Chemical Pathology Dr Swathikan Chidambaram MBBS BSc Hons
Chemical Pathology Dr Swathikan Chidambaram, MBBS BSc (Hons) Academic Foundation Doctor, Oxford
General Tips and Resources • Study material • Lectures • Pathology Guide • Questions • • Past paper questions Meeran’s questions – quizzes, in-lecture questions Pathbase - https: //candidate. speedexam. net/signin. aspx? site=pathbase Pathology SBAs by Sukhpreet Singh Dubb • References for chemical pathology • Clinical Chemistry by Marshall and Bangert
Overview • Calcium • Acid Base • LFTs • Diabetes • Other endocrine disorders • Porphyrias
Calcium physiology • Basics • Calcium • • 99% in bone. 1 % remainder. Free (“ionised”) ~50% - biologically active Protein-bound ~40% - albumin* Complexed ~10% - citrate / phosphate
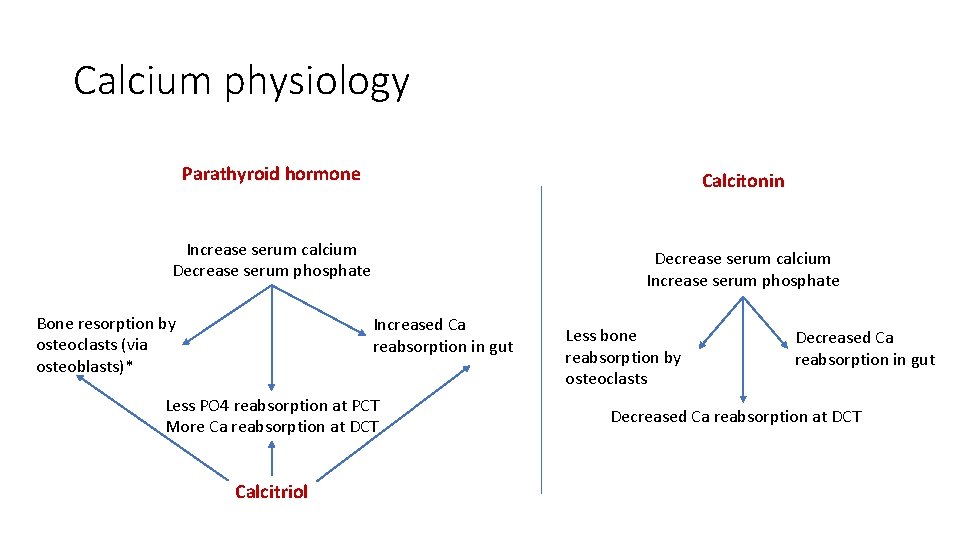
Calcium physiology Parathyroid hormone Calcitonin Increase serum calcium Decrease serum phosphate Bone resorption by osteoclasts (via osteoblasts)* Decrease serum calcium Increase serum phosphate Increased Ca reabsorption in gut Less PO 4 reabsorption at PCT More Ca reabsorption at DCT Calcitriol Less bone reabsorption by osteoclasts Decreased Ca reabsorption in gut Decreased Ca reabsorption at DCT
Calcium pathology • Osteoporosis • Osteomalacia • Paget’s disease • Parathyroid bone disease • Renal osteodystrophy • Malignancy • Familial hypocalciuric hypercalcaemia
Hypercalcemia • False – always repeat sample • If repeat sample shows hypercalcemia, the next best test is PTH level*. • True • Primary • Secondary • Tertiary
Repeat it! • Causes of erroneously high Ca: • Drip arm (Calcium gluconate infusion) • Cuffed sample (raised albumin, normal urea) • Dehydration (raised albumin and urea) • Albumin • High albumin -> artificially elevated calcium; look at corrected calcium instead
