Chapter three Syphilis Serology Acknowledgements Addis Ababa University
Chapter three Syphilis Serology

Acknowledgements Addis Ababa University Jimma University Hawassa University Haramaya University of Gondor American Society for clinical Pathology Center for Disease Control and Prevention Ethiopia
Learning objective § At the end of this chapter, the students should be able to: § Describe the etiology and sign and symptoms of primary, secondary, latent and late (tertiary) syphilis § Discuss the principle and clinical applications of the qualitative and quantitative VDRL procedure and RPR card test § Describe specific and non specific Treponemal antibodies
Outline 3. 1. Introduction 3. 2. The stage of syphilis 3. 3. Immune response 3. 4. Diagnosis of syphilis 3. 5. Serological technique 3. 6. Serological technique
3. 1. Introduction Definition Primary chancre is a stage syphilis appears at the site of inoculation, initially painless papule that quickly erodes and becomes indurated
3. 1. Introduction § Reported in the medical literature as early as 1495. § In 1905 it was discovered that syphiluis was caused by a spirochete type of bacteria, § T. pallidum (originally called spirochaeta pallida). § The first diagnostic blood test, the Wassermann test, was developed in 1906.
3. 1. Introduction § Syphilis is a chronic systemic disease, which leads to lesions on the body. § It is derived from a Greek word "syphilos" meaning crippled, maimed (heart victim).
3. 1. Introduction § Is a systematic infection caused by the spirochate Treponema pallidium § Transmitted by: § Mainly Sexual contact (Venereal syphilis) § Less commonly via the placenta (congenital syphilis) OR § By accidental inoculation from infectious material e. g. fresh blood transfusion
3. 1. Introduction § Hours to days after penetrates intact mucosa or abraded skin travel via lymphatic's to general circulation and disseminates throughout body (all organs including CNS) § Incubation period directly proportional to size of inoculums § Host has immune response resulting inflammation responsible for clinical manifestation

3. 2. Stages of syphilis Infection with T. pallidium Primary Syphilis Primary Chancre Secondary Syphilis Secondary lesions 40% Relapse 60% Latent Syphilis Tertiary Syphilis Gumma (5 Yrs) Trans placental Transmission Persistent Asymptomatic Cardiovascular Tabes Dorsalis Syphilis (20 Yrs) (10 -15 Yrs) Congenital Syphilis

3. 2. Stages of syphilis Primary chancre § Appears at the site of inoculation, initially painless papule that quickly erodes and becomes indurated § Appears as a hard erythematus nodule about 1 cm in diameter with regional lymph node enlarged. § Persists for some weeks and heals § In women it commonly develops in the vulva or cervix § In HIV-infected patients, may see multiple or atypical chancres, or no primary lesion
