CHOOSING THE RIGHT MEDICAL TREATMENT AND RECENT ADVANCES
































- Slides: 53
CHOOSING THE RIGHT MEDICAL TREATMENT AND RECENT ADVANCES NEELIMA THAKUR, MD.
Epilepsy Burden • The lifetime likelihood of – Experiencing at least 1 seizure is ~ 9%. – Receiving a diagnosis of epilepsy is ~3%. • Approximately 200, 000 new cases of seizures and epilepsy occur each year. • Epilepsy and seizures affect nearly 3 million Americans of all ages, at an estimated annual cost of $17. 6 billion in direct and indirect costs.
Seizures are defined as abnormal discharge of electrical activity from brain neurons resulting in transient loss of motor, sensory or mental function.

Seizure types • Provoked seizures • Acute symptomatic. • Often a reversible cause. not epilepsy. • Unprovoked seizures • By definition, these are • 2 unprovoked seizures 24 hrs apart is considered epilepsy.

First unprovoked seizure – risk of seizur recurrence. • 24 -74 % in first 5 years. – Normal EEG and imaging studies – 24% – Abnormal EEG and imaging studies- 74% • After 2 nd unprovoked seizure – 80%

First unprovoked seizure • Risk factors for seizure recurrence – Family history - Abnormal EEG - Abnormal neuroimaging. - Seizure in sleep.

First unprovoked seizure • 50 % seizures recur in the first year • 80% with in two years.

First unprovoked seizure • Current Guidelines – No antiepileptic drugs (AEDs) if • There are no other risk factors • Normal EEG.

Anti epileptic Drugs
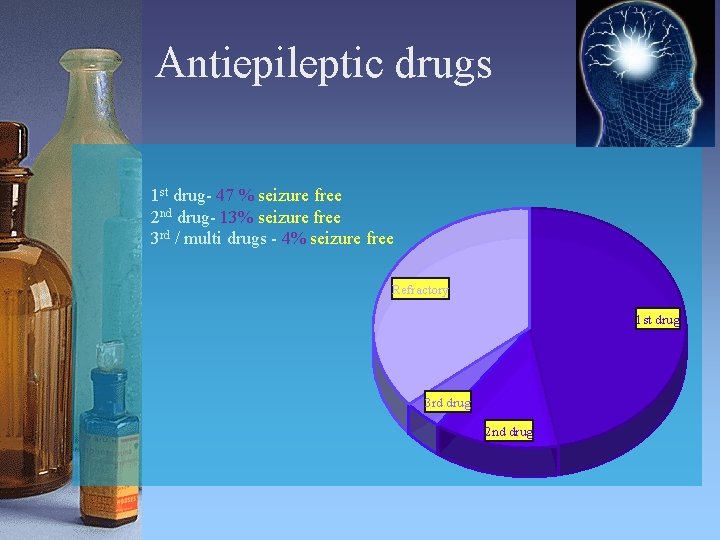
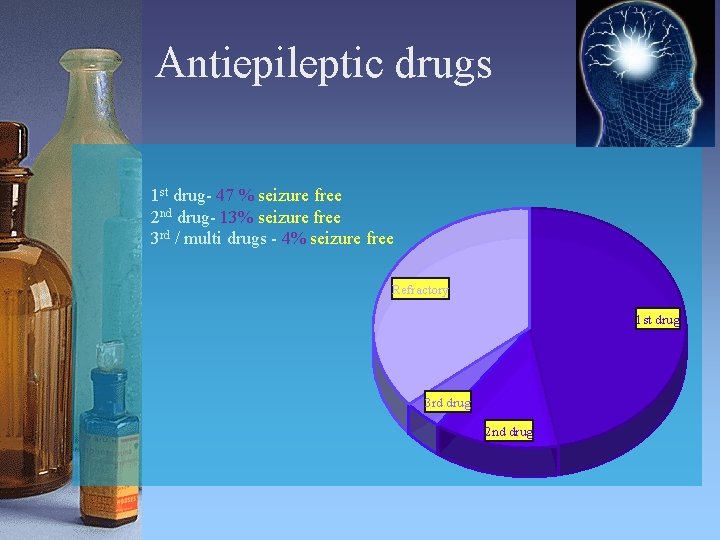
Antiepileptic drugs 1 st drug- 47 % seizure free 2 nd drug- 13% seizure free 3 rd / multi drugs - 4% seizure free Refractory 1 st drug 3 rd drug 2 nd drug

