Chronic kidney disease Dr Bandar ghazal GFR 60
Chronic kidney disease Dr. Bandar ghazal
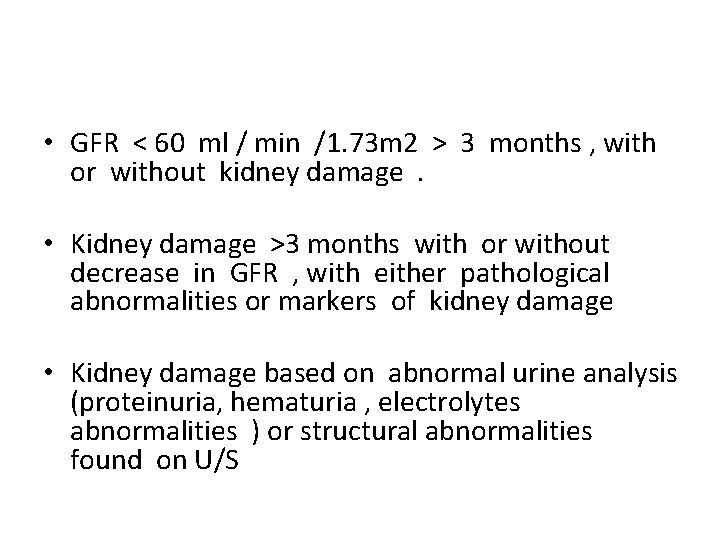
• GFR < 60 ml / min /1. 73 m 2 > 3 months , with or without kidney damage. • Kidney damage >3 months with or without decrease in GFR , with either pathological abnormalities or markers of kidney damage • Kidney damage based on abnormal urine analysis (proteinuria, hematuria , electrolytes abnormalities ) or structural abnormalities found on U/S
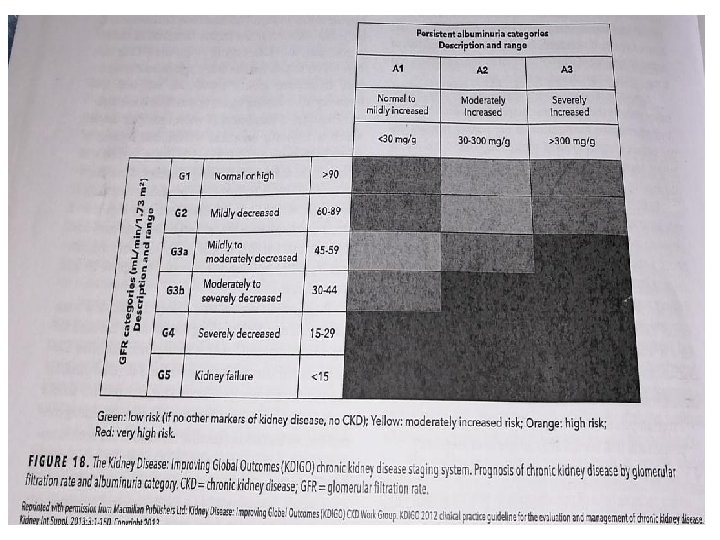
• Grade 1 and 2 do not associated with decrease in GFR and defined by presence of anatomical defects or marker of kidney damage ( hematuria , proteinuria , electrolytes abnormalities ). • CKD may result from various etiologies that cause chronic damage to glomeruli , tubulointerstitium or both. • Not all PT with CKD will progress into ESKD most predictors values are : Baseline GFR Degree of proteinuria , albuminuria.
Risk factors • • DM. HTN. Age >60. Family history of CKD. Cardiovascular disease. Intrinsic kidney disease. Systemic disease.
• CKD typically asymptomatic until reaching stage 4 -5 • Is rarely reversible and leads to progressive decline in renal function. • Reduction in renal mass leads to hypertrophy of the remaining nephrons with hyper filtration , the GFR is transiently at super normal level these adaptation plays a burden of remaining nephrons leading to progressive glomerular sclerosis and interstitial fibrosis , suggesting that hyper filtration in these nephrons worsen renal function
Clinical manifestations • • • • Symptoms are developing slowly Pt may remain asymptomatic until CKD stage 4 -5 Symptoms of uremia : Fatigue Nausea Weakness Pruritis pericarditis Anorexia , nausea , vomiting Metallic taste Hiccups Insomnia Impaired memory Irritability Infertility Menstrual irregularities
• Symptoms of anemia due to reduced erythropoietin. • 1. 25 dihydroxy vitamin deficiency
Examinations • • • Ill PT. HTN common. Skin maybe yellow with evidence of bruising. Uremic breath (fishy breath ). Signs of volume over load.
Labs : • KFT • GFR if less than 60 , refer pt to nephrologist • Urine analysis • Kidney biopsy : In case of glomerulonephritis , unexplained tubulointertitial disease • Anemia on CBC • Metabolic acidosis • Hyperphophatermia • Hypocalcemia • Hyperkalemia • Renal ultrasound : Finding of small echogenic kideney less than 10 cm , support diagnosis of CKD • Renal biopsy is not indicated when size of kidney <9 cm , because it indicates shrunken irreversible kidney.
