Child with Integumentary Disorder Integumentary Disorders Exposure to






- Slides: 24

Child with Integumentary Disorder

Integumentary Disorders • Exposure to: – Infectious microorganisms – Hypersensitivity reactions – Hormonal influences – Injuries Mild and self-limiting Chronic Severe Life-threatening Major threat to psychological status
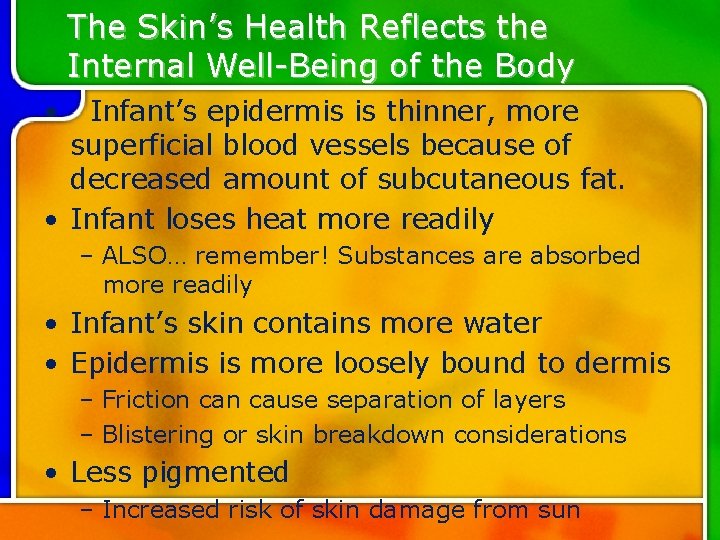
The Skin’s Health Reflects the Internal Well-Being of the Body • Infant’s epidermis is thinner, more superficial blood vessels because of decreased amount of subcutaneous fat. • Infant loses heat more readily – ALSO… remember! Substances are absorbed more readily • Infant’s skin contains more water • Epidermis is more loosely bound to dermis – Friction cause separation of layers – Blistering or skin breakdown considerations • Less pigmented – Increased risk of skin damage from sun
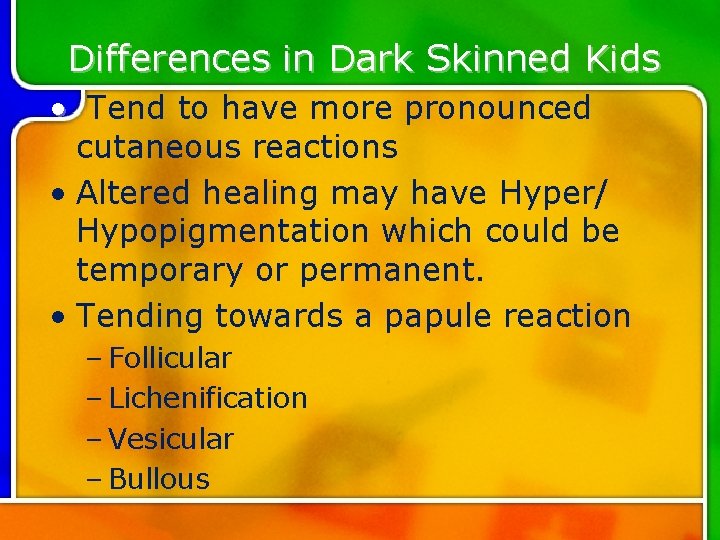
Differences in Dark Skinned Kids • Tend to have more pronounced cutaneous reactions • Altered healing may have Hyper/ Hypopigmentation which could be temporary or permanent. • Tending towards a papule reaction – Follicular – Lichenification – Vesicular – Bullous
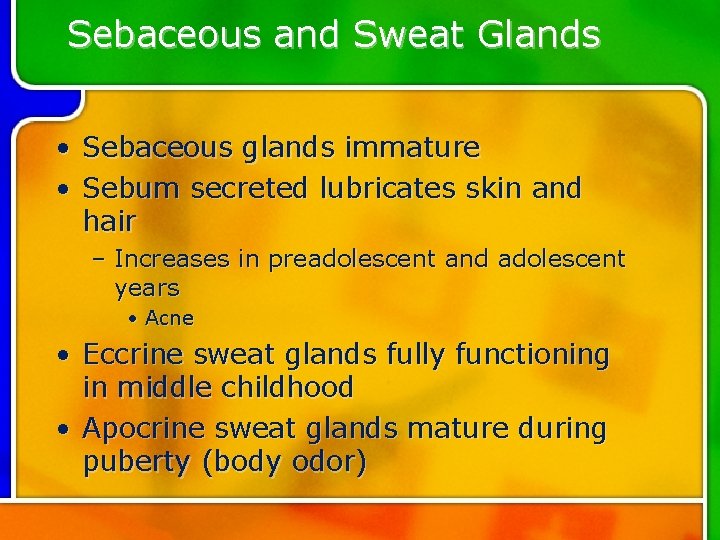
Sebaceous and Sweat Glands • Sebaceous glands immature • Sebum secreted lubricates skin and hair – Increases in preadolescent and adolescent years • Acne • Eccrine sweat glands fully functioning in middle childhood • Apocrine sweat glands mature during puberty (body odor)

