Chemical Pathology Slido 35050 www slido com Matthew





- Slides: 59

Chemical Pathology Slido 35050 www. slido. com Matthew Machin mm 5512@ic. ac. uk
Overview • • Acid base Calcium LFTs Diabetes

Go forward in time… Dr L #HELP ege nd
Clinical Scenario 1 It’s 01: 00, you are on-call F 1 for general surgery. You are called by the nursing staff regarding a 62 -year-old gentlemen that has poor urine output and looks generally unwell. On further questioning, you elicit that he was admitted with a high out-output stoma 2 days prior. His observations score a 2 on the NEWS score. RR: 19, Sa 02: 96% RA, HR 97, BP 118/56, T: 36. 0, alert and orientated. He hasn’t produced any urine since 22: 00. He has a catheter in situ. What do you do next? a) Politely request the nursing staff give a bag of fluids and return to you ever lengthening jobs list b) Attend the patient and undertake a full clinical assessment c) Ask the nursing staff to undertaken hourly urine output and call you in 2 hours d) Call the on-call nephrologist for advice e) Order a CT KUB and review the results of the scan
Clinical Scenario 1 You attend and perform a full clinical assessment. The patient appears tachypneic and unsettled. His pulse is regular and slow at 50. He is warm centrally but peripherally cool. Chest clear. Abdo SNT. The stoma output has been 5 litres / 24 hours. UO: nil since 22: 00. What do you do next? a) Flush the catheter and ask them to call you back in a couple of hours if no luck b) Undertake a full set of bloods, blood gas sampling, ECG, and CXR and await results prior to commencing IV fluids c) Undertake a full set of bloods, blood gas sampling, ECG, and CXR commence IV fluids d) Commence IV fluids and see if the urine output picks up in 2 hours e) Undertake an ECG, and commence IV fluids
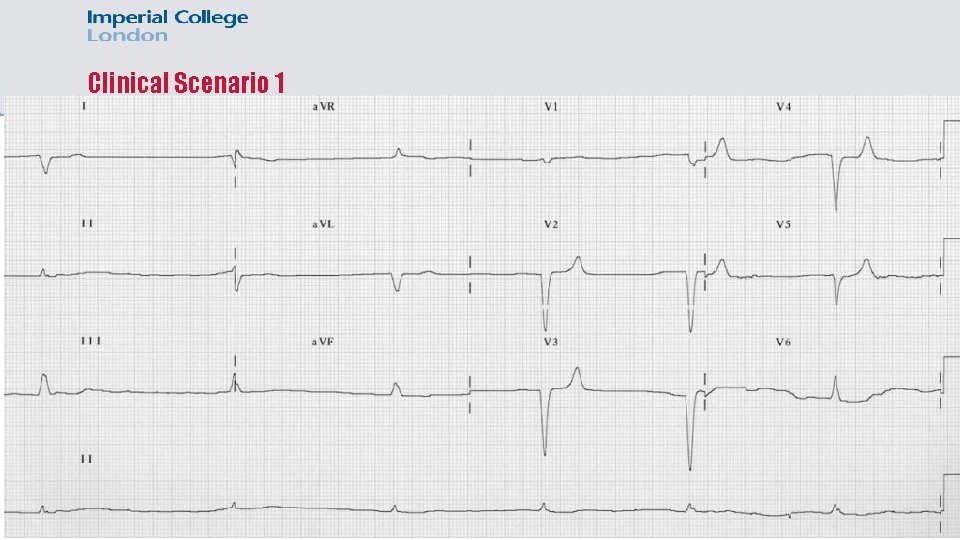
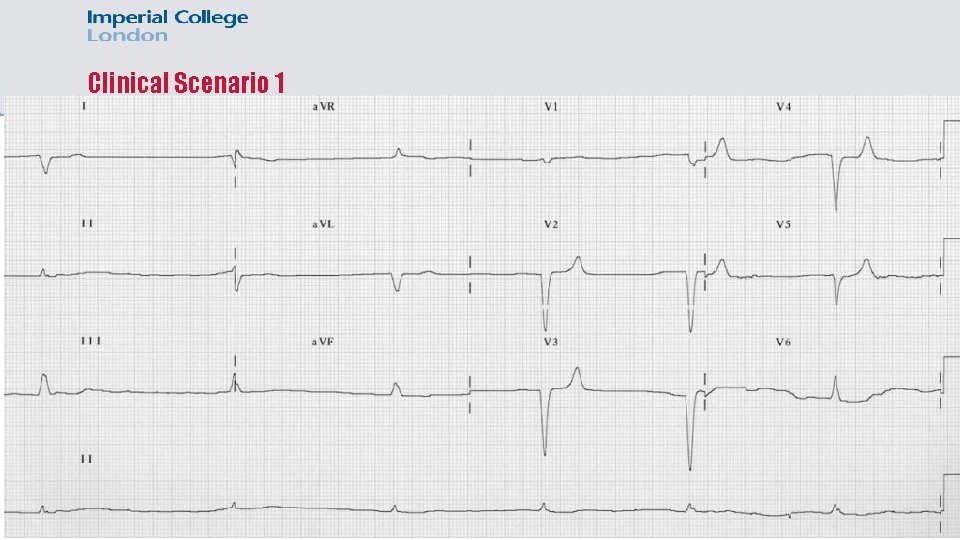
Clinical Scenario 1
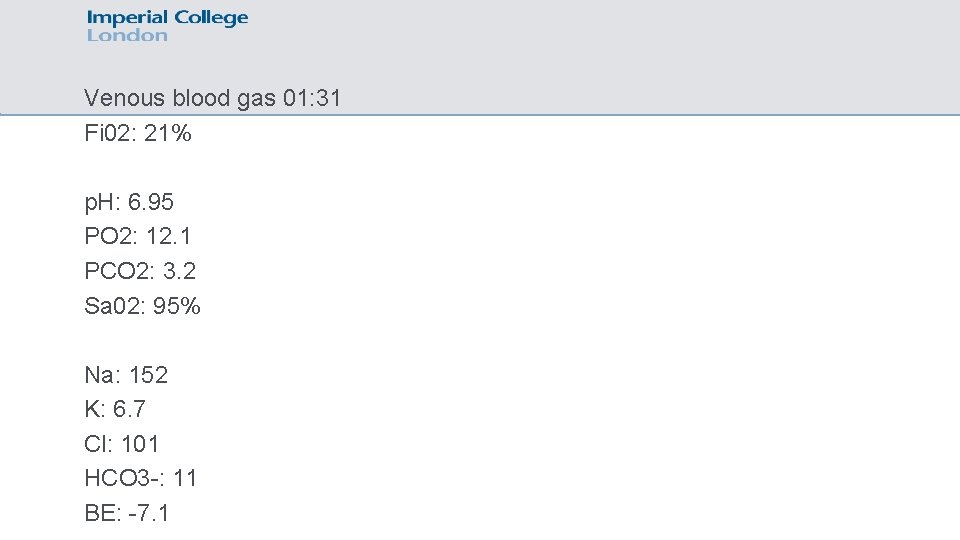
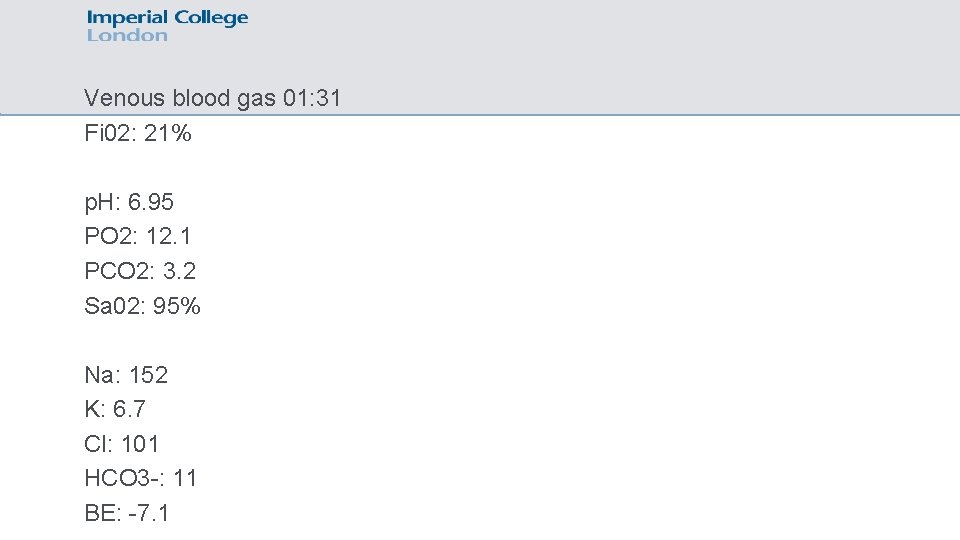
Venous blood gas 01: 31 Fi 02: 21% p. H: 6. 95 PO 2: 12. 1 PCO 2: 3. 2 Sa 02: 95% Na: 152 K: 6. 7 Cl: 101 HCO 3 -: 11 BE: -7. 1

