Charge Description Master Charge Capture Enhancing Revenue and

- Slides: 51
Charge Description Master & Charge Capture –Enhancing Revenue and Compliance PREPARED FOR AMERICAN ASSOCIATION OF HEALTHCARE ADMINISTRATIVE MANAGEMENT – WI (AAHAM) OCTOBER 4, 2019

Disclaimer EBB Coding Solutions, Inc has prepared the following information based on current, available information as of the date of this presentation. Attendees should be aware that regulatory, coding, and billing information changes frequently and the information contained in these slides may become outdated quickly. This information is not intended to replace job specific training and should only be used as a reference after confirming the accuracy and applicability of the information based upon current published laws, statutes, regulations, and guidelines. Copyright 2019 EBB Coding Solutions, Inc. 2
Agenda 5 Takeaways 1. 2. 3. 4. 5. Anatomy of a Charge Description Master and Charge Capture Review – Illustration of. Best approach and how these reviews should be conducted – How we do it. Examples of findings for this year – what we see. How it impacts your compliance program and the significant risk to your organization. Impact on net hospital reimbursement. Copyright 2019 EBB Coding Solutions, Inc. 3
Objectives § § § Understand the importance of repeated internal & external Charge Description Master (CDM) and Charge Capture Reviews (CCR). Strategies for auditing and maintaining your CDM. How to conduct claim and medical record reviews (CCR) Recommended steps to mitigate risk and promote compliance. Understanding the extreme compliance risks to your organization. Remaining compliant while maximizing reimbursement. Copyright 2019 EBB Coding Solutions, Inc. 4
Importance of Regular CDM and Charge Capture Reviews Copyright 2019 EBB Coding Solutions, Inc. 5
Importance of Regular CDM and Charge Capture Reviews How often? CDM: Internal: Quarterly (as often as possible based on resources) External: No less than once per year Charge Capture Review: Internal: Continuous External: Quarterly – Best practice. Realistically – twice per year. Copyright 2019 EBB Coding Solutions, Inc. 6
Importance of Regular CDM and Charge Capture Reviews Cautions: § 1. Purchase of CDM Software: i. The purchase of CDM software falsely provides hospital administrators and users with a false sense of security. They believe that given the cost of the software that this will be all encompass everything that is needed to keep a pristine CDM. ii. If staff does not understand coverage rules – especially the complex outpatient billing, coding, rules and regulations – you will have many, compliance and reimbursement issues. Copyright 2019 EBB Coding Solutions, Inc. 7
Importance of Regular CDM and Charge Capture Reviews Cautions: § 1. Purchase of CDM Software (continued): iii. iv. A line by line analysis – with the actual provider of the service (department manager) is by far the best practice. Sorry – this is still a very manual, tedious process and always will be. Department Managers must have ownership of their CDM. Copyright 2019 EBB Coding Solutions, Inc. 8
Importance of Regular CDM and Charge Capture Reviews Cautions: § Ownership – Who? (No Silos!): 2. CDM/CCR: a. i. iii. iv. v. viii. Administration CDM Coordinator All Department Mangers Coding Patient Financial Services Finance Compliance Officer Revenue Cycle Committee Copyright 2019 EBB Coding Solutions, Inc. 9
