CHILDHOOD OBESITY BY MBBSPPT COM Obesity in children
CHILDHOOD OBESITY BY MBBSPPT. COM
Obesity in children: An emerging concern Ø Common nutritional problem Ø In USA 22% of children and adolescents overweight Ø Prevalence increased by almost 50% in last 2 decades Ø In India: High prevalence among the urban affluent adolescents Delhi: 24. 7% overweight, 7. 4% obese Chennai: 9. 6% overweight, 6% obese Jaipur: 10. 1% overweight
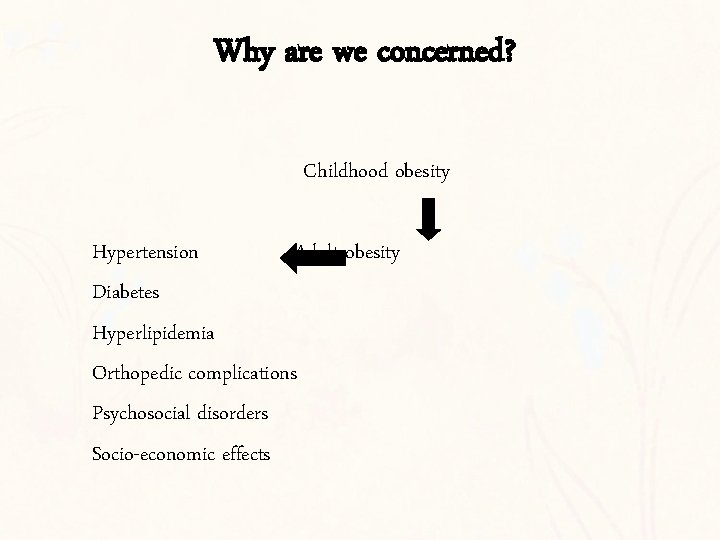
Why are we concerned? Childhood obesity Hypertension Adult obesity Diabetes Hyperlipidemia Orthopedic complications Psychosocial disorders Socio-economic effects
Obese child: obese adult Ø 10 -20% of obese infants are obese as children Ø 40% of obese children are obese during adolescence Ø 75 -80% of obese adolescents become obese adults >1/3 rds of obese children are obese as adults
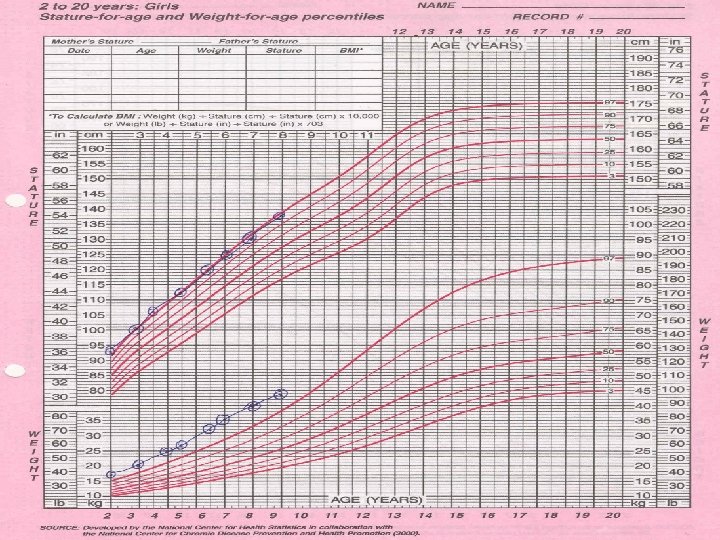
Definition & diagnostic criteria Excess body weight in relation to lean body mass Weight for height >120% Ø Does not account for body frame/ muscle mass Ø Longitudinal assessment desirable
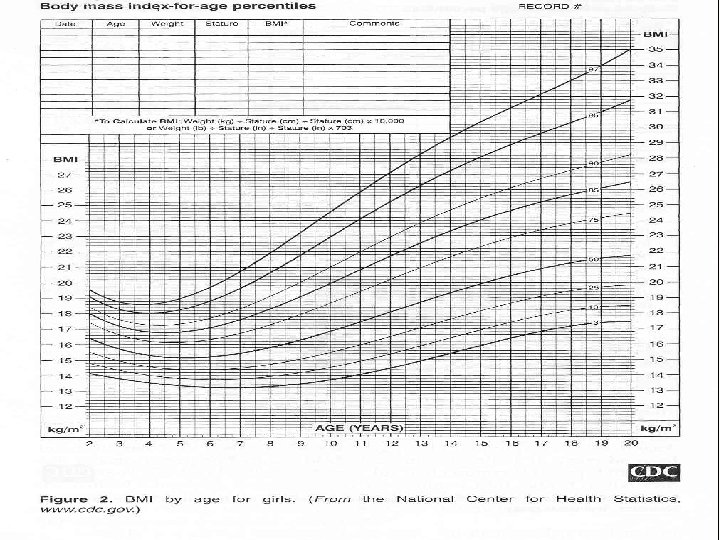
BMI: wt (Kg)/Ht(m)2 Adults: > 25 – Overweight > 30 – Obese BMI > 25: Increased risk of medical Children: BMI for age & sex > 85 th centile: At risk for obesity >95 th centile: Obese complications
v. Skin fold thickness: Estimation of regional fat distribution v. Waist Hip Ratio: WHR> 0. 8: Hyper-insulinemia, insulin resistance, NIDDM in adults v. Visceral - subcutaneous fat ratio: Estimates total & regional body adiposity Visceral fat associated with dyslipidemia, hyperinsulinemia & cardiac risk
Cause of Simple Obesity Imbalance of energy intake and output Multi-factorial origin Genetic Factors Strong role of parental fatness Ø Both obese : 80% children obese Ø One obese : 40% children obese Ø None obese : 14% children obese Rise in prevalence too steep to be accounted for by heredity