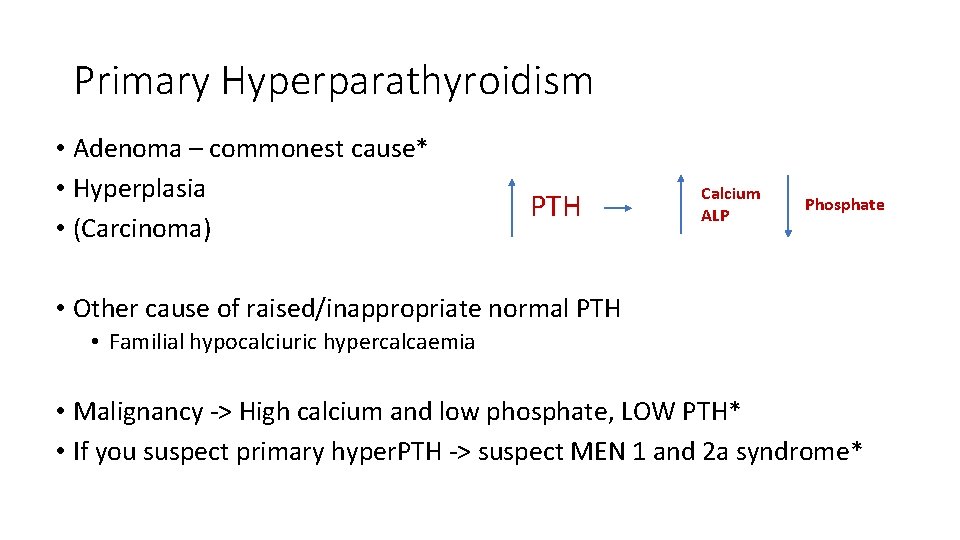
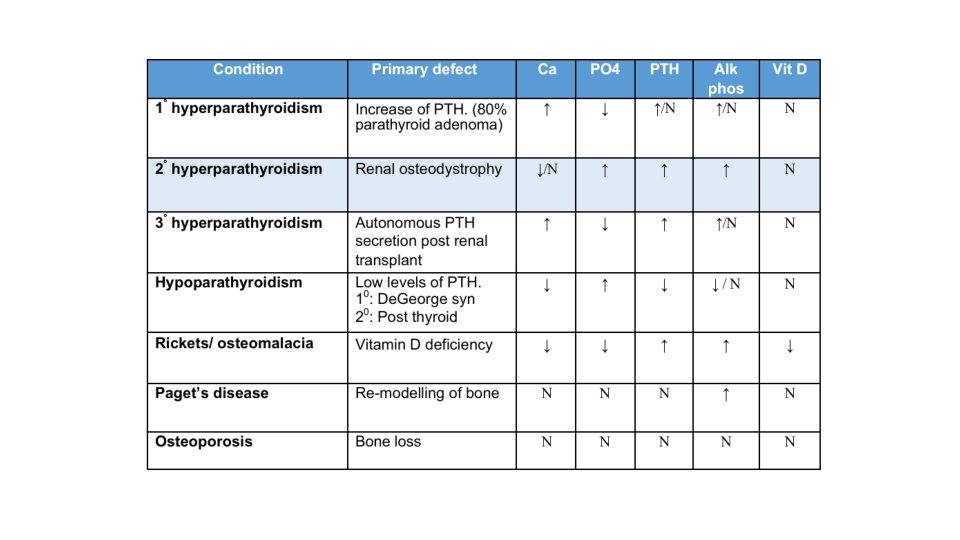
Primary Hyperparathyroidism • Adenoma – commonest cause* • Hyperplasia • (Carcinoma) PTH Calcium ALP Phosphate • Other cause of raised/inappropriate normal PTH • Familial hypocalciuric hypercalcaemia • Malignancy -> High calcium and low phosphate, LOW PTH* • If you suspect primary hyper. PTH -> suspect MEN 1 and 2 a syndrome*
Treatment • Fluids -> fluids • Surgical removal of affected glands • Cinacalcet – activates Ca. Sr protein -> lower serum calcium
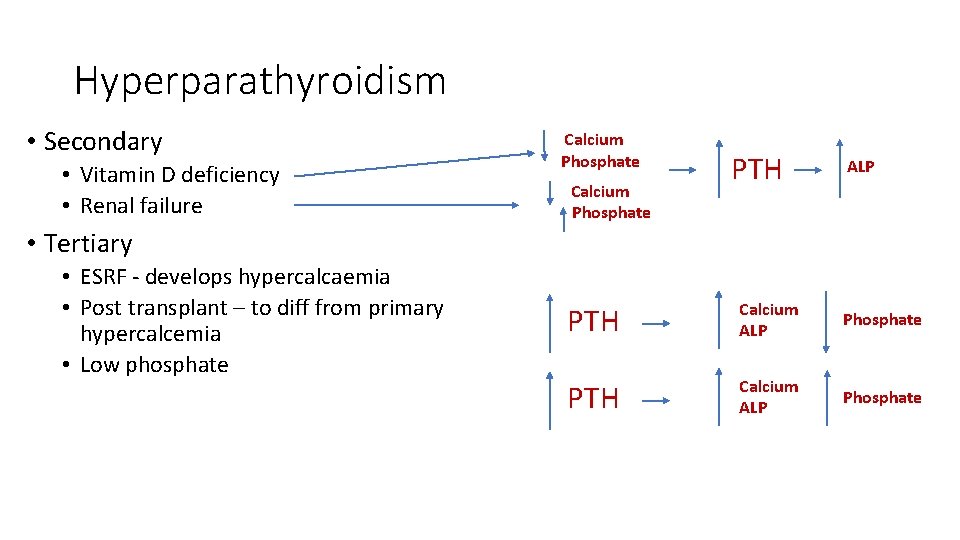
Hyperparathyroidism • Secondary • Vitamin D deficiency • Renal failure Calcium Phosphate PTH ALP • Tertiary • ESRF - develops hypercalcaemia • Post transplant – to diff from primary hypercalcemia • Low phosphate PTH Calcium ALP Phosphate
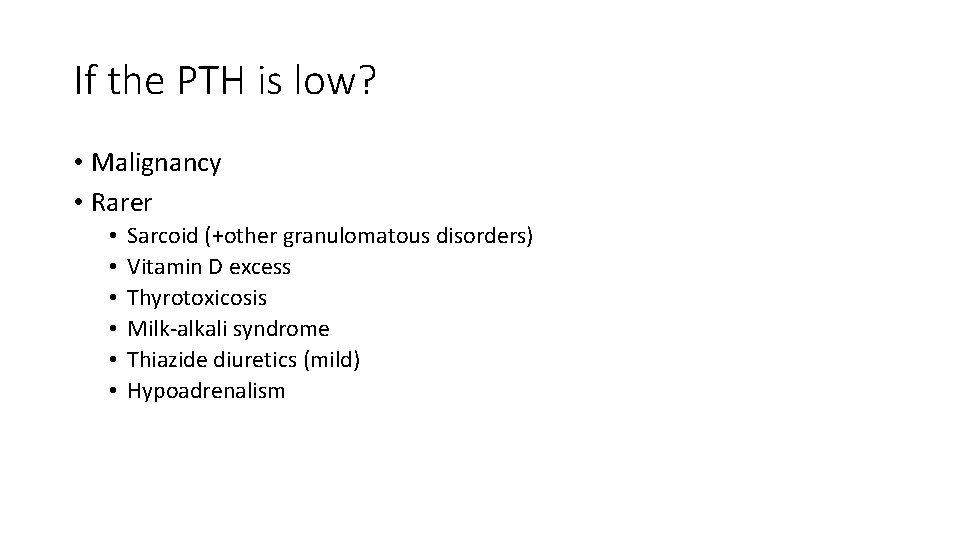
If the PTH is low? • Malignancy • Rarer • • • Sarcoid (+other granulomatous disorders) Vitamin D excess Thyrotoxicosis Milk-alkali syndrome Thiazide diuretics (mild) Hypoadrenalism
Case 1 • 51 year old women under investigation following recurrent renal calculi and constipation • Ca: 3. 0 (2. 2 -2. 6) • Phosphate 0. 70 (0. 8 -1. 4) • Other electrolytes normal • Next test(s)?
PTH • PTH: 6 (2 -7) • Normal PTH • Diagnosis?
Hypocalcaemia • Causes: • • Di. George Syndrome, Surgical removal Vit D deficiency Magnesium deficiency Pseudohypoparathyroidism • Pesudo-pseudohypo. PTH findings • Cases - no PTH - no calcitriol - reduced PTH release - PTH resistance - normal biochem with clinical
Case 3 • 79 -year-old lady admitted following and fall, found to have #NOF • Calcium – 2. 2 (2. 2 -2. 6) • Phosphate – 0. 8 (0. 8 -1. 4) • Next test(s)?
