Choices in the Treatment of Epilepsy What When


















- Slides: 66

Choices in the Treatment of Epilepsy: What, When, and Who? Juliann M Paolicchi, MA, MD Clinical Professor, Pediatrics Rutgers University Pediatric Epilepsy, Co-Director, Pediatric Clinical Research Northeastern Regional Epilepsy Group
Choices in the Treatment of Epilepsy: What, When, and Who? Epilepsy, especially when not responsive to medication, affects the patient’s and familes’ social life, peer interactions, educational and career decisions, driving ability, and reproductive life. Communication on treatment options based on discussion of patient’s treatment goals The challenge: Minimizing seizures and maximizing QOL Disclosures: -Speaker for Cyberonics, Lundbeck - Reseach: Esai, GW Pharmaceuticals
Choices in the Treatment of Epilepsy: What, When, and Who? What: are my options? Epilepsy, especially when not responsive to medication, affects the When: should I consider patient’s and familes’ social life, peer interactions, educational and these options? career decisions, driving ability, and reproductive life. Who are the best Communication on treatment options based on discussion of patient’s candidates for these treatment goals options? The challenge: Minimizing seizures and maximizing QOL Disclosures: -Speaker for Cyberonics, Lundbeck Reseach: Esai, GW Pharmaceuticals
Case Reviews Ü Case 1: The little jokester Ü Family wanted surgery Ü Case 2: The soccer goalie Ü Family wanted VNS

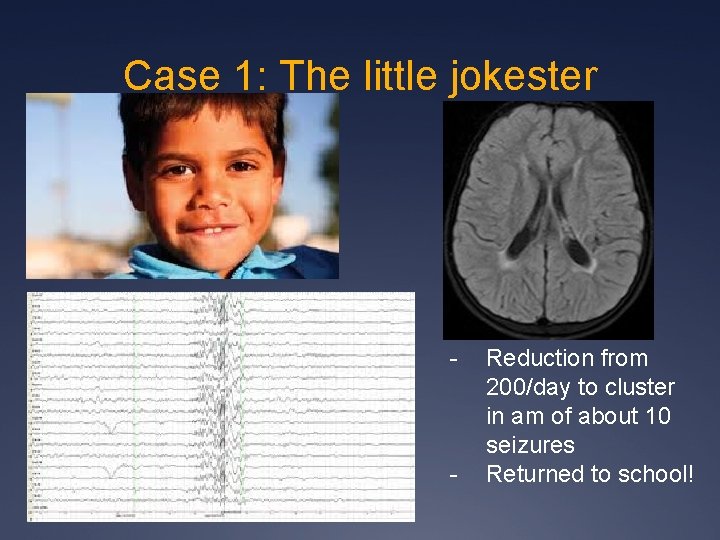
Case 1: The little Jokester 8 yo former premature boy with history of hypoxic injury at birth Right hemiparesis and expressive language deficit on exam Initially: ? 200 seizures/day = 1/10 min, 6/hour while awake
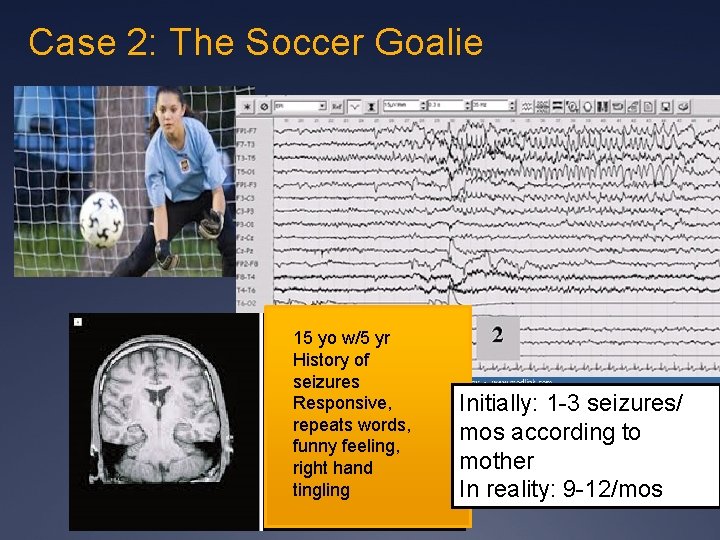
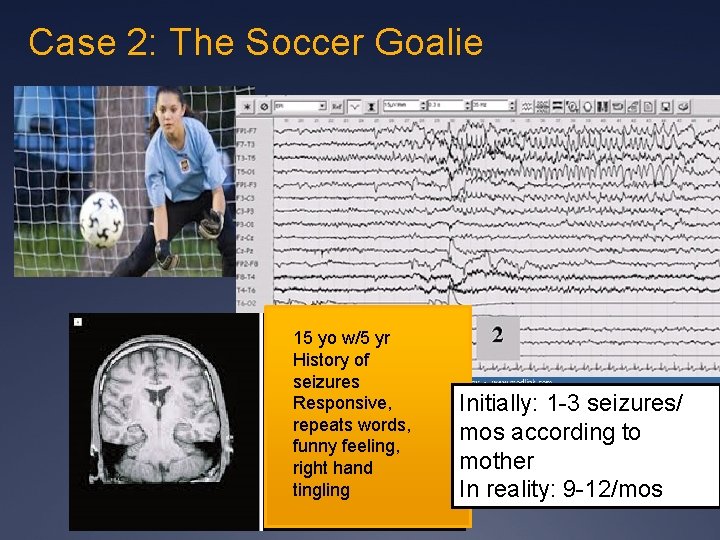
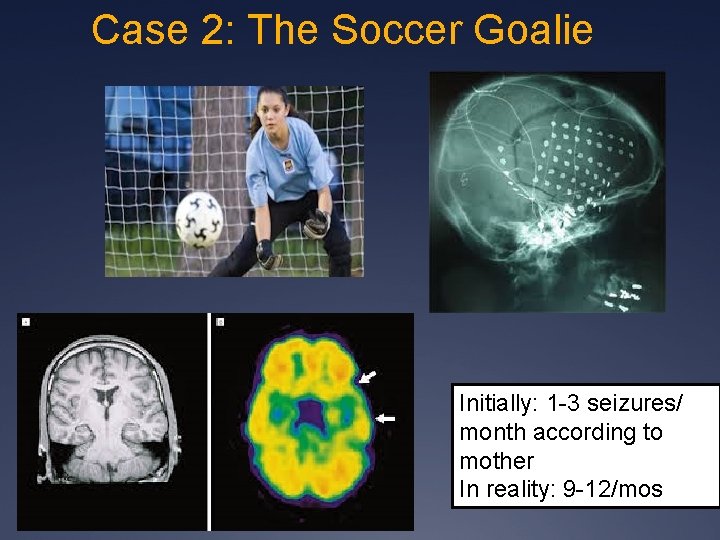
Case 2: The Soccer Goalie 15 yo w/5 yr History of seizures Responsive, repeats words, funny feeling, right hand tingling Initially: 1 -3 seizures/ mos according to mother In reality: 9 -12/mos
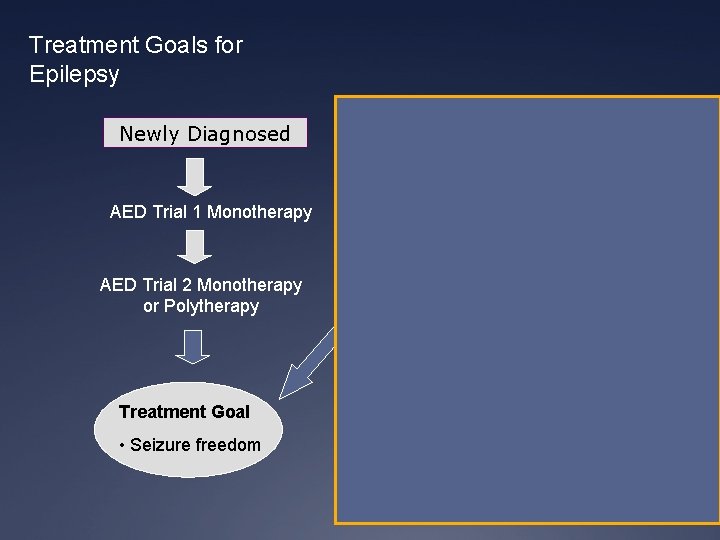
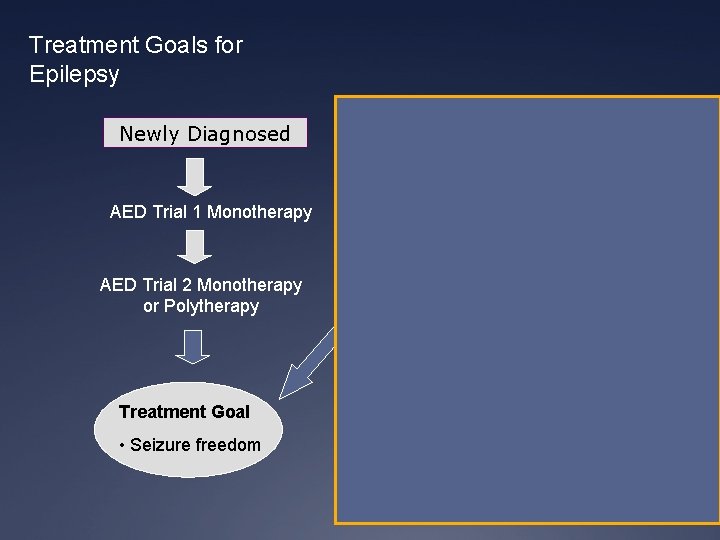
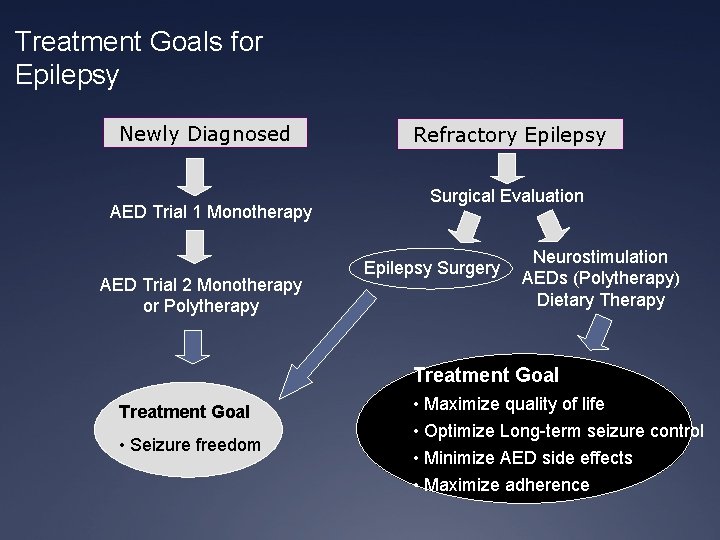
Treatment Goals for Epilepsy Newly Diagnosed AED Trial 1 Monotherapy AED Trial 2 Monotherapy or Polytherapy Refractory Epilepsy Surgical Evaluation Epilepsy Surgery VNS Therapy AEDs (Polytherapy) Ketogenic Diet Treatment Goal • Seizure freedom • Maximize quality of life • Optimize Long-term seizure control • Minimize AED side effects • Maximize adherence
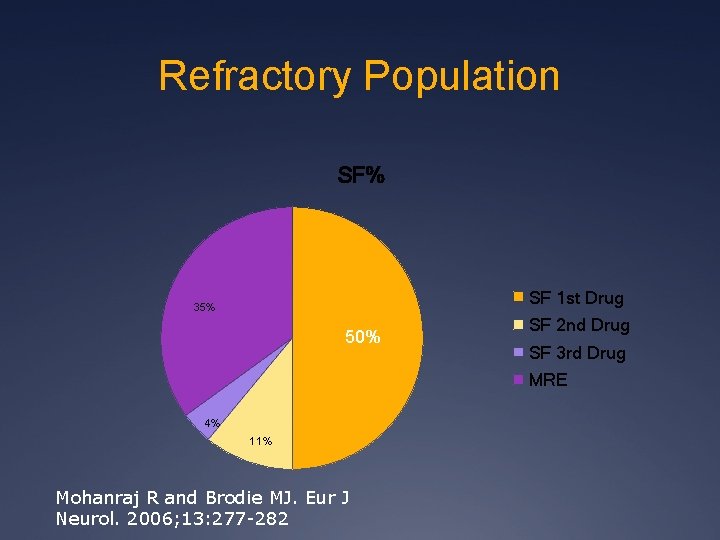
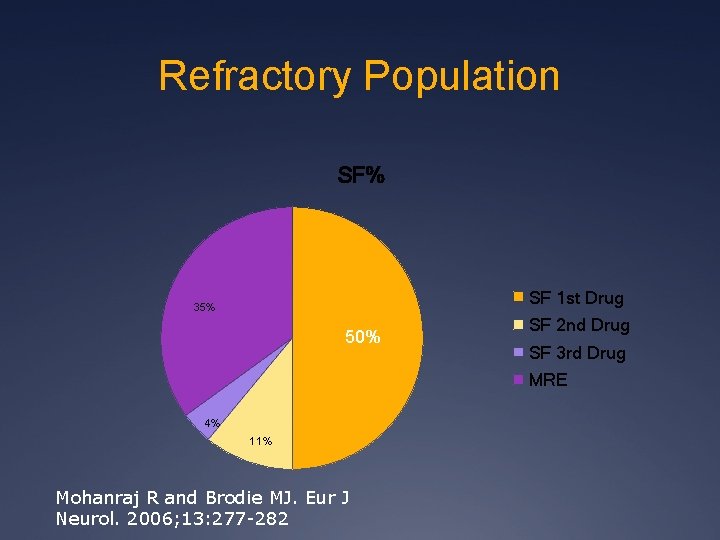
Refractory Population SF% SF 1 st Drug 35% 50% SF 2 nd Drug SF 3 rd Drug MRE 4% 11% Mohanraj R and Brodie MJ. Eur J Neurol. 2006; 13: 277 -282
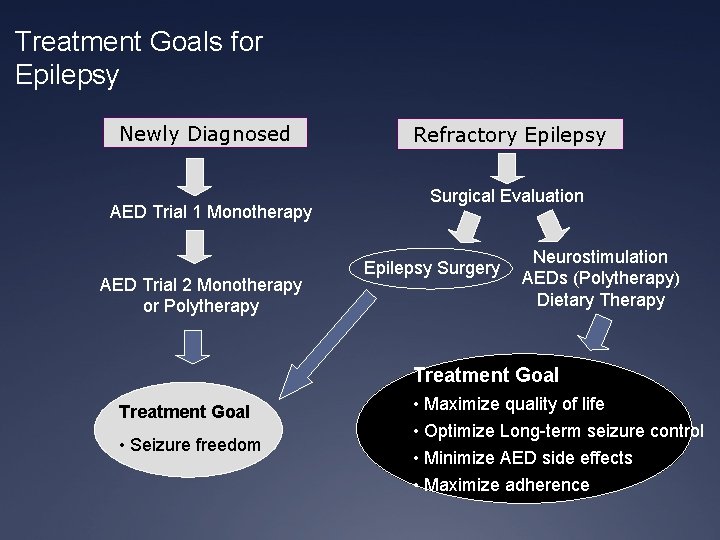
Treatment Goals for Epilepsy Newly Diagnosed AED Trial 1 Monotherapy AED Trial 2 Monotherapy or Polytherapy Refractory Epilepsy Surgical Evaluation Epilepsy Surgery Neurostimulation AEDs (Polytherapy) Dietary Therapy Treatment Goal • Seizure freedom • Maximize quality of life • Optimize Long-term seizure control • Minimize AED side effects • Maximize adherence
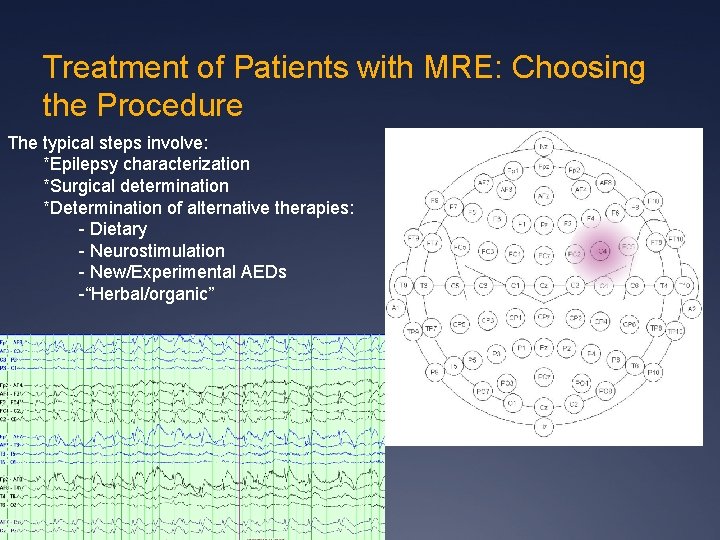
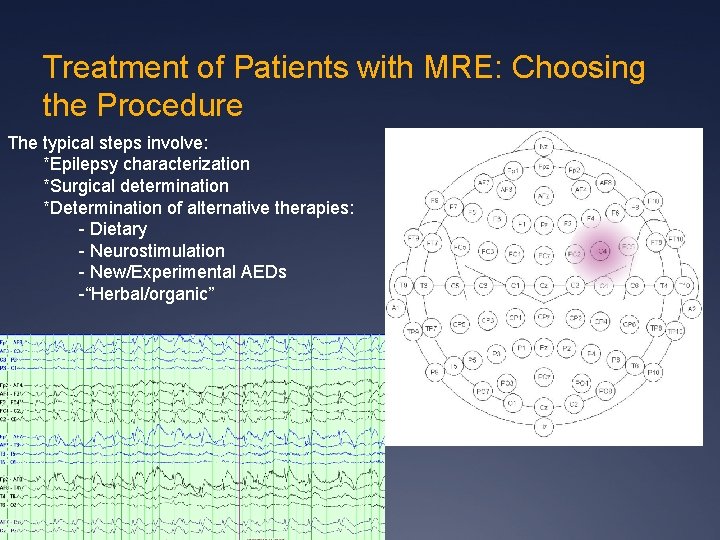
Treatment of Patients with MRE: Choosing the Procedure The typical steps involve: *Epilepsy characterization *Surgical determination *Determination of alternative therapies: - Dietary - Neurostimulation - New/Experimental AEDs -“Herbal/organic”
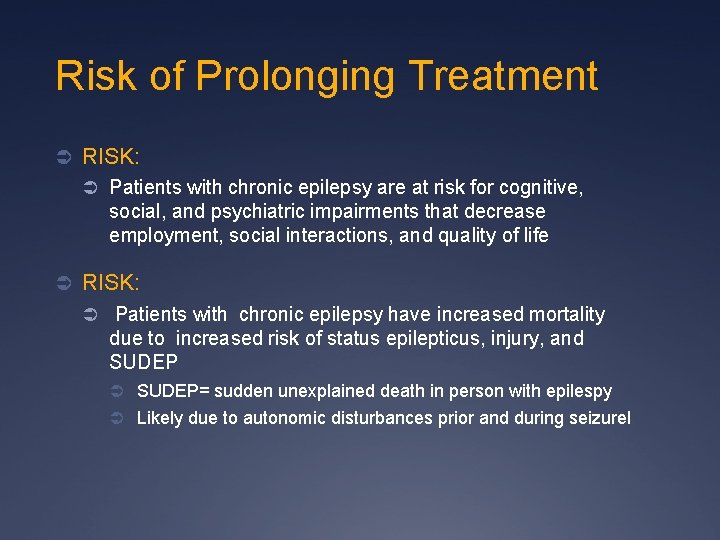
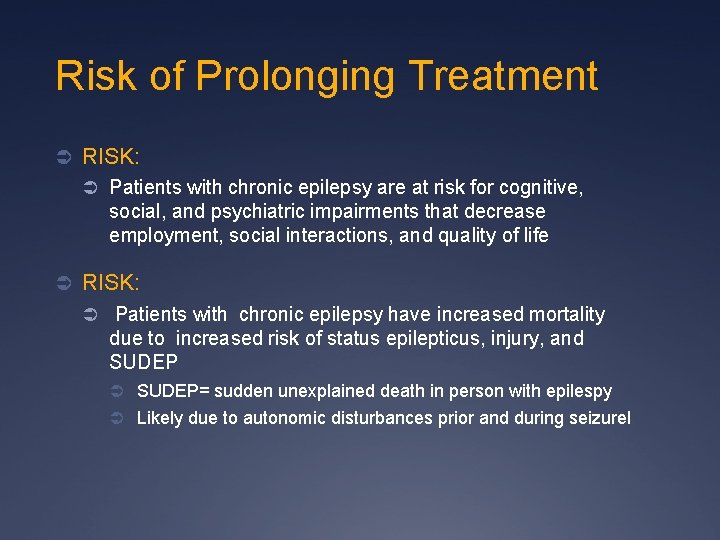
Risk of Prolonging Treatment Ü RISK: Ü Patients with chronic epilepsy are at risk for cognitive, social, and psychiatric impairments that decrease employment, social interactions, and quality of life Ü RISK: Ü Patients with chronic epilepsy have increased mortality due to increased risk of status epilepticus, injury, and SUDEP Ü SUDEP= sudden unexplained death in person with epilespy Ü Likely due to autonomic disturbances prior and during seizurel
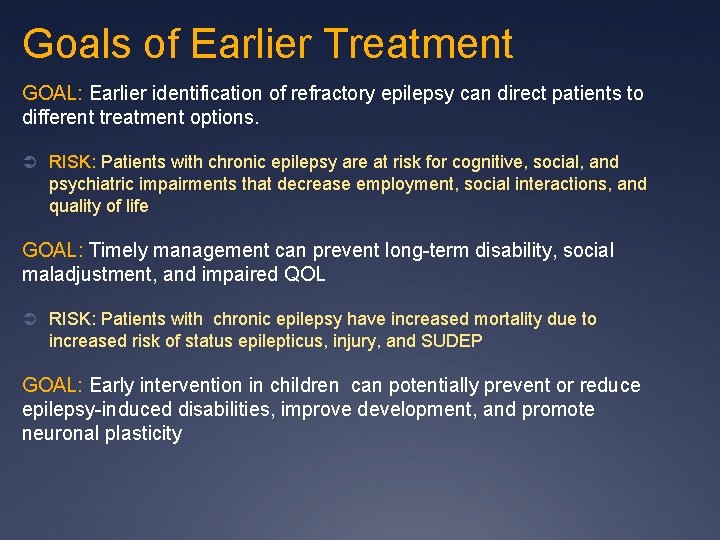
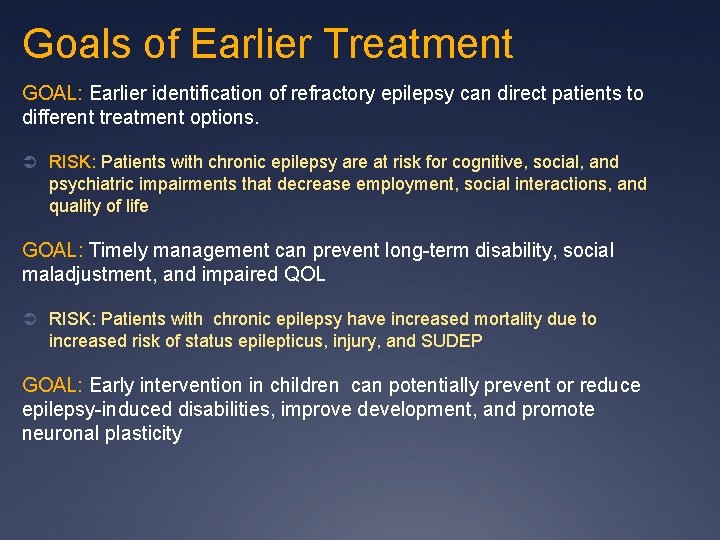
Goals of Earlier Treatment GOAL: Earlier identification of refractory epilepsy can direct patients to different treatment options. Ü RISK: Patients with chronic epilepsy are at risk for cognitive, social, and psychiatric impairments that decrease employment, social interactions, and quality of life GOAL: Timely management can prevent long-term disability, social maladjustment, and impaired QOL Ü RISK: Patients with chronic epilepsy have increased mortality due to increased risk of status epilepticus, injury, and SUDEP GOAL: Early intervention in children can potentially prevent or reduce epilepsy-induced disabilities, improve development, and promote neuronal plasticity

