Checking of Anaesthetic Equipment Description Anaesthetic practice involves

- Slides: 30
Checking of Anaesthetic Equipment Description Anaesthetic practice involves the extensive daily use of equipment. Routine checking of this equipment is essential in the safe delivery of anaesthetic care. This session provides an overview of the principles of checking the anaesthetic equipment used in current common practice, in accordance with the recommendations of the Association of Anaesthetists in Great Britain and Ireland.
Session introduction Learning objectives: • Describe the tests performed in checking the anaesthetic equipment. • Identify potential equipment malfunctions in anaesthetic practice. • Recognize the design modifications of modern anaesthetic equipment to prevent such malfunction.

introduction • Anaesthetic practice involves the extensive, daily use of equipment. Routine checking of this equipment is essential for the safe delivery of anaesthetic care.
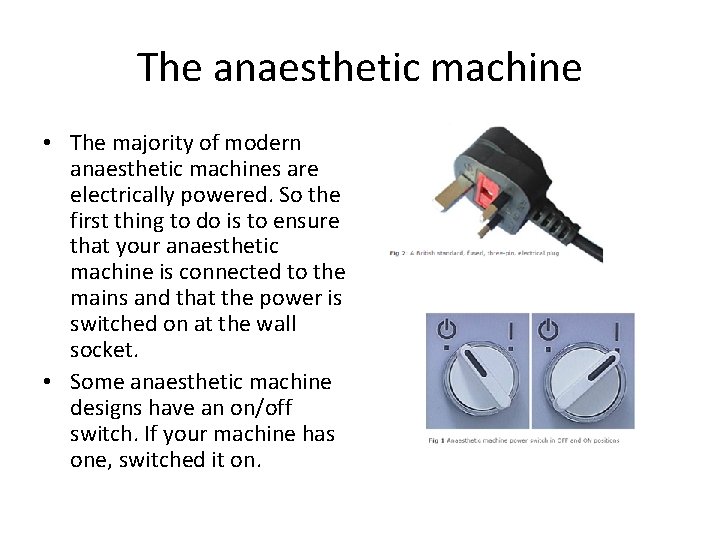
The anaesthetic machine • The majority of modern anaesthetic machines are electrically powered. So the first thing to do is to ensure that your anaesthetic machine is connected to the mains and that the power is switched on at the wall socket. • Some anaesthetic machine designs have an on/off switch. If your machine has one, switched it on.
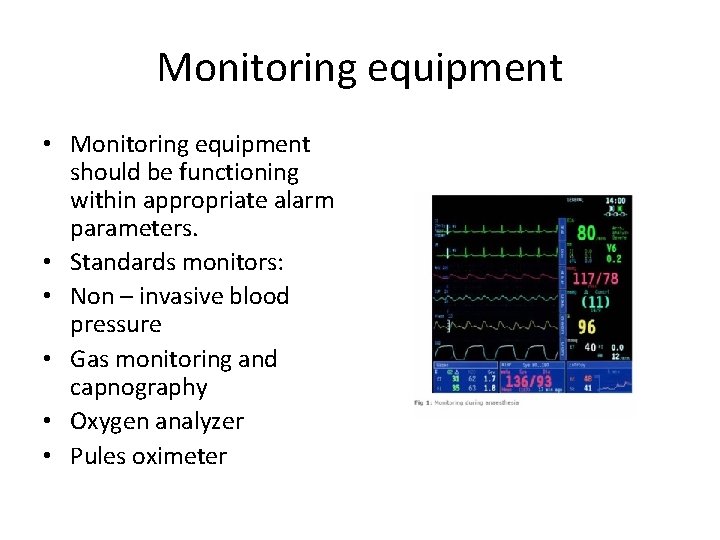
Monitoring equipment • Monitoring equipment should be functioning within appropriate alarm parameters. • Standards monitors: • Non – invasive blood pressure • Gas monitoring and capnography • Oxygen analyzer • Pules oximeter
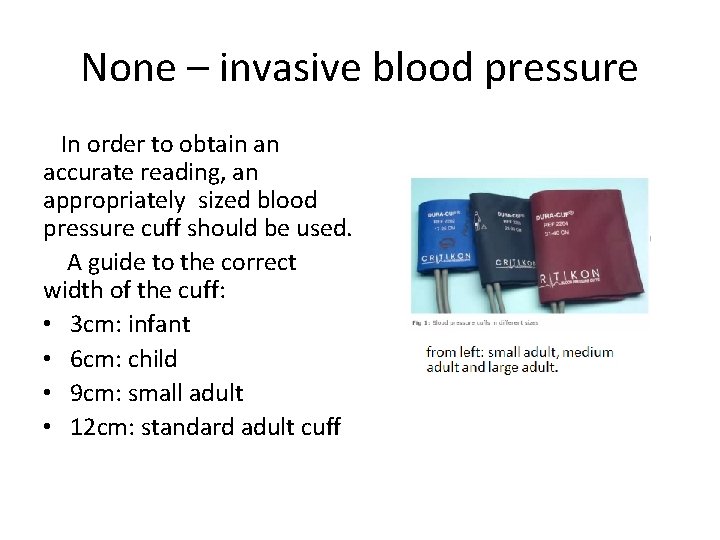
None – invasive blood pressure In order to obtain an accurate reading, an appropriately sized blood pressure cuff should be used. A guide to the correct width of the cuff: • 3 cm: infant • 6 cm: child • 9 cm: small adult • 12 cm: standard adult cuff
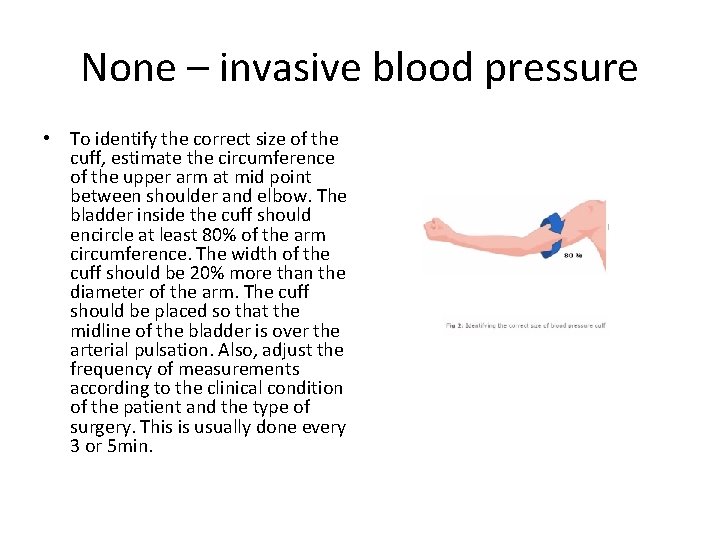
None – invasive blood pressure • To identify the correct size of the cuff, estimate the circumference of the upper arm at mid point between shoulder and elbow. The bladder inside the cuff should encircle at least 80% of the arm circumference. The width of the cuff should be 20% more than the diameter of the arm. The cuff should be placed so that the midline of the bladder is over the arterial pulsation. Also, adjust the frequency of measurements according to the clinical condition of the patient and the type of surgery. This is usually done every 3 or 5 min.