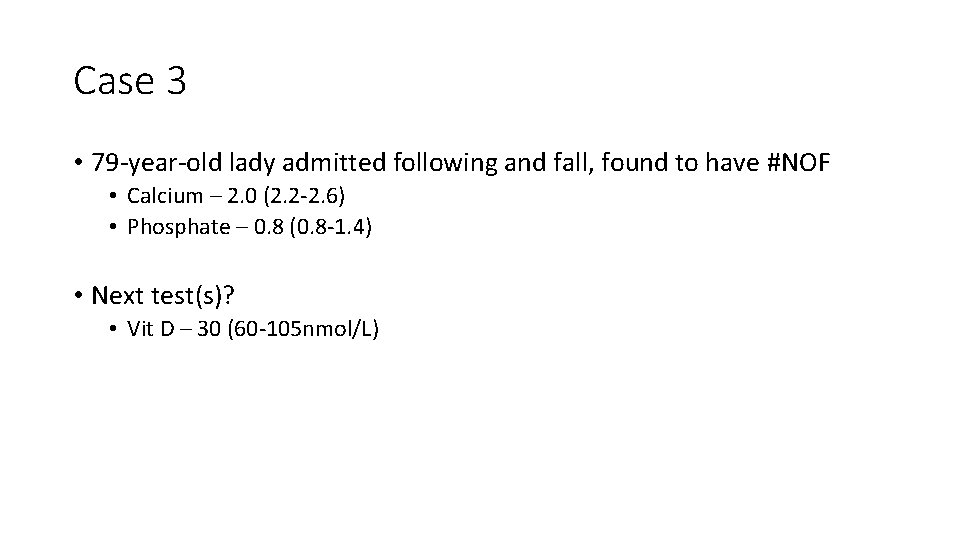
Case 3 • 79 -year-old lady admitted following and fall, found to have #NOF • Calcium – 2. 0 (2. 2 -2. 6) • Phosphate – 0. 8 (0. 8 -1. 4) • Next test(s)? • Vit D – 30 (60 -105 nmol/L)
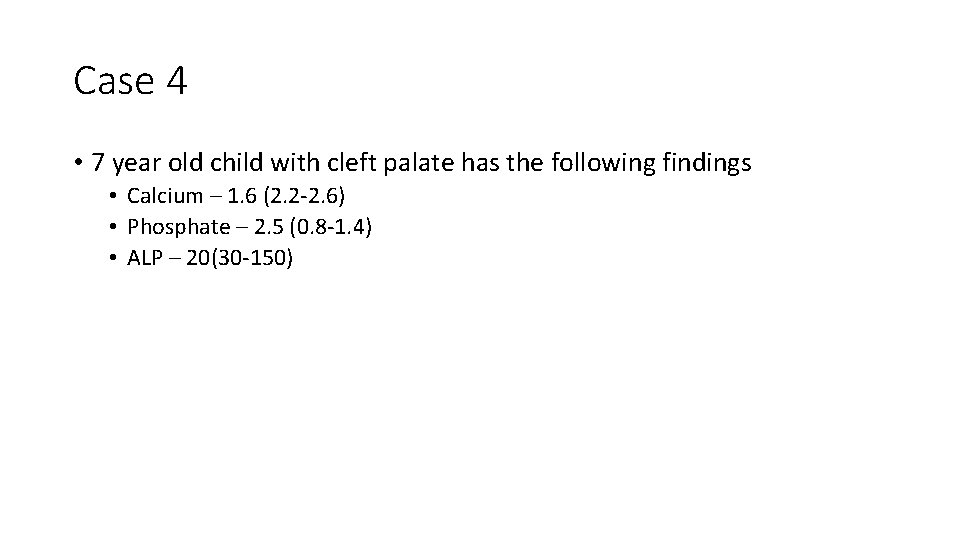
Case 4 • 7 year old child with cleft palate has the following findings • Calcium – 1. 6 (2. 2 -2. 6) • Phosphate – 2. 5 (0. 8 -1. 4) • ALP – 20(30 -150)
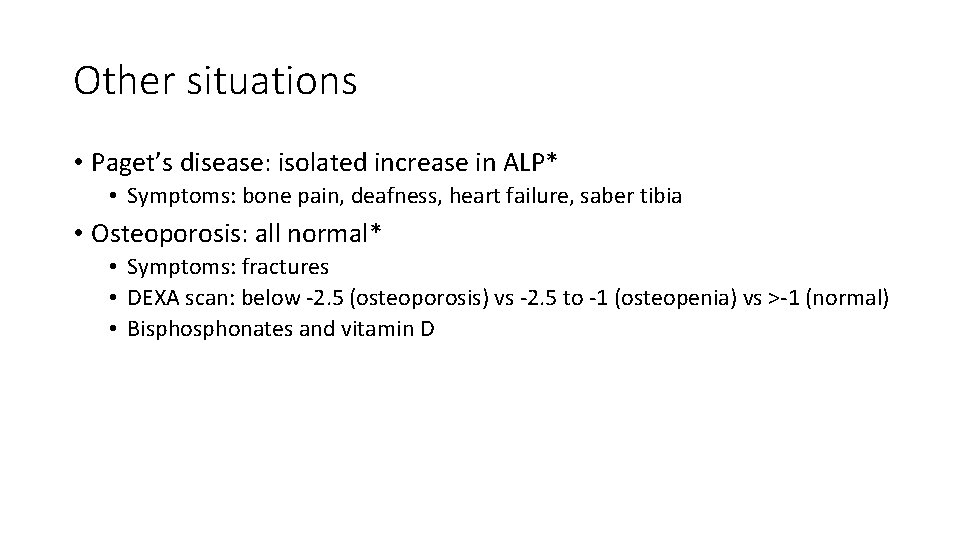
Other situations • Paget’s disease: isolated increase in ALP* • Symptoms: bone pain, deafness, heart failure, saber tibia • Osteoporosis: all normal* • Symptoms: fractures • DEXA scan: below -2. 5 (osteoporosis) vs -2. 5 to -1 (osteopenia) vs >-1 (normal) • Bisphonates and vitamin D
Hypoglycemia • Whipple’s triad. Actual number varies with patient. • Causes • Insulinoma, sulphonylurea abuse, factitious insulin • Treatment – consciousness, intact swallow • Oral glucose* • Glucagon – refractory hypoglycemia*
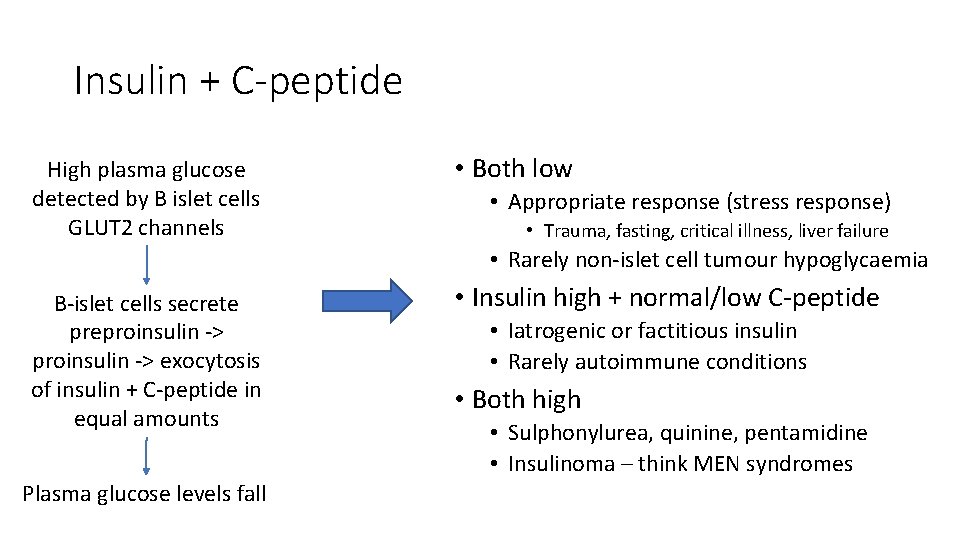
Insulin + C-peptide High plasma glucose detected by B islet cells GLUT 2 channels • Both low • Appropriate response (stress response) • Trauma, fasting, critical illness, liver failure • Rarely non-islet cell tumour hypoglycaemia B-islet cells secrete preproinsulin -> exocytosis of insulin + C-peptide in equal amounts Plasma glucose levels fall • Insulin high + normal/low C-peptide • Iatrogenic or factitious insulin • Rarely autoimmune conditions • Both high • Sulphonylurea, quinine, pentamidine • Insulinoma – think MEN syndromes
