CHEW ON THIS TEACHING PREREQUISITE SKILLS TO INCREASE
- Slides: 39
CHEW ON THIS: TEACHING PREREQUISITE SKILLS TO INCREASE FOOD ACCEPTANCE Connie Ng & Sarah Leadley
About Us Connie Ng Sarah Leadley Acknowledgements : Dr. Laura Grow
Feeding Disorders O Includes the following topographies (Field et al, 2003) O Food refusal - Refusal to eat all/most foods & failure to meet caloric needs O Selectivity by type O Selectivity by texture O Oral motor problems (chewing etc. ) O Dysphagia (swallowing)
Oral motor skills: • Chewing: 5 18 mo. • Tongue lateralisation: 7 • Lip closure: 7 15 mo. 12 mo. O’Brien et al. , (1991), Overland, M. & Rosenfield-Johnson (1993)
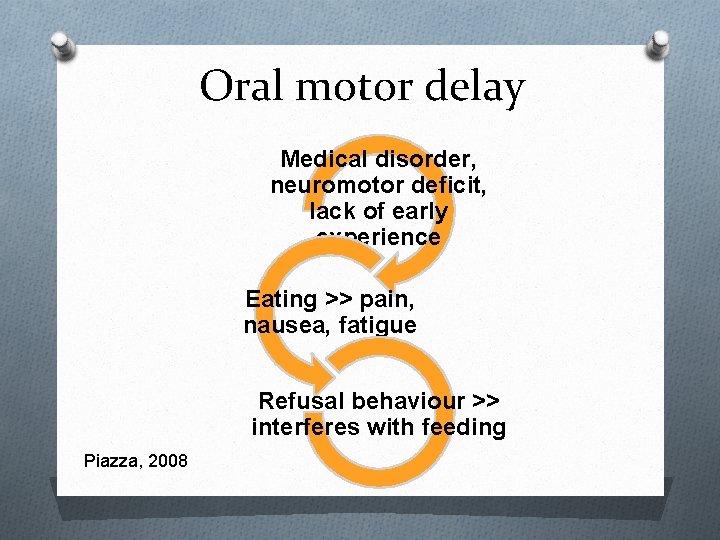
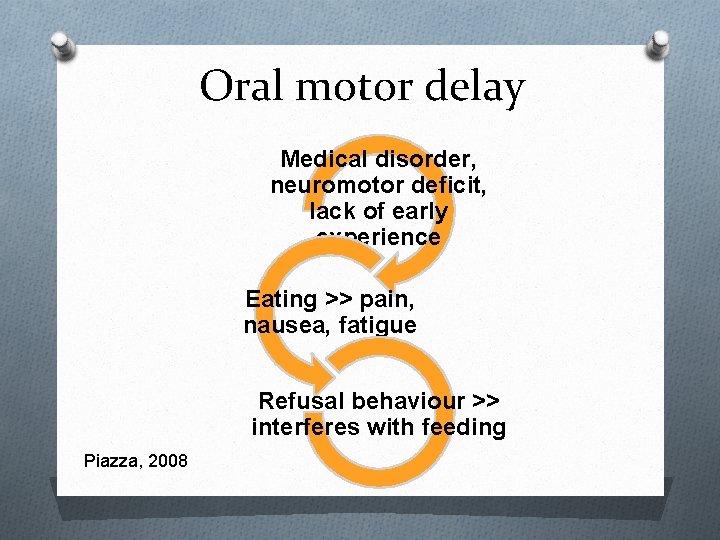
Oral motor delay Medical disorder, neuromotor deficit, lack of early experience Eating >> pain, nausea, fatigue Refusal behaviour >> interferes with feeding Piazza, 2008
Teaching oral motor skills: Limited Research Gisel (1996), OT O Taught tongue lateralisation with foods placed in mouth, lip closure around a licorice stick/straw, and chewing with small pieces of gelatin/cookies. O No behavioural procedures O No measure of food consumption, but reported increase in solids during session O No generalisation
Teaching oral motor skills: Limited Research Eckman et al. (2008) ABA O Taught chewing, tongue lateralisation, and lip closure using an open cup O Reinforcement, shaping, escape ext. O Texture fading to progress to table foods O Parent training and generalisation to meals O Substantial increase in foods eaten O In both studies, potential for child to swallow without chewing
Case Study - Client background O 9 years old O Down Syndrome and ASD O Significant medical concerns in early life & hospitalisation O Lack of early feeding experience O New home program O Buy-in gained with toilet training
Feeding concerns O Daily intake = baby food/yoghurt (11 g/meal) and 5 -6 cans of pediasure. O History of verbal refusal, gagging/spitting when more solid foods presented and risk of choking O No medical concerns prohibiting eating O Often fed by an adult O Interested in some solid/soft foods in novel contexts
Initial programs O Self-feeding to independence O GMI of chewing & Video modeling O Safety concerns O Referral made to Feeding Skills Team for further consultation O Attempts to replicate Eckman et al. , (2008)
Feeding team recommendations O Spit out bowl O Combine foods with preferred dips O Play and exploration O Place foods into mouth for chewing practice with model O Add increased texture to family meals O Goal – to eat a solid meal by end of summer (<2 mo. )
Seeking further consultation O Concerns with risk in using solid food O Video of sessions Dr. Grow @ UBC O Stop use of solid food in intervention sessions and concentrate on building jaw muscles for chewing O And, rule out food selectivity
Constructive Collaboration O Follow-up with recommendations from the feeding team Image from: http: //purehealthguide. com/2012/04/healthy-party-snacks-dips/
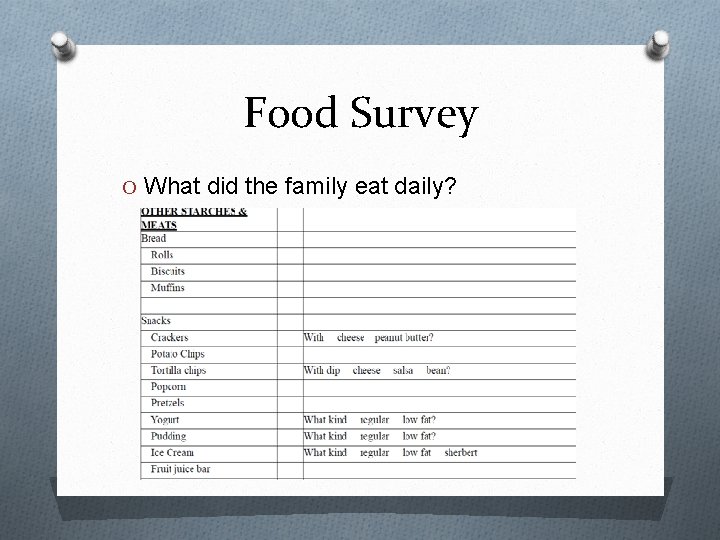
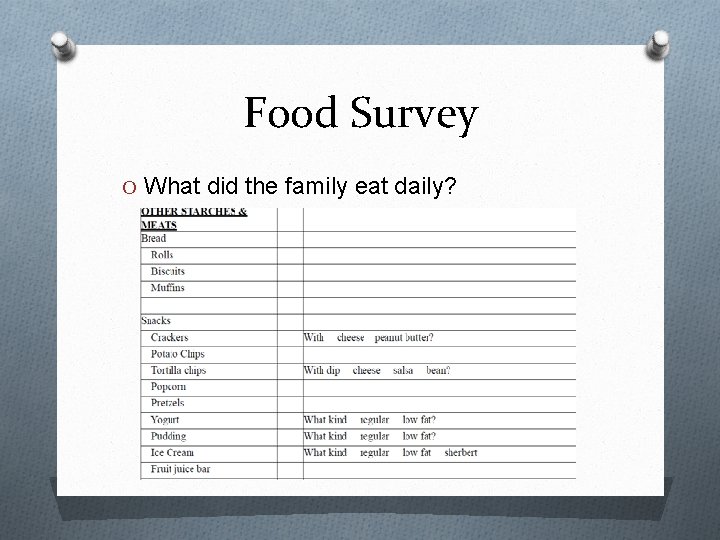
Food Survey O What did the family eat daily?
