Chronic Heart Failure Fluid Overload Hyponatremia and Increased

- Slides: 34
Chronic Heart Failure: Fluid Overload, Hyponatremia, and Increased Creatinine John Lynn Jefferies, MD, MPH, FACC, FAHA Director, Advanced Heart Failure and Cardiomyopathy Associate Professor, Pediatric Cardiology and Adult Cardiovascular Diseases Associate Professor, Division of Human Genetics The Heart Institute Cincinnati Children’s Hospital Medical Center
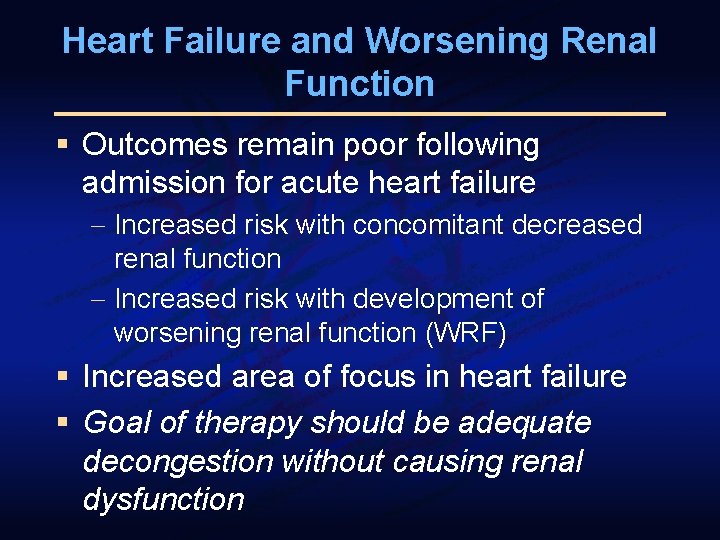
Heart Failure and Worsening Renal Function § Outcomes remain poor following admission for acute heart failure - Increased risk with concomitant decreased renal function - Increased risk with development of worsening renal function (WRF) § Increased area of focus in heart failure § Goal of therapy should be adequate decongestion without causing renal dysfunction
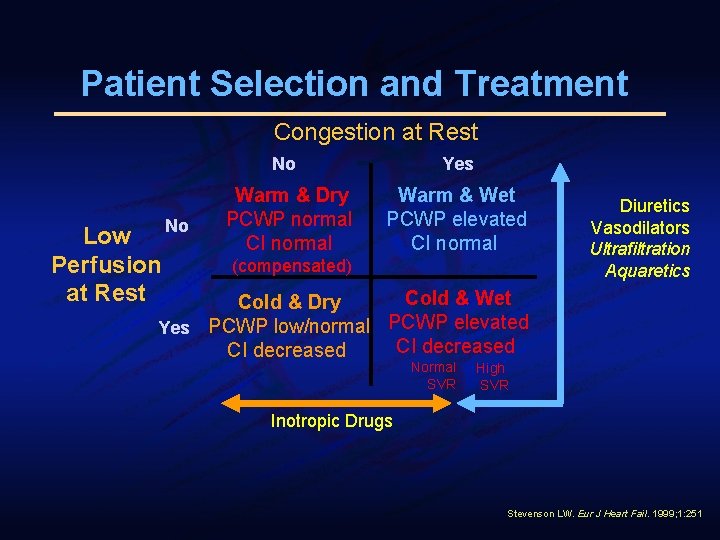
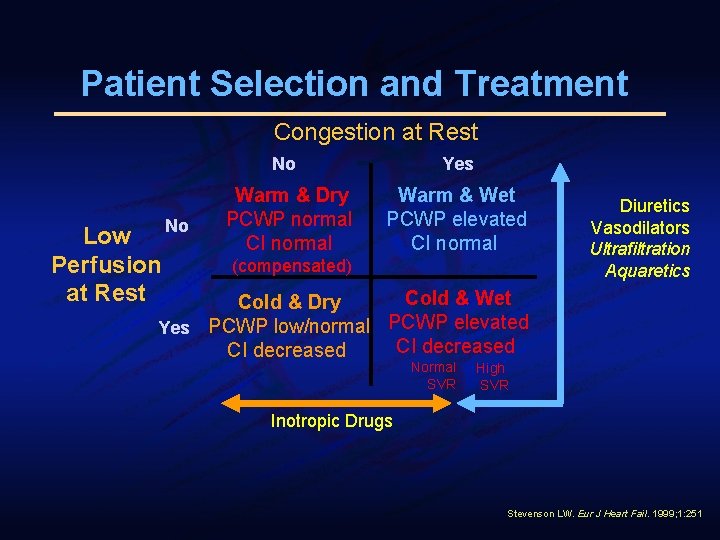