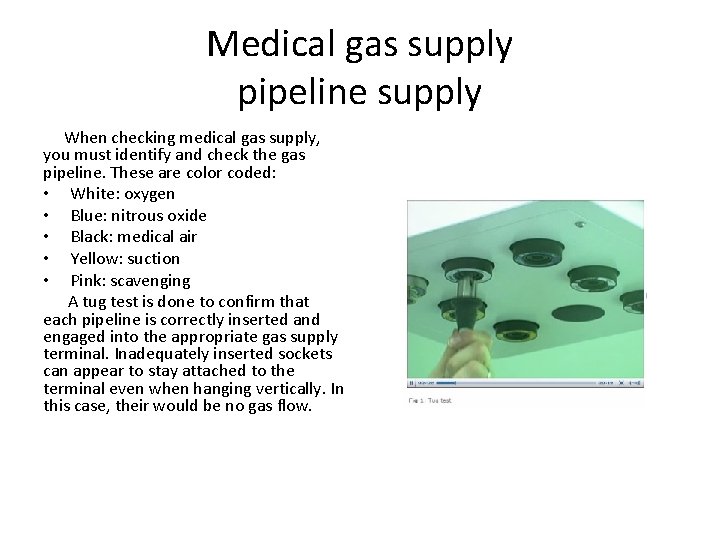
Medical gas supply pipeline supply When checking medical gas supply, you must identify and check the gas pipeline. These are color coded: • White: oxygen • Blue: nitrous oxide • Black: medical air • Yellow: suction • Pink: scavenging A tug test is done to confirm that each pipeline is correctly inserted and engaged into the appropriate gas supply terminal. Inadequately inserted sockets can appear to stay attached to the terminal even when hanging vertically. In this case, their would be no gas flow.
Medical gas supply reserve gas cylinders Reserve gas cylinders should be available to ensure a continuous supply of medical gases, even in cases of central gas supply failure. Normally, oxygen, nitrous oxide and air cylinders are attached to the anaesthetic machine as a reserve supply. Carbone dioxide cylinders should not normally present on the anaesthetic machine due to risk of administering high concentration of CO 2.
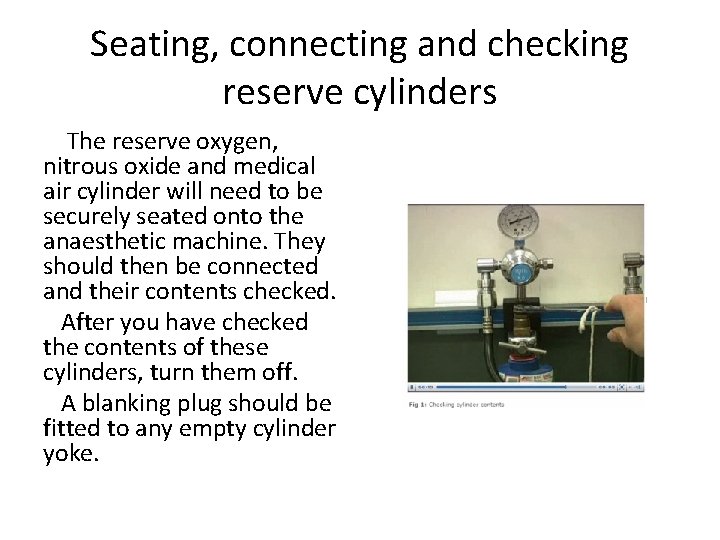
Seating, connecting and checking reserve cylinders The reserve oxygen, nitrous oxide and medical air cylinder will need to be securely seated onto the anaesthetic machine. They should then be connected and their contents checked. After you have checked the contents of these cylinders, turn them off. A blanking plug should be fitted to any empty cylinder yoke.