Epilepsy outcome at >7 years. • Seizure free >7 years - 59 % • Seizure free >1 year and relapses- 16 %

Which AED to choose?

Anti epileptic Drugs • • • 1850 : Bromides 1910: Phenobarbital 1940: Phenytoin 1950: Ethosuximide 1958: ACTH 1954: Primidone 1968: Carbamazepine 1975: Clonazepam 1978: Depakote
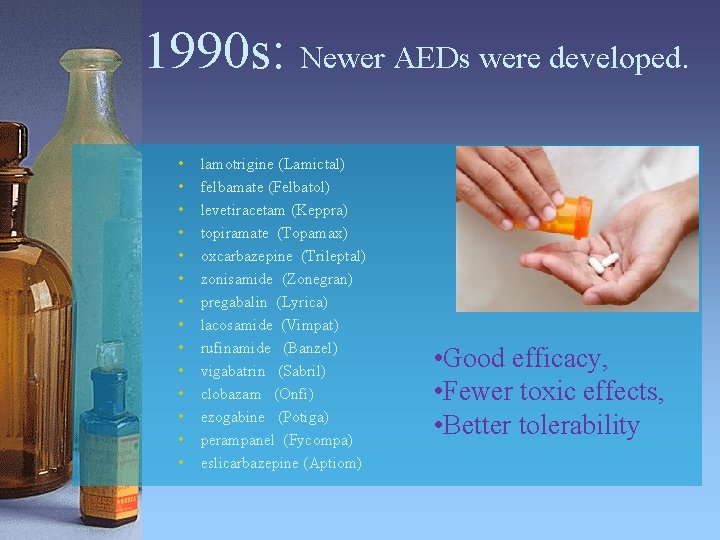
1990 s: Newer AEDs were developed. • • • • lamotrigine (Lamictal) felbamate (Felbatol) levetiracetam (Keppra) topiramate (Topamax) oxcarbazepine (Trileptal) zonisamide (Zonegran) pregabalin (Lyrica) lacosamide (Vimpat) rufinamide (Banzel) vigabatrin (Sabril) clobazam (Onfi) ezogabine (Potiga) perampanel (Fycompa) eslicarbazepine (Aptiom) • Good efficacy, • Fewer toxic effects, • Better tolerability
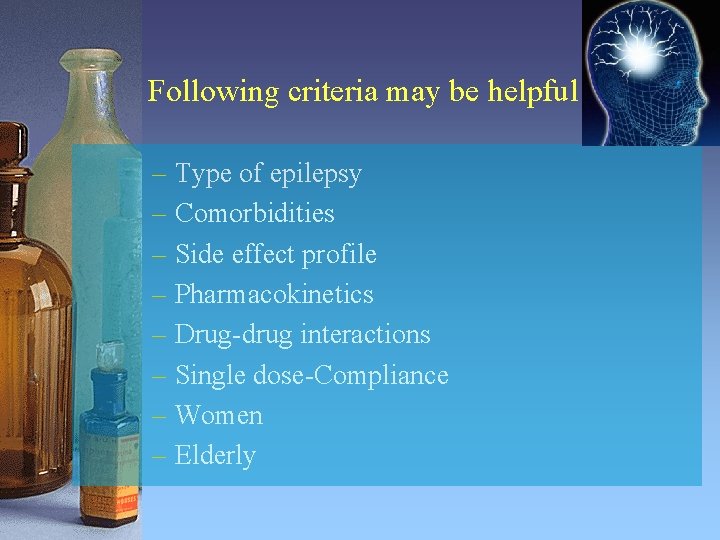
Following criteria may be helpful – Type of epilepsy – Comorbidities – Side effect profile – Pharmacokinetics – Drug-drug interactions – Single dose-Compliance – Women – Elderly

