Choosing Interfaces for Noninvasive Ventilation Annual Symposium on





- Slides: 41
Choosing Interfaces for Noninvasive Ventilation Annual Symposium on Emergency and Critical Care Medicine 2012 – NEW IMAGE, NEW DEVELOPMENT 6 th October 2012 Dr Arthur Chun-Wing Lau Halloween Masquerade Associate Consultant Department of Intensive Care Pamela Youde Nethersole Eastern Hospital, Hong Kong

Technical and clinical comparisons of various interfaces 1. Fitness for different NIV ventilator circuits 2. Materials 3. Deadspace, CO 2 rebreathing, Exhalation port position 4. Patient-ventilator synchrony 5. Noise 6. Complications 7. Overall clinical efficacy
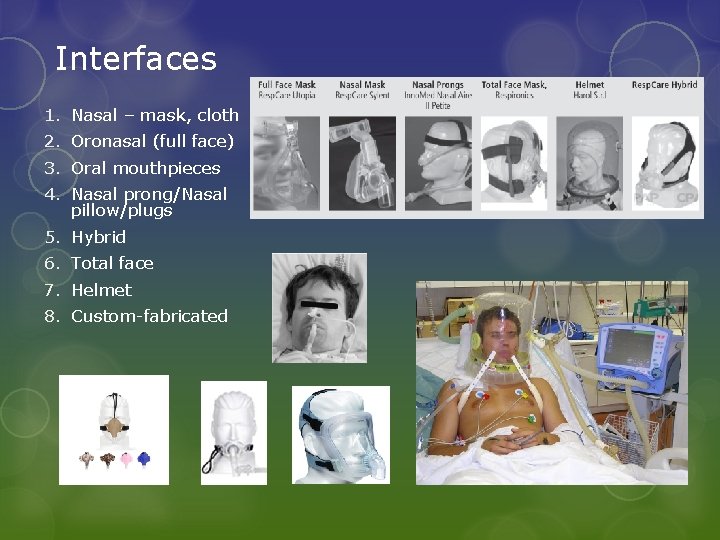
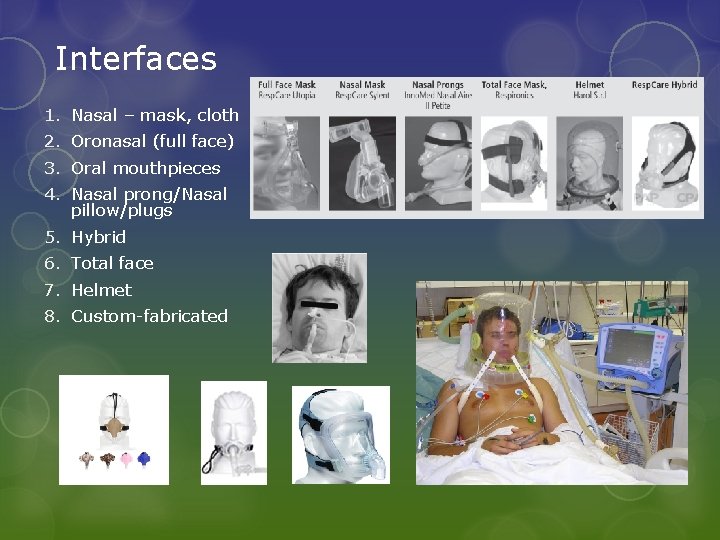
Interfaces 1. Nasal – mask, cloth 2. Oronasal (full face) 3. Oral mouthpieces 4. Nasal prong/Nasal pillow/plugs 5. Hybrid 6. Total face 7. Helmet 8. Custom-fabricated
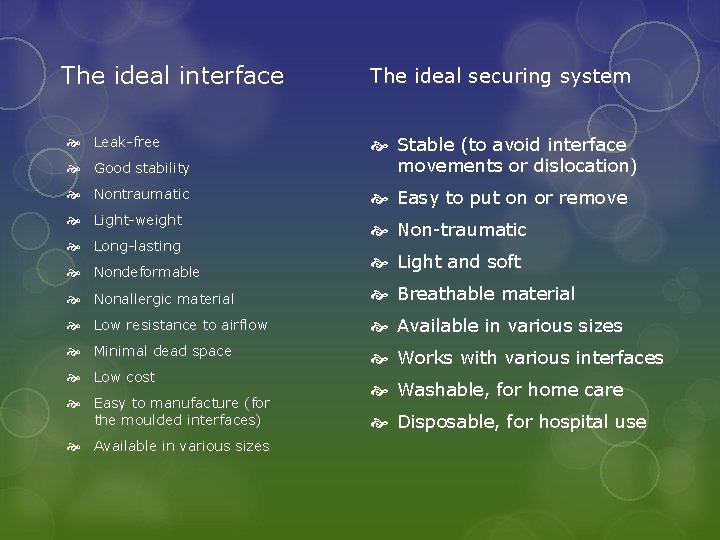
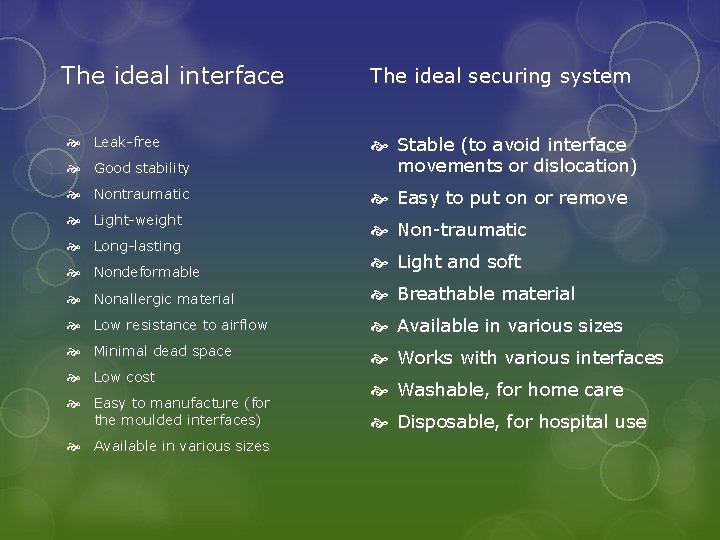
The ideal interface Leak-free The ideal securing system Good stability Stable (to avoid interface movements or dislocation) Nontraumatic Easy to put on or remove Light-weight Non-traumatic Long-lasting Nondeformable Light and soft Nonallergic material Breathable material Low resistance to airflow Available in various sizes Minimal dead space Works with various interfaces Low cost Easy to manufacture (for the moulded interfaces) Available in various sizes Washable, for home care Disposable, for hospital use
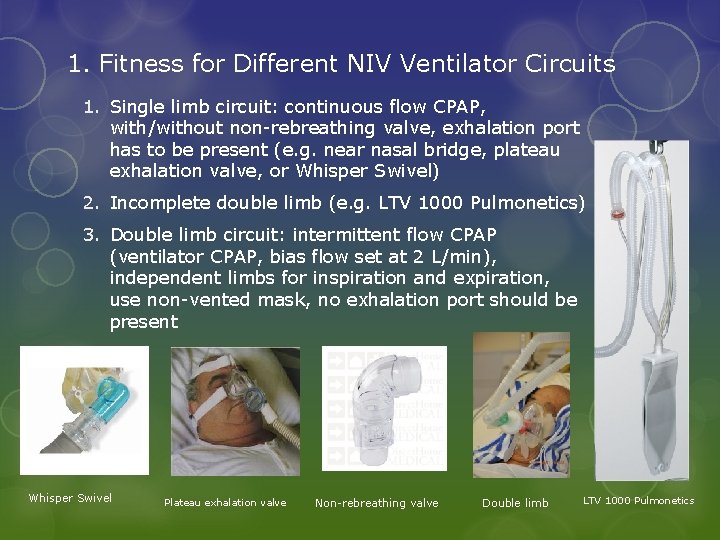
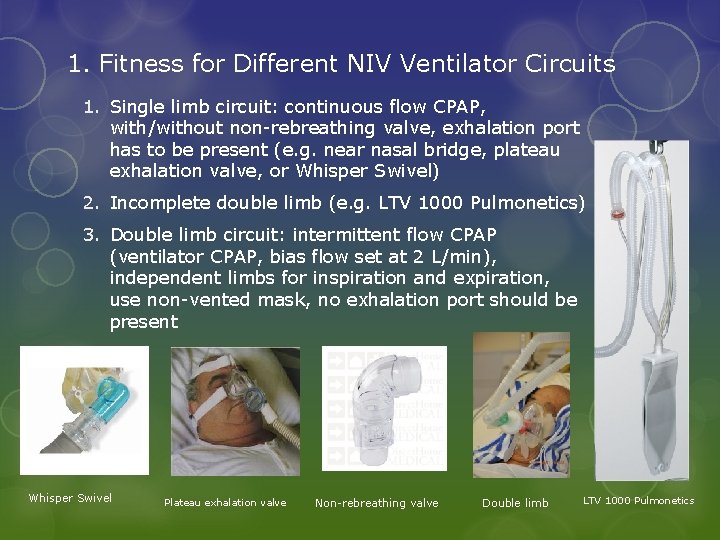
1. Fitness for Different NIV Ventilator Circuits 1. Single limb circuit: continuous flow CPAP, with/without non-rebreathing valve, exhalation port has to be present (e. g. near nasal bridge, plateau exhalation valve, or Whisper Swivel) 2. Incomplete double limb (e. g. LTV 1000 Pulmonetics) 3. Double limb circuit: intermittent flow CPAP (ventilator CPAP, bias flow set at 2 L/min), independent limbs for inspiration and expiration, use non-vented mask, no exhalation port should be present Whisper Swivel Plateau exhalation valve Non-rebreathing valve Double limb LTV 1000 Pulmonetics

ICU ventilators. Have to be equipped with a “noninvasive mode” Viasys Avea Puritan Bennett 840 Siemens Servo i Dräger Evita 4 NIV ventilators Respironi cs Bi. PAP Vision Respironic s Bi. PAP STD Sma rt. Air ST
