Chapter 8 Smooth Muscles Smooth Muscles Location Structure
- Slides: 15
Chapter 8: Smooth Muscles
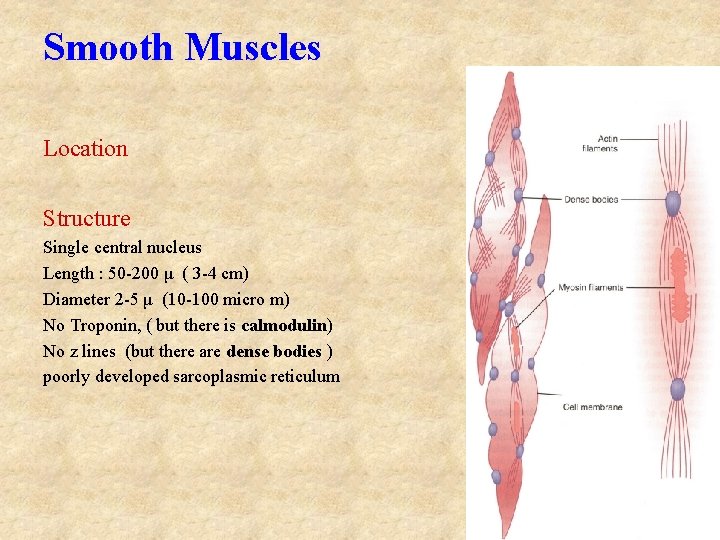
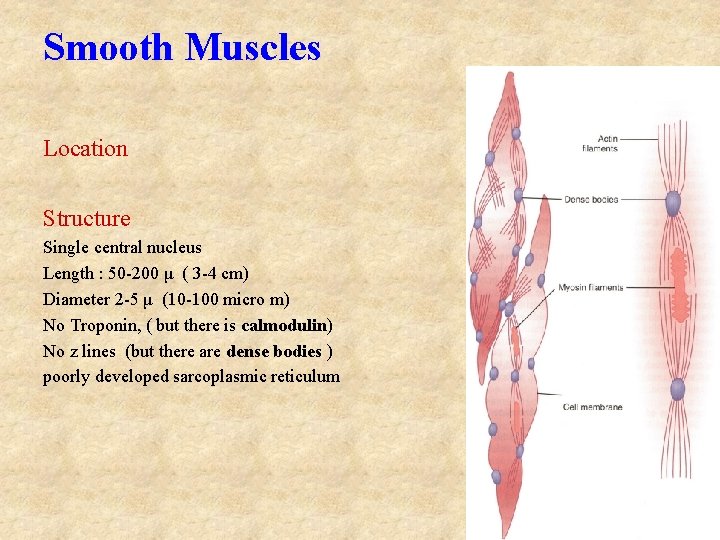
Smooth Muscles Location Structure Single central nucleus Length : 50 -200 μ ( 3 -4 cm) Diameter 2 -5 μ (10 -100 micro m) No Troponin, ( but there is calmodulin) No z lines (but there are dense bodies ) poorly developed sarcoplasmic reticulum
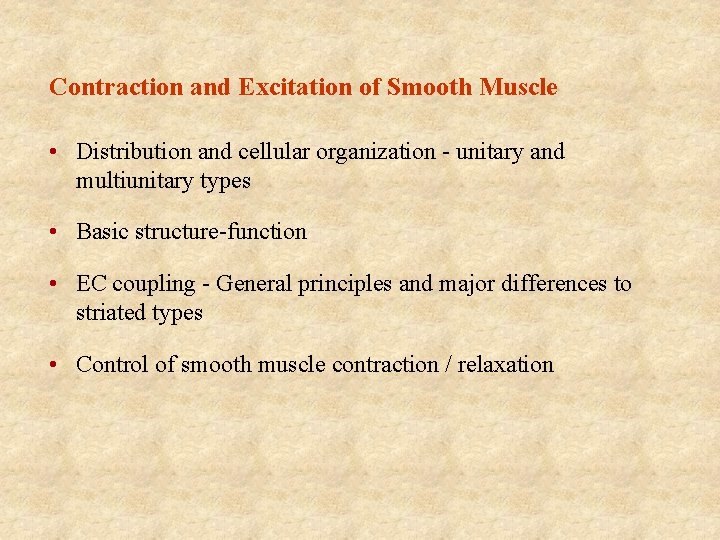
Contraction and Excitation of Smooth Muscle • Distribution and cellular organization - unitary and multiunitary types • Basic structure-function • EC coupling - General principles and major differences to striated types • Control of smooth muscle contraction / relaxation
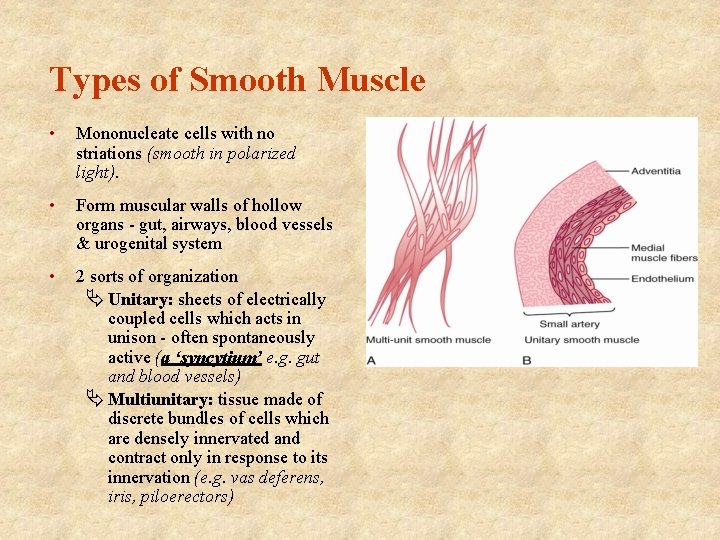
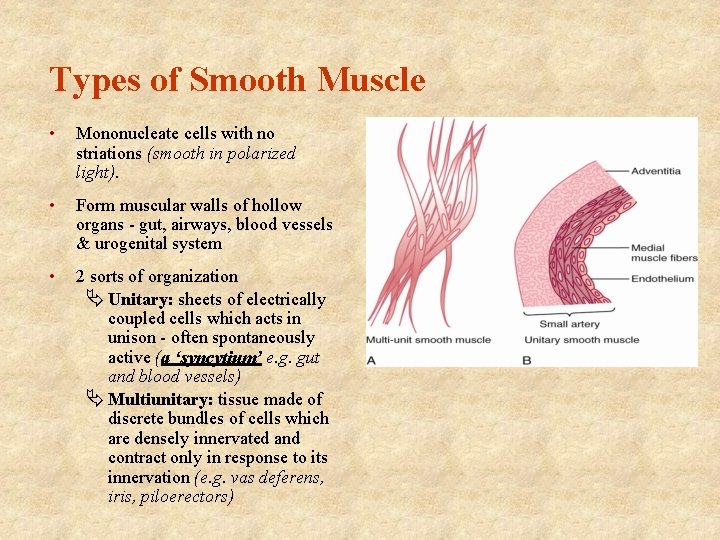
