Child Health Nursing Partnering with Children Families Jane









- Slides: 80
Child Health Nursing Partnering with Children & Families Jane W. Ball Ruth C. Bindler Chapter 31 Alterations in Genitourinary Function Child Health Nursing: Partnering with Children & Families By Jane W. Ball and Ruth C. Bindler © 2006 Pearson Education, Inc. Pearson Prentice Hall Upper Saddle River, NJ 07458
Urinary System • Maintains balance • Removal of waste products • Functionally immature until puberty
Urinary System • Functions: – Excrete wastes – Maintain acid-base and fluid and electrolyte balance – Regulation of Blood pressure – Stimulation of production of erythropoietin – Regulation of calcium metabolism • By activation of vitamin D
Review of Urinary A&P • The key structures of the urinary sx are the Kidneys and the Urinary Tract • To produce urine, the various parts of the kidney perform 3 basic functions – Glomerular filtration (the process of filtering blood as it flows through the kidneys) – Tubular resorption (necessary fluids, electrolytes, proteins + blood cells are retained) – Tubular secretion (waste products+ fluids filtered out)
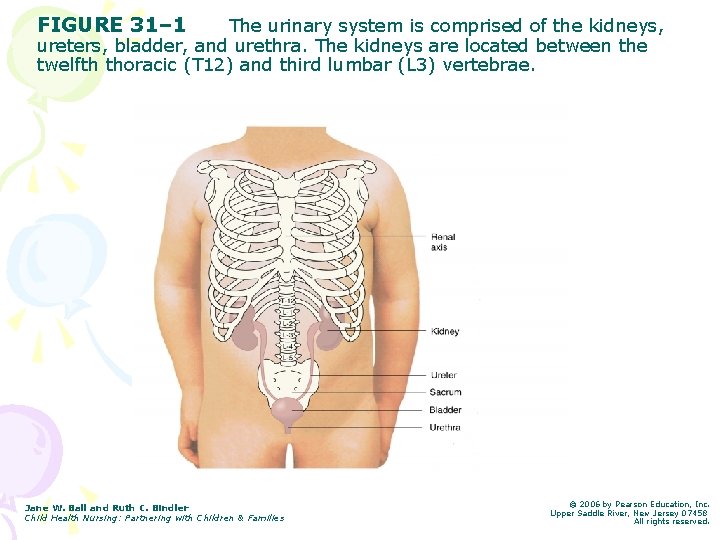
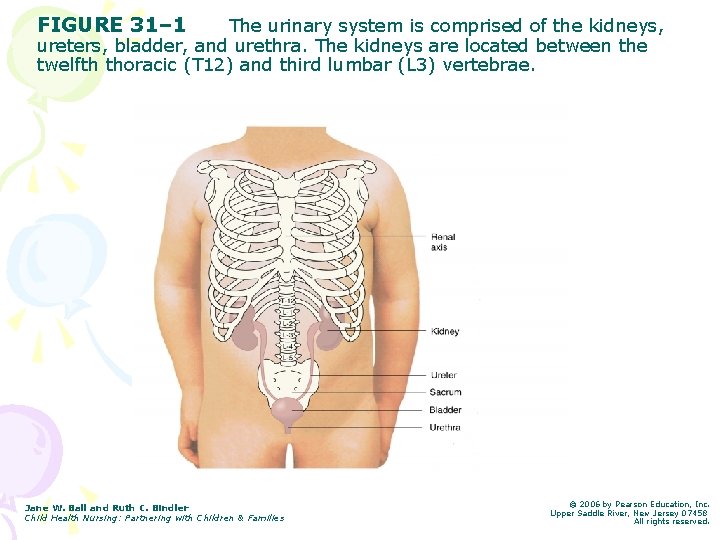
FIGURE 31– 1 The urinary system is comprised of the kidneys, ureters, bladder, and urethra. The kidneys are located between the twelfth thoracic (T 12) and third lumbar (L 3) vertebrae. Jane W. Ball and Ruth C. Bindler Child Health Nursing: Partnering with Children & Families © 2006 by Pearson Education, Inc. Upper Saddle River, New Jersey 07458 All rights reserved.

Urinary System • Ureters – Carry waste fluid from kidneys to bladder • Bladder – Stores urine – Bladder capacity in ounces estimated by adding 2 to child’s age – Bladder can hold 1 -1 ½ ounces for every year of age – Muscular organ
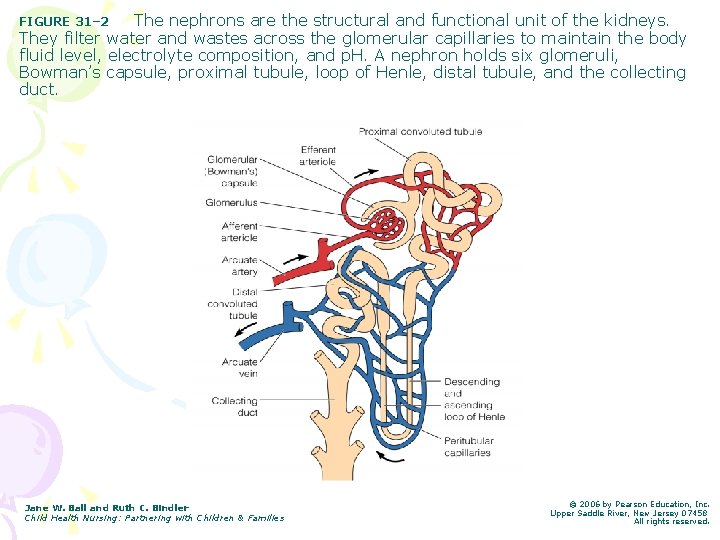
Urinary System • Kidneys: – Nephrons • Perform filtration, reabsorption and secretion – Filtration occurs at the glomerulus, Bowman’s capsule and the basement membrane – Most renal growth occurs during the first 5 years of life. This increase in size is d/t the enlargement of the nephrons.
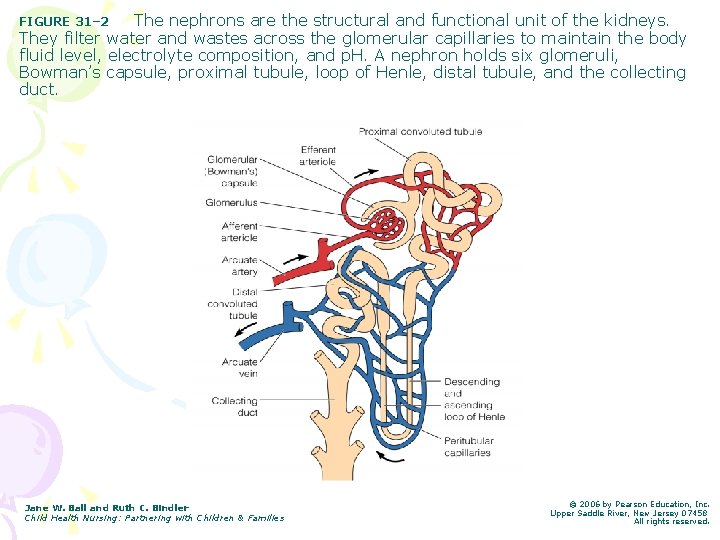
The nephrons are the structural and functional unit of the kidneys. They filter water and wastes across the glomerular capillaries to maintain the body fluid level, electrolyte composition, and p. H. A nephron holds six glomeruli, Bowman’s capsule, proximal tubule, loop of Henle, distal tubule, and the collecting duct. FIGURE 31– 2 Jane W. Ball and Ruth C. Bindler Child Health Nursing: Partnering with Children & Families © 2006 by Pearson Education, Inc. Upper Saddle River, New Jersey 07458 All rights reserved.