Overview Ü Approach to the MRE patient Ü New/Emerging and Experimental Therapies Ü New Anti-epileptic Agents Ü Old Meds/New Uses Ü Organic Medications, esp CBD, MMJ Ü Epilepsy surgery: review of types Ü Dietary therapies Ü Neurostimulation: Multiplel types: VNS, Neuropace, DBS
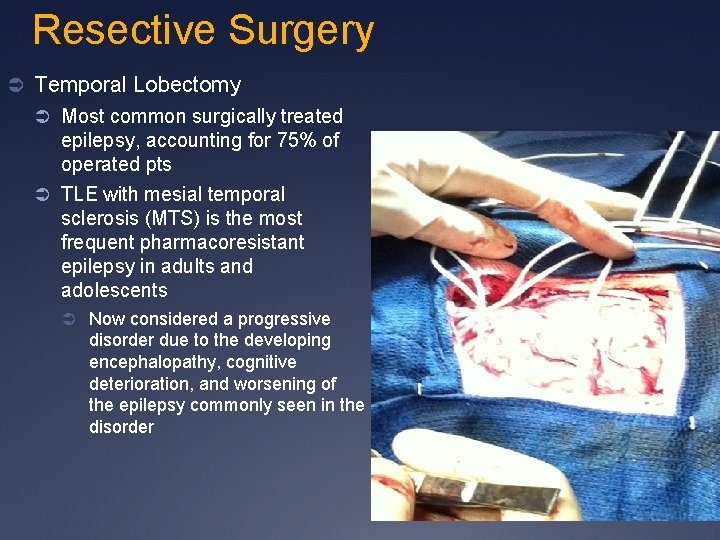
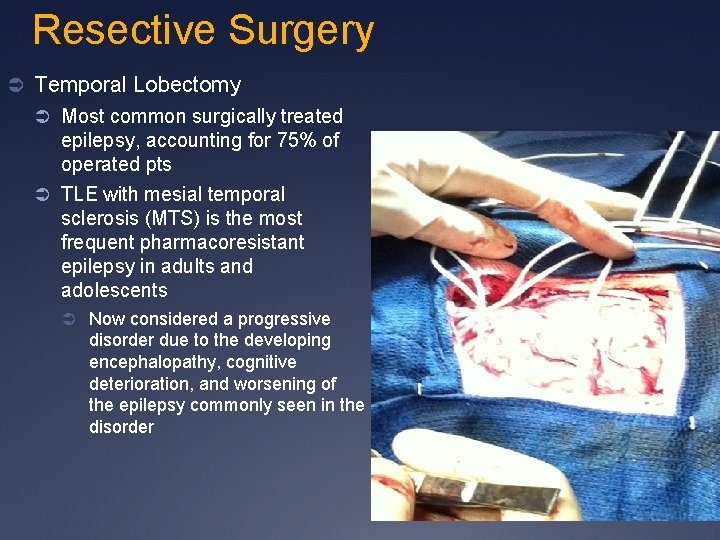
Resective Surgery Ü Temporal Lobectomy Ü Most common surgically treated epilepsy, accounting for 75% of operated pts Ü TLE with mesial temporal sclerosis (MTS) is the most frequent pharmacoresistant epilepsy in adults and adolescents Ü Now considered a progressive disorder due to the developing encephalopathy, cognitive deterioration, and worsening of the epilepsy commonly seen in the disorder