Patient Selection and Treatment Congestion at Rest Low No Perfusion at Rest No Yes Warm & Dry PCWP normal CI normal Warm & Wet PCWP elevated CI normal (compensated) Diuretics Vasodilators Ultrafiltration Aquaretics Cold & Wet Cold & Dry Yes PCWP low/normal PCWP elevated CI decreased Normal SVR High SVR Inotropic Drugs Stevenson LW. Eur J Heart Fail. 1999; 1: 251
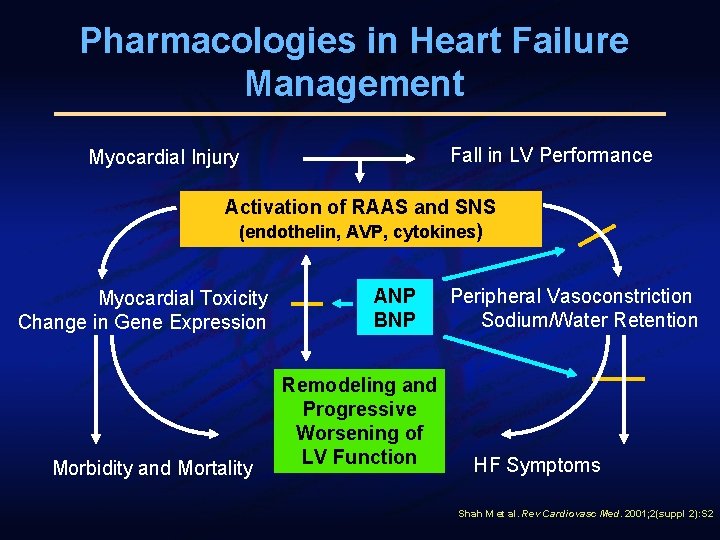
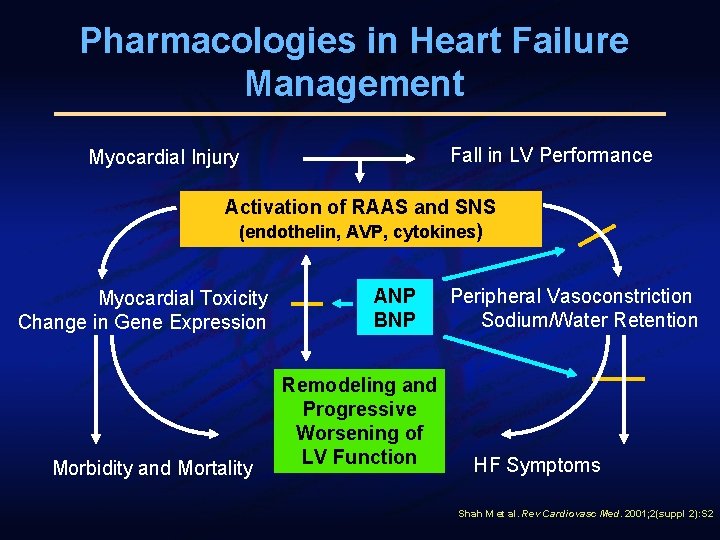
Pharmacologies in Heart Failure Management Fall in LV Performance Myocardial Injury Activation of RAAS and SNS (endothelin, AVP, cytokines) Myocardial Toxicity Change in Gene Expression Morbidity and Mortality ANP BNP Remodeling and Progressive Worsening of LV Function Peripheral Vasoconstriction Sodium/Water Retention HF Symptoms Shah M et al. Rev Cardiovasc Med. 2001; 2(suppl 2): S 2
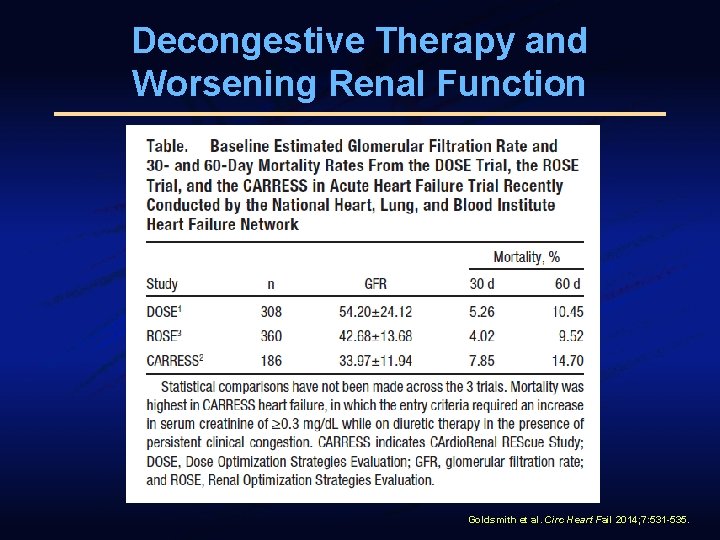
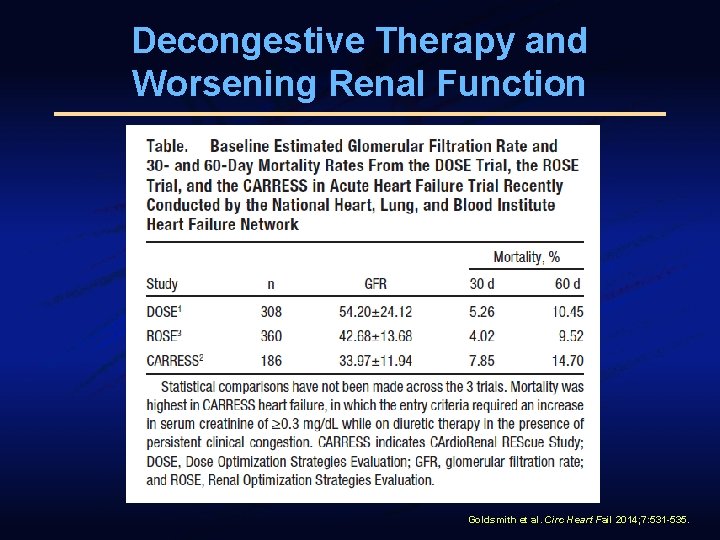
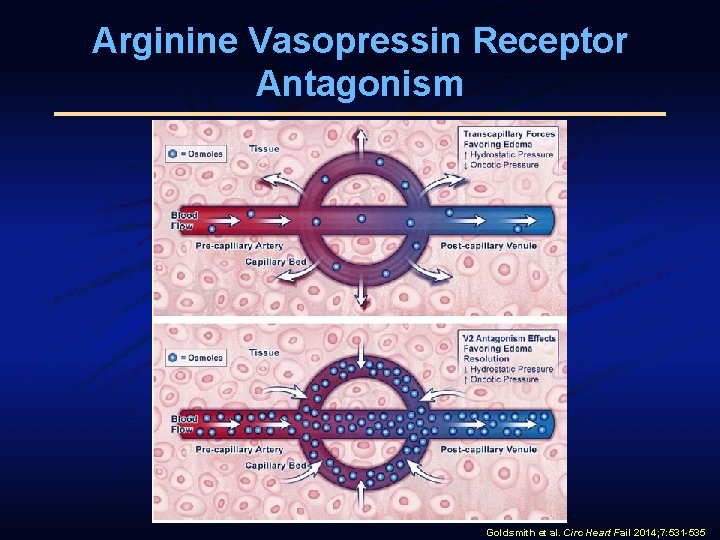
Decongestive Therapy and Worsening Renal Function Goldsmith et al. Circ Heart Fail 2014; 7: 531 -535.