Types of Smooth Muscle • Mononucleate cells with no striations (smooth in polarized light). • Form muscular walls of hollow organs - gut, airways, blood vessels & urogenital system • 2 sorts of organization Ä Unitary: sheets of electrically coupled cells which acts in unison - often spontaneously active (a ‘syncytium’ e. g. gut and blood vessels) Ä Multiunitary: tissue made of discrete bundles of cells which are densely innervated and contract only in response to its innervation (e. g. vas deferens, iris, piloerectors)
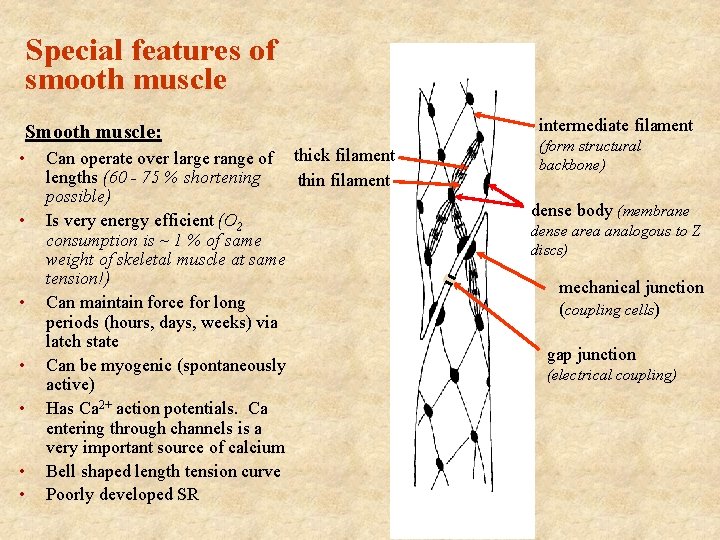
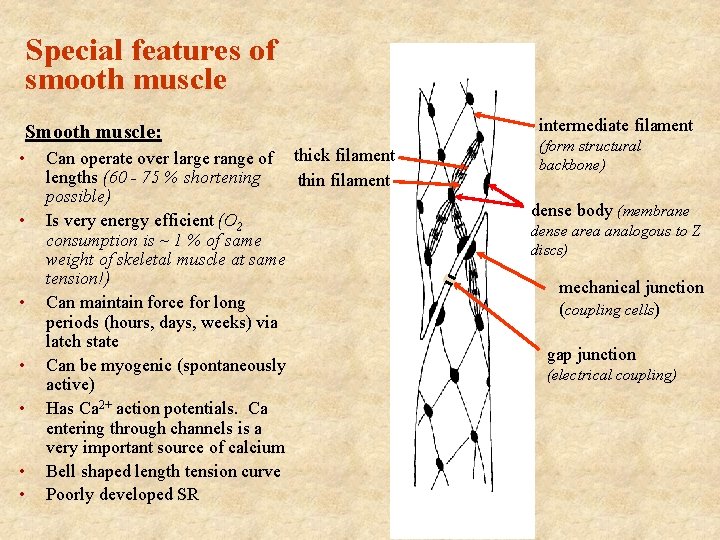
Special features of smooth muscle Smooth muscle: • • Can operate over large range of thick filament lengths (60 - 75 % shortening thin filament possible) Is very energy efficient (O 2 consumption is ~ 1 % of same weight of skeletal muscle at same tension!) Can maintain force for long periods (hours, days, weeks) via latch state Can be myogenic (spontaneously