CHRONIC ABDOMINAL PAIN IS IT IN YOUR HEAD
CHRONIC ABDOMINAL PAIN: IS IT IN YOUR HEAD OR IN YOUR GUT? Michelle Tobin, MD Clinical Assistant Professor, Department of Pediatrics Division of Pediatric Gastroenterology and Nutrition Stony Brook Children's Hospital
DISCLOSURE • I have no financial relationships to disclose
CLINICAL VIGNETTE • 16 yr old female previously healthy with intermittent crampy, periumbilical abdominal pain x 2 months • Associated nausea, vomiting, diarrhea and fatigue o 1 -6 episodes of nonbloody watery stool o Treated with Prevacid o Nausea persisted • ROS negative: fever, joint pain, oral sores, rashes, weight loss, nocturnal symptoms • She denies recent travel or visitors from outside the country or sick contacts • Missed several school days due to her symptoms
CLINICAL VIGNETTE CONT. • Labwork results normal o CBC, CMP, ESR, CRP, amylase, lipase, ASCA, ANCA and TFTs • Stool Studies Negative o c. difficile, culture, O+P, and H. pylori

DIAGNOSIS • Red Flags o o o o Unexplained weight loss Growth retardation Delayed puberty Significant vomiting/diarrhea Family hx of IBD GI blood loss Unexplained fever, rash, arthralgia
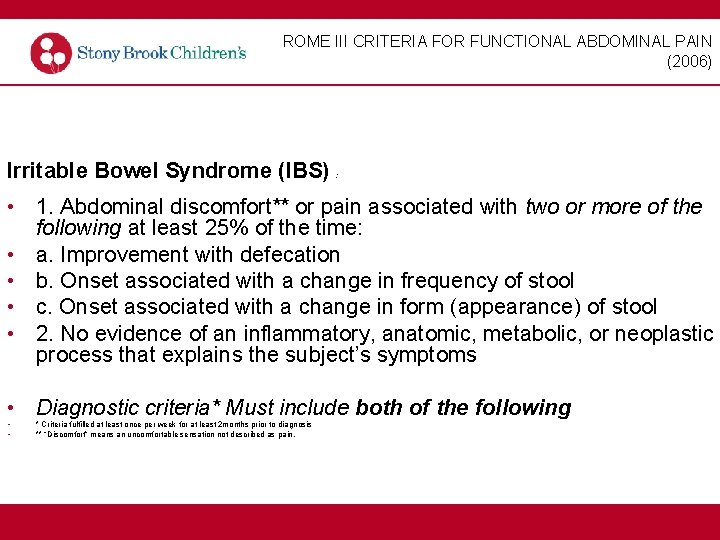
ROME III CRITERIA FOR FUNCTIONAL ABDOMINAL PAIN (2006) Irritable Bowel Syndrome (IBS) : • 1. Abdominal discomfort** or pain associated with two or more of the following at least 25% of the time: • a. Improvement with defecation • b. Onset associated with a change in frequency of stool • c. Onset associated with a change in form (appearance) of stool • 2. No evidence of an inflammatory, anatomic, metabolic, or neoplastic process that explains the subject’s symptoms • Diagnostic criteria* Must include both of the following • • * Criteria fulfilled at least once per week for at least 2 months prior to diagnosis ** “Discomfort” means an uncomfortable sensation not described as pain.