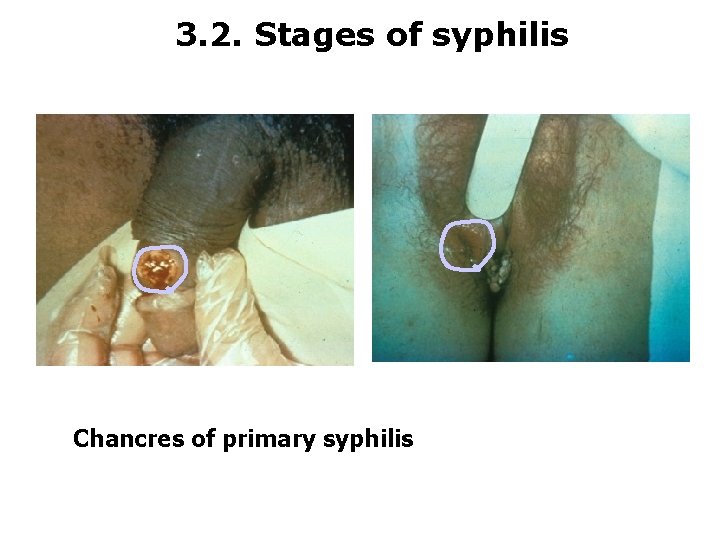
3. 2. Stages of syphilis Chancres of primary syphilis

3. 2. Stages of syphilis Secondary syphilis § Always wide spread erythematus skin about 1 cm in diameter with regional lymph node enlarged. § Ulcerates with a clear rim § The ulcer is painless, persists for some weeks and heals § In women it commonly develops in the vulva or cervix
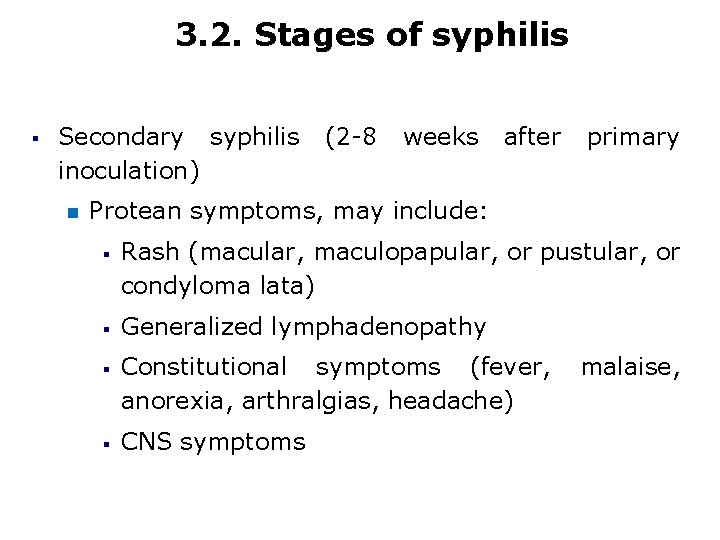
3. 2. Stages of syphilis § Secondary syphilis inoculation) (2 -8 weeks after primary Protean symptoms, may include: § § Rash (macular, maculopapular, or pustular, or condyloma lata) Generalized lymphadenopathy Constitutional symptoms (fever, anorexia, arthralgias, headache) CNS symptoms malaise,
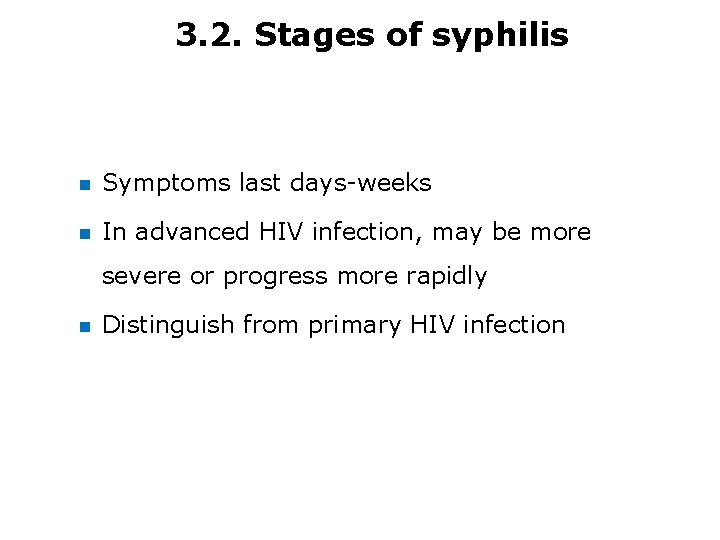
3. 2. Stages of syphilis Symptoms last days-weeks In advanced HIV infection, may be more severe or progress more rapidly Distinguish from primary HIV infection
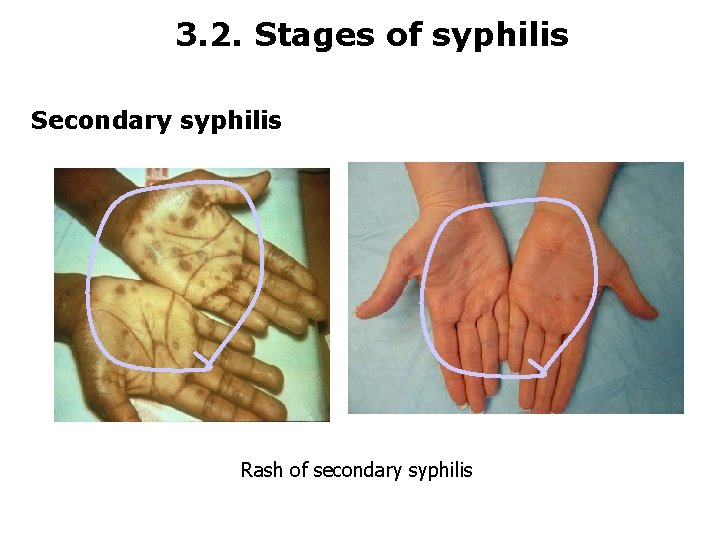
3. 2. Stages of syphilis Secondary syphilis Rash of secondary syphilis
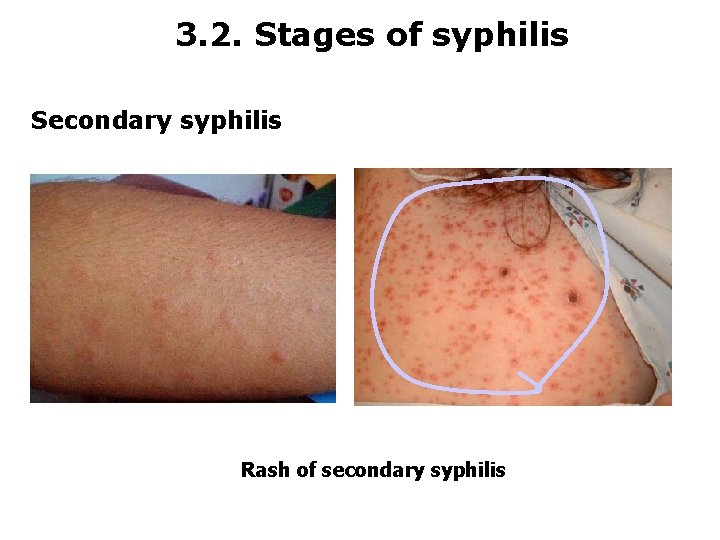
3. 2. Stages of syphilis Secondary syphilis Rash of secondary syphilis
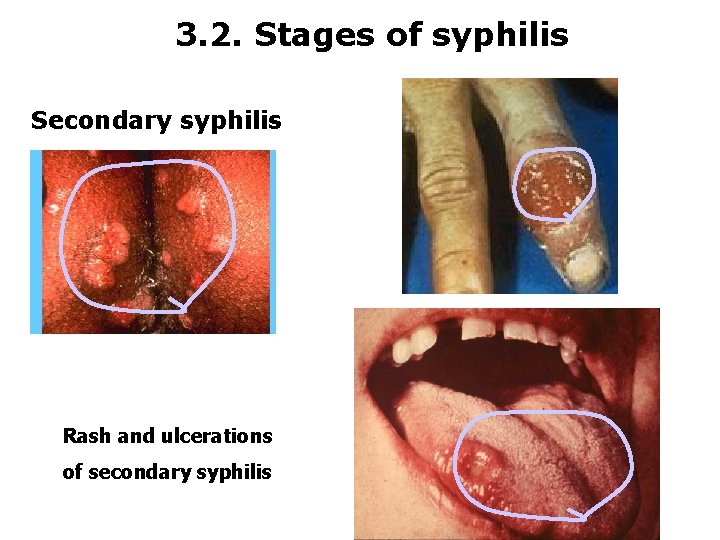
3. 2. Stages of syphilis Secondary syphilis Rash and ulcerations of secondary syphilis
3. 2. Stages of syphilis Tertiary syphilis § Appears irregularly over succeeding years and may cause series and permanent damage by means of chronic inflammation. § If untreated about 25% died directly by late syphilis

3. 2. Stages of syphilis 3 basic forms of late syphilis § § § Gumma- necrotic masses appear in skin, liver, testes and bones Cardiovascular lesions- lesions on the veins, valves and muscles of the heart. Neurosyphilis - meningo vascular - general paralysis - tabes dorsalis –degeneration of posterior column of the spinal cord
3. 2. Stages of syphilis § Latent syphilis: no overt signs/symptoms, though relapse of manifestations of secondary syphilis may occur § Late syphilis: neurosyphilis, cardiovascular syphilis, gummatous syphilis; or slowly progressive disease in any organ system

3. 2. Stages of syphilis Neurosyphilis § Neurologic complications or neurosyphilis may occur earlier or progress more rapidly in HIVpositive patients ü Meningitis, meningovascular, or parenchymatous disease similar in HIV-uninfected patients ü Concomitant uveitis and meningitis more common in HIV-positive patients § Asymptomatic neurosyphilis (CSF with elevated protein, lymphocytosis, or positive serologic test, in absence of symptoms): not a late complication or manifestation
