Chapter 8 Head Assessment face and neck Faculty
- Slides: 21
Chapter (8) Head Assessment, face and neck Faculty of Nursing-IUG
Assessment of the Head Inspects the size, shape, and contour of head. The skull is generally round with anterior & posterior prominences. Large infant's head may be hydrocephalus. Large adult's head & facial bones resulting of acromegaly. Palpates the skull for nodules or masses Assessment of the eye Assess external eye structures and pupils, visual acuity, ocular movements, Peripheral vision. Assessment of external eye structures: position and alignment of eyes, eye brow, eye lids, eye lashes, lacrimal glands, pupils and iris. Assessment of pupils done by using penlight which produce constriction of pupils to show accommodation and
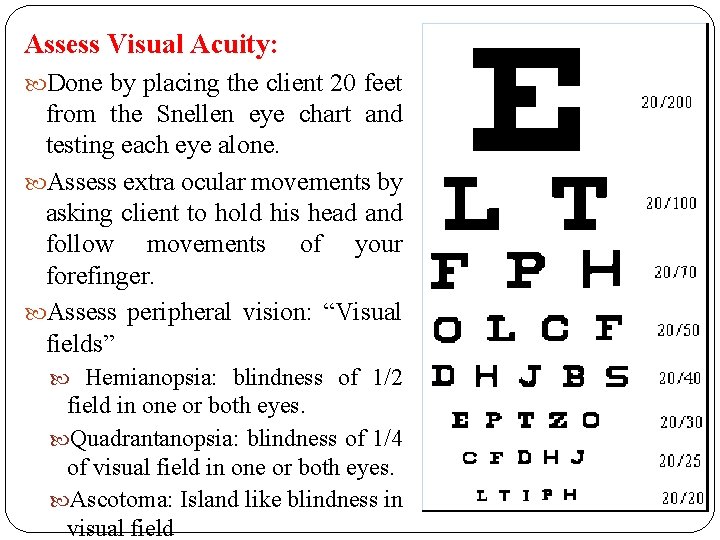
Assess internal eye structures e. g. iris , retina, macula etc Consider the following Factors: Age use of corrective lens, artificial eye, allergies, pain, visual disturbances Health related factors such increase Blood Pressure, or Diabetes mellitus Using the following equipment to assess the eyes: Eye chart (Snellen chart), Chart or newsprint. Cover card. Penlight, and ophthalmoscope Ask the client about history of previous eye surgery, 3 trauma, use of corrective glasses or contact lenses, blurred vision, Diplopia, strabismus, recent changes in vision, date of previous vision test, allergies, eye redness, and frequent watering discharge