Mechanism Ø Increased metabolic efficiency Lower BMR: BMR of children with at-least one obese parent 10% lower than children of lean parents Ø Lower spontaneous physical activity: Decreased energy expenditure upto 500 Cal/day in obese children as a result of spontaneous activity(ie fidgeting)
Environmental factors Ø Sedentary life style: 20% children do not perform > 2 hrs of rigorous physical activity/ week Ø TV viewing/computers: 33% of 10 -15 year olds watch > 5 hrs of TV/day Ø Unlimited access to food Ø Academic pressures Ø Feeding practices: Eating out Eating in front of TV Skipping breakfast Ø ? Over-estimated energy requirements
Dietary factors Ø Unlimited availability of palatable and high Cal density food Ø Increased soft drink consumption Ø Amount of fat in household cooking Ø Decreased energy requirement in obese due to decreased fat free mass Ø is-reporting of food intake & physical activity
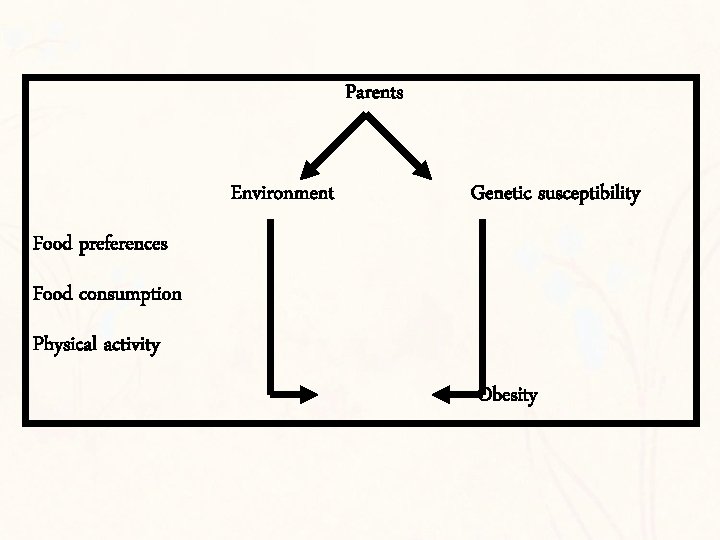
Parents Environment Genetic susceptibility Food preferences Food consumption Physical activity Obesity
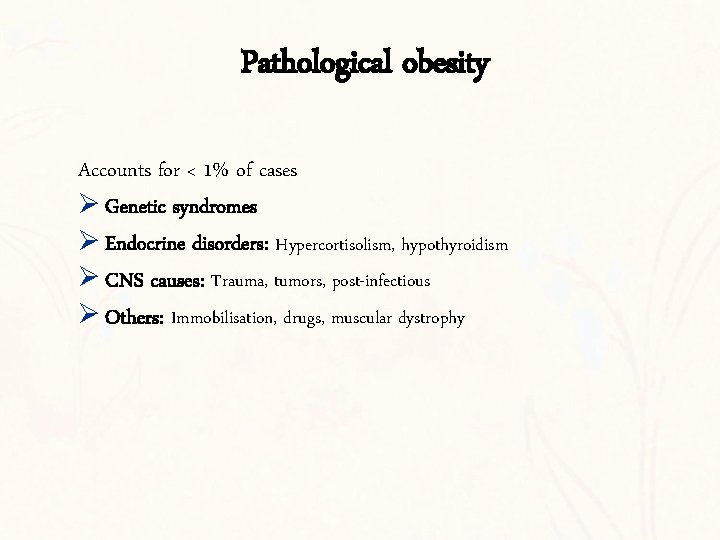
Pathological obesity Accounts for < 1% of cases Ø Genetic syndromes Ø Endocrine disorders: Hypercortisolism, hypothyroidism Ø CNS causes: Trauma, tumors, post-infectious Ø Others: Immobilisation, drugs, muscular dystrophy
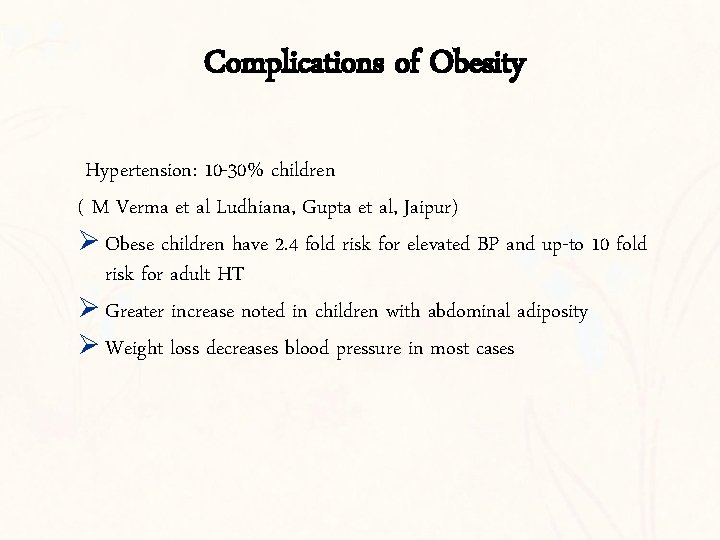
Complications of Obesity Hypertension: 10 -30% children ( M Verma et al Ludhiana, Gupta et al, Jaipur) Ø Obese children have 2. 4 fold risk for elevated BP and up-to 10 fold risk for adult HT Ø Greater increase noted in children with abdominal adiposity Ø Weight loss decreases blood pressure in most cases
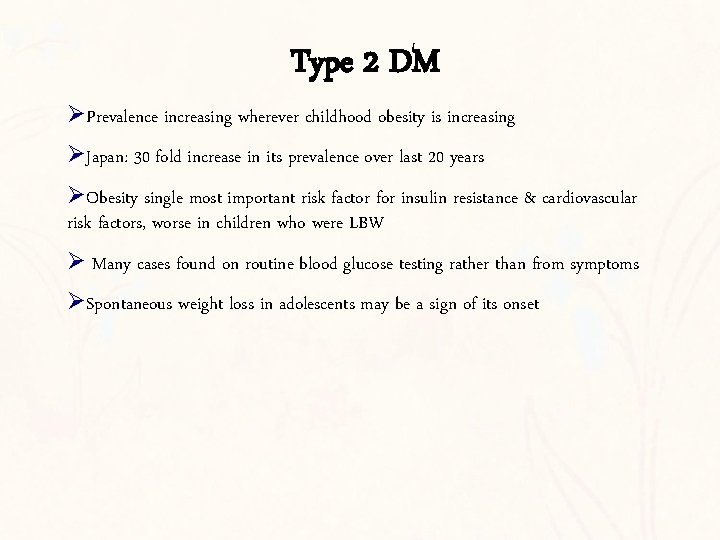
Type 2 DM ØPrevalence increasing wherever childhood obesity is increasing ØJapan: 30 fold increase in its prevalence over last 20 years ØObesity single most important risk factor for insulin resistance & cardiovascular risk factors, worse in children who were LBW Ø Many cases found on routine blood glucose testing rather than from symptoms ØSpontaneous weight loss in adolescents may be a sign of its onset
