Chapter 9 Articulations Part 1 9 1 9
- Slides: 75
Chapter 9 Articulations Part 1, 9. 1 -9. 4 1
What are articulations? • Any place of contact between bones • Place of articulation is called a joint – arthrology = study of joints (arthro = joint) 2
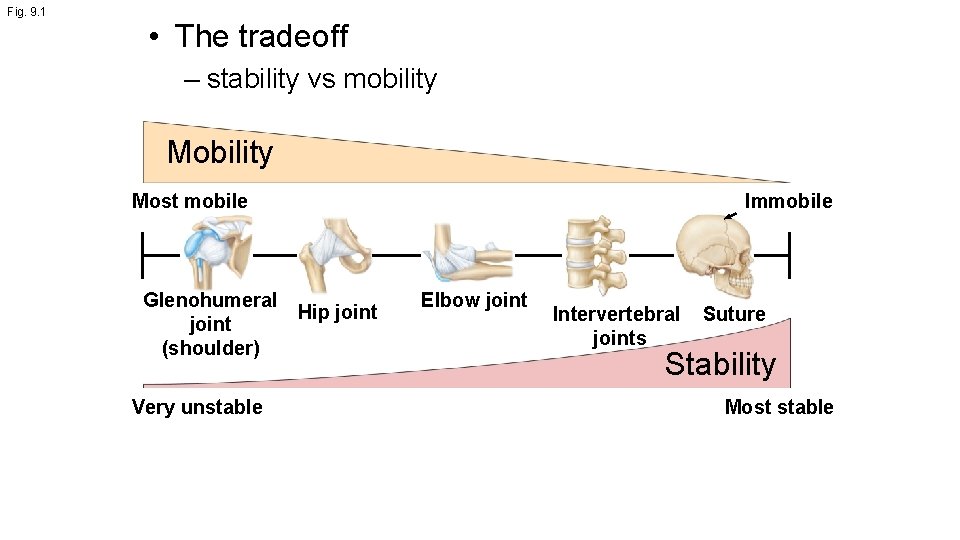
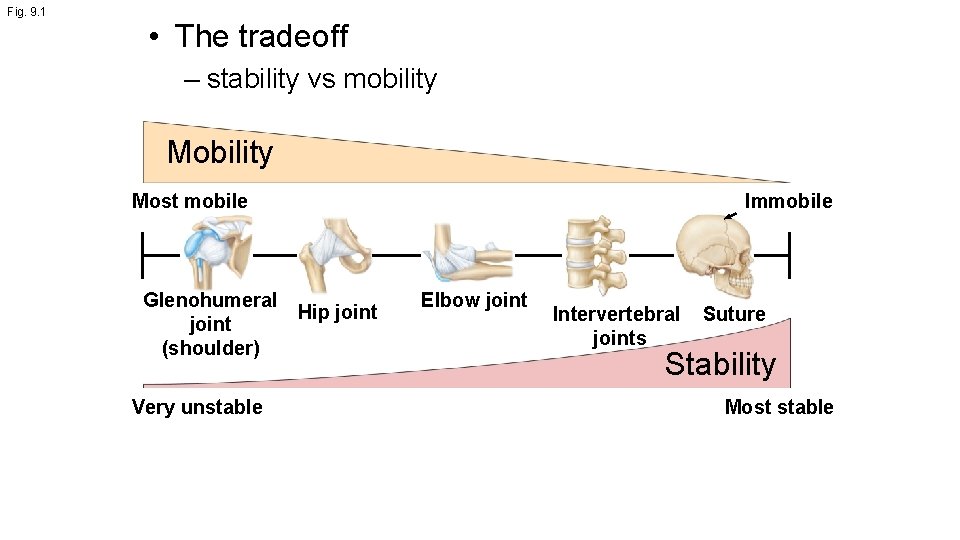
Fig. 9. 1 • The tradeoff – stability vs mobility Most mobile Glenohumeral Hip joint (shoulder) Very unstable Immobile Elbow joint Intervertebral joints Suture Stability Most stable
Joint classifications — Structural • Fibrous – bones held together by dense regular connective tissue • Cartilaginous – bones joined by cartilage • Synovial – has fluid-filled cavity – fluid separates cartilage-covered bone surfaces – bone surfaces enclosed in cavity, joined by ligaments 4
Joint classifications — Functional • Synarthrosis – immobile • Amphiarthrosis – slightly mobile • Diarthrosis – freely mobile 5
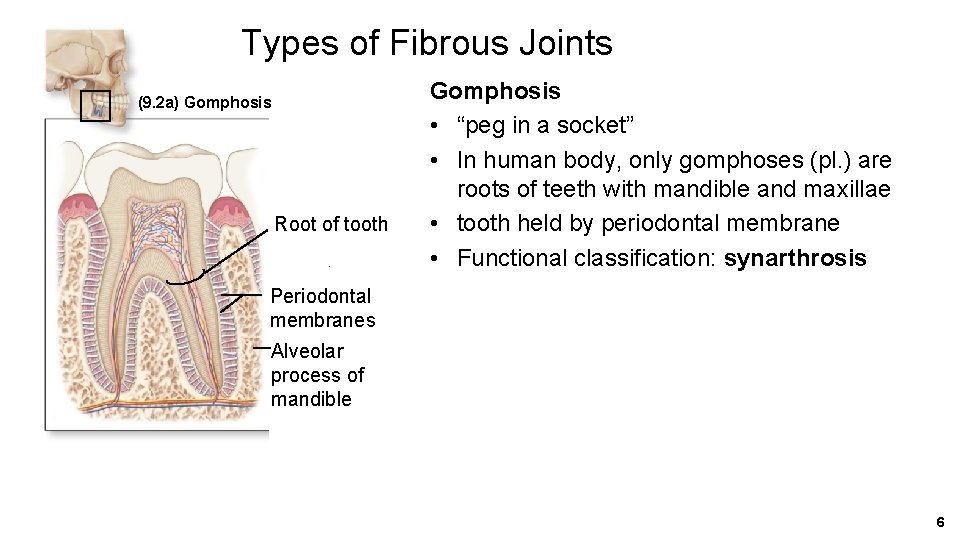
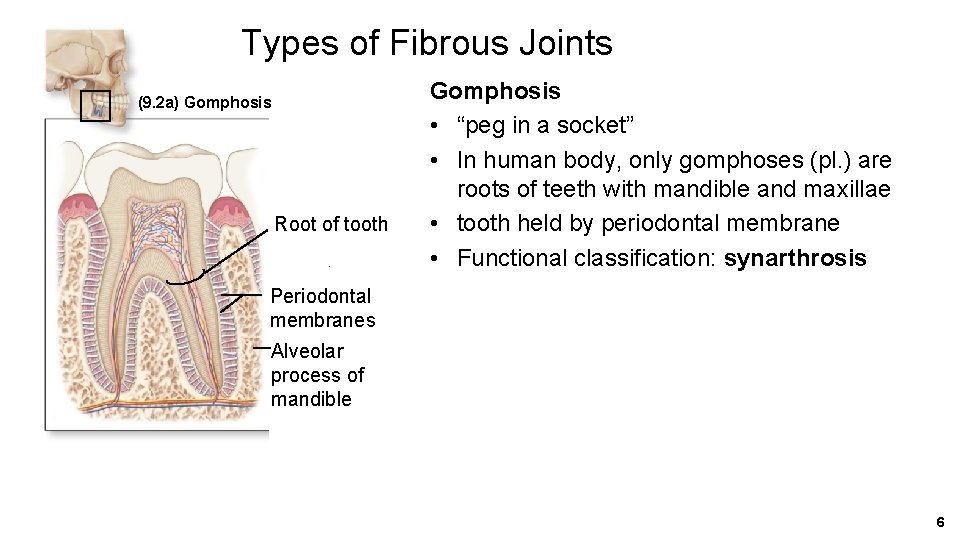
Types of Fibrous Joints (9. 2 a) Gomphosis Root of tooth Gomphosis • “peg in a socket” • In human body, only gomphoses (pl. ) are roots of teeth with mandible and maxillae • tooth held by periodontal membrane • Functional classification: synarthrosis Periodontal membranes Alveolar process of mandible 6
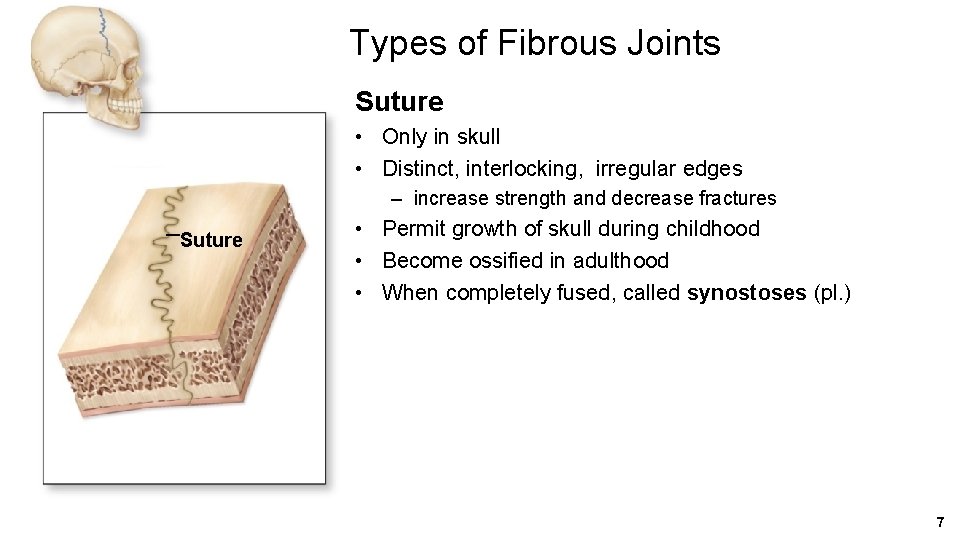
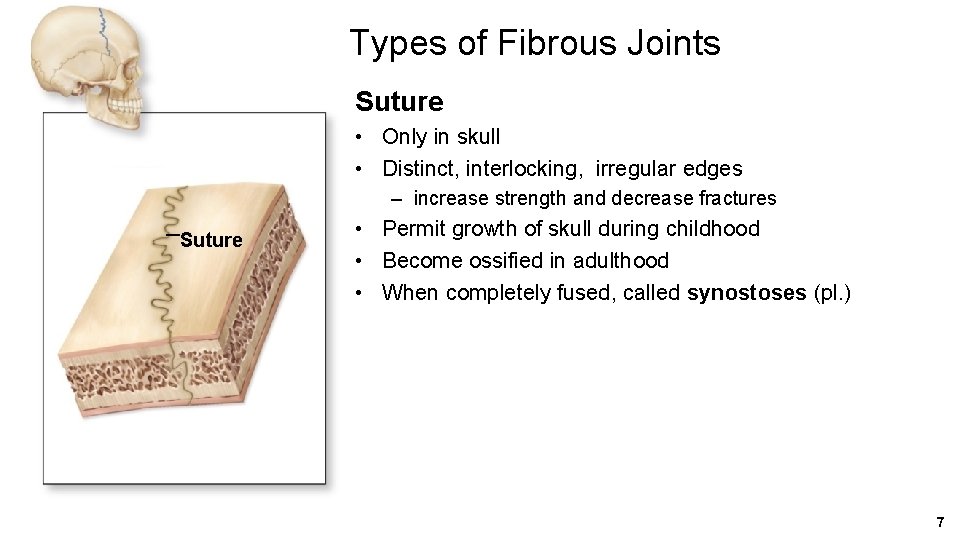
Types of Fibrous Joints Suture • Only in skull • Distinct, interlocking, irregular edges – increase strength and decrease fractures Suture • Permit growth of skull during childhood • Become ossified in adulthood • When completely fused, called synostoses (pl. ) 7
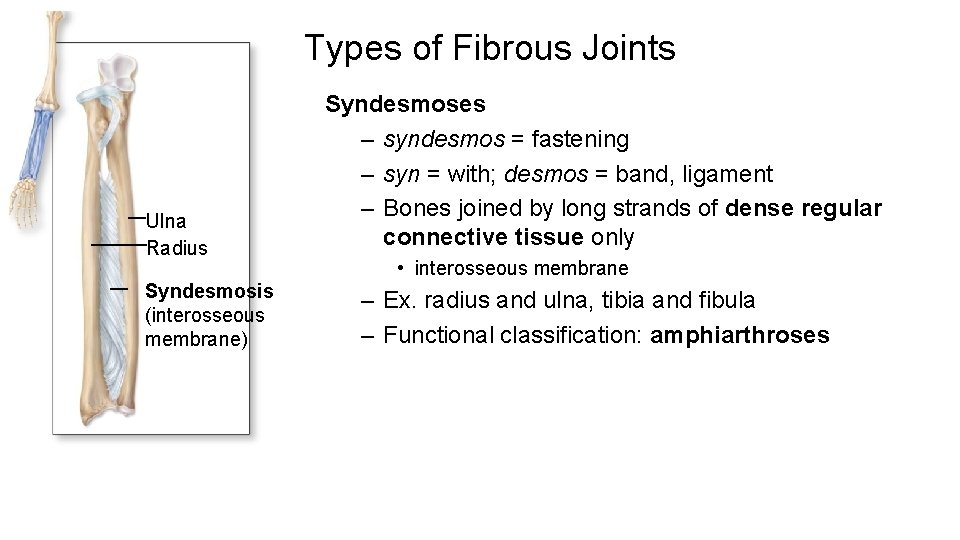
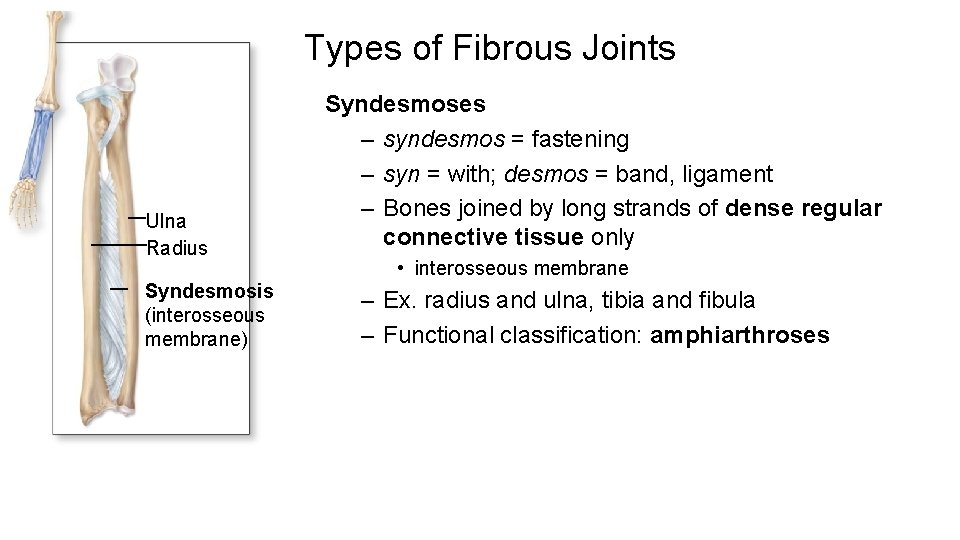
Types of Fibrous Joints Ulna Radius Syndesmosis (interosseous membrane) Syndesmoses – syndesmos = fastening – syn = with; desmos = band, ligament – Bones joined by long strands of dense regular connective tissue only • interosseous membrane – Ex. radius and ulna, tibia and fibula – Functional classification: amphiarthroses
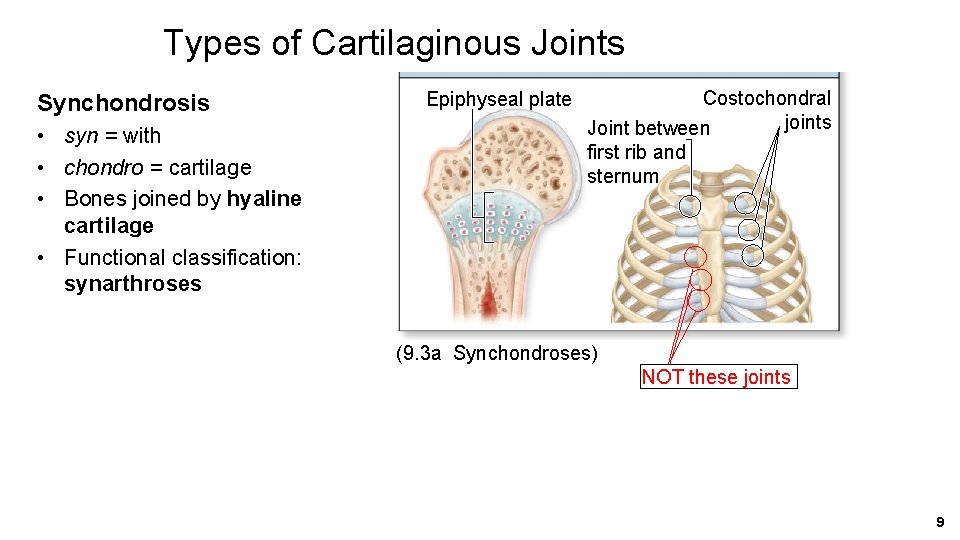
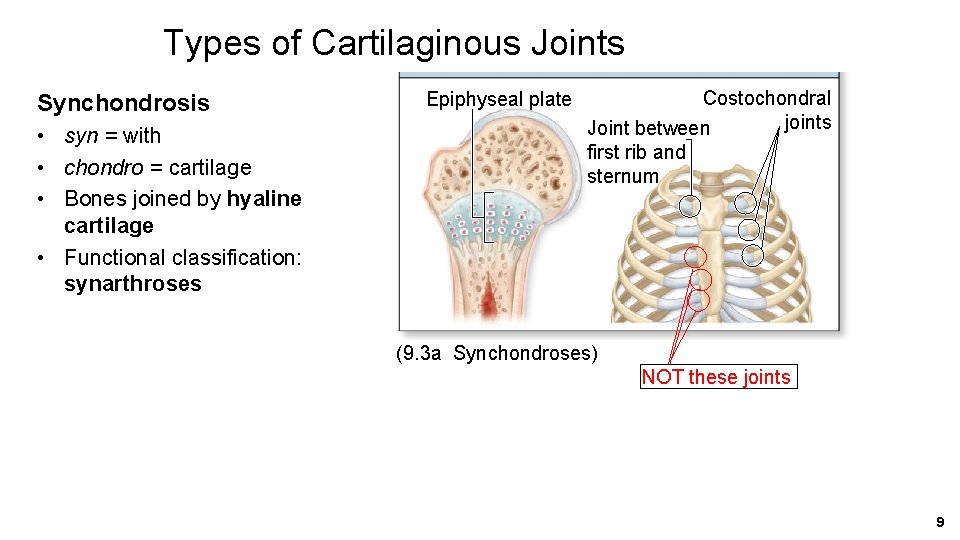
Types of Cartilaginous Joints Synchondrosis • syn = with • chondro = cartilage • Bones joined by hyaline cartilage • Functional classification: synarthroses Epiphyseal plate Costochondral joints Joint between first rib and sternum (9. 3 a Synchondroses) NOT these joints 9
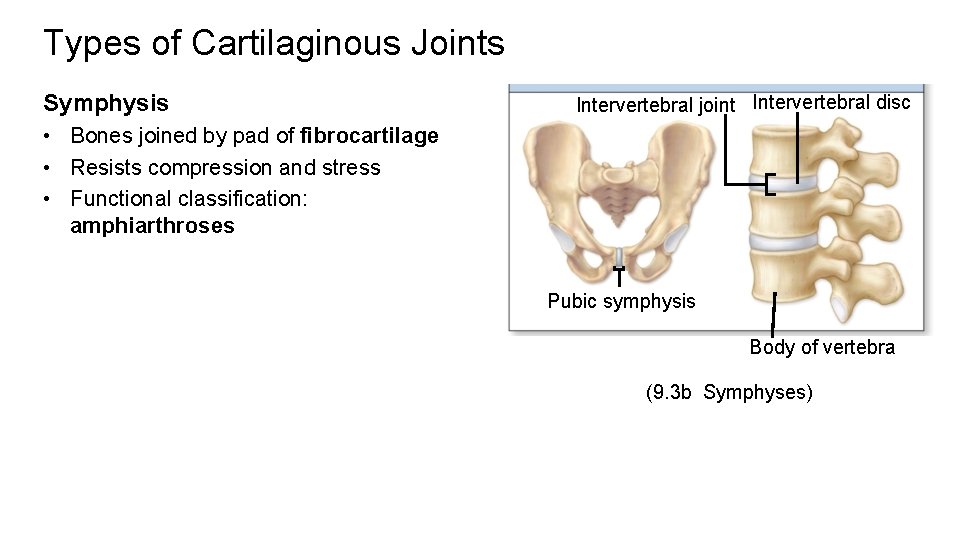
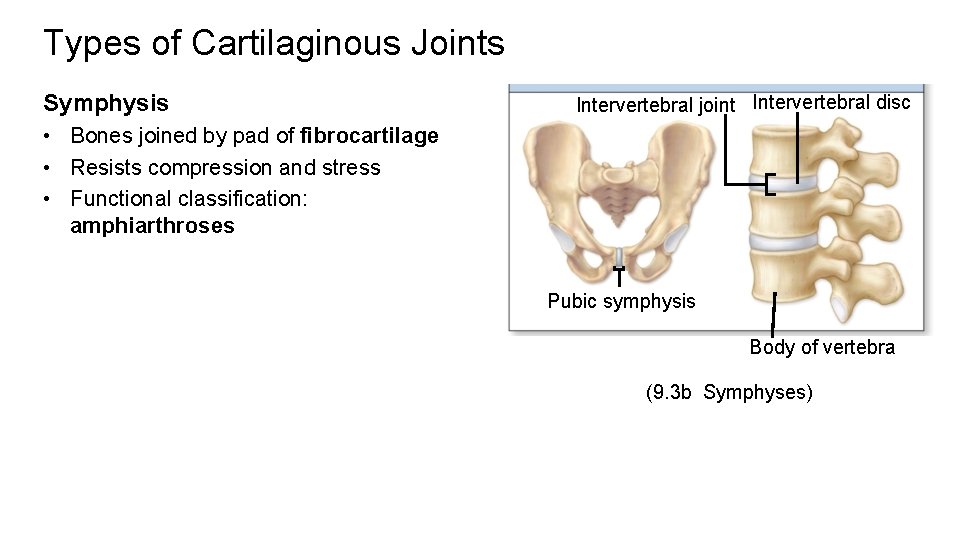