active) Has Ca 2+ action potentials. Ca entering through channels is a very important source of calcium Bell shaped length tension curve Poorly developed SR intermediate filament (form structural backbone) dense body (membrane dense area analogous to Z discs) mechanical junction (coupling cells) gap junction (electrical coupling)
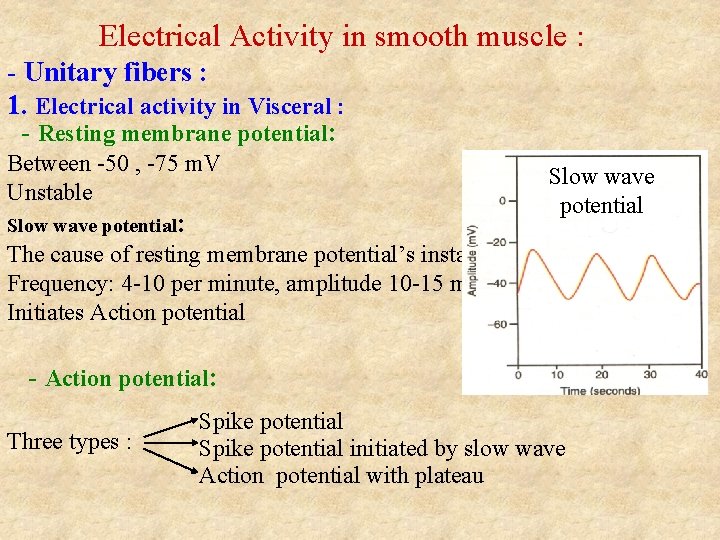
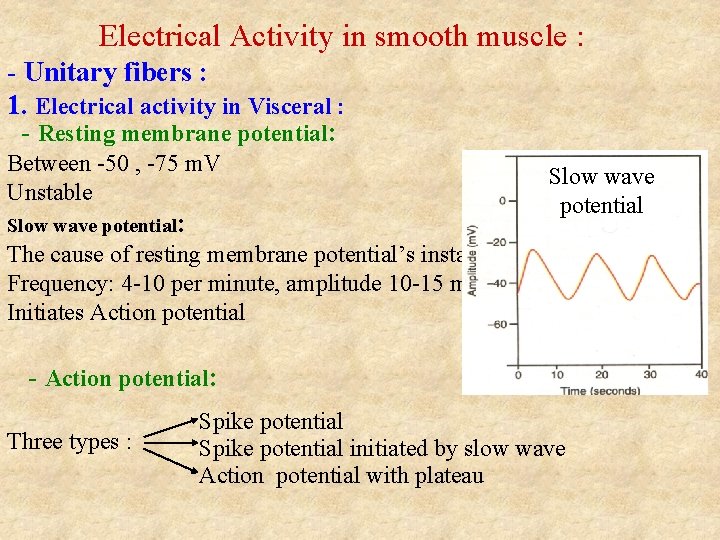
Electrical Activity in smooth muscle : - Unitary fibers : 1. Electrical activity in Visceral : - Resting membrane potential: Between -50 , -75 m. V Unstable Slow wave potential: Slow wave potential The cause of resting membrane potential’s instability Frequency: 4 -10 per minute, amplitude 10 -15 m. V Initiates Action potential - Action potential: Three types : Spike potential initiated by slow wave Action potential with plateau
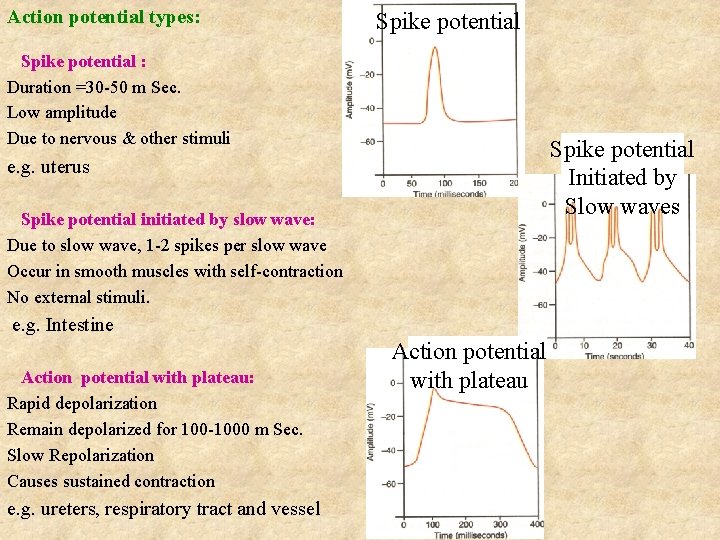
