Chronic disease Practice Policy Presentation to AHS Health









- Slides: 22

Chronic disease Practice & Policy Presentation to AHS Health Policy Advisory Group Tom O’Dowd & Susan Smith

Patients with multiple chronic illnesses : • • Die prematurely Longer hospital stays More depression More medications Poorer function Poorer access to specialists Excluded from trials
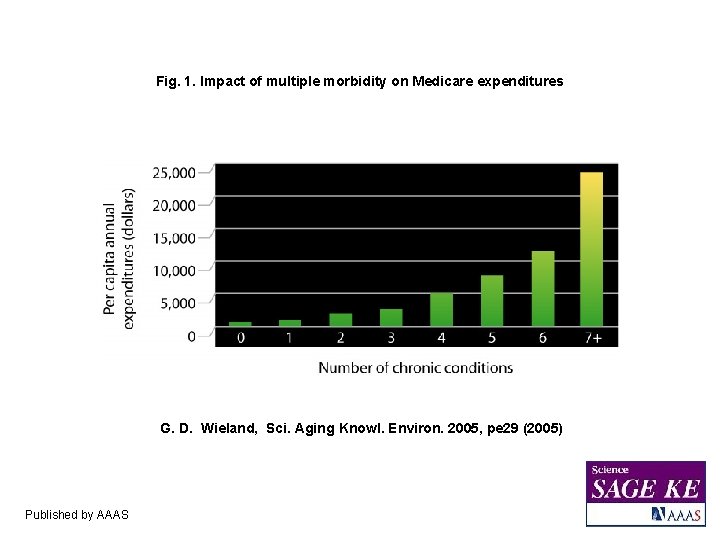
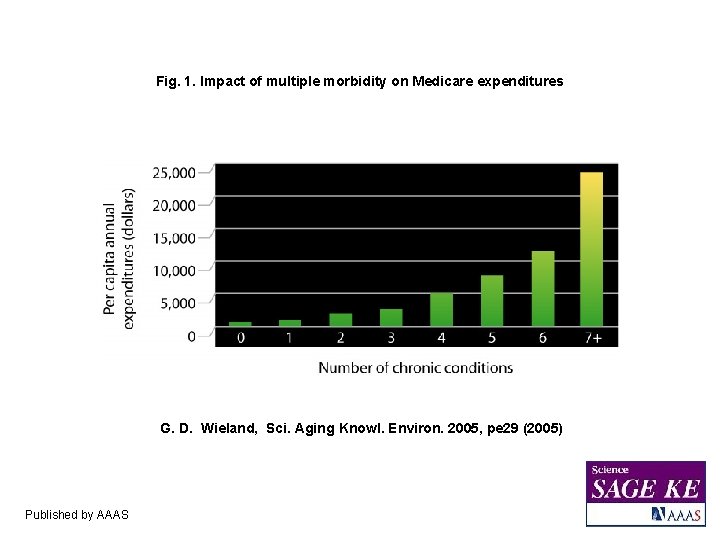
Fig. 1. Impact of multiple morbidity on Medicare expenditures G. D. Wieland, Sci. Aging Knowl. Environ. 2005, pe 29 (2005) Published by AAAS