Types of Cartilaginous Joints Symphysis Intervertebral joint Intervertebral disc • Bones joined by pad of fibrocartilage • Resists compression and stress • Functional classification: amphiarthroses Pubic symphysis Body of vertebra (9. 3 b Symphyses)
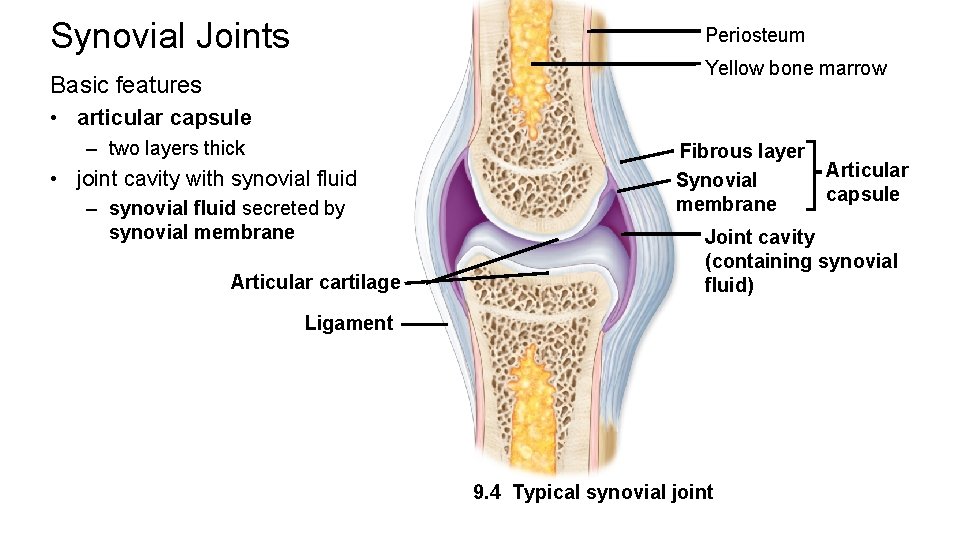
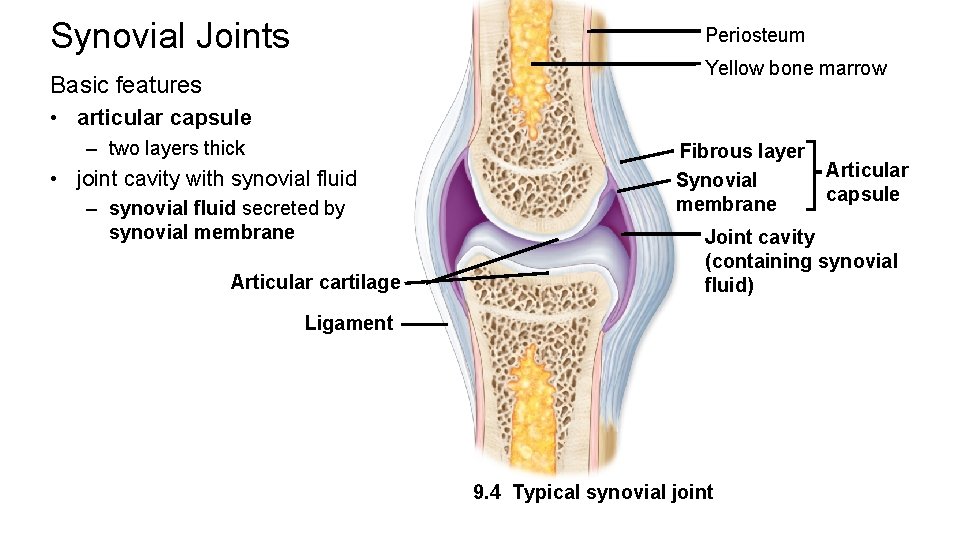
Synovial Joints Periosteum Yellow bone marrow Basic features • articular capsule – two layers thick • joint cavity with synovial fluid – synovial fluid secreted by synovial membrane Articular cartilage Fibrous layer Synovial membrane Articular capsule Joint cavity (containing synovial fluid) Ligament 9. 4 Typical synovial joint
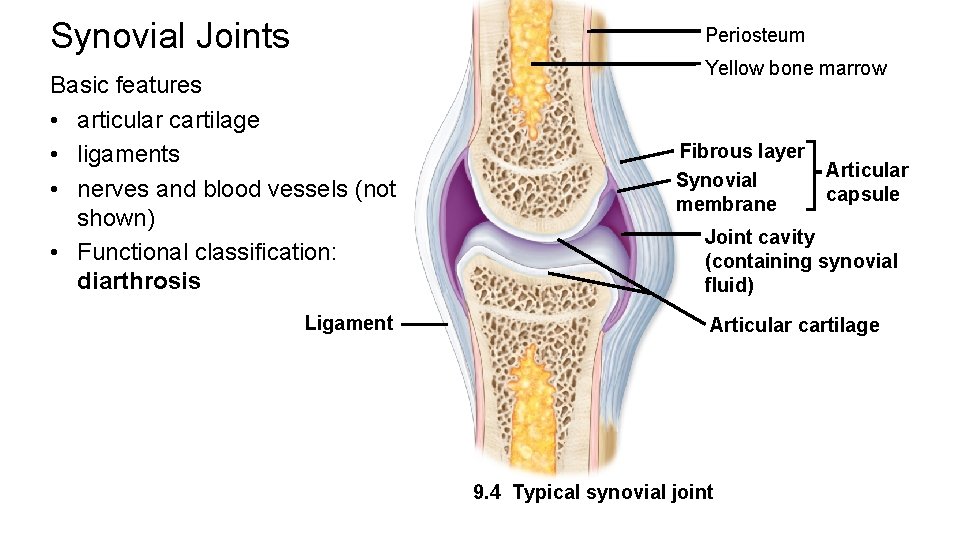
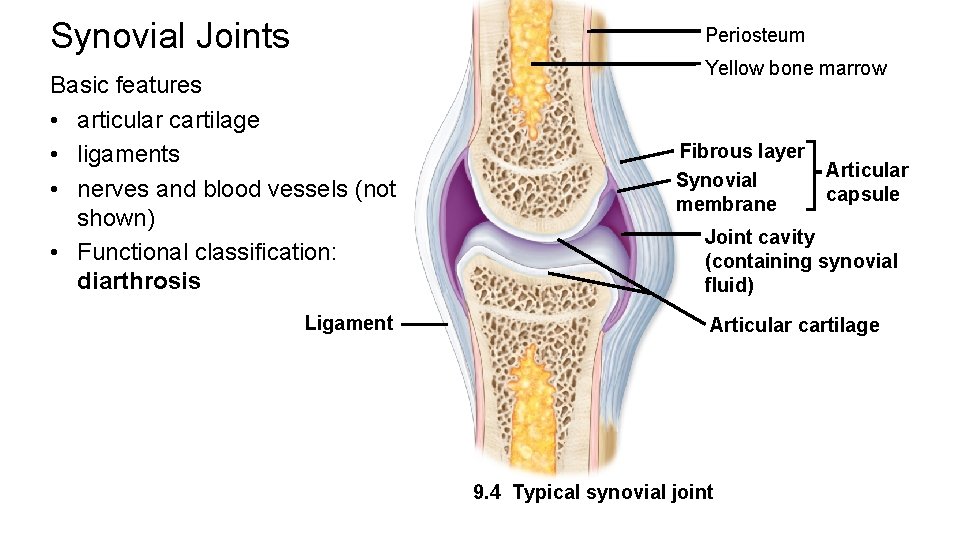
Synovial Joints Periosteum Basic features • articular cartilage • ligaments • nerves and blood vessels (not shown) • Functional classification: diarthrosis Ligament Yellow bone marrow Fibrous layer Synovial membrane Articular capsule Joint cavity (containing synovial fluid) Articular cartilage 9. 4 Typical synovial joint
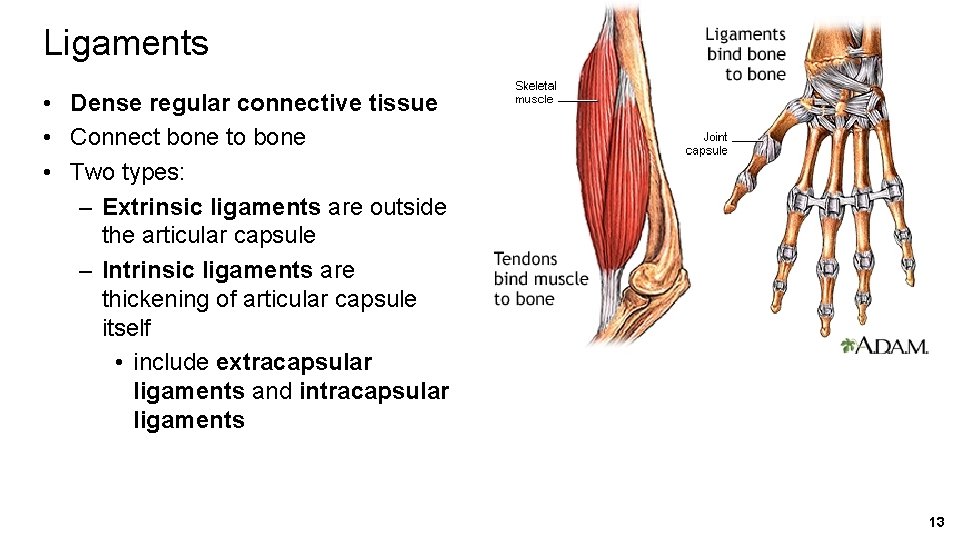
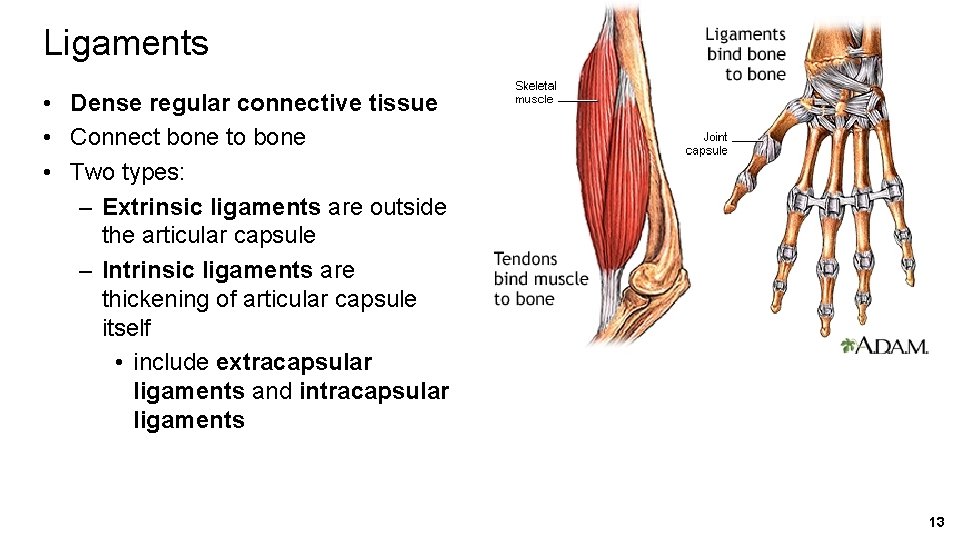
Ligaments • Dense regular connective tissue • Connect bone to bone • Two types: – Extrinsic ligaments are outside the articular capsule – Intrinsic ligaments are thickening of articular capsule itself • include extracapsular ligaments and intracapsular ligaments 13
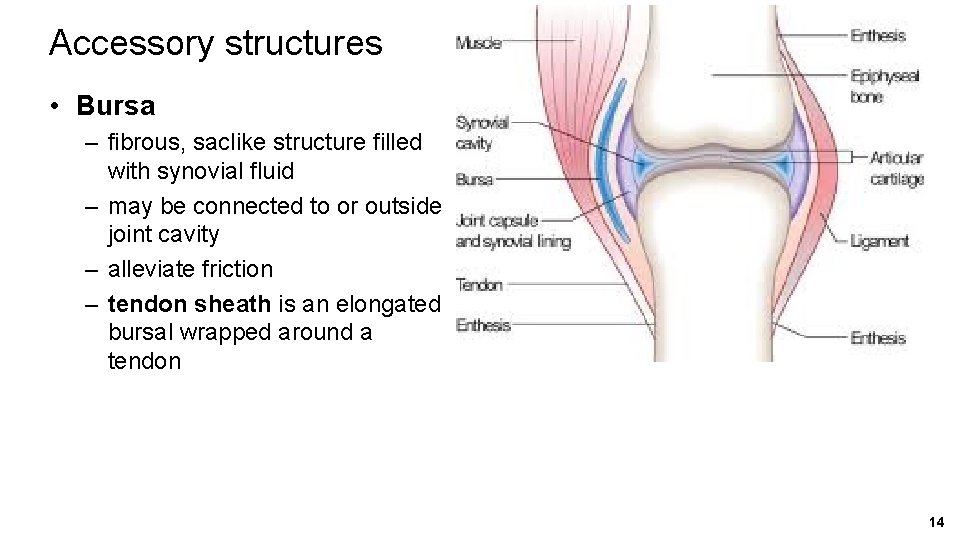
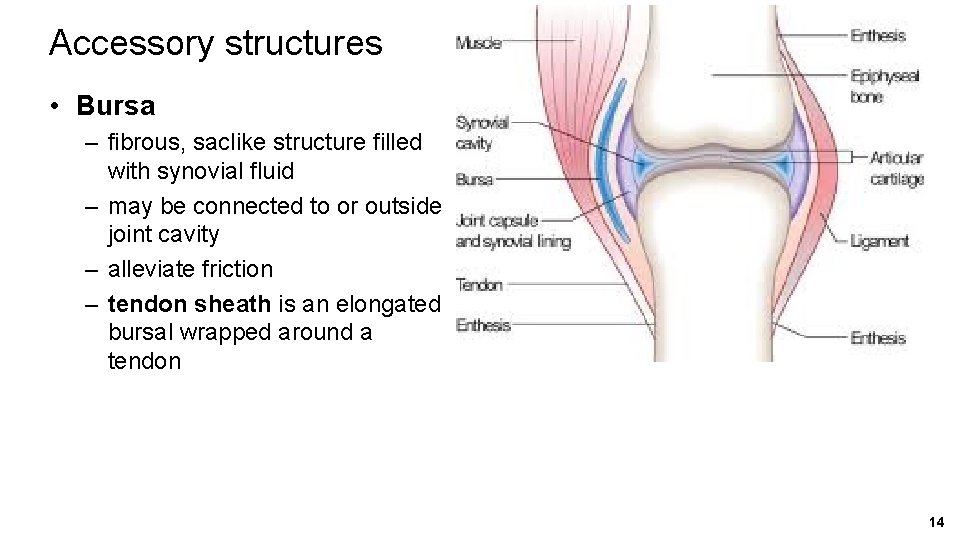
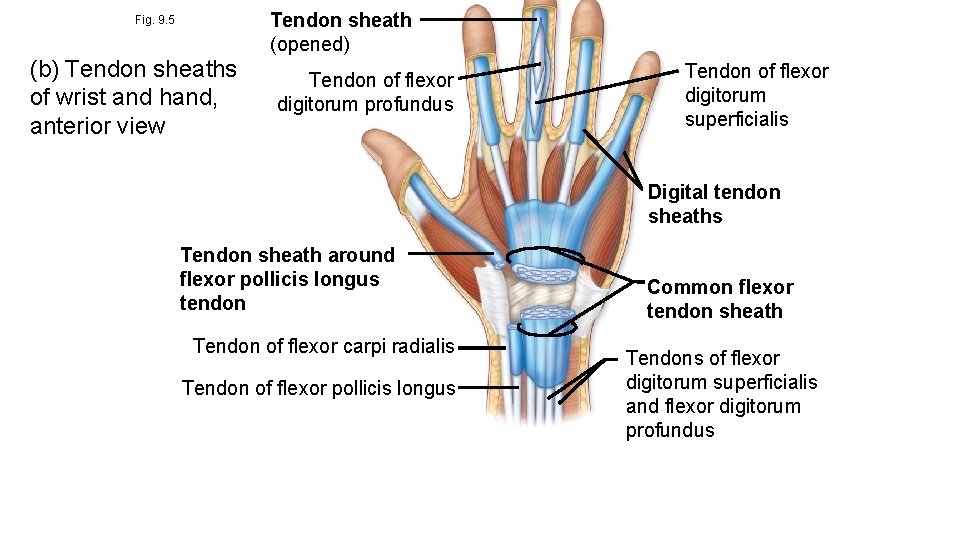
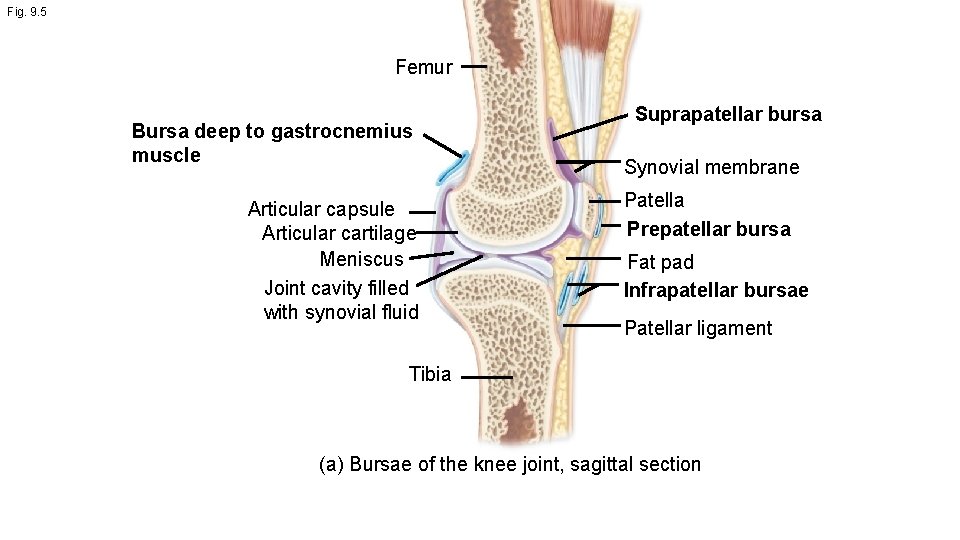
Accessory structures • Bursa – fibrous, saclike structure filled with synovial fluid – may be connected to or outside joint cavity – alleviate friction – tendon sheath is an elongated bursal wrapped around a tendon 14
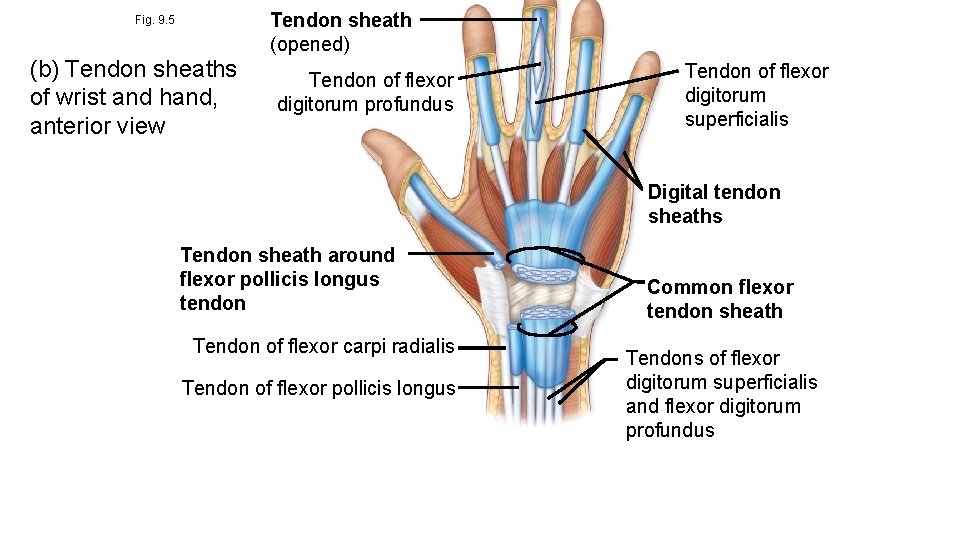
Fig. 9. 5 (b) Tendon sheaths of wrist and hand, anterior view Tendon sheath (opened) Tendon of flexor digitorum profundus Tendon of flexor digitorum superficialis Digital tendon sheaths Tendon sheath around flexor pollicis longus tendon Tendon of flexor carpi radialis Tendon of flexor pollicis longus Common flexor tendon sheath Tendons of flexor digitorum superficialis and flexor digitorum profundus
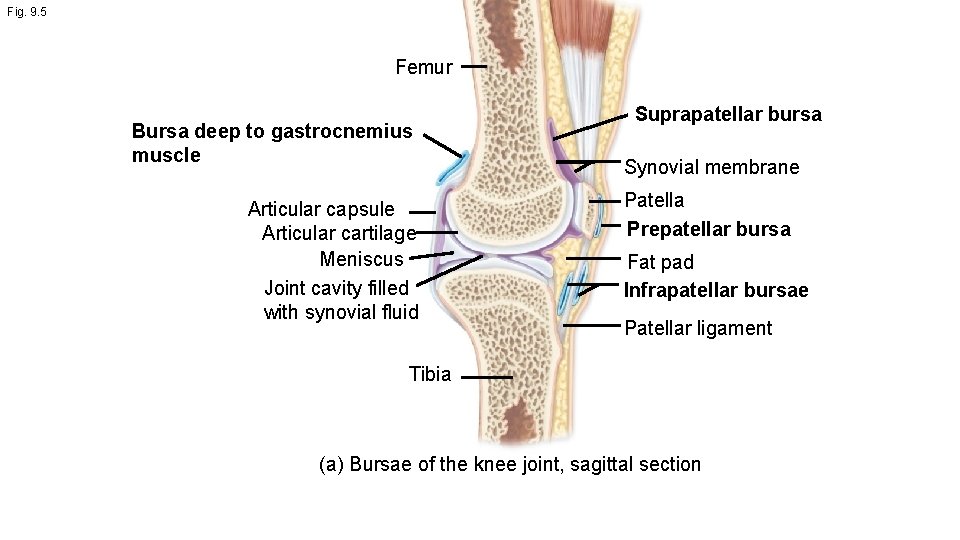
Fig. 9. 5 Femur Bursa deep to gastrocnemius muscle Articular capsule Articular cartilage Meniscus Joint cavity filled with synovial fluid Suprapatellar bursa Synovial membrane Patella Prepatellar bursa Fat pad Infrapatellar bursae Patellar ligament Tibia (a) Bursae of the knee joint, sagittal section