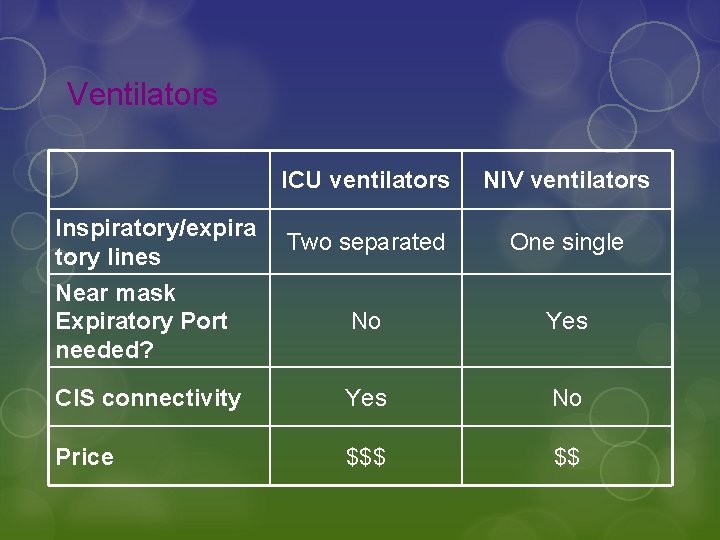
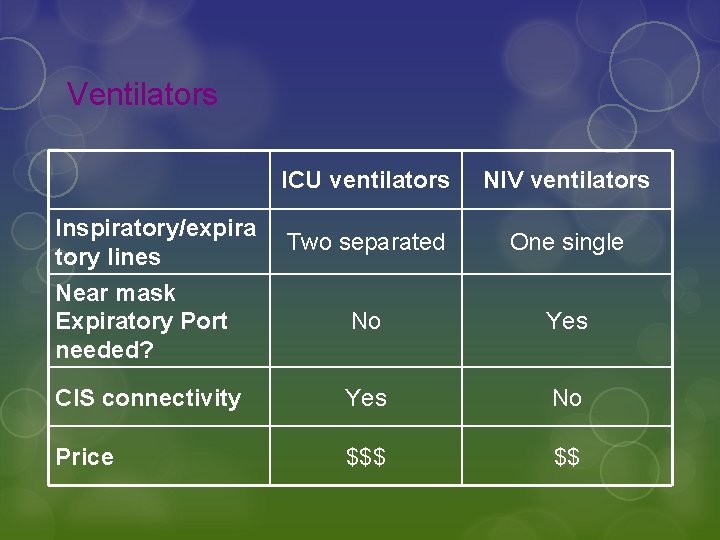
Ventilators ICU ventilators NIV ventilators Two separated One single Near mask Expiratory Port needed? No Yes CIS connectivity Yes No Price $$$ $$ Inspiratory/expira tory lines
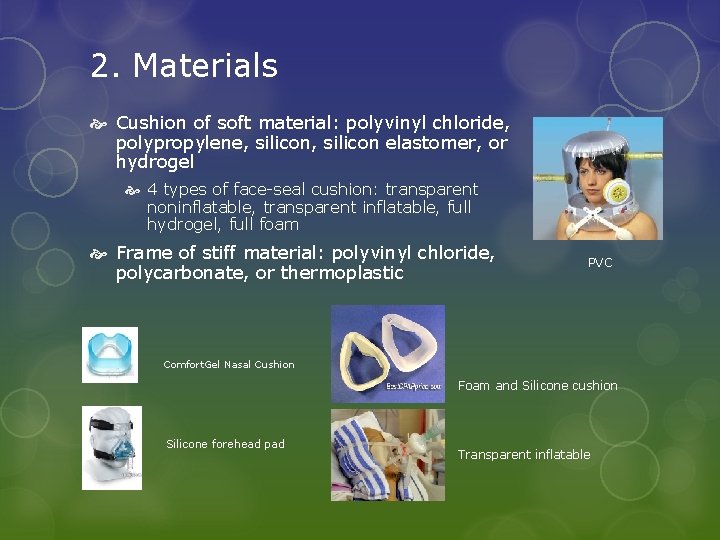
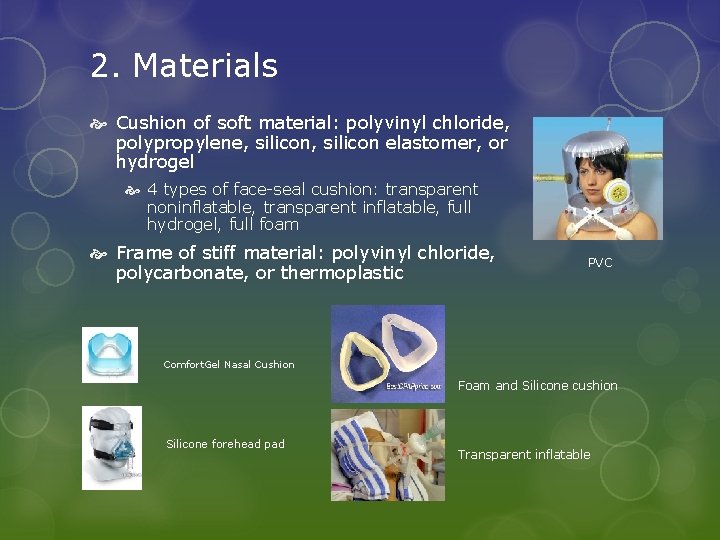
2. Materials Cushion of soft material: polyvinyl chloride, polypropylene, silicon elastomer, or hydrogel 4 types of face-seal cushion: transparent noninflatable, transparent inflatable, full hydrogel, full foam Frame of stiff material: polyvinyl chloride, polycarbonate, or thermoplastic PVC Comfort. Gel Nasal Cushion Foam and Silicone cushion Silicone forehead pad Transparent inflatable
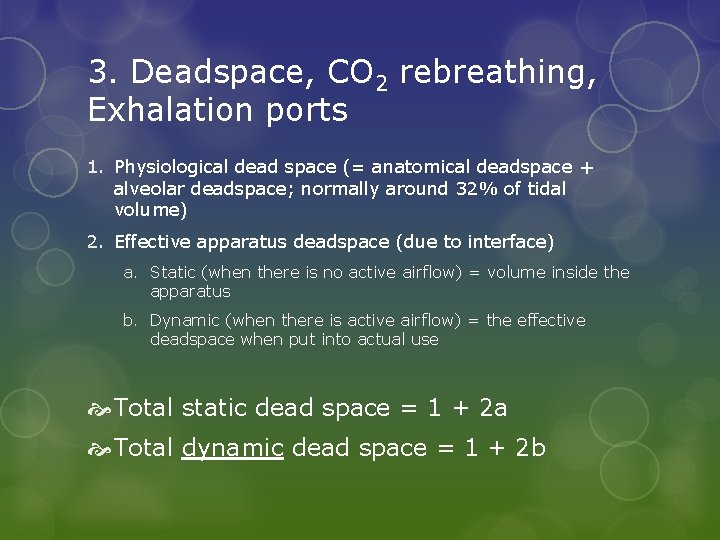
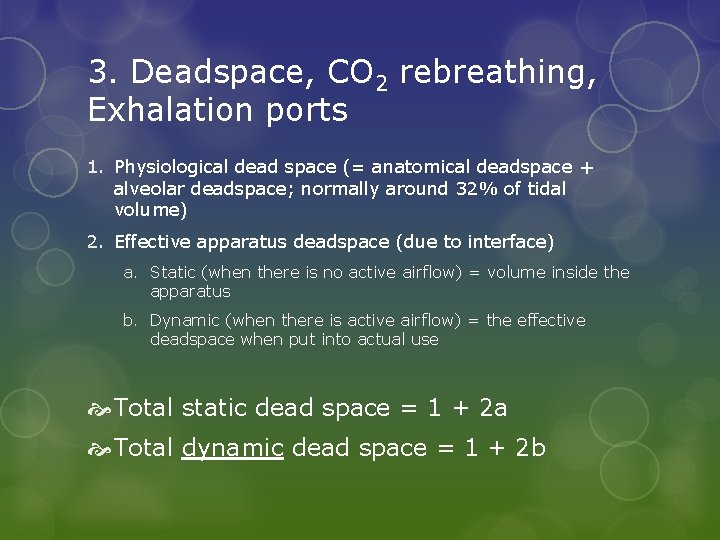
3. Deadspace, CO 2 rebreathing, Exhalation ports 1. Physiological dead space (= anatomical deadspace + alveolar deadspace; normally around 32% of tidal volume) 2. Effective apparatus deadspace (due to interface) a. Static (when there is no active airflow) = volume inside the apparatus b. Dynamic (when there is active airflow) = the effective deadspace when put into actual use Total static dead space = 1 + 2 a Total dynamic dead space = 1 + 2 b
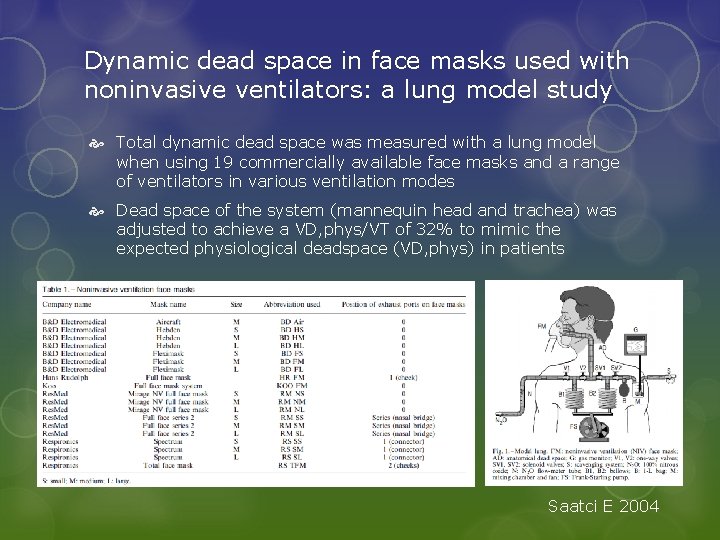
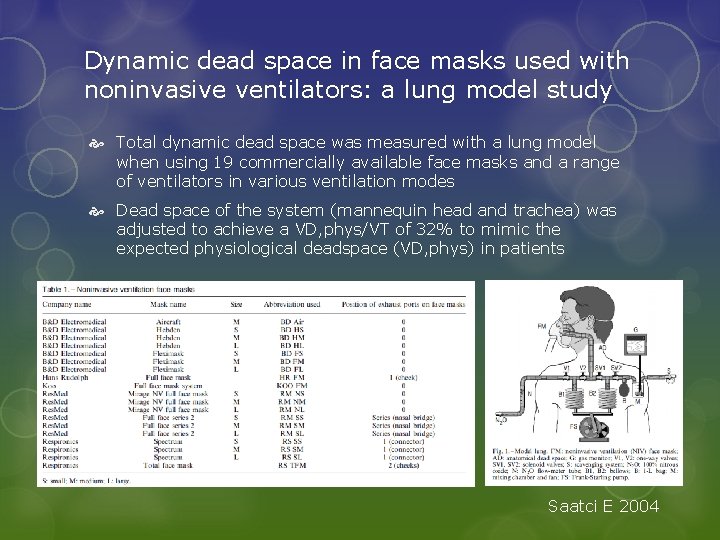
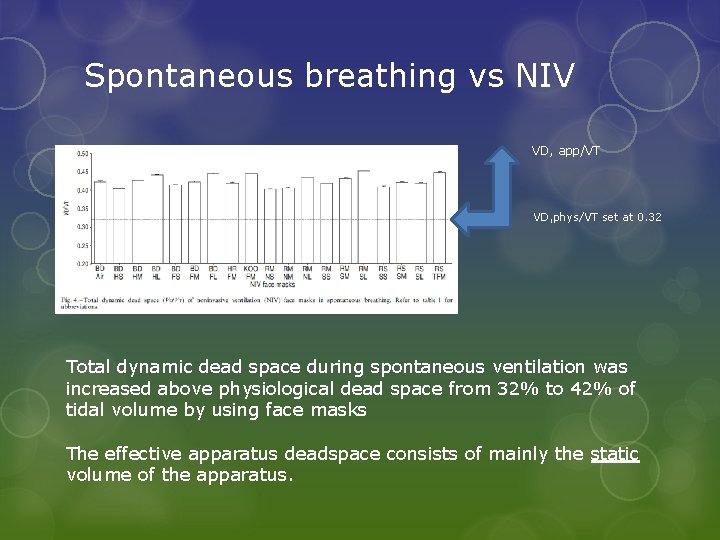
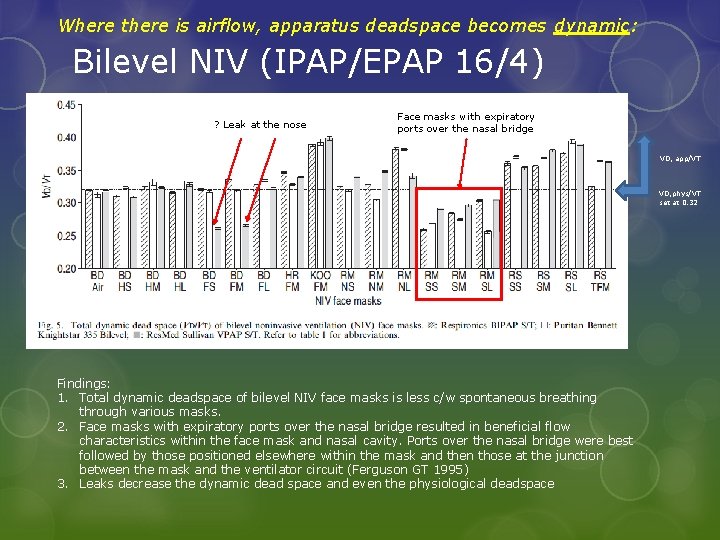
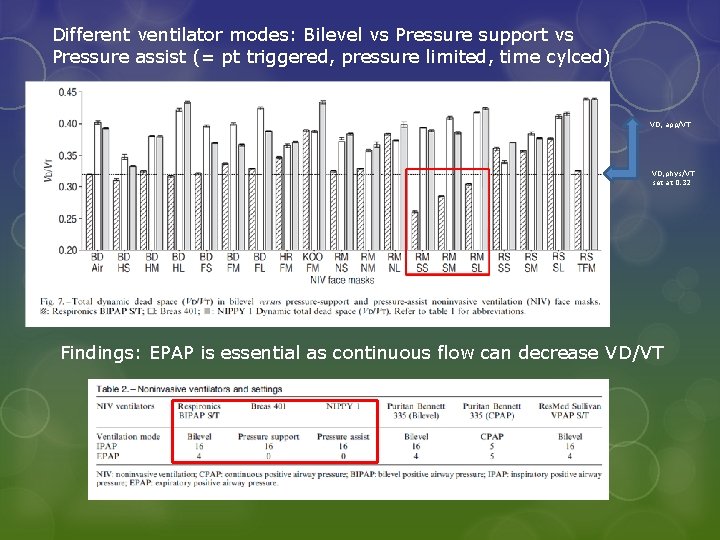
Dynamic dead space in face masks used with noninvasive ventilators: a lung model study Total dynamic dead space was measured with a lung model when using 19 commercially available face masks and a range of ventilators in various ventilation modes Dead space of the system (mannequin head and trachea) was adjusted to achieve a VD, phys/VT of 32% to mimic the expected physiological deadspace (VD, phys) in patients Saatci E 2004
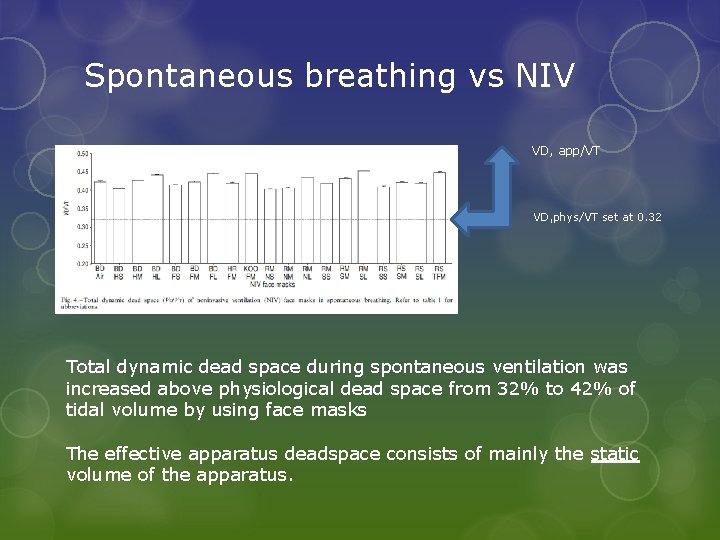
Spontaneous breathing vs NIV VD, app/VT VD, phys/VT set at 0. 32 Total dynamic dead space during spontaneous ventilation was increased above physiological dead space from 32% to 42% of tidal volume by using face masks The effective apparatus deadspace consists of mainly the static volume of the apparatus.