Kidneys • Kidneys are immature at birth. As child grows, concentration of urine becomes more efficient – Refer to Box 31 -3 – First 2 years of life: less efficient at regulating f/e and acid/base balance – Urine output per kg body weight is greater in infancy than childhood/ adolescents. • Kidney less able to concentrate urine
Urinary System • For the kidneys to function effectively, the following conditions need to be present – Unimpaired renal blood flow – Adequate glomerular ultrafiltration – Normal tubular function – Unobstructed urine flow
Urinary System • Diagnostic tests for Urinary System Conditions: – Refer to Table 31 -2 p 1178 in text • Normal Urinalysis Results: – Refer to Table 31 -3 p 1179 in text

Structural Defects of the Urinary System • Bladder Exstrophy • Hypospadias and Epispadias • Obstructive Uropathy • Congenital Hydronephrosis • Vesicoureteral Reflux
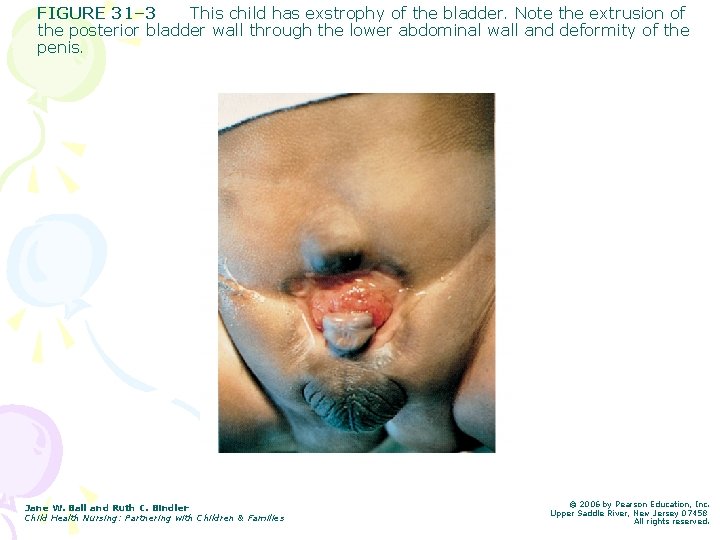
Bladder Exstrophy • Rare congenital defect (1 in 40, 000 newborns) • Etiology: failure of abdominal wall to close during fetal development – Leads to eversion of the bladder • Treatment: – Surgical reconstruction in several stages • Nursing care: – Cover w/ wet sterile gauze postdelivery, prepare for surgery
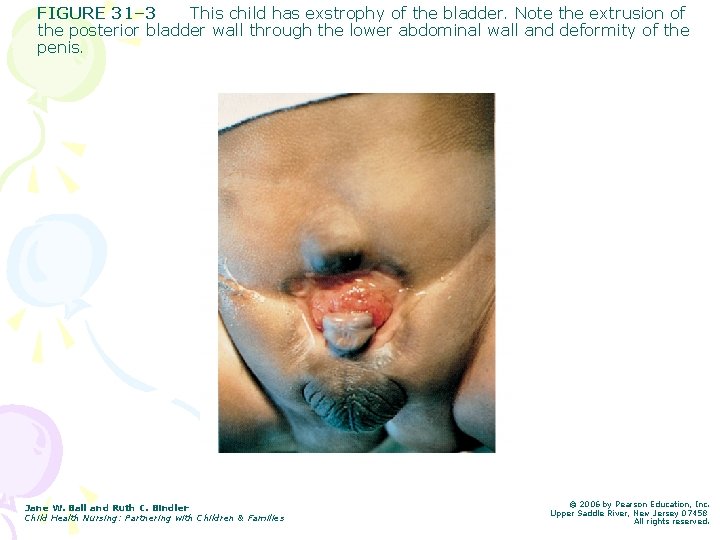
FIGURE 31– 3 This child has exstrophy of the bladder. Note the extrusion of the posterior bladder wall through the lower abdominal wall and deformity of the penis. Jane W. Ball and Ruth C. Bindler Child Health Nursing: Partnering with Children & Families © 2006 by Pearson Education, Inc. Upper Saddle River, New Jersey 07458 All rights reserved.
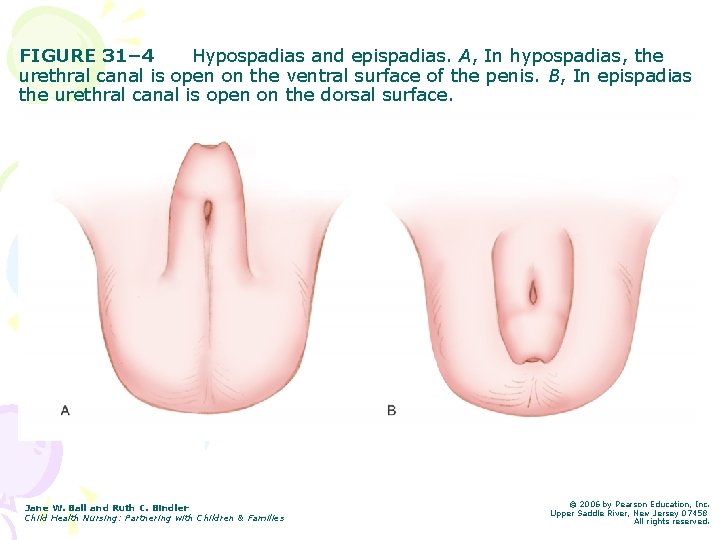
Hypospadias and Epispadias • Congenital anomalies involving and abnormal location of the urethral meatus • Result from failure of the urethra folds to fuse completely over the urethral groove • Familial tendency but exact mechanism unknown • Hypospadias often occurs in conjunction with congenital inguinal hernias, undescended testes, chordee • Epispadias often occurs with bladder exstrophy
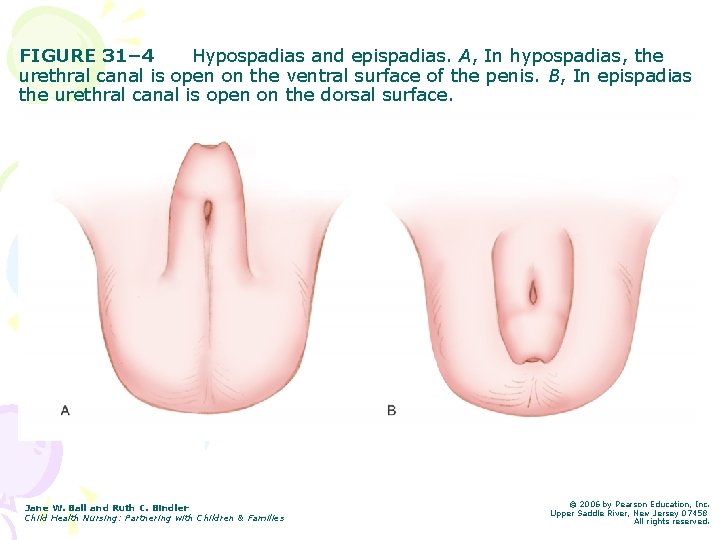
FIGURE 31– 4 Hypospadias and epispadias. A, In hypospadias, the urethral canal is open on the ventral surface of the penis. B, In epispadias the urethral canal is open on the dorsal surface. Jane W. Ball and Ruth C. Bindler Child Health Nursing: Partnering with Children & Families © 2006 by Pearson Education, Inc. Upper Saddle River, New Jersey 07458 All rights reserved.
Hypospadias vs epispadias • The urethral meatus may be located anywhere along the course of the ventral surface of the penile shaft • The meatal opening islocated on the dorsal surface of the penile shaft, and may be at the level of the bladder neck.