3. 2. Stages of syphilis Congenital syphilis § Pregnancy does not alter the course of syphilis in adults § Transmission and adverse outcomes highest with early syphilis § Syphilis may increase risk of perinatal HIV transmission to infants = congenital syphilis § Screening: § At first prenatal visit in all women; in highprevalence areas or high-risk women, repeat at 28 weeks and at delivery
3. 3. Immune response § § Infection with T. pallidum involves both CMI and humoral immune response. Antigens Wasserman Ag- phospholipid diphosphatidyl glycerol = cardiolipin Is a normal constituent of host tissue Antibodies Wasserman Antibody=Anticardiolipin=Reagin Is an Ab to Ags of treponemal proteins as carriers and cardiolipin as immunogenic determinant.
3. 3. Immune response Treponemal Antigens From one or more pathogenic species Shared by many/different strains, spps, sub spps or specific to spps or sub spps Produce anti-treponemal Abs = Abs to components of treponems Treponemal Antibodies could be: - Non specific directed against proteins common to pathogenic/non-pathgenic treponems - Specific directed to pathogenic treponems only
3. 4. Diagnosis of syphilis 1. Tests that detect the etiologic agent 2. Serologic tests for syphilis 1. Tests that detect the etiologic agent Dark field (Dark ground) Indian ink (Negative stain) Phase contrast microscopy Electron microscopy Silver stain Fluorescent stain (DF)
3. 4. Diagnosis of syphilis Morphological x-ics may be studied microscopically. Usual methods: Dark field (Dark ground) Wet preparation Indian ink (Negative stain) Phase contrast microscopy Electron microscopy Silver stain Fluorescent stain (DF) Dry preparation
3. 4. Diagnosis of syphilis Dark field microscopy § For symptomatic patients with primary syphilis, dark field microscopy is the test choice. § A dark field examination is also suggested for immediate results in cases of secondary syphilis with a VDRL titer follow-up test.

3. 4. Diagnosis of syphilis
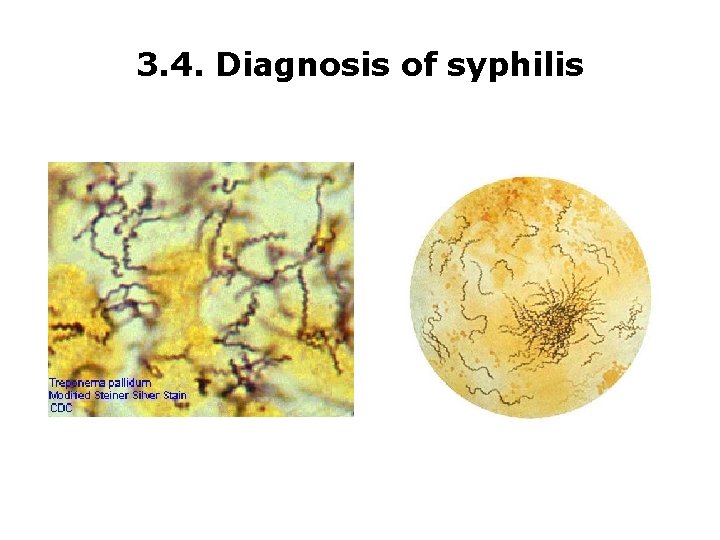
3. 4. Diagnosis of syphilis
3. 5. Serologic tests for syphilis § § More than 200 tests developed and only few are used currently. Generally grouped into TWO, based upon the type of Ag used and Ab detected A. Reagin tests for syphilis (Non-treponemal/ Non-specific tests) B. Treponemal tests for syphilis (Specific tests)
3. 5. Serologic tests for syphilis A. Non- Treponemal Tests for Syphilis § A non- treponemal test employs an antigen (E. g. , cardiolipin-lecithin), § Are used to detect an antibody like substances or “reagin” antibody, § Are not 100% specific for syphilis antibodies, but are highly sensitive for syphilis
3. 5. Serologic tests for syphilis § Advantages of being practical, inexpensive and widely available. § Basically of two types: I. Flocculation (tube or slide) and II. Complement fixation tests.