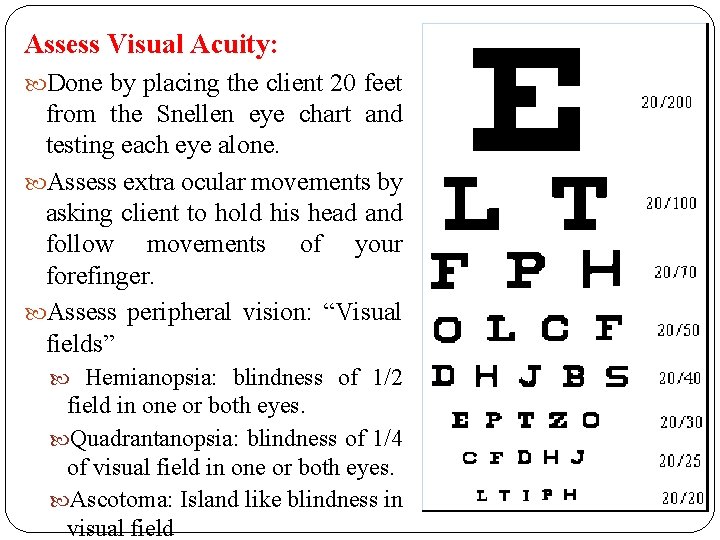
Assess Visual Acuity: Done by placing the client 20 feet from the Snellen eye chart and testing each eye alone. Assess extra ocular movements by asking client to hold his head and follow movements of your forefinger. Assess peripheral vision: “Visual fields” Hemianopsia: blindness of 1/2 field in one or both eyes. Quadrantanopsia: blindness of 1/4 of visual field in one or both eyes. Ascotoma: Island like blindness in visual field
Ear Assessment Take history of ear surgery, trauma, frequent infection, ear pain, drainage, hearing loss, tinnitus, vertigo, ototoxic medications, and last hearing examination Assess client in sitting position & inspects the auricle’s placement, size, symmetry, and color. Redness: sign of inflammation or fever. Color of ears must be the same as of the face. Pallor: indicate frost bite. Palpate the auricles for texture, tenderness, and skin lesion. If client complains of pain: pull the auricle and press on the tragus and behind the ear over the mastoid process if pain increase, means external ear infection, if pain is not increase, means middle ear infection may be present. 5
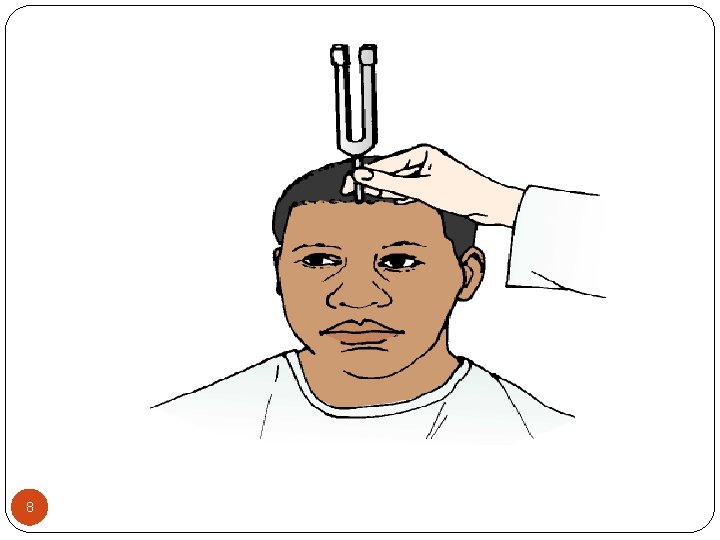
