Chapter 8 Excretion of the Kidneys Major Functions



- Slides: 123
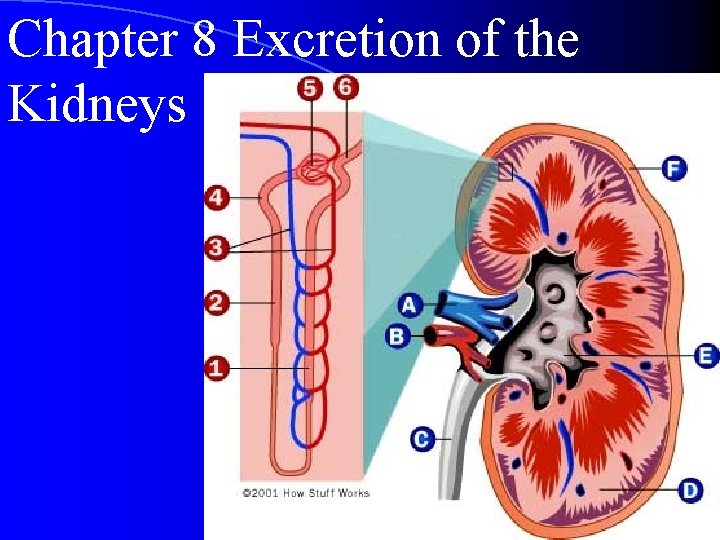
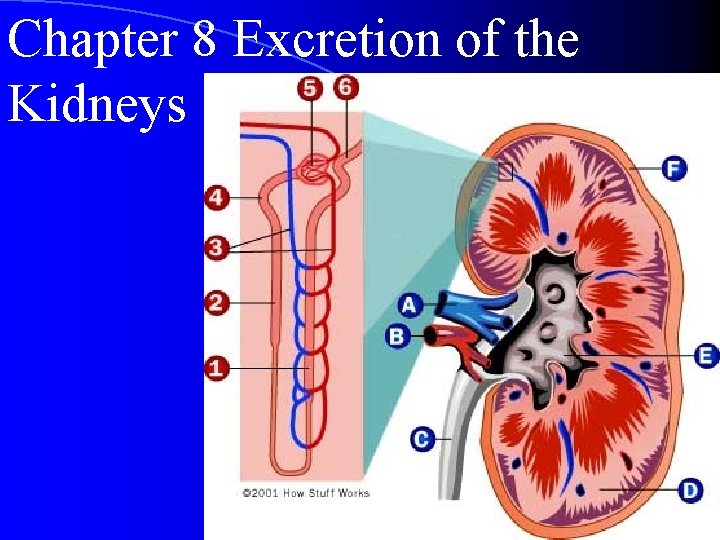
Chapter 8 Excretion of the Kidneys
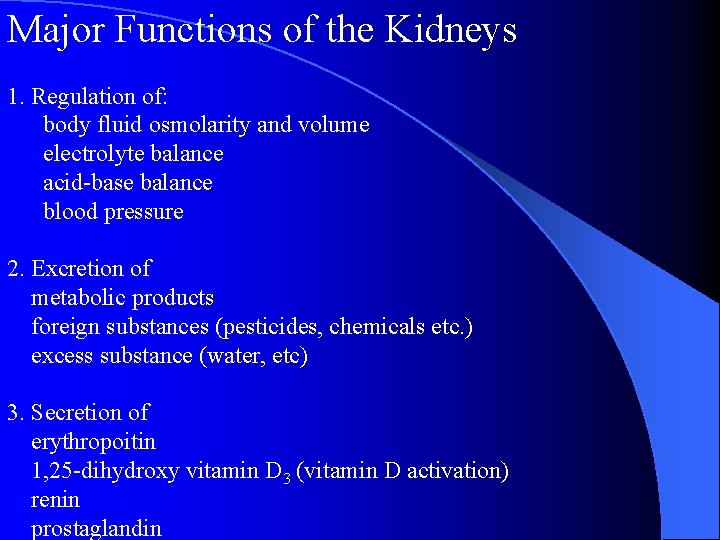
Major Functions of the Kidneys 1. Regulation of: body fluid osmolarity and volume electrolyte balance acid-base balance blood pressure 2. Excretion of metabolic products foreign substances (pesticides, chemicals etc. ) excess substance (water, etc) 3. Secretion of erythropoitin 1, 25 -dihydroxy vitamin D 3 (vitamin D activation) renin prostaglandin
Section 1 Characteristics of Renal Structure and Function I. Physiological Anatomy of the Kidney
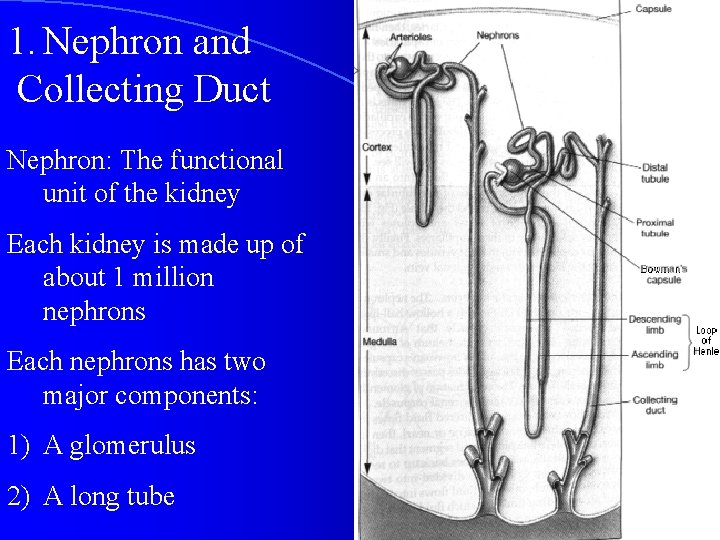
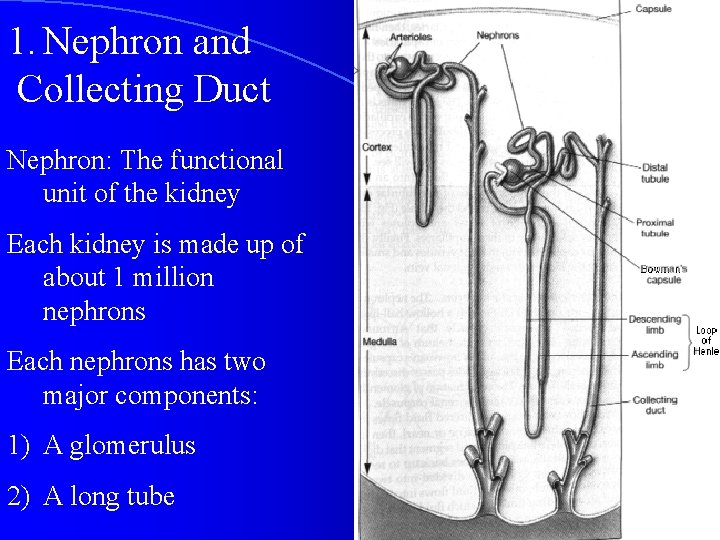
1. Nephron and Collecting Duct Nephron: The functional unit of the kidney Each kidney is made up of about 1 million nephrons Each nephrons has two major components: 1) A glomerulus 2) A long tube
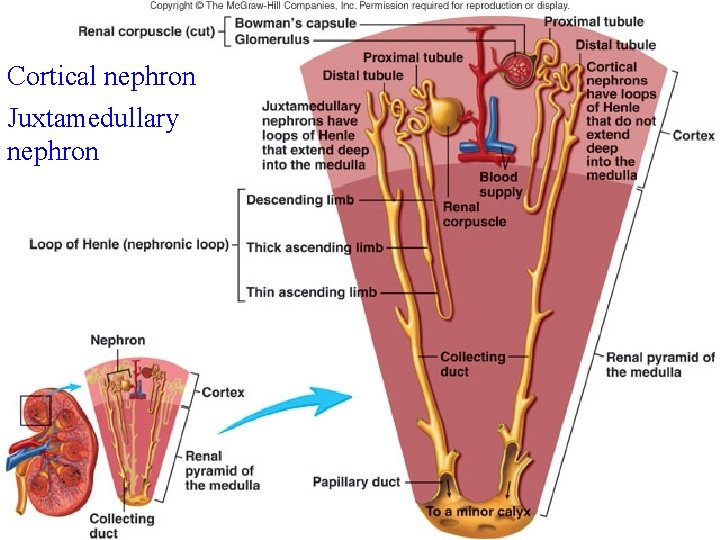
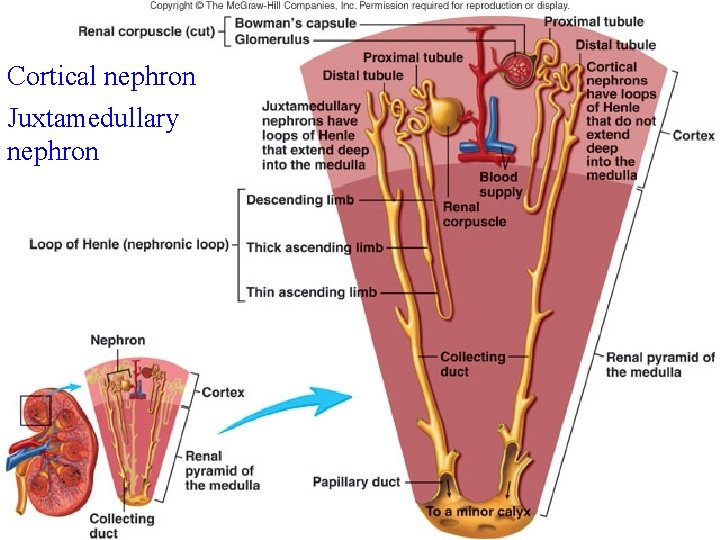
Cortical nephron Juxtamedullary nephron
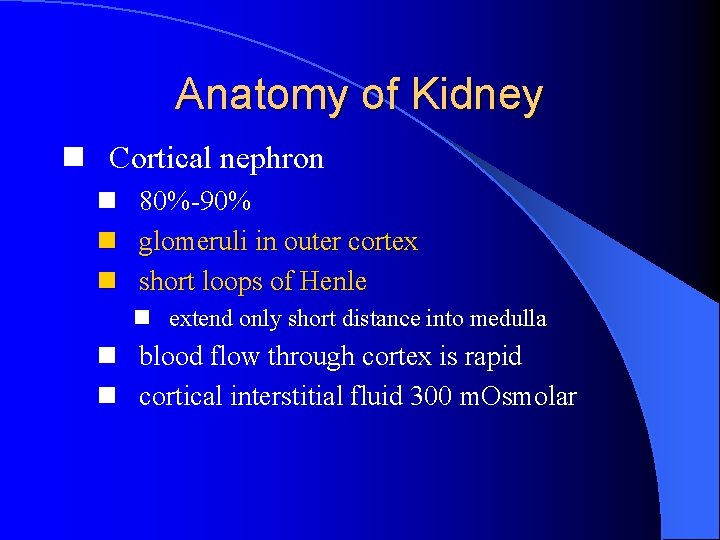
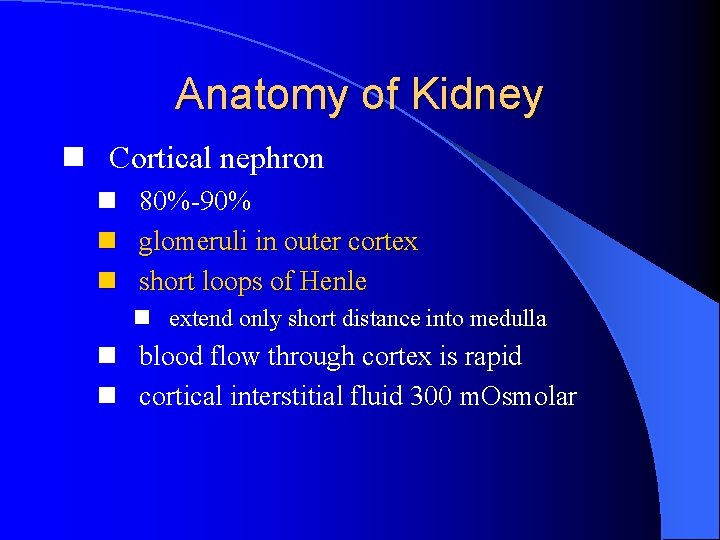
Anatomy of Kidney n Cortical nephron n 80%-90% n glomeruli in outer cortex n short loops of Henle n extend only short distance into medulla n blood flow through cortex is rapid n cortical interstitial fluid 300 m. Osmolar
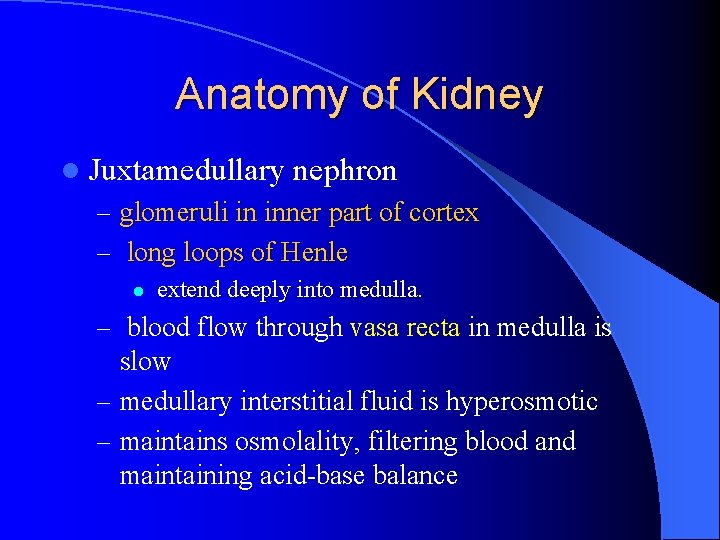
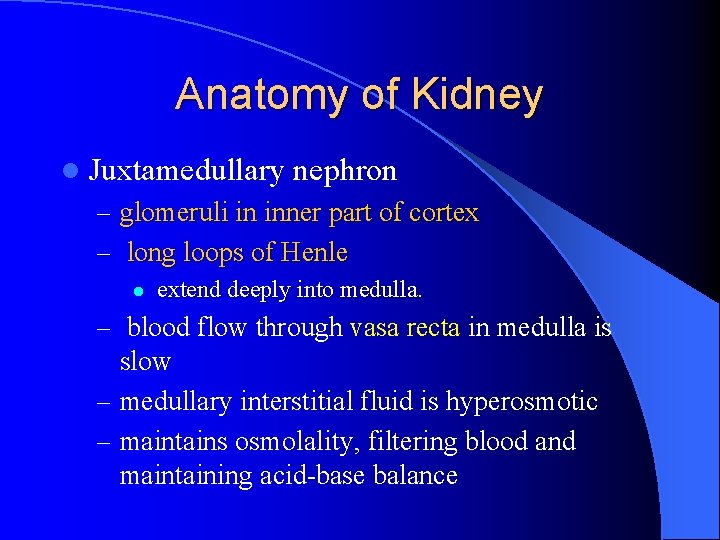
Anatomy of Kidney l Juxtamedullary nephron – glomeruli in inner part of cortex – long loops of Henle l extend deeply into medulla. – blood flow through vasa recta in medulla is slow – medullary interstitial fluid is hyperosmotic – maintains osmolality, filtering blood and maintaining acid-base balance
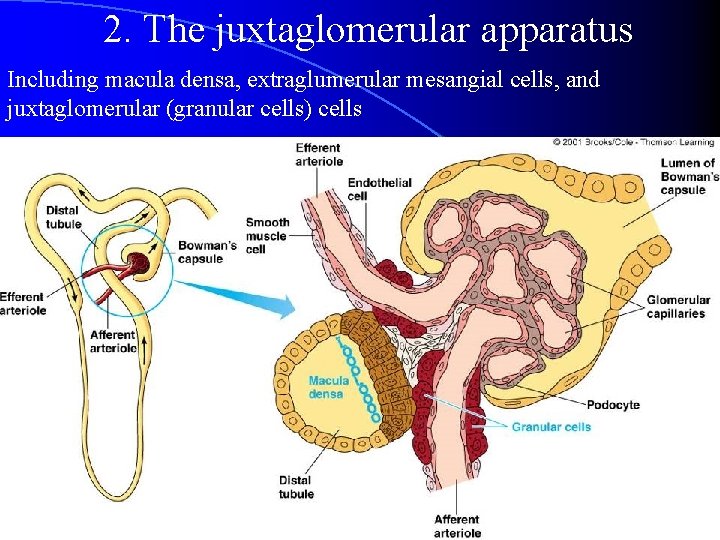
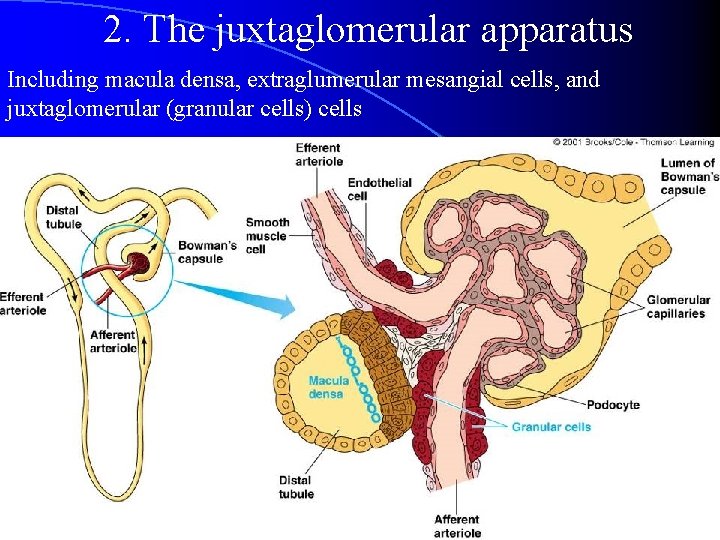
2. The juxtaglomerular apparatus Including macula densa, extraglumerular mesangial cells, and juxtaglomerular (granular cells) cells
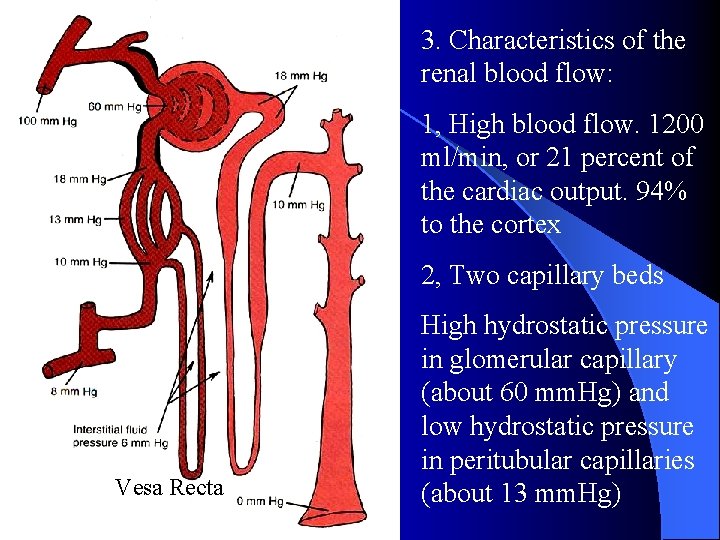
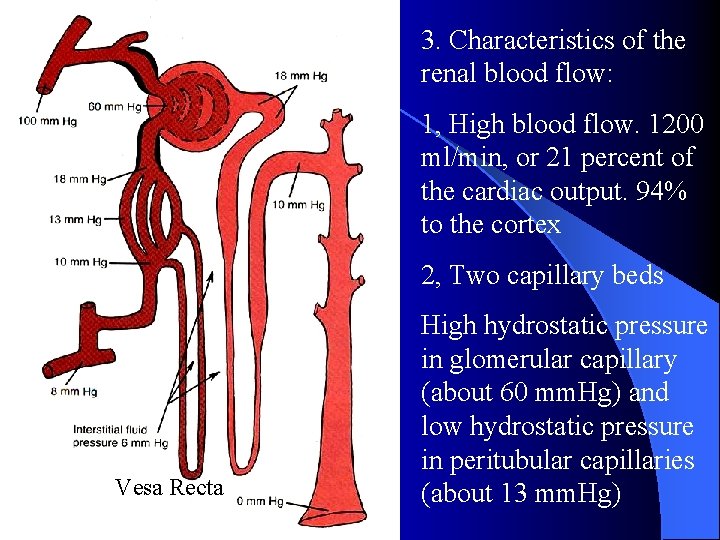
3. Characteristics of the renal blood flow: 1, High blood flow. 1200 ml/min, or 21 percent of the cardiac output. 94% to the cortex 2, Two capillary beds Vesa Recta High hydrostatic pressure in glomerular capillary (about 60 mm. Hg) and low hydrostatic pressure in peritubular capillaries (about 13 mm. Hg)
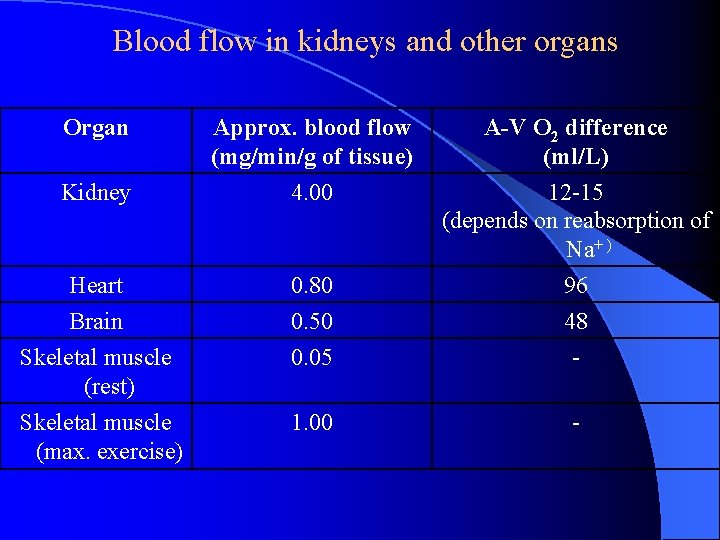
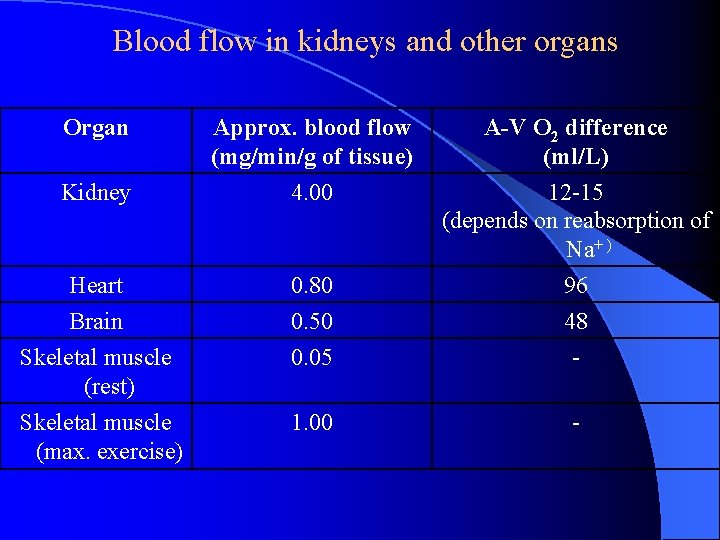
Blood flow in kidneys and other organs Organ Approx. blood flow (mg/min/g of tissue) 4. 00 A-V O 2 difference (ml/L) 12 -15 (depends on reabsorption of Na+ ) Heart Brain Skeletal muscle (rest) 0. 80 0. 50 0. 05 96 48 - Skeletal muscle (max. exercise) 1. 00 - Kidney