3. 5. Serologic tests for syphilis I. Flocculation Tests a. Slide flocculation tests, § needs small amount of clinical specimen and antigen suspension § are rapidly performed § results are usually read microscopically § It utilizes cardiolipin, lecithin, cholesterol antigen and heat inactivated serum. § Performed on slide or tube E. g. , VDRL
3. 5. Serologic tests for syphilis b. Tube flocculation tests § are performed in test tubes § requires large quantities of specimen and antigen suspension § are more complicated § are read with or without magnification. Eg. , ü Kliane flocculation Test ü Khan flocculation Test ü VDRL ü Mazzini test ü Hinton (serum) test
3. 5. Serologic tests for syphilis c. Card flocculation tests (Rapid reagin tests): § RPR (rapid plasma reagin) § PCT- plasma Cri. T § RPR (Teardrop) card test § RPR (18 -mm circle) card tests
3. 5. Serologic tests for syphilis II. Complement fixation Test (CFT) § Complement components are thermo labile proteins found in normal serum. § It is also found in other animals. § It is destroyed at 56 C for 30 minutes. § But up on standing at 7 -370 C, it may regain part of its activity. § Therefore, previously heated serum must be reheated for 10 min. at 560 C before a test can be performed.
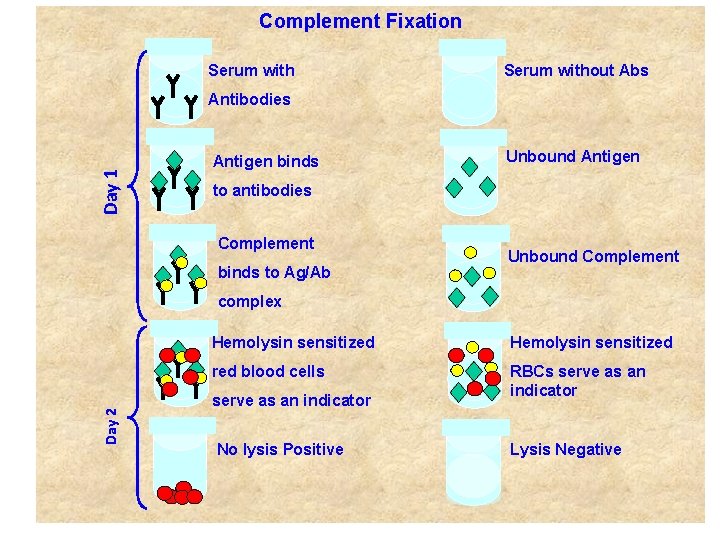
Complement Fixation Serum without Abs Day 1 Antibodies Antigen binds Unbound Antigen to antibodies Complement binds to Ag/Ab Unbound Complement Day 2 complex Hemolysin sensitized red blood cells RBCs serve as an indicator No lysis Positive Lysis Negative
3. 6. Serological technique RPR (Rapid reagain card test for syphilis) Principle § Destructive syphilitic lesions cause tissue damage. Circulating antibodies called reagain are produced against some of the tissue components. The rapid regain card test uses a modified form of the VDRL (Vernal Disease Research Laboratory) antigen called cardiolipin in suspension with carbon particles. When cardiolipin antigen reacts with reagain antibody in patient’s serum the carbon particles in the suspension clump together.
3. 6. Serological technique Materials § The following are provided in the test kits: § Reagin antigen suspension § Reagin positive control serum § Reagin negative control serum § Reagin test card § Dispensing bottle and needle § Dropper tubes § Mixing sticks
3. 6. Serological technique Qualitative RPR test method Procedure § Let the reagents and specimens warm up to room temperature. § Dispense one drop of negative control serum on to one circle on the test card using a disposable dropper tube. § Repeat step two with the positive control serum using a clean dropper tube. § Dispense on drop of each sample serum or plasma on to one circle on the card using a clean dropper tube for each specimen.
3. 6. Serological technique Procedure § Spread all the drops to cover the whole area of the circles using the mixing sticks. § Mix with reagain antigen suspension in the dispensing bottle. Hold the bottle vertically and dispense one drop on to each test sample. Do not mix again. § Place the card on the rotor for 8 minutes at 100 rpm.