Type of epilepsy • Primarily generalized epilepsies. – – – – – ethosuximide ( Absence seizures) valproate topiramate zonisamide lamotrigine levetiracetam rufinamaide clobazam vigabatrin.

Primarily generalized epilepsies • Avoid carbamazepine, gabapentin, Phenytoin.

Efficacy Primarily generalized epilepsy • Absence seizures – ethosuximide, valproate are effective than lamotrigine. • Atonic seizures : clobazam. • Primarily generalized epilepsies: valproate>topamax and leviteracetam.
Type of epilepsy • Partial Epilepsies All AEDs except ethosuximide.
Efficacy-Partial seizures • Not possible to compare efficacy as there are no major head to head trials. • The study population, inclusion and exclusion criteria are different. ‘

Mechanism of action Rational polypharmacy.
Comorbidities • Bipolar disorder/depression/anxiety: valproate, lamotrigine, carbamazepine, oxcarbazepine. • Migraines: valproate, topiramate, zonisamide. • Obesity: topiramate, zonisamide • Neuropathy: gabapentin, lyrica, carbamazepine, oxcarbazepine.

Comorbidities AEDs to avoid • Psychiatric/behavorial problems: levetiracetam. • Osteoporosis: phenobarbital, phenytoin, valproate, carbamazepine. • Renal stones : topamax, zonegran. • Obesity: valproate, pregabalin, gabapentin. • Diabetes: valproate.

Liver dysfunction Drugs of choice • leviteracetam • lacosamide • pregabalin • gabapentin
Renal dysfunction Decrease drug doses that are cleared primarily by kidneys – levetiracetam – lacosamide – pregabalin – gabapentin

Hemodialysis Risk of drug removal is high for non protein bound drugs Doses need to be adjusted accordingly. • High risk levetiracetam lacosamide phenobarbital topiramate. • Low risk phenytoin valproate lamotrigine. carbamazepine

Drug interactions Liver enzyme(CYP 450 & UGT) inducers phenytoin, phenobarbital, carbamazepine, oxcarbazepine, topiramate, felbamate, rufinamide. • Liver enzyme inhibitors – valproate, felbamate.

