Chronic myelocytic leukemia Definition Clonal myeloproliferative disorder of




- Slides: 46
Chronic myelocytic leukemia • Definition: Clonal myeloproliferative disorder of a pluripotent hematopoietic stem cell with a specific cytogenetic abnormalities, the Philadelphia Chromosome (Ph) • Chronic, accelerating, and blastic phases • At any age, but peak in the age group of 50 - 60
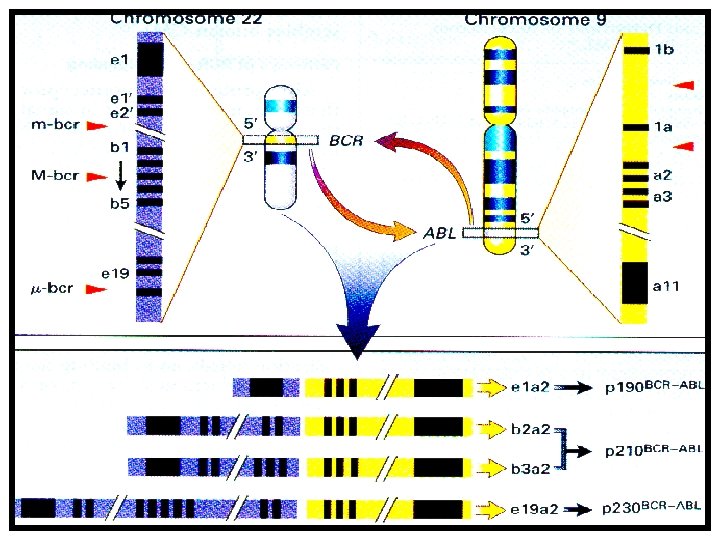
Pathophysiology Philadelphia chromosome: t(9; 22)(q 34; q 11) bcr-abl fusion gene : BCR/ABL m. RNA Bcr/Abl fusion protein (p 210 BCR-ABL) normal abl gene: p 145, tyrosine kinase Functional change Active tyrosine kinase : prevent apoptosis Attenuated DNA protein-binding activity Enhanced Abl binding to cytoskeletal actin

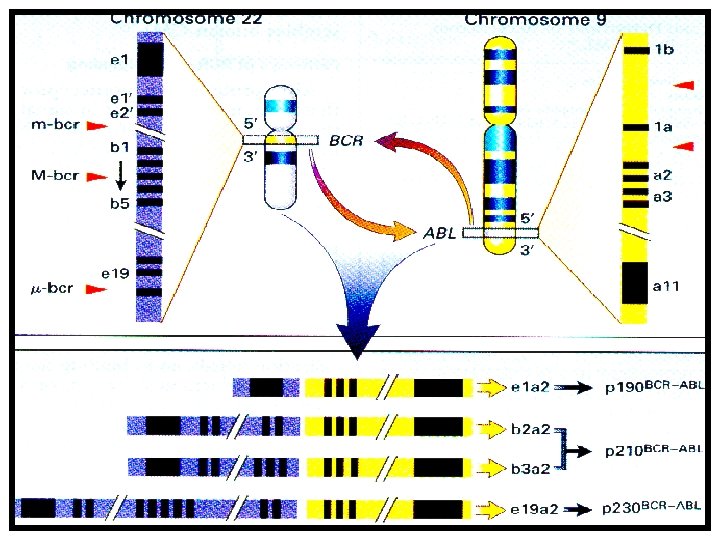

BCR/ABL + in 25 -30% (BM)
Natural course of CML • Chronic phase • Intermediate, accelerating phase • Blastic (acute transforming) phase
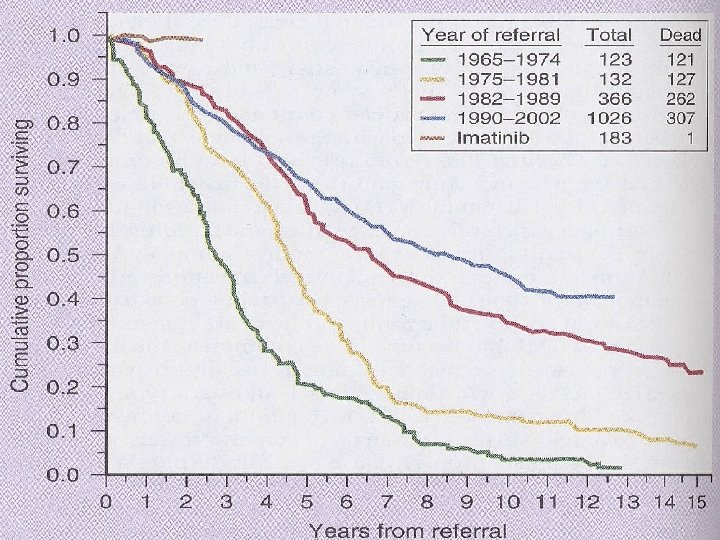
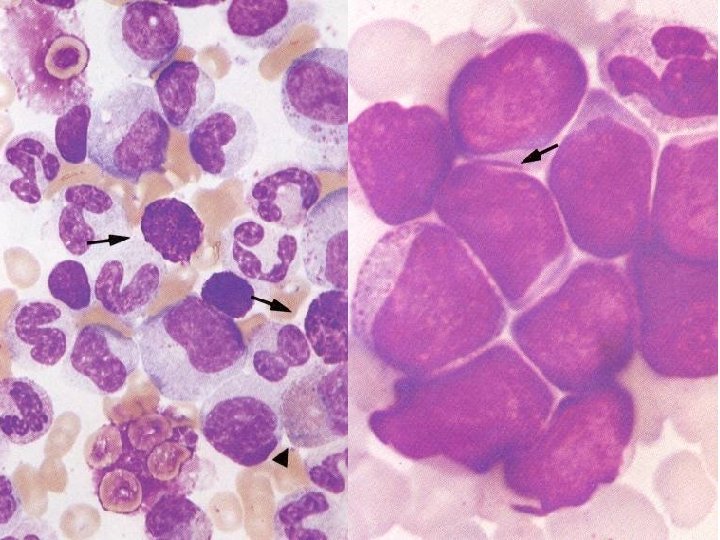