Clinical Scenario 1 What do you think is going on? a) b) c) d) Sepsis from intra-abdominal collection leading to acidosis and hyperkalaemia Obstructive nephropathy with sepsis leading to acidosis and hyperkalaemia Dehydration from high out-put stoma, leading to acute renal failure Undiagnosed cardiac event leading to pump failure and subsequent renal failure
Clinical Scenario 1 What do you do next? a) Put out a medical emergency call b) Give calcium gluconate, IV actrapid and glucose, nebulized salbutamol, IV fluids and escalate to ITU on-call reg c) Give IV fluid bolus and see how the respond d) Phone the on-call nephrologist for advice e) Repeat ECG and venous gas
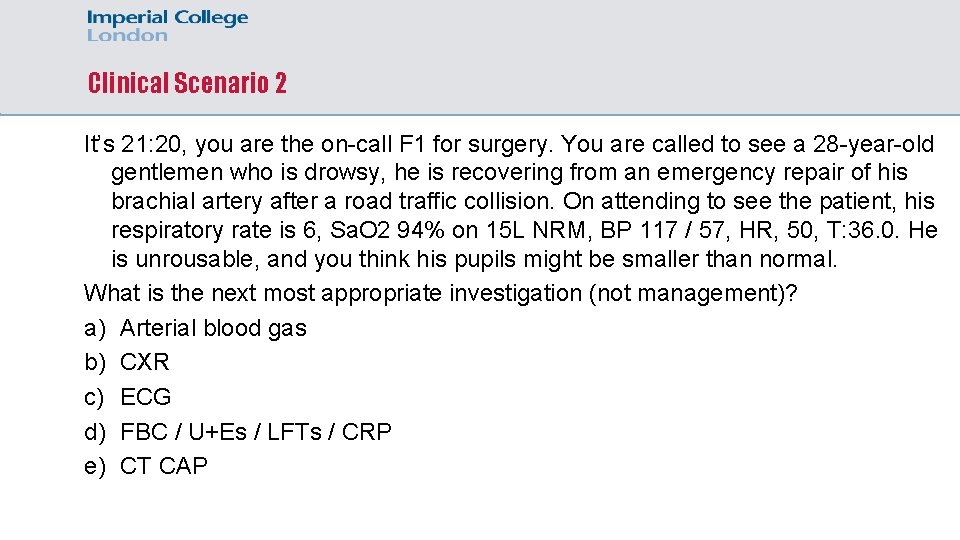
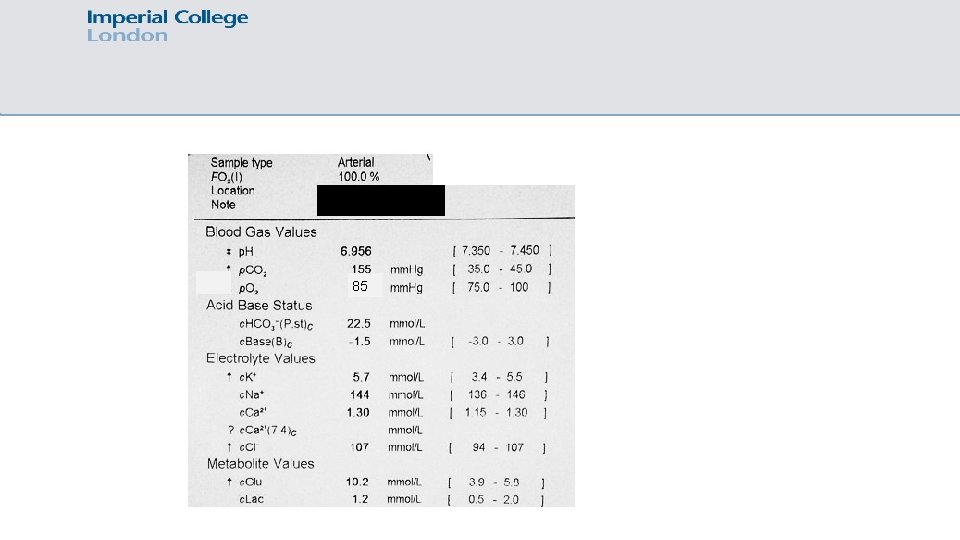
Clinical Scenario 2 It’s 21: 20, you are the on-call F 1 for surgery. You are called to see a 28 -year-old gentlemen who is drowsy, he is recovering from an emergency repair of his brachial artery after a road traffic collision. On attending to see the patient, his respiratory rate is 6, Sa. O 2 94% on 15 L NRM, BP 117 / 57, HR, 50, T: 36. 0. He is unrousable, and you think his pupils might be smaller than normal. What is the next most appropriate investigation (not management)? a) Arterial blood gas b) CXR c) ECG d) FBC / U+Es / LFTs / CRP e) CT CAP
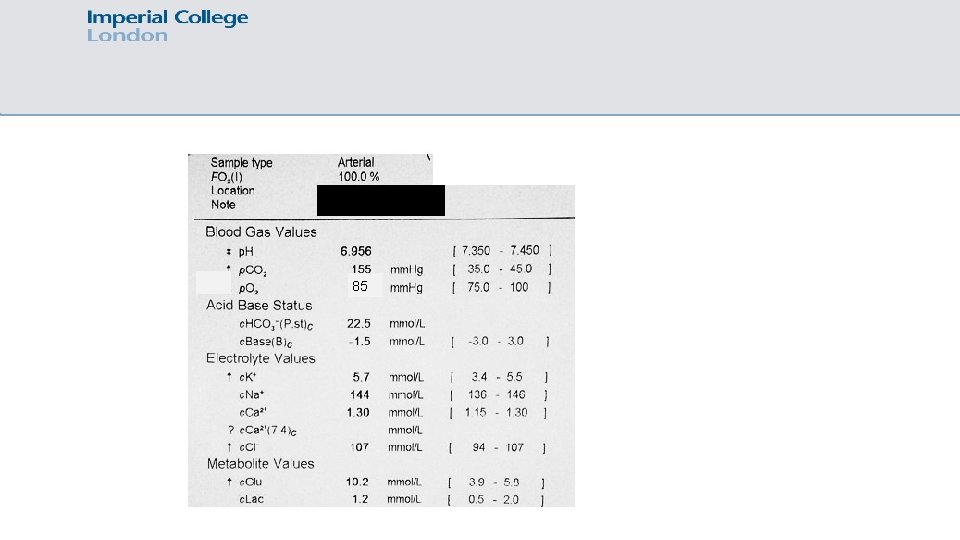
85

Clinical scenario 2 It’s 21: 20, you are the on-call F 1 for surgery. You are called to see a 28 -year-old gentlemen who is drowsy, he is recovering from an emergency repair of his brachial artery after a road traffic collision. On attending to see the patient, his respiratory rate is 6, Sa. O 2 94% on 15 L NRM, BP 117 / 57, HR, 50, T: 36. 0. He is unrousable, and you think his pupils might be smaller than normal. What is the next most appropriate management? a) CPAP b) Intubation and ventilation c) Naloxone d) Nebulised salbutamol e) Optiflow
Clinical Scenario 3 At handover, the day team handover a repeat blood gas on a patient with know CCF on a furosemide infusion to check the potassium. You are the on-call medical F 1 overnight. It’s now 22: 30 and you undertake the blood gas and get the following results. p. H: 7. 54, PO 2: 4. 5 PCO 2: 5. 1, Sa. O 2: 67%, Na: 131, K 3. 4, Cl-: 96, HCO 3 -: 31 What do you do next? a) Review the patient, look at their observations, check their UO, and review the drug chart b) Carry on, everything seems to be OK c) Prescribe a bag of 40 mmol KCL over 10 hours and leave d) Prescribe maintenance fluids and leave e) Repeat the blood gas
