Chest physiotherapy Edinburgh 23 November 2019 The morning

Chest physiotherapy Edinburgh 23 November 2019

The morning after the night before
What is chest physiotherapy l l l Physiotherapists , mucous clearance from breathing passages of patients (wikipedia) A physical technique to remove musous from healthy passages( healthyhearty) ( AAAGGGRRRR my daughter 2019) ATS and BTS none Speciality that assess, treats and maintains optimum human lung function
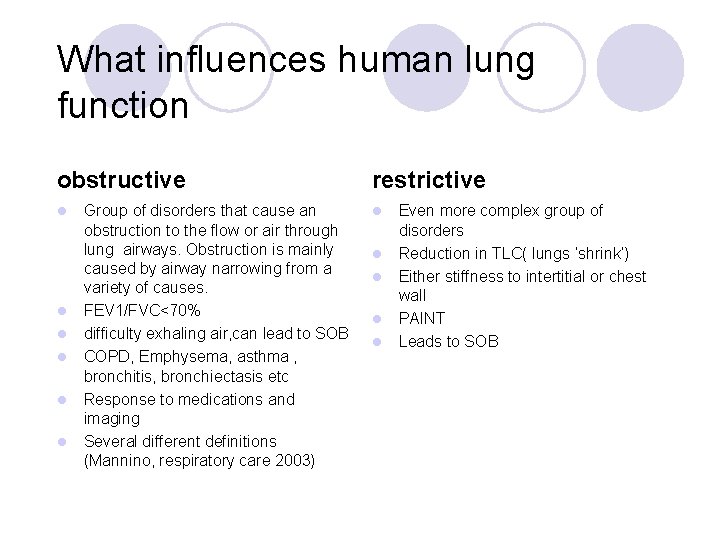
What influences human lung function obstructive l l l Group of disorders that cause an obstruction to the flow or air through lung airways. Obstruction is mainly caused by airway narrowing from a variety of causes. FEV 1/FVC<70% difficulty exhaling air, can lead to SOB COPD, Emphysema, asthma , bronchitis, bronchiectasis etc Response to medications and imaging Several different definitions (Mannino, respiratory care 2003) restrictive l l l Even more complex group of disorders Reduction in TLC( lungs ‘shrink’) Either stiffness to intertitial or chest wall PAINT Leads to SOB
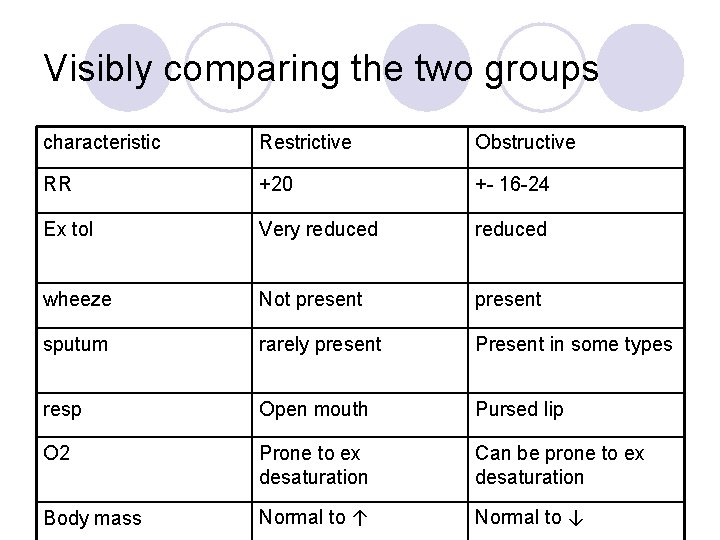
Visibly comparing the two groups characteristic Restrictive Obstructive RR +20 +- 16 -24 Ex tol Very reduced wheeze Not present sputum rarely present Present in some types resp Open mouth Pursed lip O 2 Prone to ex desaturation Can be prone to ex desaturation Body mass Normal to ↑ Normal to ↓

Obstructive vs Restrictive flow loops obstructive restrictive
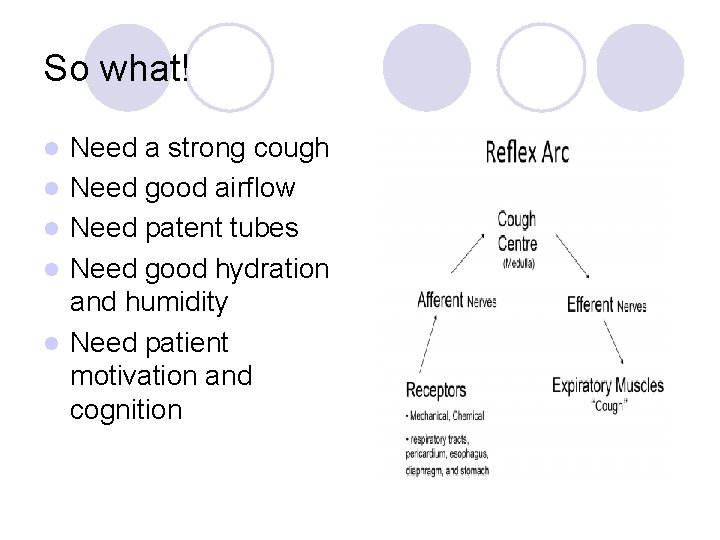
So what! l l l Need a strong cough Need good airflow Need patent tubes Need good hydration and humidity Need patient motivation and cognition
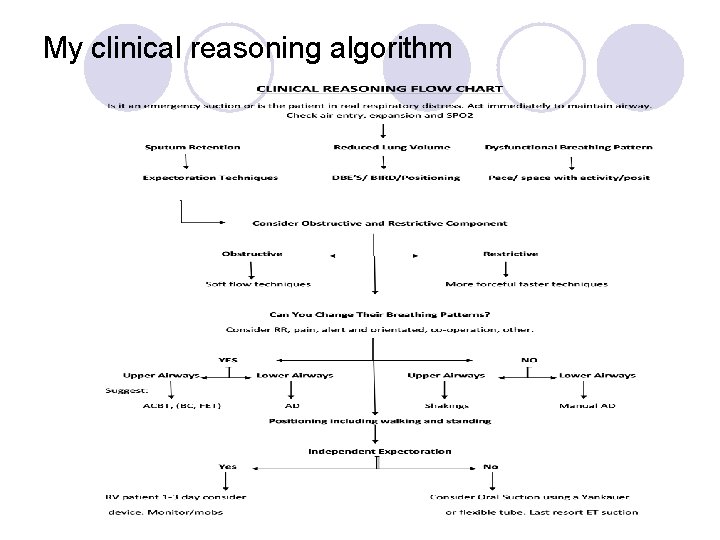
