CHF Dementia and Palliative Care Lisa Dusch CRNP











- Slides: 30

CHF, Dementia and Palliative Care Lisa Dusch, CRNP Gallagher Home Health September 9, 2015
CHF • DEFINITION - Heart failure is a complex clinical syndrome that results from any structural or functional disorder that impairs the ability of the ventricles to fill with or eject blood at a rate to fulfill the body’s needs. If there are clinical signs and symptoms of volume overload the term congestive heart failure is used.
CHF • 10 in 1000 aged 65 or older will develop heart failure • 80% of patients who develop heart failure are 65 or older • 2012 estimated 30. 7 billion dollars 80% of that is related to hospitalization • 83% of those diagnosed with heart failure were admitted once and 43% at least four times
CHF • • • Abdominal distention Acute confusional state, delirium Anorexia Anxiety or restlessness Decline in functional status • • • Decreased exercise tolerance Dizziness Dyspnea at rest Dyspnea on exertion Fatigue • Orthopnea (sensation of breathlessness in a recumbent position, relieved by sitting or standing; sleeping on two or more pillows to relieve the sensation of breathlessness is suggestive of heart failure. In a patient with cognitive impairment or difficulty in using language, orthopnea may present as restlessness or agitation when supine) • Paroxysmal nocturnal dyspnea (sensation of shortness of breath that awakens the patient, often after 1 or 2 hours of sleep, that is usually relieved in the upright position) • Unexplained cough (typically a dry, nonproductive cough) or wheezing, especially at night
Signs of advanced heart failure • Ascites or increased abdominal girth • Increased jugular venous pressure • Lower limb edema not used by venous insufficiency or obstruction (sacral edema must also be assessed with attention to patients with decreased mobility) • • • Positive hepatojugular reflux Rales on lung exam Tachycardia, tachypnea, hypotension, or hypoxia Third heart sound (S 3) Weight gain
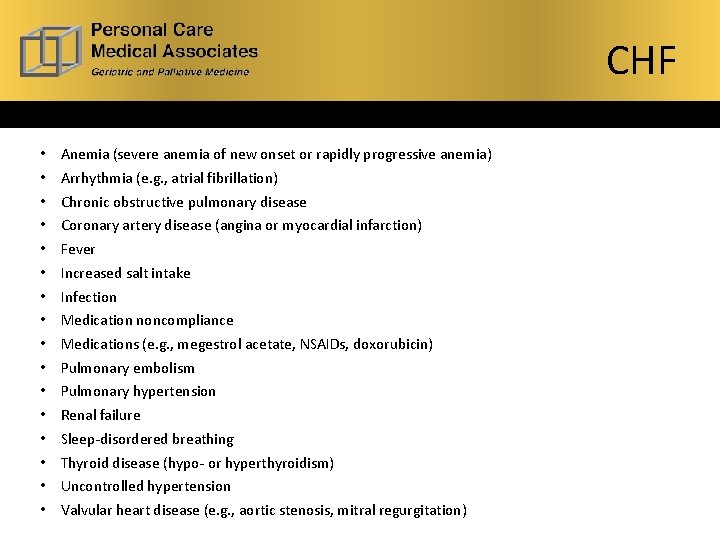
CHF Common Risk Factors for Heart Failure Exacerbation • • • • Anemia (severe anemia of new onset or rapidly progressive anemia) Arrhythmia (e. g. , atrial fibrillation) Chronic obstructive pulmonary disease Coronary artery disease (angina or myocardial infarction) Fever Increased salt intake Infection Medication noncompliance Medications (e. g. , megestrol acetate, NSAIDs, doxorubicin) Pulmonary embolism Pulmonary hypertension Renal failure Sleep-disordered breathing Thyroid disease (hypo- or hyperthyroidism) Uncontrolled hypertension Valvular heart disease (e. g. , aortic stenosis, mitral regurgitation)
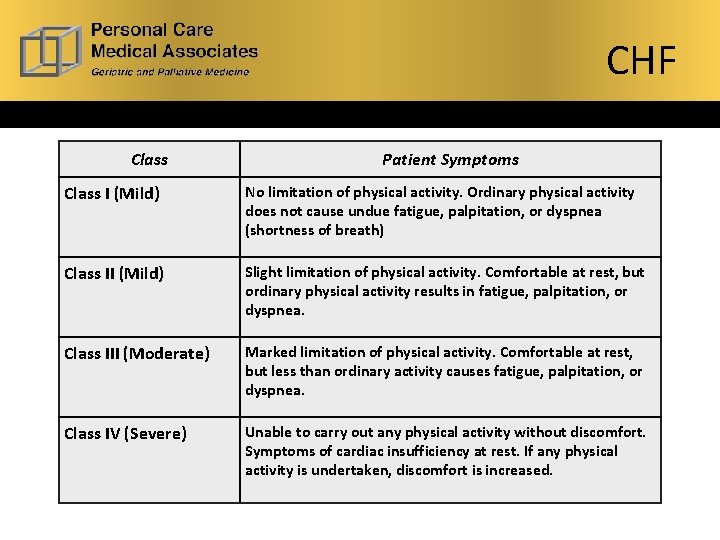
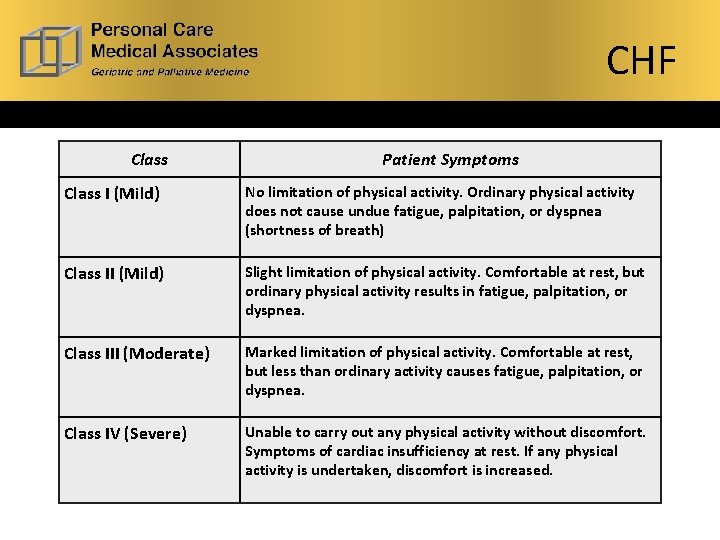
CHF Class Patient Symptoms Class I (Mild) No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, or dyspnea (shortness of breath) Class II (Mild) Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in fatigue, palpitation, or dyspnea. Class III (Moderate) Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes fatigue, palpitation, or dyspnea. Class IV (Severe) Unable to carry out any physical activity without discomfort. Symptoms of cardiac insufficiency at rest. If any physical activity is undertaken, discomfort is increased.