Importance of Regular CDM and Charge Capture Reviews Cautions (continued): § Timing: 3. a. b. c. d. Belief that an external CDM review be completed every 3 years. Annual - if ever - external Charge Capture/Coding Reviews? Without continuous reviews – we have found that most department Administrator and Department Managers believe that everything is “OK”. Not true! And will be illustrated later. Ongoing internal/external assessment and feedback are necessary FOR EVERYONE to best capture all revenue possible and keep you compliant in the process. Copyright 2019 EBB Coding Solutions, Inc. 10
Importance of Regular CDM and Charge Capture Reviews § Missing common services, supplies and procedures ü ü Regular communications with department personnel is critical for purposes of identifying procedures, services and supplies that are commonly provided but are not included in the chargemaster and charge capture activities and policies. Your clinical department staff is the best source of information you have when it comes to identifying potential lost revenues or revenue opportunities. Copyright 2019 EBB Coding Solutions, Inc. 11
Importance of Regular CDM and Charge Capture Reviews § The impact of the CDM & CCR on portions of the revenue cycle is immeasurable. A inaccurate/incomplete CDM can cause countless errors on the claim and lack of ongoing CCR’s impacts those areas of the revenue cycle mentioned. Every batch of claims sent daily to payors, may have or lead to: Inaccurate CPT/HCPCS reporting Incorrect unit reporting Incomplete claims Overstating claims Inaccurate descriptions - services provided - mis-represented on the claim Incorrect charges – both over and under reporting Potential compliance issues – submission of false claims Increased rejections & denials Possibility of more frequent audits Increased Additional Development Requests (ADR) Patient satisfaction? Increased Write – offs? Copyright 2019 EBB Coding Solutions, Inc. 12
Importance of Regular CDM and Charge Capture Reviews § There a variety of errors that are commonly seen within a chargemaster and charge capture review. The types of errors most commonly noted include: ü Deleted/invalid CPT/HCPCS codes ü CPT/HCPCS description errors ü Unit errors ü Pricing errors ü Hard-coded modifiers ü Missing common services/procedures ü Revenue code errors ü Payor specific coding requirements ü Lack of supporting documentation ü Lack of understanding of complex coverage & regulatory requirements ü Other issues Copyright 2019 EBB Coding Solutions, Inc. 13
– How we do it Refer to Spreadsheets – Present: – “Charge Description Master Review Example of” & Charge Capture Review – Data Gathering with Examples – AAHAM”. 14 Copyright 2019 EBB Coding Solutions, Inc. Anatomy of a Charge Description Master and Charge Capture Review – Illustration of
Examples of findings – what we see § Unit errors ü Unit reporting errors can be responsible for both lost revenue and increased compliance risk. • CPT/HCPCS descriptions may indicate the service(s) should be reported for each additional. • Failure to include these important descriptors within your chargemaster can lead to frequent coding errors. Found during a CCR: o o o CPT 26600 - Closed treatment of metacarpal fracture; without manipulation, each bone Patient undergoes closed treatment of 3 separate metacarpal fractures. The service was reported as 26600 x 1. i. CDM description did not include the term each The service should have been reported as 26600 x 3. Lost revenue of at least $344 for one encounter. Copyright 2019 EBB Coding Solutions, Inc. 15