Resective Surgery: Temporal Lobectomy Ü For Diagnostic accuracy: Ü MRI: Ü Tumor: 98 – 100 % accurate Ü Hippocampal Sclerosis: 90 -97% accurate Ü Cortical dysplasia: 41 - 46% accurate Ü FDG-PET: 85% Ü Ictal SPECT: 85% Ü Interictal SPECT: 65% Ü MEG: 56%
Resective Surgery: Temporal Lobectomy Ü 1 st Randomized control trial of efficacy (Wiebe, et al, 2001 NEJM) Ü 80 pts with medically intractable TLE randomized to surgery vs continued medical therapy. Ü 58% surgical group SF ( seizurefree) vs 8% medical group (p < 0. 001). 83 Ü Surgical group: improved scores of QOL, employment rates, school attendance, decreased mortality

Temporal Lobecotomy Ü 1 st Randomized control trial of efficacy (Wiebe, et al, 2001 NEJM) Ü 80 pts with medically intractable TLE randomized to surgery vs continued medical therapy. Ü 58% surgical group SF ( seizure -free) vs 8% medical group (p < 0. 001). 83 Ü Surgical group: improved scores of QOL, employment rates, school attendance, decreased mortality Ü 2 nd Randomized control trail: ERST Trial( Engel et al, JAMA, 2012) Ü Randomized trial to early surgical intervention vs medical therapy after 2 years of epilepsy and 2 failed AEDs Ü Trial halted due to slow enrollment and early outcome data Ü 0/23 medical vs 11/15 surgical SF, 2 years outcome (p<0. 001, 95%CI)
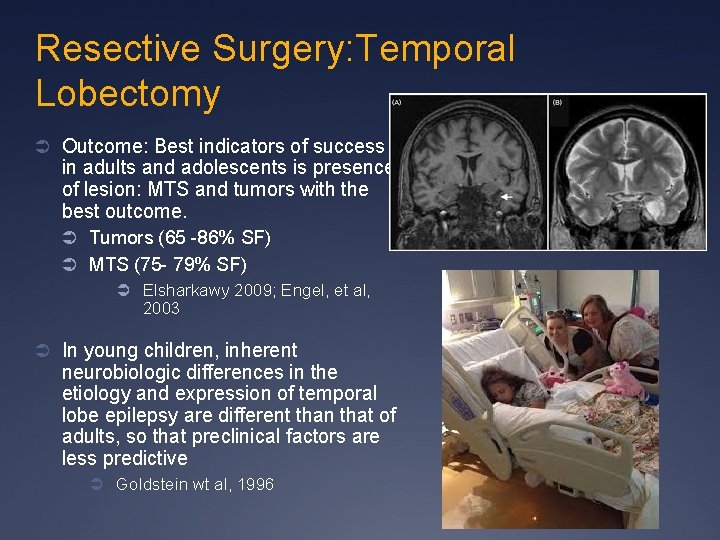
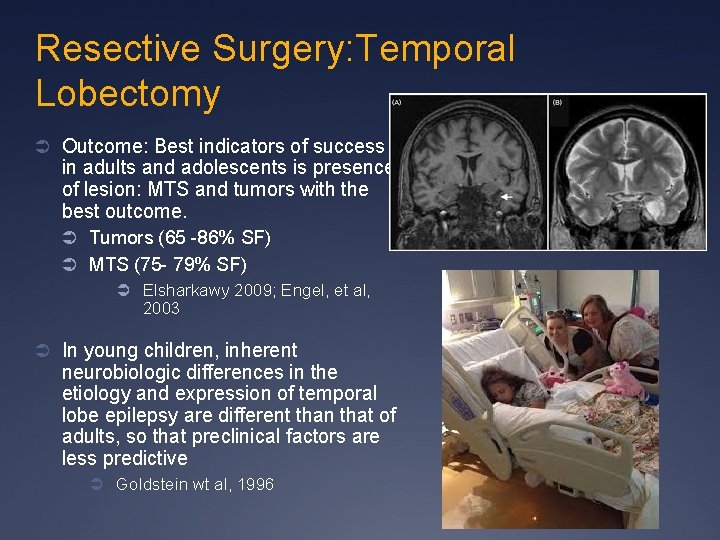
Resective Surgery: Temporal Lobectomy Ü Outcome: Best indicators of success in adults and adolescents is presence of lesion: MTS and tumors with the best outcome. Ü Tumors (65 -86% SF) Ü MTS (75 - 79% SF) Ü Elsharkawy 2009; Engel, et al, 2003 Ü In young children, inherent neurobiologic differences in the etiology and expression of temporal lobe epilepsy are different than that of adults, so that preclinical factors are less predictive Ü Goldstein wt al, 1996
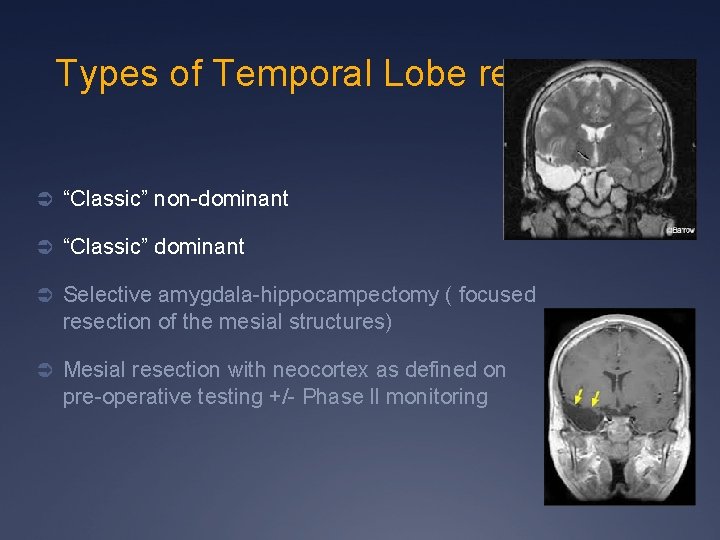
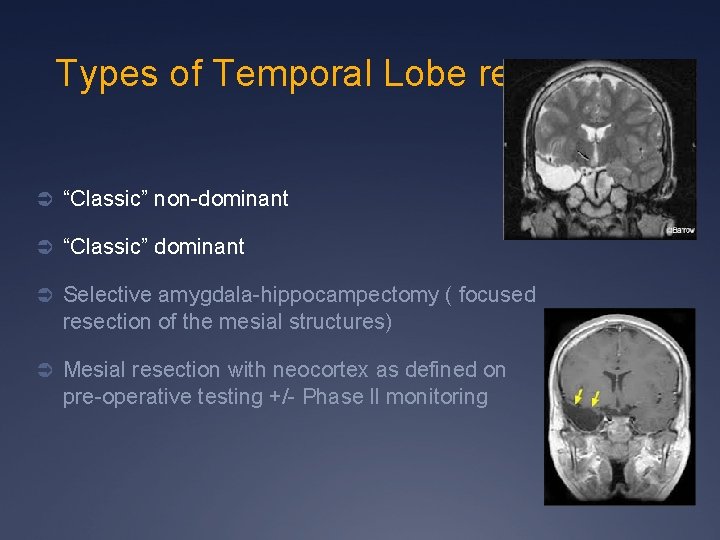
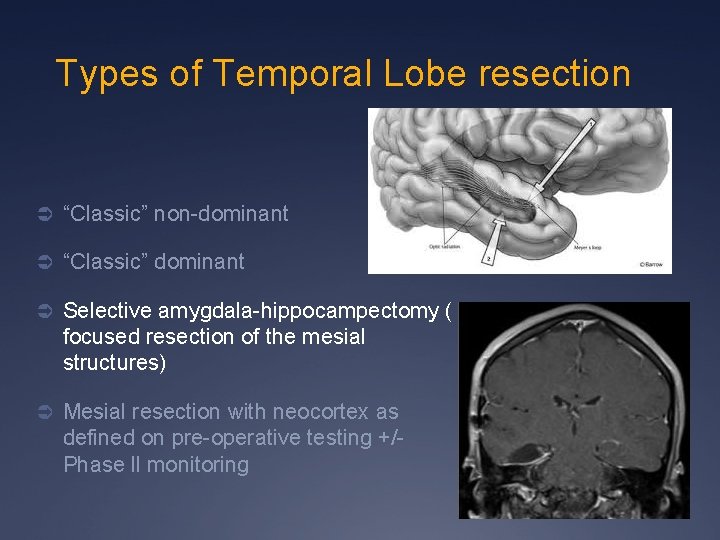
Types of Temporal Lobe resection Ü “Classic” non-dominant Ü “Classic” dominant Ü Selective amygdala-hippocampectomy ( focused resection of the mesial structures) Ü Mesial resection with neocortex as defined on pre-operative testing +/- Phase ll monitoring
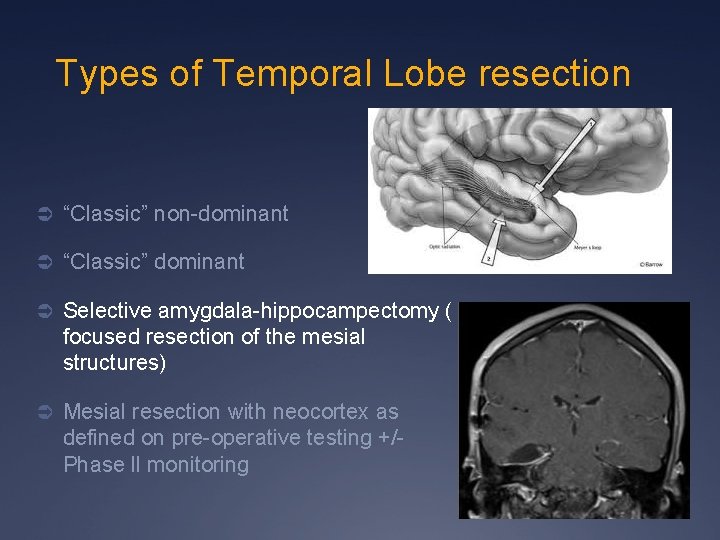
Types of Temporal Lobe resection Ü “Classic” non-dominant Ü “Classic” dominant Ü Selective amygdala-hippocampectomy ( focused resection of the mesial structures) Ü Mesial resection with neocortex as defined on pre-operative testing +/- Phase ll monitoring
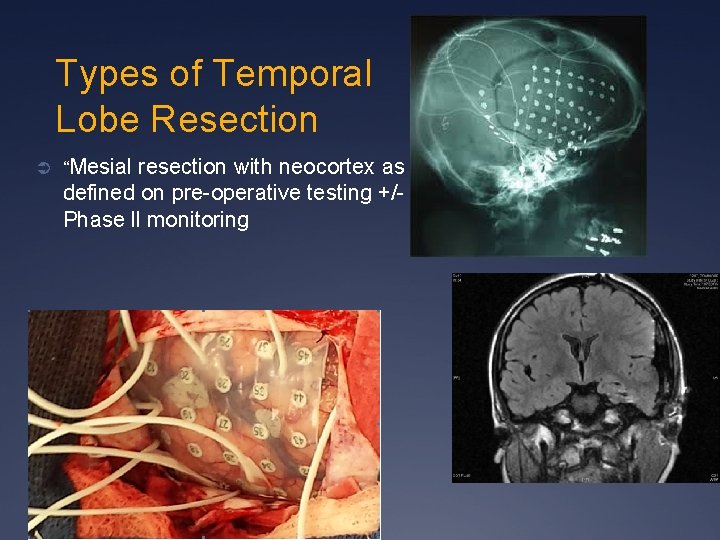
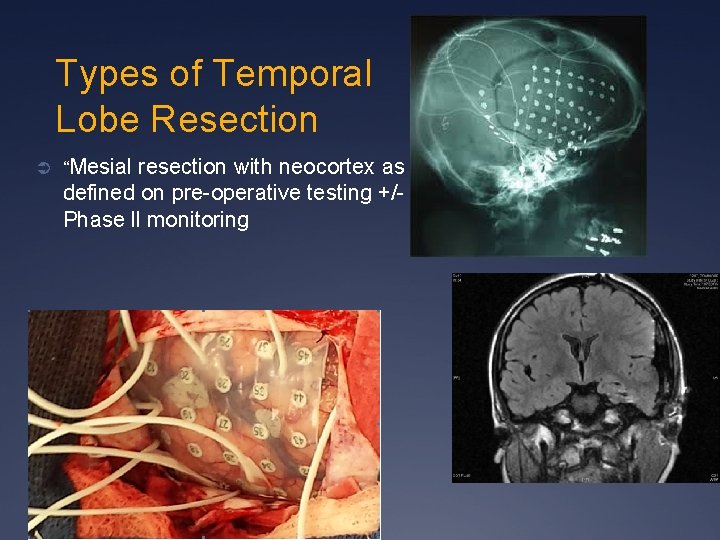
Types of Temporal Lobe Resection Ü “Mesial resection with neocortex as defined on pre-operative testing +/- Phase ll monitoring
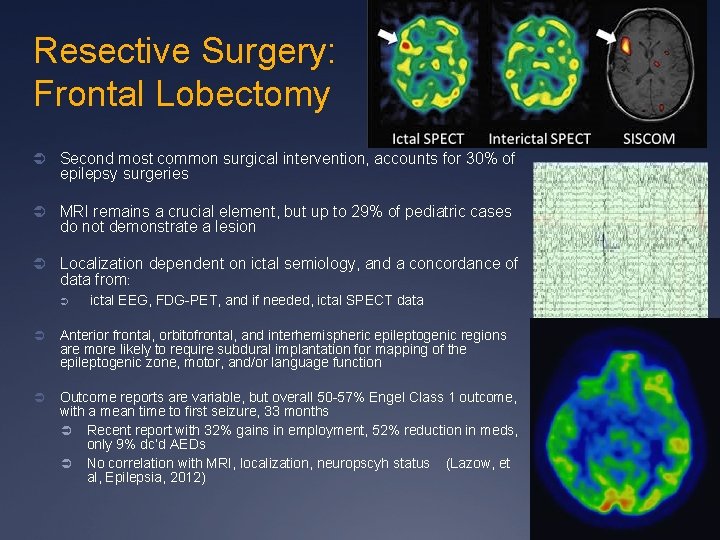
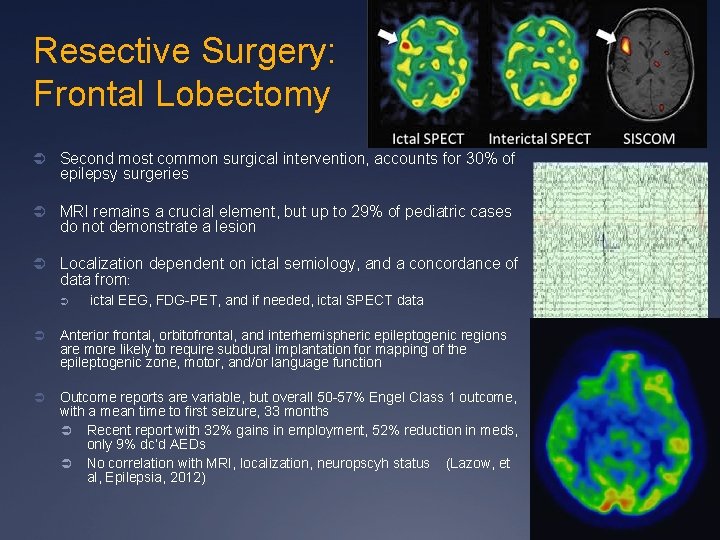
Resective Surgery: Frontal Lobectomy Ü Second most common surgical intervention, accounts for 30% of epilepsy surgeries Ü MRI remains a crucial element, but up to 29% of pediatric cases do not demonstrate a lesion Ü Localization dependent on ictal semiology, and a concordance of data from: Ü ictal EEG, FDG-PET, and if needed, ictal SPECT data Ü Anterior frontal, orbitofrontal, and interhemispheric epileptogenic regions are more likely to require subdural implantation for mapping of the epileptogenic zone, motor, and/or language function Ü Outcome reports are variable, but overall 50 -57% Engel Class 1 outcome, with a mean time to first seizure, 33 months Ü Recent report with 32% gains in employment, 52% reduction in meds, only 9% dc’d AEDs Ü No correlation with MRI, localization, neuropscyh status (Lazow, et al, Epilepsia, 2012)