Ruling out food selectivity O Acceptance Image from: ”http: //babyawearnessblogspot. ca/2010_09_01_archive. html O 92% success rate during baseline phase
Constructive collaboration O Effort made to use feeding team strategies… BUT: - Use of dips/exploration unsuccessful and counter productive - Food refusal ruled out - Info shared with FT, including new plan to teach chewing - Agreement gained
Intervention 1: Teaching ‘hard chews’ Image from: http: //www. alibaba. com/productgs/407985589/yellow_dipped_natural_latex_tubing. html
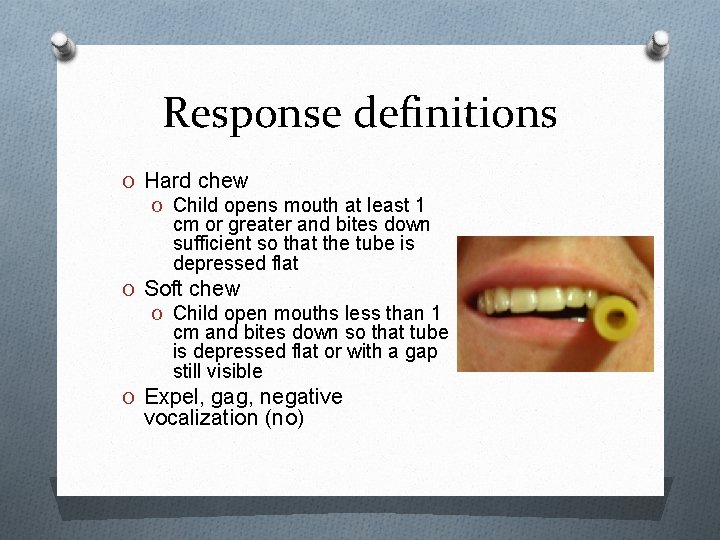
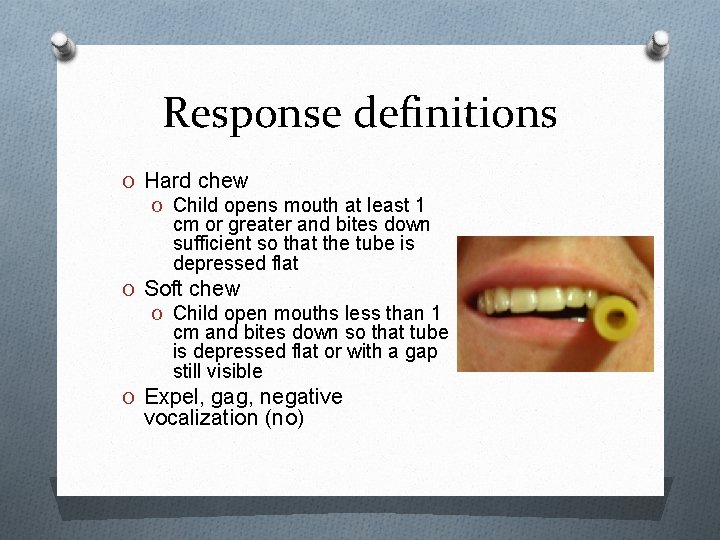
Response definitions O Hard chew O Child opens mouth at least 1 cm or greater and bites down sufficient so that the tube is depressed flat O Soft chew O Child open mouths less than 1 cm and bites down so that tube is depressed flat or with a gap still visible O Expel, gag, negative vocalization (no) /
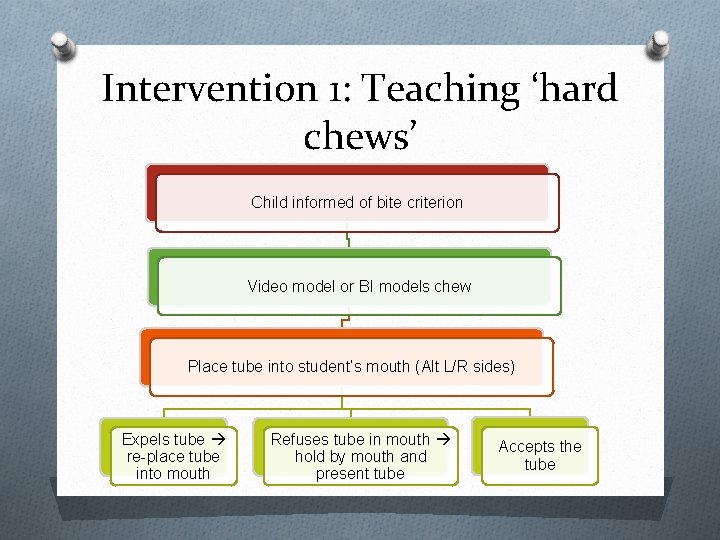
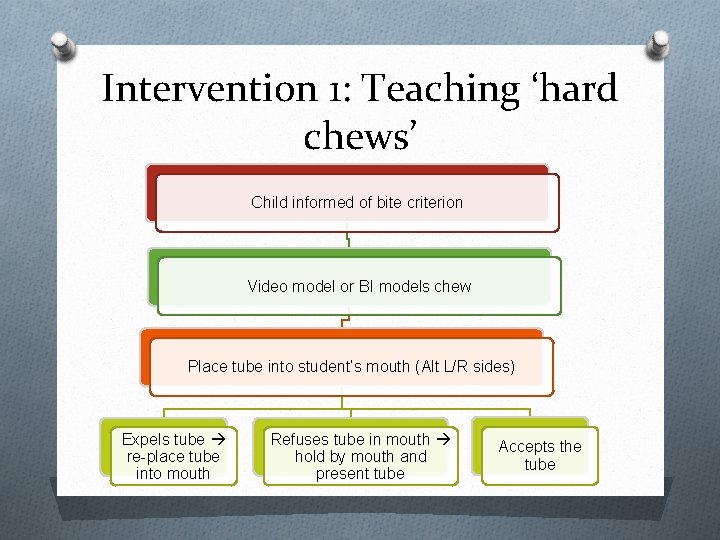
Intervention 1: Teaching ‘hard chews’ Child informed of bite criterion Video model or BI models chew Place tube into student’s mouth (Alt L/R sides) Expels tube re-place tube into mouth Refuses tube in mouth hold by mouth and present tube Accepts the tube