Section 2 Function of Glomerular Filtration
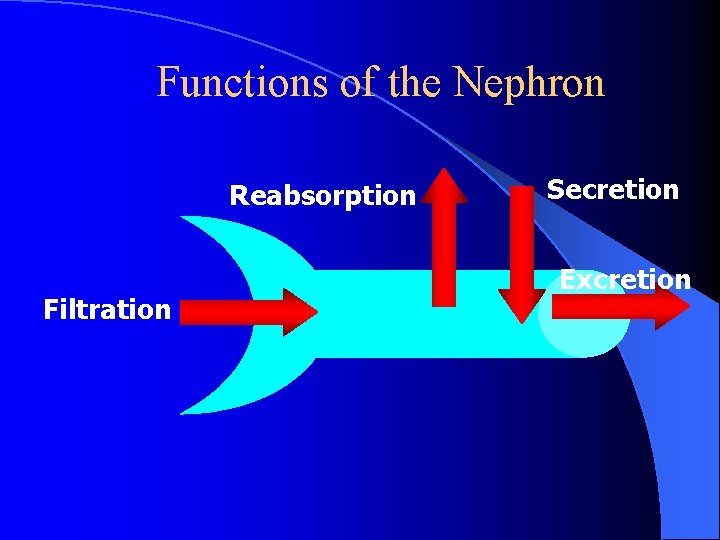
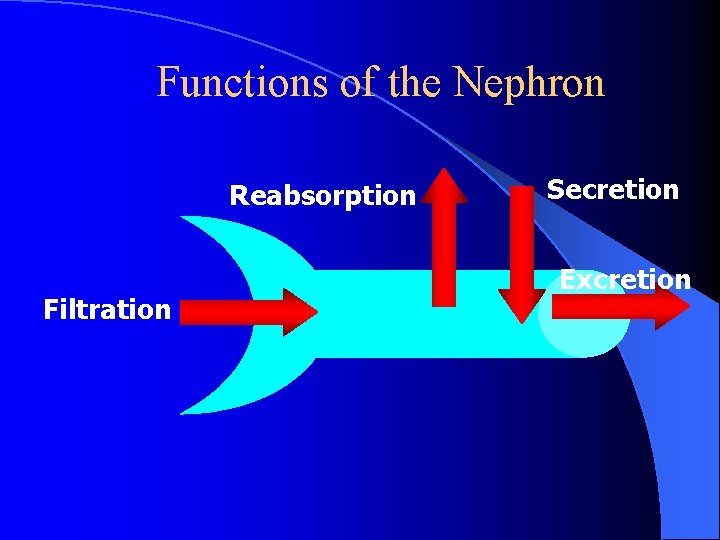
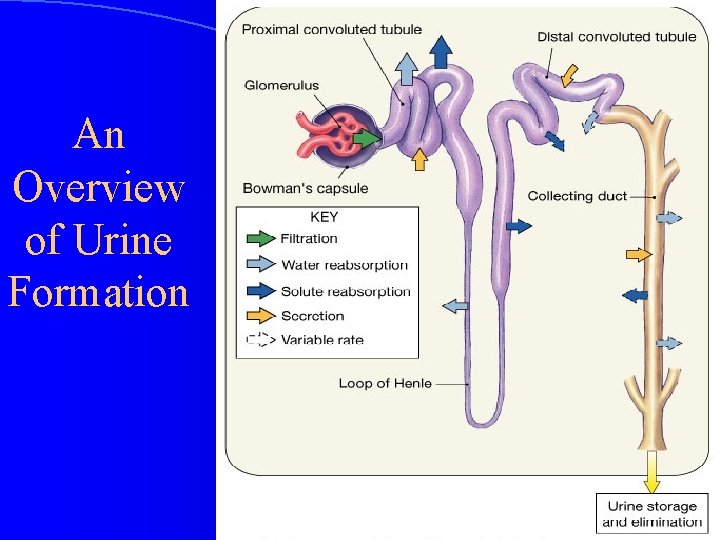
Functions of the Nephron Reabsorption Filtration Secretion Excretion
Filtration l First step in urine formation l Bulk transport of fluid from blood to kidney tubule – Isosmotic filtrate – Blood cells and proteins don’t filter l Result of hydraulic pressure l GFR = 180 L/day
Reabsorption l Process of returning filtered material to bloodstream l 99% of what is filtered l May involve transport proteins l Normally glucose is totally reabsorbed
Secretion l Material added to lumen of kidney from blood l Active transport (usually) of toxins and foreign substances – Saccharine (糖精) – Penicillin
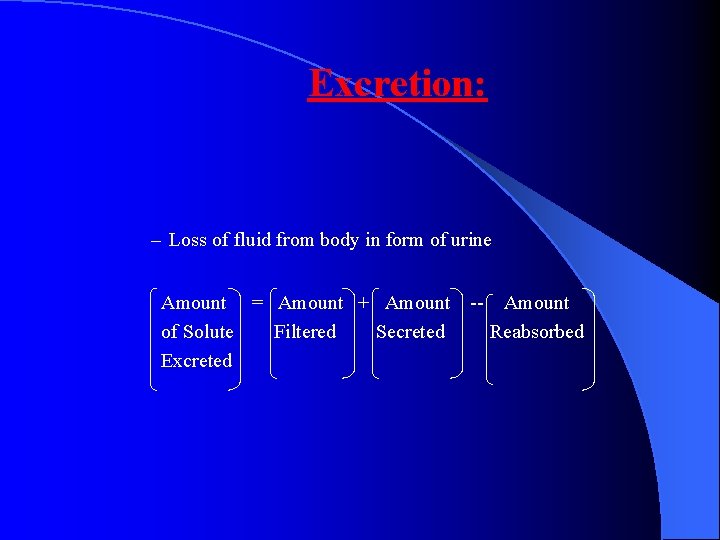
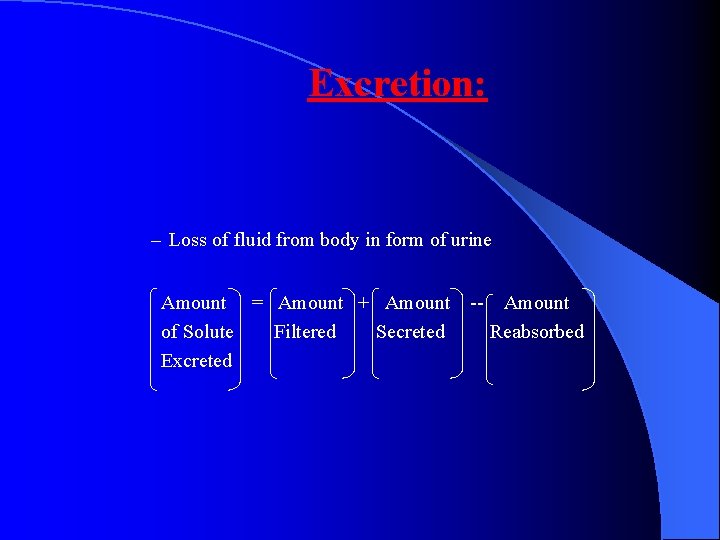
Excretion: – Loss of fluid from body in form of urine Amount = Amount + Amount -- Amount of Solute Filtered Secreted Reabsorbed Excreted

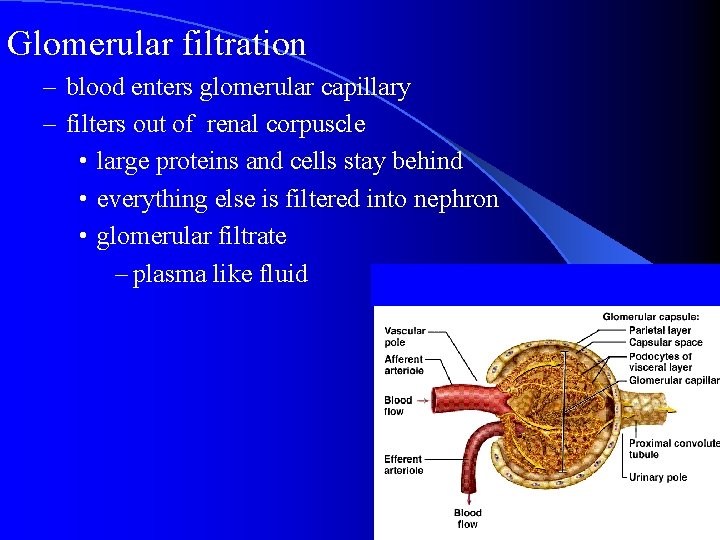
Glomerular filtration
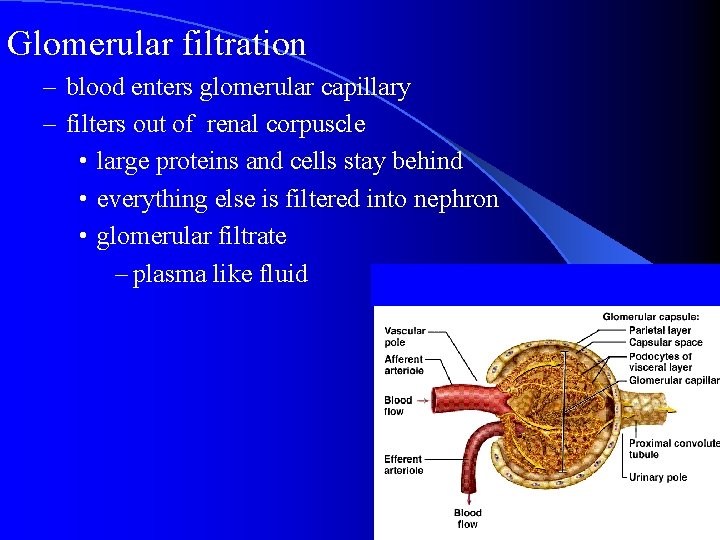
Glomerular filtration – blood enters glomerular capillary – filters out of renal corpuscle • large proteins and cells stay behind • everything else is filtered into nephron • glomerular filtrate – plasma like fluid
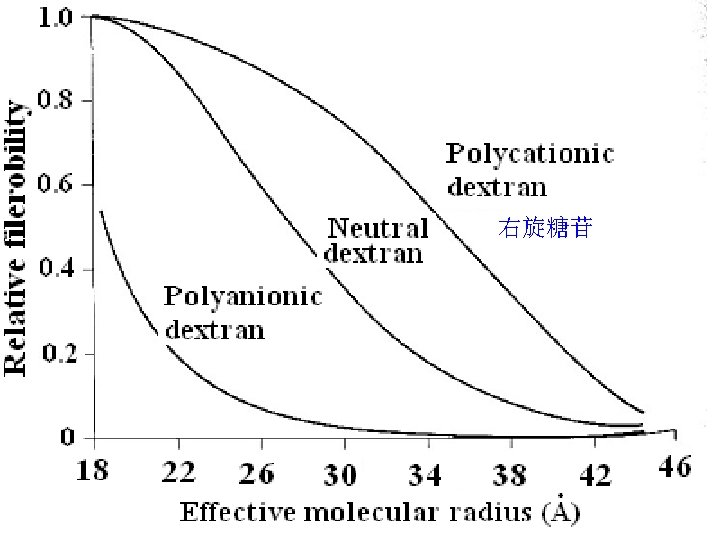
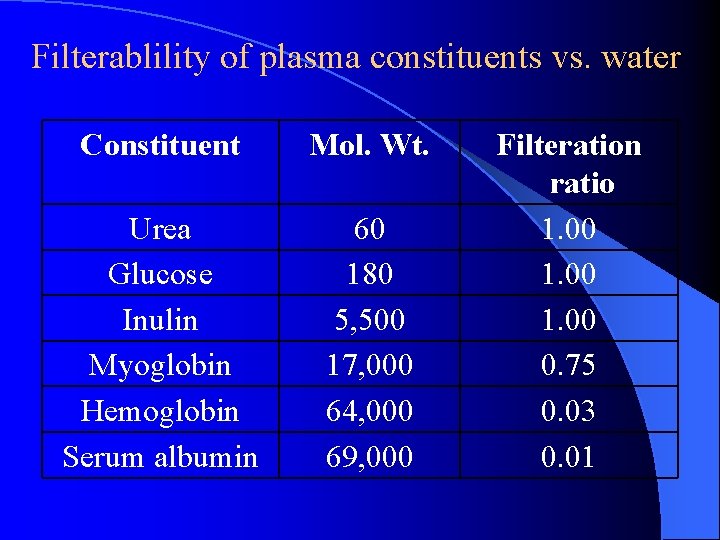
Factors that determining the glumerular filterability Molecular weight l Charges of the molecule l
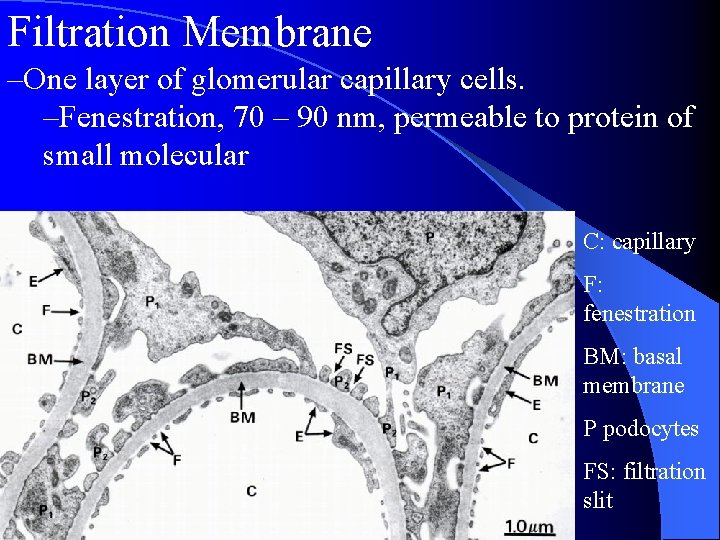
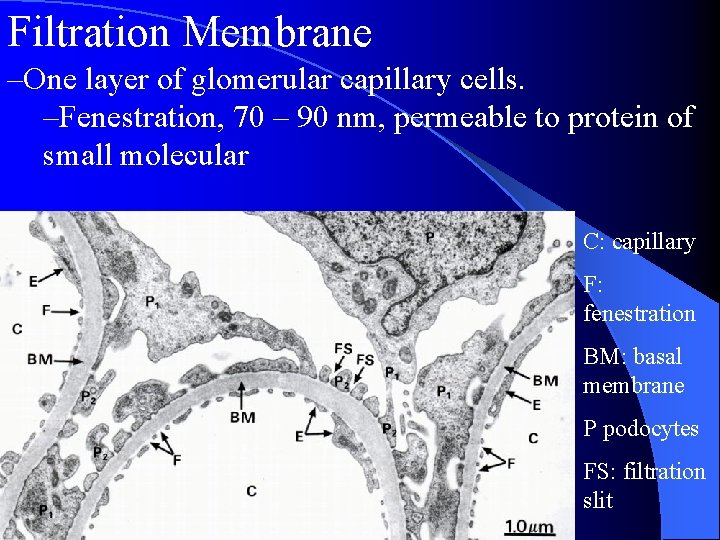
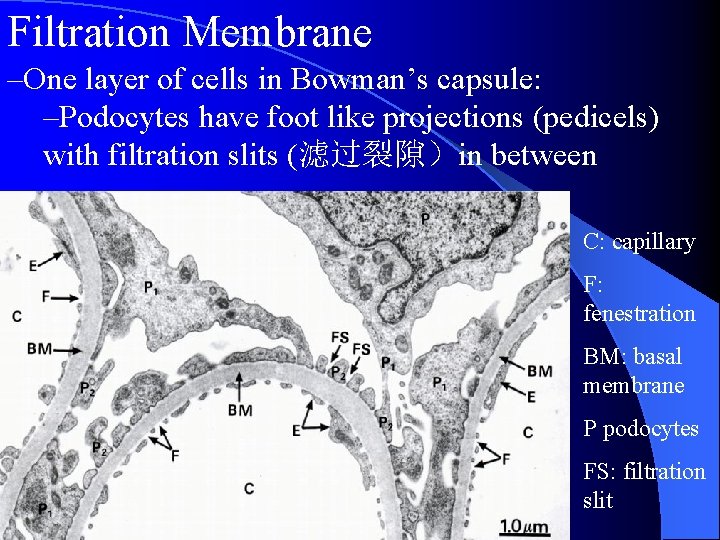
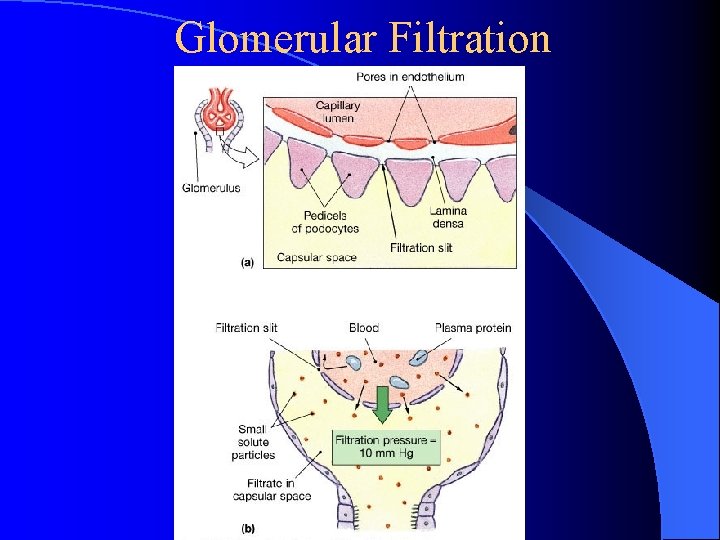
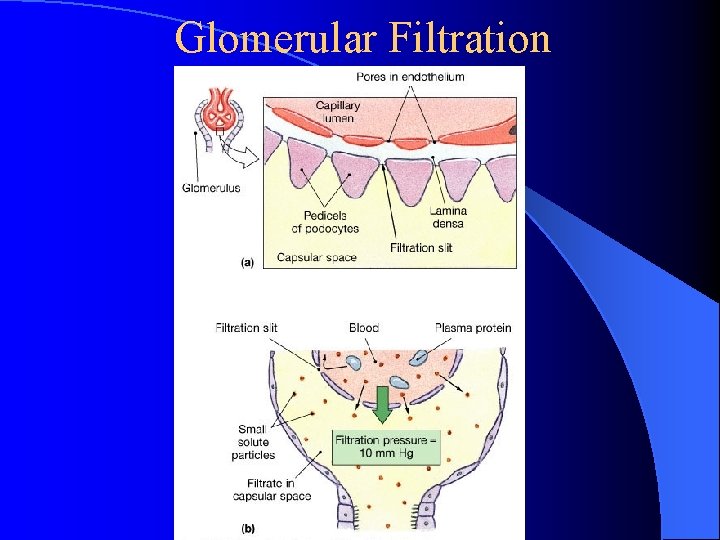
Filtration Membrane –One layer of glomerular capillary cells. –Fenestration, 70 – 90 nm, permeable to protein of small molecular C: capillary F: fenestration BM: basal membrane P podocytes FS: filtration slit
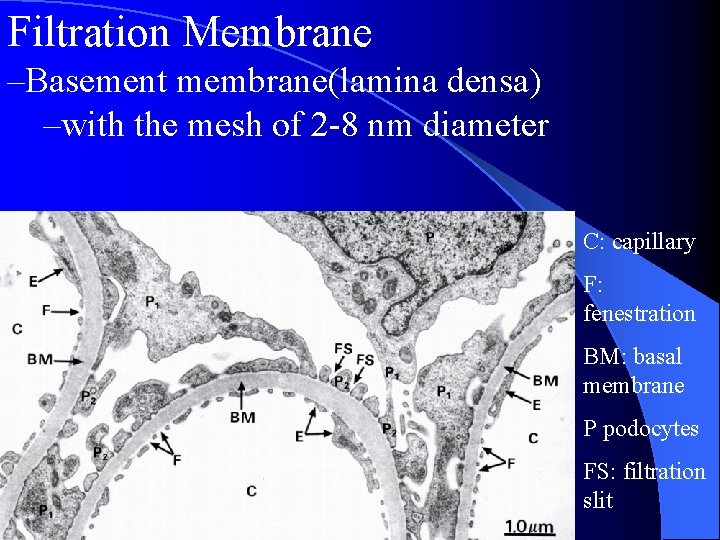
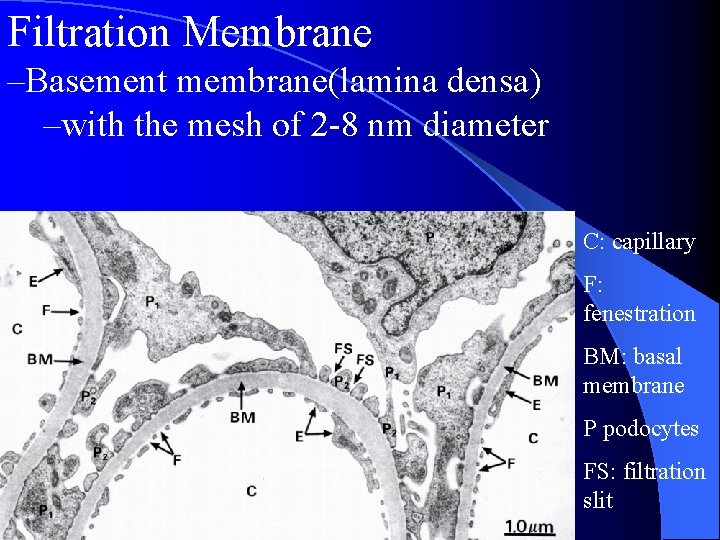
Filtration Membrane –Basement membrane(lamina densa) –with the mesh of 2 -8 nm diameter C: capillary F: fenestration BM: basal membrane P podocytes FS: filtration slit
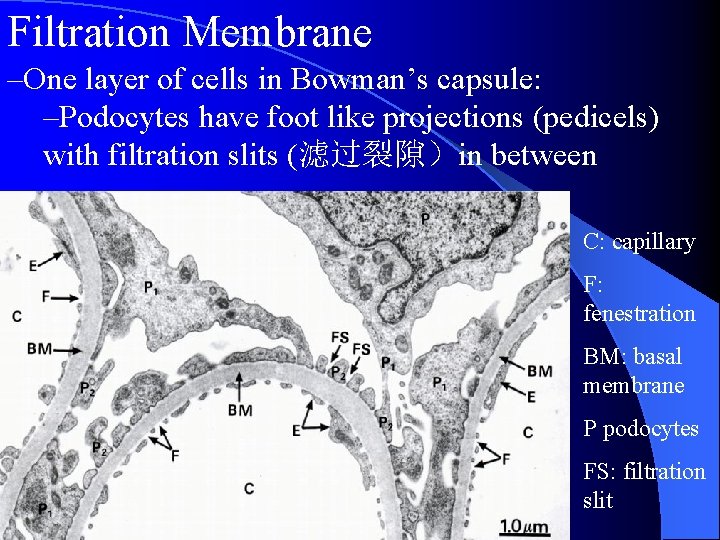
Filtration Membrane –One layer of cells in Bowman’s capsule: –Podocytes have foot like projections (pedicels) with filtration slits (滤过裂隙)in between C: capillary F: fenestration BM: basal membrane P podocytes FS: filtration slit
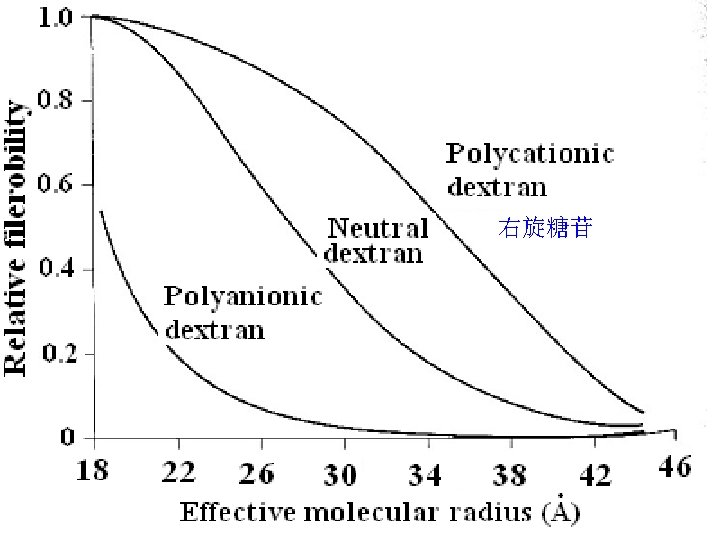