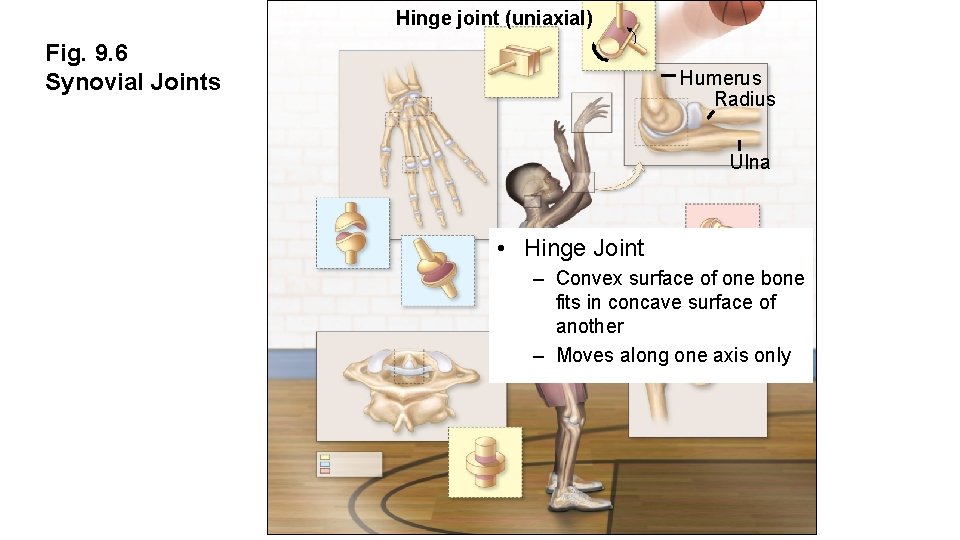
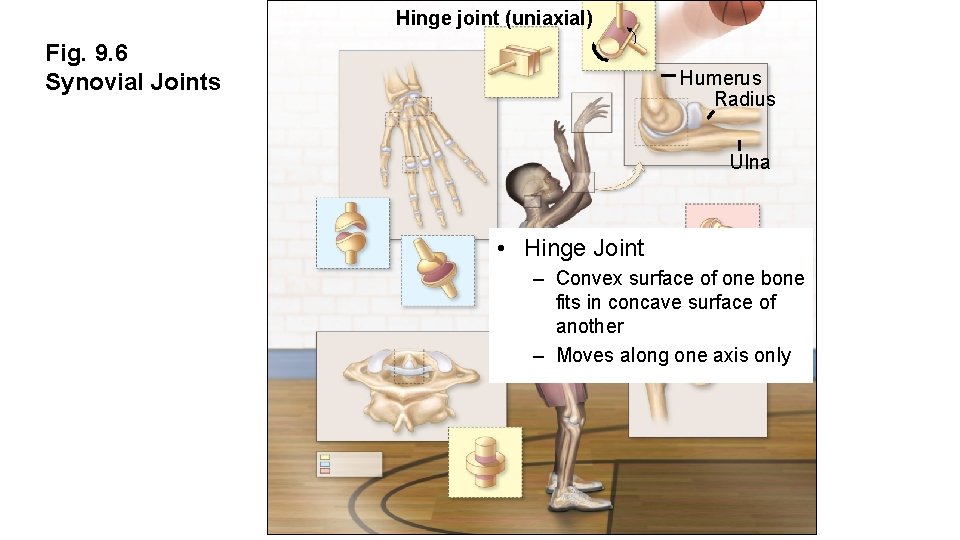
Hinge joint (uniaxial) Fig. 9. 6 Synovial Joints Humerus Radius Ulna • Hinge Joint – Convex surface of one bone fits in concave surface of another – Moves along one axis only
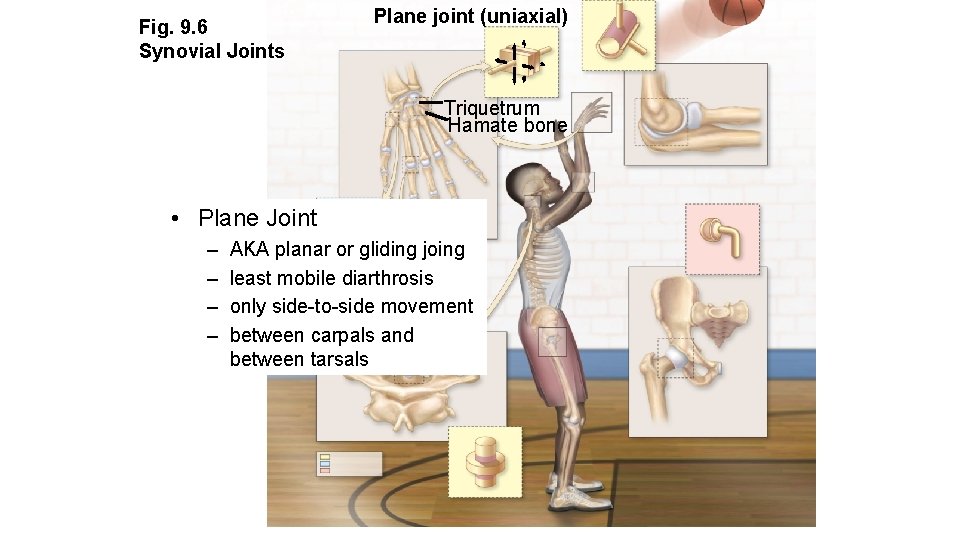
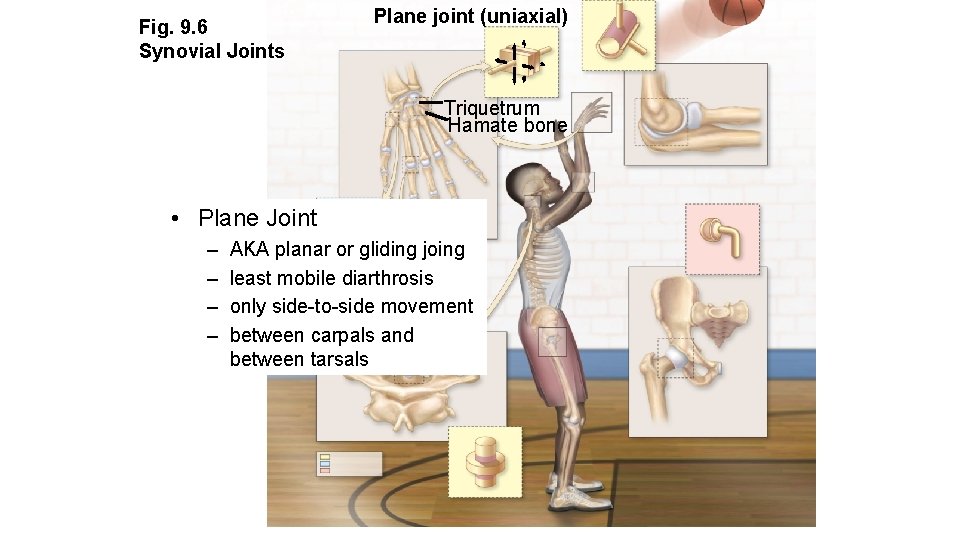
Fig. 9. 6 Synovial Joints Plane joint (uniaxial) Triquetrum Hamate bone • Plane Joint – – AKA planar or gliding joing least mobile diarthrosis only side-to-side movement between carpals and between tarsals
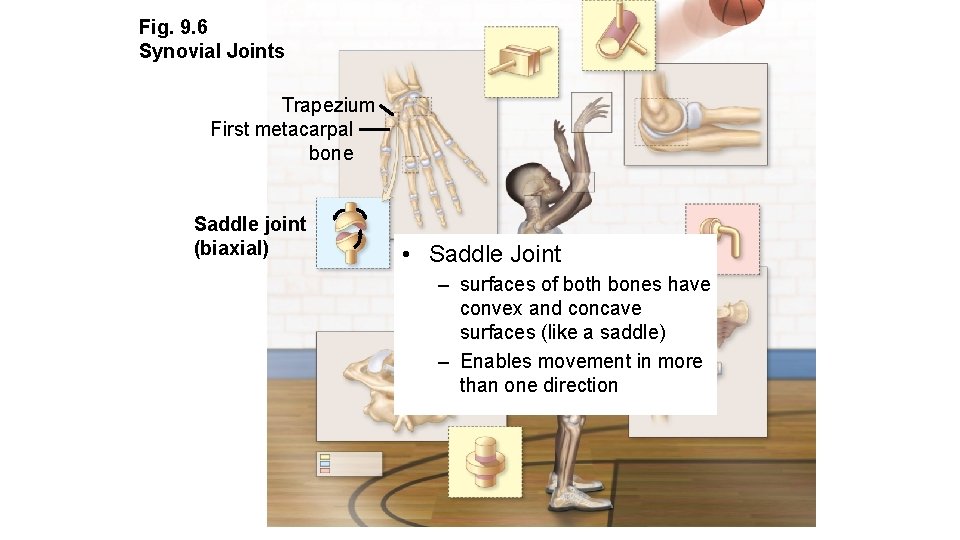
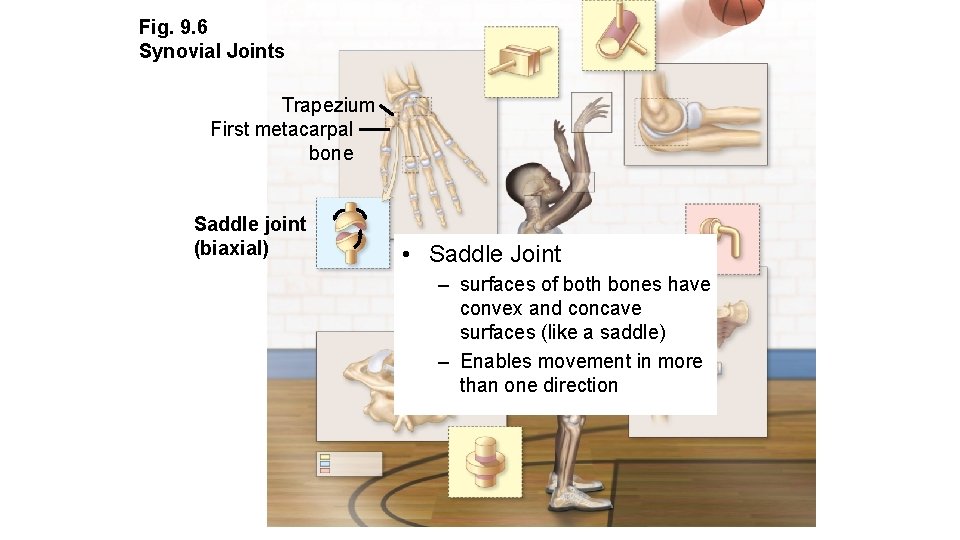
Fig. 9. 6 Synovial Joints Trapezium First metacarpal bone Saddle joint (biaxial) • Saddle Joint – surfaces of both bones have convex and concave surfaces (like a saddle) – Enables movement in more than one direction
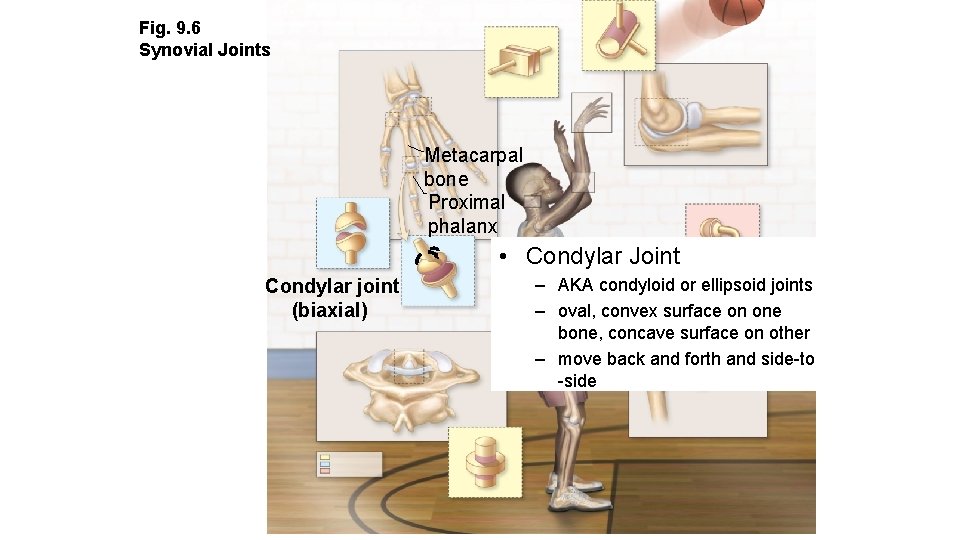
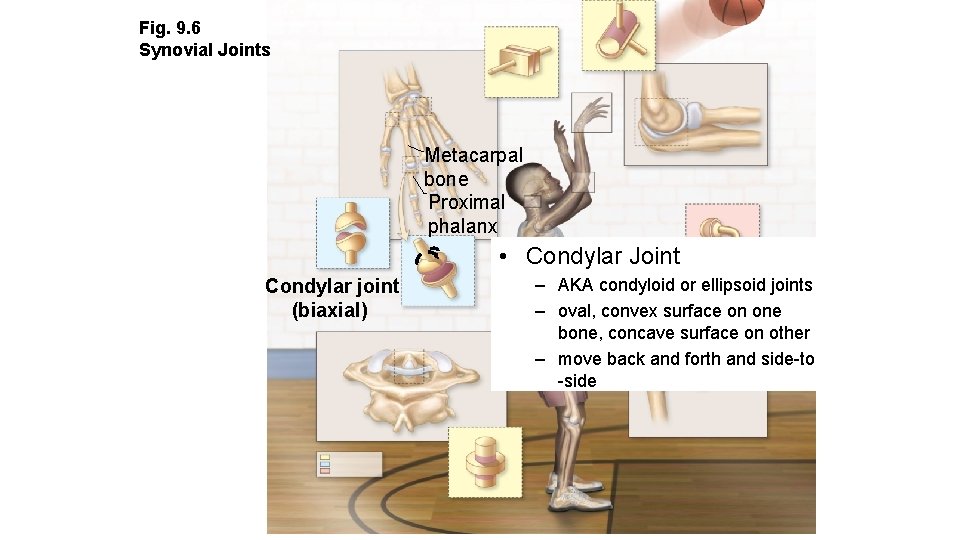
Fig. 9. 6 Synovial Joints Metacarpal bone Proximal phalanx • Condylar Joint Condylar joint (biaxial) – AKA condyloid or ellipsoid joints – oval, convex surface on one bone, concave surface on other – move back and forth and side-to -side
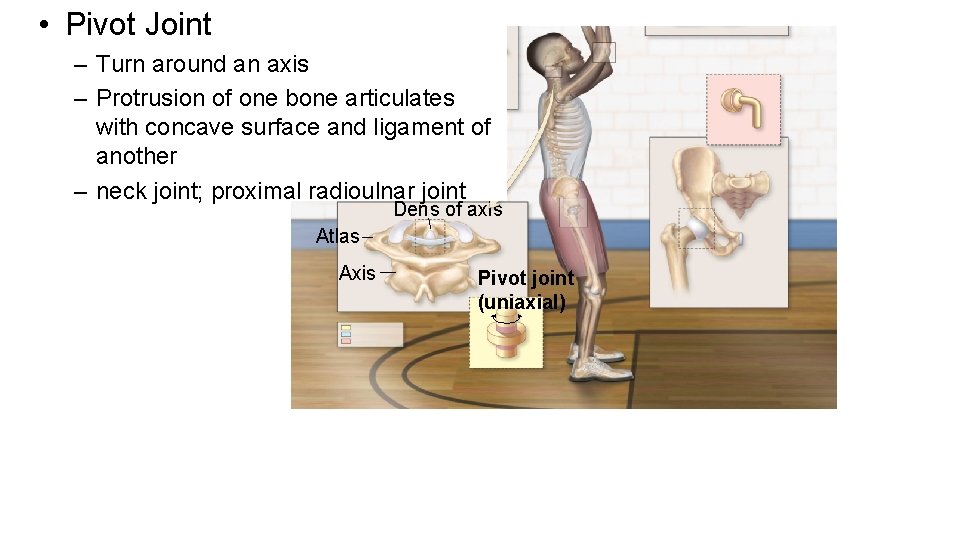
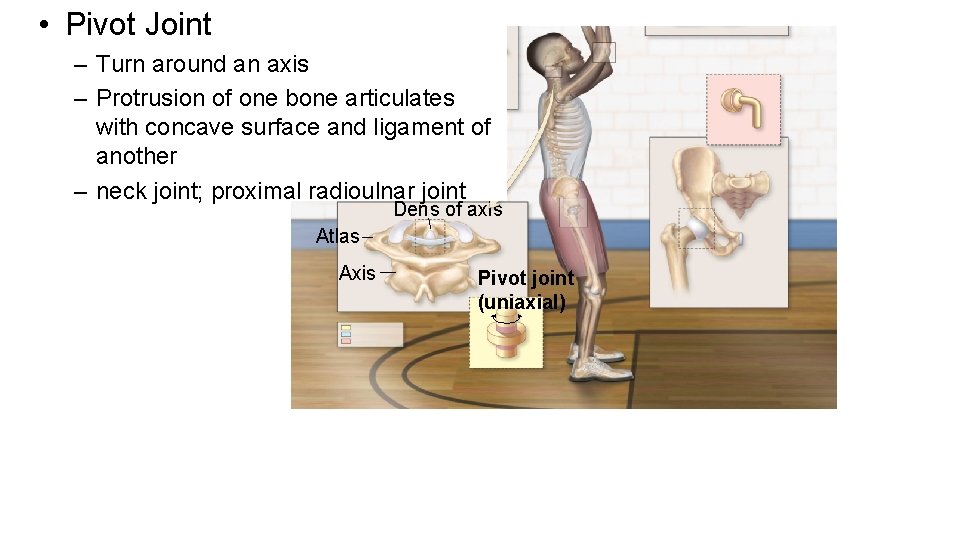
• Pivot Joint – Turn around an axis – Protrusion of one bone articulates with concave surface and ligament of another – neck joint; proximal radioulnar joint Dens of axis Atlas Axis Pivot joint (uniaxial)
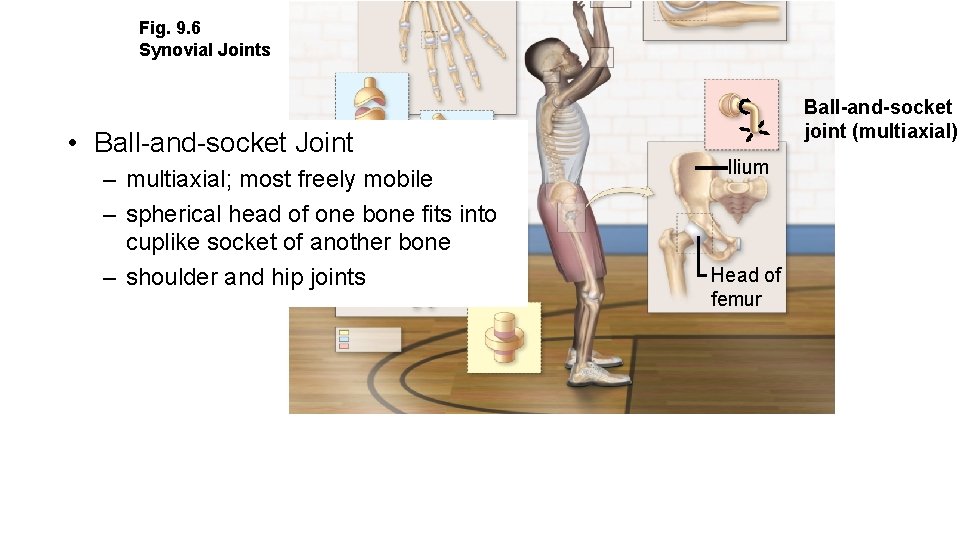
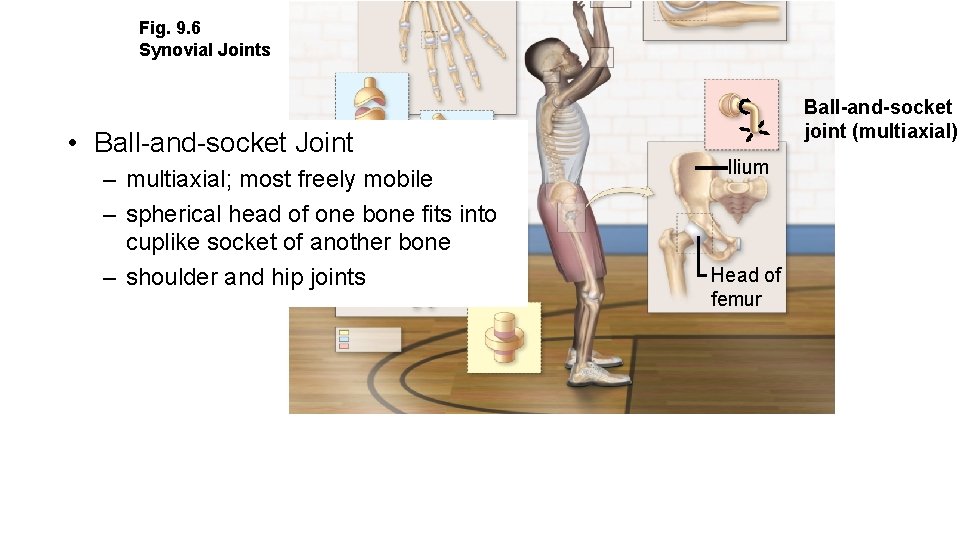
Fig. 9. 6 Synovial Joints • Ball-and-socket Joint – multiaxial; most freely mobile – spherical head of one bone fits into cuplike socket of another bone – shoulder and hip joints Ball-and-socket joint (multiaxial) Ilium Head of femur
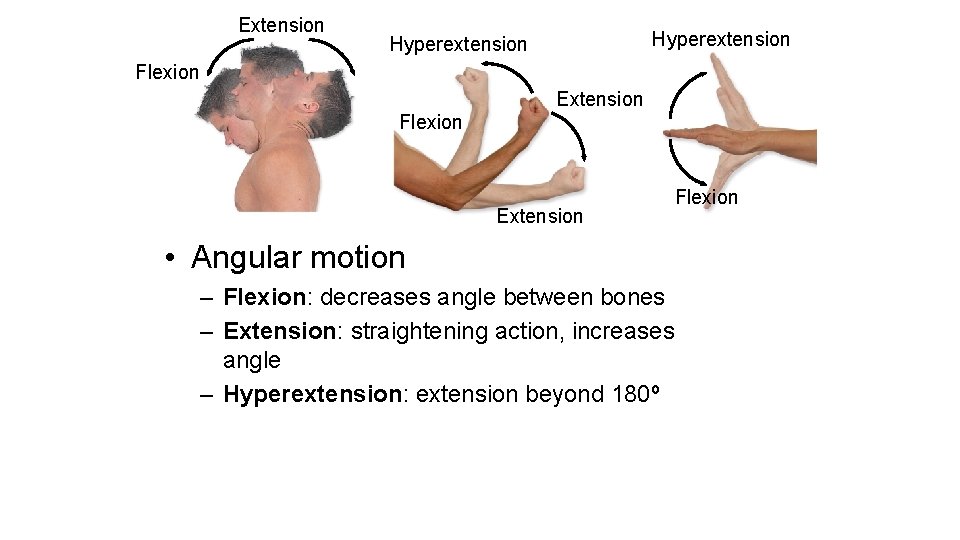
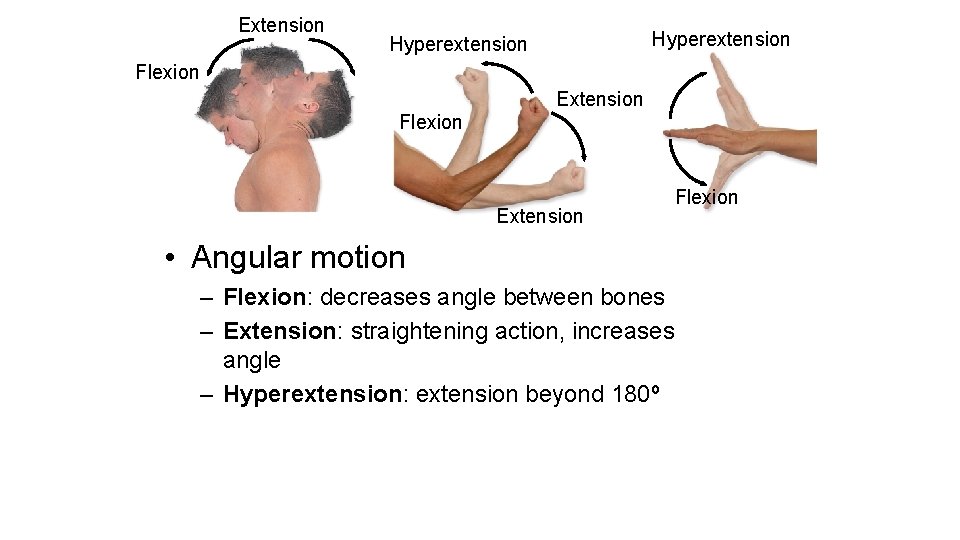
Extension Hyperextension Flexion Extension Flexion • Angular motion – Flexion: decreases angle between bones – Extension: straightening action, increases angle – Hyperextension: extension beyond 180º
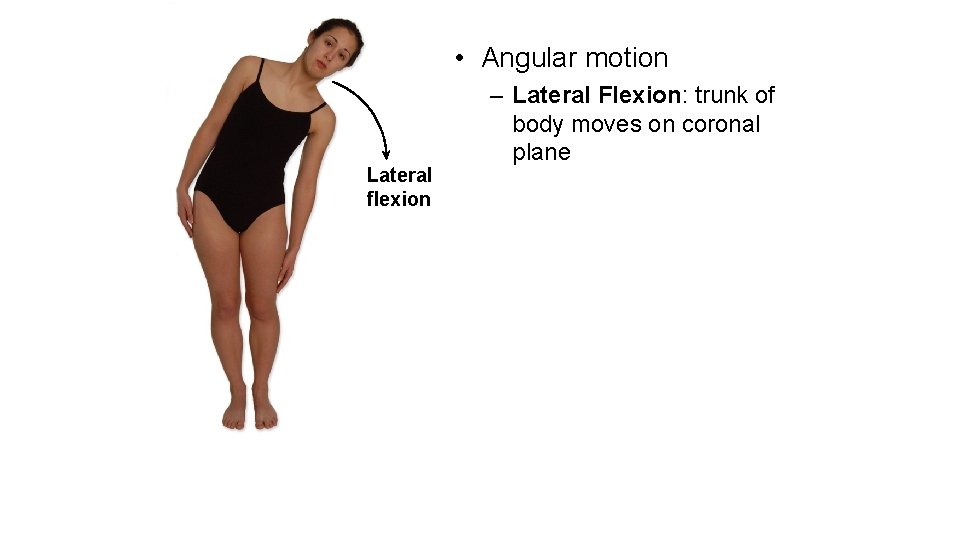
• Angular motion Lateral flexion – Lateral Flexion: trunk of body moves on coronal plane
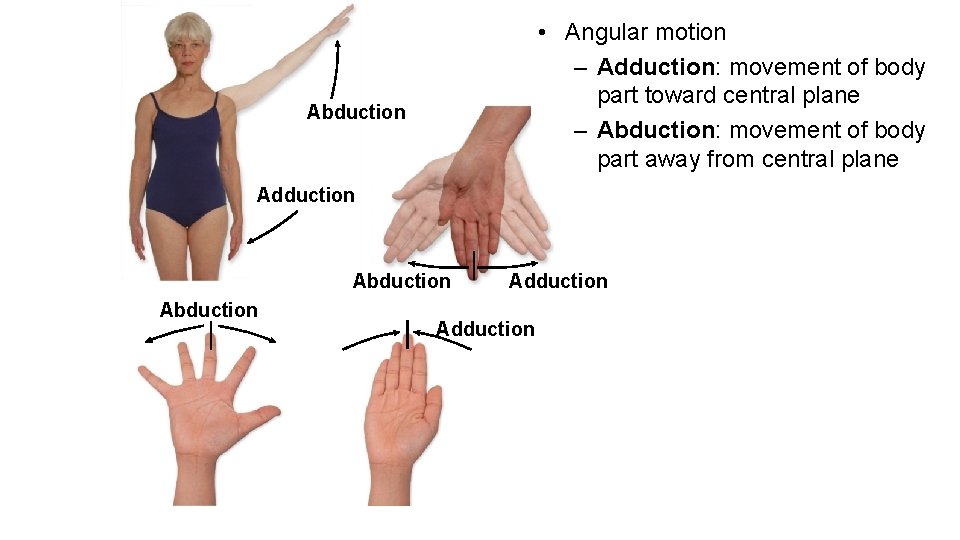
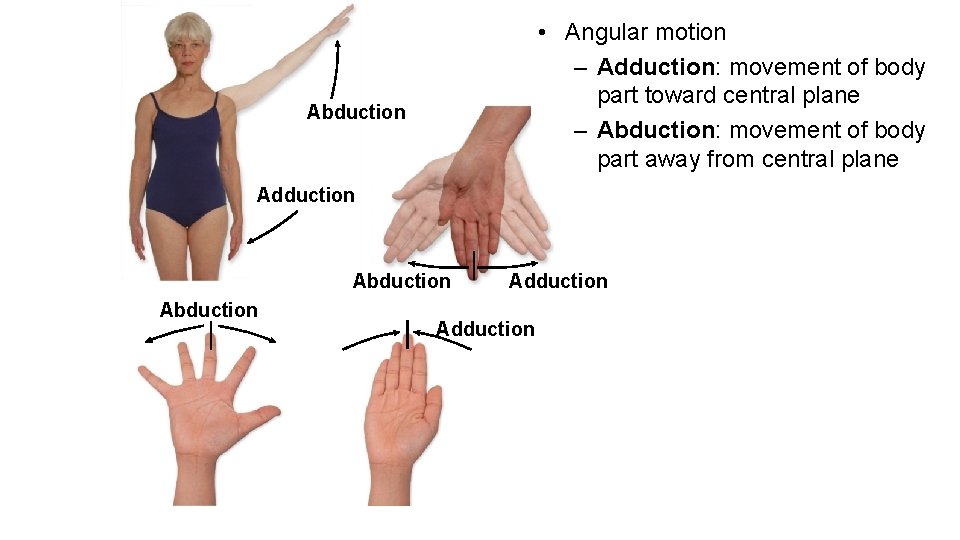
• Angular motion – Adduction: movement of body part toward central plane – Abduction: movement of body part away from central plane Abduction Adduction
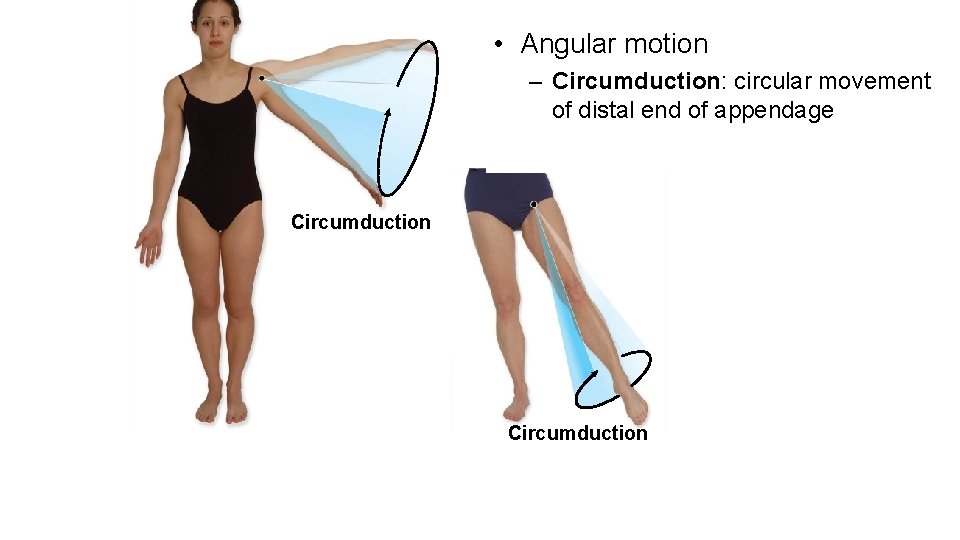
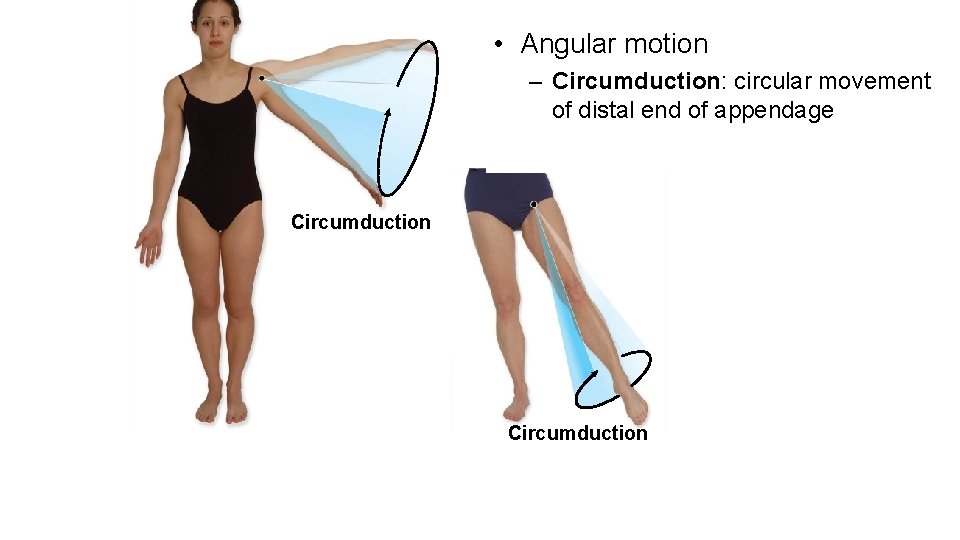
• Angular motion – Circumduction: circular movement of distal end of appendage Circumduction