Inspection the ear canal for size and discharge. Assessment of cerumen if it is yellow or green may indicate infection. Assessment of hearing acuity: done simply by identification of voice tones, with the client repeating testing words spoken by the nurse (whisper test) N. B: deeper structure and middle ear can be observed only by otoscope. Whisper Test (patient with normal acuity can correctly repeat what was whispered) Weber Test (uses bone conduction to test lateralization of sound by a tuning fork) Rinne Test (useful for distinguishing between conductive and sensorineural hearing losses) 6
Weber Test: A tuning fork, set in motion by grasping it firmly by its stem and tapping it on the examiner’s hand, is placed on the patient’s head. A person with normal hearing will hear the sound equally in both ears or describe the sound as centered in the middle of the head. In an abnormal patient, the sound is heard louder in one ear (lateralization). Rinne Test The examiner shifts the stem of a vibrating tuning fork between two positions: 2 inches from the opening of the ear canal (for air conduction) and against the mastoid bone (for bone conduction). Patient is asked to indicate which tone is louder or when the tone is no longer audible. Normally, sound heard by air conduction is audible longer and louder than sound heard by bone conduction. With a conductive hearing loss, bone-conducted sound is heard
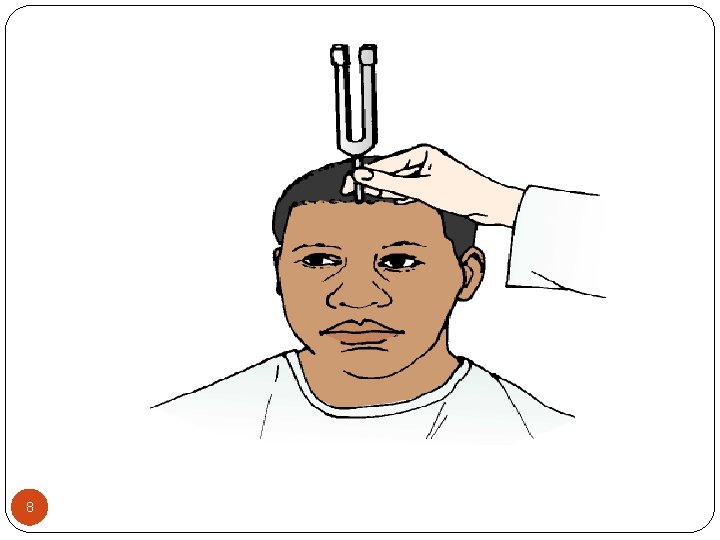
8