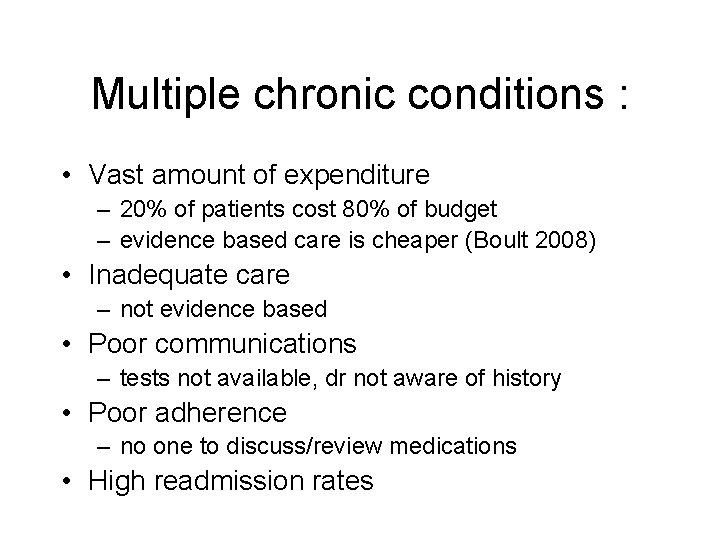
Multiple chronic conditions : • Vast amount of expenditure – 20% of patients cost 80% of budget – evidence based care is cheaper (Boult 2008) • Inadequate care – not evidence based • Poor communications – tests not available, dr not aware of history • Poor adherence – no one to discuss/review medications • High readmission rates
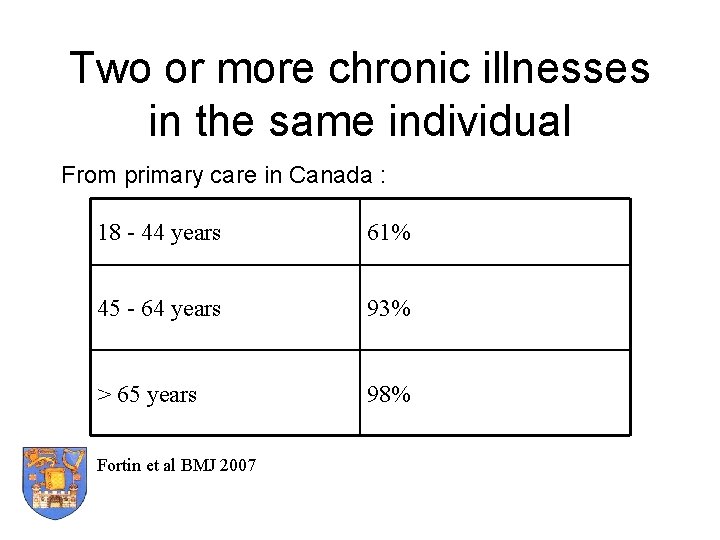
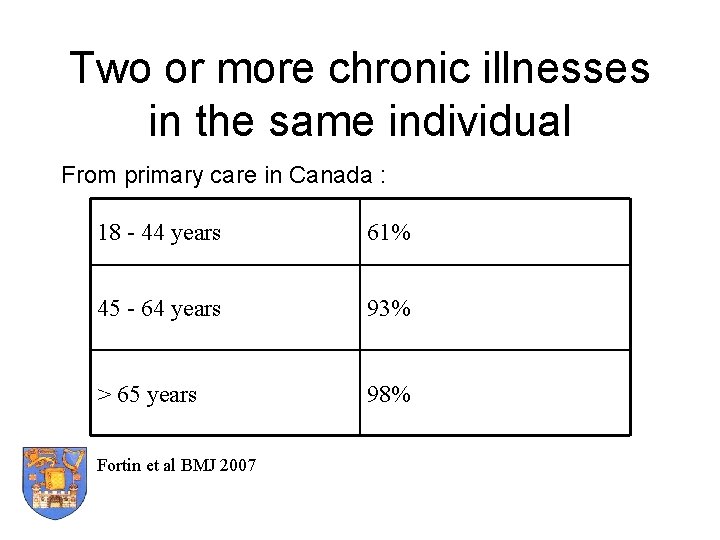
Two or more chronic illnesses in the same individual From primary care in Canada : 18 - 44 years 61% 45 - 64 years 93% > 65 years 98% Fortin et al BMJ 2007