Chronic phase • Excessive proliferation and accumulation of granulocytes and their precursors; WBC often more than 200, 000/mm 3; myeloblast less than 5% in peripheral blood • 20% asymptomatic: incidentally diagnosed • Transformation rate: after first 6 to 12 months, 25% per year • 85% die in blastic phase • Over all survival: 3. 5 years

Symptoms and signs • Splenomegaly, hepatomegaly, rare lymphadenopathy • Hypermetabolism: weight loss, fatigue, fever elevated uric acid • Bone pain, arthralgia, pain from splenic infarction • Thrombohemorrhagic complication
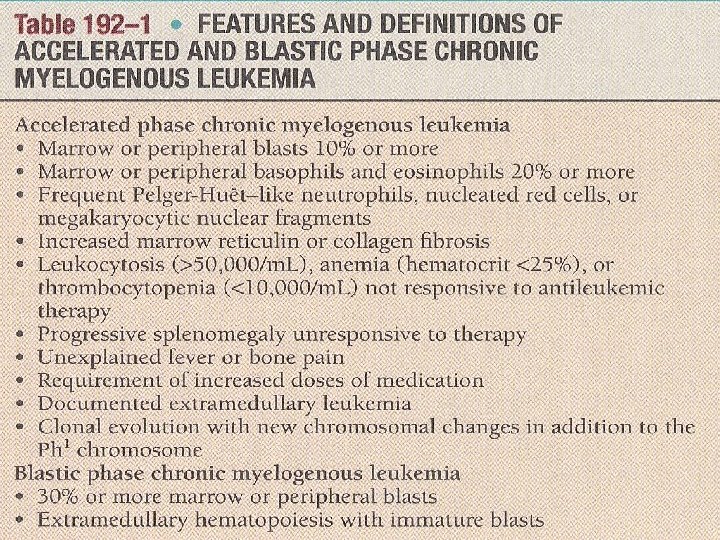
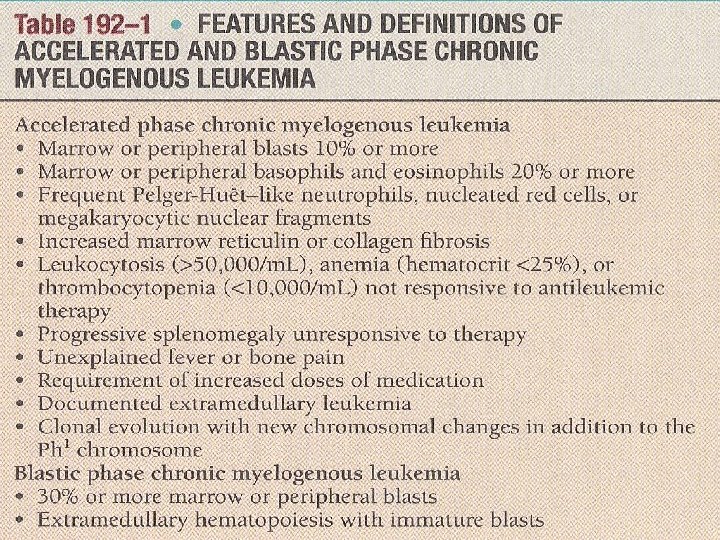
Late stage • Accelerated phase: – Increasing resistance to therapy – Progressive organomegaly – Worsening anemia, fever, myelofibrosis – Thrombocytosis or thrombocytopenia • Blastic phase: – Signs and symptoms of acute leukemia often with extramedullary disease
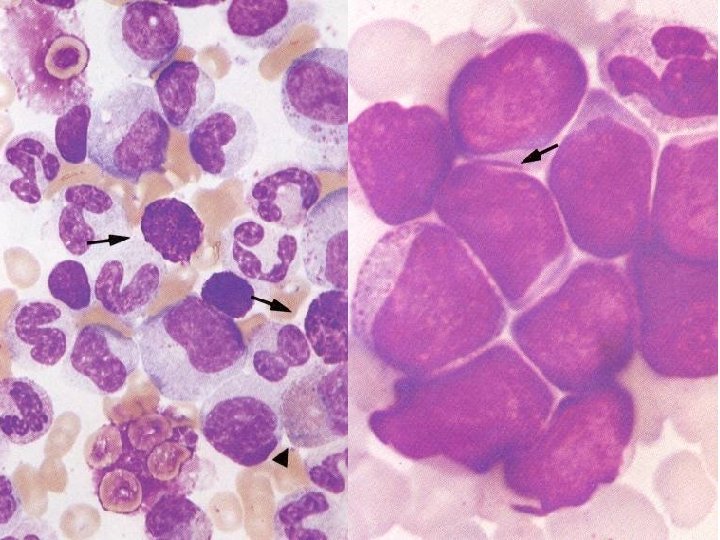
Lab findings • Leukocytosis: left shift, eosinophilia, basophilia • Thrombocytosis: normal morphology and function • Increased vitamin B 12 and binding capacity • Reduced LAP score • Hyperuricemia • Gaucher cells or see-blue histiocytes in BM