Causes of Worsening Renal Function § § Underdiuresis Progression of underlying disease Overdiuresis Transient reduction in intravascular volume - “Plasma refill rate” or the rate that the intravascular volume is replenished by the extravascular space
Treatment Strategies § Diuretics § Ultrafiltration § “Aquaretics”
Diuretics

Diuretics and the Cardiorenal Syndrome § Treatment of symptoms is an important consideration in management of ADHF § Typically involves use of intravenous diuretics § Diuretics may worsen renal function § Continued use of diuretics may result in further kidney injury Ronco et al. J Am Coll Cardiol 2012; 60: 1031 -42. Felker GM, Mentz RJ. J Am Coll Cardiol 2012; 59: 2145 -53.
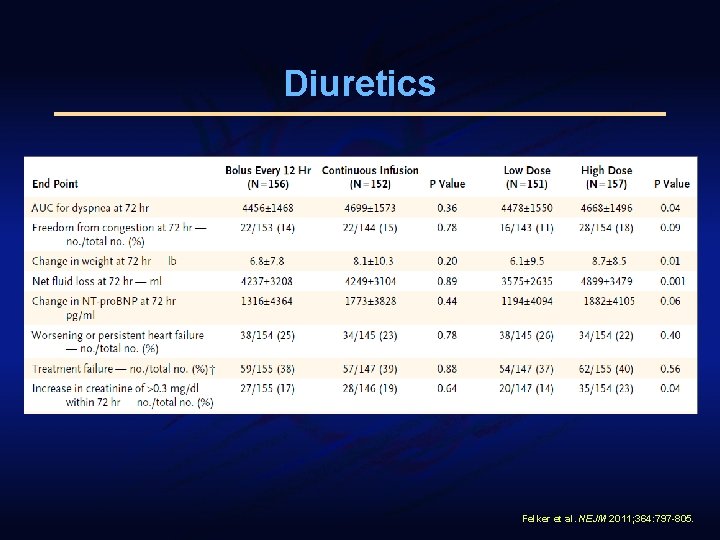
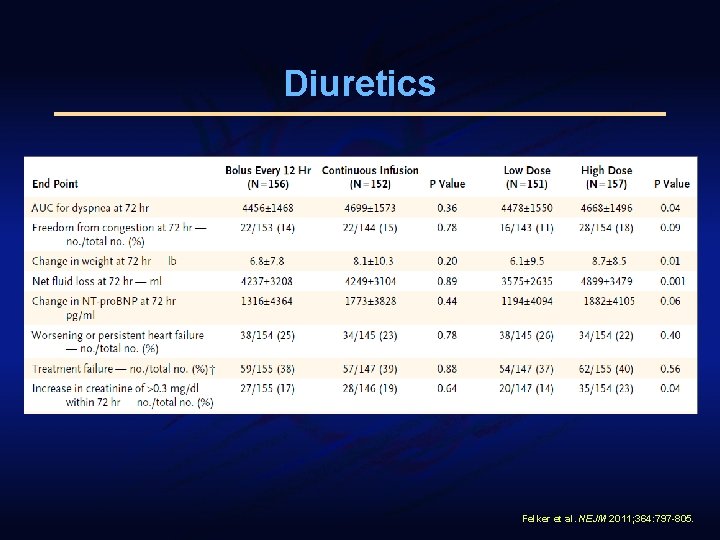
Diuretics Felker et al. NEJM 2011; 364: 797 -805.
Ultrafiltration
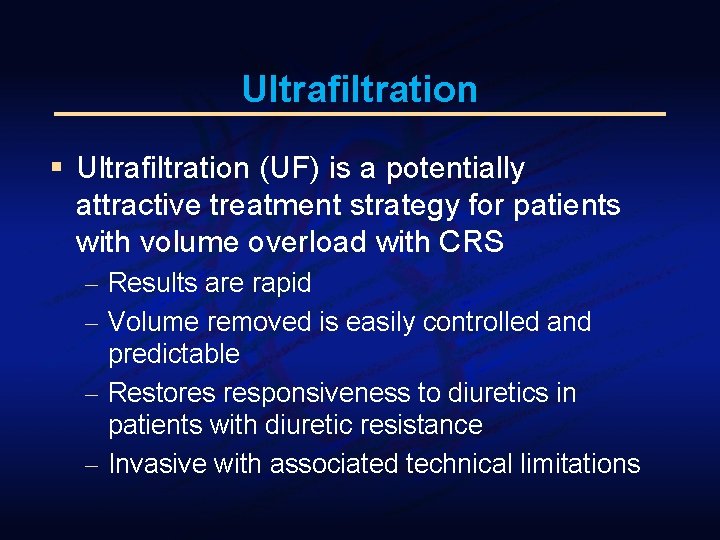
Ultrafiltration § Ultrafiltration (UF) is a potentially attractive treatment strategy for patients with volume overload with CRS - Results are rapid - Volume removed is easily controlled and predictable - Restores responsiveness to diuretics in patients with diuretic resistance - Invasive with associated technical limitations
Ultrafiltration § Additional advantages that may be of benefit in ADHF - Little to no activation of the neurohormonal system that diuretics - No significant deleterious effects on electrolytes Schrier RW. J Am Coll Cardiol 2006; 47: 1 -8.