Complications • Hyperkalemia. • Metabolic acidosis • Cardiovascular disease : Leading cause of death among pt with CKD Mortality risk increase with decline GFR , and increasing albuminuria. Atherosclerosis increase Calcification increase on valves , calcification of arteries Risk of CAD increase Pericarditis due to uremia HF HTN Dyslipidemia : high LDL , low HDL
• Anemia : • Normochromic normocytic anemia • Coagulapathy : PLT dysfunction Mild plt count decrease Bleeding time prolonged Abnormal adhesion and aggregation Petechia , purpura Dialysis decrease bleeding time , but does not normalize it

• Uremic encephalopathy When GFR drop to 15 Neuropathy is found in 65 % of pts with GFR less than 10 %
• Calcium and phosphorus : 3 hormones responsible for regulating PTH ( most important ) VIT D Fibroblast growth factor 23 FGF 23 : PTH : stimulates osteoclast to resorb bone Stimulate formation of 1. 25 dihydroxy vit D Reabsorption of Ca from kidney Increase PO 4 Excretion FGF 23 : Peptide secreted by osteoclast and osteocyte Act on kidney to induce phophateuria , down regulate production of 1. 25 vit d It rise in CKD stage 3 Preceding PTH elevation
With worsening GFR 1. 25 vit d is reduced leading to decrease CA reabsorption FGF Increased Increase PTH due to hypocalcaemia (secondary hyperparathyrodism ) Leading to bone resorption.
• Renal osteodystrophy : Alteration of bone morphology in PT with CKD. Osteitis fibrosa cystica : Due to high bone turn over resulted from exposure to PTH , associated with increased number and activity of osteoclasts And osteoblast and expansion of osteiod surface and replacement of fibrous tissue and cyst Pt may have bone pain (increased turnover with normal mineralization )

• Adynamic bone disease : Lack of bone cell activity and marked reduced rate of bone turnover (Decreased turn over and abnormal minerlaization ) Resulting in increase risk of fracture and bone pain. • Osteomalacia : Decrease mineralization of osteoid • Osteoporosis
• Circulating insulin level are higher due to decrease insulin clearance.
Management • Diet : Minimize salt intake to less than 2 g / d Protein intake less than 1 g/kg K restriction once GFR < 20 ml/min/1. 73 m 2 Less than 60 meq / d Phosphorus restriction Serum PO 4 less than 4. 6 /dl PO 4 binders required when GFR <30 ml / min/1. 73 m 2 MG restriction ( no MG containing laxative or antacids ) • Control of DM. HBA 1 C < 7.
Anemia Common , prevalence increase with stages of CKD. Anemia most often is normocytic , largely caused by lack of erythropoietin due to decline renal mass , other causes such erythropoietin resistance , neocytolysis (decrease survival time of RBC ) and IDA. • Erythropoiesis stimulating agent ESA. For pt with CKD and HB <10 g/dl. • • Trials showed increased CV risk and stroke with ESA and HB >11 g/dl. ESA also showed increased mortality and progression of malignancy in pt with active malignancy. Always check for IDA … goal to keep ferritin > 500 ng/ml Transferrin sat > 30 % By oral or IV ferrous Blood transfusion for pt with sever symptomatic anemia
Metabolic acidosis • • • Defective acid excretion , resulting in reduced bicarbonate generation , Untreated acidosis leads to : Bone loss Muscle loss In early disease metabolic acidosis is typically normal anion gap. With declining GFR organic and inorganic ions retained resulting in high anion gap Studies showed low bicarbonate level increase progression of disease and mortality Alkali therapy : NA bicarbonate , NA citrate When serum HCO 3 persistently < 22 meq/l. Dose of alkali should bring bicarbonate to normal level without causing alkalosis , as alkalosis with reduced GFR increase mortality Despite NA in alkali salt , it does not cause volume expansion or edema , most likely because the accompanying anion is not chloride.
Nephrotoxin • Avoid nephrotoxic medications : NSAIDS ACE , ARBS , in case of hypotension , AKI. PPI , H 2 blocker may cause IN , it also may progress CKD. Adjustment of antibiotics • Adjust doses of medications to avoid accumulation and potential side effect
HTN and dyslipedemia • Target BP <130 /80. • ACE , ARBS are preferred in stage 3 and more also slow progression of CKD. • Other anti HTN is indicated to control BP Statin for dyslipedmia
Proteinuria • Its unclear whether proteinuria is simply a marker of of underlying severity of kidney disease or if proteinuria it self activates inflammatory pathways and contributes to tubulointerstitial fibrosis • ACE I , ARBS , direct renin inhibitor showed decrease proteinuria. • Combination of these medication have no clinical benefit and increase risk of hyperkalemia , low BP, AKI )
For bone dystrophy and hyperphosphatemia • Calcium supplements Calcium carbonate and calcium acetate • 1. 25 vit D.
Fluid overload • Loop diuretics in high doses
VACCINATION • Annual influenza vaccine for all pt with CKD but with ESKD should receive inactivated influenza vaccine • Pt with CKD and nephrotic syndrome should receive pneumococcal vaccine • Advanced CKD and on dialysis should receive vaccination for HEP B virus
• Dialysis : • Peritoneal • Hemodialysis Should be started when GFR of 10 / ml / min Diabetic pt when GFR of 15 ml / min Indications for dialysis : Uremic pericarditis Uremic encephalopathy Coagulopathy Fluid overload unresponsive to diuresis Refractory hyperkalemia Sever metabolic acidosis ph : < 7. 2
• Kidney transplant
- Slides: 31