Examples of findings – what we see § Unit errors ü High volumes of errors related to reporting of drug units • • • Multiple published audits by the OIG focused on improper drug unit reporting. Units in the chargemaster are commonly set based on manufacturer information rather than the HCPCS reporting descriptions. Examples to follow at the end of this presentation. Units in the chargemaster also assume that waste will be appropriately documented and separately reportable. Copyright 2019 EBB Coding Solutions, Inc. 16
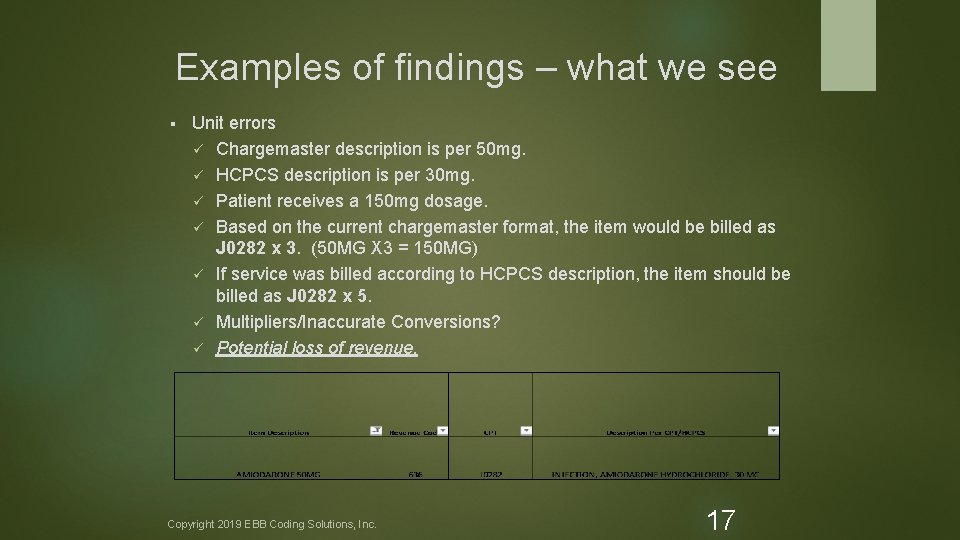
Examples of findings – what we see § Unit errors ü Chargemaster description is per 50 mg. ü HCPCS description is per 30 mg. ü Patient receives a 150 mg dosage. ü Based on the current chargemaster format, the item would be billed as J 0282 x 3. (50 MG X 3 = 150 MG) ü If service was billed according to HCPCS description, the item should be billed as J 0282 x 5. ü Multipliers/Inaccurate Conversions? ü Potential loss of revenue. Copyright 2019 EBB Coding Solutions, Inc. 17
Examples of findings – what we see § Unit errors ü Chargemaster description is per 1 mg. ü HCPCS description is per 250 mg. ü Patient receives a 500 mg dosage. ü Based on the current chargemaster format, and as noted in a CCR, the item would be billed as J 0696 x 500. ü If service was billed according to HCPCS description, the item would be billed as J 0696 x 2. ü Potential overpayment and compliance risk. Copyright 2019 EBB Coding Solutions, Inc. 18
Examples of findings – what we see § Pricing errors ü Careful consideration to pricing should be given when reviewing a chargemaster. ü Many factors to consider when assigning charges to services: • Payor mix/contracts • Market conditions • Geographic competitiveness • Costs • Profitability Copyright 2019 EBB Coding Solutions, Inc. 19
Examples of findings – what we see § Pricing errors ü ü ü Most payors reimburse providers based on the lesser of the charge or allowed amount. Most non-government payors’ reimbursement rates are higher than Medicare. Analysis should be performed to ensure charges are set at least 150% above the current Medicare reimbursement rates. Attention should also be given to ensure prices are reasonable and not “excessive”. We recommend charges under 110% and over 400% of the Medicare OPPS reimbursement be reviewed. Copyright 2019 EBB Coding Solutions, Inc. 20
Examples of findings – what we see Pricing errors ü A standardized, thoughtful approach to evaluating and assigning prices should be utilized. ü Prices should be uniform across all payors. • You cannot charge a non-government payor less than what you charge a government payor for the same service. ü Prices should be uniform across the same services. • You should not charge more for a 2 view x-ray of the right hip than you charge for a 2 view x-ray of the left hip. Copyright 2019 EBB Coding Solutions, Inc. 21
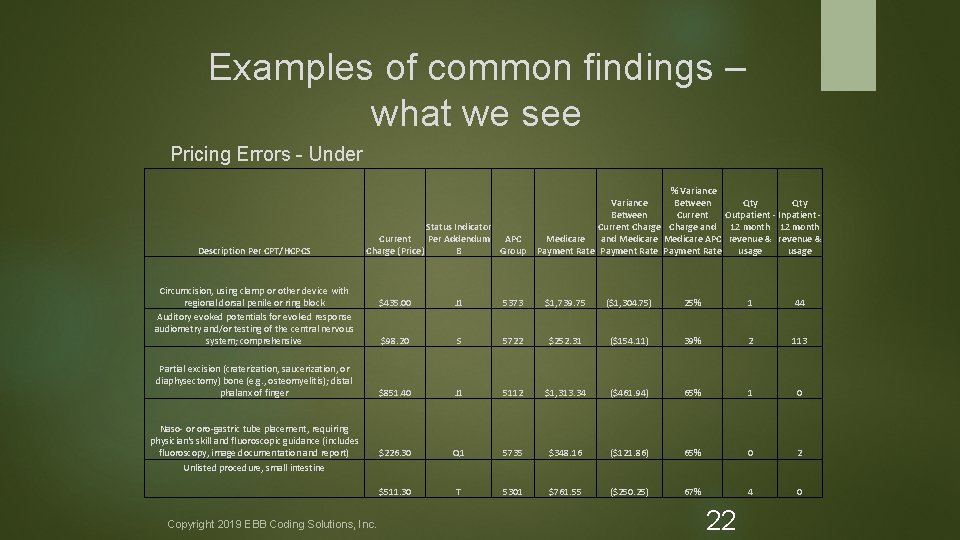
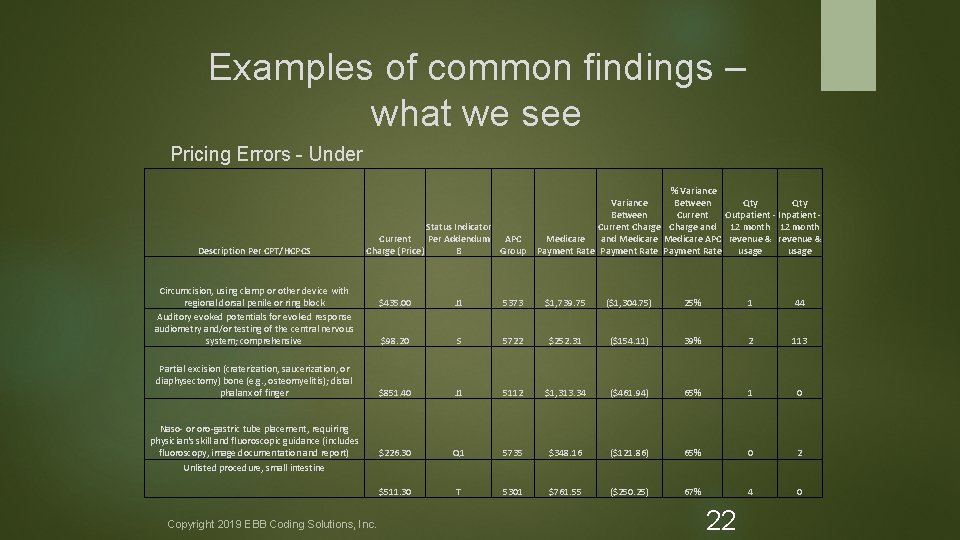
Examples of common findings – what we see Pricing Errors - Under Description Per CPT/HCPCS Status Indicator Current Per Addendum APC Charge (Price) B Group Circumcision, using clamp or other device with regional dorsal penile or ring block Auditory evoked potentials for evoked response audiometry and/or testing of the central nervous system; comprehensive Partial excision (craterization, saucerization, or diaphysectomy) bone (e. g. , osteomyelitis); distal phalanx of finger Naso- or oro-gastric tube placement, requiring physician's skill and fluoroscopic guidance (includes fluoroscopy, image documentation and report) Unlisted procedure, small intestine Copyright 2019 EBB Coding Solutions, Inc. % Variance Between Qty Between Current Outpatient - Inpatient Current Charge and 12 month Medicare and Medicare APC revenue & Payment Rate usage $435. 