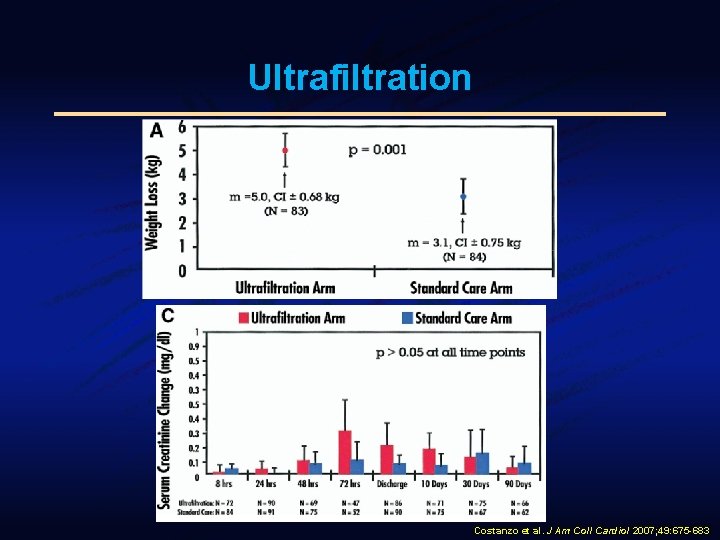
Ultrafiltration in Heart Failure § Initial data was generated in heart failure with low ejection fraction (HFLEF) § Costanzo et al. reported on 200 patients randomized to intravenous diuretics or ultrafiltration § No differences in serum creatinine between the two treatments Costanzo et al. J Am Coll Cardiol 2007; 49: 675 -683
