child youth Pediatric Telehealth Rounds Todays topic Sleep







- Slides: 69
child & youth Pediatric Telehealth Rounds Today’s topic: Sleep Disorders in Children Speaker: Dr. Hilary Myron MD FRCPC General Pediatrician March 10, 2017

If you are connected by videoconference: Please mute your system while the speaker is presenting. Complete today’s evaluation & apply for professional credits

Please feel free to ask questions! Complete today’s evaluation & apply for professional credits
By registering for today’s event… You may also want to… You will have had an opportunity to apply for professional credits or a certificate of attendance You will receive an email with a link to today’s online evaluation Visit our website to download slides and view archived events Sign-up to our distribution list to receive our event notifications Questions? pedtelehealthrounds@cheo. on. ca

Speaker has nothing to disclose with regard to commercial support. Declaration of conflict Speaker does not plan to discuss unlabeled/ investigational uses of commercial product.
Introduction
Objectives Learn the key elements of an age-appropriate history and physical examination to support the diagnosis of sleep disorders in children Recognize red-flag symptoms related to sleep disorders Identify key disorders of sleep in children
Overview Sleep 101 Childhood Sleep Requirements Disorders of Sleep History and Physical Cases Red Flags

Why Sleep? Restorative Memory & Cognition Growth and Development Protective (immunity)
Not Enough Sleep… Studies show that insufficient sleep in children and teens is associated with poorer outcomes for: Academic achievement tardiness and absenteeism attention, memory, abstract thinking, verbal creativity, working memory, organization, time management Physical health obesity risk metabolic dysfunction drowsy driving Mental health addictions aggression and poor impulse control vulnerability to stress

What is sleep? Non-REM Stages 1 & 2: Stage 3 (N 3): deep sleep, highly restorative children do most of this in first 1/3 of night plus one episode in early morning REM = dream sleep No muscle tone, only eye movement More and longer stretches as the night goes on Very important for memory and cognition
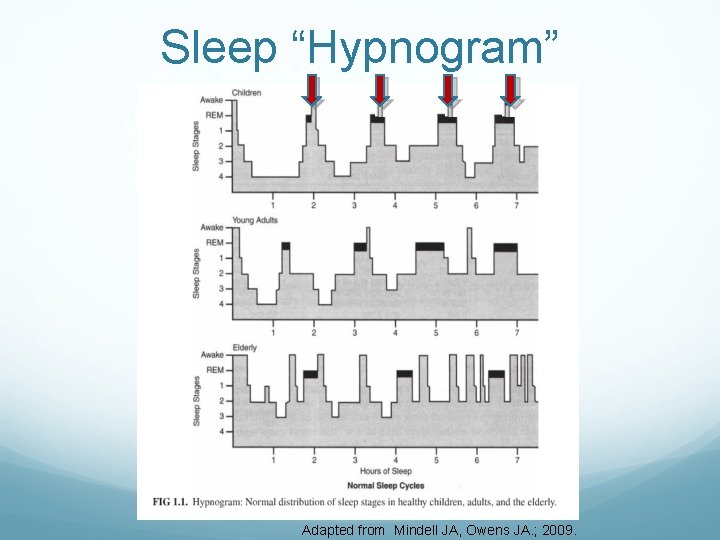
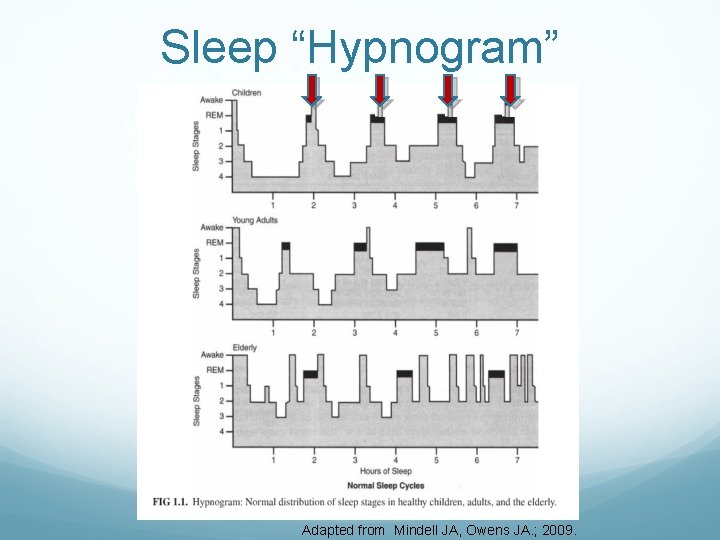
Sleep “Hypnogram” Adapted from Mindell JA, Owens JA. ; 2009.
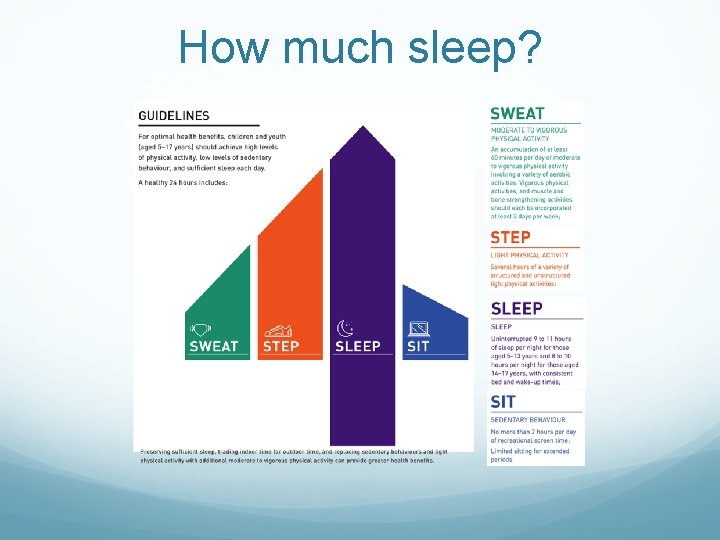
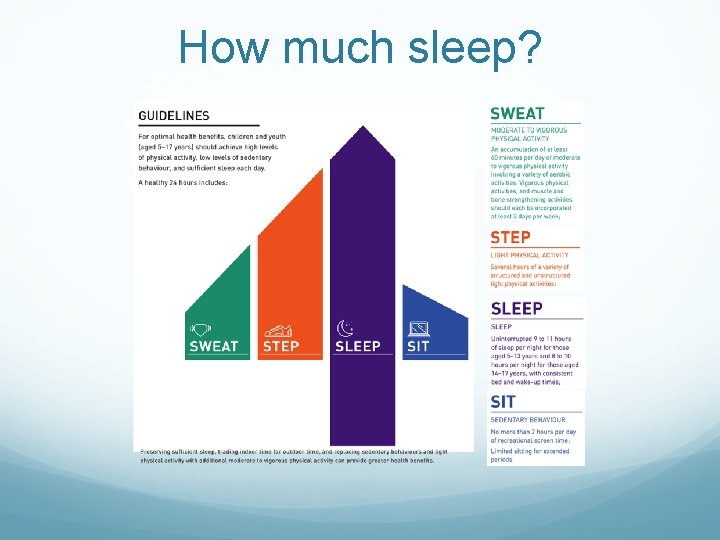
How much sleep?
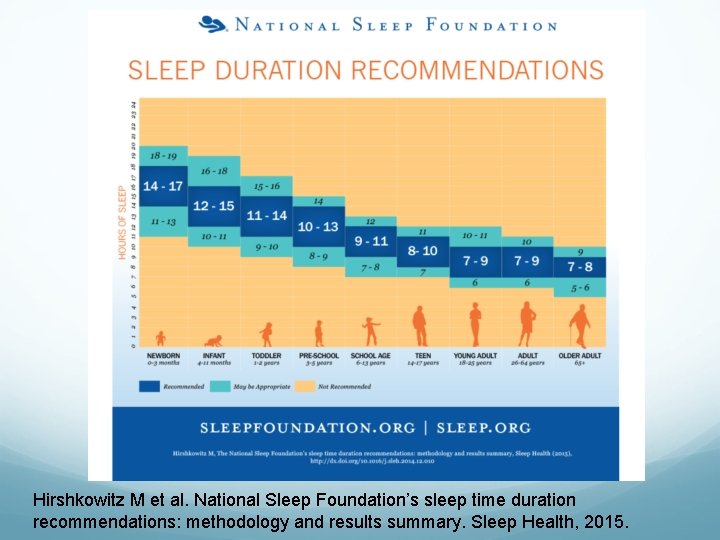
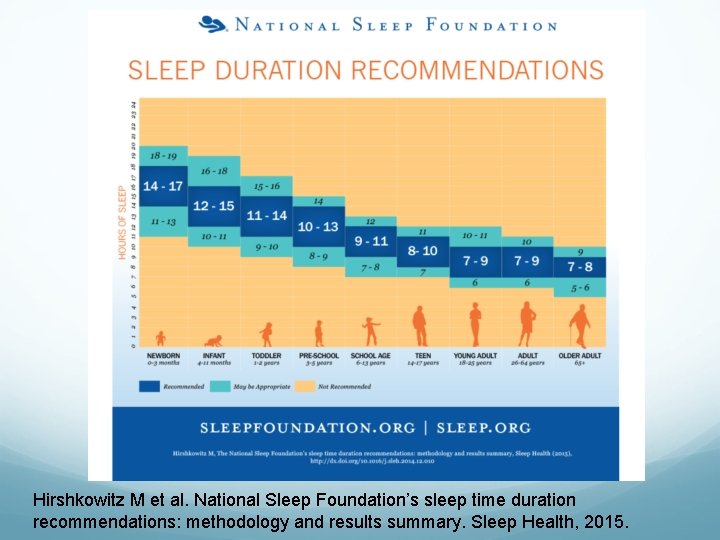
Hirshkowitz M et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health, 2015.