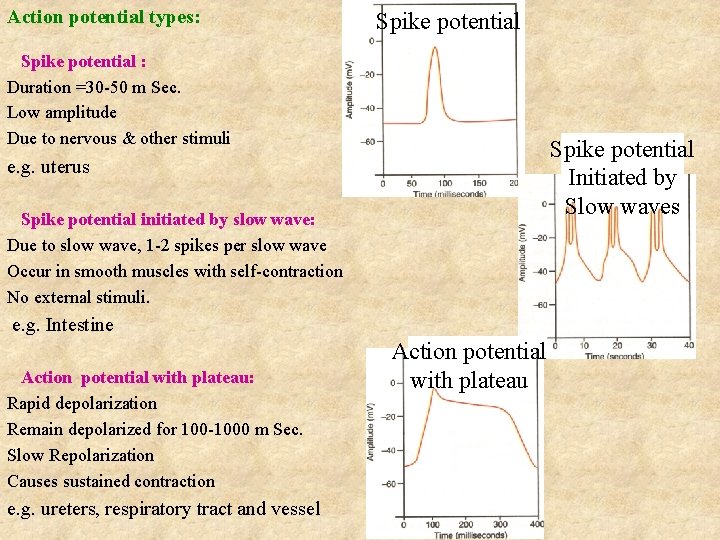
Action potential types: Spike potential : Duration =30 -50 m Sec. Low amplitude Due to nervous & other stimuli Spike potential Initiated by Slow waves e. g. uterus Spike potential initiated by slow wave: Due to slow wave, 1 -2 spikes per slow wave Occur in smooth muscles with self-contraction No external stimuli. e. g. Intestine Action potential with plateau: Rapid depolarization Remain depolarized for 100 -1000 m Sec. Slow Repolarization Causes sustained contraction e. g. ureters, respiratory tract and vessel Action potential with plateau
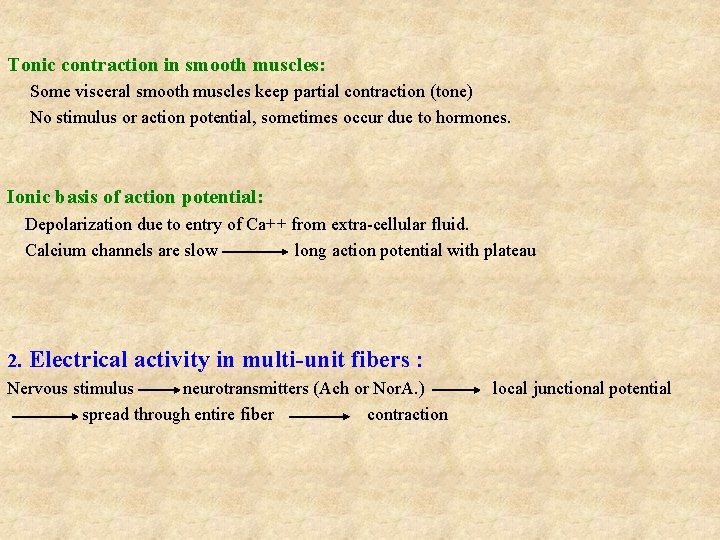
Tonic contraction in smooth muscles: Some visceral smooth muscles keep partial contraction (tone) No stimulus or action potential, sometimes occur due to hormones. Ionic basis of action potential: Depolarization due to entry of Ca++ from extra-cellular fluid. Calcium channels are