Question • Type 1 diabetic with hypoglycaemia • Insulin – low • C-peptide – low 1. 2. 3. 4. 5. Insulinoma Factitious insulin Fasting Sulphonylurea Non-islet cell tumour hypoglycaemia
Question • Type 1 diabetic with hypoglycaemia • Insulin – high • C-peptide – low 1. 2. 3. 4. 5. Insulinoma Factitious insulin Fasting Sulphonylurea Non-islet cell tumour hypoglycaemia
Question • Type 2 diabetic with hypoglycaemia • Insulin – High • C-peptide – High 1. 2. 3. 4. 5. Insulinoma Factitious insulin Fasting Sulphonylurea Non-islet cell tumour hypoglycaemia
DKA • Usually in T 1 DM • Rarely can occur in T 2 DM • Omitted insulin or increased requirement e. g. infection, trauma, acute illness • DM diagnosis, p. H<7. 35, ketones >3 M, T 1 DM • HONK: normal p. H, no ketones, high osmolality, T 2 DM
DKA • First step in management? 1. 2. 3. 4. 5. Crystalloid fluid - rehydration Insulin – drive glucose into cells Potassium – insulin drives K into cells Bicarbonate – if needed, correct alkalosis Dextrose – rebound hypoglycemia from insulin
HONK/HNK • Only in T 2 DM • Extreme dehydration, and plasma osmolality > 320 m. Osm • Insulin still present in small amounts -> no ketosis • Fluids • Insulin • Potassium • ± Heparin/LMWH

Liver • Function • Enzymes • Serology
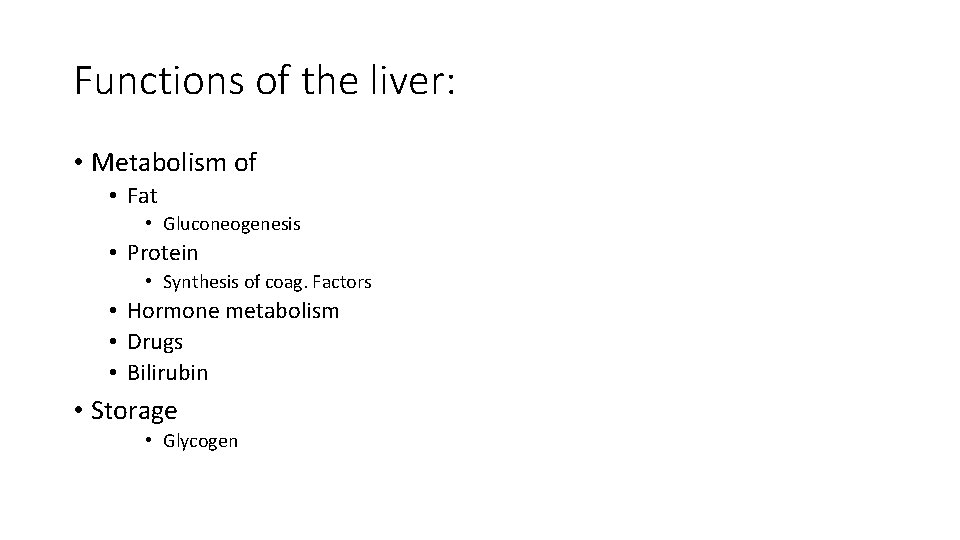
Functions of the liver: • Metabolism of • Fat • Gluconeogenesis • Protein • Synthesis of coag. Factors • Hormone metabolism • Drugs • Bilirubin • Storage • Glycogen
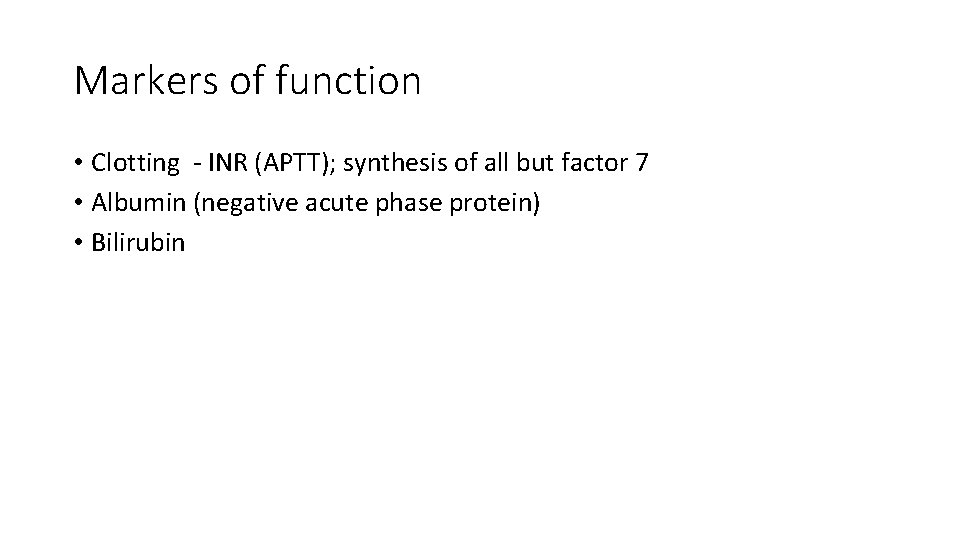