Hyposapdias/ Epispadias Treatment • For mild cases of hypospadias, no intervention is necessary • Surgical correction is the tx of choice – Corrected during the first year of life • DO NOT CIRCUMCISE as foreskin tissue may be used in reconstruction • Goals of Surgery: – Placement of the urethral meatus at the end of the glans penis allowing for good urine stream – Release of chordee to straighten penis – Cosmetic appearance
Hypospadias/ Epispadias Nursing Responsibilities • Assist in the identification of defects in complete newborn exam • Prevent potential complications • Promote parental understanding and attachment • Promote normal voiding pattern
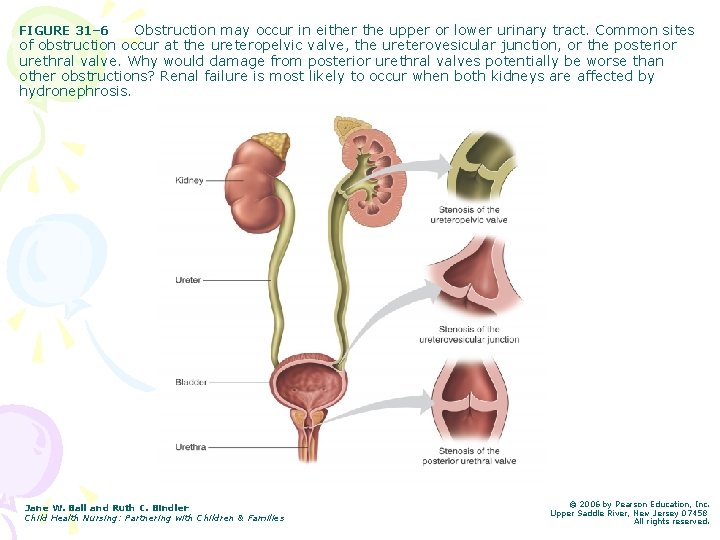
Obstructive Uropathy • Structural or functional abnormalities of the urinary system that interferes with urine flow and results in urine backflow into the kidneys. • The condition can occur anywhere along the urinary tract. • Pressure caused by urine backup often leads to hydronephrosis
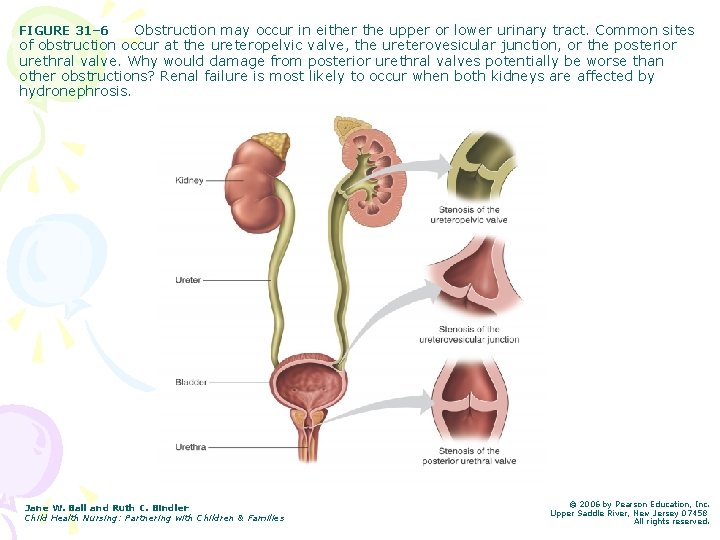
Obstruction may occur in either the upper or lower urinary tract. Common sites of obstruction occur at the ureteropelvic valve, the ureterovesicular junction, or the posterior urethral valve. Why would damage from posterior urethral valves potentially be worse than other obstructions? Renal failure is most likely to occur when both kidneys are affected by hydronephrosis. FIGURE 31– 6 Jane W. Ball and Ruth C. Bindler Child Health Nursing: Partnering with Children & Families © 2006 by Pearson Education, Inc. Upper Saddle River, New Jersey 07458 All rights reserved.
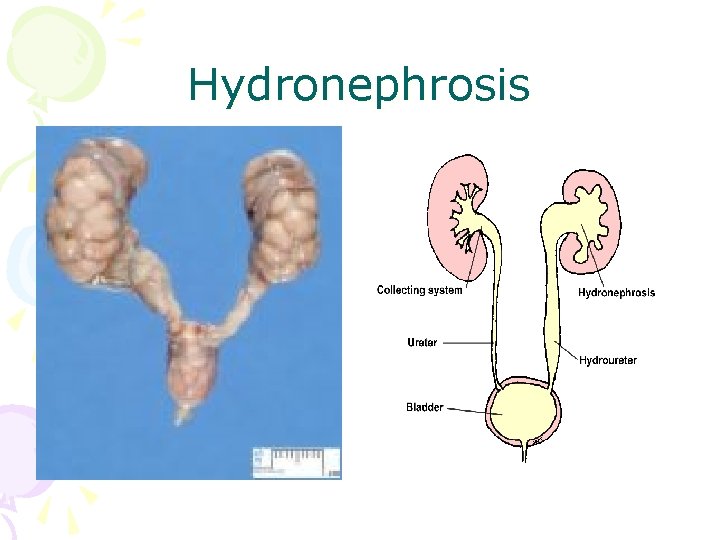
Hydronephrosis • An accumulation of urine in the renal pelvis as a result of obstructed outflow, and compromises kidney function. • Most children with hydronephrosis are born with the condition although it can develop during childhood. It is the most common urinary tract anomaly (abnormality) and ranges in severity. In mild hydronephrosis, the pelvic (the part of the kidney that collects the urine) dilation is barely noticeable, whereas in severe hydronephrosis the swelling occupies much of the abdomen.
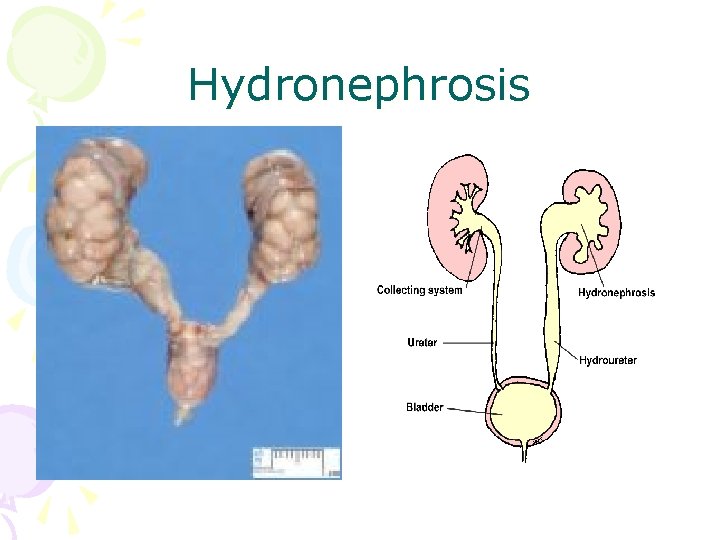
Hydronephrosis
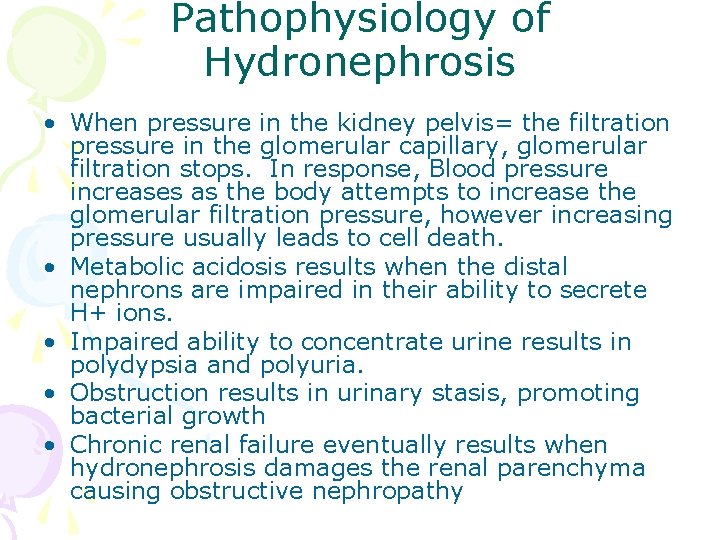
Pathophysiology of Hydronephrosis • When pressure in the kidney pelvis= the filtration pressure in the glomerular capillary, glomerular filtration stops. In response, Blood pressure increases as the body attempts to increase the glomerular filtration pressure, however increasing pressure usually leads to cell death. • Metabolic acidosis results when the distal nephrons are impaired in their ability to secrete H+ ions. • Impaired ability to concentrate urine results in polydypsia and polyuria. • Obstruction results in urinary stasis, promoting bacterial growth • Chronic renal failure eventually results when hydronephrosis damages the renal parenchyma causing obstructive nephropathy
Hydronephrosis • Facts about hydronephrosis • It is four to five times more common in males than females. • It can occur in one or both kidneys. • Most mild cases and even some moderate cases may resolve on their own. • More severe cases may require surgery.
