Chronic Daily Headaches Medication Overuse Headache Diagnosis and




- Slides: 55

Chronic Daily Headaches & Medication Overuse Headache Diagnosis and Management 4 th Biennial Hull-BASH Headache Meeting Jan 20 th 2011 Dr Brendan Davies North Midlands Regional Headache Clinic University Hospital of North Staffordshire
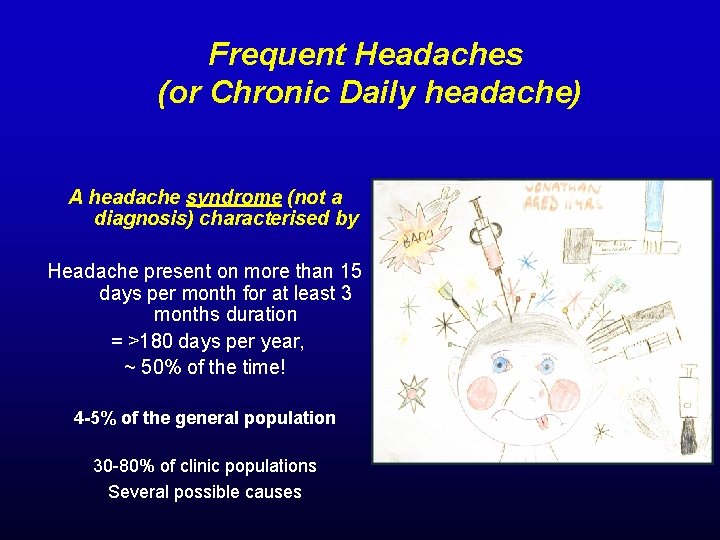
Frequent Headaches (or Chronic Daily headache) A headache syndrome (not a diagnosis) characterised by Headache present on more than 15 days per month for at least 3 months duration = >180 days per year, ~ 50% of the time! 4 -5% of the general population 30 -80% of clinic populations Several possible causes
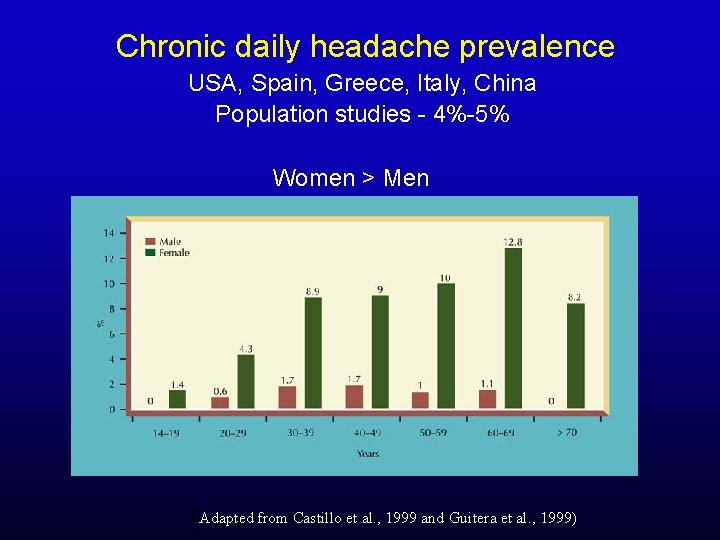
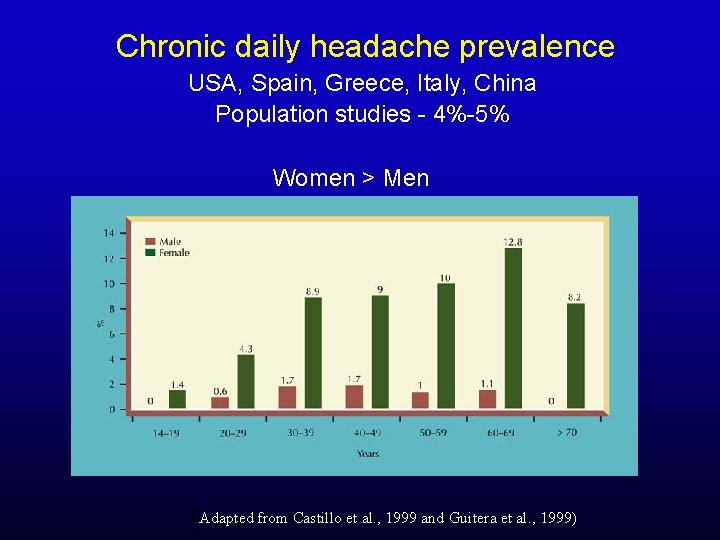
Chronic daily headache prevalence USA, Spain, Greece, Italy, China Population studies - 4%-5% Women > Men (Adapted from Castillo et al. , 1999 and Guitera et al. , 1999)
Recognition of the Problem is the first step !!
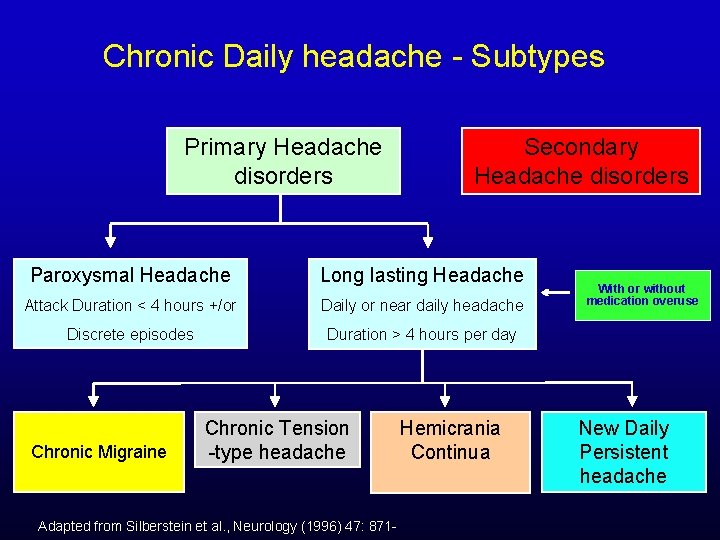
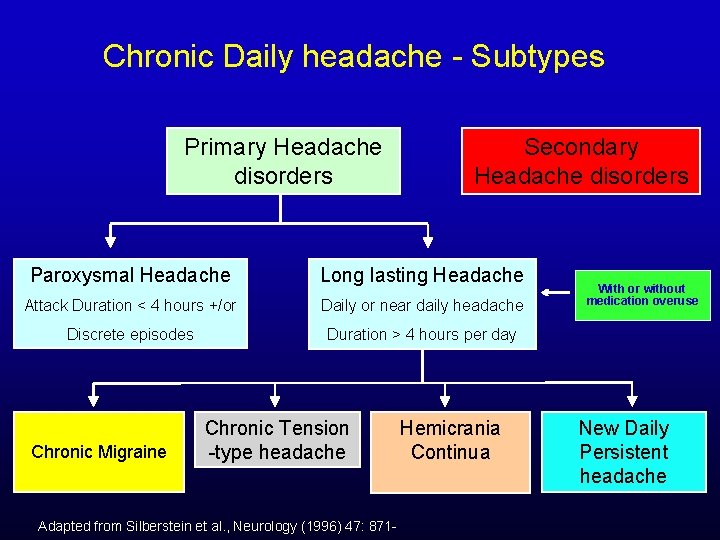
Chronic Daily headache - Subtypes Primary Headache disorders Secondary Headache disorders Paroxysmal Headache Long lasting Headache Attack Duration < 4 hours +/or Daily or near daily headache Discrete episodes Duration > 4 hours per day Chronic Migraine Chronic Tension -type headache Adapted from Silberstein et al. , Neurology (1996) 47: 871 - Hemicrania Continua With or without medication overuse New Daily Persistent headache
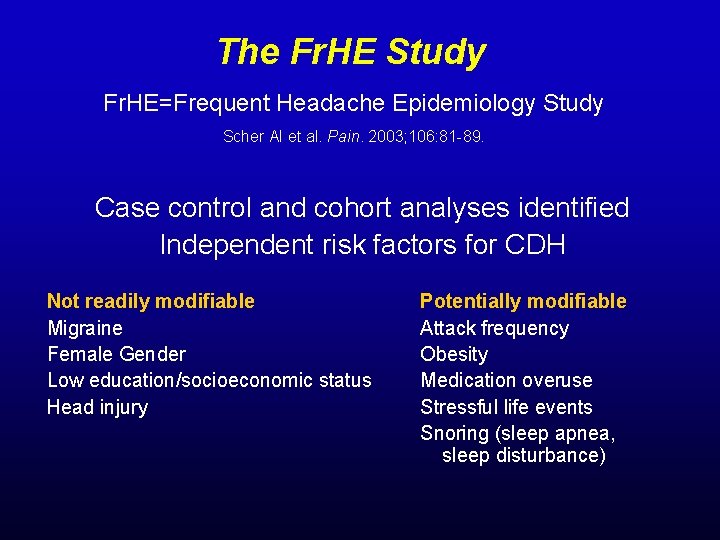
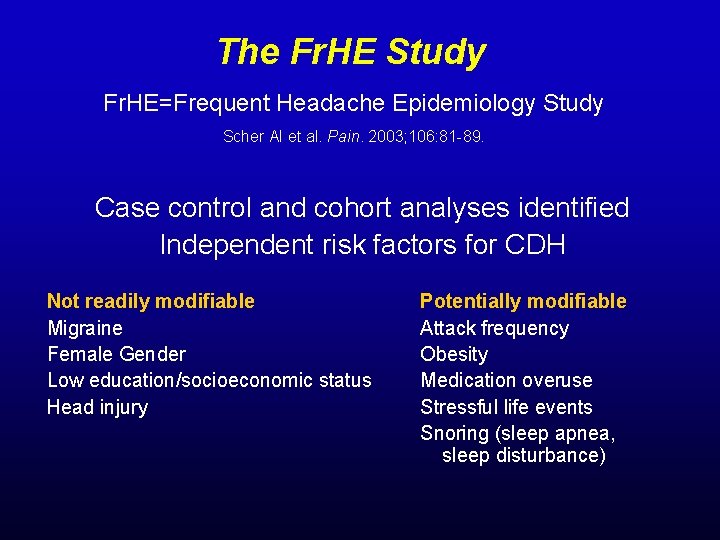
The Fr. HE Study Fr. HE=Frequent Headache Epidemiology Study Scher AI et al. Pain. 2003; 106: 81 -89. Case control and cohort analyses identified Independent risk factors for CDH Not readily modifiable Migraine Female Gender Low education/socioeconomic status Head injury Potentially modifiable Attack frequency Obesity Medication overuse Stressful life events Snoring (sleep apnea, sleep disturbance)
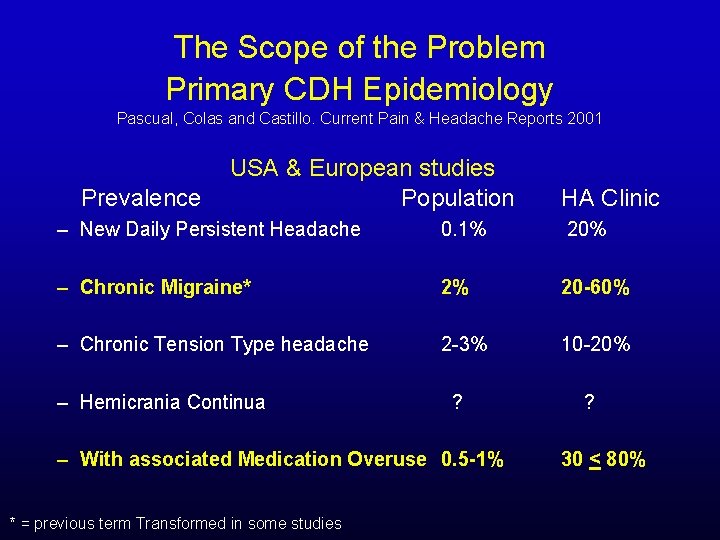
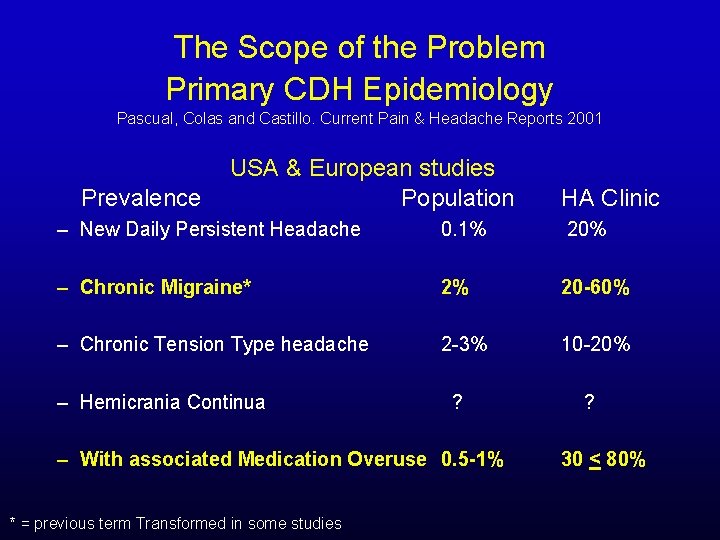
The Scope of the Problem Primary CDH Epidemiology Pascual, Colas and Castillo. Current Pain & Headache Reports 2001 Prevalence USA & European studies Population HA Clinic – New Daily Persistent Headache 0. 1% 20% – Chronic Migraine* 2% 20 -60% – Chronic Tension Type headache 2 -3% 10 -20% – Hemicrania Continua ? – With associated Medication Overuse 0. 5 -1% * = previous term Transformed in some studies ? 30 < 80%