00 J 1 5373 $1, 739. 75 ($1, 304. 75) 25% 1 44 $98. 20 S 5722 $252. 31 ($154. 11) 39% 2 113 $851. 40 J 1 5112 $1, 313. 34 ($461. 94) 65% 1 0 $226. 30 Q 1 5735 $348. 16 ($121. 86) 65% 0 2 $511. 30 T 5301 $761. 55 ($250. 25) 67% 4 0 22
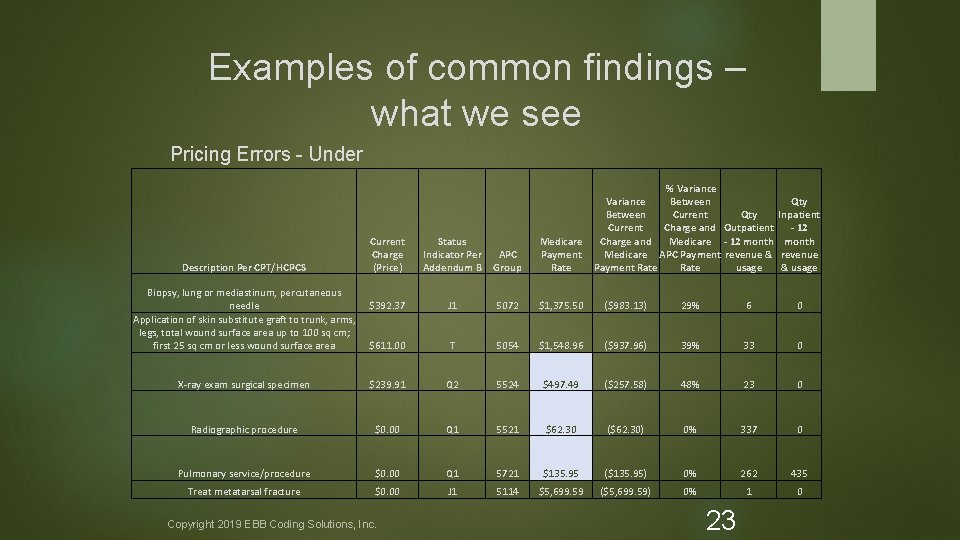
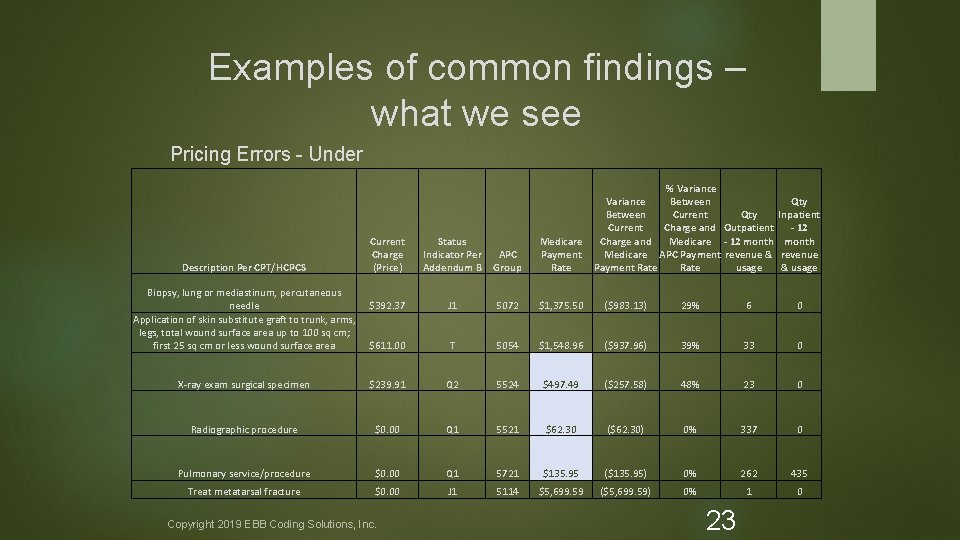
Examples of common findings – what we see Pricing Errors - Under % Variance Between Qty Between Current Charge and Outpatient Charge and Medicare - 12 month Medicare APC Payment revenue & Payment Rate usage Qty Inpatient - 12 month revenue & usage Current Charge (Price) Status Indicator Per Addendum B APC Group Medicare Payment Rate $392. 37 J 1 5072 $1, 375. 50 ($983. 13) 29% 6 0 $611. 00 T 5054 $1, 548. 96 ($937. 96) 39% 33 0 X-ray exam surgical specimen $239. 91 Q 2 5524 $497. 49 ($257. 58) 48% 23 0 Radiographic procedure $0. 00 Q 1 5521 $62. 30 ($62. 30) 0% 337 0 Pulmonary service/procedure $0. 00 Q 1 5721 $135. 95 ($135. 95) 0% 262 435 Treat metatarsal fracture $0. 00 J 1 5114 $5, 699. 59 ($5, 699. 59) 0% 1 0 Description Per CPT/HCPCS Biopsy, lung or mediastinum, percutaneous needle Application of skin substitute graft to trunk, arms, legs, total wound surface area up to 100 sq cm; first 25 sq cm or less wound surface area Copyright 2019 EBB Coding Solutions, Inc. 23
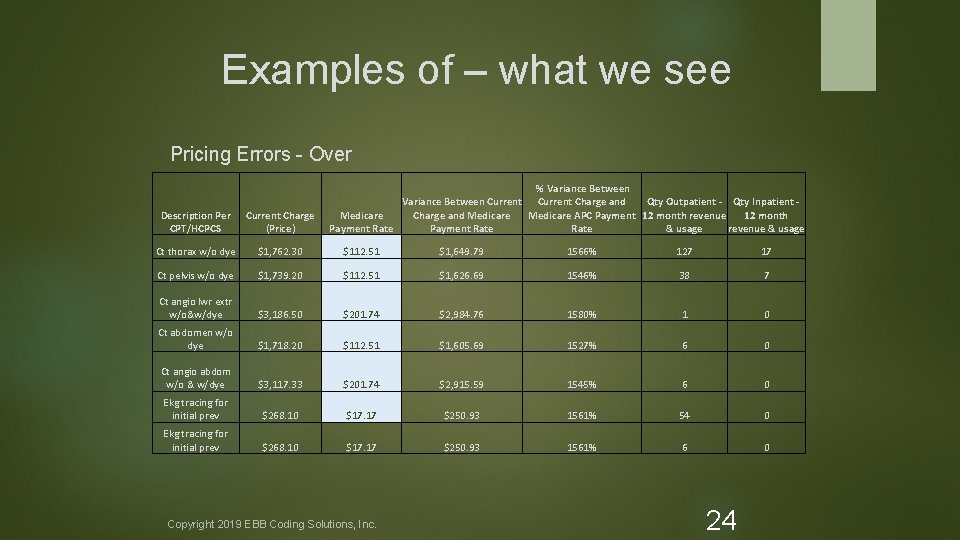
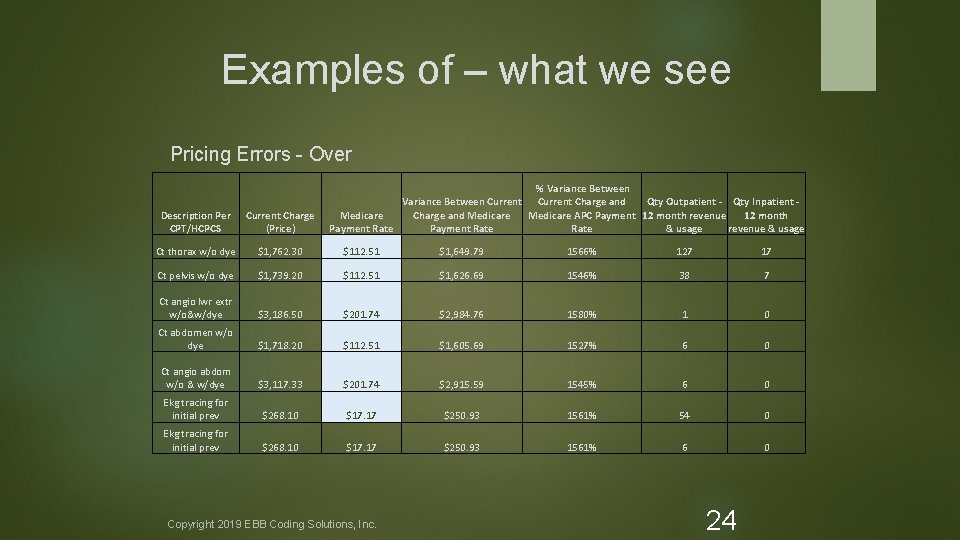
Examples of – what we see Pricing Errors - Over % Variance Between Current Charge and Qty Outpatient - Qty Inpatient Charge and Medicare 12 month Medicare APC Payment 12 month revenue Payment Rate & usage revenue & usage Description Per CPT/HCPCS Current Charge (Price) Ct thorax w/o dye $1, 762. 30 $112. 51 $1, 649. 79 1566% 127 17 Ct pelvis w/o dye $1, 739. 20 $112. 51 $1, 626. 69 1546% 38 7 Ct angio lwr extr w/o&w/dye $3, 186. 50 $201. 74 $2, 984. 76 1580% 1 0 Ct abdomen w/o dye $1, 718. 20 $112. 51 $1, 605. 69 1527% 6 0 Ct angio abdom w/o & w/dye $3, 117. 33 $201. 74 $2, 915. 59 1545% 6 0 Ekg tracing for initial prev $268. 10 $17. 17 $250. 93 1561% 54 0 Ekg tracing for initial prev $268. 10 $17. 17 $250. 93 1561% 6 0 Copyright 2019 EBB Coding Solutions, Inc. 24
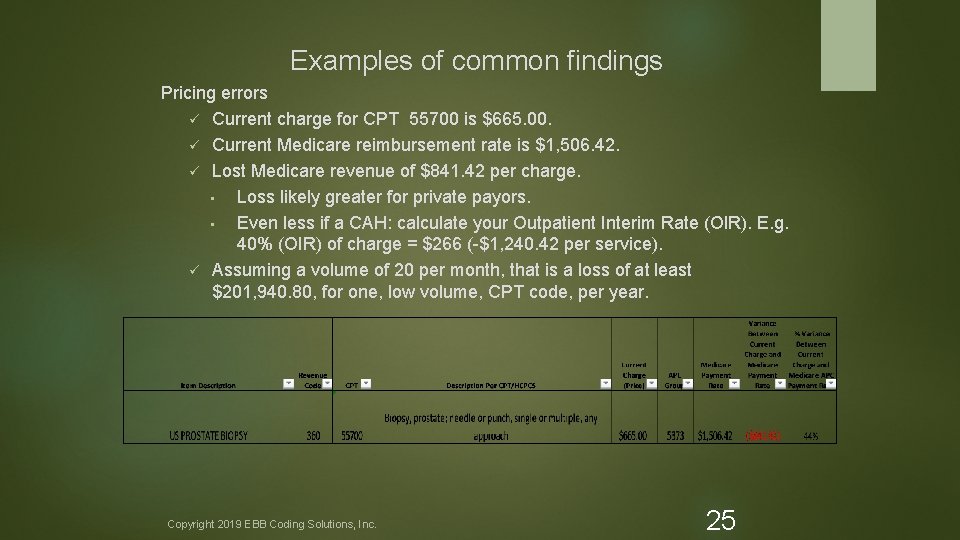
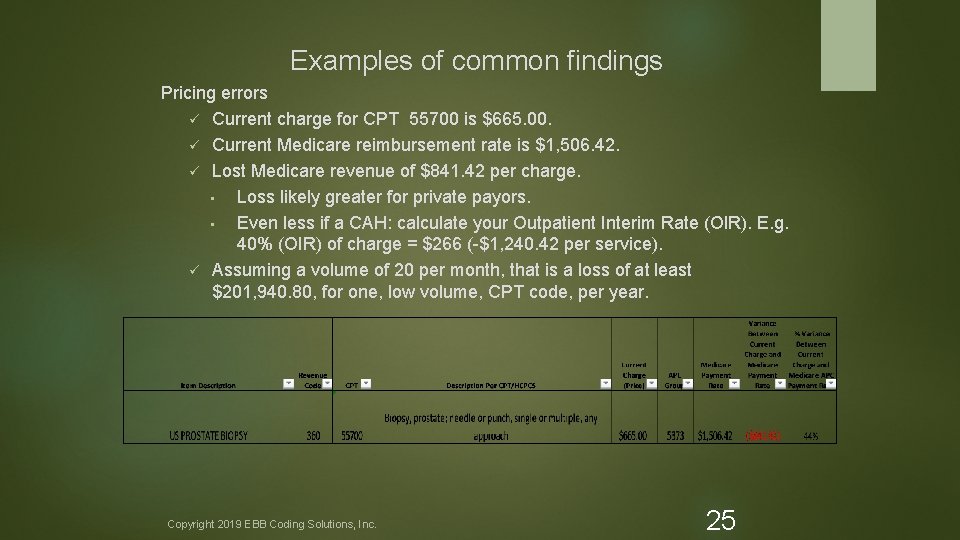
Examples of common findings Pricing errors ü Current charge for CPT 55700 is $665. 00. ü Current Medicare reimbursement rate is $1, 506. 42. ü Lost Medicare revenue of $841. 42 per charge. • Loss likely greater for private payors. • Even less if a CAH: calculate your Outpatient Interim Rate (OIR). E. g. 40% (OIR) of charge = $266 (-$1, 240. 42 per service). ü Assuming a volume of 20 per month, that is a loss of at least $201, 940. 80, for one, low volume, CPT code, per year. Copyright 2019 EBB Coding Solutions, Inc. 25
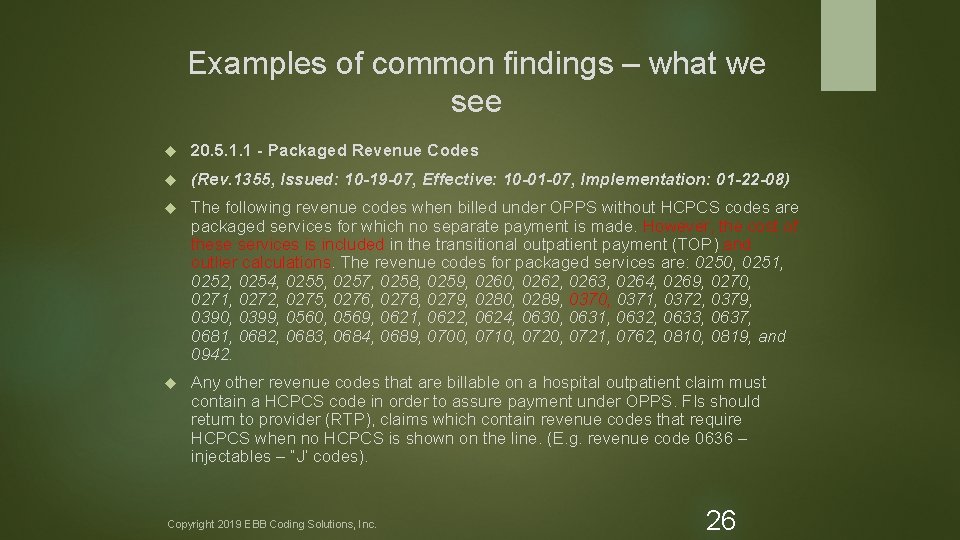