New concept : Multimorbidity • Existence of 2 or more chronic conditions in the same patient • Can co-exist like CVD & DM – or not - like arthritis & asthma • Literature review : most references come from primary care


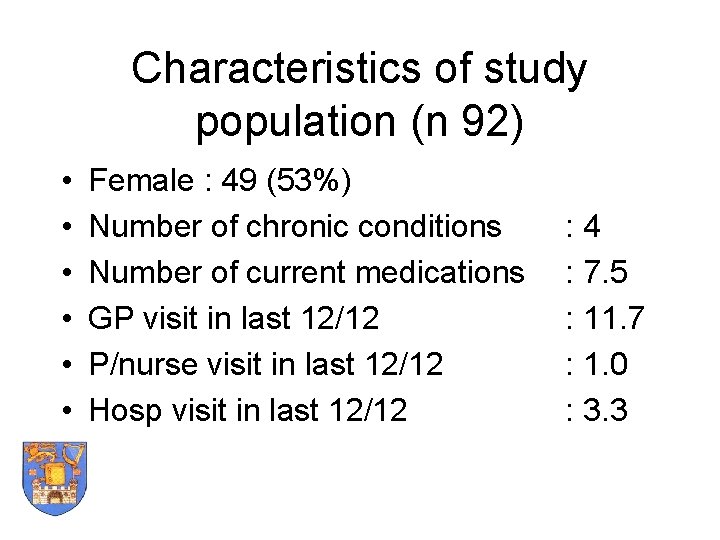
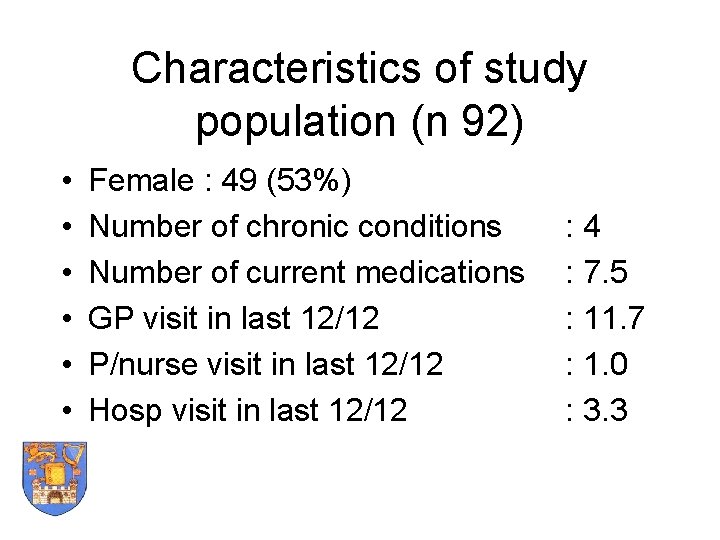
Characteristics of study population (n 92) • • • Female : 49 (53%) Number of chronic conditions Number of current medications GP visit in last 12/12 P/nurse visit in last 12/12 Hosp visit in last 12/12 : 4 : 7. 5 : 11. 7 : 1. 0 : 3. 3