Resective Surgery: Multi-Lobar Resection Ü Account for < 2% of procedures Ü Typically reserved for known, static etiologies of epilepsy: Ü Ü large cortical dysplasias pre and perinatal insults vascular insults leading to porencephalic cysts Defined lesions such as tumors, trauma, and Sturge-Weber syndrome (SWS) Ü Outcomes are generally lower than single lobar resections -- expected given the extent of epileptogenic region Ü Palliation or Seizure reduction rather than seizure freedom may be the goal
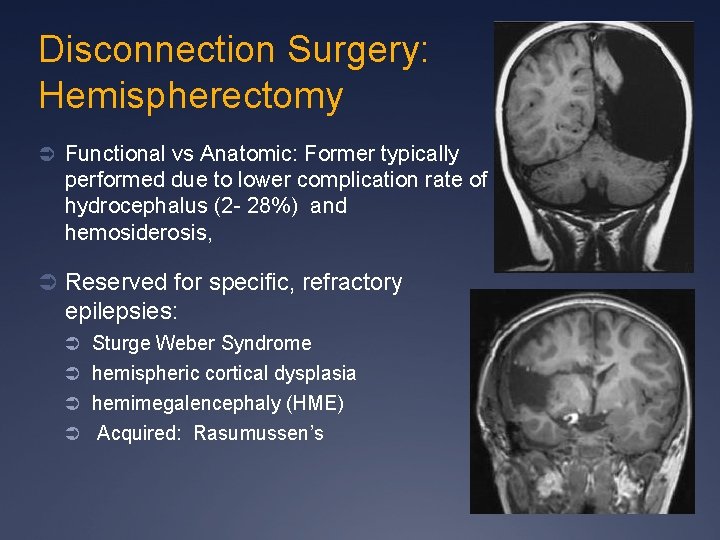
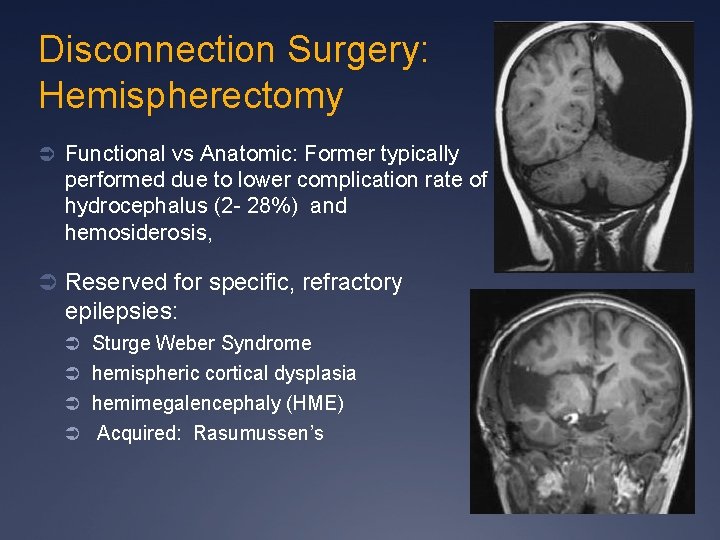
Disconnection Surgery: Hemispherectomy Ü Functional vs Anatomic: Former typically performed due to lower complication rate of hydrocephalus (2 - 28%) and hemosiderosis, Ü Reserved for specific, refractory epilepsies: Ü Sturge Weber Syndrome Ü hemispheric cortical dysplasia Ü hemimegalencephaly (HME) Ü Acquired: Rasumussen’s

Disconnection Surgery: Hemisphereotomy Ü Mortality 7% Ü Outcomes: Ü In multiple studies, Rasmussen’s, SWS, and postperinatal infarction: 70 -90%SF Ü Cortical dysplasia, HME: 60 -80% SF Ü Developmental outcome improved, even in patients with severe developmental quotients Ü Deficit: Hemiparesis of hand, foot drop, and homonymous hemiparesis are expected deficits and included in pre-operative counseling Ü Kossoff et al, 2003
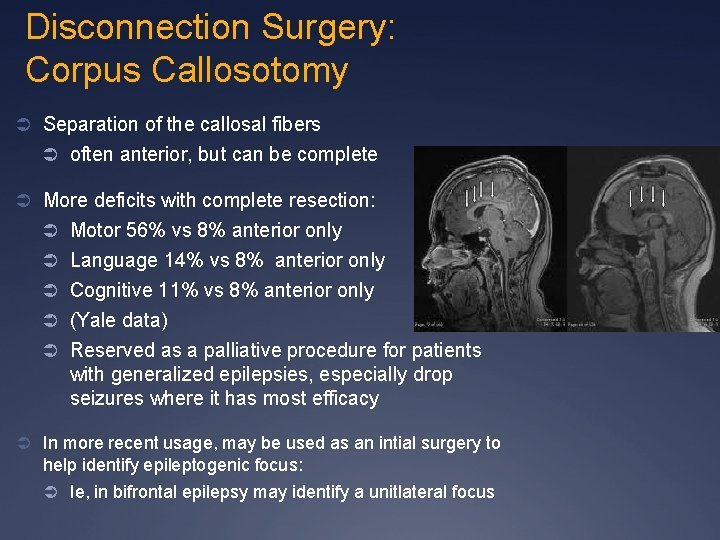
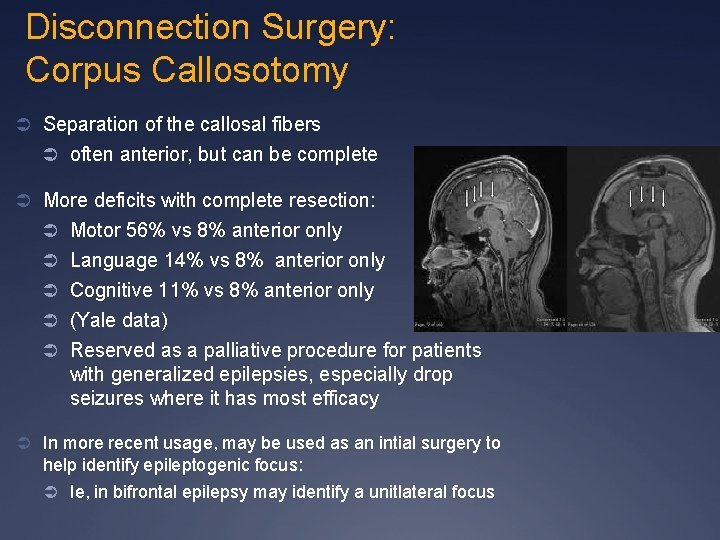
Disconnection Surgery: Corpus Callosotomy Ü Separation of the callosal fibers Ü often anterior, but can be complete Ü More deficits with complete resection: Ü Motor 56% vs 8% anterior only Ü Language 14% vs 8% anterior only Ü Cognitive 11% vs 8% anterior only Ü (Yale data) Ü Reserved as a palliative procedure for patients with generalized epilepsies, especially drop seizures where it has most efficacy Ü In more recent usage, may be used as an intial surgery to help identify epileptogenic focus: Ü Ie, in bifrontal epilepsy may identify a unitlateral focus
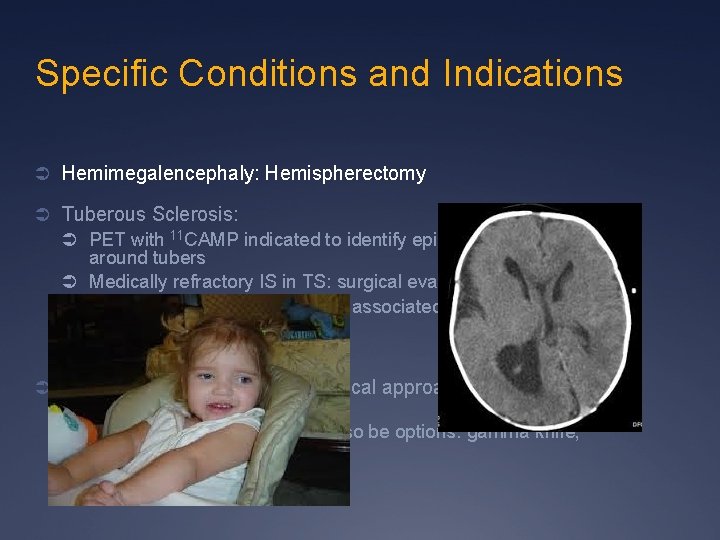
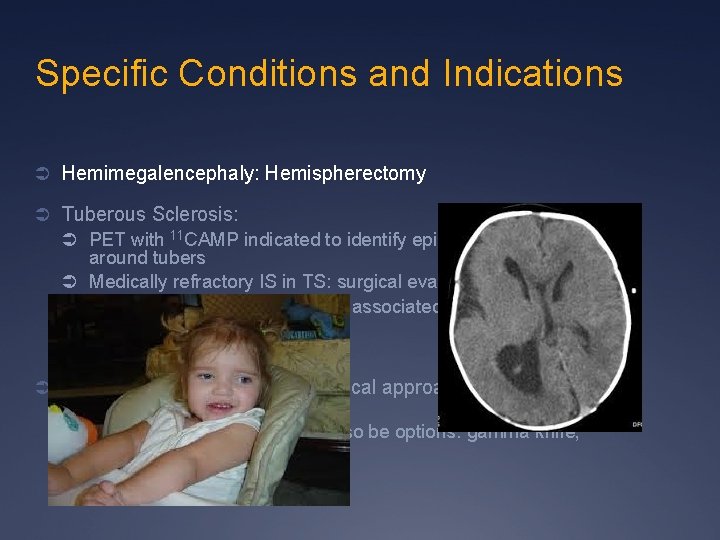
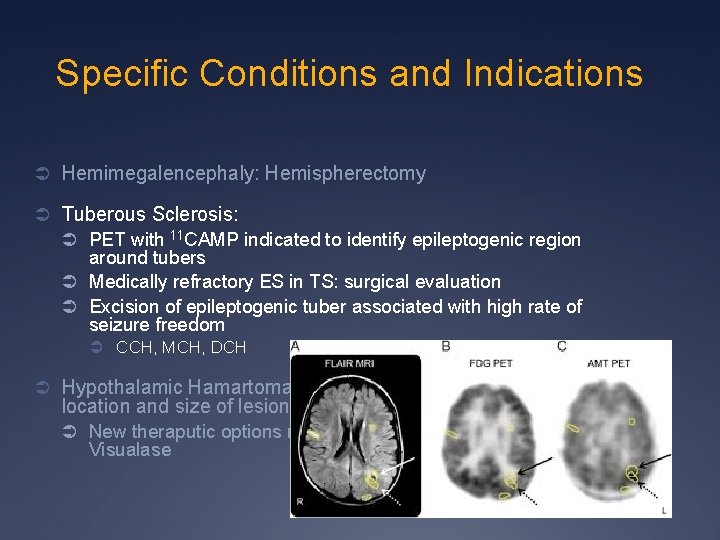
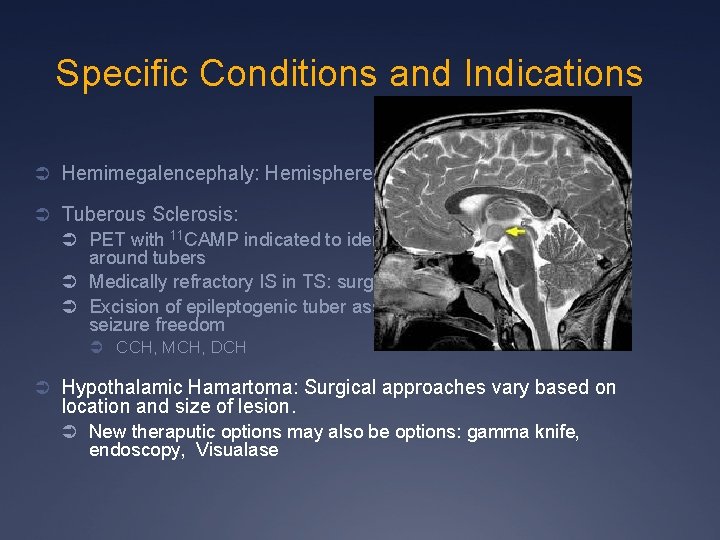
Specific Conditions and Indications Ü Hemimegalencephaly: Hemispherectomy Ü Tuberous Sclerosis: Ü PET with 11 CAMP indicated to identify epileptogenic region around tubers Ü Medically refractory IS in TS: surgical evaluation Ü Excision of epileptogenic tuber associated with high rate of seizure freedom Ü CCH, MCH, DCH Ü Hypothalamic Hamartoma: Surgical approaches vary based on location and size of lesion. Ü New theraputic options may also be options: gamma knife, Visualase
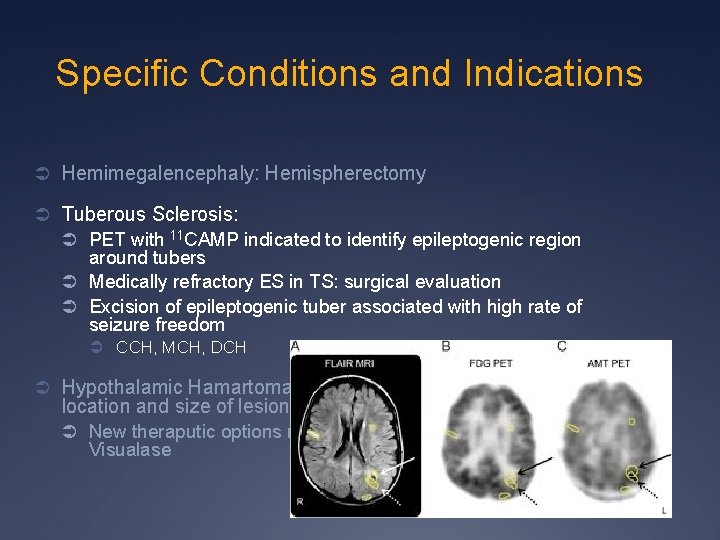
Specific Conditions and Indications Ü Hemimegalencephaly: Hemispherectomy Ü Tuberous Sclerosis: Ü PET with 11 CAMP indicated to identify epileptogenic region around tubers Ü Medically refractory ES in TS: surgical evaluation Ü Excision of epileptogenic tuber associated with high rate of seizure freedom Ü CCH, MCH, DCH Ü Hypothalamic Hamartoma: Surgical approaches vary based on location and size of lesion. Ü New theraputic options may also be options: gamma knife, Visualase
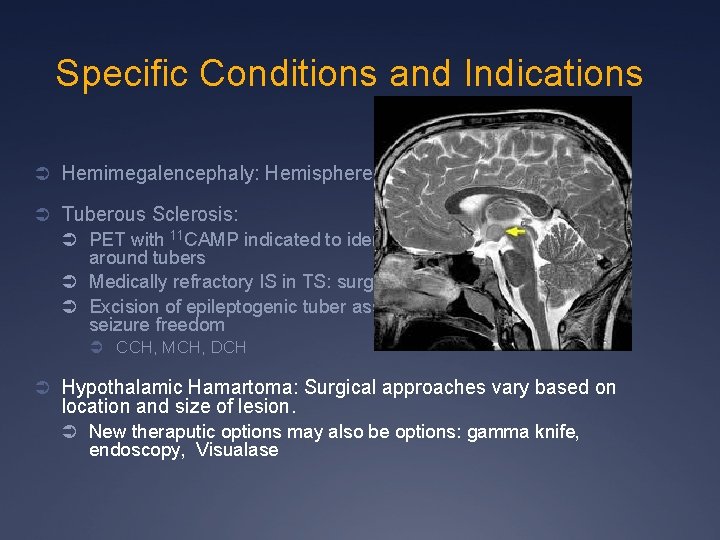
Specific Conditions and Indications Ü Hemimegalencephaly: Hemispherectomy Ü Tuberous Sclerosis: Ü PET with 11 CAMP indicated to identify epileptogenic region around tubers Ü Medically refractory IS in TS: surgical evaluation Ü Excision of epileptogenic tuber associated with high rate of seizure freedom Ü CCH, MCH, DCH Ü Hypothalamic Hamartoma: Surgical approaches vary based on location and size of lesion. Ü New theraputic options may also be options: gamma knife, endoscopy, Visualase

