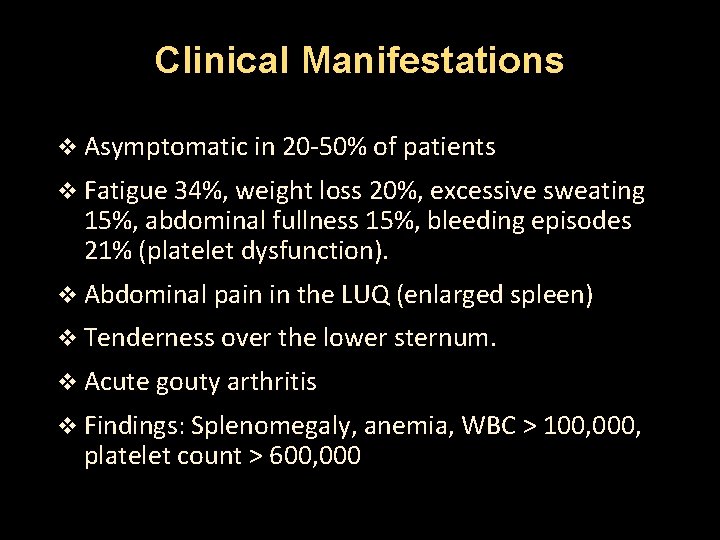
Clinical Manifestations v Asymptomatic in 20 -50% of patients v Fatigue 34%, weight loss 20%, excessive sweating 15%, abdominal fullness 15%, bleeding episodes 21% (platelet dysfunction). v Abdominal pain in the LUQ (enlarged spleen) v Tenderness over the lower sternum. v Acute gouty arthritis v Findings: Splenomegaly, anemia, WBC > 100, 000, platelet count > 600, 000
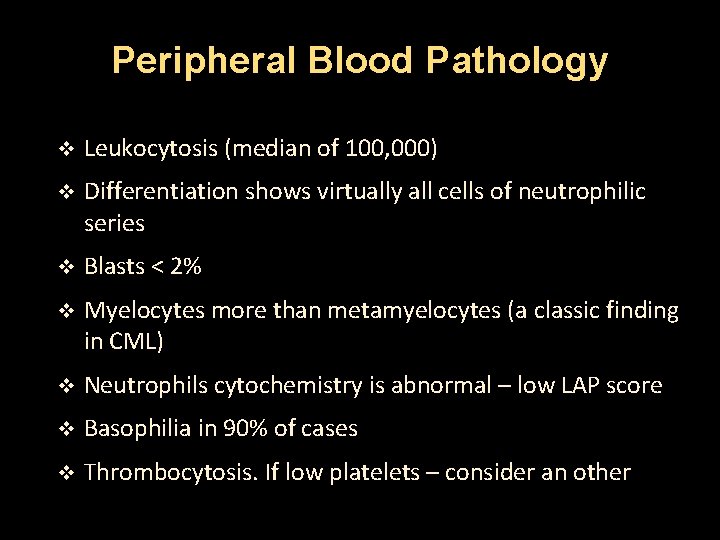
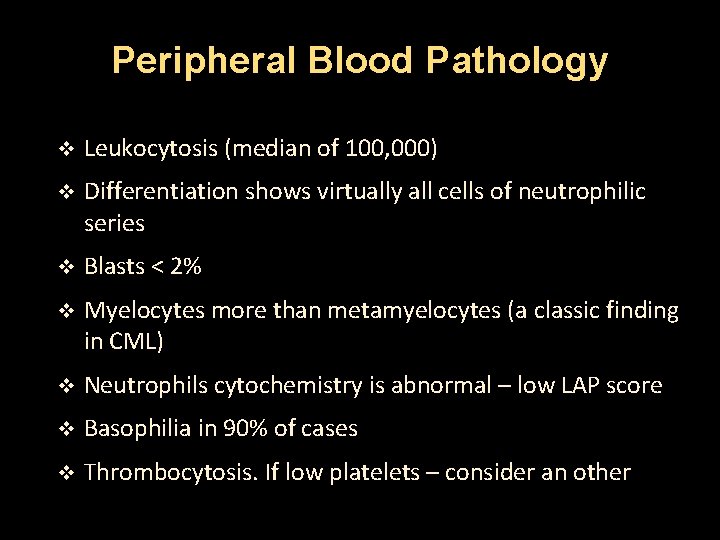
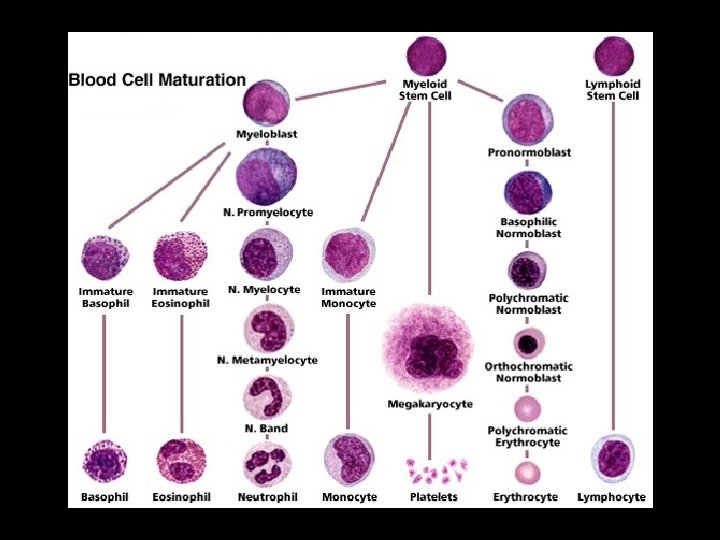
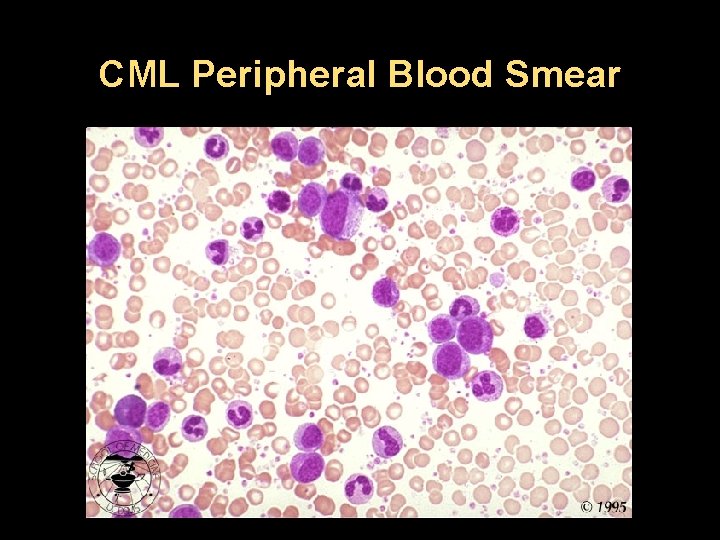
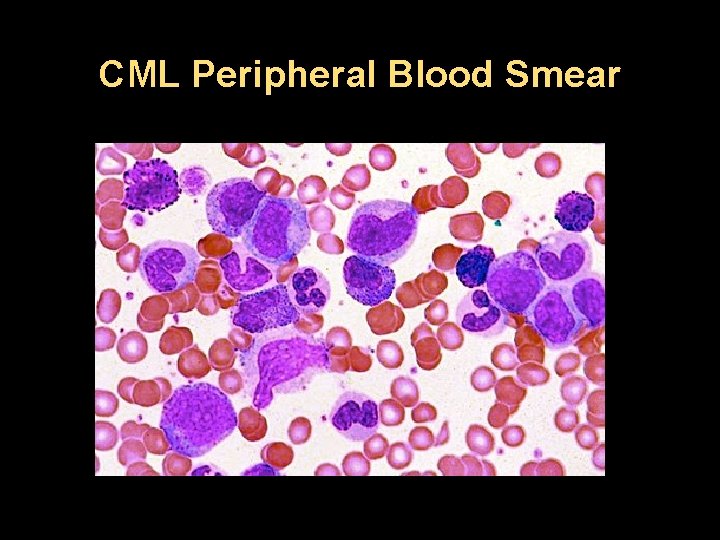
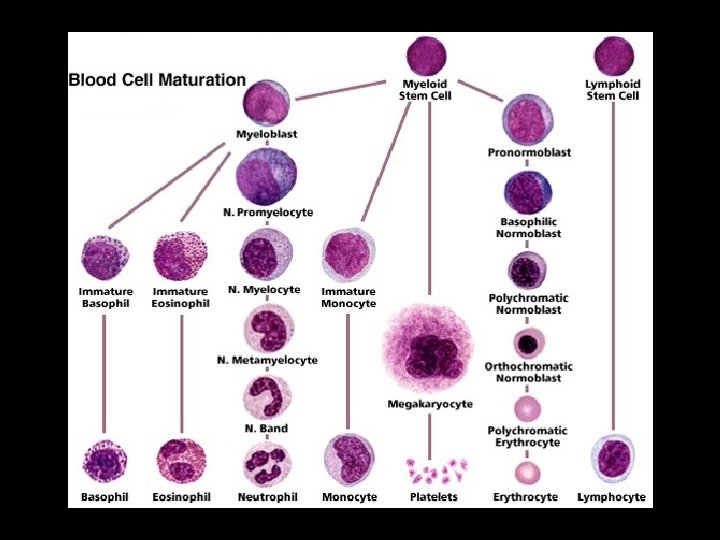
Peripheral Blood Pathology v Leukocytosis (median of 100, 000) v Differentiation shows virtually all cells of neutrophilic series v Blasts < 2% v Myelocytes more than metamyelocytes (a classic finding in CML) v Neutrophils cytochemistry is abnormal – low LAP score v Basophilia in 90% of cases v Thrombocytosis. If low platelets – consider an other
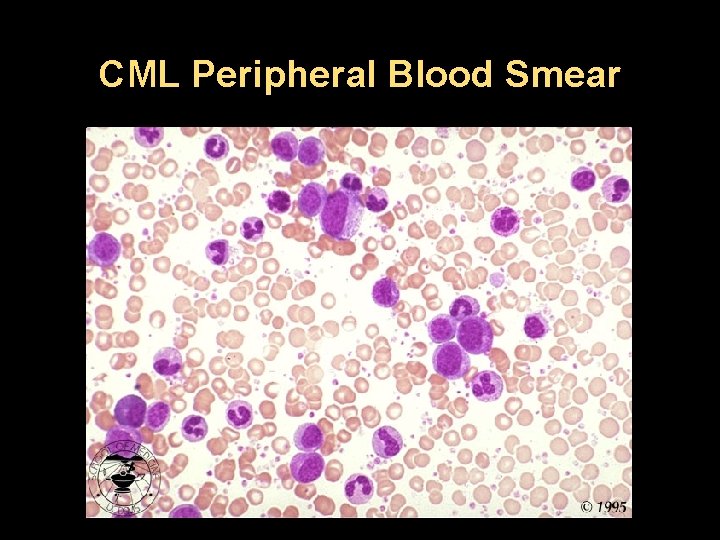
CML Peripheral Blood Smear
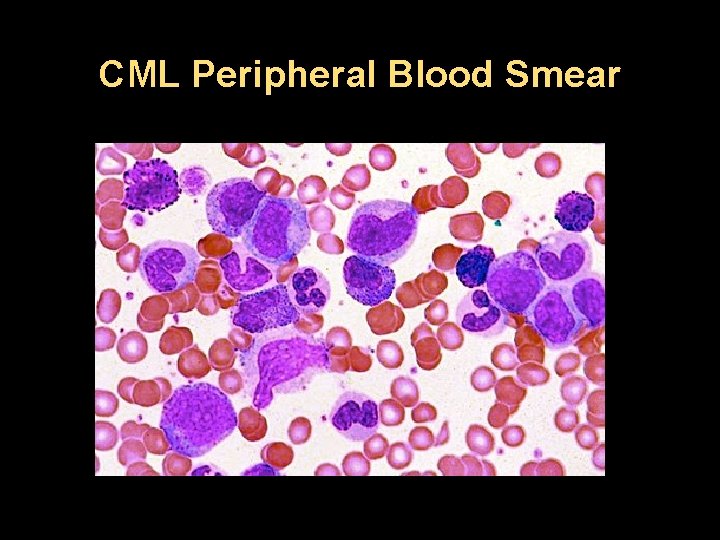
CML Peripheral Blood Smear
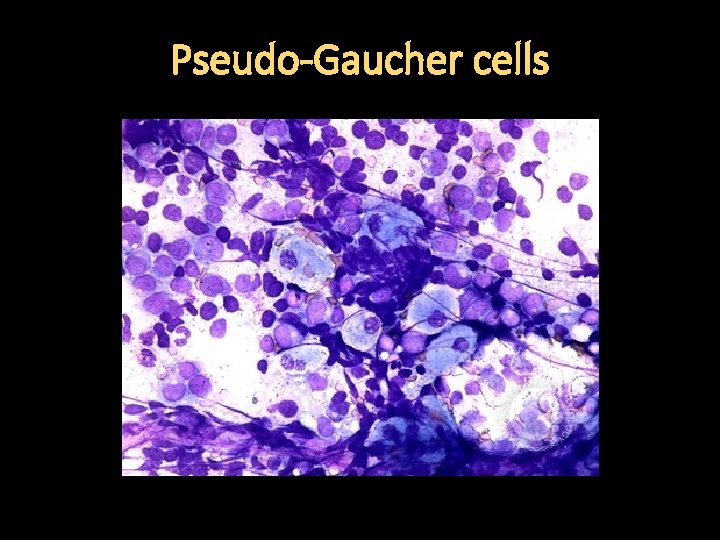
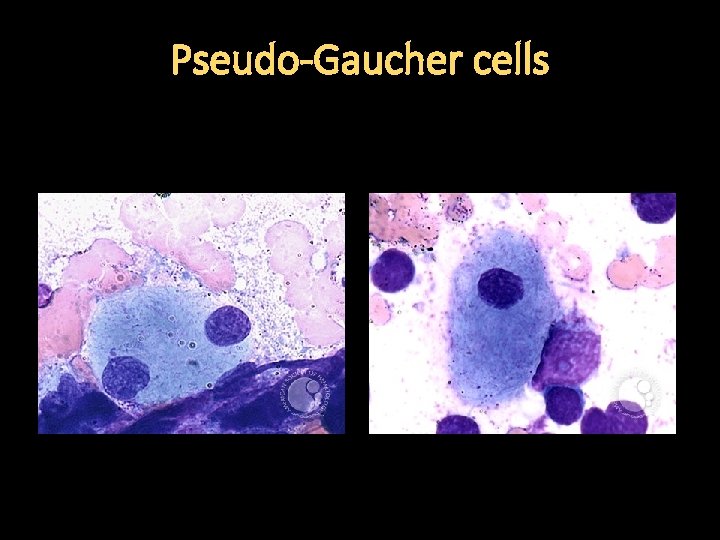
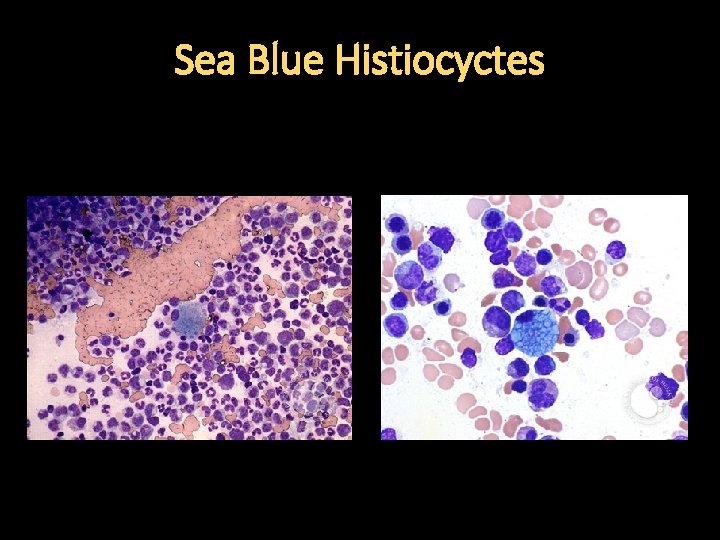
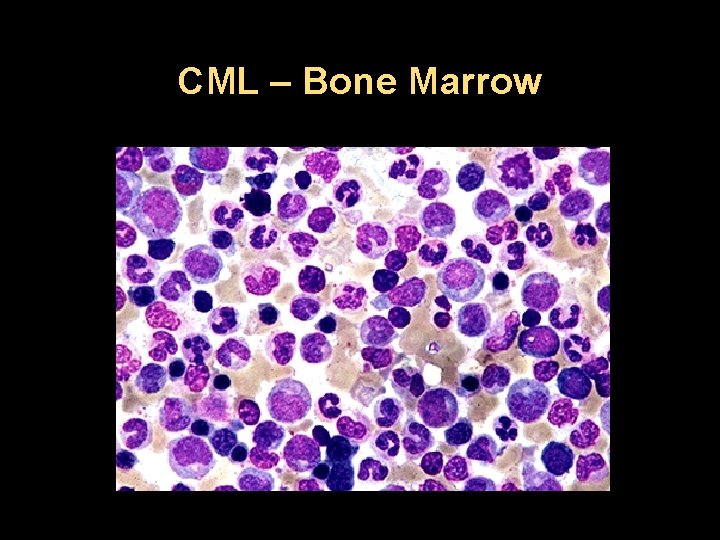
Bone Marrow Pathology v Granulocytic maturation pattern same as in the peripheral blood v Increased reticulin fibrosis and vascularity v Erythroid islands are reduced in number and size v Dwarf megakaryocytes v Pseudo-Gaucher’s cells and Sea Blue histiocytes (markers of increased cell turnover) v Iron-laden macrophages are reduced or absent
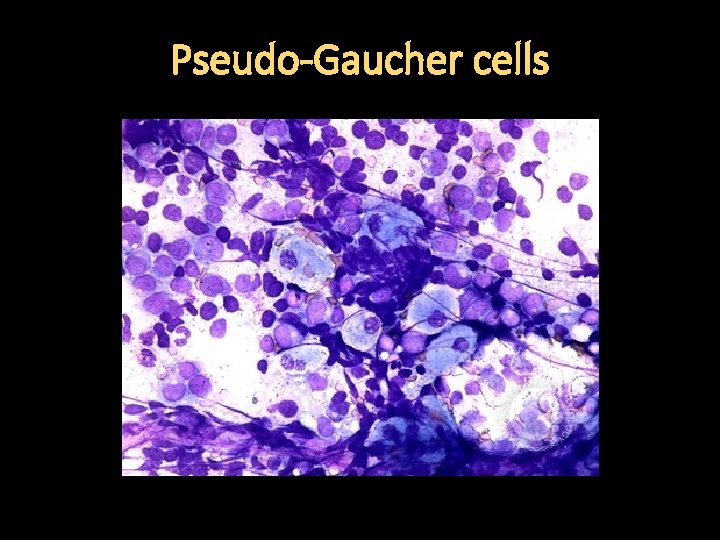
Pseudo-Gaucher cells
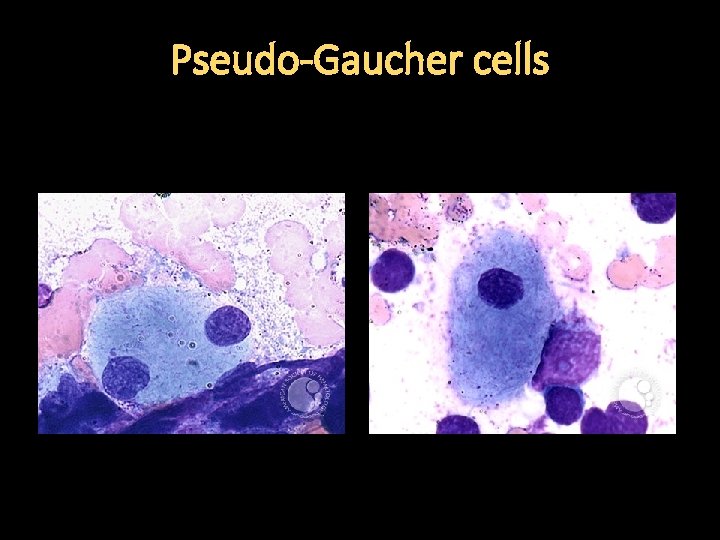
Pseudo-Gaucher cells
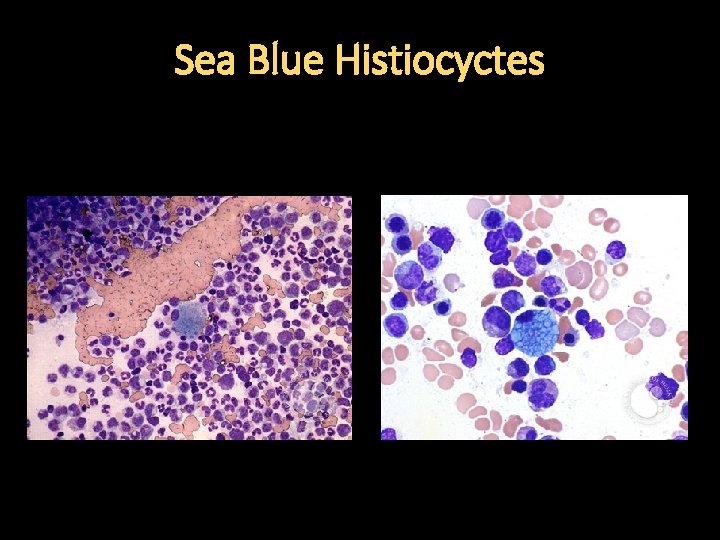
Sea Blue Histiocyctes
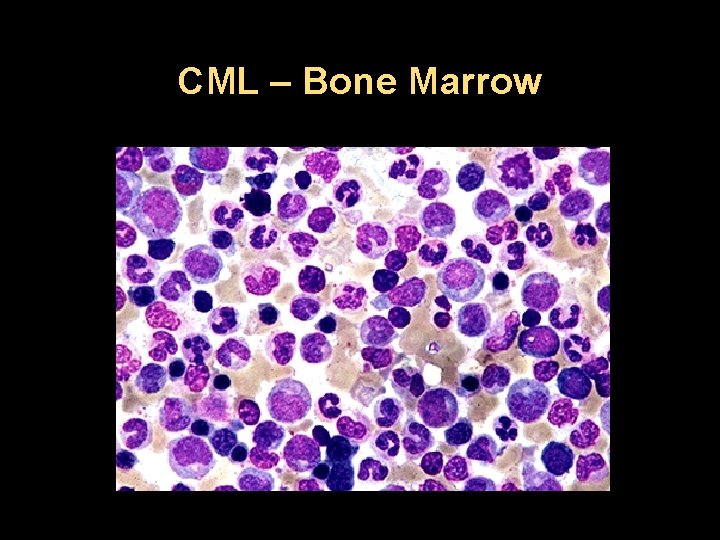
CML – Bone Marrow
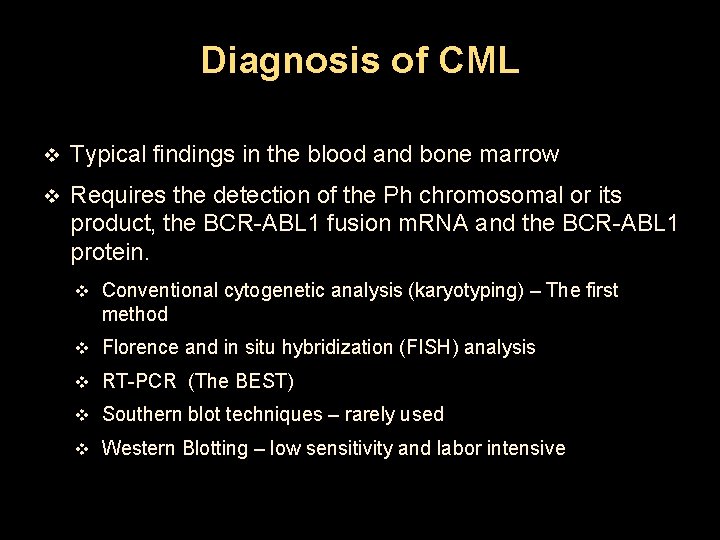
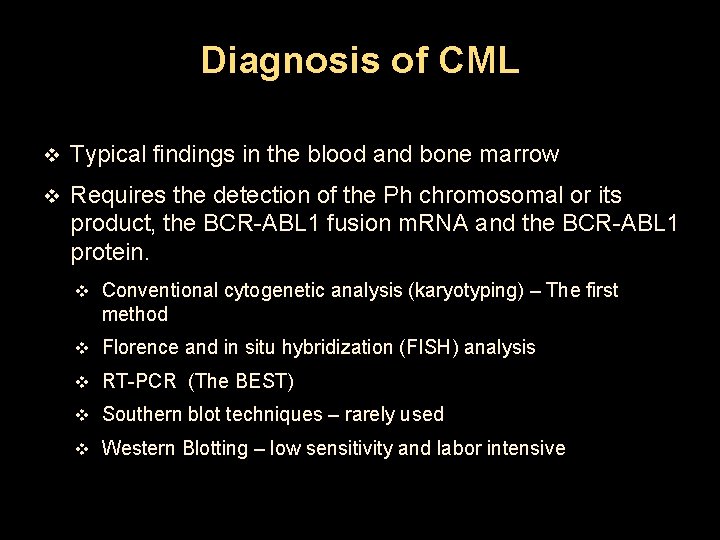
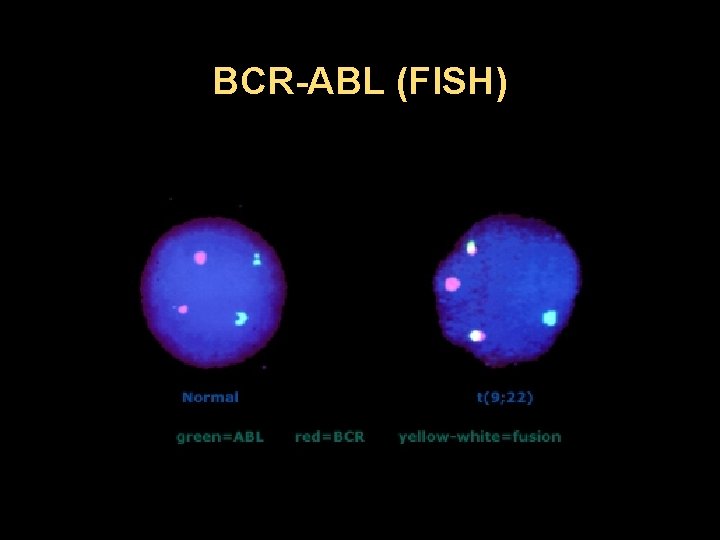