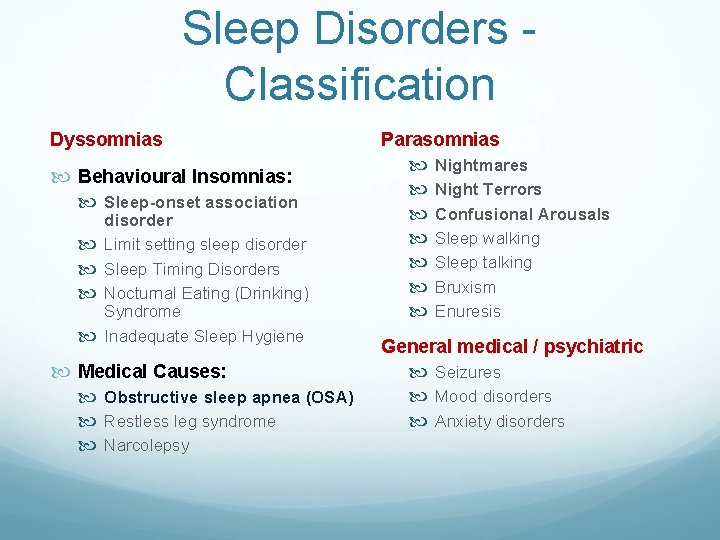
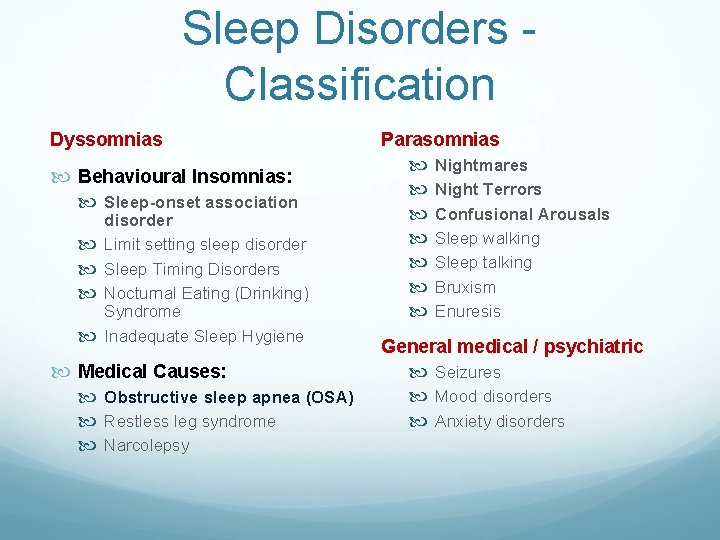
Sleep Disorders Classification Dyssomnias Behavioural Insomnias: Sleep-onset association disorder Limit setting sleep disorder Sleep Timing Disorders Nocturnal Eating (Drinking) Syndrome Inadequate Sleep Hygiene Medical Causes: Obstructive sleep apnea (OSA) Restless leg syndrome Narcolepsy Parasomnias Nightmares Night Terrors Confusional Arousals Sleep walking Sleep talking Bruxism Enuresis General medical / psychiatric Seizures Mood disorders Anxiety disorders
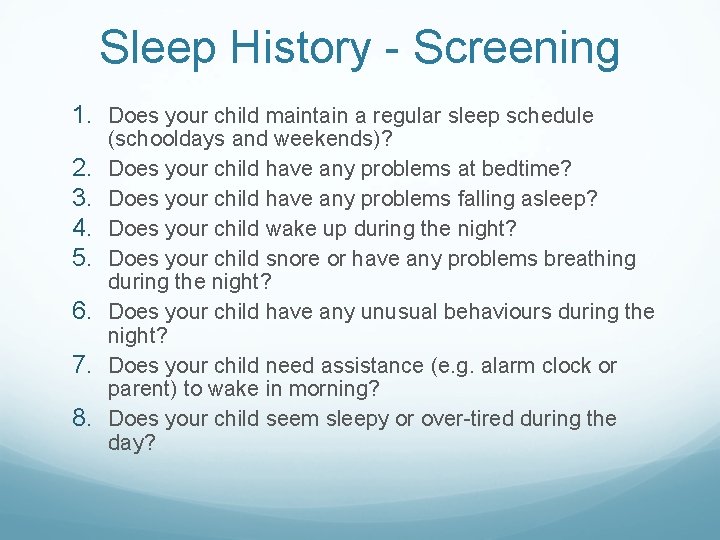
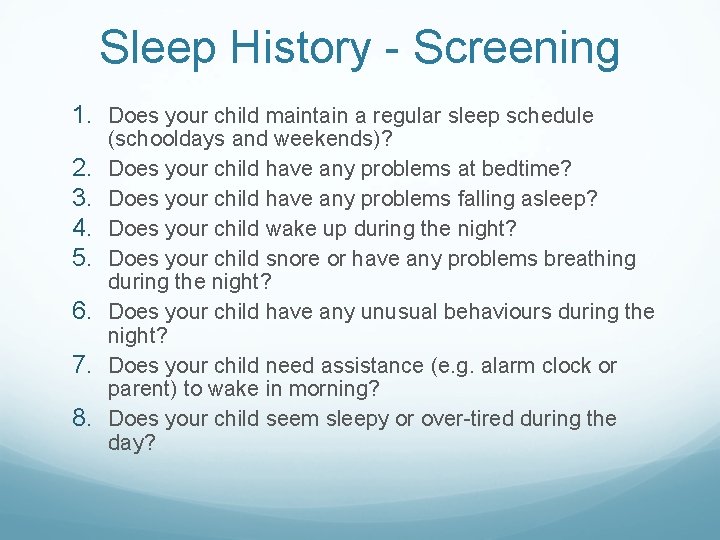
Sleep History - Screening 1. Does your child maintain a regular sleep schedule 2. 3. 4. 5. 6. 7. 8. (schooldays and weekends)? Does your child have any problems at bedtime? Does your child have any problems falling asleep? Does your child wake up during the night? Does your child snore or have any problems breathing during the night? Does your child have any unusual behaviours during the night? Does your child need assistance (e. g. alarm clock or parent) to wake in morning? Does your child seem sleepy or over-tired during the day?
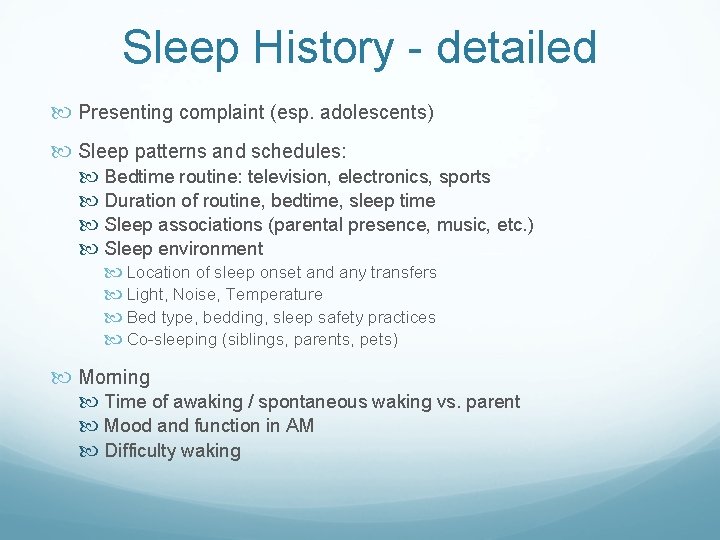
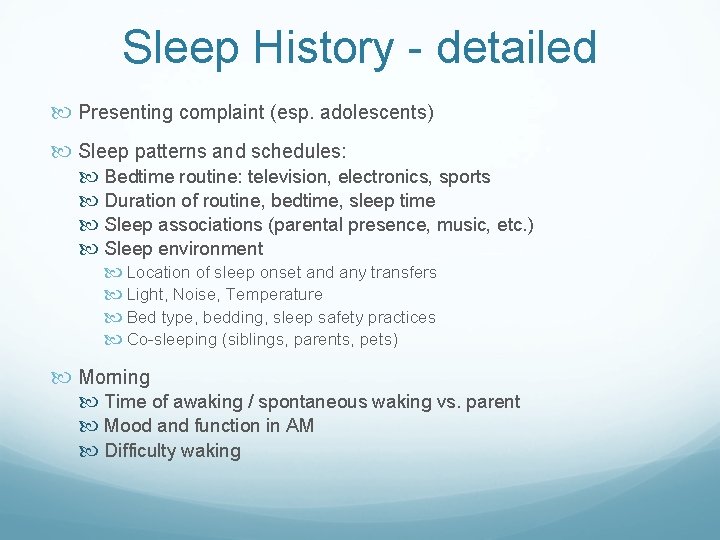
Sleep History - detailed Presenting complaint (esp. adolescents) Sleep patterns and schedules: Bedtime routine: television, electronics, sports Duration of routine, bedtime, sleep time Sleep associations (parental presence, music, etc. ) Sleep environment Location of sleep onset and any transfers Light, Noise, Temperature Bed type, bedding, sleep safety practices Co-sleeping (siblings, parents, pets) Morning Time of awaking / spontaneous waking vs. parent Mood and function in AM Difficulty waking
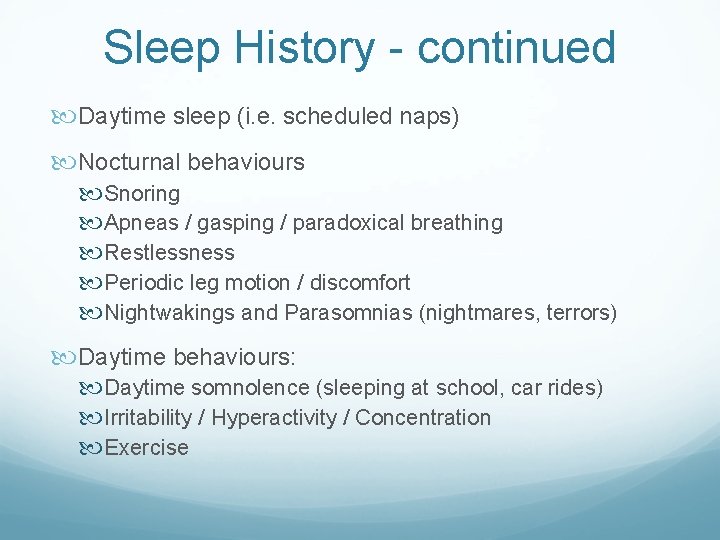
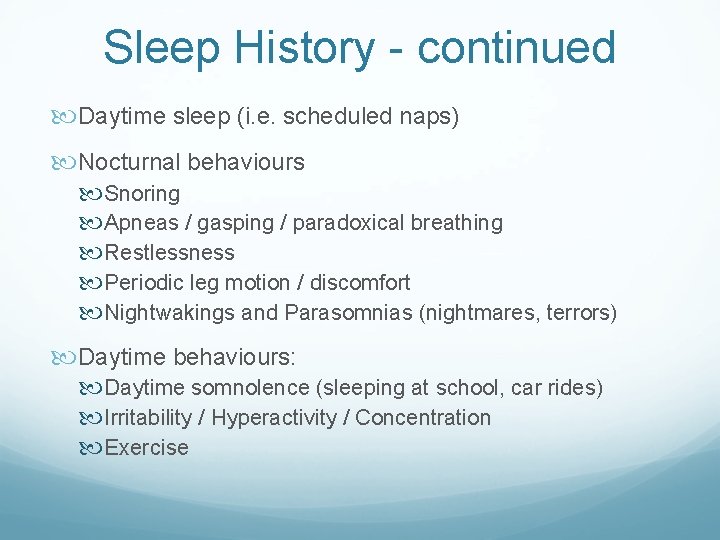