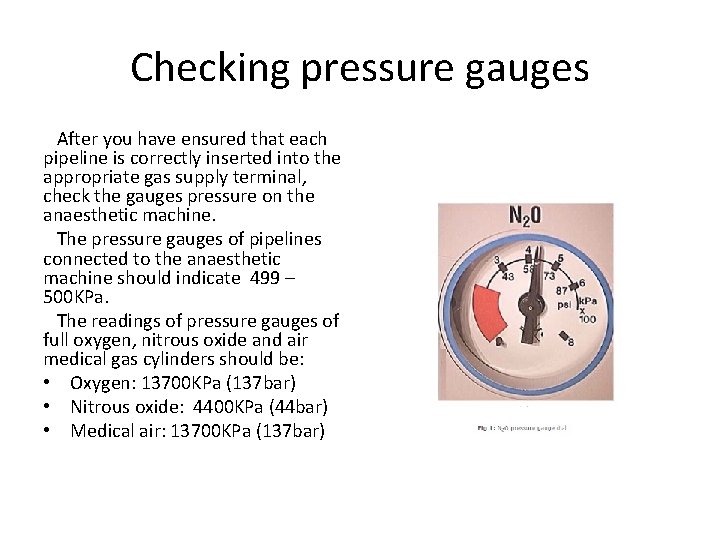
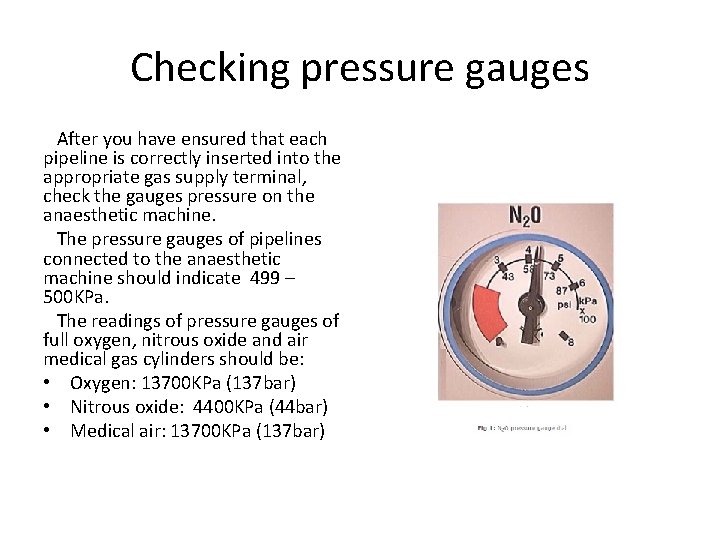
Checking pressure gauges After you have ensured that each pipeline is correctly inserted into the appropriate gas supply terminal, check the gauges pressure on the anaesthetic machine. The pressure gauges of pipelines connected to the anaesthetic machine should indicate 499 – 500 KPa. The readings of pressure gauges of full oxygen, nitrous oxide and air medical gas cylinders should be: • Oxygen: 13700 KPa (137 bar) • Nitrous oxide: 4400 KPa (44 bar) • Medical air: 13700 KPa (137 bar)
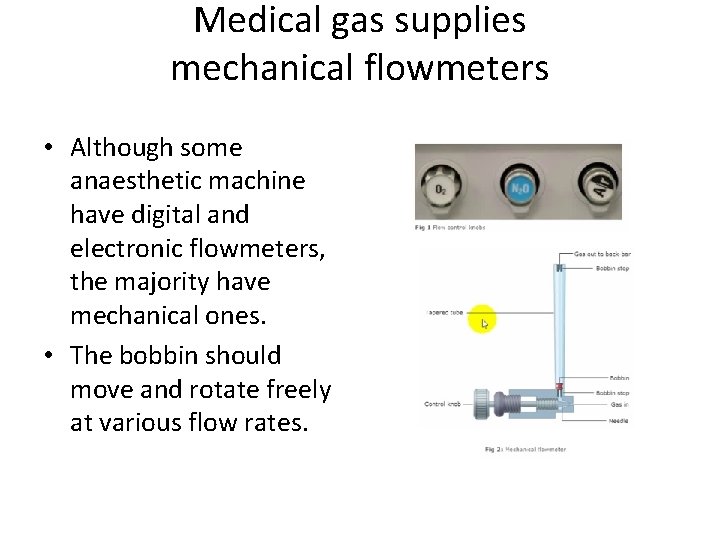
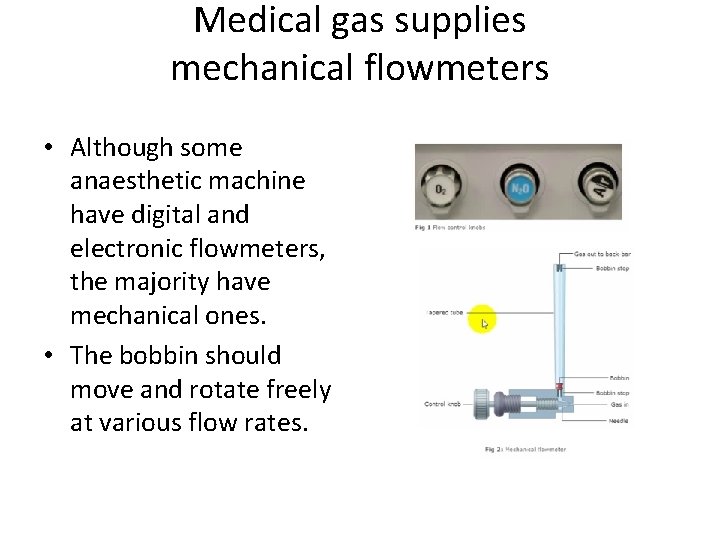
Medical gas supplies mechanical flowmeters • Although some anaesthetic machine have digital and electronic flowmeters, the majority have mechanical ones. • The bobbin should move and rotate freely at various flow rates.