Examples of common findings – what we see 20. 5. 1. 1 - Packaged Revenue Codes (Rev. 1355, Issued: 10 -19 -07, Effective: 10 -01 -07, Implementation: 01 -22 -08) The following revenue codes when billed under OPPS without HCPCS codes are packaged services for which no separate payment is made. However, the cost of these services is included in the transitional outpatient payment (TOP) and outlier calculations. The revenue codes for packaged services are: 0250, 0251, 0252, 0254, 0255, 0257, 0258, 0259, 0260, 0262, 0263, 0264, 0269, 0270, 0271, 0272, 0275, 0276, 0278, 0279, 0280, 0289, 0370, 0371, 0372, 0379, 0390, 0399, 0560, 0569, 0621, 0622, 0624, 0630, 0631, 0632, 0633, 0637, 0681, 0682, 0683, 0684, 0689, 0700, 0710, 0721, 0762, 0810, 0819, and 0942. Any other revenue codes that are billable on a hospital outpatient claim must contain a HCPCS code in order to assure payment under OPPS. FIs should return to provider (RTP), claims which contain revenue codes that require HCPCS when no HCPCS is shown on the line. (E. g. revenue code 0636 – injectables – “J’ codes). Copyright 2019 EBB Coding Solutions, Inc. 26
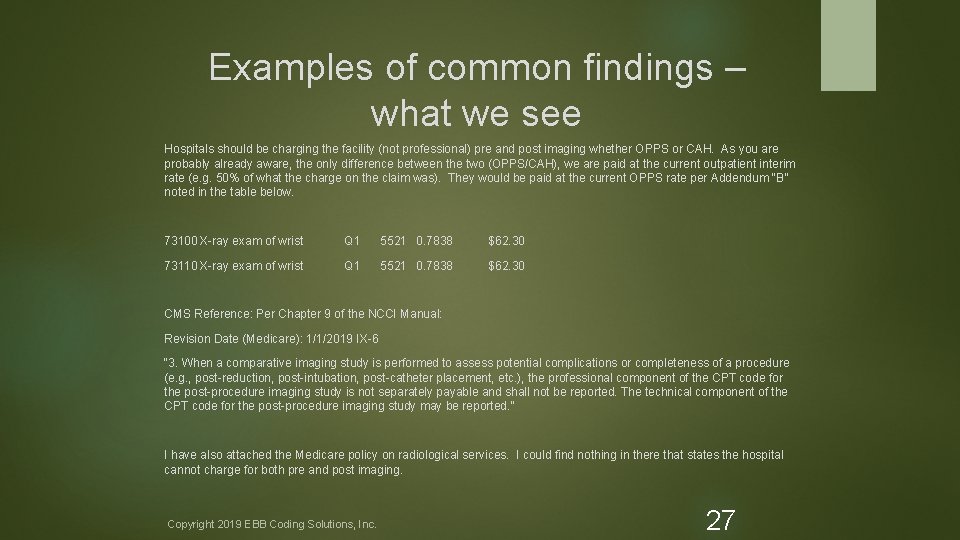
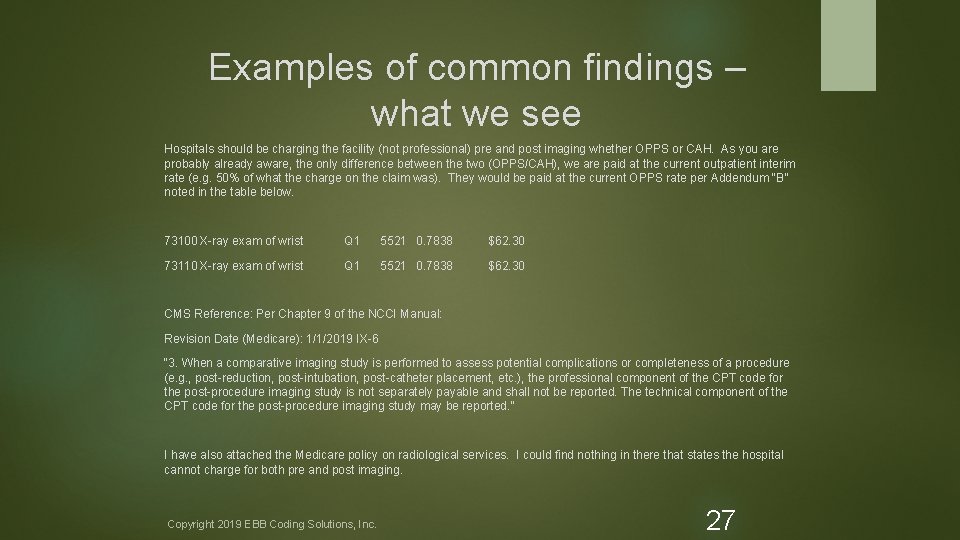
Examples of common findings – what we see Hospitals should be charging the facility (not professional) pre and post imaging whether OPPS or CAH. As you are probably already aware, the only difference between the two (OPPS/CAH), we are paid at the current outpatient interim rate (e. g. 50% of what the charge on the claim was). They would be paid at the current OPPS rate per Addendum “B” noted in the table below. 73100 X-ray exam of wrist Q 1 5521 0. 7838 $62. 30 73110 X-ray exam of wrist Q 1 5521 0. 7838 $62. 30 CMS Reference: Per Chapter 9 of the NCCI Manual: Revision Date (Medicare): 1/1/2019 IX-6 “ 3. When a comparative imaging study is performed to assess potential complications or completeness of a procedure (e. g. , post-reduction, post-intubation, post-catheter placement, etc. ), the professional component of the CPT code for the post-procedure imaging study is not separately payable and shall not be reported. The technical component of the CPT code for the post-procedure imaging study may be reported. ” I have also attached the Medicare policy on radiological services. I could find nothing in there that states the hospital cannot charge for both pre and post imaging. Copyright 2019 EBB Coding Solutions, Inc. 27
Examples of common findings – what we see • “A: CPT code 94640 can only be reported once during an episode of care regardless of the number of separate inhalation treatments that are administrated. Inhaled medication can be reported separately. The date of service would be the date the patient received the first treatment. Q: Is it correct that since providers are to report only one unit of 94640 per episode of care, providers should also charge for only one unit regardless of the number of inhalation treatments provided during the episode of care? If that is correct, please provide the authoritative citation for charging as if only one treatment had been provided. The cost to provide multiple inhalation treatments during an episode of care is not the same as the cost to provide one inhalation treatment. • A: The actual charge for the line would be the cost for all the services provided. For example, if you provide 5 treatments and each is $25 the total billed would be is $125, but the units are 1. The method of reimbursement is set per CMS. ” Copyright 2019 EBB Coding Solutions, Inc. 28
