Chronic inflammations of Larynx Classification Chronic nonspecific laryngitis


- Slides: 34
Chronic inflammations of Larynx

Classification �Chronic nonspecific laryngitis �Chronic specific laryngitis
Chronic Laryngitis Without Hyperplasia (Chronic Hyperaemic Laryngitis) � • Diffuse inflammatory condition symmetrically � involving whole larynx, i. e. true cords, ventricular bands, interarytenoid region and root of the epiglottis
Aetiology Incompletely resolved /recurrent attacks of acute laryngitis. • Chronic infection in PNS, teeth, tonsils and chest • Occupational exposure to dust &fumes - miners, strokers, gold & iron smiths, chemical industry workers. • Smoking and alcohol • Persistent cough • Vocal abuse
Clinical features � Hoarseness - Voice- easily tired and aphonic by end of day � • Constant hawking - dryness and intermittent tickling in the throat � • Discomfort in throat & dry and irritating cough
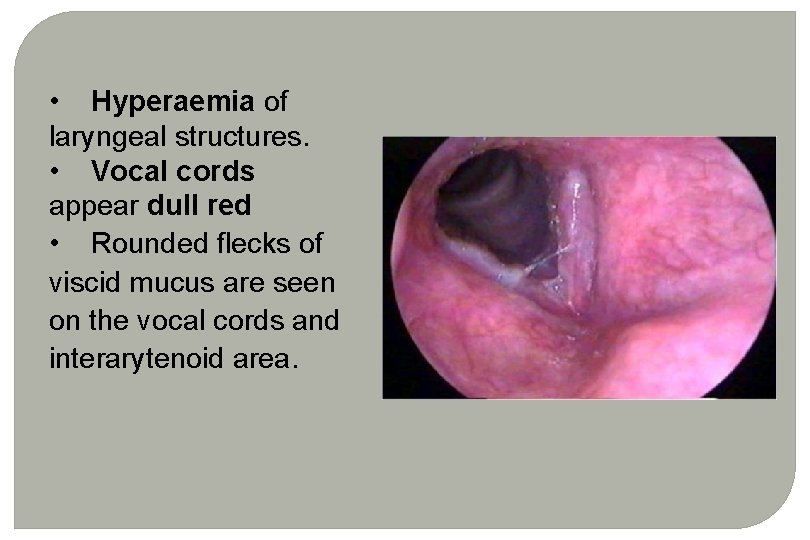
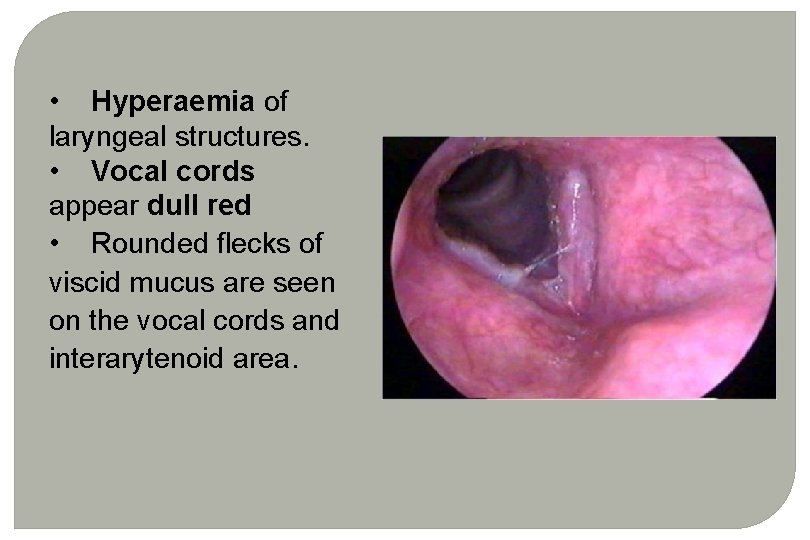
• Hyperaemia of laryngeal structures. • Vocal cords appear dull red • Rounded flecks of viscid mucus are seen on the vocal cords and interarytenoid area.