Hydronephrosis • What are the symptoms of hydronephrosis? – In mild cases and even some moderate cases of hydronephrosis, children will have no symptoms and the condition may disappear on its own within the first year of life. – In more severe cases, when kidney function is affected, the infant or child can experience pain, bleeding and infections. These symptoms may not develop until months or years after hydronephrosis is first detected. – Tx= surgery to correct blockage
Vesicoureteral Reflux • VUR results in backflow of urine from the bladder into the kidneys • Prevents complete emptying of the bladder and creates a reservoir for bacterial growth • The defect results from incomplete development of the ureterovesical junction, or from a structural anomaly.
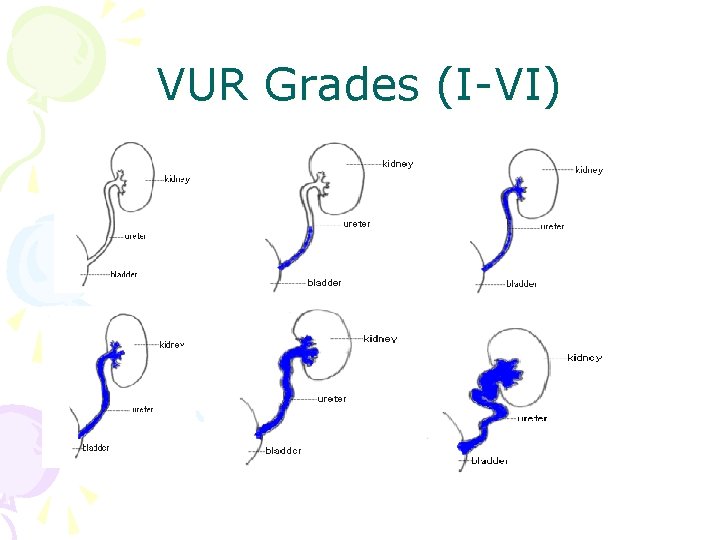
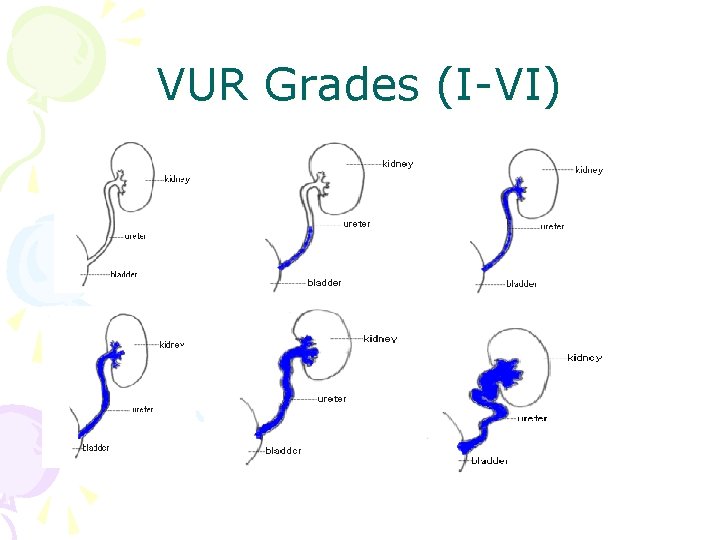
VUR Grades (I-VI)
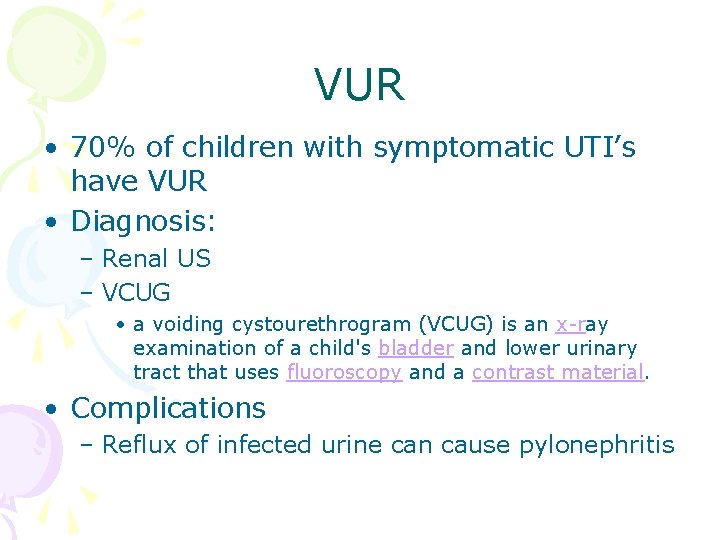
VUR • 70% of children with symptomatic UTI’s have VUR • Diagnosis: – Renal US – VCUG • a voiding cystourethrogram (VCUG) is an x-ray examination of a child's bladder and lower urinary tract that uses fluoroscopy and a contrast material. • Complications – Reflux of infected urine can cause pylonephritis
Disorders Affecting Urinary Elimination • Urinary Tract Infections (UTI’s) • Enuresis
UTI • A microbial invasion of the kidneys, ureters, bladder, or urethra • In the neonatal period, UTI’s occur most commonly in males, possibly b/c of the higher incidence of congenital abnormalities • By age 4 months, UTIs are more common in females b/c of the placement and size of the urethra

UTI • Causes: – Incomplete bladder emptying – Irritation by bubble baths – Poor hygiene – VUR – Urinary tract obstruction • Pathophysiology: – Bacteria enter the urethra and ascend the urinary tract – E. coli (Gram -) causes approximately 75 -90% of all UTIs in females
UTI • What is the difference b/t these 3 conditions? – Cystitis (bladder) – Urethritis (urethra) – Pyelonephritis (ureters, renal pelvis and renal parenchyma) – Most common disorder of GU tract in children
UTI • Complications: – Risk of renal failure: • UTI under age 1 • Delay in diagnosis • Anatomic or neurologic obstruction • Recurrent episodes of upper UTI
UTI • Complications: – VUR – Glomerulonephritis – Bacteremia – Sepsis – Septic Shock • Tests: – Clean catch Urine Analysis and urine Cxresults yield large amounts of bacteria – Increased urine p. H
UTI • Clinical Findings: – Abdominal pain – Enuresis – Frequency and Urgency – Pain/ burning w/ urination (dysuria) – Hematuria – Lethargy or irritability – Poor feeding patterns – Cloudy, foul-smelling urine
UTI • What is the most common clinical presentation of UTI in the child under 2? – Fever with associated s/sx including: • • • V/D Irritability Poor PO intake Malodorous urine Oliguria Constipation – Please Refer to Table on page 1187 for other clinical manifestations of UTIs
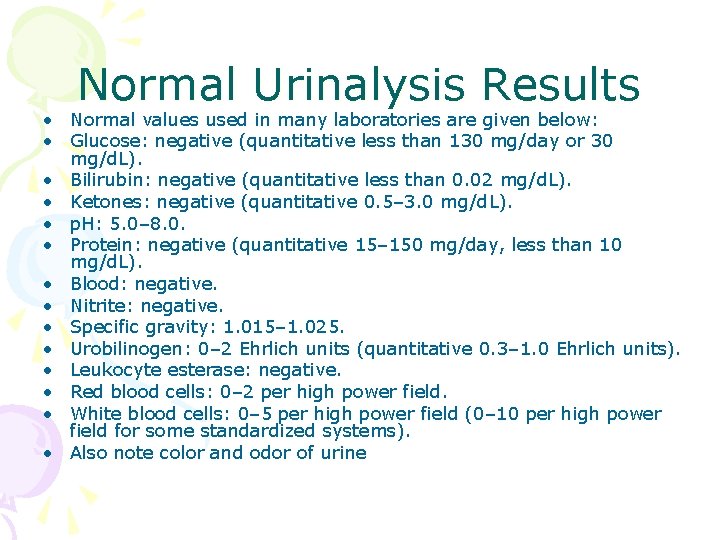
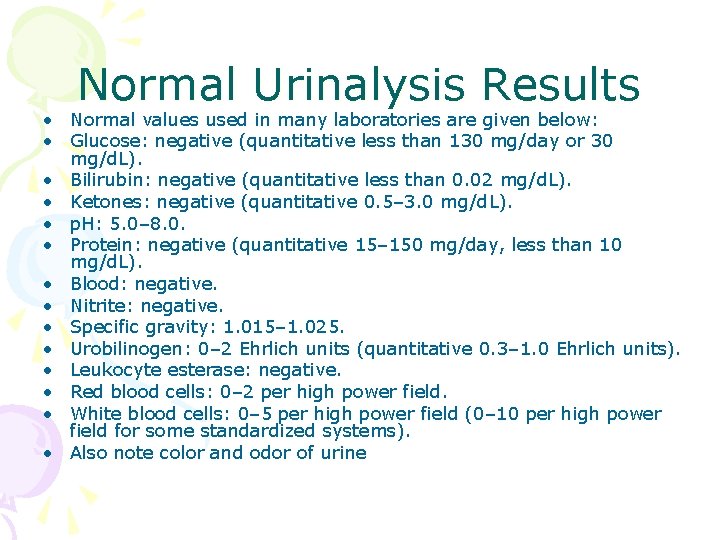
Normal Urinalysis Results • Normal values used in many laboratories are given below: • Glucose: negative (quantitative less than 130 mg/day or 30 mg/d. L). • Bilirubin: negative (quantitative less than 0. 02 mg/d. L). • Ketones: negative (quantitative 0. 5– 3. 0 mg/d. L). • p. H: 5. 0– 8. 0. • Protein: negative (quantitative 15– 150 mg/day, less than 10 mg/d. L). • Blood: negative. • Nitrite: negative. • Specific gravity: 1. 015– 1. 025. • Urobilinogen: 0– 2 Ehrlich units (quantitative 0. 3– 1. 0 Ehrlich units). • Leukocyte esterase: negative. • Red blood cells: 0– 2 per high power field. • White blood cells: 0– 5 per high power field (0– 10 per high power field for some standardized systems). • Also note color and odor of urine
