CHILDRENS ORTHOPAEDICS COMMON LOWER LIMB PROBLEMS By Linda
CHILDREN’S ORTHOPAEDICS COMMON LOWER LIMB PROBLEMS By Linda Walsh COOP Practitioner
OBJECTIVES Introduction to COOP Overview of common children’s orthopaedic conditions Overview of optimal management of these conditions What not to miss! When and How to Refer Top tips summary
WHAT IS COOP? ? Children’s Orthopaedic Outreach Project Charity Funded 3 year project Now Substantive Posts 2 Extended Scope Physiotherapists 2 Strands of the Service General MSK COOP Linda Walsh Neuromuscular COOP Lucy Llewellyn Stanton
COOP OBJECTIVES • Enable more efficient use of consultant clinic time • Introduce outreach work in paediatric orthopaedics • To establish care pathways, protocols/guidelines • To use our care pathways, protocols/guidelines and standardised assessments to enable participation in research, development of national guidelines and prospective databases.
COOP CLINICS Now offer Physiotherapy Led Face to Face Screening and Follow up clinics To note; these clinics run alongside consultant led clinics Now running SKYPE clinics Now running Telephone clinics Run weekly outreach clinic at Newham hospital Run neuromuscular outreach clinics in special schools Offer a point of contact/liaison for queries between community and orthopaedics
PAEDIATRIC ASSESSMENT AND TREATMENT “Consistency is more valuable than talent” Have a consistent approach-complete a thorough history and a thorough examination
BASIC PREMISE ASSESSMENT Is presentation normal? Will the presentation get better? Is there any advice/Rx/intervention that can help? Evidence? ?