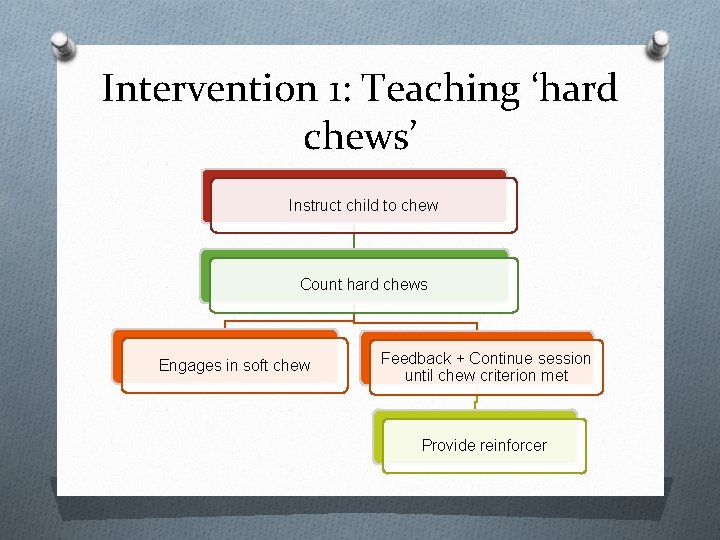
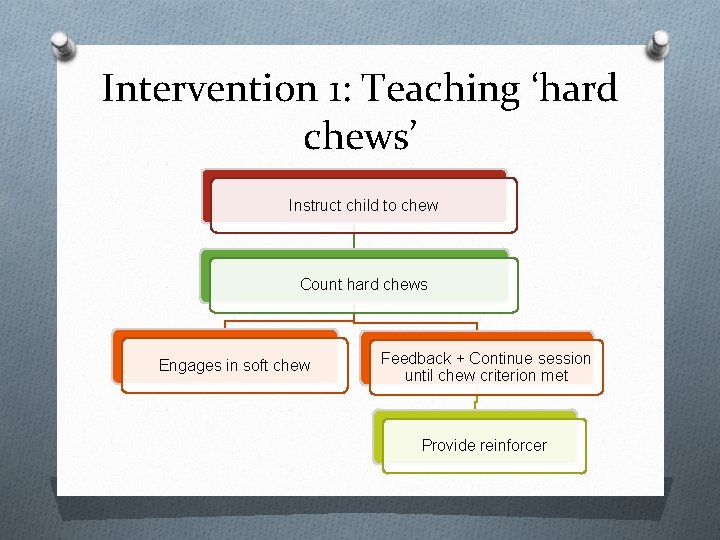
Intervention 1: Teaching ‘hard chews’ Instruct child to chew Count hard chews Engages in soft chew Feedback + Continue session until chew criterion met Provide reinforcer
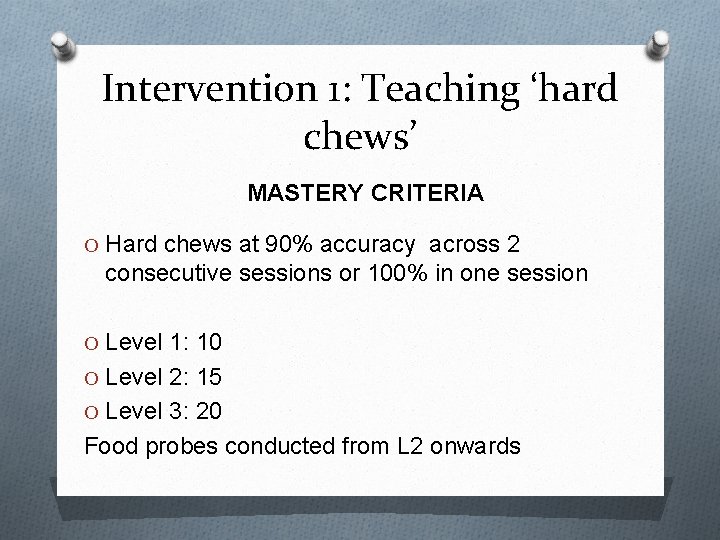
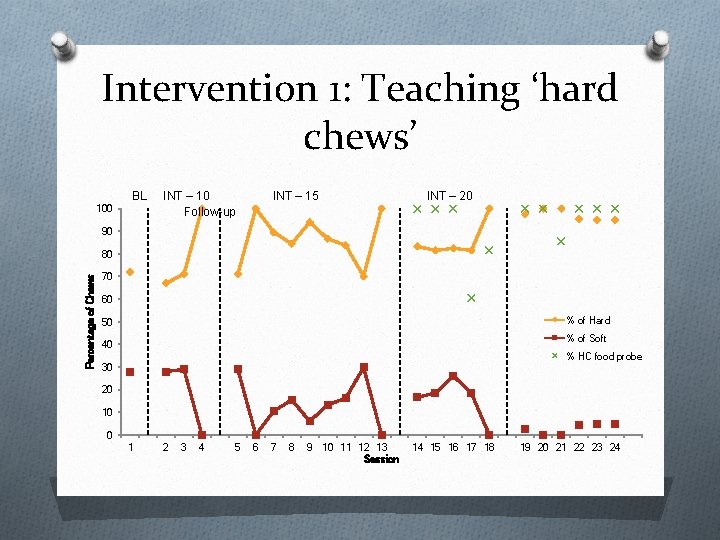
Intervention 1: Teaching ‘hard chews’ MASTERY CRITERIA O Hard chews at 90% accuracy across 2 consecutive sessions or 100% in one session O Level 1: 10 O Level 2: 15 O Level 3: 20 Food probes conducted from L 2 onwards
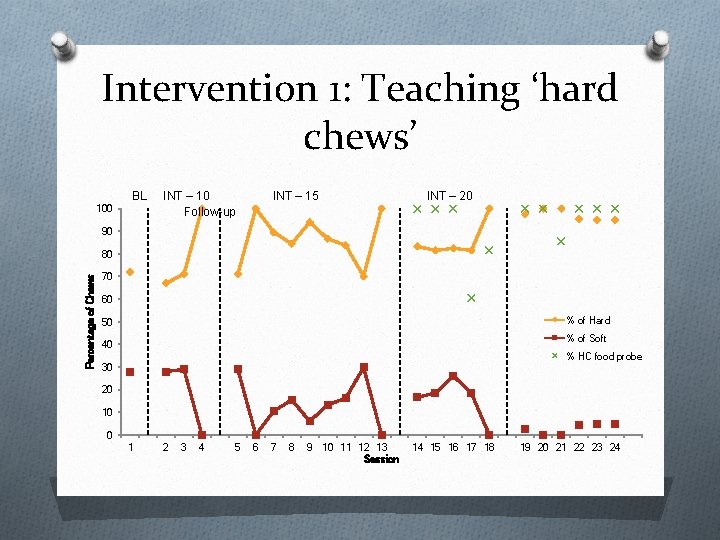
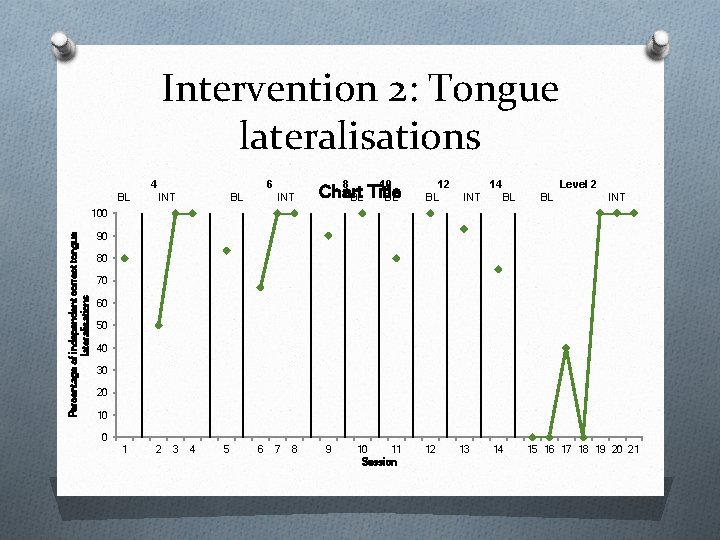
Intervention 1: Teaching ‘hard chews’ BL 100 INT – 10 Follow-up INT – 15 INT – 20 90 Percentage of Chews 80 70 60 % of Hard 50 % of Soft 40 % HC food probe 30 20 10 0 1 2 3 4 5 6 7 8 9 10 11 12 13 Session 14 15 16 17 18 19 20 21 22 23 24
Intervention 2: Tongue Lateralisations Materials Image from: http: //fineartamerica. com/featured/close-up -of-q-tips-yali-shi. html Image from: http: //www. bakingandboys. com/2009/02/worldnutella-day-celebrate-with. html
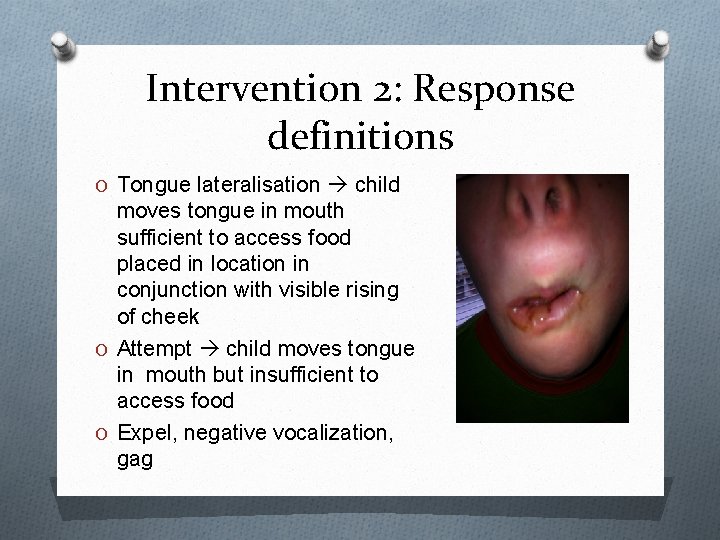
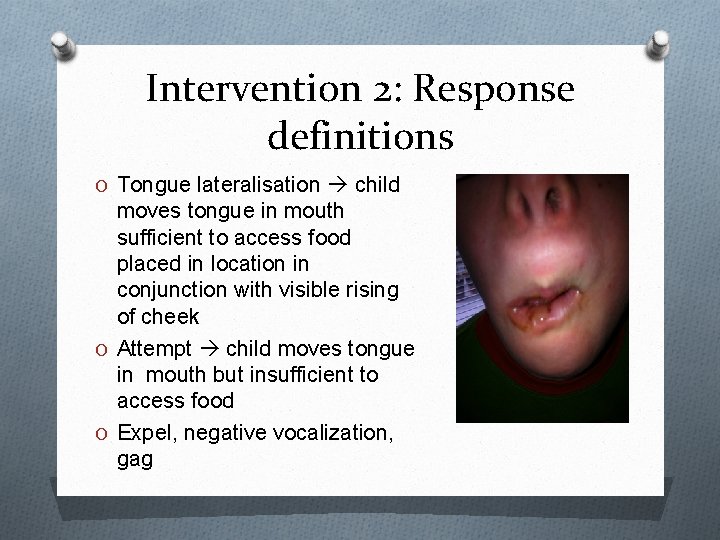