Urine Culture • A urine culture is a diagnostic laboratory test performed to detect the presence of bacteria in the urine (bacteriuria). • Usually takes 24 -48 hours for results • If symptomatic, treat empirically

Nursing care of UTI’s • Administer abx as Rx’d; instruct parents to complete entire course of abx • Encourage fluids to help to flush infection from the urinary tract • Teach proper toileting hygeine • Encourage child to use toilet every 2 hours • Discourage bubble baths • Teach parents about s/sx of UTIs
Enuresis • Repeated involuntary voiding by a child who has reached an age which bladder control is expected (5 -6 y. o) – Enuresis at night= nocturnal enuresis • 50% of cases • More common in boys – Enuresis during day= diurnal enuresis • More common in girls – Further categorized as primary, intermittent and secondary
• Primary: Enuresis – Child has never had a dry night; attributed to maturational delay and small functional bladder • Intermittent: – Child has occasional nights or periods of dryness • Secondary: – Child begins bedwetting who has been reliably dry for 6 -12 months; associated with stress, infections and sleep disorders
Enuresis • Clinical manifestations for diurnal enuresis: – Frequency – Urgency – Constant dribbling – Involuntary loss of control after voiding • Clinical manifestations for nocturnal enuresis: – bedwetting
Enuresis • A thorough hx is obtained. See Box 31 -3 • Clinical therapy: – Spontaneous cure rate in 15% of cases/year – Multitreatment approach most efficient • 1/3 of nocturnal enuresis tx’d w/ meds • See page 1191 for meds used to tx enuresis • Behavioral interventions – Fluid intake programs, bladder alarms, and bladder training
Enuresis • Nursing management: – Thorough hx – Evaluate if parents and child are equally motivated to resolve problem – Teaching
Kidney Disorders • Nephrotic Syndrome • Renal Failure • Glomerulonephritis • Hemolytic Uremic Syndrome • Polycystic Kidney Disease
Nephrotic Syndrome • Condition in which the kidneys lose a significant amount of protein in the urine, resulting in low blood levels of protein. • Nephrotic syndrome refers not to a specific disease but to a clinical state characterized by: – Proteinuria – Hypoalbuminemai – Hyperlipidemia – edema
Nephrotic Syndrome • If nephron’s allow increased protein to escape from the blood what does this lead to?

Nephrotic Syndrome
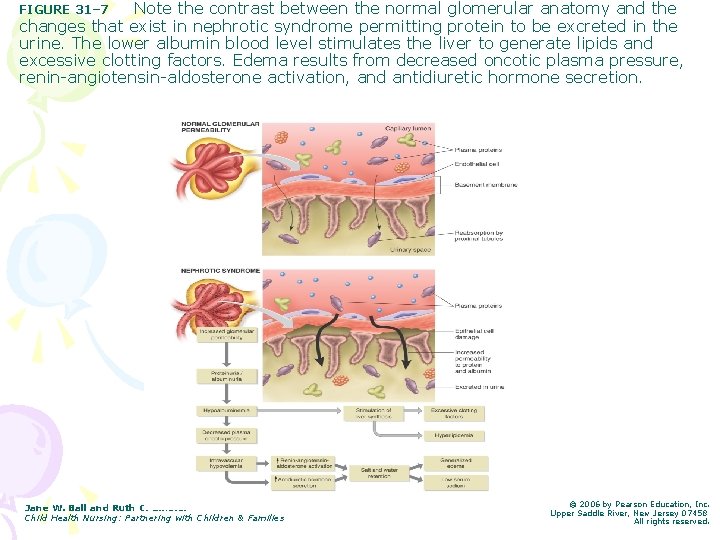
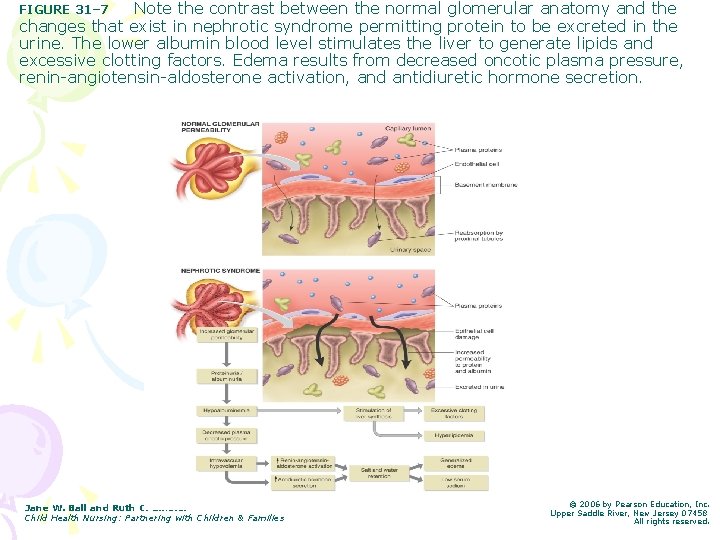
Note the contrast between the normal glomerular anatomy and the changes that exist in nephrotic syndrome permitting protein to be excreted in the urine. The lower albumin blood level stimulates the liver to generate lipids and excessive clotting factors. Edema results from decreased oncotic plasma pressure, renin-angiotensin-aldosterone activation, and antidiuretic hormone secretion. FIGURE 31– 7 Jane W. Ball and Ruth C. Bindler Child Health Nursing: Partnering with Children & Families © 2006 by Pearson Education, Inc. Upper Saddle River, New Jersey 07458 All rights reserved.