D Dx • Leukemoid reactions associated with infection or neoplasms – – – Splenomegaly Low LAP score Basophilia Ph : chromosome analysis or FISH BCR/ABL : RT-PCR • Myelodysplastic syndromes • Myeloproliferative syndromes
Blast crisis • Usually myeloid, 30% lymphoid, rarely erythroid, basophilic, megakaryoblastic • Cytogenetic: other chromosomal abnormality – double Ph 1 – aneuploidy etc.
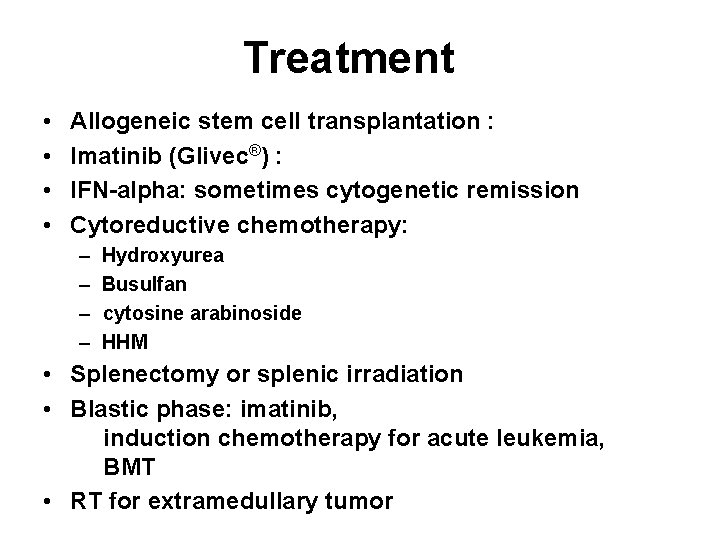
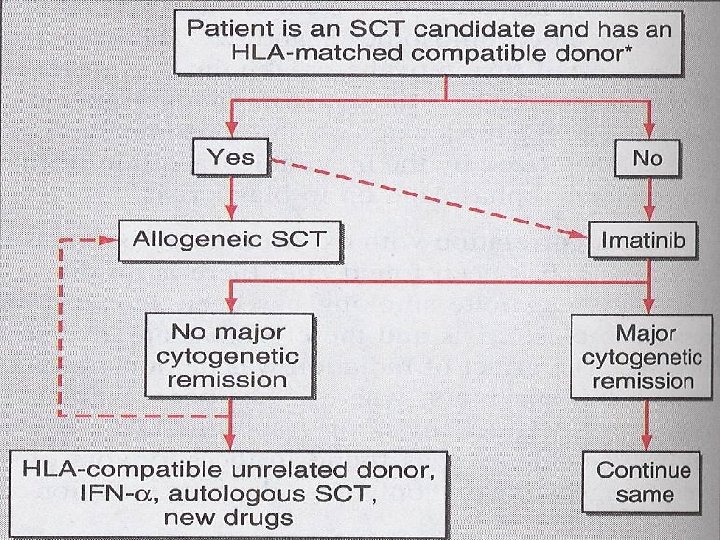
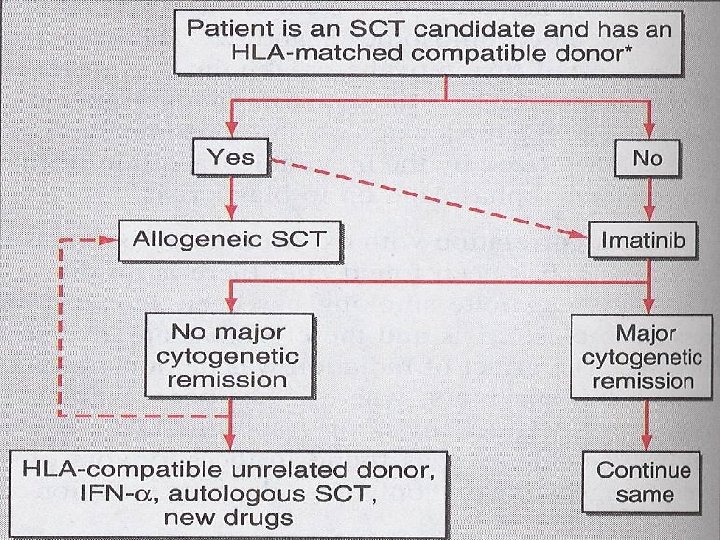
Treatment • • Allogeneic stem cell transplantation : Imatinib (Glivec®) : IFN-alpha: sometimes cytogenetic remission Cytoreductive chemotherapy: – – Hydroxyurea Busulfan cytosine arabinoside HHM • Splenectomy or splenic irradiation • Blastic phase: imatinib, induction chemotherapy for acute leukemia, BMT • RT for extramedullary tumor
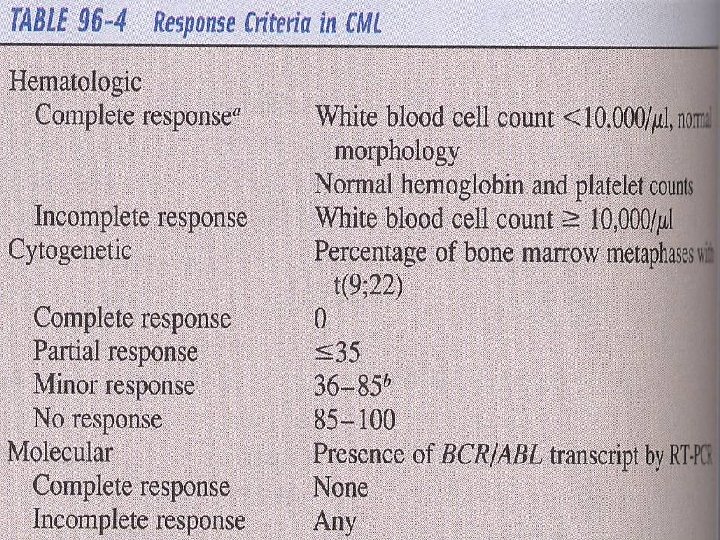
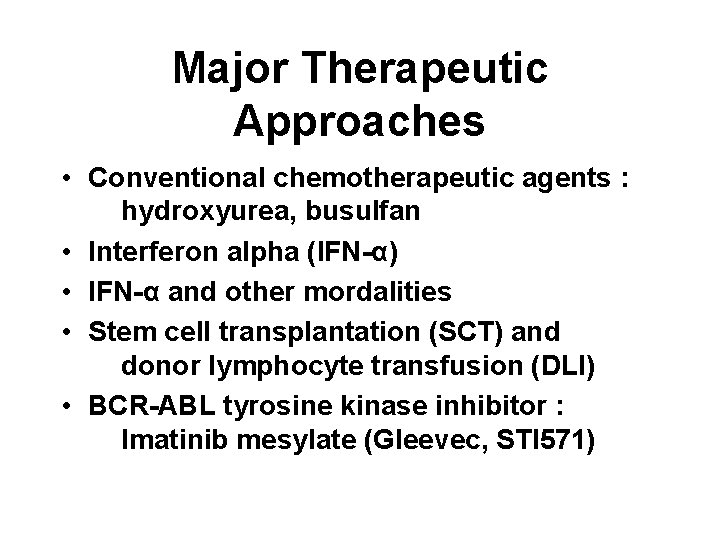
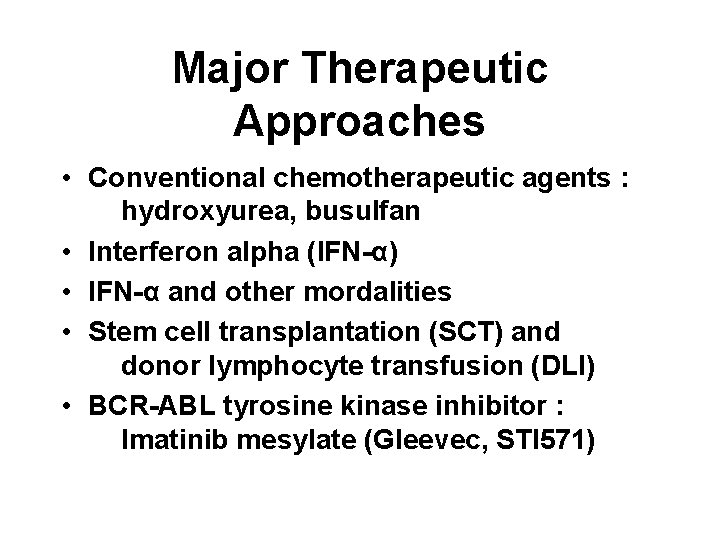
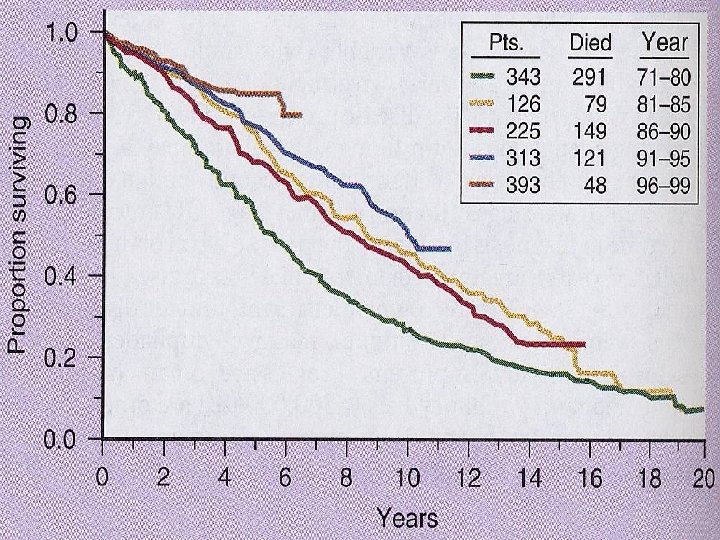
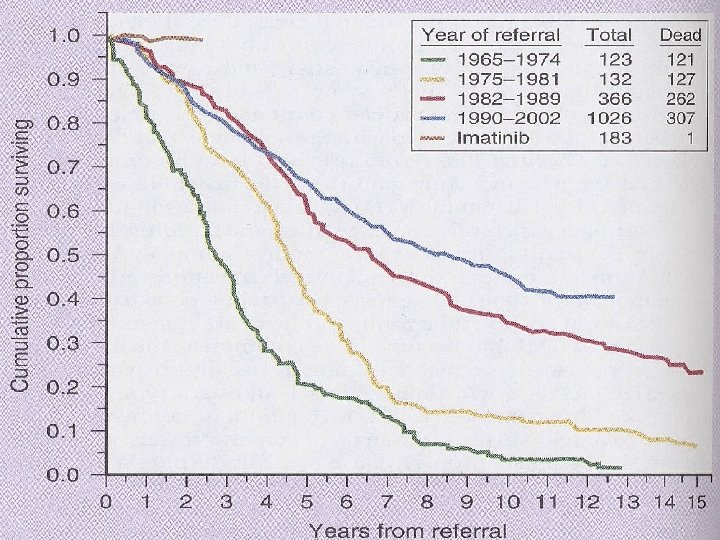