Treatment • Eliminate infection of upper or lower respiratory tract • Avoidance of irritating factors - smoking, alcohol, polluted environment, dust and fumes • Voice rest and speech therapy • Steam inhalation. • Expectorants
Chronic Hypertrophic Laryngitis (Chronic Hyperplastic Laryngitis) � Diffuse and symmetrical process /localised � appearing like a tumour of the larynx. � • Localised - dysphonia plica ventricularis, vocal nodules, vocal polyp, Reinke's oedema and contact ulcer
• Aetiology - Same as chronic laryngitis without hyperplasia • Pathology - starts in the glottis and later may extend to false cords, base of epiglottis and subglottis. • Mucosa, submucosa, mucous glands, in later stages intrinsic muscles and joints may be affected.
• Initially, there is hyperaemia, oedema and cellular infiltration in the submucosa. • Pseudostratified celiated epithelium ^ squamous type & squamous epithelium of the VCs ^ hyperplasia and keratinisation. • Mucous glands - hypertrophy at first but later atrophy ^diminished secretion and dryness of larynx.
Clinical features • Males (8: 1) in 30 -50 years. • Hoarseness, constant desire to clear throat, dry cough, tiredness of voice, and discomfort in throat. Changes - diffuse and symmetrical
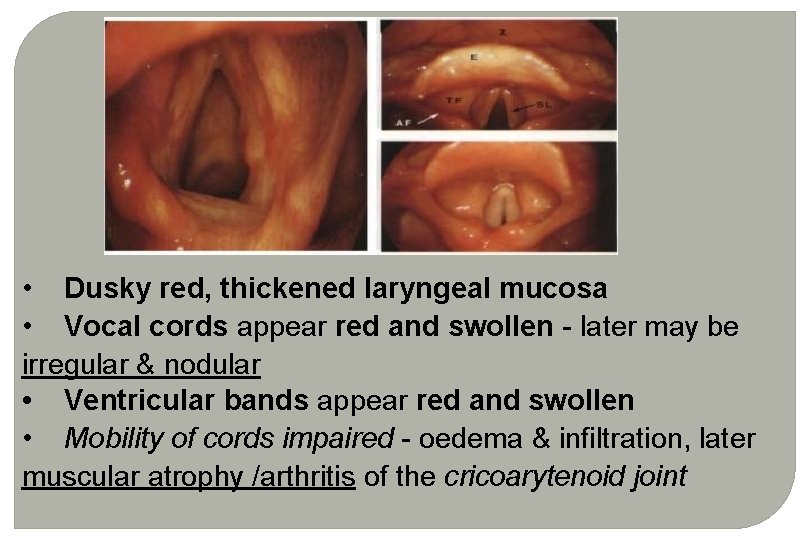
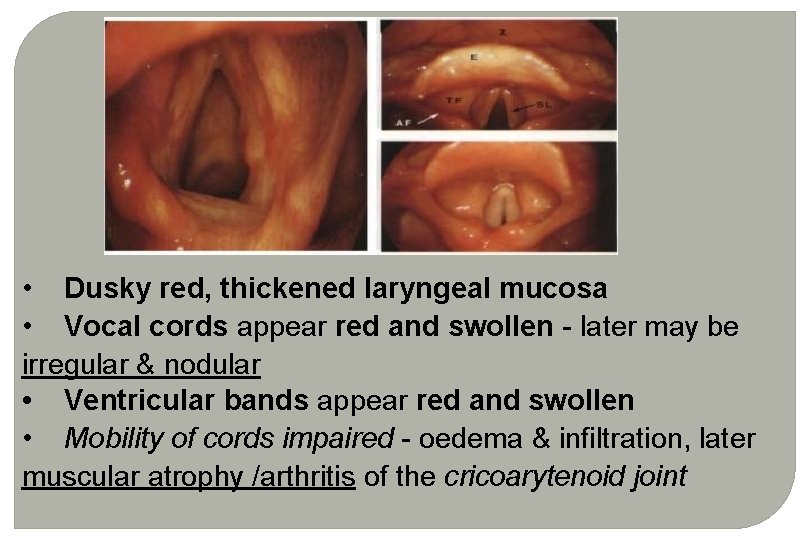
• Dusky red, thickened laryngeal mucosa • Vocal cords appear red and swollen - later may be irregular & nodular • Ventricular bands appear red and swollen • Mobility of cords impaired - oedema & infiltration, later muscular atrophy /arthritis of the cricoarytenoid joint