Single daily dose Improves Patient compliance. XR formulations may have lesser side effects. • Q day AEDs Phenytoin, Phenobarbital and zonegran. • XR formulation Depakote ER, Lamictal XR, Keppra XR, Oxtellar XR and Trokendi XR.
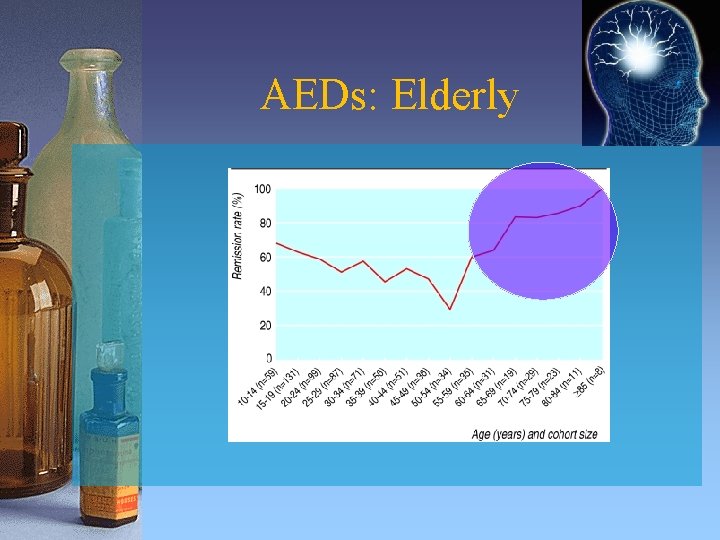
Epilepsy in Elderly • The prevalence and incidence of epilepsy are highest in later life!! • Approximately 7% of seniors have epilepsy. • 25% of new cases occur in elderly
AEDs : Elderly • Older people with a first unprovoked seizure are more likely to develop recurring seizures than are younger adults. • Starting AEDs after a single unprovoked seizure may be appropriate in some cases.
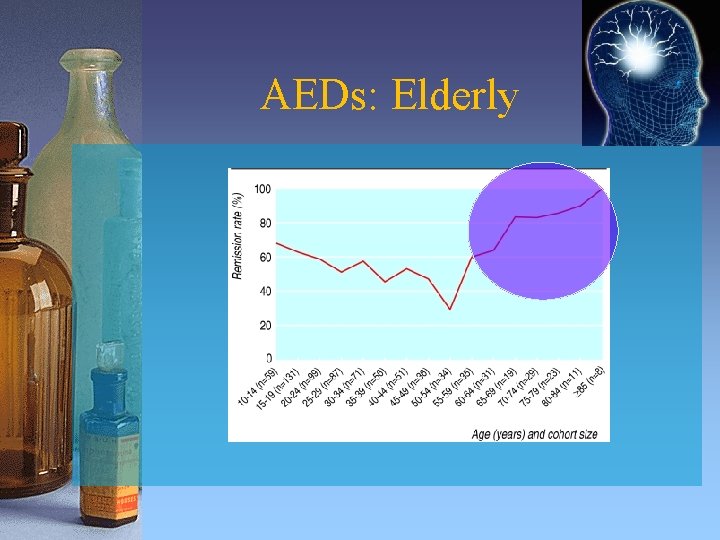
AEDs: Elderly

AEDs - Elderly TREAT CAUTIOUSLY! – Elderly are more susceptible to the adverse effects of drugs than their younger patients. – Pharmacokinetics and pharmacodynamics of AEDs differ in old age. – Drug-drug interactions

AEDs- Elderly Treatment Challenges • Comorbidities complicate the treatment options. • Polypharmacy make them susceptible to drug interactions. • Adherence may not be as good in elderly patients with epilepsy.

AEDs - Elderly • Pharmacokinetic – Albumin results in free fraction phenytoin, carbamazepine and valproate. – Drug metabolism is affected by decreased liver enzymes. – Drug excretion is affected by decreased renal clearance.

AEDs - Elderly • In general the preferred drugs are – levetiracetam – lamotrigine – gabapentin

AEDs-Pregnancy Concerns – Effect of AEDs on Fetus and infant during • Pregnancy • Breast feeding. – AED pharmacokinetics affecting levels during • Pregnancy • Postpartum