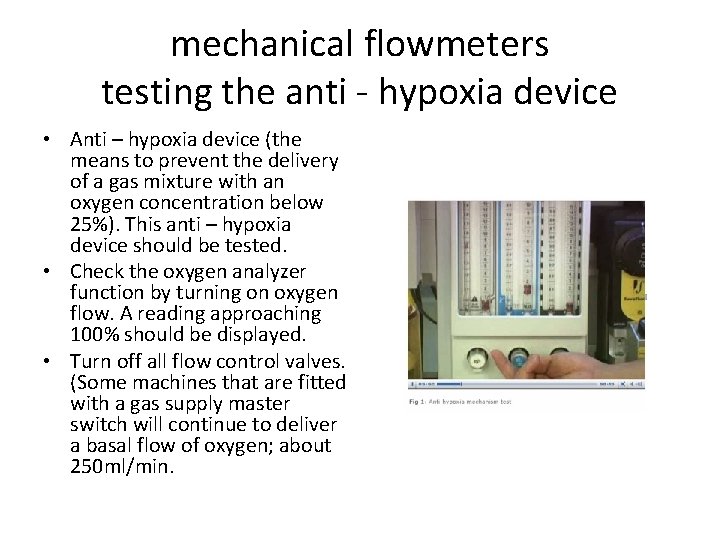
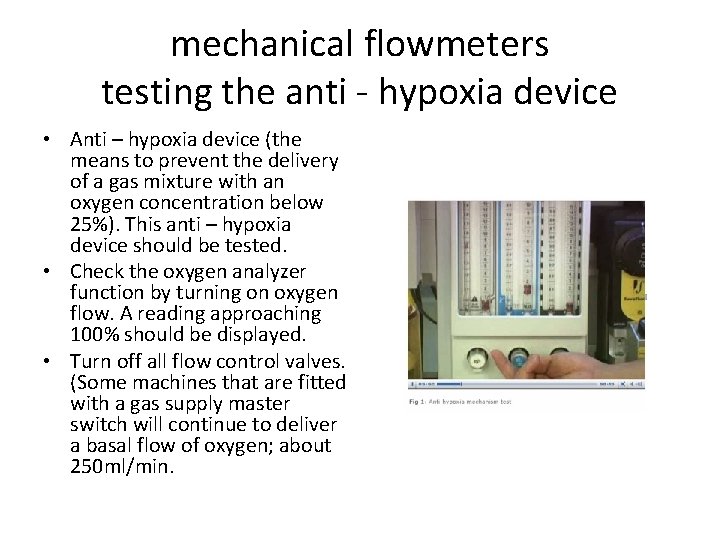
mechanical flowmeters testing the anti - hypoxia device • Anti – hypoxia device (the means to prevent the delivery of a gas mixture with an oxygen concentration below 25%). This anti – hypoxia device should be tested. • Check the oxygen analyzer function by turning on oxygen flow. A reading approaching 100% should be displayed. • Turn off all flow control valves. (Some machines that are fitted with a gas supply master switch will continue to deliver a basal flow of oxygen; about 250 ml/min.
Oxygen flash oxygen bypass • The emergency oxygen bypass control should be checked next. When the bypass button is pressed, the oxygen flow without significant decrease in the pipeline supply pressure. It is important to check that the control valve shuts off when the button is released. • The emergency oxygen flash, when activated, supplies pure oxygen with flow of about 35 – 75 L/min at a pressure of about 400 KPa. • As a safety feature, the button is recessed in a housing to prevent accidental activation.
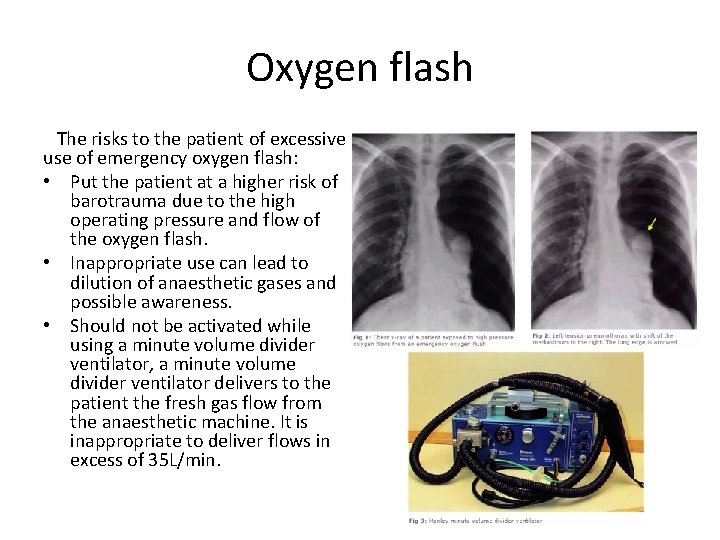
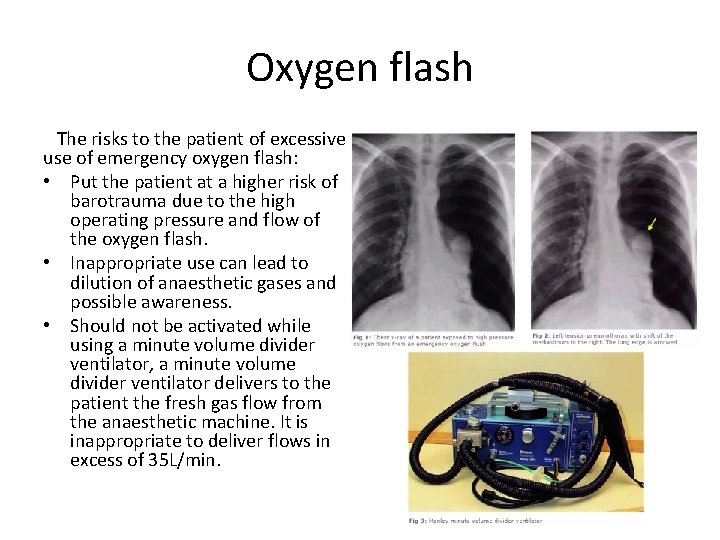
Oxygen flash The risks to the patient of excessive use of emergency oxygen flash: • Put the patient at a higher risk of barotrauma due to the high operating pressure and flow of the oxygen flash. • Inappropriate use can lead to dilution of anaesthetic gases and possible awareness. • Should not be activated while using a minute volume divider ventilator, a minute volume divider ventilator delivers to the patient the fresh gas flow from the anaesthetic machine. It is inappropriate to deliver flows in excess of 35 L/min.