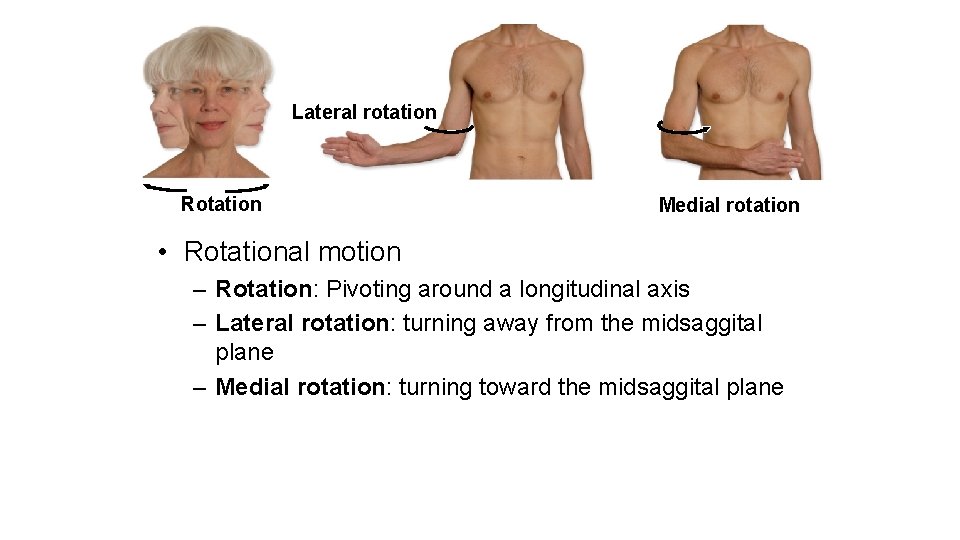
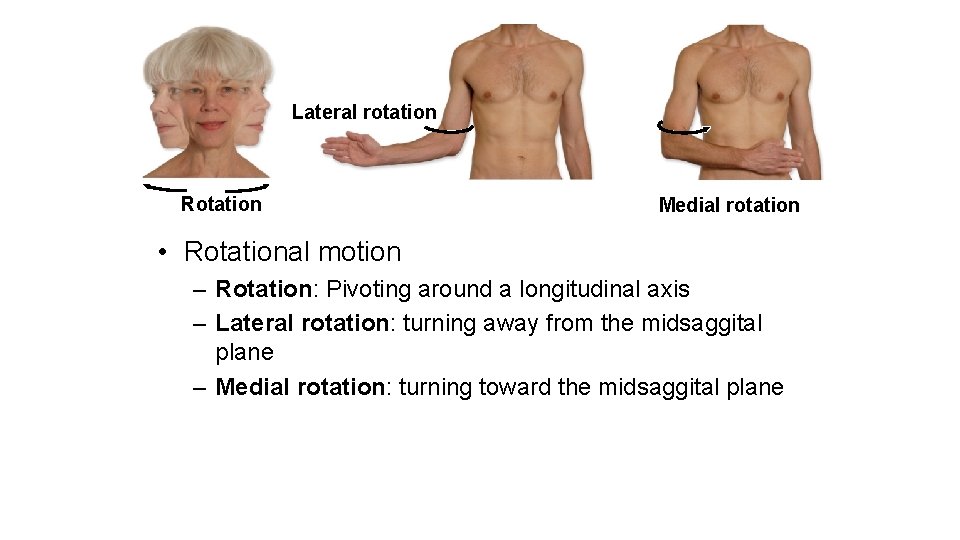
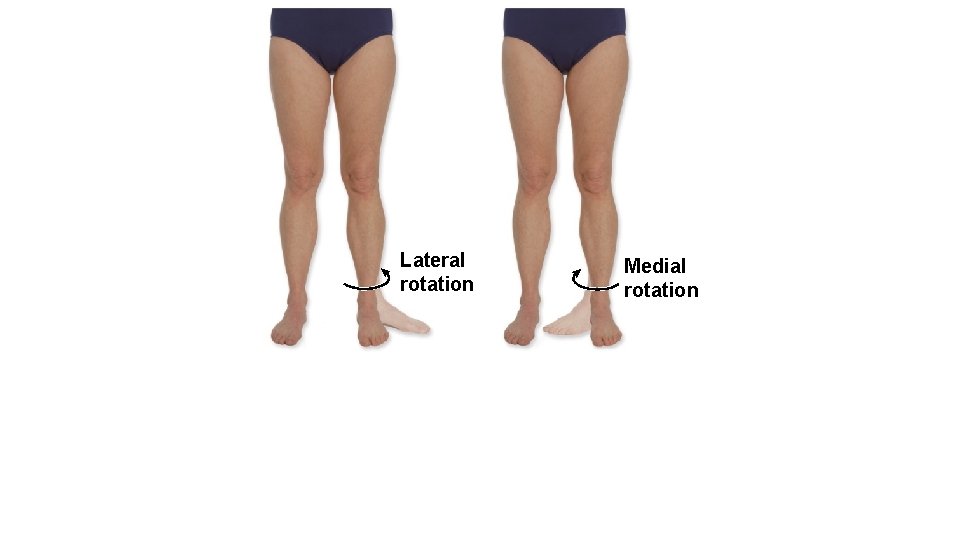
Lateral rotation Rotation Medial rotation • Rotational motion – Rotation: Pivoting around a longitudinal axis – Lateral rotation: turning away from the midsaggital plane – Medial rotation: turning toward the midsaggital plane
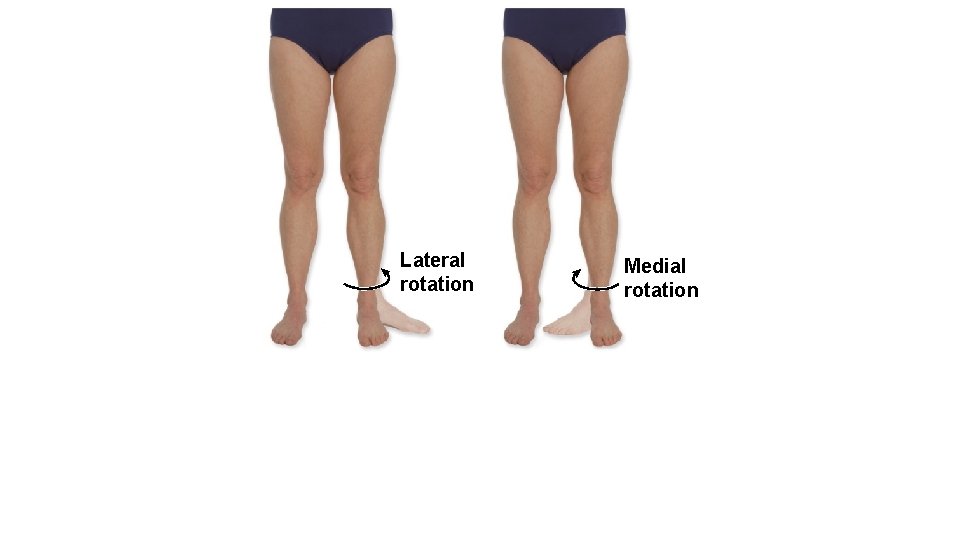
Lateral rotation Medial rotation
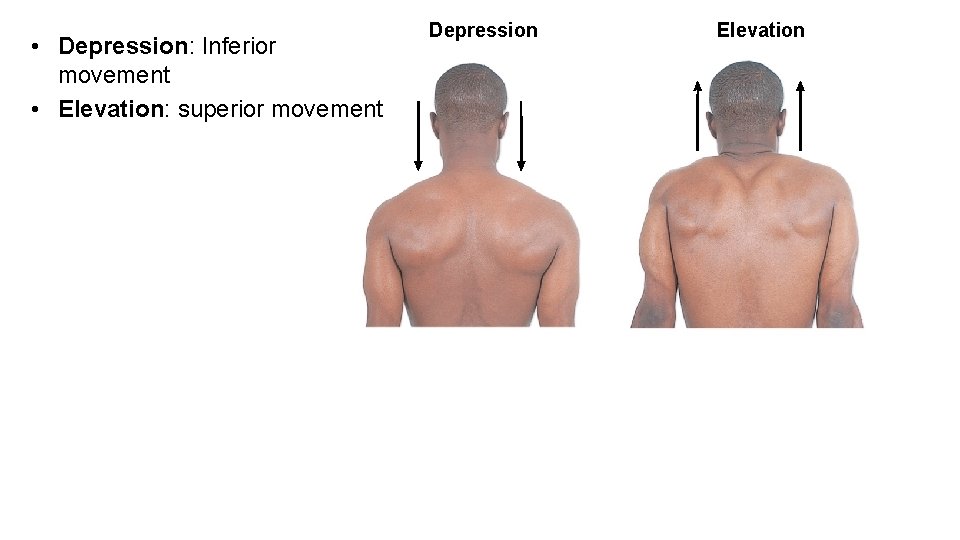
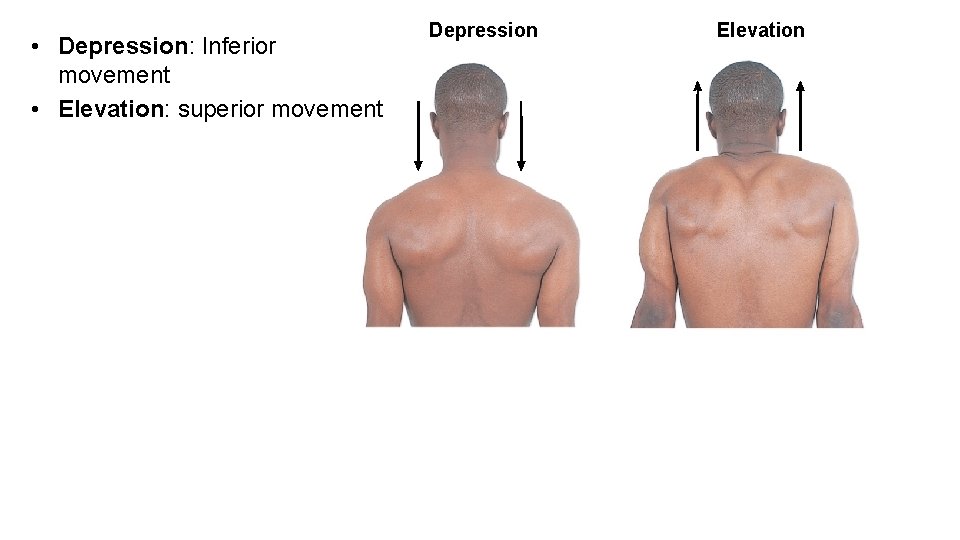
• Depression: Inferior movement • Elevation: superior movement Depression Elevation
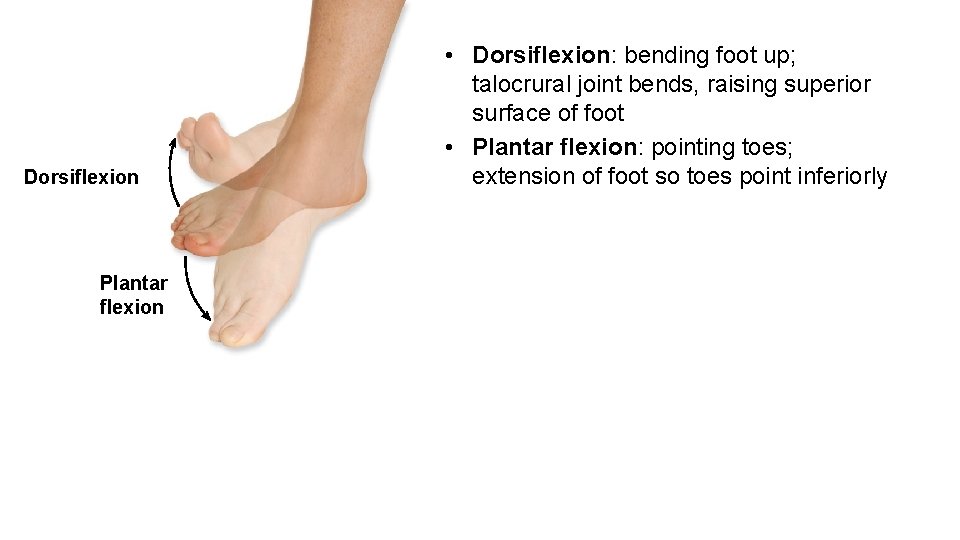
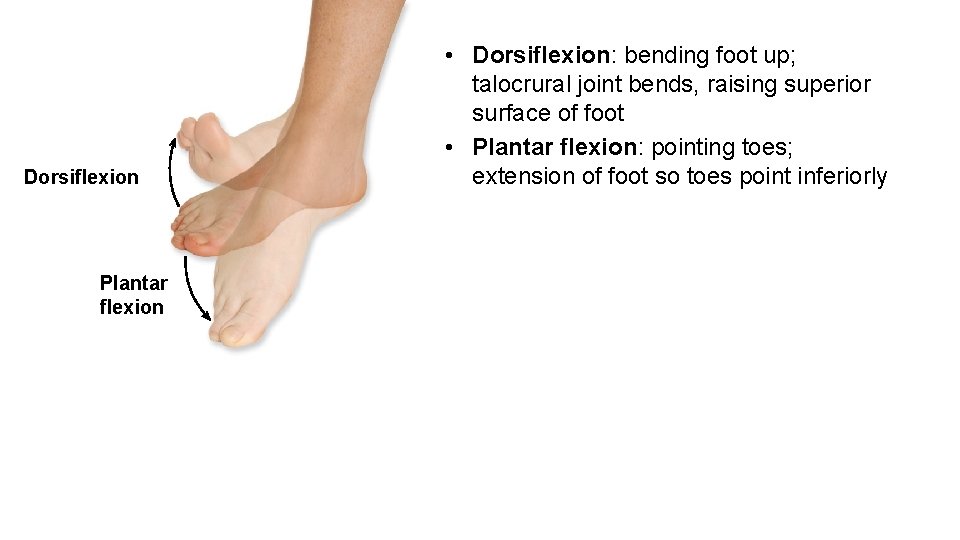
Dorsiflexion Plantar flexion • Dorsiflexion: bending foot up; talocrural joint bends, raising superior surface of foot • Plantar flexion: pointing toes; extension of foot so toes point inferiorly
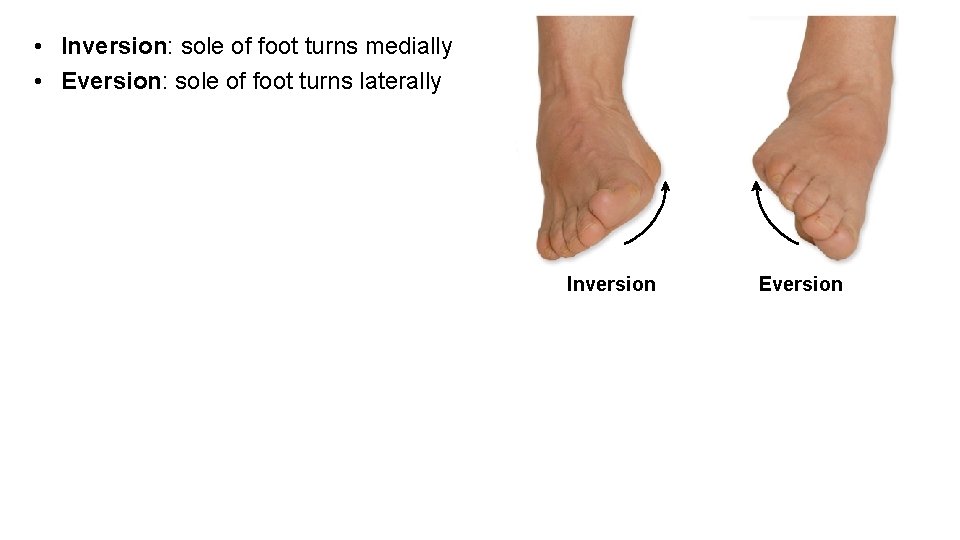
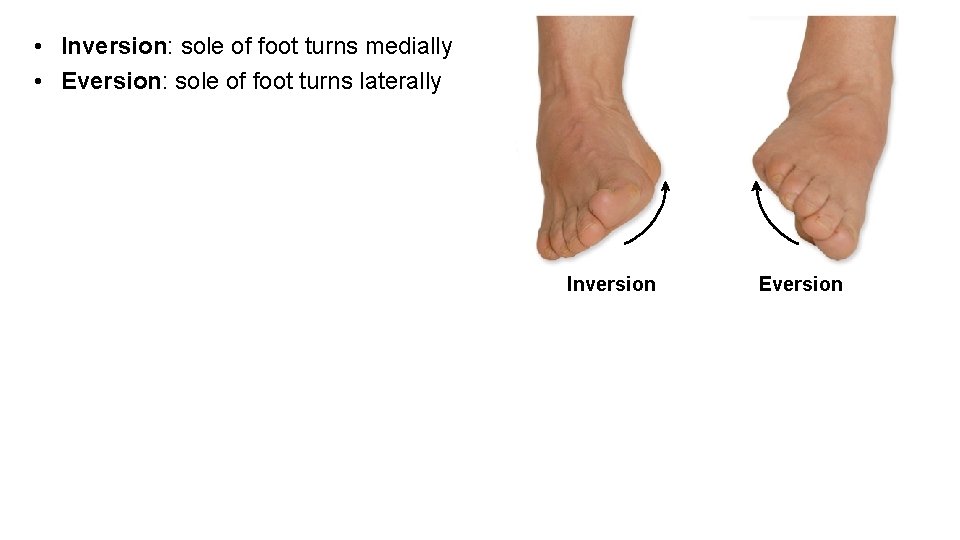
• Inversion: sole of foot turns medially • Eversion: sole of foot turns laterally Inversion Eversion
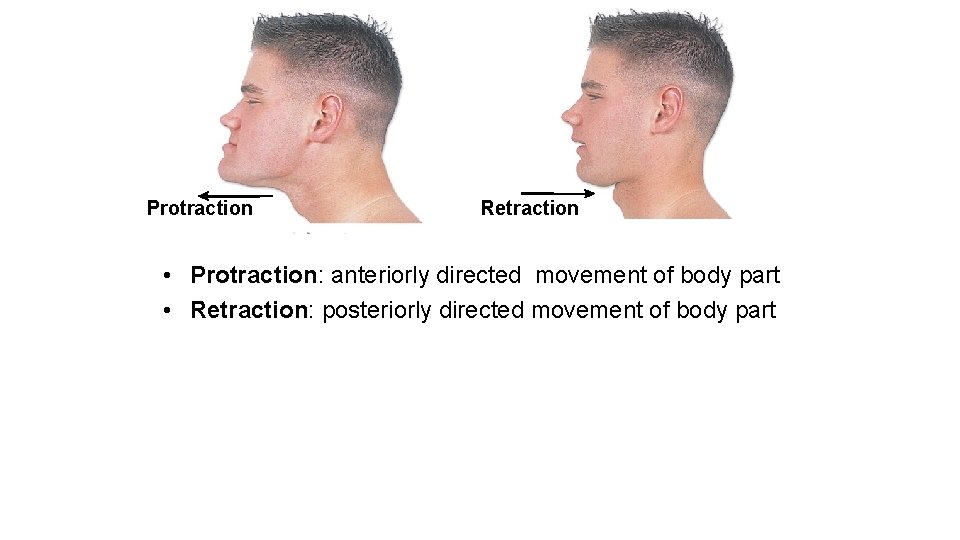
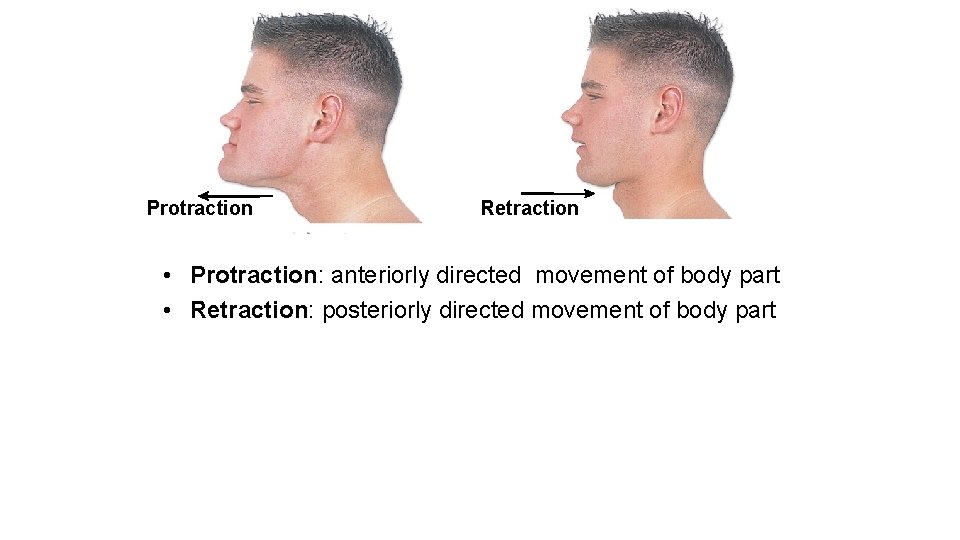
Protraction Retraction • Protraction: anteriorly directed movement of body part • Retraction: posteriorly directed movement of body part
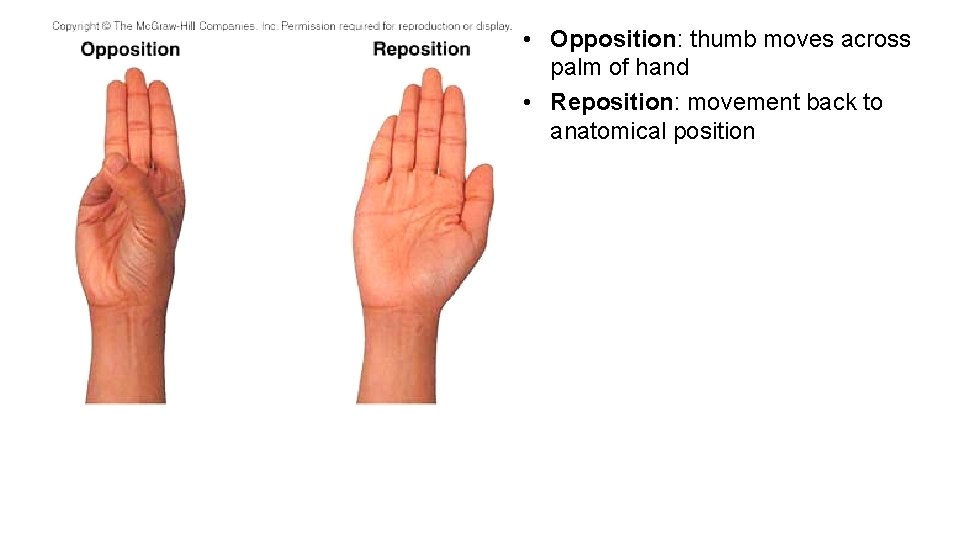
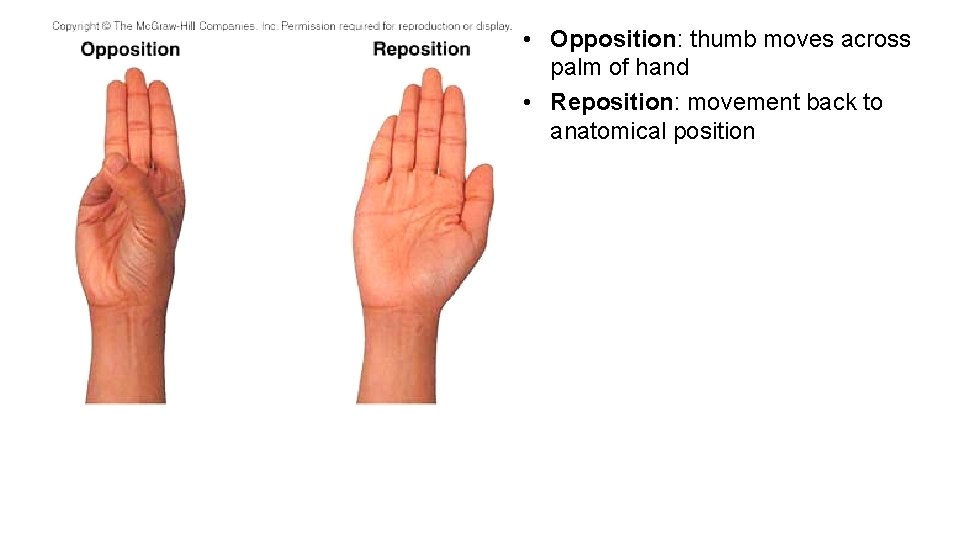
• Opposition: thumb moves across palm of hand • Reposition: movement back to anatomical position
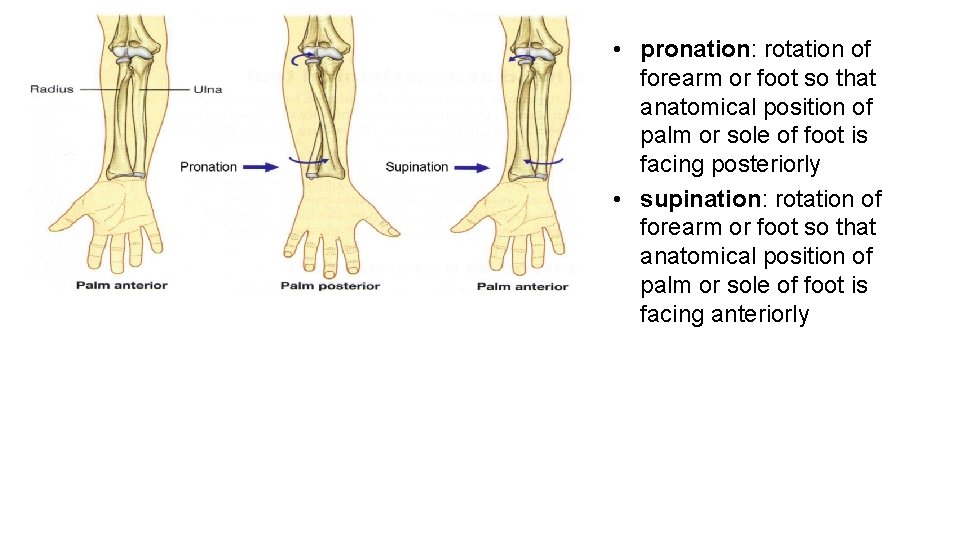
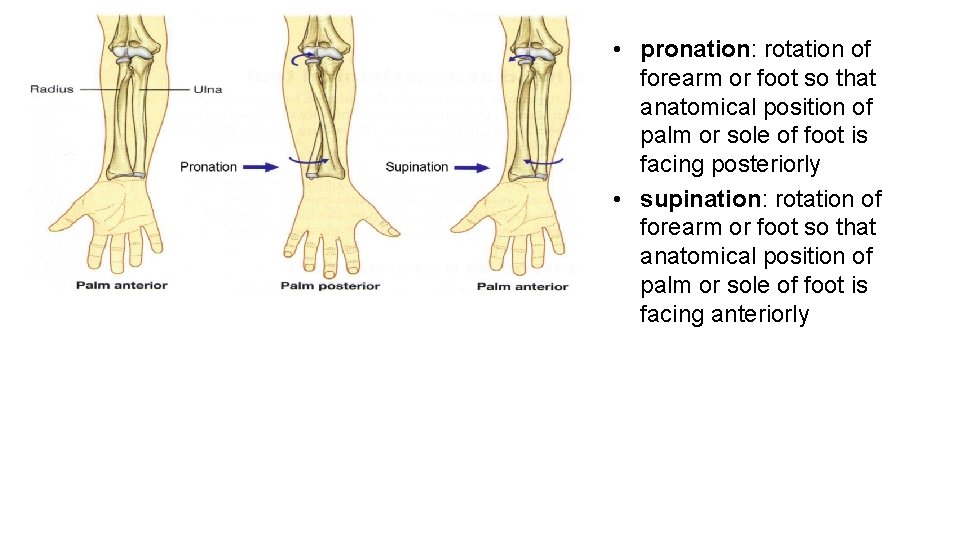
• pronation: rotation of forearm or foot so that anatomical position of palm or sole of foot is facing posteriorly • supination: rotation of forearm or foot so that anatomical position of palm or sole of foot is facing anteriorly
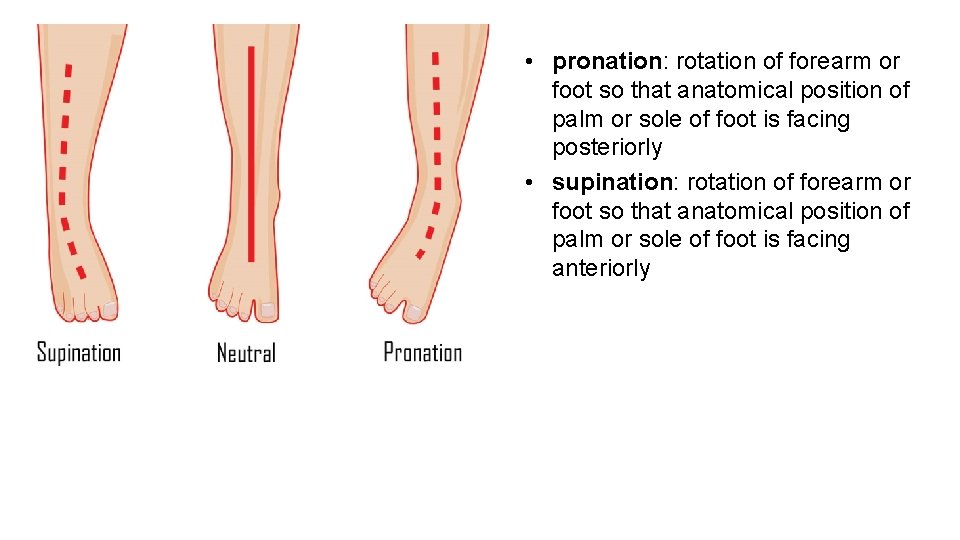
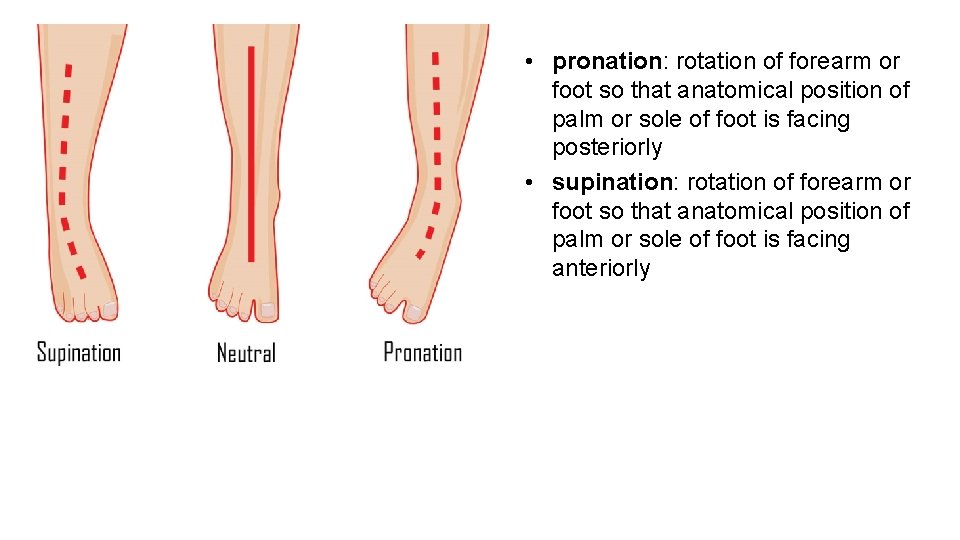
• pronation: rotation of forearm or foot so that anatomical position of palm or sole of foot is facing posteriorly • supination: rotation of forearm or foot so that anatomical position of palm or sole of foot is facing anteriorly
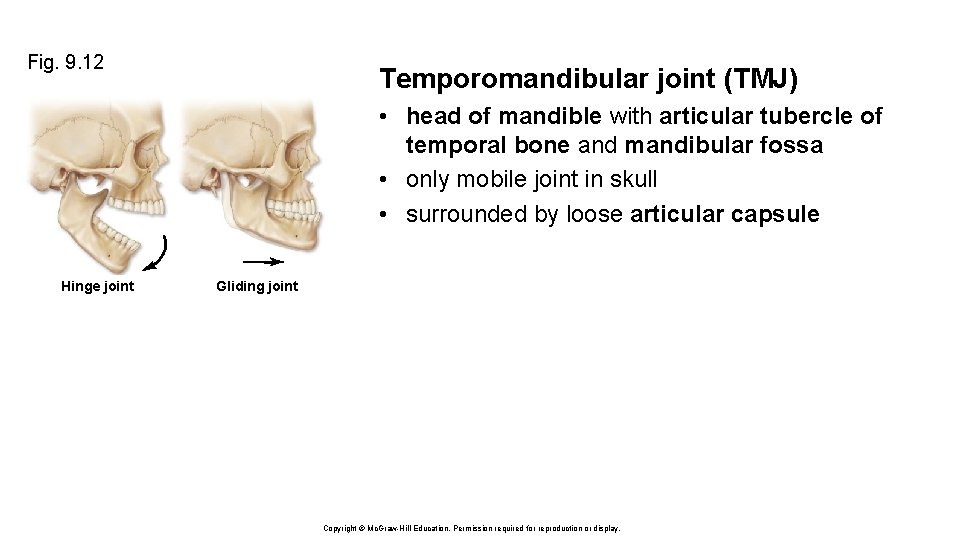
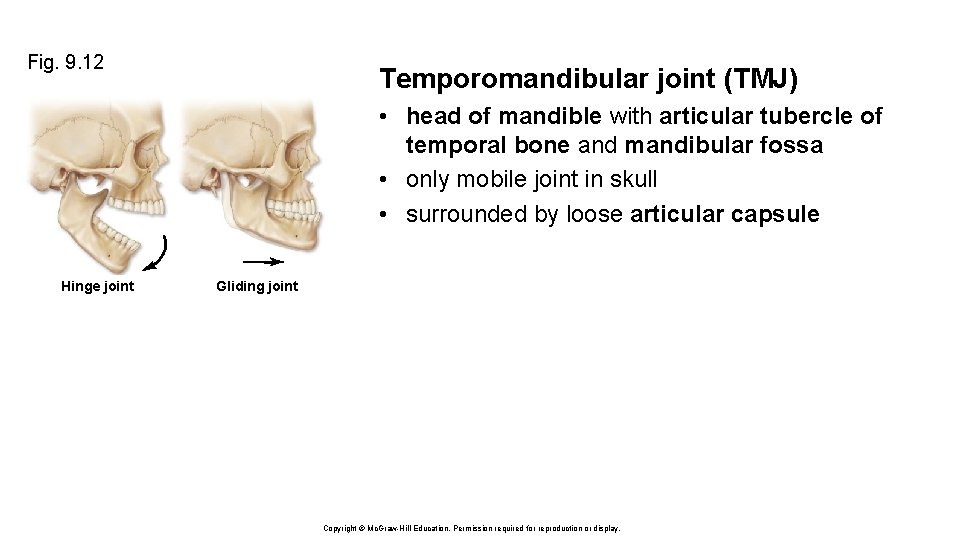
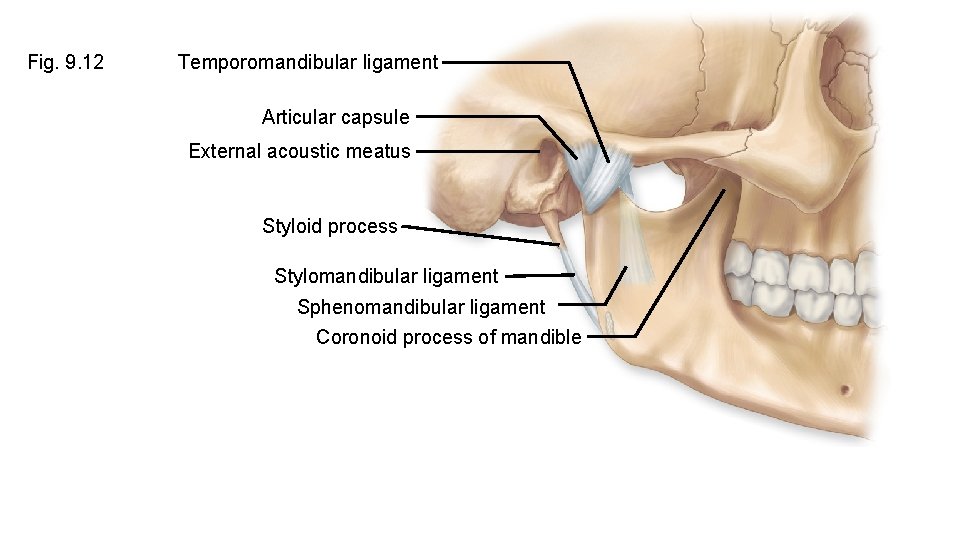
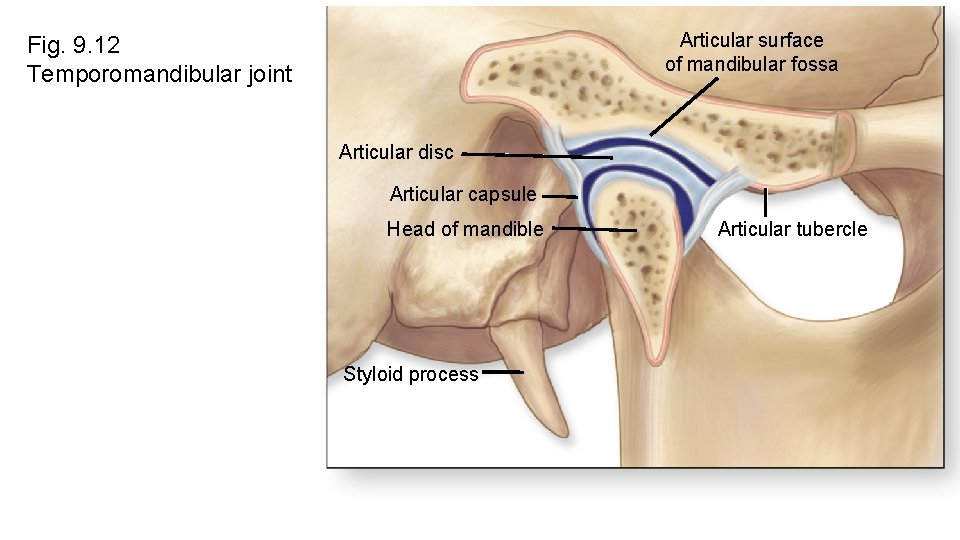
Fig. 9. 12 Temporomandibular joint (TMJ) • head of mandible with articular tubercle of temporal bone and mandibular fossa • only mobile joint in skull • surrounded by loose articular capsule Hinge joint Gliding joint Copyright © Mc. Graw-Hill Education. Permission required for reproduction or display.