My clinical reasoning algorithm
Non intubated techniques
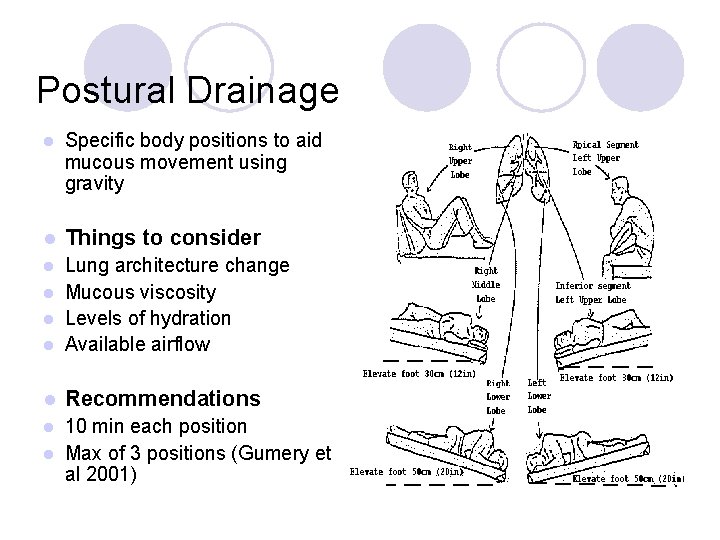
Postural Drainage l Specific body positions to aid mucous movement using gravity l Things to consider Lung architecture change l Mucous viscosity l Levels of hydration l Available airflow l l Recommendations 10 min each position l Max of 3 positions (Gumery et al 2001) l
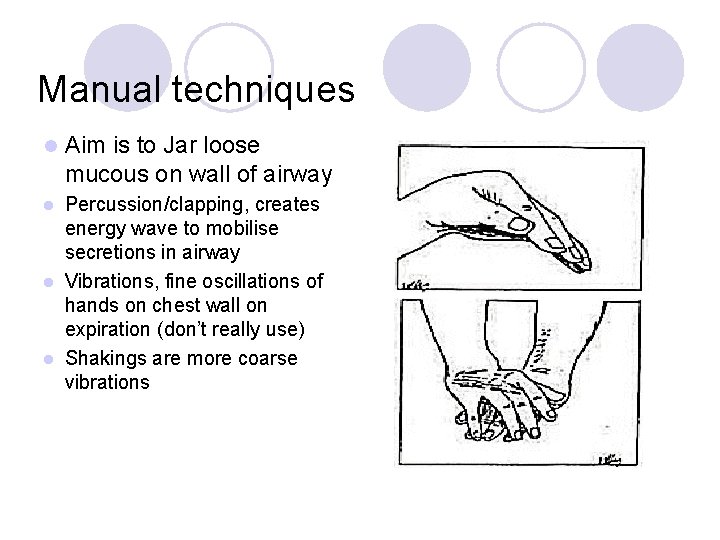
Manual techniques l Aim is to Jar loose mucous on wall of airway Percussion/clapping, creates energy wave to mobilise secretions in airway l Vibrations, fine oscillations of hands on chest wall on expiration (don’t really use) l Shakings are more coarse vibrations l
Evidence PD+FET vs PD+ FET +Percussion( fast and slow)( Gallon, A, 1991): 9 stable bronchiectatics studied over three weeks with three regimes: Results no adverse effects but no change in LFT. Fast slow percussion when producing more sputum than PD+FET alone. l AD vs Percussion(Giles et al, 1995): AD may be better tolerated by patients with CF, less likely to produce O 2 desaturation, produces similar benefits in sputum clearance. l Cochrane review 2000 (Jones and Rowe): 7 trials included, 126 patients with COPD and bronchiectasis, Results= no change in LFT but helps clear mucous, Conclusion not enough evidence to refute/support. PD +percussion. l Percussion in acute COPD(Mc. Crory et al 2001) Chest percussion is ineffective in improving symptoms or lung function and causes transient reduction in SP 02. l
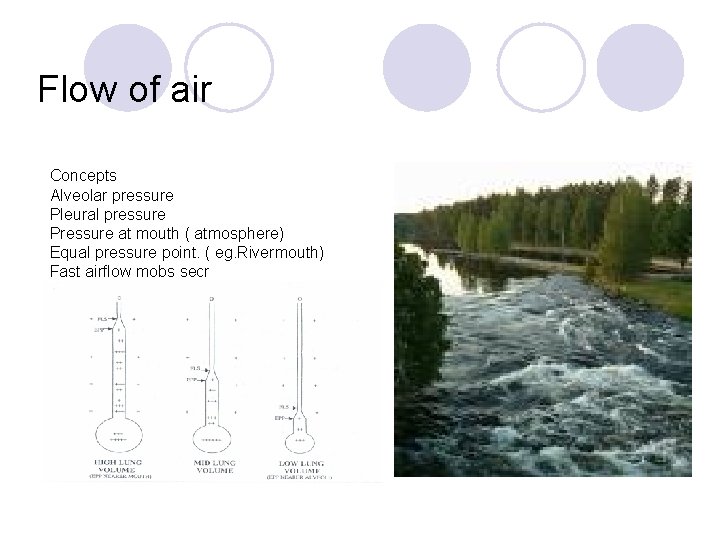
Flow of air Concepts Alveolar pressure Pleural pressure Pressure at mouth ( atmosphere) Equal pressure point. ( eg. Rivermouth) Fast airflow mobs secr