Sleep History - continued Daytime sleep (i. e. scheduled naps) Nocturnal behaviours Snoring Apneas / gasping / paradoxical breathing Restlessness Periodic leg motion / discomfort Nightwakings and Parasomnias (nightmares, terrors) Daytime behaviours: Daytime somnolence (sleeping at school, car rides) Irritability / Hyperactivity / Concentration Exercise
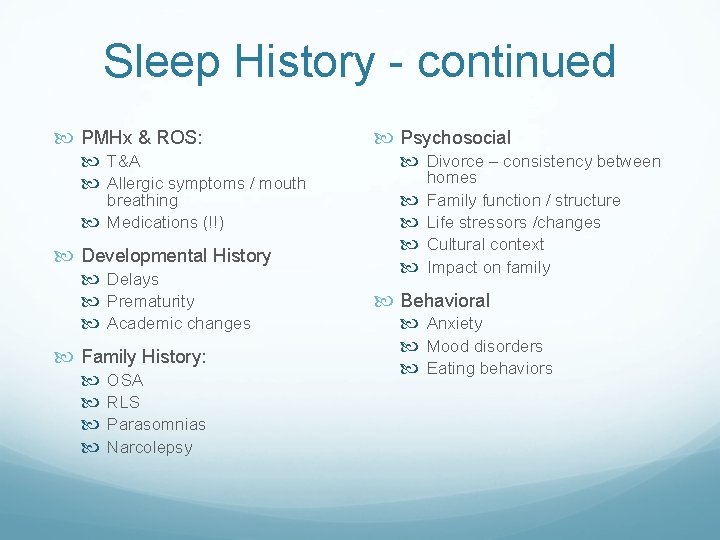
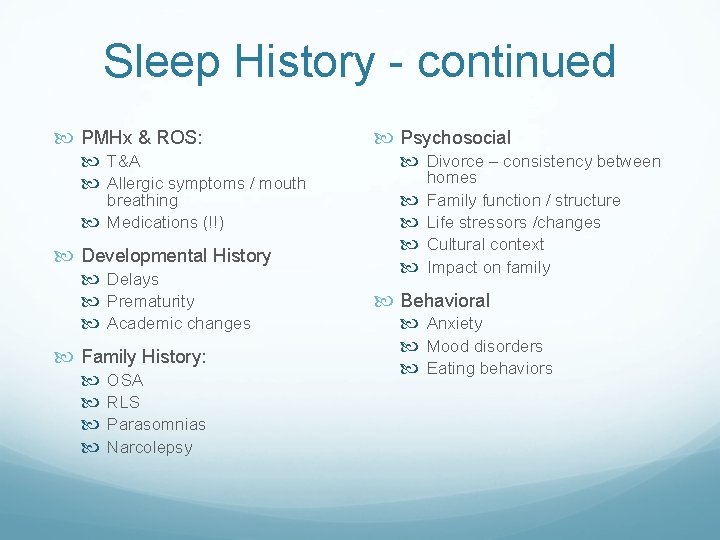
Sleep History - continued PMHx & ROS: T&A Allergic symptoms / mouth breathing Medications (!!) Developmental History Delays Prematurity Academic changes Family History: OSA RLS Parasomnias Narcolepsy Psychosocial Divorce – consistency between homes Family function / structure Life stressors /changes Cultural context Impact on family Behavioral Anxiety Mood disorders Eating behaviors
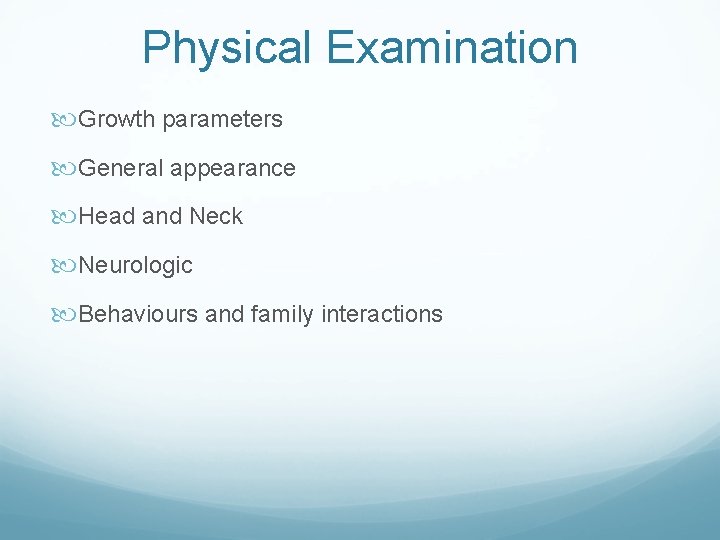
Physical Examination Growth parameters General appearance Head and Neck Neurologic Behaviours and family interactions
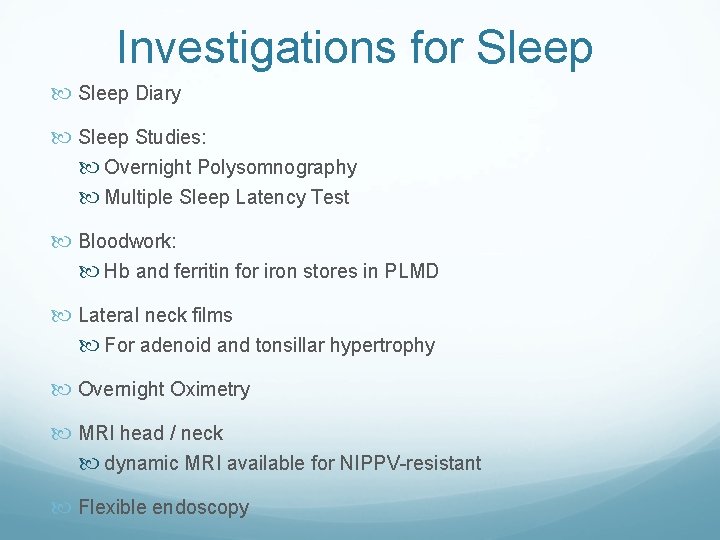
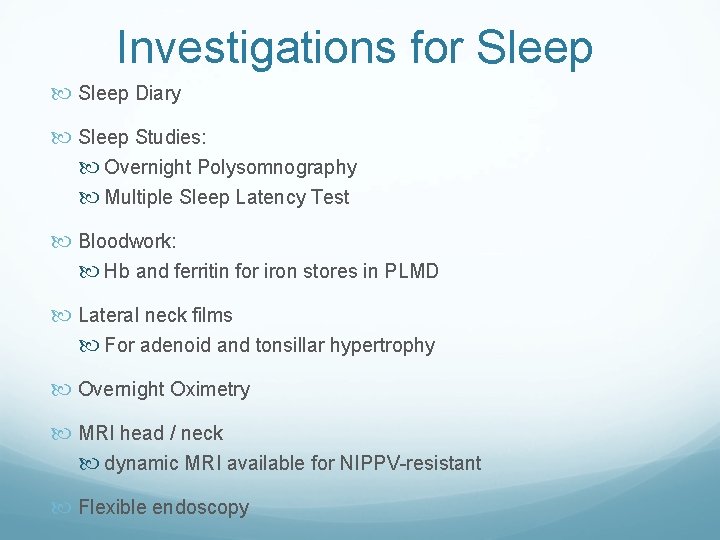
Investigations for Sleep Diary Sleep Studies: Overnight Polysomnography Multiple Sleep Latency Test Bloodwork: Hb and ferritin for iron stores in PLMD Lateral neck films For adenoid and tonsillar hypertrophy Overnight Oximetry MRI head / neck dynamic MRI available for NIPPV-resistant Flexible endoscopy
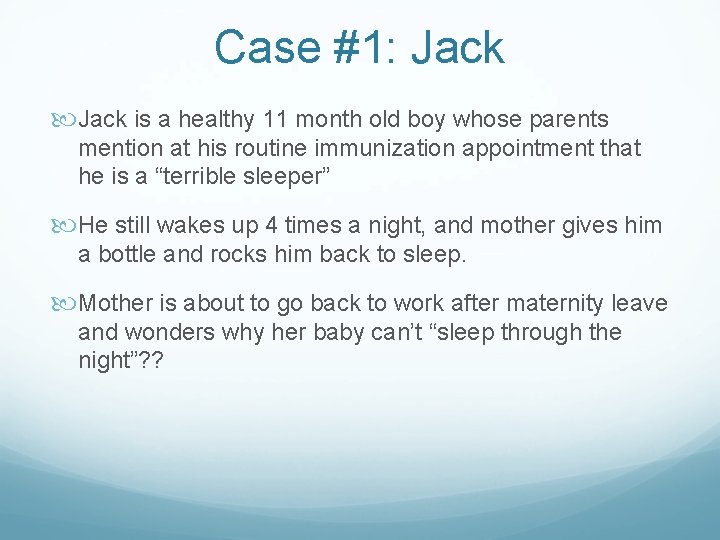
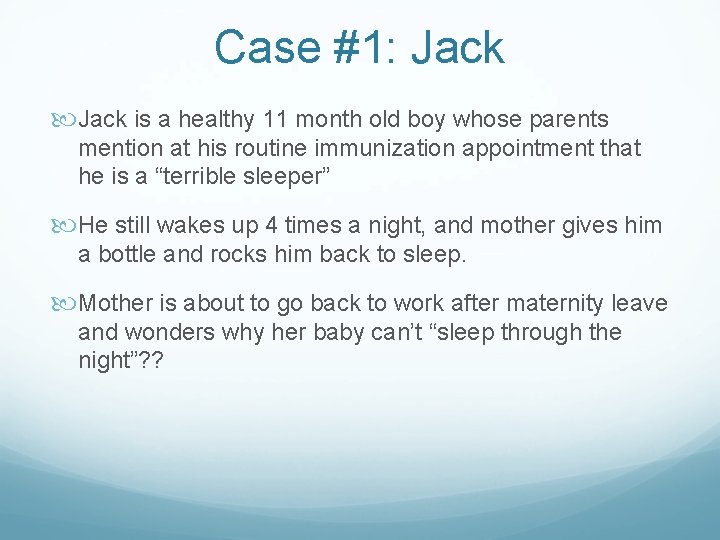
Case #1: Jack is a healthy 11 month old boy whose parents mention at his routine immunization appointment that he is a “terrible sleeper” He still wakes up 4 times a night, and mother gives him a bottle and rocks him back to sleep. Mother is about to go back to work after maternity leave and wonders why her baby can’t “sleep through the night”? ?