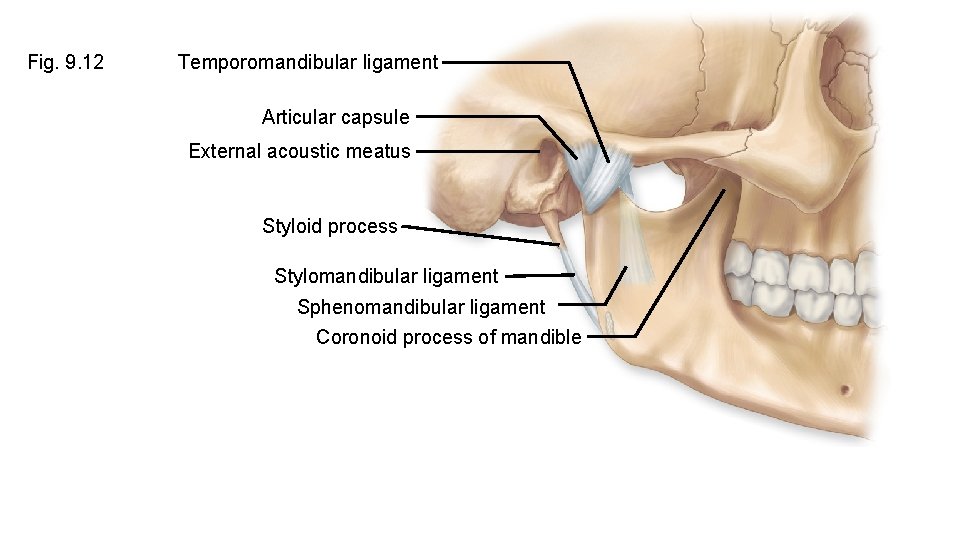
Fig. 9. 12 Temporomandibular ligament Articular capsule External acoustic meatus Styloid process Stylomandibular ligament Sphenomandibular ligament Coronoid process of mandible
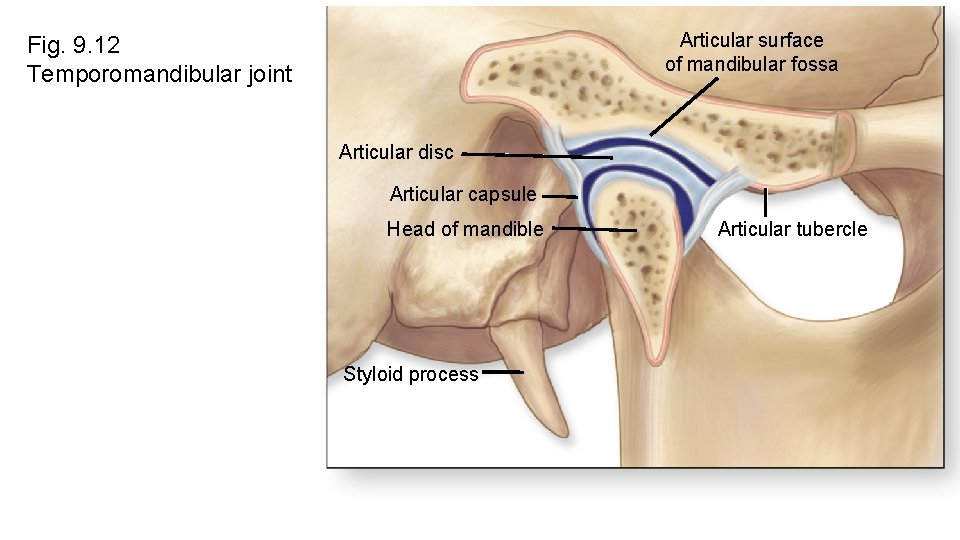
Articular surface of mandibular fossa Fig. 9. 12 Temporomandibular joint Articular disc Articular capsule Head of mandible Styloid process Articular tubercle
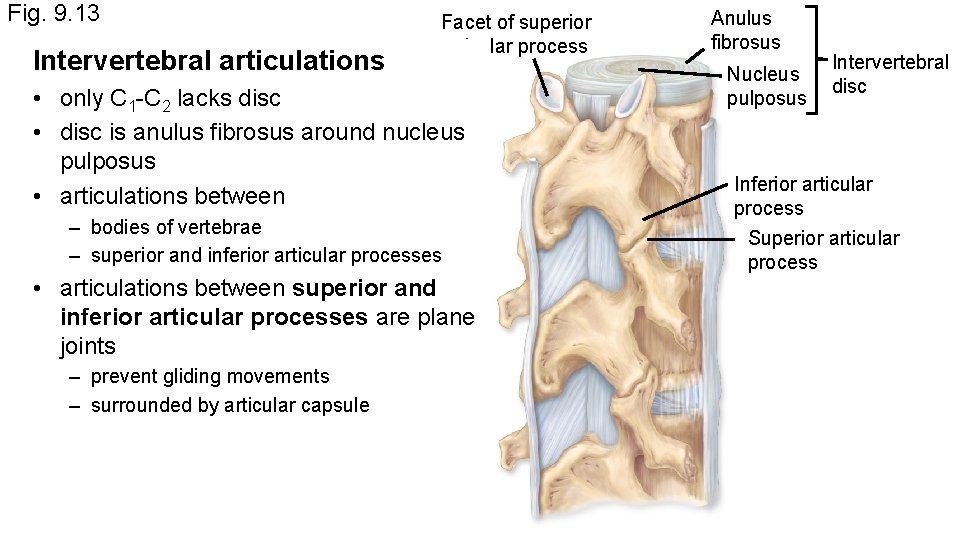
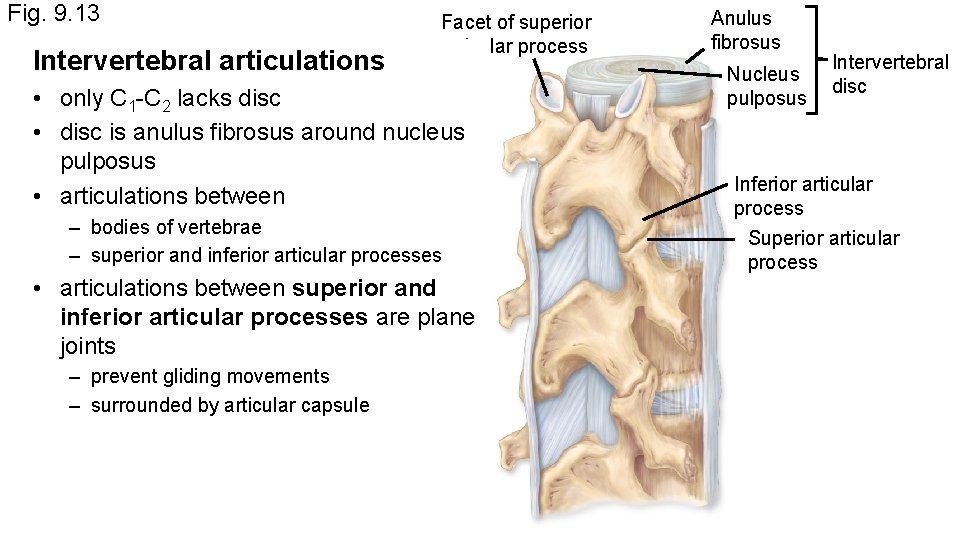
Fig. 9. 13 Intervertebral articulations Facet of superior articular process • only C 1 -C 2 lacks disc • disc is anulus fibrosus around nucleus pulposus • articulations between – bodies of vertebrae – superior and inferior articular processes • articulations between superior and inferior articular processes are plane joints – prevent gliding movements – surrounded by articular capsule Anulus fibrosus Nucleus pulposus Intervertebral disc Inferior articular process Superior articular process
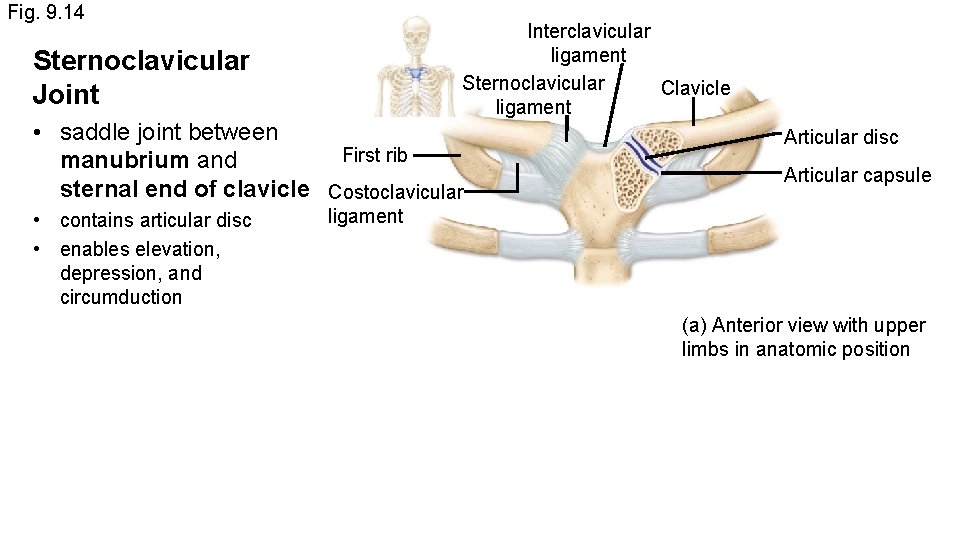
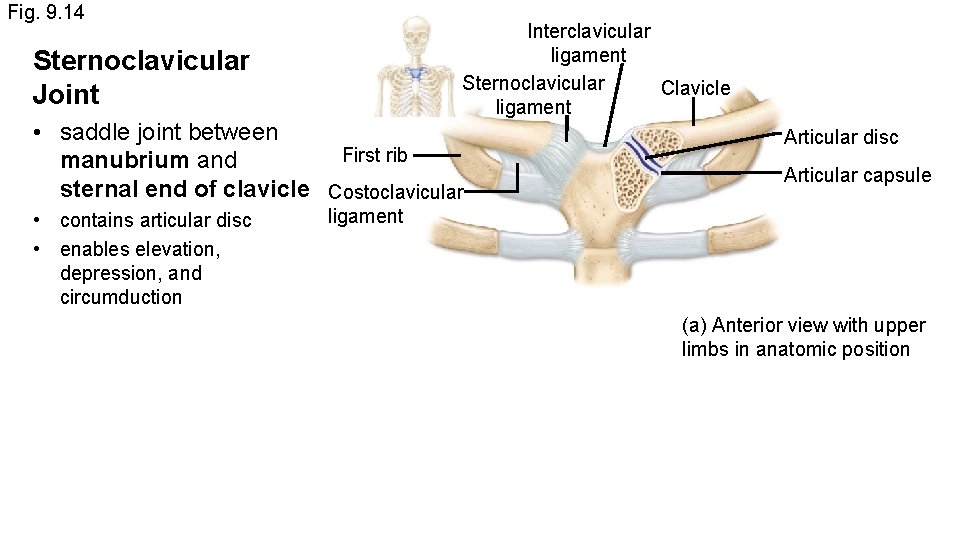
Fig. 9. 14 Interclavicular ligament Sternoclavicular Clavicle ligament Sternoclavicular Joint • saddle joint between First rib manubrium and sternal end of clavicle Costoclavicular • contains articular disc • enables elevation, depression, and circumduction Articular disc Articular capsule ligament (a) Anterior view with upper limbs in anatomic position
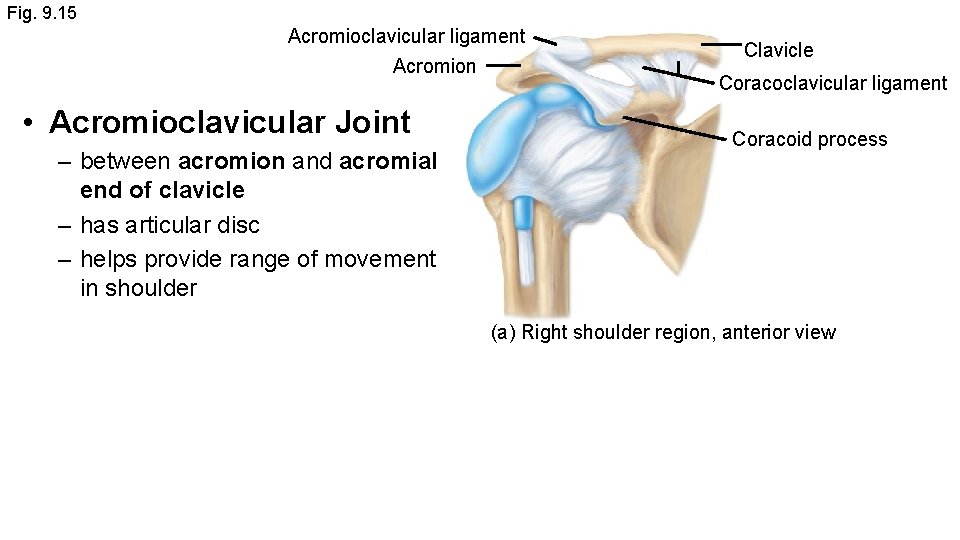
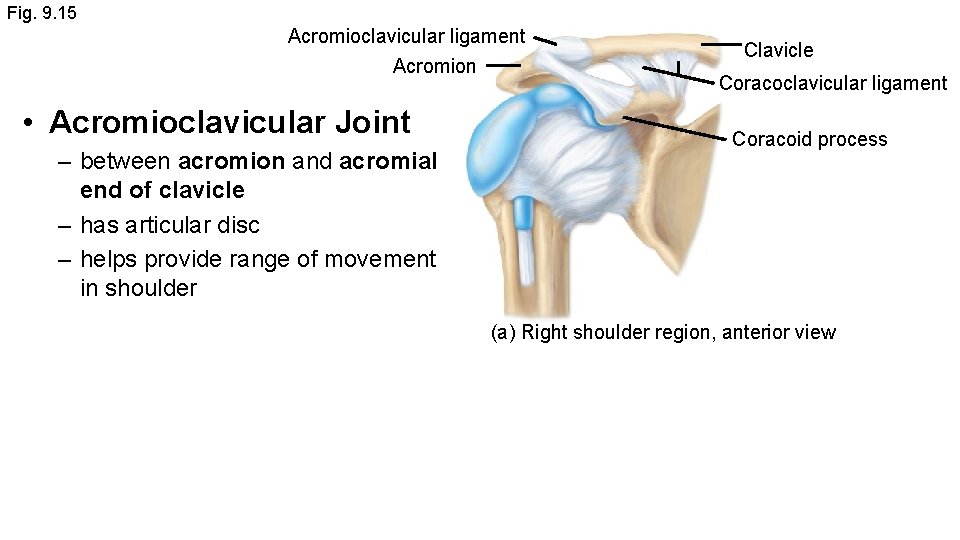
Fig. 9. 15 Acromioclavicular ligament Acromion • Acromioclavicular Joint – between acromion and acromial end of clavicle – has articular disc – helps provide range of movement in shoulder Clavicle Coracoclavicular ligament Coracoid process (a) Right shoulder region, anterior view
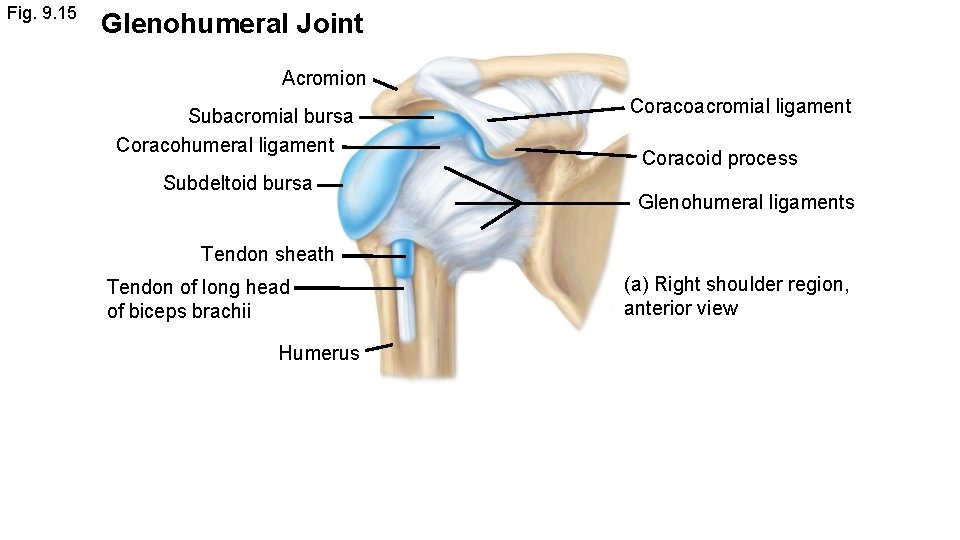
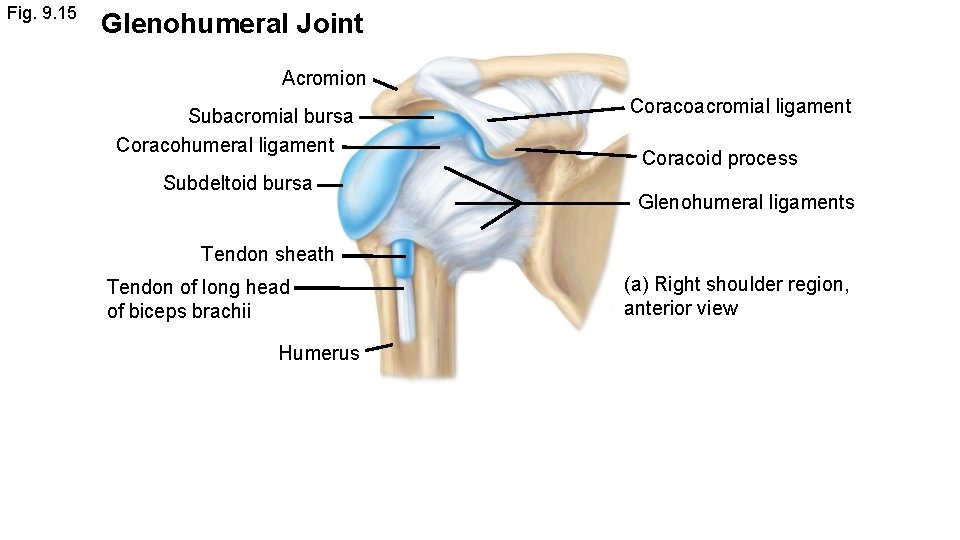
Fig. 9. 15 Glenohumeral Joint Acromion Subacromial bursa Coracohumeral ligament Subdeltoid bursa Coracoacromial ligament Coracoid process Glenohumeral ligaments Tendon sheath Tendon of long head of biceps brachii Humerus (a) Right shoulder region, anterior view
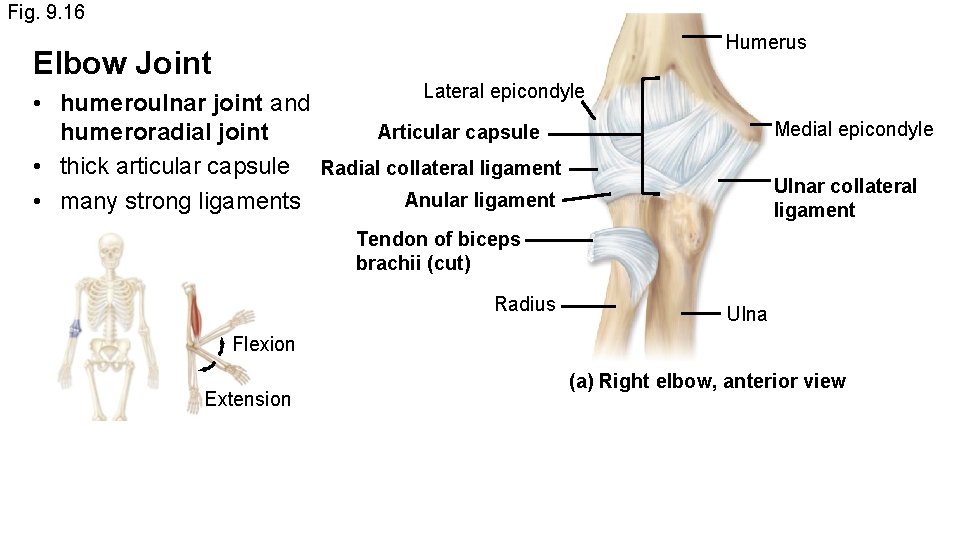
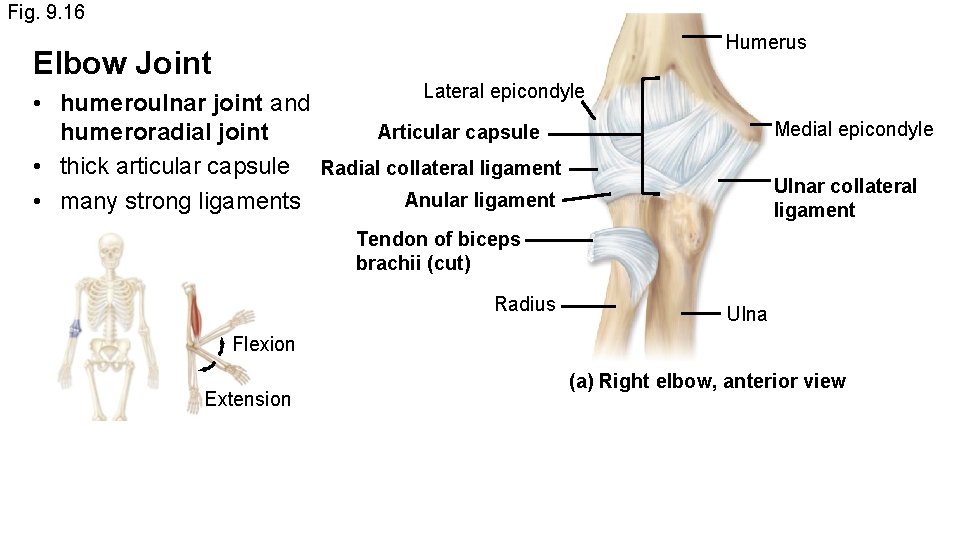
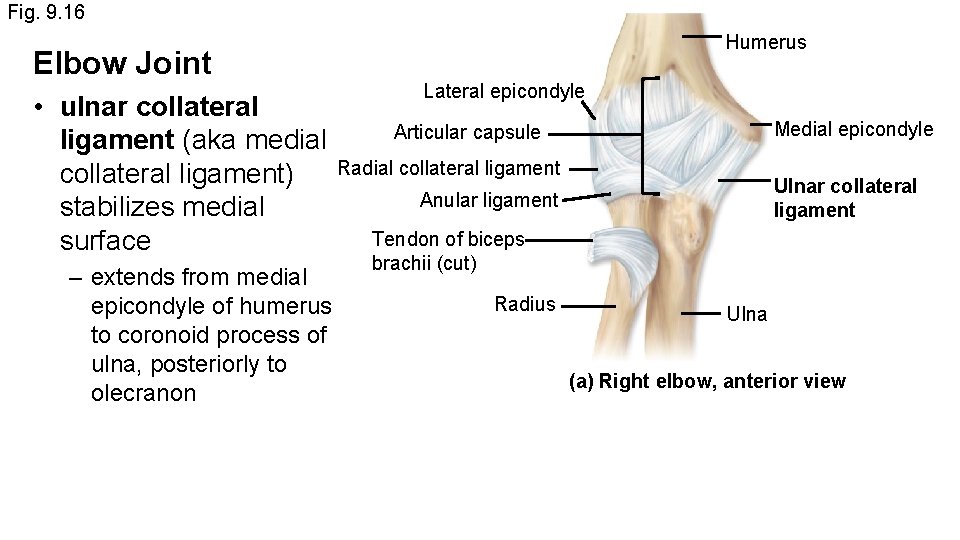
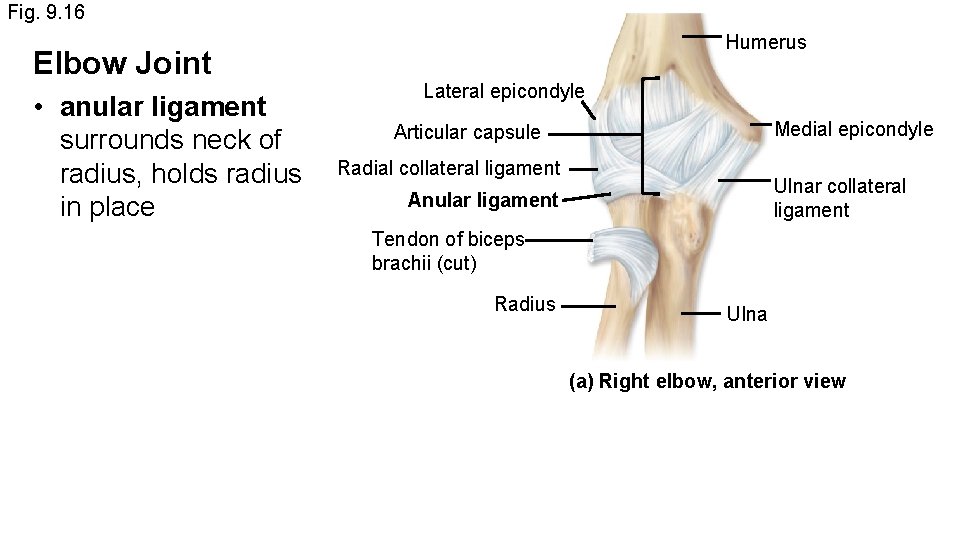
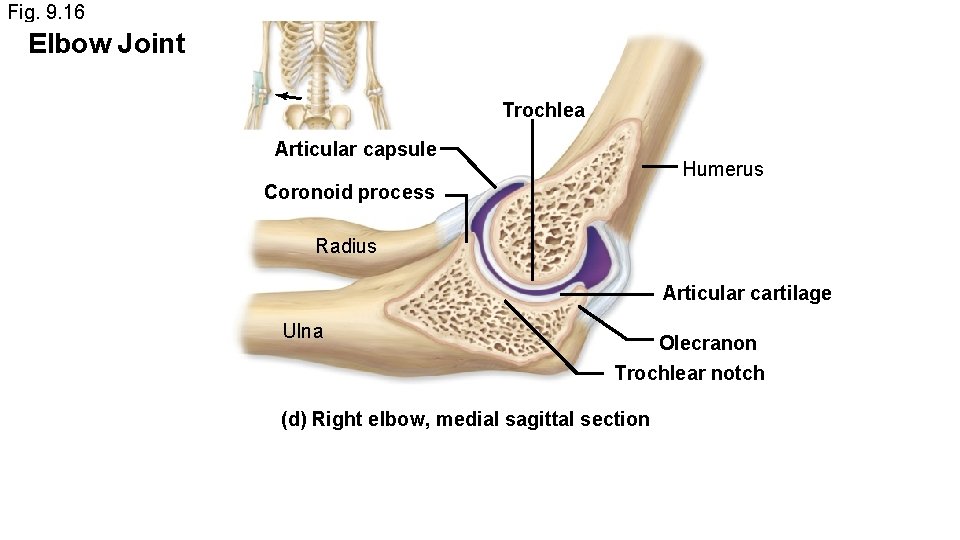
Fig. 9. 16 Humerus Elbow Joint Lateral epicondyle • humeroulnar joint and Articular capsule humeroradial joint • thick articular capsule Radial collateral ligament Anular ligament • many strong ligaments Medial epicondyle Ulnar collateral ligament Tendon of biceps brachii (cut) Radius Ulna Flexion Extension (a) Right elbow, anterior view
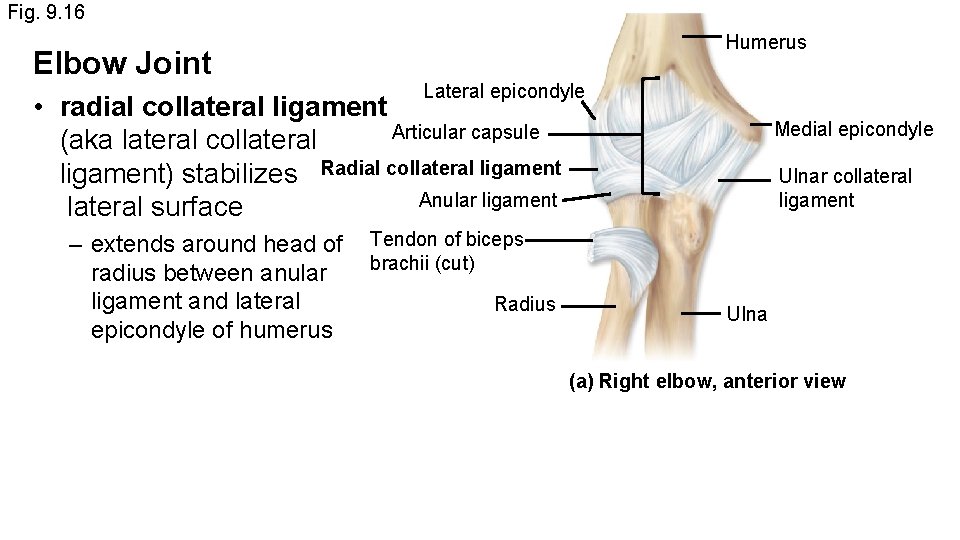
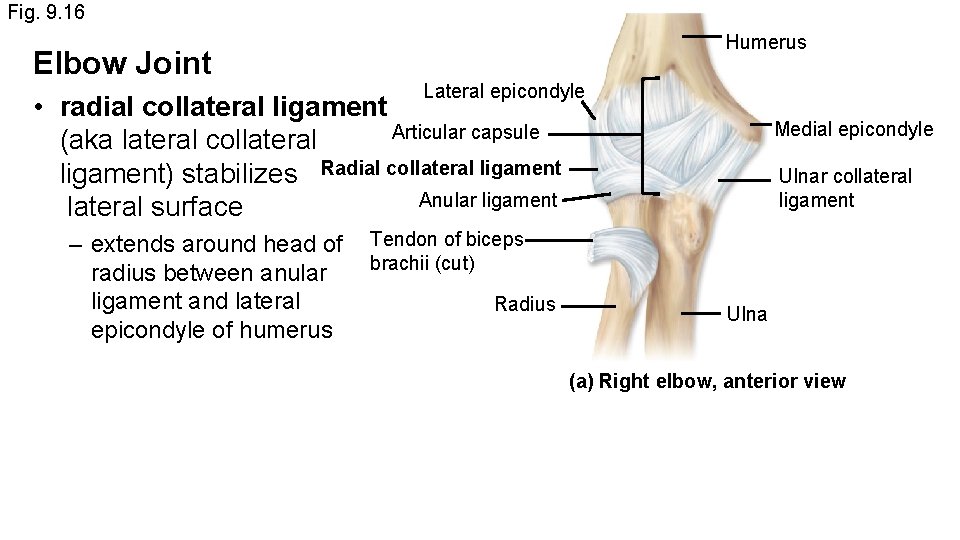
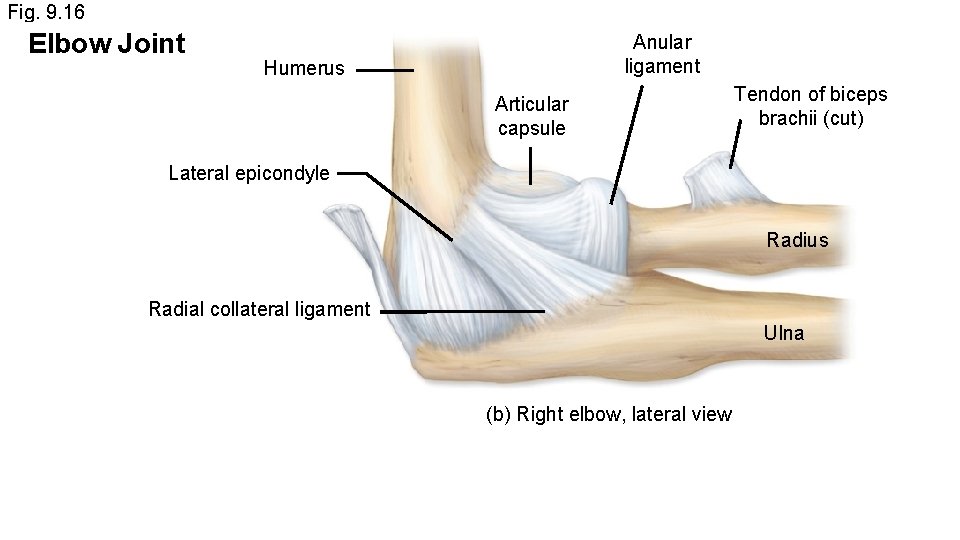
Fig. 9. 16 Elbow Joint Humerus Lateral epicondyle • radial collateral ligament Articular capsule (aka lateral collateral ligament) stabilizes Radial collateral ligament Anular ligament lateral surface – extends around head of Tendon of biceps brachii (cut) radius between anular ligament and lateral Radius epicondyle of humerus Medial epicondyle Ulnar collateral ligament Ulna (a) Right elbow, anterior view
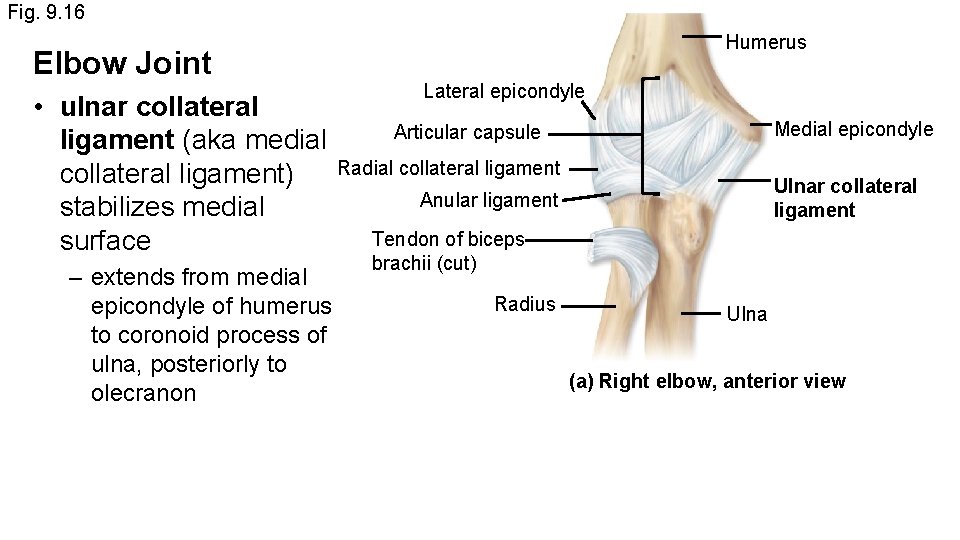
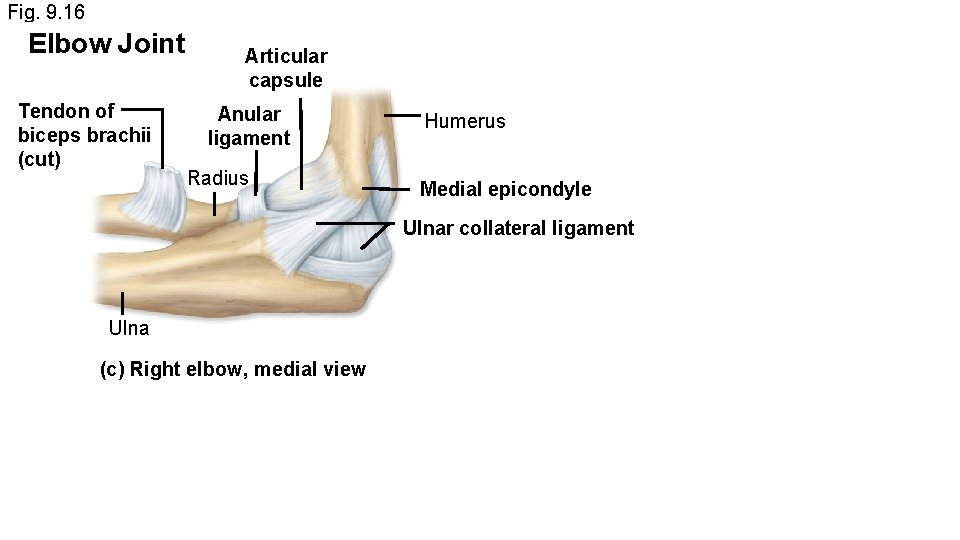
Fig. 9. 16 Elbow Joint Humerus Lateral epicondyle • ulnar collateral Articular capsule ligament (aka medial collateral ligament) Radial collateral ligament Anular ligament stabilizes medial Tendon of biceps surface – extends from medial epicondyle of humerus to coronoid process of ulna, posteriorly to olecranon Medial epicondyle Ulnar collateral ligament brachii (cut) Radius Ulna (a) Right elbow, anterior view
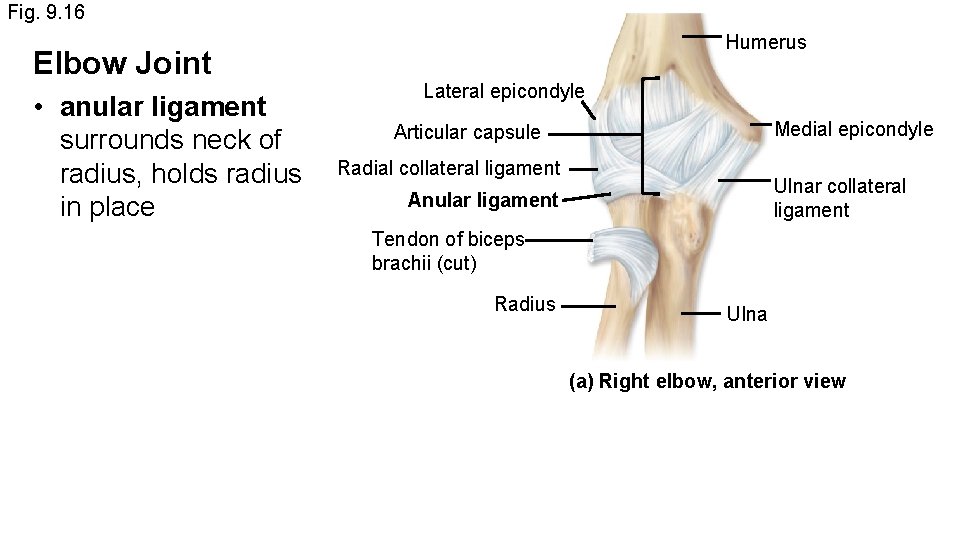
Fig. 9. 16 Elbow Joint • anular ligament surrounds neck of radius, holds radius in place Humerus Lateral epicondyle Medial epicondyle Articular capsule Radial collateral ligament Ulnar collateral ligament Anular ligament Tendon of biceps brachii (cut) Radius Ulna (a) Right elbow, anterior view
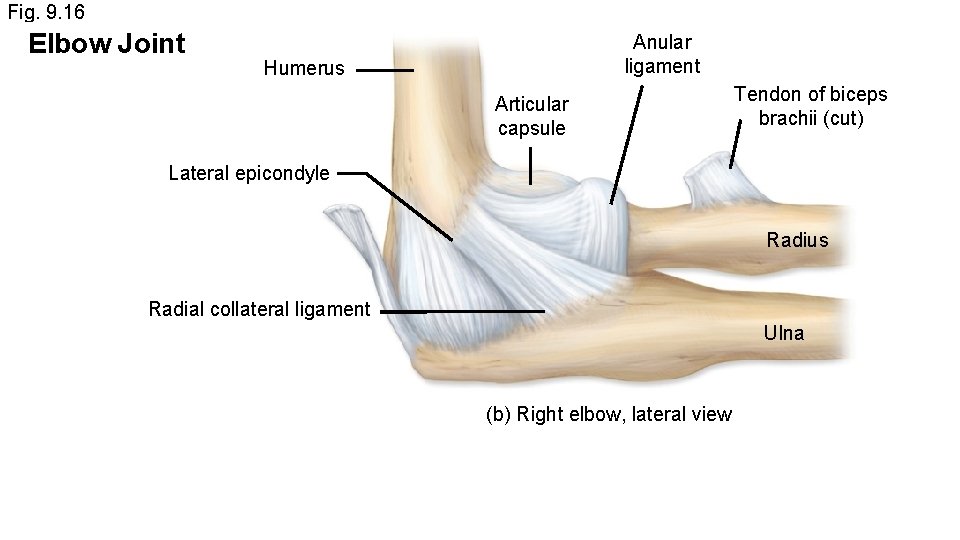
Fig. 9. 16 Elbow Joint Anular ligament Humerus Articular capsule Tendon of biceps brachii (cut) Lateral epicondyle Radius Radial collateral ligament Ulna (b) Right elbow, lateral view
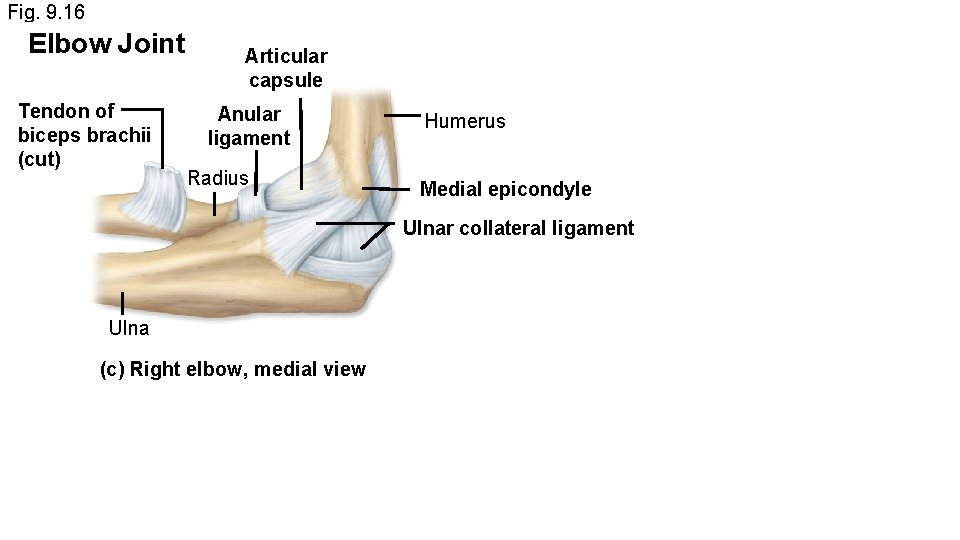
Fig. 9. 16 Elbow Joint Tendon of biceps brachii (cut) Articular capsule Anular ligament Radius Humerus Medial epicondyle Ulnar collateral ligament Ulna (c) Right elbow, medial view
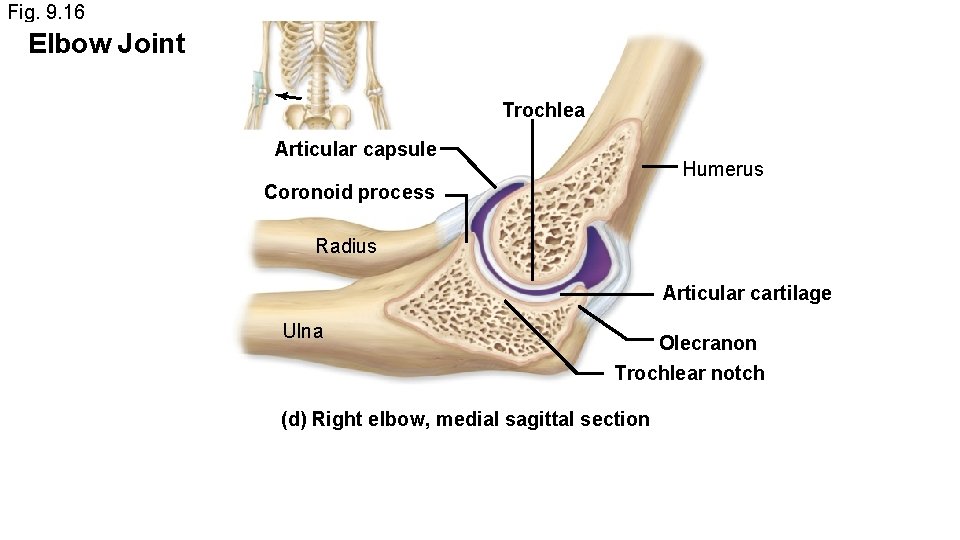
Fig. 9. 16 Elbow Joint Trochlea Articular capsule Humerus Coronoid process Radius Articular cartilage Ulna Olecranon Trochlear notch (d) Right elbow, medial sagittal section
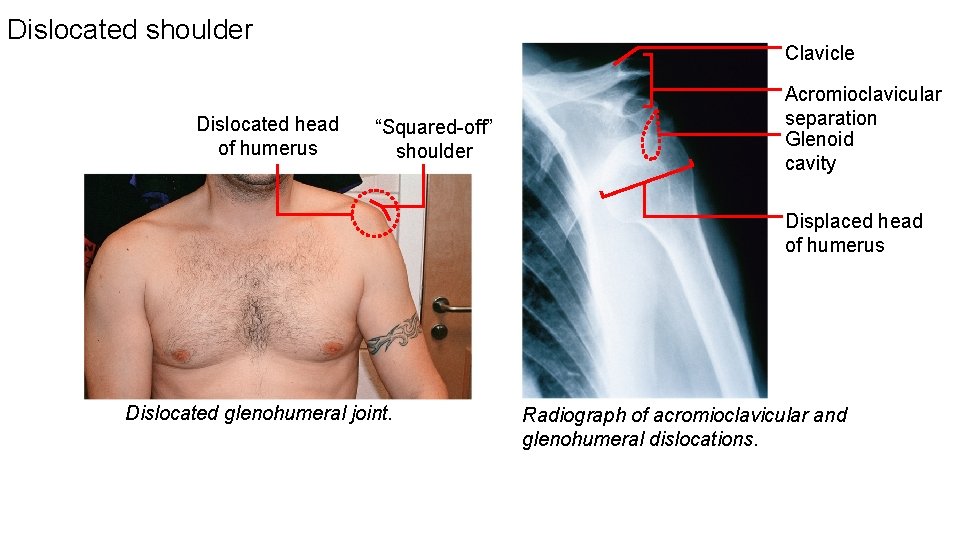
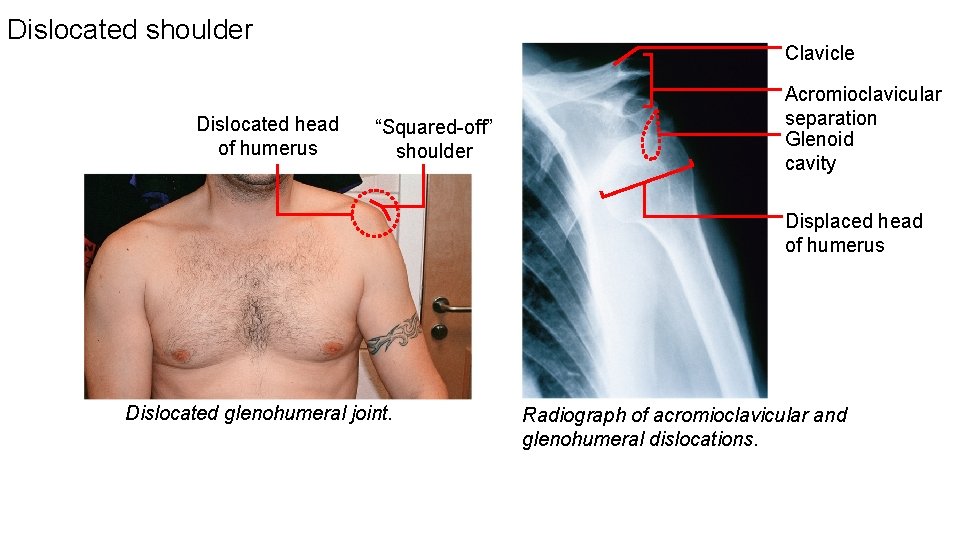
Dislocated shoulder Dislocated head of humerus Clavicle “Squared-off” shoulder Acromioclavicular separation Glenoid cavity Displaced head of humerus Dislocated glenohumeral joint. Radiograph of acromioclavicular and glenohumeral dislocations.