New Techniques/Procedures Ü Visualase: Ü MRI directed laser resection. MR-guided laser interstitial thermal therapy (MRg. LITT) allows for real-time thermal monitoring of the ablation process and feedback control over the laser energy delivery. Ü Gamma knife procedure: Ü Targeted radiosurgery that is noninvasive, and has excellent side effect profile. Indicated for small, deep lesions, ie Small Hypothalamic hamartomas, but effects are delayed
Outcome in Pediatric Epilepsy Pts: Need to be Complete! § In a large study of children undergoing surgery over a 10 year period: § Overall: 78% good outcome (SF or >90% reduction), 60% SF (seizure-free) § Lesional cases vs Non-lesional cases : § § § Site of seizures: § § § 80% good outcome, 65% SF 74% good outcome, 51% SF (no statistical difference) Temporal 80% good, 70% SF, Non-temporal 78% good outcome, 61% SF (no statistical difference) Most significant feature: § Completeness of the resection: 92% good outcome, 76% SF (p<0. 0001) § Paolicchi et al, Neurology 2000; 54 (3): 642 -647
Outcome in Pediatric Epilepsy Pts: Need to be Complete! Ü Single best determinant of outcome in children: completeness of the resection. Ü Probability of poor outcome 11 x greater for incomplete resections Ü No other presurgical factor ( etiology, lobe, pathology, cognitive state, duration of epilepsy, age statistically significant variable) Ü Similar reports from CCF, have shown 88% seizure freedom after complete resection Ü Wylie et al, 1998 Ü Other studies have demonstrated improved outcomes in patients with MRI-visible lesions, unilobar resections, and tumors

Developmental Outcome of Epilepsy Surgery in Children Ü Developmental outcome improved after early resection: Ü Variable factors of influence, but including for children with low development at baseline, Ü Several studies have demonstrated that earlier age, epileptic spasms, and/or less duration of epilepsy show more improvement with developmental outcome Factors that improve developmental outcome: § § § Younger age at the time of surgery Short duration of epilepsy Seizure freedom/outcome Improved developmental, dependent on the study is estimated at 59 -70% § Paolicchi, Nature Clinical Practice Neurology, 2007; 3, 662 -663.

Treatments for MRE Dietary Treatments
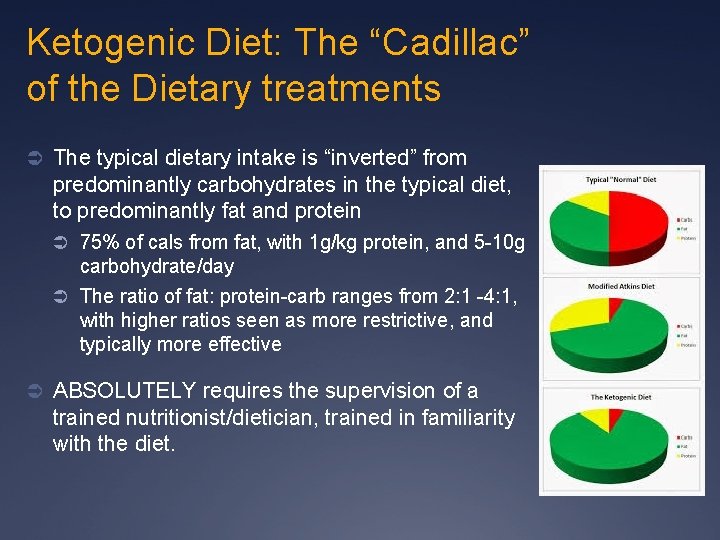
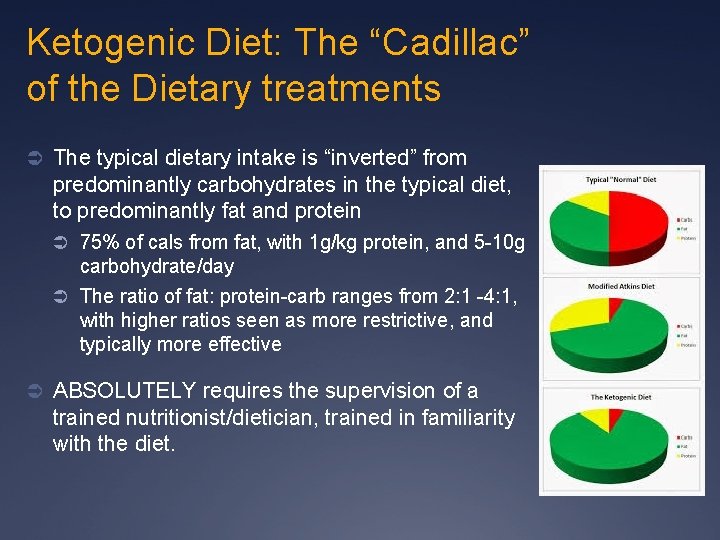
Ketogenic Diet: The “Cadillac” of the Dietary treatments Ü The typical dietary intake is “inverted” from predominantly carbohydrates in the typical diet, to predominantly fat and protein Ü 75% of cals from fat, with 1 g/kg protein, and 5 -10 g carbohydrate/day Ü The ratio of fat: protein-carb ranges from 2: 1 -4: 1, with higher ratios seen as more restrictive, and typically more effective Ü ABSOLUTELY requires the supervision of a trained nutritionist/dietician, trained in familiarity with the diet.

Ketogenic Diet Ü Meals include typical protein/fat sources: Ü Bacon, eggs, tuna, shrimp, mayonnaise, heavy cream, sausage, beef jerky Ü Fat is dietary, but supplemented by dairy ( cream), nut (sesame/peanut), vegetable ( coconut) or MCT ( medium chain triglyceride) oil which has made the diet better tolerated, palpated, less side effects Ü Available for multi-cultures, customable to the patient Ü Can continue infants on breastfeeding Ü Easiest for patients who are bottle or GT fed Ü Variety of formulas available for use on the diet
Ketogenic Diet Ü Best Indications? Ü Studied most extensively in children, but NOT restricted to use in this population. Ü Certain Epilepsy conditions: Ü 1. Epileptic spasms: Ü Abdelmoity ( 2014) prospective: >50% achieved in 70% of pts in 3 mos, majority after 1 mos of the diet ( 60%). Less EEG improvement (60%) Ü Kosoff, et al ( 2002): New onset, >50% in 70% in 3 mos, > in mos, 38% > 90% improved, Less EEG improvement ( 50%); 56% remained on diet for 12 mos, all were > 50% improved Ü Developmental improvements noted in both studies tied to seizure control
Ketogenic Diet Ü 2. Dravet Syndrome ( SCN 1 a mutation) Multiple, small, adjunctive treatment trials of MRE pts demonstrate benefit of KD in this group of patients [Caraballo, et al, 2011 : >75% reduction in 10/13 children] Ü Prospective trial of 14 pts ( Nabbout et al, 2011): 75% improvement in 10/15 pts ( 67%), 40% continued to respond at 9 mos. Behavioral improvement ( hyperactivity/inattention) 56% Ü Ü 3. Lennox-Gastaut Syndrome Ü Ü Frequently used for this syndrome JHU trial of 41 pts after 6 mos on diet: (Lemmon et al, 2012): 51% > 50% improvement, 23%>90%, 1% SF (41 pts) Ü 4. Tuberous Sclerosis Complex: multiple, small studies indicating longterm safety, and indication that children with TSC more likely to have ruecurrence after weaning KD (Nangia, et al, 2012) Ü 5. NCL ( neuronal Ceroid Lipofusinosis) Ü 6. FIRES ( Febrile infection-related epilepsy syndome
Ketogenic Diet Ü Direct Indications Ü 1 Doose Syndrome/Epilepsy with Myoclonic-Atonic Seizures: Ü Multiple, small clinical trials have demonstrated significant benefit on seizures, AND EEG Ü ie Caraballo et al ( 2006): after 18 mos on KD, 66%> 50% improved, 44% > 75% improved, 22% SF Ü 2. GLUT 1 deficiency ( glucose transporter 1 deficiency Ü 3. PDH: pyruvate dehydrogenase deficiency
Ketogenic diet and other dietary treatments for epilepsy Review of Results: - Kossoff 2007: less seizures in 10 g Carb KD vs 20 g MA - Neal 2008: KD seizure improvement > control, p>. 0001 -Seo 2007: KD 4: 1 less seizures than 3: 1, p<0. 05 Side effects: -GI: 30%; Long term potential: Cardiovascular -Discontinuation primarily due to lack of effectiveness or restrictive nature: -only 10% on diet at 3 -6 yrs. Robert G Levy 1, *, et al Editorial Group: Cochrane Epilepsy Group Published Online: 14 MAR 2012 Assessed as up-to-date: 28 JAN 2012 DOI: 10. 1002/14651858. CD 001903. pub 2 The Cochrane Library
Epilepsy Behav. 2013 Dec; 29(3): 437 -42. A decade of the modified Atkins diet (2003– 2013): Results, insights, and future directions. Kossoff EH, Cervenka MC, Henry BJ, Haney CA, Turner Z. Abstract -The modified Atkins diet has been used since 2003 for the treatment of children and adults with MRE -10 years of continued use, approximately 400 patients have been reported in over 30 studies of the modified Atkins diet as treatment for intractable seizures -Results demonstrating similar efficacy to the ketogenic diet and improved tolerability. -The modified Atkins diet is being increasingly used in the adult population.
LGI: Low-glycemic index diet Ü Less available research for epilepsy, but extensive use in metabolic syndrome ( pre-diabetes) Ü Easily accessible for most families, and more straightforward as an add-on adjunctive treatment Ü Does not require the complete “buy-in” and weighing of all foods as the keto diet