PPS/CAH Reimbursement and Impact of CDM & Charge Capture PPS Supply Reimbursement PPS hospitals are currently not reimbursed by Medicare for non-routine supplies when reported on the claim form unless a HCPCS code is available and has a payment rate assigned (e. g. prosthetics/orthotics). Most supplies are bundled into the cost of the service or procedure. Although Medicare may not pay for most non-routine supplies, it is collecting data on every claim submitted that may impact the PPS hospitals RCC (Ratio to Cost of Charges) and cost report data. For commercial payors that pay a percent of gross charges, it is critical to continue reporting supplies in order to capture net reimbursement. These must be incorporated into the CDM. Copyright 2019 EBB Coding Solutions, Inc. 29
PPS/CAH Reimbursement and Impact of CDM & Charge Capture CAH Supply Reimbursement Inpatient: A set daily payment rate for inpatient services is paid by Medicare to a CAH. Reporting non-routine supplies on the inpatient claim is important and may impact future inpatient rates paid to the hospital. For commercial payors, total gross charges may also impact reimbursement if paid by a percent of charges. Outpatient Services: An outpatient interim rate (OIR) is calculated several times per year based on claim information received by Medicare from the CAH. For example, if the OIR is 40% for a facility, if the claim total is a charge for $100, the net reimbursement for that claim will be $40. Copyright 2019 EBB Coding Solutions, Inc. 30
PPS/CAH Reimbursement and Impact of CDM & Charge Capture CAH Supply Reimbursement It is critical that all hospitals (especially CAH) report all non-routine supplies in the CDM and on the claim form to be certain they are getting these costs reported on the PS&R data to the MAC. This has an enormous impact on future payments by Medicare and may have an immediate impact on commercial payments. Copyright 2019 EBB Coding Solutions, Inc. 31
Prosthetic/Orthotic in the CDM & Claims Reviews Prosthetics/Orthotic in the CDM: There is a common misconception that prosthetics/orthotics are “DME”. Although they are a sub-component of DME they have actual OPPS payment rates assigned within the prosthetic/orthotic fee schedule that is reimbursed. It may or may not include fitting and adjustment. Services provided will have to either be bundled or unbundled depending on the HCPCS description. These are typically excluded from the CDM and never captured. Patients are often billed for these items erroneously – out of pocket. Copyright 2019 EBB Coding Solutions, Inc. 32
Prosthetic/Orthotic in the CDM & Claims Reviews Example: These items are commonly missed and never reported or implemented in the CDM. In addition, many hospitals believe they are “bundled” and should not be reported on the claim which is incorrect. Per the AMA HCPCS Level II 2019 Professional Edition Manual (page 334): “Knee- ankle-foot orthosis, fracture orthosis, femoral fracture cast orthosis, thermoplastic type casting material, custom fabricated” (KAFO). The correct HCPCS must be reported with is“L 2126”and revenue code 0274. Per the Medicare “Durable Medical Equipment Prosthetic Orthotic”(DMEPOS) revised “ 2019 Fee Schedule” the payment rate for this item is $1, 267. 80. Because “fitting and adjustment” is not stated with “L 2126”, you may also bill CPT 97760 “Orthotic(s) management and training (including assessment and fitting when not otherwise reported), upper extremity(s), lower extremity(s) and/or trunk, each 15 min. Also, see CPT 97763 for 2019. Copyright 2019 EBB Coding Solutions, Inc. 33
How it impacts your compliance program and the significant risk to your organization Copyright 2019 EBB Coding Solutions, Inc. 34
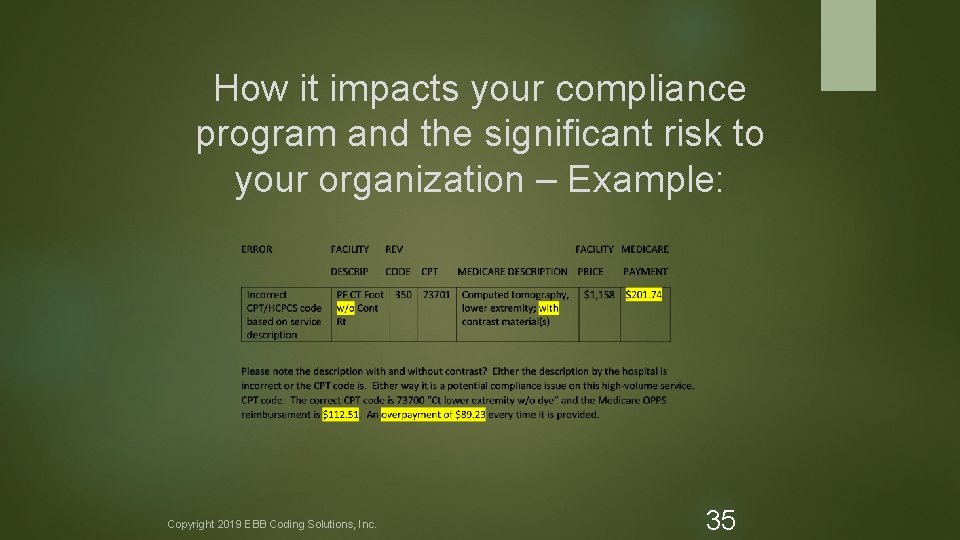
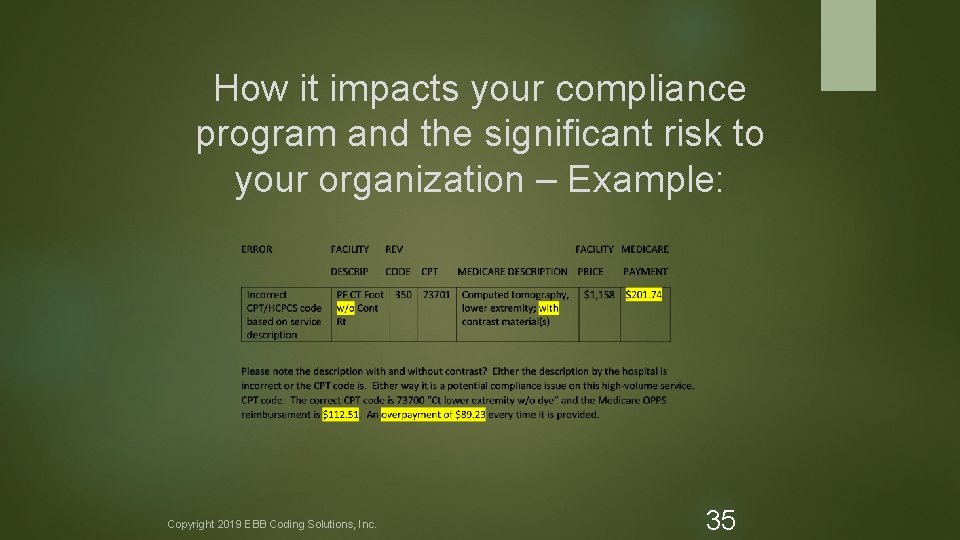
How it impacts your compliance program and the significant risk to your organization – Example: Copyright 2019 EBB Coding Solutions, Inc. 35