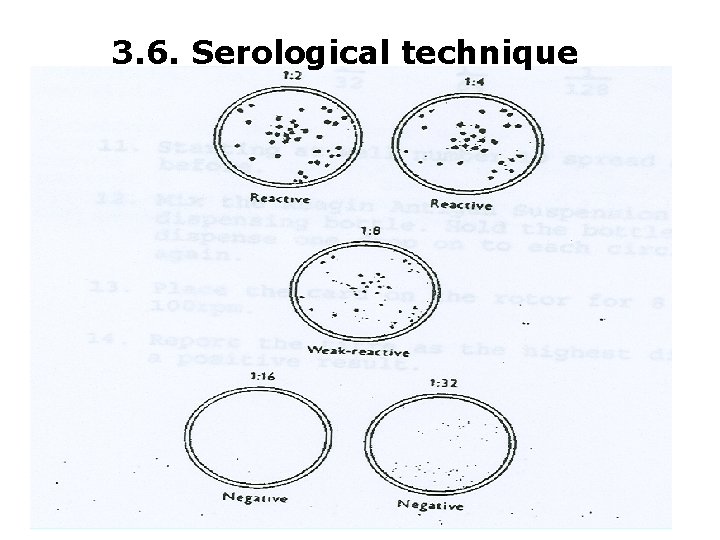
3. 6. Serological technique Reading the results § Negative result: The carbon particles remain in an even suspension § = Non reactive Positive result: The carbon particles clump together = Reactive
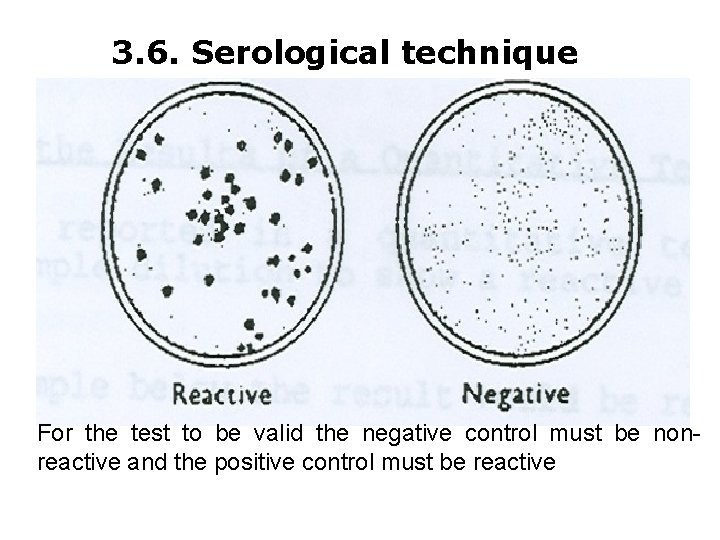
3. 6. Serological technique For the test to be valid the negative control must be nonreactive and the positive control must be reactive
3. 6. Serological technique Reporting results of a qualitative test § Qualitative results should be reported as reactive or Non-reactive
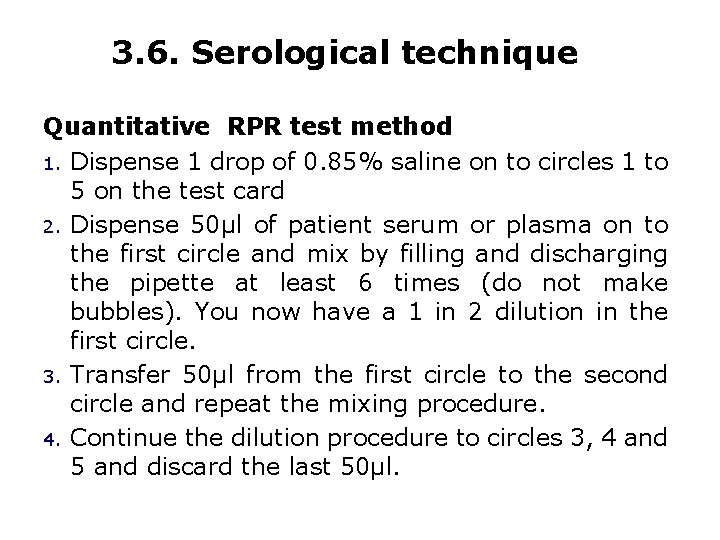
3. 6. Serological technique Quantitative RPR test method 1. Dispense 1 drop of 0. 85% saline on to circles 1 to 5 on the test card 2. Dispense 50µl of patient serum or plasma on to the first circle and mix by filling and discharging the pipette at least 6 times (do not make bubbles). You now have a 1 in 2 dilution in the first circle. 3. Transfer 50µl from the first circle to the second circle and repeat the mixing procedure. 4. Continue the dilution procedure to circles 3, 4 and 5 and discard the last 50µl.
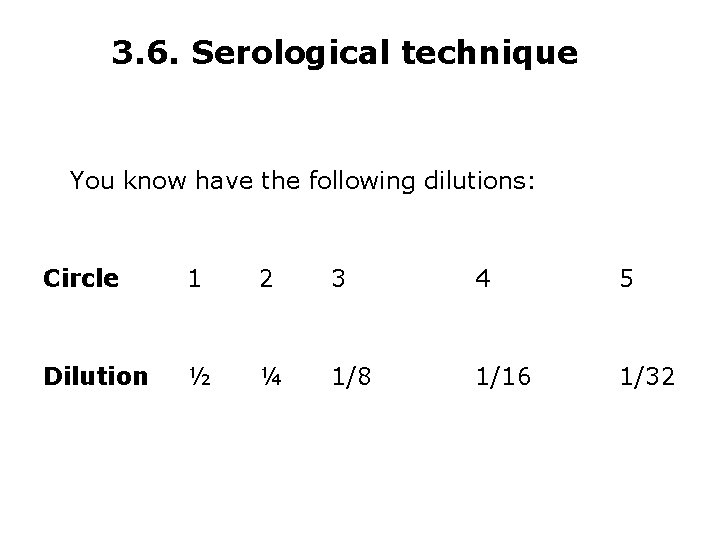
3. 6. Serological technique You know have the following dilutions: Circle 1 2 3 4 5 Dilution ½ ¼ 1/8 1/16 1/32
3. 6. Serological technique 5. Starting at circler number 5 uses a mixing stick to spread all the drops to cover the whole area of the circles. 6. Mix the regain antigen suspension in the dispensing bottle. Hold the bottle vertically and dispense one drop on to each test sample. Do not mix again. 7. Place the card on the rotor for 8 minutes at 100 rpm.