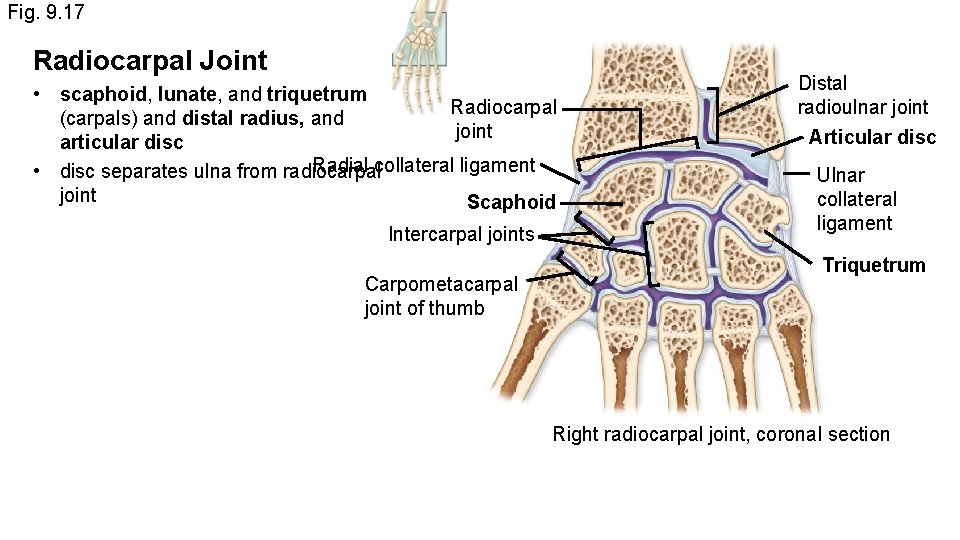
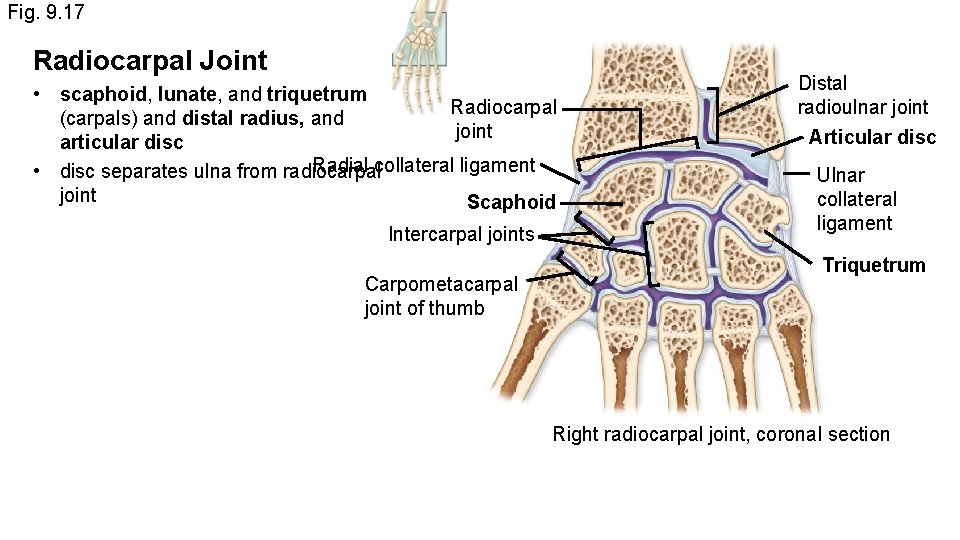
Fig. 9. 17 Radiocarpal Joint • scaphoid, lunate, and triquetrum Radiocarpal (carpals) and distal radius, and joint articular disc Radial collateral ligament • disc separates ulna from radiocarpal joint Scaphoid Intercarpal joints Carpometacarpal joint of thumb Distal radioulnar joint Articular disc Ulnar collateral ligament Triquetrum Right radiocarpal joint, coronal section
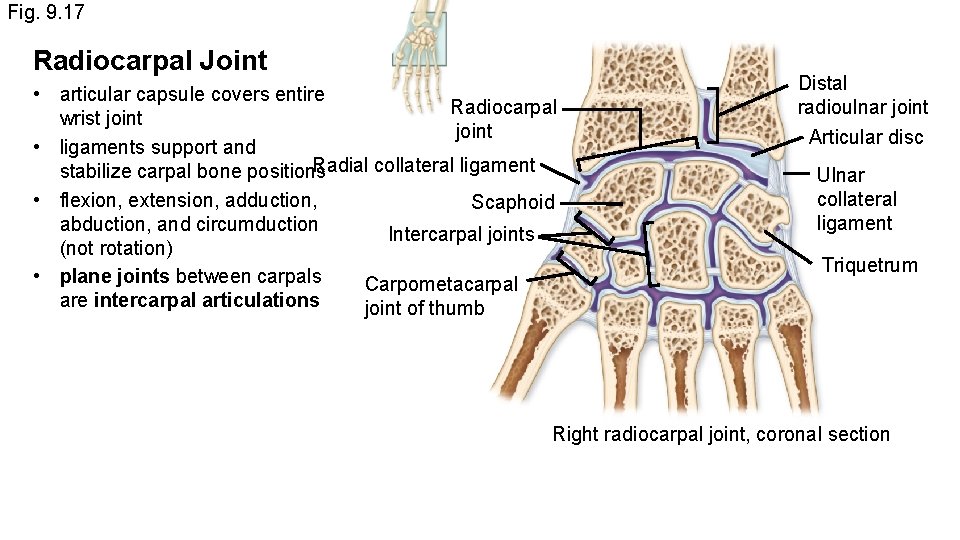
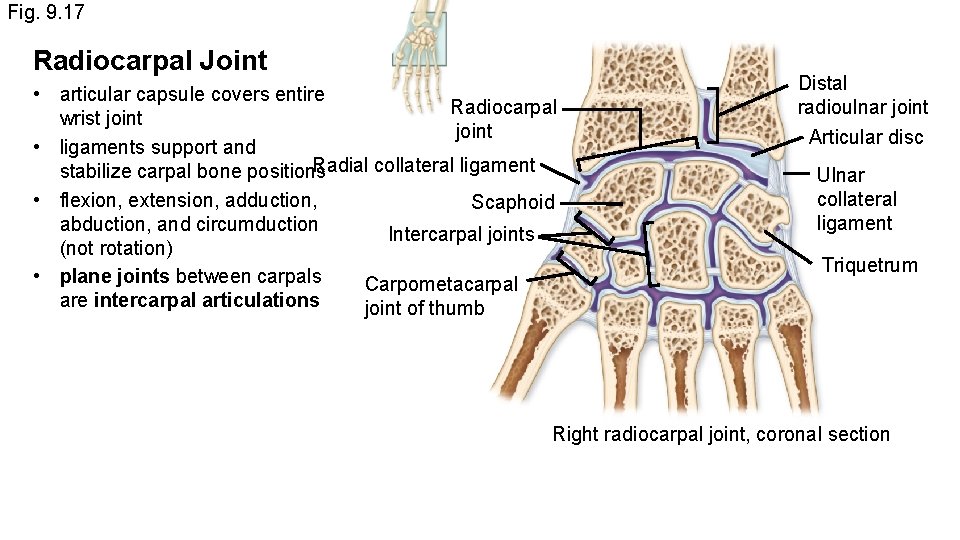
Fig. 9. 17 Radiocarpal Joint • articular capsule covers entire Radiocarpal wrist joint • ligaments support and Radial collateral ligament stabilize carpal bone positions • flexion, extension, adduction, Scaphoid abduction, and circumduction Intercarpal joints (not rotation) • plane joints between carpals Carpometacarpal are intercarpal articulations joint of thumb Distal radioulnar joint Articular disc Ulnar collateral ligament Triquetrum Right radiocarpal joint, coronal section
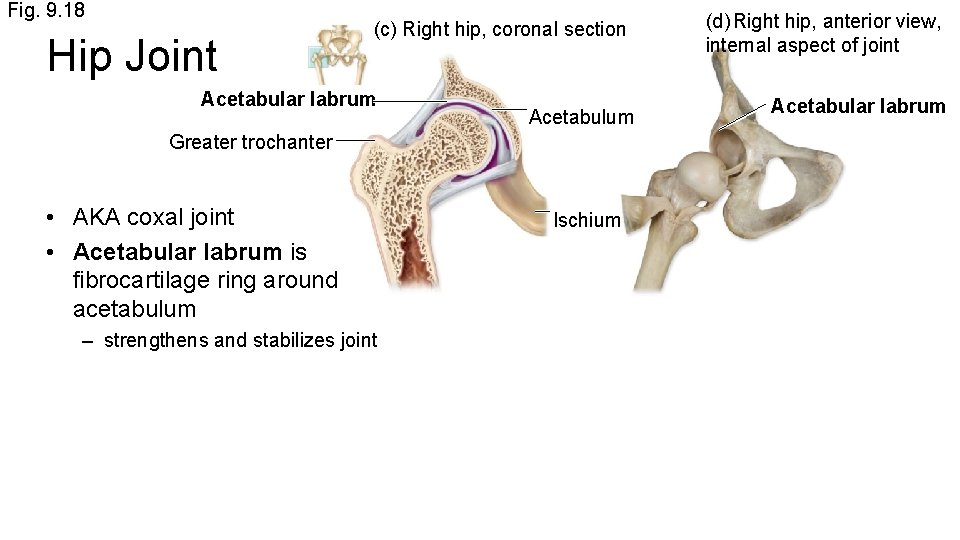
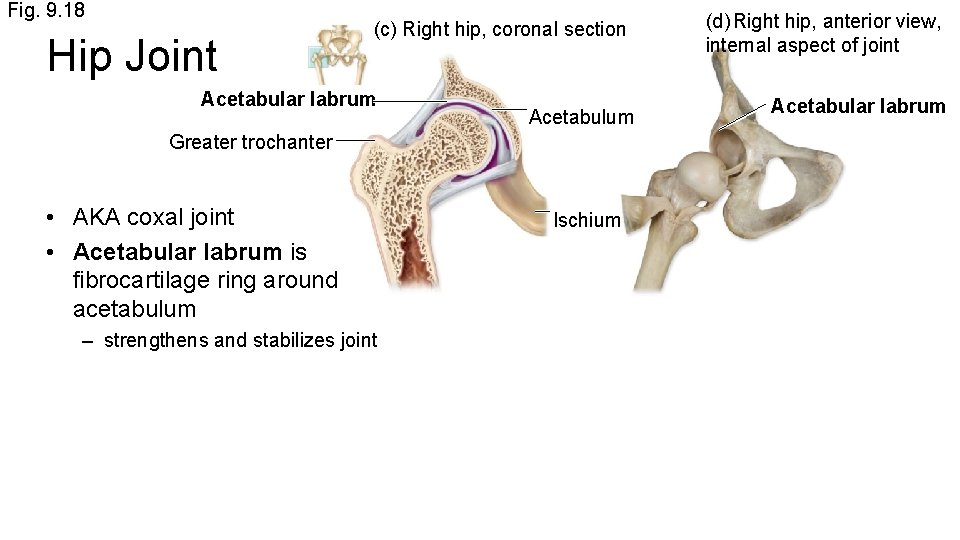
Fig. 9. 18 Hip Joint (c) Right hip, coronal section Acetabular labrum Acetabulum Greater trochanter • AKA coxal joint • Acetabular labrum is fibrocartilage ring around acetabulum – strengthens and stabilizes joint Ischium (d) Right hip, anterior view, internal aspect of joint Acetabular labrum
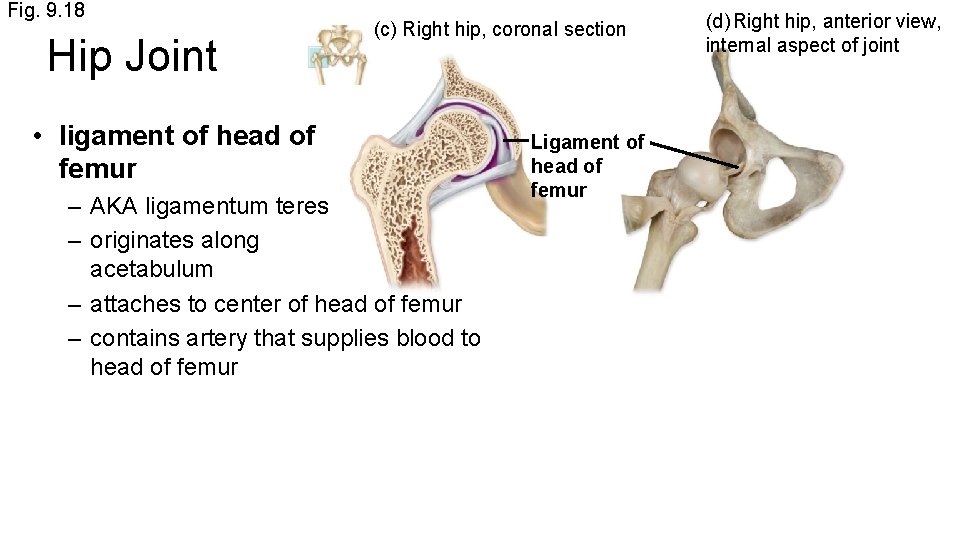
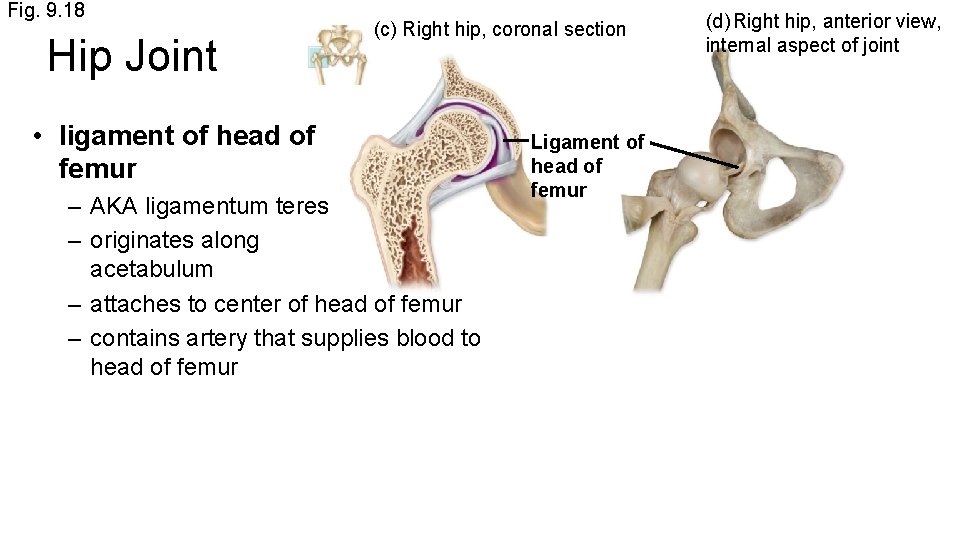
Fig. 9. 18 Hip Joint (c) Right hip, coronal section • ligament of head of femur – AKA ligamentum teres – originates along acetabulum – attaches to center of head of femur – contains artery that supplies blood to head of femur Ligament of head of femur (d) Right hip, anterior view, internal aspect of joint
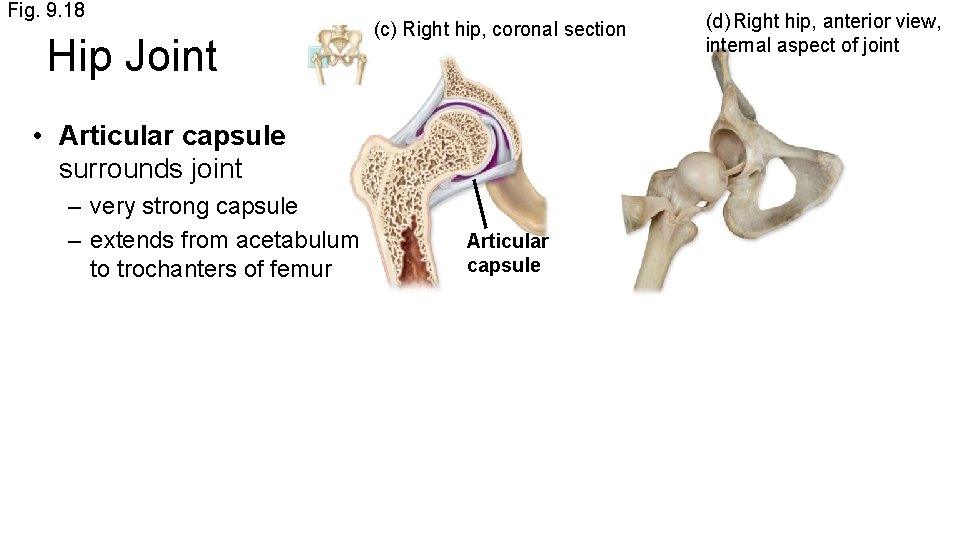
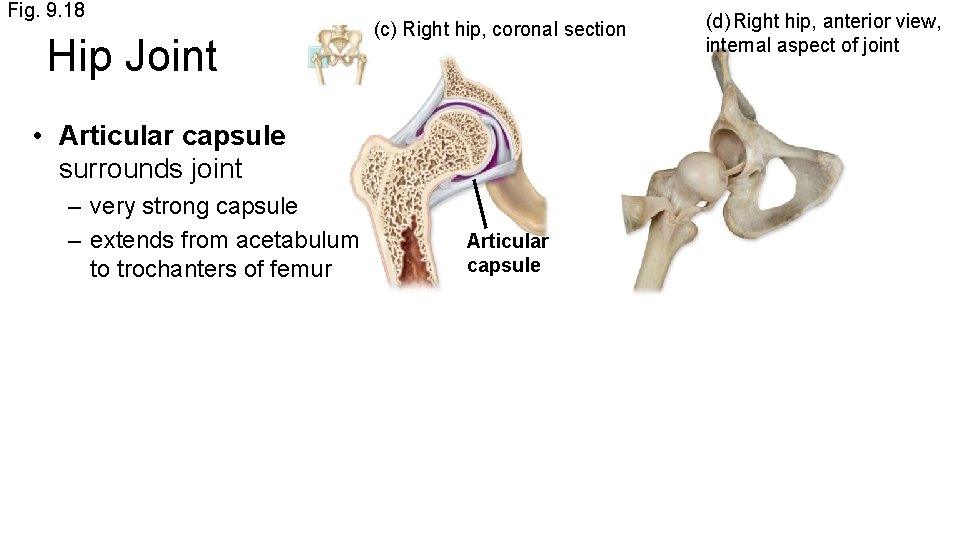
Fig. 9. 18 Hip Joint (c) Right hip, coronal section • Articular capsule surrounds joint – very strong capsule – extends from acetabulum to trochanters of femur Articular capsule (d) Right hip, anterior view, internal aspect of joint
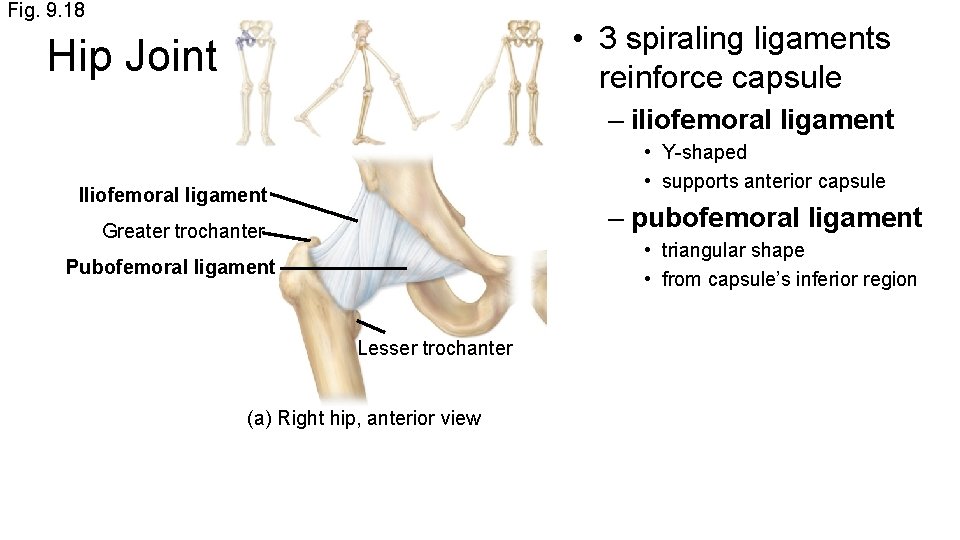
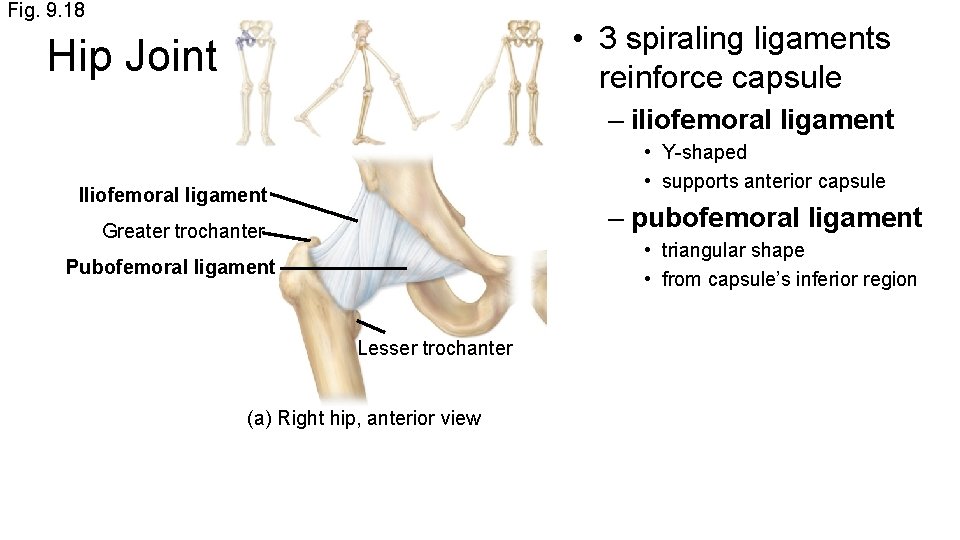
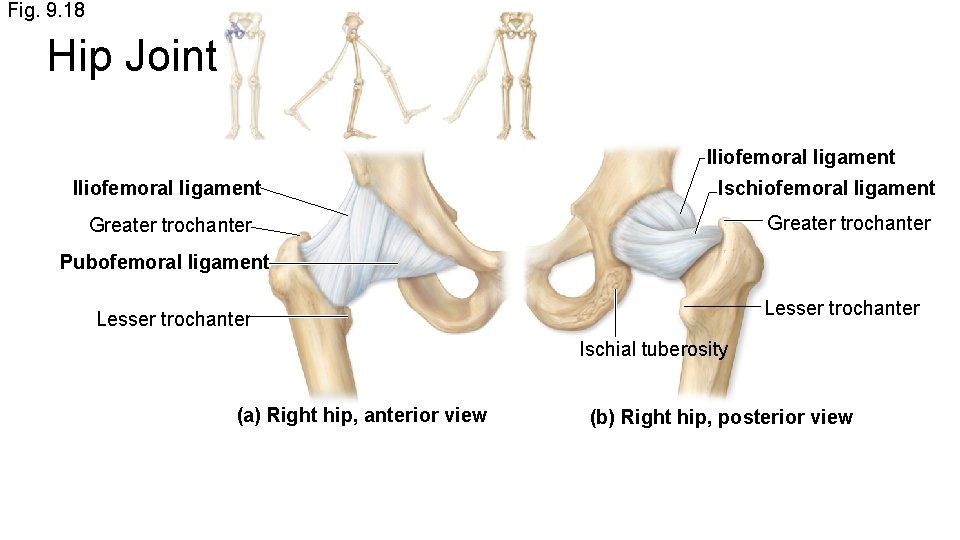
Fig. 9. 18 • 3 spiraling ligaments reinforce capsule Hip Joint – iliofemoral ligament • Y-shaped • supports anterior capsule Iliofemoral ligament – pubofemoral ligament Greater trochanter • triangular shape • from capsule’s inferior region Pubofemoral ligament Lesser trochanter (a) Right hip, anterior view
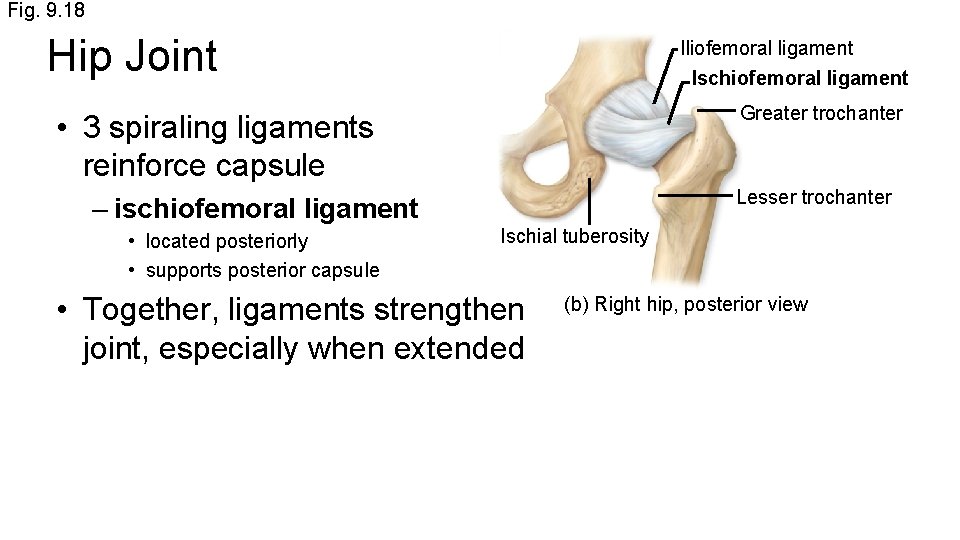
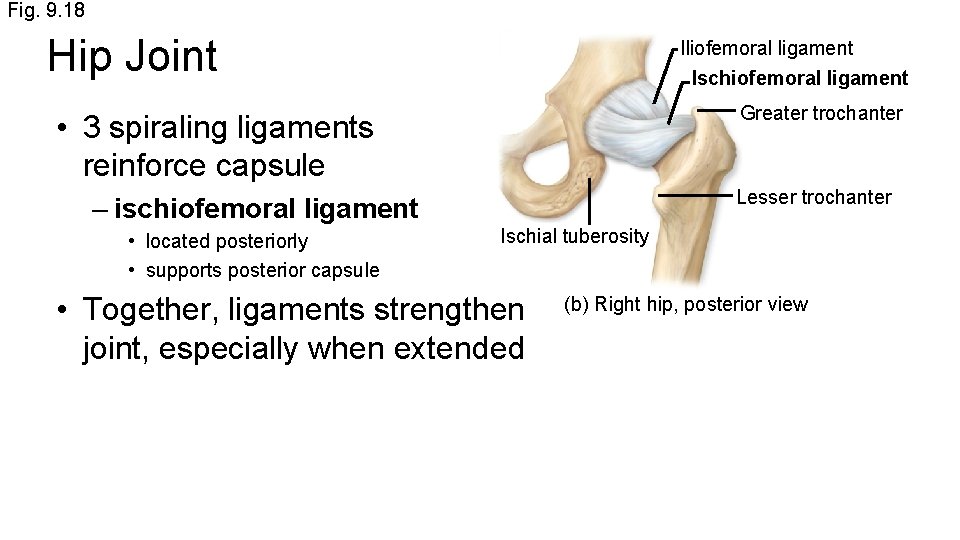
Fig. 9. 18 Hip Joint Iliofemoral ligament Ischiofemoral ligament Greater trochanter • 3 spiraling ligaments reinforce capsule Lesser trochanter – ischiofemoral ligament • located posteriorly • supports posterior capsule Ischial tuberosity • Together, ligaments strengthen joint, especially when extended (b) Right hip, posterior view
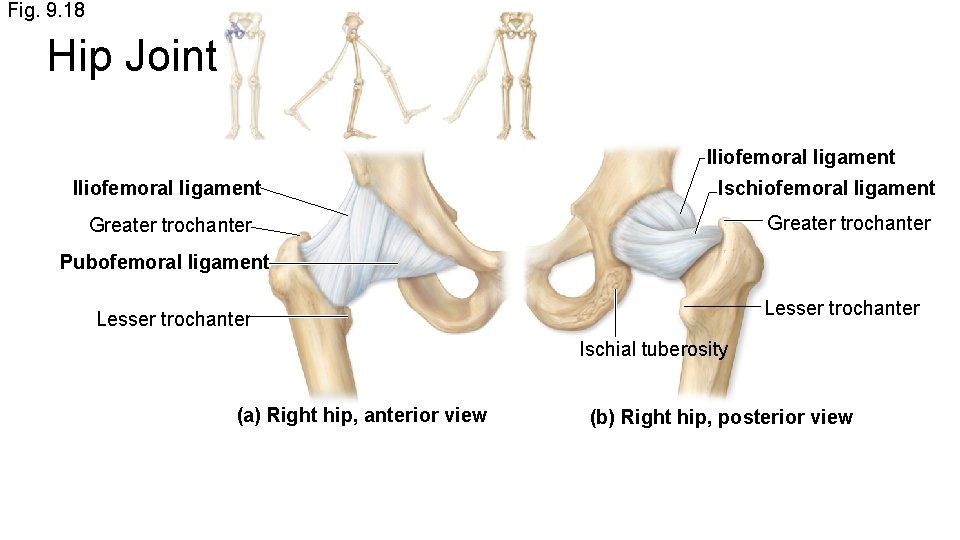
Fig. 9. 18 Hip Joint Iliofemoral ligament Ischiofemoral ligament Greater trochanter Pubofemoral ligament Lesser trochanter Ischial tuberosity (a) Right hip, anterior view (b) Right hip, posterior view
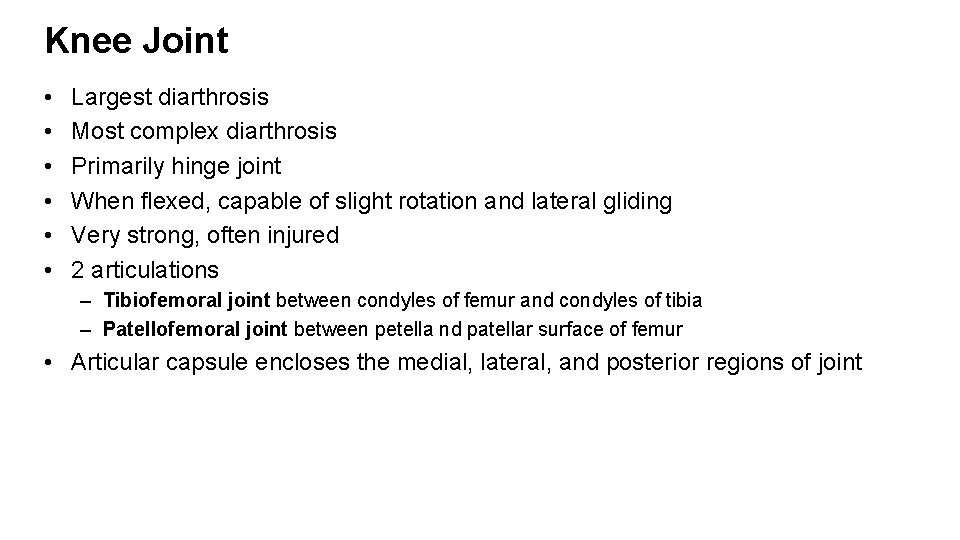
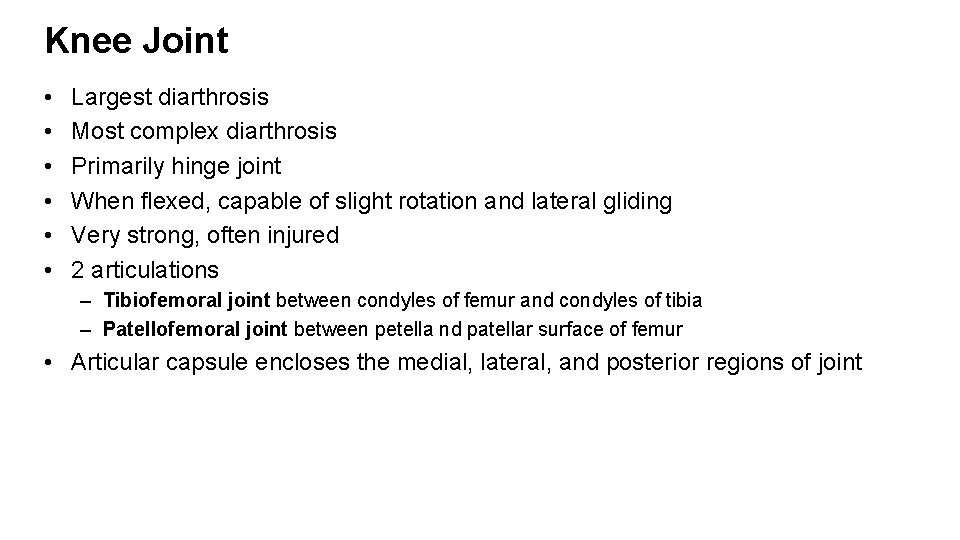
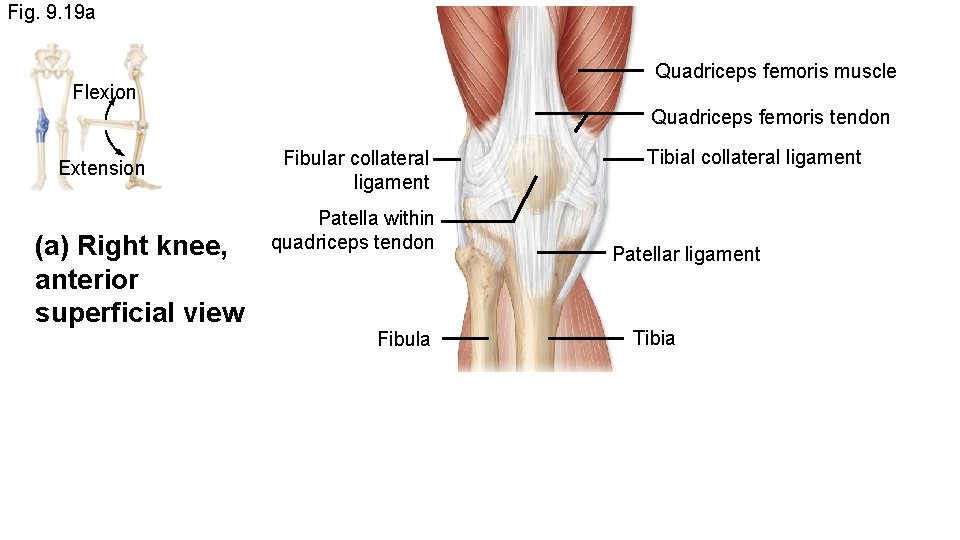
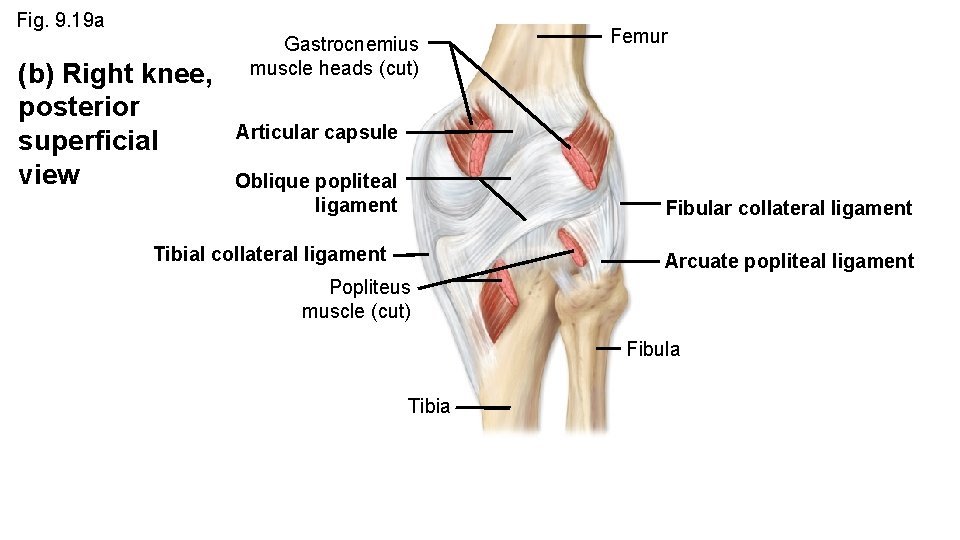
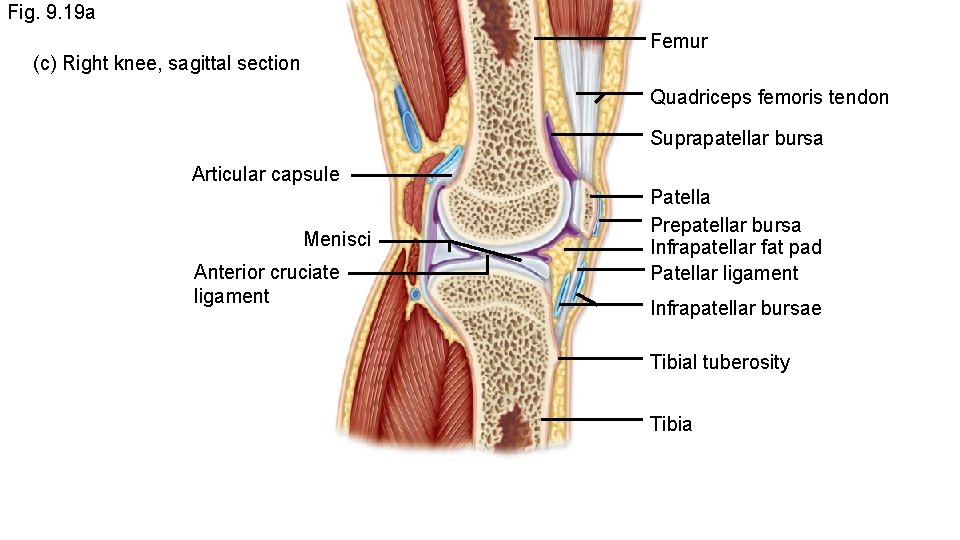