Markers of function • Clotting - INR (APTT); synthesis of all but factor 7 • Albumin (negative acute phase protein) • Bilirubin
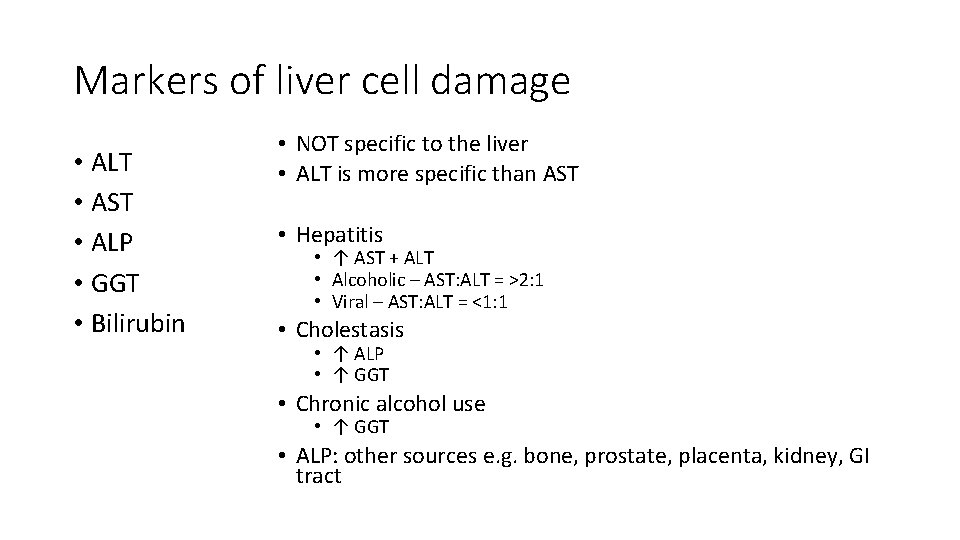
Markers of liver cell damage • ALT • AST • ALP • GGT • Bilirubin • NOT specific to the liver • ALT is more specific than AST • Hepatitis • ↑ AST + ALT • Alcoholic – AST: ALT = >2: 1 • Viral – AST: ALT = <1: 1 • Cholestasis • ↑ ALP • ↑ GGT • Chronic alcohol use • ↑ GGT • ALP: other sources e. g. bone, prostate, placenta, kidney, GI tract
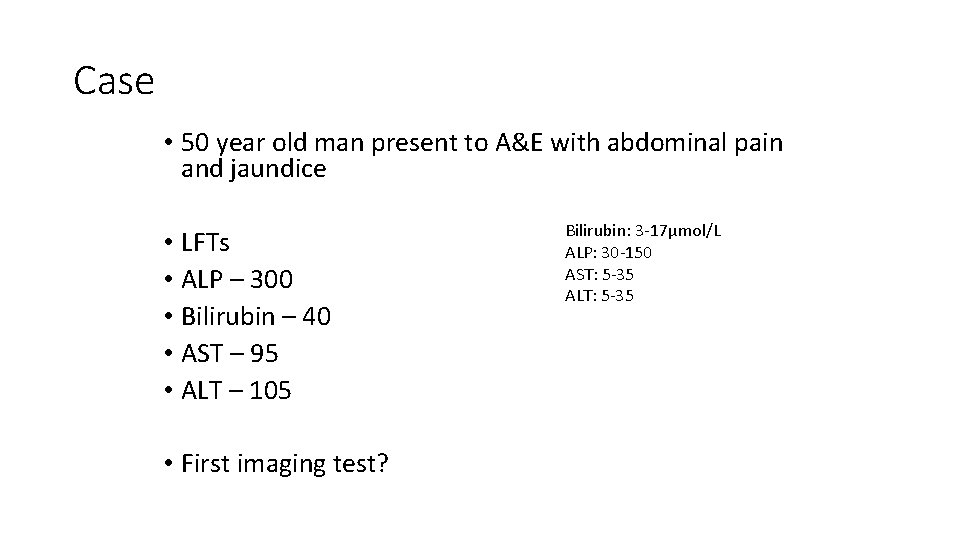
Case • 50 year old man present to A&E with abdominal pain and jaundice • LFTs • ALP – 300 • Bilirubin – 40 • AST – 95 • ALT – 105 • First imaging test? Bilirubin: 3 -17μmol/L ALP: 30 -150 AST: 5 -35 ALT: 5 -35
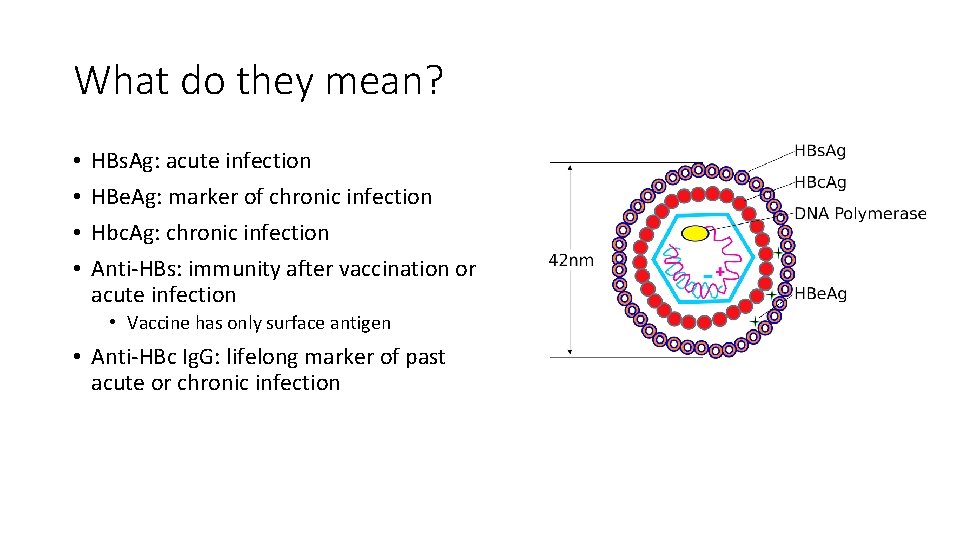
What do they mean? • • HBs. Ag: acute infection HBe. Ag: marker of chronic infection Hbc. Ag: chronic infection Anti-HBs: immunity after vaccination or acute infection • Vaccine has only surface antigen • Anti-HBc Ig. G: lifelong marker of past acute or chronic infection
Hepatitis • 24 year old gentleman returns from a year of travelling, feeling generally unwell. • • 1. 2. 3. 4. 5. Hep B surface antigen: negative Hep B surface antibody: positive Hep B core antibody (Ig. G): negative Hep B core antibody (Ig. M): negative Past infection Acute infection Chronic infection Immunised None of the above