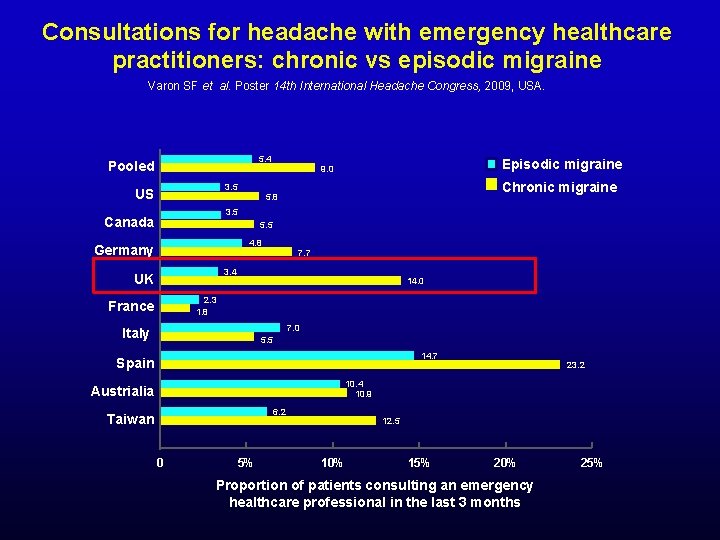
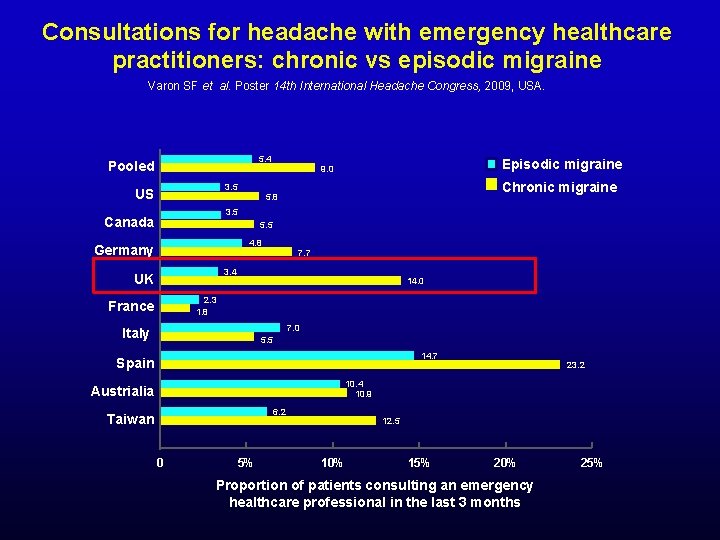
Consultations for headache with emergency healthcare practitioners: chronic vs episodic migraine Varon SF et al. Poster 14 th International Headache Congress, 2009, USA. 5. 4 Pooled 3. 5 US Episodic migraine 9. 0 Chronic migraine 5. 8 3. 5 Canada 5. 5 4. 8 Germany 7. 7 3. 4 UK 14. 0 2. 3 1. 8 France 7. 0 Italy 5. 5 14. 7 Spain 23. 2 10. 4 10. 9 Austrialia 6. 2 Taiwan 0 5% 12. 5 10% 15% 20% Proportion of patients consulting an emergency healthcare professional in the last 3 months 25%
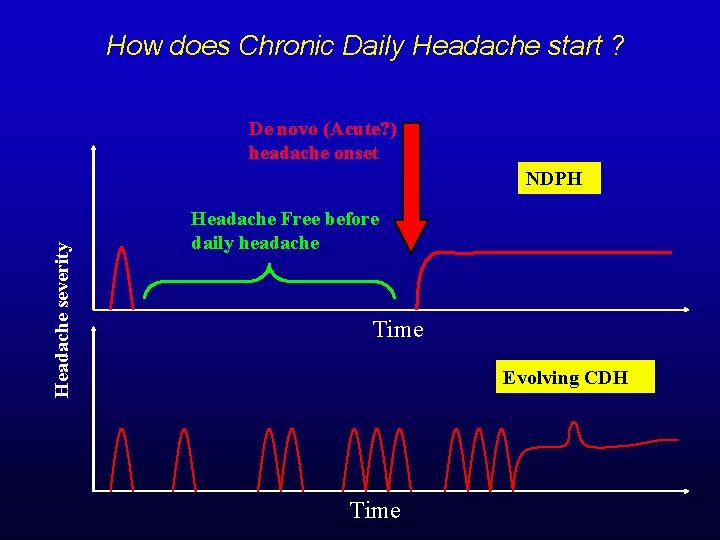
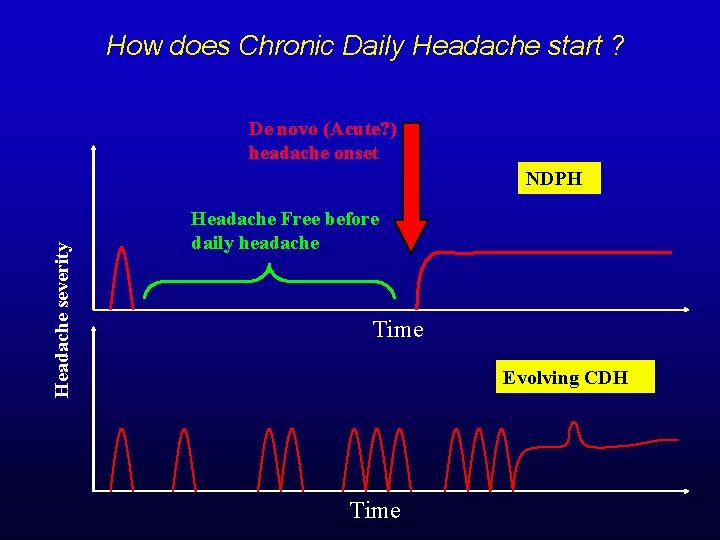
How does Chronic Daily Headache start ? De novo (Acute? ) headache onset Headache severity NDPH Headache Free before daily headache Time Evolving CDH Time
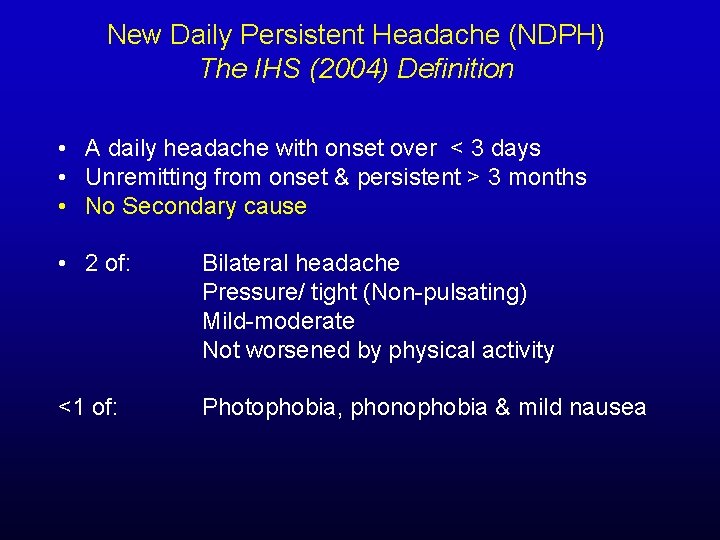
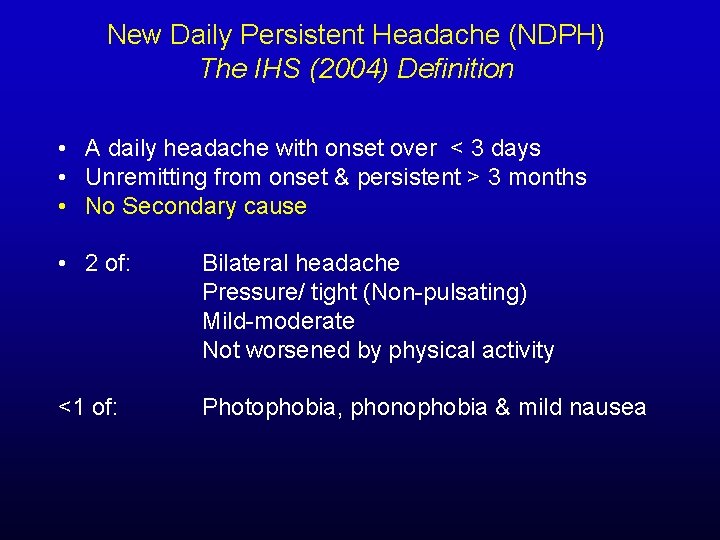
New Daily Persistent Headache (NDPH) The IHS (2004) Definition • A daily headache with onset over < 3 days • Unremitting from onset & persistent > 3 months • No Secondary cause • 2 of: Bilateral headache Pressure/ tight (Non-pulsating) Mild-moderate Not worsened by physical activity <1 of: Photophobia, phonophobia & mild nausea
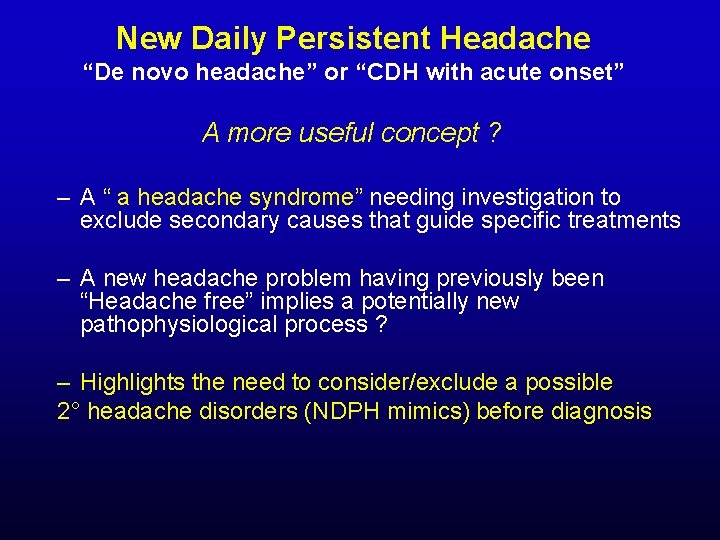
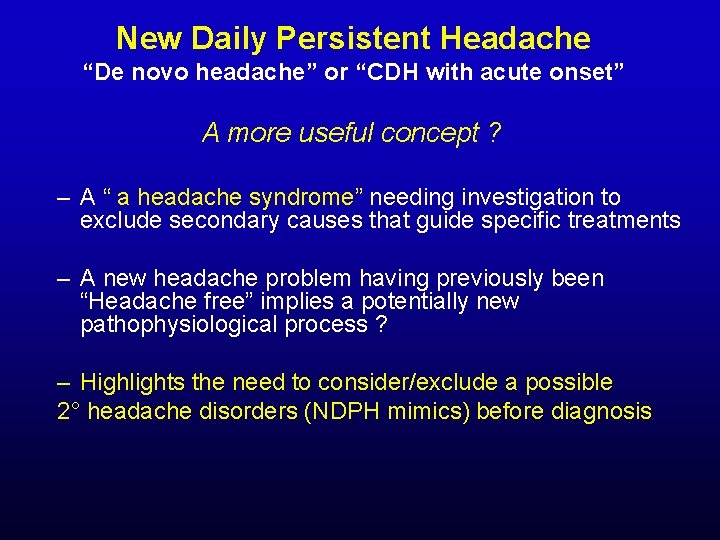
New Daily Persistent Headache “De novo headache” or “CDH with acute onset” A more useful concept ? – A “ a headache syndrome” needing investigation to exclude secondary causes that guide specific treatments – A new headache problem having previously been “Headache free” implies a potentially new pathophysiological process ? – Highlights the need to consider/exclude a possible 2° headache disorders (NDPH mimics) before diagnosis
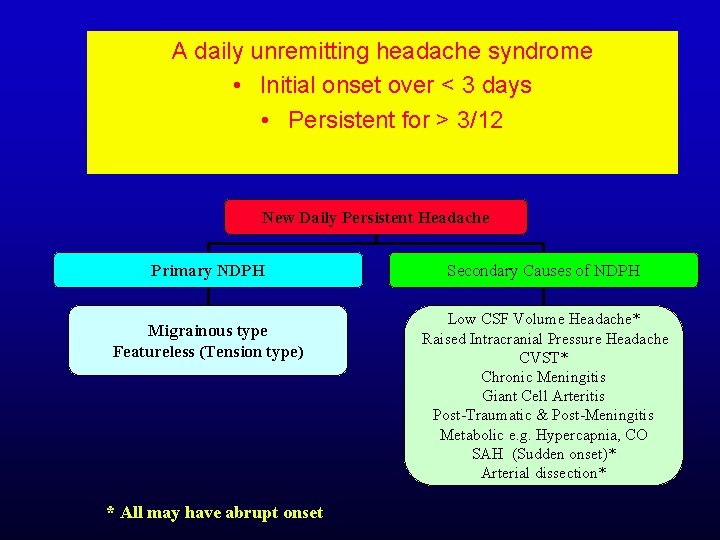
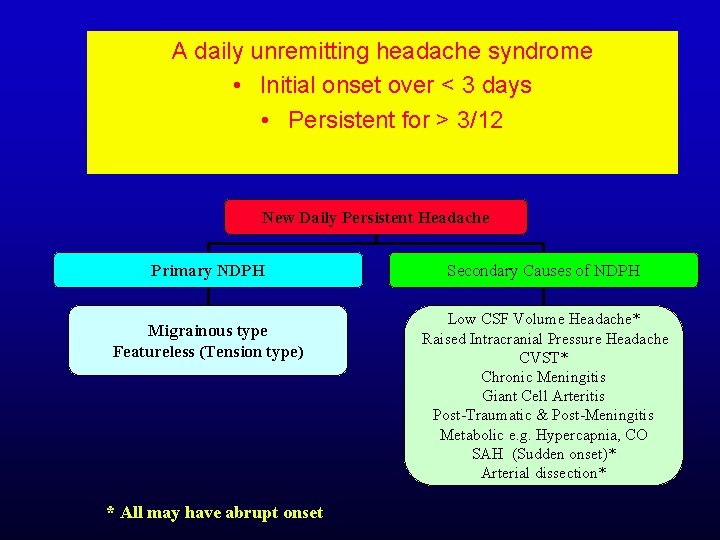
A daily unremitting headache syndrome • Initial onset over < 3 days • Persistent for > 3/12 New Daily Persistent Headache Primary NDPH Migrainous type Featureless (Tension type) * All may have abrupt onset Secondary Causes of NDPH Low CSF Volume Headache* Raised Intracranial Pressure Headache CVST* Chronic Meningitis Giant Cell Arteritis Post-Traumatic & Post-Meningitis Metabolic e. g. Hypercapnia, CO SAH (Sudden onset)* Arterial dissection*