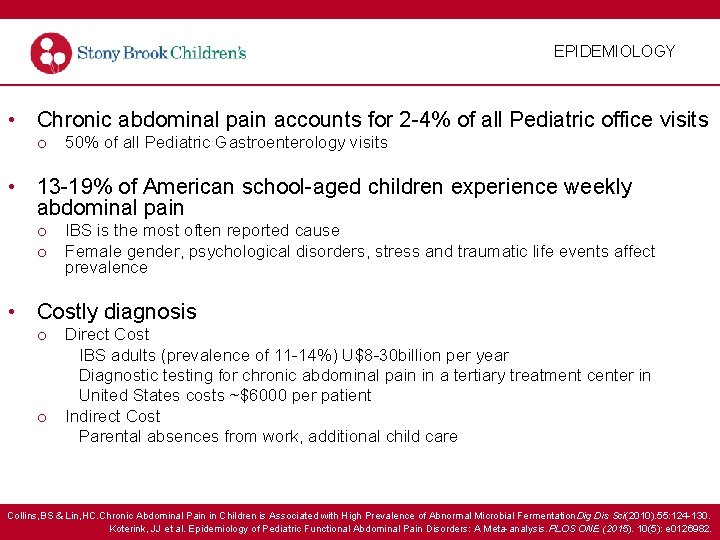
EPIDEMIOLOGY • Chronic abdominal pain accounts for 2 -4% of all Pediatric office visits o 50% of all Pediatric Gastroenterology visits • 13 -19% of American school-aged children experience weekly abdominal pain o o IBS is the most often reported cause Female gender, psychological disorders, stress and traumatic life events affect prevalence • Costly diagnosis o o Direct Cost IBS adults (prevalence of 11 -14%) U$8 -30 billion per year Diagnostic testing for chronic abdominal pain in a tertiary treatment center in United States costs ~$6000 per patient Indirect Cost Parental absences from work, additional child care Collins, BS & Lin, HC. Chronic Abdominal Pain in Children is Associated with High Prevalence of Abnormal Microbial Fermentation. Dig Dis Sci(2010). 55: 124 -130. Koterink, JJ et al. Epidemiology of Pediatric Functional Abdominal Pain Disorders: A Meta-analysis. PLOS ONE (2015). 10(5): e 0126982.
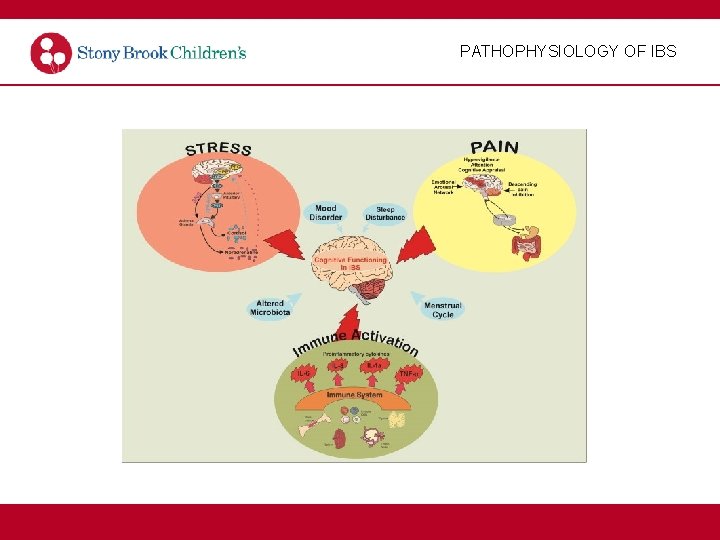
PATHOPHYSIOLOGY OF IBS

TREATMENT FOR IBS
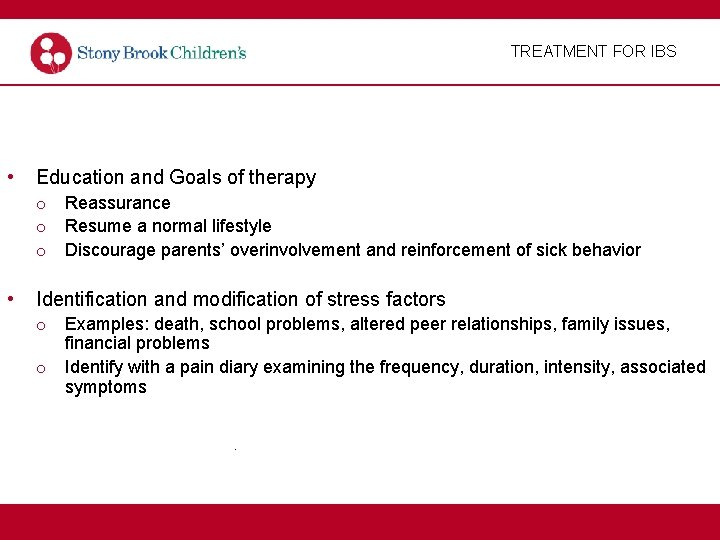
TREATMENT FOR IBS • Education and Goals of therapy o Reassurance o Resume a normal lifestyle o Discourage parents’ overinvolvement and reinforcement of sick behavior • Identification and modification of stress factors o Examples: death, school problems, altered peer relationships, family issues, financial problems o Identify with a pain diary examining the frequency, duration, intensity, associated symptoms.