Major Therapeutic Approaches • Conventional chemotherapeutic agents : hydroxyurea, busulfan • Interferon alpha (IFN-α) • IFN-α and other mordalities • Stem cell transplantation (SCT) and donor lymphocyte transfusion (DLI) • BCR-ABL tyrosine kinase inhibitor : Imatinib mesylate (Gleevec, STI 571)
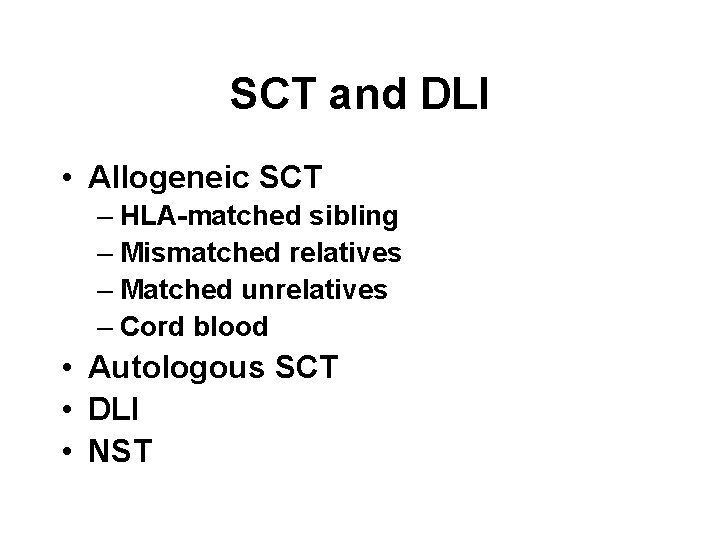
SCT and DLI • Allogeneic SCT – HLA-matched sibling – Mismatched relatives – Matched unrelatives – Cord blood • Autologous SCT • DLI • NST
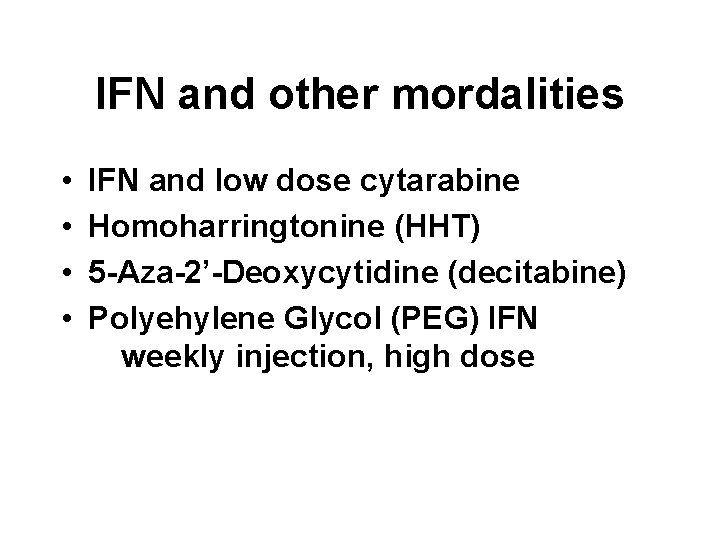
IFN and other mordalities • • IFN and low dose cytarabine Homoharringtonine (HHT) 5 -Aza-2’-Deoxycytidine (decitabine) Polyehylene Glycol (PEG) IFN weekly injection, high dose

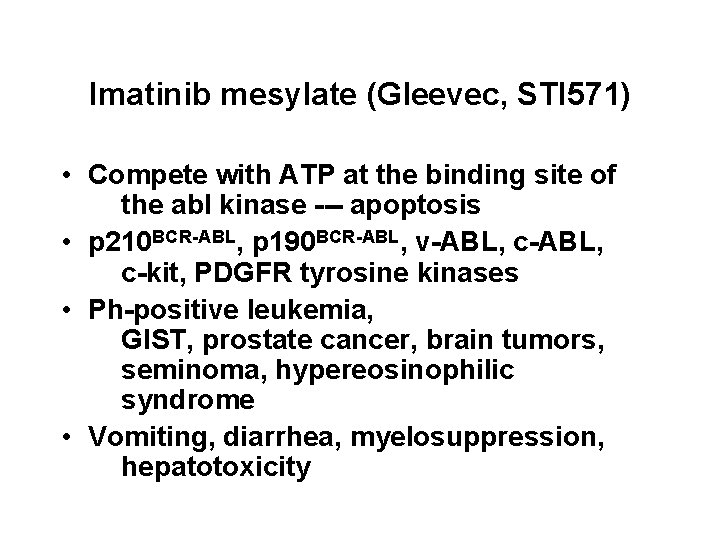
Imatinib mesylate (Gleevec, STI 571) • Compete with ATP at the binding site of the abl kinase --- apoptosis • p 210 BCR-ABL, p 190 BCR-ABL, v-ABL, c-kit, PDGFR tyrosine kinases • Ph-positive leukemia, GIST, prostate cancer, brain tumors, seminoma, hypereosinophilic syndrome • Vomiting, diarrhea, myelosuppression, hepatotoxicity
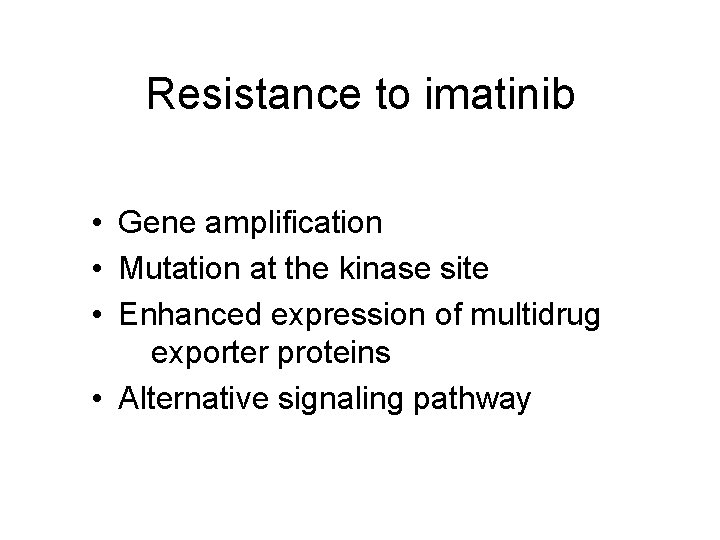
Resistance to imatinib • Gene amplification • Mutation at the kinase site • Enhanced expression of multidrug exporter proteins • Alternative signaling pathway