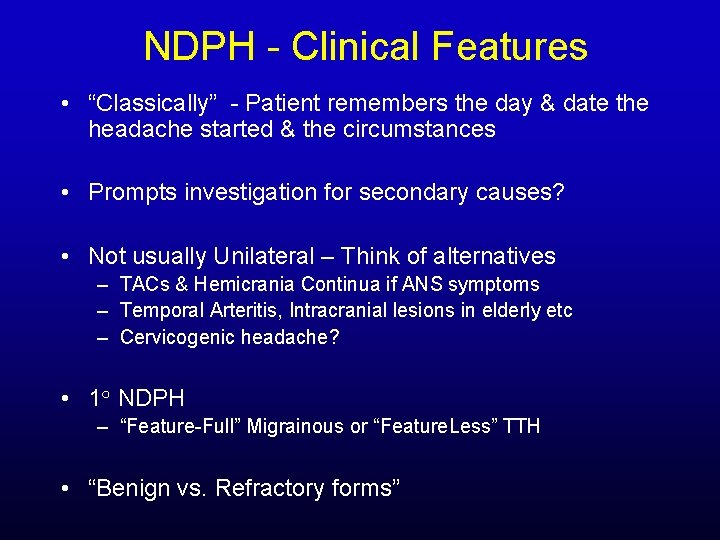
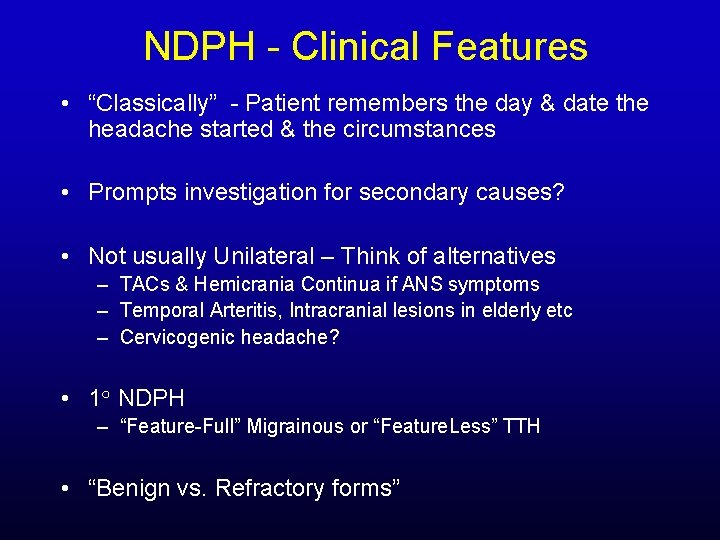
NDPH - Clinical Features • “Classically” - Patient remembers the day & date the headache started & the circumstances • Prompts investigation for secondary causes? • Not usually Unilateral – Think of alternatives – TACs & Hemicrania Continua if ANS symptoms – Temporal Arteritis, Intracranial lesions in elderly etc – Cervicogenic headache? • 1○ NDPH – “Feature-Full” Migrainous or “Feature. Less” TTH • “Benign vs. Refractory forms”

Diagnostic Studies in NDPH if Suspected Low CSF volume/pressure • Always ask about effect of posture & otological symptoms? • CT Brain Normal !! “Beware” Bilateral Subdurals? • CSF Pressure < 60 mm H 20 ? (but can be normal!) – Normal glucose but may - WCC, Protein, RBC • Gd-DTPA is investigation of choice – Diffuse linear Non-nodular Pachymeningeal enhancement – Tonsillar descent & Brain sagging – Bilateral subdural
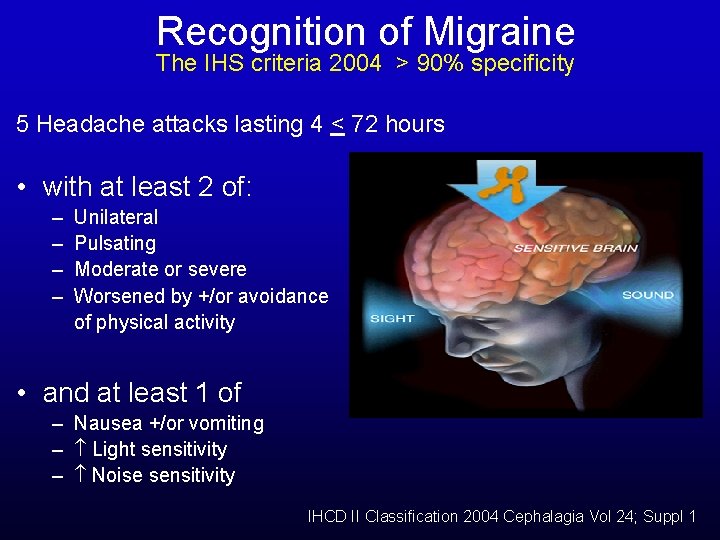
Recognition of Migraine The IHS criteria 2004 > 90% specificity 5 Headache attacks lasting 4 < 72 hours • with at least 2 of: – – Unilateral Pulsating Moderate or severe Worsened by +/or avoidance of physical activity • and at least 1 of – Nausea +/or vomiting – Light sensitivity – Noise sensitivity IHCD II Classification 2004 Cephalagia Vol 24; Suppl 1
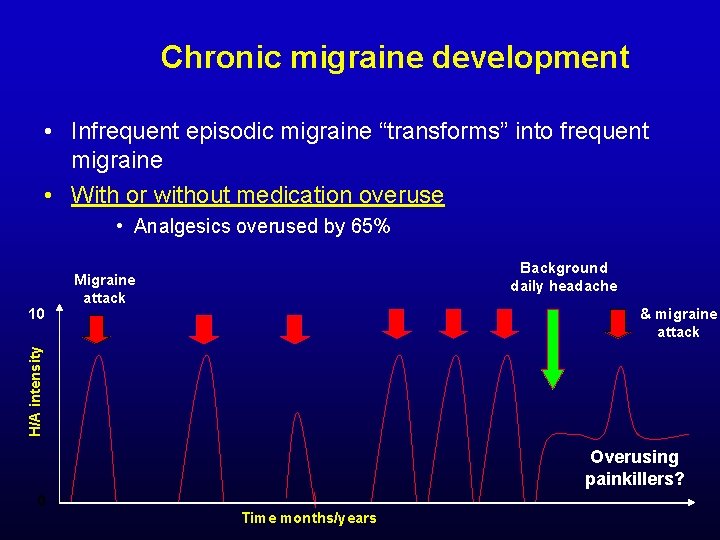
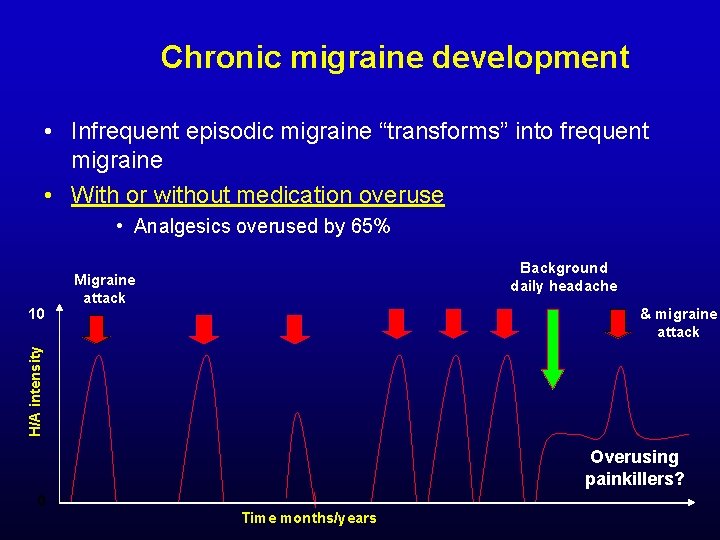
Chronic migraine development • Infrequent episodic migraine “transforms” into frequent migraine • With or without medication overuse • Analgesics overused by 65% & migraine attack H/A intensity 10 Background daily headache Migraine attack Overusing painkillers? 0 Time months/years
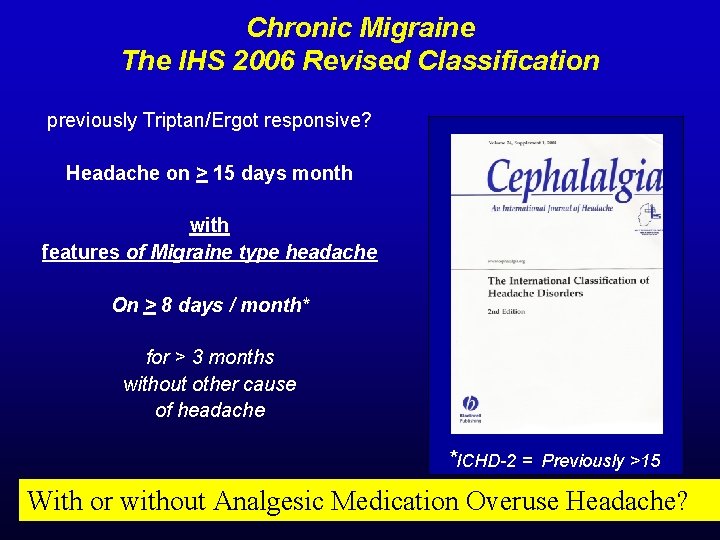
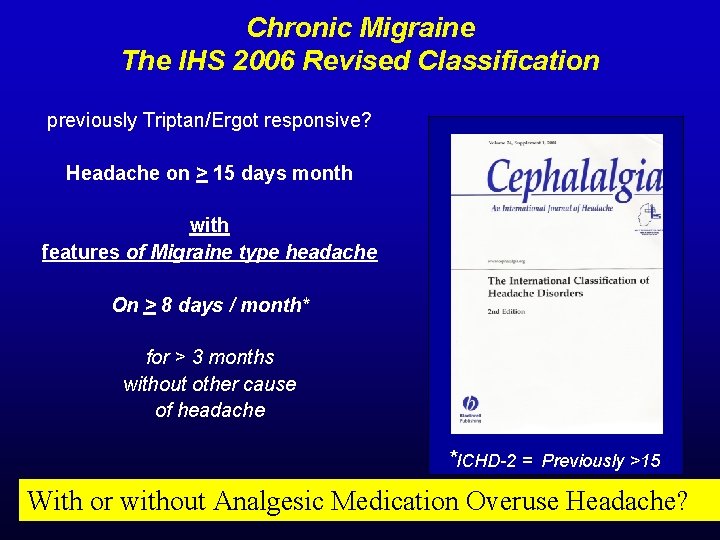
Chronic Migraine The IHS 2006 Revised Classification previously Triptan/Ergot responsive? Headache on > 15 days month with features of Migraine type headache On > 8 days / month* for > 3 months without other cause of headache *ICHD-2 = Previously >15 With or without Analgesic Medication Overuse Headache?