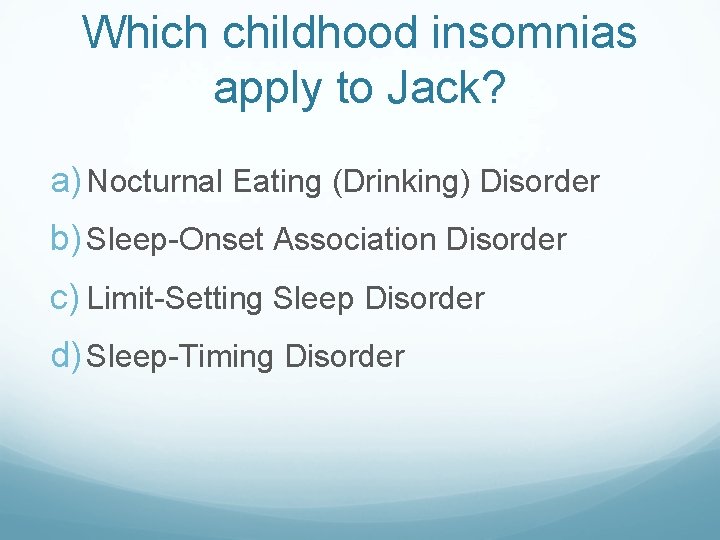
Which childhood insomnias apply to Jack? a) Nocturnal Eating (Drinking) Disorder b) Sleep-Onset Association Disorder c) Limit-Setting Sleep Disorder d) Sleep-Timing Disorder
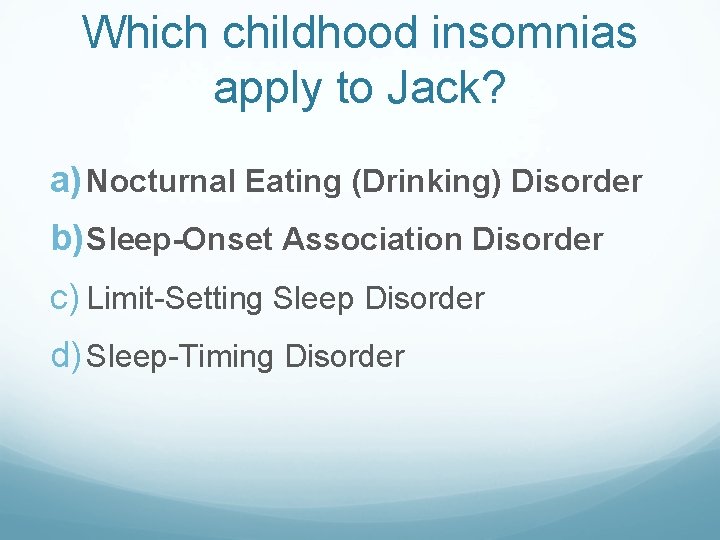
Which childhood insomnias apply to Jack? a) Nocturnal Eating (Drinking) Disorder b) Sleep-Onset Association Disorder c) Limit-Setting Sleep Disorder d) Sleep-Timing Disorder
Behavioural Insomnia 25% of all children will experience insomnia 80% of children with developmental disorders will experience insomnia Not all insomnias of childhood cause daytime fatigue in the child (usually in the parent!) The most common causes of childhood insomnias are behavioural Behaviour modification is highly effective at treating behavioural insomnias
“Sleep Training” Loaded terminology A variety of “methods”, “solutions” available in books, internet, sleep experts What all (well researched) methods have in common: 1. 2. 3. 4. Wean nocturnal feedings Help child to learn to fall asleep alone Set limits so child can fall asleep alone Adjust the timing of your child’s sleep preference
Nocturnal Eating (Drinking) Syndrome
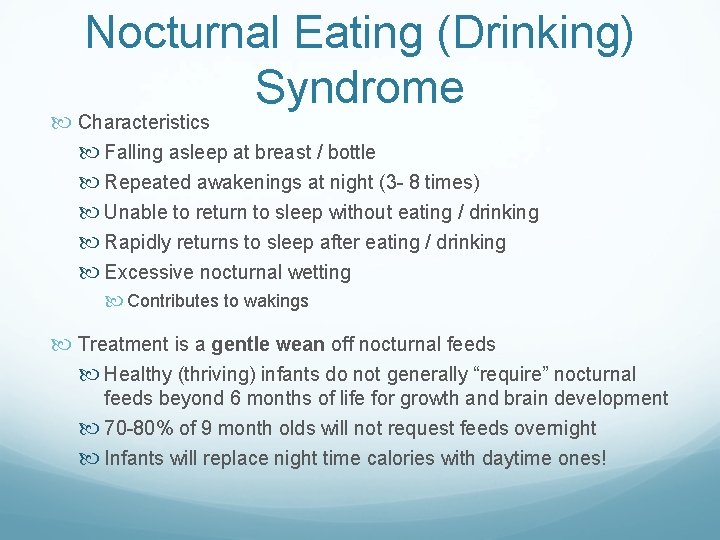
Nocturnal Eating (Drinking) Syndrome Characteristics Falling asleep at breast / bottle Repeated awakenings at night (3 - 8 times) Unable to return to sleep without eating / drinking Rapidly returns to sleep after eating / drinking Excessive nocturnal wetting Contributes to wakings Treatment is a gentle wean off nocturnal feeds Healthy (thriving) infants do not generally “require” nocturnal feeds beyond 6 months of life for growth and brain development 70 -80% of 9 month olds will not request feeds overnight Infants will replace night time calories with daytime ones!
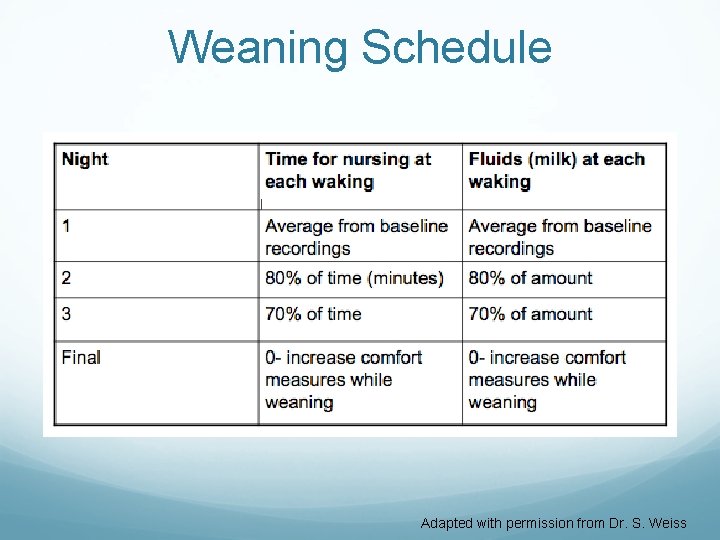
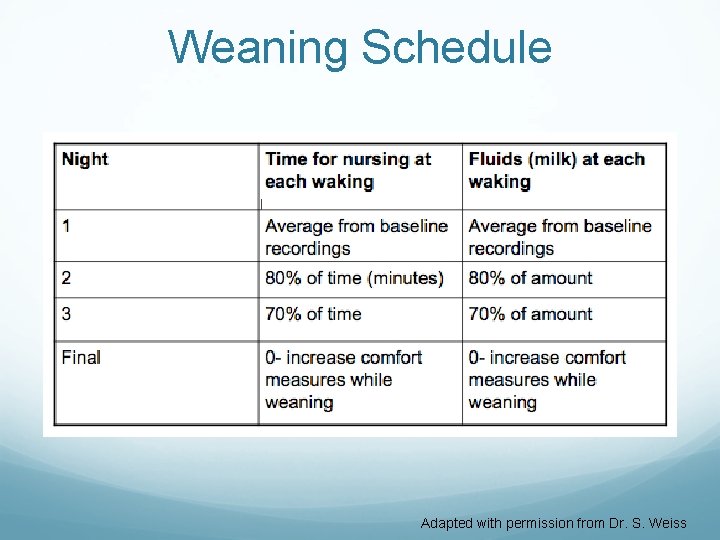
Weaning Schedule Adapted with permission from Dr. S. Weiss
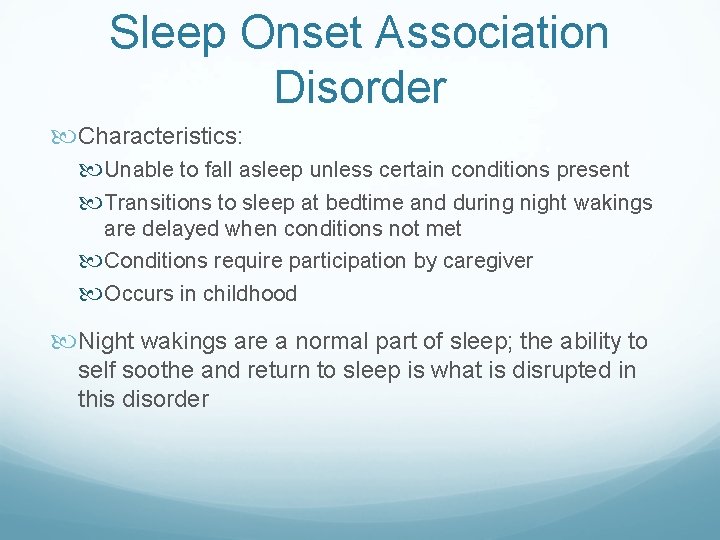
Sleep Onset Association Disorder Characteristics: Unable to fall asleep unless certain conditions present Transitions to sleep at bedtime and during night wakings are delayed when conditions not met Conditions require participation by caregiver Occurs in childhood Night wakings are a normal part of sleep; the ability to self soothe and return to sleep is what is disrupted in this disorder
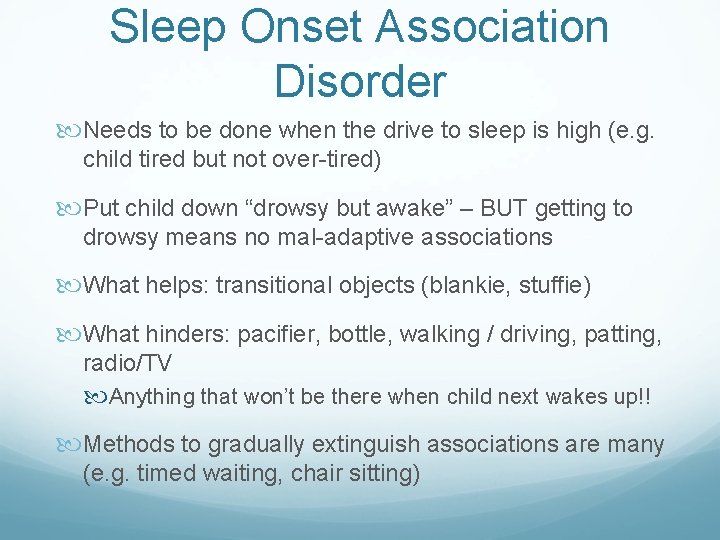
Sleep Onset Association Disorder Needs to be done when the drive to sleep is high (e. g. child tired but not over-tired) Put child down “drowsy but awake” – BUT getting to drowsy means no mal-adaptive associations What helps: transitional objects (blankie, stuffie) What hinders: pacifier, bottle, walking / driving, patting, radio/TV Anything that won’t be there when child next wakes up!! Methods to gradually extinguish associations are many (e. g. timed waiting, chair sitting)
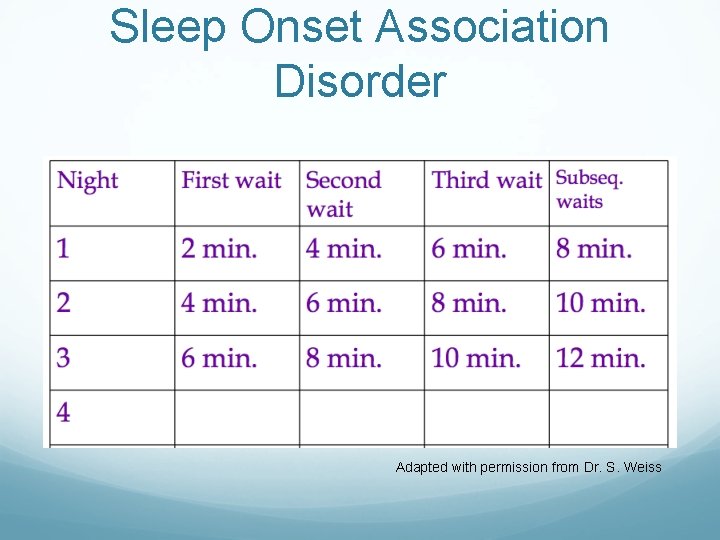
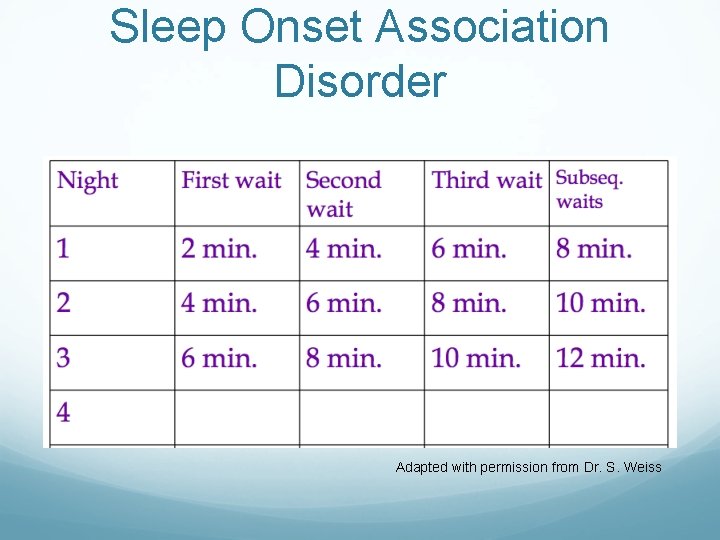
Sleep Onset Association Disorder Adapted with permission from Dr. S. Weiss
Case #2: Stephanie is a 16 year old competitive swimmer, and was referred for fatigue with daytime sleepiness. Her physical exam and bloodwork were normal.