Treatment • Conservative - as for chronic laryngitis without hyperplasia • Surgical - Stripping of vocal cords, removing the hyperplastic, oedematous mucosa, may be done in selected cases
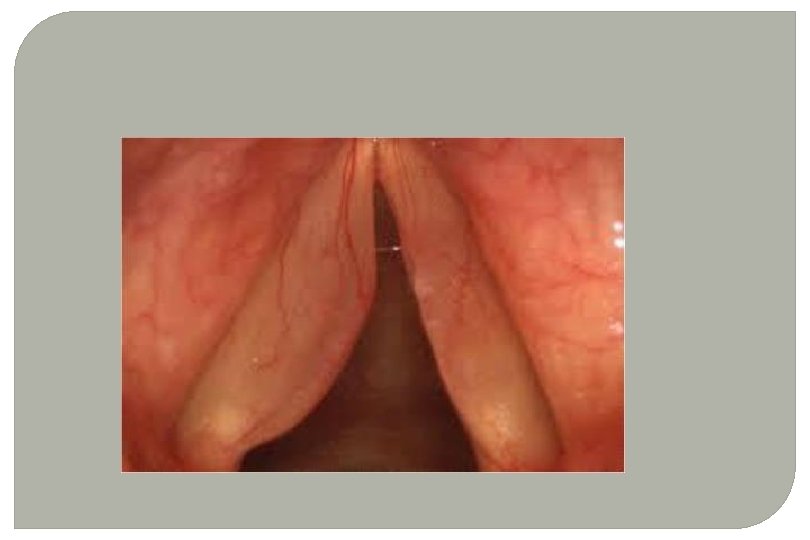
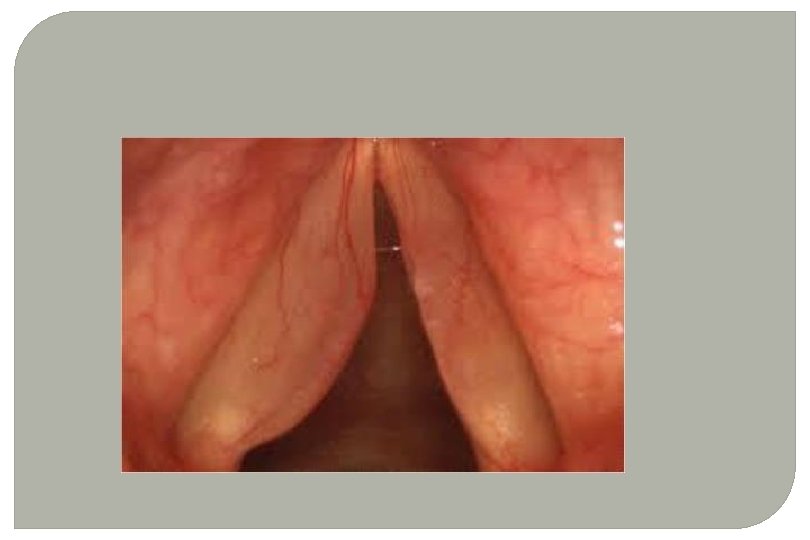
POLYPOID DEGENERATION OF VOCAL CORDS (REINKE'S OEDEMA) • Bilateral symmetrical swelling of membranous part of the VCs. • Middle-aged men and women • Oedema of the subepithelial space (Reinke’s space) of the VCs • Chronic irritation of VCs due to misuse of voice, heavy smoking, chronic sinusitis and laryngopharyngeal reflex
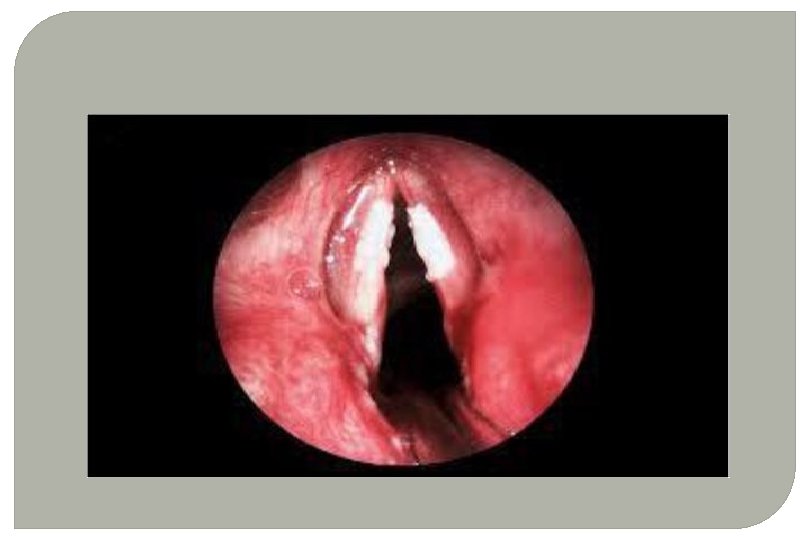
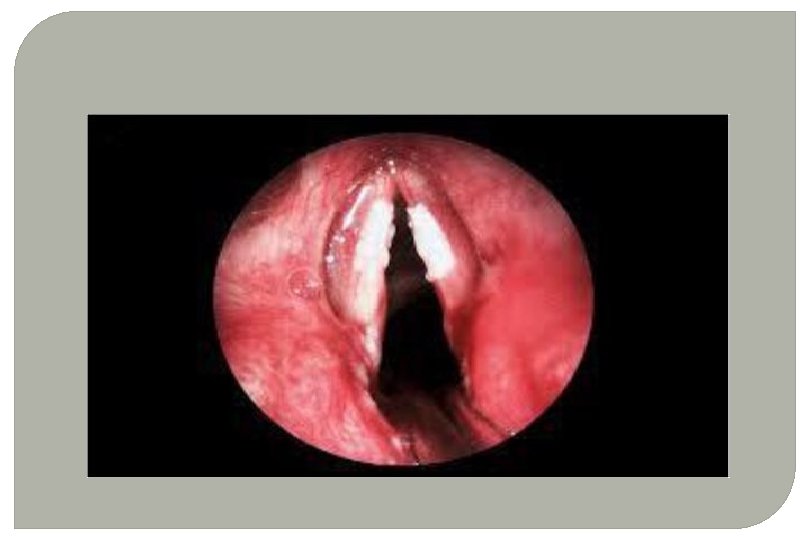
Clinical Features • Hoarseness • False cords for voice production - low pitched and rough voice • VCs - fusiform swellings with pale translucent look. • Ventricular bands may appear hyperaemic and hypertrophic
Treatment • Decortication of the vocal cords - removal of strip of epithelium. • Voice rest. • Speech therapy
PACHYDERMIA LARYNGIS • Form of chronic hypertrophic laryngitis affecting posterior part of larynx - interarytenoid and posterior part of the vocal cords. • Hoarseness or husky voice and irritation in the throat • Heaping up of red or grey granulation tissue in the interarytenoid region and posterior thirds of VCs
• latter some times showing ulceration -contact ulcer • Bilateral and symmetrical. • It does not undergo malignant change • Biopsy - to differentiate from carcinoma and tuberculosis