CHF Heart failure defined by Left ventricular dysfunction, may be: systolic, diastolic, or both 1. Heart failure with reduced left ventricular ejection fraction = systolic heart failure 2. Heart failure with preserved left ventricular ejection fraction = diastolic heart failure Most common causes of both: CAD and HTN
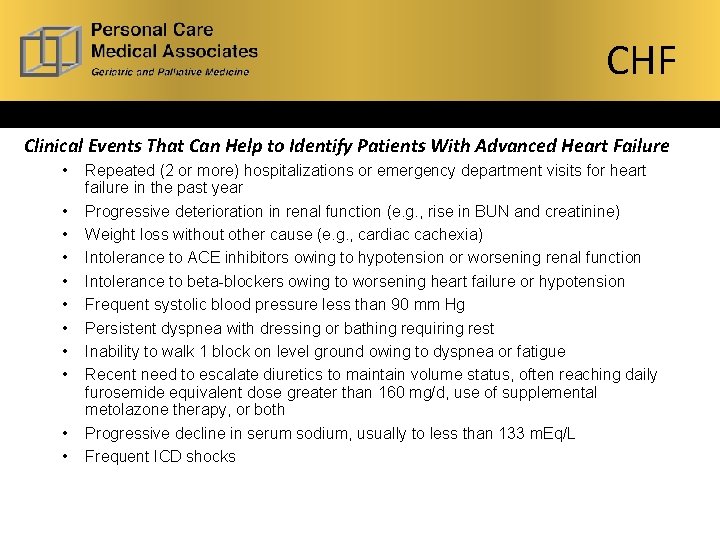
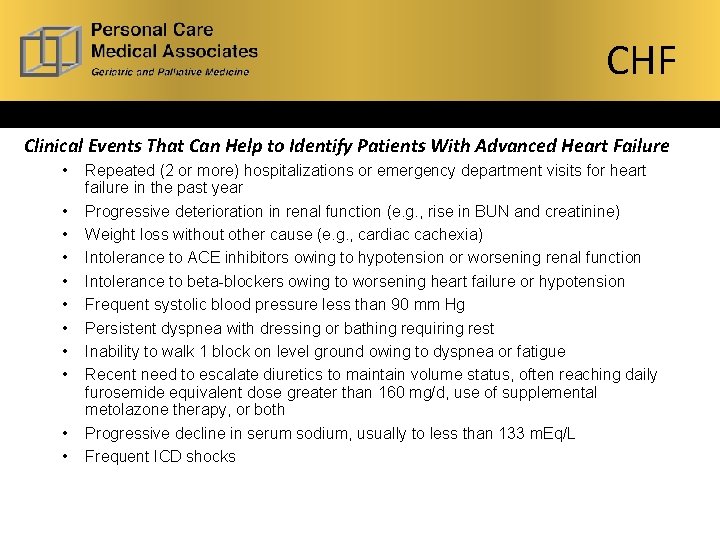
CHF Clinical Events That Can Help to Identify Patients With Advanced Heart Failure • • • Repeated (2 or more) hospitalizations or emergency department visits for heart failure in the past year Progressive deterioration in renal function (e. g. , rise in BUN and creatinine) Weight loss without other cause (e. g. , cardiac cachexia) Intolerance to ACE inhibitors owing to hypotension or worsening renal function Intolerance to beta-blockers owing to worsening heart failure or hypotension Frequent systolic blood pressure less than 90 mm Hg Persistent dyspnea with dressing or bathing requiring rest Inability to walk 1 block on level ground owing to dyspnea or fatigue Recent need to escalate diuretics to maintain volume status, often reaching daily furosemide equivalent dose greater than 160 mg/d, use of supplemental metolazone therapy, or both Progressive decline in serum sodium, usually to less than 133 m. Eq/L Frequent ICD shocks