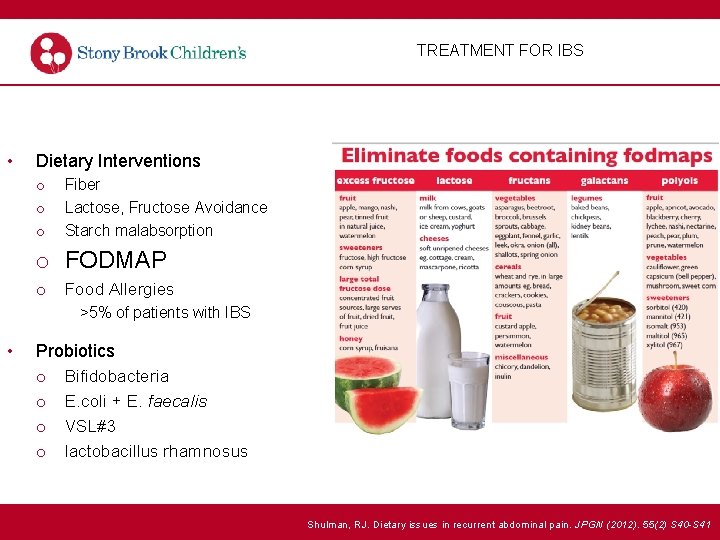
TREATMENT FOR IBS • Dietary Interventions o o o Fiber Lactose, Fructose Avoidance Starch malabsorption o FODMAP o Food Allergies >5% of patients with IBS • Probiotics o Bifidobacteria o E. coli + E. faecalis o VSL#3 o lactobacillus rhamnosus Shulman, RJ. Dietary issues in recurrent abdominal pain. JPGN (2012). 55(2) S 40 -S 41

TREATMENT FOR IBS • Pharmacological Treatment o H 2 Blockers o Serotonergic Agents o Tricyclic Antidepressants • Complementary Therapy o Peppermint o Ginger o Massage therapy/Acupuncture • Psychological Interventions o Cognitive behavioral therapy o Gut directed hypnotherapy
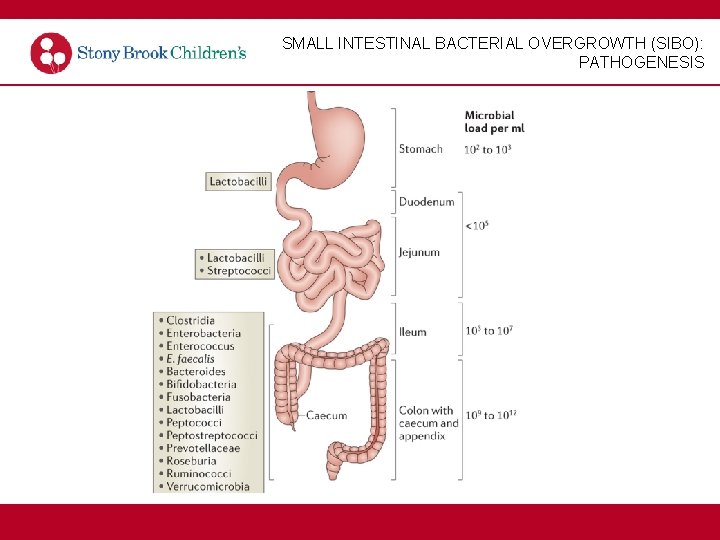
SMALL INTESTINAL BACTERIAL OVERGROWTH (SIBO): PATHOGENESIS
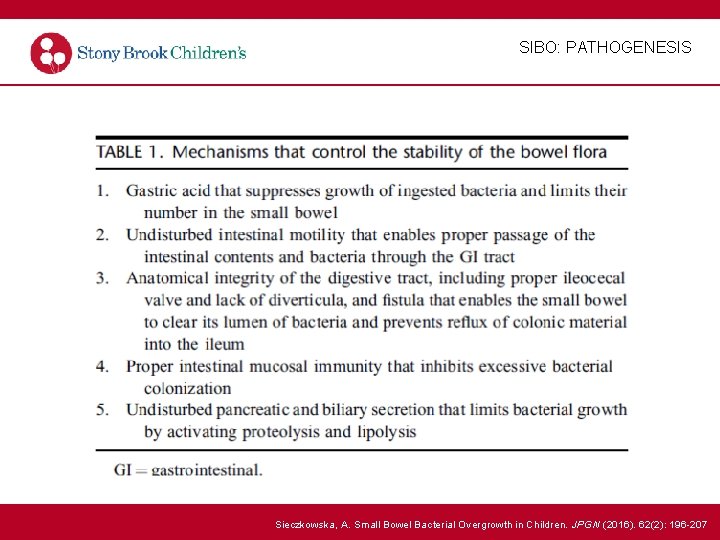
SIBO: PATHOGENESIS Sieczkowska, A. Small Bowel Bacterial Overgrowth in Children. JPGN (2016). 62(2): 196 -207
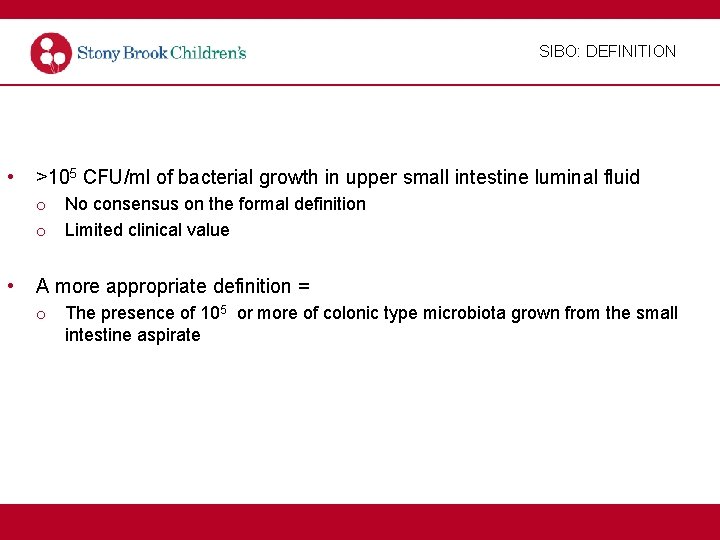
SIBO: DEFINITION • >105 CFU/ml of bacterial growth in upper small intestine luminal fluid o No consensus on the formal definition o Limited clinical value • A more appropriate definition = o The presence of 105 or more of colonic type microbiota grown from the small intestine aspirate