• Mostly men who indulge in excessive alcohol and smoking • Excessive forceful talking and GERD • Treatment - removal of granulation tissue under operating microscope. • Control of acid reflux • Speech therapy.
ATROPHIC LARYNGITIS (LARYNGITIS SICCA) • Atrophy of laryngeal mucosa and crust formation • Women, associated with atrophic rhinitis and pharyngitis. • Hoarseness, temporarily improves on coughing and removal of crusts. • Dry irritating cough and sometimes dyspnoea
• Atrophic mucosa covered with foul smelling crusts removed - may show excoriation and bleeding • Treatment - elimination of cause and humidification. • Laryngeal sprays- glucose in glycerine / oil of pine • Expectorants with ammonium chloride or iodides • Treat associated nasal and pharyngeal conditions
TUBERCULOSIS OF LARYNX • Secondary to pulmonary tuberculosis, • Mostly males in middle age group. • Tubercle bacilli reach the larynx by bronchogenic or haematogenous spread.
Pathology ■ Tubercle bacilli, carried by sputum from the bronchi, settle and penetrate the intact laryngeal mucosa particularly in the interarytenoid region Affects posterior larynx - interarytenoid fold, false cords, VCs and epiglottis, in that order ■ formation of submucosal tubercles ■ caseation and ulceration ■ Laryngeal mucosa appears red and swollen due to cellular infiltration (pseudoedema) ■ Stage of perichondritis and cartilage necrosis
Symptoms Clinical features depend on the stage of tuberculosis. ■ Weakness of voice is the earliest symptom ■ Hoarseness ■ Severe pain which may radiate to the ears ■ Odynophagia ■ Marked dysphagia in later stages.