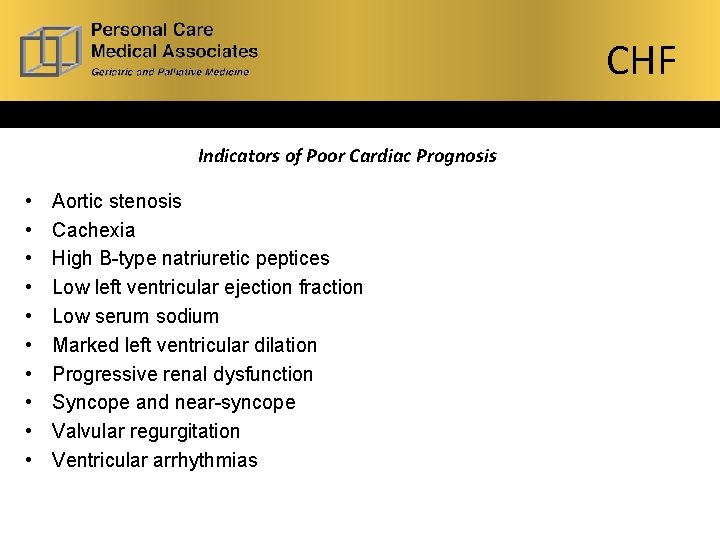
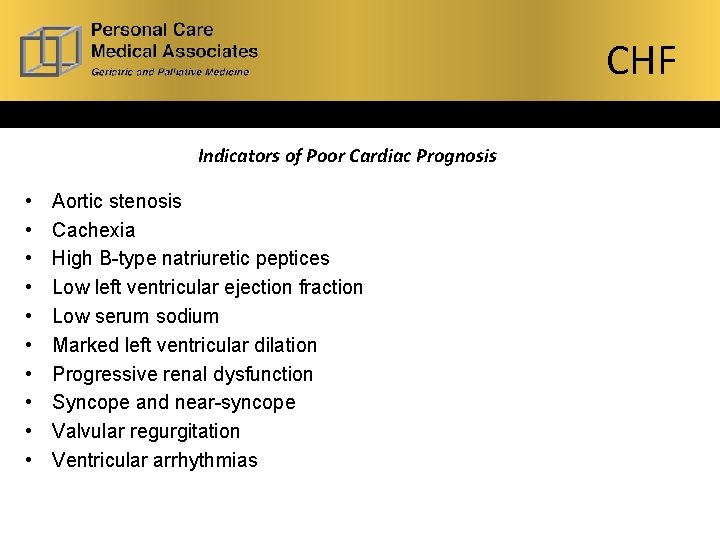
CHF Indicators of Poor Cardiac Prognosis • • • Aortic stenosis Cachexia High B-type natriuretic peptices Low left ventricular ejection fraction Low serum sodium Marked left ventricular dilation Progressive renal dysfunction Syncope and near-syncope Valvular regurgitation Ventricular arrhythmias
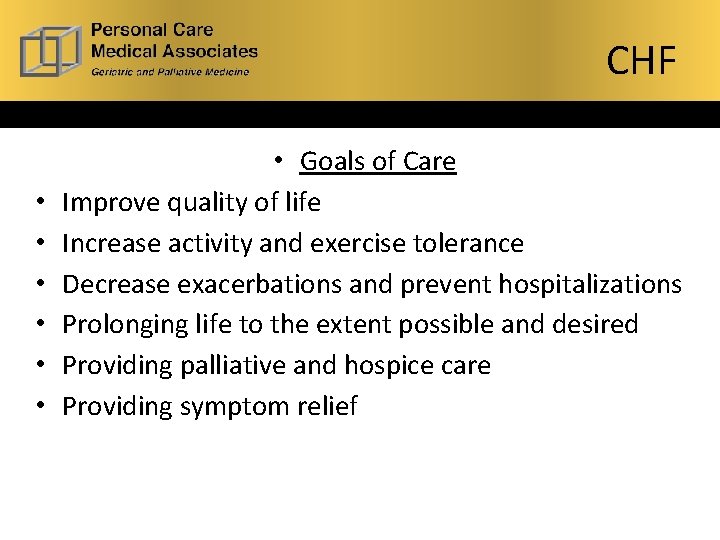
CHF • • Goals of Care Improve quality of life Increase activity and exercise tolerance Decrease exacerbations and prevent hospitalizations Prolonging life to the extent possible and desired Providing palliative and hospice care Providing symptom relief
CHF • Routine Care –goal is to improve symptoms, slow or reverse deterioration of myocardial function, and reduce mortality. • Pharmocologic interventions- diuretics, Ace I, ARBs, B Blockers, Aldosterone receptor antagonists, hyadralazine, isosorbide dinitrate, digoxin, anti coagulation, statins. • Lifestyle modifications: Cessation of smoking, restriction of alcohol consumption, salt restriction, fluid restriction, weight reduction, daily weight monitoring • Device therapy- ICD, CRT (bi ventricular pacing)