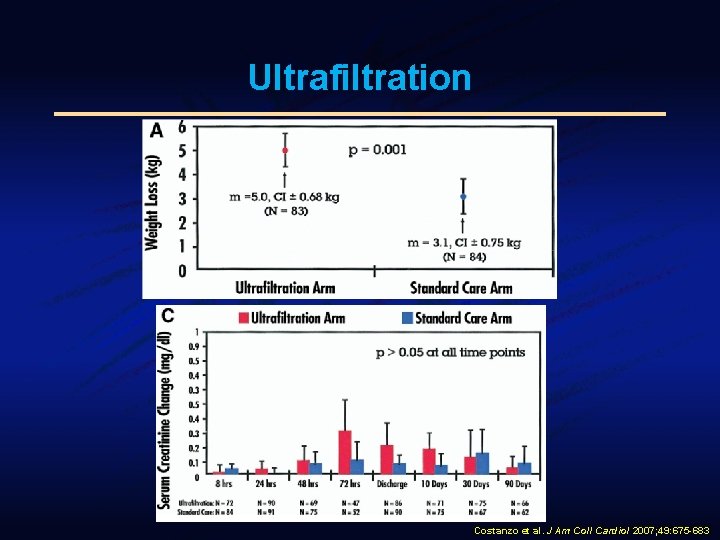
Ultrafiltration Costanzo et al. J Am Coll Cardiol 2007; 49: 675 -683
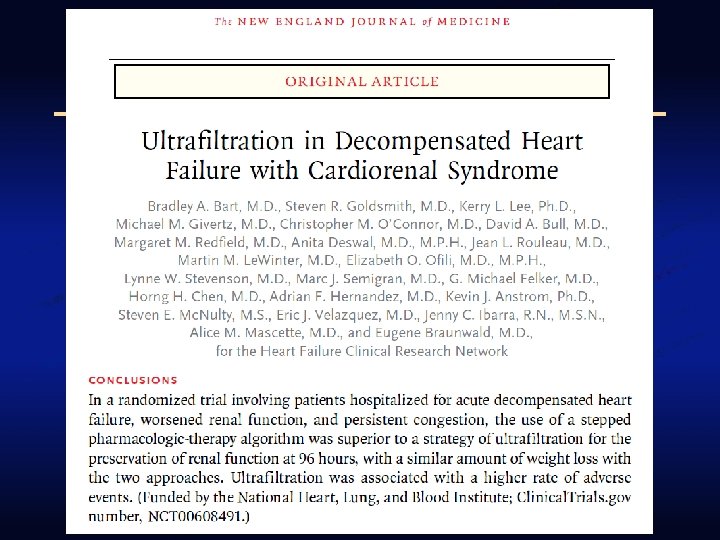
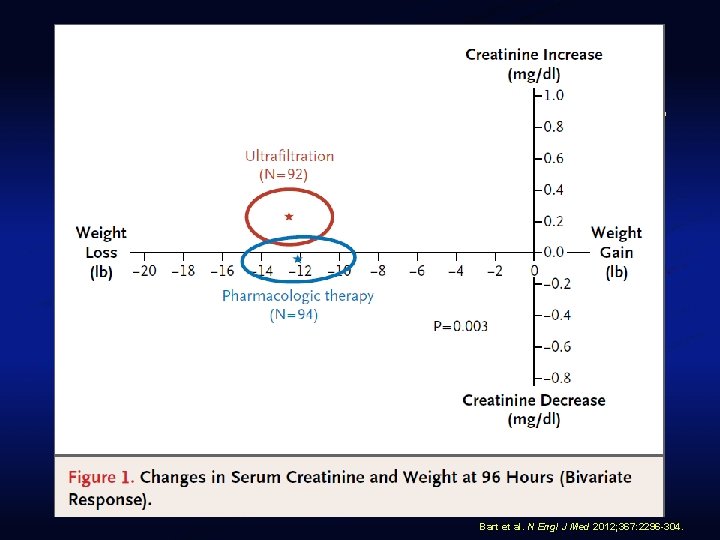
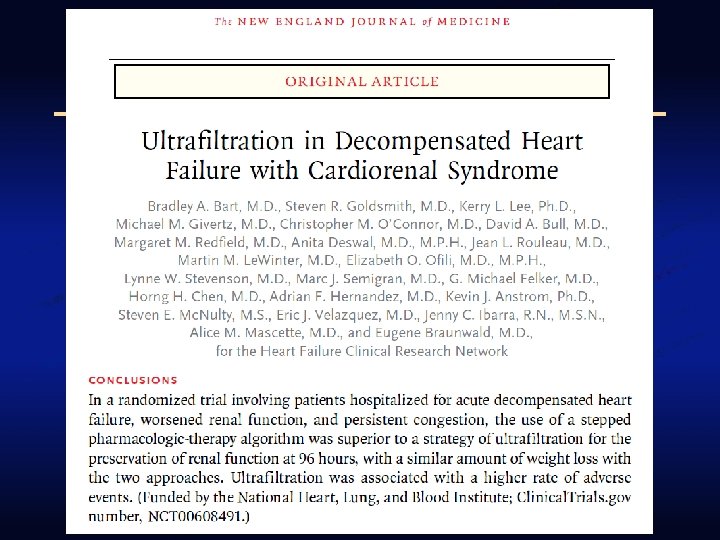
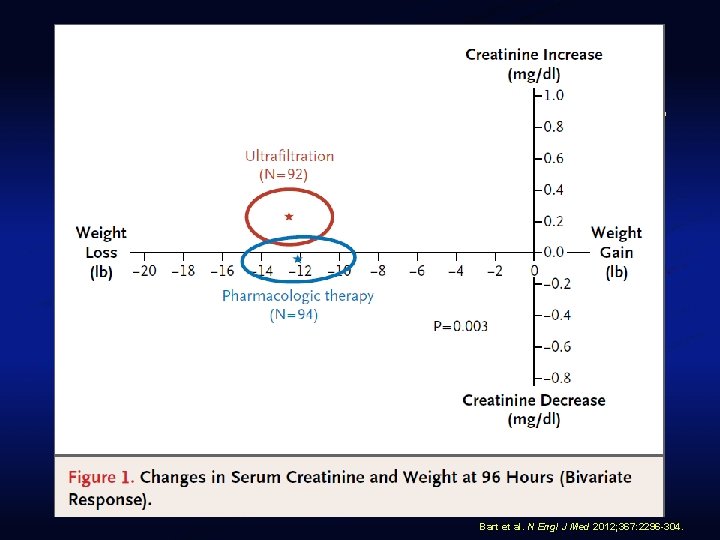
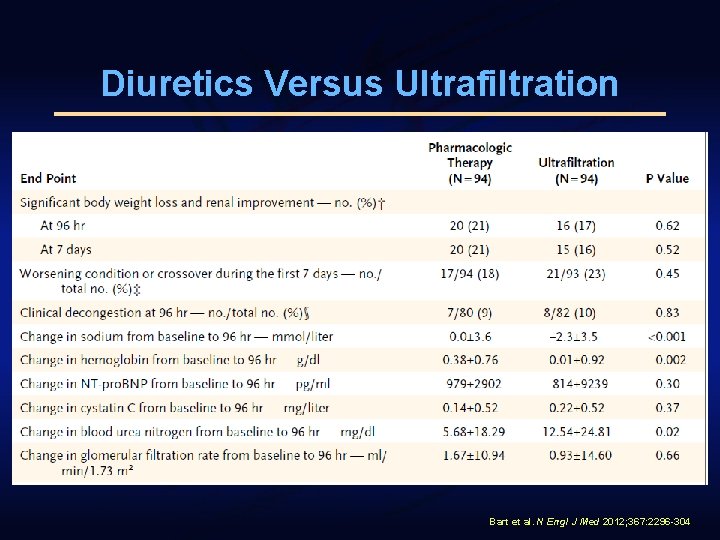
Bart et al. N Engl J Med 2012; 367: 2296 -304.