DISTINGUISHING WHAT IS NORMAL Normal variants Normal gait Normal motor milestones Normal range of motion Variations related to families, race, age Pediatric REMS, Foster 2008 Intro-Look-Feel- Move- Ax function, Foster 2011
THE 5 ORTHOPAEDIC S’S Symmetry Symptoms Stiffness Systemic Disease Skeletal Dysplasia
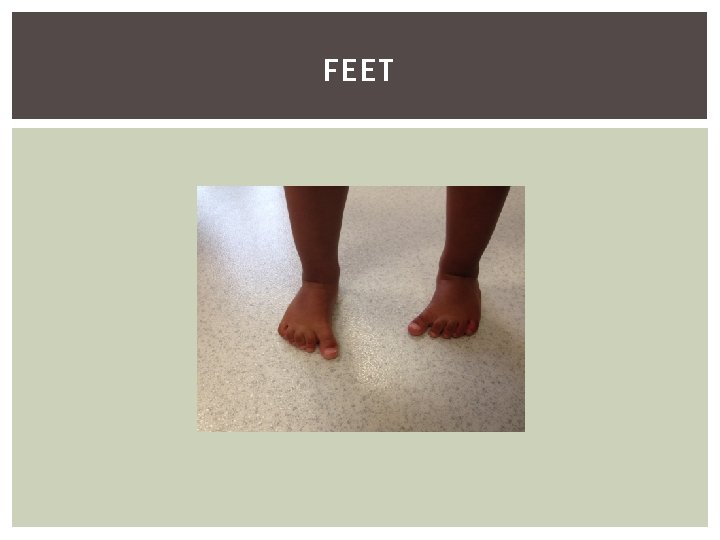
FEET
COMMON CONDITIONS Metatarsus Adductus Calcaneo-Valgus CTEV Curly toes Flat Foot Tarsal Coalition Pes Cavus Severs
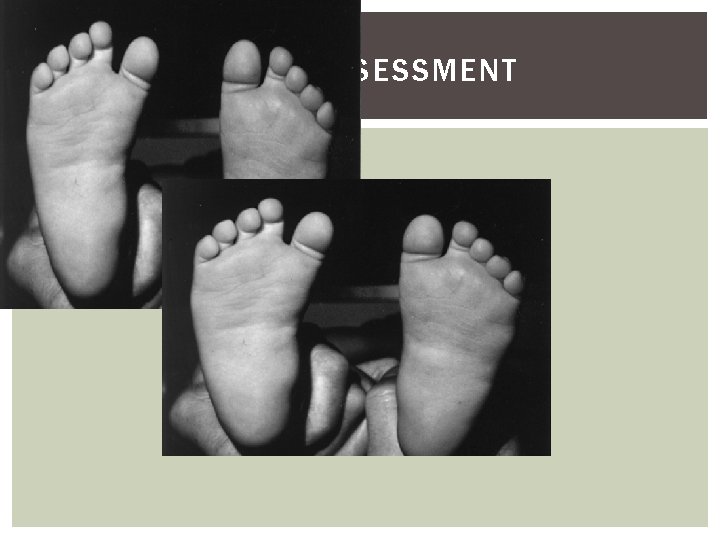
FOOT - ASSESSMENT
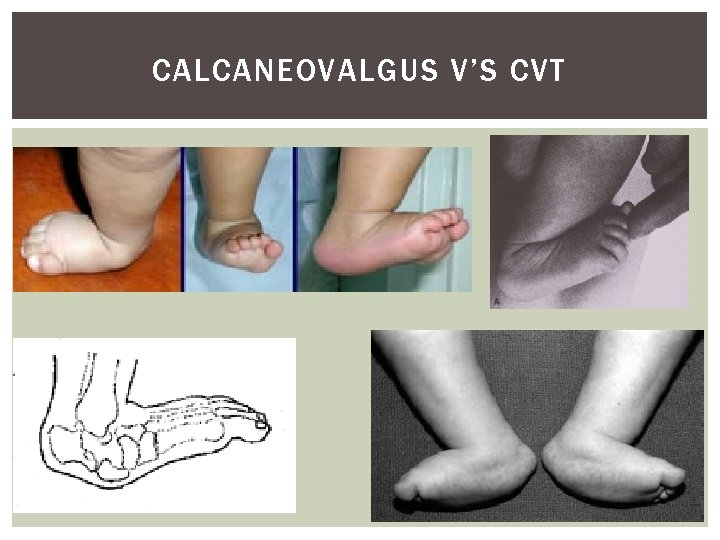
CALCANEOVALGUS V’S CVT
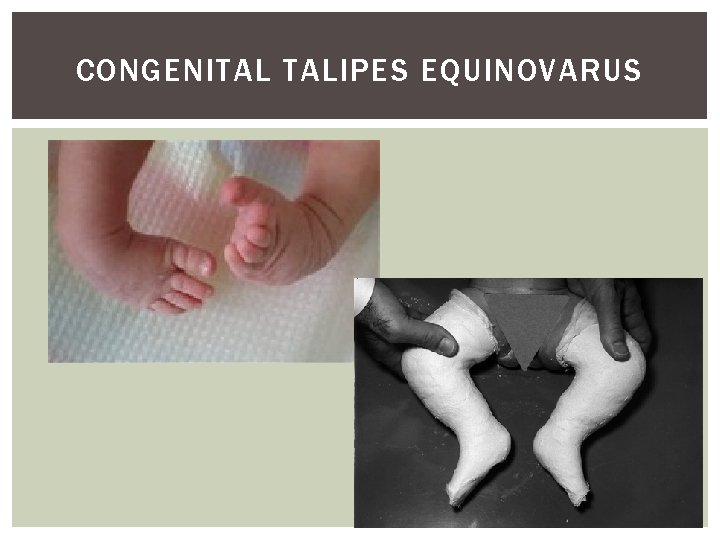
CONGENITAL TALIPES EQUINOVARUS
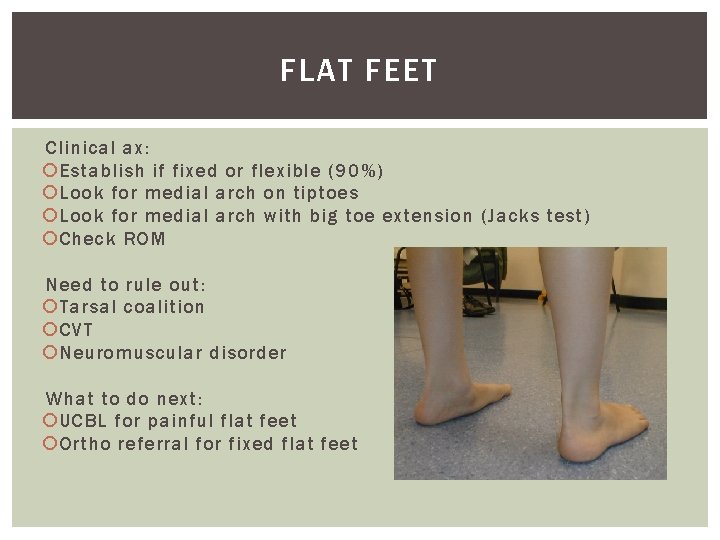