Diagnosis of CML v Typical findings in the blood and bone marrow v Requires the detection of the Ph chromosomal or its product, the BCR-ABL 1 fusion m. RNA and the BCR-ABL 1 protein. v Conventional cytogenetic analysis (karyotyping) – The first method v Florence and in situ hybridization (FISH) analysis v RT-PCR (The BEST) v Southern blot techniques – rarely used v Western Blotting – low sensitivity and labor intensive
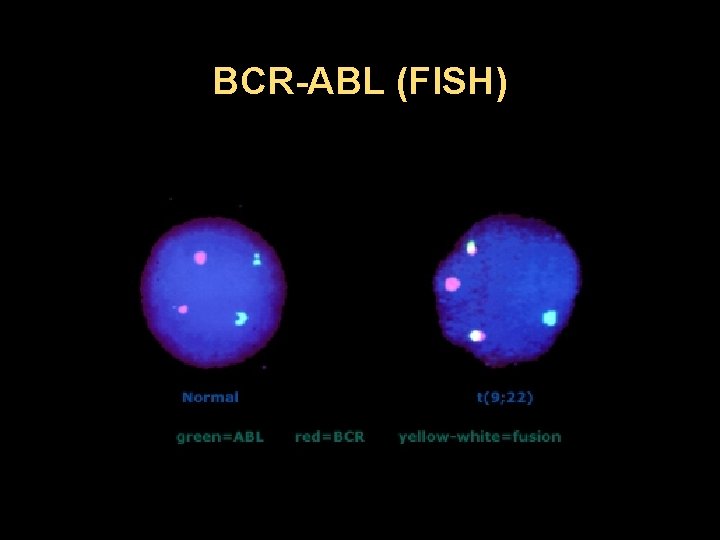
BCR-ABL (FISH)
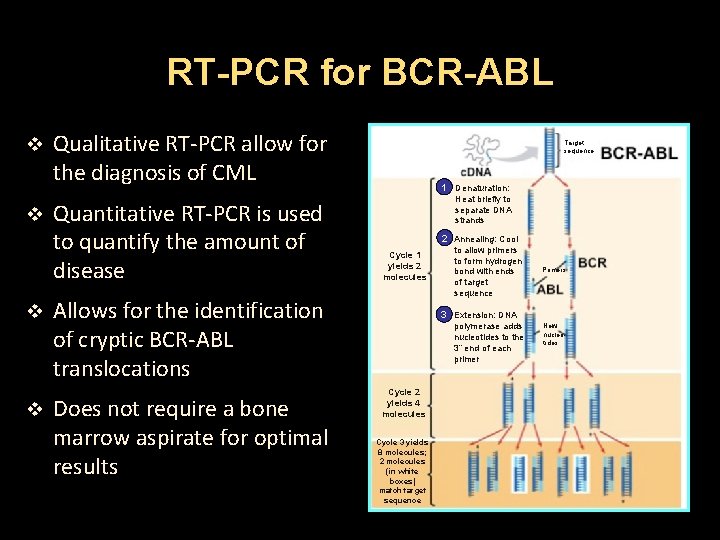
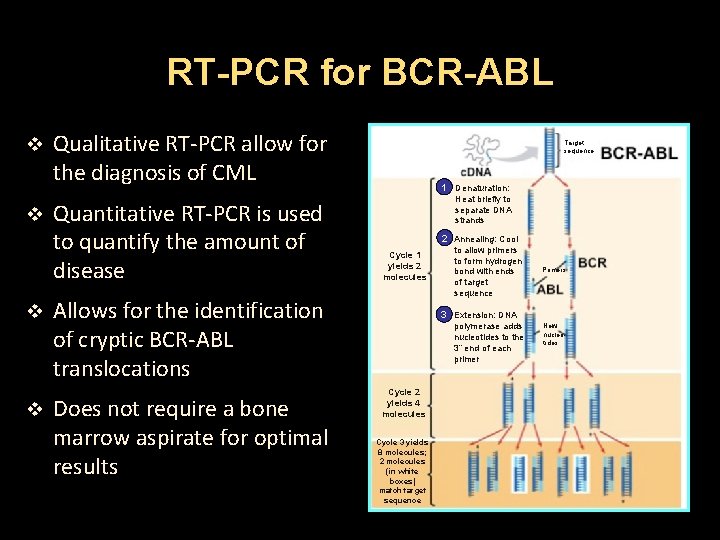
RT-PCR for BCR-ABL v v Qualitative RT-PCR allow for the diagnosis of CML Quantitative RT-PCR is used to quantify the amount of disease Target sequence 1 Denaturation: Heat briefly to separate DNA strands 2 Annealing: Cool Cycle 1 yields 2 molecules Allows for the identification of cryptic BCR-ABL translocations Does not require a bone marrow aspirate for optimal results to allow primers to form hydrogen bond with ends of target sequence Primers 3 Extension: DNA polymerase adds nucleotides to the 3” end of each primer Cycle 2 yields 4 molecules Cycle 3 yields 8 molecules; 2 molecules (in white boxes) match target sequence New nucleotides
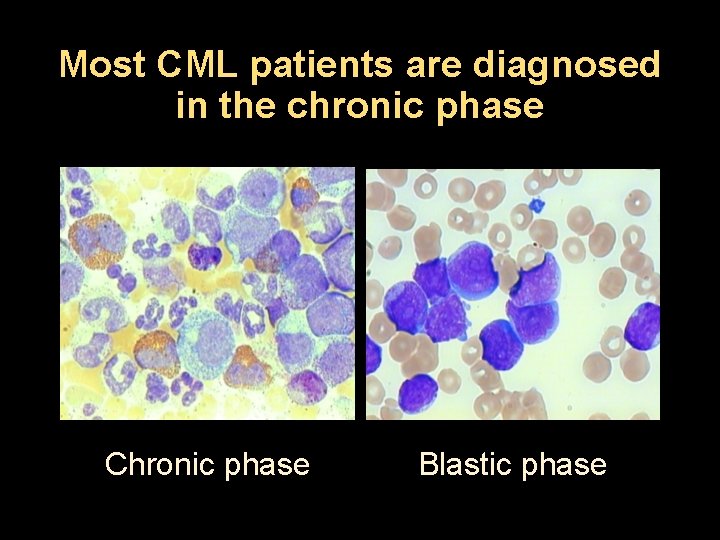
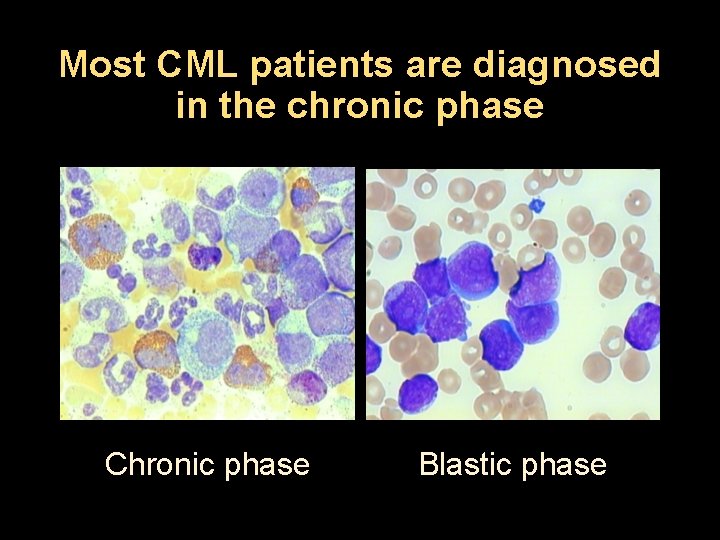
Most CML patients are diagnosed in the chronic phase Chronic phase Blastic phase
Differential Diagnosis v Leukemoid reaction v Juvenile myelomonocytic leukemia (JMML) v Chronic myelomonocytic leukemia (CMML) v Atypical CML v Chronic eosinophilic leukemia v Chronic neutrophilic leukemia v Other myeloproliferative neoplasms v Other Ph chromosome positive malignancies
Accelerated Phase CML v 10 -19% blasts in the peripheral blood or bone marrow v Peripheral blood basophils ≥ 20% v Platelets < 100, 000/micro. L, unrelated to therapy v Platelets > therapy 1, 000/micro. L, unresponsive to v Progressive splenomegaly and increasing WBC, unresponsive to therapy v Cytogenic evolution
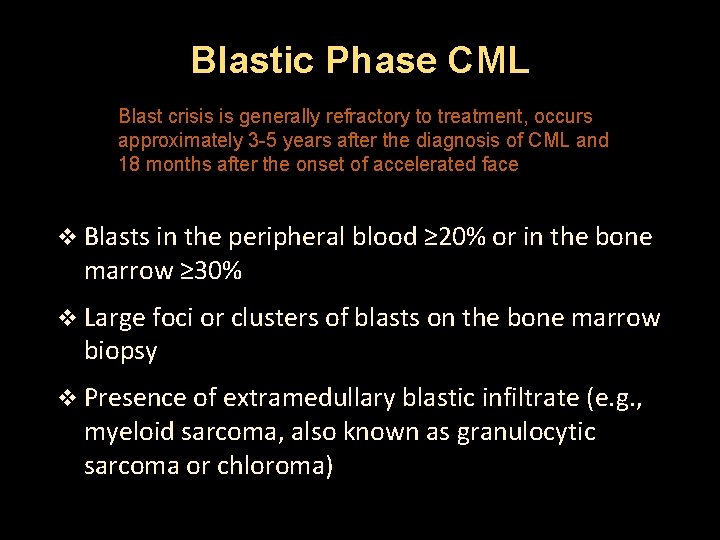
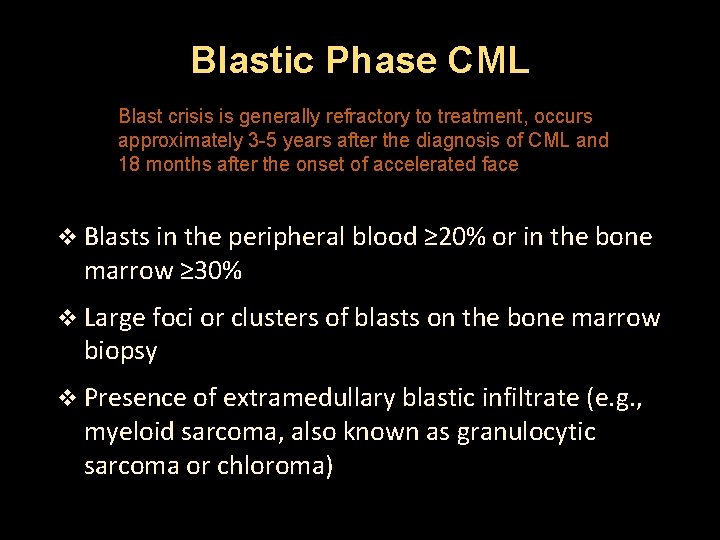