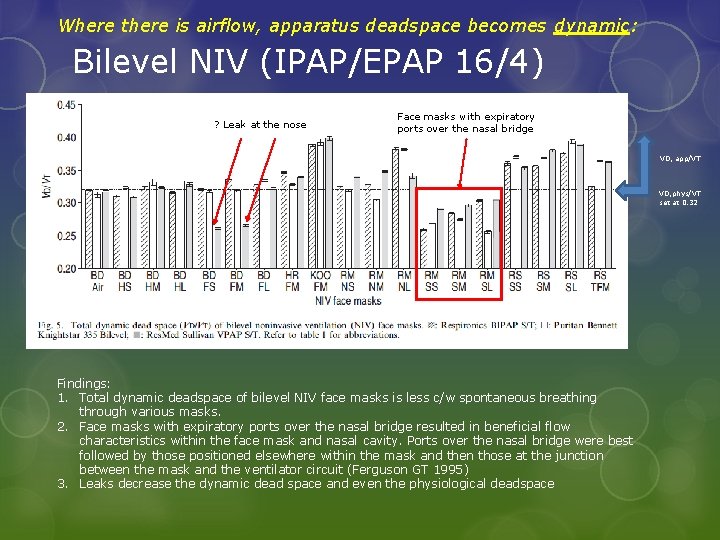
Where there is airflow, apparatus deadspace becomes dynamic: Bilevel NIV (IPAP/EPAP 16/4) ? Leak at the nose Face masks with expiratory ports over the nasal bridge VD, app/VT VD, phys/VT set at 0. 32 Findings: 1. Total dynamic deadspace of bilevel NIV face masks is less c/w spontaneous breathing through various masks. 2. Face masks with expiratory ports over the nasal bridge resulted in beneficial flow characteristics within the face mask and nasal cavity. Ports over the nasal bridge were best followed by those positioned elsewhere within the mask and then those at the junction between the mask and the ventilator circuit (Ferguson GT 1995) 3. Leaks decrease the dynamic dead space and even the physiological deadspace

Ventilation modes: Bilevel vs CPAP Both modes give continuous flow during expiration VD, app/VT VD, phys/VT set at 0. 32 No important difference in VD/VT between Bilevel and CPAP in term of VD/VT
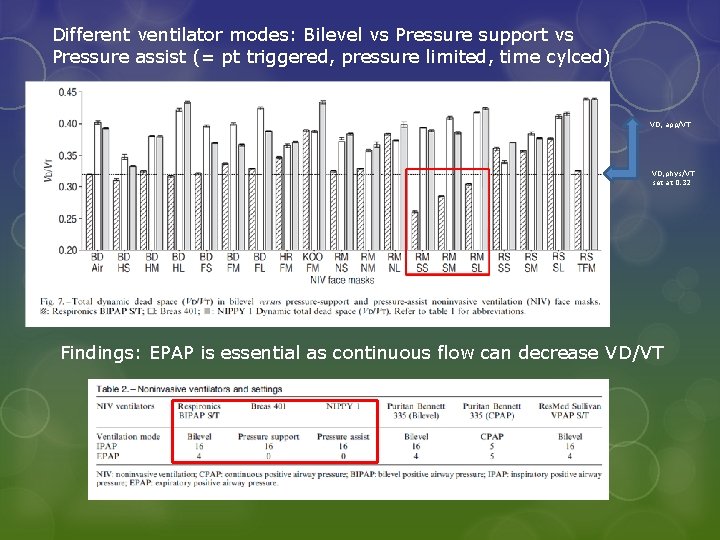
Different ventilator modes: Bilevel vs Pressure support vs Pressure assist (= pt triggered, pressure limited, time cylced) VD, app/VT VD, phys/VT set at 0. 32 Findings: EPAP is essential as continuous flow can decrease VD/VT
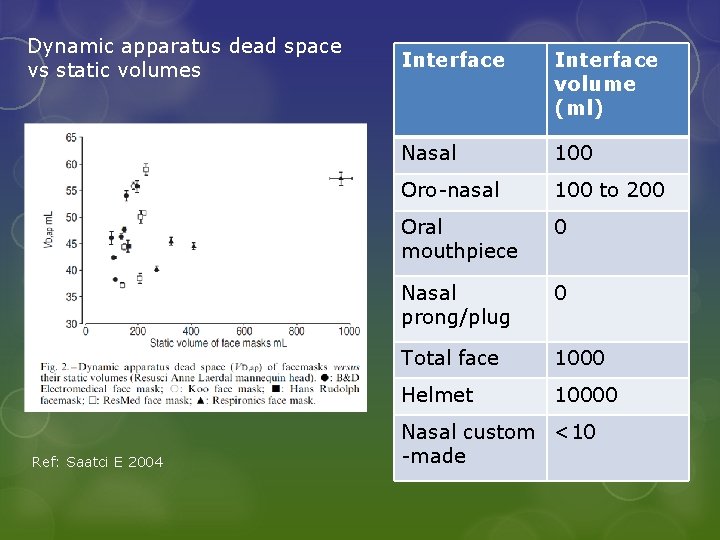
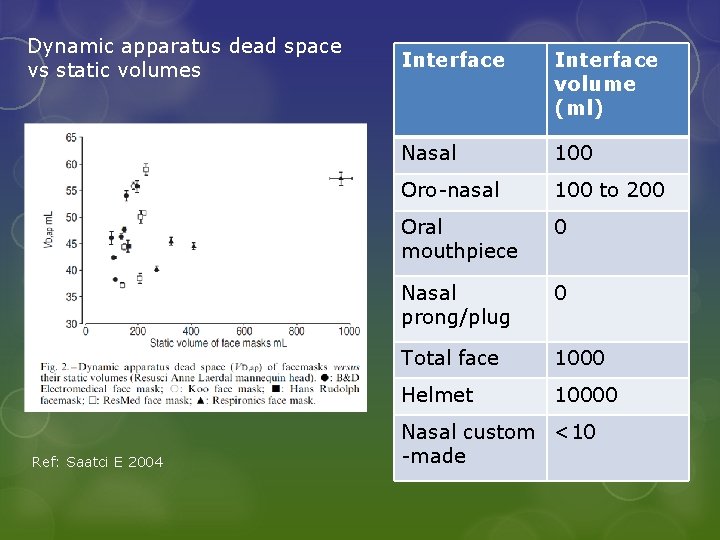
Dynamic apparatus dead space vs static volumes Ref: Saatci E 2004 Interface volume (ml) Nasal 100 Oro-nasal 100 to 200 Oral mouthpiece 0 Nasal prong/plug 0 Total face 1000 Helmet 10000 Nasal custom <10 -made
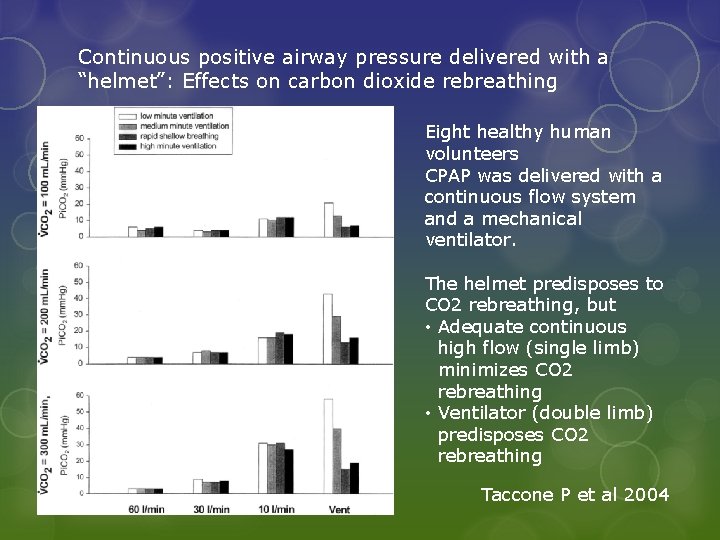
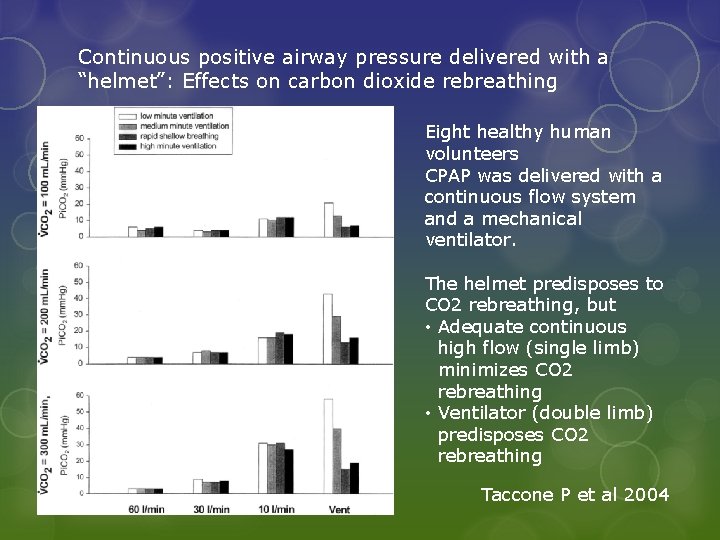
Continuous positive airway pressure delivered with a “helmet”: Effects on carbon dioxide rebreathing Eight healthy human volunteers CPAP was delivered with a continuous flow system and a mechanical ventilator. The helmet predisposes to CO 2 rebreathing, but • Adequate continuous high flow (single limb) minimizes CO 2 rebreathing • Ventilator (double limb) predisposes CO 2 rebreathing Taccone P et al 2004