FLAT FEET Clinical ax: Establish if fixed or flexible (90%) Look for medial arch on tiptoes Look for medial arch with big toe extension (Jacks test) Check ROM Need to rule out: Tarsal coalition CVT Neuromuscular disorder What to do next: UCBL for painful flat feet Ortho referral for fixed flat feet
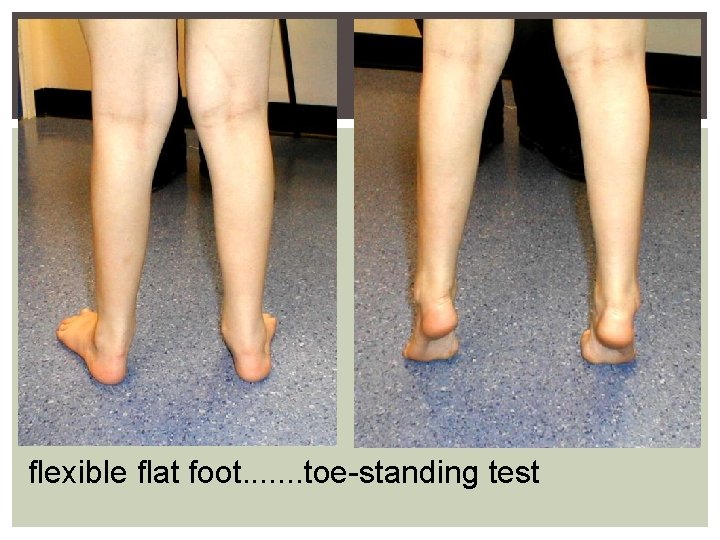
flexible flat foot. . . . toe-standing test
CURLY TOES Do nothing as most correct. If anything needs doing – not until the age of 4 years
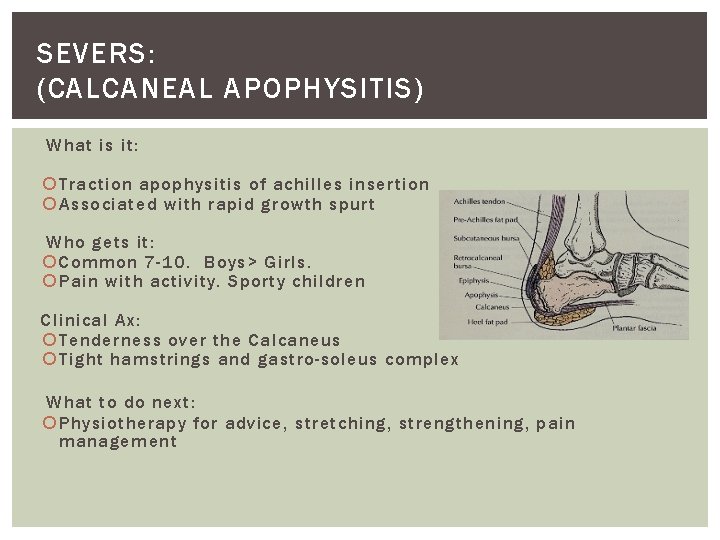
SEVERS: (CALCANEAL APOPHYSITIS) What is it: Traction apophysitis of achilles insertion Associated with rapid growth spurt Who gets it: Common 7 -10. Boys> Girls. Pain with activity. Sporty children Clinical Ax: Tenderness over the Calcaneus Tight hamstrings and gastro-soleus complex What to do next: Physiotherapy for advice, stretching, strengthening, pain management