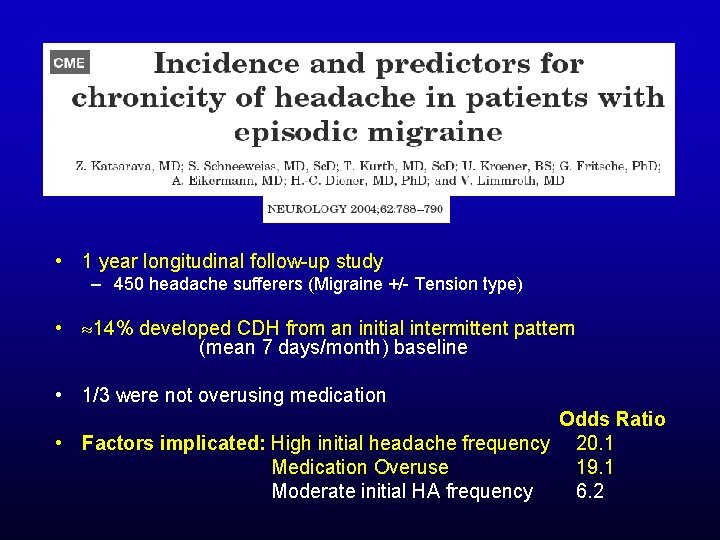
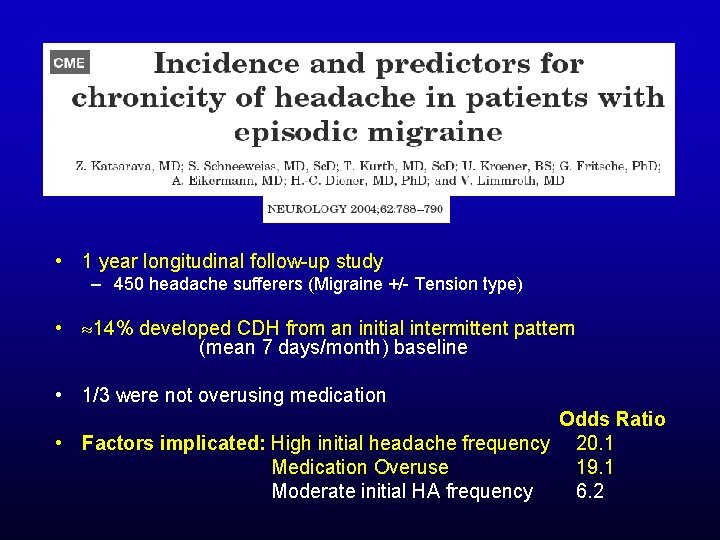
• 1 year longitudinal follow-up study – 450 headache sufferers (Migraine +/- Tension type) • 14% developed CDH from an initial intermittent pattern (mean 7 days/month) baseline • 1/3 were not overusing medication Odds Ratio • Factors implicated: High initial headache frequency 20. 1 Medication Overuse 19. 1 Moderate initial HA frequency 6. 2
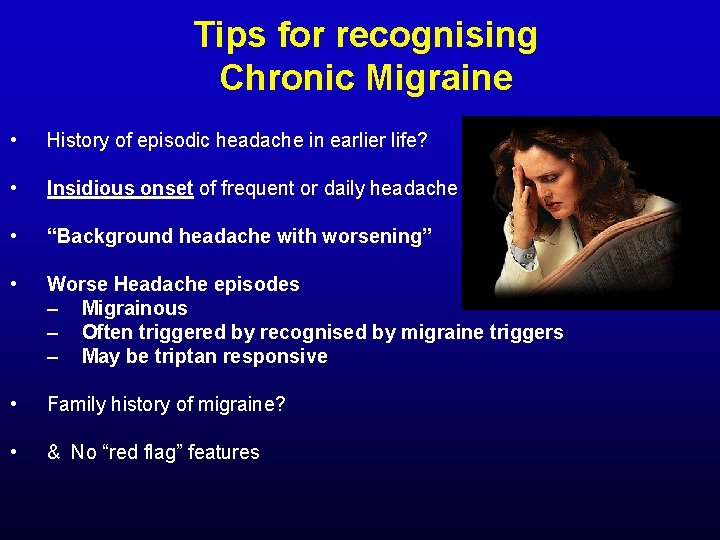
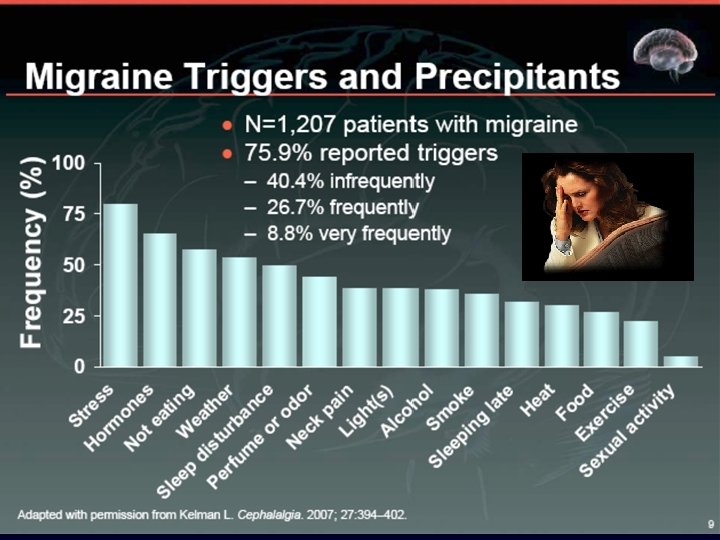
Tips for recognising Chronic Migraine • History of episodic headache in earlier life? • Insidious onset of frequent or daily headache • “Background headache with worsening” • Worse Headache episodes – Migrainous – Often triggered by recognised by migraine triggers – May be triptan responsive • Family history of migraine? • & No “red flag” features
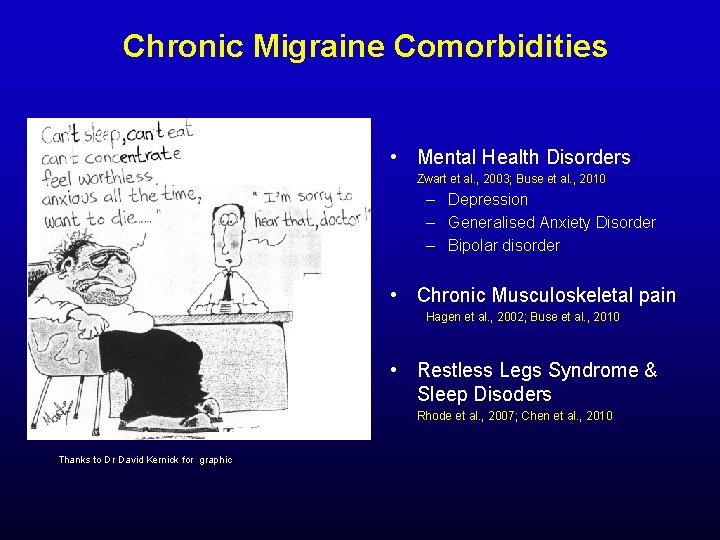
Chronic Migraine Comorbidities • Mental Health Disorders Zwart et al. , 2003; Buse et al. , 2010 – Depression – Generalised Anxiety Disorder – Bipolar disorder • Chronic Musculoskeletal pain Hagen et al. , 2002; Buse et al. , 2010 • Restless Legs Syndrome & Sleep Disoders Rhode et al. , 2007; Chen et al. , 2010 Thanks to Dr David Kernick for graphic
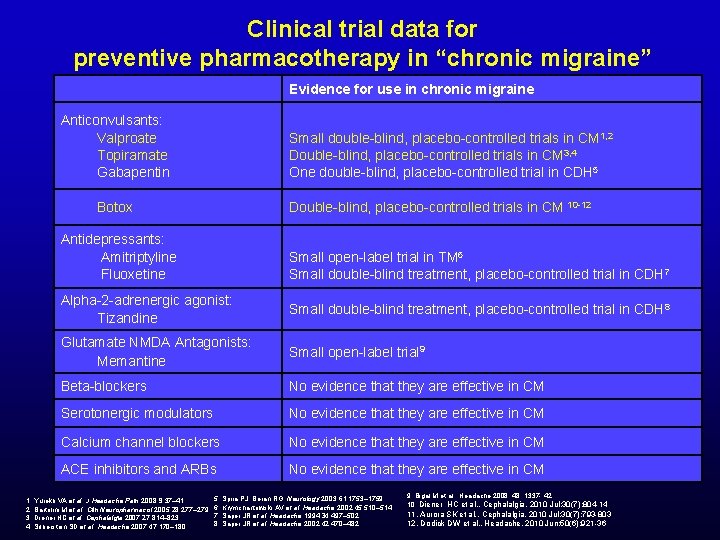
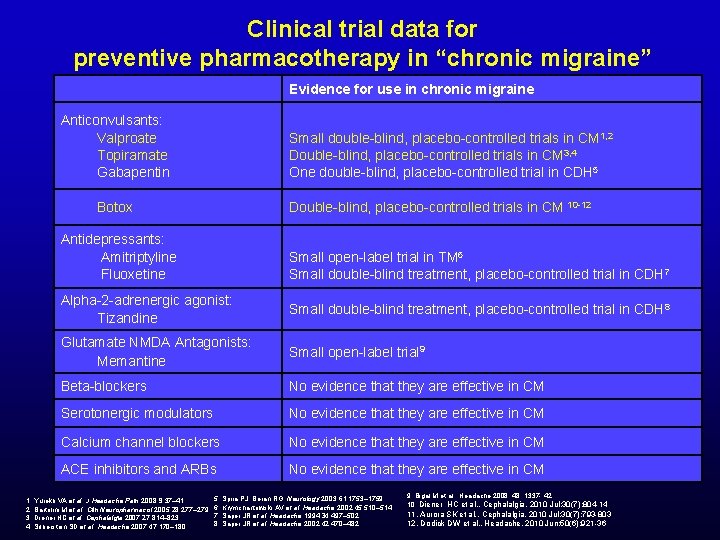
Clinical trial data for preventive pharmacotherapy in “chronic migraine” Evidence for use in chronic migraine Anticonvulsants: Valproate Topiramate Gabapentin Small double-blind, placebo-controlled trials in CM 1, 2 Double-blind, placebo-controlled trials in CM 3, 4 One double-blind, placebo-controlled trial in CDH 5 Botox Double-blind, placebo-controlled trials in CM 10 -12 Antidepressants: Amitriptyline Fluoxetine Small open-label trial in TM 6 Small double-blind treatment, placebo-controlled trial in CDH 7 Alpha-2 -adrenergic agonist: Tizandine Small double-blind treatment, placebo-controlled trial in CDH 8 Glutamate NMDA Antagonists: Memantine Small open-label trial 9 Beta-blockers No evidence that they are effective in CM Serotonergic modulators No evidence that they are effective in CM Calcium channel blockers No evidence that they are effective in CM ACE inhibitors and ARBs No evidence that they are effective in CM 1. Yurekli VA et al. J Headache Pain 2008; 9: 37– 41. 2. Bartolini M et al. Clin Neuropharmacol 2005; 28: 277– 279. 3. Diener HC et al. Cephalalgia 2007; 27: 814– 823. 4. Silberstein SD et al. Headache 2007; 47: 170– 180. 5. Spira PJ, Beran RG. Neurology 2003; 61: 1753– 1759. 6. Krymchantowski AV et al. Headache 2002; 45: 510– 514. 7. Saper JR et al. Headache 1994; 34: 497– 502. 8. Saper JR et al. Headache 2002; 42: 470– 482. 9. Bigal M et al. , Headache 2008; 48; 1337 - 42 10. Diener HC et al. , Cephalalgia. 2010 Jul; 30(7): 804 -14 11. Aurora SK et al. , Cephalalgia. 2010 Jul; 30(7): 793 -803 12. Dodick DW et al. , Headache. 2010 Jun; 50(6): 921 -36
Analgesic Medication Use 1 -3 % of the population take analgesics on a regular basis 7% take analgesics at least 1 x/wk
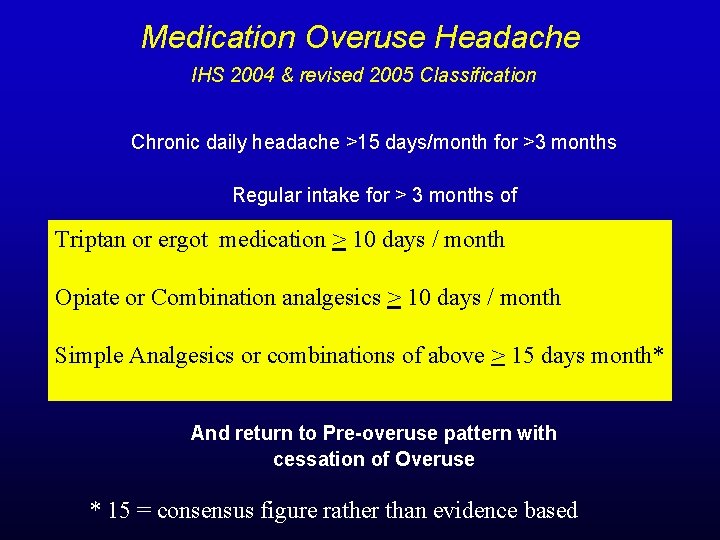
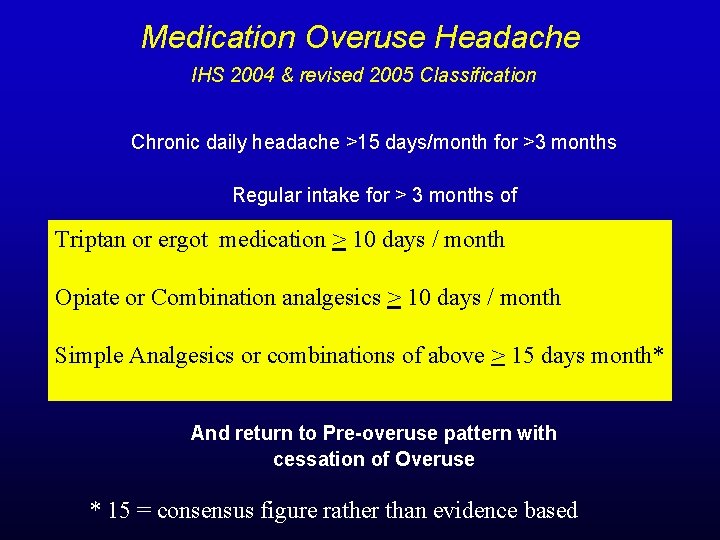