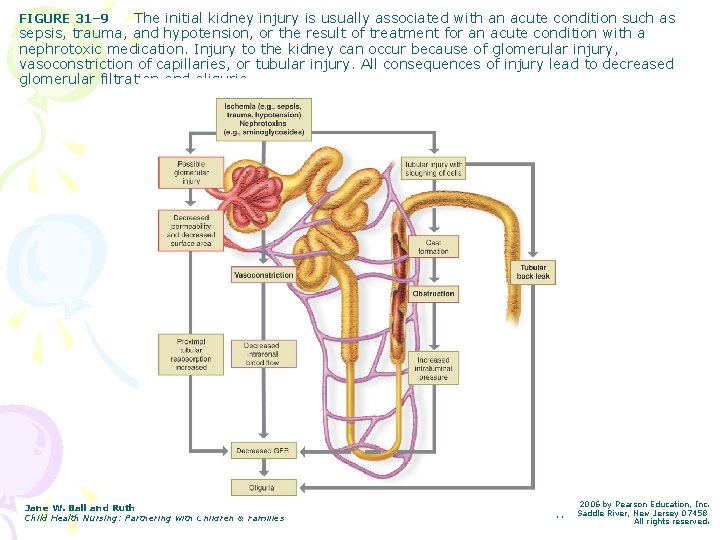
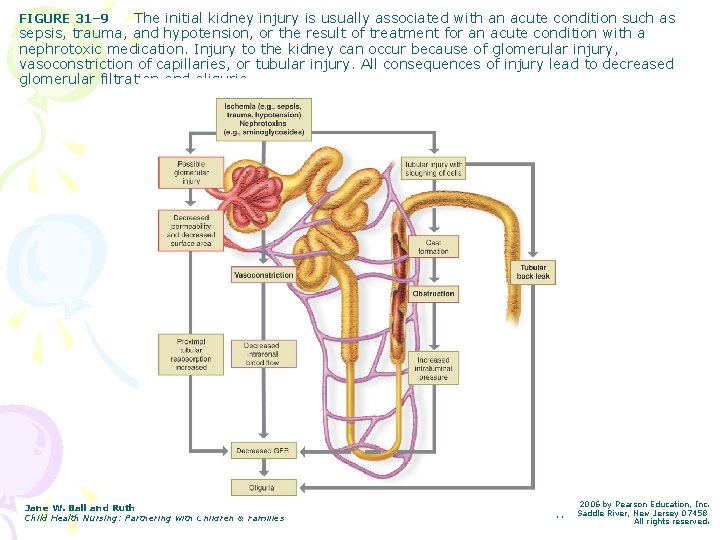
The initial kidney injury is usually associated with an acute condition such as sepsis, trauma, and hypotension, or the result of treatment for an acute condition with a nephrotoxic medication. Injury to the kidney can occur because of glomerular injury, vasoconstriction of capillaries, or tubular injury. All consequences of injury lead to decreased glomerular filtration and oliguria. FIGURE 31– 9 Jane W. Ball and Ruth C. Bindler Child Health Nursing: Partnering with Children & Families © 2006 by Pearson Education, Inc. Upper Saddle River, New Jersey 07458 All rights reserved.

Nephrotic Syndrome • Primary nephrotic syndrome occurs predominantly in preschool children • Incidence peaks b/t ages 2 -3 years • Syndrome rare after age 8 • More common in boys • Some forms may progress to ESRD
Nephrotic Syndrome • How does this happen? – Injury to glomerular filtraiton membrane allows the loss of plasma proteins (especially albumin and immunoglobulin) – This results in decreased levels of serum albumin (hypoalbuminemia) – Hypoalbuminemia results in decreased colloidal osmotic pressure and fluid accumulation in the interstitial spaces. – Edema results from Na and H 2 O retention
Nephrotic Syndrome • Clinical Manifestations by body system: – Renal • Oliguria, and dark, frothy urine – CV • HTN (later stages), tachycardia – Vascular • Thrombosis – Gastrointestinal • Anorexia, abd pains, n/v/d – Skin • Pallor, shiny w/ prominent veins, brittle hair, edema, skin breakdown – Pulmonary • Respiratory distress and pulmonary congestion
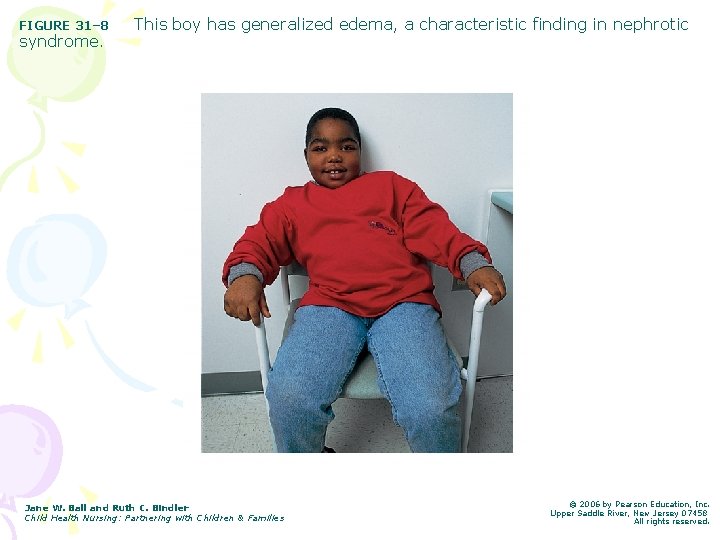
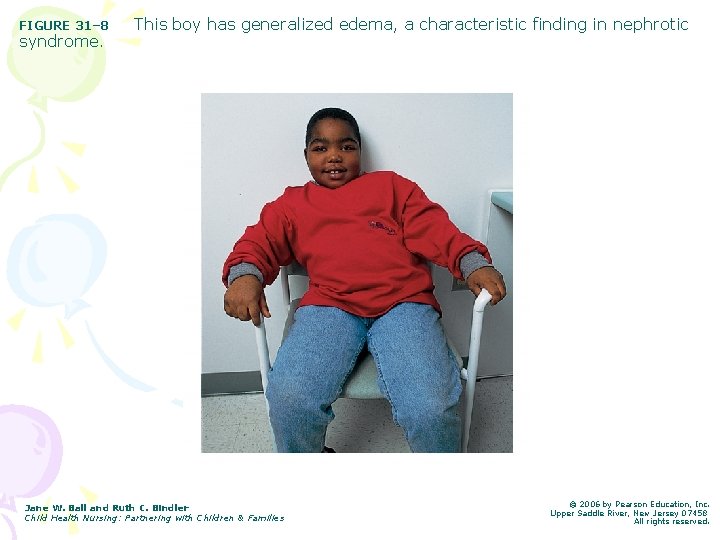
FIGURE 31– 8 syndrome. This boy has generalized edema, a characteristic finding in nephrotic Jane W. Ball and Ruth C. Bindler Child Health Nursing: Partnering with Children & Families © 2006 by Pearson Education, Inc. Upper Saddle River, New Jersey 07458 All rights reserved.