Hepatitis • 24 year old gentleman returns from a year of travelling, feeling generally unwell. • • 1. 2. 3. 4. 5. Hep B surface antigen: positive Hep B surface antibody: negative Hep B core antibody (Ig. G): negative Hep B core antibody (Ig. M): positive Past infection Acute infection Chronic infection Immunised None of the above
Questions • 60 year old male with known gallstones, presents with jaundice 1. 2. 3. 4. 5. ALP – 400, ALT – 600 ALP – 500, ALT – 20 ALP – 500, ALT – 120 ALP – 40, ALT – 600 ALP – 40, ALT – 30 Bilirubin: 3 -17μmol/L ALP: 30 -150 AST: 5 -35 ALT: 5 -35

Questions • 24 year old male presents following an overdose of paracetamol 1. 2. 3. 4. 5. ALP – 400, ALT – 600 ALP – 500, ALT – 20 ALP – 500, ALT – 120 ALP – 40, ALT – 600 ALP – 40, ALT – 30 Bilirubin: 3 -17μmol/L ALP: 30 -150 AST: 5 -35 ALT: 5 -35

Questions • Asymptomatic 24 year old male with bilirubin of 40. His cousin has the same condition 1. 2. 3. 4. 5. ALP – 400, ALT – 600 ALP – 500, ALT – 20 ALP – 500, ALT – 120 ALP – 40, ALT – 600 ALP – 40, ALT – 30 Bilirubin: 3 -17μmol/L ALP: 30 -150 AST: 5 -35 ALT: 5 -35
Questions • 50 year old male, presents with jaundice, ALP 700, ALT – 200. USS shows no evidence of gallstones, no biliary tree dilatation • Next test(s)? Bilirubin: 3 -17μmol/L ALP: 30 -150 AST: 5 -35 ALT: 5 -35
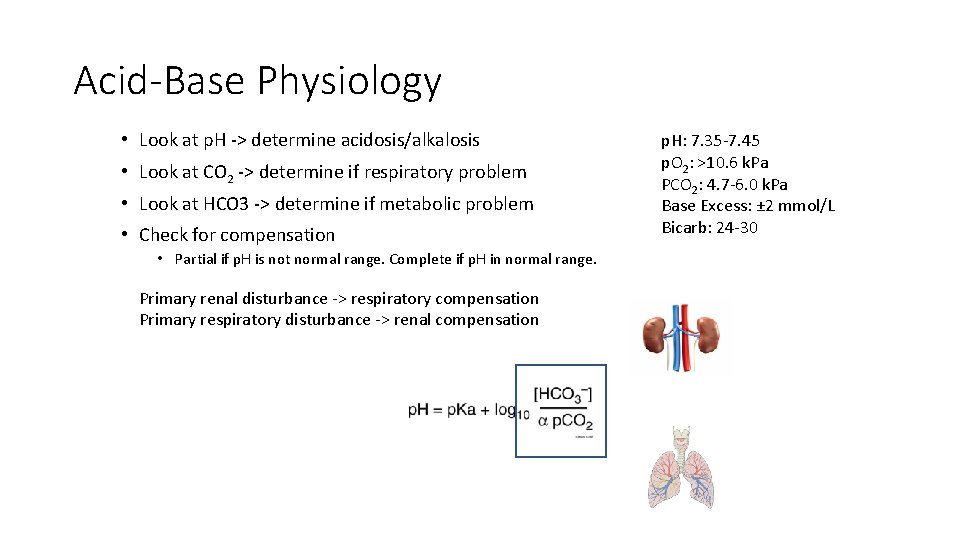
Acid-Base Physiology • Look at p. H -> determine acidosis/alkalosis • Look at CO 2 -> determine if respiratory problem • Look at HCO 3 -> determine if metabolic problem • Check for compensation • Partial if p. H is not normal range. Complete if p. H in normal range. Primary renal disturbance -> respiratory compensation Primary respiratory disturbance -> renal compensation p. H: 7. 35 -7. 45 p. O 2: >10. 6 k. Pa PCO 2: 4. 7 -6. 0 k. Pa Base Excess: ± 2 mmol/L Bicarb: 24 -30