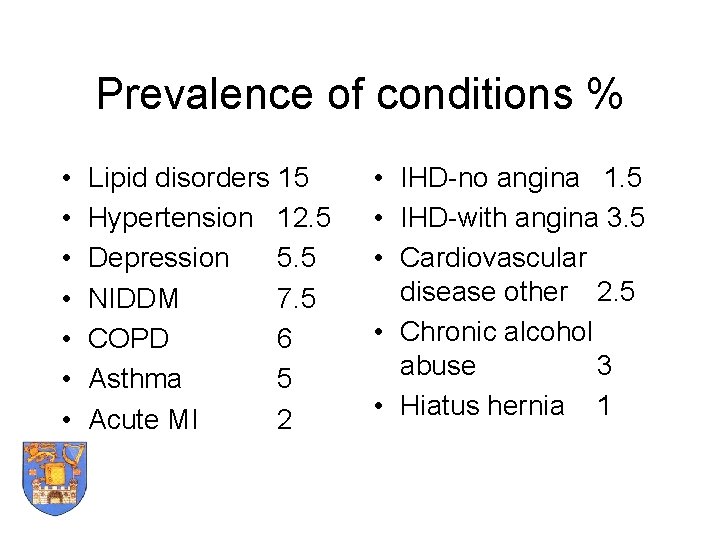
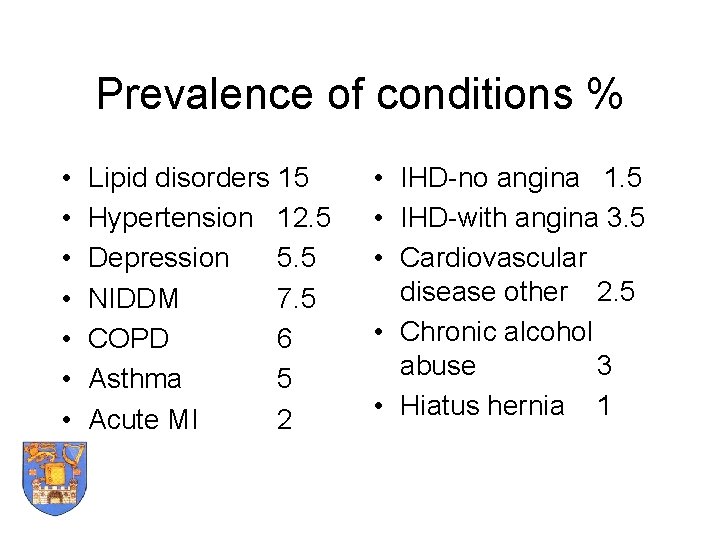
Prevalence of conditions % • • Lipid disorders 15 Hypertension 12. 5 Depression 5. 5 NIDDM 7. 5 COPD 6 Asthma 5 Acute MI 2 • IHD-no angina 1. 5 • IHD-with angina 3. 5 • Cardiovascular disease other 2. 5 • Chronic alcohol abuse 3 • Hiatus hernia 1
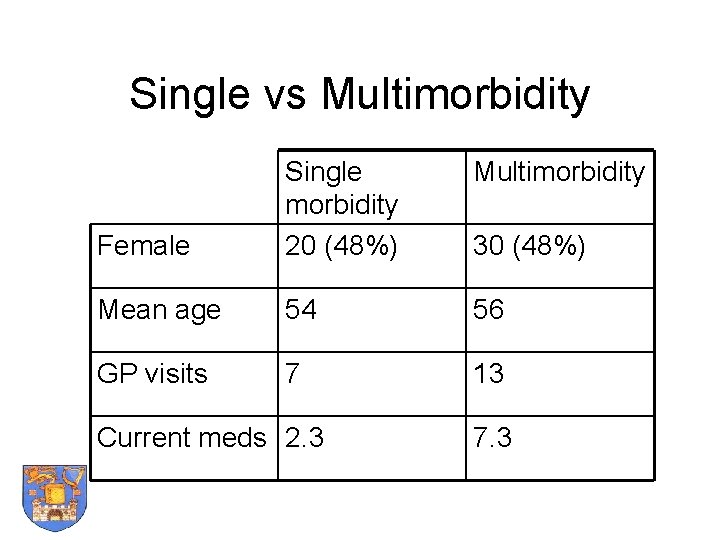
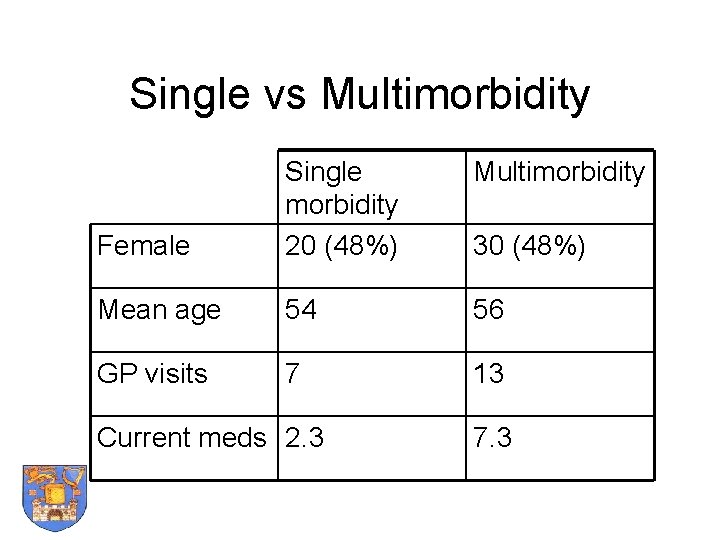
Single vs Multimorbidity Female Single morbidity 20 (48%) Mean age 54 56 GP visits 7 13 Current meds 2. 3 30 (48%) 7. 3
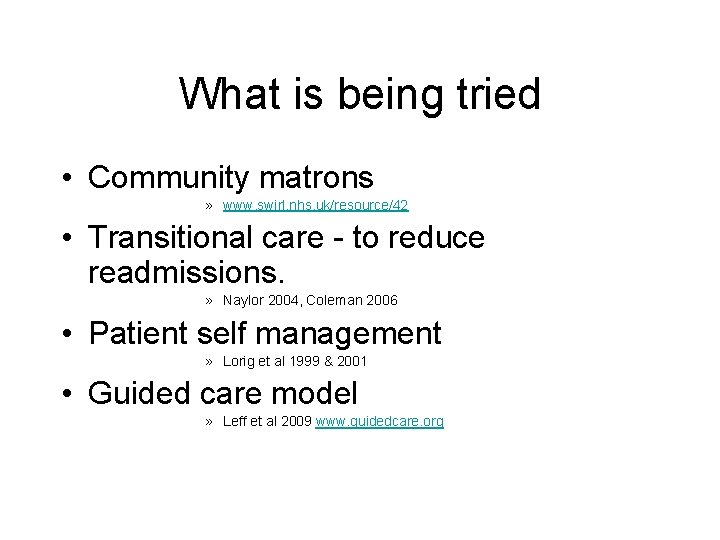