Intervention 2: Response definitions O Tongue lateralisation child moves tongue in mouth sufficient to access food placed in location in conjunction with visible rising of cheek O Attempt child moves tongue in mouth but insufficient to access food O Expel, negative vocalization, gag
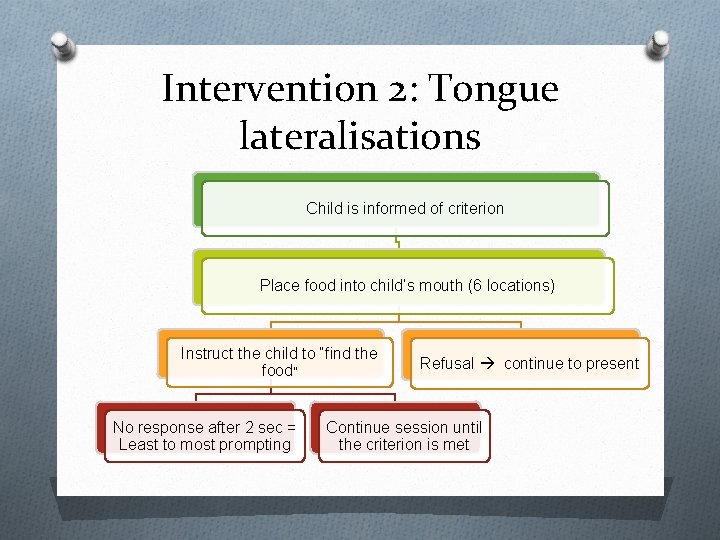
Intervention 2: Tongue lateralisations Child is informed of criterion Place food into child’s mouth (6 locations) Instruct the child to “find the food” No response after 2 sec = Least to most prompting Refusal continue to present Continue session until the criterion is met
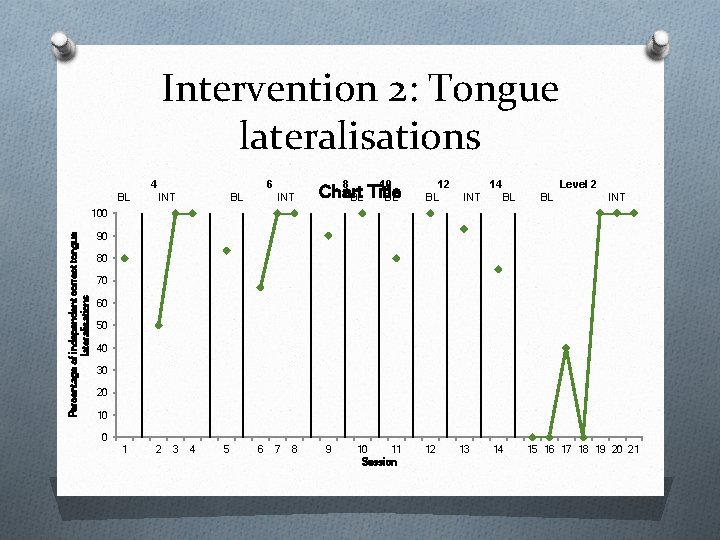
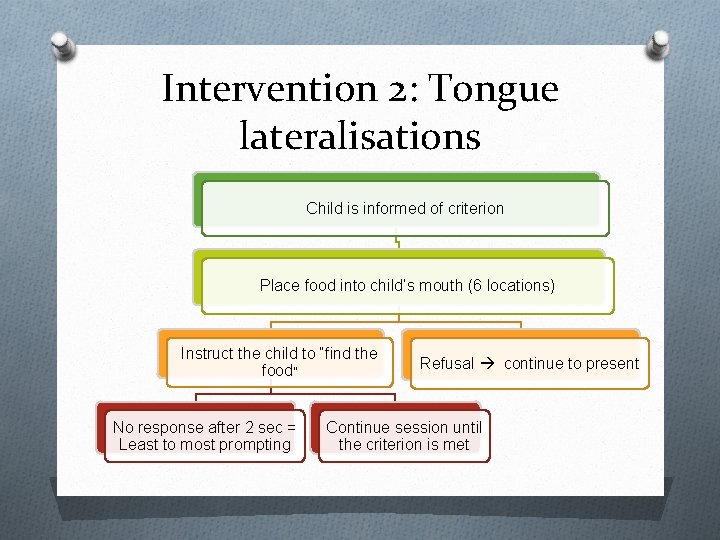
Intervention 2: Tongue lateralisations 4 BL 6 INT BL 8 INT 10 Chart BL Title BL 12 BL 14 INT Level 2 BL BL INT Percentage of independent correct tongue lateralisations 100 90 80 70 60 50 40 30 20 10 0 1 2 3 4 5 6 7 8 9 10 11 Session 12 13 14 15 16 17 18 19 20 21
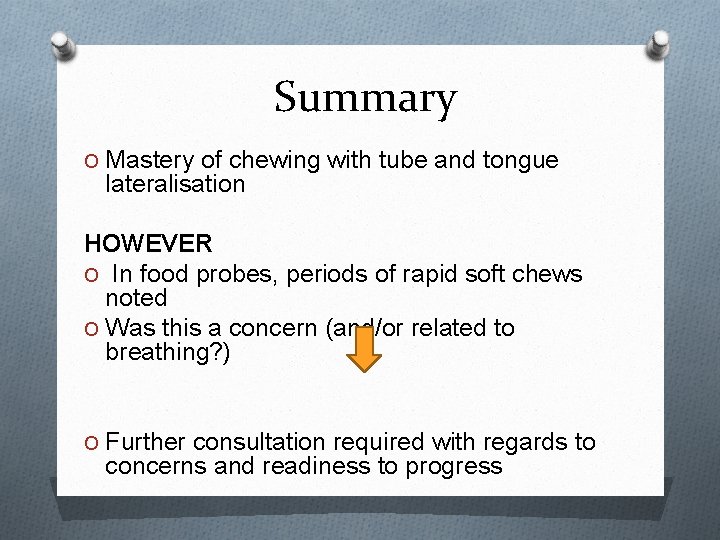
Summary O Mastery of chewing with tube and tongue lateralisation HOWEVER O In food probes, periods of rapid soft chews noted O Was this a concern (and/or related to breathing? ) O Further consultation required with regards to concerns and readiness to progress