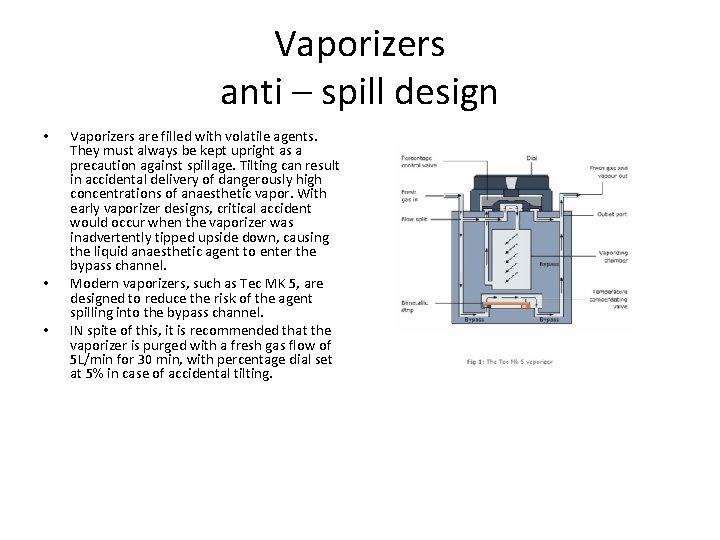
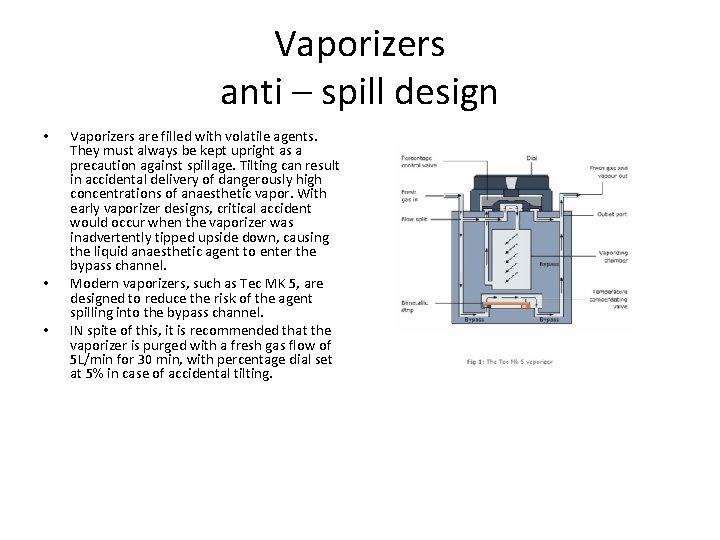
Vaporizers anti – spill design • • • Vaporizers are filled with volatile agents. They must always be kept upright as a precaution against spillage. Tilting can result in accidental delivery of dangerously high concentrations of anaesthetic vapor. With early vaporizer designs, critical accident would occur when the vaporizer was inadvertently tipped upside down, causing the liquid anaesthetic agent to enter the bypass channel. Modern vaporizers, such as Tec MK 5, are designed to reduce the risk of the agent spilling into the bypass channel. IN spite of this, it is recommended that the vaporizer is purged with a fresh gas flow of 5 L/min for 30 min, with percentage dial set at 5% in case of accidental tilting.