What is being tried • Community matrons » www. swirl. nhs. uk/resource/42 • Transitional care - to reduce readmissions. » Naylor 2004, Coleman 2006 • Patient self management » Lorig et al 1999 & 2001 • Guided care model » Leff et al 2009 www. guidedcare. org


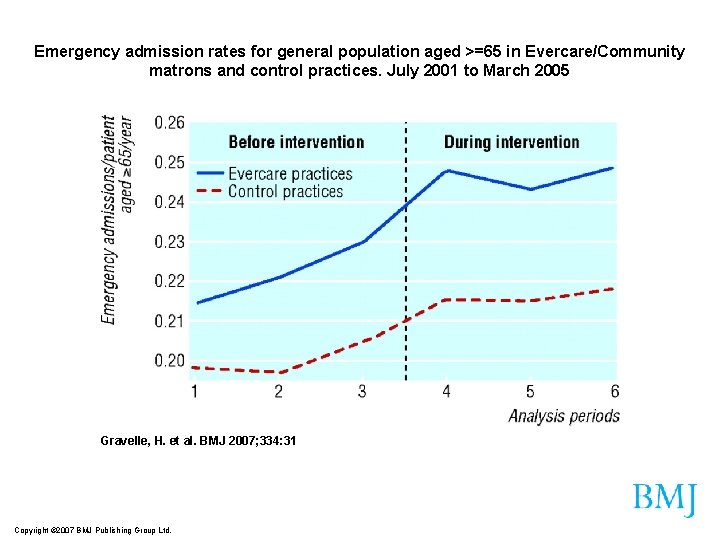
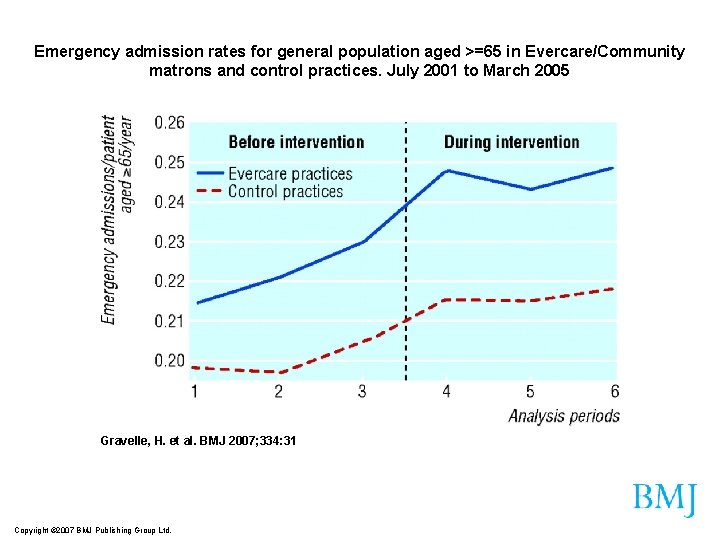
Emergency admission rates for general population aged >=65 in Evercare/Community matrons and control practices. July 2001 to March 2005 Gravelle, H. et al. BMJ 2007; 334: 31 Copyright © 2007 BMJ Publishing Group Ltd.