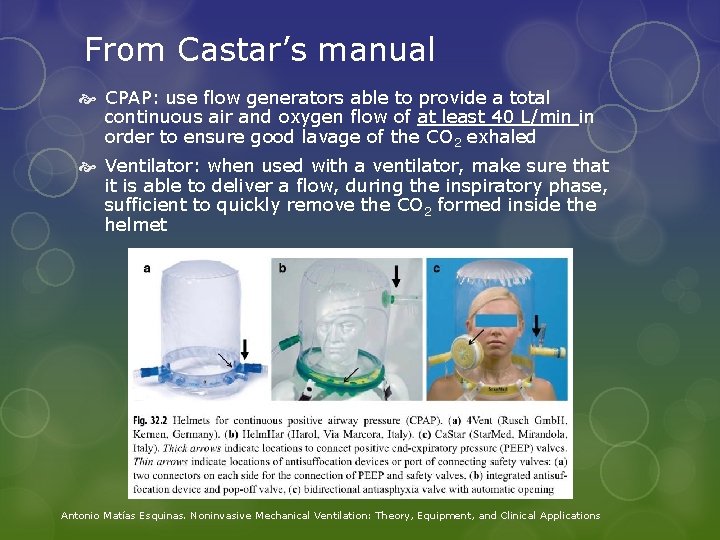
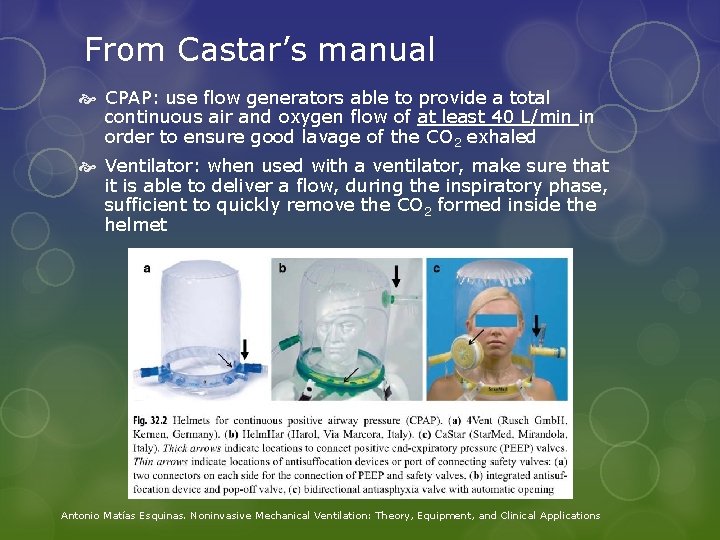
From Castar’s manual CPAP: use flow generators able to provide a total continuous air and oxygen flow of at least 40 L/min in order to ensure good lavage of the CO 2 exhaled Ventilator: when used with a ventilator, make sure that it is able to deliver a flow, during the inspiratory phase, sufficient to quickly remove the CO 2 formed inside the helmet Antonio Matías Esquinas. Noninvasive Mechanical Ventilation: Theory, Equipment, and Clinical Applications
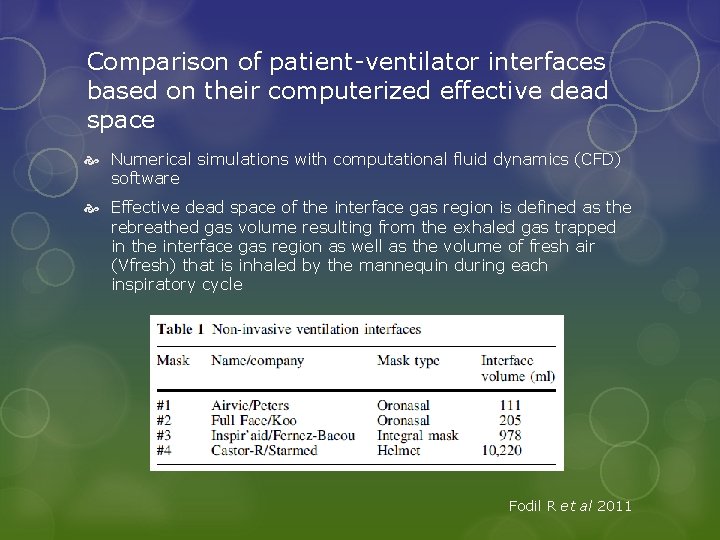
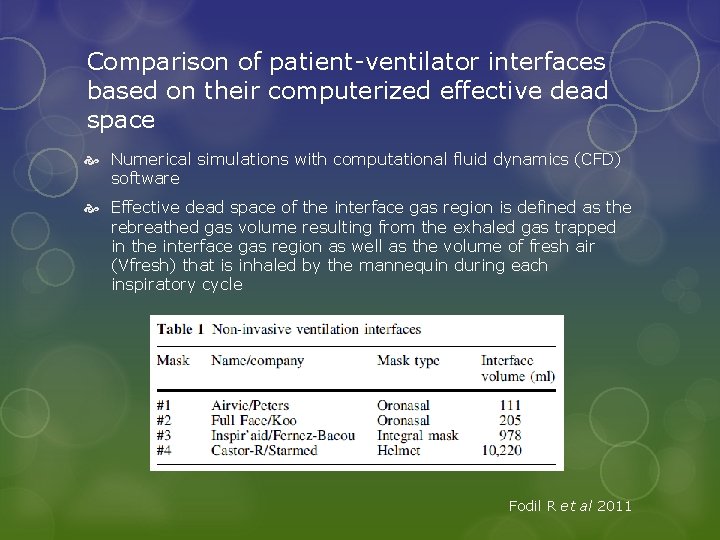
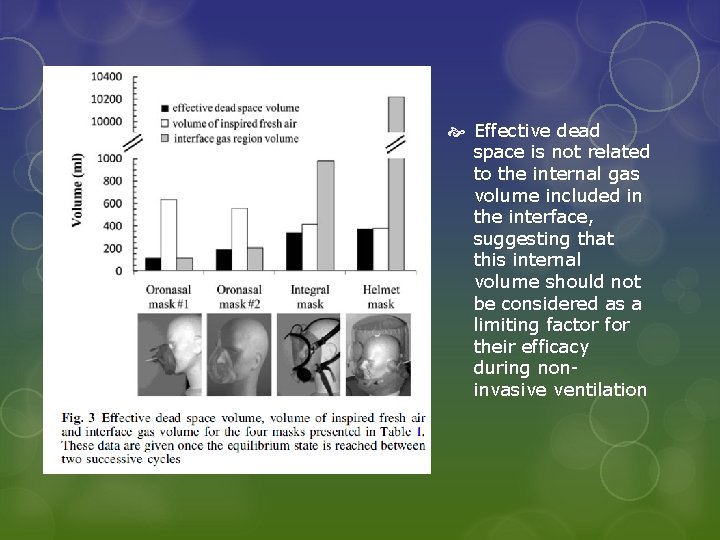
Comparison of patient-ventilator interfaces based on their computerized effective dead space Numerical simulations with computational fluid dynamics (CFD) software Effective dead space of the interface gas region is defined as the rebreathed gas volume resulting from the exhaled gas trapped in the interface gas region as well as the volume of fresh air (Vfresh) that is inhaled by the mannequin during each inspiratory cycle Fodil R et al 2011
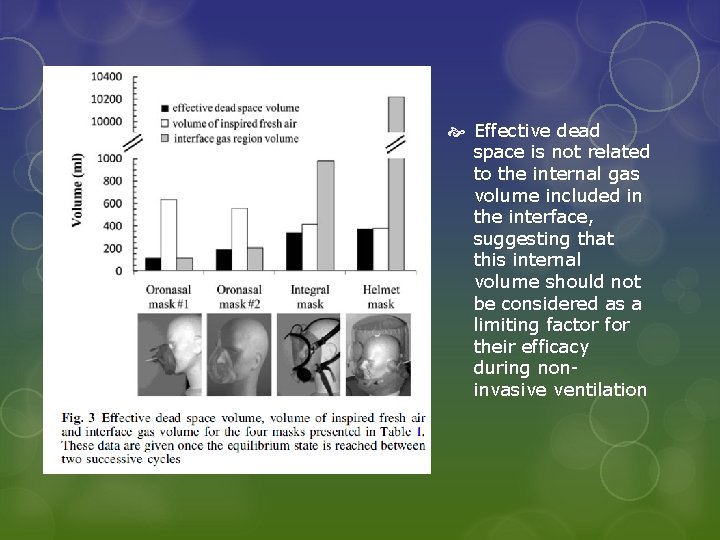
Effective dead space is not related to the internal gas volume included in the interface, suggesting that this internal volume should not be considered as a limiting factor for their efficacy during noninvasive ventilation
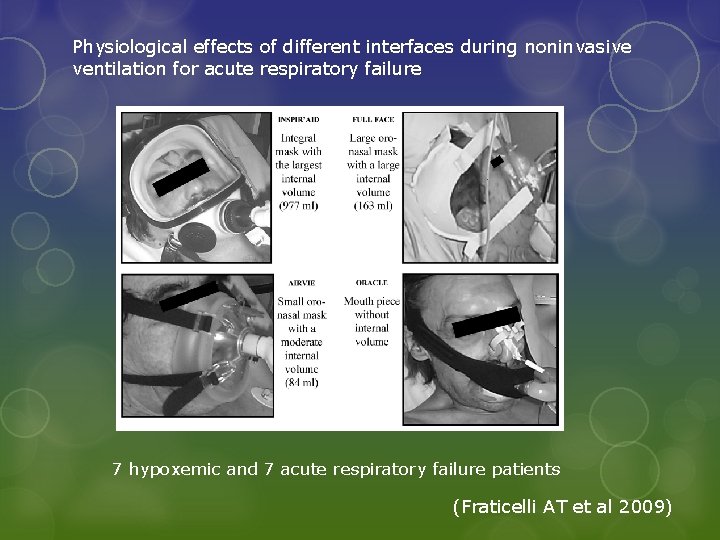
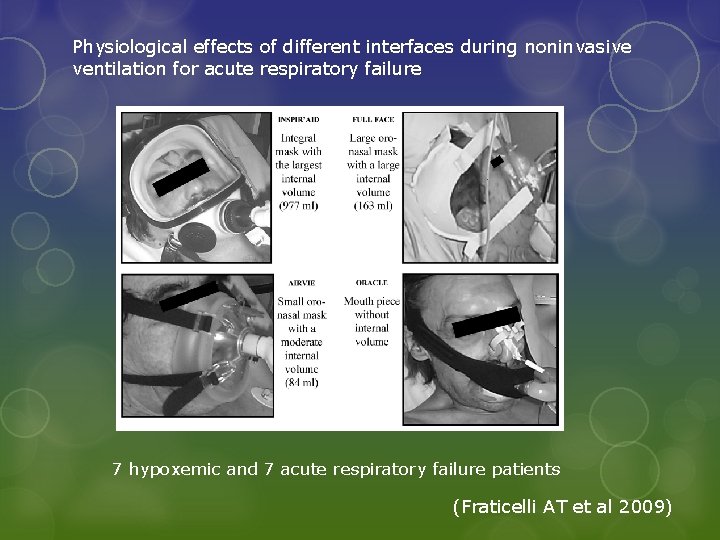
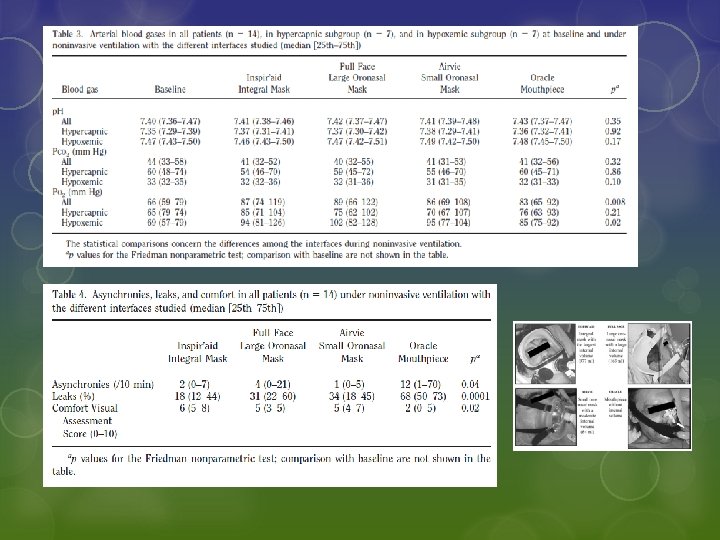
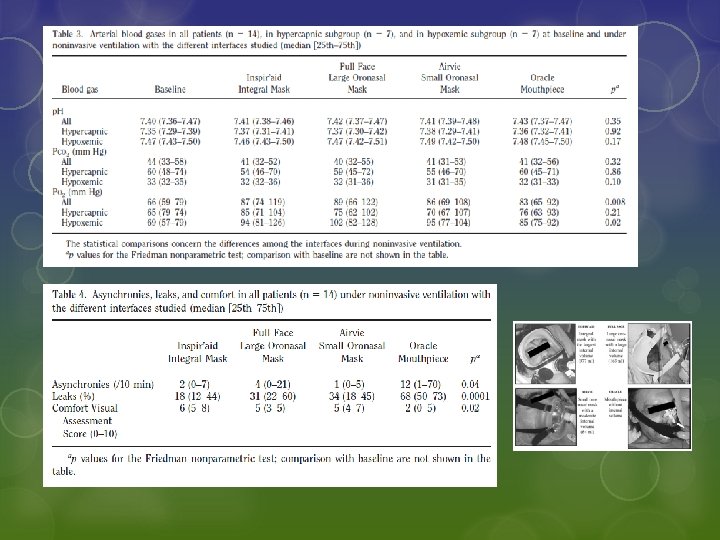
Physiological effects of different interfaces during noninvasive ventilation for acute respiratory failure 7 hypoxemic and 7 acute respiratory failure patients (Fraticelli AT et al 2009)
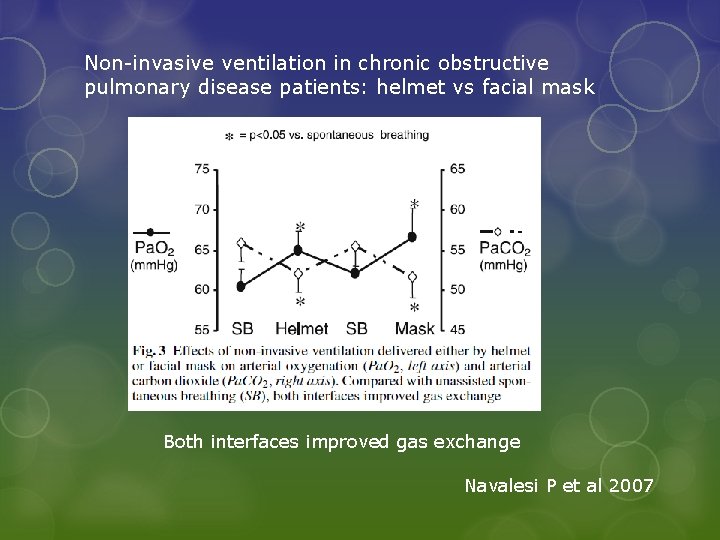
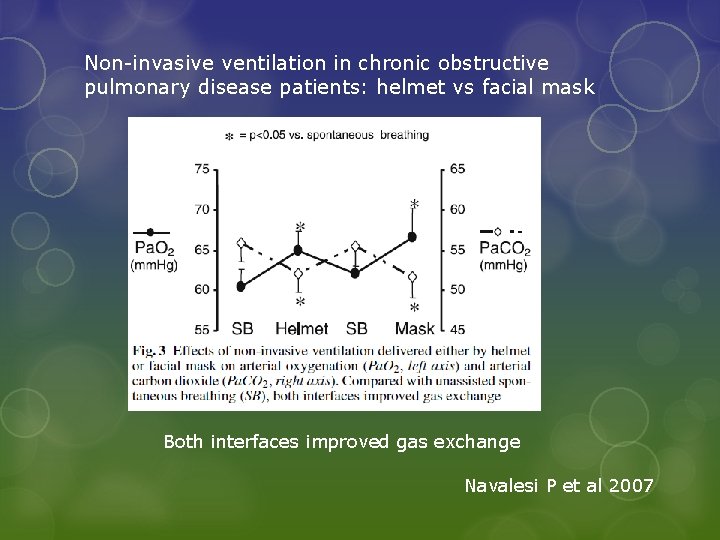
Non-invasive ventilation in chronic obstructive pulmonary disease patients: helmet vs facial mask Both interfaces improved gas exchange Navalesi P et al 2007