Examples of common findings – what we see - Compliance Other issues ü ü Some providers have programmed their chargemaster with “exploding” charges. There are significant compliance risks associated with exploding charges. The OIG has identified this practice as fraud. • • ü Charging for services not ordered. Charging for services not performed. For example: • • Pathology selects the chargemaster item for a surgical pathology examination (CPT 88305). The system automatically adds the following codes: o o 88311 - pathology consult, frozen section during surgery 88311 - decalcification procedure 88312 - Group 1, special stain 88313 - Group 2, special stain Copyright 2019 EBB Coding Solutions, Inc. 36
How it impacts your compliance program and the significant risk to your organization – Example: § Using an Independent Review Organization (IRO) is typically more objective and effective than internal reviews. Staff members do not like to admit they have made a mistake(s) or point a finger at a peer with regard to coding and charge capture. We typically see some staff go into a defensive posture or will try to undermine the external review results. Simply because this may reflect poorly on them. § With the findings from external reviews, staff fear reprisals of a poor annual review, probation or even job termination. § DO NOT TAKE THIS PERSONAL. THIS IS COMPLICATED STUFF! Compliance, reimbursement and the overall good of the hospital depends on it. Copyright 2019 EBB Coding Solutions, Inc. 37
How it impacts your compliance program and the significant risk to your organization – Example: Hard-coded modifiers ü ü ü ü The appropriate use of payment modifiers like modifiers 25 and 59 should only be applied by the coding department, when the use of the modifier is supported by the medical record documentation. Inappropriate use of modifiers 25 and 59 have been a long-standing focus area of the OIG. See -59 2018 Update at: https: //www. cms. gov/Outreach-and-Education/Medicare-Learning-Network. MLN/MLNMatters. Articles/Downloads/se 1418. pdf Including hard-coded payment modifiers within the chargemaster leads to significantly increased potential for improper claims, payments and increased compliance risk. Copyright 2019 EBB Coding Solutions, Inc. 38
Compliance Recommendations CDM § § Restrict chargemaster modification access to a limited number of individuals (2 -3) that have undergone appropriate training. Develop formal policies and procedures for requesting and making interim modifications to the chargemaster. The policies and procedures should require a two-fold confirmation process before changes are made. The policies and procedures should also require claims testing to confirm changes are reflected accurately on claims. Any changes should be communicated with affected staff. Copyright 2019 EBB Coding Solutions, Inc. 39
Compliance Recommendations CCR The results of the CCR must be shared with the area reviewed. Customized education must be provided based on findings. § Follow-up reviews where errors were originally identified must take place. § Any compliance issues identified must be dealt with immediately. § § § Corrections made Claim adjustments for any overpayment if still within timely filing If not, repayment back to payor Medicare allows up to a 5% error rate. These reviews are an allowable cost on the Medicare cost report and expected for any good compliance program. Not conducting regular reviews will be frowned upon by the Government (this is why it is an allowable expense on the cost report). Copyright 2019 EBB Coding Solutions, Inc. 40