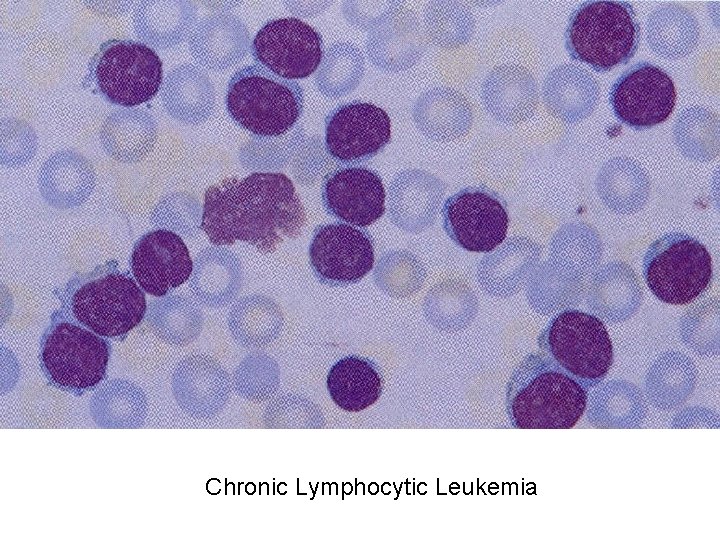
CLL • Definition: Hematologic neoplasm characterized by the accumulation of mature-appearing small lymphocyte in the peripheral blood associated with infiltration of the bone marrow, spleen and lymph nodes
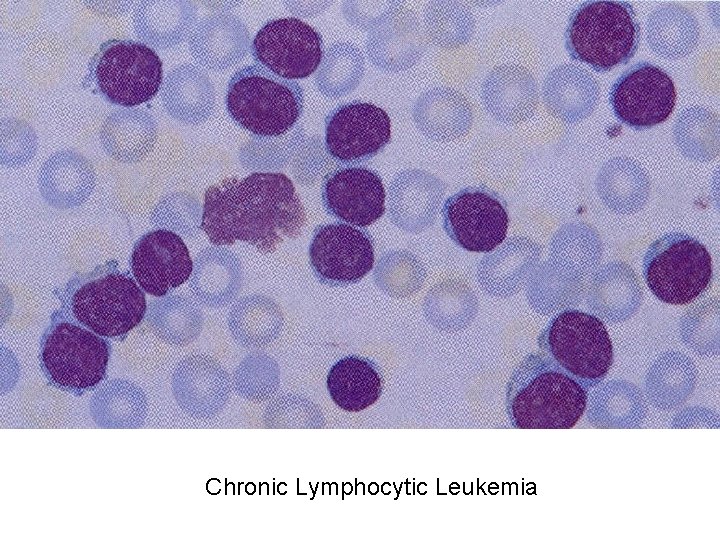
Chronic Lymphocytic Leukemia
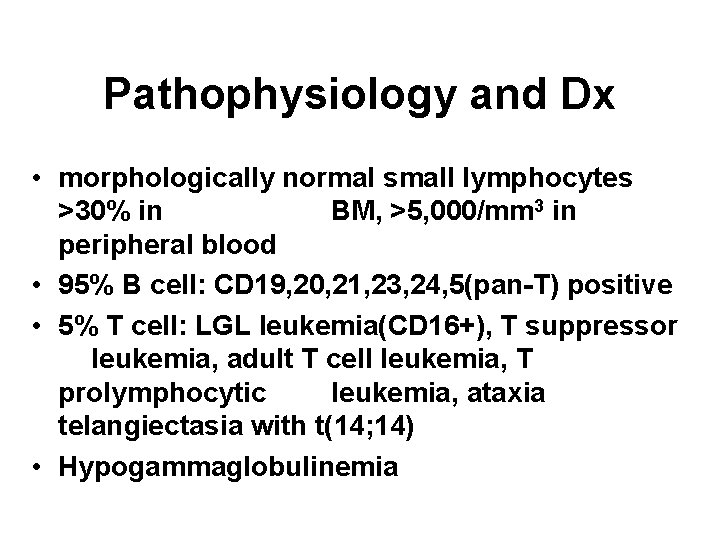
Pathophysiology and Dx • morphologically normal small lymphocytes >30% in BM, >5, 000/mm 3 in peripheral blood • 95% B cell: CD 19, 20, 21, 23, 24, 5(pan-T) positive • 5% T cell: LGL leukemia(CD 16+), T suppressor leukemia, adult T cell leukemia, T prolymphocytic leukemia, ataxia telangiectasia with t(14; 14) • Hypogammaglobulinemia
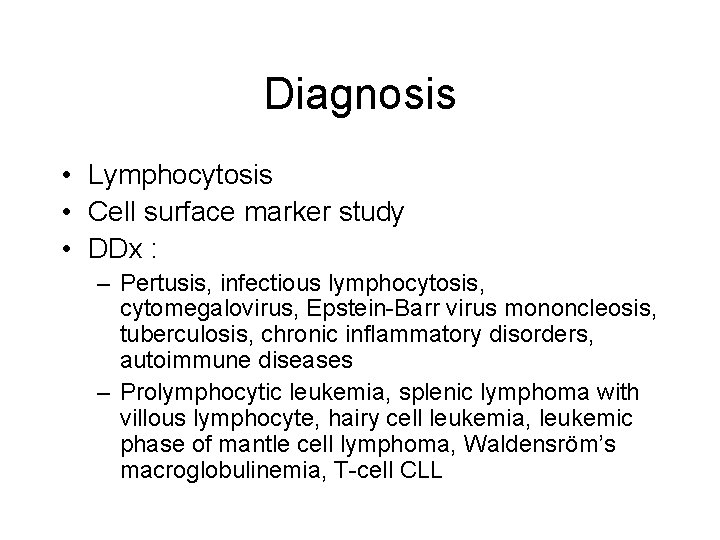
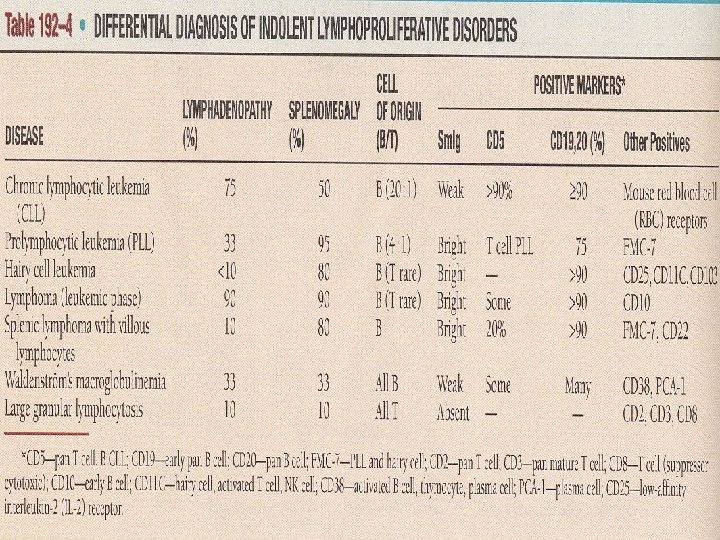
Diagnosis • Lymphocytosis • Cell surface marker study • DDx : – Pertusis, infectious lymphocytosis, cytomegalovirus, Epstein-Barr virus mononcleosis, tuberculosis, chronic inflammatory disorders, autoimmune diseases – Prolymphocytic leukemia, splenic lymphoma with villous lymphocyte, hairy cell leukemia, leukemic phase of mantle cell lymphoma, Waldensröm’s macroglobulinemia, T-cell CLL