Case#2: Stephanie When you inquire about her sleep, she describes coming home tired and taking a nap after school for 2 hours. She starts her homework at 11 PM while chatting online with her friends. She gets in bed at 2: 30 but often doesn’t fall asleep until 3: 30. She is supposed to be up at 5: 30 AM for swim practice, but cannot. She usually skips breakfast and is late for school. She drinks 3 cups of coffee per day
Circadian Rhythm Disorder A disconnect between desired sleep / wake times and internal circadian rhythms Examples: Delayed / Advanced sleep phase syndrome Change in rhythm from jet lag / shift work Non-24 -hr sleep-wake syndrome The majority of ALL behavioral sleep problems (especially children and teens) can be solved through attention to Sleep Hygiene Principles of sleep hygiene should begin in infancy and carry through childhood and into adulthood for healthy sleep
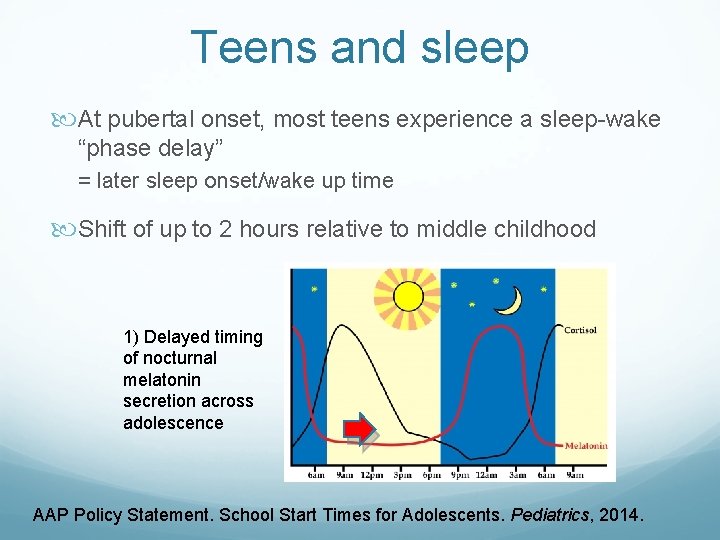
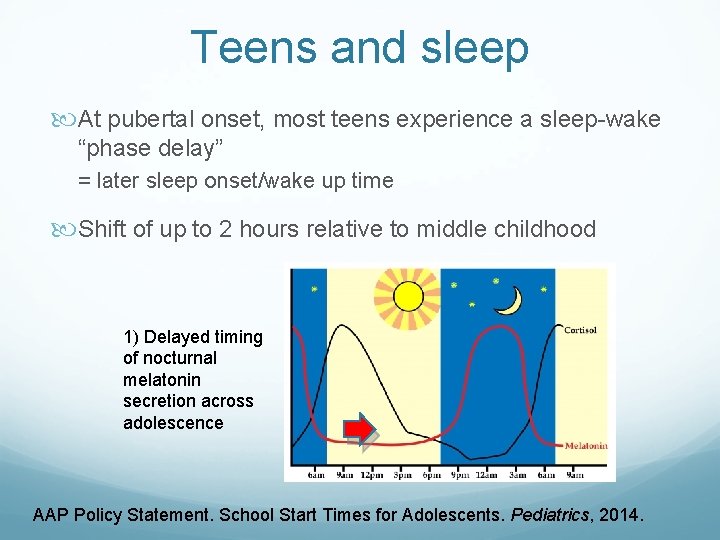
Teens and sleep At pubertal onset, most teens experience a sleep-wake “phase delay” = later sleep onset/wake up time Shift of up to 2 hours relative to middle childhood 1) Delayed timing of nocturnal melatonin secretion across adolescence AAP Policy Statement. School Start Times for Adolescents. Pediatrics, 2014.
Sleep Tips for everyone Regular sleep and wake times 7 days a week do not vary bedtime and wake time by more than 30 minutes ensure morning light exposure Keep all screens out of the bedrooms Establish a consistent bedtime routine Maintain a consistent, dark sleep environment Make sleep routines a priority!
Sleep Tips for Teens Avoid caffeine Support the teen in getting sufficient hours of sleep: help him / her to schedule the day to allow for enough sleep set limits on technology in the bedroom parents respect own sleep needs, and set a good example Advocate for reasonable school hours for teens, and demands on a teen’s time
American Academy of Pediatrics Says…Let them Sleep!
Devices and sleep!
Get devices out of the bedroom! Consider a family charging station Consider shutting off the internet at a defined hour every night Think about your own media use!
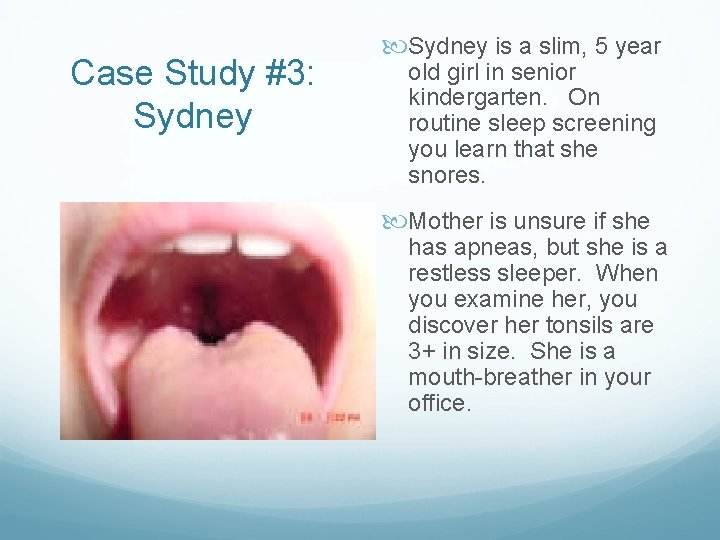
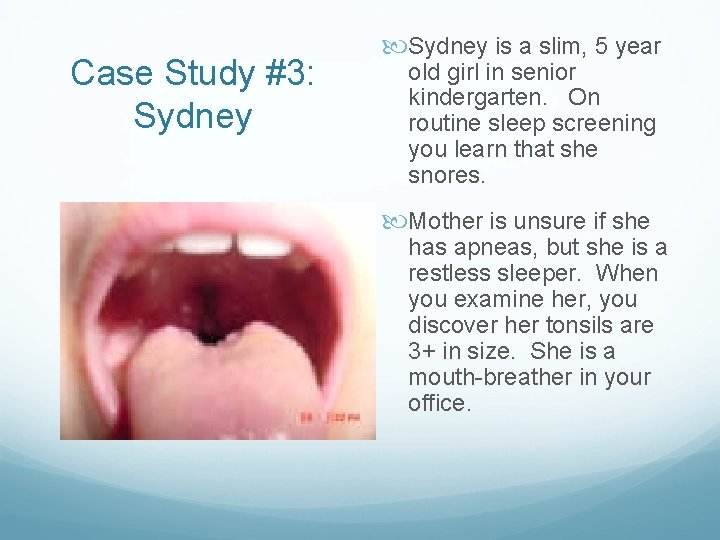
Case Study #3: Sydney is a slim, 5 year old girl in senior kindergarten. On routine sleep screening you learn that she snores. Mother is unsure if she has apneas, but she is a restless sleeper. When you examine her, you discover her tonsils are 3+ in size. She is a mouth-breather in your office.