Dextran filterability 右旋糖苷 Stanton BA & Koeppen BM: ‘The Kidney’ in Physiology, Ed. Berne & Levy, Mosby, 1998 2934
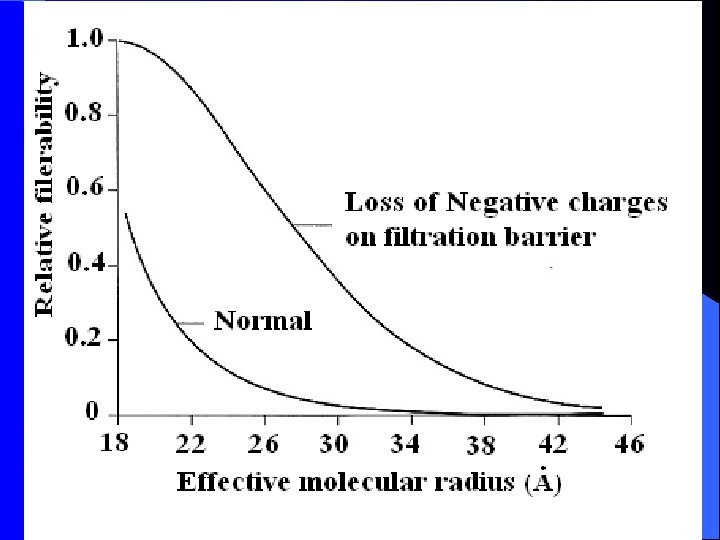
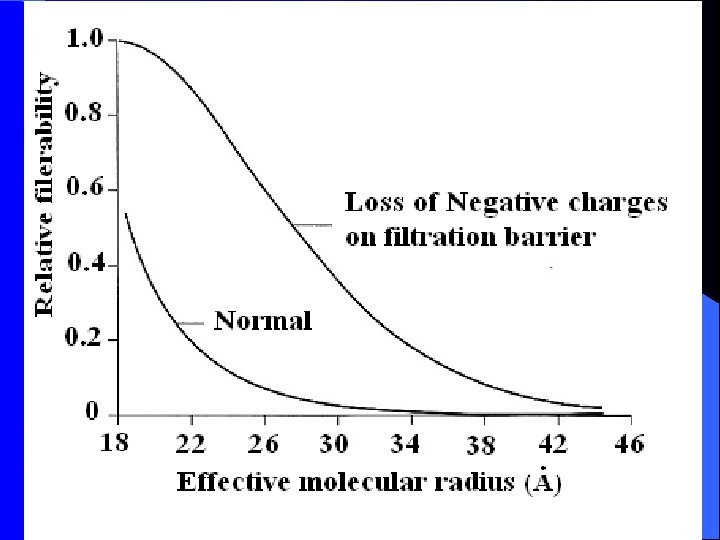
Protein filtration: influence of negative charge on glomerular wall
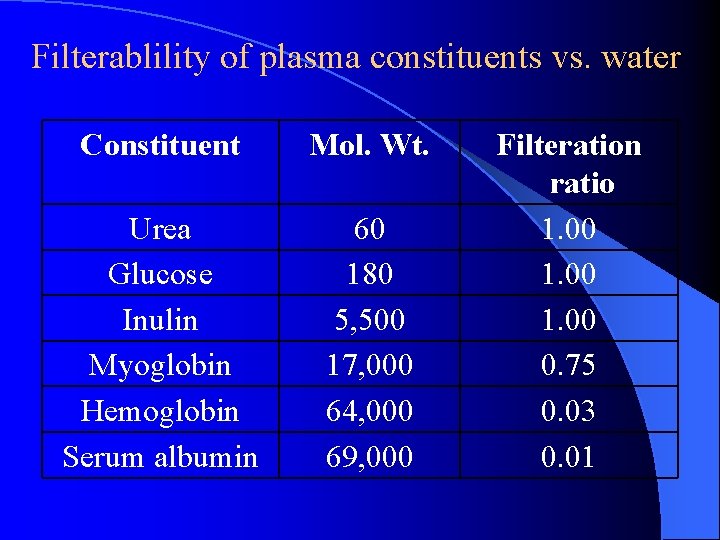
Filterablility of plasma constituents vs. water Constituent Mol. Wt. Urea Glucose Inulin Myoglobin Hemoglobin Serum albumin 60 180 5, 500 17, 000 64, 000 69, 000 Filteration ratio 1. 00 0. 75 0. 03 0. 01
Starling Forces Involved in Filtration: What forces favor/oppose filtration?
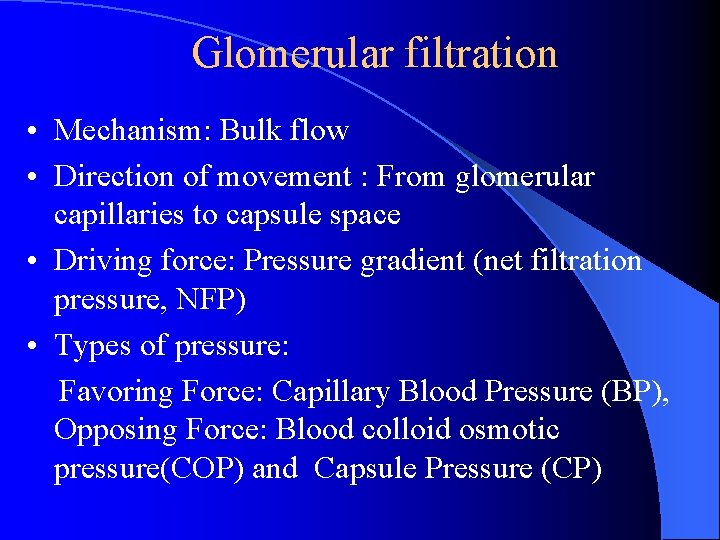
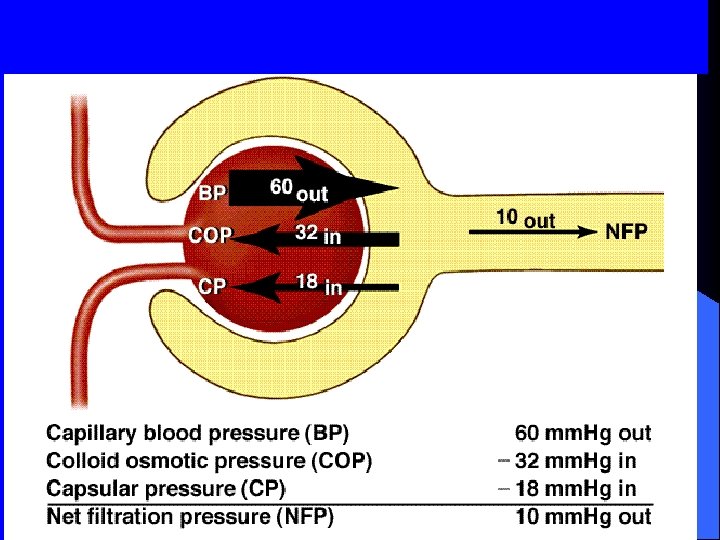
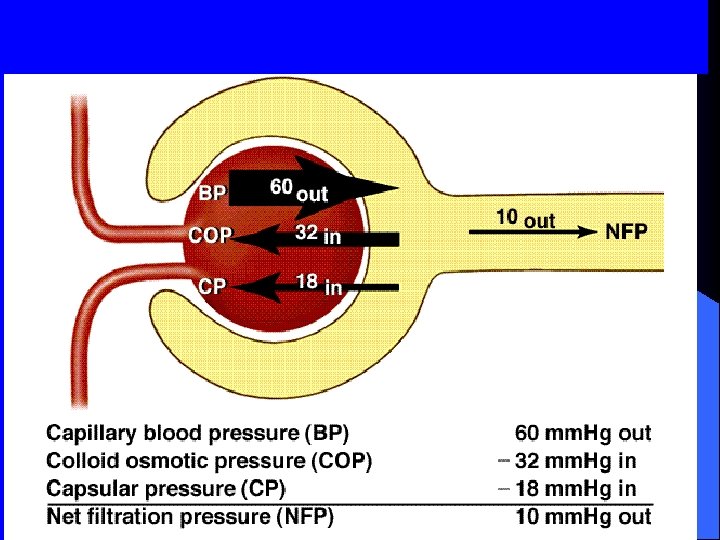
Glomerular filtration • Mechanism: Bulk flow • Direction of movement : From glomerular capillaries to capsule space • Driving force: Pressure gradient (net filtration pressure, NFP) • Types of pressure: Favoring Force: Capillary Blood Pressure (BP), Opposing Force: Blood colloid osmotic pressure(COP) and Capsule Pressure (CP)
Glomerular Filtration
Glomerular filtration rate (GFR) • Amount of filtrate produced in the kidneys each minute. 125 m. L/min = 180 L/day • Factors that alter filtration pressure change GFR. These include: – Increased renal blood flow -- Increased GFR – Decreased plasma protein -- Increased GFR. Causes edema. – Hemorrhage -- Decreased capillary BP -- Decreased GFR – Capsular pressure
GFR regulation : Adjusting blood flow • GFR is regulated by three mechanisms 1. Renal Autoregulation 2. Neural regulation 3. Hormonal regulation All three mechanism adjust renal blood pressure and resulting blood flow
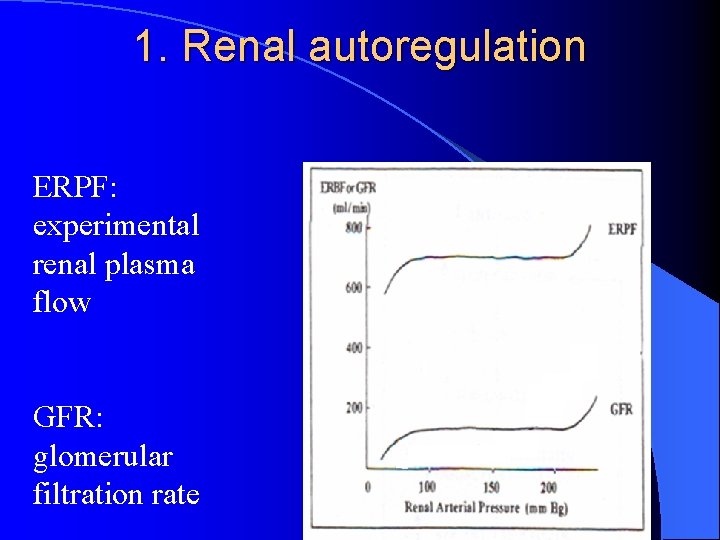
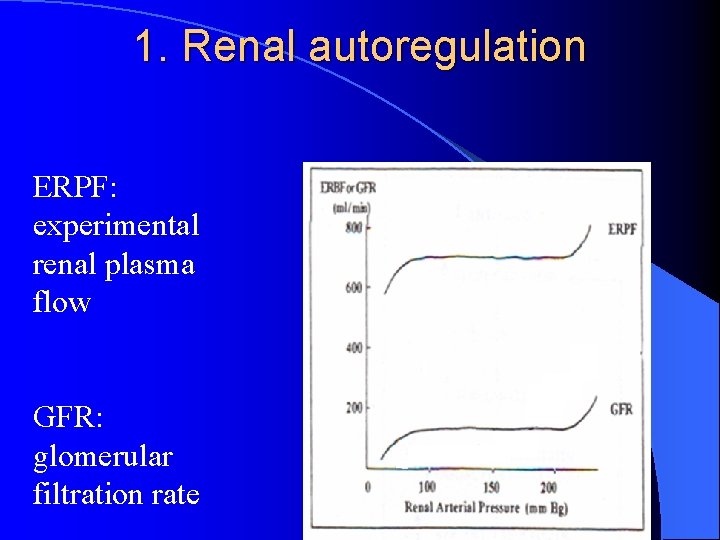
1. Renal autoregulation ERPF: experimental renal plasma flow GFR: glomerular filtration rate
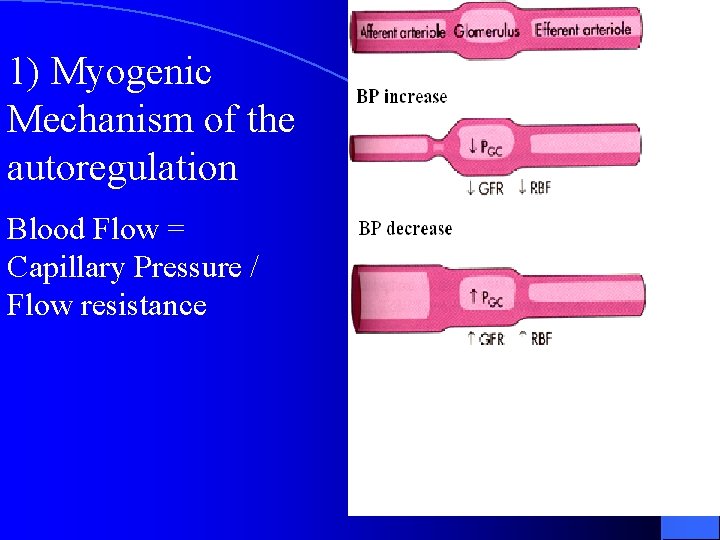
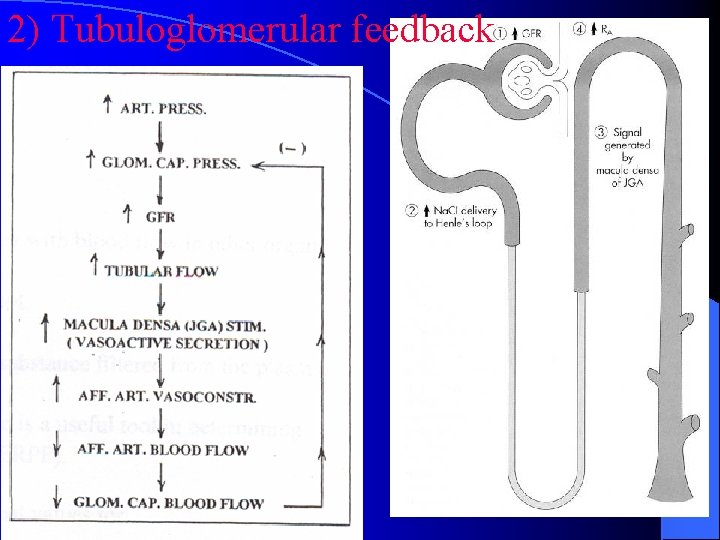
Mechanism? l Myogenic Mechanism l Tubuloglomerular feedback
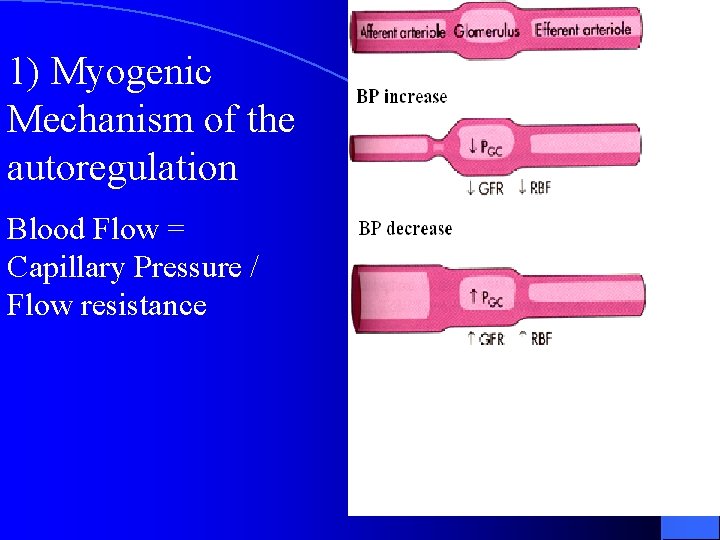
1) Myogenic Mechanism of the autoregulation Blood Flow = Capillary Pressure / Flow resistance
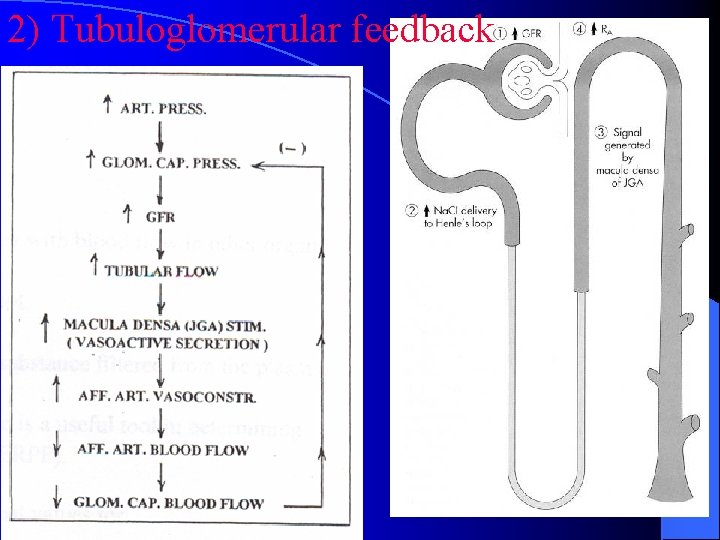
2) Tubuloglomerular feedback 2934
2. Neural regulation of GFR • Sympathetic nerve fibers innervate afferent and efferent arteriole • Normally sympathetic stimulation is low but can increase during hemorrhage and exercise
3. Hormonal regulation of GFR • Angiotensin II. • a potent vasoconstrictor. • Reduces GFR • ANP (Atrial Natriuretic Peptide) • increases GFR by relaxing the afferent arteriole NO • Endothelin • Prostaglandin E 2