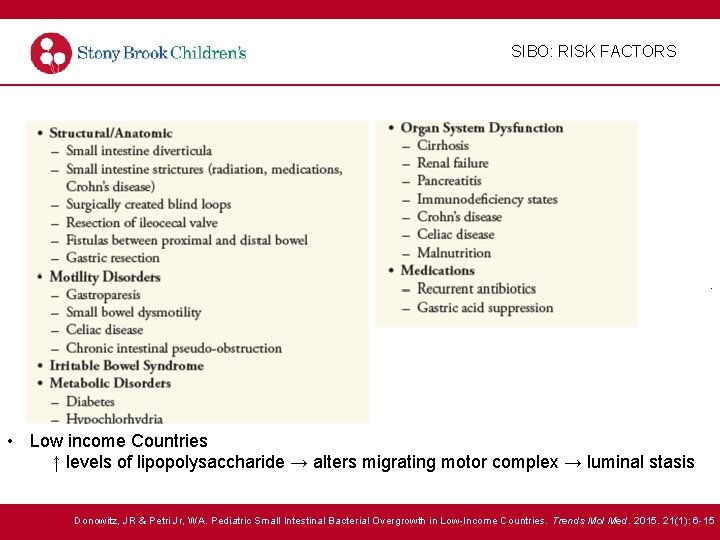
SIBO: RISK FACTORS . • Low income Countries ↑ levels of lipopolysaccharide → alters migrating motor complex → luminal stasis Donowitz, JR & Petri Jr, WA. Pediatric Small Intestinal Bacterial Overgrowth in Low-Income Countries. Trends Mol Med. 2015. 21(1): 6 -15
SIBO: EPIDEMIOLOGY • Epidemiology o Prevalence is increasing Due to readily available diagnostic tests and increased awareness o Overall prevalence is unknown o In healthy adults, 5. 9% of young adults were positive for SIBO vs 15. 6% in the older population o 64% IBS patients SIBO+ compared to controls 7% in outpatient setting o 63% children IBS patients SIBO+, 40 girls 67. 8%, 23 boys (56. 1%) in inpatient setting o 34% of children with abdominal pain and/or diarrhea were SIBO+ vs healthy controls o 54% of children with IBS-C were SIBO+ Scarpellini E. et al. Prevalence of Small Intestinal Bacterial Overgrowth in Children with Irritable Bowel Syndrome: A Case-Control Study. The Journal of Pediatrics(2009). 155: 416 -420. Siniewicz-Luzenczyk, K. et al. Small intestinal bacterial overgrowth syndrome in children. Prz Gastroenterol (2015). 10: 28 -32.