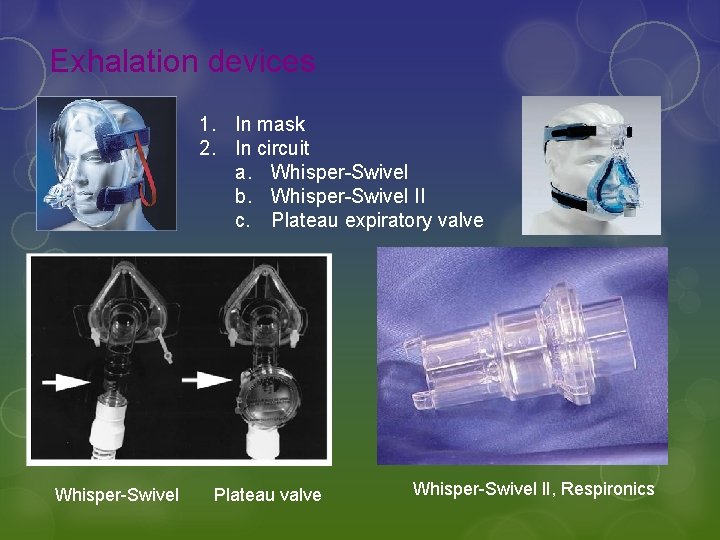
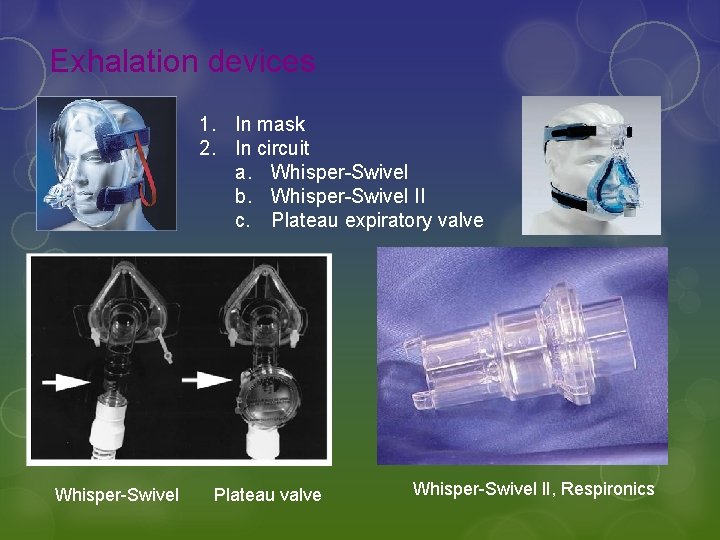
Exhalation devices 1. In mask 2. In circuit a. Whisper-Swivel b. Whisper-Swivel II c. Plateau expiratory valve Whisper-Swivel Plateau valve Whisper-Swivel II, Respironics
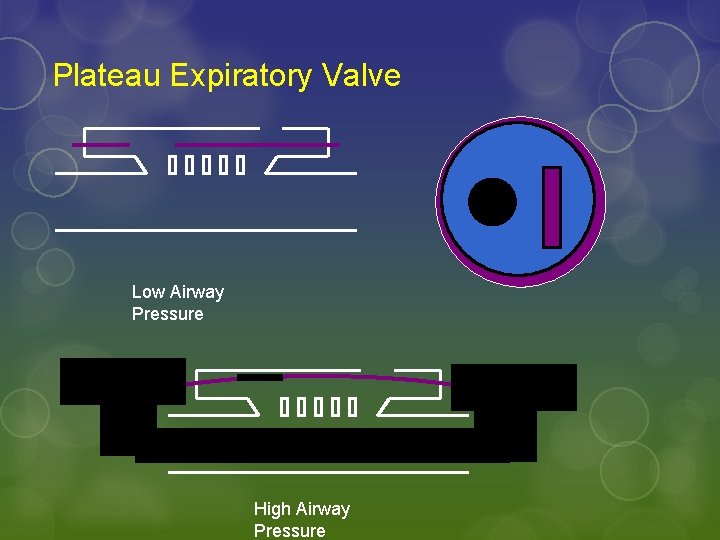
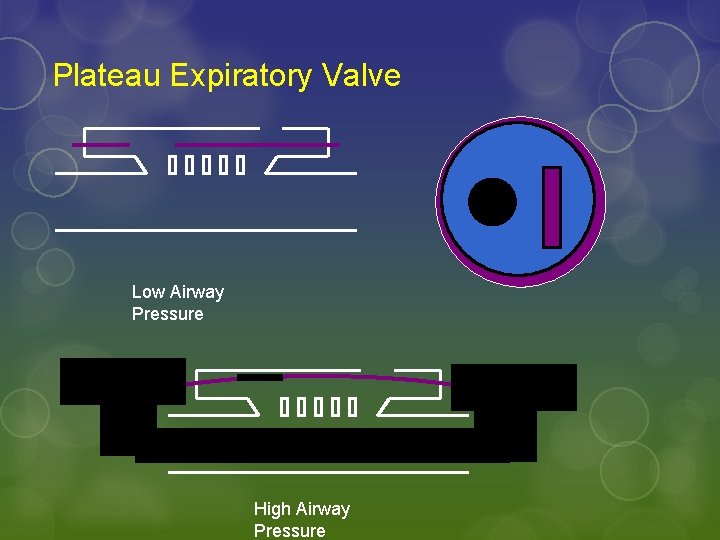
Plateau Expiratory Valve Low Airway Pressure High Airway Pressure
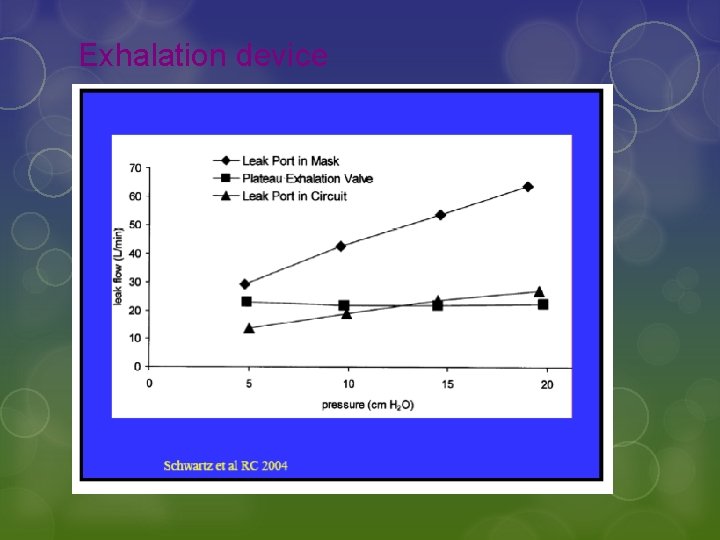
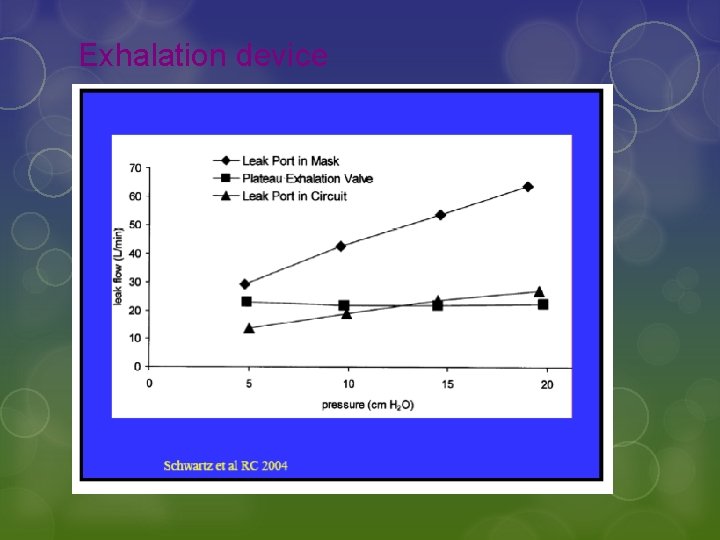
Exhalation device
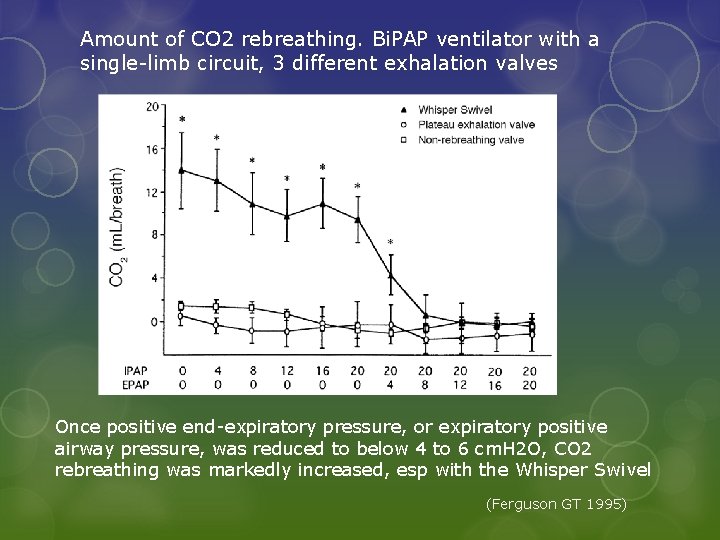
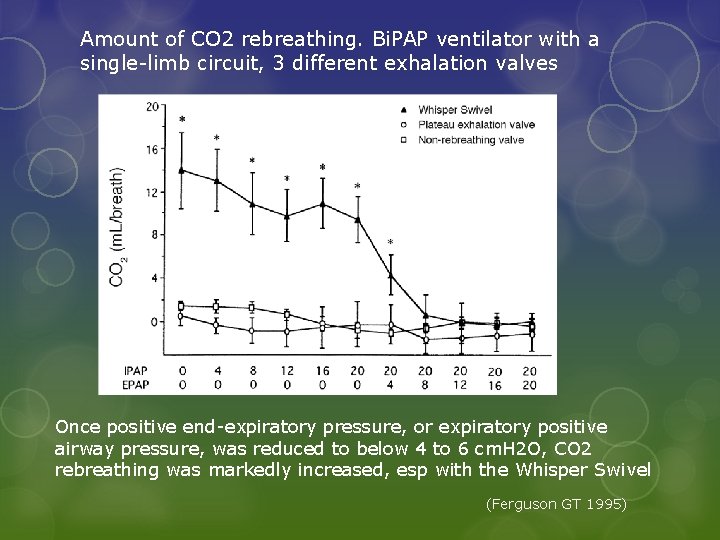
Amount of CO 2 rebreathing. Bi. PAP ventilator with a single-limb circuit, 3 different exhalation valves Once positive end-expiratory pressure, or expiratory positive airway pressure, was reduced to below 4 to 6 cm. H 2 O, CO 2 rebreathing was markedly increased, esp with the Whisper Swivel (Ferguson GT 1995)
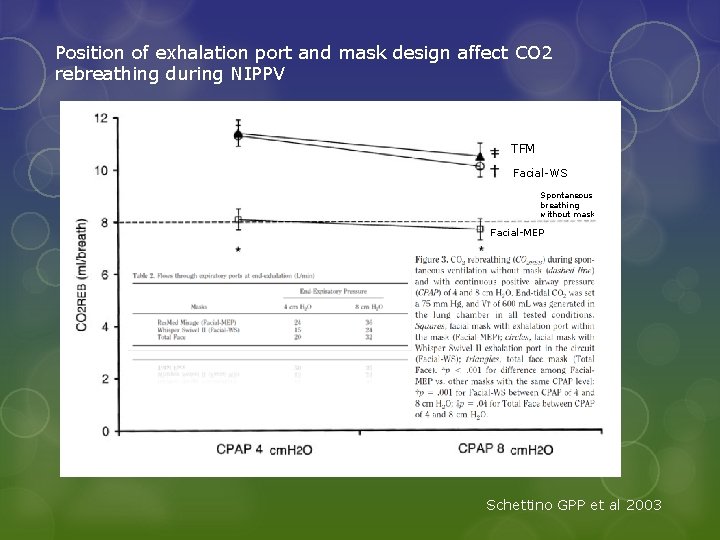
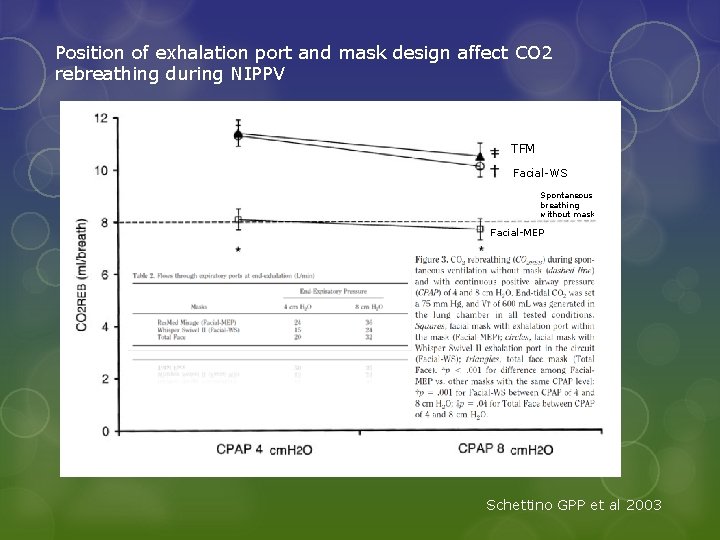
Position of exhalation port and mask design affect CO 2 rebreathing during NIPPV TFM Facial-WS Spontaneous breathing without mask Facial-MEP Schettino GPP et al 2003
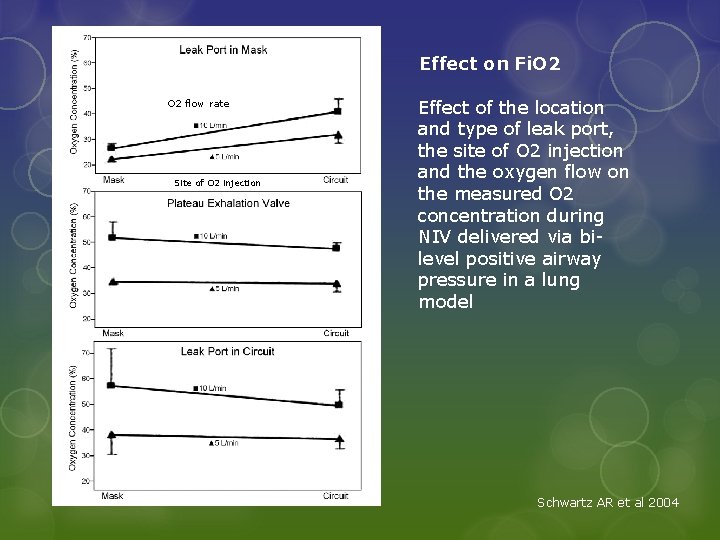
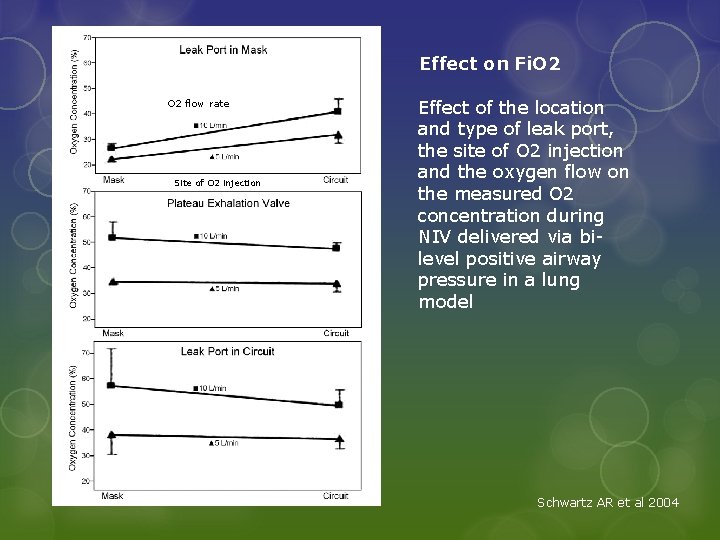
Effect on Fi. O 2 flow rate Site of O 2 injection Effect of the location and type of leak port, the site of O 2 injection and the oxygen flow on the measured O 2 concentration during NIV delivered via bilevel positive airway pressure in a lung model Schwartz AR et al 2004


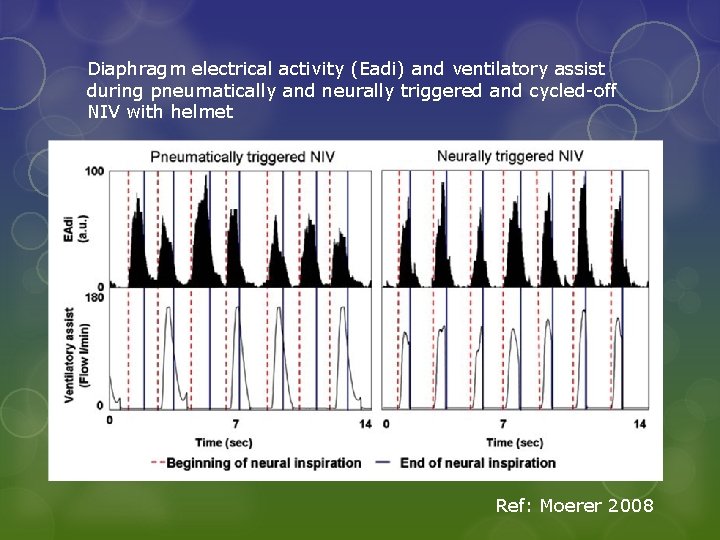
4. Patient-ventilator synchrony Helmet Navalesi Paolo et al 2007
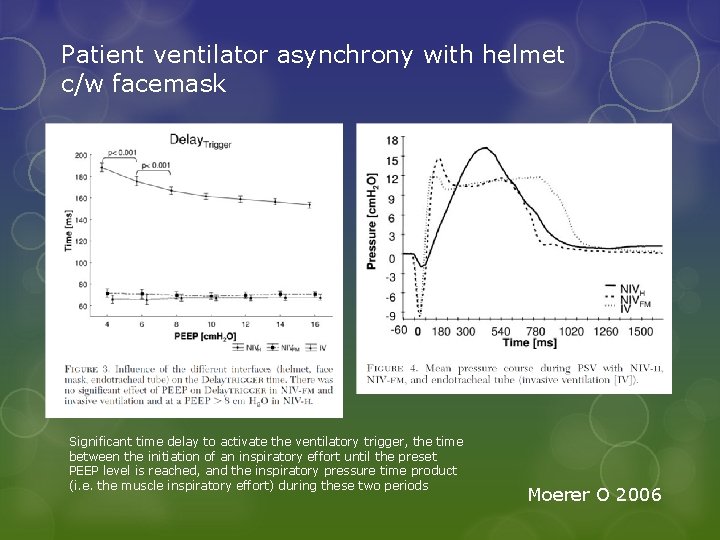
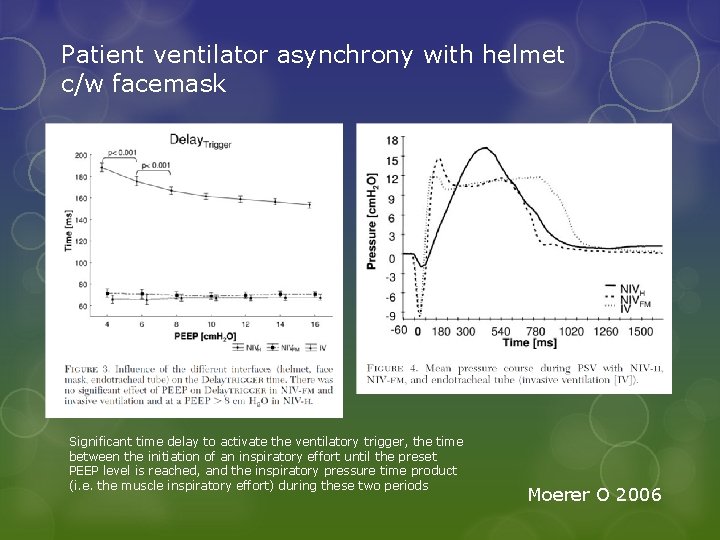
Patient ventilator asynchrony with helmet c/w facemask Significant time delay to activate the ventilatory trigger, the time between the initiation of an inspiratory effort until the preset PEEP level is reached, and the inspiratory pressure time product (i. e. the muscle inspiratory effort) during these two periods Moerer O 2006