Medication Overuse Headache IHS 2004 & revised 2005 Classification Chronic daily headache >15 days/month for >3 months Regular intake for > 3 months of Triptan or ergot medication > 10 days / month Opiate or Combination analgesics > 10 days / month Simple Analgesics or combinations of above > 15 days month* And return to Pre-overuse pattern with cessation of Overuse * 15 = consensus figure rather than evidence based
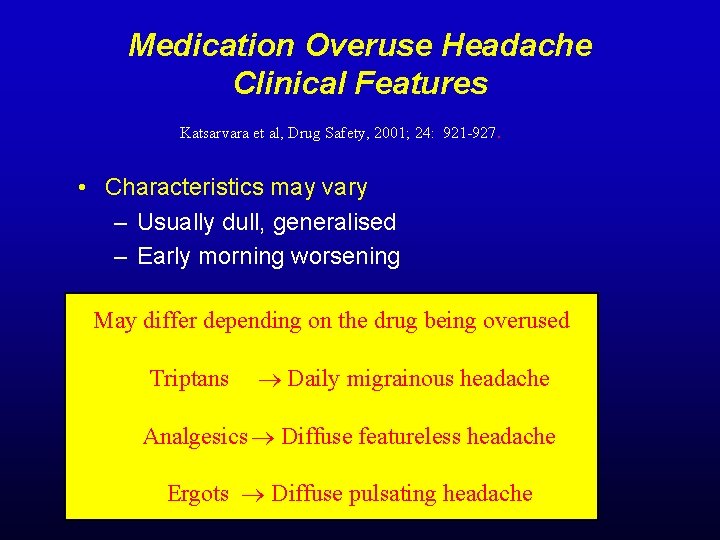
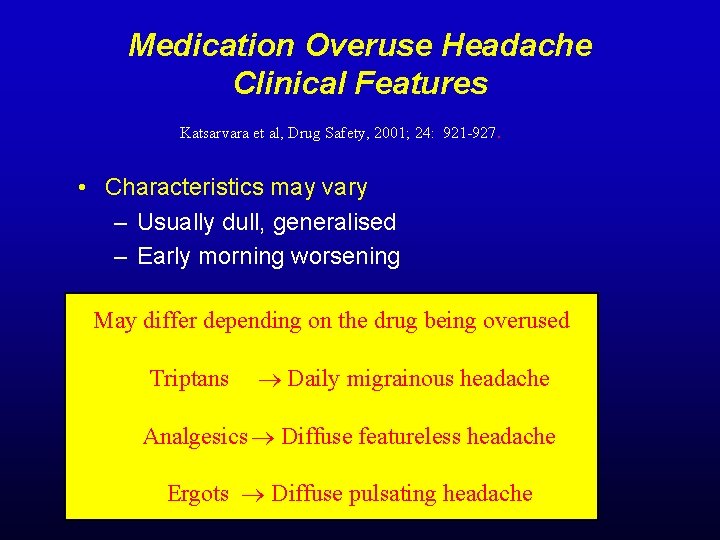
Medication Overuse Headache Clinical Features Katsarvara et al, Drug Safety, 2001; 24: 921 -927. • Characteristics may vary – Usually dull, generalised – Early morning worsening May differ depending on the drug being overused Triptans Daily migrainous headache Analgesics Diffuse featureless headache Ergots Diffuse pulsating headache
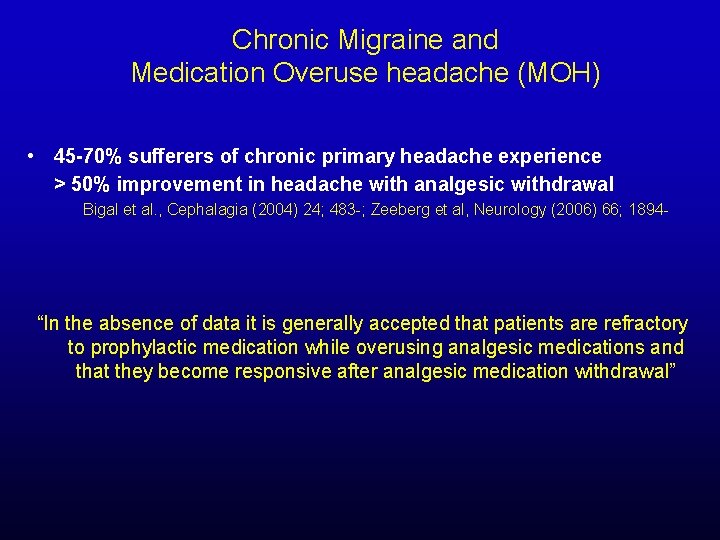
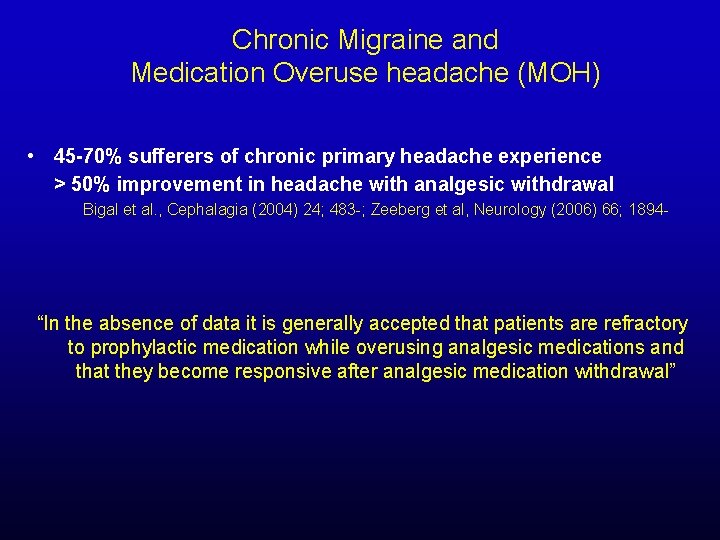
Chronic Migraine and Medication Overuse headache (MOH) • 45 -70% sufferers of chronic primary headache experience > 50% improvement in headache with analgesic withdrawal Bigal et al. , Cephalagia (2004) 24; 483 -; Zeeberg et al, Neurology (2006) 66; 1894 - “In the absence of data it is generally accepted that patients are refractory to prophylactic medication while overusing analgesic medications and that they become responsive after analgesic medication withdrawal”
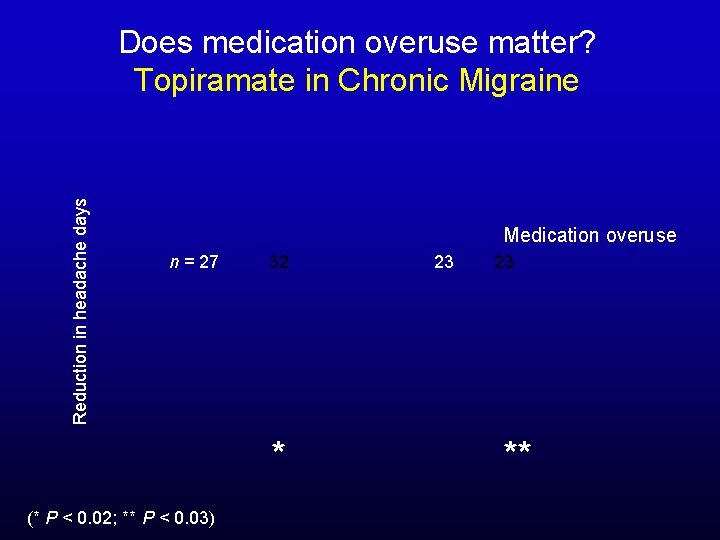
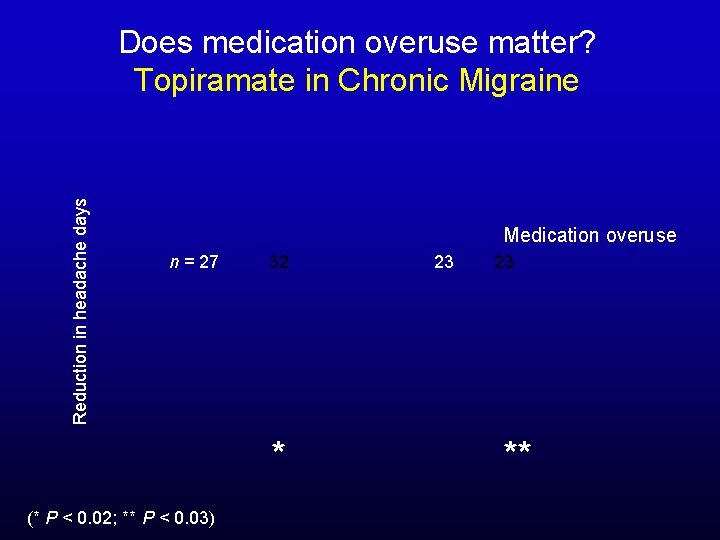
Reduction in headache days Does medication overuse matter? Topiramate in Chronic Migraine Medication overuse n = 27 32 * (* P < 0. 02; ** P < 0. 03) 23 23 **
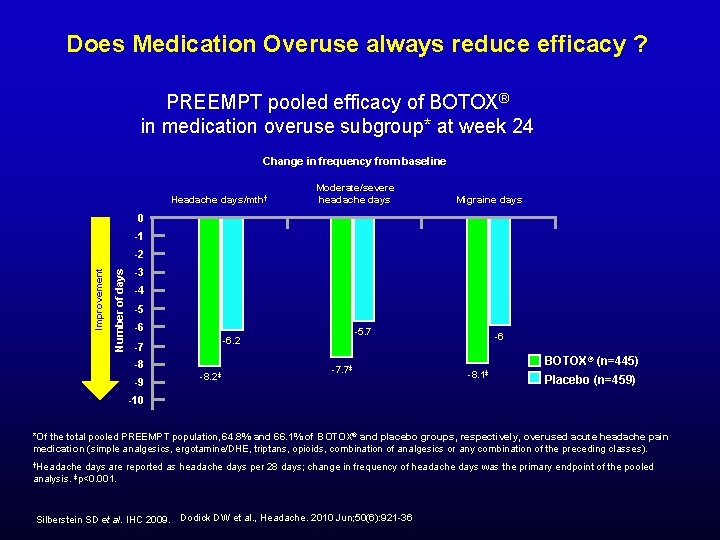
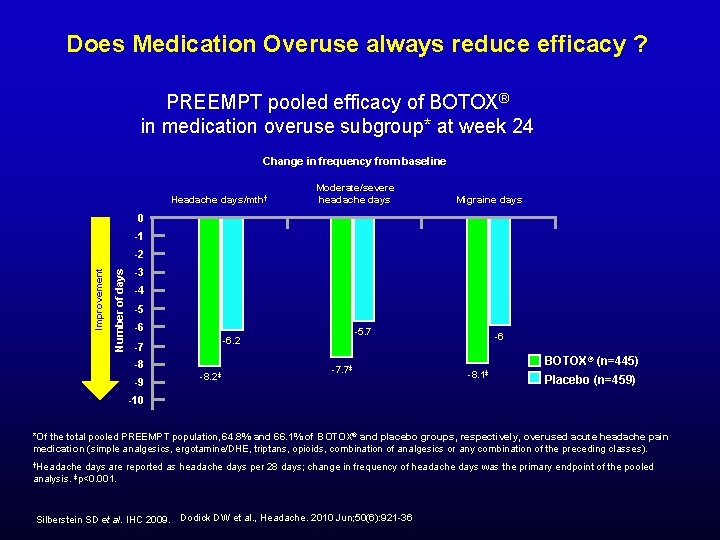
Does Medication Overuse always reduce efficacy ? PREEMPT pooled efficacy of BOTOX® in medication overuse subgroup* at week 24 Change in frequency from baseline Headache days/mth† Moderate/severe headache days Migraine days 0 -1 Number of days Improvement -2 -3 -4 -5 -6 -7 -8 -9 -5. 7 -6. 2 -8. 2‡ -7. 7‡ -6 BOTOX® (n=445) -8. 1‡ Placebo (n=459) -10 *Of the total pooled PREEMPT population, 64. 8% and 66. 1% of BOTOX® and placebo groups, respectively, overused acute headache pain medication (simple analgesics, ergotamine/DHE, triptans, opioids, combination of analgesics or any combination of the preceding classes). †Headache days are reported as headache days per 28 days; change in frequency of headache days was the primary endpoint of the pooled analysis. ‡p<0. 001. Silberstein SD et al. IHC 2009. Dodick DW et al. , Headache. 2010 Jun; 50(6): 921 -36
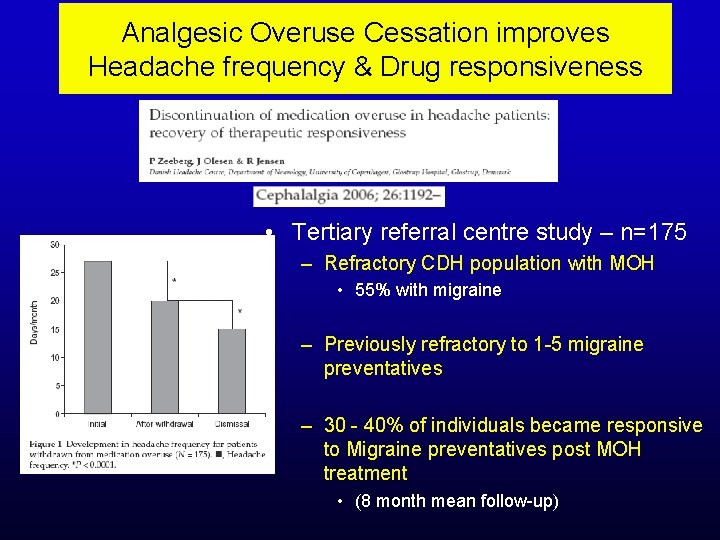
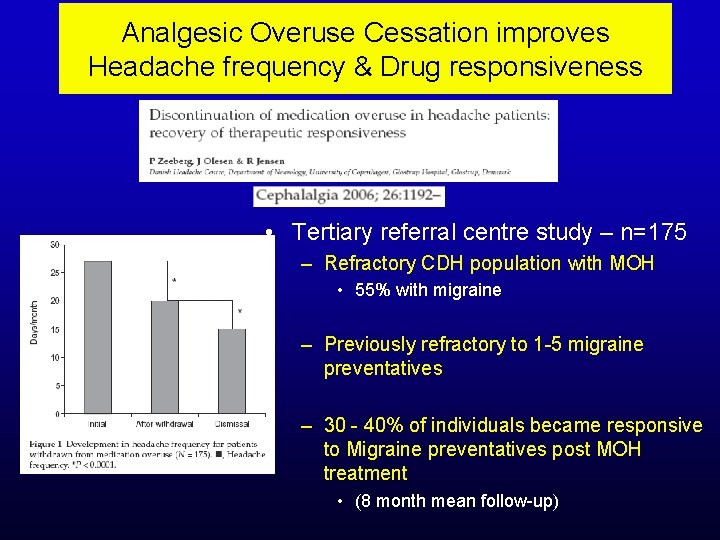
Analgesic Overuse Cessation improves Headache frequency & Drug responsiveness • Tertiary referral centre study – n=175 – Refractory CDH population with MOH • 55% with migraine – Previously refractory to 1 -5 migraine preventatives – 30 - 40% of individuals became responsive to Migraine preventatives post MOH treatment • (8 month mean follow-up)
Chronic Migraine & Medication Overuse Headache “Management controversies? ” What is the most effective strategy for initial MOH management?