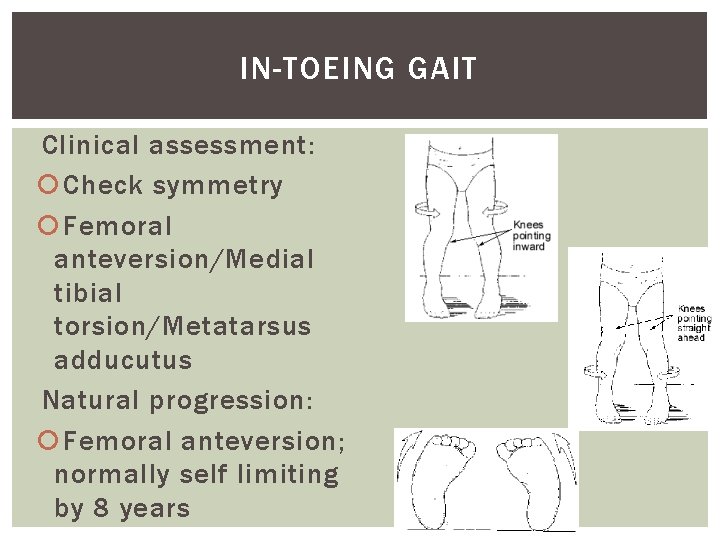
IN-TOEING GAIT Clinical assessment: Check symmetry Femoral anteversion/Medial tibial torsion/Metatarsus adducutus Natural progression: Femoral anteversion; normally self limiting by 8 years
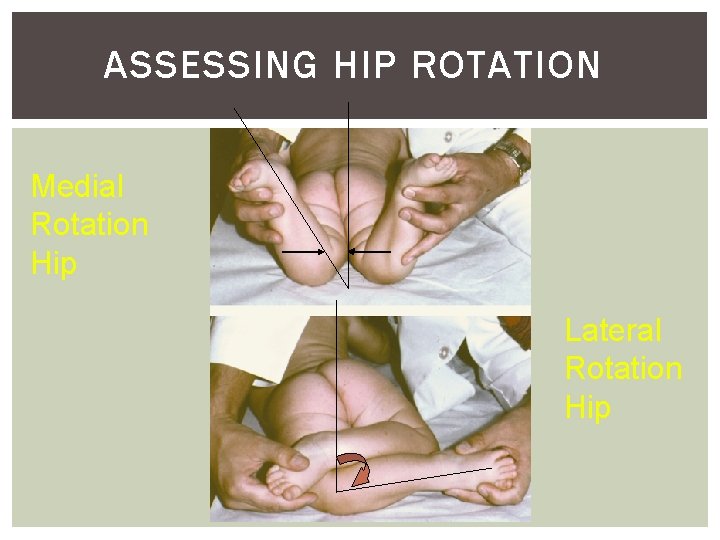
ASSESSING HIP ROTATION Medial Rotation Hip Lateral Rotation Hip
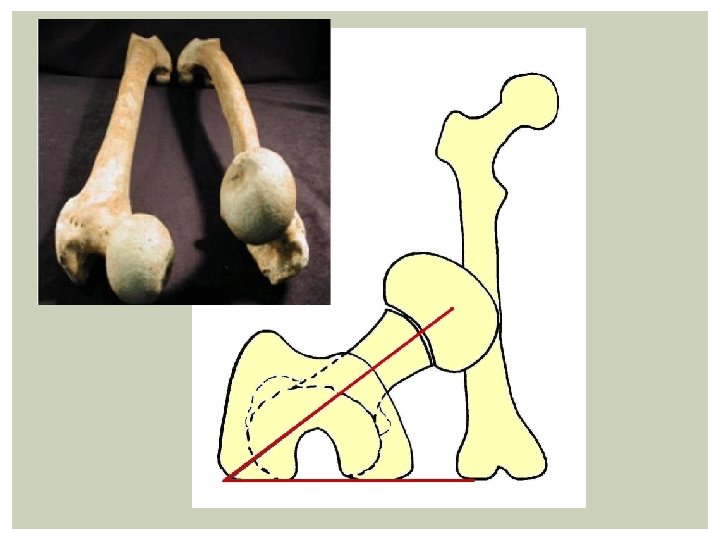
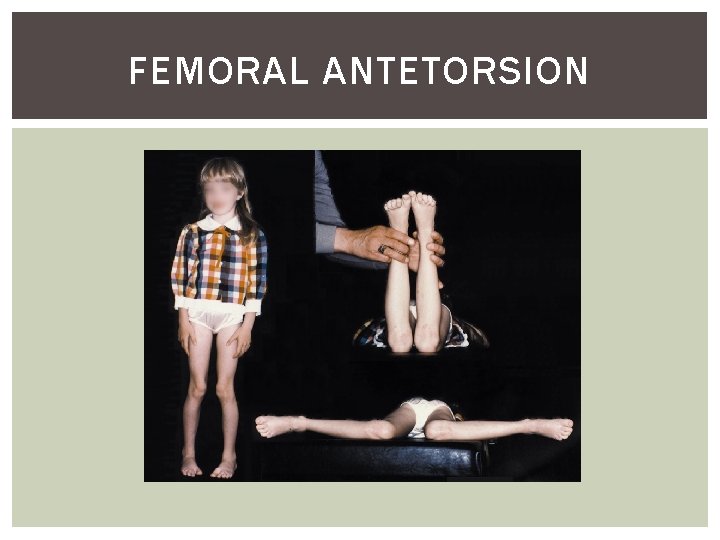
FEMORAL ANTETORSION
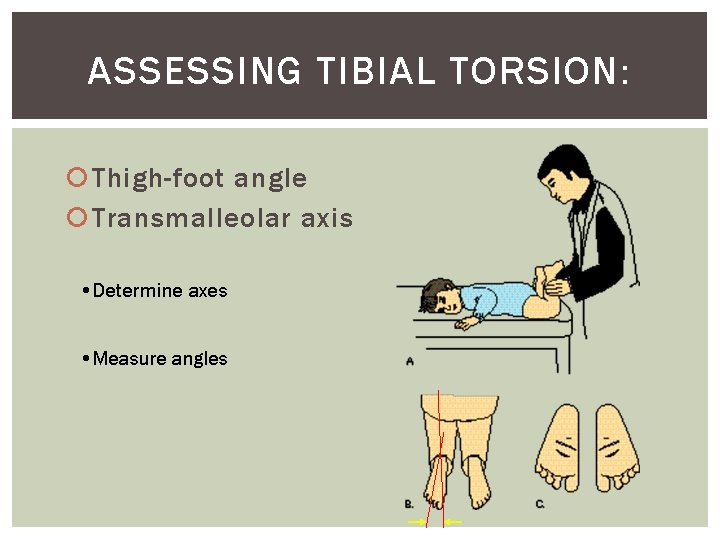
ASSESSING TIBIAL TORSION: Thigh-foot angle Transmalleolar axis • Determine axes • Measure angles
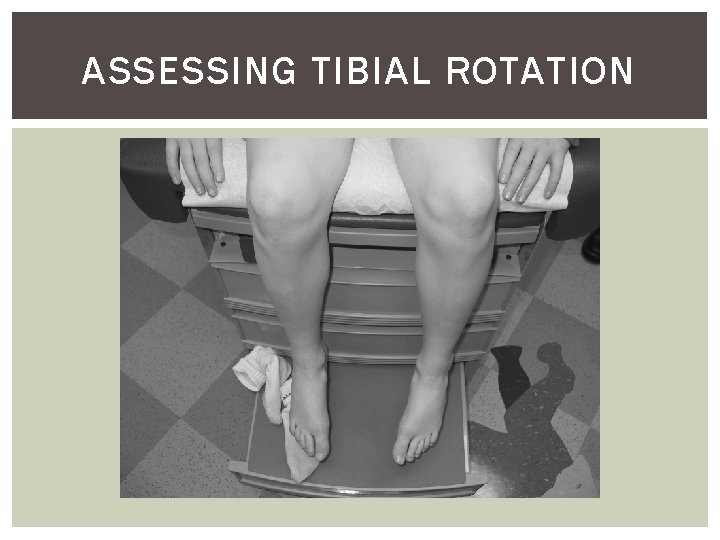
ASSESSING TIBIAL ROTATION
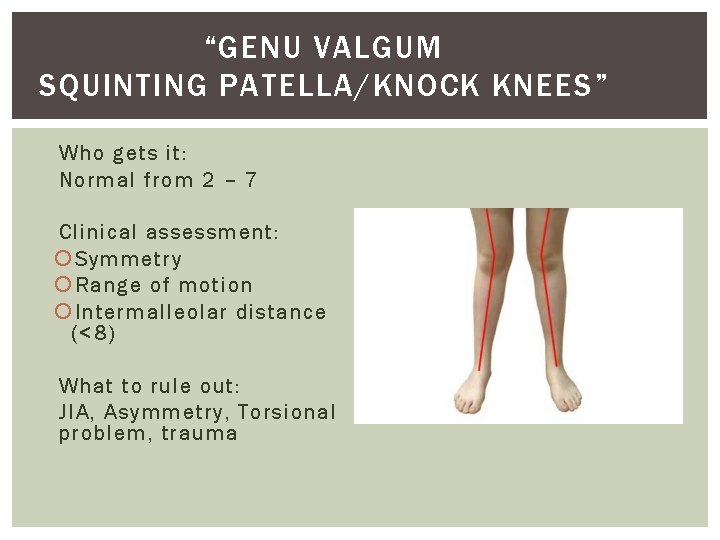