Measuring GFR • 125 ml/min, 180 L/day • plasma clearance: • The amount of a kind of substance present in urine • The substance: filtered but neither reabsorbed nor secreted, • If plasma conc. is 3 mg/L then 3 mg/L X 180/day = 540 mg/day (known) (unknown) (known)
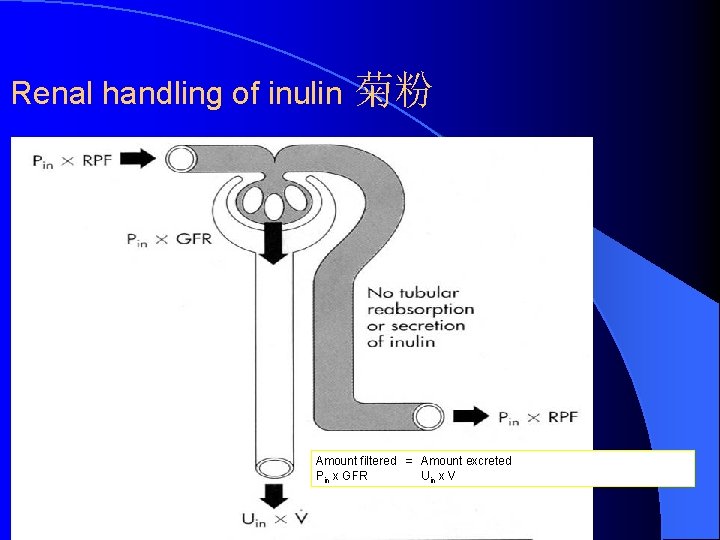
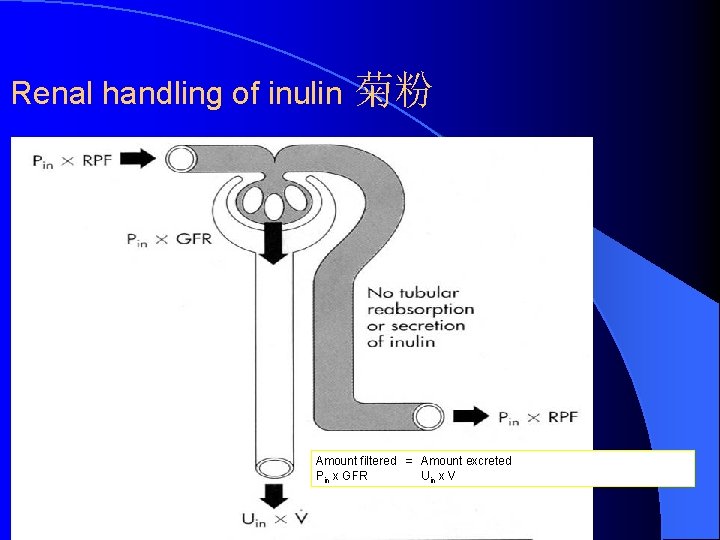
Renal handling of inulin 菊粉 Amount filtered = Amount excreted Pin x GFR Uin x V
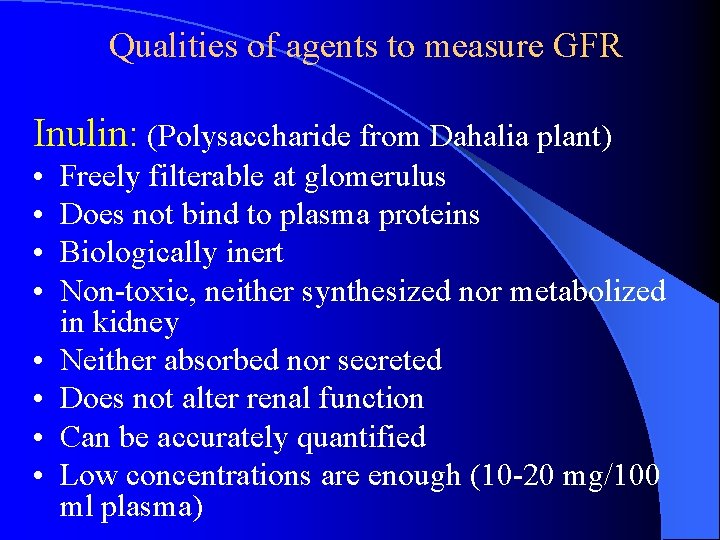
Qualities of agents to measure GFR Inulin: (Polysaccharide from Dahalia plant) • • Freely filterable at glomerulus Does not bind to plasma proteins Biologically inert Non-toxic, neither synthesized nor metabolized in kidney Neither absorbed nor secreted Does not alter renal function Can be accurately quantified Low concentrations are enough (10 -20 mg/100 ml plasma)
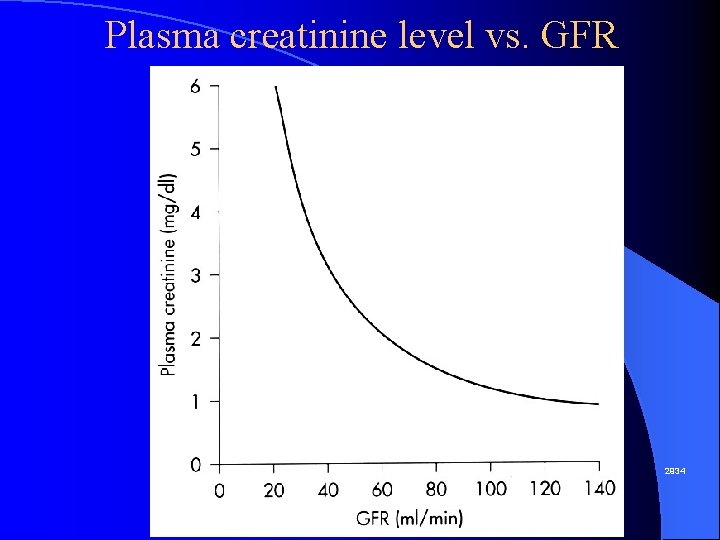
Qualities of agents to measure GFR Creatinine (肌氨酸酐): End product of muscle creatine (肌氨酸) metabolism Used in clinical setting to measure GFR but less accurate than inulin method Small amount secreted from the tubule
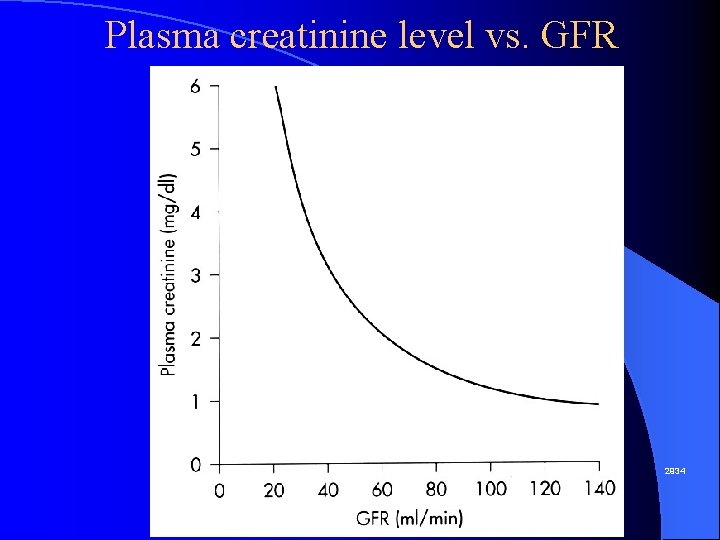
Plasma creatinine level vs. GFR 2934
Section 3 Reabsorption and Secretion Concept of Reabsorption and Secretion
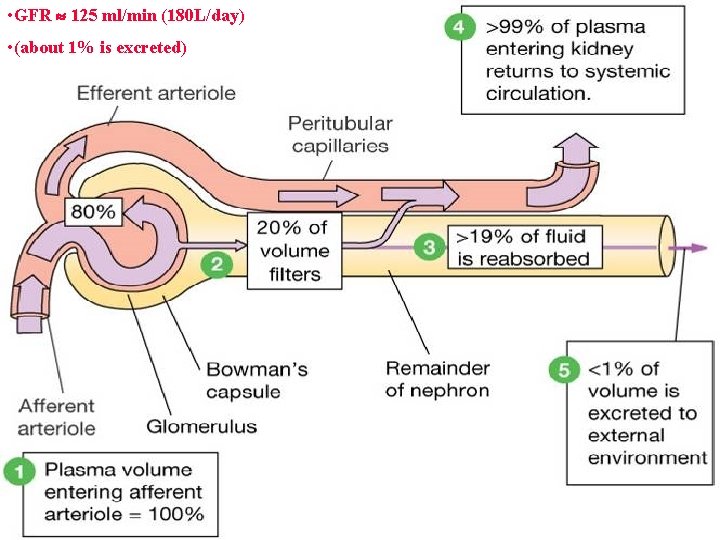
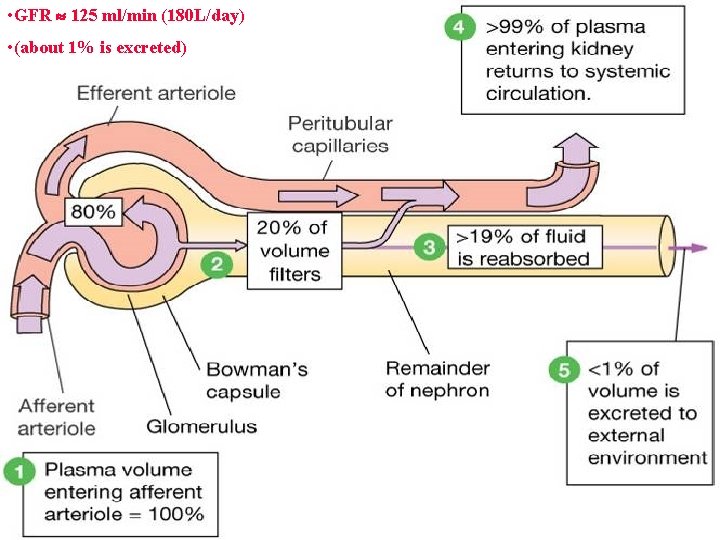
• GFR 125 ml/min (180 L/day) • (about 1% is excreted)
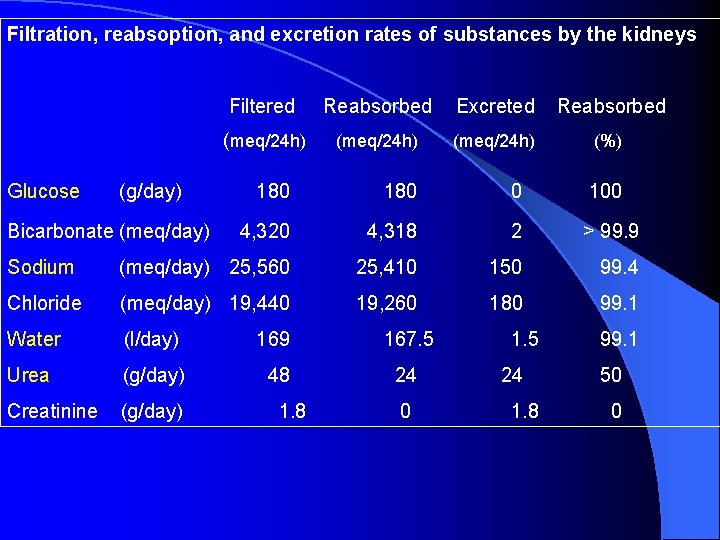
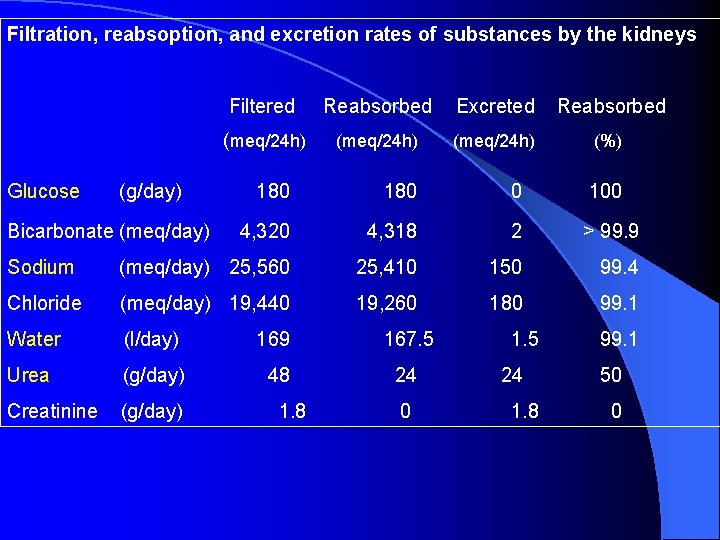
Filtration, reabsoption, and excretion rates of substances by the kidneys Glucose (g/day) Filtered Reabsorbed Excreted Reabsorbed (meq/24 h) (%) 180 0 100 4, 320 4, 318 2 > 99. 9 Sodium (meq/day) 25, 560 25, 410 150 99. 4 Chloride (meq/day) 19, 440 19, 260 180 99. 1 Water (l/day) 169 167. 5 Urea (g/day) 48 24 Creatinine (g/day) Bicarbonate (meq/day) 1. 8 0 1. 5 24 1. 8 99. 1 50 0
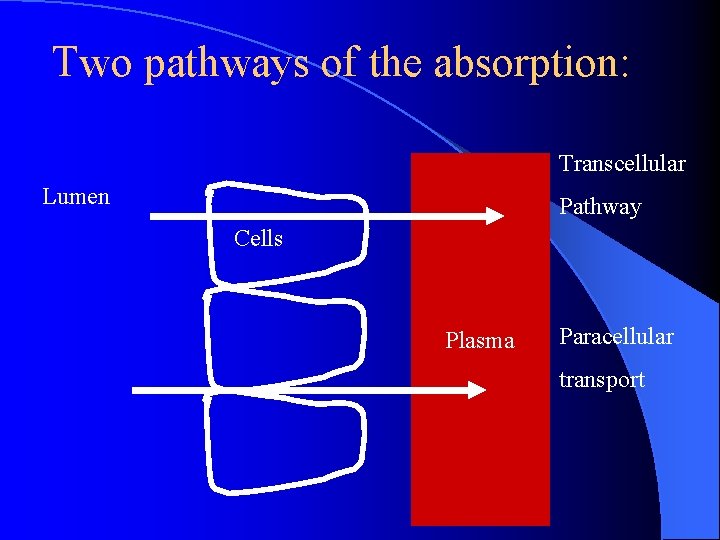
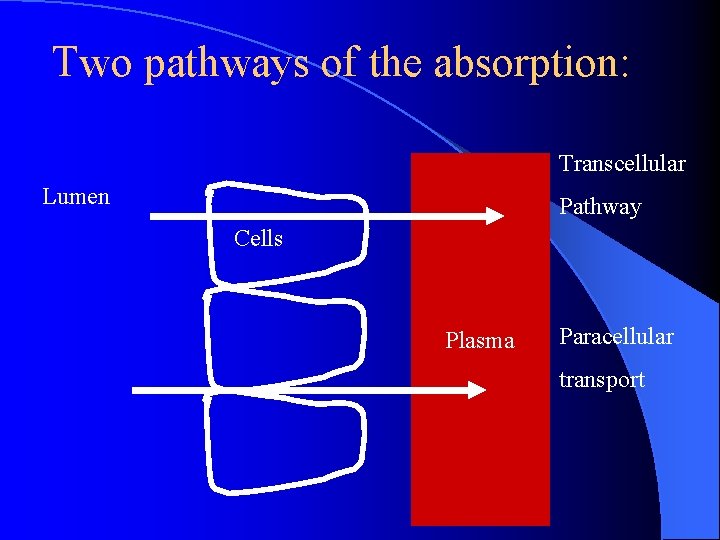
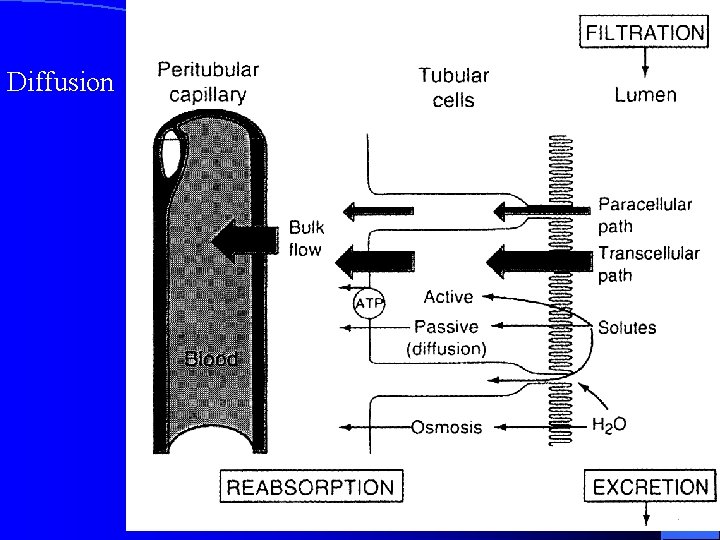
Two pathways of the absorption: Transcellular Lumen Pathway Cells Plasma Paracellular transport
Mechanism of Transport 1, Primary Active Transport 2, Secondary Active Transport 3, Pinocytosis 4, Passive Transport
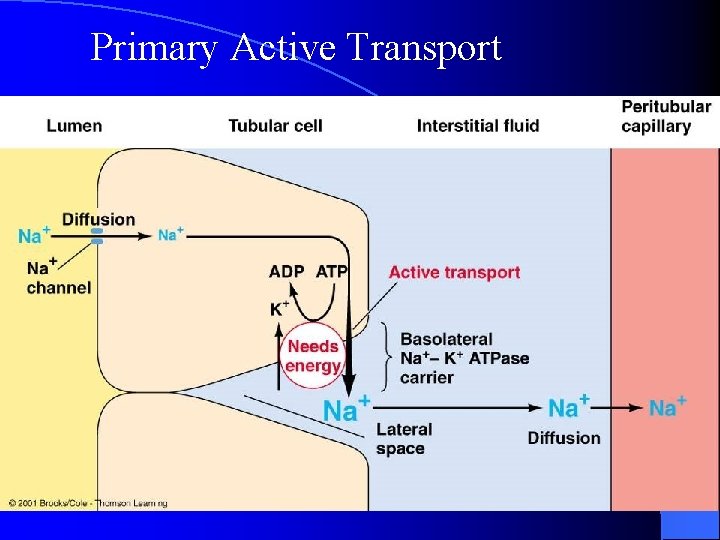
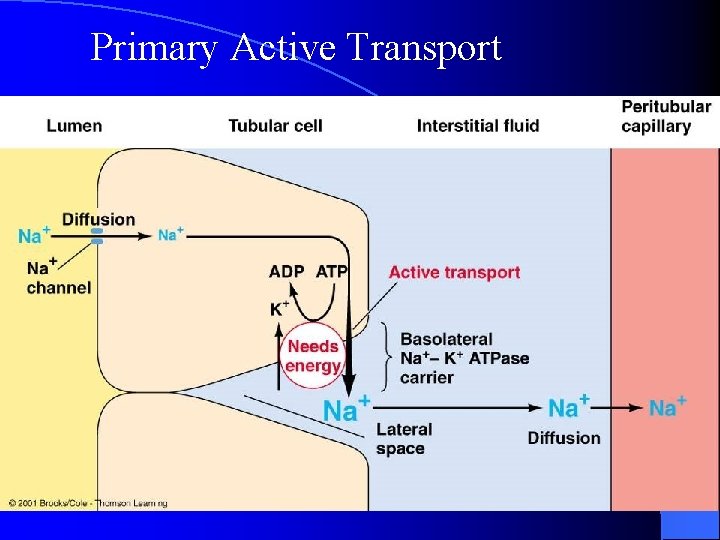
Primary Active Transport
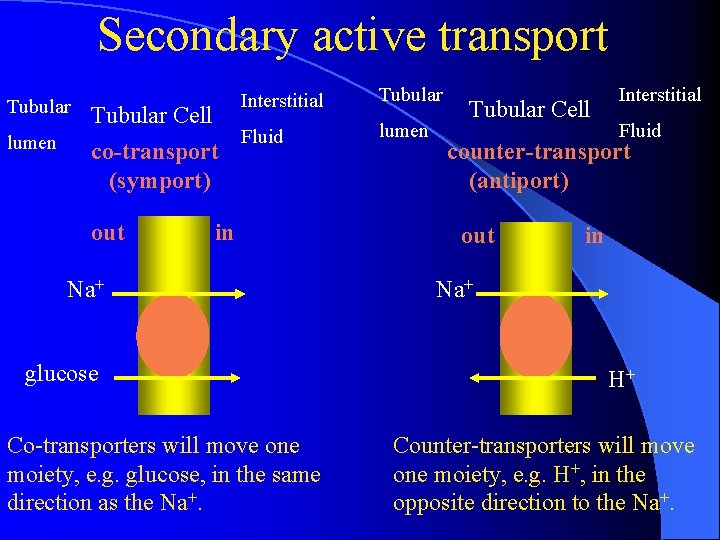
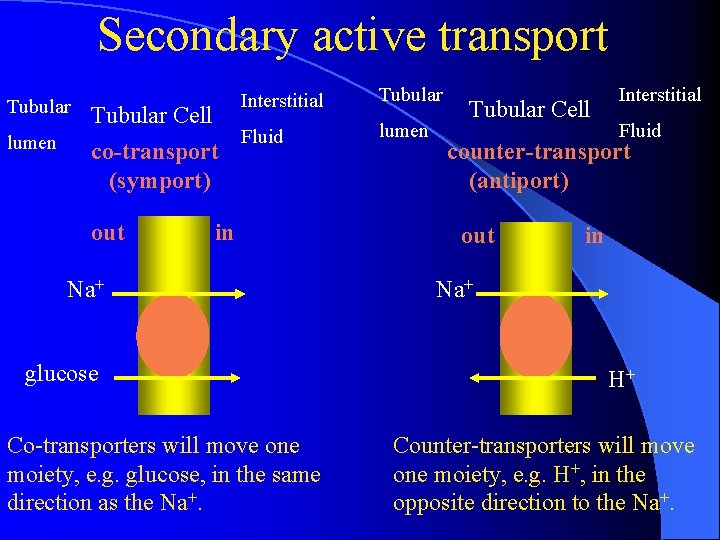
Secondary active transport Tubular Cell Interstitial lumen Fluid lumen co-transport counter-transport (symport) (antiport) out in Na+ glucose Co-transporters will move one moiety, e. g. glucose, in the same direction as the Na+. out in Na+ H+ Counter-transporters will move one moiety, e. g. H+, in the opposite direction to the Na+.