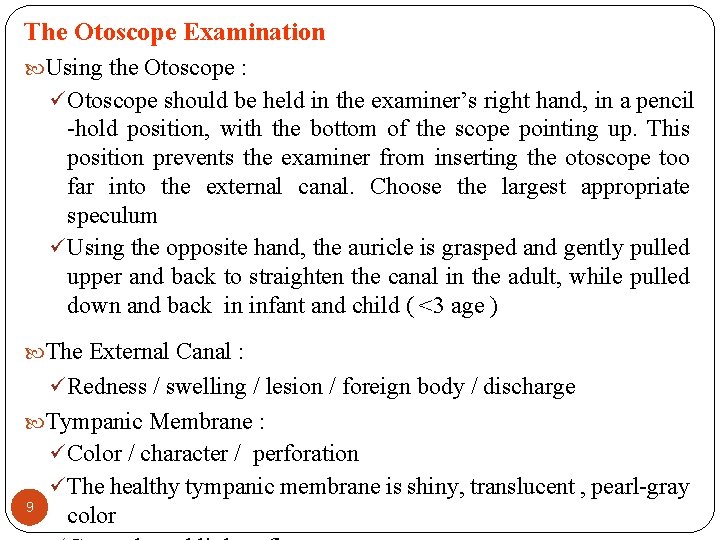
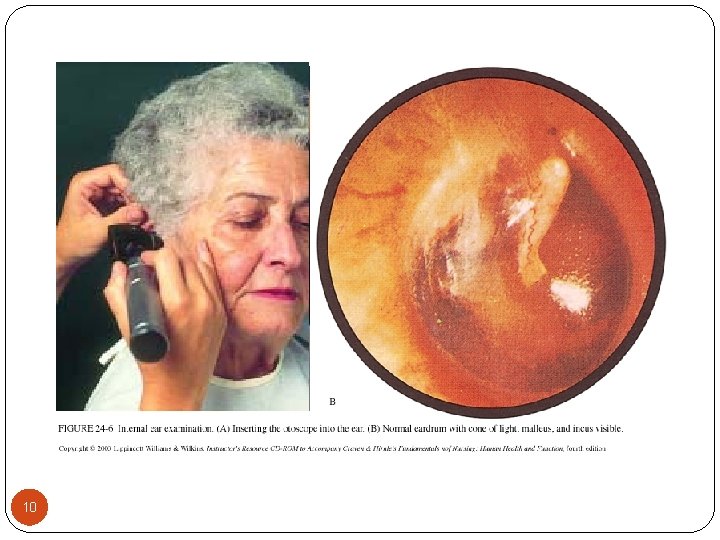
The Otoscope Examination Using the Otoscope : ü Otoscope should be held in the examiner’s right hand, in a pencil -hold position, with the bottom of the scope pointing up. This position prevents the examiner from inserting the otoscope too far into the external canal. Choose the largest appropriate speculum ü Using the opposite hand, the auricle is grasped and gently pulled upper and back to straighten the canal in the adult, while pulled down and back in infant and child ( <3 age ) The External Canal : ü Redness / swelling / lesion / foreign body / discharge Tympanic Membrane : ü Color / character / perforation ü The healthy tympanic membrane is shiny, translucent , pearl-gray 9 color
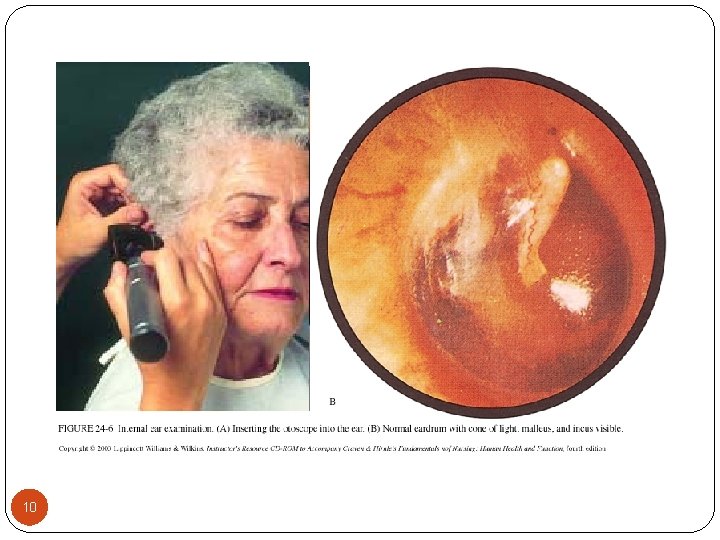
10
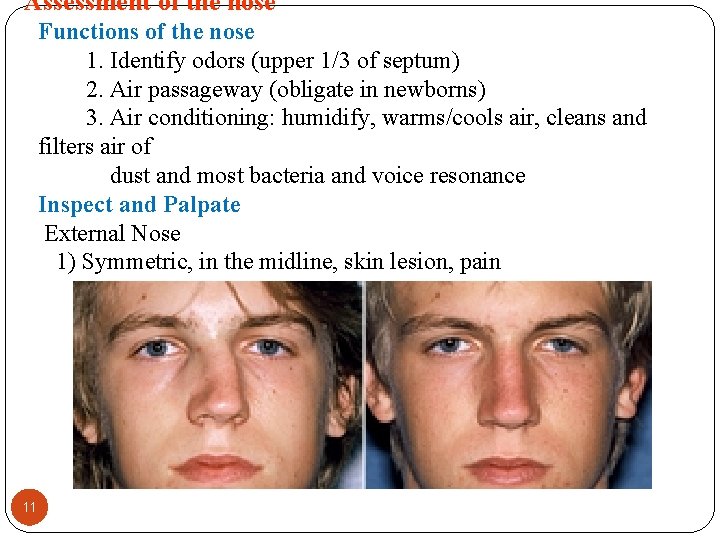
Assessment of the nose Functions of the nose 1. Identify odors (upper 1/3 of septum) 2. Air passageway (obligate in newborns) 3. Air conditioning: humidify, warms/cools air, cleans and filters air of dust and most bacteria and voice resonance Inspect and Palpate External Nose 1) Symmetric, in the midline, skin lesion, pain 11
Nostril patency: Inspect & observe symmetry, inflammation & deformity. In case of swelling or deformities of nose, the nose is palpated gently for tenderness, swelling and underlying deviations. Normally the