Complications contd Ø Hypercholesterolemia, decreased HDL, increased TG, LDL Increased risk of CAD Ø Early menarche, menstrual disturbances Ø Orthopedic Complications: Genu valgum, slipped femoral head epiphysis, Blount disease, flat feet Ø Sleep apnea: central & obstructive, chronic hypoxemia, hypercapnea, day time somnolence Ø Inter-triginous infections
Psychological complications ØViewed as clumsy, unattractive, over-indulgent ØTeased on the play ground, excluded from games ØLowered self-image, withdrawal from social contact
Evaluation of an obese child: History Ø Dietary details Ø Activity pattern Ø Mental development Ø School performance Ø Drug intake, H/O CNS injury/infection Ø Psycho-social concerns Ø Prevalence of obesity & body fat distribution in other family members Ø Risk of obesity related morbidity in family
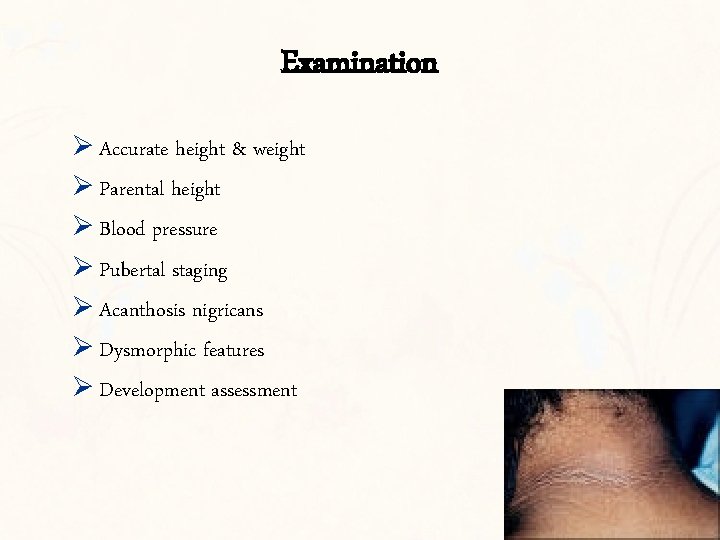
Examination Ø Accurate height & weight Ø Parental height Ø Blood pressure Ø Pubertal staging Ø Acanthosis nigricans Ø Dysmorphic features Ø Development assessment
Investigations Guided by clinical presentation Simple obesity: Ø Lipid profile Ø Fasting blood glucose Ø Bone age Suspected pathological obesity: Ø Thyroid profile Ø Plasma cortisol Ø GH studies Ø Pituitary evaluation
Management Ø Difficult & frustrating to treat Ø Physicians avoid taking care of obese children - Parental fault - Psychological problem Ø Dieticians hand out meal plans unsuccessful on previous many occasions
Some myths Ø Obesity equates with health Fact: Obese children have well documented morbidity Ø Obesity will reduce/disappear during growth Fact: It does not Ø Dietary restriction will impair normal growth and development Fact: only 2 -4% of daily energy requirement is used for growth & obese children are over-nourished