Blastic Phase CML Blast crisis is generally refractory to treatment, occurs approximately 3 -5 years after the diagnosis of CML and 18 months after the onset of accelerated face v Blasts in the peripheral blood ≥ 20% or in the bone marrow ≥ 30% v Large foci or clusters of blasts on the bone marrow biopsy v Presence of extramedullary blastic infiltrate (e. g. , myeloid sarcoma, also known as granulocytic sarcoma or chloroma)
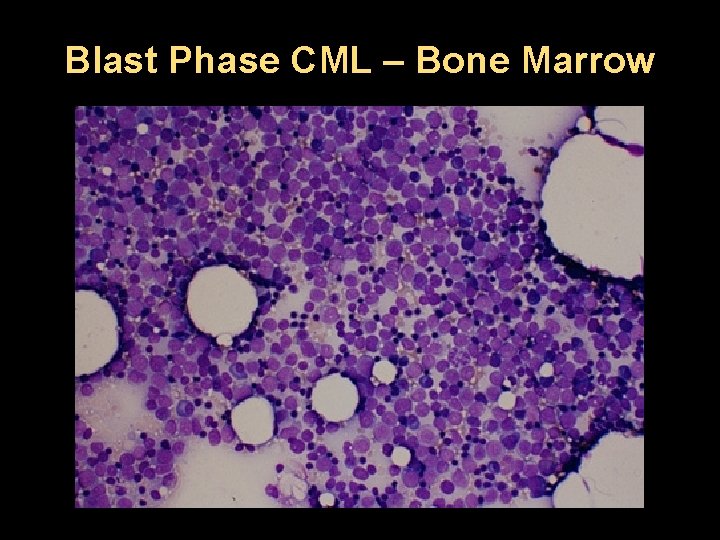
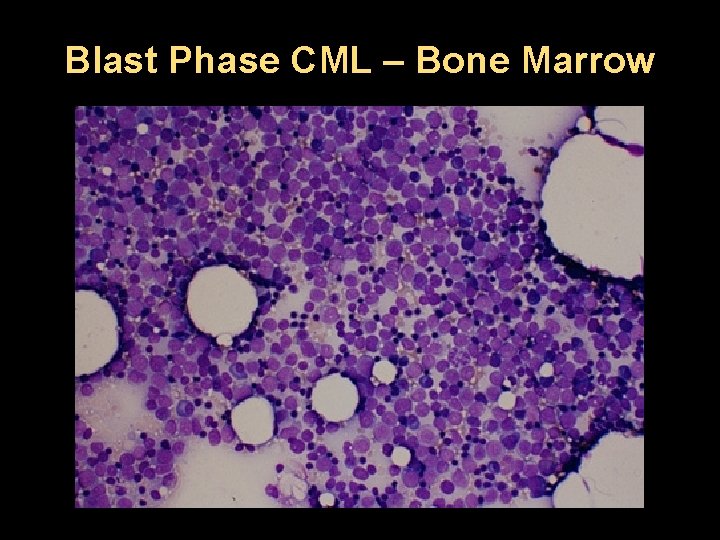
Blast Phase CML – Bone Marrow

Blast Phase CML – Bone Marrow
Clinical Debate What is the optimal frontline therapy for CML?
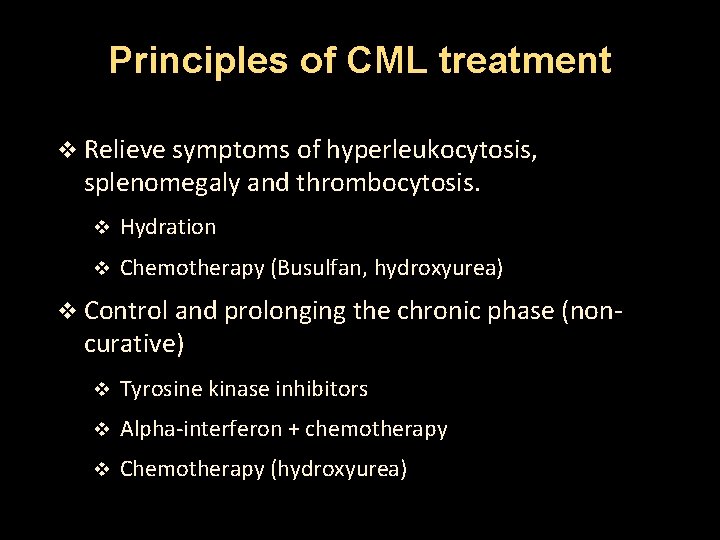
Principles of CML treatment v Relieve symptoms of hyperleukocytosis, splenomegaly and thrombocytosis. v Hydration v Chemotherapy (Busulfan, hydroxyurea) v Control and prolonging the chronic phase (non- curative) v Tyrosine kinase inhibitors v Alpha-interferon + chemotherapy v Chemotherapy (hydroxyurea)
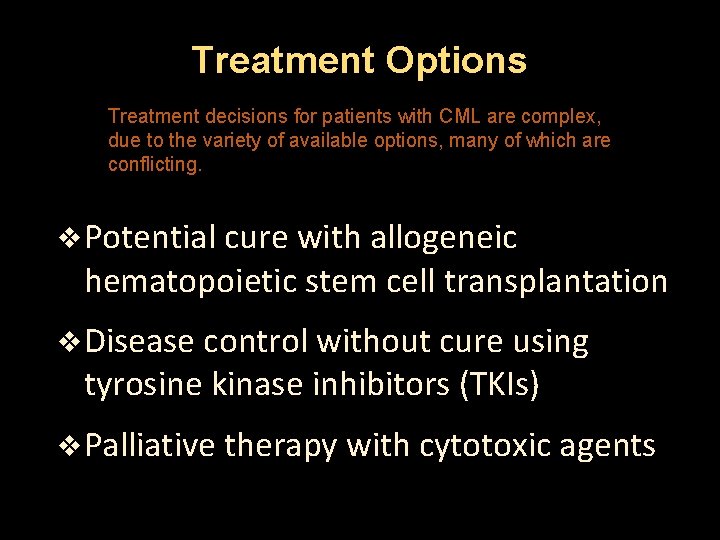
Treatment Options Treatment decisions for patients with CML are complex, due to the variety of available options, many of which are conflicting. v Potential cure with allogeneic hematopoietic stem cell transplantation v Disease control without cure using tyrosine kinase inhibitors (TKIs) v Palliative therapy with cytotoxic agents
Factors influencing choice of therapy v Phase of CML v Availability of a donor for allogeneic stem cell transplant v Patient age v Presence of medical co-morbidities v Response to treatment with TKIs
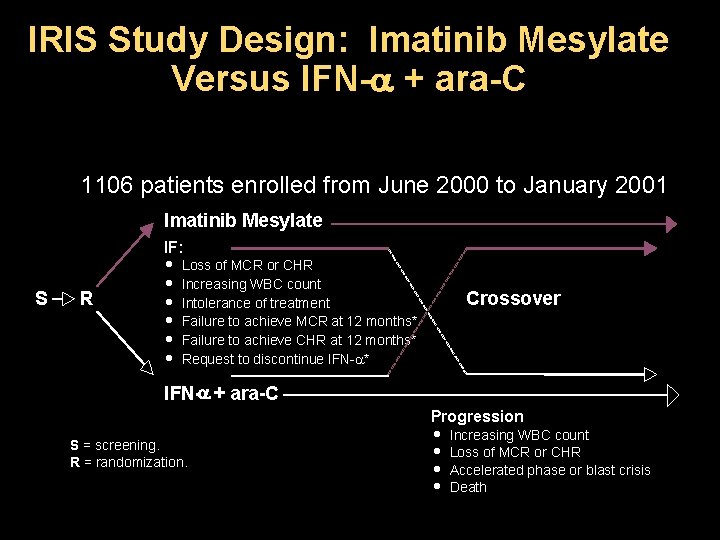
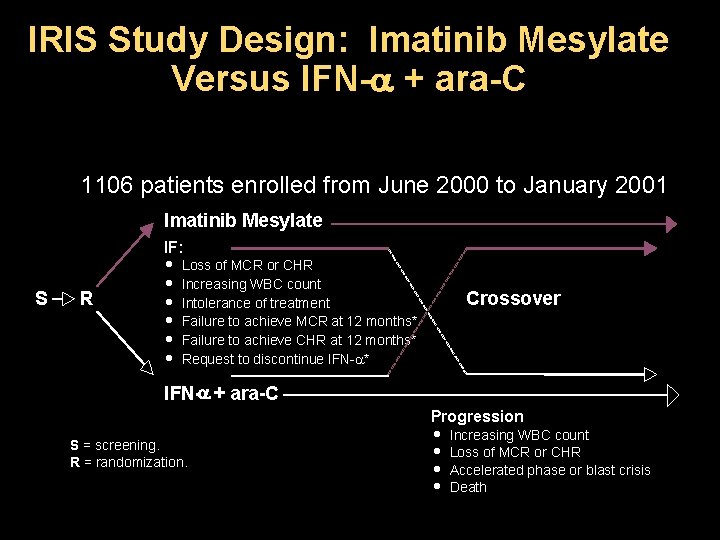
IRIS Study Design: Imatinib Mesylate Versus IFN- + ara-C 1106 patients enrolled from June 2000 to January 2001 Imatinib Mesylate S R IF: · Loss of MCR or CHR · Increasing WBC count · Intolerance of treatment · Failure to achieve MCR at 12 months* · Failure to achieve CHR at 12 months* · Request to discontinue IFN- * Crossover IFN- + ara-C S = screening. R = randomization. Progression · Increasing WBC count · Loss of MCR or CHR · Accelerated phase or blast crisis · Death