“GENU VALGUM SQUINTING PATELLA/KNOCK KNEES” Who gets it: Normal from 2 – 7 Clinical assessment : Symmetry Range of motion Intermalleolar distance (<8) What to rule out: JIA, Asymmetry, Torsional problem, trauma

ASYMMETRY
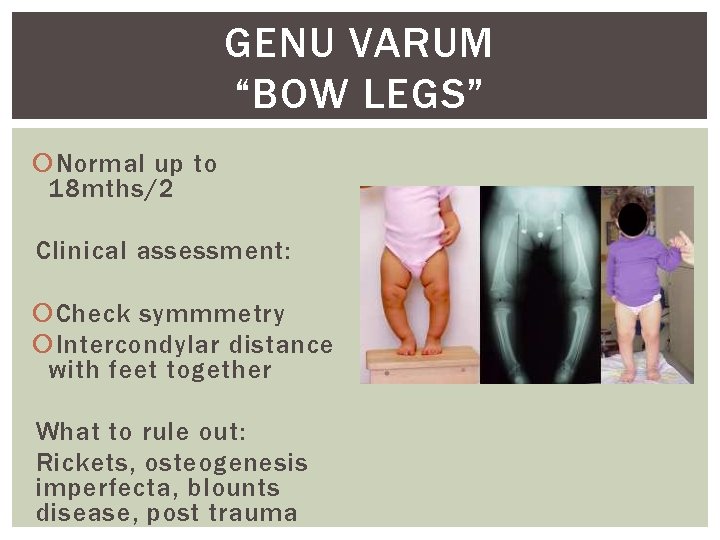
GENU VARUM “BOW LEGS” Normal up to 18 mths/2 Clinical assessment: Check symmmetry Intercondylar distance with feet together What to rule out: Rickets, osteogenesis imperfecta, blounts disease, post trauma
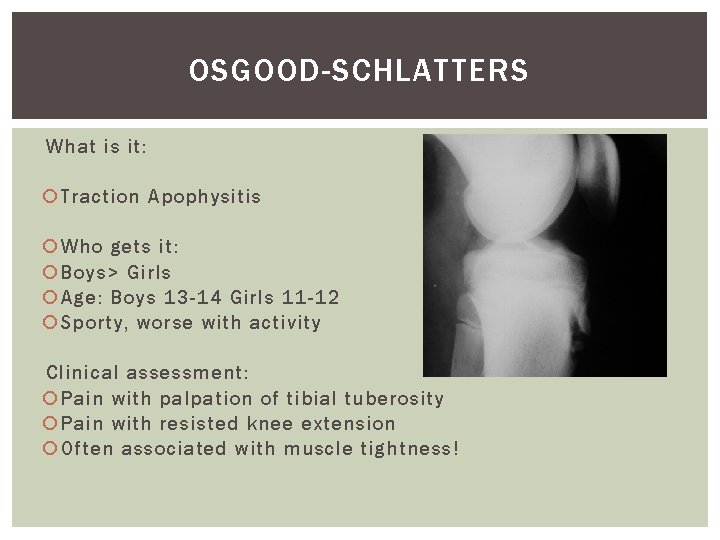
OSGOOD-SCHLATTERS What is it: Traction Apophysitis Who gets it: Boys> Girls Age: Boys 13 -14 Girls 11 -12 Sporty, worse with activity Clinical assessment: Pain with palpation of tibial tuberosity Pain with resisted knee extension Often associated with muscle tightness!