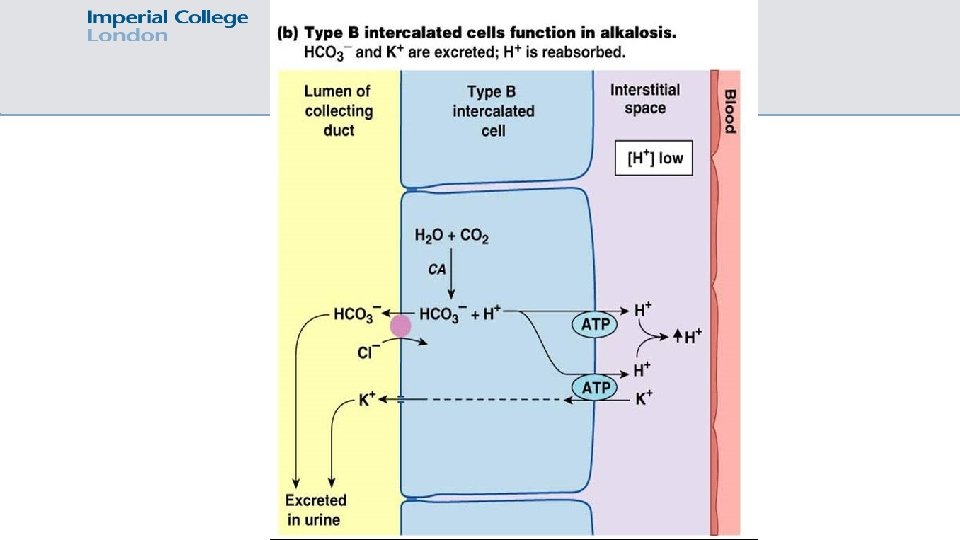
Clinical Scenario 3 You attend and perform a full clinical assessment. The patient appears comfortable at rest, warm and well perfused, with a regular pulse. They are oedematous, with pitting oedema up to the mid calf. They have occasional crackles at their bases. Their UO is 120 ml / hour. They are prescribed oral Sando K, and 240 mg Furosemide / 24 hours. p. H: 7. 54, PO 2: 4. 5 PCO 2: 5. 1, Sa. O 2: 67%, Na: 131, K 3. 4, Cl-: 96, HCO 3 -: 31 What do you do think is the cause of the abnormality seen on the blood gas? a) Pulmonary embolism b) Post obstructive polyuria c) Fluid overload secondary to CCF d) Diuretics e) Sando K
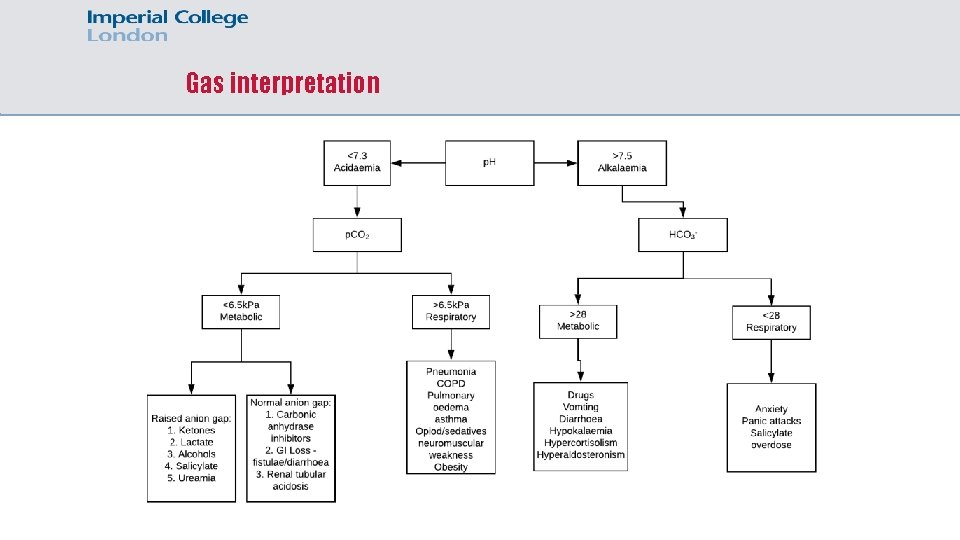
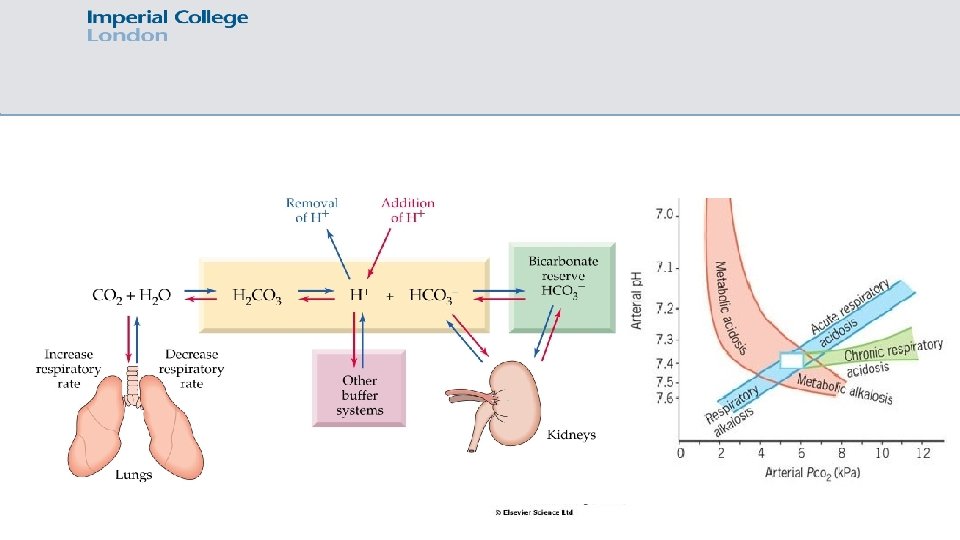
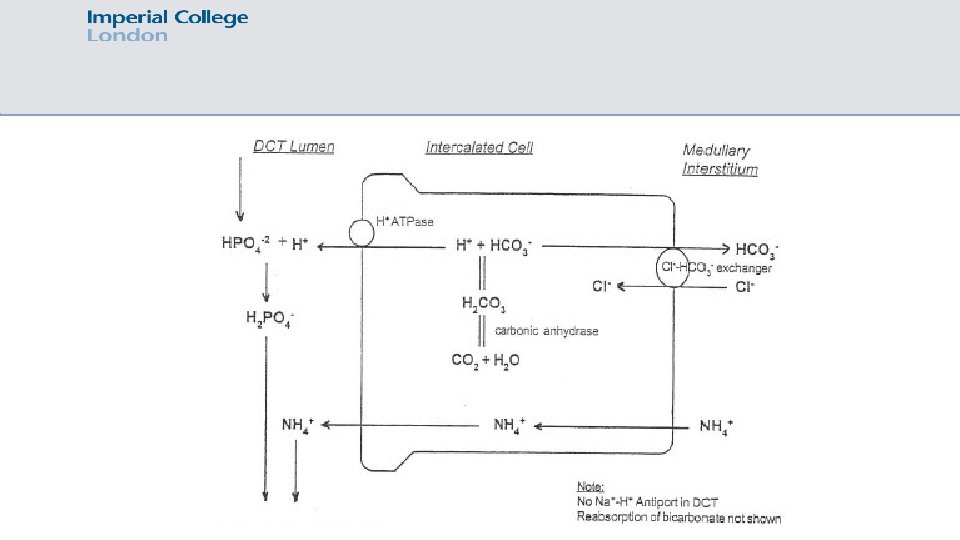
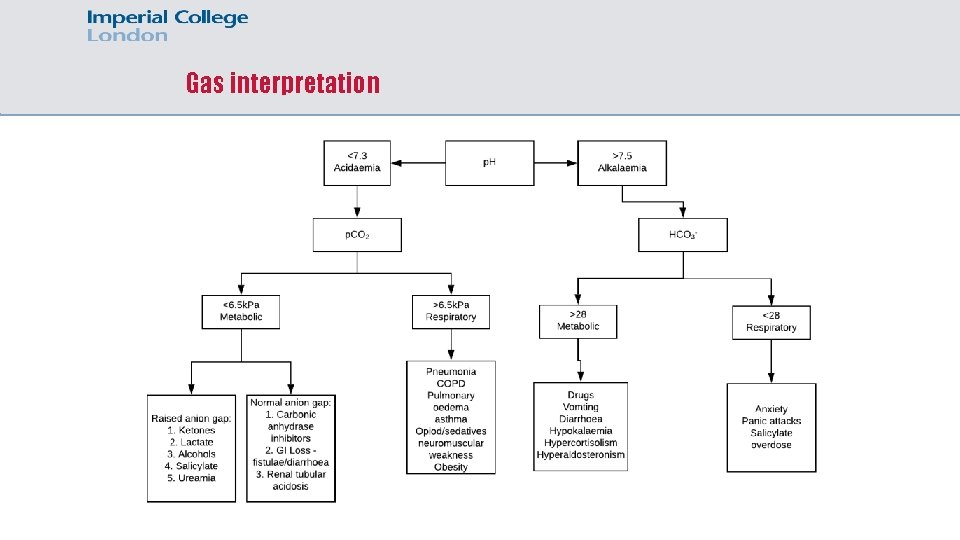
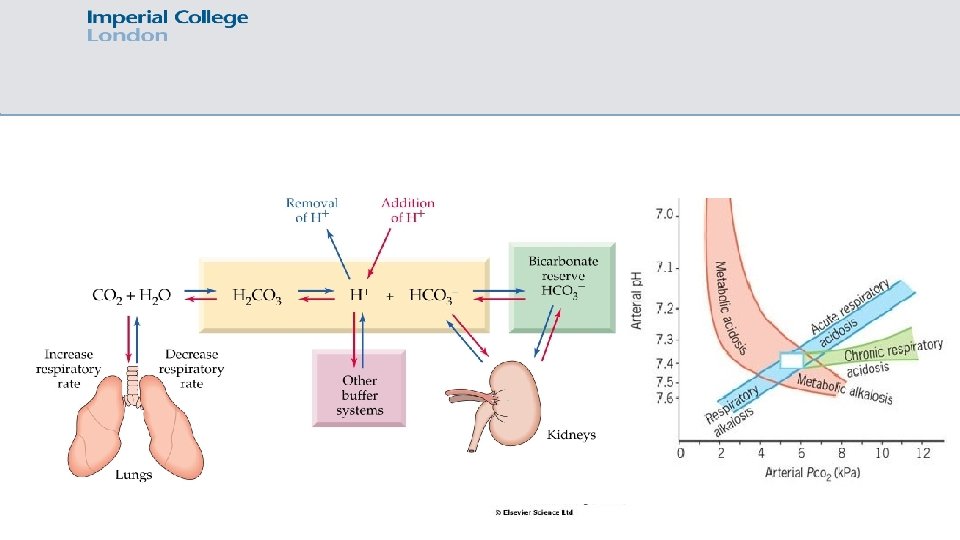
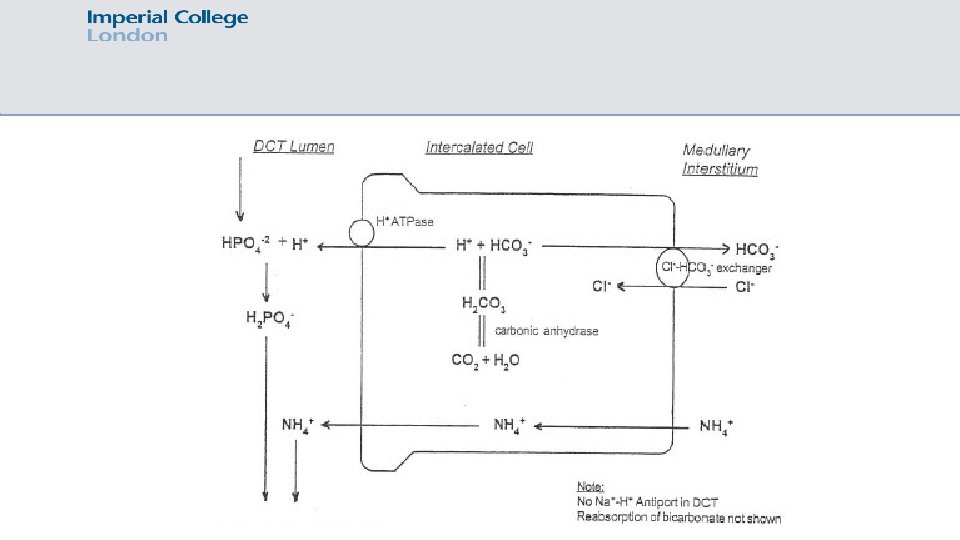
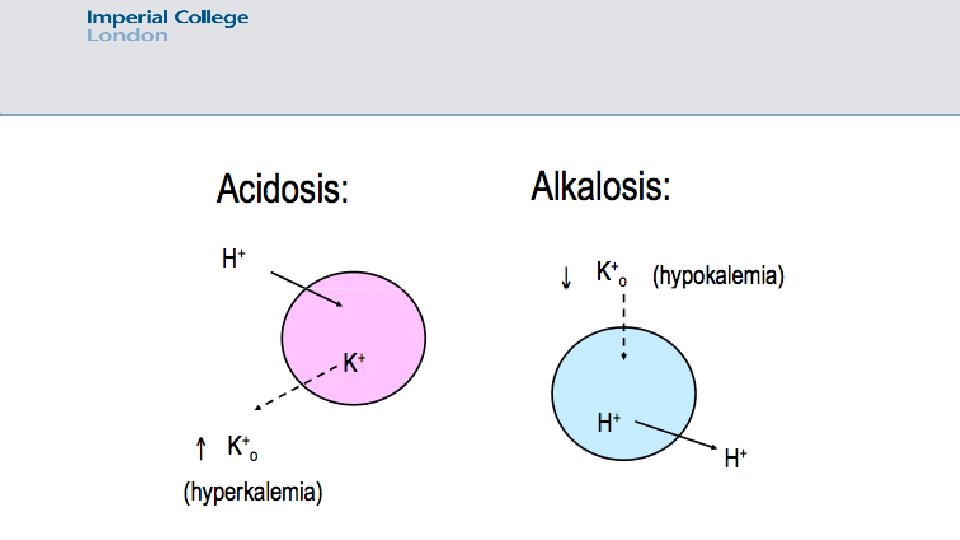
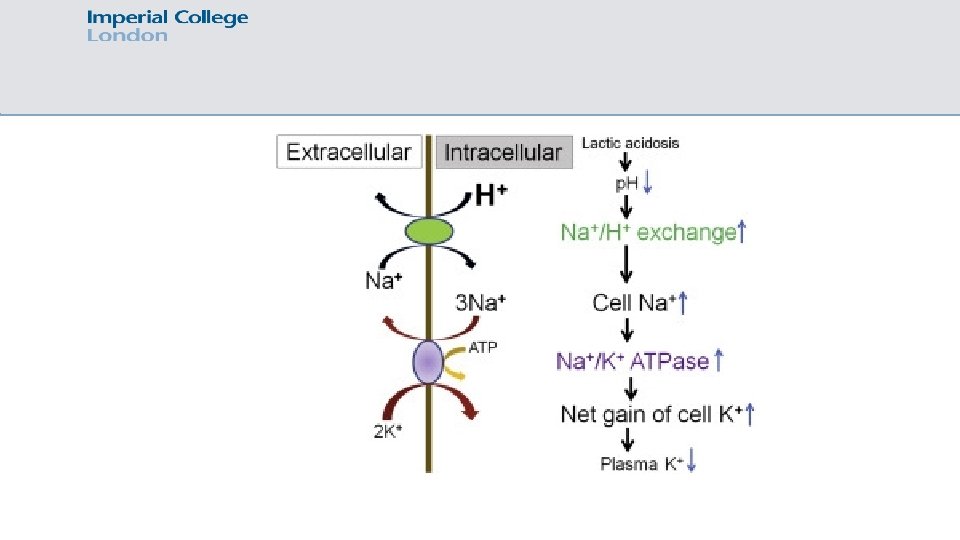
Gas interpretation
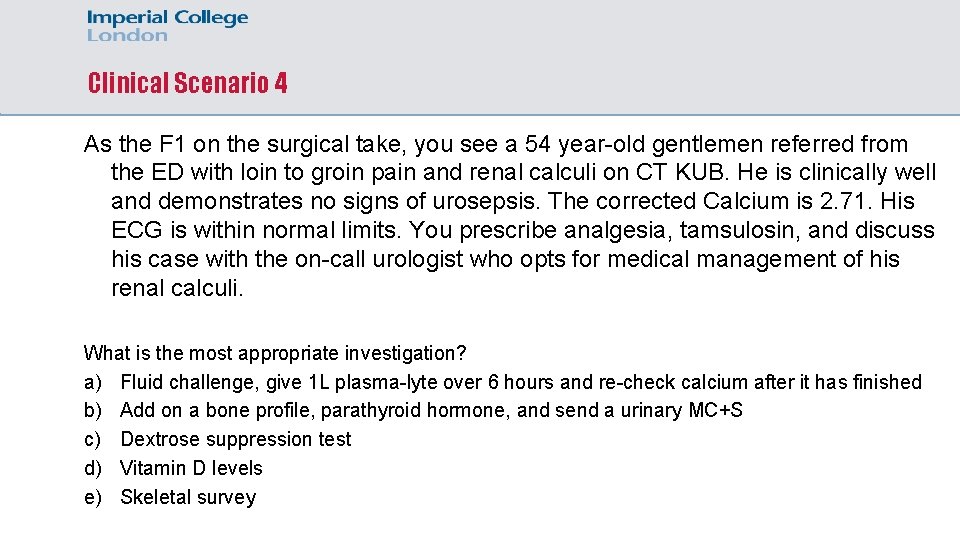
Clinical Scenario 4 As the F 1 on the surgical take, you see a 54 year-old gentlemen referred from the ED with loin to groin pain and renal calculi on CT KUB. He is clinically well and demonstrates no signs of urosepsis. The corrected Calcium is 2. 71. His ECG is within normal limits. You prescribe analgesia, tamsulosin, and discuss his case with the on-call urologist who opts for medical management of his renal calculi. What is the most appropriate investigation? a) Fluid challenge, give 1 L plasma-lyte over 6 hours and re-check calcium after it has finished b) Add on a bone profile, parathyroid hormone, and send a urinary MC+S c) Dextrose suppression test d) Vitamin D levels e) Skeletal survey
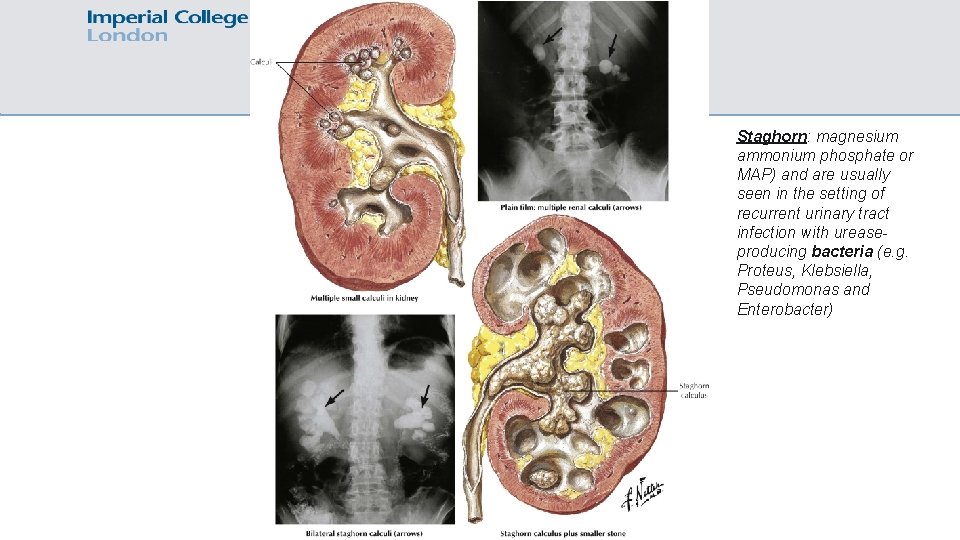
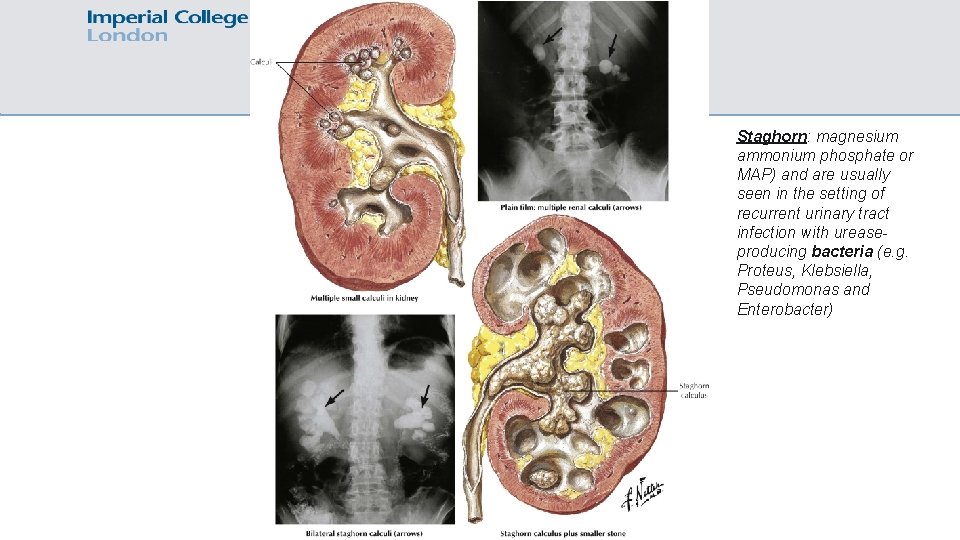
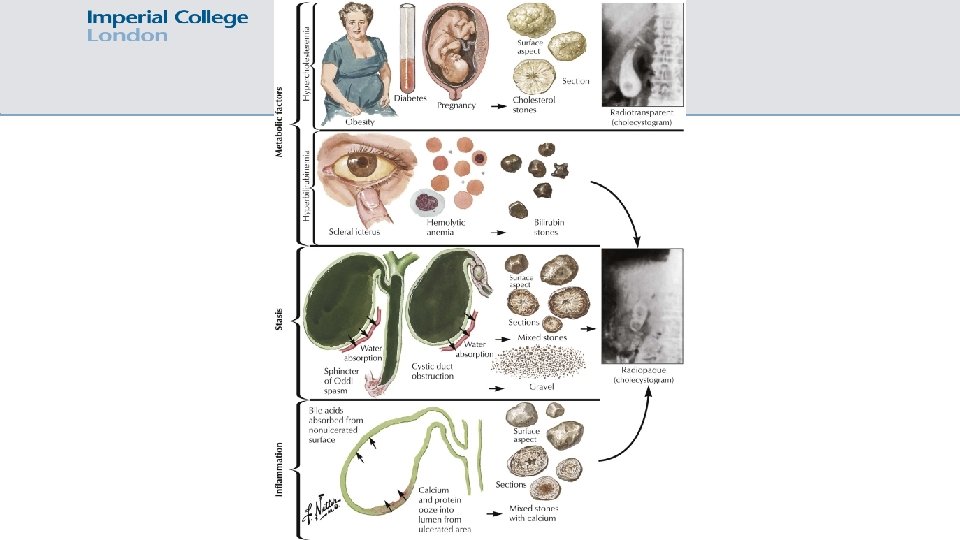
Staghorn: magnesium ammonium phosphate or MAP) and are usually seen in the setting of recurrent urinary tract infection with ureaseproducing bacteria (e. g. Proteus, Klebsiella, Pseudomonas and Enterobacter)