CHF Palliative care – goal is symptom management and addressing patients goals for medical care. • Fluid overload- diuretics- monitor daily weights, may "self manage if pt or caregiver able to adjust dose with weights" • Fatigue- improve dietary compliance with fluids and sodium. - consider treatment of anemia with erythropoietin, to improve exercise capacity. -opioids and caffeine may improve exertional fatigue. -thigh strengthening may improve fatigue. -CPAP – improves LVF, daytime alertness, and exercise capacity

CHF • Dyspnea – medications as mentioned previously -Exercise training focusing on thigh strengthening. -Morphine- acts by reducing chemo sensitivity , reduce hypoxic ventilatory drive, act on opioid receptors in the lung, and may unload volume. Improving exercise tolerance and exercise related dyspnea. • Pain management – 40 to 75 % of pts with advanced HF -try local treatments if appropriate. -NO NSAIDs due to may impair renal function and Can cause Na and fluid retention – worsening HF -consider pain management with low renal such as Fentanyl or hydromorophone
CHF • Nausea- 50 % of HF puts report nausea in last 6 months - due to medications, liver, kidney disease, or increased gastric acidity. - consider dig toxicity, eliminate medications one by one if necessary - PPI, anti emetics if vomiting - Lorazepam may be best first choice – no effect on QT like other anti emetics
CHF • Depression- discuss concerns, spiritual, social, personal? - consider SSRI – paxil did well in studies with HF • ICD deactivation- discuss with pt and family - discuss benefits and burdens of ICD and when or if pt desires Device to be disabled
Dementia Definition: Dementia is a disorder that is characterized by a decline in cognition involving one or more cognitive domains. The deficits must represent a decline from previous level of function and be severe enough to interfere with daily function and independence.
Dementia Syndromes: • Alzheimer's disease- neurodegenerative disease, most common form of dementia, usually occurs after the age of 60, most common early symptom is memory loss • Dementia with Lewy Bodies –characterized by deficits in attention and visuospatial function, fluctuating cognition, visual hallucinations, and motor features of parkinsonism