3. 6. Serological technique Reporting the results of a quantitative test § The titer reported in a quantitative test is the highest sample dilution to show a reactive (positive) result. § In the example below the result would be reported as: § Reactive to 1/8
3. 6. Serological technique
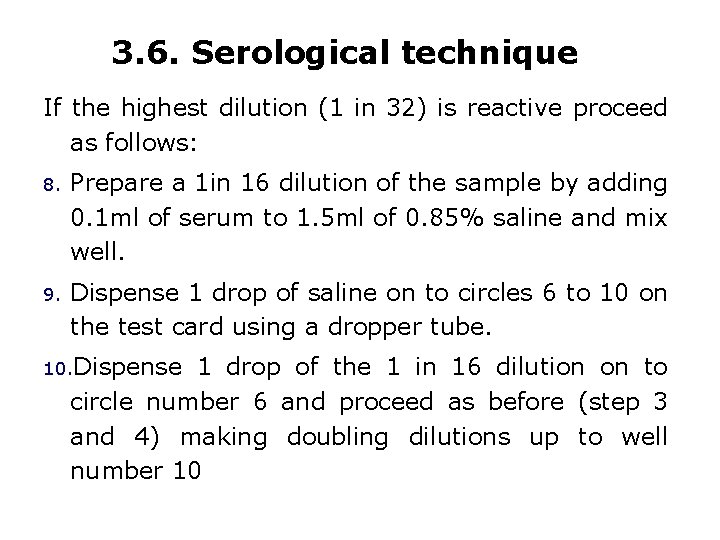
3. 6. Serological technique If the highest dilution (1 in 32) is reactive proceed as follows: 8. Prepare a 1 in 16 dilution of the sample by adding 0. 1 ml of serum to 1. 5 ml of 0. 85% saline and mix well. 9. Dispense 1 drop of saline on to circles 6 to 10 on the test card using a dropper tube. 10. Dispense 1 drop of the 1 in 16 dilution on to circle number 6 and proceed as before (step 3 and 4) making doubling dilutions up to well number 10
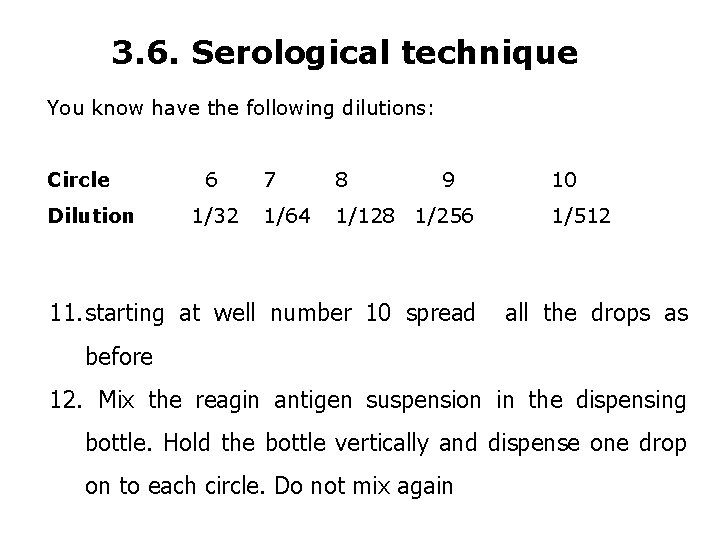
3. 6. Serological technique You know have the following dilutions: Circle Dilution 6 1/32 7 8 9 1/64 1/128 1/256 11. starting at well number 10 spread 10 1/512 all the drops as before 12. Mix the reagin antigen suspension in the dispensing bottle. Hold the bottle vertically and dispense one drop on to each circle. Do not mix again
3. 6. Serological technique 13. place the card on the rotor for 8 minute at 100 rpm 14. report the titer as the highest dilution to show a positive result
3. 6. Serological technique Limitation of the test § The rapid regain card test is a non-specific test for syphilis. A positive reaction indicates tissue damage such as that caused by destructive syphilitic lesions. § False negative reactions can occur in the early and later stages of syphilis when there is not a lot of tissue damage.
3. 6. Serological technique § False positive reactions can occur due to other diseases which result in tissue damage such as malaria, leprosy, viral infections, autoimmune diseases and many other conditions including pregnancy. § It is very important that reactive specimens are checked by another test procedure which is specific for syphilis. § In the CPHL this is done by the Wellcosph HA test which is specific for antibodies to T. pallidum, the bacterium which causes syphilis.
3. 6. Serological technique VDRL TEST Slide Qualitative VDRL Test Principle § During the period of infection with syphilis, reagin, a substance with the properties of an antibody, appears in the serum affected patients. Reagin has the ability to combine with a colloidal suspension extracted from animal tissue and clump together to form visible masses, a process known as flocculation.
3. 6. Serological technique Procedure: 1. Pipette 0. 05 ml or 1 drop of inactivated serum into one ring of the ringed glass slide. 2. Add one-drop (1/60 ml) antigen suspension onto each serum. 3. Rotate slide for 4 minutes. (If rotated by hand on a flat surface, this movement should roughly circumscribed a 2 inch/5 mm diameter circle). 4. Tests are read immediately after rotation microscopically with a 10 x ocular and a 10 x objective.