ACBT l l l Thought to work better on larger airways but may aid movement of mucous from smaller airways. Any position Relaxed abdominal breathing ( relaxes airways) Deep inspirations ( collateral ventilation, opens airways, air behind secr) Relaxed abdominal breathing ( relaxes airways) 1 -2 huffs at low lung volume ( mobilises secr) Cont Points to consider Work progressively from lower lung vol-more upper lung vol Don’t use deep quick breaths in (secr back) or out ( bronchoconstriction) Don’t cough too soon ( accessibility) Work secr at EPP
AD l l l Creating high airflow at appropriate airway ( where there are secr) Thought to drain secr from small airways to large Good technique for chronic hypersecretory disease Any position Practice open glottal breathing Deep slow inspiration hold 1 -4 sec ( collateral ventilation, opens airways, air behind secr) Expirations down to level where you hear secr move Keep tidal volumes at level that you hear secr move Follow secretions with tidal volumes ( progressively fill lungs up as secr move proximally) Don’t cough too soon, cough suppression ( accessibility) swallow Phases, unstick ( crackles) , collect( crackles at different vol) , evacuate ( cough)
Flow or air cont l Hough (2002) AD and ACBT are based on the same principle and physiotherapists are advised to develop own technique based on both!!!!! l Adapt to pt understanding l Adapt to fatigue l Adapt to expiratory effort and cough l Adapt to wheeze