slow long action potential with plateau 2. Electrical activity in multi-unit fibers : Nervous stimulus neurotransmitters (Ach or Nor. A. ) spread through entire fiber contraction local junctional potential
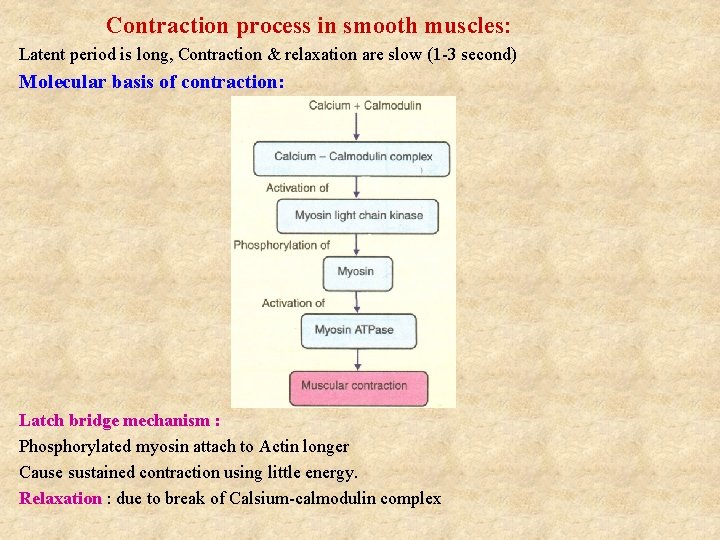
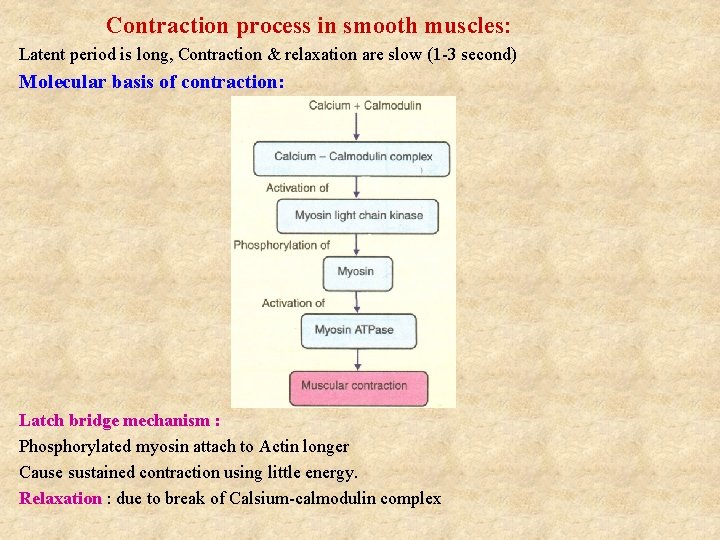
Contraction process in smooth muscles: Latent period is long, Contraction & relaxation are slow (1 -3 second) Molecular basis of contraction: Latch bridge mechanism : Phosphorylated myosin attach to Actin longer Cause sustained contraction using little energy. Relaxation : due to break of Calsium-calmodulin complex
Hormones’ effect on smooth muscle : Depends on receptors : excitatory receptors inhibitory receptors depolarization hyperpolarization Innervation of smooth muscle : Innervated by sympathetic & parasympathetic nerves. Nerves control (but can’t initiate) muscular activities The Tone is not