Common Medical Treatments • Wet Dressings – Use lukewarm sterile water • Sunscreen – All over age 6 months – Fragrance free, PABA free – SPF 15 – Apply 30 minutes before sun, reapply every 2 hours; 60 to 80 minutes in H 2 O – Use during summer even with clouds!
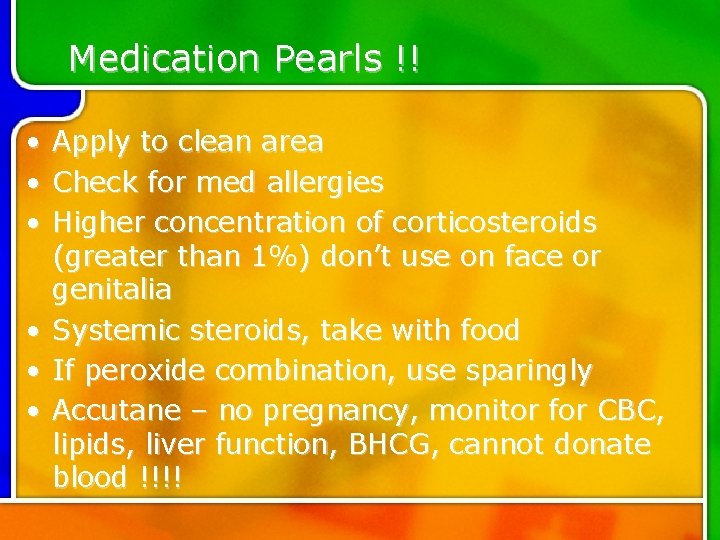
Medication Pearls !! • • • Apply to clean area Check for med allergies Higher concentration of corticosteroids (greater than 1%) don’t use on face or genitalia Systemic steroids, take with food If peroxide combination, use sparingly Accutane – no pregnancy, monitor for CBC, lipids, liver function, BHCG, cannot donate blood !!!!
Overview • Many rashes may be associated with other, often serious illness • Health history – Immunizations – Pets that go outside? – Change in food, detergent?
Assessment • Physical Examination-Focused/Thorough • Specific Lab tests – CBC • Diff helpful for infection • Affected by myelosuppressive drugs – ESR • Send sample immediately to lab (old samples give false low values) – KOH prep • Reveals fungus – Patch or skin testing • Have emergency equipment available – Ig. E • Elevated in allergies
Bacterial Infections • Normal flora – Staphyloccus aureus – B-hemolytic • Impetigo, folliculitis, cellulitis • Usually self-limiting • Rarely severe
Bacterial Infections • Impetigo – Easily recognizable – Sequela to traumatic event – Secondary bacterial infection • Atopic dermititis – Could have developed from intact skin
Bacterial Infections • Folliculitis – Infection of the hair follicle – From occlusion of hair follicle – “May” result from poor hygiene – Prolonged contact with contaminated H 2 O – Maceration – Moist environment – Use of occlusive emollient products
Bacterial Infections • Cellulitis – Localized infection and inflammation of the skin and subcutaneous tissues – Proceeded by skin trauma • Staphylococcal scalded Skin Syndrome – Caused by S. aureus – Produces toxin, causing exfoliation, erythema and tenderness – Babies and the very young
Bacterial Infections • CA-MRSA – Commonly acquired bacterial infection – Caused by methicillin resistant S. aureus – “Campers disease” • Teams using same sweaty wet equipment • Daycare • Gyms – Requires more often than not, systemic ABX, topical
Fungal Infections • Epidermophyton, microsporum, and trichophyton – The “Tenias” – Tinea pedis – feet – Tinea corporis – arms and legs – Tinea vesicolor – trunk and extremities – Tinea capitis – scalp, eyebrows, eyelashes – Tinea cruis – groin

Inflammatory Skin Conditions • • • Diaper rash – caused by C. albicans Diaper Dermatis – inflammatory reaction to prolonged exposure to urine and feces Hx and appearance A and D ointment or zinc oxide Avoid rubber pants, change frequently, avoid harsh soaps KEEP CLEAN !!!

Inflammatory Skin Conditions • Atopic Dermatitis – AKA eczema – Member of the atopy group • Allergic rhinitis • Asthma – Chronic itching, reddened and swollen, vesicles – Relapse and remitting nature – Interferes with sleep, school, self-image, irritable – Good skin hydration, topical corticosteroids, immune modulators, oral antihistamines and…. – Antibiotics for secondary infection – Cetaphil, aquanil, unscented Dove®, Caress®
Inflammatory Skin Conditions • Contact Dermatitis – Cell-mediated response, inflammatory – Antigen attaches to cells – Allergic – Weeping, crusty – Spreads with fingernails – Watch for eyes ! – Topical or systemic corticosteroids – Poison ivy – plant’s oil gets all over
Erythemia Multiforme – Uncommon in kids – Acute, self-limiting hypersensitivity reaction – May be sequela of virus or drugs – Generally resolves on its own – Fever, malaise, pruritis, macule rash • Stevens-Johnson Syndrome – 10% MR – Hospitalization, isolation, fluid and electrolyte replacement, treatment of any secondary infections
Urticaria • • • AKA Hives Type 1 hypersensitivity reaction Caused by immunologically mediated antigen-antibody response of HISTAMINE release Vasodilation and increased vascular permeability results in erythema and wheals Food, drugs, extremes of temp, Treatment – antihistamines and/or corticosteroids Should resolve in 6 weeks
Seborrhea • Chronic inflammatory dermatitis on skin or scalp. Possible reaction to fungus exposure • “Craddle Cap” • Corticosteroid creams or lotions • Anti-dandruff shampoos containing selenium sulfide • Anti-fungal creams containing ketoconazole • Mineral oil to scalp for infants to lift crusts
Psoriasis • • Chronic inflammatory skin disease Periods of remission and exacerbation Control not cure Hyperproliferation of epidermis at sites of mechanical, thermal, or physical trauma • Therapeutic management – Skin hydration – Tar preparations – Ultraviolet light – Topical retinoid preparation
Acne • Common throughout life – crazy during puberty • All races, colors, hits both genders equally • Acne Neonatorum – baby acne • Acne vulgaris – extreme – Results in scarring – Terrible self-image, social issues, increased suicide incidence