Triggering and Cycling off With the helmet: the initial part of the inspiratory pressure applied was dissipated to pressurize its soft wall (Chiumello D 2003) Cycling off seems to occur in response to flow changes caused by the mechanical characteristics of the helmet rather than by the patient’s effort and mechanical characteristics (Rocca F 2005) Leading to patient ventilator asynchrony (Rocca F 2005, Navalesi P 2007)
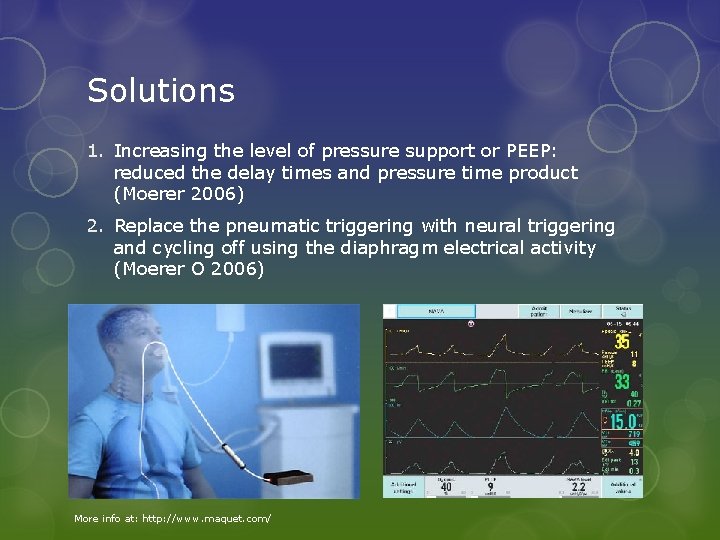
Solutions 1. Increasing the level of pressure support or PEEP: reduced the delay times and pressure time product (Moerer 2006) 2. Replace the pneumatic triggering with neural triggering and cycling off using the diaphragm electrical activity (Moerer O 2006) More info at: http: //www. maquet. com/
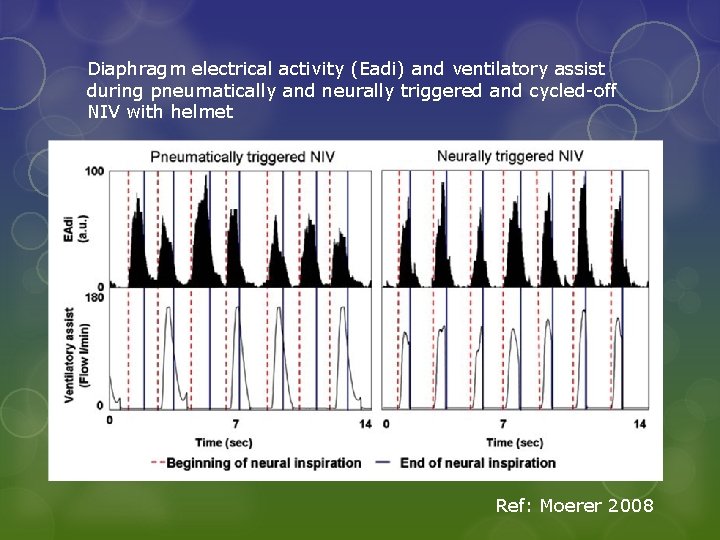
Diaphragm electrical activity (Eadi) and ventilatory assist during pneumatically and neurally triggered and cycled-off NIV with helmet Ref: Moerer 2008
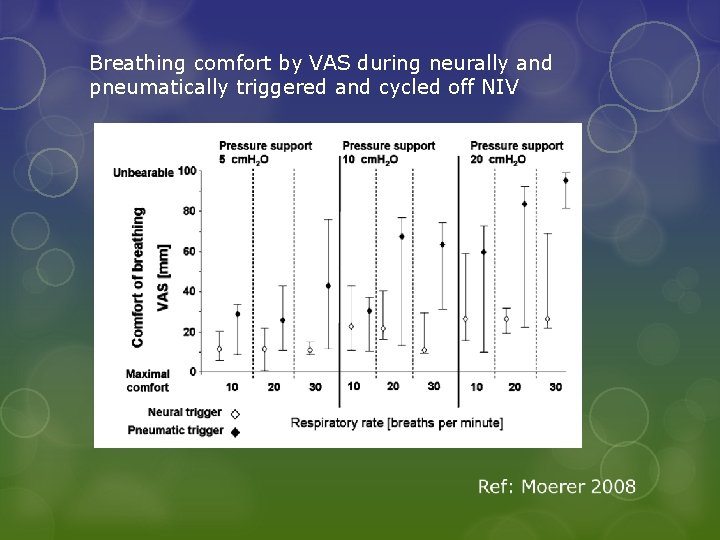
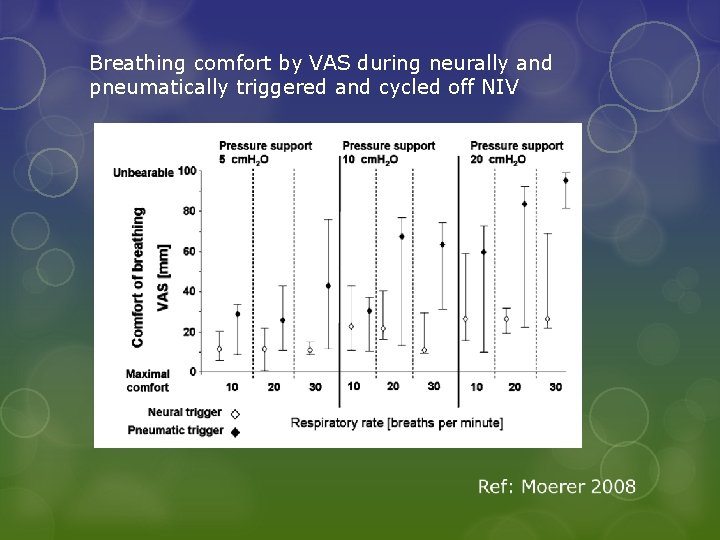
Breathing comfort by VAS during neurally and pneumatically triggered and cycled off NIV
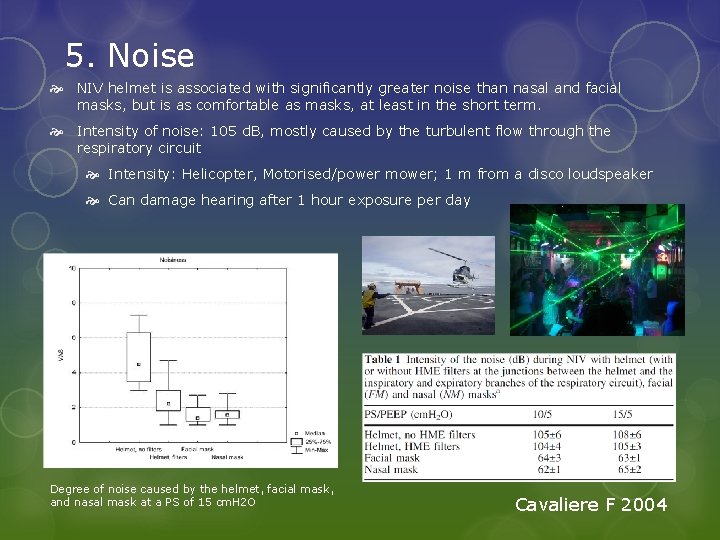
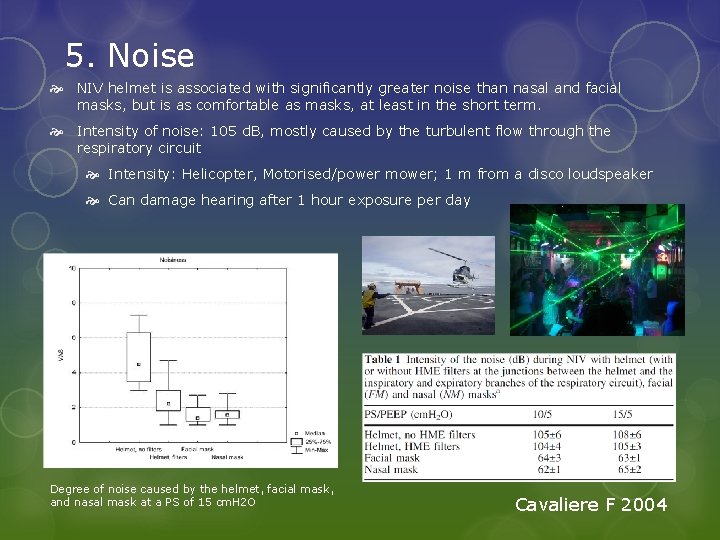
5. Noise NIV helmet is associated with significantly greater noise than nasal and facial masks, but is as comfortable as masks, at least in the short term. Intensity of noise: 105 d. B, mostly caused by the turbulent flow through the respiratory circuit Intensity: Helicopter, Motorised/power mower; 1 m from a disco loudspeaker Can damage hearing after 1 hour exposure per day Degree of noise caused by the helmet, facial mask, and nasal mask at a PS of 15 cm. H 2 O Cavaliere F 2004
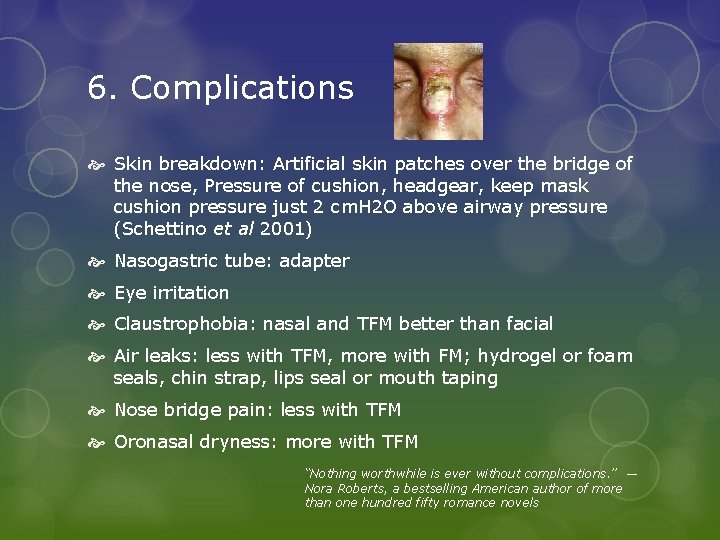
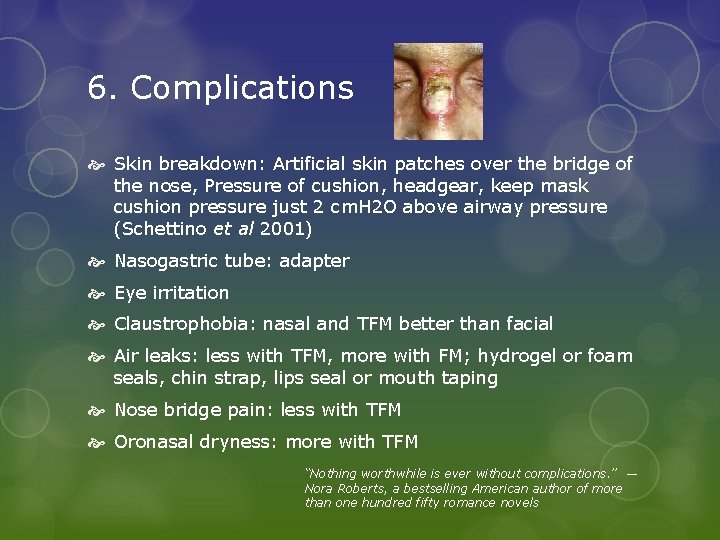