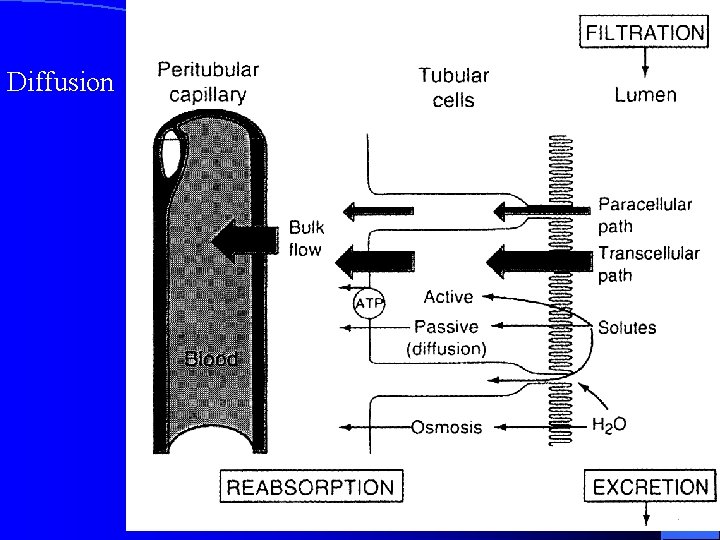
Passive Transport Diffusion
Pinocytosis l proximal tubule l reabsorb large molecules such as proteins
1. Transportation of Sodium, Water and Chloride l (1) in proximal tubule, including – – proximal convoluted tubule thick descending segment of the loop
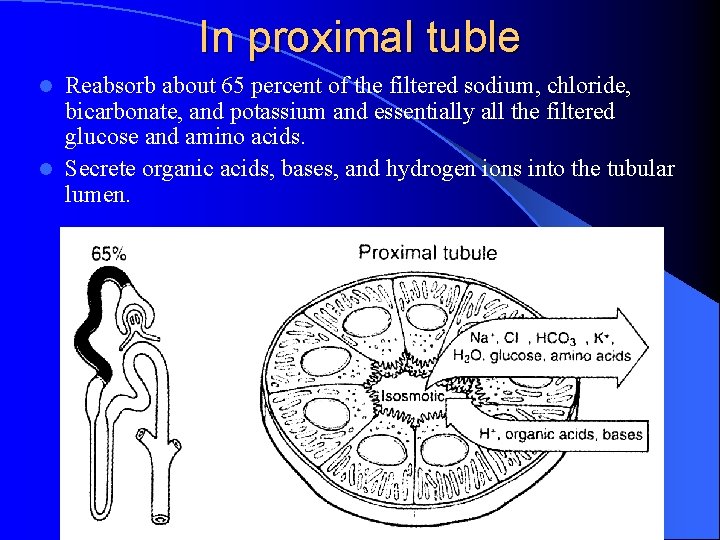
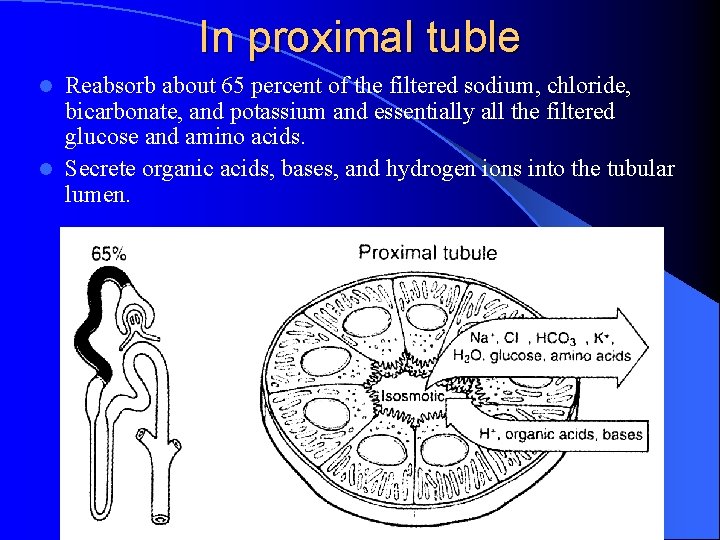
In proximal tuble Reabsorb about 65 percent of the filtered sodium, chloride, bicarbonate, and potassium and essentially all the filtered glucose and amino acids. l Secrete organic acids, bases, and hydrogen ions into the tubular lumen. l
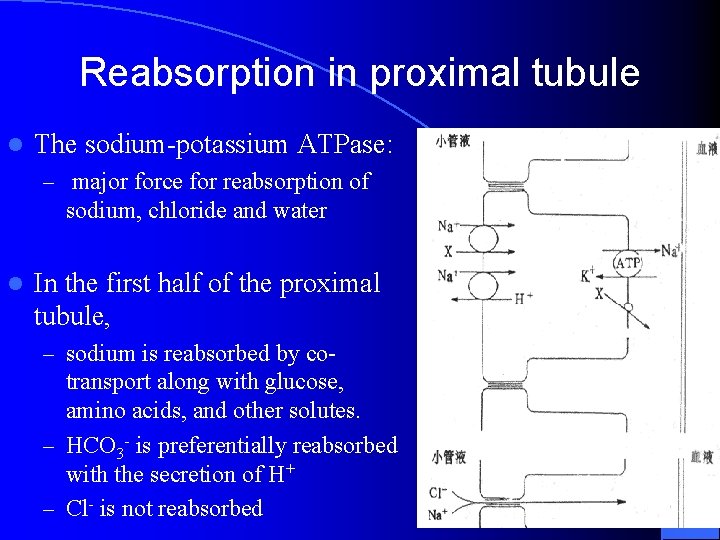
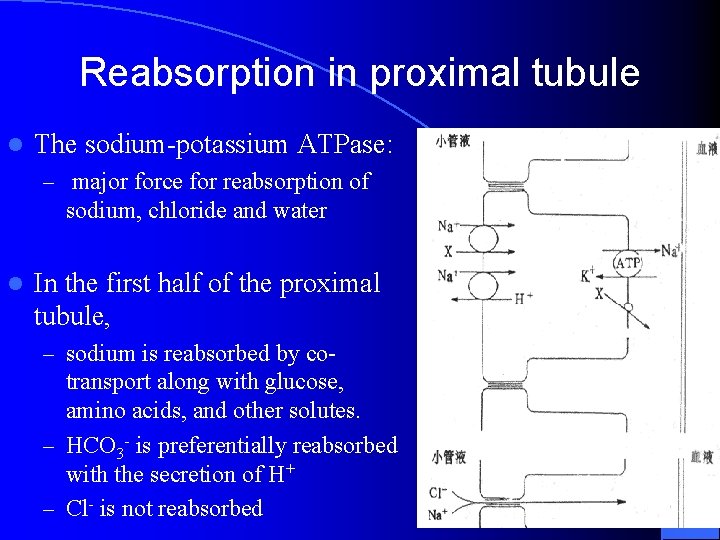
Reabsorption in proximal tubule l The sodium-potassium ATPase: – major force for reabsorption of sodium, chloride and water l In the first half of the proximal tubule, – sodium is reabsorbed by co- transport along with glucose, amino acids, and other solutes. – HCO 3 - is preferentially reabsorbed with the secretion of H+ – Cl- is not reabsorbed
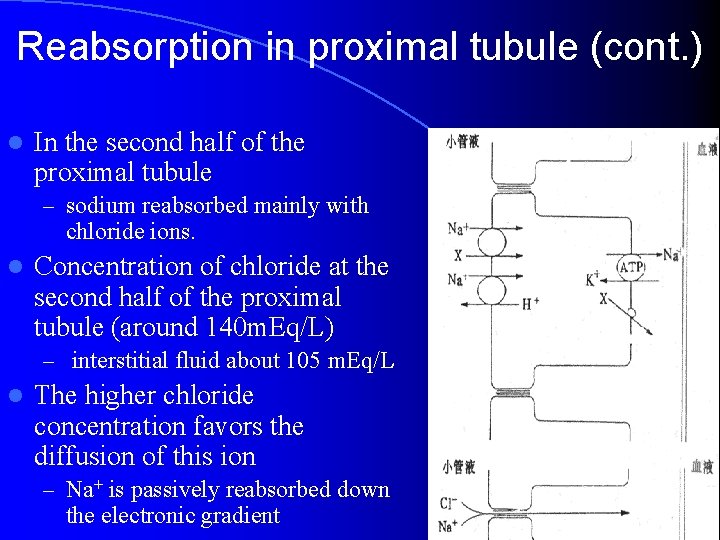
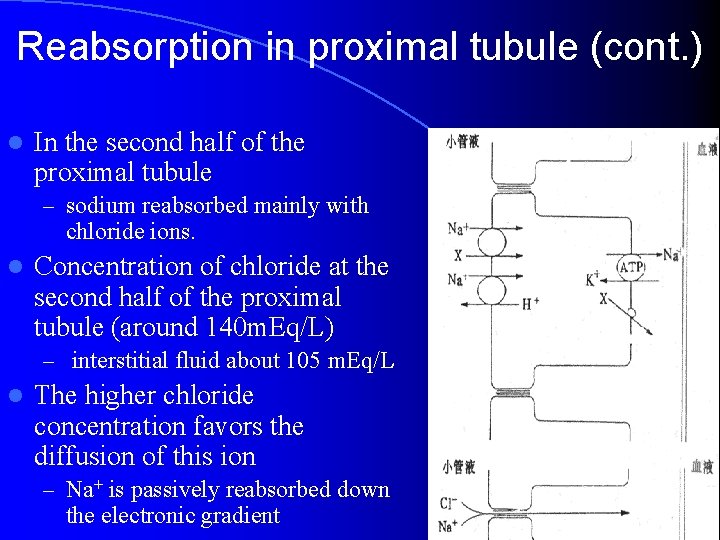
Reabsorption in proximal tubule (cont. ) l In the second half of the proximal tubule – sodium reabsorbed mainly with chloride ions. l Concentration of chloride at the second half of the proximal tubule (around 140 m. Eq/L) – interstitial fluid about 105 m. Eq/L l The higher chloride concentration favors the diffusion of this ion – Na+ is passively reabsorbed down the electronic gradient
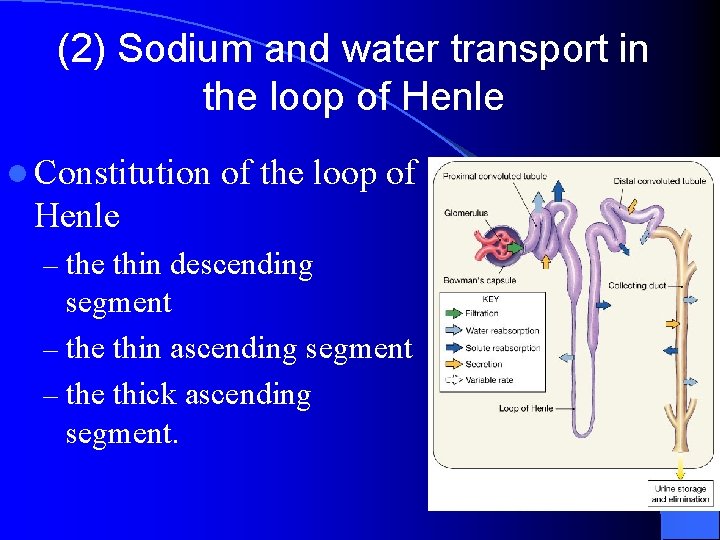
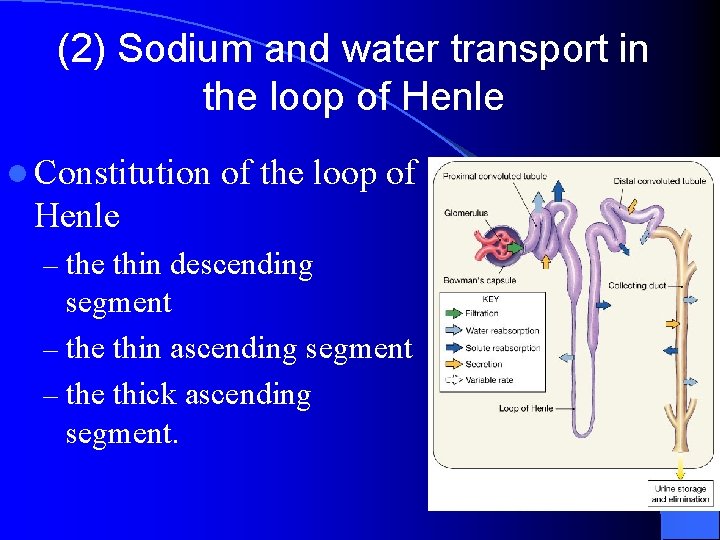
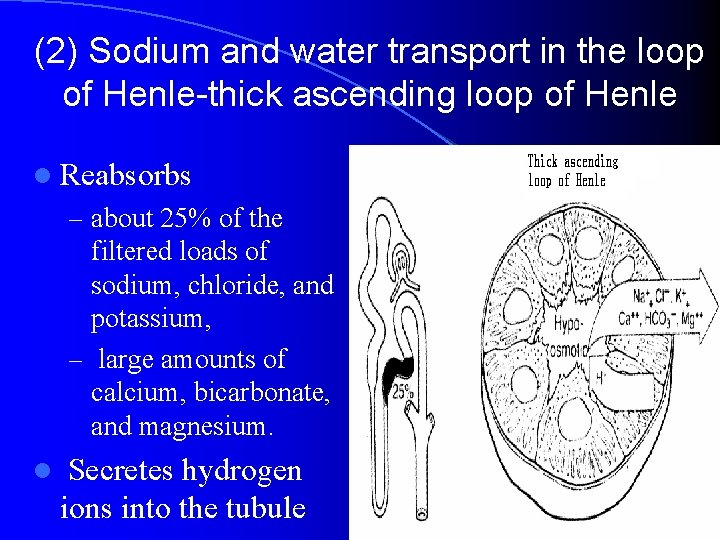
(2) Sodium and water transport in the loop of Henle l Constitution of the loop of Henle – the thin descending segment – the thin ascending segment – the thick ascending segment.
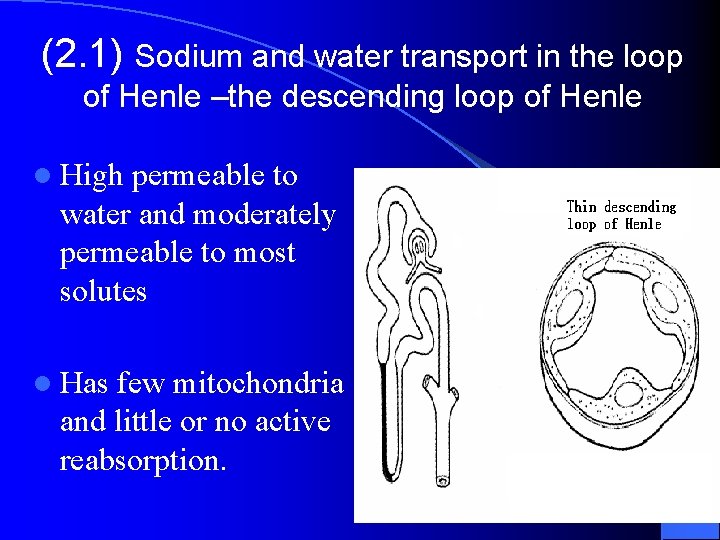
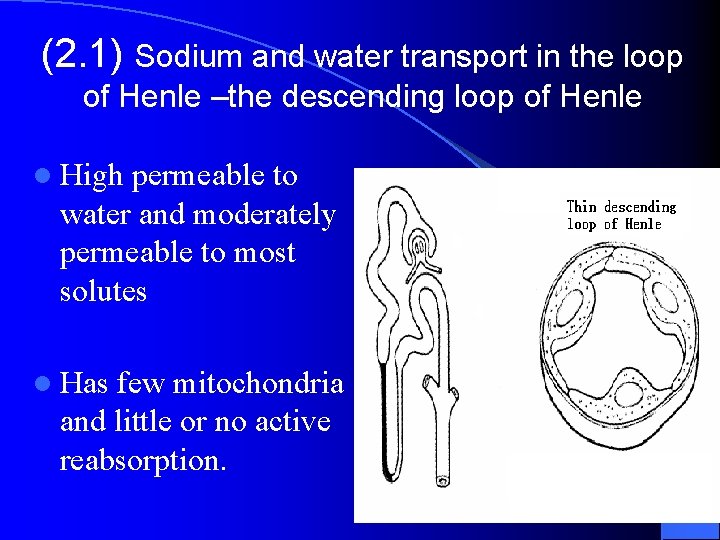
(2. 1) Sodium and water transport in the loop of Henle –the descending loop of Henle l High permeable to water and moderately permeable to most solutes l Has few mitochondria and little or no active reabsorption.