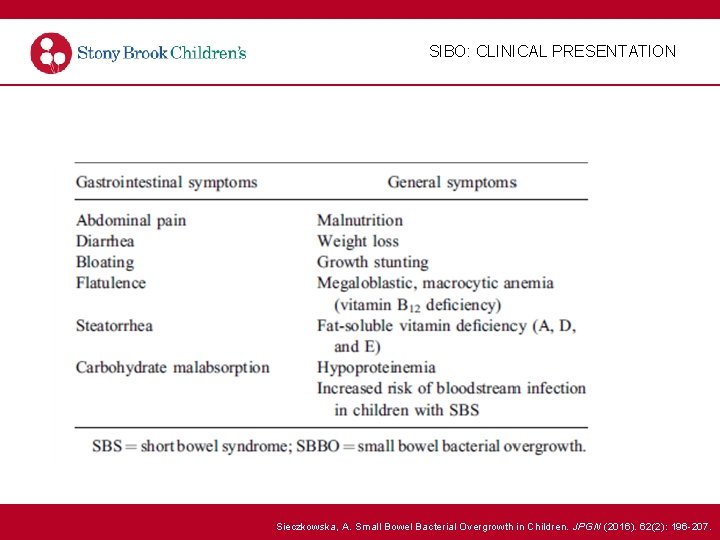
SIBO: CLINICAL PRESENTATION Sieczkowska, A. Small Bowel Bacterial Overgrowth in Children. JPGN (2016). 62(2): 196 -207.
SIBO: CLINICAL PRESENTATION • Vitamin Deficiencies o Vitamin B 2 (riboflavin) fatigue, slowed growth, cheilosis, glossitis, seborrhea, photophobia o Vitamin B 6 (pyridoxine) dermatitis, cheilosis, glossitis, microcytic anemia, weight loss, peripheral neuritis, irritability, seizure o Vitamin B 12 (cyanocobalamin) megaloblastic, macrocytic anemia, diarrhea, shortness of breath, demyelinating, posterior spinal column changes o Folic acid megaloblastic anemia, neutropenia, altered amino acid metabolism, impaired growth, diarrhea
SIBO: DIAGNOSIS • Diagnosis o Gold Standard: Jejunal aspirate Disadvantages: Invasive requires endoscopy Costly Anesthesia – conscious sedation/general anesthesia Technical issues
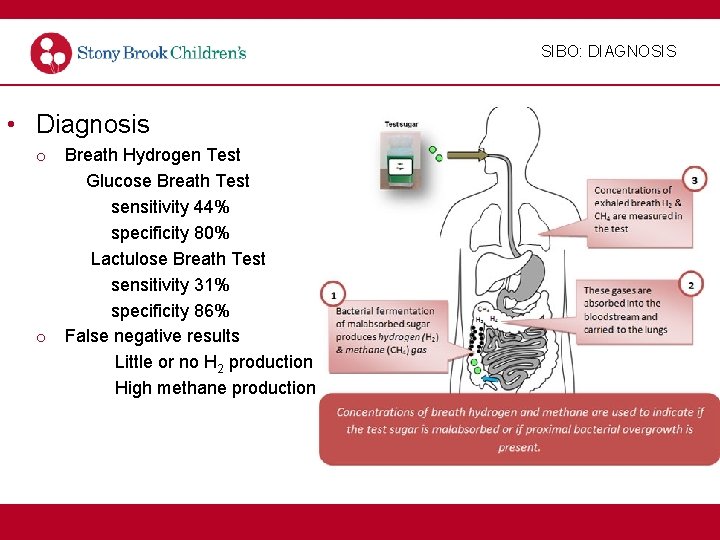
SIBO: DIAGNOSIS • Diagnosis o Breath Hydrogen Test Glucose Breath Test sensitivity 44% specificity 80% Lactulose Breath Test sensitivity 31% specificity 86% o False negative results Little or no H 2 production High methane production
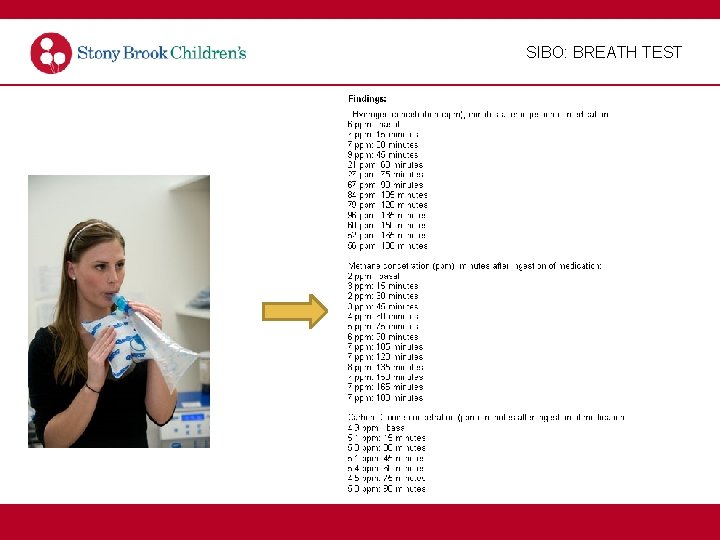
SIBO: BREATH TEST
SIBO: DIAGNOSIS • Diagnosis o 13 Carbon Labeled Breath Test sensitivity 100% specificity 67% rarely used due to limited accessibility of analyzing equipment o Serum D-Lactate >1 mmol/L rarely used; only useful in patients at risk of acidosis o Urine Indican Concentration rarely use; requires 24 hr urine collection o Fecal Calprotectin no increase seen in SIBO+ pts Fundaro C. et al. Fecal Calprotectin concentration in children affected by SIBO. European Review for Medical and Phamacological Sciences. (2011). 15: 1328 -1335.