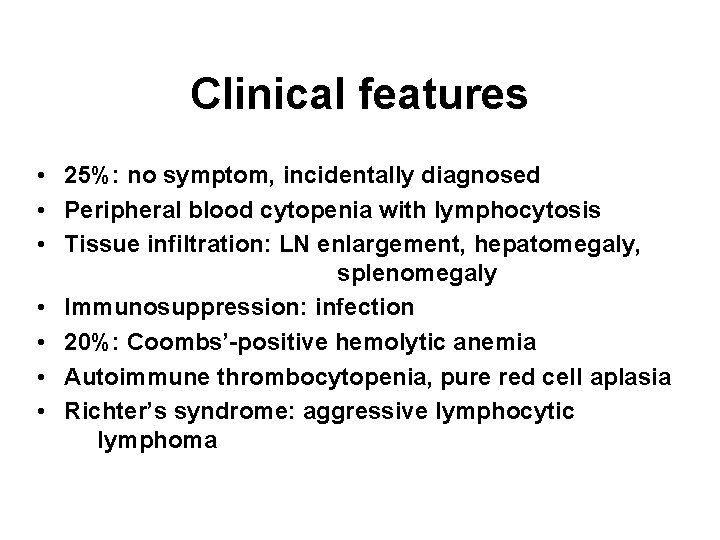
Clinical features • 25%: no symptom, incidentally diagnosed • Peripheral blood cytopenia with lymphocytosis • Tissue infiltration: LN enlargement, hepatomegaly, splenomegaly • Immunosuppression: infection • 20%: Coombs’-positive hemolytic anemia • Autoimmune thrombocytopenia, pure red cell aplasia • Richter’s syndrome: aggressive lymphocytic lymphoma
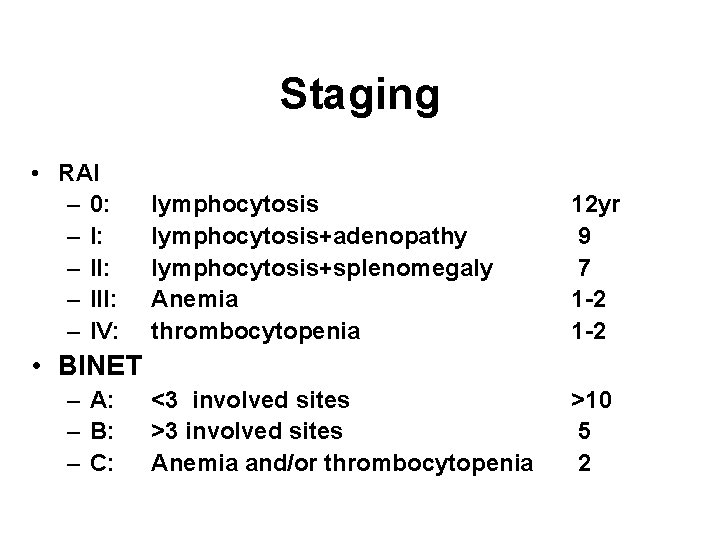
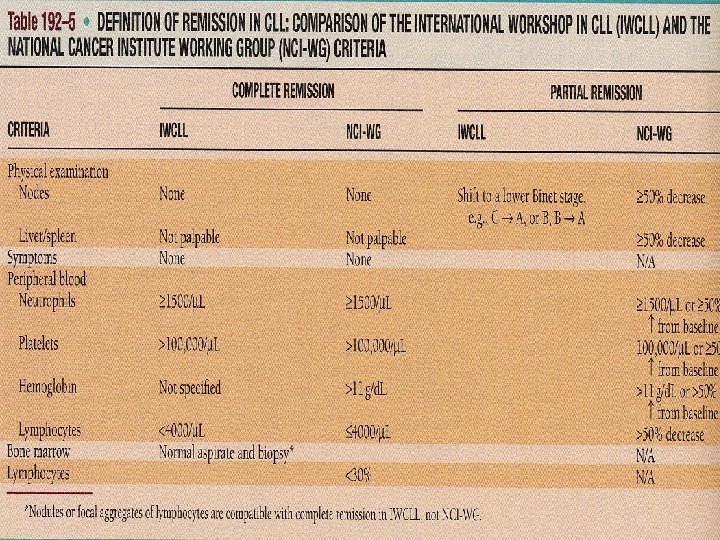
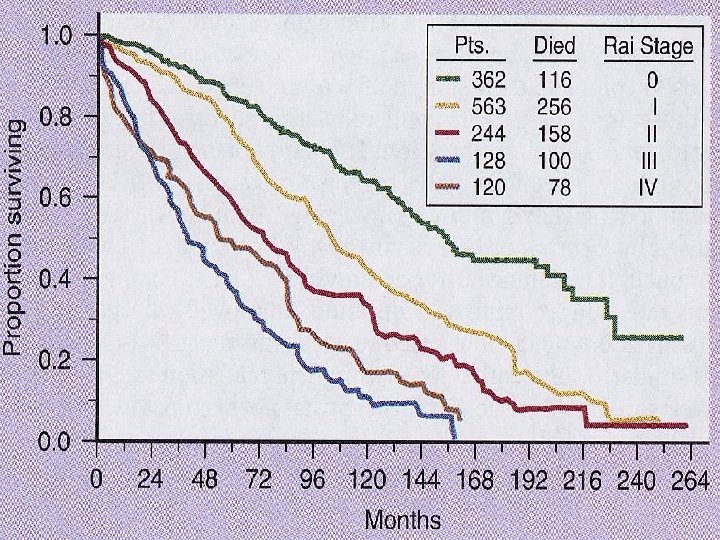
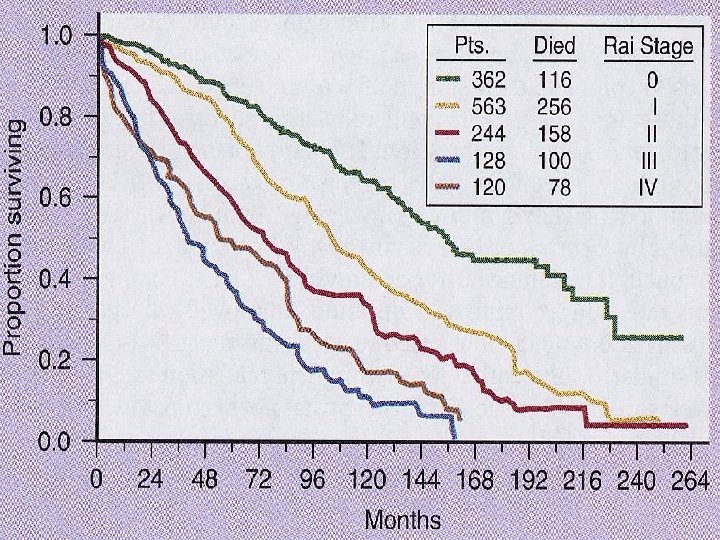
Staging • RAI – 0: – II: – III: – IV: lymphocytosis+adenopathy lymphocytosis+splenomegaly Anemia thrombocytopenia 12 yr 9 7 1 -2 <3 involved sites >3 involved sites Anemia and/or thrombocytopenia >10 5 2 • BINET – A: – B: – C:
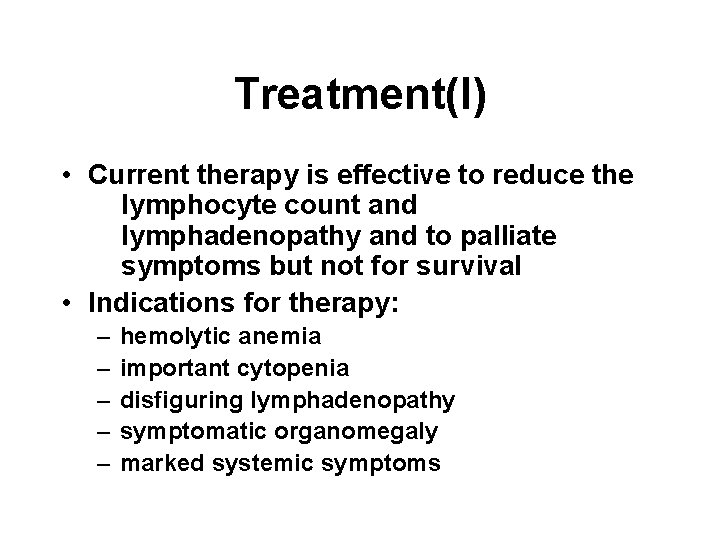
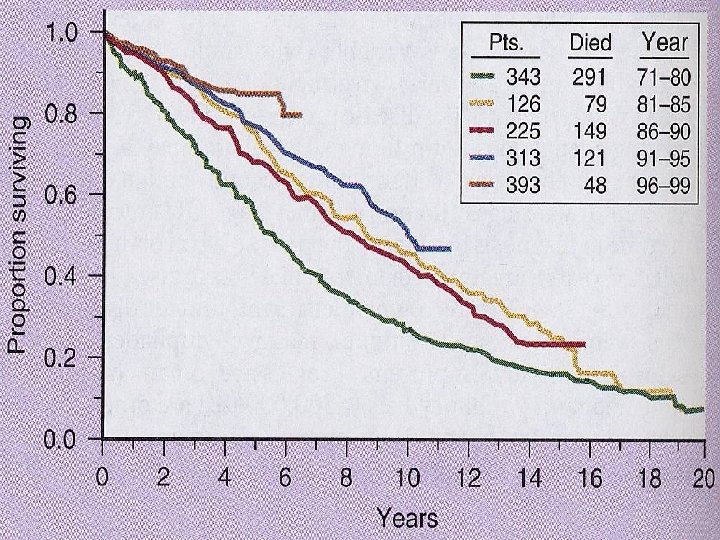
Treatment(I) • Current therapy is effective to reduce the lymphocyte count and lymphadenopathy and to palliate symptoms but not for survival • Indications for therapy: – – – hemolytic anemia important cytopenia disfiguring lymphadenopathy symptomatic organomegaly marked systemic symptoms