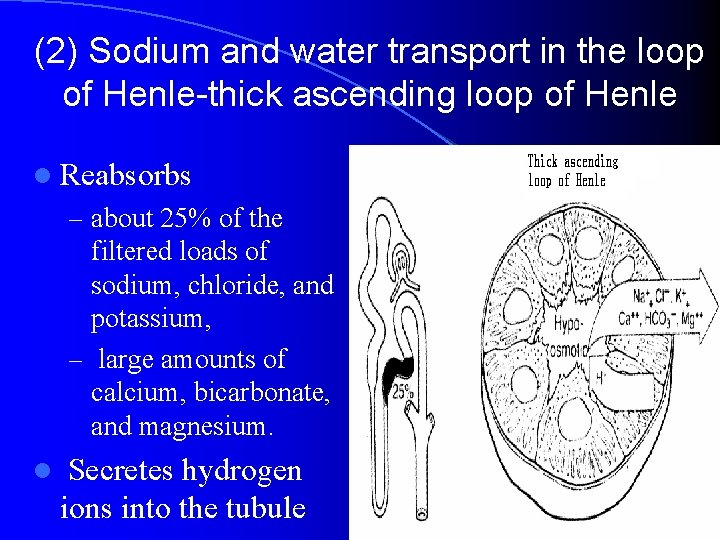
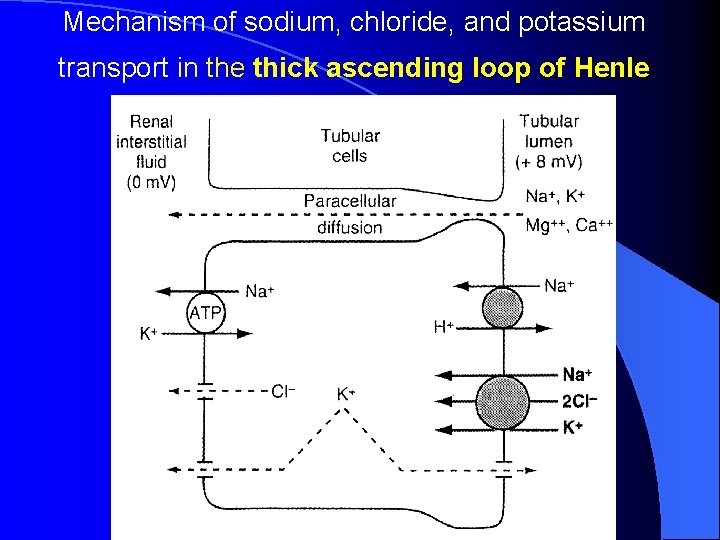
(2) Sodium and water transport in the loop of Henle-thick ascending loop of Henle l Reabsorbs – about 25% of the filtered loads of sodium, chloride, and potassium, – large amounts of calcium, bicarbonate, and magnesium. l Secretes hydrogen ions into the tubule
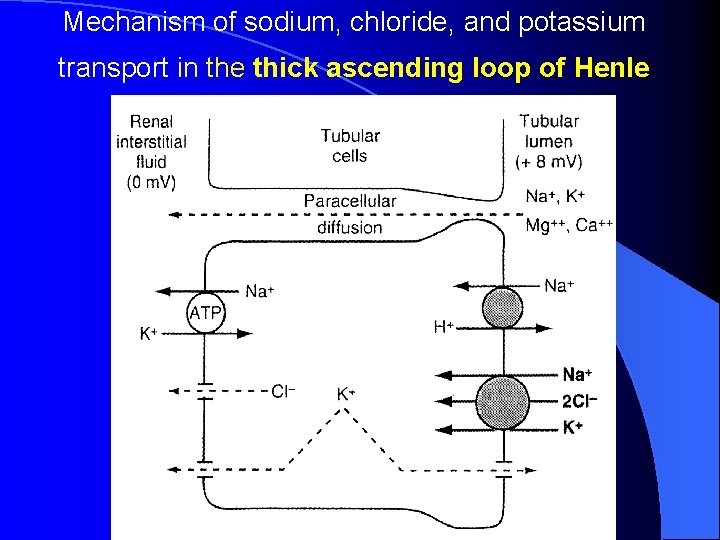
Mechanism of sodium, chloride, and potassium transport in the thick ascending loop of Henle
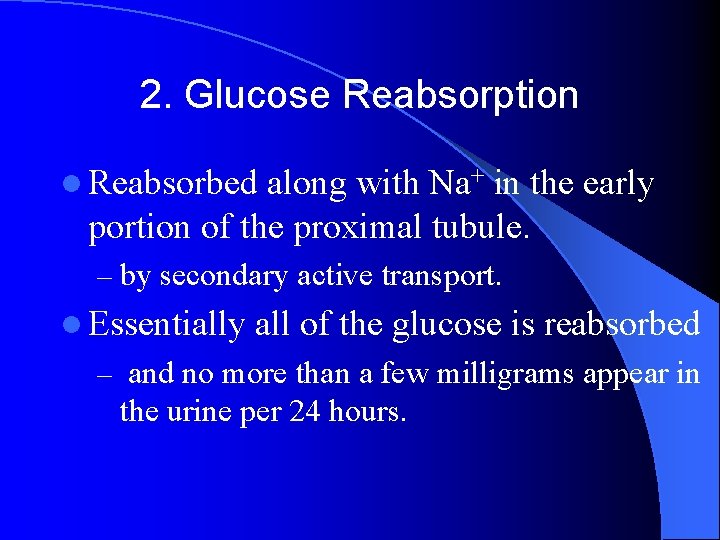
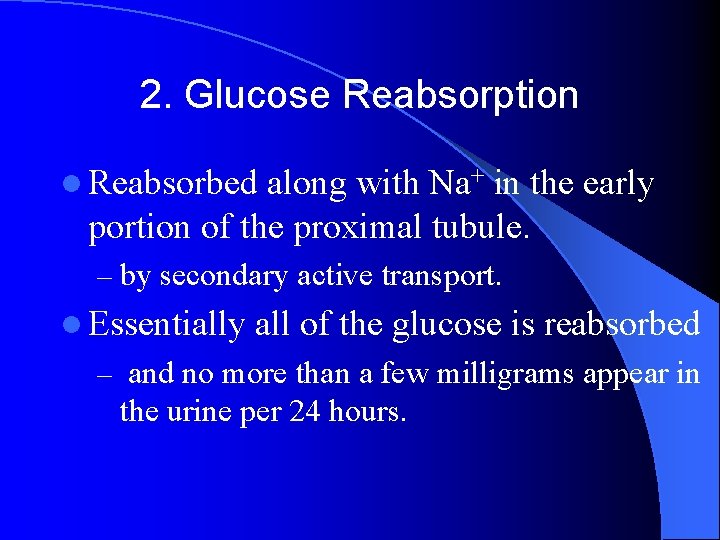
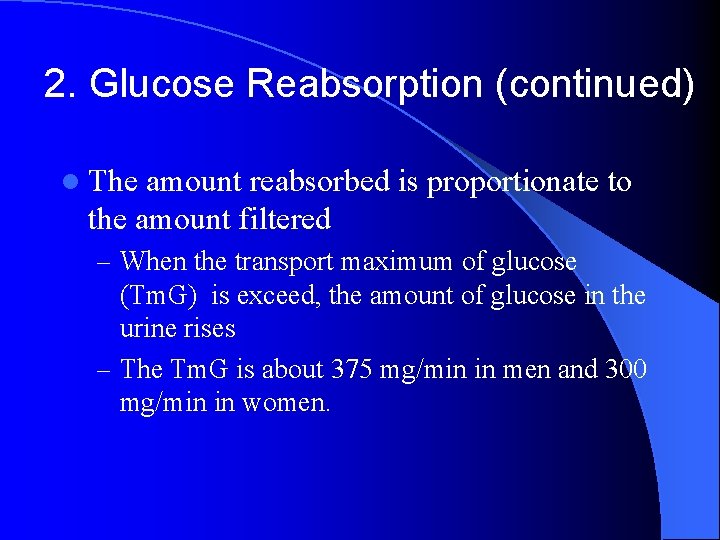
2. Glucose Reabsorption l Reabsorbed along with Na+ in the early portion of the proximal tubule. – by secondary active transport. l Essentially all of the glucose is reabsorbed – and no more than a few milligrams appear in the urine per 24 hours.
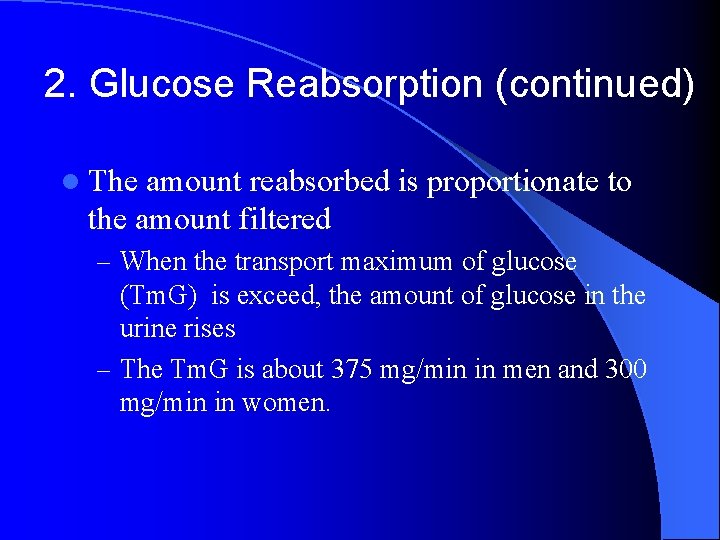
2. Glucose Reabsorption (continued) l The amount reabsorbed is proportionate to the amount filtered – When the transport maximum of glucose (Tm. G) is exceed, the amount of glucose in the urine rises – The Tm. G is about 375 mg/min in men and 300 mg/min in women.
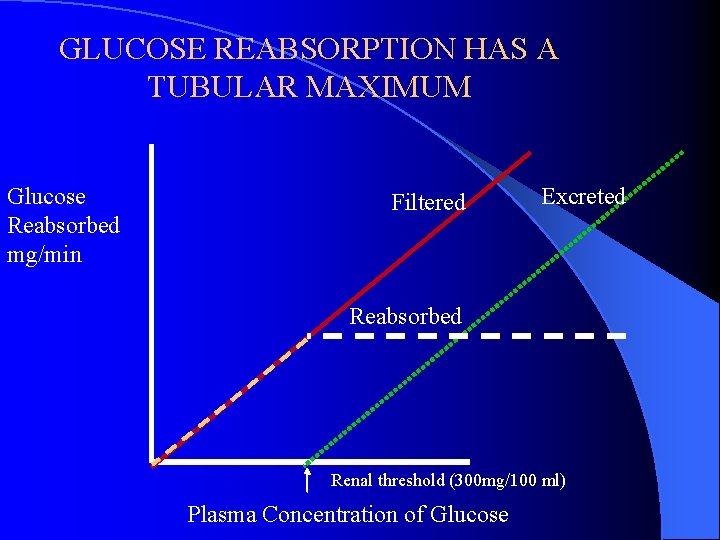
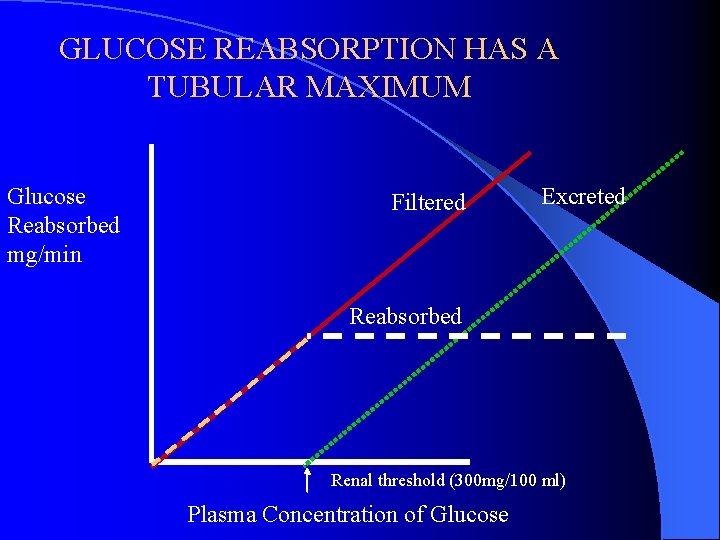
GLUCOSE REABSORPTION HAS A TUBULAR MAXIMUM Glucose Reabsorbed mg/min Filtered Excreted Reabsorbed Renal threshold (300 mg/100 ml) Plasma Concentration of Glucose
The renal threshold for glucose l The plasma level at which the glucose first appears in the urine. – 200 mg/dl of arterial plasma, – 180 mg/dl of venous blood
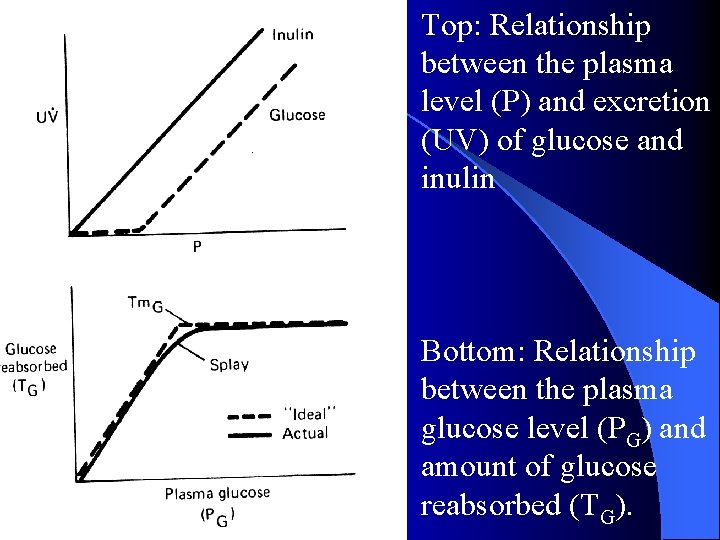
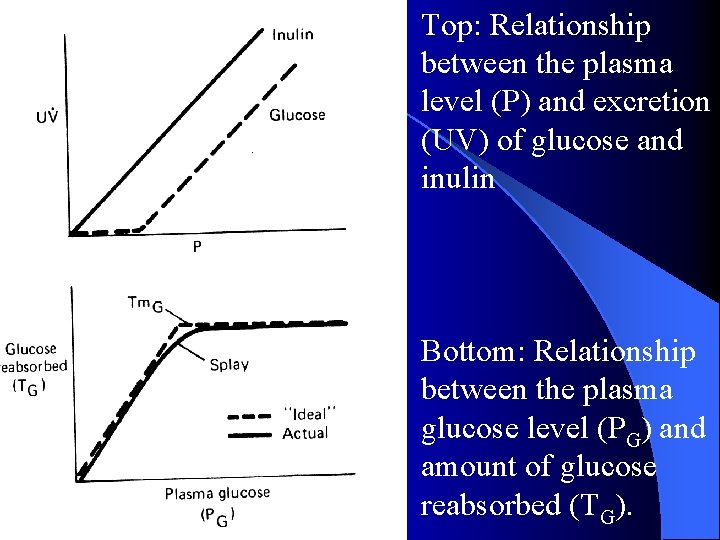
Top: Relationship between the plasma level (P) and excretion (UV) of glucose and inulin Bottom: Relationship between the plasma glucose level (PG) and amount of glucose reabsorbed (TG).
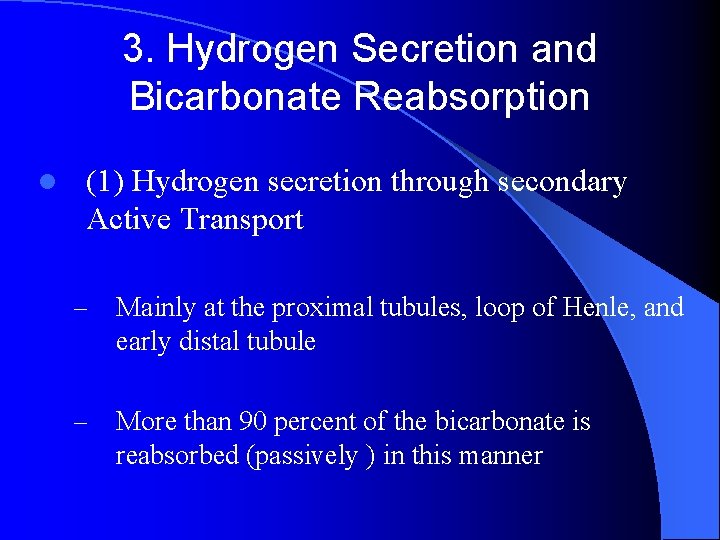
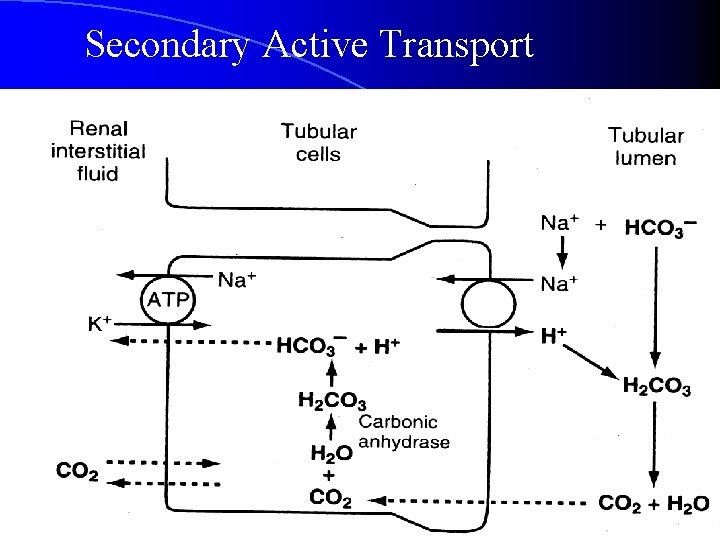
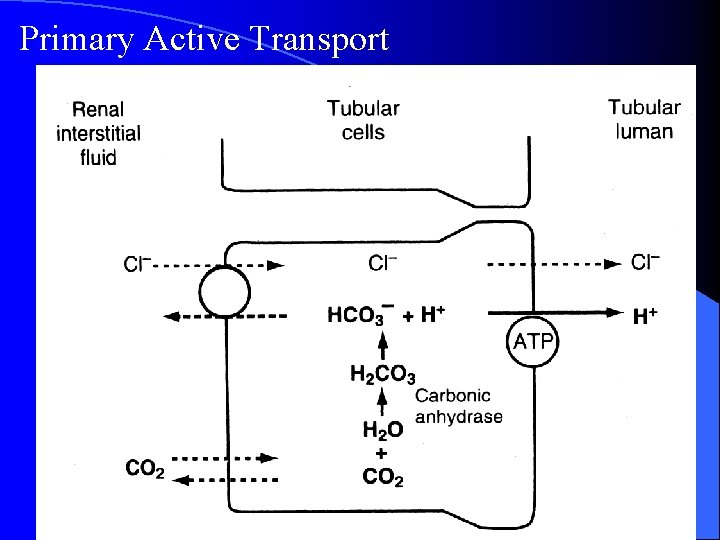
3. Hydrogen Secretion and Bicarbonate Reabsorption l (1) Hydrogen secretion through secondary Active Transport – Mainly at the proximal tubules, loop of Henle, and early distal tubule – More than 90 percent of the bicarbonate is reabsorbed (passively ) in this manner
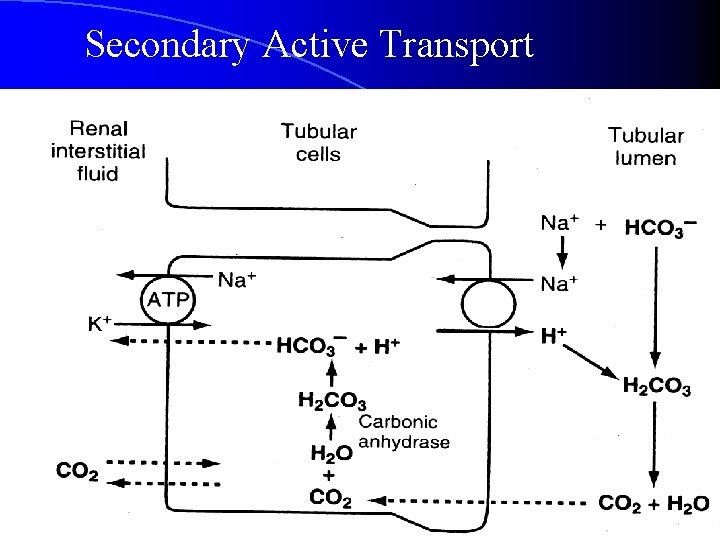
Secondary Active Transport
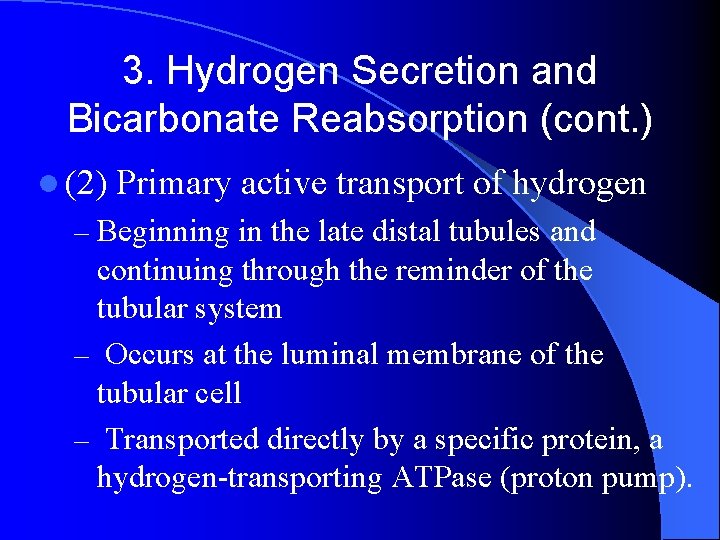
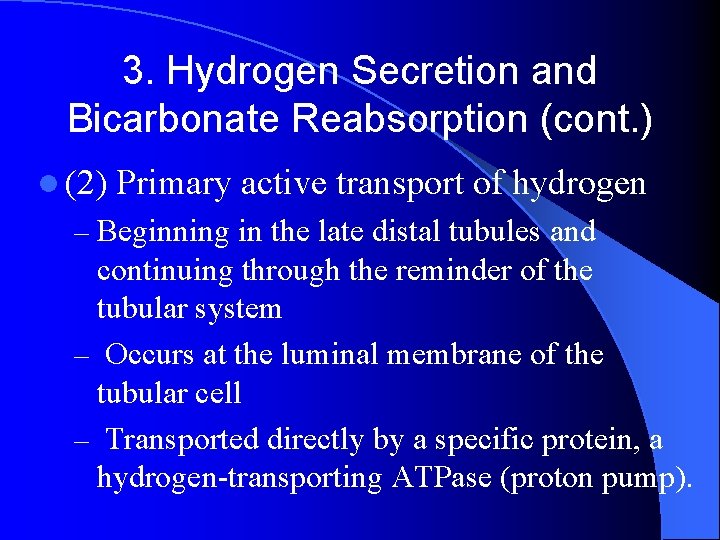
3. Hydrogen Secretion and Bicarbonate Reabsorption (cont. ) l (2) Primary active transport of hydrogen – Beginning in the late distal tubules and continuing through the reminder of the tubular system – Occurs at the luminal membrane of the tubular cell – Transported directly by a specific protein, a hydrogen-transporting ATPase (proton pump).