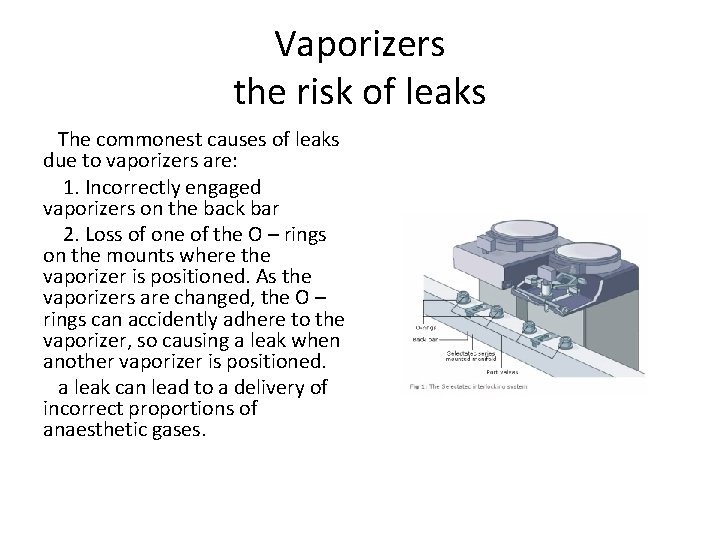
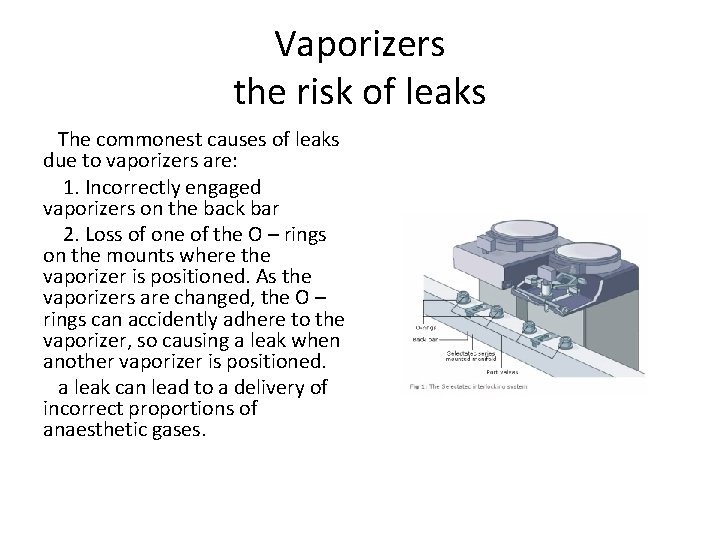
Vaporizers the risk of leaks The commonest causes of leaks due to vaporizers are: 1. Incorrectly engaged vaporizers on the back bar 2. Loss of one of the O – rings on the mounts where the vaporizer is positioned. As the vaporizers are changed, the O – rings can accidently adhere to the vaporizer, so causing a leak when another vaporizer is positioned. a leak can lead to a delivery of incorrect proportions of anaesthetic gases.
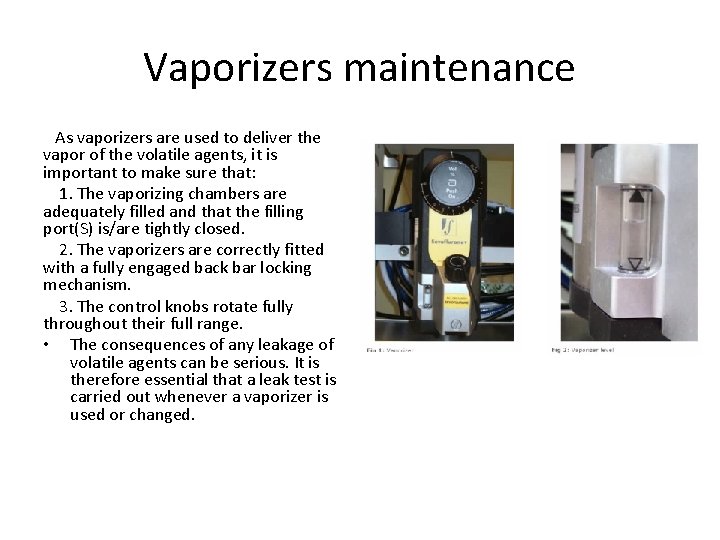
Vaporizers maintenance As vaporizers are used to deliver the vapor of the volatile agents, it is important to make sure that: 1. The vaporizing chambers are adequately filled and that the filling port(S) is/are tightly closed. 2. The vaporizers are correctly fitted with a fully engaged back bar locking mechanism. 3. The control knobs rotate fully throughout their full range. • The consequences of any leakage of volatile agents can be serious. It is therefore essential that a leak test is carried out whenever a vaporizer is used or changed.
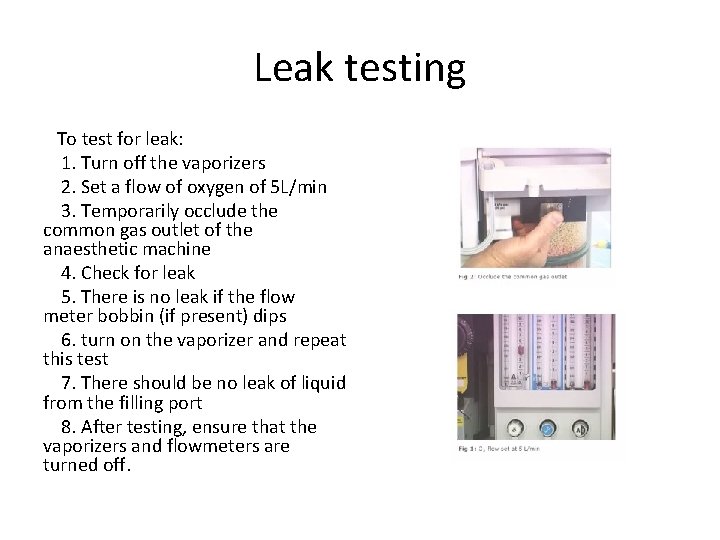
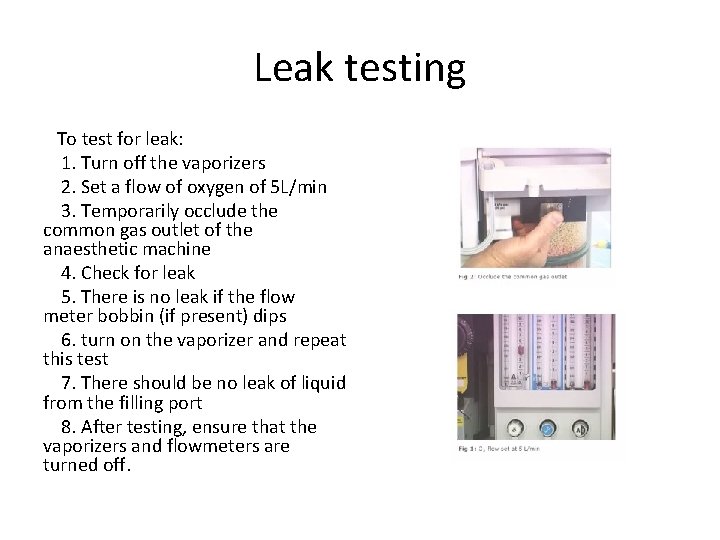
Leak testing To test for leak: 1. Turn off the vaporizers 2. Set a flow of oxygen of 5 L/min 3. Temporarily occlude the common gas outlet of the anaesthetic machine 4. Check for leak 5. There is no leak if the flow meter bobbin (if present) dips 6. turn on the vaporizer and repeat this test 7. There should be no leak of liquid from the filling port 8. After testing, ensure that the vaporizers and flowmeters are turned off.