Low Glycemic Index Diet Essential basis is to limit the TYPE of carbohydrates, as opposed to the proportion: -Low glycemic index carbohydrates: --Whole grain rice --Whole grain bread --Whole grain pasta --Eliminate fruit juices, starches, dried fruits --NO PROCESSED SUGARS; sugar substitutes accessible
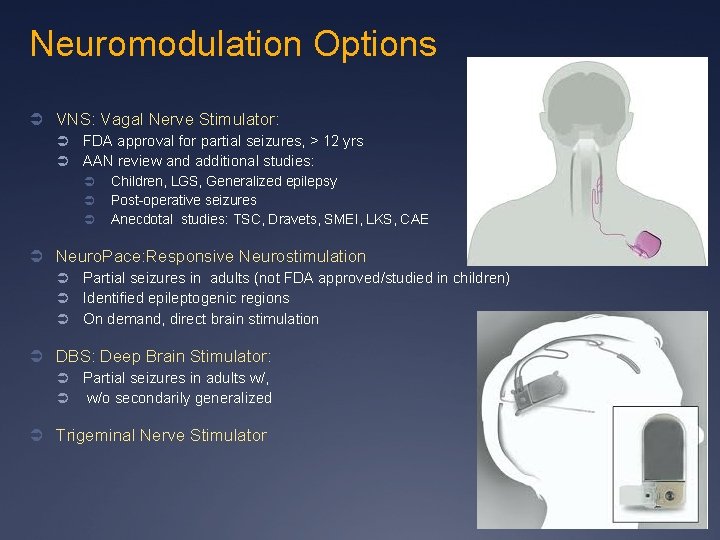
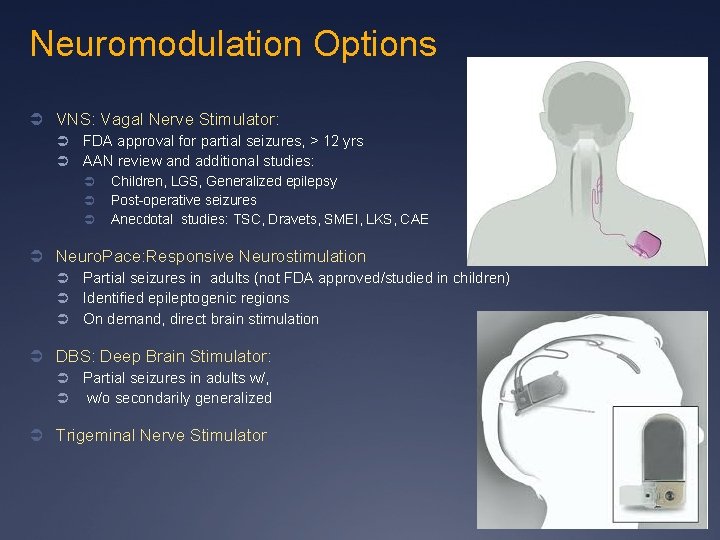
Neuromodulation Options Ü VNS: Vagal Nerve Stimulator: Ü Ü FDA approval for partial seizures, > 12 yrs AAN review and additional studies: Ü Ü Ü Children, LGS, Generalized epilepsy Post-operative seizures Anecdotal studies: TSC, Dravets, SMEI, LKS, CAE Ü Neuro. Pace: Responsive Neurostimulation Ü Ü Ü Partial seizures in adults (not FDA approved/studied in children) Identified epileptogenic regions On demand, direct brain stimulation Ü DBS: Deep Brain Stimulator: Ü Ü Partial seizures in adults w/, w/o secondarily generalized Ü Trigeminal Nerve Stimulator
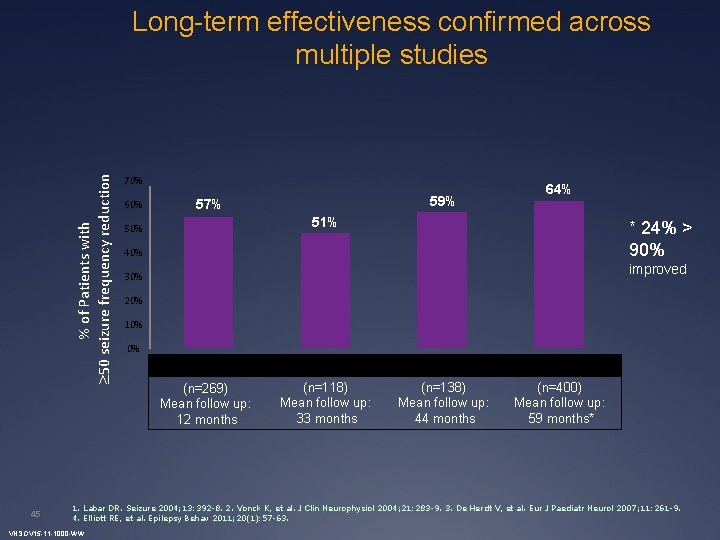
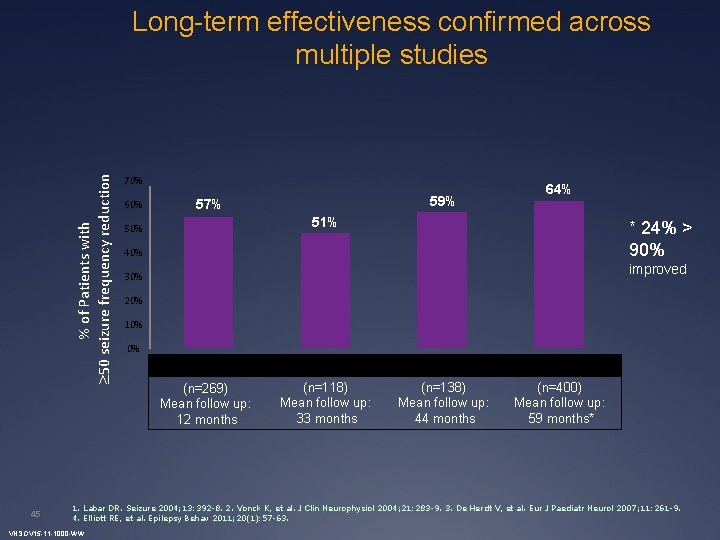
% of Patients with 50 seizure frequency reduction Long-term effectiveness confirmed across multiple studies 45 70% 60% 59% 57% 64% 51% 50% * 24% > 90% 40% improved 30% 20% 10% 0% Labar Vonck De Herdt Elliott (n=269) Mean follow up: 12 months (n=118) Mean follow up: 33 months (n=138) Mean follow up: 44 months (n=400) Mean follow up: 59 months* 1. Labar DR. Seizure 2004; 13: 392 -8. 2. Vonck K, et al. J Clin Neurophysiol 2004; 21: 283 -9. 3. De Herdt V, et al. Eur J Paediatr Neurol 2007; 11: 261 -9. 4. Elliott RE, et al. Epilepsy Behav 2011; 20(1): 57 -63. VNSOV 15 -11 -1000 -WW