Clinical Scenario 4 The parathyroid hormone level comes back as 43 pg/ml (normal). His vitamin D is also normal. What is the most likely diagnosis? a) Primary hyperparathyroidism b) Secondary hyperparathyroidism c) Tertiary hyperparathyroidism d) Malignancy of unknown primary e) Sarcoidosis
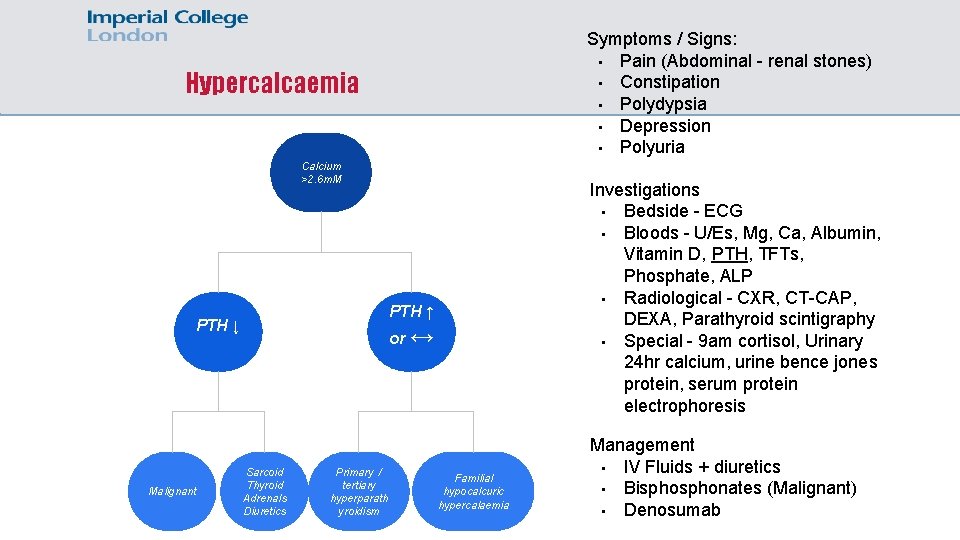
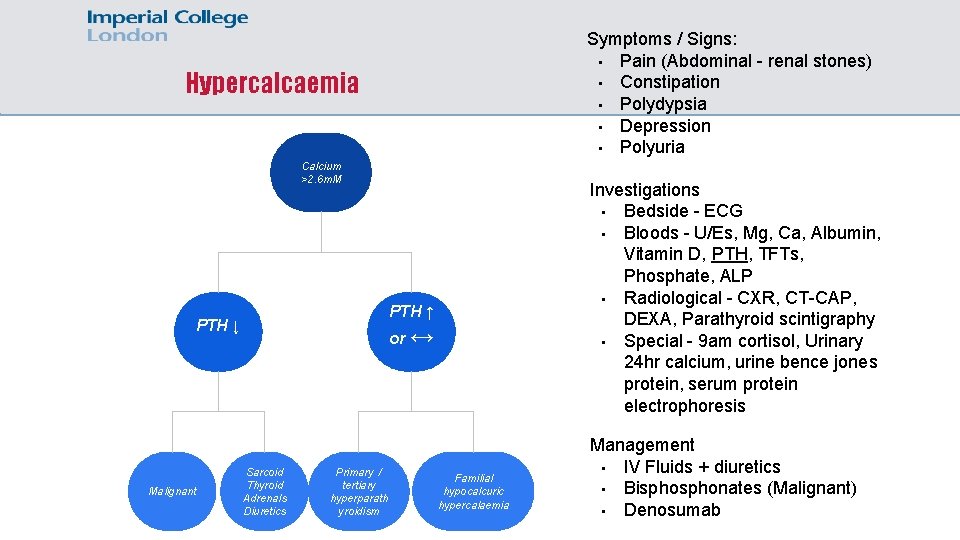
Symptoms / Signs: • Pain (Abdominal - renal stones) • Constipation • Polydypsia • Depression • Polyuria Hypercalcaemia Calcium >2. 6 m. M PTH ↑ PTH ↓ Malignant Investigations • Bedside - ECG • Bloods - U/Es, Mg, Ca, Albumin, Vitamin D, PTH, TFTs, Phosphate, ALP • Radiological - CXR, CT-CAP, DEXA, Parathyroid scintigraphy • Special - 9 am cortisol, Urinary 24 hr calcium, urine bence jones protein, serum protein electrophoresis or ↔ Sarcoid Thyroid Adrenals Diuretics Primary / tertiary hyperparath yroidism Familial hypocalcuric hypercalaemia Management • IV Fluids + diuretics • Bisphonates (Malignant) • Denosumab
Clinical Scenario 5 You are the F 1 working the standard day on a medical ward. Whilst checking the blood results from the inpatients, you see that a patient has a corrected calcium of 1. 91. The patient has known chronic kidney disease secondary to type II diabetes with an e. GFR of 60. What is the next most appropriate investigation? a) b) c) d) e) 1 alpha hydroxlase levels Alkaline phosphatase Urinary calcium Vitamin D Repeat calcium
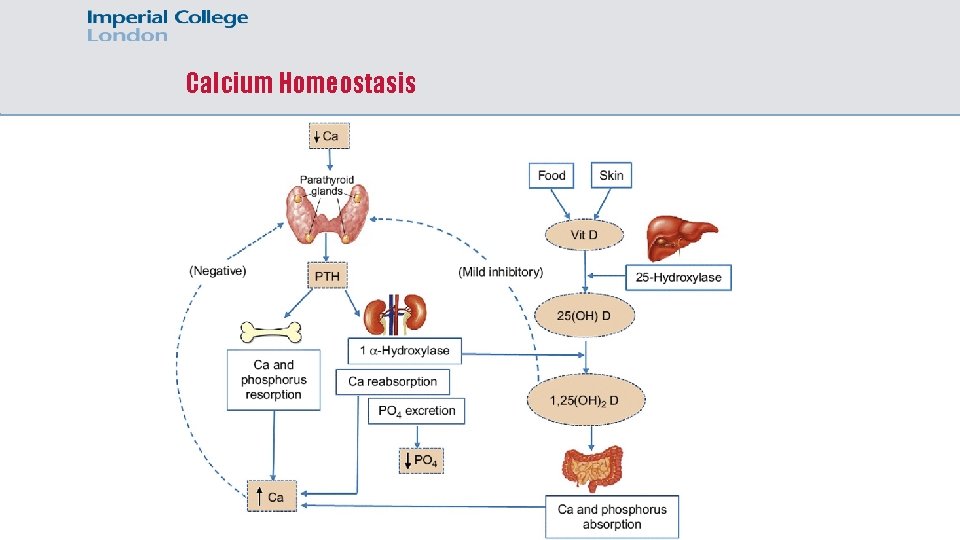
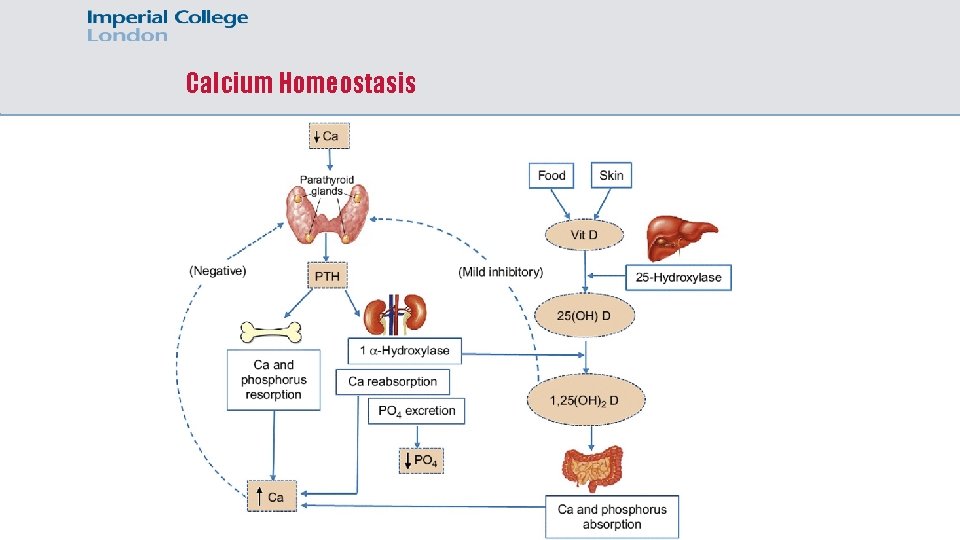
Calcium Homeostasis
Clinical Scenario 5 You are the F 1 working the standard day on a medical ward. Whilst checking the blood results from the inpatients, you see that a patient has a corrected calcium of 1. 91. The patient has known chronic kidney disease secondary to type II diabetes with an e. GFR of 60. What is the next most appropriate management? a) b) c) d) e) Oral calcium and vitamin D supplementation IM calcium depot Repeat calcium, it will be transiently low in illness IV calcium gluconate 10 ml 10% STAT IV calcium gluconate 100 ml 10% diluted in 1 litre over 24 hours
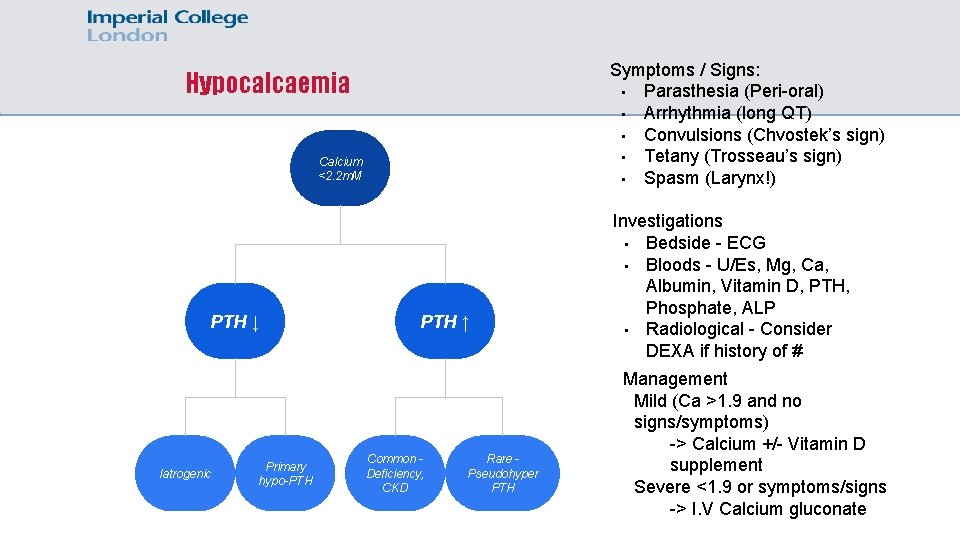
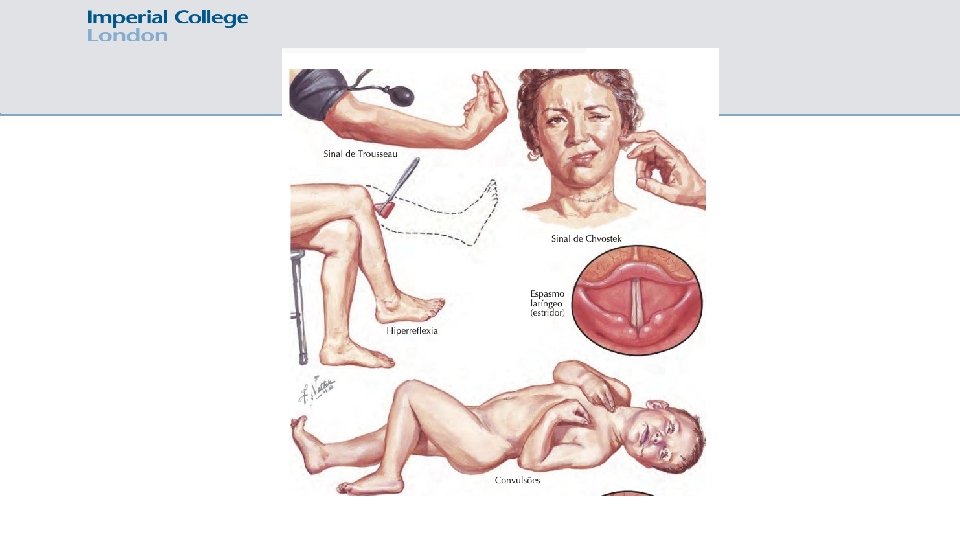
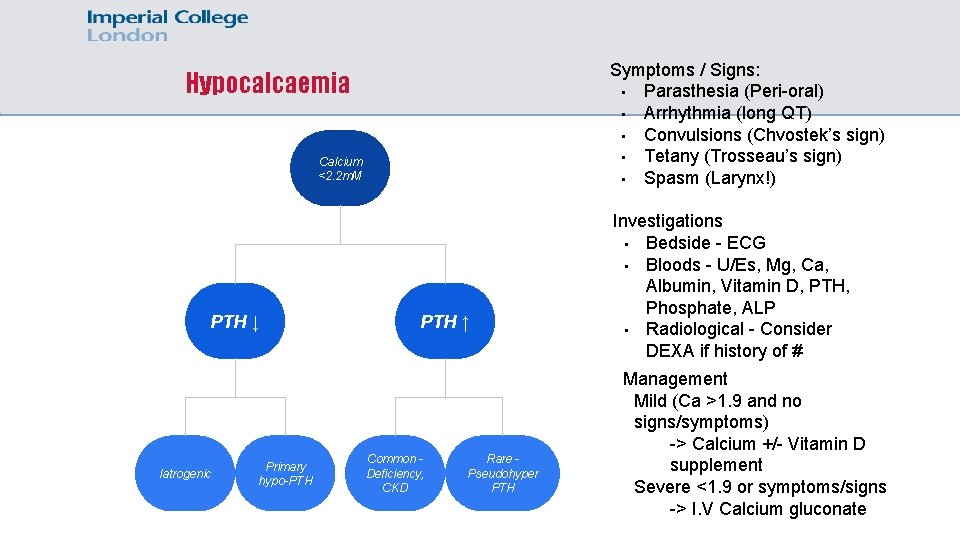
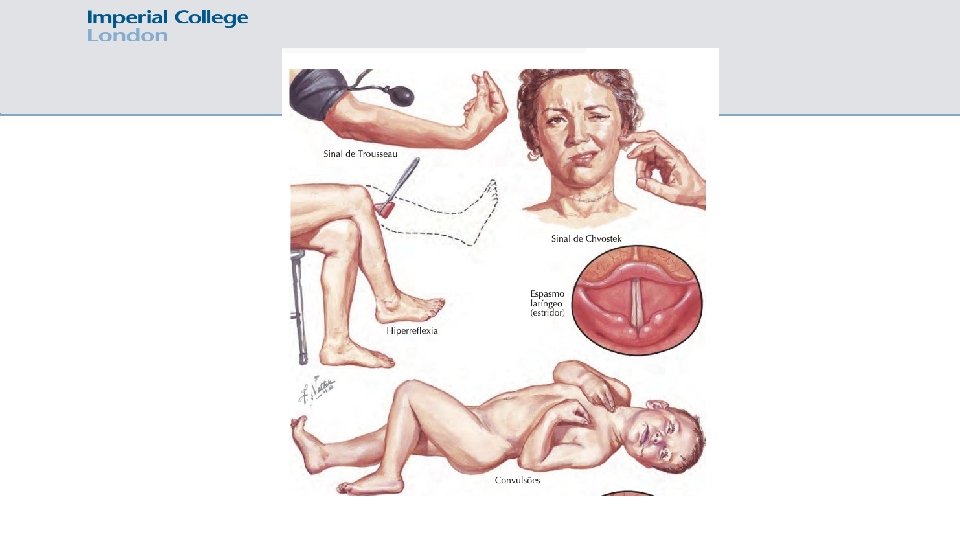