Dementia • Frontotemporal Dementia- earlier onset, of neurodegenerative disorders characterized by prominent changes in social behavior and personality. Disinhibition, hyperorality, compulsive behaviors, apathy and the loss of empathy.
• Vascular dementia-characterized by deficits in executive function while memory impairment is quite mild in early phase of disease. Large artery infarction so, small artery infarctions, and chronic subcorticall ischemia aren't he pathological entities thought to contribute to vascular dementia.

Dementia • Parkinson's disease with dementia- cognitive dysfunction is common in PD, prevalence increases with the duration of the movement disorder. Dementia often surpasses the motor features of PD and becomes the major cause of disability and mortality.
Dementia Cognitive testing MMSE – copyrighted, covers most cognitive domains, particularly for AD. http: //www. sco. edu/assets/1813/course_5_b_handout. pdf Mini Cog – clock drawing task and uncued recall of 3 unrelated words. High sensitivity for predicting dementia status, short testing time and diagnostic value is not limited by the subjects education or language. http: //www. alz. org/documents_custom/minicog. pdf Clock drawing – covers multiple cognitive domains in a single task. Draw a clock and ask for hands to tell a certain time. Are numbers sequential and in appropriate place? https: //www. healthcare. uiowa. edu/igec/tools/cognitive/clock. Drawi ng. pdf

Dementia • Early treatment - cholinesterase inhibitors – Aricept (donepezil) and Exelon (rivastigmine) - the average benefit of cholinesterase inhibitors in patients with dementia is a small improvement in cognition and ADLs. Unsure if significant improvement in long-term outcomes, such as need for nursing home placement or maintaining ADLS. Evidence is conflicting. -stop treatment after no improvement or worsening of symptoms. If symptoms worsen after d/c, restart medication. -add memantine for moderate to severe disease, now in a combo capsule - manage environment, address safety issues, add services as necessary - refer family/caregivers to support groups

Dementia • Palliative care of dementia Delusions/hallucinations –if fleeting or unobtrusive to pt and caregiver, do not medicate -if severe or obtrusive – rule out medical issues such as infection or medication toxicity. - antibiotics only with evidence of infection and reason to treat. i. e. UTI with dysuria and fever and/or mental status changes, not just foul smelling urine
Dementia • Mild to moderate agitation -non pharm – controlled environment, personcentered care, aromatherapy, music therapy, distraction, redirection. Pharmacologic interventions -pain control – scheduled analgesics, start low and go slow, monitor effectiveness. - uncertain benefit – tegretol, valproate, gabapentin, lamotrigine - avoid – benzodiazepines, antihistamines

Dementia • Severe aggression/psychosis - antipsychotic drugs- may increase mortality, if benefits outweigh risks and families are advised of risk, using medication may be necessary. -olanzapine – start 2. 5 mg increase to 5. 0 mg BID - Risperdal after more than 1. 0 mg daily increased side effects - quetapine- starting at 25 mg hs and titration up to 75 mg bid
Dementia • Eating problems – onset is a hallmark of advanced dementia - cause: oral dysphasia (pocketing, spitting) - pharyngeal dysphasia – delayed swallowing, aspiration - oral vs tube feeding, recommendations from AGS – spoon feeding as effective as PEG

Dementia Family/Caregiver support • Recommend accepting help from others • Encourage respite periods • Recommend support groups/web sites • Extend emotional support

What’s next The next presentation on 9/30/2015 will cover COPD disease process and treatment along with a discussion of advanced directives and POLST completion.
This presentation is the property of Personal Care Medical Associates and is not to be distributed to, nor shared with any other organization without written consent from authors.