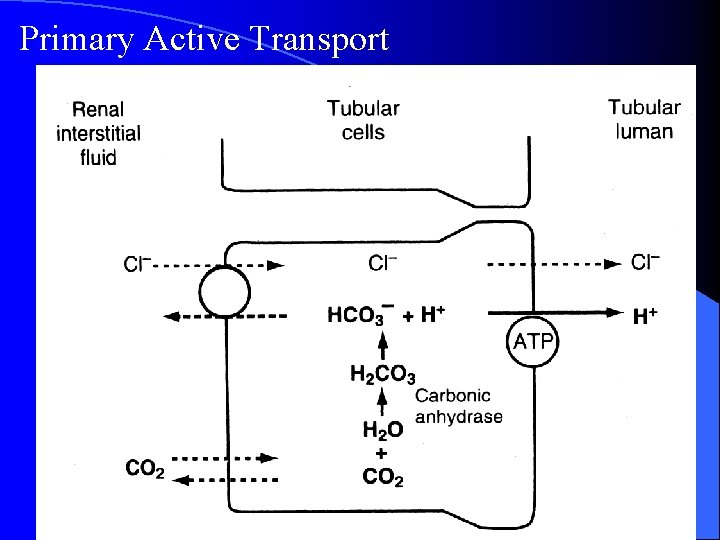
Primary Active Transport
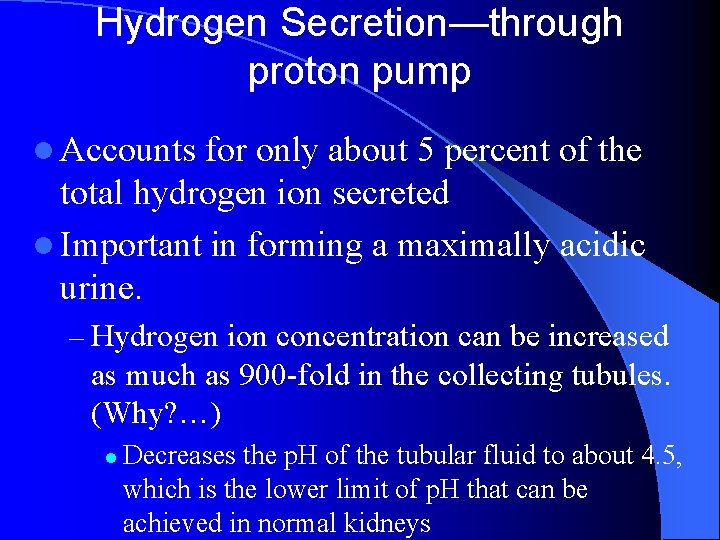
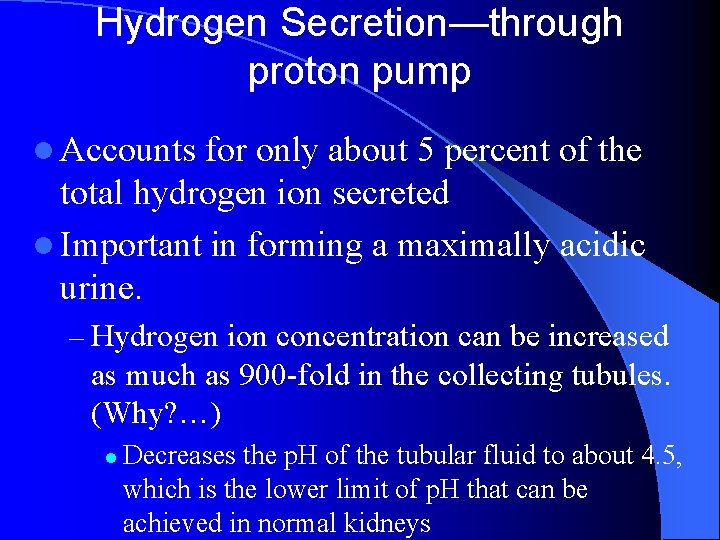
Hydrogen Secretion—through proton pump l Accounts for only about 5 percent of the total hydrogen ion secreted l Important in forming a maximally acidic urine. – Hydrogen ion concentration can be increased as much as 900 -fold in the collecting tubules. (Why? …) l Decreases the p. H of the tubular fluid to about 4. 5, which is the lower limit of p. H that can be achieved in normal kidneys
4. Ammonia (氨) Buffer System l. Excretion of excess hydrogen ions l. Generation of new bicarbonate
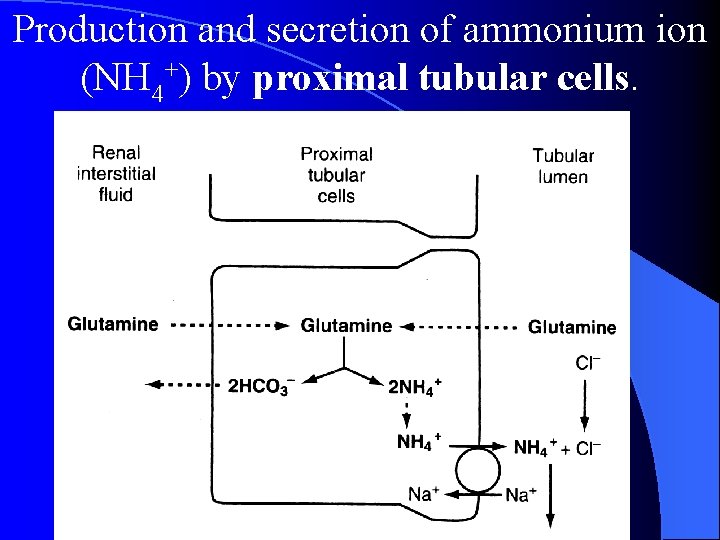
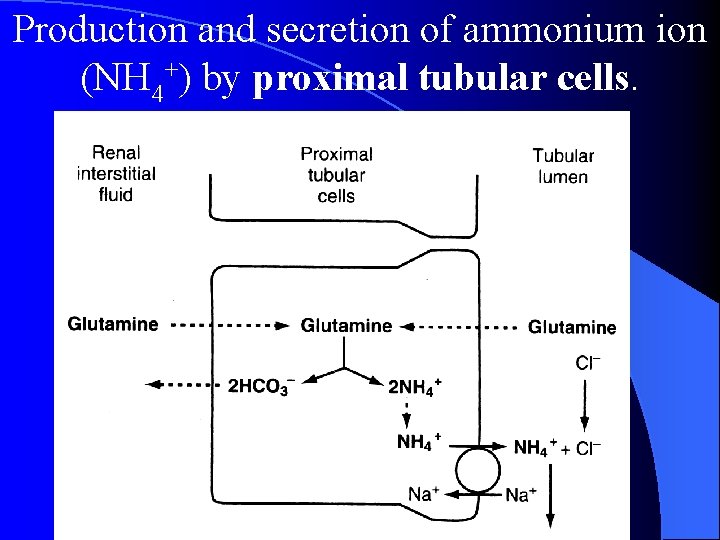
Production and secretion of ammonium ion (NH 4+) by proximal tubular cells.
4. Ammonia Buffer System (continued) l For each molecule of glutamine metabolized – two NH 4+ ions are secreted into the urine – two HCO 3 - ions are reabsorbed into the blood. l The HCO 3 - generated by this process constitutes new bicarbonate.
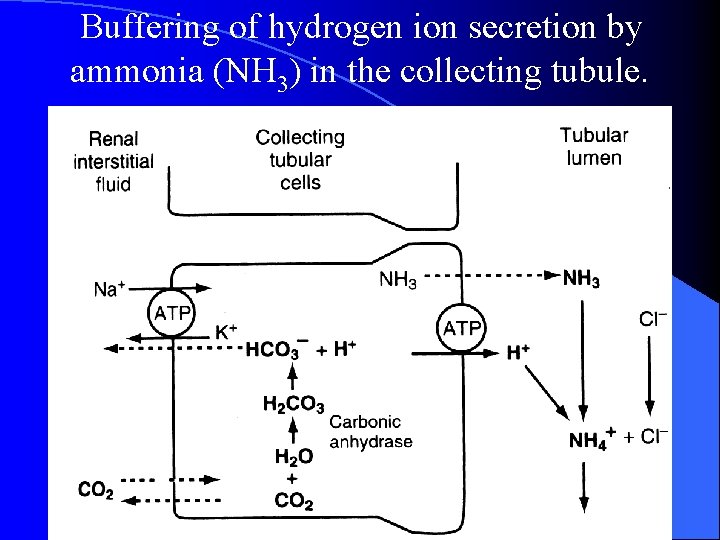
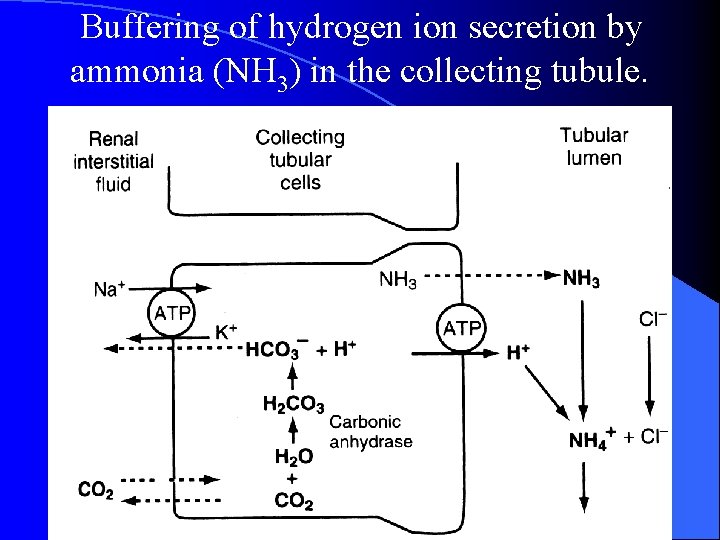
Buffering of hydrogen ion secretion by ammonia (NH 3) in the collecting tubule.
Ammonia Buffer System (continued) l Renal ammonium-ammonia buffer system is subject to physiological control. l Increase in extracellular fluid hydrogen ion concentration stimulates renal glutamine metabolism – increase the formation of NH 4+ and new bicarbonate to be used in hydrogen ion buffering l Decrease in hydrogen ion concentration has the opposite effect.
Ammonia Buffer System (continued) l with chronic acidosis, the dominant mechanism by which acid is eliminated of NH 4+ – the most important mechanism for generating new bicarbonate during chronic acidosis
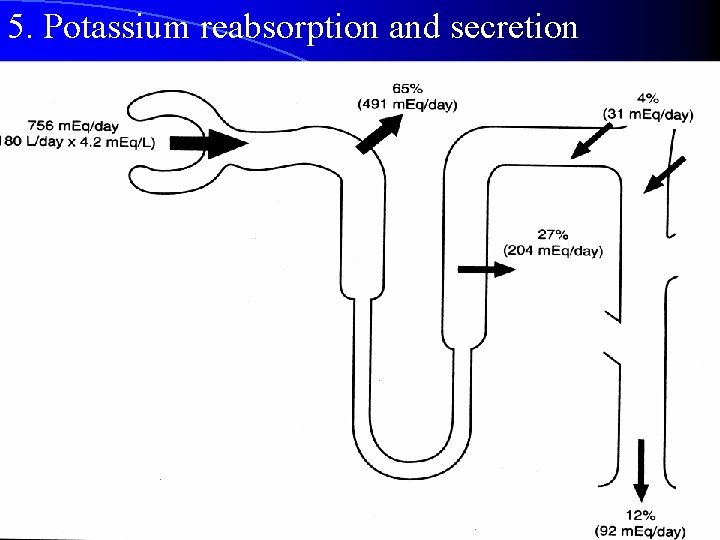
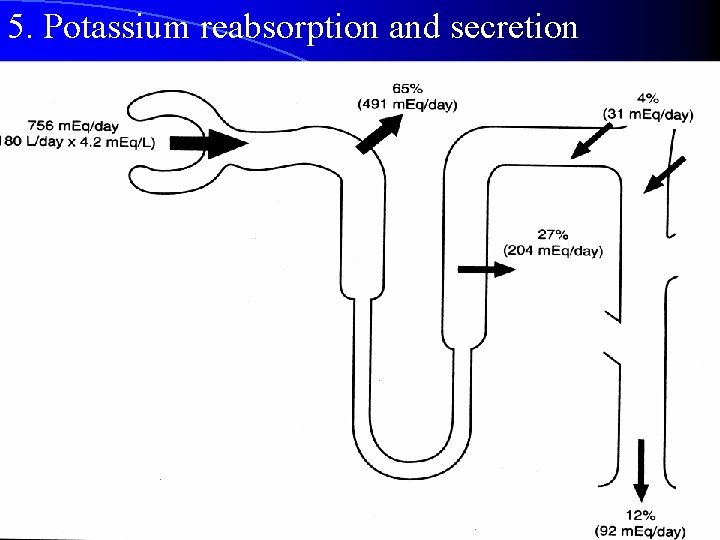
5. Potassium reabsorption and secretion
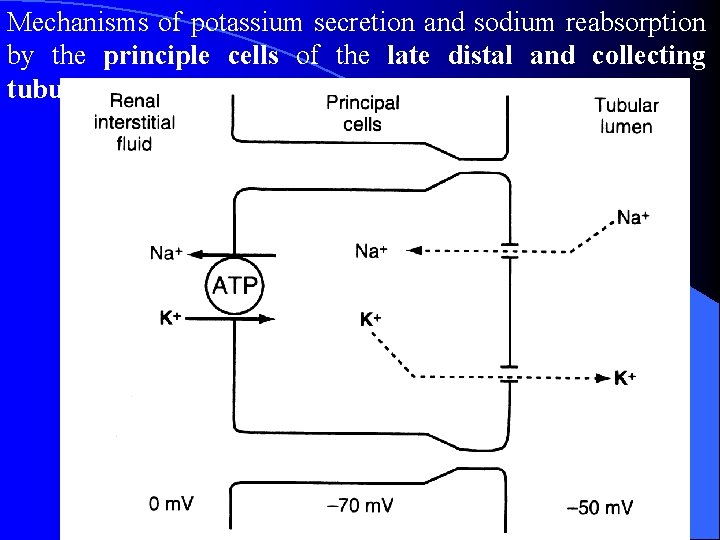
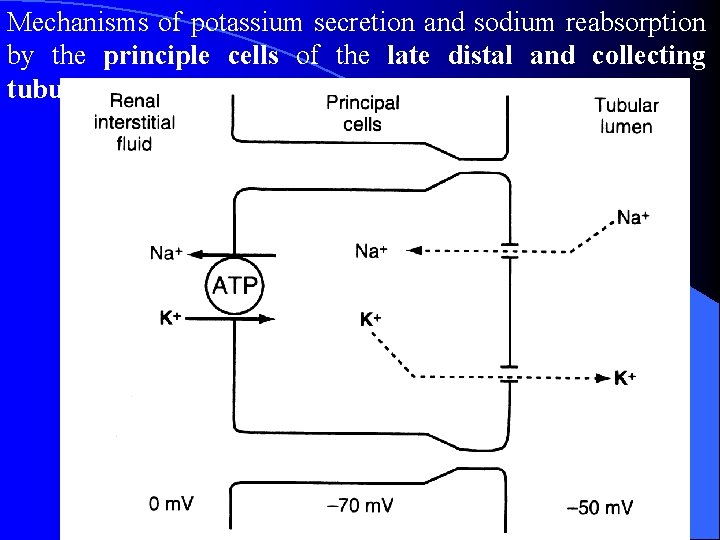
Mechanisms of potassium secretion and sodium reabsorption by the principle cells of the late distal and collecting tubules.