6. Complications Skin breakdown: Artificial skin patches over the bridge of the nose, Pressure of cushion, headgear, keep mask cushion pressure just 2 cm. H 2 O above airway pressure (Schettino et al 2001) Nasogastric tube: adapter Eye irritation Claustrophobia: nasal and TFM better than facial Air leaks: less with TFM, more with FM; hydrogel or foam seals, chin strap, lips seal or mouth taping Nose bridge pain: less with TFM Oronasal dryness: more with TFM “Nothing worthwhile is ever without complications. ” ― Nora Roberts, a bestselling American author of more than one hundred fifty romance novels
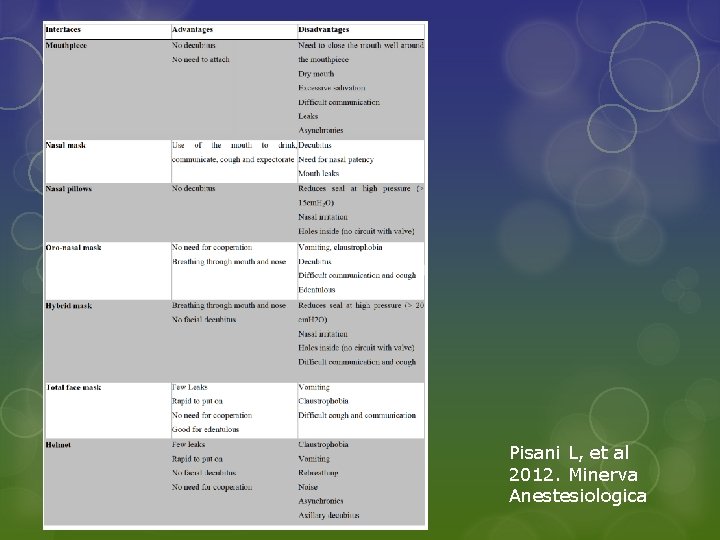
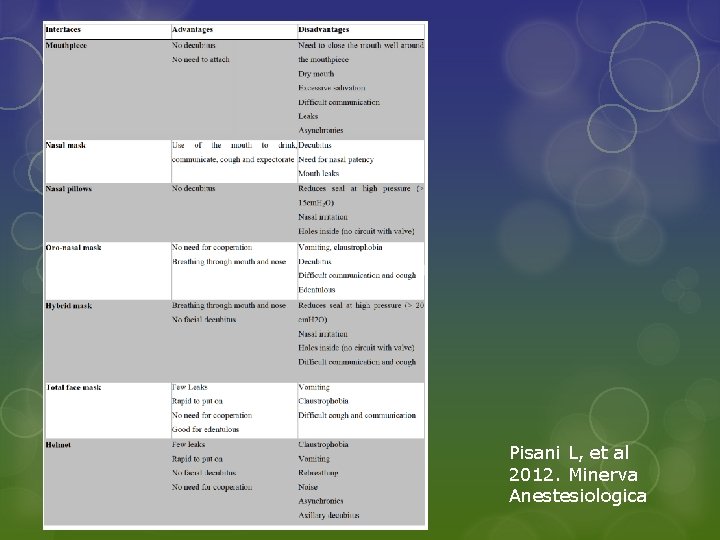
Pisani L, et al 2012. Minerva Anestesiologica
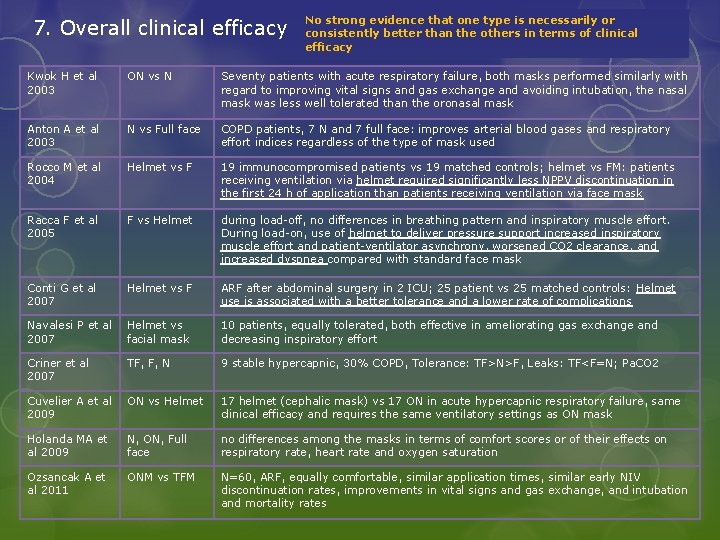
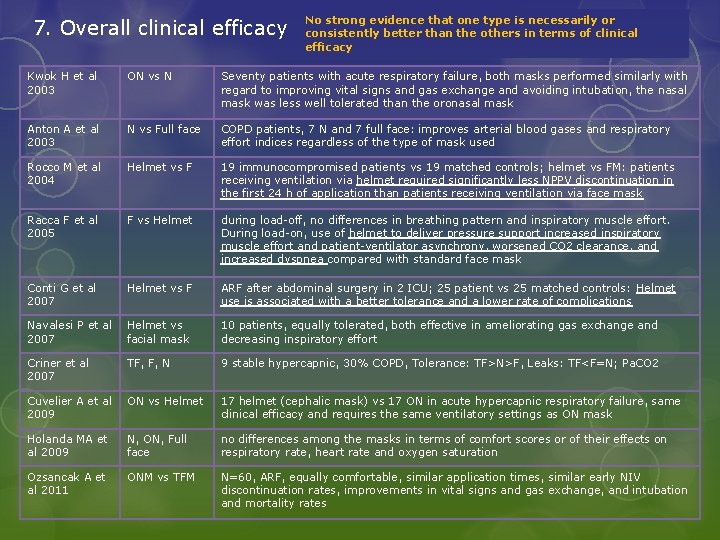
7. Overall clinical efficacy No strong evidence that one type is necessarily or consistently better than the others in terms of clinical efficacy Kwok H et al 2003 ON vs N Seventy patients with acute respiratory failure, both masks performed similarly with regard to improving vital signs and gas exchange and avoiding intubation, the nasal mask was less well tolerated than the oronasal mask Anton A et al 2003 N vs Full face COPD patients, 7 N and 7 full face: improves arterial blood gases and respiratory effort indices regardless of the type of mask used Rocco M et al 2004 Helmet vs F 19 immunocompromised patients vs 19 matched controls; helmet vs FM: patients receiving ventilation via helmet required significantly less NPPV discontinuation in the first 24 h of application than patients receiving ventilation via face mask Racca F et al 2005 F vs Helmet during load-off, no differences in breathing pattern and inspiratory muscle effort. During load-on, use of helmet to deliver pressure support increased inspiratory muscle effort and patient-ventilator asynchrony, worsened CO 2 clearance, and increased dyspnea compared with standard face mask Conti G et al 2007 Helmet vs F ARF after abdominal