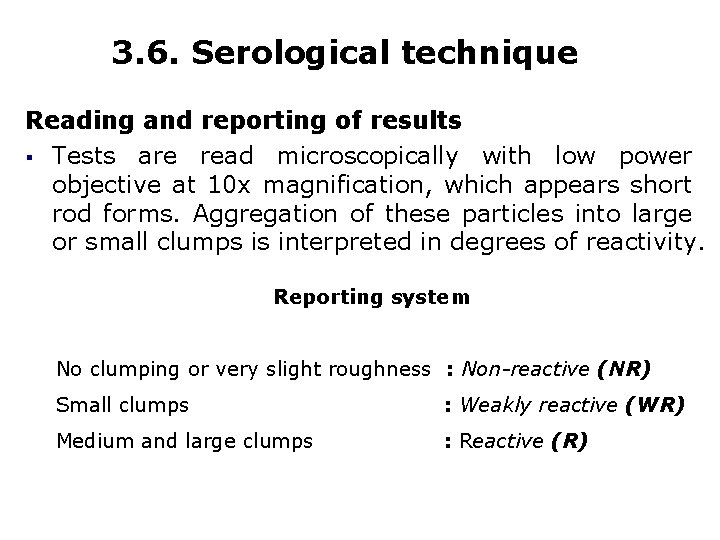
3. 6. Serological technique Reading and reporting of results § Tests are read microscopically with low power objective at 10 x magnification, which appears short rod forms. Aggregation of these particles into large or small clumps is interpreted in degrees of reactivity. Reporting system No clumping or very slight roughness : Non-reactive (NR) Small clumps : Weakly reactive (WR) Medium and large clumps : Reactive (R)
3. 6. Serological technique Standard Treponemal tests for syphilis 1. T. pallidum immobilization test (TPI) 2. RPCF test ( Reiter protein complement fixation test) 3. Fluorescent Treponnema antibody Absorption test (FTA-ABS-test) 4. Treponoma pallidum Methylene Blue tests. 5. Treponomal pallidum agglutination test. 6. Treponemal pallidum complement fixation test.
3. 8. Serological technique 1. T. pallidum immobilization test (TPI) Principle: Treponema pallidum immobilization test is the most specific and extremely valuable test for syphilis. It becomes positive after the second week of infection. The test is however quite complicated and relatively costy to perform. The test, where available, is used for reference and to rule out false-positive sero reactors of other tests.
3. 6. Serological technique Method: § Patient’s serum is placed in a test tube with living spirochetes and complement. § After incubation in an atmosphere free of 02, slide preparations are made and examined by dark field illumination. § The spirochetes will be immobilized by syphilitic serum but will be actively motile in normal serum. The TPI test has its greatest value in confirming syphilis or ruling out biological false positive reaction.
3. 6. Serological technique Limitation of the test § It requires live treponemas from infected animals and is difficult to § perform. It does not distinguish the various treponematoses (i. e. yaws, pinta, bejel) § It fails to detect early syphilis § It cannot be used as an index of therapeutic response. § It is ineffective when the patient is on antibiotics.
3. 6. Serological technique Advantage: § On the positive side, the test is the one of choice for spinal fluids, especially for detecting neurosyphilis when reagin tests give non-reactive results.
3. 6. Serological technique 2. RPCF test ( Reiter protein complement fixation test) § RPCF is a test with treponemal antigen § is performed for the diagnosis of syphilis § less specific and sensitive than TPI § the test is simple to perform and quite cheap
3. 6. Serological technique 3. Fluorescent Treponnema antibody Absorption test (FTA-ABS-test) § A modified form of fluorescent treponemal antibody test (FTA-Test) with treponemal antigen employing indirect immunofluorescence § FTA-used for diagnosis of syphilis § It is a specific and sensitive test
3. 6. Serological technique Principle § The FTA-ABS observation. test is Although a not direct method recommended of for screening, it is the most sensitive serologic procedure in the detection of primary syphilis. Limitation of the test § This test is recommended as a confirmatory test for syphilis. § It is recommended for screening test. § A reagin test such as the VDRL or RPR is not recommended for screening.

3. 6. Serological technique Stage Primary Secondary Late VDRL 70% 99% 1% RPR 80% 99% 0% FTA-ABS 85% 100% 95% TPHA-TP 65% 100% 95% TPI 50% 97% - Non Treponemal (Reagin tests) Specific Treponemal test
3. 6. Serological technique Non standard non treponemal and treponemal test § ELISA § CAPTIA-syphilis G test § CAPTIA-syphilis M test § Syphilis Rapid test device
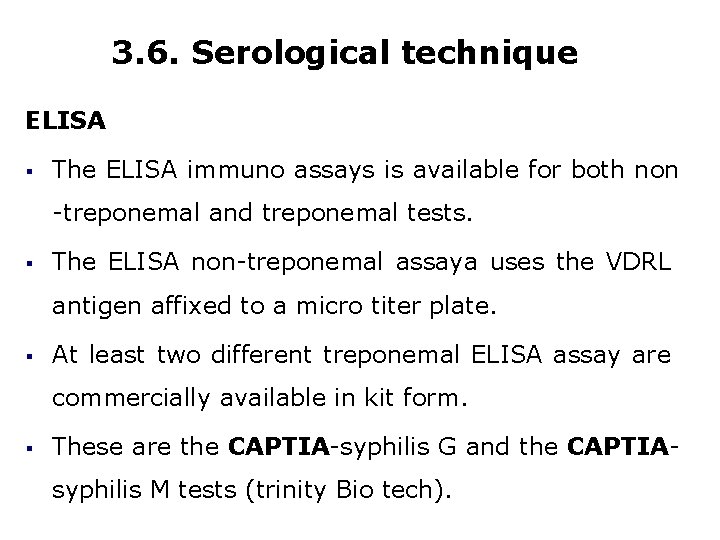
3. 6. Serological technique ELISA § The ELISA immuno assays is available for both non -treponemal and treponemal tests. § The ELISA non-treponemal assaya uses the VDRL antigen affixed to a micro titer plate. § At least two different treponemal ELISA assay are commercially available in kit form. § These are the CAPTIA-syphilis G and the CAPTIAsyphilis M tests (trinity Bio tech).