controlled by nerves. Neuromuscular junction in smooth muscles: No defined neuromuscular junction, Neurotransmitters are released into interstitial fluid contraction no contraction
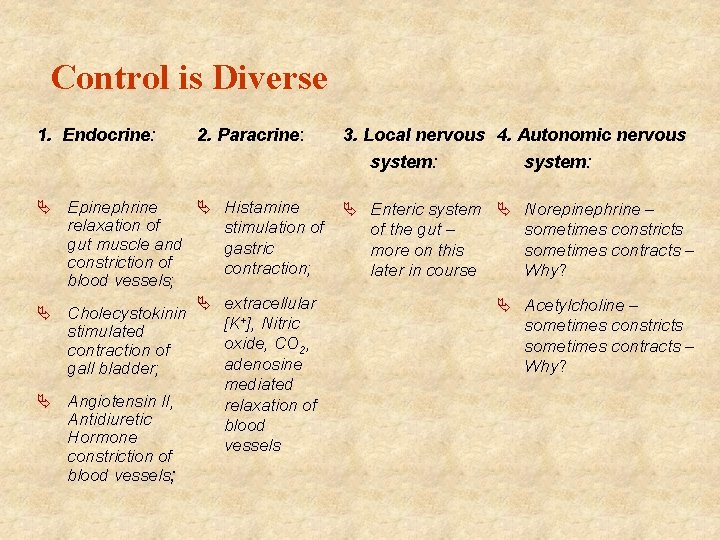
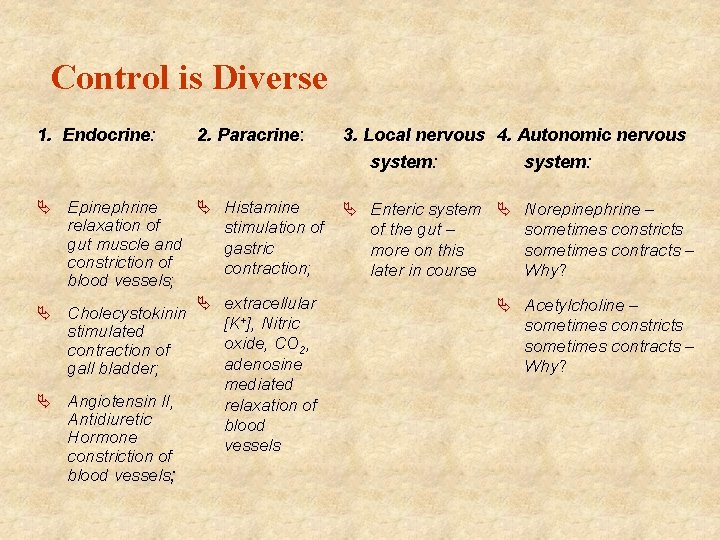
Control is Diverse 1. Endocrine: 2. Paracrine: 3. Local nervous 4. Autonomic nervous system: Ä Histamine Ä Epinephrine relaxation of stimulation of gut muscle and gastric constriction of contraction; blood vessels; Ä extracellular Ä Cholecystokinin +], Nitric [K stimulated oxide, CO 2, contraction of adenosine gall bladder; mediated Ä Angiotensin II, relaxation of Antidiuretic blood Hormone vessels constriction of blood vessels; system: Ä Enteric system Ä Norepinephrine – of the gut – sometimes constricts more on this sometimes contracts – later in course Why? Ä Acetylcholine – sometimes constricts sometimes contracts – Why?