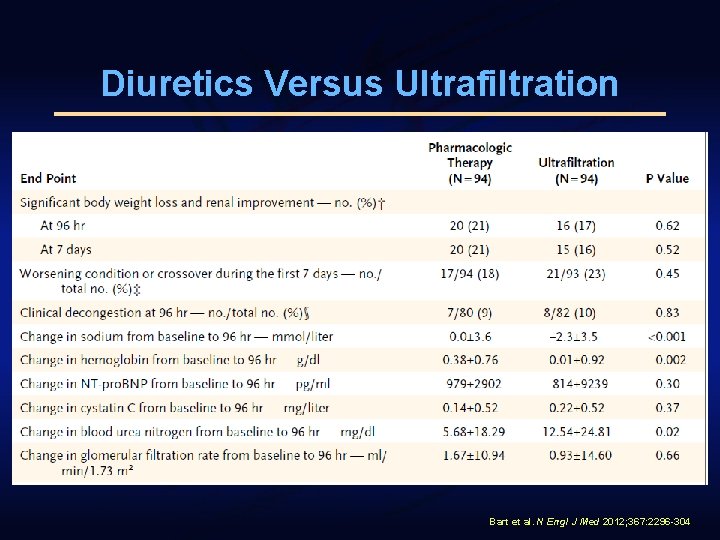
Diuretics Versus Ultrafiltration Bart et al. N Engl J Med 2012; 367: 2296 -304
Ultrafiltration in Heart Failure § Evidence primarily in HFLEF population § Some patients in UNLOAD had LVEF>40% § Suggested that therapy may be an option in heart failure with preserved ejection fraction (HFPEF) § Single center study comparing ultrafiltration in HFLEF versus HFPEF Jefferies et al. Circ Heart Fail 2013; 6: 733 -739
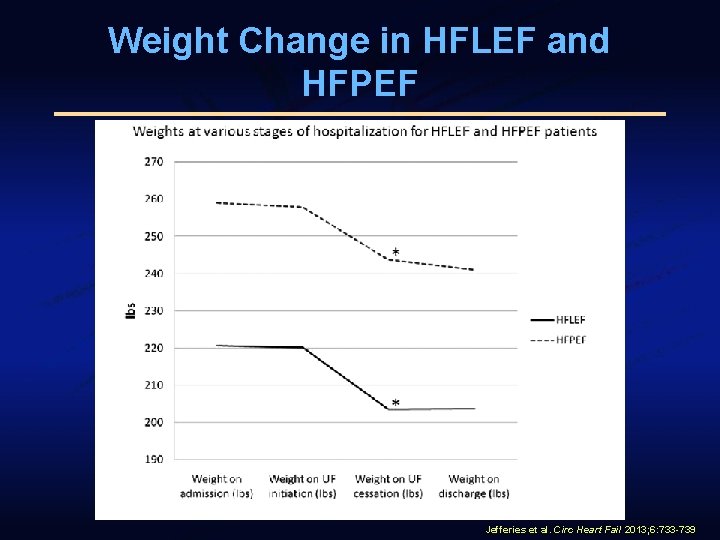
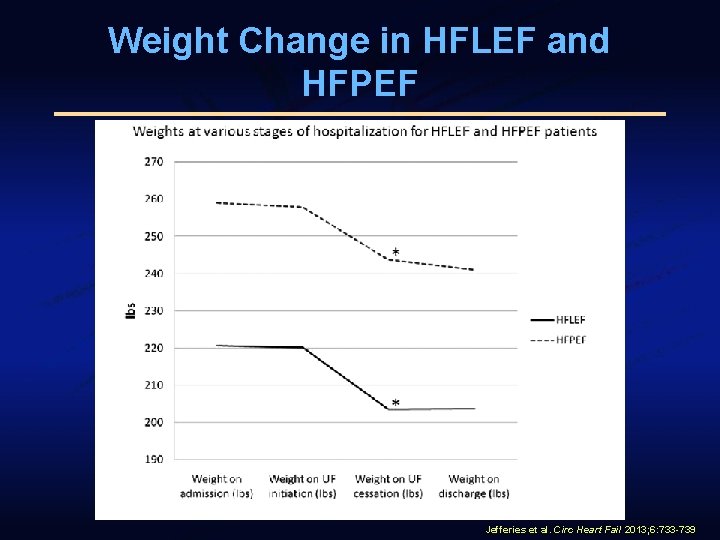
Weight Change in HFLEF and HFPEF Jefferies et al. Circ Heart Fail 2013; 6: 733 -739
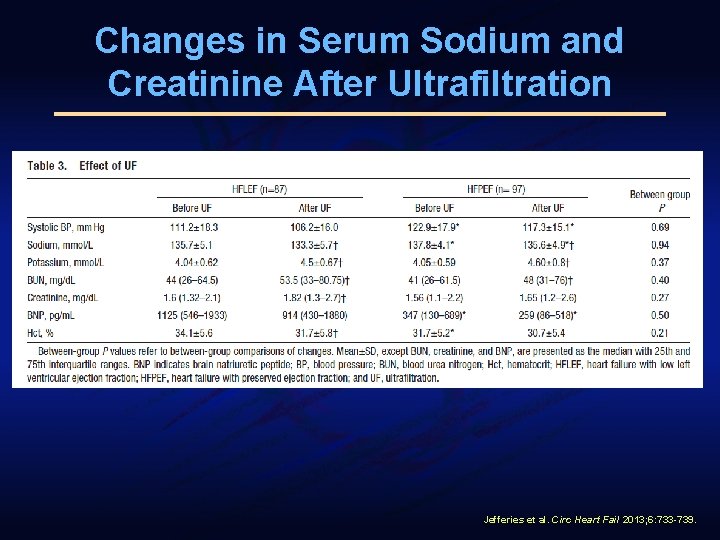
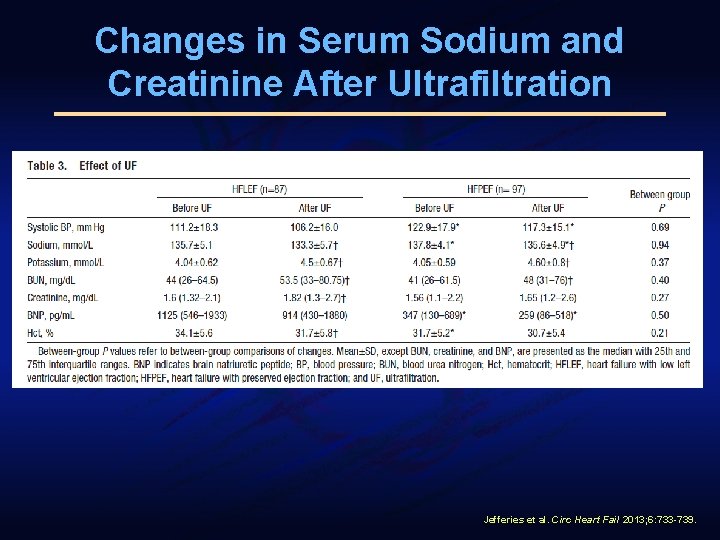
Changes in Serum Sodium and Creatinine After Ultrafiltration Jefferies et al. Circ Heart Fail 2013; 6: 733 -739.