Constructive Collaboration #2 O Session videos sent to Feeding Team O Joint appointment arranged O FT Recommended all meals to be presented solid
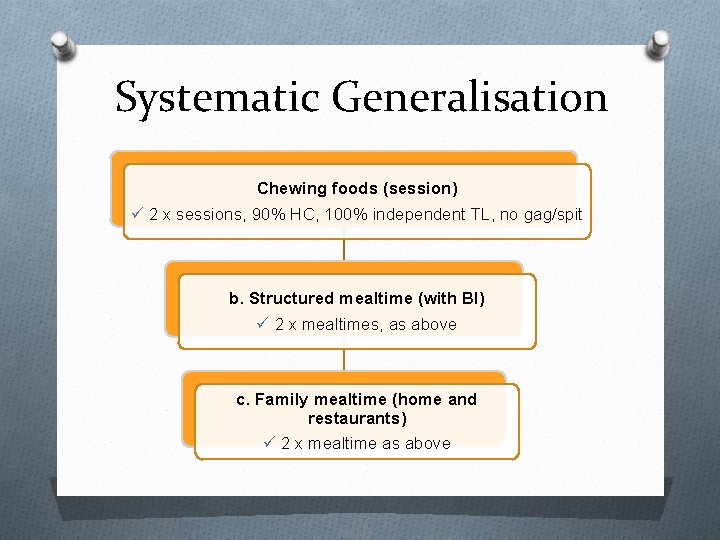
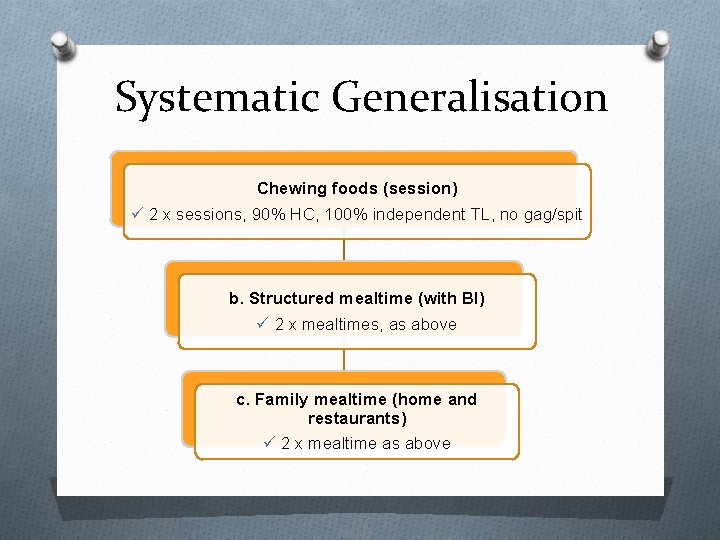
Systematic Generalisation Chewing foods (session) 2 x sessions, 90% HC, 100% independent TL, no gag/spit b. Structured mealtime (with BI) 2 x mealtimes, as above c. Family mealtime (home and restaurants) 2 x mealtime as above
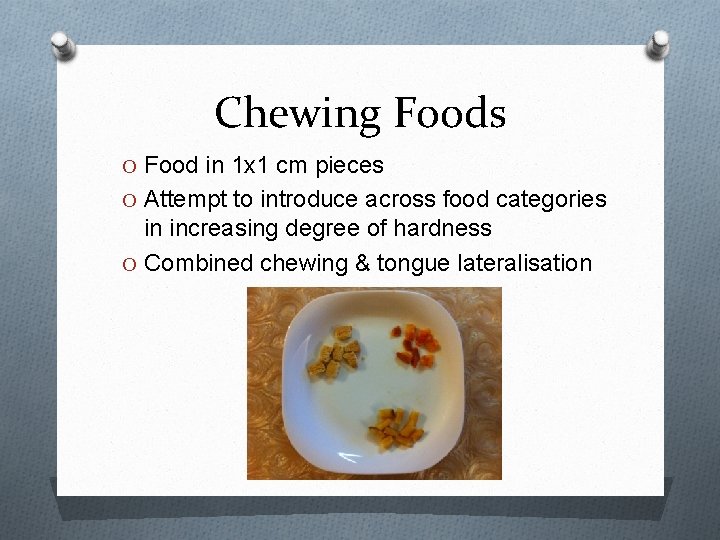
Chewing Foods O Food in 1 x 1 cm pieces O Attempt to introduce across food categories in increasing degree of hardness O Combined chewing & tongue lateralisation
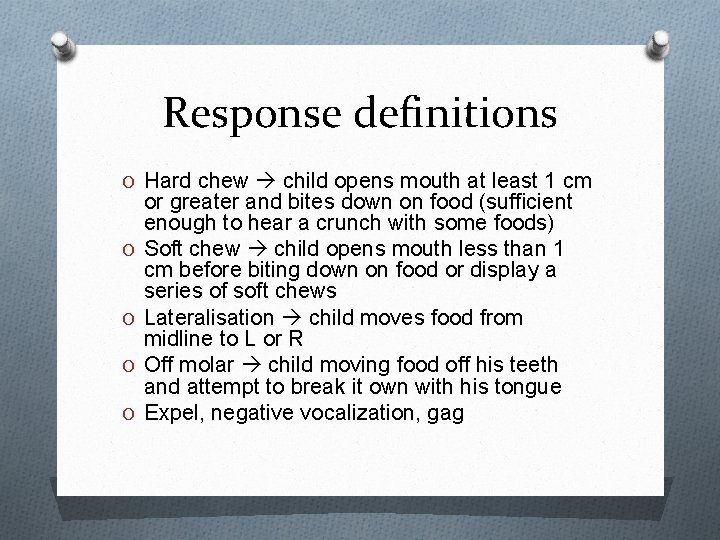
Response definitions O Hard chew child opens mouth at least 1 cm O O or greater and bites down on food (sufficient enough to hear a crunch with some foods) Soft chew child opens mouth less than 1 cm before biting down on food or display a series of soft chews Lateralisation child moves food from midline to L or R Off molar child moving food off his teeth and attempt to break it own with his tongue Expel, negative vocalization, gag
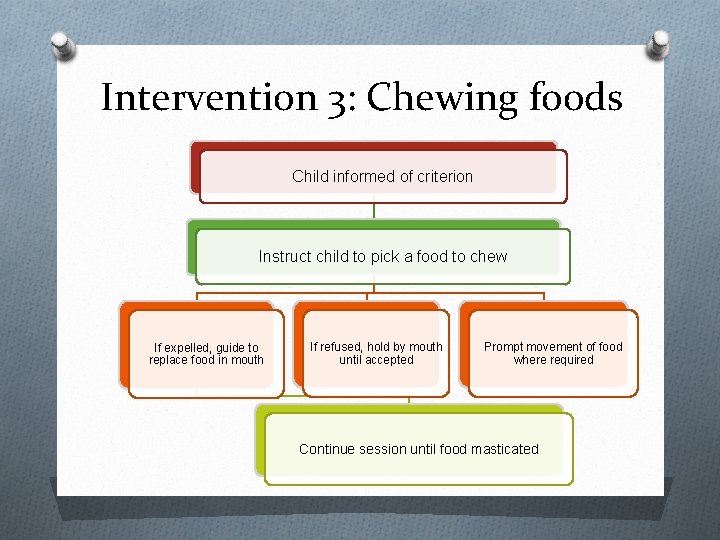
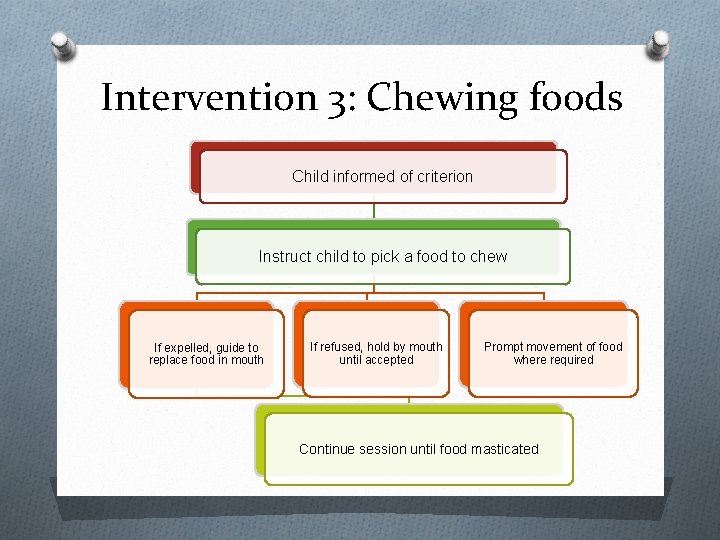