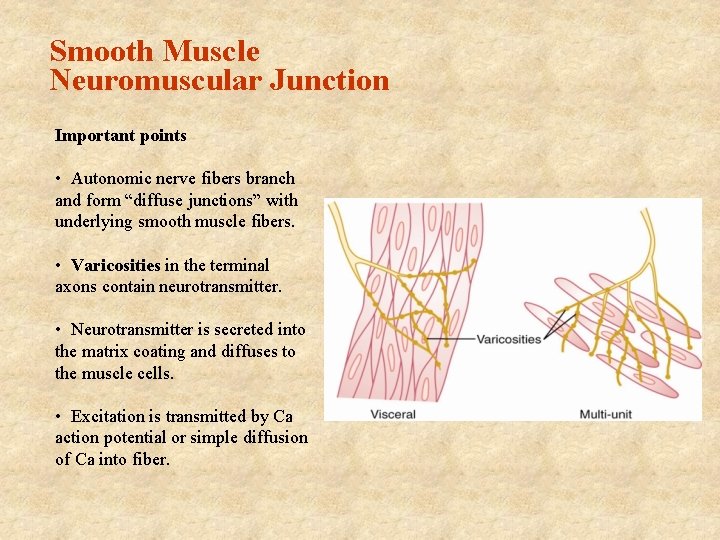
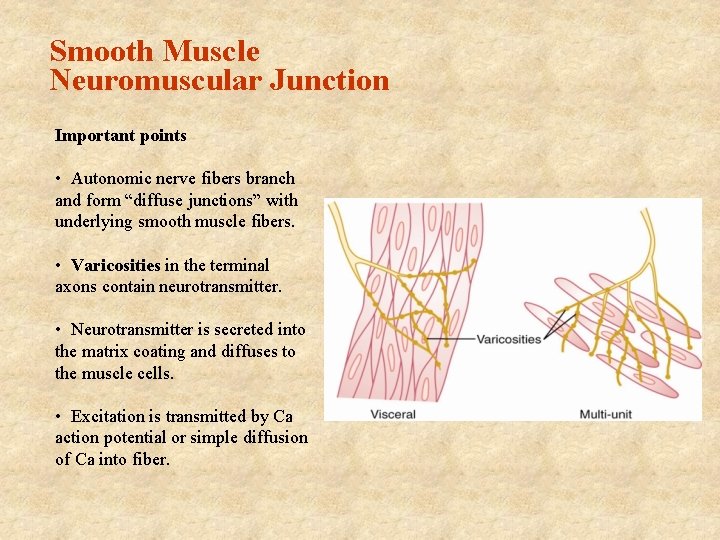
Smooth Muscle Neuromuscular Junction Important points • Autonomic nerve fibers branch and form “diffuse junctions” with underlying smooth muscle fibers. • Varicosities in the terminal axons contain neurotransmitter. • Neurotransmitter is secreted into the matrix coating and diffuses to the muscle cells. • Excitation is transmitted by Ca action potential or simple diffusion of Ca into fiber.
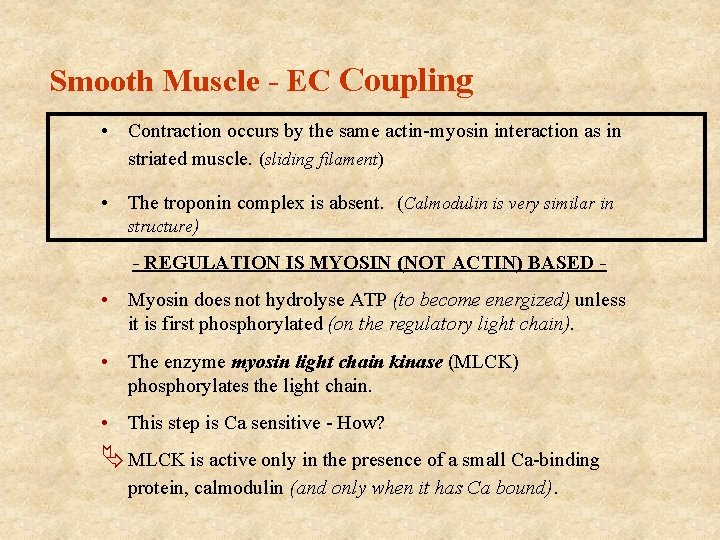
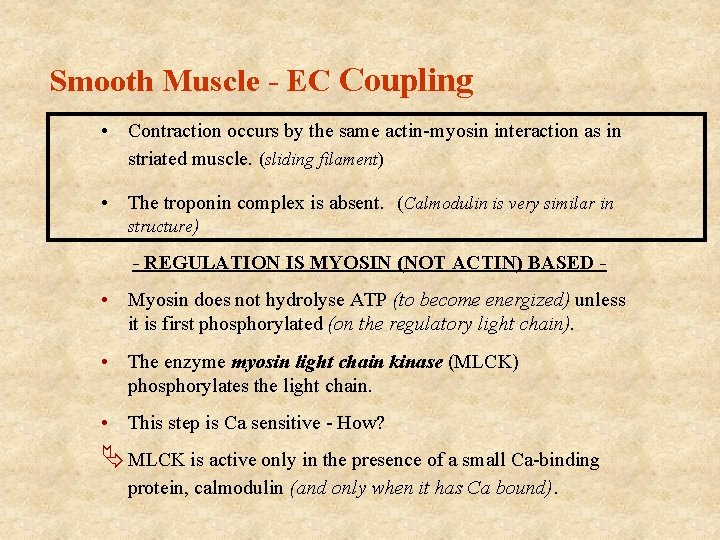
Smooth Muscle - EC Coupling • Contraction occurs by the same actin-myosin interaction as in striated muscle. (sliding filament) • The troponin complex is absent. (Calmodulin is very similar in structure) - REGULATION IS MYOSIN (NOT ACTIN) BASED - • Myosin does not hydrolyse ATP (to become energized) unless it is first phosphorylated (on the regulatory light chain). • The enzyme myosin light chain kinase (MLCK) phosphorylates the light chain. • This step is Ca sensitive - How? Ä MLCK is active only in the presence of a small Ca-binding protein, calmodulin (and only when it has Ca bound).