Symptoms / Signs: • Parasthesia (Peri-oral) • Arrhythmia (long QT) • Convulsions (Chvostek’s sign) • Tetany (Trosseau’s sign) • Spasm (Larynx!) Hypocalcaemia Calcium <2. 2 m. M PTH ↓ Iatrogenic Primary hypo-PTH ↑ Common Deficiency, CKD Rare Pseudohyper PTH Investigations • Bedside - ECG • Bloods - U/Es, Mg, Ca, Albumin, Vitamin D, PTH, Phosphate, ALP • Radiological - Consider DEXA if history of # Management Mild (Ca >1. 9 and no signs/symptoms) -> Calcium +/- Vitamin D supplement Severe <1. 9 or symptoms/signs -> I. V Calcium gluconate
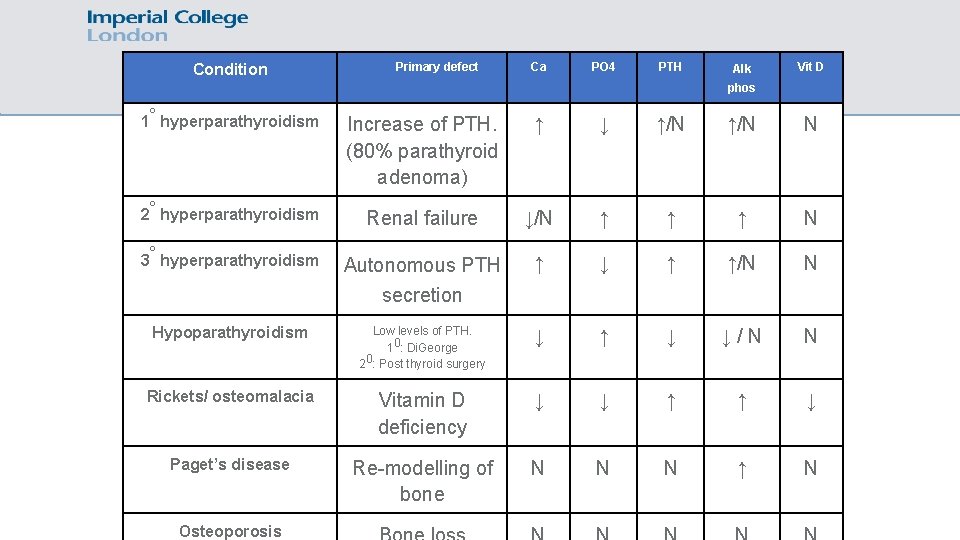
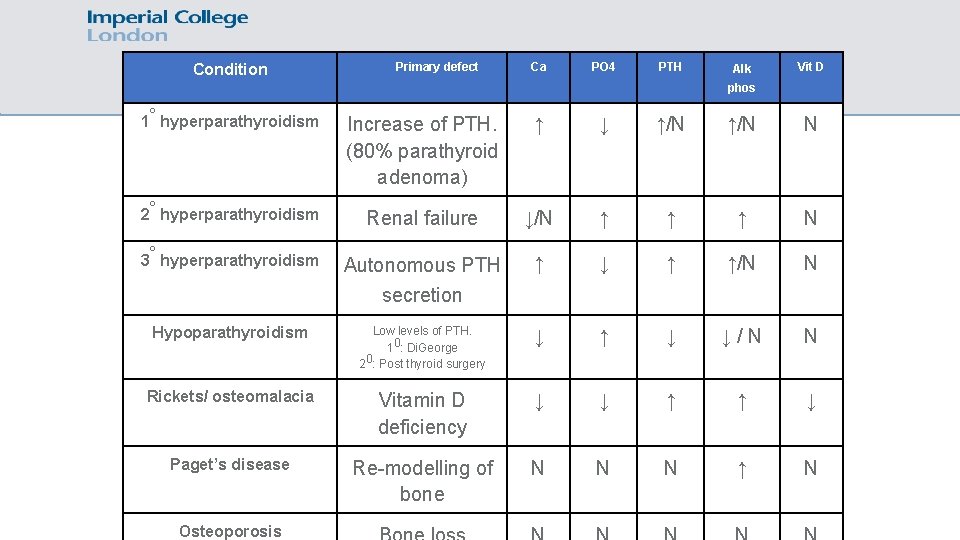
Condition Calcium chart Primary defect Ca PO 4 PTH Alk Vit D phos 1° hyperparathyroidism Increase of PTH. (80% parathyroid adenoma) ↑ ↓ ↑/N N 2° hyperparathyroidism Renal failure ↓/N ↑ ↑ ↑ N Autonomous PTH secretion ↑ ↓ ↑ ↑/N N Hypoparathyroidism Low levels of PTH. 10: Di. George 20: Post thyroid surgery ↓ ↑ ↓ ↓/N N Rickets/ osteomalacia Vitamin D deficiency ↓ ↓ ↑ ↑ ↓ Paget’s disease Re-modelling of bone N N N ↑ N 3° hyperparathyroidism Osteoporosis
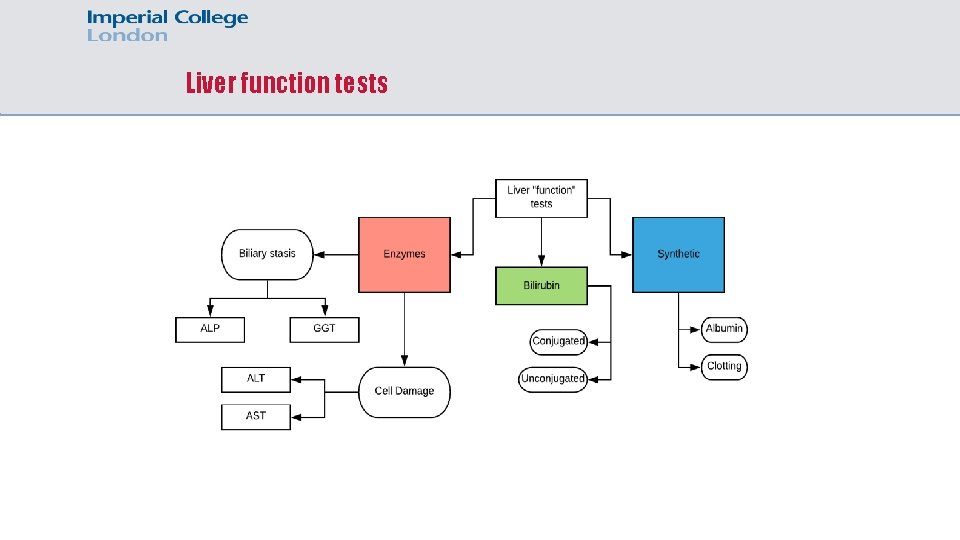
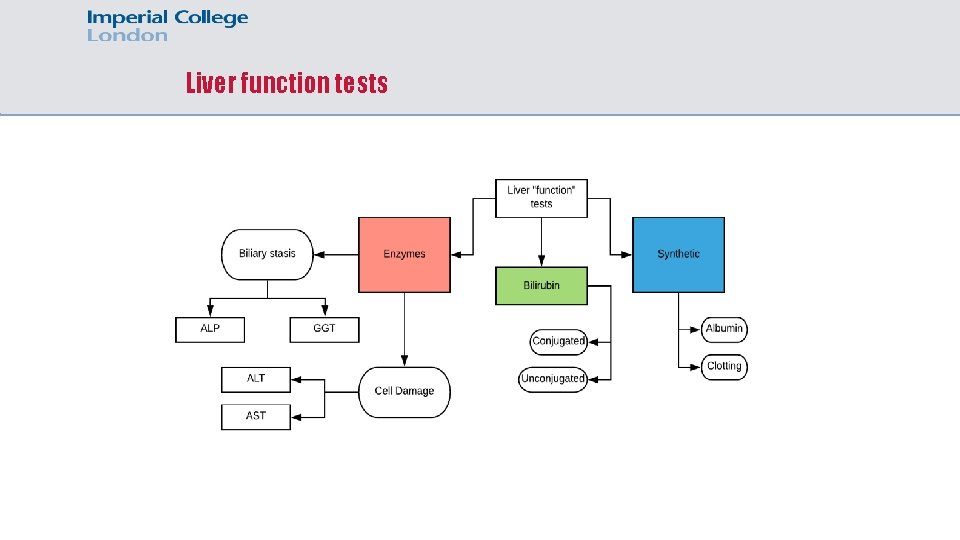
Liver function tests
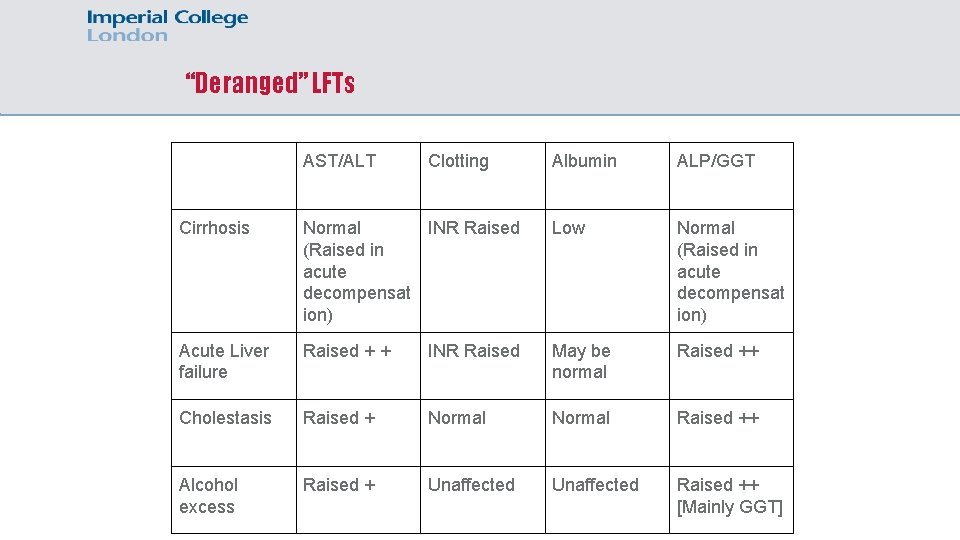
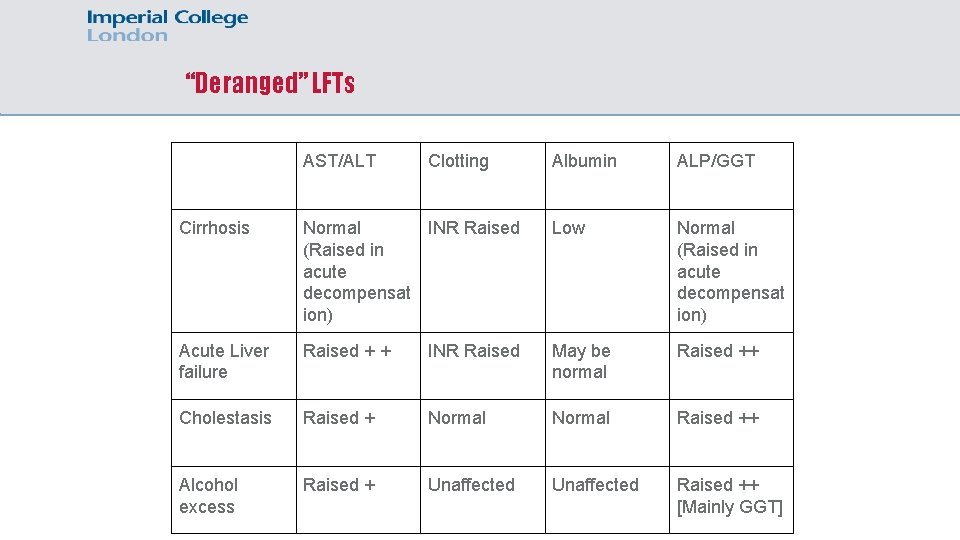
“Deranged” LFTs AST/ALT Clotting Albumin ALP/GGT Cirrhosis Normal INR Raised (Raised in acute decompensat ion) Low Normal (Raised in acute decompensat ion) Acute Liver failure Raised + + INR Raised May be normal Raised ++ Cholestasis Raised + Normal Raised ++ Alcohol excess Raised + Unaffected Raised ++ [Mainly GGT]
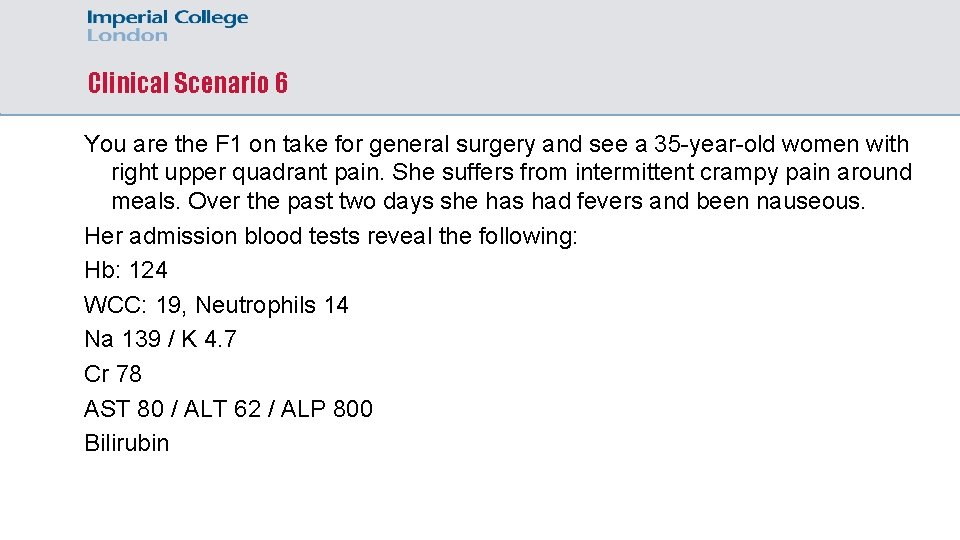
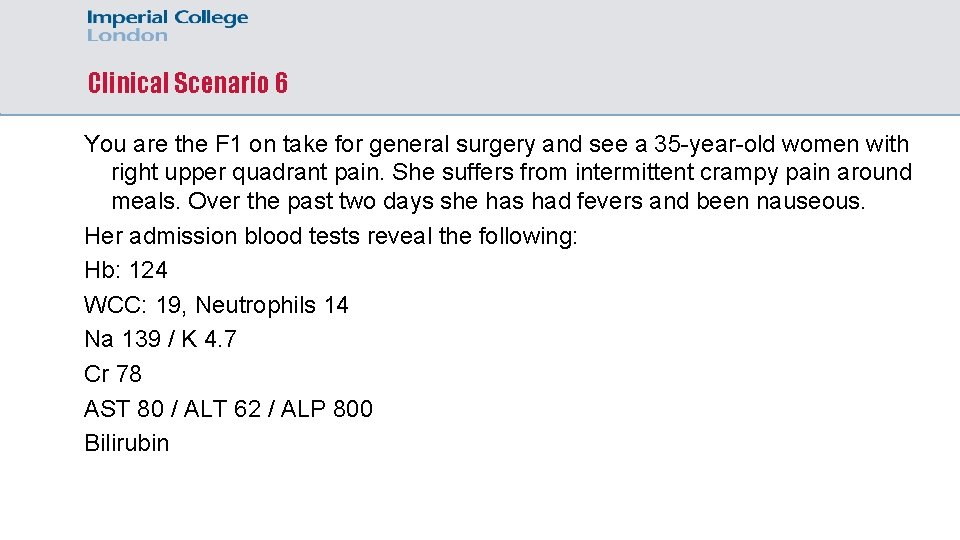
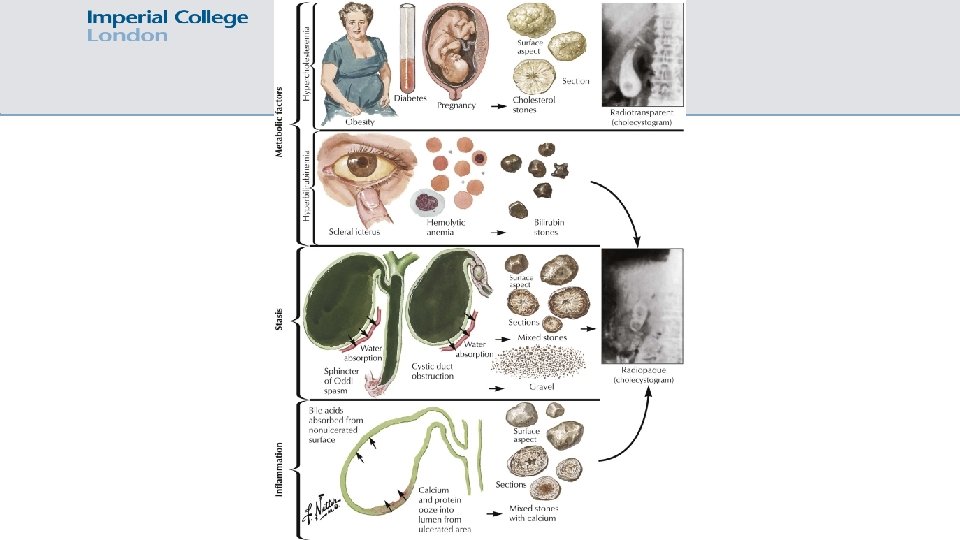
Clinical Scenario 6 You are the F 1 on take for general surgery and see a 35 -year-old women with right upper quadrant pain. She suffers from intermittent crampy pain around meals. Over the past two days she has had fevers and been nauseous. Her admission blood tests reveal the following: Hb: 124 WCC: 19, Neutrophils 14 Na 139 / K 4. 7 Cr 78 AST 80 / ALT 62 / ALP 800 Bilirubin
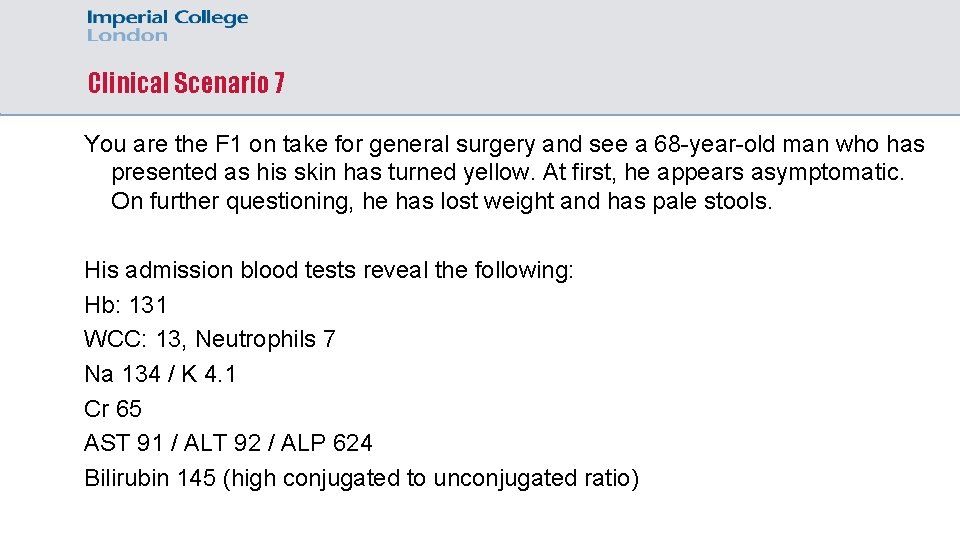
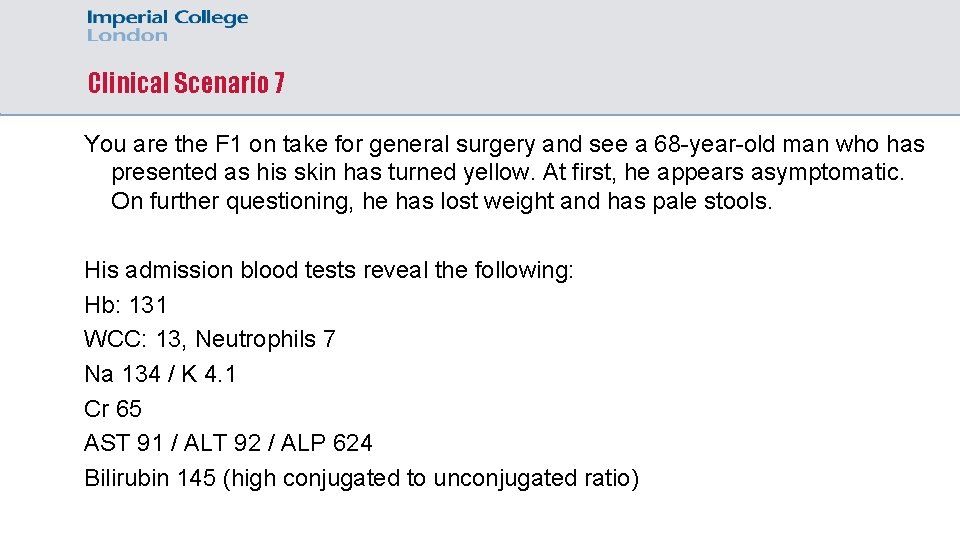
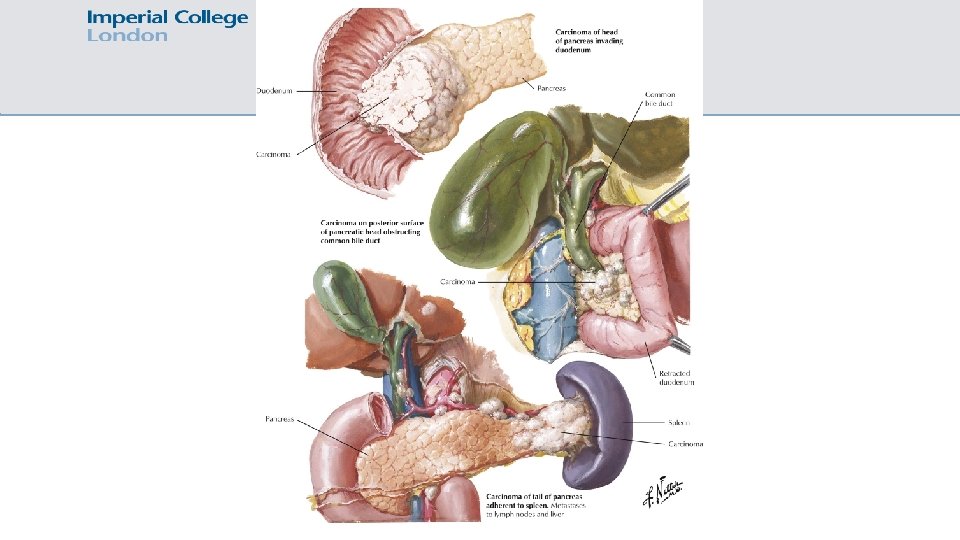
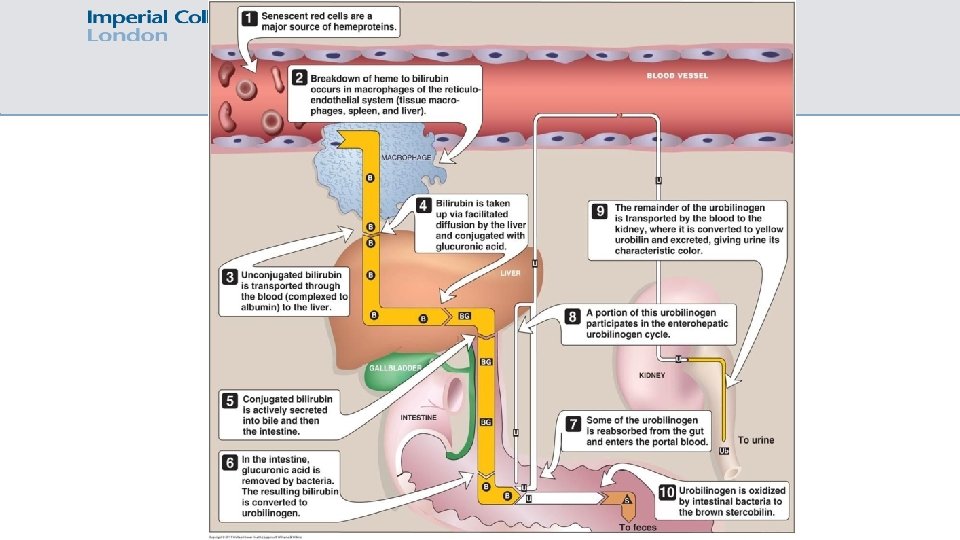
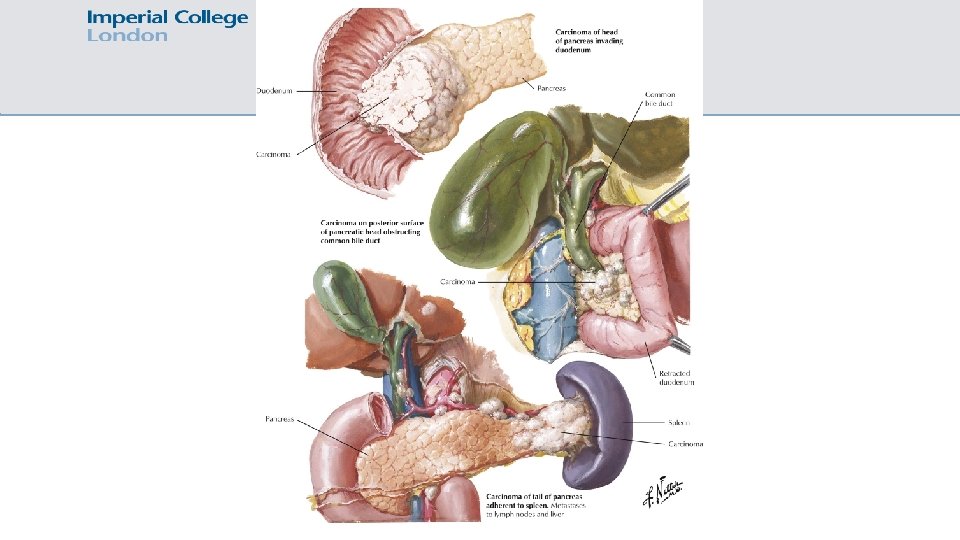