Blood gases • p. O 2 – 8 • p. CO 2 – 8 • p. H – 7. 24 • Bicarb - 25 p. H: 7. 35 -7. 45 p. O 2: >10. 6 k. Pa PCO 2: 4. 7 -6. 0 k. Pa Base Excess: ± 2 mmol/L Bicarb: 24 -30 • Lung injury/dysfunction Respiratory acidosis • COPD • Aspiration • Fibrosis • Decreased ventilation • Neuromuscular disease • Anaesthetics/sedatives
Blood gases • PO 2 – 11 • PCO 2 – 5. 6 • p. H – 7. 3 • Bicarb - 12 p. H: 7. 35 -7. 45 p. O 2: >10. 6 k. Pa PCO 2: 4. 7 -6. 0 k. Pa Base Excess: ± 2 mmol/L Bicarb: 24 -30 Metabolic acidosis • Increased H+ formation • Lactic acidosis • DKA • Decreased H+ excretion • Renal tubular acidosis (type 1 and 4) • Renal failure • Loss of bicarb • • Diarrhoea Ileostomy Fistulae Renal tubular acidosis (type 2)
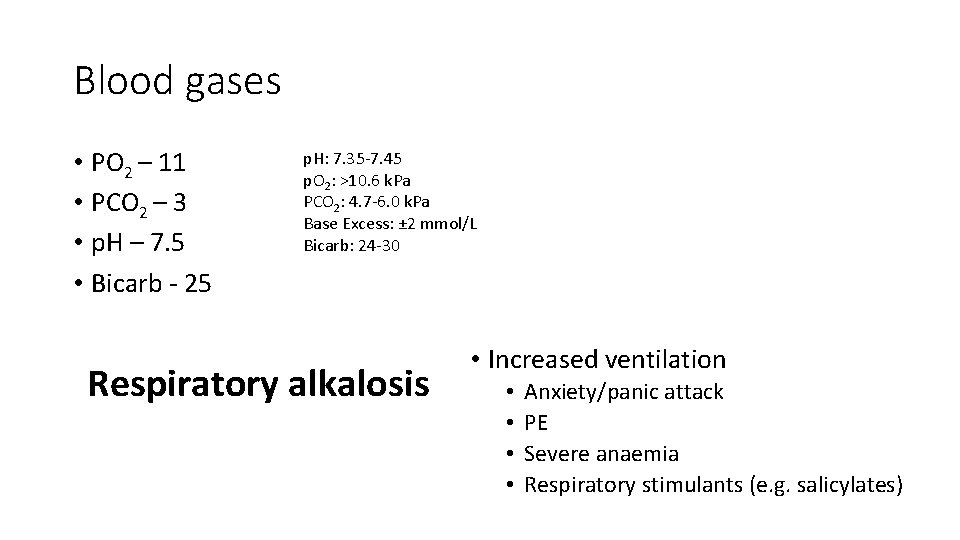
Blood gases • PO 2 – 11 • PCO 2 – 3 • p. H – 7. 5 • Bicarb - 25 p. H: 7. 35 -7. 45 p. O 2: >10. 6 k. Pa PCO 2: 4. 7 -6. 0 k. Pa Base Excess: ± 2 mmol/L Bicarb: 24 -30 Respiratory alkalosis • Increased ventilation • • Anxiety/panic attack PE Severe anaemia Respiratory stimulants (e. g. salicylates)
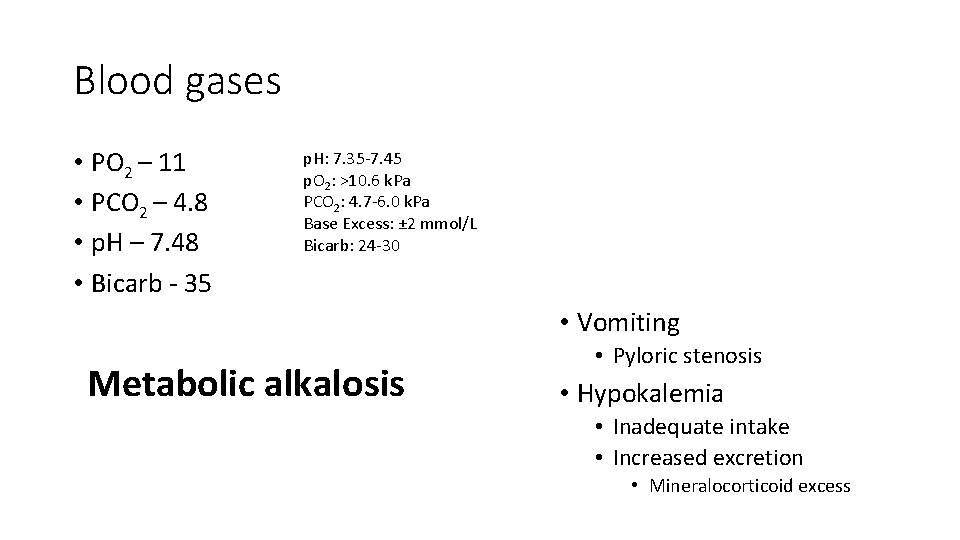
Blood gases • PO 2 – 11 • PCO 2 – 4. 8 • p. H – 7. 48 • Bicarb - 35 p. H: 7. 35 -7. 45 p. O 2: >10. 6 k. Pa PCO 2: 4. 7 -6. 0 k. Pa Base Excess: ± 2 mmol/L Bicarb: 24 -30 • Vomiting Metabolic alkalosis • Pyloric stenosis • Hypokalemia • Inadequate intake • Increased excretion • Mineralocorticoid excess