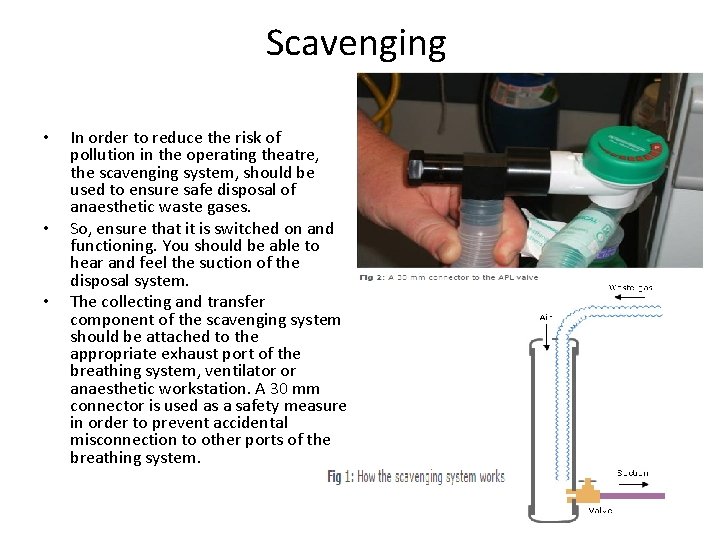
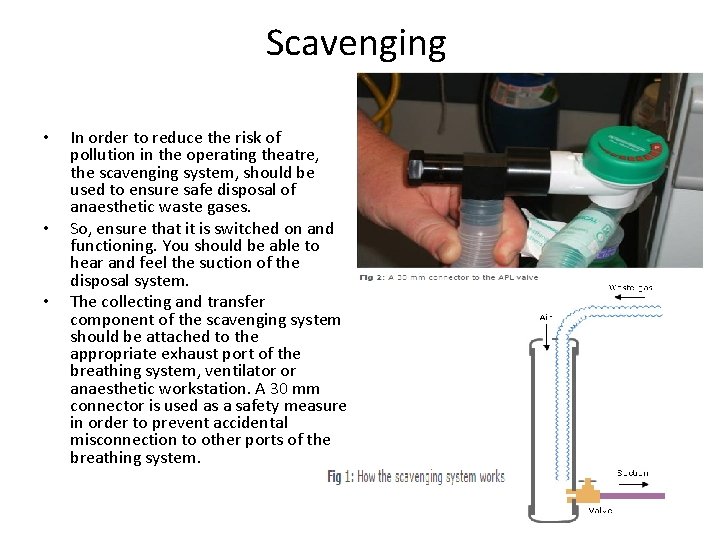
Scavenging • • • In order to reduce the risk of pollution in the operating theatre, the scavenging system, should be used to ensure safe disposal of anaesthetic waste gases. So, ensure that it is switched on and functioning. You should be able to hear and feel the suction of the disposal system. The collecting and transfer component of the scavenging system should be attached to the appropriate exhaust port of the breathing system, ventilator or anaesthetic workstation. A 30 mm connector is used as a safety measure in order to prevent accidental misconnection to other ports of the breathing system.
Suction equipment Functioning suction equipment is essential for safe conduct of anaesthesia. This allows secretions or vomitus to be suctioned away from the upper airway. To test the suction system: 1. Ensure that the vacuum probe is firmly engaged with its outlet and that all connection are secure 2. Switch on the suction and occlude the suction tubing. This is to test for the rapid development of an adequate negative pressure 3. A suction unit should take no longer than 10 S to generate a vacuum of 500 mm. Hg with a displacement of air of 25 L/min Ensure that the patient trolley, bed or operating table can be tilted head – down rapidly.