Nephrotic Syndrome • Diagnostic Tests: – Ua= severe proteinuria (primary indicator), hematuria and casts; also an elevated spec grav b/c of the proteinuria – Renal biopsy= identifies the type of nephrotic syndrome the child has, and can be used to monitor response to medical management – Blood studies show: serum creatinine, BUN, choles
Minimal Change Nephrotic Syndrome • Glomeruli appear normal or show only minimal changes on microscopic eval. • Most common form of Nephrotic Syndrome – MCNS affects 85% children w/ nephrotic syndrome – Usually affects children b/t 2 -7 years – Poorer prognosis, progresses more rapidly to renal failure
MCNS • Etiology and Pathophysiology: – Cause unknown; immune-mediated • (often preceded by URI) – The glomeruli appear normal or only have a minimal change in appearance, but their permeability is greatly affected – Characteristic symptoms include • • Edema…weight gain Excessive clotting factors Hyperlipidemia Low serum sodium
Nursing Care of the Child with Nephrotic Syndrome • Physiologic/ Psychosocial assessment • Administer medications • Prevent infections • Prevent skin breakdown • Nutrition/ fluid needs • Promote rest • Provide emotional support • Teaching/ DC planning
Nephrotic Syndrome • Medications: refer to pgs 1196 -1197 • Corticosteroid therapy • Alylating/ Cytotoxic Agents • Cylosporine Therapy (immunosuppressants) • Diuretics • ACE Inhibitors • Antithrombolitic therapy • NSAIDS
Nephrotic Syndrome • Medications: – Prednisone or prednisolone • Stimulates remission by reducing the excretion of protein in the urine • Children who respond to this therapy will continue to take Rx X 6 weeks, and then taper
Nephrotic Syndrome • Discharge Planning: – Parents need to monitor protein in urine daily using dipsticks – Understand that relapses do occur – No added salt diet – Monitor weight
Acute and Chronic Renal Failure • Occurs when the kidney is unable to excrete wastes and concentrate urine • Acute- occurs suddenly and may be reversible • Chronic-occurs gradually and permanently • Azotemia: accumulation of nitrogenous wastes in blood • Oliguria: urine output 0. 5 -1 ml/kg/hour • Anuria: absent urine output
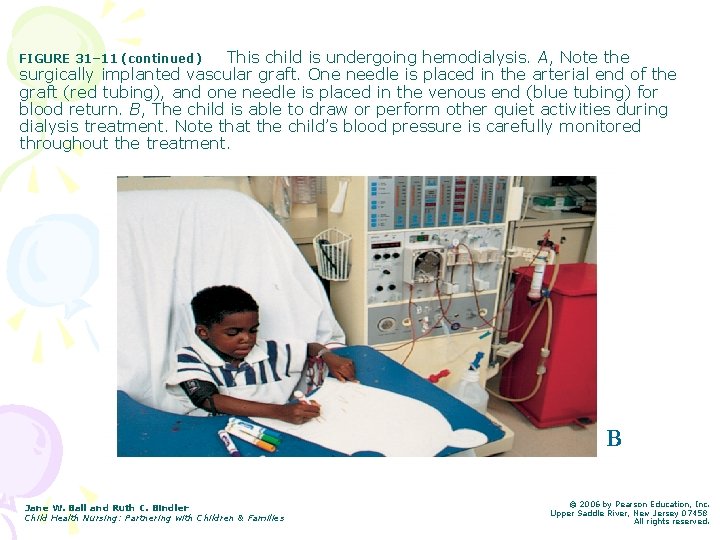
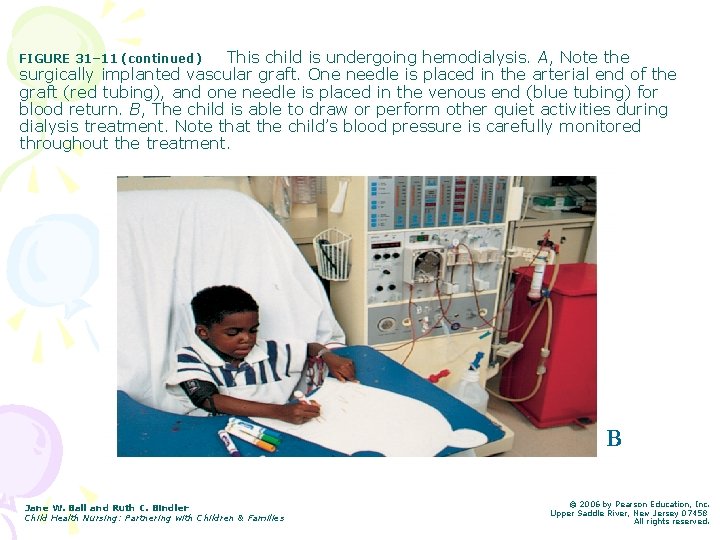
This child is undergoing hemodialysis. A, Note the surgically implanted vascular graft. One needle is placed in the arterial end of the graft (red tubing), and one needle is placed in the venous end (blue tubing) for blood return. B, The child is able to draw or perform other quiet activities during dialysis treatment. Note that the child’s blood pressure is carefully monitored throughout the treatment. FIGURE 31– 11 (continued) B Jane W. Ball and Ruth C. Bindler Child Health Nursing: Partnering with Children & Families © 2006 by Pearson Education, Inc. Upper Saddle River, New Jersey 07458 All rights reserved.
Renal Failure • Acute Renal Failure: – Refer to Table on pg 1200 for Clinical Manifestations • Nursing Management: – Monitor side effects of medications – Prevent infection – Meet nutritional needs (Table 31 -8 p 1207) – Maintain fluid restrictions – Provide emotional support – D/C planning: anticipatory teaching
Acute Postinfectious Glomerulonephritis • Glomerulonephritis: an inflammation of the glomeruli of the kidneys – Acute or chronic – In children, most often a response to GABHS infection of skin or pharynx (aka Post-Strep Glomerulonephritis) – Other organisms: Staph, Pneumococcus and coxsackievirus – Abx are not a tx for APIGN. Abx are Rx’d to tx the original infection
APIGN • Highest in children ages 2 -12 • More common during winter and spring months • The child typically has a h/o a recent respiratory infection (w/in 1 -2 weeks) or impetigo. • The child recovers from infection, then develops APIGN after 8 -14 days • Glomerular damage occurs as a result of an immune complex reaction that localizes on the glomerular capillary wall
APIGN • Clinical Manifestations: – % of children are asymptomatic – Abrupt onset of abdominal pain – Irritability – Microscopic hematuria (most all cases) – Acute HTN • Nonspecific symptoms – These can include general malaise, weakness, and anorexia and are present in 50% of patients. – Approximately 15% of patients complain of nausea and vomiting.
APIGN • Clinical Manifestations: • Dark urine (brown-, tea-, or cola-colored) – This is often the first clinical symptom. – Dark urine is caused by hemolysis of red blood cells that have penetrated the glomerular basement membrane and have passed into the tubular system. • Periorbital edema and dependent edema – The onset of puffiness of the face or eyelids is sudden. It is usually prominent upon awakening and, if the patient is active, tends to subside at the end of the day. – In some cases, generalized edema and other features of circulatory congestion, such as dyspnea, may be present. – Edema is a result of a defect in renal excretion of salt and water, and can result in HTN
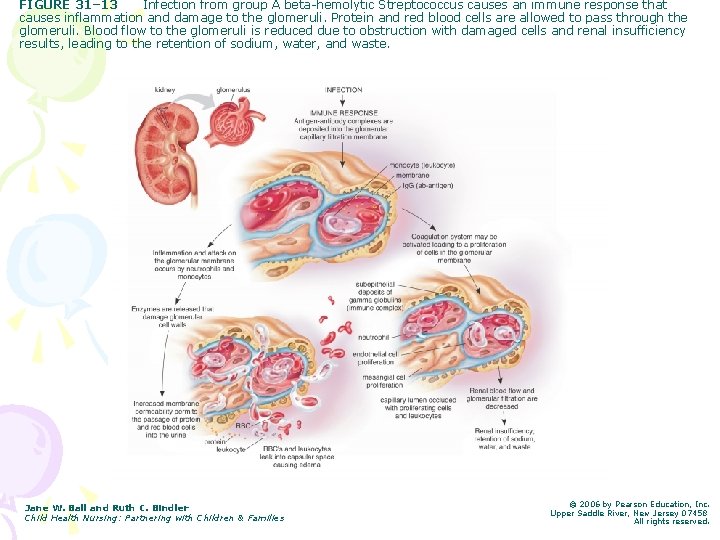
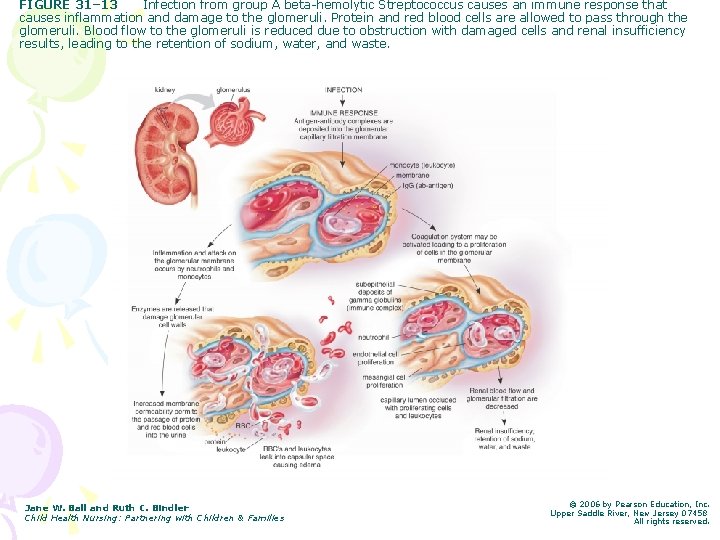
FIGURE 31– 13 Infection from group A beta-hemolytic Streptococcus causes an immune response that causes inflammation and damage to the glomeruli. Protein and red blood cells are allowed to pass through the glomeruli. Blood flow to the glomeruli is reduced due to obstruction with damaged cells and renal insufficiency results, leading to the retention of sodium, water, and waste. Jane W. Ball and Ruth C. Bindler Child Health Nursing: Partnering with Children & Families © 2006 by Pearson Education, Inc. Upper Saddle River, New Jersey 07458 All rights reserved.