What do you do? a) Order a sleep study b) Start her on CPAP c) Refer her to ENT for evaluation for tonsil and adeniodectomy d) Do an overnight oximetry e) Order a lateral next xray
What do you do? a) Order a sleep study b) Start her on CPAP c) Refer her to ENT for evaluation for tonsil and adeniodectomy d) Do an overnight oximetry e) Order a lateral neck xray
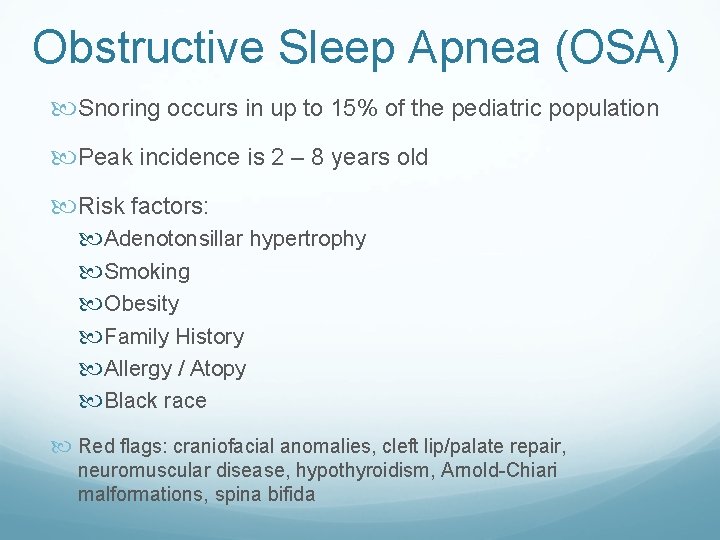
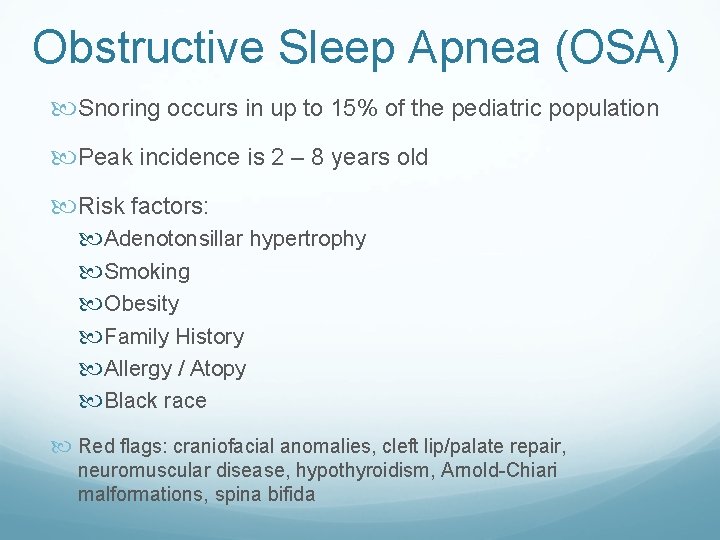
Obstructive Sleep Apnea (OSA) Snoring occurs in up to 15% of the pediatric population Peak incidence is 2 – 8 years old Risk factors: Adenotonsillar hypertrophy Smoking Obesity Family History Allergy / Atopy Black race Red flags: craniofacial anomalies, cleft lip/palate repair, neuromuscular disease, hypothyroidism, Arnold-Chiari malformations, spina bifida
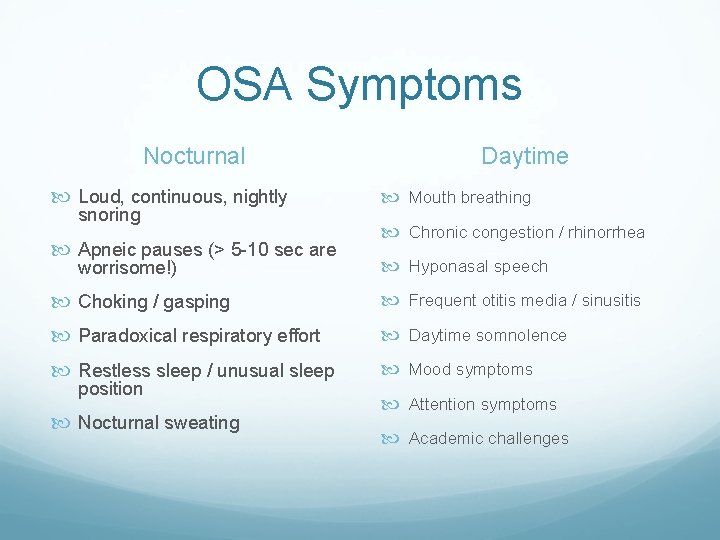
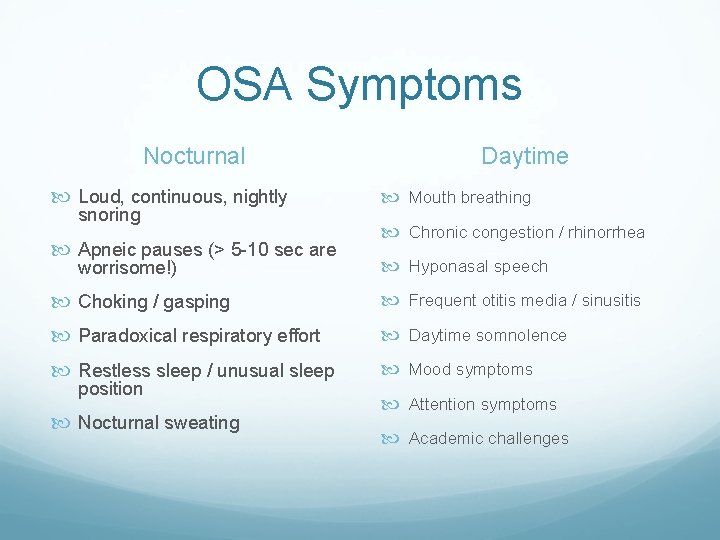
OSA Symptoms Nocturnal Loud, continuous, nightly snoring Apneic pauses (> 5 -10 sec are worrisome!) Daytime Mouth breathing Chronic congestion / rhinorrhea Hyponasal speech Choking / gasping Frequent otitis media / sinusitis Paradoxical respiratory effort Daytime somnolence Restless sleep / unusual sleep Mood symptoms position Nocturnal sweating Attention symptoms Academic challenges
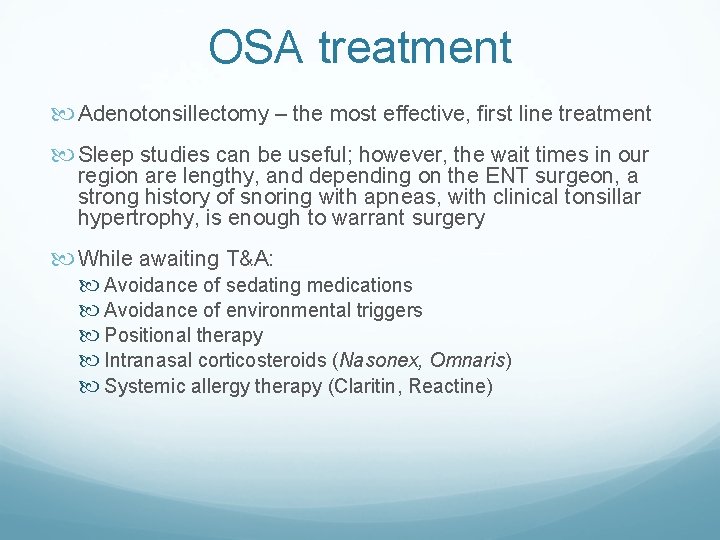
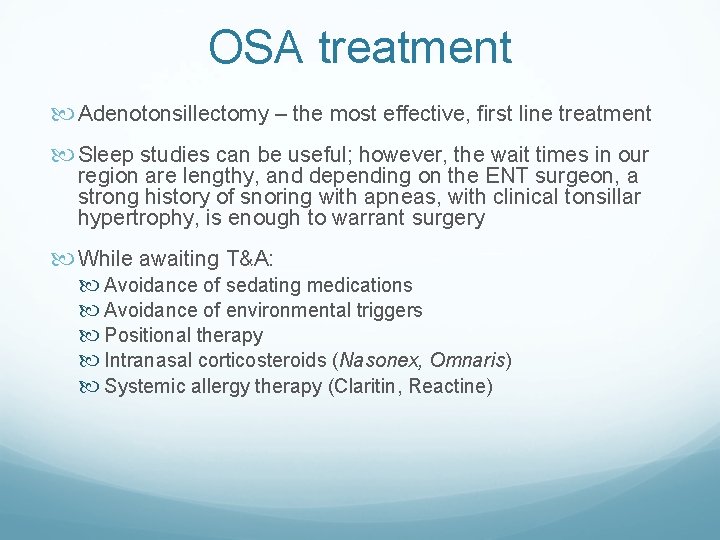
OSA treatment Adenotonsillectomy – the most effective, first line treatment Sleep studies can be useful; however, the wait times in our region are lengthy, and depending on the ENT surgeon, a strong history of snoring with apneas, with clinical tonsillar hypertrophy, is enough to warrant surgery While awaiting T&A: Avoidance of sedating medications Avoidance of environmental triggers Positional therapy Intranasal corticosteroids (Nasonex, Omnaris) Systemic allergy therapy (Claritin, Reactine)
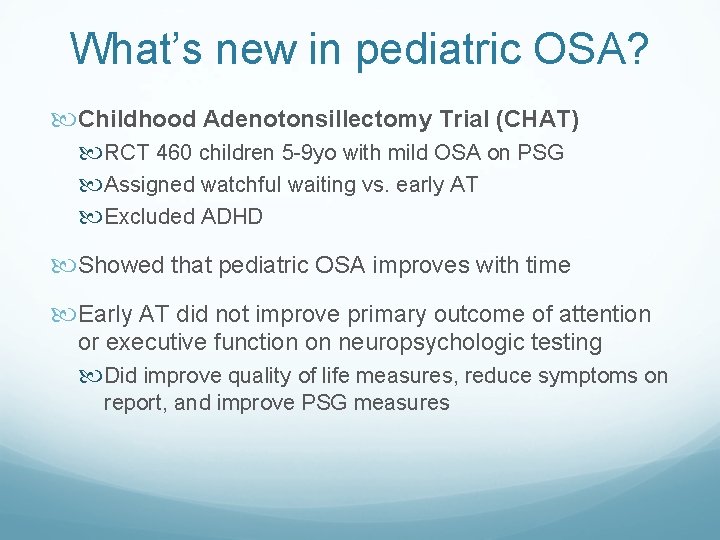
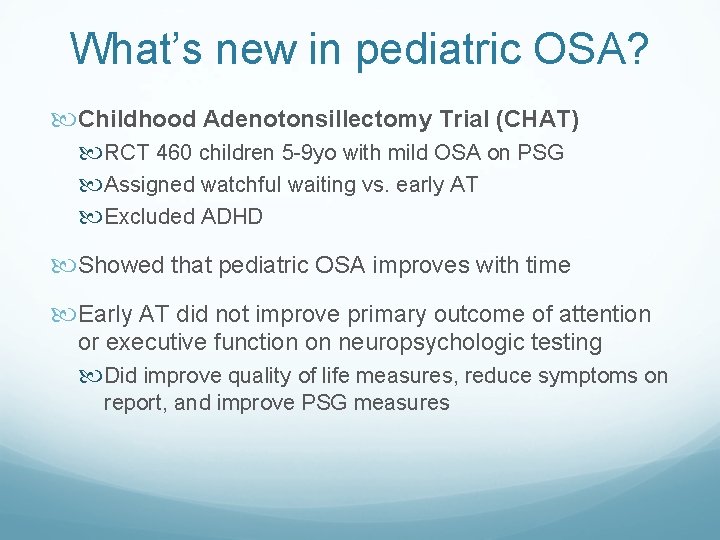
What’s new in pediatric OSA? Childhood Adenotonsillectomy Trial (CHAT) RCT 460 children 5 -9 yo with mild OSA on PSG Assigned watchful waiting vs. early AT Excluded ADHD Showed that pediatric OSA improves with time Early AT did not improve primary outcome of attention or executive function on neuropsychologic testing Did improve quality of life measures, reduce symptoms on report, and improve PSG measures
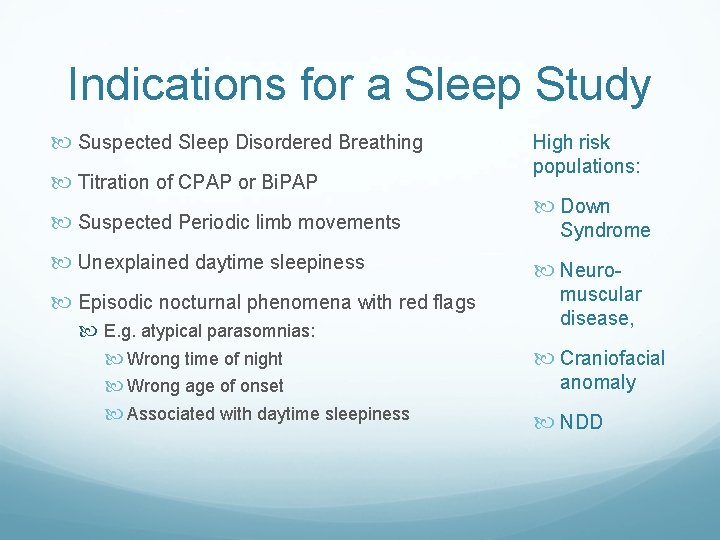
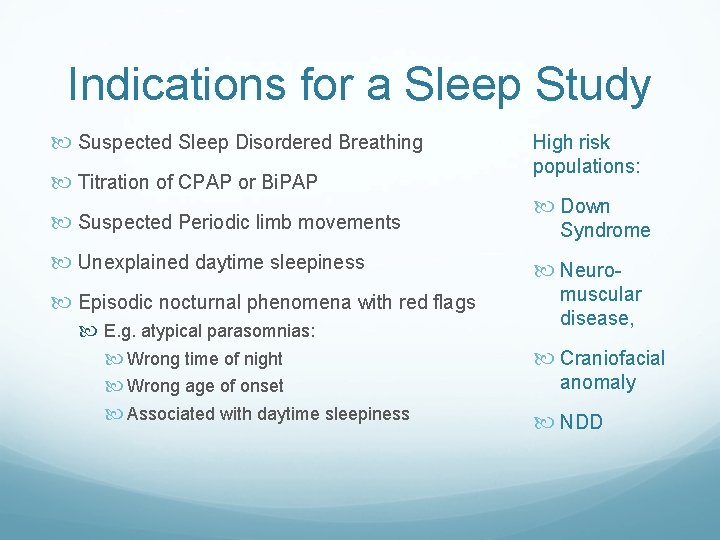