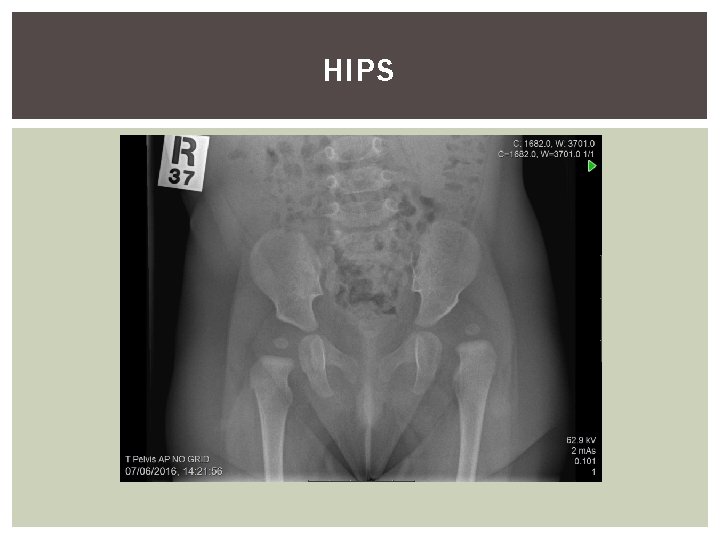
HIPS
THE HIP NB children are poor locators of pain, and hip pain is often referred to the knee! Complete hip ax for all children complaining of knee pain.
ABNORMAL HIP MOTION THINGS TO WATCH OUT FOR 1. DDH 2. PERTHES DISEASE 3. SCFE
PATHOLOGIES TO CONSIDER Infants and toddlers § Hip dysplasia § Neuromuscular disease -Cerebral palsy Toddlers § Legg-Calve-Perthes disease Pre-teens § Legg-Calve-Perthes disease § Slipped Capital femoral epiphysis
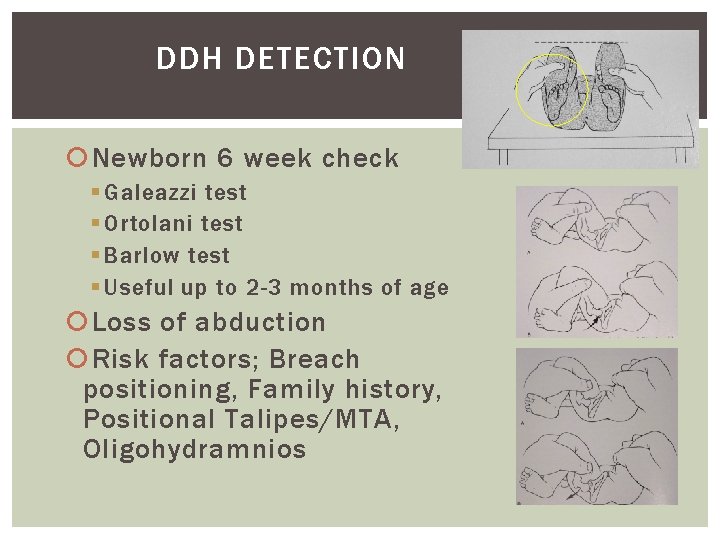
DDH DETECTION Newborn 6 week check § Galeazzi test § Ortolani test § Barlow test § Useful up to 2 -3 months of age Loss of abduction Risk factors; Breach positioning, Family history, Positional Talipes/MTA, Oligohydramnios

DDH
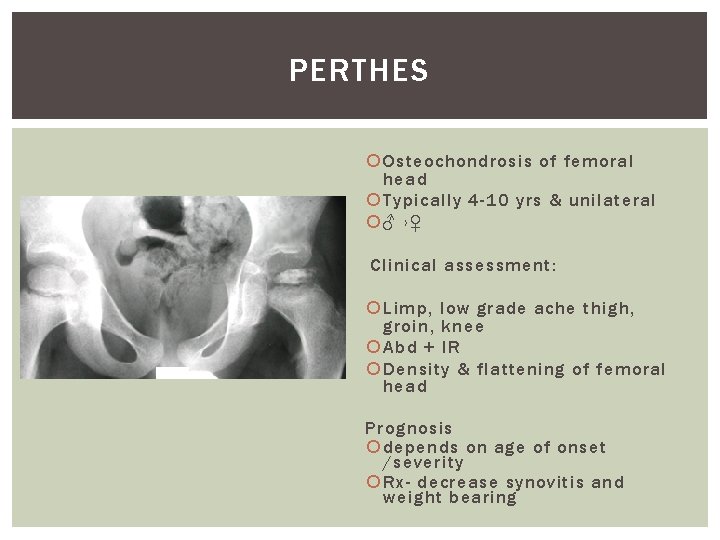
PERTHES Osteochondrosis of femoral head Typically 4 -10 yrs & unilateral ♂ ›♀ Clinical assessment: Limp, low grade ache thigh, groin, knee Abd + IR Density & flattening of femoral head Prognosis depends on age of onset /severity Rx- decrease synovitis and weight bearing
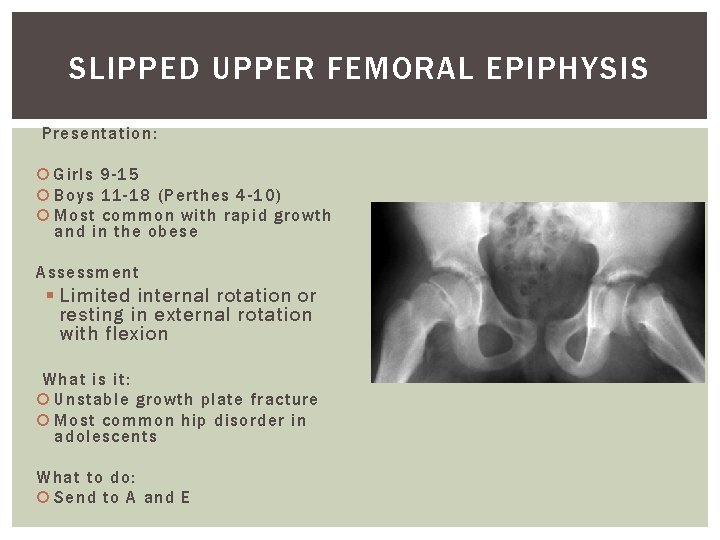