Mean Seizure Reduction Seizure reduction improves over time and is sustained for at least 10 years post-VNS Therapy 75. 5% 76. 3% 58. 3% 60. 4% 2 Years 4 Years 65. 7% 52. 1% 35. 7% 6 months 1 Year 6 Years 8 years 10 Years LVCF • Seizure frequency was significantly reduced from baseline at each of the recorded intervals (P<0. 01); N=65 46 VNSOV 15 -11 -1000 -WW Elliott RE, et al. Epilepsy & Behavior 20: 57 -63, 2011
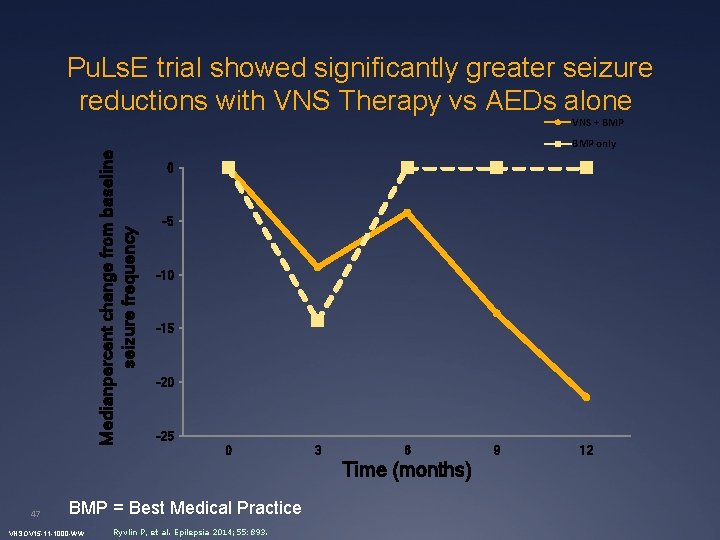
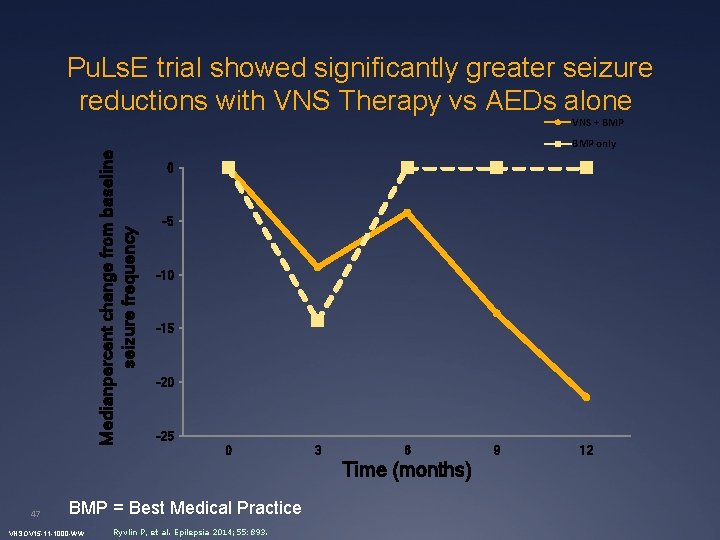
Pu. Ls. E trial showed significantly greater seizure reductions with VNS Therapy vs AEDs alone Medianpercent change from baseline seizure frequency VNS + BMP only 0 -5 -10 -15 -20 -25 0 3 6 Time (months) 47 BMP = Best Medical Practice VNSOV 15 -11 -1000 -WW Ryvlin P, et al. Epilepsia 2014; 55: 893. 9 12
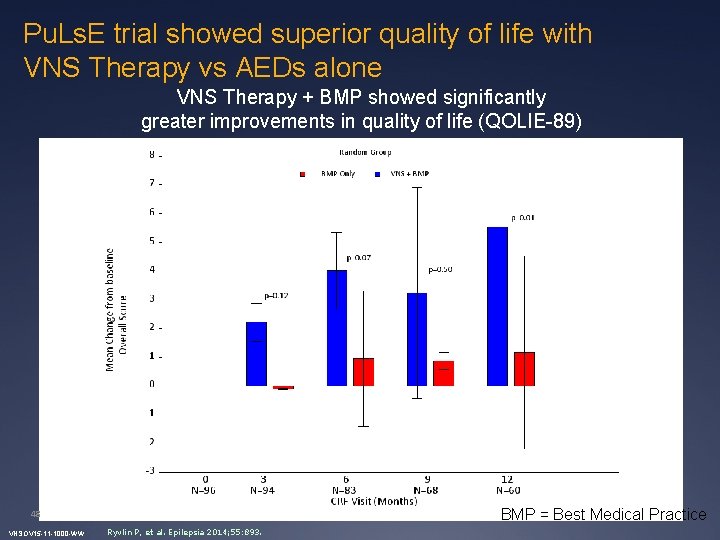
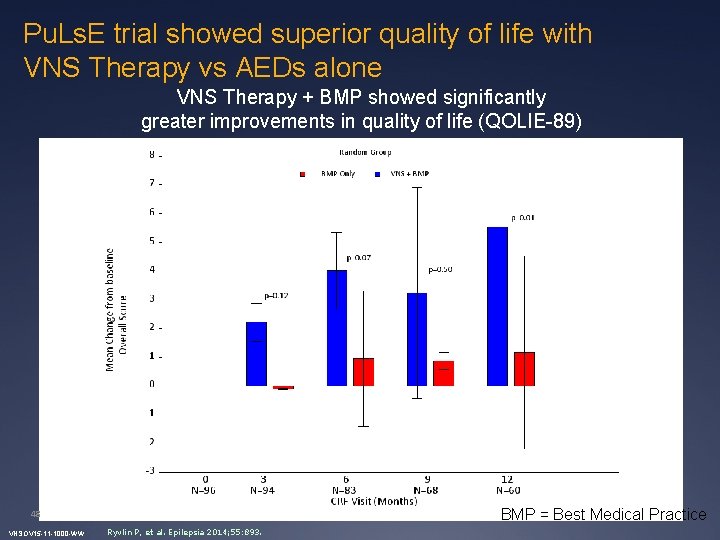
Pu. Ls. E trial showed superior quality of life with VNS Therapy vs AEDs alone VNS Therapy + BMP showed significantly greater improvements in quality of life (QOLIE-89) Ryvlin P. et al Epilepsia (in press) 2014 BMP = Best Medical Practice 48 VNSOV 15 -11 -1000 -WW Ryvlin P, et al. Epilepsia 2014; 55: 893.
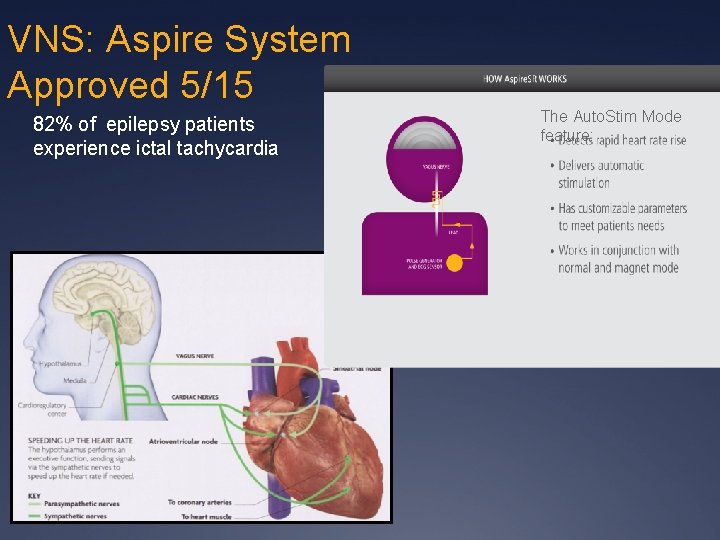
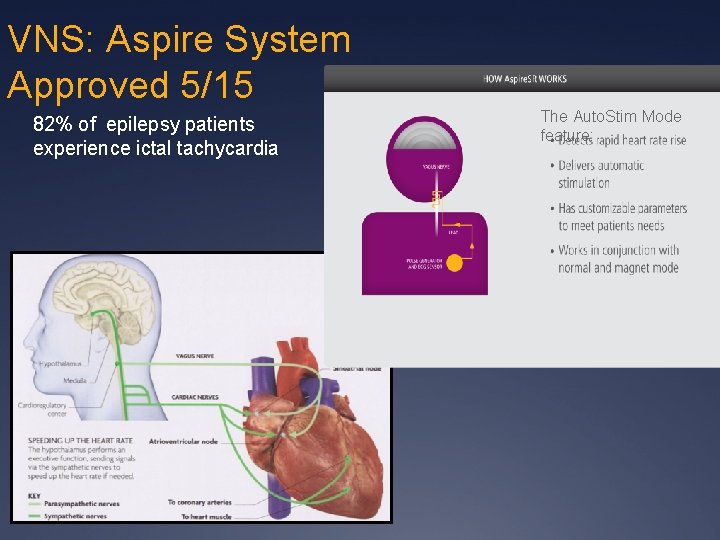
VNS: Aspire System Approved 5/15 82% of epilepsy patients experience ictal tachycardia The Auto. Stim Mode feature:
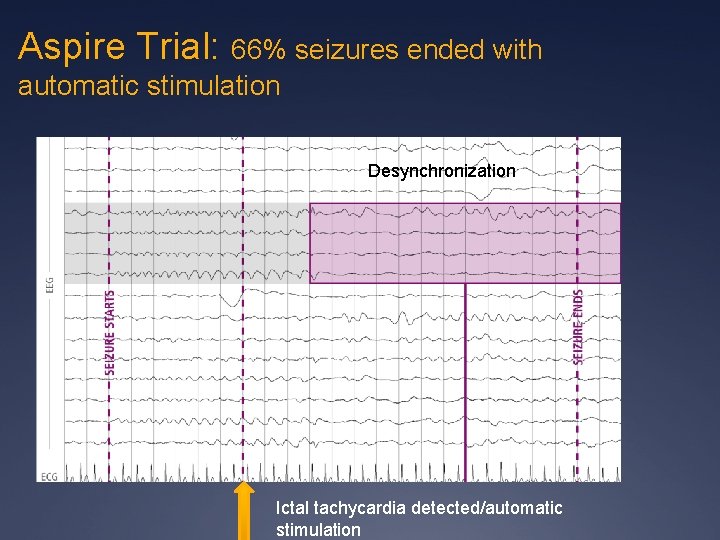
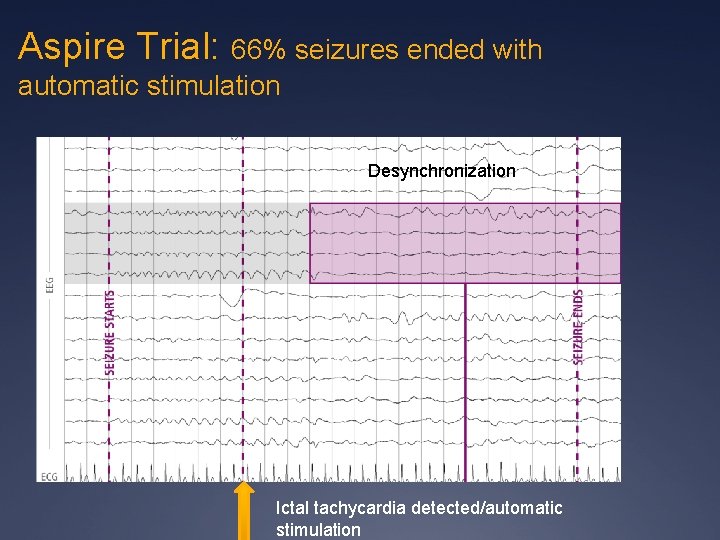
Aspire Trial: 66% seizures ended with automatic stimulation Desynchronization Ictal tachycardia detected/automatic stimulation
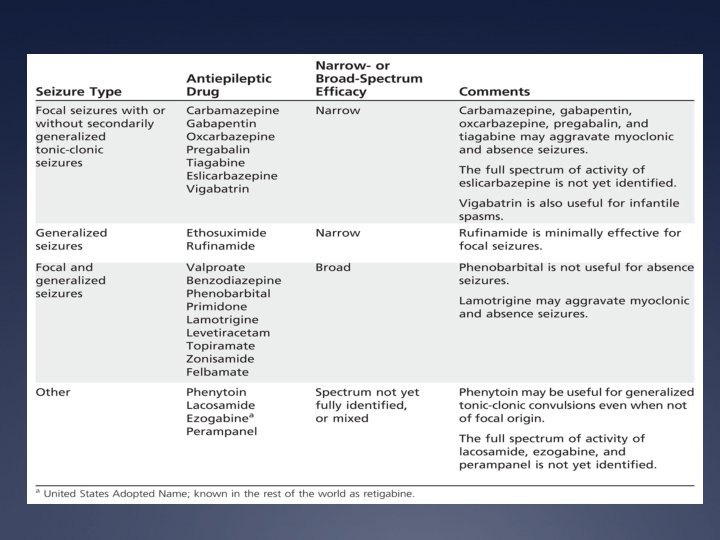
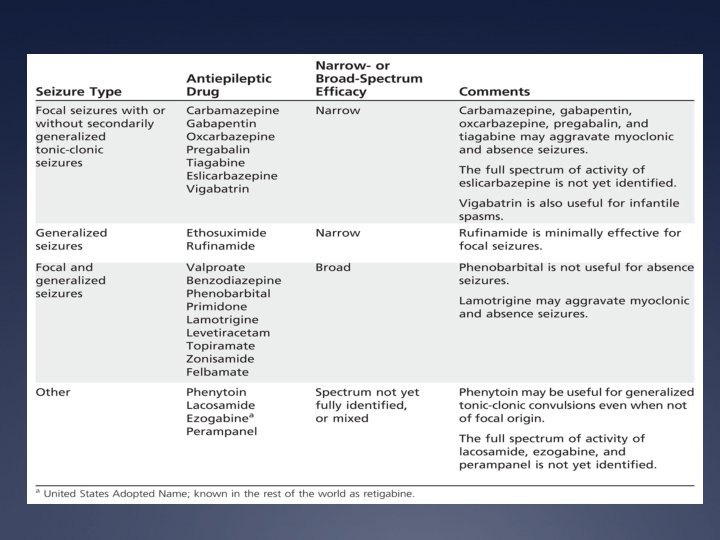
Narrow Versus Broad Spectrum AEDs

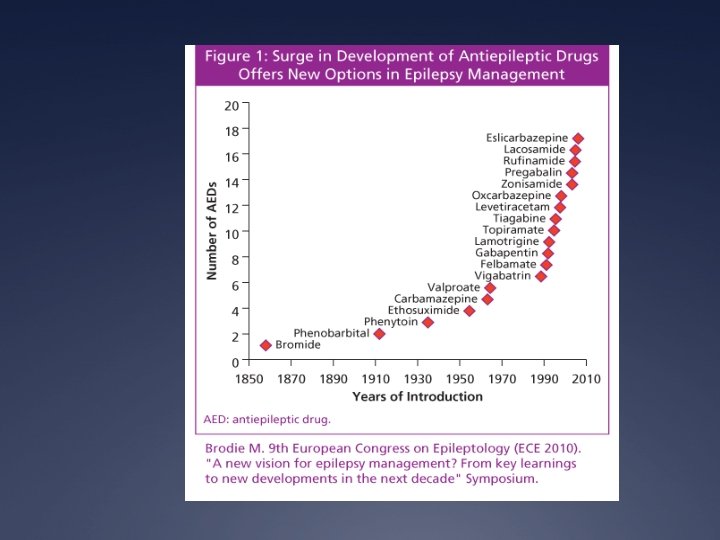
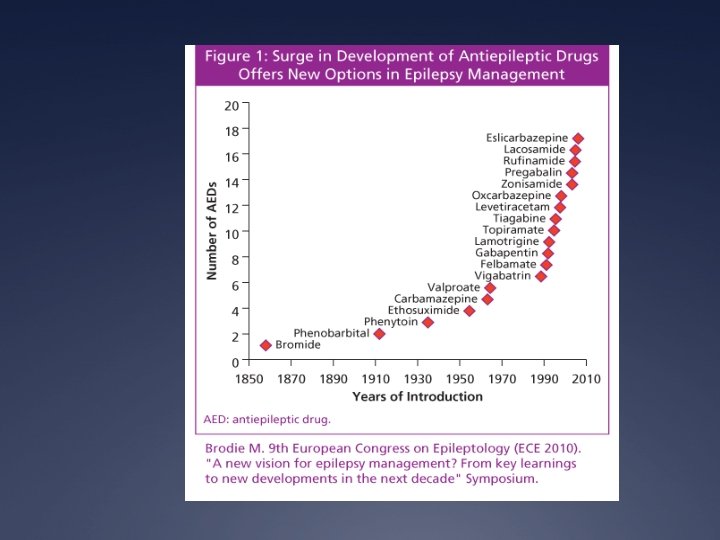
New/Emerging Therapies Ü New(er) AEDs: Novel Mechanisms Ü Ezogabine: partial seizures (Volt-gated K channels) Ü Vigabatrin: Epileptic seizures and refractory partial seizures ( irreversible inhibition of GABA transaminase) Ü Perampanel: partial and generalized seizures ( antagonist of AMPA receptors - glutamate) Ü Eslicarbazepine acetate: Oxcarbmaxepine analog/daily dosing schedule Ü Specific AEDs: Ü Stiripentol ( alcohol compound than increases opening of GABA channels) Ü Fenflouramine: Used for cardiac disease– effect in genetic epilepsies