Aim of therapy Ø Life long weight control Ø Decrease energy intake while allowing normal growth Ø If weight reduction is planned: Serious commitment of all involved Ø Weight cycling to be avoided Ø Individualized plan according to the current eating pattern, intellect & degree of motivation
Therapeutic strategies Ø Nutrition education Ø Regular exercise program Ø Lifestyle/ behavior modification Ø Psychological & family therapy Ø ? Drugs Ø ? Surgery
Diet Ø Same nutritional principals as those for healthy children Ø Fats<30% of total calories, proteins 15% & CHO (mostly complex) >55% Ø Advisable to refrain from calorie counting Ø Avoid use of term “on diet”:
Diet therapy Severe dietary restriction avoided: Ø Loss of lean body mass, nutritional deficiencies & other unphysiological changes Ø May lead to repeated weight loss failures & non-compliance Ø Does not promote healthy eating behavior Ø Safety & long term benefits not documented in children
Diet therapy Ø Generally sufficient to reduce fat & sugar intake by avoiding high Cal & fried food Ø Reducing cooking fat Ø Avoiding mid-meal snacks/ replacing with low Cal snacks Ø Increasing fiber content Ø Ensuring family participation in the diet Ø Role of intensive dietary regimens: Limited to grossly obese children who have achieved their final height and have obesity related complications: Protein sparing modified fast (PSMF)
Exercise Ø Important conjunct to diet therapy in a wt loss program Ø Little effect on short term wt loss but significant long term advantage Ø Ensure that active games are viewed as fun Ø Build up slowly keeping in mind child’s preferences
Behavior modification & Social Support Ø Backbone of effective weight loss program Ø Convince entire family regarding need for weight loss & ensure their participation Ø Encourage other obese family members to lose weight Ø Encourage self monitoring of weight & Cal intake, goal setting