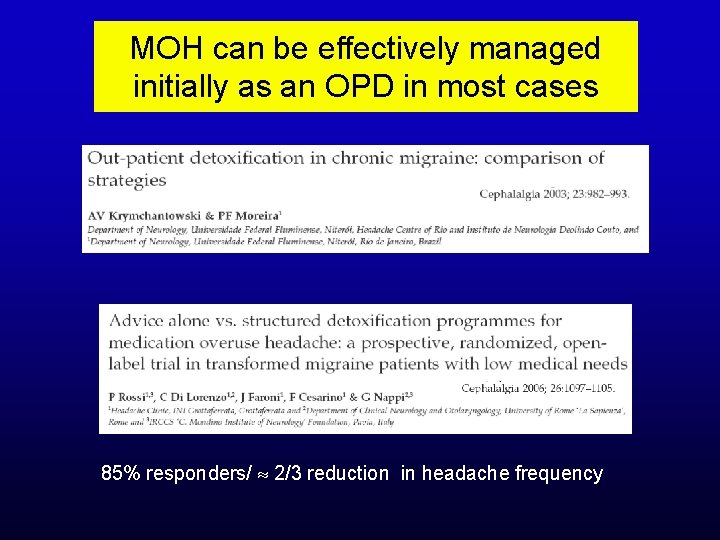
MOH can be effectively managed initially as an OPD in most cases 85% responders/ 2/3 reduction in headache frequency
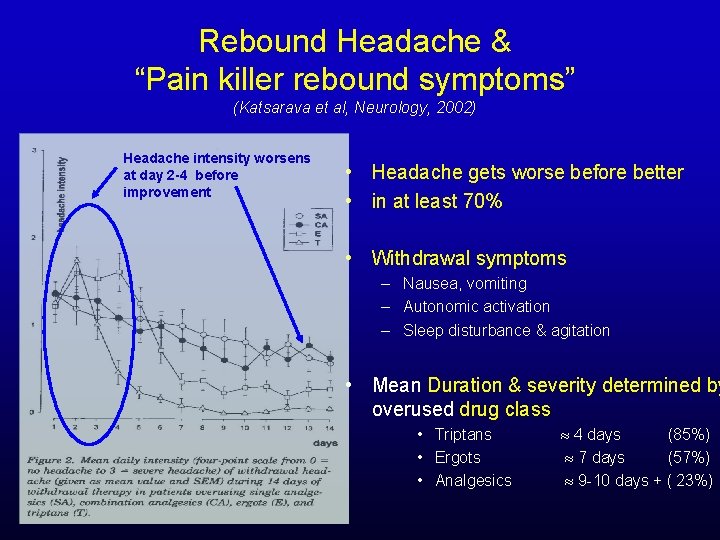
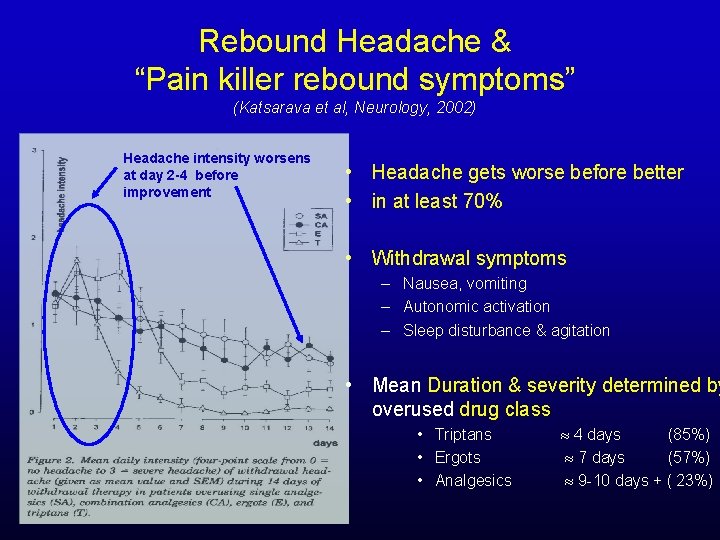
Rebound Headache & “Pain killer rebound symptoms” (Katsarava et al, Neurology, 2002) Headache intensity worsens at day 2 -4 before improvement • Headache gets worse before better • in at least 70% • Withdrawal symptoms – Nausea, vomiting – Autonomic activation – Sleep disturbance & agitation • Mean Duration & severity determined by overused drug class • Triptans • Ergots • Analgesics 4 days (85%) 7 days (57%) 9 -10 days + ( 23%)
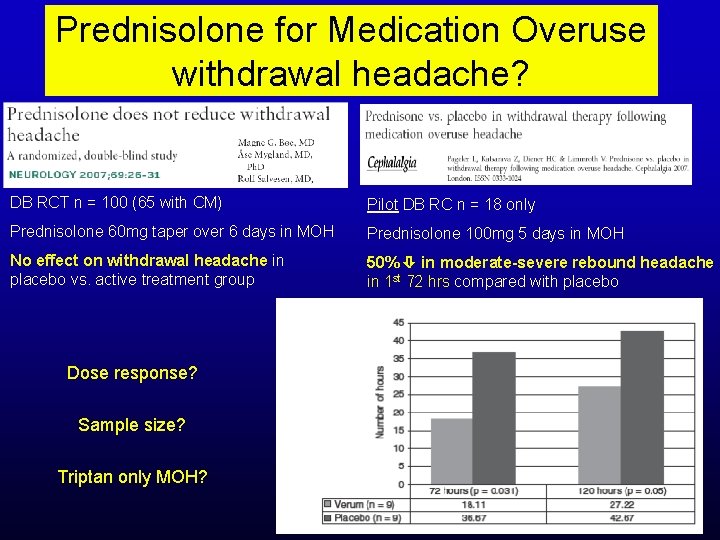
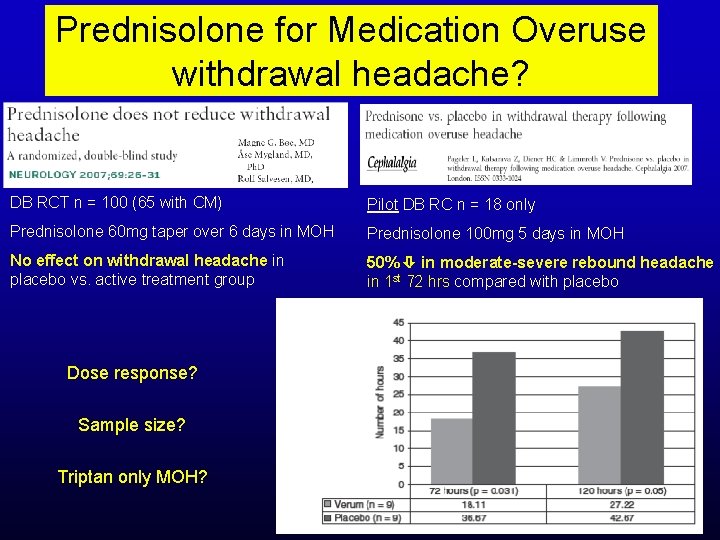
Prednisolone for Medication Overuse withdrawal headache? DB RCT n = 100 (65 with CM) Pilot DB RC n = 18 only Prednisolone 60 mg taper over 6 days in MOH Prednisolone 100 mg 5 days in MOH No effect on withdrawal headache in placebo vs. active treatment group 50% in moderate-severe rebound headache in 1 st 72 hrs compared with placebo Dose response? Sample size? Triptan only MOH?
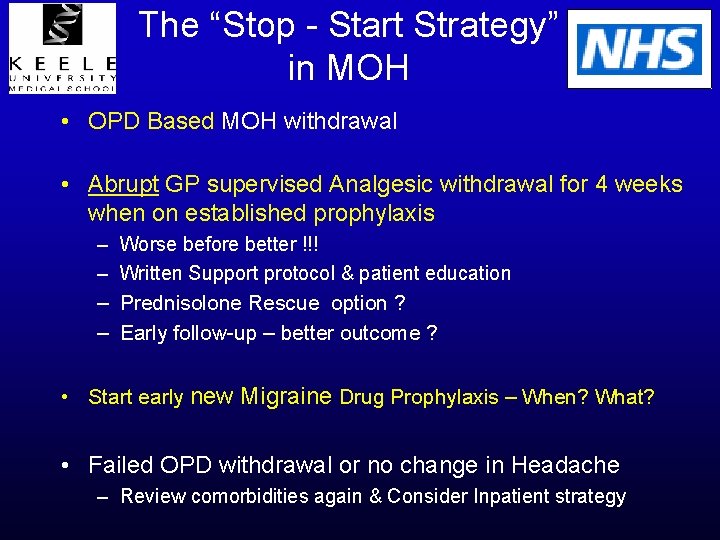
The “Stop - Start Strategy” in MOH • OPD Based MOH withdrawal • Abrupt GP supervised Analgesic withdrawal for 4 weeks when on established prophylaxis – – Worse before better !!! Written Support protocol & patient education Prednisolone Rescue option ? Early follow-up – better outcome ? • Start early new Migraine Drug Prophylaxis – When? What? • Failed OPD withdrawal or no change in Headache – Review comorbidities again & Consider Inpatient strategy
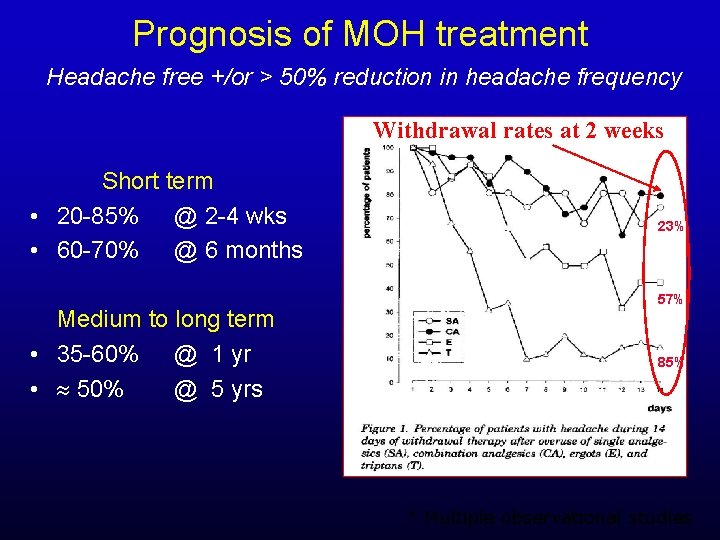
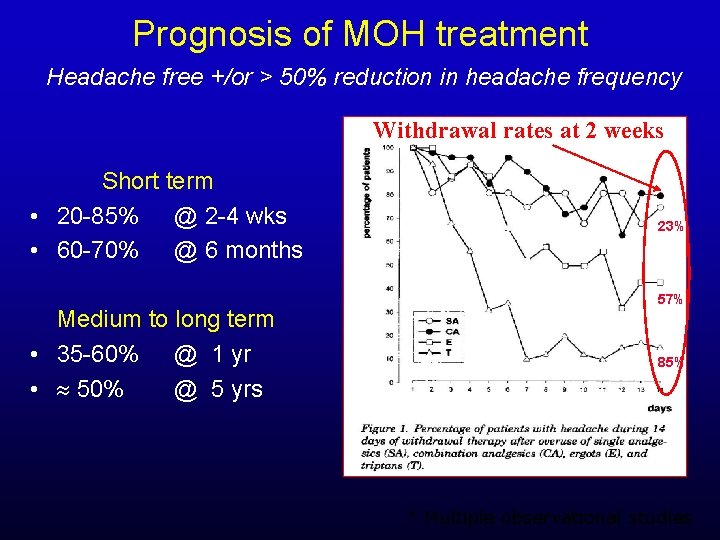
Prognosis of MOH treatment Headache free +/or > 50% reduction in headache frequency Withdrawal rates at 2 weeks Short term • 20 -85% @ 2 -4 wks • 60 -70% @ 6 months Medium to long term • 35 -60% @ 1 yr • 50% @ 5 yrs 23% 57% 85% * Multiple observational studies
Medication Overuse Headache If 6 -8 weeks after acute analgesic medication withdrawal there is no improvement The initial diagnosis of Medication Overuse Headache is not tenable Review the Initial Diagnosis !
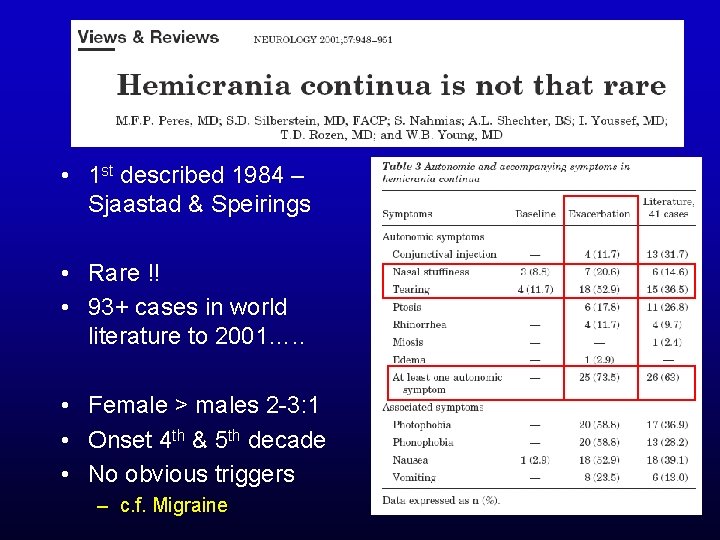
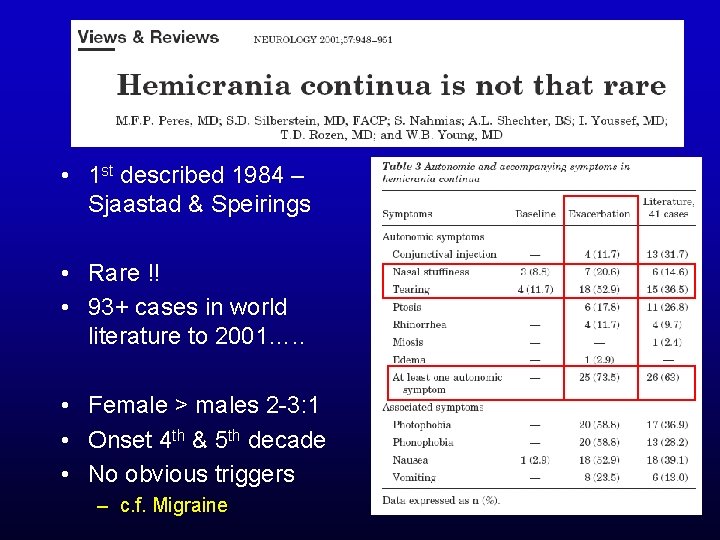
• 1 st described 1984 – Sjaastad & Speirings • Rare !! • 93+ cases in world literature to 2001…. . • Female > males 2 -3: 1 • Onset 4 th & 5 th decade • No obvious triggers – c. f. Migraine

Hemicrania Continua “Women with constant Hemicrania tearing & nasal congestion” • (Daily) mild-moderate Strictly side-locked unilateral pain • Mild-moderate background intensity with exacerbations • Exacerbations associated with – Ipsilateral autonomic symptoms in up to ¾ patients – Minimal or Absent autonomic symptoms in up to 1/3 – Photophobia, phonophobia & nausea in ~1/2 • Absolute headache response to Indometacin treatment – Mean oral dosage <150 mg / day (ensure tried up to 225 mg) +/- “ blinded Indotest” Rare cause but very treatable cause of CDH/NDPH Consider Indometacin trial in all with new onset side locked especially refractory hemicrania
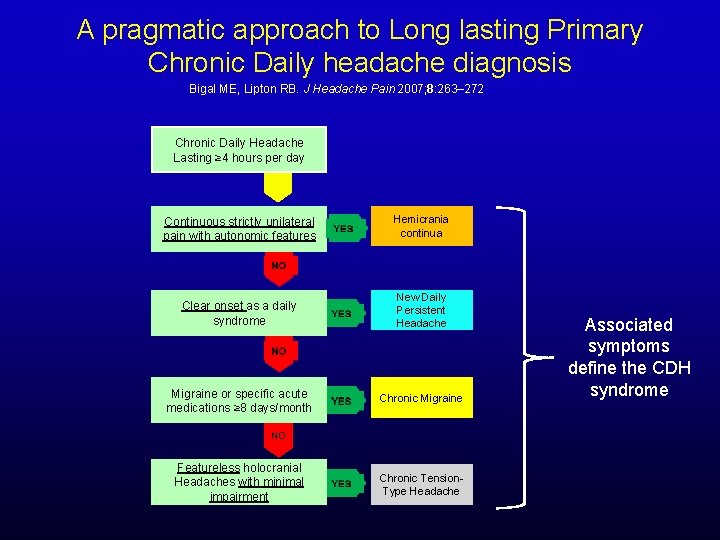
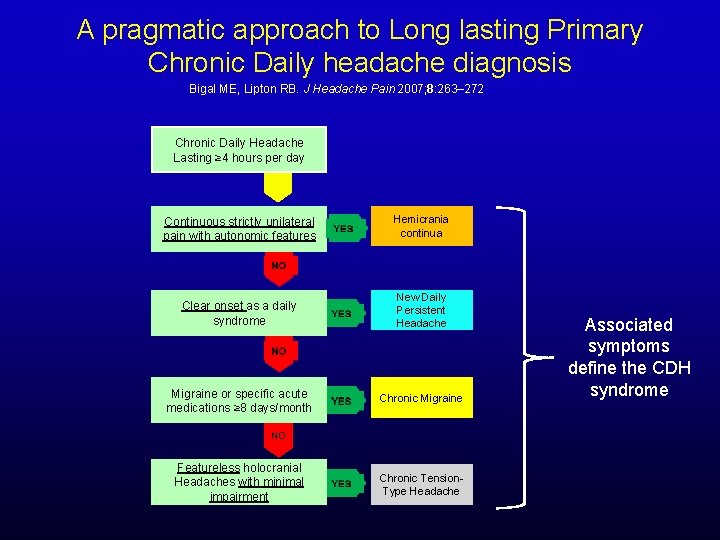
A pragmatic approach to Long lasting Primary Chronic Daily headache diagnosis Bigal ME, Lipton RB. J Headache Pain 2007; 8: 263– 272. Chronic Daily Headache Lasting ≥ 4 hours per day Continuous strictly unilateral pain with autonomic features Hemicrania continua Clear onset as a daily syndrome New Daily Persistent Headache Migraine or specific acute medications ≥ 8 days/month Chronic Migraine NO Featureless holocranial Headaches with minimal impairment Chronic Tension. Type Headache Associated symptoms define the CDH syndrome
Need to know more about best practice in Headache management Join BASH !! & Go & buy this book !!!