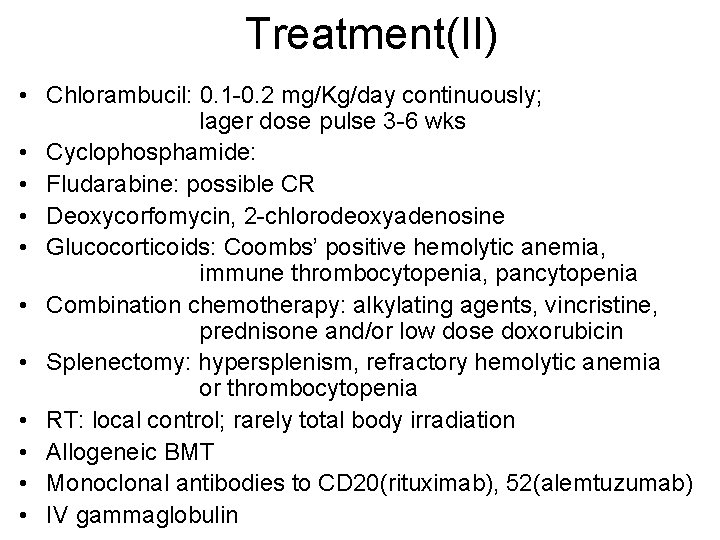
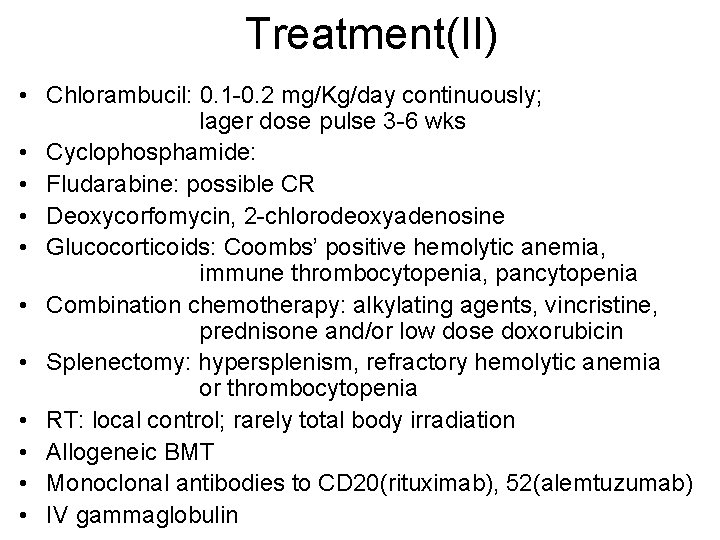
Treatment(II) • Chlorambucil: 0. 1 -0. 2 mg/Kg/day continuously; lager dose pulse 3 -6 wks • Cyclophosphamide: • Fludarabine: possible CR • Deoxycorfomycin, 2 -chlorodeoxyadenosine • Glucocorticoids: Coombs’ positive hemolytic anemia, immune thrombocytopenia, pancytopenia • Combination chemotherapy: alkylating agents, vincristine, prednisone and/or low dose doxorubicin • Splenectomy: hypersplenism, refractory hemolytic anemia or thrombocytopenia • RT: local control; rarely total body irradiation • Allogeneic BMT • Monoclonal antibodies to CD 20(rituximab), 52(alemtuzumab) • IV gammaglobulin
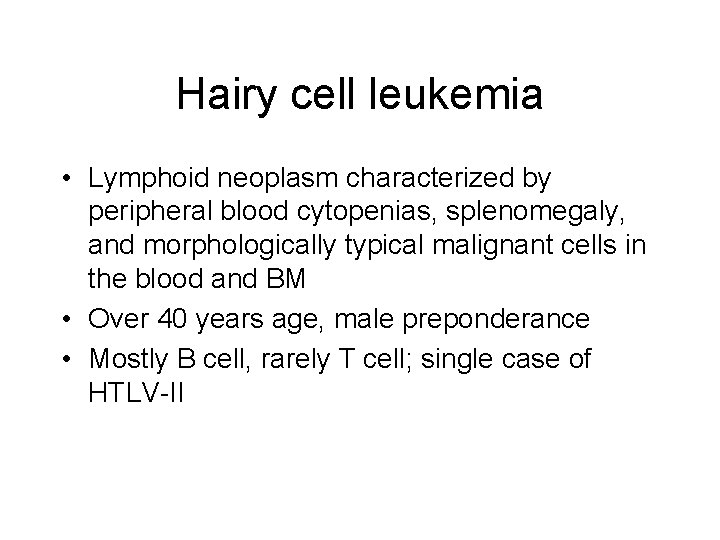
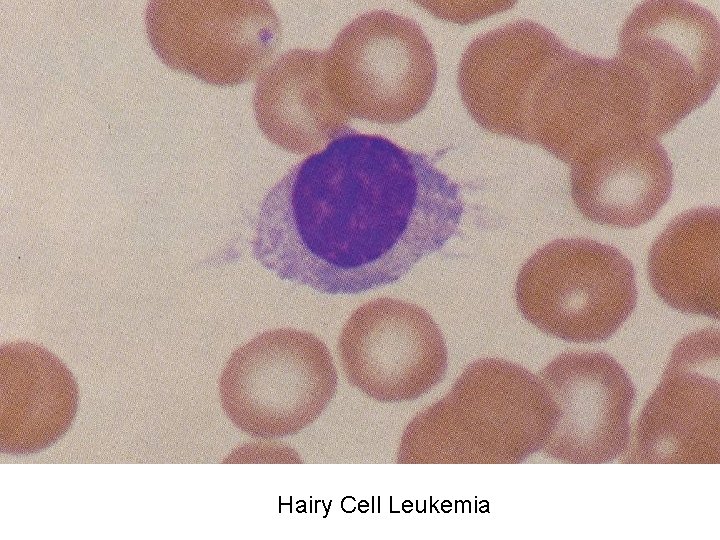
Hairy cell leukemia • Lymphoid neoplasm characterized by peripheral blood cytopenias, splenomegaly, and morphologically typical malignant cells in the blood and BM • Over 40 years age, male preponderance • Mostly B cell, rarely T cell; single case of HTLV-II
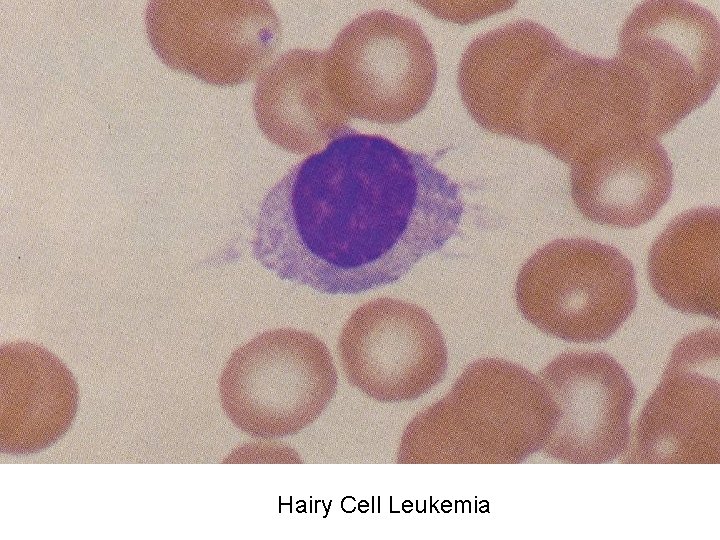
Hairy Cell Leukemia
Clinical features • Splenomegaly; uncommon hepatomegaly; rare lymphadenopathy • Vasculitis: erythema nodosum, cutaneous nodules and polyarteritis nodosa-like • Moderate pancytopenia • Infection caused by impaired host defense: Legionella pneumonitis, toxoplasmosis, Tbc, atypical mycobacterial disease, nocardiosis and pyogenic infection
Diagnosis • Hairy cell: 15 -20 um, eccentrically placed nucleus with foamy cytoplasm, cytoplasmic projection(hairs), positive tartrate-resistant acid phosphatase, B cell antigen, CD 25, IL-2 receptor • Bone marrow aspiration: frequent dry tap due to reticulin fibrosis • DDx: CLL, prolymphocytic lymphoma, Waldenström’s macroglobulinemia
Treatment(I) • No significant cytopenia and complication (25%): no immediate Tx • Indication for Tx: – – – pancytopenia recurrent infection symptomatic splenomegaly autoimmune complication disease progression
Treatment(II) • INF-alpha, deoxycoformycin(pentostatin), 2 chlorodeoxyadenosine(2 CDA) • Splenectomy: for immediate correction of lifethreatening cytopenias • Corticosteroids: only short course for vasculitis or autoimmune Sx • HGF: for cytopenia