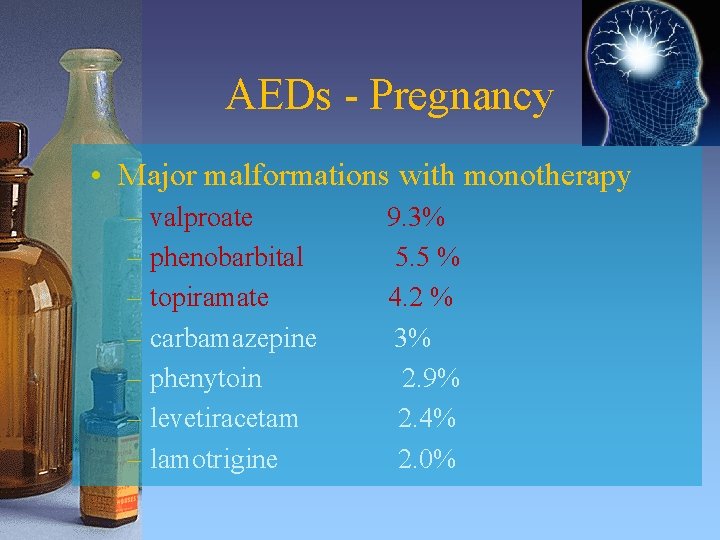
AEDs - Pregnancy Teratogenic risks mono vs polytherapy. • Single AED • Two AEDs • Three AEDs 3. 1 % 5. 8 % 8. 3%
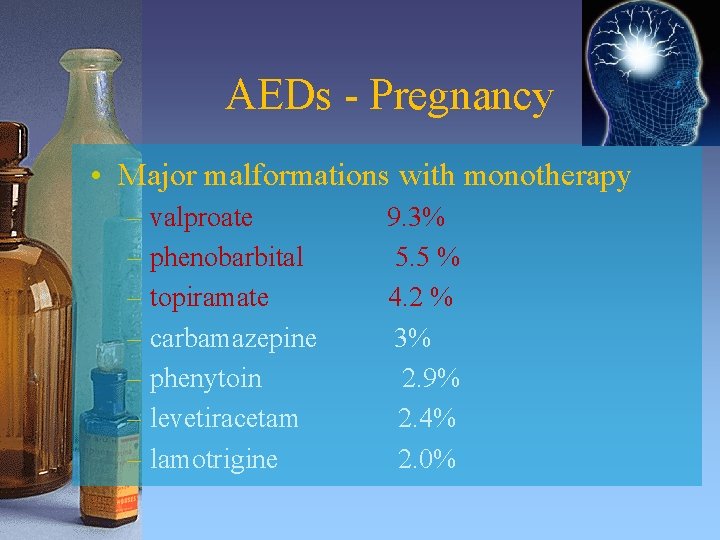
AEDs - Pregnancy • Major malformations with monotherapy – valproate – phenobarbital – topiramate – carbamazepine – phenytoin – levetiracetam – lamotrigine 9. 3% 5. 5 % 4. 2 % 3% 2. 9% 2. 4% 2. 0%
AEDs - Pregnancy • Pharmacokinetics lamotrigine & levetiracetam clearance during pregnancy level up to 50% of baseline. • Postpartumclearance returns to baseline and drug levels. • Check monthly levels and adjust dose.
AEDs - Pregnancy In general, levetiracetam, lamotrigine, oxcarbazepine and carbamazepine are considered relatively safe.

Newer AEDs • Ezogabine (Potiga) • Perampanel (Fycompa) • Eslicarbazepine (Aptiom)
Ezogabine (Potiga) 2011 • Mechanism of action: Potassium Channel • Approved for add on treatment for Partial epilepsy. • It is the first neuronal potassium channel opener developed for the treatment of epilepsy.

Ezogabine (Potiga) • Mechanism of action: Potassium Channel • Approved as add on treatment for Partial epilepsy. • First neuronal potassium channel opener developed for the treatment of epilepsy.
Ezogabine (Potiga) Absorption and Metabolism: – Well absorbed. Food has no influence. – Not known whether excreted in human milk. – Metabolized in liver. – Dosage adjustment is required in patients with moderate and greater renal or hepatic impairment. – *urine bilirubin can show falsely elevated readings

Ezogabine (Potiga) • Drug interactions – – Carbamazepine, phenytoin may Potiga levels. Potiga has no effect on other AED levels. POTIGA may digoxin serum concentrations. Alcohol systemic exposure to POTIGA
Ezogabine (Potiga) Adverse reactions FDA warning blue skin discoloration and eye abnormalities characterized by pigment changes in the retina Initial and periodic eye exams are recommended. – Urinary retention – Neuropsychiatric symptoms- confusion, psychosis – QT interval prolongation

Perampanel (Fycompa) 2012 • Mechanism of action: AMPA glutamate receptor noncompetitive antagonist. • Approved as add on treatment for Partial epilepsy.
Perampanel (Fycompa) • Absorption and Metabolism: – Well absorbed. Food has no influence. – Not known whether excreted in human milk. – Metabolized in liver. Dosage adjustment is required in patients with moderate and greater renal or hepatic impairment.