Clinical Scenario 7 You are the F 1 on take for general surgery and see a 68 -year-old man who has presented as his skin has turned yellow. At first, he appears asymptomatic. On further questioning, he has lost weight and has pale stools. His admission blood tests reveal the following: Hb: 131 WCC: 13, Neutrophils 7 Na 134 / K 4. 1 Cr 65 AST 91 / ALT 92 / ALP 624 Bilirubin 145 (high conjugated to unconjugated ratio)
Clinical Scenario 7 What will his urine dip show? a) High urinary urobilinogen b) Low urinary urobilinogen
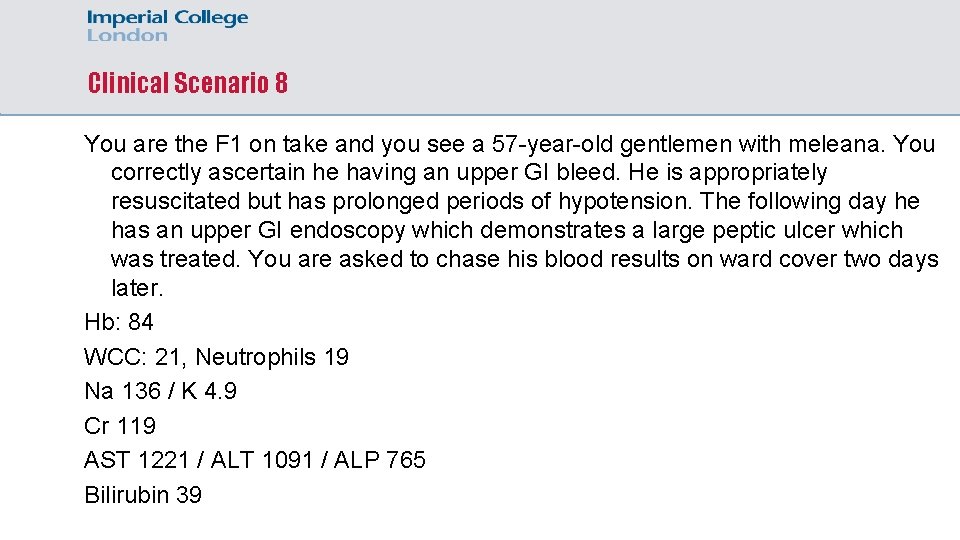
Clinical Scenario 8 You are the F 1 on take and you see a 57 -year-old gentlemen with meleana. You correctly ascertain he having an upper GI bleed. He is appropriately resuscitated but has prolonged periods of hypotension. The following day he has an upper GI endoscopy which demonstrates a large peptic ulcer which was treated. You are asked to chase his blood results on ward cover two days later. Hb: 84 WCC: 21, Neutrophils 19 Na 136 / K 4. 9 Cr 119 AST 1221 / ALT 1091 / ALP 765 Bilirubin 39
Clinical Scenario 8 Which over blood test would you like to send off?
Clinical Scenario 8 You contact the on-call registrar who is concerned. The INR comes back as 3. 2. They attend, review the patient, undertaken an ECG, arterial blood gas, and repeat LFTs and INR. They discuss with on-call ITU team as they are concerned that the patient has suffered from the following: a) b) c) d) e) Acute liver failure secondary to alcohol excess Acute renal failure secondary to UGI bleed Decompensation of chronic liver alcohol liver disease Disseminated intravascular coagulation Ischemic hepatitis
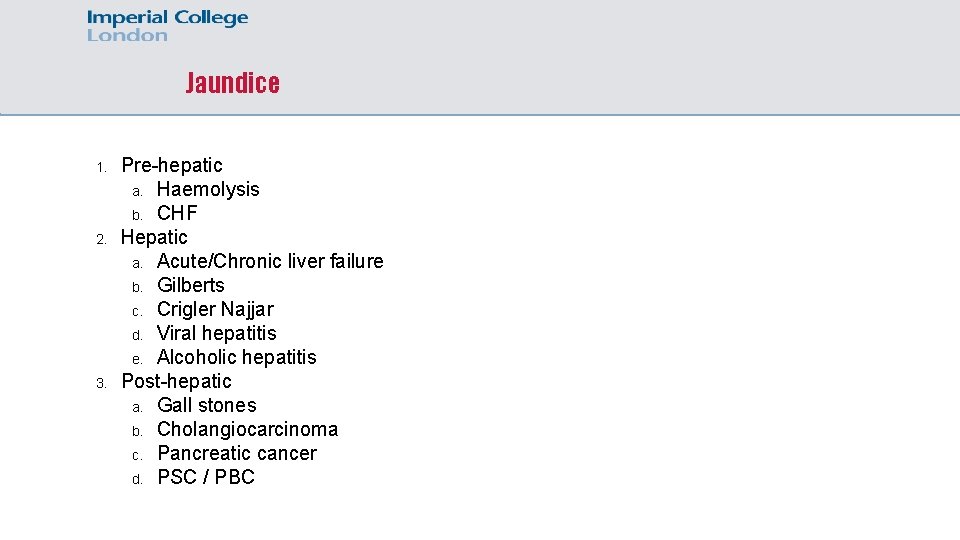
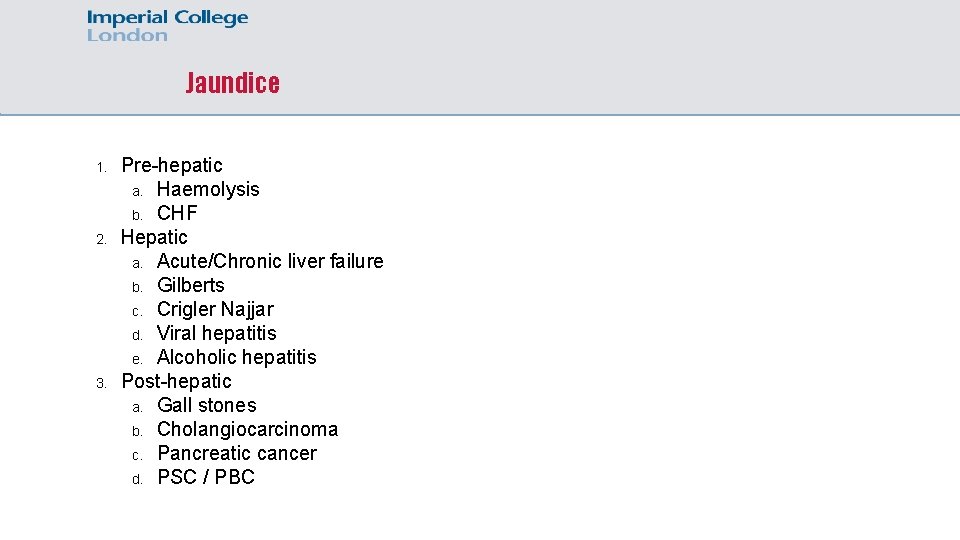
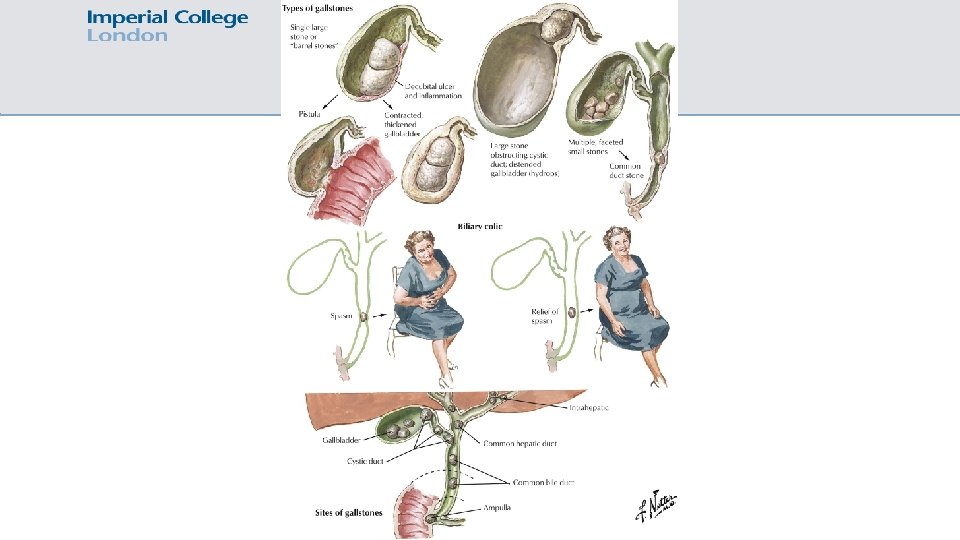
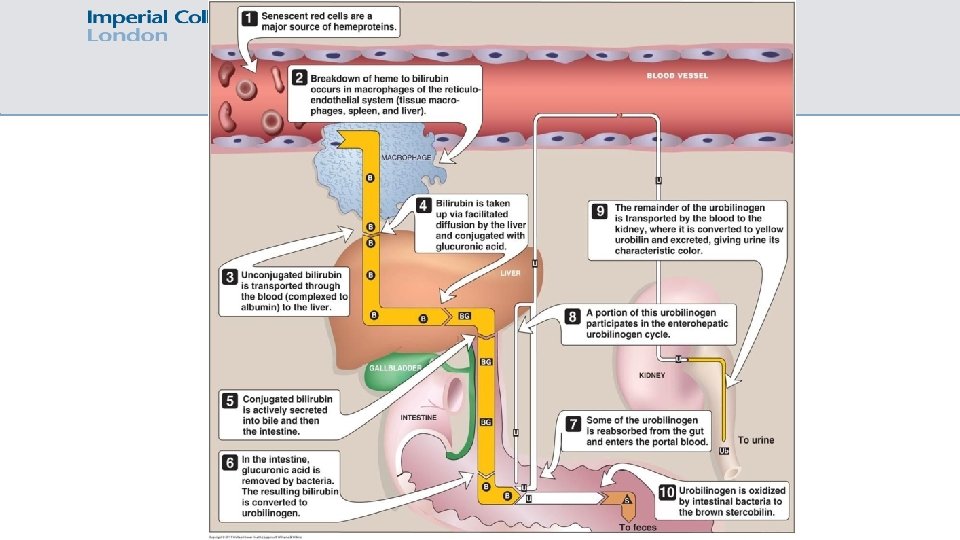
Jaundice 1. 2. 3. Pre-hepatic a. Haemolysis b. CHF Hepatic a. Acute/Chronic liver failure b. Gilberts c. Crigler Najjar d. Viral hepatitis e. Alcoholic hepatitis Post-hepatic a. Gall stones b. Cholangiocarcinoma c. Pancreatic cancer d. PSC / PBC
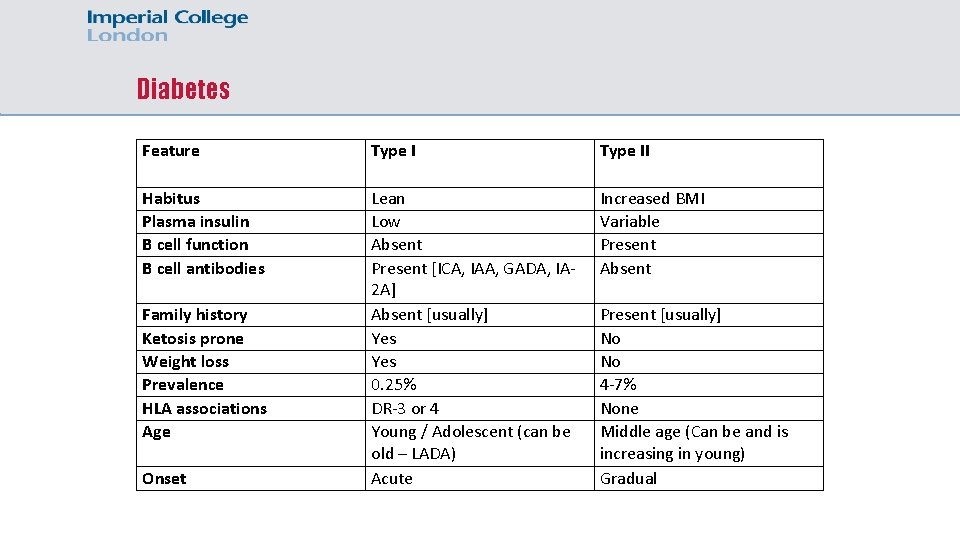
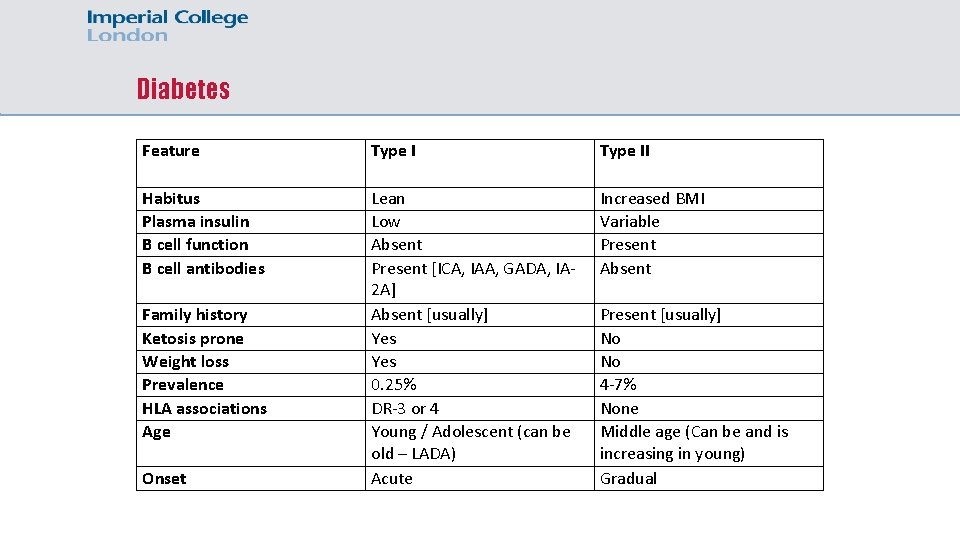
Diabetes Feature Type II Habitus Plasma insulin B cell function B cell antibodies Lean Low Absent Present [ICA, IAA, GADA, IA 2 A] Absent [usually] Yes 0. 25% DR-3 or 4 Young / Adolescent (can be old – LADA) Acute Increased BMI Variable Present Absent Family history Ketosis prone Weight loss Prevalence HLA associations Age Onset Present [usually] No No 4 -7% None Middle age (Can be and is increasing in young) Gradual