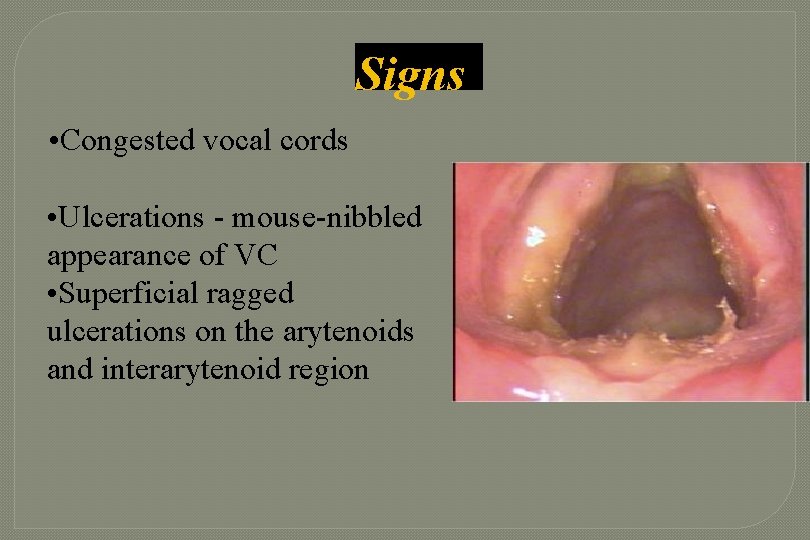
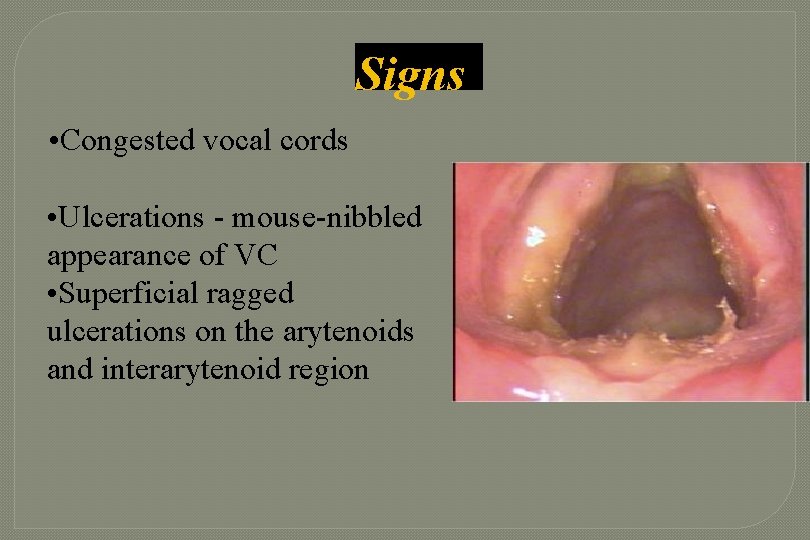
Signs • Congested vocal cords • Ulcerations - mouse-nibbled appearance of VC • Superficial ragged ulcerations on the arytenoids and interarytenoid region
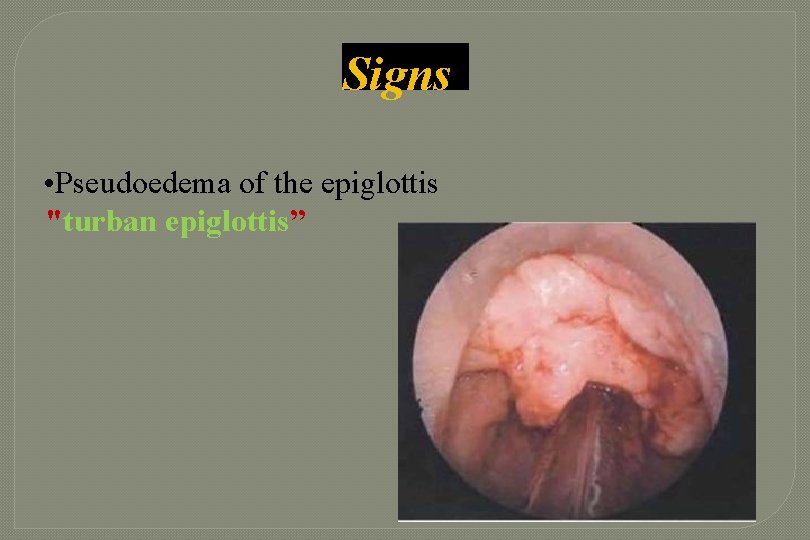
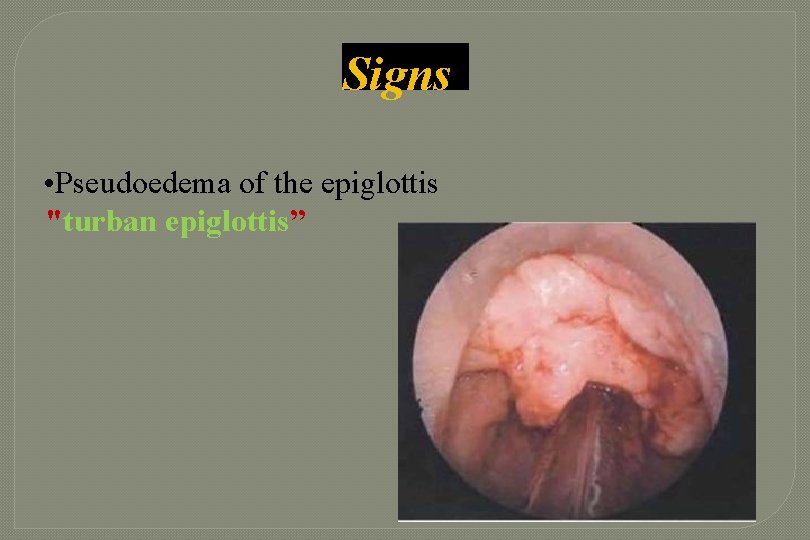
Signs • Pseudoedema of the epiglottis "turban epiglottis”