Evidence ACBT vs AD(Savci et al, 2000): long term effects comparison in stable COPD in RCT, n=30; FVC and PEFR, exercise performance, O 2 Sat improved AD>ACBT, AD as effective as ACBT for mucous clearance. l ACBT vs AD (Miller et al, 1995): randomised crossover trial; n=18; ACBT> AD improved FVC, AD>ACBT improved FEF 25 -75%, AD clears lung faster, no real clinical differences l ACBT vs AD (MOIZ, J. A. et al 2006): n= 30 Acute COPD admissions, AD=ACBT in sputum removal, both ± SPO 2, don’t affect RR and HR adversely, PEFR no diffrences between groups. l
Breathing control Dyspnoea centrally sensory perceived increased mechanical work of breathing. l Principle of breathing control is to work below threshold of sensory WOB. l Spacing: Plan, prioritise, organise events or chores l Pacing: slower mvt so that breathing is rhythmical( observe change in resp pattern) l Fans and open window draft do help with sensation of dyspnoea l
Recovery/ breathing control l l l Difficult to restore established pattern or +++ breathlessness Aim to reduce WOB and make activity more efficient for breathing Aim to work at submaximal relaxed level anxiety Use positioning (forward lean) Acc muscle use, neck exstensors, Zone of apposition, quiet breathing (O’Neil, Mc. Carthy, 1983) Standing and sitting erect positions causes ↑ rib and acc m and ↓ diaphragm use , paradoxical breathing patterns , ↑dyspnoea vs forward lean which has greater TLC, FRC and RV ( Sharp et al, 1980)
Take home nuggets l Clearance techniques: 2 -4 deep breaths in with slight holds. l About 4 -10 Open gottal breaths ( steam up mirror) or 10 bubble PEP l Cough l l Breathing control l At rest forward lean and support head on shoulders. Avoid ‘relax’ and reinforce whatever pattern feels easiest and avoid DEEP breaths and holds l During gait: 4 steps is the threshhold for changes in breathing. Regime could be 4 steps, stop recover then another 4 steps etc
Any questions
- Slides: 21