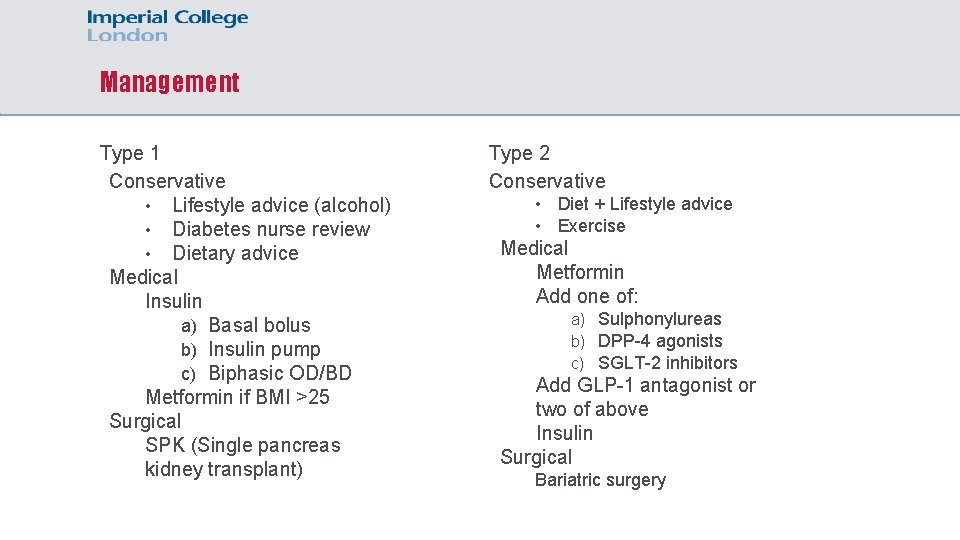
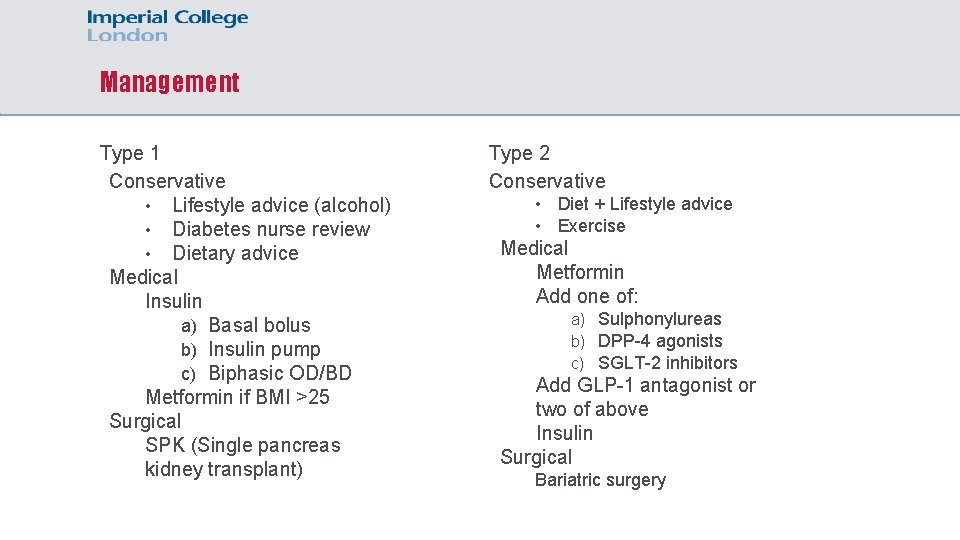
Management Type 1 Conservative • Lifestyle advice (alcohol) • Diabetes nurse review • Dietary advice Medical Insulin a) Basal bolus b) Insulin pump c) Biphasic OD/BD Metformin if BMI >25 Surgical SPK (Single pancreas kidney transplant) Type 2 Conservative • • Diet + Lifestyle advice Exercise Medical Metformin Add one of: a) Sulphonylureas b) DPP-4 agonists c) SGLT-2 inhibitors Add GLP-1 antagonist or two of above Insulin Surgical Bariatric surgery
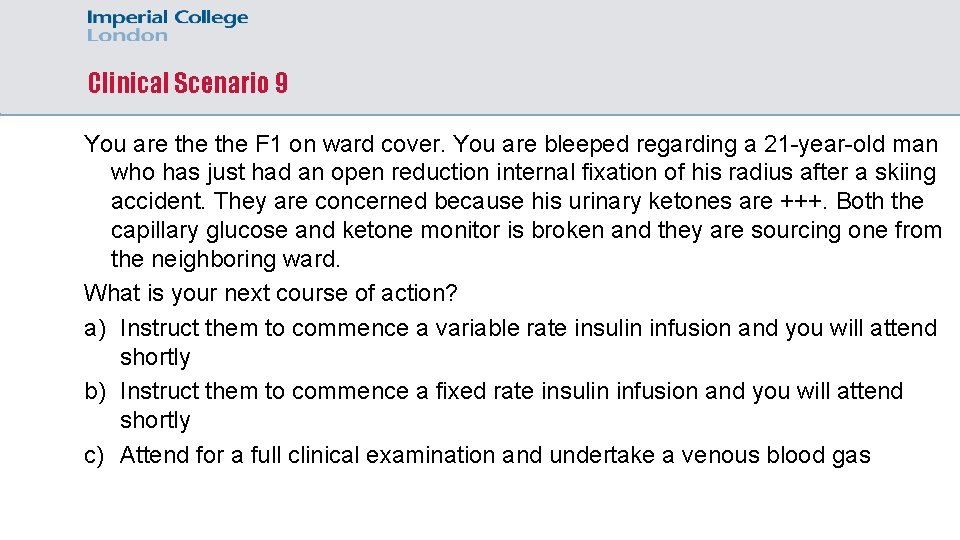
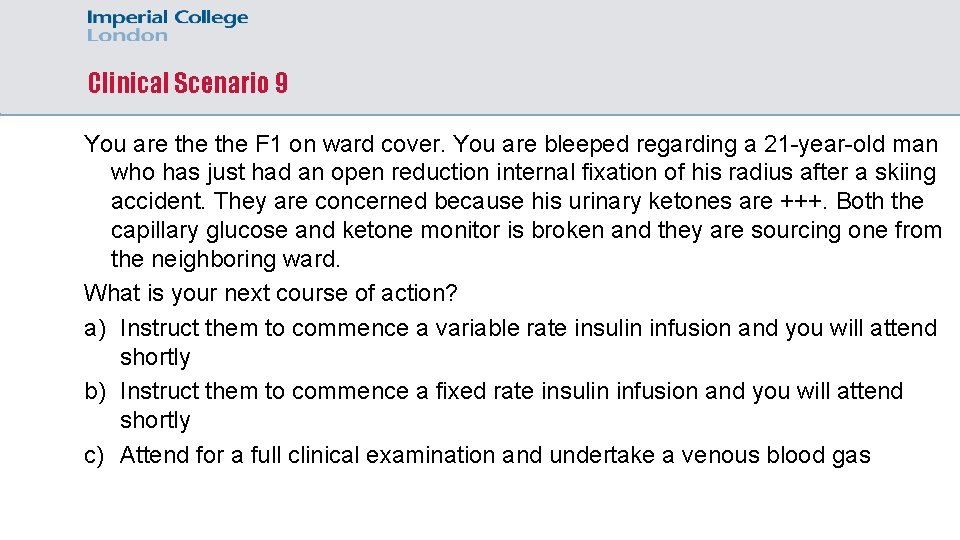
Clinical Scenario 9 You are the F 1 on ward cover. You are bleeped regarding a 21 -year-old man who has just had an open reduction internal fixation of his radius after a skiing accident. They are concerned because his urinary ketones are +++. Both the capillary glucose and ketone monitor is broken and they are sourcing one from the neighboring ward. What is your next course of action? a) Instruct them to commence a variable rate insulin infusion and you will attend shortly b) Instruct them to commence a fixed rate insulin infusion and you will attend shortly c) Attend for a full clinical examination and undertake a venous blood gas
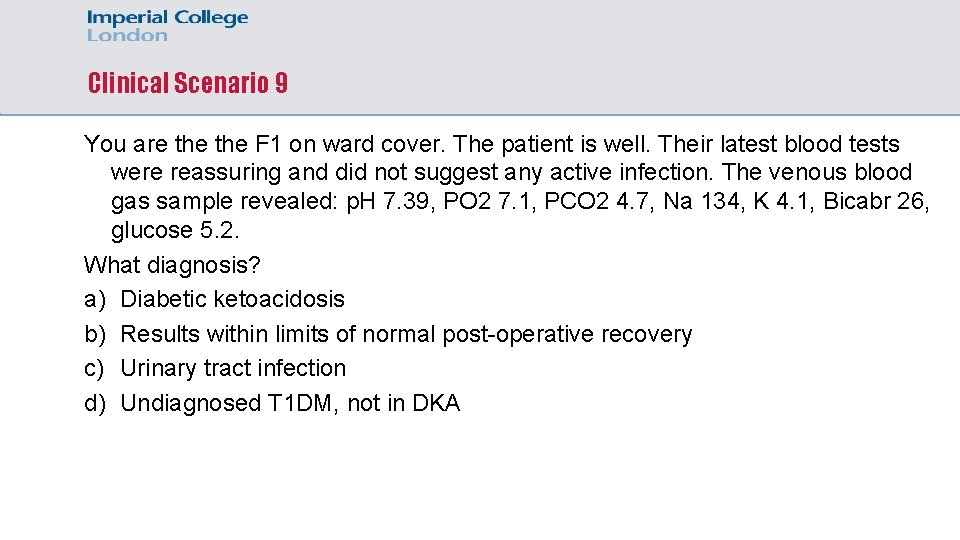
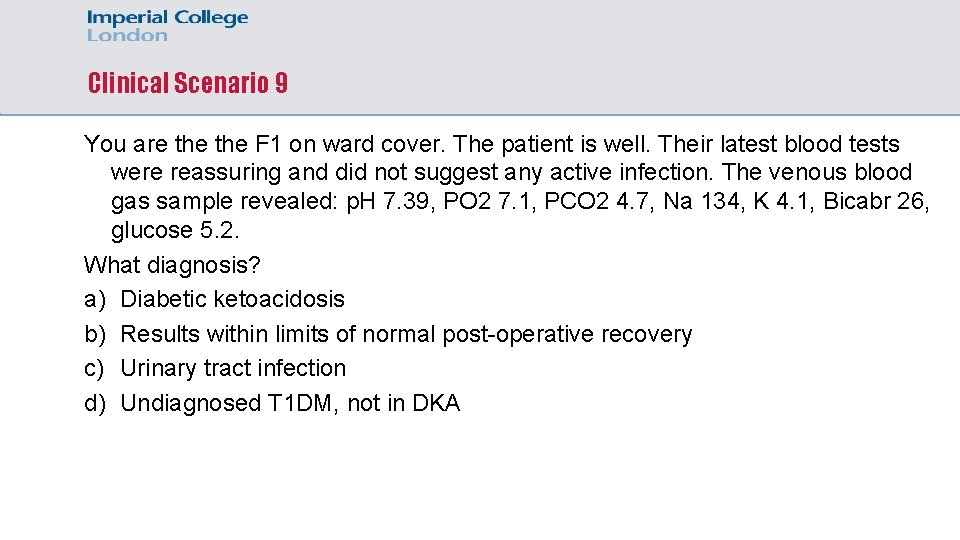
Clinical Scenario 9 You are the F 1 on ward cover. The patient is well. Their latest blood tests were reassuring and did not suggest any active infection. The venous blood gas sample revealed: p. H 7. 39, PO 2 7. 1, PCO 2 4. 7, Na 134, K 4. 1, Bicabr 26, glucose 5. 2. What diagnosis? a) Diabetic ketoacidosis b) Results within limits of normal post-operative recovery c) Urinary tract infection d) Undiagnosed T 1 DM, not in DKA
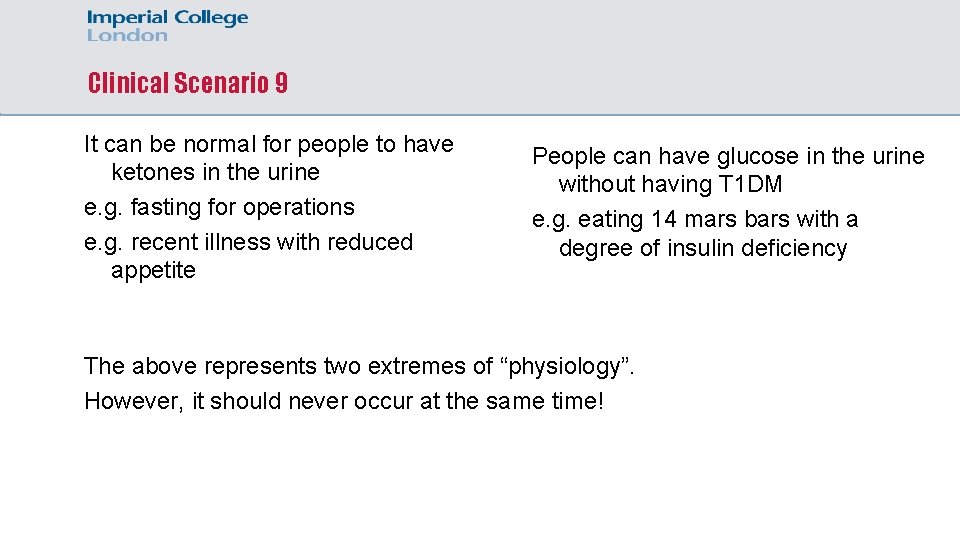
Clinical Scenario 9 It can be normal for people to have ketones in the urine e. g. fasting for operations e. g. recent illness with reduced appetite People can have glucose in the urine without having T 1 DM e. g. eating 14 mars bars with a degree of insulin deficiency The above represents two extremes of “physiology”. However, it should never occur at the same time!