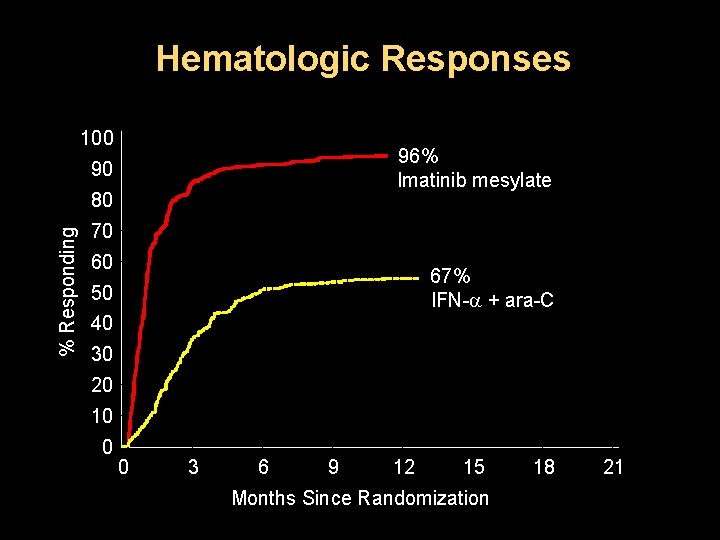
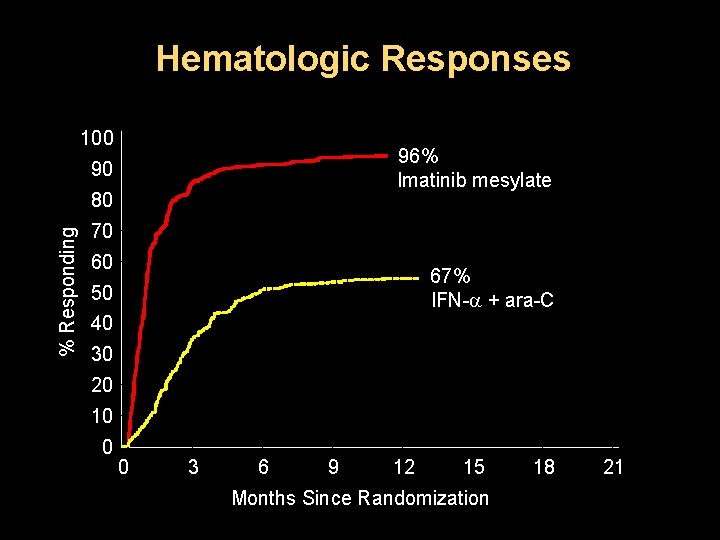
Hematologic Responses 100 96% Imatinib mesylate 90 % Responding 80 70 60 67% IFN- + ara-C 50 40 30 20 10 0 0 3 6 9 12 15 Months Since Randomization 18 21
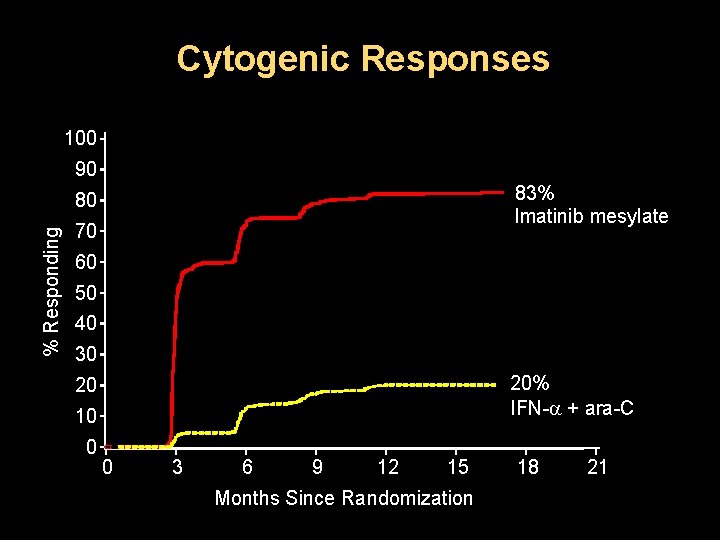
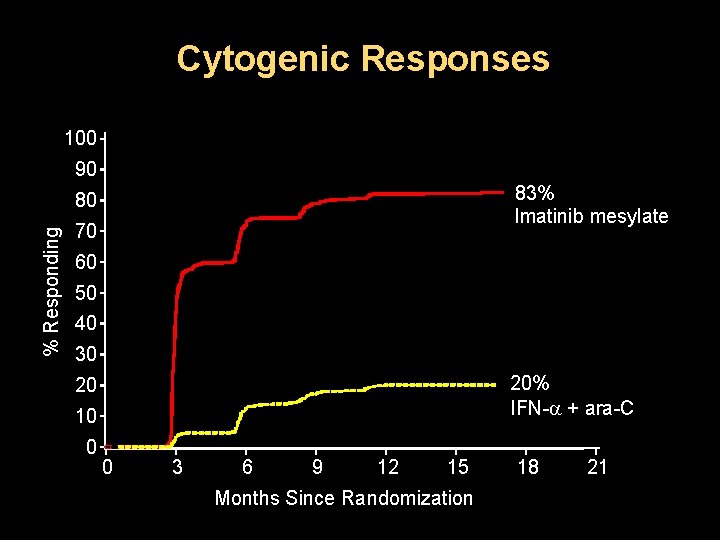
Cytogenic Responses 100 90 83% Imatinib mesylate % Responding 80 70 60 50 40 30 20% IFN- + ara-C 20 10 0 0 3 6 9 12 15 Months Since Randomization 18 21
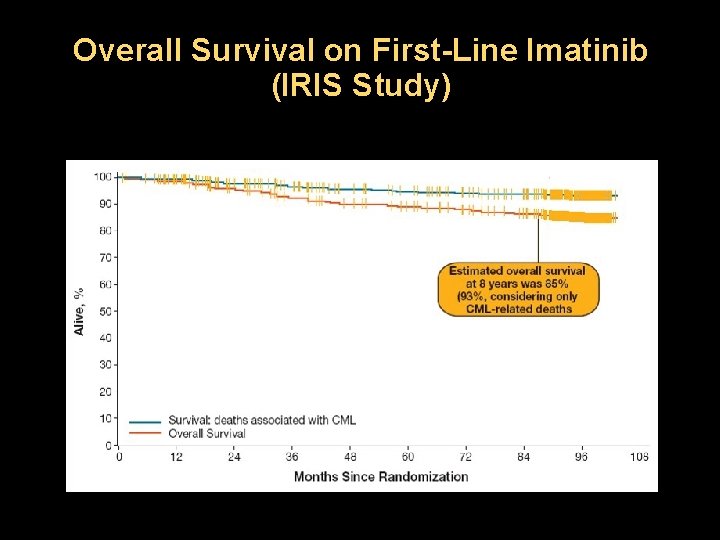
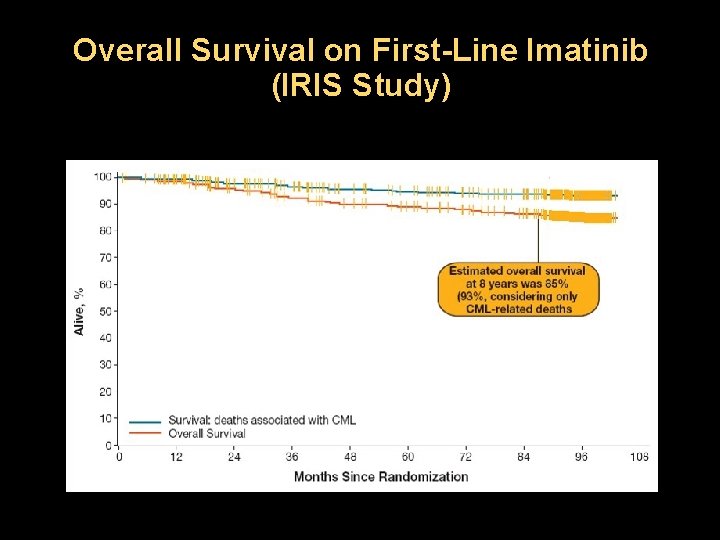
Overall Survival on First-Line Imatinib (IRIS Study)
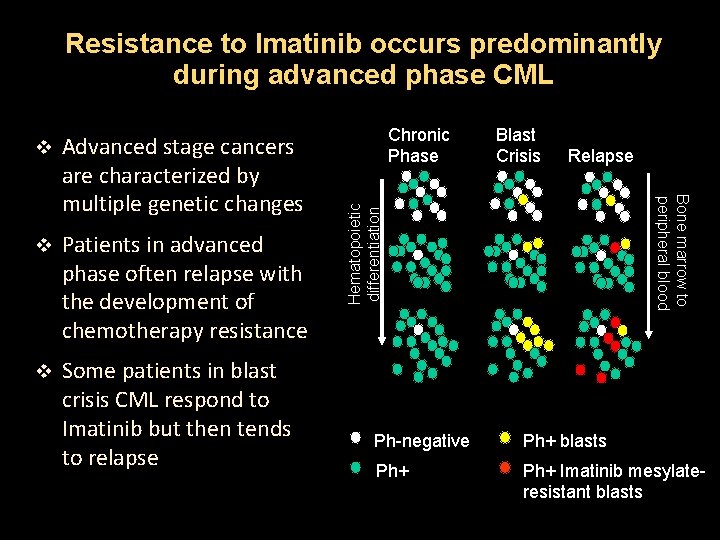
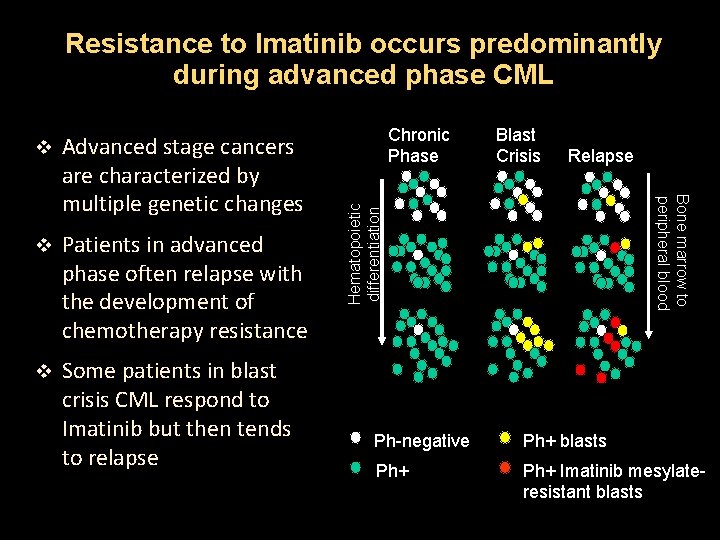
Resistance to Imatinib occurs predominantly during advanced phase CML v Patients in advanced phase often relapse with the development of chemotherapy resistance v Some patients in blast crisis CML respond to Imatinib but then tends to relapse Chronic Phase Blast Crisis Relapse Hematopoietic differentiation Advanced stage cancers are characterized by multiple genetic changes Bone marrow to peripheral blood v Ph-negative Ph+ blasts Ph+ Imatinib mesylateresistant blasts
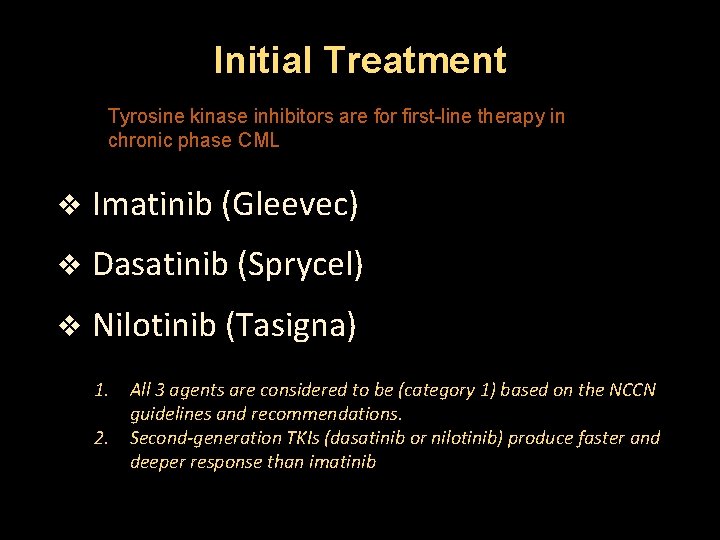
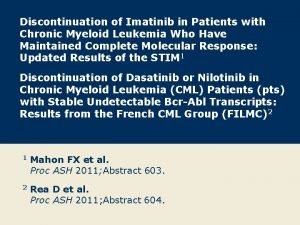
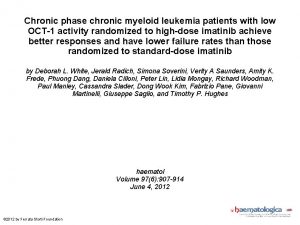
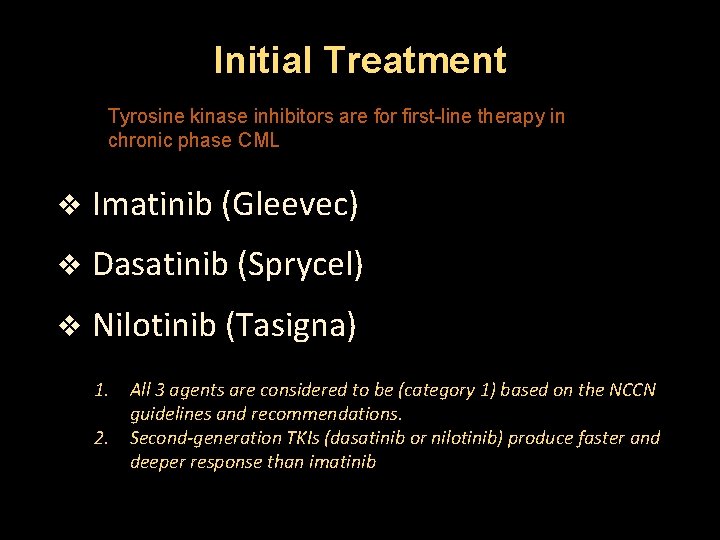
Initial Treatment Tyrosine kinase inhibitors are for first-line therapy in chronic phase CML v Imatinib (Gleevec) v Dasatinib (Sprycel) v Nilotinib (Tasigna) 1. All 3 agents are considered to be (category 1) based on the NCCN guidelines and recommendations. 2. Second-generation TKIs (dasatinib or nilotinib) produce faster and deeper response than imatinib
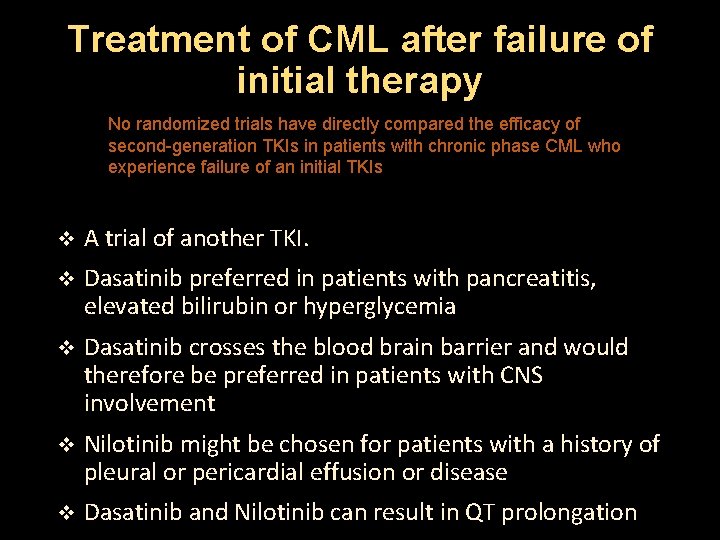
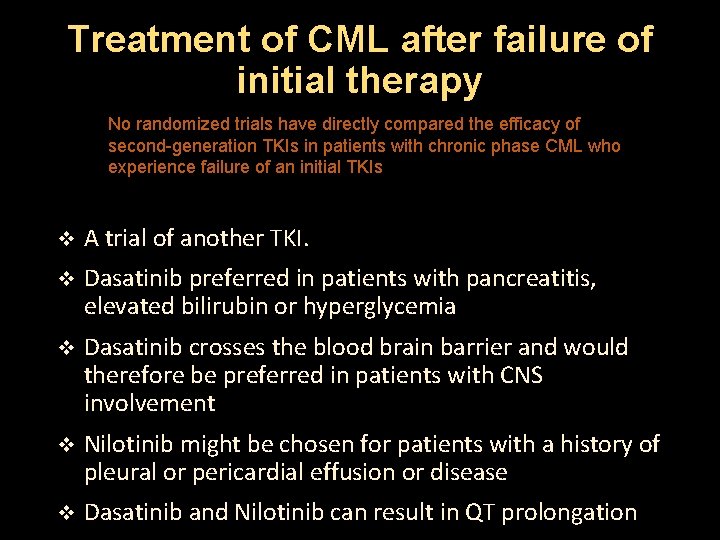
Treatment of CML after failure of initial therapy No randomized trials have directly compared the efficacy of second-generation TKIs in patients with chronic phase CML who experience failure of an initial TKIs v A trial of another TKI. v Dasatinib preferred in patients with pancreatitis, elevated bilirubin or hyperglycemia v Dasatinib crosses the blood brain barrier and would therefore be preferred in patients with CNS involvement v Nilotinib might be chosen for patients with a history of pleural or pericardial effusion or disease v Dasatinib and Nilotinib can result in QT prolongation