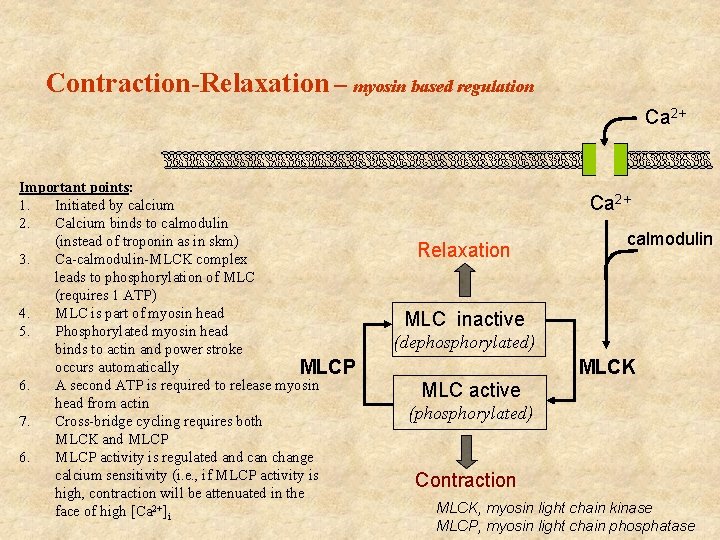
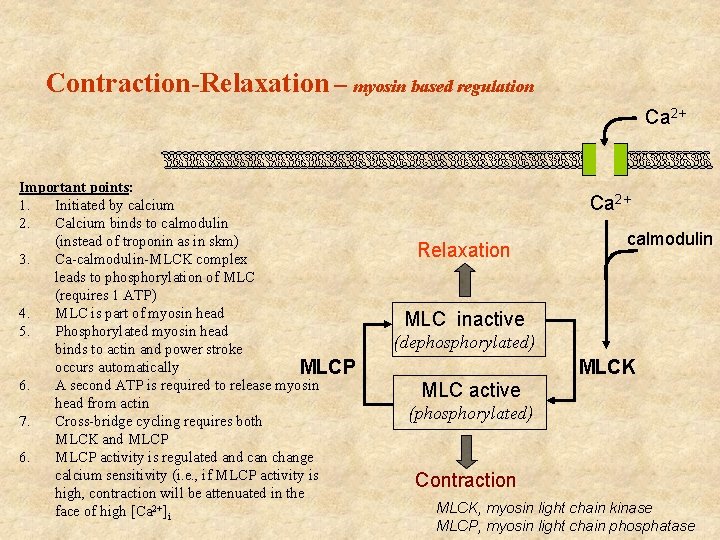
Contraction-Relaxation – myosin based regulation Ca 2+ Important points: 1. Initiated by calcium 2. Calcium binds to calmodulin (instead of troponin as in skm) 3. Ca-calmodulin-MLCK complex leads to phosphorylation of MLC (requires 1 ATP) 4. MLC is part of myosin head 5. Phosphorylated myosin head binds to actin and power stroke occurs automatically MLCP 6. A second ATP is required to release myosin head from actin 7. Cross-bridge cycling requires both MLCK and MLCP 6. MLCP activity is regulated and can change calcium sensitivity (i. e. , if MLCP activity is high, contraction will be attenuated in the face of high [Ca 2+]i Ca 2+ Relaxation calmodulin MLC inactive (dephosphorylated) MLCK MLC active (phosphorylated) Contraction MLCK, myosin light chain kinase MLCP, myosin light chain phosphatase