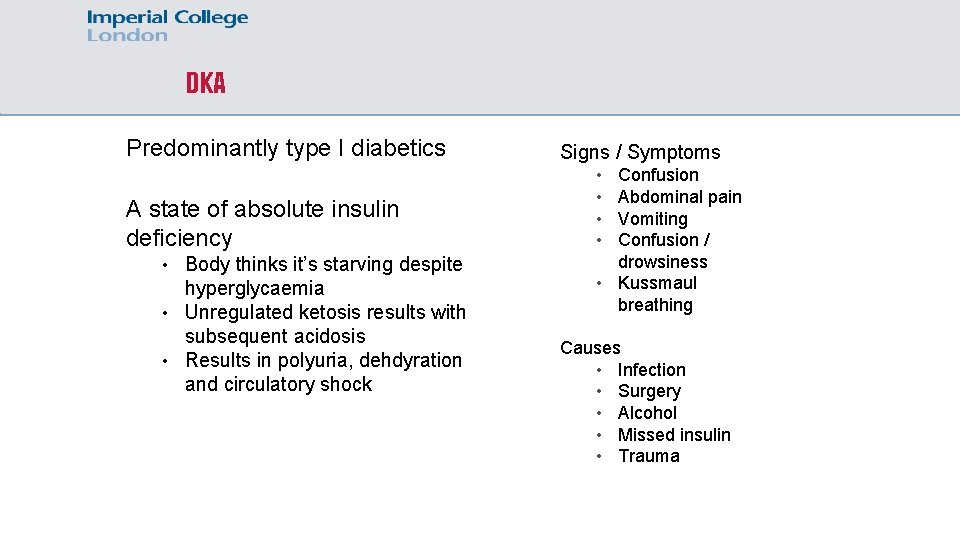
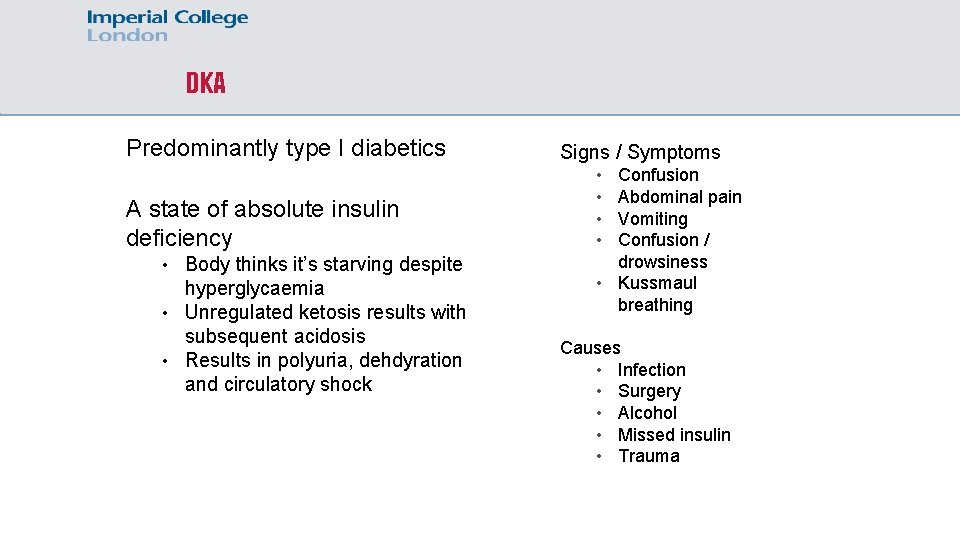
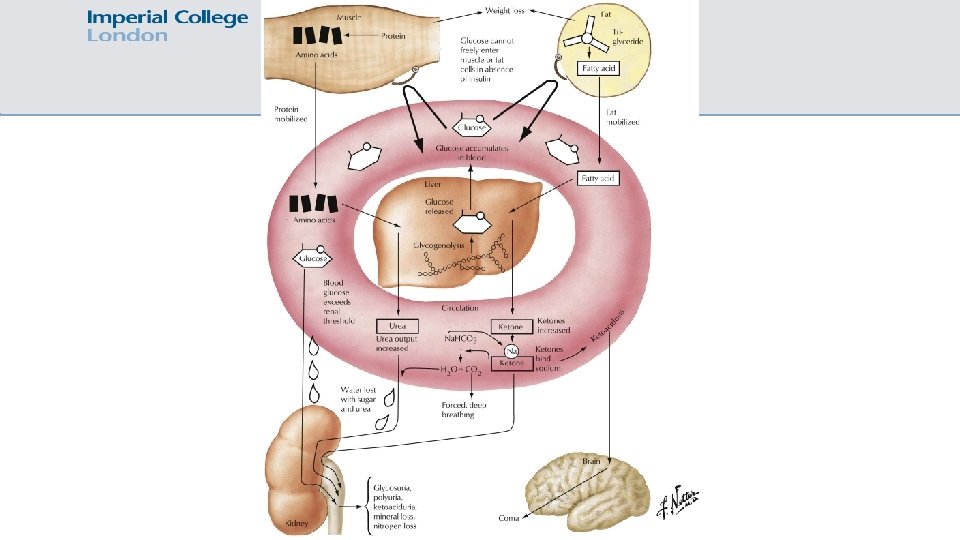
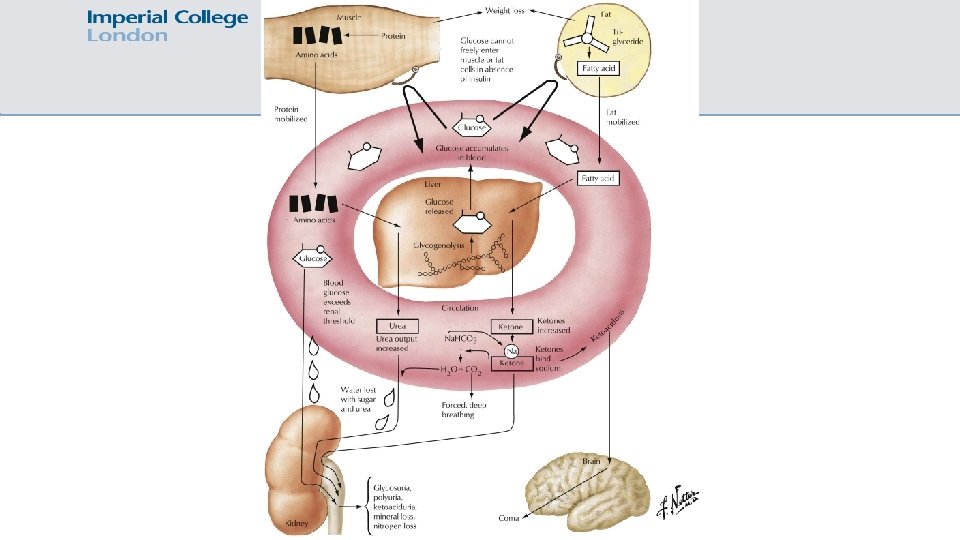
DKA Predominantly type I diabetics A state of absolute insulin deficiency • Body thinks it’s starving despite hyperglycaemia • Unregulated ketosis results with subsequent acidosis • Results in polyuria, dehdyration and circulatory shock Signs / Symptoms • • Confusion Abdominal pain Vomiting Confusion / drowsiness • Kussmaul breathing Causes • Infection • Surgery • Alcohol • Missed insulin • Trauma
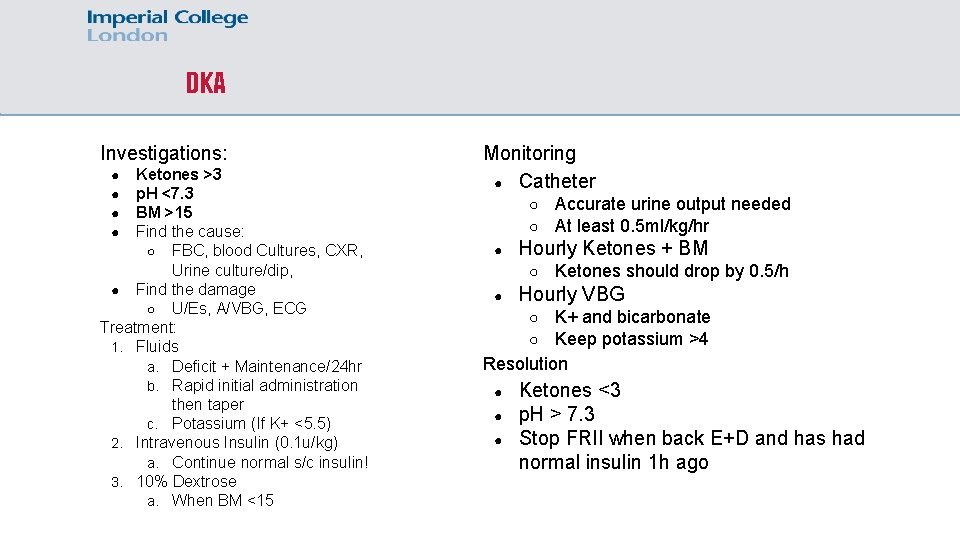
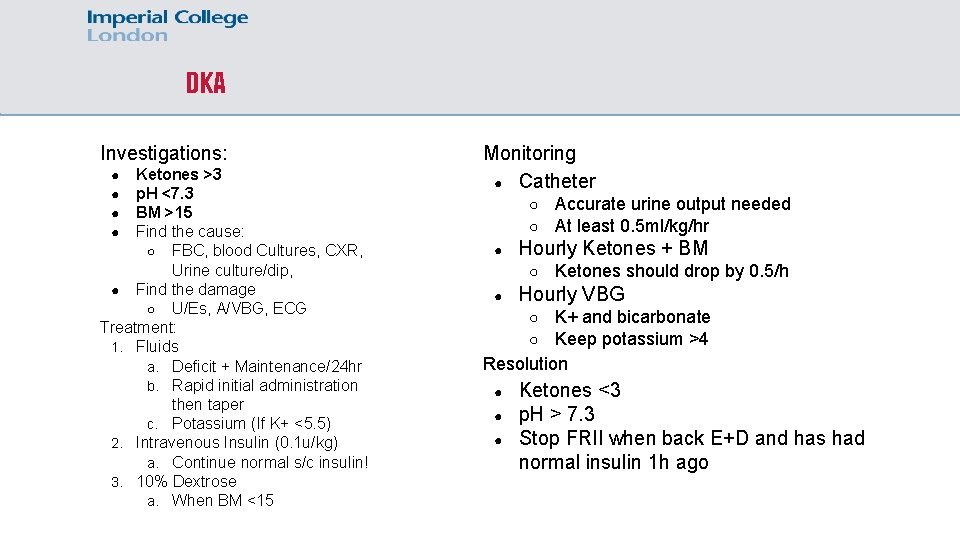
DKA Investigations: Ketones >3 p. H <7. 3 BM >15 Find the cause: ○ FBC, blood Cultures, CXR, Urine culture/dip, ● Find the damage ○ U/Es, A/VBG, ECG Treatment: 1. Fluids a. Deficit + Maintenance/24 hr b. Rapid initial administration then taper c. Potassium (If K+ <5. 5) 2. Intravenous Insulin (0. 1 u/kg) a. Continue normal s/c insulin! 3. 10% Dextrose a. When BM <15 ● ● Monitoring ● Catheter ○ ○ ● Hourly Ketones + BM ○ ● Accurate urine output needed At least 0. 5 ml/kg/hr Ketones should drop by 0. 5/h Hourly VBG K+ and bicarbonate Keep potassium >4 Resolution ○ ○ ● ● ● Ketones <3 p. H > 7. 3 Stop FRII when back E+D and has had normal insulin 1 h ago
Clinical Scenario 10 You are the F 1 on ward cover. The patient is well. Their latest blood tests were reassuring and did not suggest any active infection. The venous blood gas sample revealed: p. H 7. 39, PO 2 7. 1, PCO 2 4. 7, Na 134, K 4. 1, Bicabr 26, glucose 5. 2. What diagnosis? a) Diabetic ketoacidosis b) Results within limits of normal post-operative recovery c) Urinary tract infection d) Undiagnosed T 1 DM, not in DKA
Clinical Scenario 11 You are the F 1 on surgical ward cover. You are called about a 62 year old gentlemen who recently had a hallux amputation today for diabetic foot sepsis. The nursing staff are concerned as the patient who has become drowsy and doesn’t appear to be making any sense. You attend and undertake an A-E assessment. Airway patent. Equal air entry, no added sounds. Saturating 94% on RA. Regular, good vol radial pulse. Brisk peripheral and central cap refill. HS I + II + 0. BP 131/76, HR 82. ECG sinus rhythm. Abdomen soft, non-tender. BS normal. Foot dressing dry, no palpable collection. GCS: 14/15. PEARL. Cap glucose 16. What would you do next?
Clinical Scenario 11 Venous blood gas: p. H 6. 92, Pa. O 2 10. 9, PCO 2 5. 1, Na 135, K 4. 7, Bicarb: 16, glucose 17. 4 PMHx: Ischeamic heart disease, coronary stents, perioheral vascular disease, T 2 DM, Osteoarthritis DHx: Atorvastatin 80 mg, Aspiring 75 mg, Clopidogrel 75 mg, Gabapentin 300 mg TDS, Dapagliflozin 10 mg OD, Metformin 1 g BD CXR: small left sided pleural effusion with basal atelectasis
Clinical Scenario 11 What is the most appropriate next investigation? a) Capillary glucose (repeat) b) Capillary ketones c) Serum osmolarities d) Serum insulin e) Echocardiogram
Clinical Scenario 11 Capillary ketones: 7 What is going on?

SGLT 2 inhibitors are associated with an increased risk of DKA SGLT 2 inhibitors are an important cause a euglycaemic DKA In type-2 diabetic patients, whom do not require subcutaneous insulin, diagnosis of euglycaemic DKA secondary to SGLT 2 inhibitors is often delayed Peri-operative management of patients taking SGLT 2 inhibitors whilst fasting for surgery should include regular capillary ketone monitoring, the guidelines are yet to reflect this
Any questions? mm 5512@ic. ac. uk