external nose is symmetrical, strait, non tender, and without discharge. Assess mucosa which is normally pink in color. Yellowish or greenish discharge – means sinus infection. Pale mucosa with clear discharge – means allergy. For client with NGT, nurse should routinely checks for local breakdown of skin “Excoriation” of the nostril that characterized by redness and sloughing of the skin 12
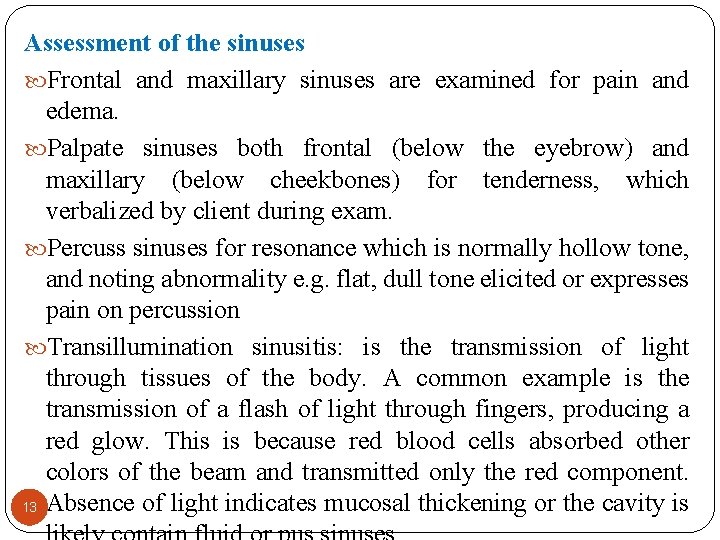
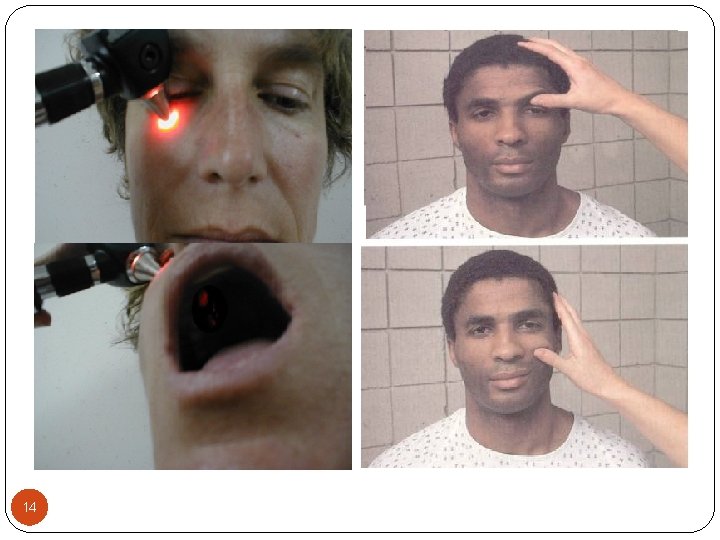
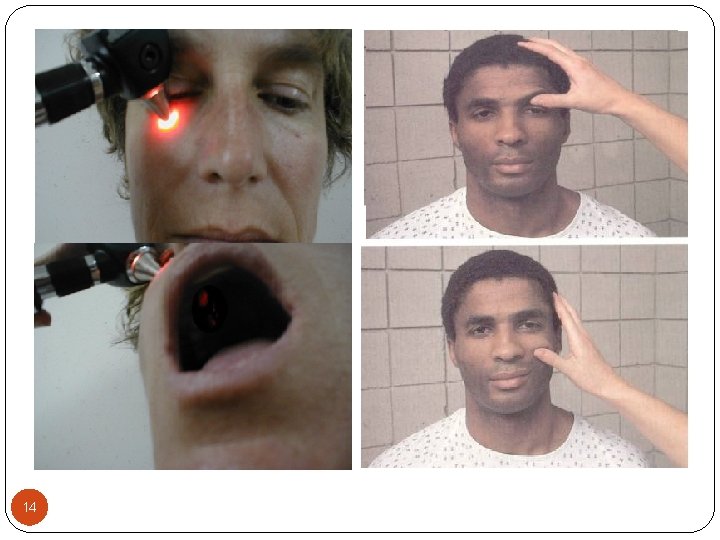
Assessment of the sinuses Frontal and maxillary sinuses are examined for pain and edema. Palpate sinuses both frontal (below the eyebrow) and maxillary (below cheekbones) for tenderness, which verbalized by client during exam. Percuss sinuses for resonance which is normally hollow tone, and noting abnormality e. g. flat, dull tone elicited or expresses pain on percussion Transillumination sinusitis: is the transmission of light through tissues of the body. A common example is the transmission of a flash of light through fingers, producing a red glow. This is because red blood cells absorbed other colors of the beam and transmitted only the red component. 13 Absence of light indicates mucosal thickening or the cavity is
14
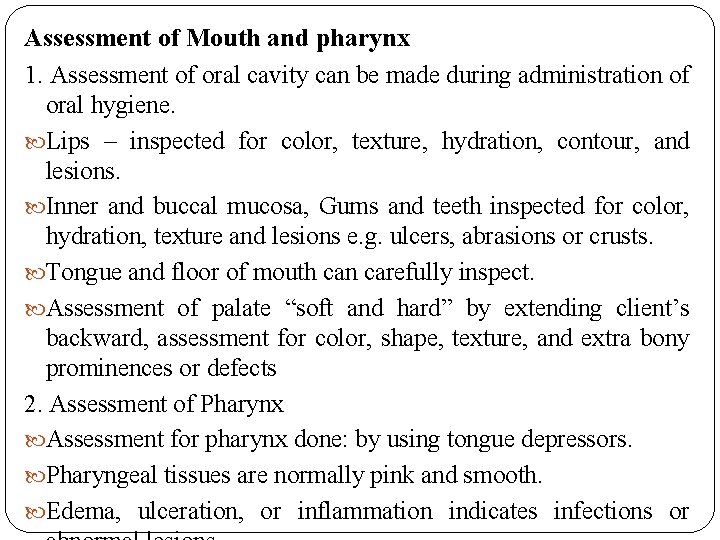
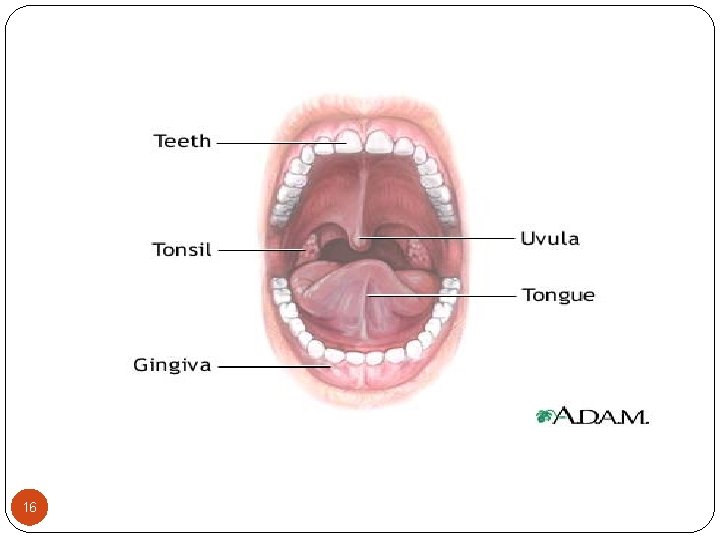