Indications for a Sleep Study Suspected Sleep Disordered Breathing Titration of CPAP or Bi. PAP Suspected Periodic limb movements Unexplained daytime sleepiness Episodic nocturnal phenomena with red flags E. g. atypical parasomnias: Wrong time of night Wrong age of onset Associated with daytime sleepiness High risk populations: Down Syndrome Neuromuscular disease, Craniofacial anomaly NDD
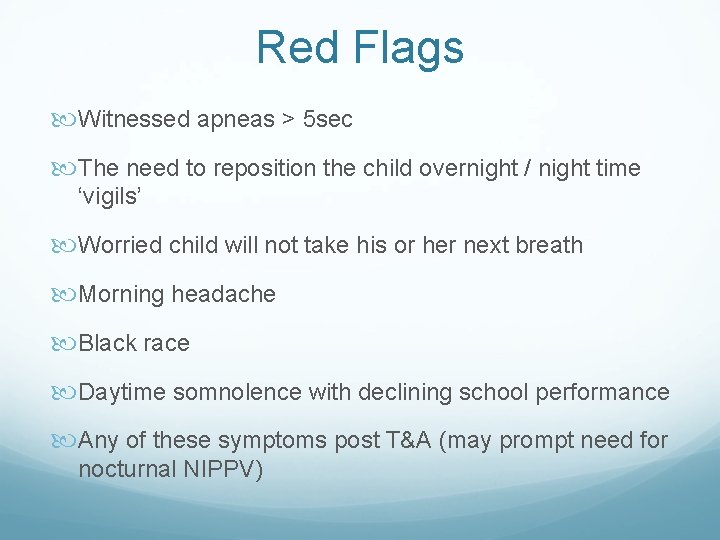
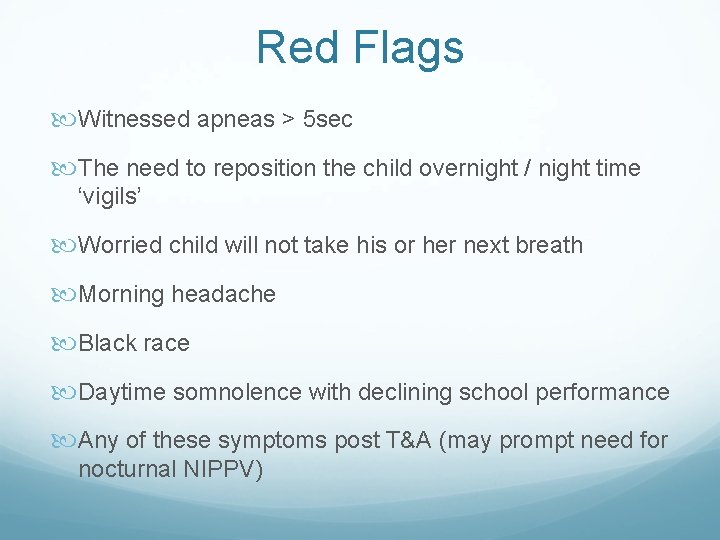
Red Flags Witnessed apneas > 5 sec The need to reposition the child overnight / night time ‘vigils’ Worried child will not take his or her next breath Morning headache Black race Daytime somnolence with declining school performance Any of these symptoms post T&A (may prompt need for nocturnal NIPPV)
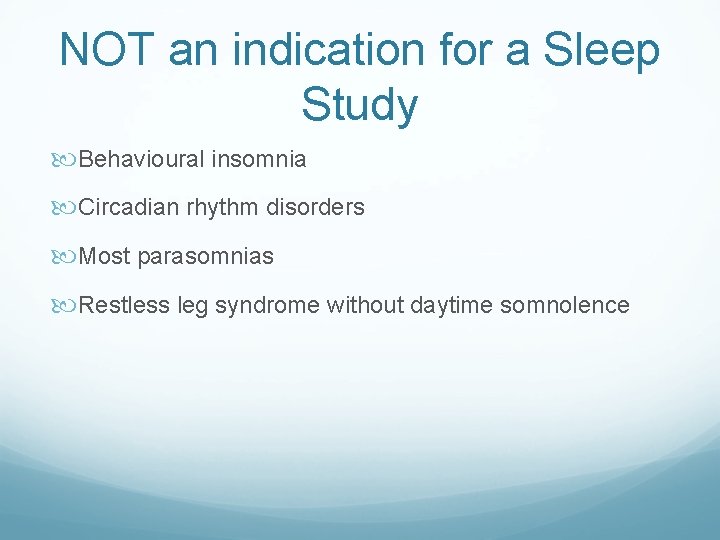
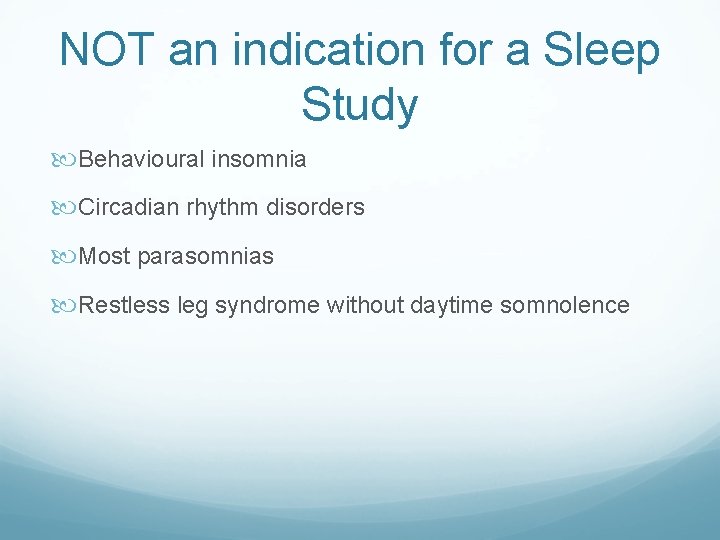
NOT an indication for a Sleep Study Behavioural insomnia Circadian rhythm disorders Most parasomnias Restless leg syndrome without daytime somnolence
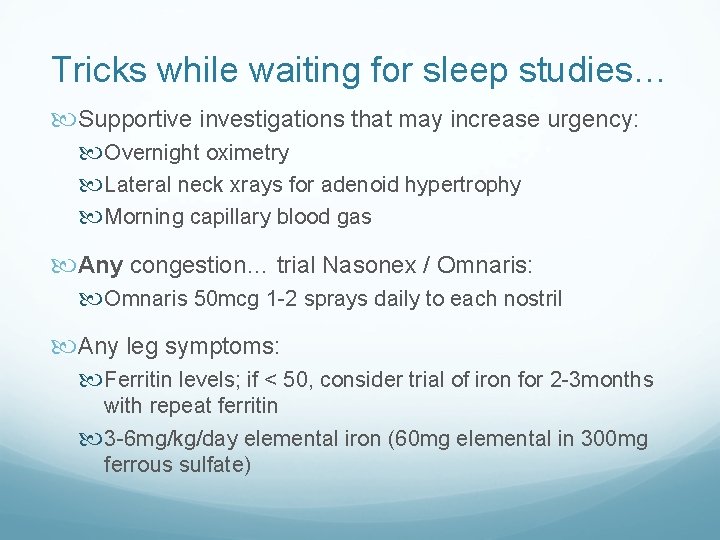
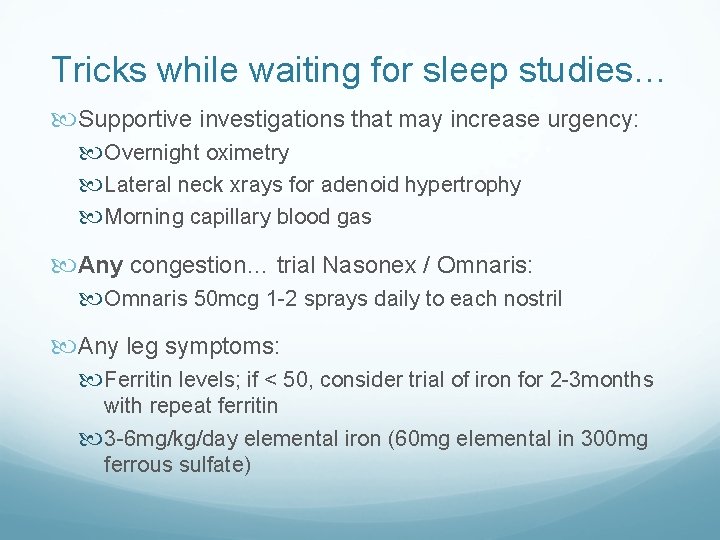
Tricks while waiting for sleep studies… Supportive investigations that may increase urgency: Overnight oximetry Lateral neck xrays for adenoid hypertrophy Morning capillary blood gas Any congestion… trial Nasonex / Omnaris: Omnaris 50 mcg 1 -2 sprays daily to each nostril Any leg symptoms: Ferritin levels; if < 50, consider trial of iron for 2 -3 months with repeat ferritin 3 -6 mg/kg/day elemental iron (60 mg elemental in 300 mg ferrous sulfate)
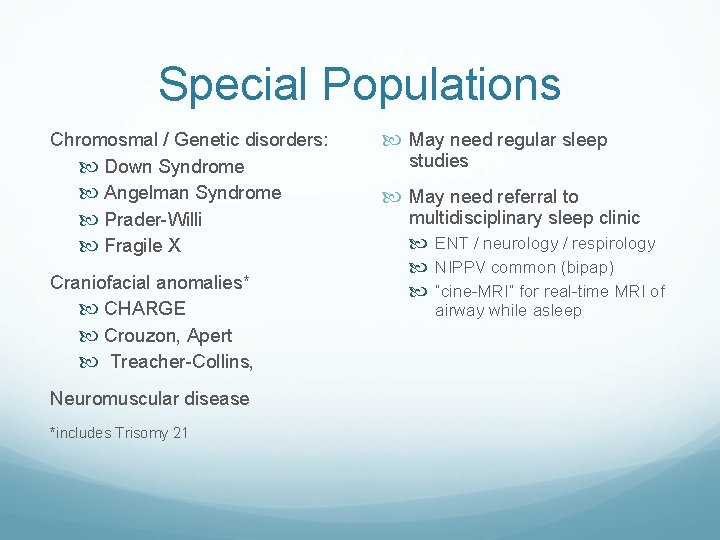
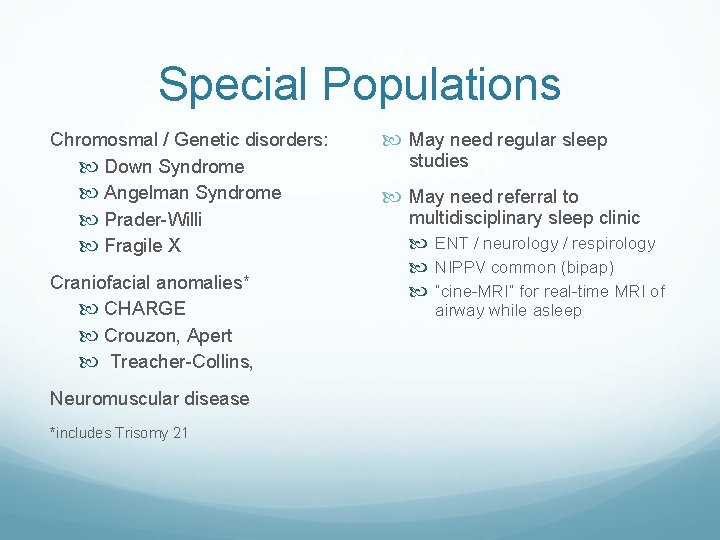
Special Populations Chromosmal / Genetic disorders: Down Syndrome Angelman Syndrome Prader-Willi Fragile X Craniofacial anomalies* CHARGE Crouzon, Apert Treacher-Collins, Neuromuscular disease *includes Trisomy 21 May need regular sleep studies May need referral to multidisciplinary sleep clinic ENT / neurology / respirology NIPPV common (bipap) “cine-MRI” for real-time MRI of airway while asleep
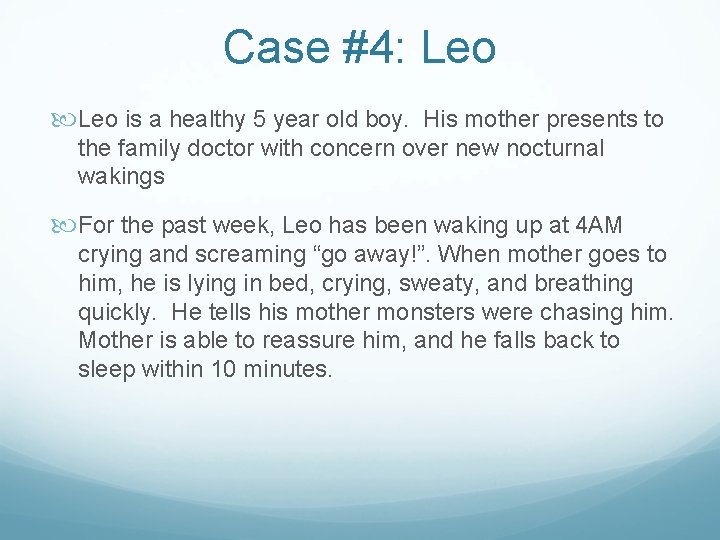
Case #4: Leo is a healthy 5 year old boy. His mother presents to the family doctor with concern over new nocturnal wakings For the past week, Leo has been waking up at 4 AM crying and screaming “go away!”. When mother goes to him, he is lying in bed, crying, sweaty, and breathing quickly. He tells his mother monsters were chasing him. Mother is able to reassure him, and he falls back to sleep within 10 minutes.