Decongestive Therapy and Renal Function § Both diuretics and ultrafiltration use may be associated with worsening renal function § Diuretics result in direct neurohormonal stimulation - Increased renin levels § Ultrafiltration can lead to transient intravascular volume depletion § Necessitates a newer strategy with less likelihood of causing WRF
V 2 Receptor Antagonists “Aquaretics”
Arginine Vasopressin Receptor Antagonism § Vaptans are competitive antagonists of the vasopressin receptor - Primarily directed at the V 2 receptor § Currently approved for treatment of euvolemic or hypervolemic hyponatremia - Tolvaptan (selective V 2 RA), conivaptan (V 1/V 2 RA) § Increasing amount of interest in utility of these drugs for decongestion
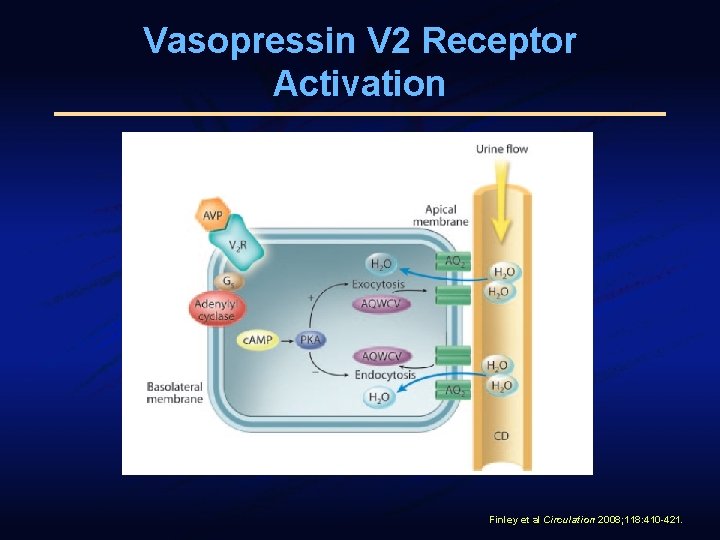
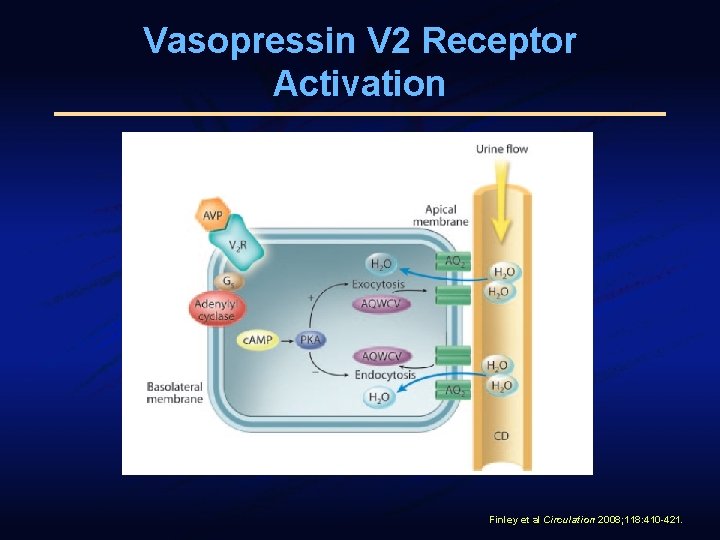
Vasopressin V 2 Receptor Activation Finley et al Circulation 2008; 118: 410 -421.
Arginine Vasopressin Receptor Antagonism § V 2 -receptor blockade in the renal collecting ducts results in: - Increase in free water clearance (aquaresis) - Increase in serum sodium - Decrease in urine osmolality - No significant changes in urinary sodium or potassium excretion - No effect on serum potassium
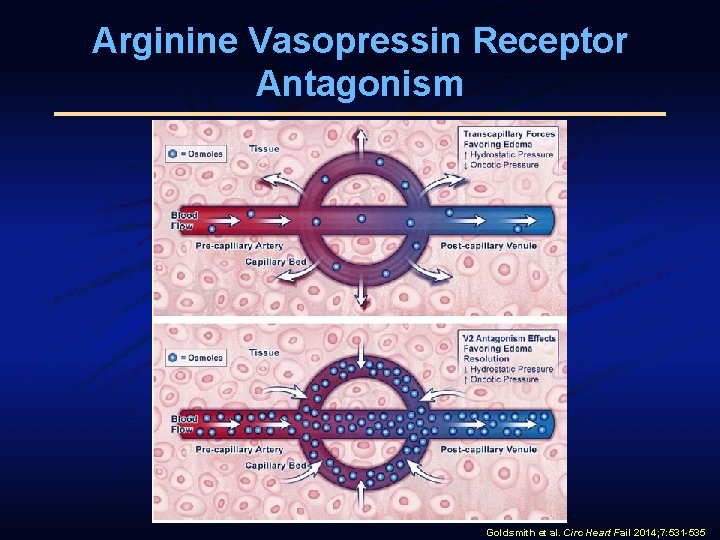
Arginine Vasopressin Receptor Antagonism Goldsmith et al. Circ Heart Fail 2014; 7: 531 -535
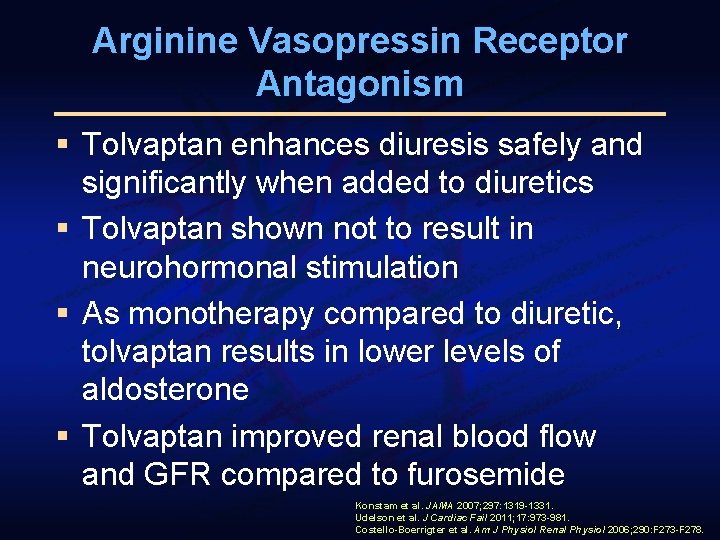
Arginine Vasopressin Receptor Antagonism § Tolvaptan enhances diuresis safely and significantly when added to diuretics § Tolvaptan shown not to result in neurohormonal stimulation § As monotherapy compared to diuretic, tolvaptan results in lower levels of aldosterone § Tolvaptan improved renal blood flow and GFR compared to furosemide Konstam et al. JAMA 2007; 297: 1319 -1331. Udelson et al. J Cardiac Fail 2011; 17: 973 -981. Costello-Boerrigter et al. Am J Physiol Renal Physiol 2006; 290: F 273 -F 278.