Assessment of Mouth and pharynx 1. Assessment of oral cavity can be made during administration of oral hygiene. Lips – inspected for color, texture, hydration, contour, and lesions. Inner and buccal mucosa, Gums and teeth inspected for color, hydration, texture and lesions e. g. ulcers, abrasions or crusts. Tongue and floor of mouth can carefully inspect. Assessment of palate “soft and hard” by extending client’s backward, assessment for color, shape, texture, and extra bony prominences or defects 2. Assessment of Pharynx Assessment for pharynx done: by using tongue depressors. Pharyngeal tissues are normally pink and smooth. Edema, ulceration, or inflammation indicates infections or
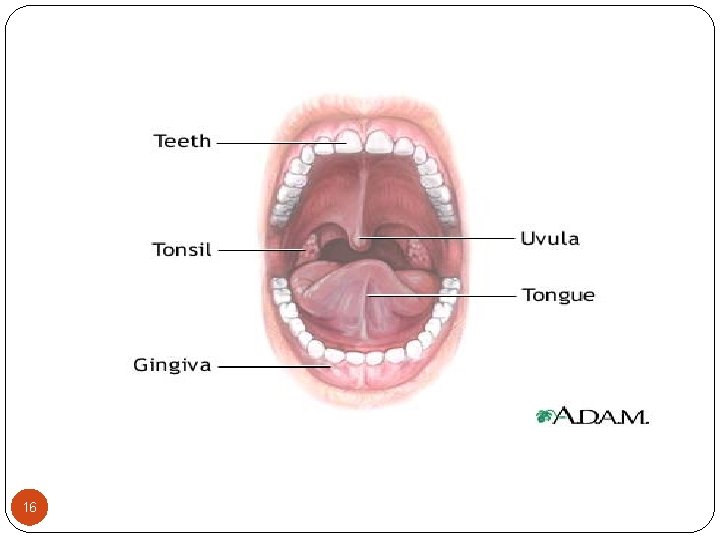
16
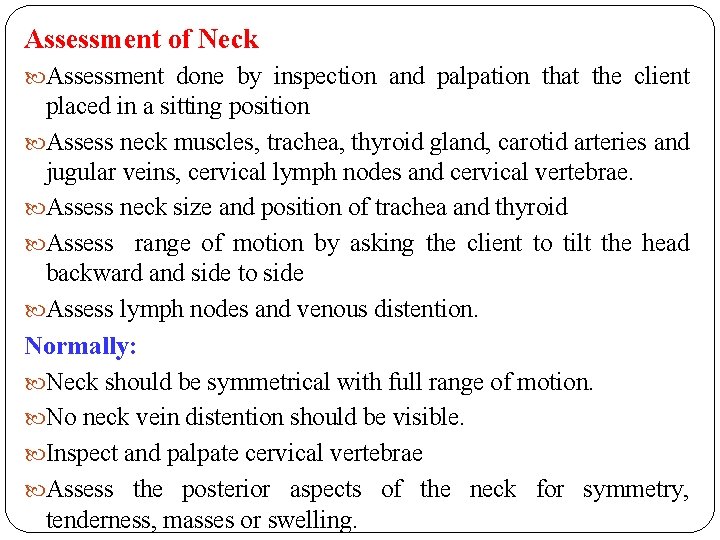
Assessment of Neck Assessment done by inspection and palpation that the client placed in a sitting position Assess neck muscles, trachea, thyroid gland, carotid arteries and jugular veins, cervical lymph nodes and cervical vertebrae. Assess neck size and position of trachea and thyroid Assess range of motion by asking the client to tilt the head backward and side to side Assess lymph nodes and venous distention. Normally: Neck should be symmetrical with full range of motion. No neck vein distention should be visible. Inspect and palpate cervical vertebrae Assess the posterior aspects of the neck for symmetry, tenderness, masses or swelling.