What kind of parasomnia is this? a) Sleep Terror b) Nightmare c) Somnambulism d) Confusional Arousal
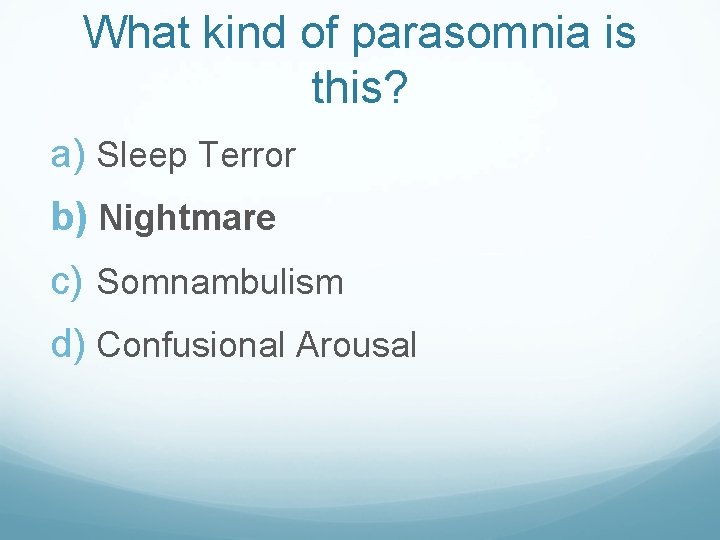
What kind of parasomnia is this? a) Sleep Terror b) Nightmare c) Somnambulism d) Confusional Arousal
Parasomnias Can be normal (dreams) or abnormal (sleepwalking) Partial Arousal Parasomnias (night terrors, confusional arousals) tend to occur in the first third of the night, when children are transitioning from a slow wave sleep to another phase Stuck between awake and asleep! Positive family history is common Not dangerous
Nightmares Most frequent between 3 and 6 years of age Developmentally appropriate: young children: monsters, animals, separation adolescents: natural disasters, crime and violence More frequently in the early morning hours (where there is more REM sleep) Somatic symptoms common, but when awakened, are fully aroused; usually have memory of the event the next morning Problematic when frequent / persistent (> 1 month), affect daytime function, disturbing content screen for abuse
Nightmare Treatment Avoid sleep deprivation Decrease exposure to frightening information News Violent television shows Horror movies Respond positively Use a security object Wind down at night
Sleep Terrors Epidemiology: 2 – 4 years old at onset Usually resolve in 1 to 3 years ~ 6% of children Characteristics: First third of the night Sitting up in bed, screaming, terrified Not aware / responsive to parents No memory of the event Management: Ensure good sleep hygiene – avoid sleep deprivation Consider waking 20 mins before usual episode
Other Parasomnias Confusional arousals are similar to night terrors except: Usually don’t scream, instead stare Usually don’t walk around Shorter than sleep terrors Sleepwalking Bizzare behaviours Confusion, agitation No memory of event Management is to ensure safety during event, and… good sleep hygiene!
Sleep Red Flags The following symptoms should prompt a referral to a sleep clinic: Loud nightly snoring or breathing difficulties at night (refer to ENT as well) Extreme restlessness or repeated unusual movements in sleep Insomnia in child with mental health and/or physical health comorbidity that does not respond to behavioural treatment Significant daytime behaviour disorder in addition to behavioural insomnia Insomnia leading to school failure or academic difficulties Excessive daytime sleepiness not explained by behavioural insomnia
Resources Books: Better Sleep for your Baby and Child – A parent’s step-by-step guide to healthy sleep habits The Sleepeasy Solution: The Exhausted Parent's Guide to Getting Your Child to Sleep from Birth to Age 5 Online resources: Caring for Kids CPS Recommendations for Safe Sleep Environments Canadian Sleep Society Insomnia Rounds Special Groups: Sleep Toolkit produced by the Autism Treatment Network
QUESTIONS? ?
References Mindell JA, Owens JA. A Clinical Guide to Pediatric Sleep: Diagnosis and Management of Sleep Problems. 2 nd ed. Philadelphia (PA): Lippincott Williams & Wilkins; 2009. Weiss SK. Better Sleep for your Baby and Child. Toronto (ON): Robert. Rose Inc; 2006.

Questions or Comments? Video-conferencers: Unmute&your to Complete today’s evaluation applysystem for professional credits ask a question Webcasters: Type your question

Hot Topics - Melatonin Two effects: Hypnotic – makes you sleepy Chronobiotic – affects circadian rhythms Everyone (except those with cortical blindness) makes melatonin Natural melatonin peak prior to sleep onset is called “dim light melatonin onset” (DLMO) Blue-light from screens alters DLMO
Melatonin - dosing Therapeutic doses are orders of magnitude higher than endogenous production Usual doses 0. 5 to 10 mg start at ½ the smallest dose available give 30 -45 mins before desired sleep time for hypnotic effect – has less chronobiotic effect given in another phase of day (not DLMO), will induce chronobiotic effect therefore, giving melatonin in the middle of the night is like giving a patient jet lag every night Commercial preparations are highly variable
 Telenursing and remote access telehealth
Telenursing and remote access telehealth Ctel telehealth
Ctel telehealth Office for the advancement of telehealth
Office for the advancement of telehealth Telehealth and telemedicine
Telehealth and telemedicine Flo telehealth
Flo telehealth Module 23 sleep patterns and sleep theories
Module 23 sleep patterns and sleep theories Come sleep o sleep
Come sleep o sleep Module 23 sleep patterns and sleep theories
Module 23 sleep patterns and sleep theories Adults spend about ______% of their sleep in rem sleep.
Adults spend about ______% of their sleep in rem sleep. Module 23 sleep patterns and sleep theories
Module 23 sleep patterns and sleep theories Sick child definition
Sick child definition A childs sleep
A childs sleep Broad topic and specific topic examples
Broad topic and specific topic examples Narrow down the topic
Narrow down the topic Certificate 4 in child youth and family intervention
Certificate 4 in child youth and family intervention Child, youth and family services act, 2017
Child, youth and family services act, 2017 Duke family medicine and community health
Duke family medicine and community health Readiness rounds
Readiness rounds Five layers of neurosis
Five layers of neurosis Sam rounds
Sam rounds What does 75 round to
What does 75 round to Nursing grand rounds presentation example
Nursing grand rounds presentation example Breech face gun
Breech face gun A is an odd number which rounds to 100 000
A is an odd number which rounds to 100 000 Quality teaching rounds coding sheet
Quality teaching rounds coding sheet Christmas table quiz seomra ranga
Christmas table quiz seomra ranga Richard elmore harvard
Richard elmore harvard Maintenance rounds
Maintenance rounds Red white and blue tortilla chips
Red white and blue tortilla chips Tabular dimensioning
Tabular dimensioning Schwartz rounds facilitator training
Schwartz rounds facilitator training Utmb grand rounds
Utmb grand rounds 전위 순회
전위 순회 Todays match
Todays match No thats not it
No thats not it Todays final jeopardy question
Todays final jeopardy question What is todays temperature
What is todays temperature Todays final jeopardy
Todays final jeopardy Todays software
Todays software Date frui
Date frui Todays objective
Todays objective Todays objective
Todays objective Todays lab
Todays lab Todays plan
Todays plan Today's goal
Today's goal Todays price of asda shares
Todays price of asda shares Are we having class today
Are we having class today Todays jeopardy
Todays jeopardy Handcuff nomenclature
Handcuff nomenclature Todays objective
Todays objective Todays concept
Todays concept Todays globl
Todays globl Todays science
Todays science Todays objective
Todays objective Todays objective
Todays objective Today planetary position
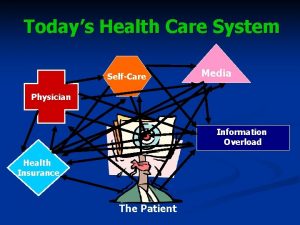
Today planetary position Todays health
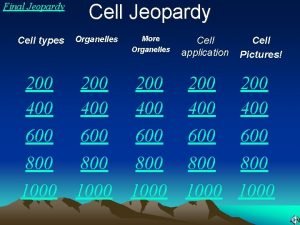
Todays health Cell jeopardy
Cell jeopardy Todays sabbath lesson
Todays sabbath lesson Todays class
Todays class Welcome to today's class
Welcome to today's class Multiple choice comma quiz
Multiple choice comma quiz Good morning students good
Good morning students good Todays weather hull
Todays weather hull Todays whether
Todays whether Whats todays temperature
Whats todays temperature Whats todays wordlw
Whats todays wordlw Todays objective
Todays objective Resume objectives examples
Resume objectives examples Mla first page
Mla first page