Drug therapy Ø Obesity is a chronic condition requiring continuous treatment Ø Both long & short term risks and benefits should be considered before drugs are prescribed Ø No long term, randomized, double blind, placebo controlled trials comparing the efficacy of drug treatment against that of a program including diet, exercise & behavior modification Ø In adults used for severe obesity with associated co-morbidities Ø Current role limited to research studies only
Drug therapy Mode of action: Ø Decreased energy intake Ø Increased energy output Ø Decreased absorption of nutrients Drugs currently recommended for use in adults: Ø Sibutramine –now banned Ø Orlistat Ø Metformin
Prevention: Critical period for intervention Critical periods for development of obesity: Ø Pre-natal period Ø Period of obesity rebound Ø Adolescence Pre-school years best period for intervention : Limit proliferation of adipose cells
Prevention Ø Parental education: Emphasize their role as models of healthy behavior Ø Knowledge regarding correct diet principles Ø Encourage development of healthy eating habits Ø Avoid force feeding Ø Keep fat intake moderate Ø Avoid fast foods, soft drinks Ø Sweets and other nutrient poor foods should be allowed in limited amounts
Prevention Ø Encourage physical sports & outdoor games Ø Restrict TV time Ø Schools should offer healthy food choices in cafeterias Ø Express affection & approval through ways other than food Ø Early focus on children at risk of obesity: specially those with obese parents or obese siblings Ø HEAT IT UP: Healthy eating and activity together
Challenge ahead: Role of physicians Ø Identify overweight & obese children: Take height and weight at visits Up-to 35% of parents do not recognize their weight problem Ø Look for obesity related complications Ø Promote a healthy life-style
Thank You
- Slides: 38