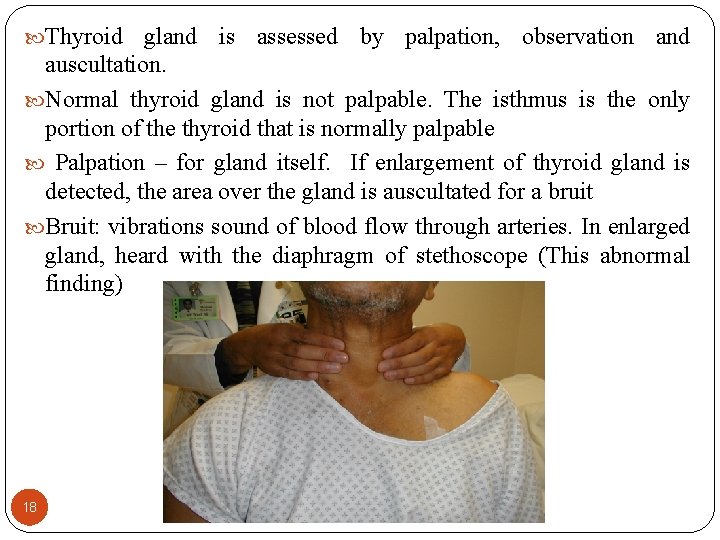
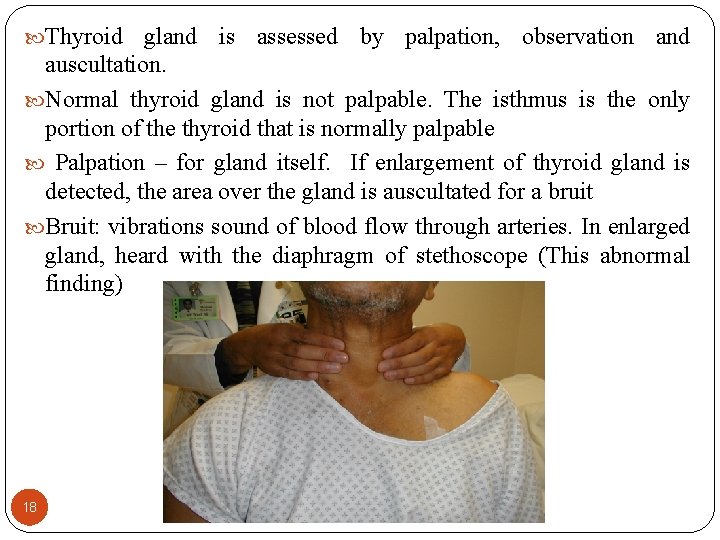
Thyroid gland is assessed by palpation, observation and auscultation. Normal thyroid gland is not palpable. The isthmus is the only portion of the thyroid that is normally palpable Palpation – for gland itself. If enlargement of thyroid gland is detected, the area over the gland is auscultated for a bruit Bruit: vibrations sound of blood flow through arteries. In enlarged gland, heard with the diaphragm of stethoscope (This abnormal finding) 18
Trachea normally centered; (at the suprasternal notch) The cartilages should be smooth, non tender and move easily under examiner’s fingers when the client swallow Palpation done by placing the thumb and forefinger on each side of the trachea Assessment of the lymphatic system Lymphatic System consists of a network of collecting ducts, lymph fluids e. g. spleen, thymus, tonsils, adenoids--- etc Functions of lymphatic system Movement and transportation of lymphocytes Production of lymphocytes. Production of antibodies. Phagocytosis Absorption of fat and fat soluble substances.