surgery in 2 ICU; 25 patient vs 25 matched controls: Helmet use is associated with a better tolerance and a lower rate of complications Navalesi P et al 2007 Helmet vs facial mask 10 patients, equally tolerated, both effective in ameliorating gas exchange and decreasing inspiratory effort Criner et al 2007 TF, F, N 9 stable hypercapnic, 30% COPD, Tolerance: TF>N>F, Leaks: TF<F=N; Pa. CO 2 Cuvelier A et al 2009 ON vs Helmet 17 helmet (cephalic mask) vs 17 ON in acute hypercapnic respiratory failure, same clinical efficacy and requires the same ventilatory settings as ON mask Holanda MA et al 2009 N, ON, Full face no differences among the masks in terms of comfort scores or of their effects on respiratory rate, heart rate and oxygen saturation Ozsancak A et al 2011 ONM vs TFM N=60, ARF, equally comfortable, similar application times, similar early NIV discontinuation rates, improvements in vital signs and gas exchange, and intubation and mortality rates
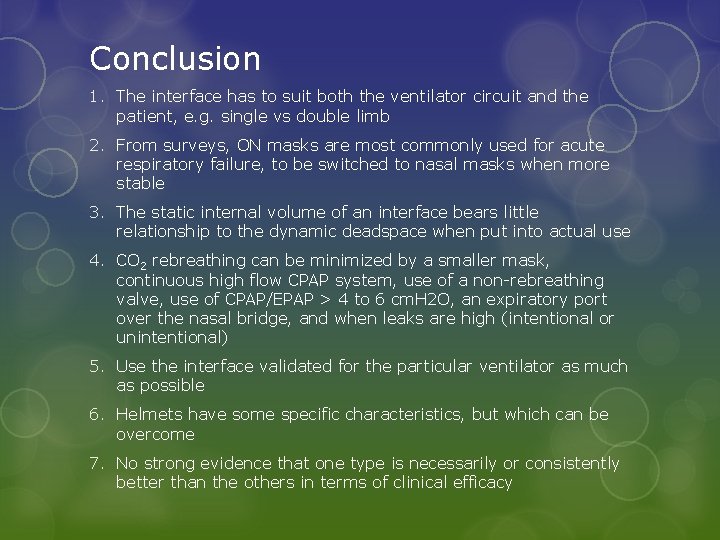
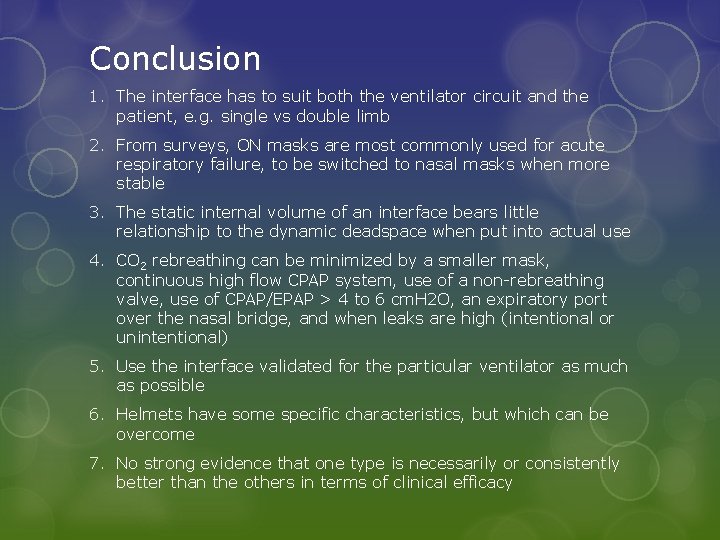
Conclusion 1. The interface has to suit both the ventilator circuit and the patient, e. g. single vs double limb 2. From surveys, ON masks are most commonly used for acute respiratory failure, to be switched to nasal masks when more stable 3. The static internal volume of an interface bears little relationship to the dynamic deadspace when put into actual use 4. CO 2 rebreathing can be minimized by a smaller mask, continuous high flow CPAP system, use of a non-rebreathing valve, use of CPAP/EPAP > 4 to 6 cm. H 2 O, an expiratory port over the nasal bridge, and when leaks are high (intentional or unintentional) 5. Use the interface validated for the particular ventilator as much as possible 6. Helmets have some specific characteristics, but which can be overcome 7. No strong evidence that one type is necessarily or consistently better than the others in terms of clinical efficacy
End Thank you!