Compliance - Strategies for Auditing/Maintaining § § § If your organization does not have the resources to conduct quarterly audits, or to review the entire chargemaster on a quarterly basis, audits should be conducted no less than on an annual basis. 30 record Charge Capture Reviews done NLT per quarter (combination of internal/external – hospital size dependent). Chargemaster software alone is not enough. If you don’t have the resources in-house, outsource to an external organization. Annual reviews by an external source is strongly recommended and is an allowable cost on the Medicare Cost Report. Copyright 2019 EBB Coding Solutions, Inc. 41
Compliance - Strategies for Auditing/Maintaining Prioritize the project, if necessary, to make it more manageable. ü Known high risk departments • Pharmacy ü Known payment risks • Hard coded modifiers ü High volume departments Supplies – not reported – due to bundling ü High volume procedures ü High volume denials Copyright 2019 EBB Coding Solutions, Inc. 42
Compliance - Strategies for Auditing/Maintaining Looking at the chargemaster in isolation is also not enough. ü ü ü Compare to CMS statistics Compare to CPT and HCPCS updates Department feedback Medical record documentation Claims data Is the data populating the claim the way you anticipated? ü ü Claims denials Conduct regular claim and documentations reviews (Charge Capture) Copyright 2019 EBB Coding Solutions, Inc. 43
Recommendations § § Assign a dedicated team of individuals that are responsible and accountable for the accuracy and completeness of your chargemaster and claims. The chargemaster & charge capture team/committee should include: ü ü ü Certified coders Billing staff Clinical personnel representing each department IT Finance Copyright 2019 EBB Coding Solutions, Inc. 44
Recommendations § Develop formal policies and procedures that outline the frequency and process for conducting chargemaster and charge capture reviews. ü Remember codes (hundreds!!) change every January 1 st and every quarter throughout the year thereafter. • ü The policies and procedures should also address the process for validating and implementing recommendations in a timely manner and outline a process for confirming updates are accurately reflected. • • ü Quarterly reviews are preferred. QA process Claims testing There should also be a formal process for providing Customized education and training (relevant & meaningful) to each department affected by the revisions. Copyright 2019 EBB Coding Solutions, Inc. 45
Client – CDM Review Report Summary Copyright 2019 EBB Coding Solutions, Inc. 46
Client – CDM Review Report Summary
CDM Review Note § These are the results of a CDM review provided for a 25 bed Critical Access Hospital (CAH) in 2019. § This client had a CDM review done, by another firm, in 2015. § We have provided this to you, to illustrate the extreme importance of having, an external review done at least annually. Copyright 2019 EBB Coding Solutions, Inc. 48
Open Discussion Copyright 2019 EBB Coding Solutions, Inc. 49
Thank You! Copyright 2019 EBB Coding Solutions, Inc. 50
Timothy P. Eaton MBA, Major–US Army (Retired), COC (CPC – H) President EBB Coding Solutions, Inc. S 64 W 37838 Hwy ZZ Eagle, WI 53119 (262) 443 -0265 teaton@ebbcsi. com EBBCSI. COM PREPARED FOR AMERICAN ASSOCIATION OF HEALTHCARE ADMINISTRATIVE MANAGEMENT – WI (AAHAM) OCTOBER 4, 2019