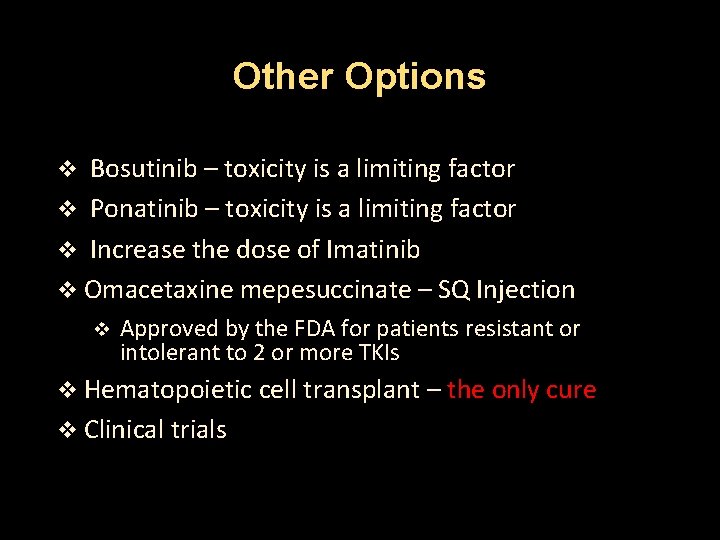
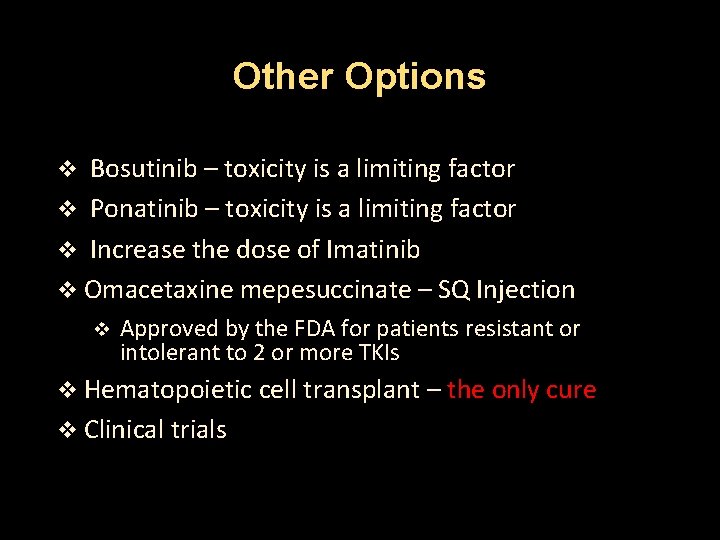
Other Options Bosutinib – toxicity is a limiting factor v Ponatinib – toxicity is a limiting factor v Increase the dose of Imatinib v Omacetaxine mepesuccinate – SQ Injection v v Approved by the FDA for patients resistant or intolerant to 2 or more TKIs v Hematopoietic cell transplant – the only cure v Clinical trials
Other Options Patients who are ineligible for HCT but have either a contraindication to a second-generation TKI or have failed to respond to treatment with available TKI v Interferon alfa plus cytarabine v Hydroxyurea v Busulfan
Response Criteria v Hematologic response v Cytogenic response v Molecular response
Resistance to treatment v Primary resistance – patient fails to achieve a desired response to initial treatment v Secondary resistance – patient with an initial response to a TKI ultimately relapses
Loss of Response Patients should be re-evaluated with a bone marrow biopsy with cytogenetics, and BCR-ABL kinase mutation analysis v T 315 I mutation v Resistant to all TKIs, except Ponatinib v Patient should be evaluated for SCT v Y 253 H, E 255 k/V and F 359 V/C/I mutations v Resistant to Imatinib and Nilotinib but sensitive to Dasatinib v F 317 L/V/I/C, V 299 L and T 315 A mutations v Sensitive to Nilotinib but with intermediate sensitivity to Imatinib and Dasatinib
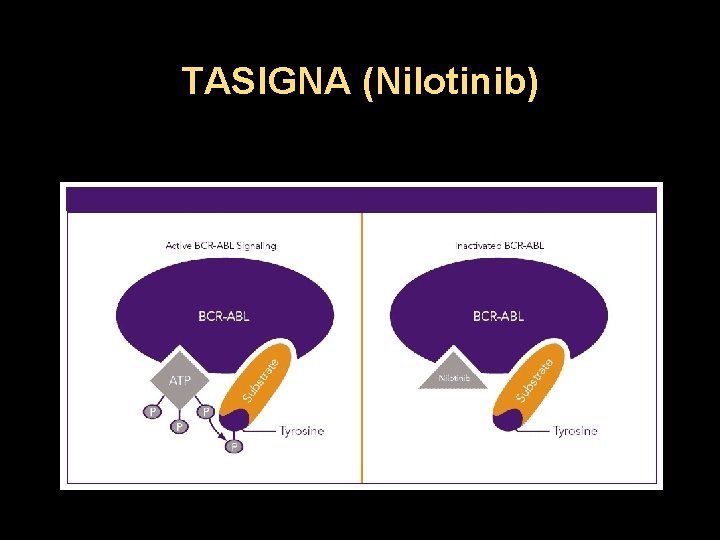
Mechanisms of action TKIs v They block the initiation of bcr-abl pathway v Many TKIs also affect other signaling pathways v Dasatinib and Bosutinib inhibit both Bcr-Abl and Src kinases. v Nilotinib inhibits Bcr-Abl, c-kit and platelet derived growth factor receptor (PDGFR) v These differences in targeted pathways may be responsible for their varied clinical effects in tumors