Knee Joint • • • Largest diarthrosis Most complex diarthrosis Primarily hinge joint When flexed, capable of slight rotation and lateral gliding Very strong, often injured 2 articulations – Tibiofemoral joint between condyles of femur and condyles of tibia – Patellofemoral joint between petella nd patellar surface of femur • Articular capsule encloses the medial, lateral, and posterior regions of joint
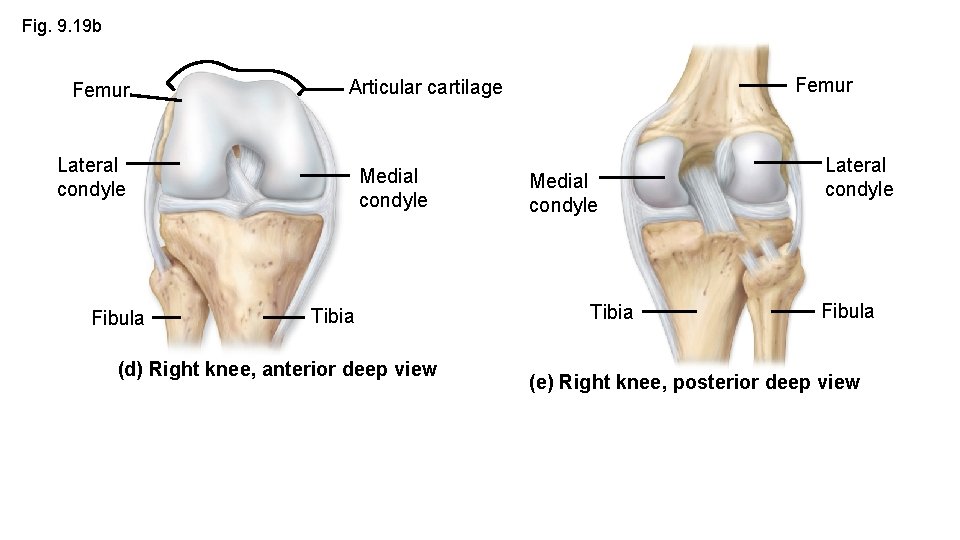
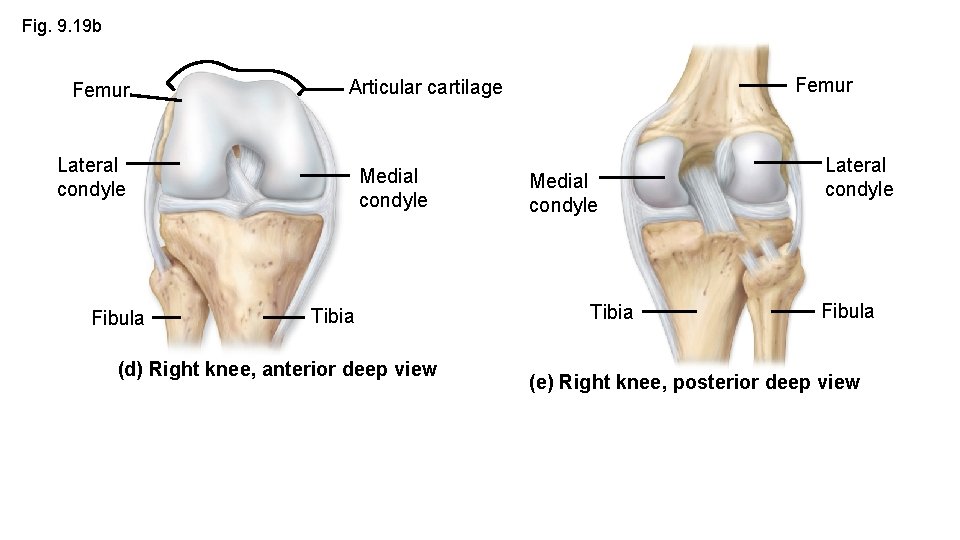
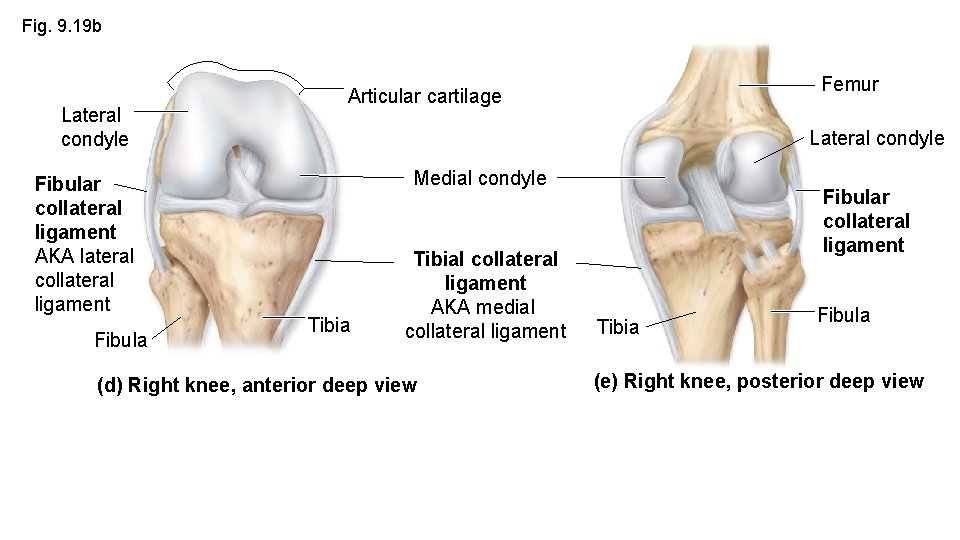
Fig. 9. 19 b Femur Lateral condyle Fibula Femur Articular cartilage Medial condyle Tibia (d) Right knee, anterior deep view Medial condyle Tibia Lateral condyle Fibula (e) Right knee, posterior deep view
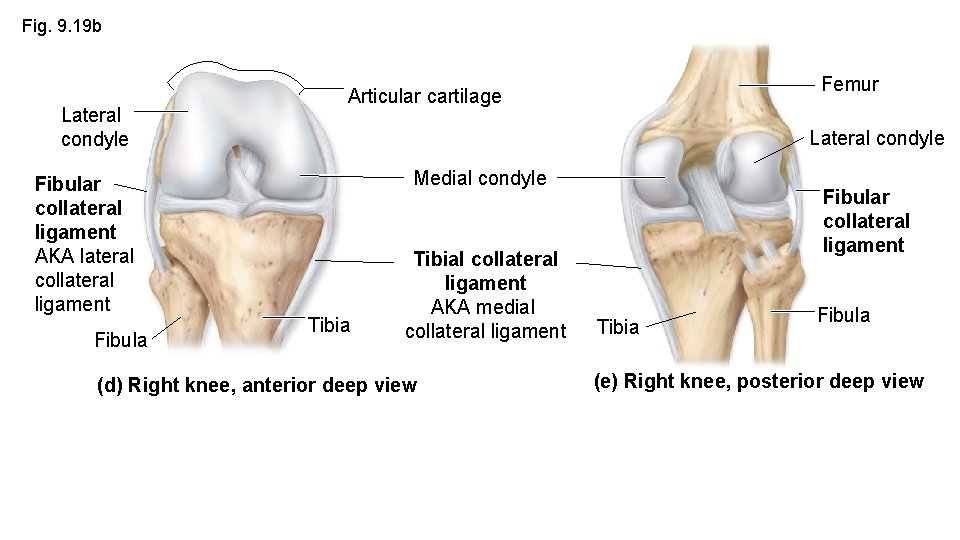
Fig. 9. 19 b Lateral condyle Fibular collateral ligament AKA lateral collateral ligament Fibula Femur Articular cartilage Lateral condyle Medial condyle Tibial collateral ligament AKA medial collateral ligament (d) Right knee, anterior deep view Fibular collateral ligament Tibia Fibula (e) Right knee, posterior deep view
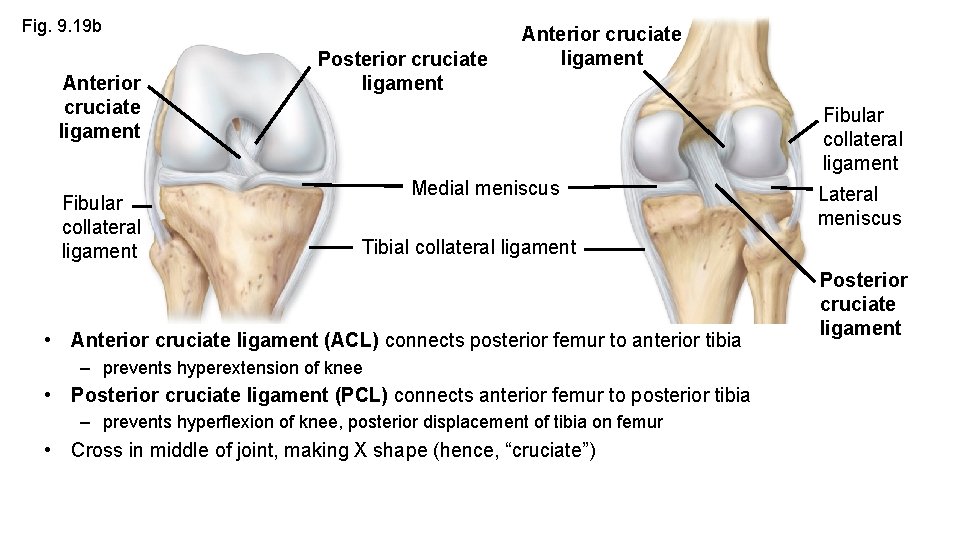
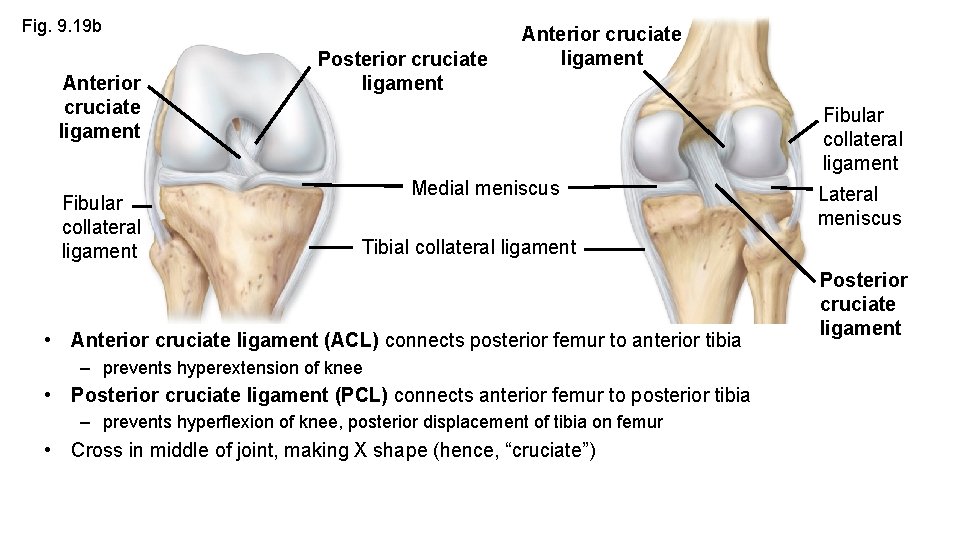
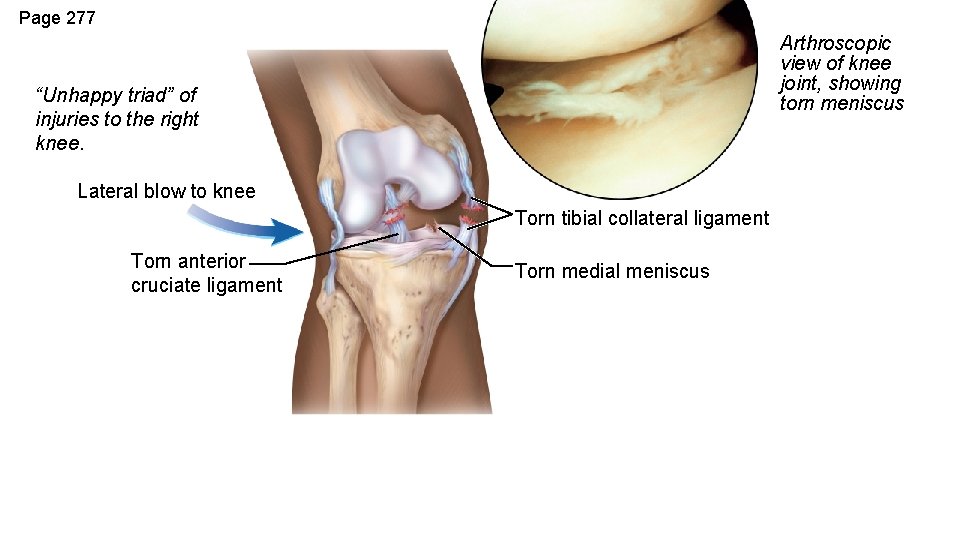
Fig. 9. 19 b Anterior cruciate ligament Fibular collateral ligament Posterior cruciate ligament Anterior cruciate ligament Fibular collateral ligament Medial meniscus Lateral meniscus Tibial collateral ligament • Anterior cruciate ligament (ACL) connects posterior femur to anterior tibia – prevents hyperextension of knee • Posterior cruciate ligament (PCL) connects anterior femur to posterior tibia – prevents hyperflexion of knee, posterior displacement of tibia on femur • Cross in middle of joint, making X shape (hence, “cruciate”) Posterior cruciate ligament
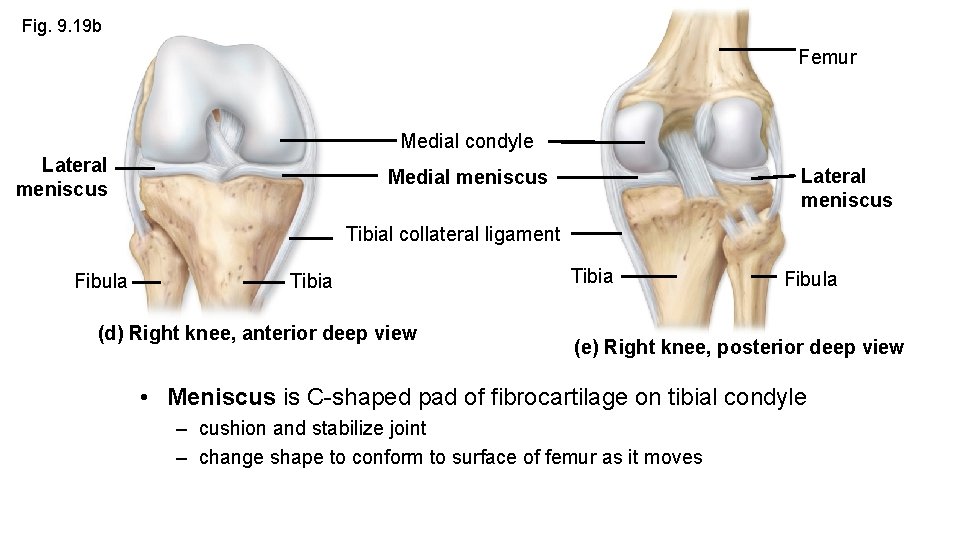
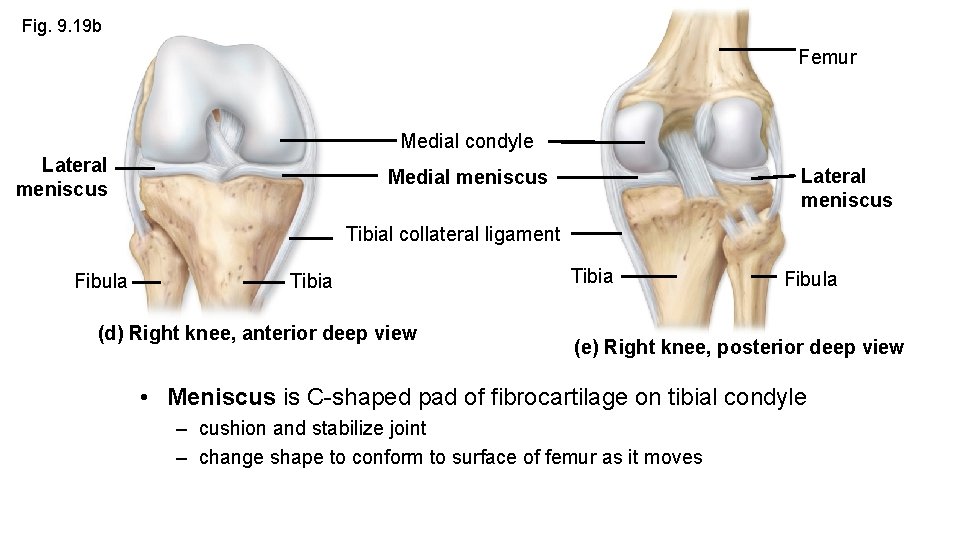
Fig. 9. 19 b Femur Medial condyle Lateral meniscus Medial meniscus Tibial collateral ligament Fibula Tibia (d) Right knee, anterior deep view Tibia Fibula (e) Right knee, posterior deep view • Meniscus is C-shaped pad of fibrocartilage on tibial condyle – cushion and stabilize joint – change shape to conform to surface of femur as it moves
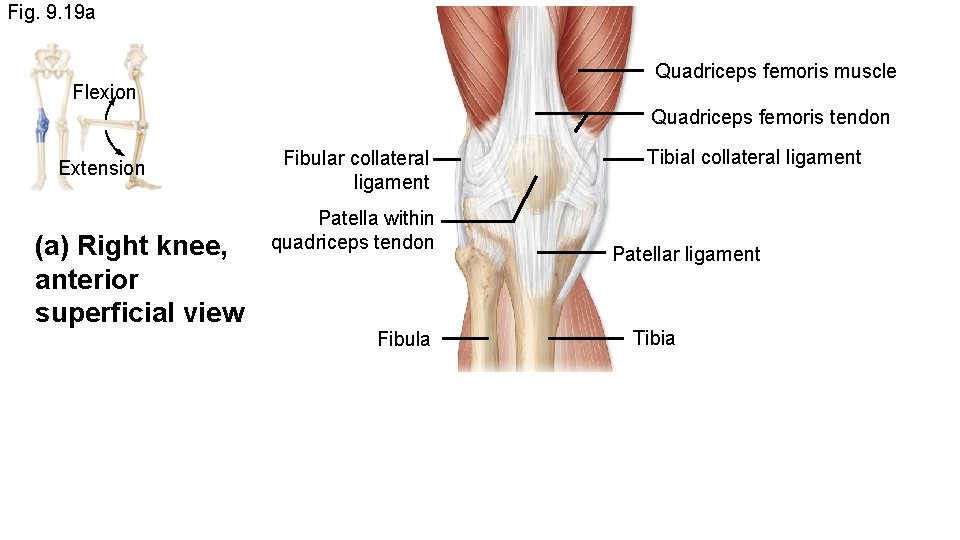
Fig. 9. 19 a Quadriceps femoris muscle Flexion Quadriceps femoris tendon Extension (a) Right knee, anterior superficial view Fibular collateral ligament Patella within quadriceps tendon Fibula Tibial collateral ligament Patellar ligament Tibia
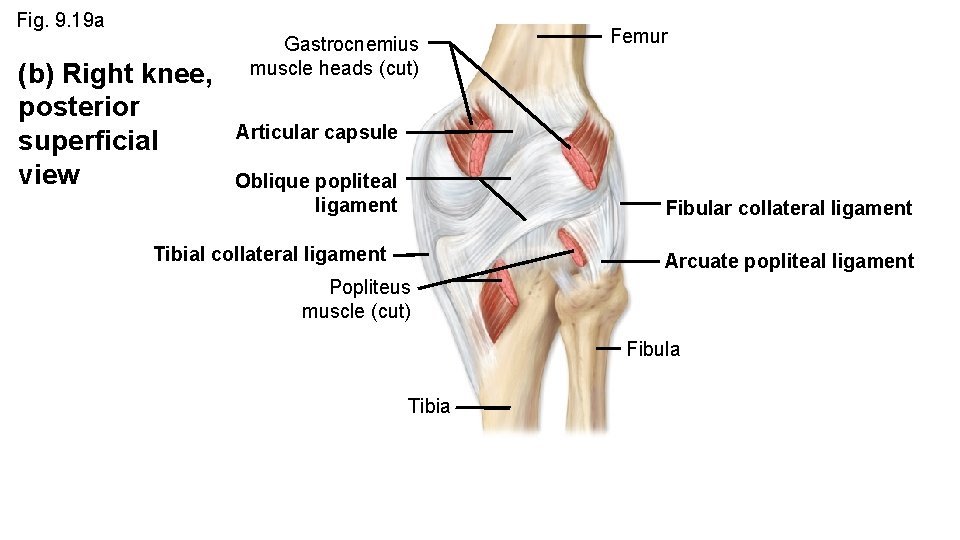
Fig. 9. 19 a (b) Right knee, posterior superficial view Gastrocnemius muscle heads (cut) Femur Articular capsule Oblique popliteal ligament Fibular collateral ligament Tibial collateral ligament Arcuate popliteal ligament Popliteus muscle (cut) Fibula Tibia
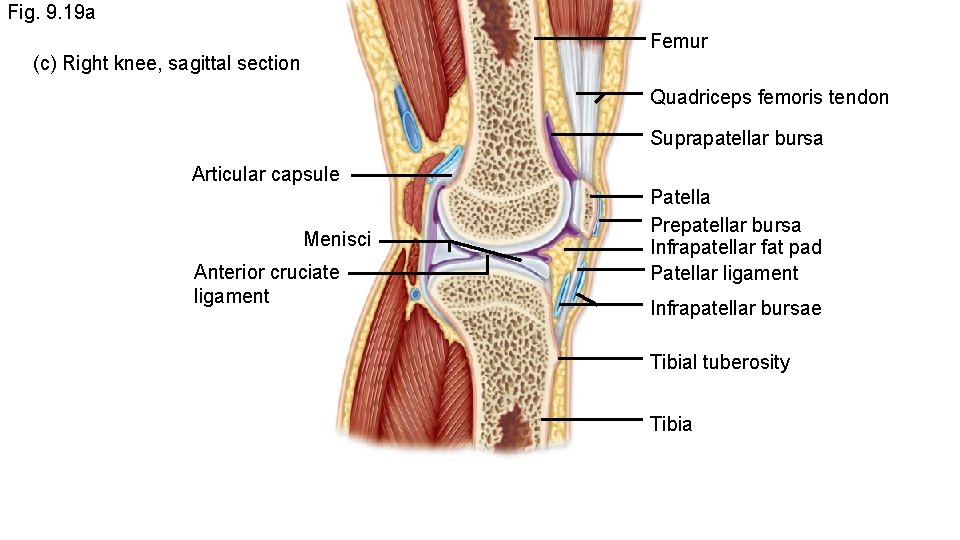
Fig. 9. 19 a Femur (c) Right knee, sagittal section Quadriceps femoris tendon Suprapatellar bursa Articular capsule Menisci Anterior cruciate ligament Patella Prepatellar bursa Infrapatellar fat pad Patellar ligament Infrapatellar bursae Tibial tuberosity Tibia
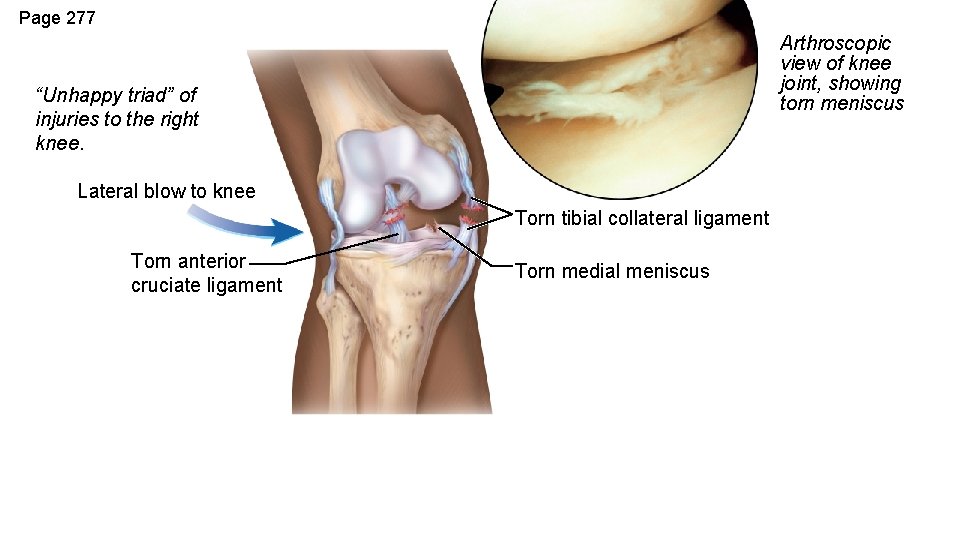
Page 277 Arthroscopic view of knee joint, showing torn meniscus “Unhappy triad” of injuries to the right knee. Lateral blow to knee Torn tibial collateral ligament Torn anterior cruciate ligament Torn medial meniscus
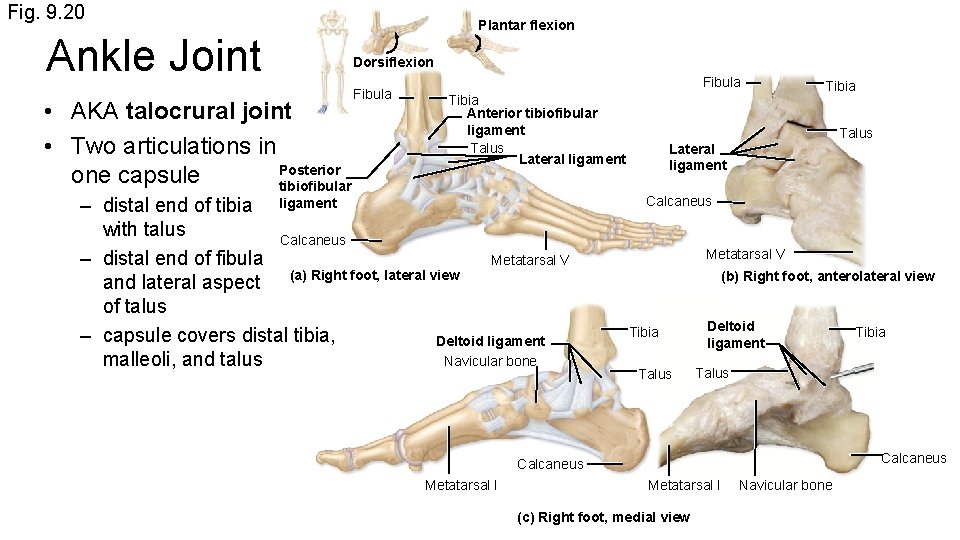
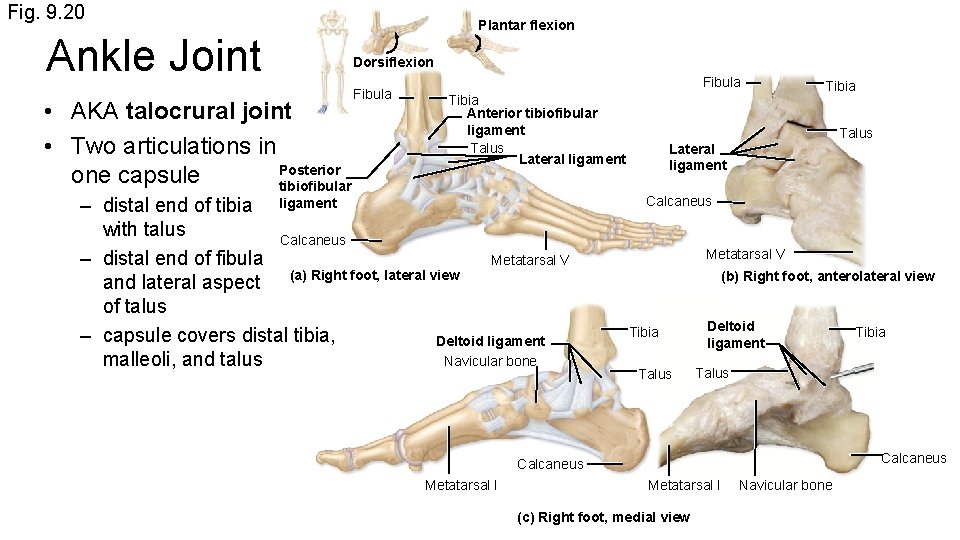