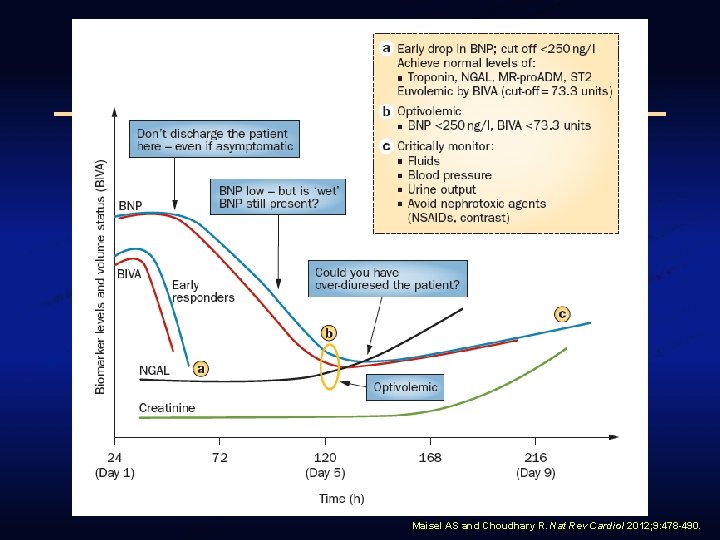
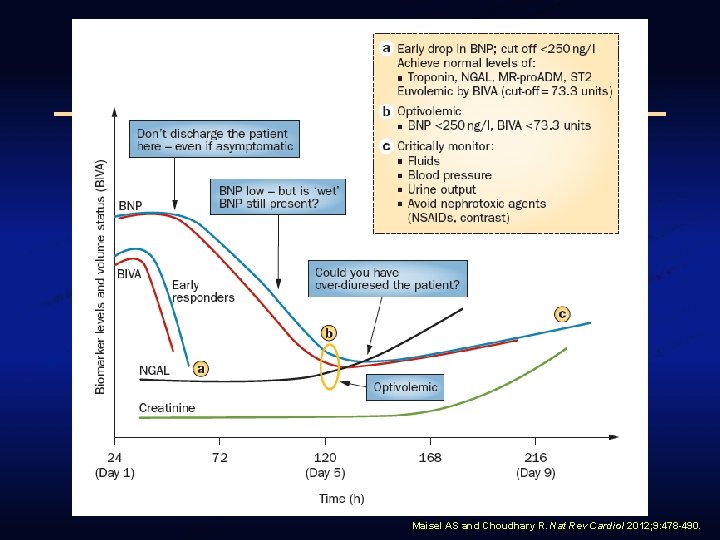
Maisel AS and Choudhary R. Nat Rev Cardiol 2012; 9: 478 -490.
Best Decongestive Strategy? § Prospective randomized study in adults with acute heart failure and volume overload § Three arms of therapy - Usual care + tolvaptan - Ultrafiltration
Best Decongestive Strategy? § Primary endpoint: Net change in weight § Secondary endpoints: - 30 day all cause readmission - 30 day all cause death - Serum creatinine change (baseline to peak and baseline to discharge) - Serum sodium and potassium changes - Length of stay and dyspnea score - Net volume loss - Changes in urine n. GAL (AKI biomarker)
Conclusions § Management of volume overload in acute heart failure continues to offer unique challenges § Increasingly common to have concomitant electrolyte derangement or renal dysfunction § Use of diuretics continues to be the most widely available option § Unfavorable impacts have prompted interest in alternative modalities
Conclusions § Mixed results for ultrafiltration in adult populations § Ongoing assessment with different biomarkers may help define institution and duration of ultrafiltration § Different populations such as HFPEF and pediatric patients may offer insights into optimal use of this technology § Improved surveillance techniques needed to avoid intravascular depletion
Conclusions § Aquaretic therapy either alone or in combination with otherapies may be a viable opportunity § May result in safer and more effective decongestion without negatively impacting renal function or electrolytes § Underscores need for individualized therapies