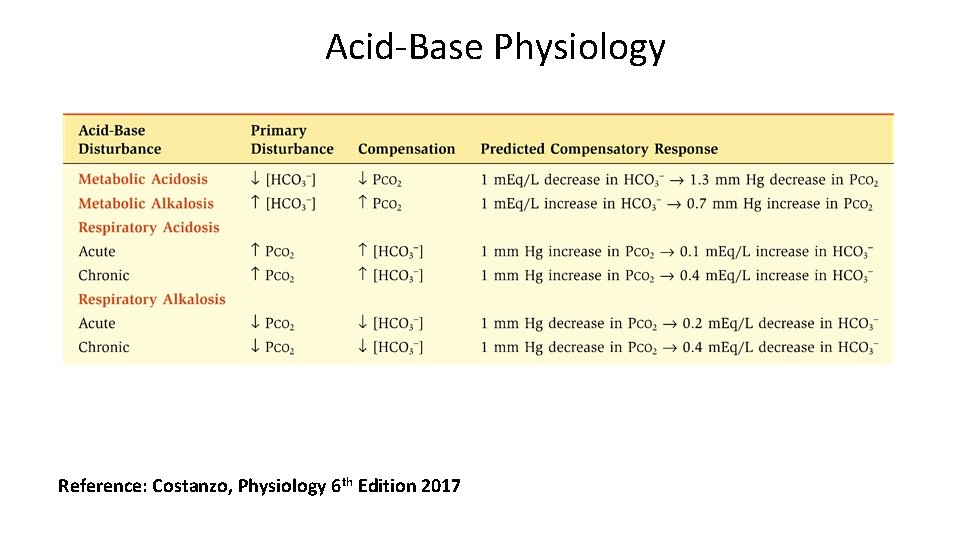
Acid-Base Physiology Reference: Costanzo, Physiology 6 th Edition 2017
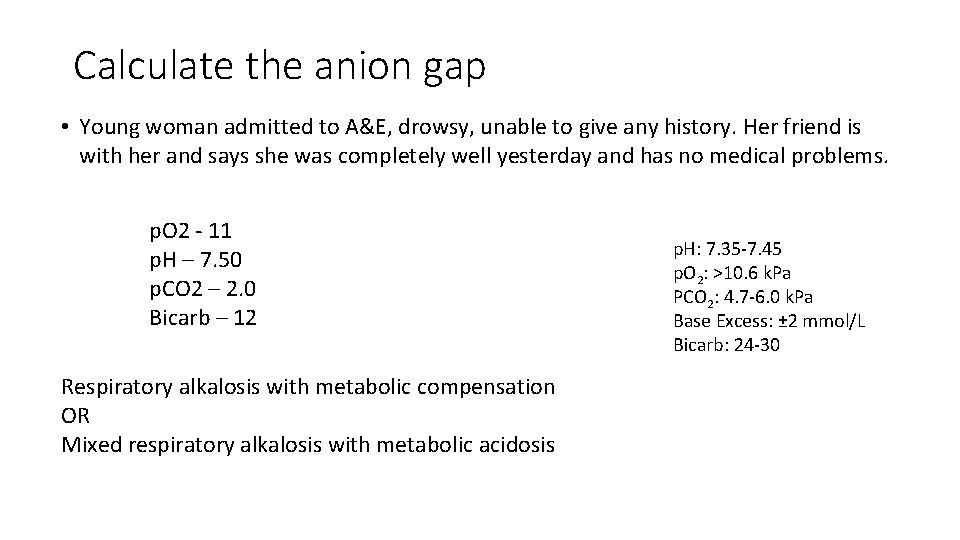
Calculate the anion gap • Young woman admitted to A&E, drowsy, unable to give any history. Her friend is with her and says she was completely well yesterday and has no medical problems. p. O 2 - 11 p. H – 7. 50 p. CO 2 – 2. 0 Bicarb – 12 Respiratory alkalosis with metabolic compensation OR Mixed respiratory alkalosis with metabolic acidosis p. H: 7. 35 -7. 45 p. O 2: >10. 6 k. Pa PCO 2: 4. 7 -6. 0 k. Pa Base Excess: ± 2 mmol/L Bicarb: 24 -30
Calculate the anion gap Na - 140 K – 4. 5 Cl – 106 Bicarb – 12 Glucose – 5. 0 Urea – 8
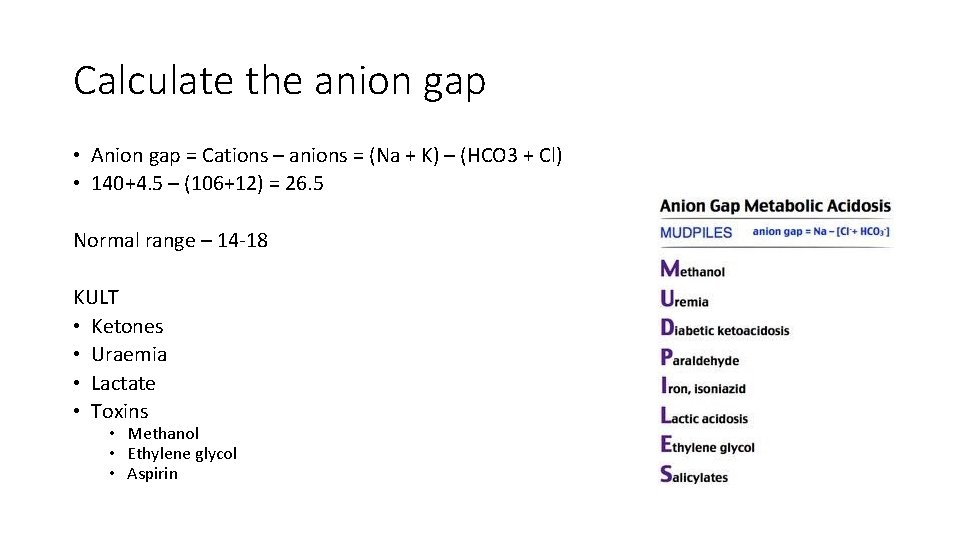
Calculate the anion gap • Anion gap = Cations – anions = (Na + K) – (HCO 3 + Cl) • 140+4. 5 – (106+12) = 26. 5 Normal range – 14 -18 KULT • Ketones • Uraemia • Lactate • Toxins • Methanol • Ethylene glycol • Aspirin
Porphyria • 7 disorders • Neurovisceral • AIP • Skin • CEP • EPP - photosensitivity • PCT • NV + Skin • HCP • VP ALA synthase is the rate limiting step*
Neuro-visceral attacks • Abdominal pain and vomiting • Tachycardia and hypertension • Constipation, urinary incontinence • Hyponatremia +/- seizures • Psychological symptoms • Sensory loss / muscle weakness • Arrhythmias / cardiac arrest
THE END All the best. Fill in feedback. Any questions: sc 3312@ic. ac. uk
- Slides: 52