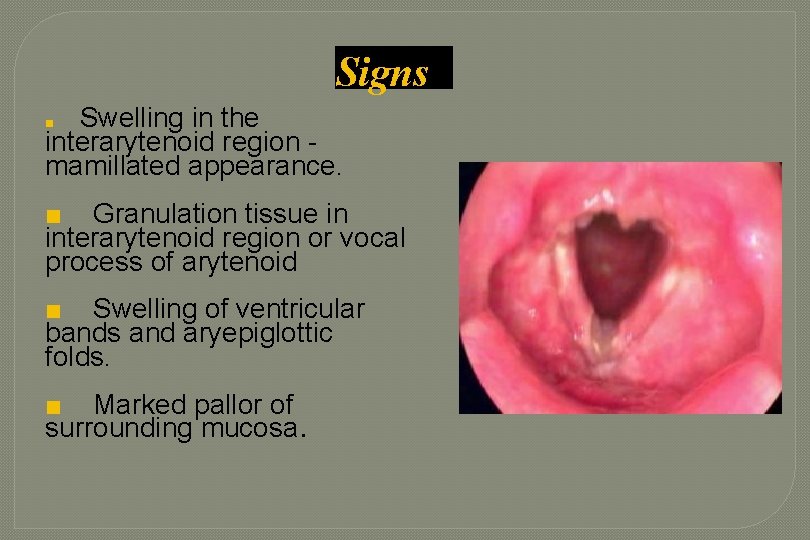
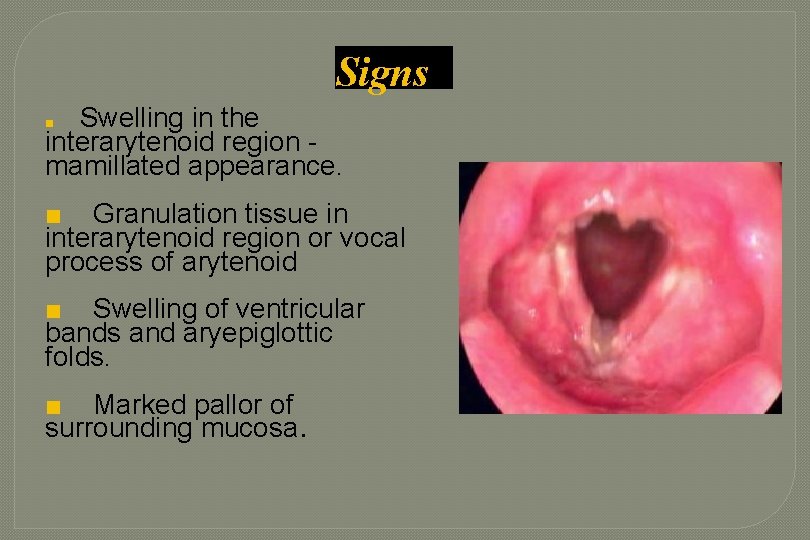
Signs Swelling in the interarytenoid region mamillated appearance. ■ ■ Granulation tissue in interarytenoid region or vocal process of arytenoid ■ Swelling of ventricular bands and aryepiglottic folds. ■ Marked pallor of surrounding mucosa.