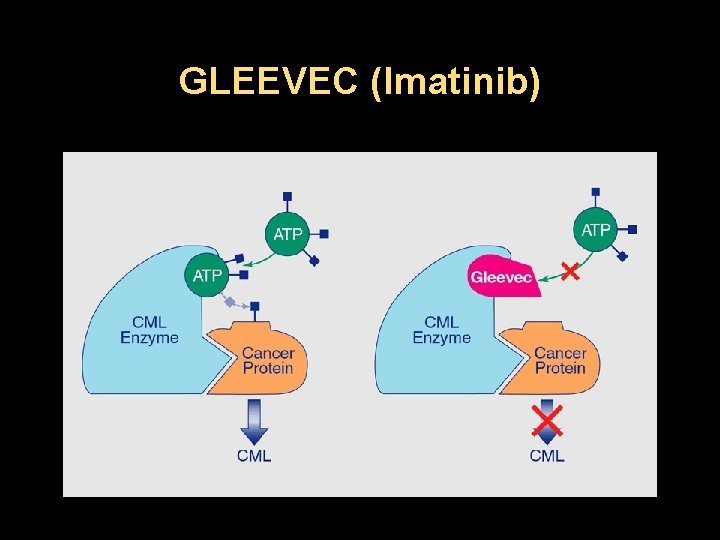
Mechanisms of Action, Imatinib v Competitively inhibits the inactive configuration of the Bcr-Abl protein tyrosine kinase v Blocking the ATP binding site and thereby preventing a conformational switch to the active form v Inhibits cellular proliferation and tumor formation v Produces 95% decrease in CML colony growth v Inhibits platelet-derived growth factor and c-kit
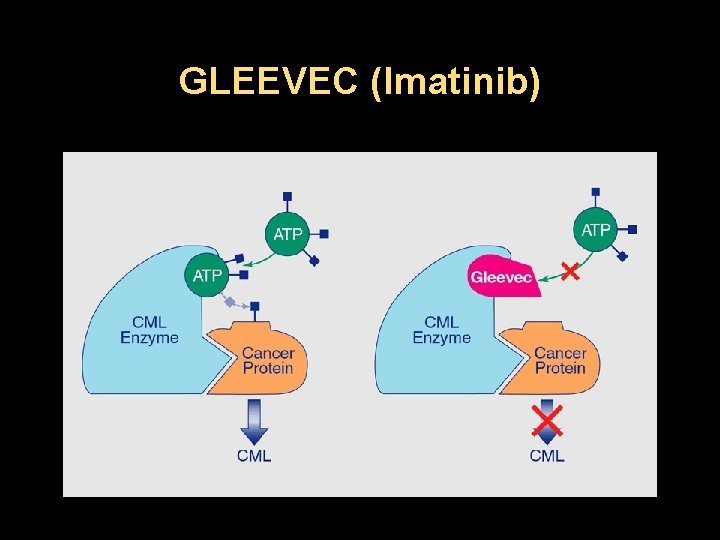
GLEEVEC (Imatinib)
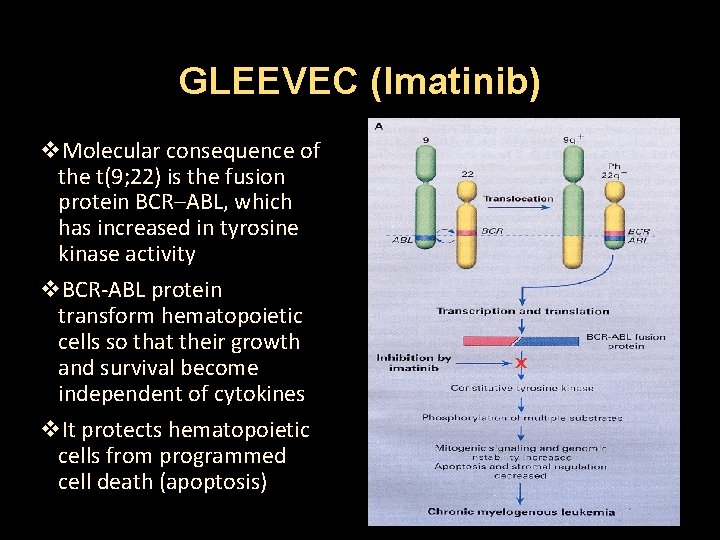
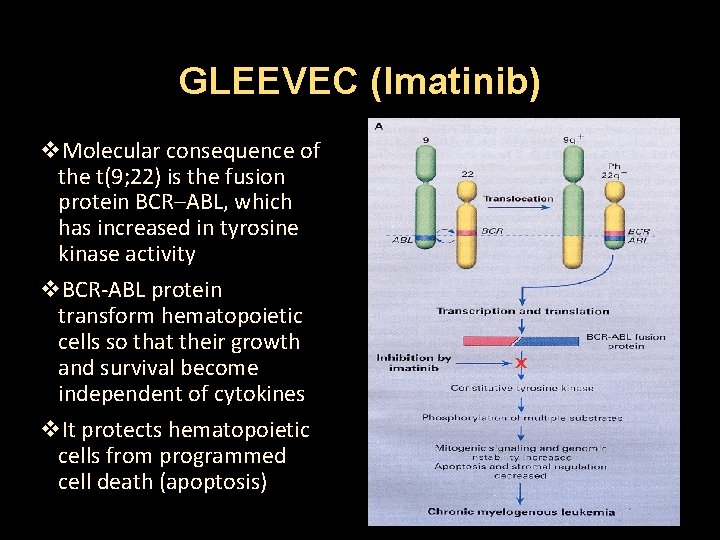
GLEEVEC (Imatinib) v. Molecular consequence of the t(9; 22) is the fusion protein BCR–ABL, which has increased in tyrosine kinase activity v. BCR-ABL protein transform hematopoietic cells so that their growth and survival become independent of cytokines v. It protects hematopoietic cells from programmed cell death (apoptosis)
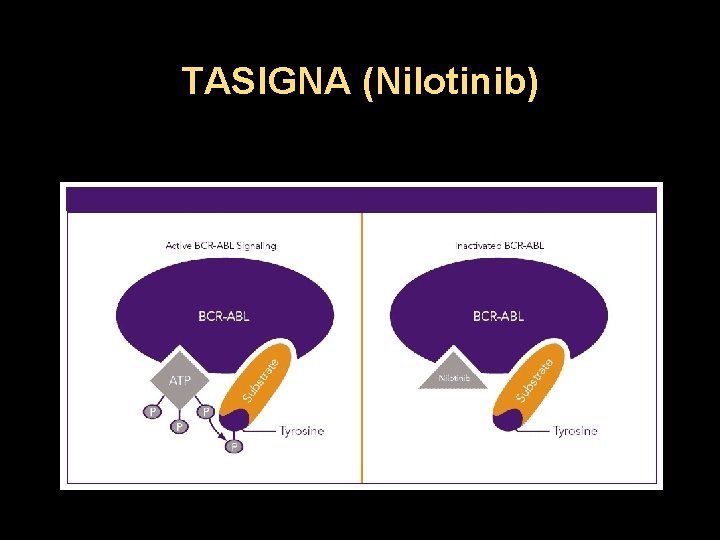
TASIGNA (Nilotinib)
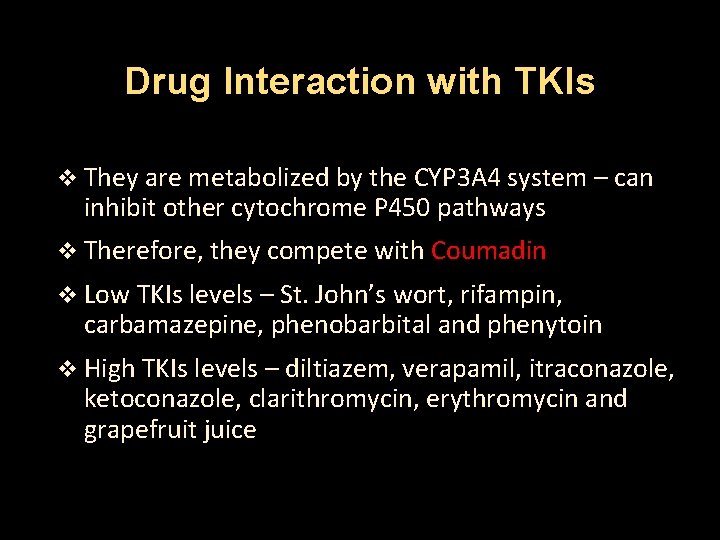
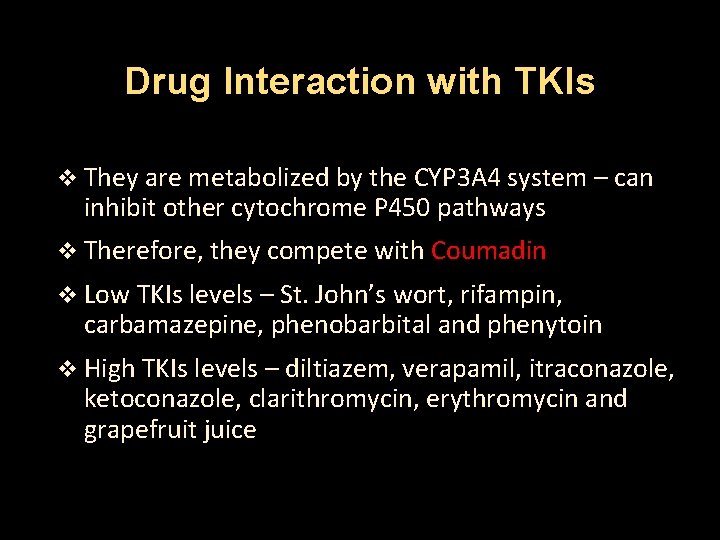
Drug Interaction with TKIs v They are metabolized by the CYP 3 A 4 system – can inhibit other cytochrome P 450 pathways v Therefore, they compete with Coumadin v Low TKIs levels – St. John’s wort, rifampin, carbamazepine, phenobarbital and phenytoin v High TKIs levels – diltiazem, verapamil, itraconazole, ketoconazole, clarithromycin, erythromycin and grapefruit juice
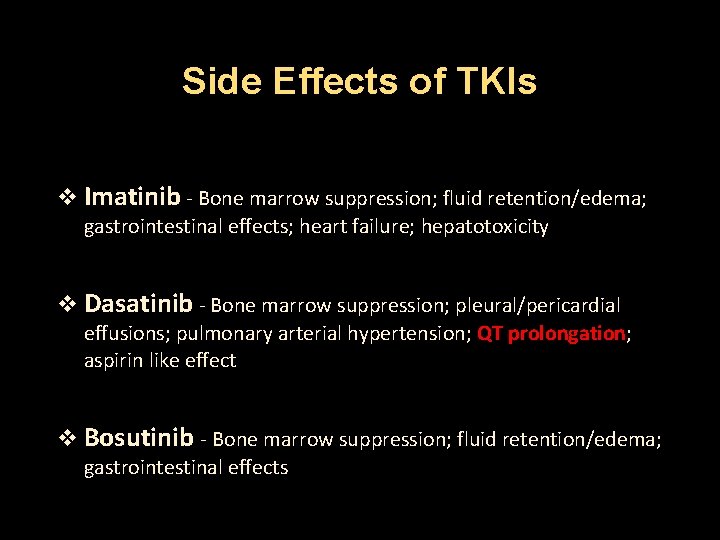
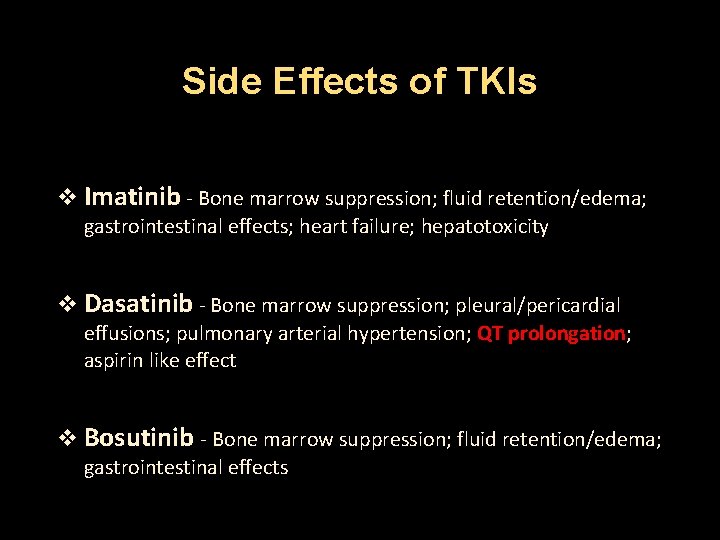
Side Effects of TKIs v Imatinib - Bone marrow suppression; fluid retention/edema; gastrointestinal effects; heart failure; hepatotoxicity v Dasatinib - Bone marrow suppression; pleural/pericardial effusions; pulmonary arterial hypertension; QT prolongation; aspirin like effect v Bosutinib - Bone marrow suppression; fluid retention/edema; gastrointestinal effects
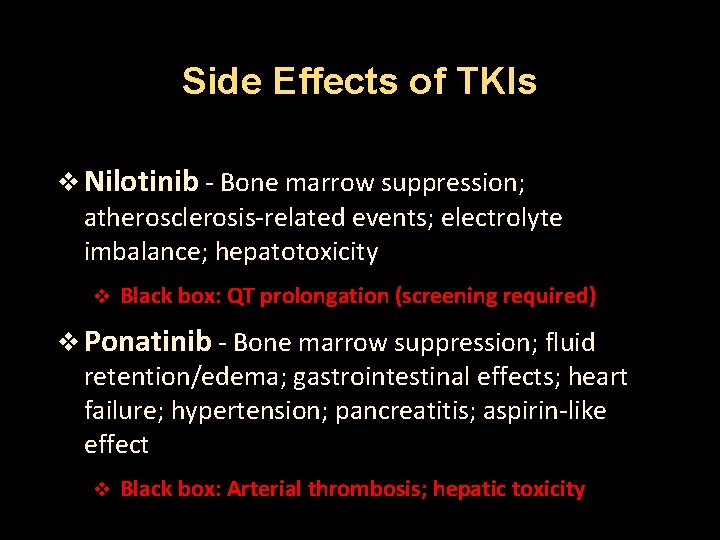
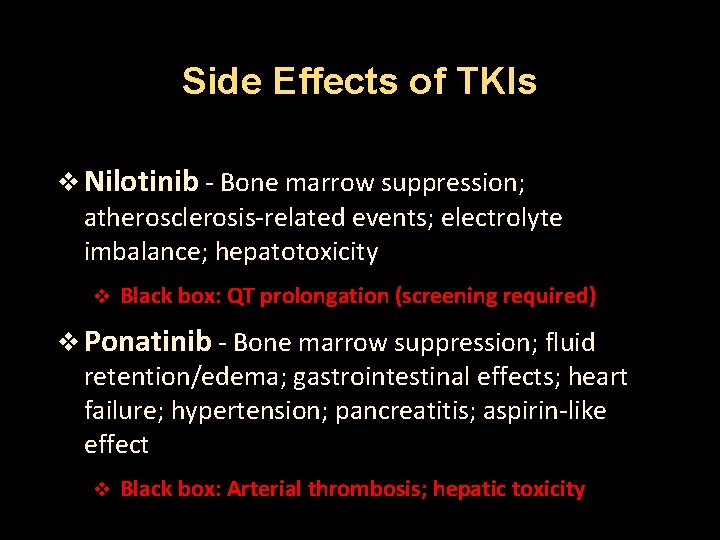