Fig. 9. 20 Ankle Joint • AKA talocrural joint • Two articulations in Posterior one capsule tibiofibular Plantar flexion Dorsiflexion Fibula Tibia Anterior tibiofibular ligament Talus Lateral ligament – distal end of tibia ligament with talus Calcaneus – distal end of fibula Metatarsal V and lateral aspect (a) Right foot, lateral view of talus – capsule covers distal tibia, Deltoid ligament Navicular bone malleoli, and talus Tibia Talus Lateral ligament Calcaneus Metatarsal V (b) Right foot, anterolateral view Tibia Talus Deltoid ligament Talus Calcaneus Metatarsal I Tibia Metatarsal I (c) Right foot, medial view Navicular bone
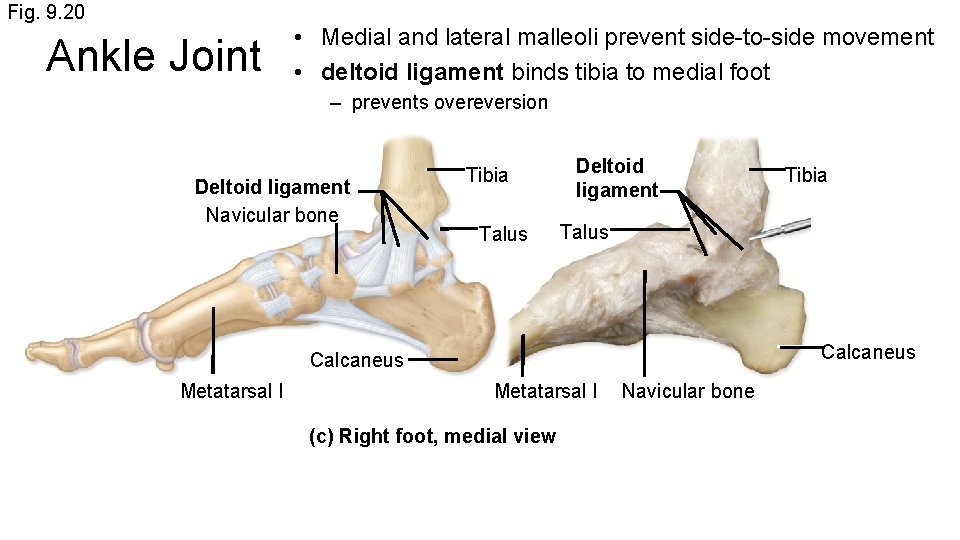
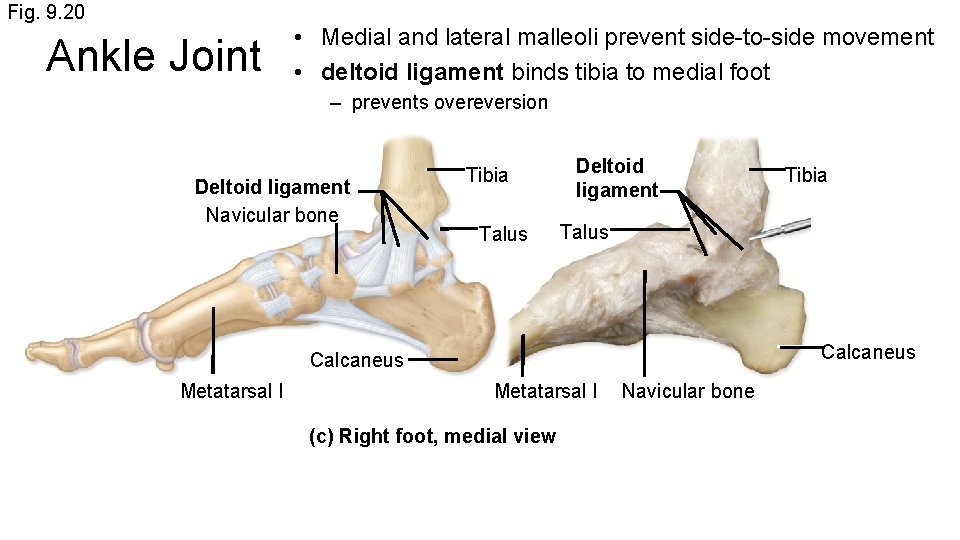
Fig. 9. 20 Ankle Joint • Medial and lateral malleoli prevent side-to-side movement • deltoid ligament binds tibia to medial foot – prevents overeversion Deltoid ligament Navicular bone Tibia Talus Deltoid ligament Talus Calcaneus Metatarsal I Tibia Metatarsal I (c) Right foot, medial view Navicular bone
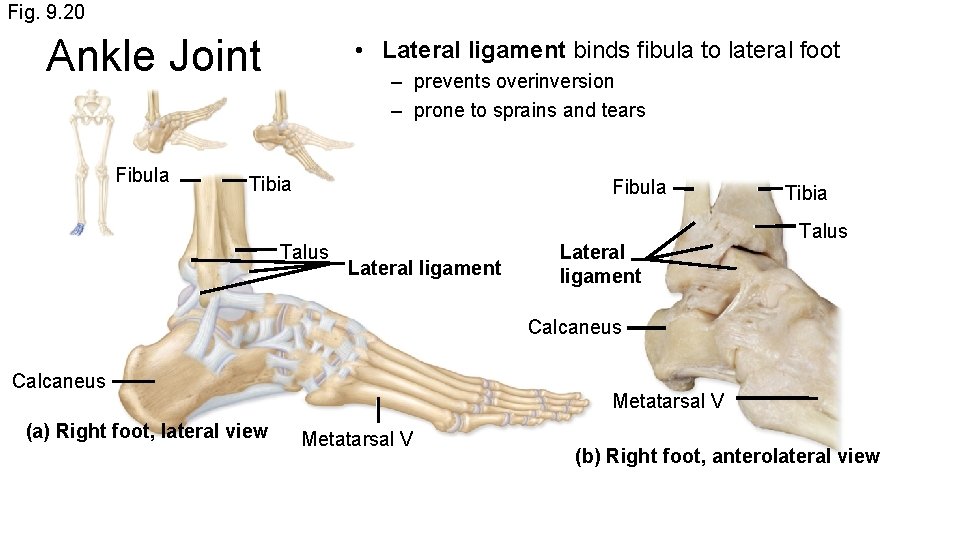
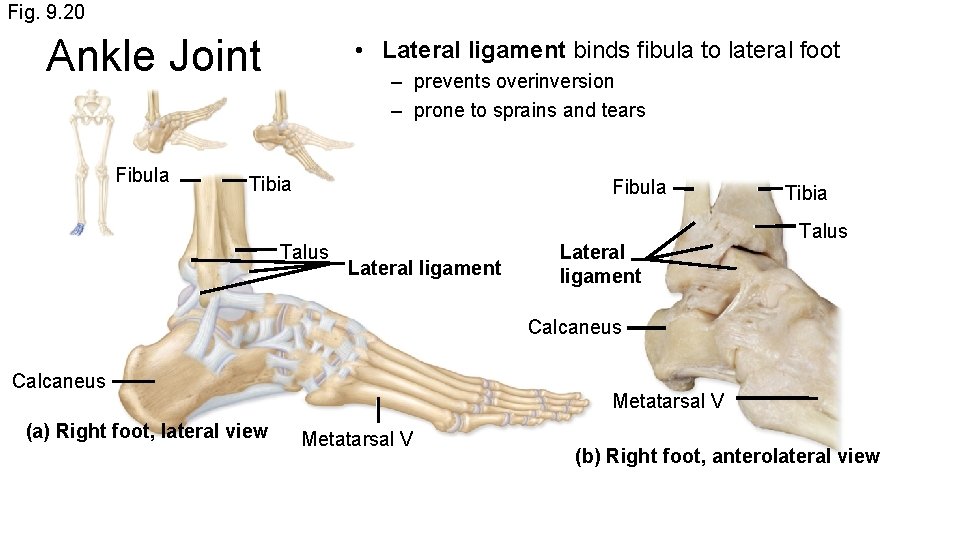
Fig. 9. 20 Ankle Joint Fibula • Lateral ligament binds fibula to lateral foot – prevents overinversion – prone to sprains and tears Tibia Fibula Talus Lateral ligament Tibia Talus Calcaneus (a) Right foot, lateral view Metatarsal V (b) Right foot, anterolateral view
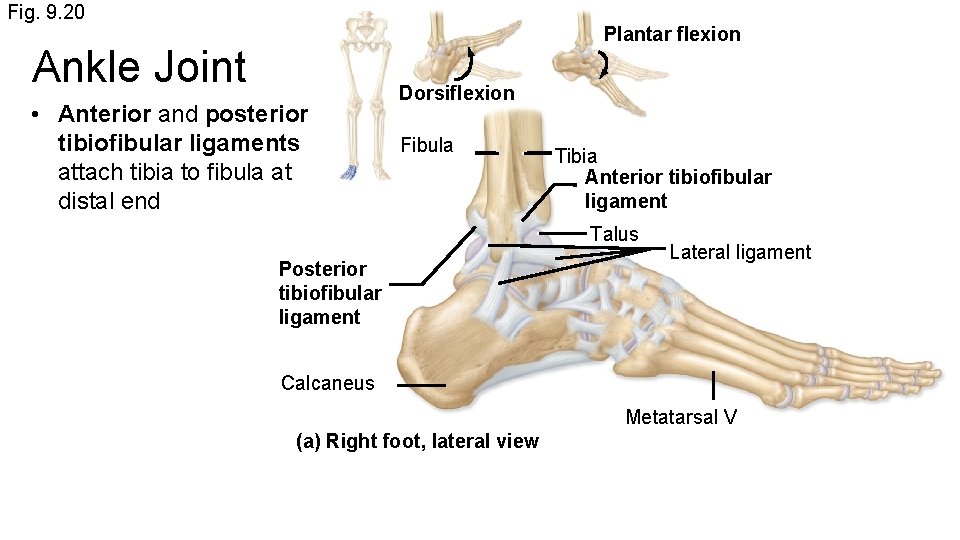
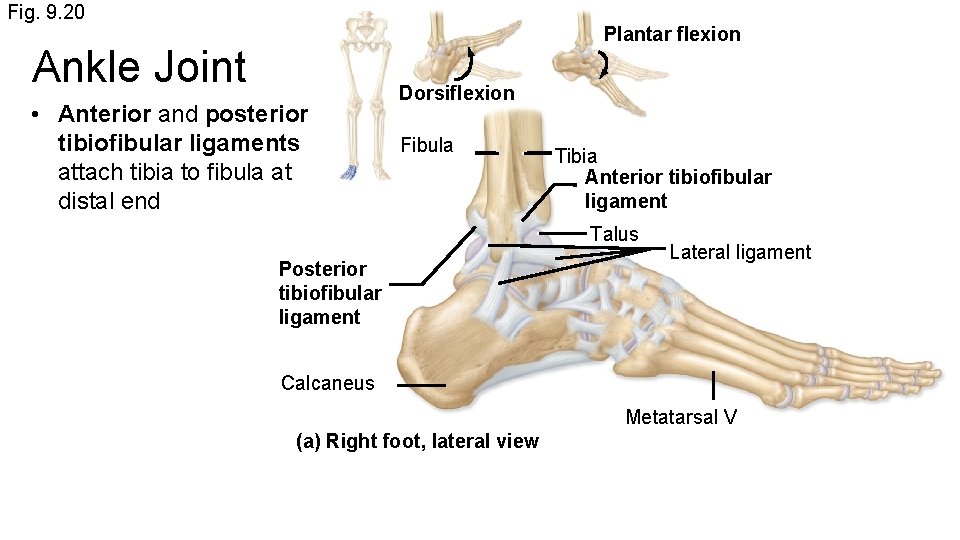
Fig. 9. 20 Plantar flexion Ankle Joint • Anterior and posterior tibiofibular ligaments attach tibia to fibula at distal end Dorsiflexion Fibula Tibia Anterior tibiofibular ligament Talus Posterior tibiofibular ligament Lateral ligament Calcaneus Metatarsal V (a) Right foot, lateral view
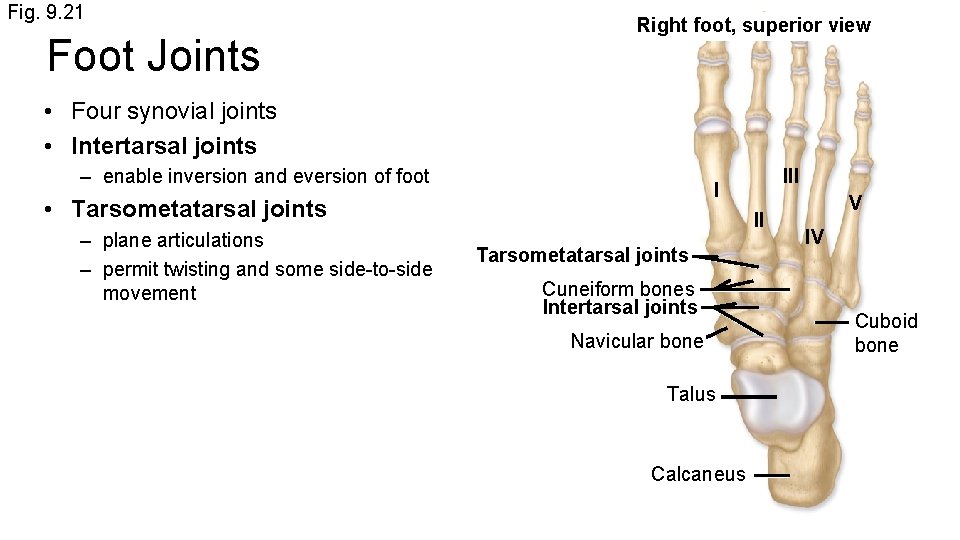
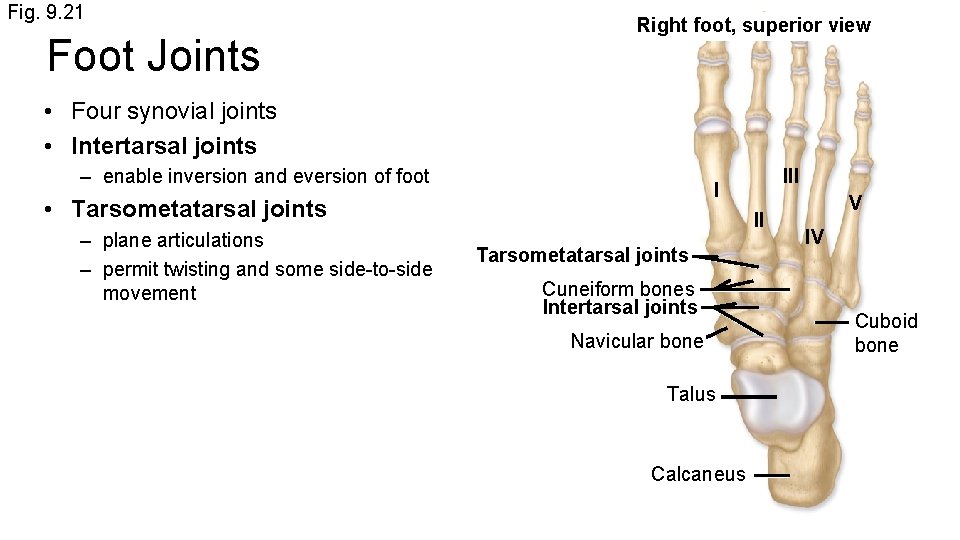
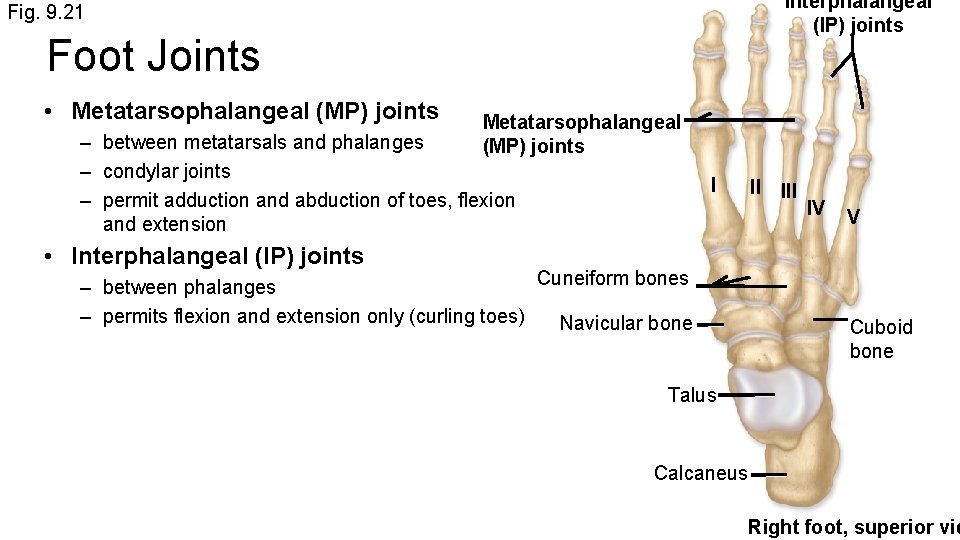
Fig. 9. 21 Foot Joints Right foot, superior view • Four synovial joints • Intertarsal joints – enable inversion and eversion of foot I • Tarsometatarsal joints – plane articulations – permit twisting and some side-to-side movement III II Tarsometatarsal joints Cuneiform bones Intertarsal joints Navicular bone Talus Calcaneus V IV Cuboid bone
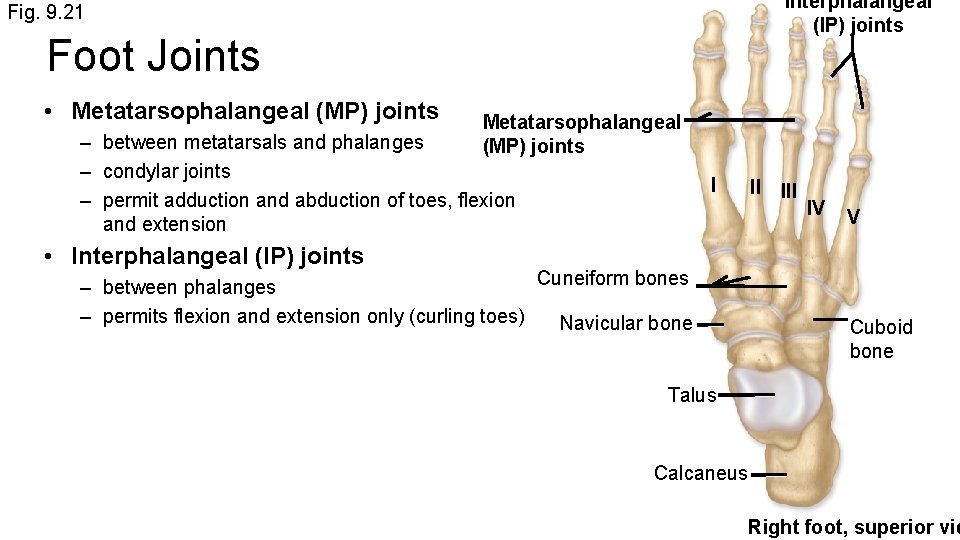
Interphalangeal (IP) joints Fig. 9. 21 Foot Joints • Metatarsophalangeal (MP) joints – between metatarsals and phalanges – condylar joints – permit adduction and abduction of toes, flexion and extension I II IV V • Interphalangeal (IP) joints Cuneiform bones – between phalanges – permits flexion and extension only (curling toes) Navicular bone Cuboid bone Talus Calcaneus Right foot, superior vie
Aging of the Joints • Size, flexibility and shape of joints affected and modified by use – active joints have larger and thicker capsules – active joints have larger ligaments and bones • Age or injury can cause calcification or synostosis of joint • Arthritis involves damage to articular cartilage – osteoarthritis (degenerative arthritis) usually results from wear and tear – exercise compresses articular cartilages, synovial fluid squeezed out and pulled back in, providing nutrients to joints – exercise strengthens muscles supporting joints – extreme exercise may aggravate joint problems, leading to osteoarthritis
Other forms of arthritis • Gouty arthritis (gout) results from uric acid buildup in blood – often seen in middle age and older, especially in males – urate crystals accumulate in blood, synovial fluid, and synovial membranes – causes joint pain • Rheumatoid arthritis (RA) is autoimmune disease – usually develops in young or middle-aged people – causes pain and swelling of joints, muscle weakness, osteoporosis – may lead to blindness