• Chronic Daily Headache is a symptom & not a diagnosis Questions? • Accurate diagnosis determines both treatment choice & prognosis • Medication Overuse is ubiquitous and must always be considered. . . • And more importantly properly addressed !!
BACKUP SLIDES
Chronic Refractory Migraine What do I do? & possible “Horizon” therapies?
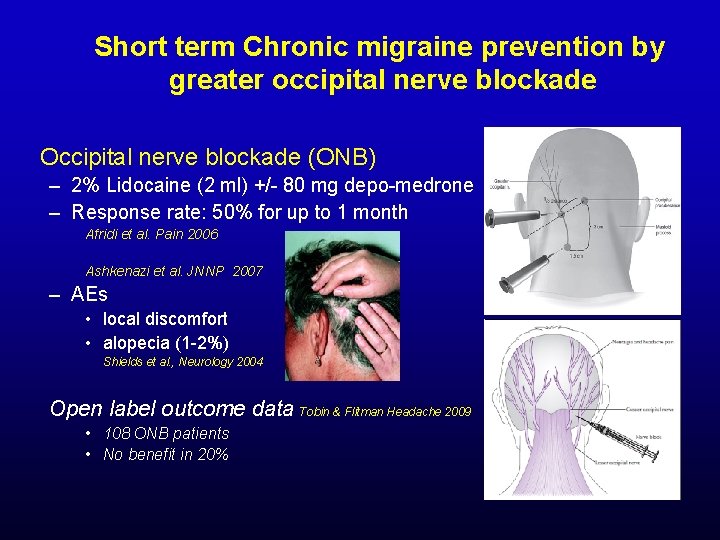
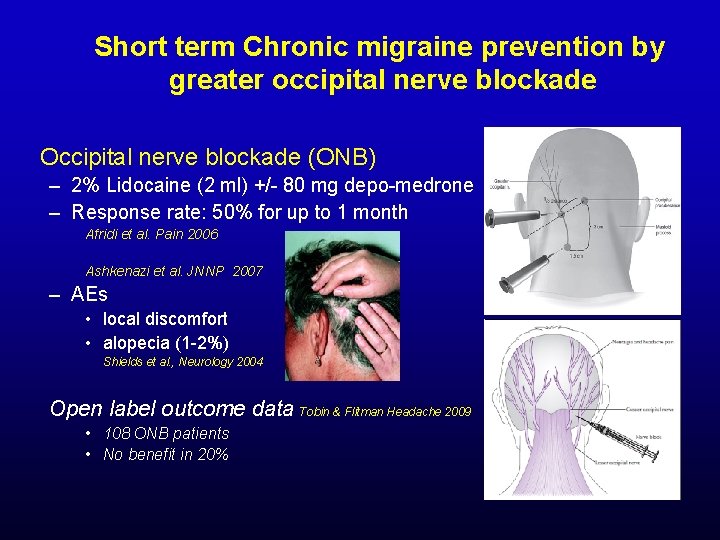
Short term Chronic migraine prevention by greater occipital nerve blockade Occipital nerve blockade (ONB) – 2% Lidocaine (2 ml) +/- 80 mg depo-medrone – Response rate: 50% for up to 1 month Afridi et al. Pain 2006 Ashkenazi et al. JNNP 2007 – AEs • local discomfort • alopecia (1 -2%) Shields et al. , Neurology 2004 Open label outcome data Tobin & Flitman Headache 2009 • 108 ONB patients • No benefit in 20%
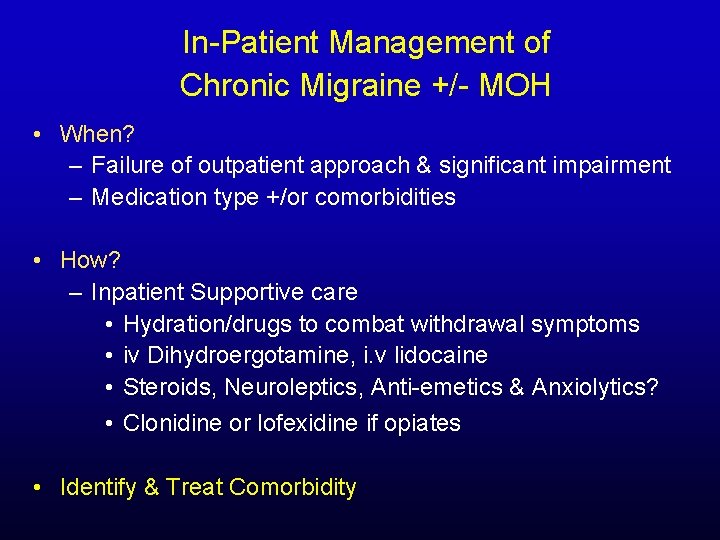
In-Patient Management of Chronic Migraine +/- MOH • When? – Failure of outpatient approach & significant impairment – Medication type +/or comorbidities • How? – Inpatient Supportive care • Hydration/drugs to combat withdrawal symptoms • iv Dihydroergotamine, i. v lidocaine • Steroids, Neuroleptics, Anti-emetics & Anxiolytics? • Clonidine or lofexidine if opiates • Identify & Treat Comorbidity
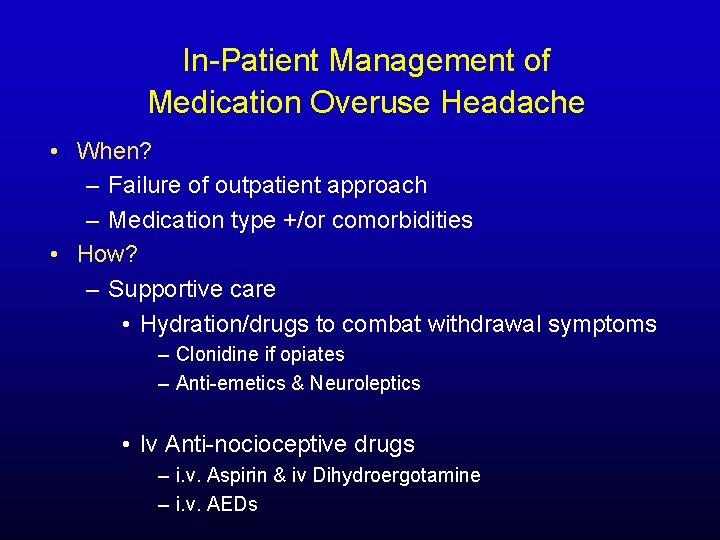
In-Patient Management of Medication Overuse Headache • When? – Failure of outpatient approach – Medication type +/or comorbidities • How? – Supportive care • Hydration/drugs to combat withdrawal symptoms – Clonidine if opiates – Anti-emetics & Neuroleptics • Iv Anti-nocioceptive drugs – i. v. Aspirin & iv Dihydroergotamine – i. v. AEDs
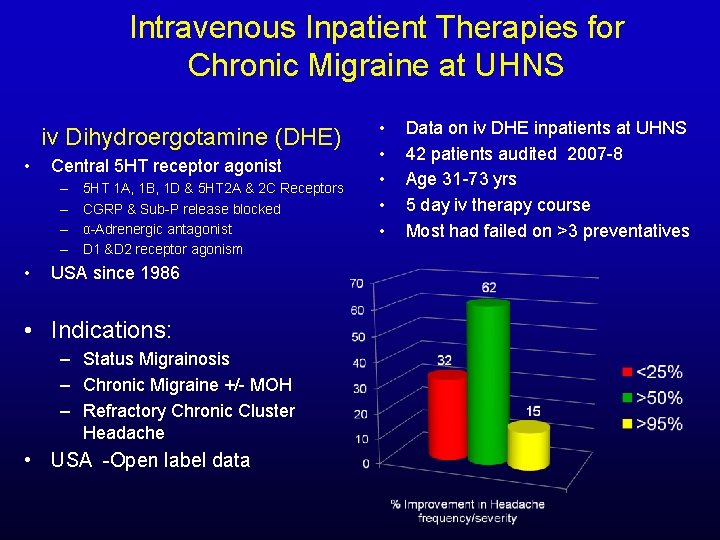
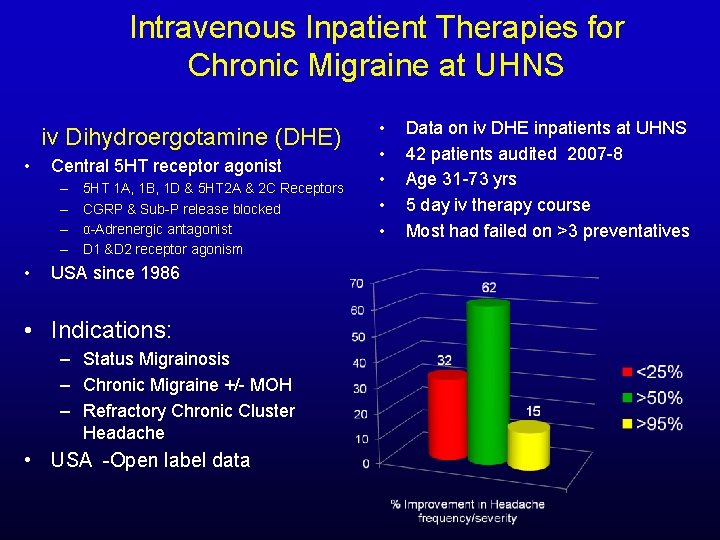
Intravenous Inpatient Therapies for Chronic Migraine at UHNS iv Dihydroergotamine (DHE) • Central 5 HT receptor agonist – – • 5 HT 1 A, 1 B, 1 D & 5 HT 2 A & 2 C Receptors CGRP & Sub-P release blocked α-Adrenergic antagonist D 1 &D 2 receptor agonism USA since 1986 • Indications: – Status Migrainosis – Chronic Migraine +/- MOH – Refractory Chronic Cluster Headache • USA -Open label data • • • Data on iv DHE inpatients at UHNS 42 patients audited 2007 -8 Age 31 -73 yrs 5 day iv therapy course Most had failed on >3 preventatives
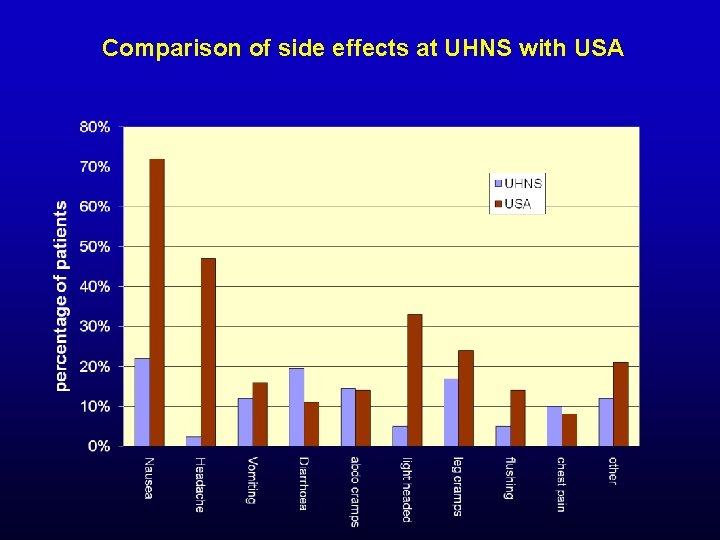
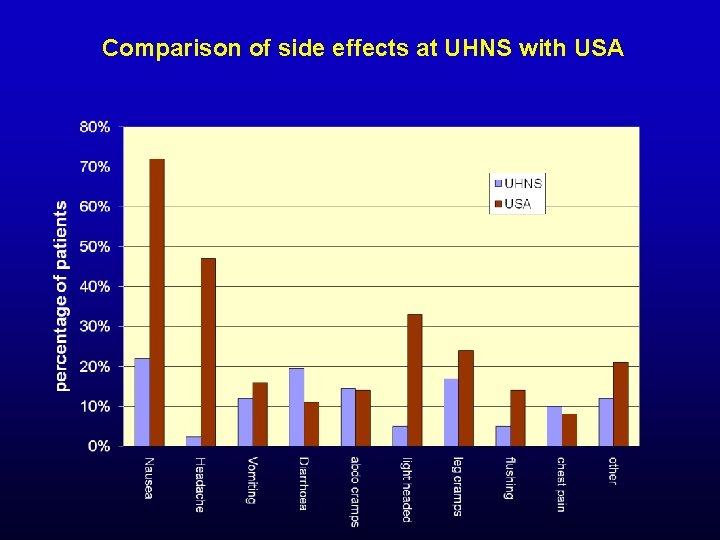
Comparison of side effects at UHNS with USA

Evidence based treatment of Chronic migraine
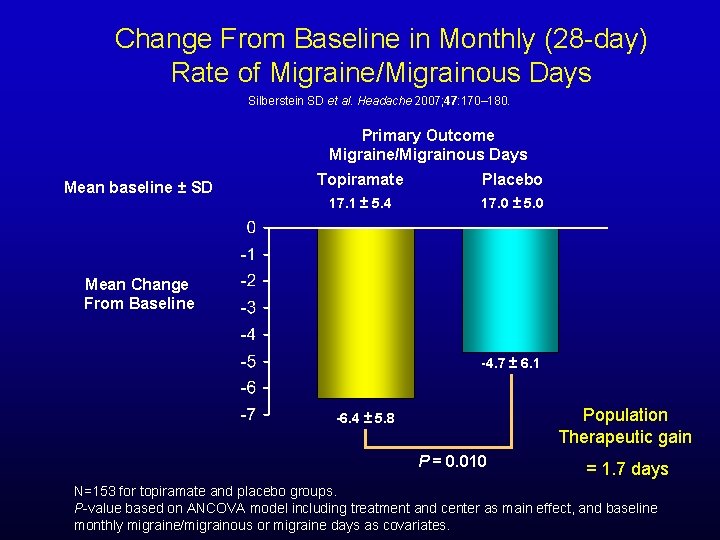
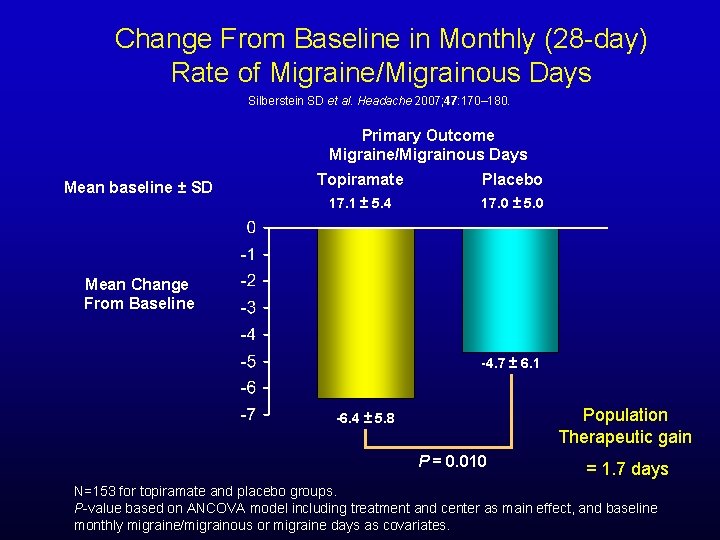
Change From Baseline in Monthly (28 -day) Rate of Migraine/Migrainous Days Silberstein SD et al. Headache 2007; 47: 170– 180. Primary Outcome Migraine/Migrainous Days Mean baseline ± SD Topiramate Placebo 17. 1 ± 5. 4 17. 0 ± 5. 0 Mean Change From Baseline -4. 7 ± 6. 1 Population Therapeutic gain -6. 4 ± 5. 8 P = 0. 010 = 1. 7 days N=153 for topiramate and placebo groups. P-value based on ANCOVA model including treatment and center as main effect, and baseline monthly migraine/migrainous or migraine days as covariates.