Side Effects of TKIs v Nilotinib - Bone marrow suppression; atherosclerosis-related events; electrolyte imbalance; hepatotoxicity v Black box: QT prolongation (screening required) v Ponatinib - Bone marrow suppression; fluid retention/edema; gastrointestinal effects; heart failure; hypertension; pancreatitis; aspirin-like effect v Black box: Arterial thrombosis; hepatic toxicity
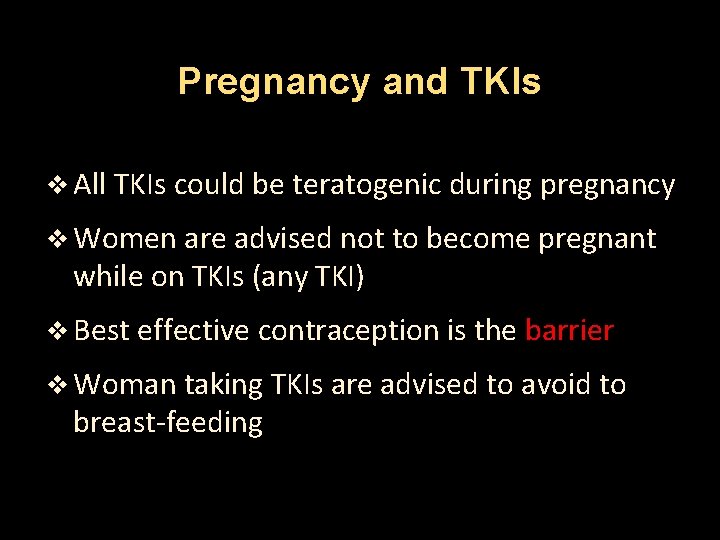
Pregnancy and TKIs v All TKIs could be teratogenic during pregnancy v Women are advised not to become pregnant while on TKIs (any TKI) v Best effective contraception is the barrier v Woman taking TKIs are advised to avoid to breast-feeding
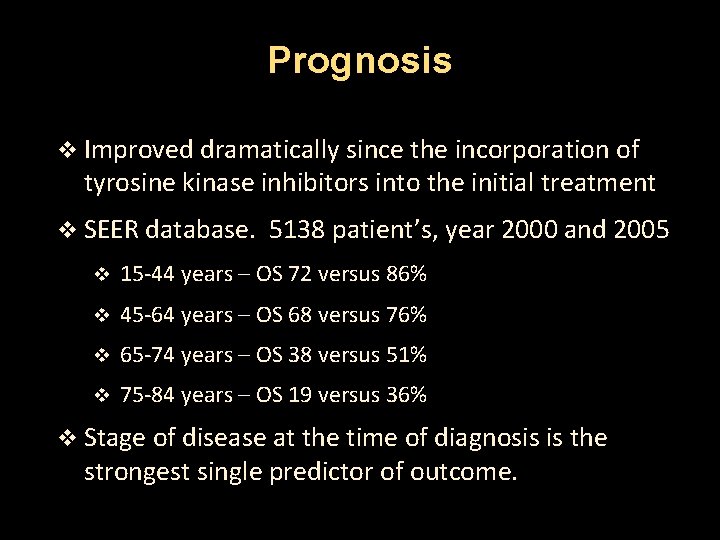
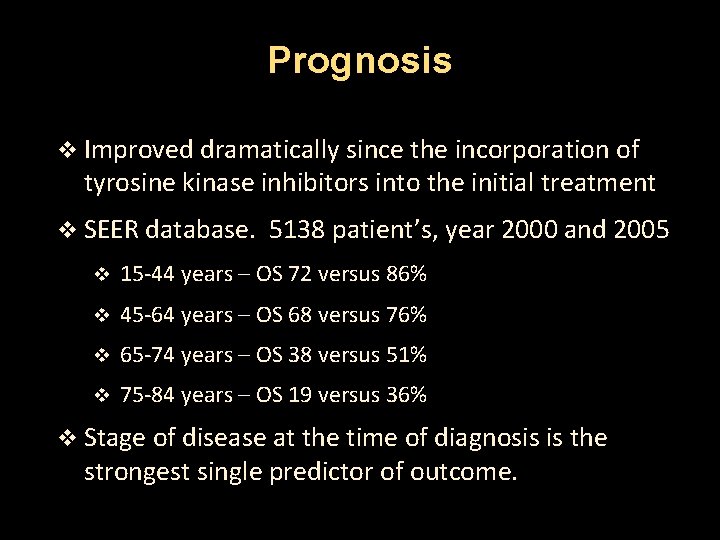
Prognosis v Improved dramatically since the incorporation of tyrosine kinase inhibitors into the initial treatment v SEER database. 5138 patient’s, year 2000 and 2005 v 15 -44 years – OS 72 versus 86% v 45 -64 years – OS 68 versus 76% v 65 -74 years – OS 38 versus 51% v 75 -84 years – OS 19 versus 36% v Stage of disease at the time of diagnosis is the strongest single predictor of outcome.
www. tallahasseecancer. com
www. tallahasseecancer. com
 Chronic myeloid leukemia treatment
Chronic myeloid leukemia treatment Chronic myeloid leukemia
Chronic myeloid leukemia Chronic myeloid leukemia
Chronic myeloid leukemia Mark juckett md
Mark juckett md Mycloblast
Mycloblast Syed amer
Syed amer Yasmeen amer
Yasmeen amer Asm microbelibrary.org
Asm microbelibrary.org Mustafa amer ismail
Mustafa amer ismail Aisha mian leaked
Aisha mian leaked Mian amer
Mian amer True or false true or false
True or false true or false Osma osnovna skola amer ćenanović
Osma osnovna skola amer ćenanović Marka amerykańskich mikroprocesorów
Marka amerykańskich mikroprocesorów Amer beitinjaneh
Amer beitinjaneh Nbone marrow
Nbone marrow Liters to gallon
Liters to gallon Leukemia vs lymphoma
Leukemia vs lymphoma Clinicaloptions
Clinicaloptions Pas stain principle
Pas stain principle Leukemia
Leukemia Leukemia statics
Leukemia statics Heinz bodies
Heinz bodies Leukemia
Leukemia Acute mylogenous leukemia