SIBO: TREATMENT • Treatment o Correction of the Underlying Cause Surgery, Dietary, Pharmacology o Nutritional Support Replenish deficiencies o Probiotics L. casei, L. plantarum, Strep. faecalis, Bifidobacterium brevis vs metronidazole was clinically more effective for SIBO treatment Administration of L. rhamnosus R 0011, L acidophilus R 0052 to patients while on omeprazole for 4 weeks did not decrease the risk of developing SIBO
SIBO: TREATMENT • Treatment o Antibiotic Therapy Goal: modify the microbiota, not eliminate Empiric therapy that covers gram negative bacteria and anaerobes o Rifaximin Nonabsorbable antibiotic Conflicting evidence on clinical effectiveness, dose and duration o Metronidazole o Trimethoprim/sulfamethoxazole Combination therapy of Bactrim and flagyl showed 95% eradication of SIBO in asymptomatic patients living in the slums in Brazil Tahan S. et al. Effectiveness of Trimethoprim-Sulfamethoxazole and Metronidazole in the Treatment of Small Intestinal Bactieral Overgrowth in Children Living in a Slum. JPGN (2013). 57(3): 316 -318.
SIBO: TREATMENT • Treatment o Other antibiotics Augmentin Tetracycline Ciprofloxacin Gentamicin Neomycin
BACK TO THE VIGNETTE … • • Patient underwent lactulose breath test Diagnosed with Small intestinal bacterial overgrowth Treated with Bactrim and Metronidazole with some improvement Treated with Rifaximin which resulted in resolution of her symptoms and normalization of her breath test results
Thank You
- Slides: 28