Intervention 3: Chewing foods Child informed of criterion Instruct child to pick a food to chew If expelled, guide to replace food in mouth If refused, hold by mouth until accepted Prompt movement of food where required Continue session until food masticated
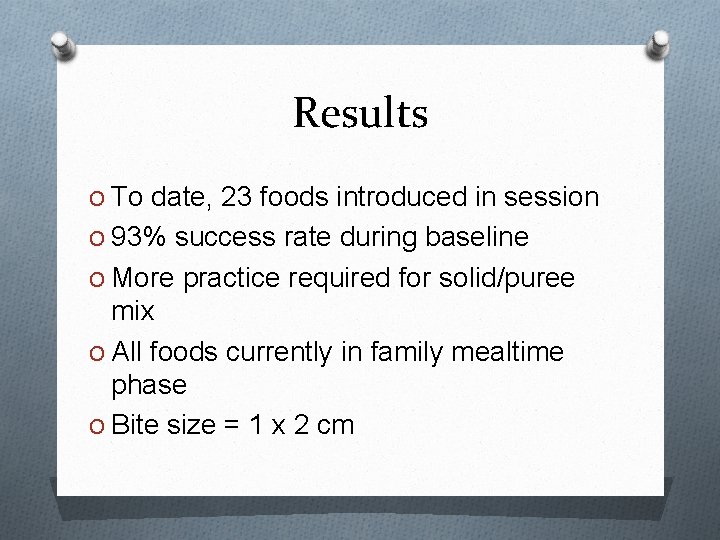
Results O To date, 23 foods introduced in session O 93% success rate during baseline O More practice required for solid/puree mix O All foods currently in family mealtime phase O Bite size = 1 x 2 cm
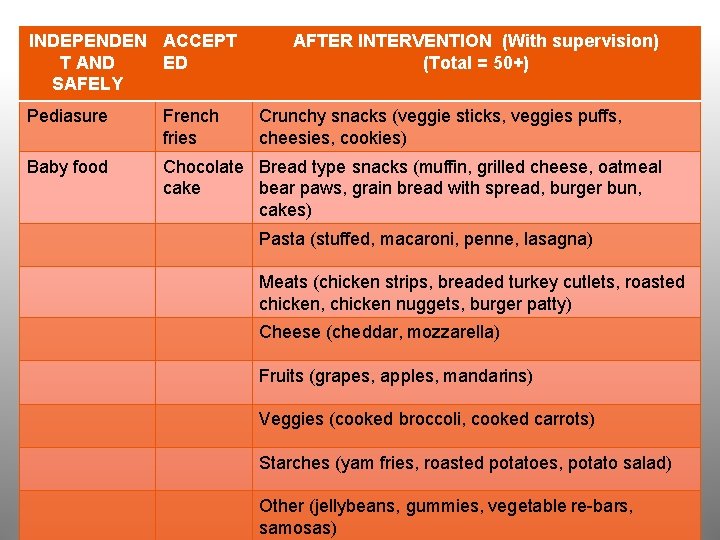
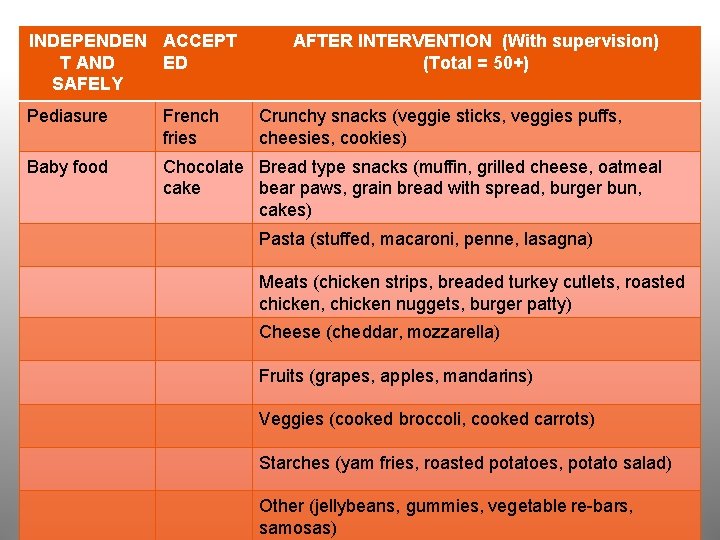
INDEPENDEN ACCEPT T AND ED SAFELY AFTER INTERVENTION (With supervision) (Total = 50+) Pediasure French fries Crunchy snacks (veggie sticks, veggies puffs, cheesies, cookies) Baby food Chocolate Bread type snacks (muffin, grilled cheese, oatmeal cake bear paws, grain bread with spread, burger bun, cakes) Pasta (stuffed, macaroni, penne, lasagna) Meats (chicken strips, breaded turkey cutlets, roasted chicken, chicken nuggets, burger patty) Cheese (cheddar, mozzarella) Fruits (grapes, apples, mandarins) Veggies (cooked broccoli, cooked carrots) Starches (yam fries, roasted potatoes, potato salad) Other (jellybeans, gummies, vegetable re-bars, samosas)