SLIPPED UPPER FEMORAL EPIPHYSIS Presentation: Girls 9 -15 Boys 11 -18 (Perthes 4 -10) Most common with rapid growth and in the obese Assessment § Limited internal rotation or resting in external rotation with flexion What is it: Unstable growth plate fracture Most common hip disorder in adolescents What to do: Send to A and E
TOE WALKING • Neurological immaturity, thus normal variant in young children • Autism and behavioural abnormalities • Congenital short TA • Cerebral palsy BEWARE UNILATERAL TOE-WALKER
TOP TIPS: Assess!!! Remember the 5 S’s § Symmetry § Stiffness § Symptoms § Skeletal Dysplasia § Systemic Illness Exclude Potential Worrying Pathology If in doubt, liaise with colleague and complete referrals
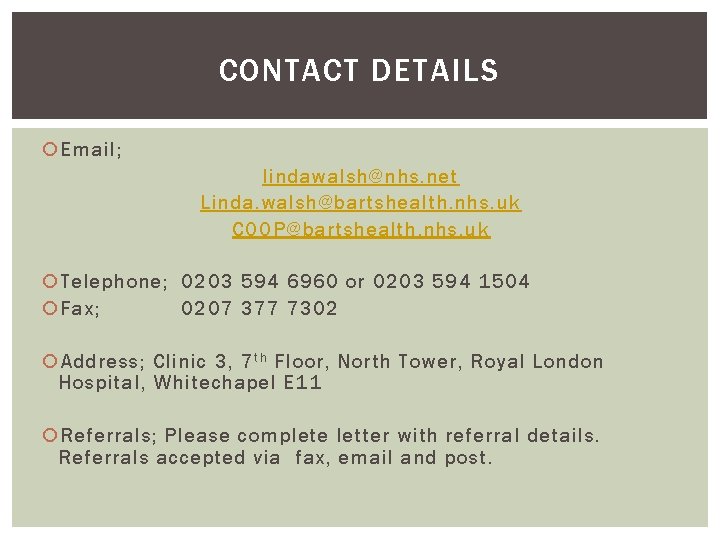
CONTACT DETAILS Email; lindawalsh@nhs. net Linda. walsh@bartshealth. nhs. uk COOP@bartshealth. nhs. uk Telephone; 0203 594 6960 or 0203 594 1504 Fax; 0207 377 7302 Address; Clinic 3, 7 t h Floor, North Tower, Royal London Hospital, Whitechapel E 11 Referrals; Please complete letter with referral details. Referrals accepted via fax, email and post.

THANK YOU!!!
- Slides: 40