Acute mylogenous leukemia Angiorrhexis nedir
Angiorrhexis nedir Zhang wang leukemia
Zhang wang leukemia How common is leukemia in adults
How common is leukemia in adults Leukemia aleukemik adalah
Leukemia aleukemik adalah Leukémia wikipédia
Leukémia wikipédia Linelidomide
Linelidomide Hairy cell leukemia
Hairy cell leukemia Lll leukemia
Lll leukemia Principle of pas stain
Principle of pas stain Nk leukemia
Nk leukemia Hematology medical terminology
Hematology medical terminology Asparagine
Asparagine Cuadro comparativo e-learning m-learning b-learning
Cuadro comparativo e-learning m-learning b-learning Angioectasia icd 10
Angioectasia icd 10 Definition of chronic toxicity
Definition of chronic toxicity Flinders model of chronic health disorders
Flinders model of chronic health disorders Ed wagner chronic care model
Ed wagner chronic care model Earthy look in chronic renal failure
Earthy look in chronic renal failure Chronic granulomatous disease
Chronic granulomatous disease Chronic care model definition
Chronic care model definition Pulp pathosis
Pulp pathosis Normocytic normochromic symptoms
Normocytic normochromic symptoms Cholecystitis pathophysiology
Cholecystitis pathophysiology Myalgic encephalomyelitis
Myalgic encephalomyelitis Stigmata of chronic liver disease
Stigmata of chronic liver disease Irreversable pulpitis
Irreversable pulpitis Differences between acute and chronic inflammation
Differences between acute and chronic inflammation Iceberg phenomenon disease
Iceberg phenomenon disease Hemolysis ldh haptoglobin
Hemolysis ldh haptoglobin Chronic unease in the workplace
Chronic unease in the workplace Pathophysiology of cholelithiasis ppt
Pathophysiology of cholelithiasis ppt Definition of chronic toxicity
Definition of chronic toxicity Chronic blood loss
Chronic blood loss Acute cholecystitis vs chronic cholecystitis
Acute cholecystitis vs chronic cholecystitis Acute subacute chronic
Acute subacute chronic Jewish chronic disease hospital study pdf
Jewish chronic disease hospital study pdf Nephrology near atwater
Nephrology near atwater