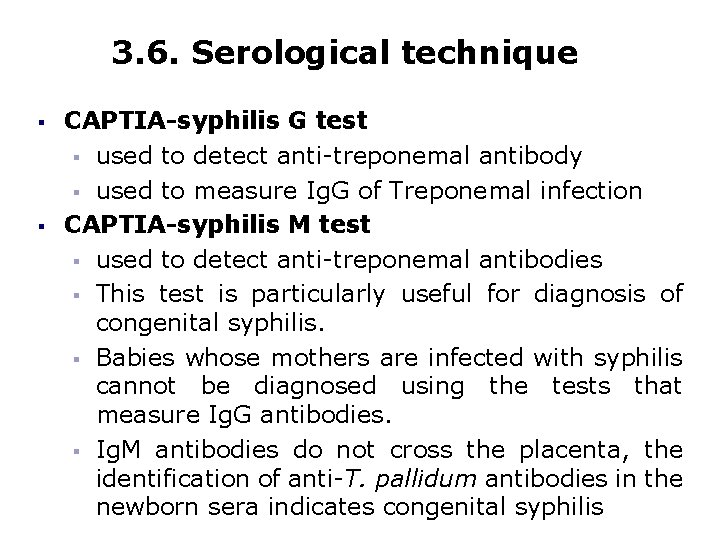
3. 6. Serological technique § § CAPTIA-syphilis G test § used to detect anti-treponemal antibody § used to measure Ig. G of Treponemal infection CAPTIA-syphilis M test § used to detect anti-treponemal antibodies § This test is particularly useful for diagnosis of congenital syphilis. § Babies whose mothers are infected with syphilis cannot be diagnosed using the tests that measure Ig. G antibodies. § Ig. M antibodies do not cross the placenta, the identification of anti-T. pallidum antibodies in the newborn sera indicates congenital syphilis

3. 6. Serological technique § Syphilis Rapid test device § it is a rapid qualitative chromatographic immunoassay that uses the affinity of protein A for Ig. G antibodies to test for treponemal antibodies § Protein A binds to the Fc region of most subclasses of Ig. G. § One of the advantages of this test is that dilutions are not required and the prozone phenomenon is not an issue as it is for tests whose end points are flocculation or agglutination.
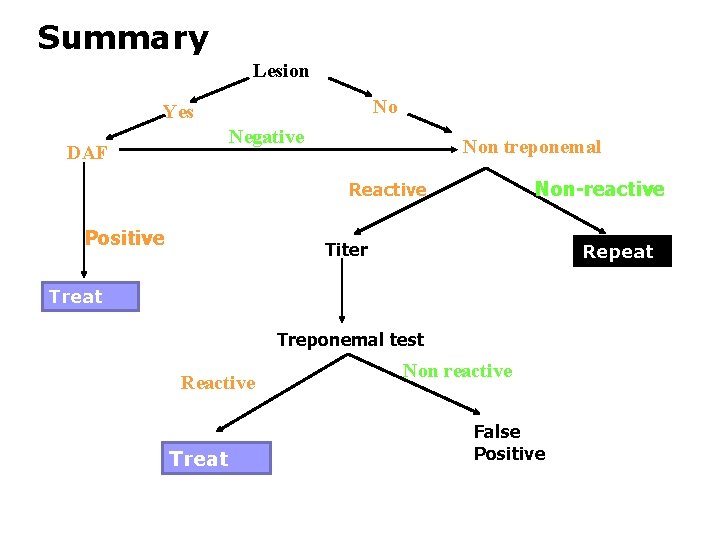
Summary Lesion No Yes Negative DAF Non treponemal Non-reactive Reactive Positive Titer Repeat Treponemal test Reactive Treat Non reactive False Positive
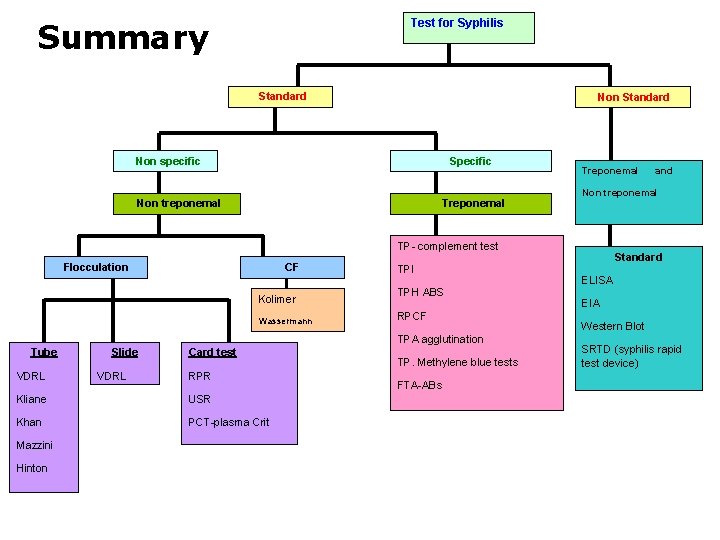
Summary Test for Syphilis Standard Non specific Specific Non treponemal Treponemal Non treponemal TP- complement test Flocculation CF Kolimer Wassermann TPI TPH ABS RPCF TPA agglutination Tube VDRL Slide VDRL Card test RPR Kliane USR Khan PCT-plasma Crit Mazzini Hinton TP. Methylene blue tests FTA-ABs and Standard ELISA EIA Western Blot SRTD (syphilis rapid test device)
Review question Explain the stages of syphilis Discuss the difference between RPR and VDRL. Write non serological test for syphilis Explain syphilis specific and non-specific serologic test for
Reference 1. Tizard. Immunology an introduction, 4 th edition , Saunders publishing, 1994 2. Naville J. Bryant Laboratory Immunology and Serology 3 rd edition. Serological services Ltd. Toronto, Ontario, Canada, 1992 3. Mary Louise . Immunology and Laboratory medicine 3 rd edition Serology in
- Slides: 75