Ancillary equipment Airway management equipment should be checked next to ensure that each item of ancillary equipment required is available and functioning correctly. Ancillary equipment include: 1. Laryngoscopes 2. Intubation aids 3. Face masks, laryngeal masks, airways, tracheal tubes and connectors
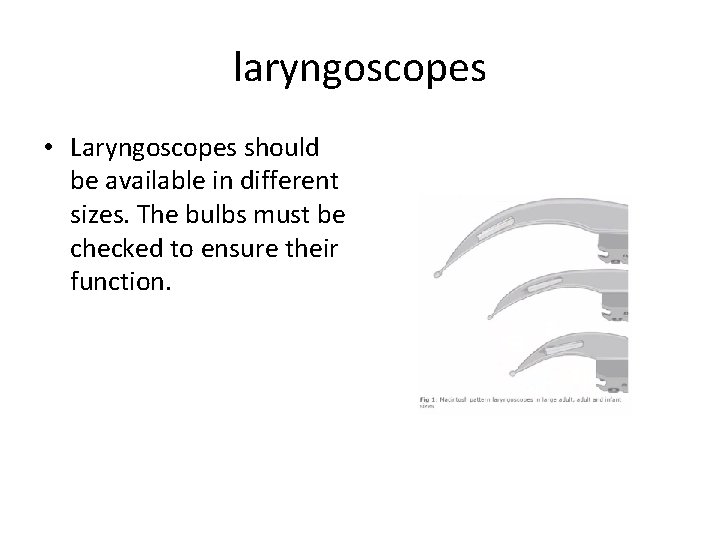
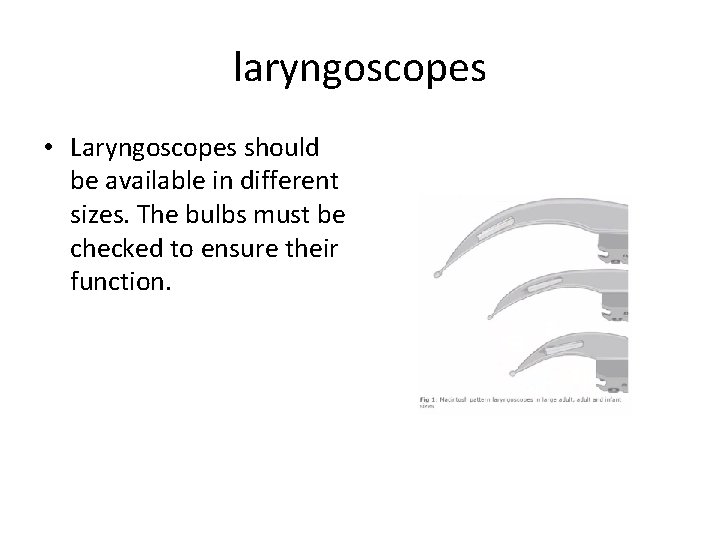
laryngoscopes • Laryngoscopes should be available in different sizes. The bulbs must be checked to ensure their function.
Intubation aids Several types of intubation aids may be required: intubation forceps, bougies, stylets, Magill forceps, etc.
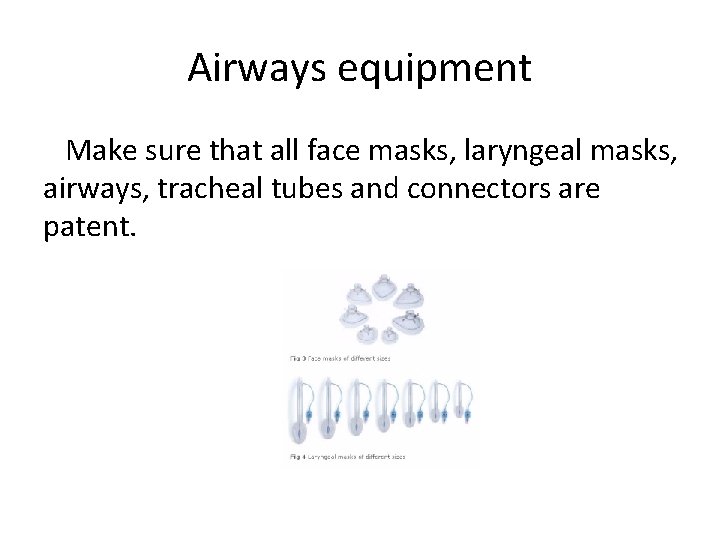
Airways equipment Make sure that all face masks, laryngeal masks, airways, tracheal tubes and connectors are patent.
Single use device In order to reduce the risk of cross - infection between patients, it is recommended that single – use equipment is used when possible. Single – use equipment will be marked with the symbol: It is recommended that when single – use equipment is used, the packing should not be removed until the point of use. This helps in infection control, identification and safety. It must be emphasized that any equipment that is designated single - use must be used for one patient only, and not re – used.
Back-Up Systems Some modern anaesthetic machines may default to little or no flow in the event of failure. In such situations, it is essential that an alternative oxygen supply and means of ventilation, such as a self-inflating bag, circuit and oxygen cylinder, must be available, and checked as functioning correctly with an adequate supply of oxygen. Alternative methods of maintaining anaesthesia in this situation should be available such as syringe pumps to administer total intravenous anaesthesia.
Record Keeping Each anaesthetic machine should have a log book in which check records are documented. The following checks should be accurately and systematically recorded: 1. Regular servicing of anaesthetic machine 2. Weekly oxygen failure alarm checks 3. Daily pre – session checks The anaesthetist should clearly document in the patients anaesthetic record that: 1. The anaesthetic machine check has been performed 2. Appropriate monitoring is in place and functional 3. The integrity, patency and safety of the whole breathing system has been assured Such documentation of the routine checking and regular servicing of anaesthetic machines, and patient breathing systems should be sufficient to permit routine auditing to be carried out a future time.
Session key points • • • Routine checking of equipment is essential in the safe delivery of anaesthetic care Ensure that you have turned on anaesthetic machine after connecting it to the mains supply Check the gas supply; both piped gases and cylinders Make sure that the monitoring equipment is working adequately Ensure that various components of the anaesthetic machine are functioning correctly – flowmeters, vaporizers, oxygen emergency flash, scavenging system and suction system. Also check for leaks Check the breathing system and its components Ensure the availability of different airway management devices When possible, use single – use devices In cases of anaesthetic machine failure, have available means of ventilation and administration of oxygen
Session summary Learning objectives: . Describe the tests performed in checking the anaesthetic equipment. Identify potential equipment malfunctions in anaesthetic practice. Recognize the design modifications of modern anaesthetic equipment to prevent such malfunction