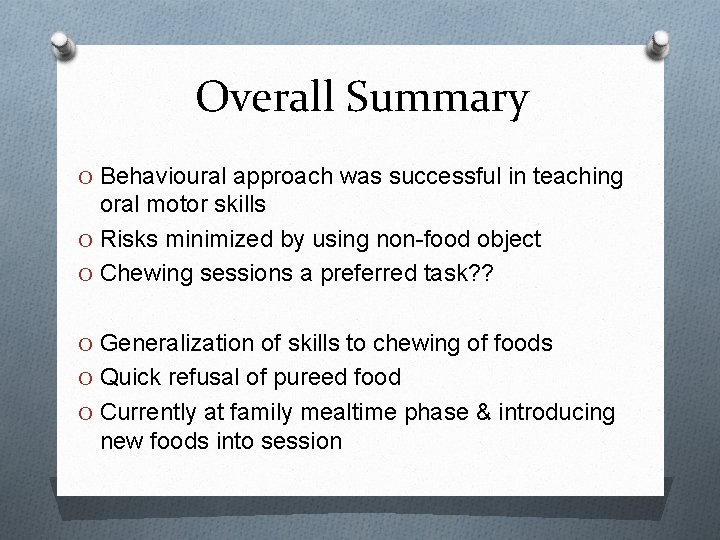
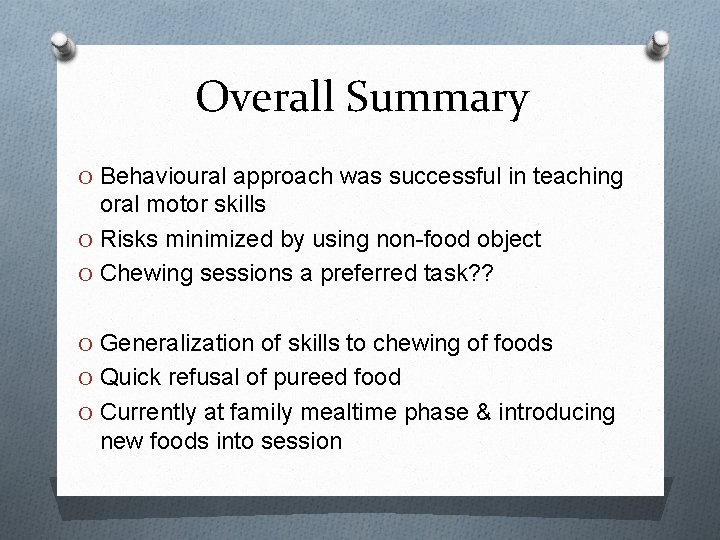
Overall Summary O Behavioural approach was successful in teaching oral motor skills O Risks minimized by using non-food object O Chewing sessions a preferred task? ? O Generalization of skills to chewing of foods O Quick refusal of pureed food O Currently at family mealtime phase & introducing new foods into session
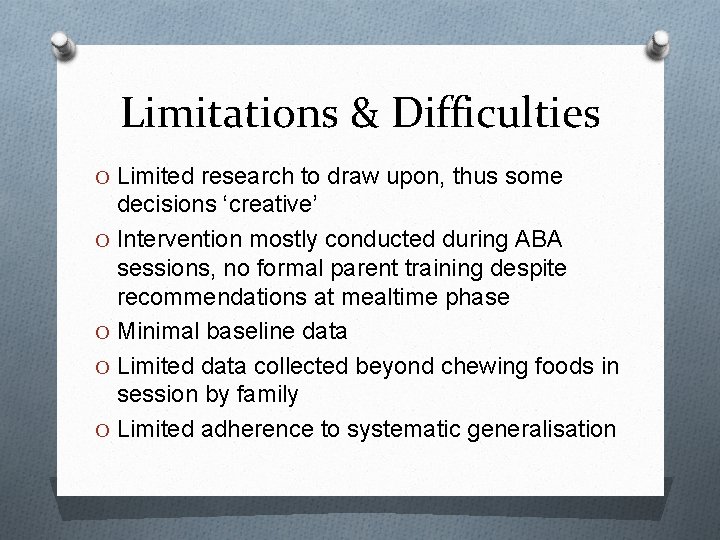
Limitations & Difficulties O Limited research to draw upon, thus some decisions ‘creative’ O Intervention mostly conducted during ABA sessions, no formal parent training despite recommendations at mealtime phase O Minimal baseline data O Limited data collected beyond chewing foods in session by family O Limited adherence to systematic generalisation
Limitations and Difficulties O Delays in progress owing to consultation/resources O Limited feeding team involvement in treatment (once/2 -3 mo. ) O Different interpretations of ‘progress’ and next steps O ‘Holding back’ without discouraging family
Future directions O Further research into feeding disorders to assess the prevalence of oral-motor difficulties O ABA research in teaching oral-motor skills O Increasing intensity of feeding team involvement to allow for more comprehensive assessment and intervention O Feeding teams to involve a BCBA where required
References Butterfield, W. H. , & Parson, R. (1973). Modeling and shaping by parents to develop chewing behaviour in their retarded child. Journal of Behavior Therapy and Experimental Psychiatry, 4, 285 -287. Eckman, N. , Williams, K. E. , Riegel, K. , & Paul, C. (2008). Teaching chewing: A structured approach. American Journal of Occupational Therapy, 62, 514 -521. Field, D. , Garland, M. , Williams, K. (2003). Correlates of specific childhood feeding problems. Journal of Pediatric Child Health, 39, 299 -304 Gisel, E. G. . (1996). Effect of oral sensorimotor treatment on measures of growth and efficiency of eating in the moderately eating-impaired child with cerebral palsy. Dysphagia, 11, 48 -58. O’Brien, S. , Repp, A. C. , Williams, G. E. & Christopherson, E. R. (1991). Pediatric feeding disorders. Behavioral Modification, 15, 394 -418. Overland, M. & Rosenfield-Johnson (1993). Normal sequence of oral motor development and eating. http: //www. keystonepediatric. com/Docs/Normal_OM. pdf Piazza, C. (2008). Feeding disorders and behavior: What have we learned? . Developmental Disabilities, 14, 174 -181