Perampanel(Fycompa) Drug interactions – Does not effect other AEDs. – Enzyme inducers perampanel levels.

Perampanel (Fycompa) • Adverse reactions – Neuro-psychiatric symptoms ( black box warning for aggression and hostility). – Dizziness , Somnolence fatigue, blurred vision. – Pregnancy category C

Eslicarbazepine (Aptiom) 2013 • Mechanism of action: Na channel blocker. the prodrug metabolizes to eslicarbazepine. . • Approved as add on treatment for Partial epilepsy.
Eslicarbazepine (Aptiom) • Absorption and Metabolism: – Well absorbed. Food has no influence. – Metabolized in liver and kidneys. • Drug interactions and Side effects Similar but more tolerable than oxcarbazepine

Thank you
 Recent advances in ceramics
Recent advances in ceramics Right product right place right time right price
Right product right place right time right price Family time
Family time Contoh perencanaan lokasi
Contoh perencanaan lokasi The right man on the right place at the right time
The right man on the right place at the right time Basic cooking methods
Basic cooking methods Choose the correct answer a-c
Choose the correct answer a-c Vocab level g unit 12
Vocab level g unit 12 Payroll in tally
Payroll in tally What is long term loans and advances
What is long term loans and advances Lurbinectedin posologie
Lurbinectedin posologie Axis powers
Axis powers Advances in technology during wwii
Advances in technology during wwii Chapter 9 intellectual development in the first year
Chapter 9 intellectual development in the first year Advances in real time rendering
Advances in real time rendering Advances in mri
Advances in mri Opto-electronic advances
Opto-electronic advances Classification of advances as per rbi
Classification of advances as per rbi Advances in memory technology
Advances in memory technology Hepburn osteometric board
Hepburn osteometric board Recent trends in ic engine
Recent trends in ic engine Recent developments in ict
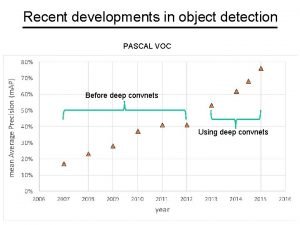
Recent developments in ict Recent developments in object detection
Recent developments in object detection Ap synthesis prompt
Ap synthesis prompt Modern trends of foreign trade in india
Modern trends of foreign trade in india Benefits of scanning in reading
Benefits of scanning in reading Recent trends in project management
Recent trends in project management Recent demographic changes in the uk
Recent demographic changes in the uk Clever myips
Clever myips Biotaphonomy
Biotaphonomy After miguel's recent automobile accident
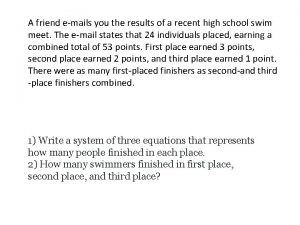
After miguel's recent automobile accident A friend emails you the results of a recent high school
A friend emails you the results of a recent high school Passive voice in the news
Passive voice in the news Https://drive.google.com/drive/
Https://drive.google.com/drive/ Udin login
Udin login Recent trends in mis
Recent trends in mis Https drive google com drive u 0 recent
Https drive google com drive u 0 recent What are the approaches to measuring performance
What are the approaches to measuring performance Defining performance and choosing a measurement approach
Defining performance and choosing a measurement approach Choosing and narrowing a topic
Choosing and narrowing a topic Narrowing topic
Narrowing topic Get in the train
Get in the train You put your right foot in
You put your right foot in Left left right right go go go
Left left right right go go go Medical terminology planes directions and positions
Medical terminology planes directions and positions Manus region
Manus region Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Lp html
Lp html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Hát lên người ơi alleluia
Hát lên người ơi alleluia Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy