Chapter 9 Injuries to the Head Neck and



















- Slides: 69
Chapter 9 Injuries to the Head, Neck, and Face
Injuries to Head, Neck, and Face • Concussions, neck sprains and strains, skull or neck fractures, facial lacerations, vision or hearing loss are only a few of the traumatic injuries that can affect the head, neck, and face. • Coaches must be especially vigilant in managing these injuries if medical personnel is not present. • Unfortunately, mismanagement can be the difference between complete recovery, permanent disability or death.
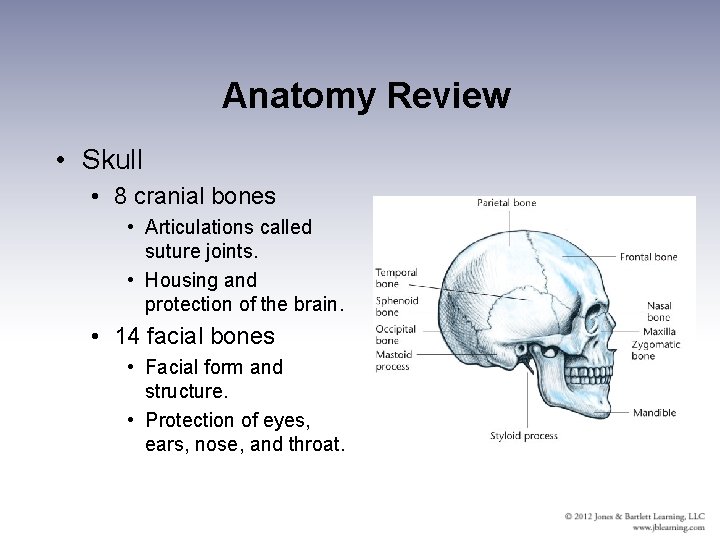
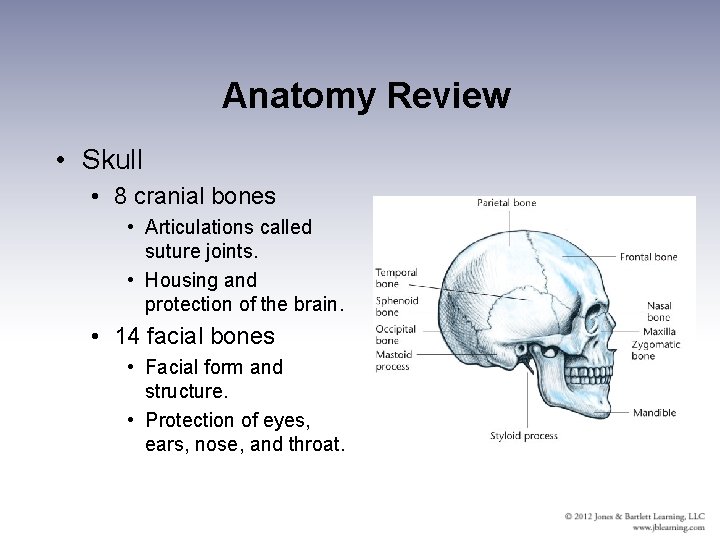
Anatomy Review • Skull • 8 cranial bones • Articulations called suture joints. • Housing and protection of the brain. • 14 facial bones • Facial form and structure. • Protection of eyes, ears, nose, and throat.
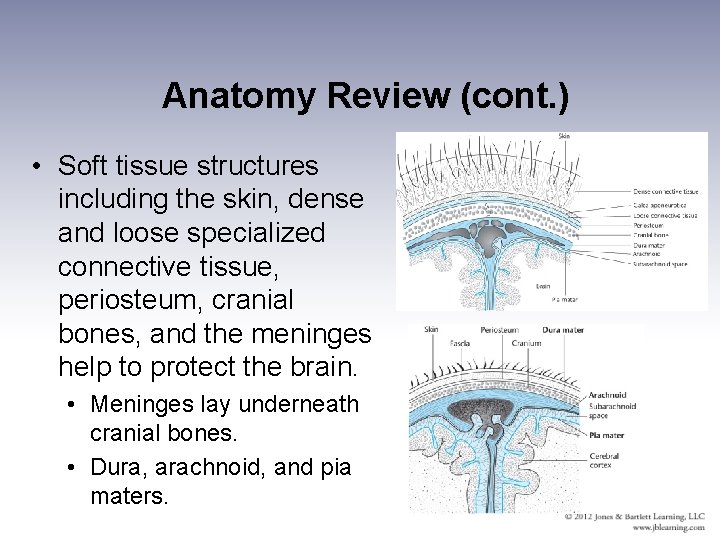
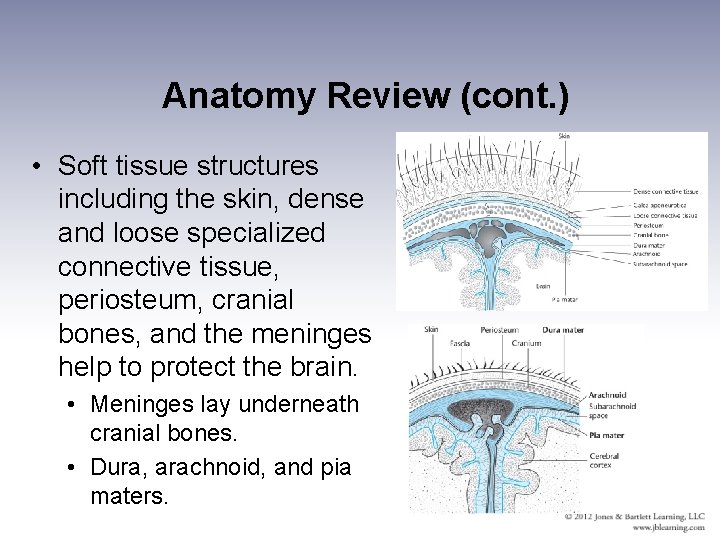
Anatomy Review (cont. ) • Soft tissue structures including the skin, dense and loose specialized connective tissue, periosteum, cranial bones, and the meninges help to protect the brain. • Meninges lay underneath cranial bones. • Dura, arachnoid, and pia maters.
Meninges • Dura mater is dense and highly vascularized. • Arachnoid (middle layer) is less dense and avascular. • Sub-arachnoid space contains cerebrospinal fluid (CSF). • CSF cushions the brain and spinal cord from external forces. • Pia mater (innermost layer) is thin, delicate, and highly vascularized.

The Face • The face is composed of skin placed over underlying bones. • Subcutaneous muscles, cartilage, and fat provide minor protection. • Several areas of the face are prone to injury, particularly orbits of the eyes, nasal bones, and mandible.
Central Nervous System (CNS) • Brain and spinal cord compose the CNS. • Highly protected by bony and soft tissue • CNS consists of gray and white matter and weighs 3 to 3. 5 lbs (adult). • Brain has three basic components – cerebrum, cerebellum, and brain stem. • Neural impulses travel to and from the CNS via 12 pairs of cranial nerves and 31 pairs of spinal nerves.

The Neck • Cervical spine • The 7 cervical vertebrae provide support for the head and protection spinal cord. • Construction allows for wide range of motion. • Tradeoff between stability and range of motion.
The Neck • The first cervical vertebra (C-1) is called the atlas. • The atlas articulates with the occipital bone to form R and L atlanto-occipital joints. • The second cervical vertebra (C-2) is called the axis. • The skull and C-1 articulate as a unit with C-2 to form the atlantoaxial joint.
Head and Neck Injuries in Sports • Even minor head trauma can result in serious injury. • Coaches need to learn to recognize head and neck injuries and render first aid when necessary. • Brain tissue is unable to repair itself. • Adolescents brains are especially susceptible. • Many will result in permanent disability (catastrophic injury). • Severe injuries can result in death.

Head and Neck Injuries in Sports • Multitude of descriptive classifications for head injuries. Three general categories: • Mild head injury or concussion • Intracranial hemorrhage • Skull fracture • Head injuries can occur in any sport. • Alarming increase in the sport of cheerleading. • Approximately 300, 000 traumatic head injuries over a 3 -year study of high school and collegiate football players. (Guskiewicz K, et al. , 2000)
Mechanisms of Head Injury • Direct mechanism of injury involves a blow to the head that causes injury at impact site (coup injury) or on the opposite side of the skull from impact (contracoup injury). • Indirect injury to the head results from damaging forces traveling from other parts of the body. • Blow to jaw, nose, or landing on tailbone. • Treat every head injury as if there is a neck injury and vice versa.

http: //www. hudl. com/v/Dg. E uv


Concussions (Mild Traumatic Head Injury) • A concussion is “a clinical syndrome characterized by immediate and transient impairment of neurologic function secondary to mechanical forces. ”(Jordan BD, 1989) • Signs and symptoms may include unconsciousness, disorientation, headache, vision changes, amnesia (anterograde or retrograde), dizziness, nausea, vomiting, ringing in ears, memory loss, and disequilibrium. • An athlete MUST only experience one sign or symptom to have experienced a concussion.
Signs and Symptoms of Concussion • Eye signs • Pupil reaction to light and equality, visual disturbances (double vision or photophobia). • Balance disturbances • Inability to maintain equilibrium. • Somatic changes • Headache, vomiting, nausea, and sleepiness
Signs and Symptoms of Concussion • Memory loss • Anterograde amnesia: inability to recall events that have transpired since the time of the injury. • Retrograde amnesia: inability to recall events that occurred prior to the injury. • Concentration deficits • Information processing deficits – slurred speech, unable to follow directions. • Emotional changes • Excessive anger or apathy. Depression or sadness.
Concussions • Grading may help the coaching staff avoid errors in judgment. • BUT, no two concussions are alike, so the medical community is moving away from grading concussions. • Cantu Evidence Based Classification (Cantu R, 2001) • Grade 1: Signs/Symptoms resolve in less than 30 minutes. • Grade 2: Loss of consciousness for less than 1 minute and/or PTA lasting longer than 30 minutes. • Grade 3: Loss of consciousness for more than a minute and/or PTA lasting more than 24 hours.
Concussions • Recent research has demonstrated: • Loss of consciousness happens in only 9% • Amnesia only happens in only 27% • Therefore, follow-up functional assessments utilizing a standardized list of typical symptoms, concentration tests, and balance/neurological assessments may provide for better care of the concussed athlete.
Concussions • Recent evidence suggests that there is some level of structural damage in all concussions. • Minor changes may include decreases in blood flow, increases in intracranial pressure, or tissue anoxia. • Any brain cells not destroyed remain extremely vulnerable to subsequent trauma. • Players sustaining a concussion had a 3 -fold increased risk of sustaining an additional concussion. • Current guidelines recommend that an adolescent athlete NOT return the same day of a concussion and NOT return until free of signs and symptoms.
Second Impact Syndrome • Second Impact Syndrome (SIS) is a serious problem. • Results when an athlete with a head injury receives another head injury before the symptoms of the initial injury have resolved. • Involves rapid, catastrophic brain swelling that can result in death. • Any athlete sustaining a head injury, no matter how minor, should be referred to a physician before being cleared to return to participation.

Head Injuries in Sports • Skull fracture • May also have associated soft tissue injury. • More severe forms of cranial injury involve depressed skull fractures • Involves bone fragments being pushed into the cranial region.

Head Injuries in Sports • Intracranial Injury • These injuries are potentially life threatening. • Majority result from blunt trauma to the head causing rapid deceleration or even rapid rotational motions of the head. • Disruption of blood vessels results in intracranial bleeding (hematoma) and swelling within the cranium. • Some degree of permanent neurologic damage and even death can result.
Intracranial Injury • Epidural hematoma • Develops quickly due to arterial bleeding. • Subdural hematoma • Develops slowly due to venous bleeding. • In some cases, symptoms don’t appear for hours or even days after the initial injury. • Intracerebral hematoma • Bleeding within brain tissue. • Cerebral contusion • Brain tissue bruising.

Initial Treatment of a Suspected Head Injury • Include an initial check and physical exam • Site of injury • Initial check and brief physical exam. • If any signs and/or symptoms of head or neck injury, he or she should not be moved until emergency medical services (EMS) personnel have arrived. • Secondary site (sideline, courtside, etc. ). • More complete physical exam.
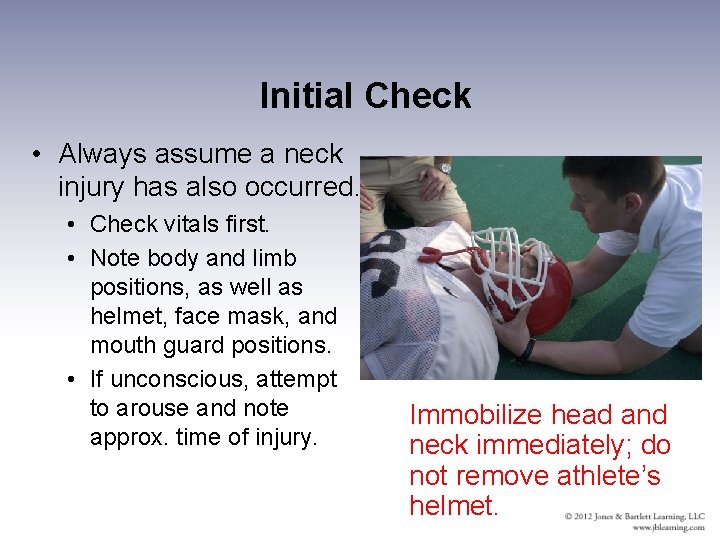
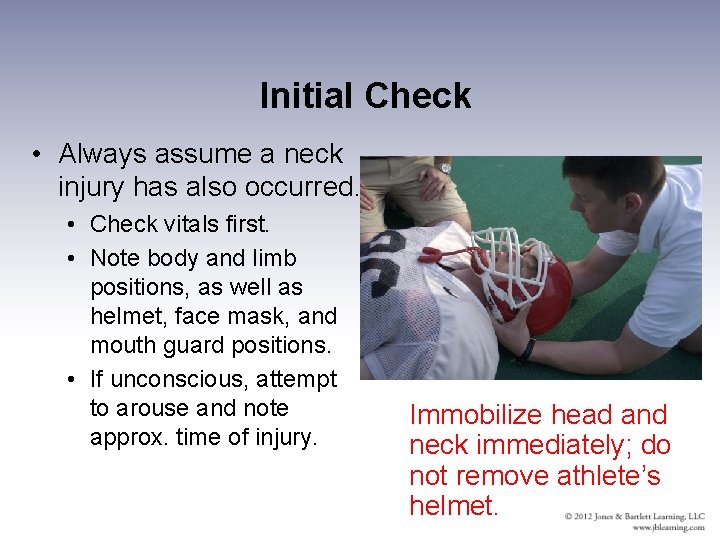
Initial Check • Always assume a neck injury has also occurred. • Check vitals first. • Note body and limb positions, as well as helmet, face mask, and mouth guard positions. • If unconscious, attempt to arouse and note approx. time of injury. Immobilize head and neck immediately; do not remove athlete’s helmet.
Initial Check • If unconscious: • Do NOT remove helmet. • Do NOT move the athlete. • Do NOT use ammonia capsules to revive athlete. • Listen near the athlete’s face for typical breathing sounds and look for movements of the thorax and/or abdomen. • If no signs of breathing or circulation are present, begin CPR and summon EMS.

Physical Examination • Coach collects as much information about the suspected head injury. • Do NOT rush through physical exam. • The physical exam must include assessments of (CEMEPS): • Consciousness or unconsciousness. • Extremity strength (if conscious) without moving the neck. • Mental function (if conscious). • Eye signs and movements. • Neck pain. • Neck musculature spasm.
Physical Exam • If athlete is conscious: • Perform bilateral grip strength tests and dorsiflexion strength. • Check for sensations on both sides of body by pinch tests. • Check pupil sizes and response to light. Evaluate ability of eyes to follow moving object side to side. • Note loss of peripheral vision or jerking eyeball movements. • Palpate neck for deformity, moving from base of skull to bottom of neck.
Physical Exam • Based on these observations, determine level of consciousness. • Athlete with grade 1 concussion should be able to walk with assistance. • Athlete with any loss of consciousness should not be moved. • Monitor vital signs. • Summon EMS.

Sideline Assessment • The objective of this phase of the evaluation is to determine the presence of any signs or symptoms of head injury that may have developed since the time of the initial injury. • This information is of vital importance when confronted with making decisions regarding medical referral, as well as clearance for return to participation.
Sideline Assessment Tools • Standardized Assessment of Concussion (SAC) • a convenient and reliable way to quickly assess neurocognitive function in the areas of orientation, immediate memory, concentration and delayed recall. • Standardized Concussion Assessment Tool 2 (SCAT 2) • Sign and symptom checklist, orientation, immediate memory, concentration and delayed recall, and balance assessment.
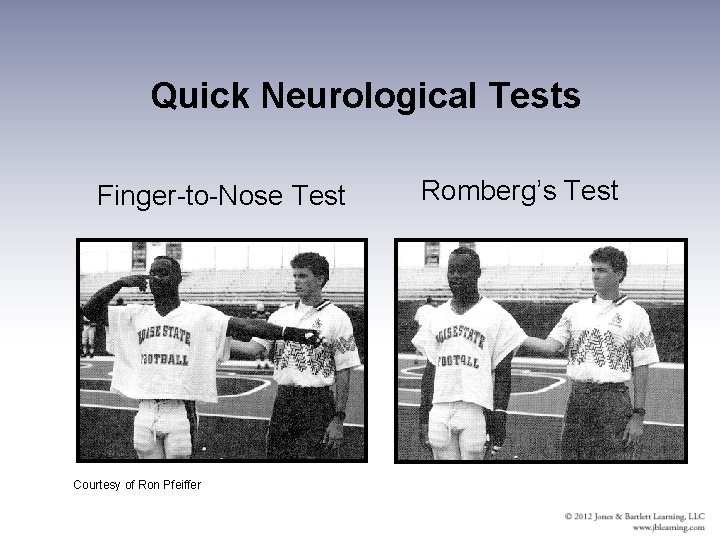
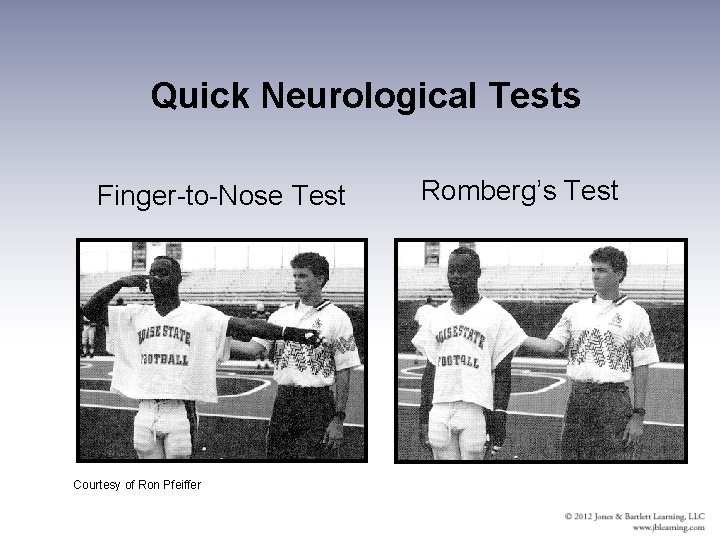
Quick Neurological Tests Finger-to-Nose Test Courtesy of Ron Pfeiffer Romberg’s Test
Cervical Spine Injuries • Cervical injuries can occur in almost any sport. • Majority occur in football, rugby, ice hockey, soccer, diving, and gymnastics. • Mechanisms of injury include hyperflexion, hyperextension, rotation, lateral flexion, and axial loading. • Serious injuries occur when intact vertebra or fragments of fractured vertebra are displaced or an intervertebral disk ruptures and places pressure on spinal cord or nerve roots.
Mechanism of Cervical Spine Injuries • Most cervical spine injuries result from an axial load. • Spearing in football produces axial load (NCAA prohibited technique in 1976). • In 2005, there was a renewed increased emphasis on proper technique to eliminate spearing and minimize neck injuries.
Types of Cervical Spine Injuries • Neck fractures and dislocations • Neck sprains • Neck strains • Muscle strains in the neck rarely involve neurologic damage. • Nerve compression or stretching • Brachial plexus injuries can produce significant but transient symptoms.

Signs and Symptoms of Cervical Injuries • Neck fractures and dislocations • Pop of snap heard. • Burning, numbness, or tingling and extremity dysfunction is likely. • Neck sprains and strains. • Very similar – location of tenderness and mechanism will vary. • Brachial Plexus Nerve Injury • Pain radiates into the affected arm. • Decrease in voluntary use of the arm (often the arm appears limp).

General Treatment Guidelines • In the absence of a medical care provider, coaching personnel must take great care when conducting an examination of an athlete suspected of having a neck injury. • Stabilize the head and neck. • Determine if the athlete is conscious. If unconscious, check airway, breathing, and pulse (circulation). • Summon EMS. • Continue monitoring “ABCs. ”
Initial Treatment of Injury Guidelines • If conscious, question the athlete regarding extremity numbness or loss of feeling, weakness, and/or neck pain. • If athlete reports the inability to move a limb or limbs or significant strength loss, stabilize head and neck and summon EMS.
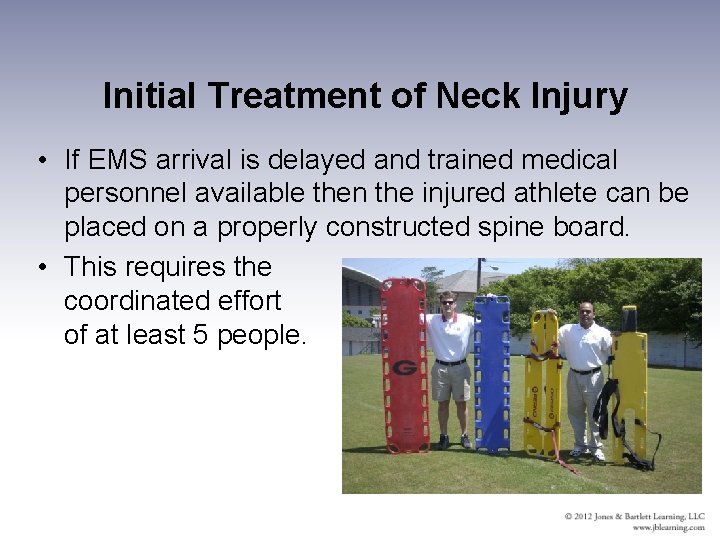
Initial Treatment of Neck Injury • If EMS arrival is delayed and trained medical personnel available then the injured athlete can be placed on a properly constructed spine board. • This requires the coordinated effort of at least 5 people.
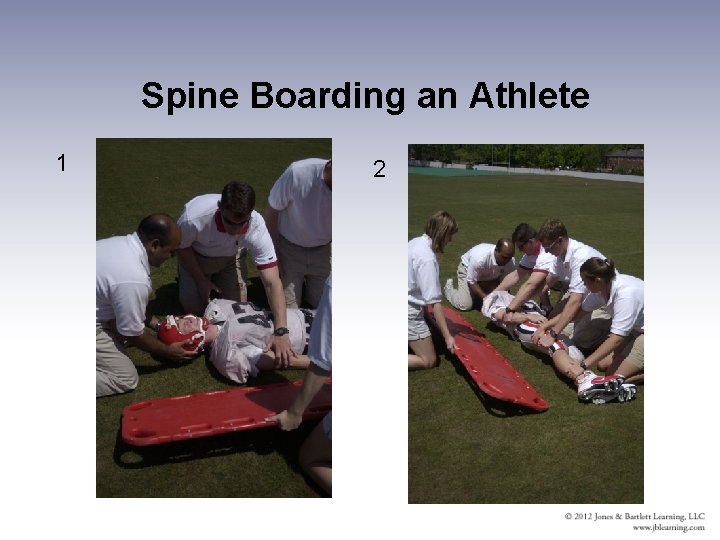
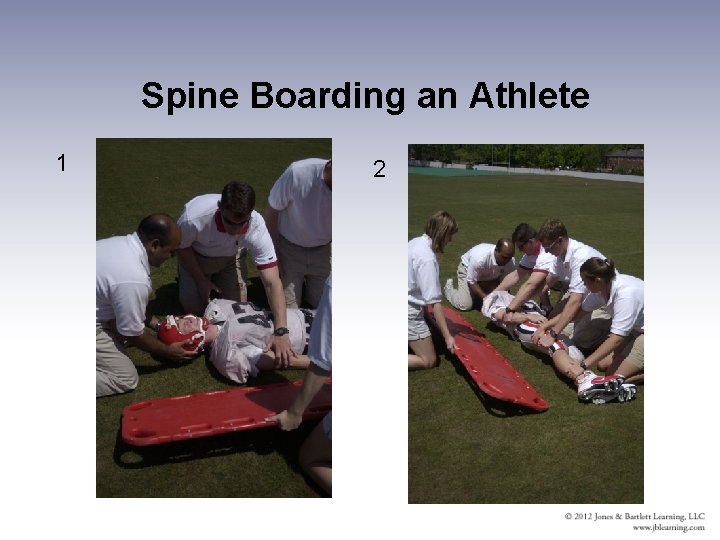
Spine Boarding an Athlete 1 2
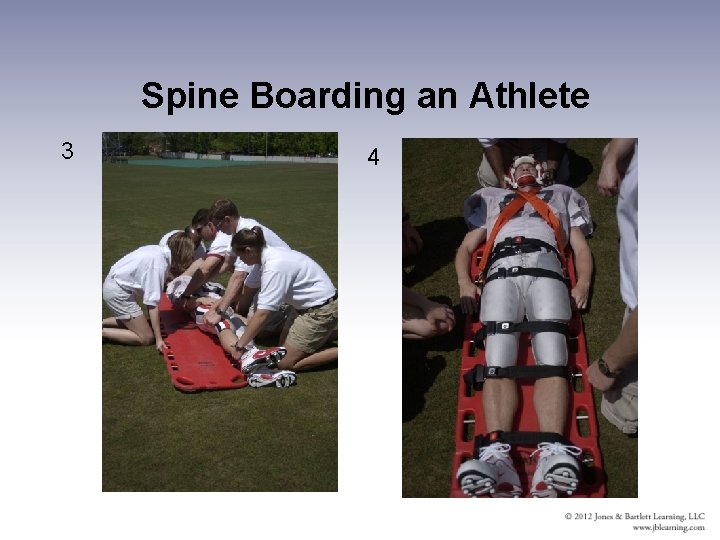
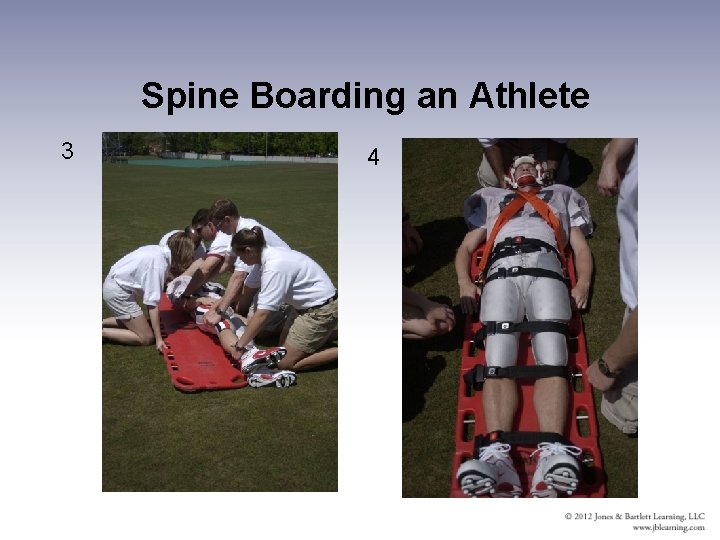
Spine Boarding an Athlete 3 4
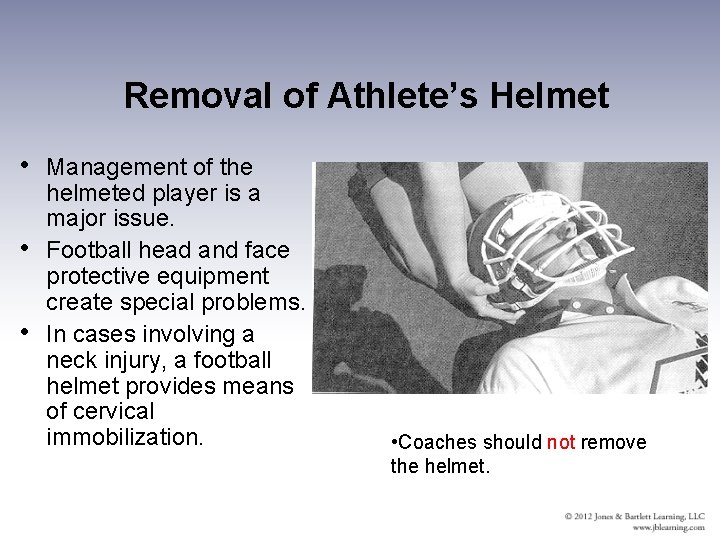
Removal of Athlete’s Helmet • Management of the helmeted player is a major issue. • Football head and face protective equipment create special problems. • In cases involving a neck injury, a football helmet provides means of cervical immobilization. • Coaches should not remove the helmet.
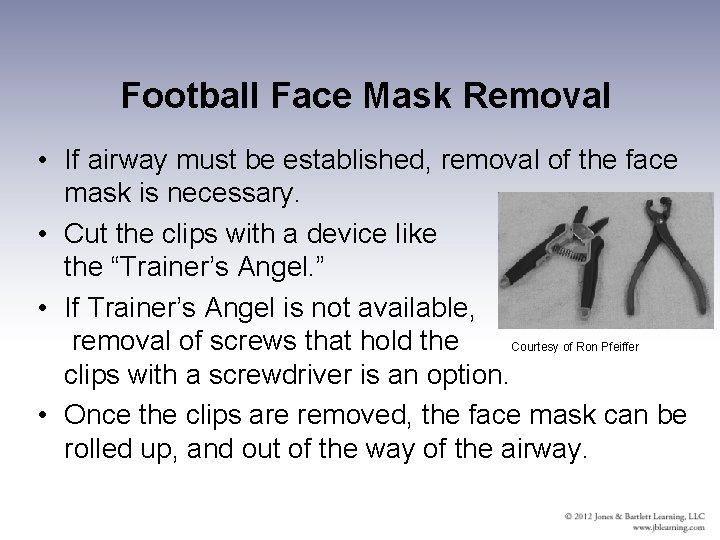
Football Face Mask Removal • If airway must be established, removal of the face mask is necessary. • Cut the clips with a device like the “Trainer’s Angel. ” • If Trainer’s Angel is not available, removal of screws that hold the Courtesy of Ron Pfeiffer clips with a screwdriver is an option. • Once the clips are removed, the face mask can be rolled up, and out of the way of the airway.

Injuries to the Maxillofacial Region • Maxillofacial injuries include those to the jaw, teeth, eyes, ears, nose, throat, facial bones, and skin. • Modern protective equipment has reduced significantly the incidence of these injuries. Such equipment includes: • Mouth guards. • Protective eye wear. • Face shields.
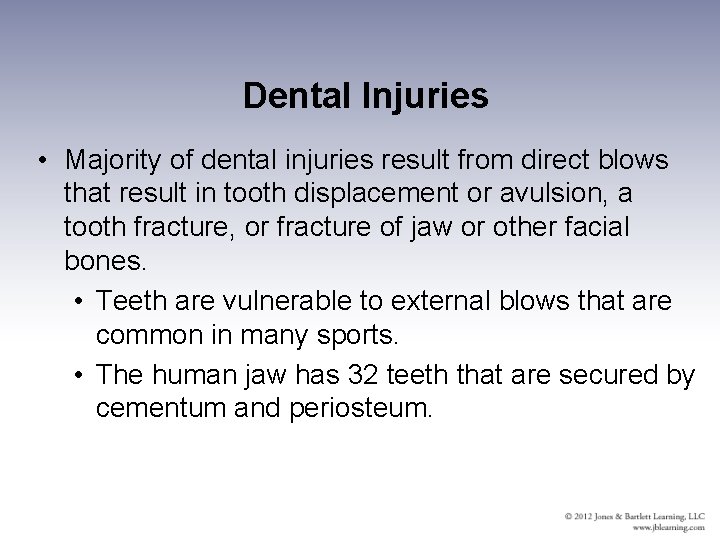
Dental Injuries • Majority of dental injuries result from direct blows that result in tooth displacement or avulsion, a tooth fracture, or fracture of jaw or other facial bones. • Teeth are vulnerable to external blows that are common in many sports. • The human jaw has 32 teeth that are secured by cementum and periosteum.
Dental Injuries • High-risk sports should require use of mouth guard. • Required for high school football players since 1966; NCAA followed suit in 1974. • Three types of mouth guards are: • Stock • Mouth-formed • Custom fitted.
Dental Injuries • When rendering first aid, take precautions to avoid bloodborne pathogens. • When examining dental injuries: • • Can athlete open and close mouth w/o pain? What is the general symmetry of the teeth? Are there any irregularities in adjacent teeth? Is there bleeding, especially along gum line? • Loosened tooth - Gently push back into place. • If tooth is avulsed, place in sterile saline and refer athlete to dentist or physician immediately.
Eye Injuries • Approximately 40, 000 sports-related eye injuries occur annually in the United States. • Majority of eye injuries are preventable. • Protective eyewear is strongly recommended. • Eye injuries in the U. S. are on the increase; basketball, baseball, and softball are leading sports for eye injuries. Racket sports are also responsible for eye injuries.
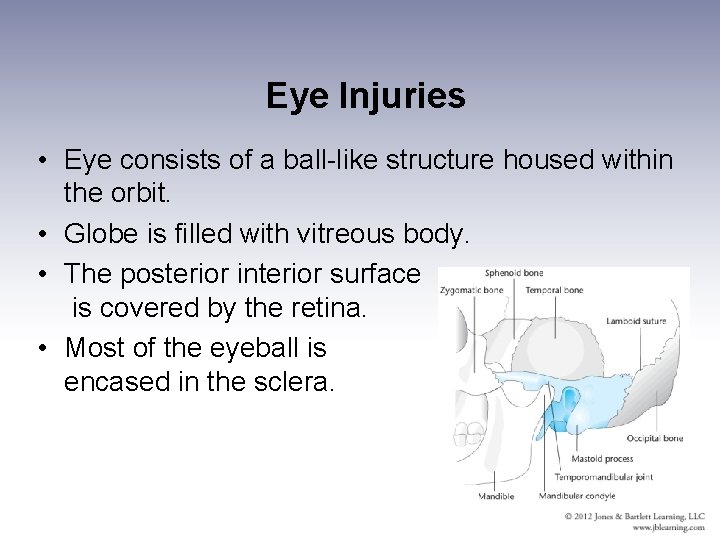
Eye Injuries • Eye consists of a ball-like structure housed within the orbit. • Globe is filled with vitreous body. • The posterior interior surface is covered by the retina. • Most of the eyeball is encased in the sclera.

Eye Injuries • Two categories of eye injuries are contusional and penetrating. • Contusional injuries vary in severity from simple corneal abrasions to major injuries such as rupture of the eye, fracture of orbit, or combinations of the two. Detached retina can also occur. • Penetrating injuries are less common than contusional injuries.
Eye Injuries • Initial Check and Treatment Guidelines • Common injuries: • Corneal abrasion. • Pain, irritation, and excessive tearing. • Distorted vision. • Small foreign object in eye. • Small foreign bodies usually found below lower eyelid or in the medial canthus. • Refer to physician if symptoms do not resolve.
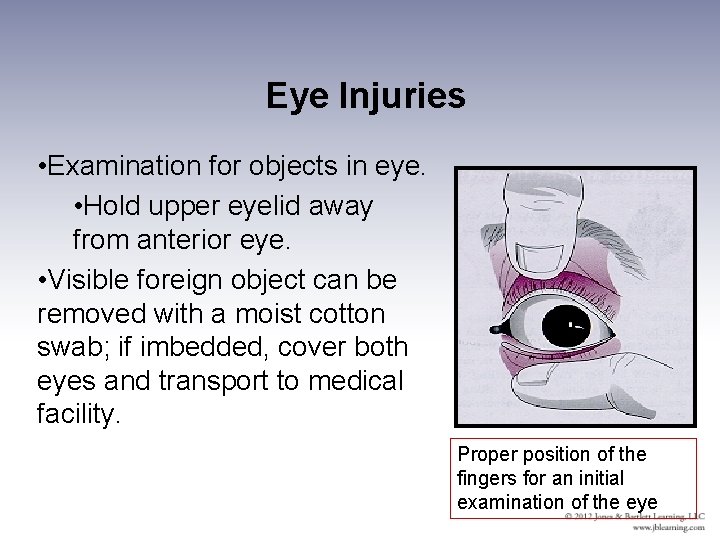
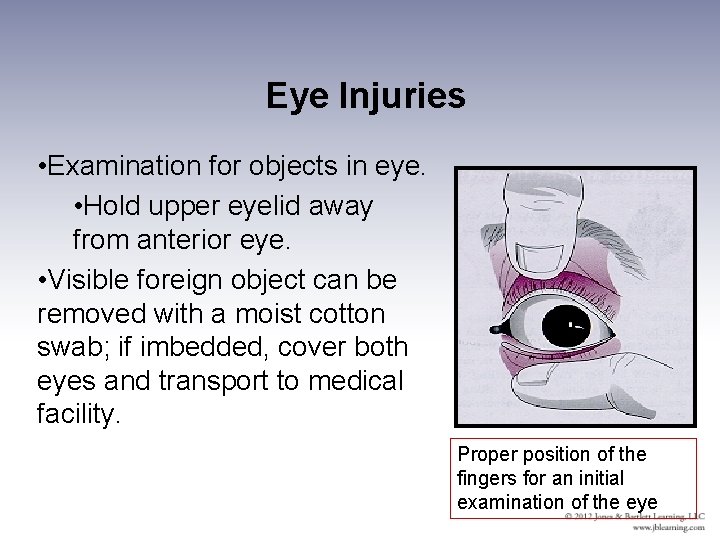
Eye Injuries • Examination for objects in eye. • Hold upper eyelid away from anterior eye. • Visible foreign object can be removed with a moist cotton swab; if imbedded, cover both eyes and transport to medical facility. Proper position of the fingers for an initial examination of the eye

Eye Injuries • Contusions may result in hemorrhage around the eye known as a “black eye. ” • More severe cases may involve bleeding into the anterior eye (“hyphema”) and orbital blowout. • Symptoms of orbital blowout include eye pain, double vision (diplopia), and obvious bleeding within the eye. • Both require referral to medical facility immediately.
Eye Injuries • Symptoms of retinal injuries develop slowly. Early symptoms include: • Floating particles in field of vision. • Distorted vision. • Changes in the amount of light seen. • Any athlete with a history of blunt trauma to the eye who later complains of these symptoms should be referred immediately for medical evaluation.

Contact Lens Problems • Many athletes wear contacts with few problems • As a rule, more problems occur with hard lenses. • Major problems include having a lens slip out of place or debris become trapped between the lens and the eye. • Coach should have first aid kit to treat common contact problems including: wetting solution, small mirror, and contact-lens case.
Nose Injuries • Anatomically, the nose is a bone-cartilage framework with skin attached. The nose includes nasal bones and the frontal processes of the maxilla. • The two nostrils are separated by the cartilaginous septum. • The nose is often injured because of its location • The nosebleed (epistaxis) may be the most common facial injury in sports.
Nose Injuries • Care of a nose bleed includes: • Wear gloves to avoid contact with blood. • Finger pressure applied directly against the nostril that is bleeding. Application of a cold compress against the nasal region. • Having the athlete lie on same side or leaning forward. • Can pack with gauze that protrudes from nostril.
Nose Injuries • Septal hematoma • Bleeding between the septum and the mucous membrane, it can lead to septal erosion. • Swelling that is usually visible both inside and outside the nose. Must be referred to medical doctor for evaluation and treatment. • Fracture • Signs of fracture a nosebleed, deformity, and swelling at the bridge of the nose. • Control any bleeding and refer to a medical doctor.
Ear Injuries • Ear has a cartilaginous framework covered with a layer of skin. • The external ear has large expanded portion (auricula) and opening to ear canal (external acoustic meatus). • The middle ear contains small group of bones that transmit sound vibrations to tympanic membrane. • Inner ear contains the labyrinth, which has a role in equilibrium.

Injuries to the Ear • Majority of ear problems are related to the external ear. • Some athletes, such as wrestlers, develop ear problems because of contact with opponents and/or playing surface. • Such contact can result in abrasions and contusions to auricle. • Required head gear has reduced incidence of such injuries.
Injuries to the Ear • Auricle has some vascularity and can develop a hematoma leading to deformity called cauliflower ear (keloid scar tissue). • Auricular hematoma should be treated with cold pack and immediately referred to a medical doctor. • Severe blows to the outer ear can result in a ruptured ear drum. • Athletes with ear infections should not participate in aquatic sports until infection has resolved.
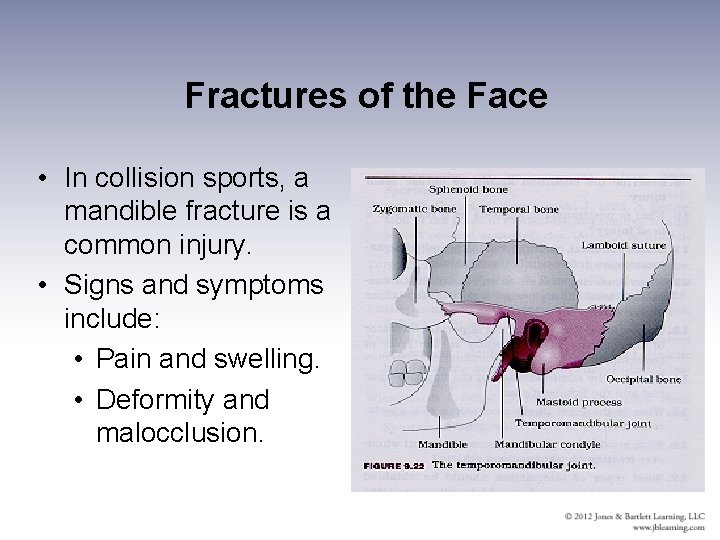
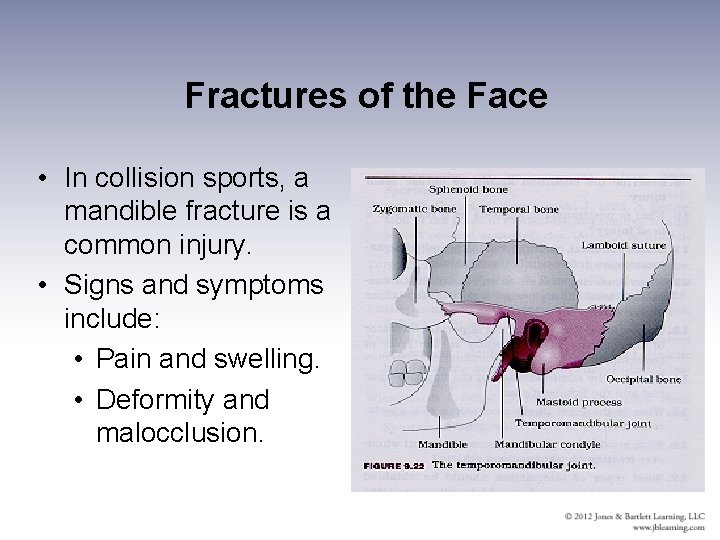
Fractures of the Face • In collision sports, a mandible fracture is a common injury. • Signs and symptoms include: • Pain and swelling. • Deformity and malocclusion.
Jaw Dislocation • Signs and symptoms include: • Extreme pain and deformity in the region of the temporomandibular joint (TMJ). • Inability to move lower jaw. • Jaw is “locked. ” • Do NOT attempt to put back into place. • Treatment includes application of ice pack and medical referral.
Zygomatic Bone Fracture • Signs and symptoms: • Pain and swelling at site of injury. • Diplopia – double vision. • Swelling and discoloration spreads to the region of the orbit. • Refer athlete to a physician for diagnosis and treatment.

Facial Wounds • Facial wounds can take many forms and treatment should follow basic first aid protocol. • Control bleeding; carefully clean with mild soap and warm water; apply sterile dressing. • Any wound with observable space between margins should be referred to a physician for suturing. Physician needs to make return-to-play decisions. • Any facial wound, even abrasion, can present cosmetic issues.