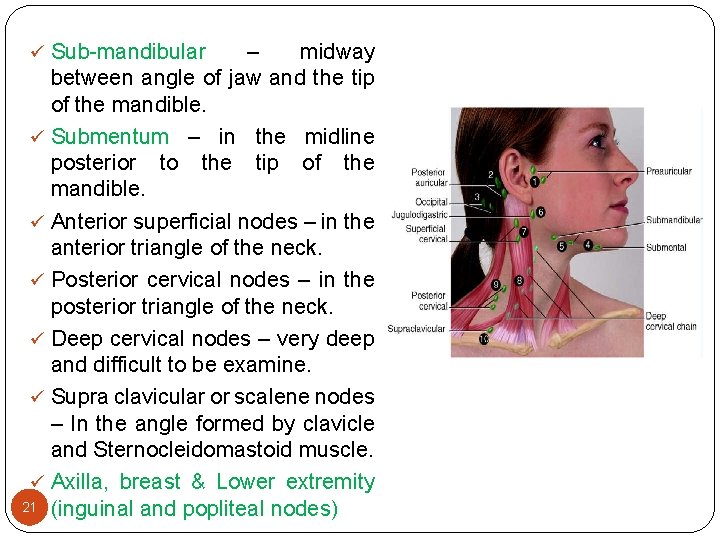
Enlargement of lymph node: provides early indication of infection or malignancy. Examination of lymphatic System : 2 steps Firstly inspection for enlarged lymph nodes, skin lesions and edema Secondly palpating gently the lymph nodes areas using pads of "2, 3, 4" fingers in gentle circular motion. Press lightly and then increasing pressure gradually. Move skin lightly over the under lying tissues & not moving the examining fingers over the skin. Large nodes due to malignancy are generally not tender vary in size, hard, asymmetrical Some Areas of lymph nodes ü Pre auricular: in front of the ear. ü Mastoid or posterior auricular – behind the ear. Above the mastoid process. ü Occipital – at the base of skull posterior. ü Parotid – near the angle of the jaw.
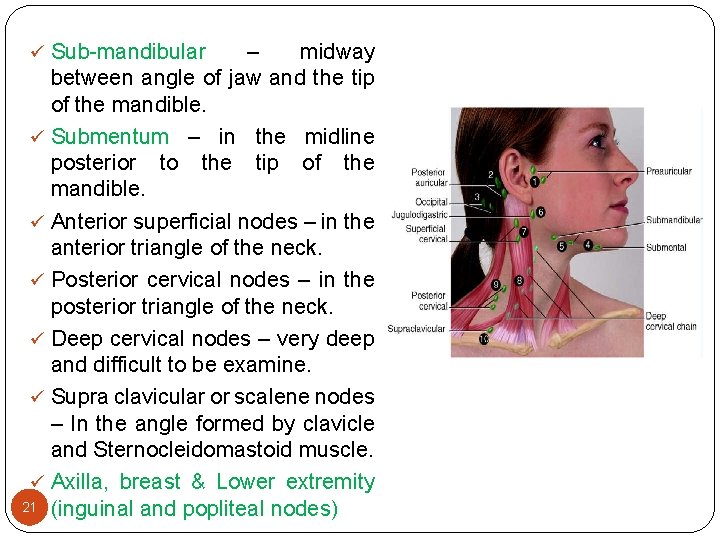
ü Sub-mandibular – midway between angle of jaw and the tip of the mandible. ü Submentum – in the midline posterior to the tip of the mandible. ü Anterior superficial nodes – in the anterior triangle of the neck. ü Posterior cervical nodes – in the posterior triangle of the neck. ü Deep cervical nodes – very deep and difficult to be examine. ü Supra clavicular or scalene nodes – In the angle formed by clavicle and Sternocleidomastoid muscle. ü Axilla, breast & Lower extremity 21 (inguinal and popliteal nodes)