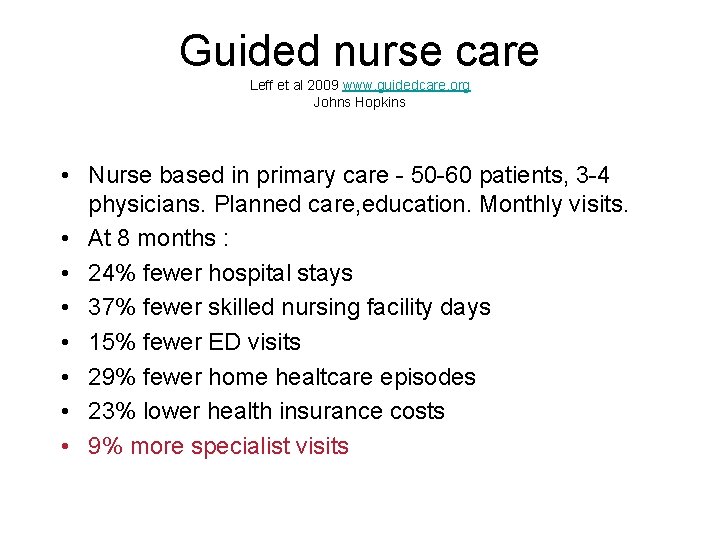
Guided nurse care Leff et al 2009 www. guidedcare. org Johns Hopkins • Nurse based in primary care - 50 -60 patients, 3 -4 physicians. Planned care, education. Monthly visits. • At 8 months : • 24% fewer hospital stays • 37% fewer skilled nursing facility days • 15% fewer ED visits • 29% fewer home healtcare episodes • 23% lower health insurance costs • 9% more specialist visits


Sneak peek Reduce admissions
Implications for health system • Common in younger patients • Big workload for practices – More illnesses more work – Care is GP centred • Polypharmacy – More illnesses more work • Socioeconomic effects • We don’t know impact on function

Categorisation of chronic illness Glauberman 2002, Martin 2005 • Simple problems : Hypertension – Protocol driven • Complicated : Open heart surgery : Angina + alcohol+DM + family problems – Need specialised expertise • Complex – Additionally need knowledge of locality, social networks • Chaotic : – Brittle clinical & social problems Angina + DM + alc binging + disadvantage
What we know - Donald Rumsfelt 2008 • Known knowns : • Hospital budgets will be smaller. Bigger role for nurses • Known unknowns : • Role of nurses, OTs, pharmacists • Unknown unknowns: • Redeployment of budgets & staff from acute care to chronic care
Policy questions • Money is not the place to start - yet – Consider transfer of resources? • Patient responsibility & accessible information • Current GMS contract is not geared to chronic illness : should it be put out to tender? • Appropriate care directed by generalists & provided by nurses? • ‘Good enough’ care : ‘Boston vs Berlin’ • Diagnostics unhitched from hospitals including radiology
 Chronic granulomatous disease
Chronic granulomatous disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Jewish chronic disease hospital study pdf
Jewish chronic disease hospital study pdf Chronic kidney disease near atwater
Chronic kidney disease near atwater Cld vs dcld
Cld vs dcld Nih stroke scale
Nih stroke scale Peripheral stigmata of cld
Peripheral stigmata of cld Stigmata of chronic liver disease
Stigmata of chronic liver disease Kate lorig stanford
Kate lorig stanford Developedbyed
Developedbyed Chronic disease
Chronic disease Stages of cirrhosis of the liver
Stages of cirrhosis of the liver Chronic disease
Chronic disease Pictures of lungs with copd
Pictures of lungs with copd Chronic rheumatic heart disease
Chronic rheumatic heart disease Srdp angewandte mathematik
Srdp angewandte mathematik Lehrplan ahs oberstufe physik
Lehrplan ahs oberstufe physik Ahs contract
Ahs contract Ahs contractor
Ahs contractor åhs prev
åhs prev Eprep portal
Eprep portal Ahs tableau
Ahs tableau Ahs asb
Ahs asb