APIGN • Lab Findings: – Hematuria – Proteinuria – Leukocytes – Decreased serum protein – Anemia – ESR increased – Serum Ig. G antibodies against Strep + – Circulatory overload causing EKG changes

APIGN Nursing Care • Assessment: – VS, especially BP – F&E’s with strict I’s & O’s, specific gravity – Daily weights – Urine dipstick for + hematuria, +proteinuria – Assess edema (periorbital, dependent) – Measure abdominal girth – Auscultate heart and lung sounds, not respiratory effort – Monitor neurologic signs secondary to HTN (LOC, HA, sz activity, vomitting)
Hemolytic Uremic Syndrome • Hemolytic uremic syndrome (HUS) is a disease primarily of infancy and early childhood. • It is characterized by the triad of hemolytic anemia, thrombocytopenia, and acute renal failure. • Diarrhea and upper respiratory infection are the most common precipitating factors. • HUS is the most common cause of acute renal failure in children. • It occurs mostly in infants and children from 6 months to 4 years.
HUS • Verotoxin causes damage to the lining of the glomerular arterioles resulting in swelling of the endothelial cells. • The lining of the glomerular arterioles becomes inflamed, swollen, and occluded w/ particles of platelets and fibrin. • RBC and PLTs are damaged as they flow through the partially occluded vessels. • As the damaged cells reach the spleen, they are destroyed and removed from circulation. This leads to hemolytic anemia. • 90% of children w/ this syndrome, have recently experienced E. coli GI infection. – Over ½ cases by contaminated beef

HUS • The bacterial infection causes endothelial cell injury in the lining of the small glomerular arterioles. • This cell damage triggers clotting mechanisms that occlude the arterioles and capillaries. • This plt aggregation results in thrombocytopenia (b/c plts are damaged by irregular blood cells), and the kidneys become swollen • Although damage occurs mainly in the endothesial lining of the glomerular arterioles, other organs can be involved (heart, pancreas)
HUS Clinical Manifestations • Prodromal stage: – URI • 1 -7 days: – fever, Irritability, weakness, lethargy, lymphadenopathy, skin rash, abdominal pain w/ N/V/D • Acute Stage: – Hemolytic anemia, HTN, Pallor and purpura, neurologic involvement, and renal failure
Management of HUS • Supportive tx to maintain kidney function • Daily plasma exchange until remission is achieved • Maintenance of fluid and electrolyte balance and correction of acidosis to prevent szs • Corticosteroids • Early dialysis if ARF develops • Management of HTN
HUS • Nursing Management: – Same as with acute kidney failure – Dialysis – Diet of small, high-calorie, high-carbohydrate – Diet of low Na++, potassium and phosphorus • Education and Prevention: – Reduce risk of consumption of cantaminated beef – Cook ground beef to 155 degrees – Wash hands when handling raw meat – Use meat thermometer
Toilet Training • Physical Readiness • Social and cultural aspects of toilet training in children (p 446 in text)
 Little families
Little families Partnering to build customer relationships
Partnering to build customer relationships The partnering initiative
The partnering initiative Mnos partnering
Mnos partnering Finance business partnering definition
Finance business partnering definition What is partnering
What is partnering Partnering session
Partnering session Effective support for children and families in essex
Effective support for children and families in essex Georgia department of children and families
Georgia department of children and families Concept of pediatric nursing
Concept of pediatric nursing Modern concept of paediatric nursing
Modern concept of paediatric nursing Pediatric nursing definition according to who
Pediatric nursing definition according to who Child health nursing gnm 2nd year question paper
Child health nursing gnm 2nd year question paper National health programmes for child
National health programmes for child Left child right sibling tree
Left child right sibling tree National health policy for children
National health policy for children Children's mental health
Children's mental health National children's digital health collaborative
National children's digital health collaborative Green paper children's mental health
Green paper children's mental health Nursing care of hospitalized child
Nursing care of hospitalized child Nursing care of hospitalized child
Nursing care of hospitalized child Hospital environment for sick child definition
Hospital environment for sick child definition Telethon institute for child health research
Telethon institute for child health research Aim of rch programme
Aim of rch programme National policies related to child health and welfare
National policies related to child health and welfare History of maternal and child health
History of maternal and child health Maternal and child health services
Maternal and child health services Preventive health and safety in the child care setting
Preventive health and safety in the child care setting Personal child health record
Personal child health record Parental rights over child's health
Parental rights over child's health Rch 2 programme
Rch 2 programme Utah department of health child care licensing
Utah department of health child care licensing Functional nursing care model
Functional nursing care model Nursing care plan for ocd patient
Nursing care plan for ocd patient Care plan of cataract
Care plan of cataract Nursing diagnosis three parts
Nursing diagnosis three parts Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Twenty point programme slideshare
Twenty point programme slideshare Types of nursing diagnosis
Types of nursing diagnosis How to write a care plan in nursing
How to write a care plan in nursing Function of community health nurse
Function of community health nurse Mental health definition in nursing
Mental health definition in nursing Community health nursing principles
Community health nursing principles Define occupational health nursing
Define occupational health nursing 5 phases of the nursing process
5 phases of the nursing process Mrbs scholarship
Mrbs scholarship Community oriented nursing definition
Community oriented nursing definition Shuster and goeppinger
Shuster and goeppinger Types of community bag
Types of community bag Cumulative index to nursing and allied health literature
Cumulative index to nursing and allied health literature Historical development of community health nursing
Historical development of community health nursing Unit eleven fitness
Unit eleven fitness Professional nursing practice: concepts and perspectives
Professional nursing practice: concepts and perspectives Characteristics of community health nursing
Characteristics of community health nursing Nola pender nursing metaparadigm
Nola pender nursing metaparadigm Phases of home visiting
Phases of home visiting Characteristics of community health nursing
Characteristics of community health nursing Objective of family health care
Objective of family health care Family care plan in community health nursing
Family care plan in community health nursing Elements of primary health care
Elements of primary health care Evolution of community health nursing
Evolution of community health nursing Culturological assessment
Culturological assessment Function of community health nursing
Function of community health nursing Legal issues in community health nursing
Legal issues in community health nursing Introduction of arthropods
Introduction of arthropods Core functions of public health nursing
Core functions of public health nursing Components of community health nursing
Components of community health nursing Conclusion of community mental health nursing
Conclusion of community mental health nursing Florida healthfinder
Florida healthfinder Epidemiology concept
Epidemiology concept Word families examples
Word families examples Propagation delay in logic families
Propagation delay in logic families Thanksgiving is celebrated in autumn fact or opinion
Thanksgiving is celebrated in autumn fact or opinion Lesson 3 keeping the family healthy
Lesson 3 keeping the family healthy Romeo and juliet intro
Romeo and juliet intro Personal facet
Personal facet Periodic table of elements families
Periodic table of elements families Periodic table element families
Periodic table element families Families in the periodic table
Families in the periodic table Varies from family to family on the periodic table
Varies from family to family on the periodic table Paradox of our time
Paradox of our time