Initial Focus on a Particularly Difficult to Treat Genetic Epileptic Syndrome: Dravet’s Syndrome Herbal/Organic: Cannabidiol Epidiolex : Class I in many states, IND in US, RCT trial for Dravet, LGS Medical Marijuana: Statewide registration laws vary “Self Trials” common
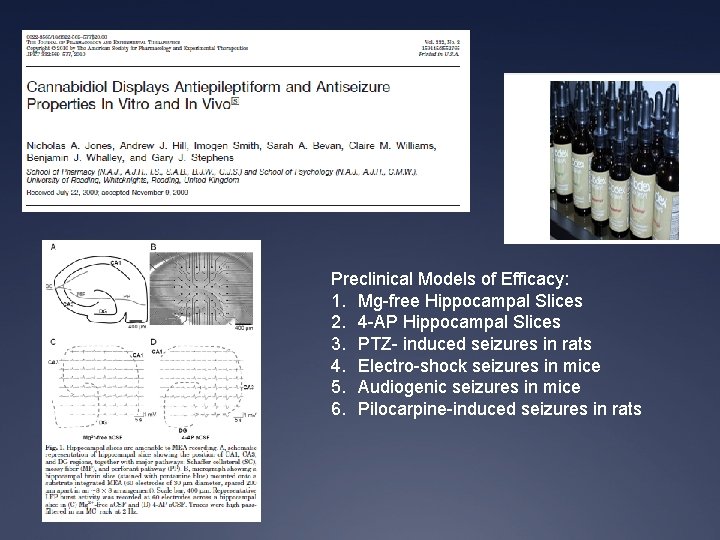
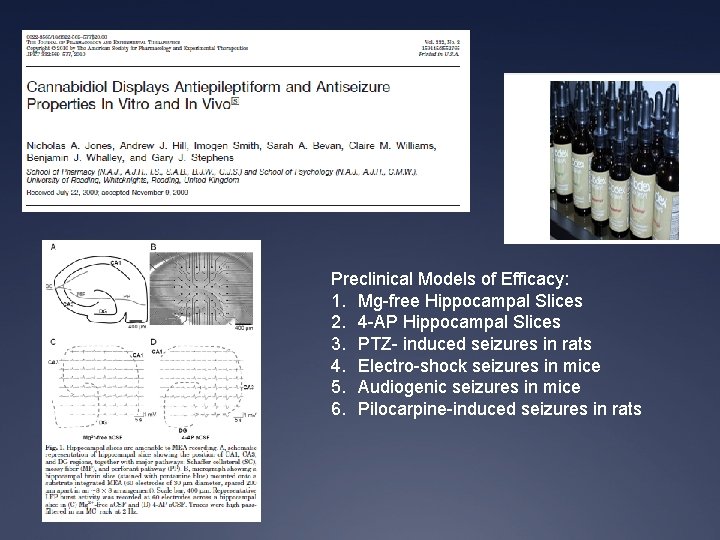
Preclinical Models of Efficacy: 1. Mg-free Hippocampal Slices 2. 4 -AP Hippocampal Slices 3. PTZ- induced seizures in rats 4. Electro-shock seizures in mice 5. Audiogenic seizures in mice 6. Pilocarpine-induced seizures in rats
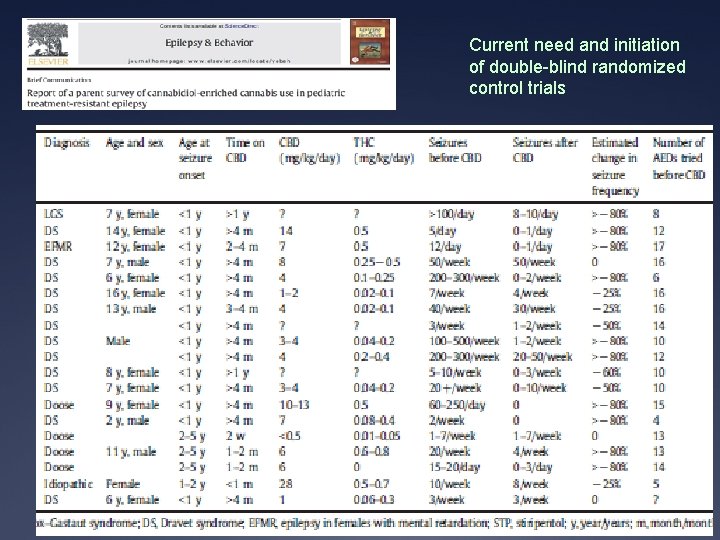
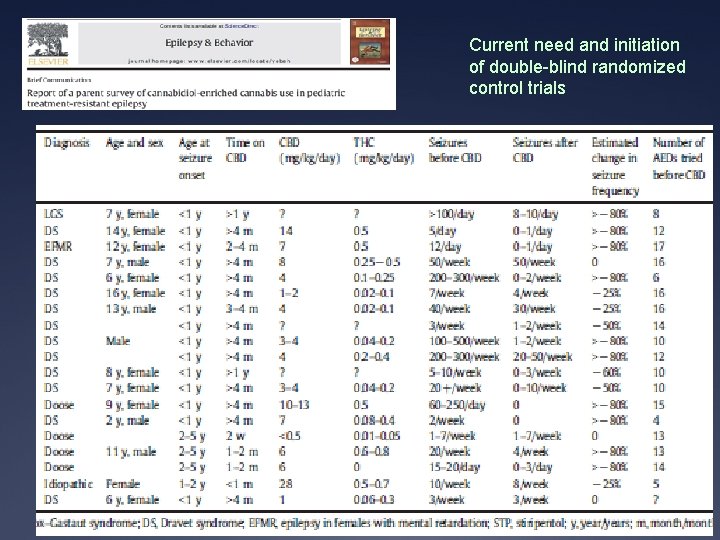
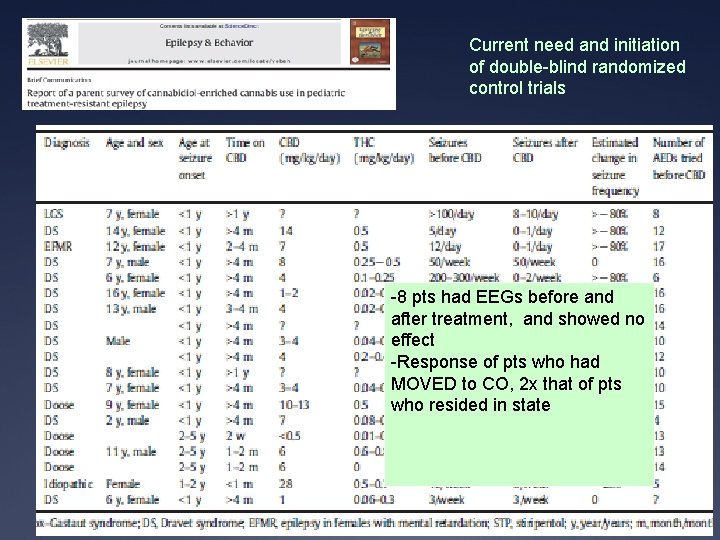
Current need and initiation of double-blind randomized control trials
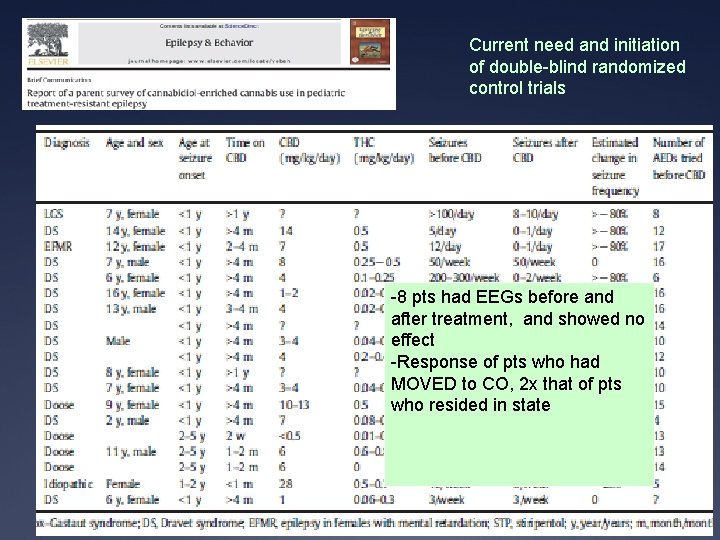
Current need and initiation of double-blind randomized control trials -8 pts had EEGs before and after treatment, and showed no effect -Response of pts who had MOVED to CO, 2 x that of pts who resided in state

Current Cannibidoil Trials Ü 1. ‘Availability” trial: 137 pts treated, mean reduction in seizure number, 54% of pts had a 50% reduction in seizures Ü 2. Effect of Cannibidoil on Neuropsychological profile for patients with refractory Epilepsy: RESULTS AVAILABLE SOON Ü 3. Randomized “Placebo” clinical trial in pts with Dravet syndrome: RESULTS AVAILABLE SOON Ü 4. Randomized “Placebo” clinical trial in pts with Lennox-Gastaut syndrome: RESULTS AVAILABLE SOON Ü 5. Smaller trials in specific patient populations
Current Cannibidoil Trials Ü NEREG TRIAL: Ü High CBD/low THC concentration MMJ Ü Open label trial Ü Various age categories Ü Variable seizure types, but all Medically refractory epilepsy Ü Following: Ü Seizure frequency Ü Effect of Anti-epileptic medications Ü Measuring Patient Questionnaires on: Sleep Ü Behavioral Health, especially Anxiety, Mood Ü -

What happened to our cases? Ü Case 1: The little jokester Ü Family wanted surgery Ü Case 2: The soccer player Ü Family wanted VNS
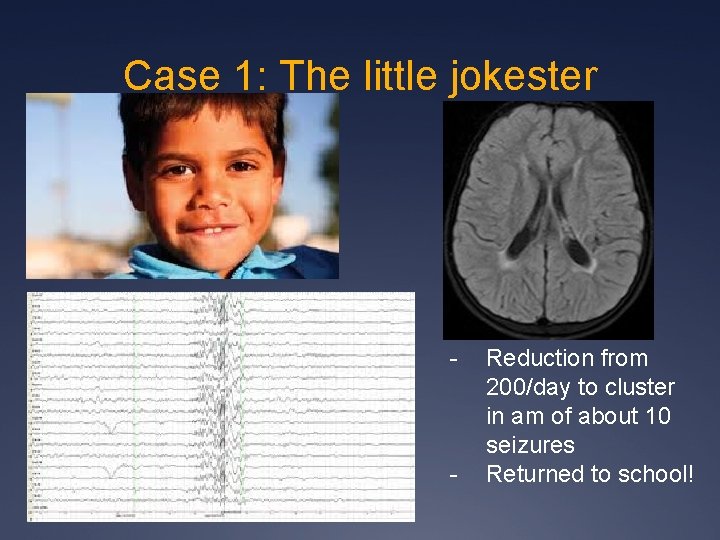
Case 1: The little jokester - - Reduction from 200/day to cluster in am of about 10 seizures Returned to school!
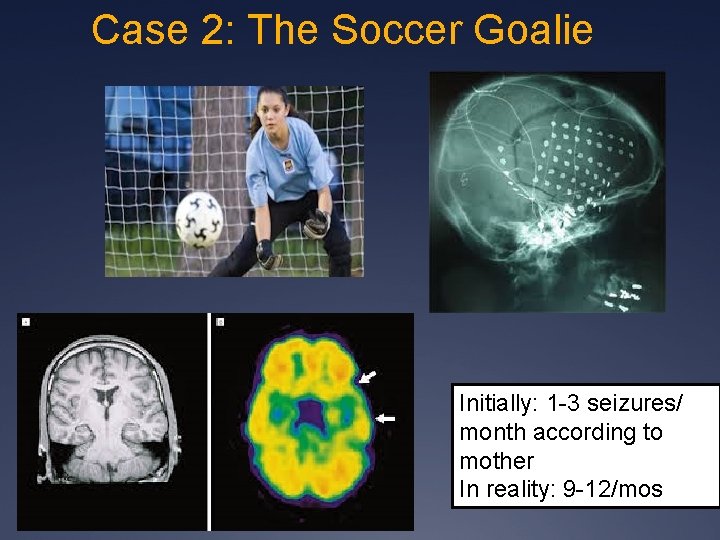
Case 2: The Soccer Goalie Initially: 1 -3 seizures/ month according to mother In reality: 9 -12/mos
Outcome: - Seizure-free w/ Intermittent auras controlled with AED changes - Driver’s License!

Summary: Treatment of Medical Intractability The typical steps involve: *Comprehensive Epilepsy Evaluation *Surgical determination *Determination of alternative therapies: - Dietary - Neurostimulation - New/Experimental AEDs -“Herbal/organic”
Choices in the Treatment of Epilepsy: What, When, and Who? What: are my options? When: should I consider these options? Who are the best candidates for these options? Timely referral can alter the progressive disability of medically intractable epilepsy Timely referral can potentially Improve the developmental outcome of patients with chronic epilepsy Timely referral can potentially reduce the need for more extensive resections/therapies
Treatment of Medically Resistant Epilepsy : If medically- resistant, the treatment goal switches to QOL: Ü Maximizing QOL, minimizing seizures and sedation Ü Goals are determined by the team of the patient, caregivers, and medical staff as to realistic and individual attainable goals Ü The family and patient are key members of that determination Ü Frequently asses the goals of the patients and caregivers as to the success of the goals, not just seizure count Questions? JM Paolicchi, MA, MD NEREG Manhattan, NY Hackensack, NJ White Plains, NJ Middleton, NY @JMPaolicchi. MD jpaolicchimd@squarespace. com
 Inflatable helmet for epilepsy
Inflatable helmet for epilepsy Young epilepsy
Young epilepsy Rolandic epilepsy icd 10
Rolandic epilepsy icd 10 Xl spikes on eeg
Xl spikes on eeg Epilepsy
Epilepsy Benign rolandic epilepsy rch
Benign rolandic epilepsy rch Shaking vs seizure
Shaking vs seizure Epilepsy society of southern ny
Epilepsy society of southern ny Northeast regional epilepsy
Northeast regional epilepsy Difference between seizure and epilepsy
Difference between seizure and epilepsy Epilepsy
Epilepsy Basic mechanisms underlying seizures and epilepsy
Basic mechanisms underlying seizures and epilepsy American epilepsy society annual meeting 2017
American epilepsy society annual meeting 2017 Ykp epilepsy
Ykp epilepsy Seizure
Seizure Romberg test positive causes
Romberg test positive causes Epilepsy trigger
Epilepsy trigger Canadian league against epilepsy
Canadian league against epilepsy Northeast regional epilepsy
Northeast regional epilepsy Epilepsy
Epilepsy Depakote epilepsy
Depakote epilepsy Catastrophic epilepsy infancy
Catastrophic epilepsy infancy Aremco epilepsy
Aremco epilepsy Dr politsky epilepsy
Dr politsky epilepsy Aremco epilepsy
Aremco epilepsy Dravet syndrome
Dravet syndrome Manori wijayath neurologist
Manori wijayath neurologist Epilepsy and seizure services near sutter creek
Epilepsy and seizure services near sutter creek Cps epilepsy
Cps epilepsy Migraine aura vs seizure aura
Migraine aura vs seizure aura Spina bifida
Spina bifida Epilepsy death
Epilepsy death û
û Reversible dementia
Reversible dementia Vanderbilt neurology residents
Vanderbilt neurology residents Seizure types and symptoms
Seizure types and symptoms Catamenial epilepsy and birth control pills
Catamenial epilepsy and birth control pills Northeast regional epilepsy group
Northeast regional epilepsy group European epilepsy database
European epilepsy database Letazol
Letazol Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Chó sói
Chó sói Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu điện thế nghỉ
điện thế nghỉ Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ Một số thể thơ truyền thống
Một số thể thơ truyền thống Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Ng-html
Ng-html Bảng số nguyên tố lớn hơn 1000
Bảng số nguyên tố lớn hơn 1000 Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Fecboak
Fecboak Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Hệ hô hấp
Hệ hô hấp Tư thế ngồi viết
Tư thế ngồi viết đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Bổ thể
Bổ thể Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton ưu thế lai là gì
ưu thế lai là gì Tư thế ngồi viết
Tư thế ngồi viết Thẻ vin
Thẻ vin Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là