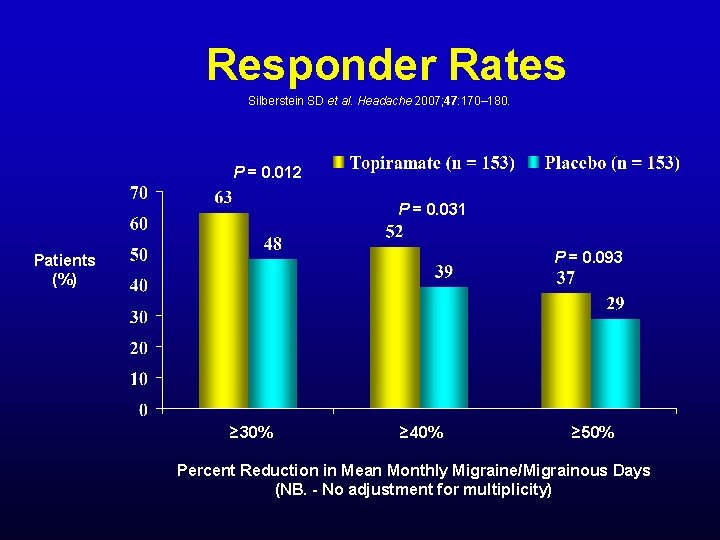
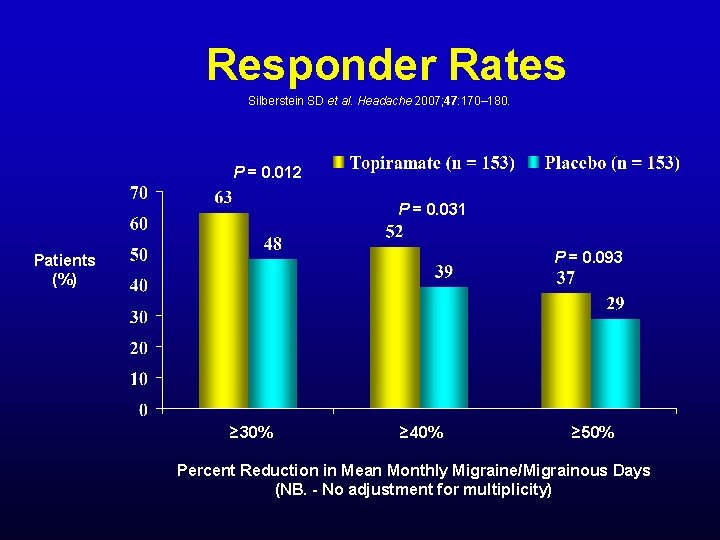
Responder Rates Silberstein SD et al. Headache 2007; 47: 170– 180. P = 0. 012 P = 0. 031 P = 0. 093 Patients (%) ≥ 30% ≥ 40% ≥ 50% Percent Reduction in Mean Monthly Migraine/Migrainous Days (NB. - No adjustment for multiplicity)
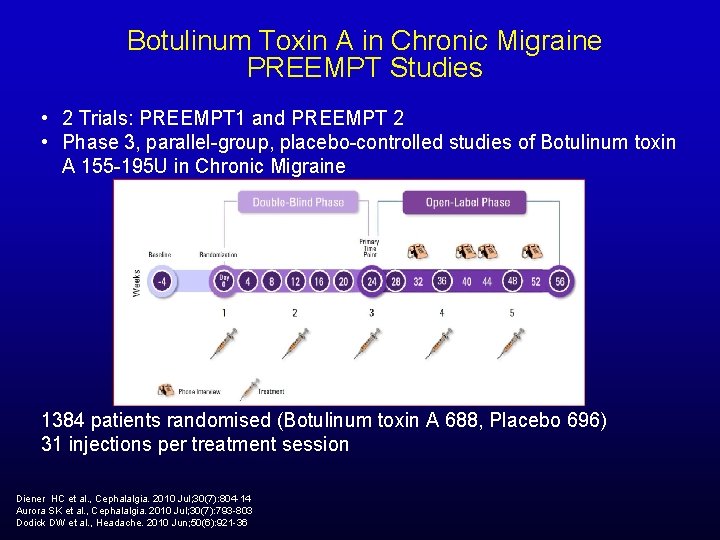
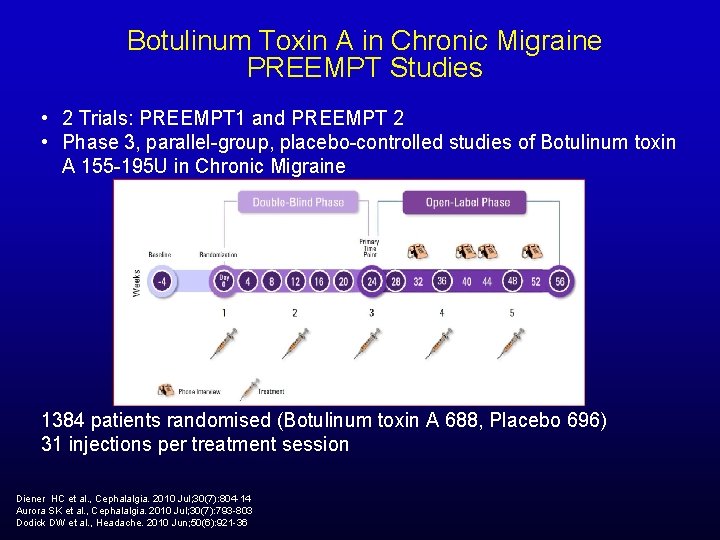
Botulinum Toxin A in Chronic Migraine PREEMPT Studies • 2 Trials: PREEMPT 1 and PREEMPT 2 • Phase 3, parallel-group, placebo-controlled studies of Botulinum toxin A 155 -195 U in Chronic Migraine 1384 patients randomised (Botulinum toxin A 688, Placebo 696) 31 injections per treatment session Diener HC et al. , Cephalalgia. 2010 Jul; 30(7): 804 -14 Aurora SK et al. , Cephalalgia. 2010 Jul; 30(7): 793 -803 Dodick DW et al. , Headache. 2010 Jun; 50(6): 921 -36
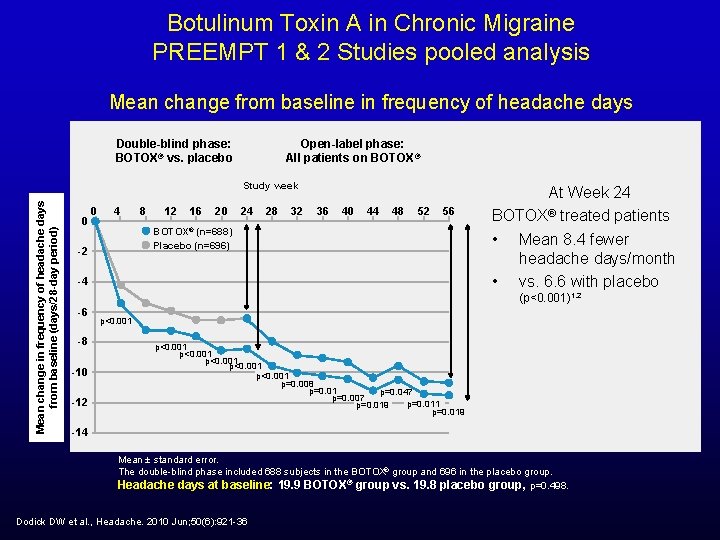
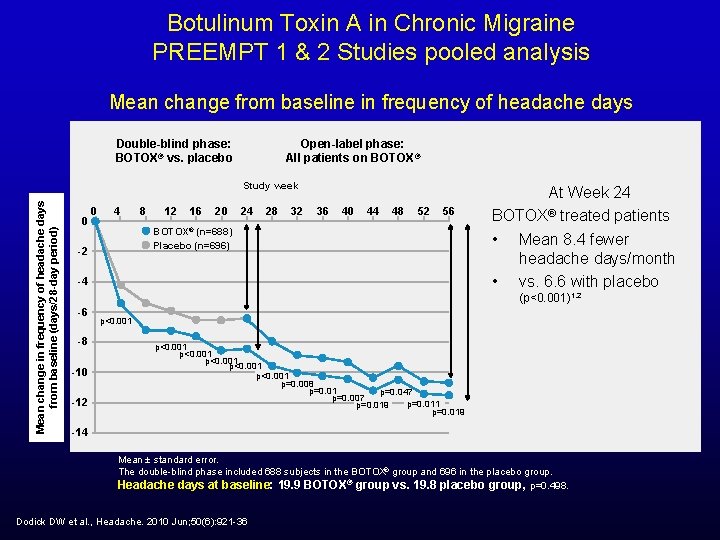
Botulinum Toxin A in Chronic Migraine PREEMPT 1 & 2 Studies pooled analysis Mean change from baseline in frequency of headache days Double-blind phase: BOTOX® vs. placebo Open-label phase: All patients on BOTOX ® Mean change in frequency of headache days from baseline (days/28 -day period) Study week 0 0 4 8 12 16 20 24 28 32 36 40 44 48 52 56 BOTOX® (n=688) Placebo (n=696) -2 -4 At Week 24 BOTOX® treated patients • Mean 8. 4 fewer headache days/month • vs. 6. 6 with placebo (p<0. 001)1, 2 -6 -8 -10 -12 p<0. 001 p<0. 001 p=0. 008 p=0. 01 p=0. 047 p=0. 007 p=0. 011 p=0. 019 -14 Mean ± standard error. The double-blind phase included 688 subjects in the BOTOX® group and 696 in the placebo group. Headache days at baseline: 19. 9 BOTOX® group vs. 19. 8 placebo group, p=0. 498. Dodick DW et al. , Headache. 2010 Jun; 50(6): 921 -36
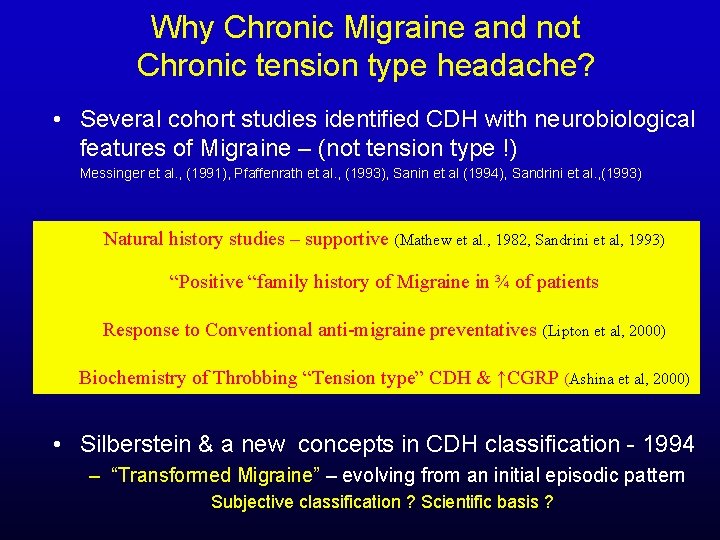
Why Chronic Migraine and not Chronic tension type headache? • Several cohort studies identified CDH with neurobiological features of Migraine – (not tension type !) Messinger et al. , (1991), Pfaffenrath et al. , (1993), Sanin et al (1994), Sandrini et al. , (1993) Natural history studies – supportive (Mathew et al. , 1982, Sandrini et al, 1993) “Positive “family history of Migraine in ¾ of patients Response to Conventional anti-migraine preventatives (Lipton et al, 2000) Biochemistry of Throbbing “Tension type” CDH & ↑CGRP (Ashina et al, 2000) • Silberstein & a new concepts in CDH classification - 1994 – “Transformed Migraine” – evolving from an initial episodic pattern Subjective classification ? Scientific basis ?