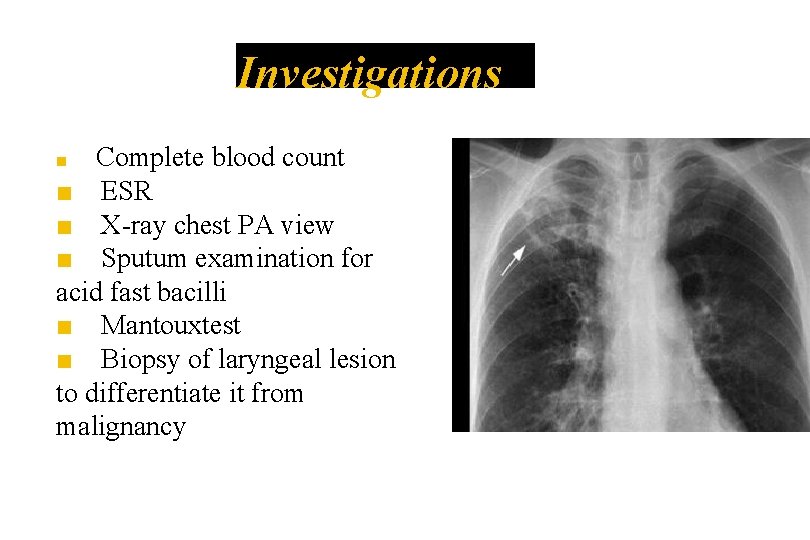
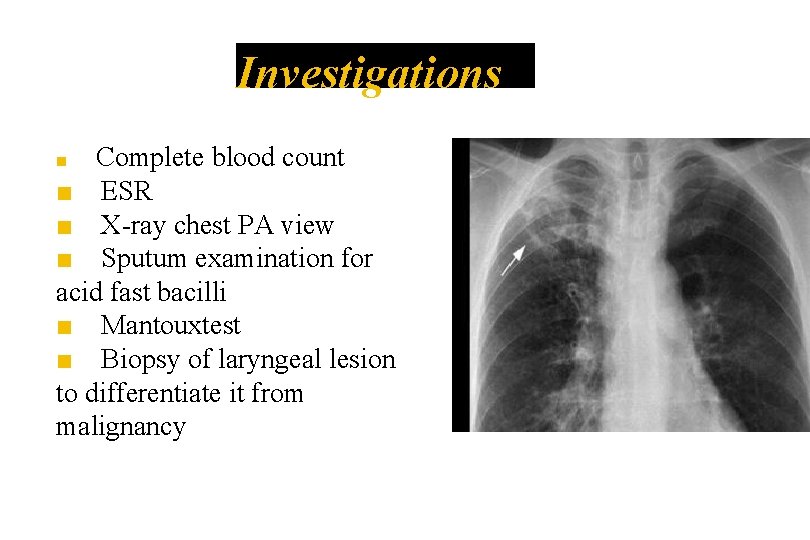
Investigations Complete blood count ■ ESR ■ X-ray chest PA view ■ Sputum examination for acid fast bacilli ■ Mantouxtest ■ Biopsy of laryngeal lesion to differentiate it from malignancy ■
Treatment ■ Treatment is the same as for pulmonary tuberculosis. ■ Category I of DOTS regimen ■ Voice rest
LUPUS OF THE LARYNX • Indolent tubercular infection associated with lupus of nose and pharynx • Anterior larynx - Epiglottis is involved first and may be completely destroyed. • Spreads to AE folds and sometimes to false cords • Painless and often asymptomatic • Treatment is antitubercular drugs

Laryngeal Syphilis �Congenital/tertiary �Anterior commissure, anterior 1/3 rd of vocal cords �Hoarse voice and stridor �ILS: Diffuse hypertrophy of mucosa, gummatous ulcer �Anti syphilitic treatment
Scleroma of larynx �Klebisella rhinoscleromatis �Submucosal involvement of subglottis �Stridor �Steroids, doxycyclin �Dilatation of stricture