6. Control of Calcium Excretion by the Kidneys l Calcium is both filtered and reabsorbed in the kidneys but not secreted l Only about 50% of the plasma calcium is ionized, with the remainder being bound to the plasma proteins. l Calcium excretion is adjusted to meet the body’s needs. l Parathyroid hormone (PTH) increases calcium reabsorption in the thick ascending lops of Henle and distal tubules, and reduces urinary excretion of calcium
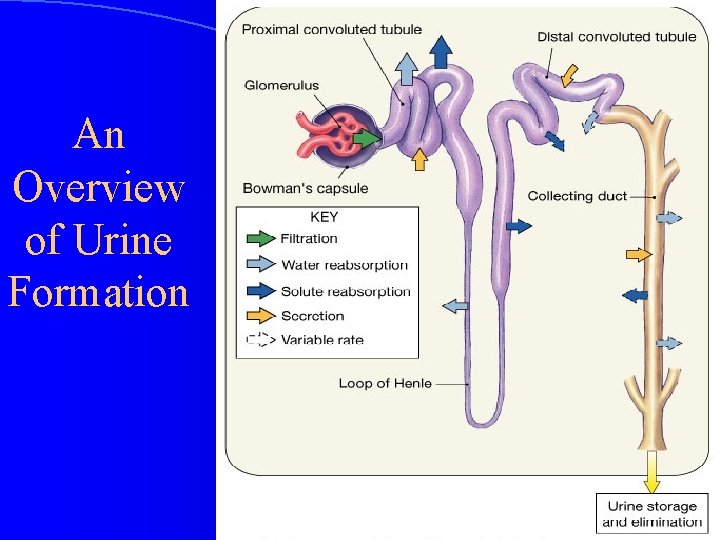
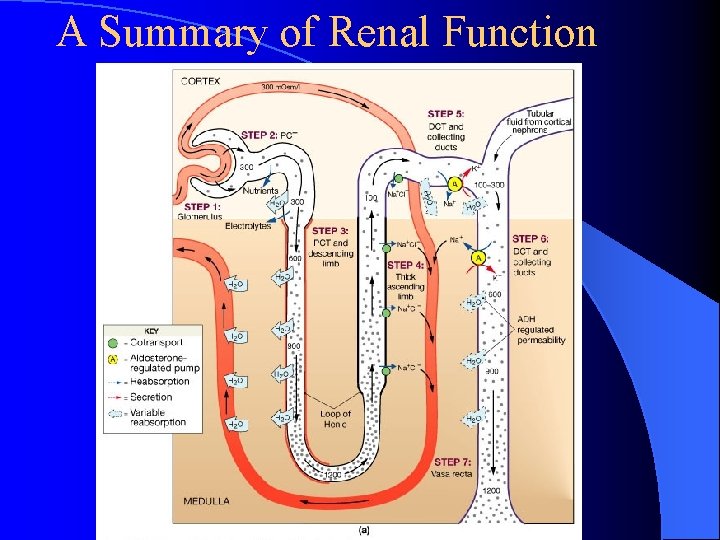
An Overview of Urine Formation
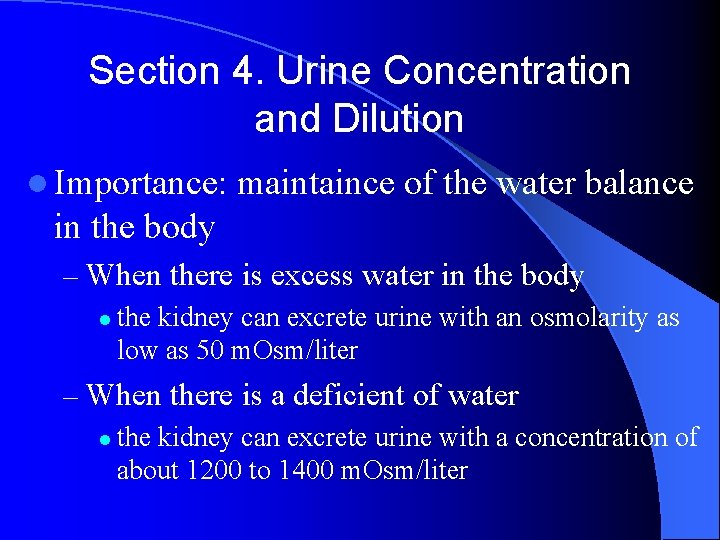
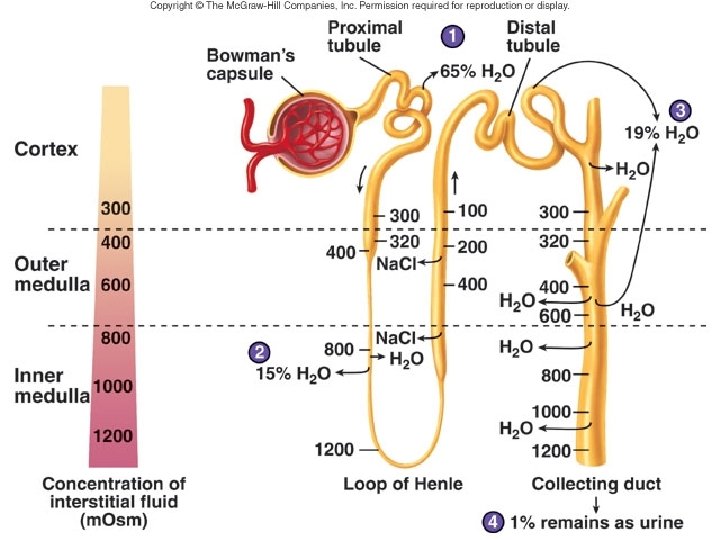
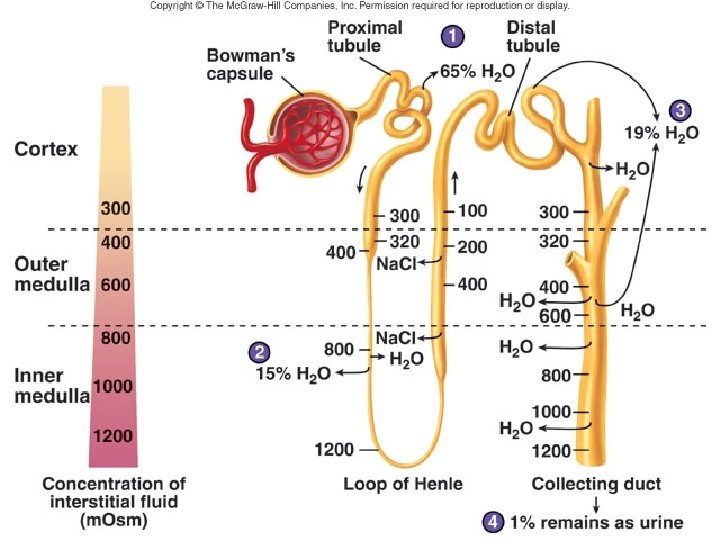
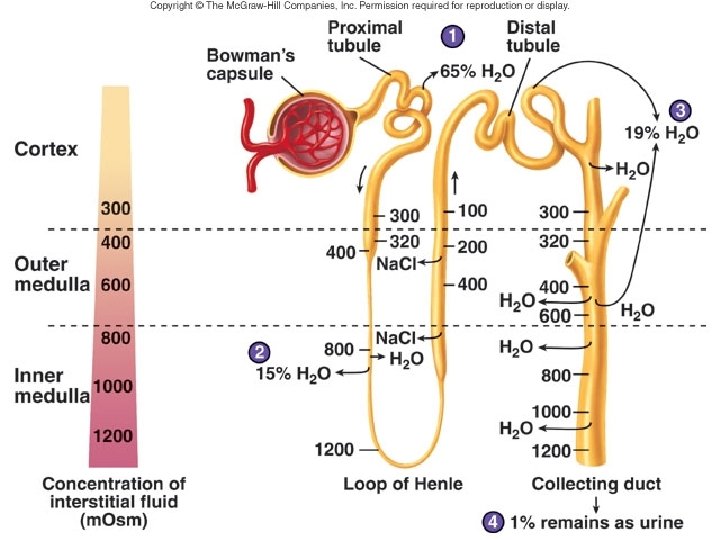
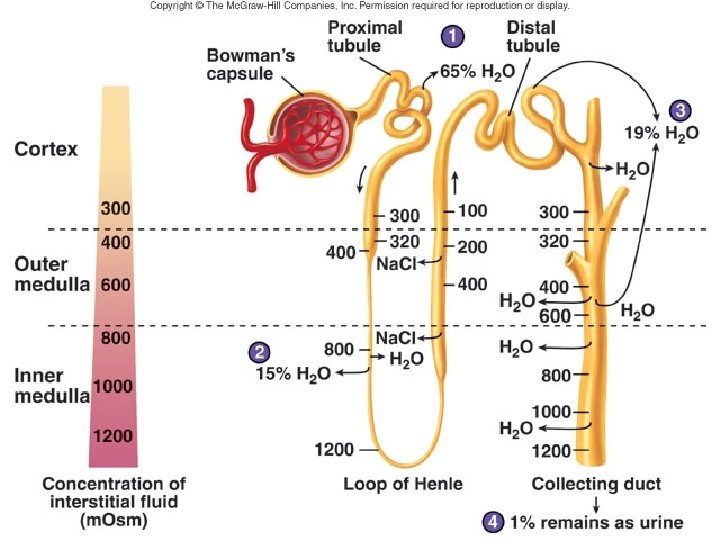
Section 4. Urine Concentration and Dilution l Importance: maintaince of the water balance in the body – When there is excess water in the body l the kidney can excrete urine with an osmolarity as low as 50 m. Osm/liter – When there is a deficient of water l the kidney can excrete urine with a concentration of about 1200 to 1400 m. Osm/liter
The basic requirements forming a concentrated or diluted urine l the controlled secretion of antidiuretic hormone (ADH) – regulates the permeability of the distal tubules and collecting ducts to water l a high osmolarity of the renal medullary interstitial fluid – provides the osmotic gradient necessary for water reabsorption to occur in the presence of high level of ADH
I The Counter-Current Mechanism Produces a Hyperosmotic Renal Medullary Interstitium
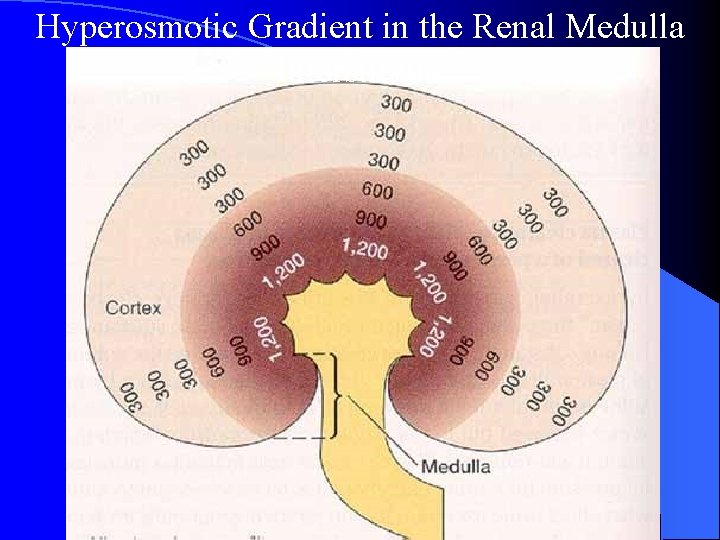
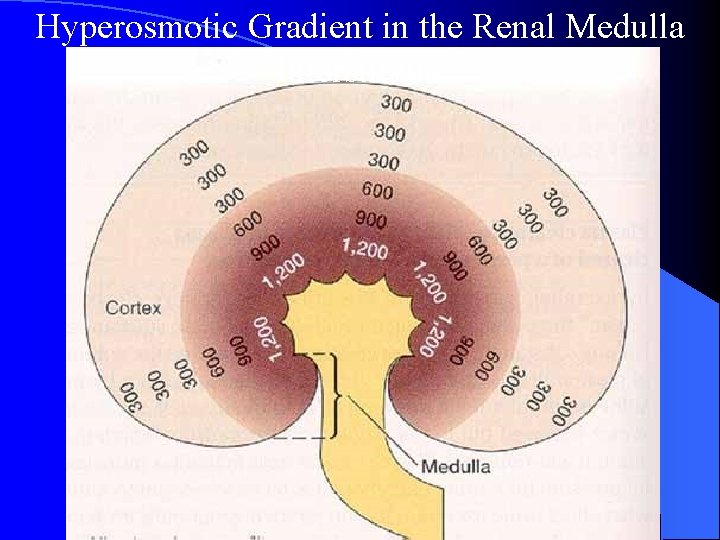
Hyperosmotic Gradient in the Renal Medulla Interstitium
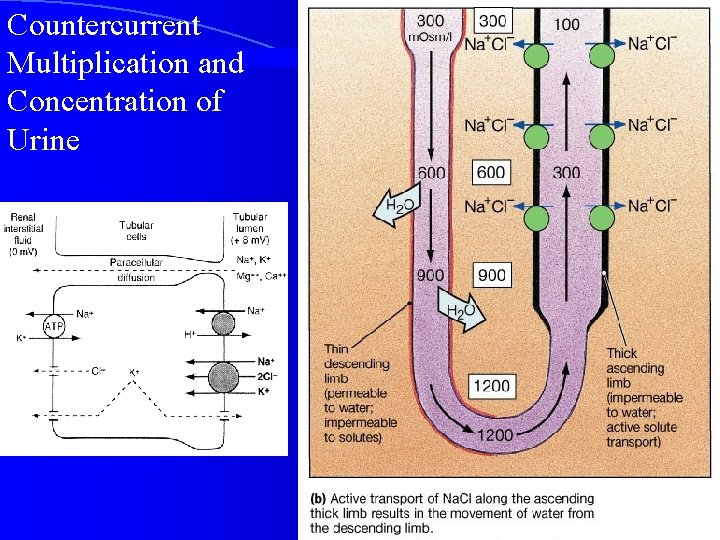
Countercurrent Multiplication and Concentration of Urine
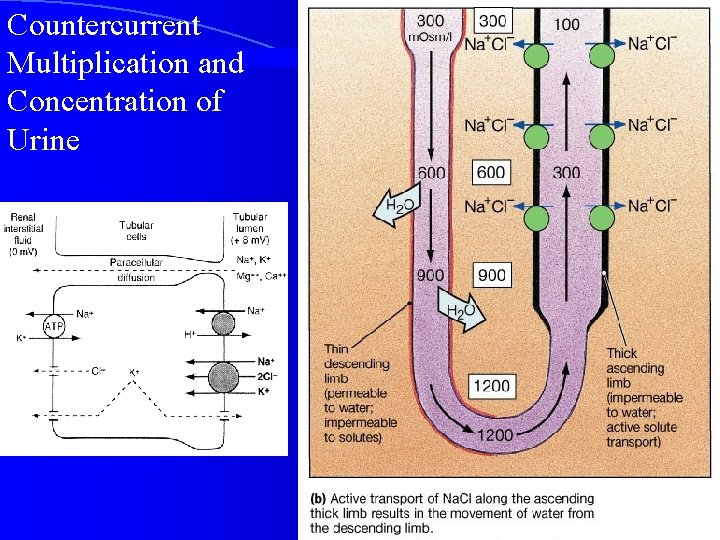
Countercurrent Multiplication and Concentration of Urine
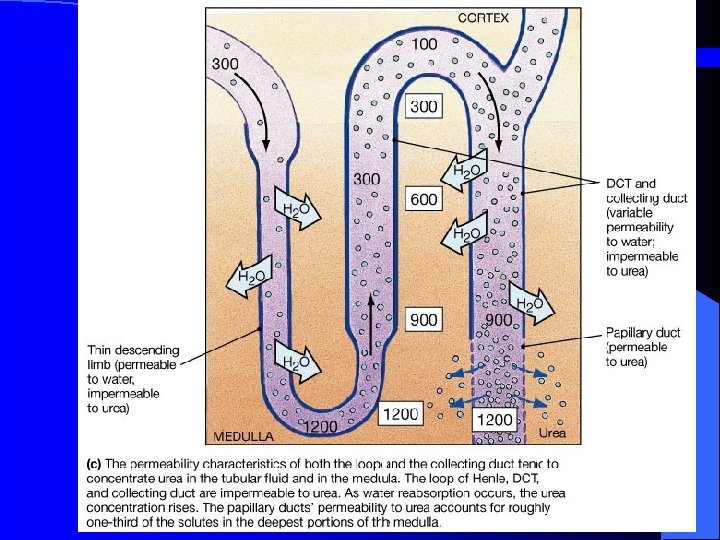
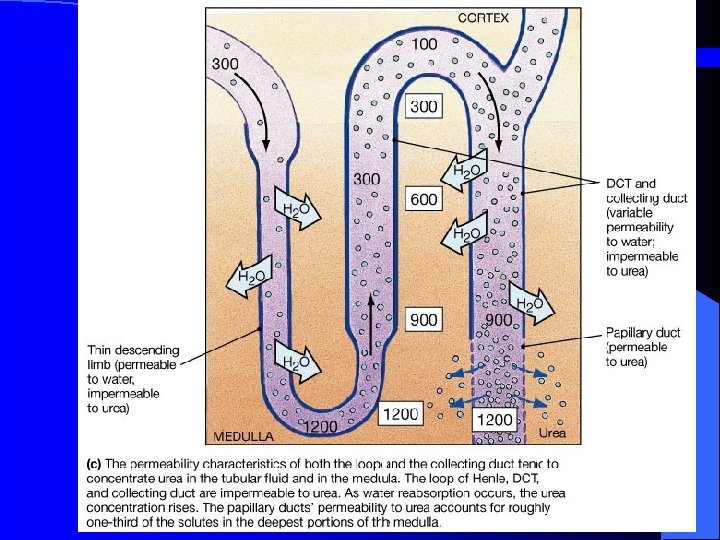
Figure 26. 13 c
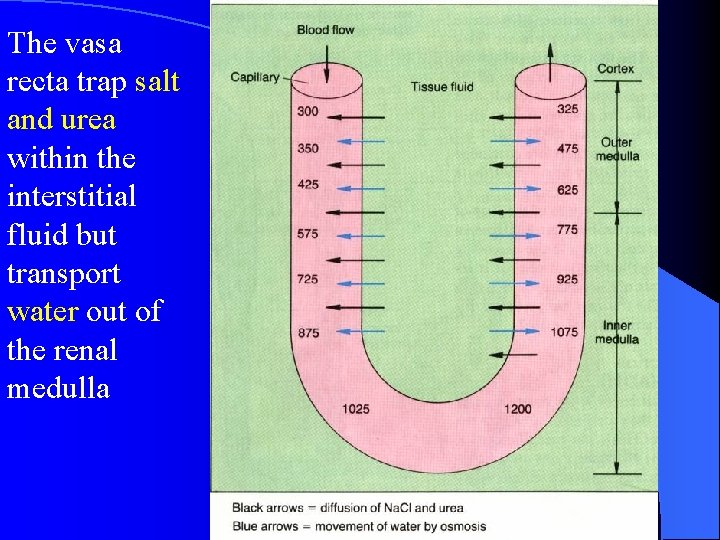
I. II. Counter-current Exchange in the Vasa Recta Preserves Hyperosmolarity of the Renal medulla
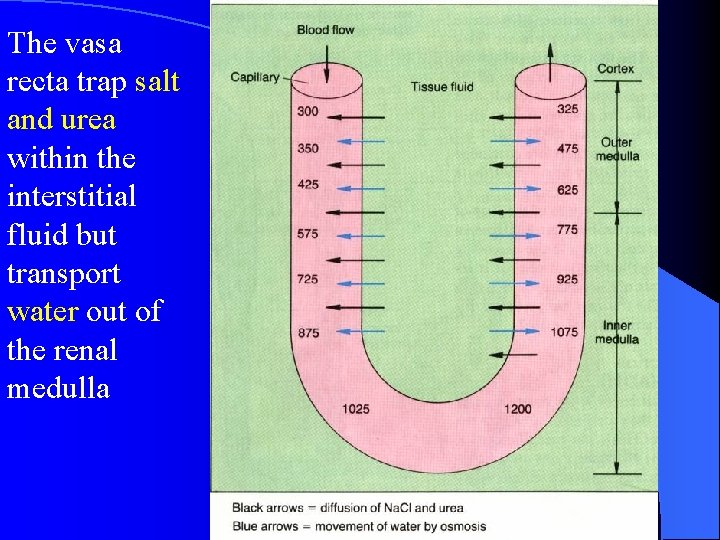
The vasa recta trap salt and urea within the interstitial fluid but transport water out of the renal medulla
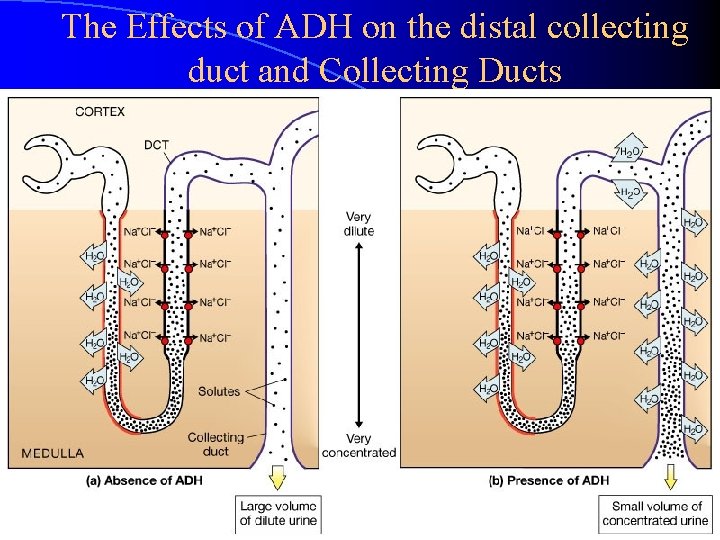
III. Role of the Distal Tubule and Collecting Ducts in Forming Concentrated or Diluted urine
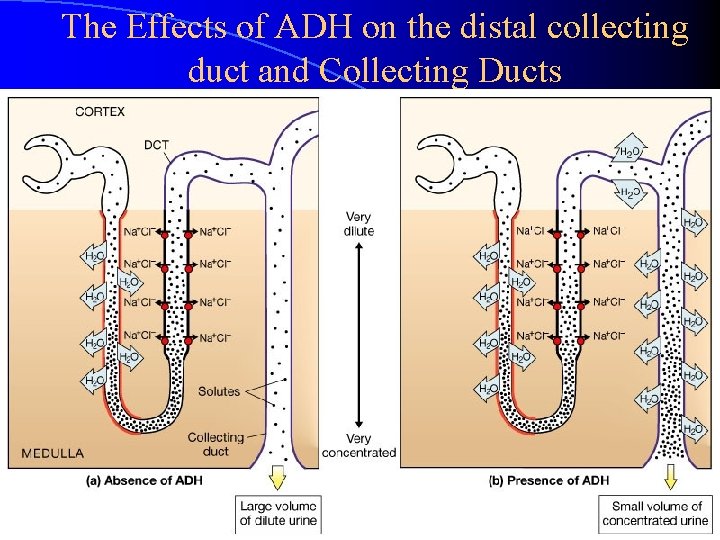
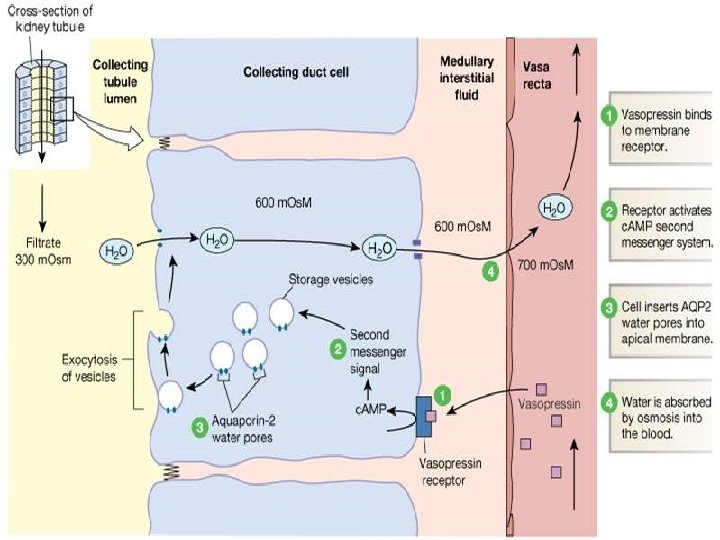
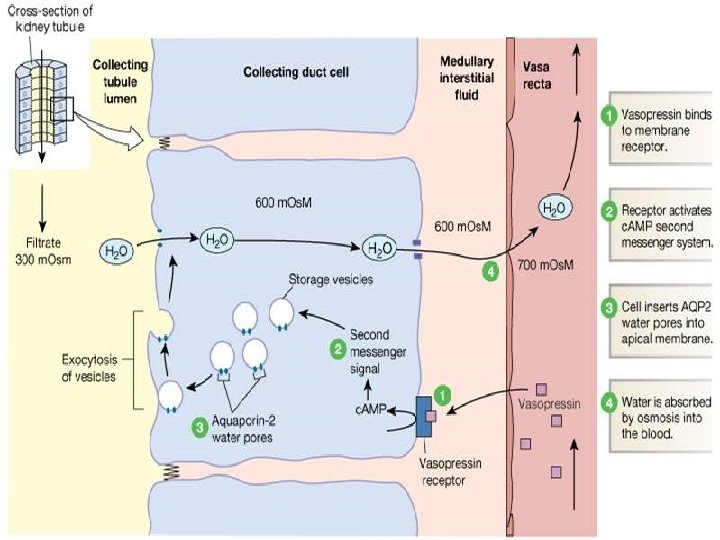
The Effects of ADH on the distal collecting duct and Collecting Ducts Figure 26. 15 a, b
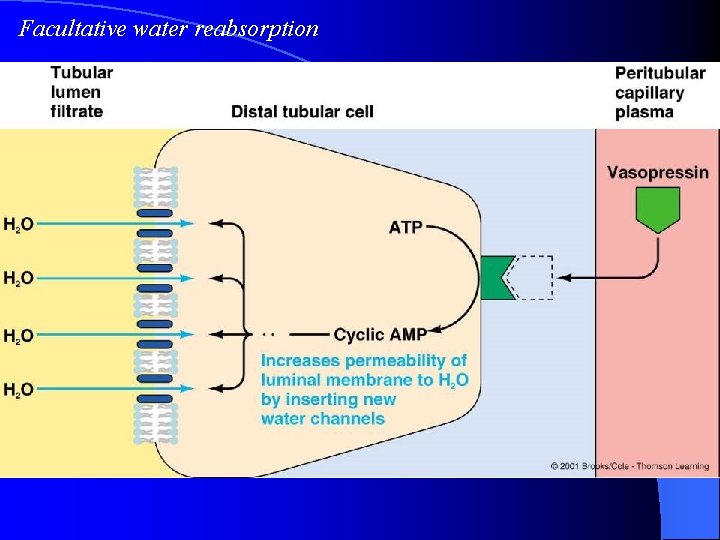
The Role of ADH • makes the wall of the collecting duct more permeable to water • Mechanism?
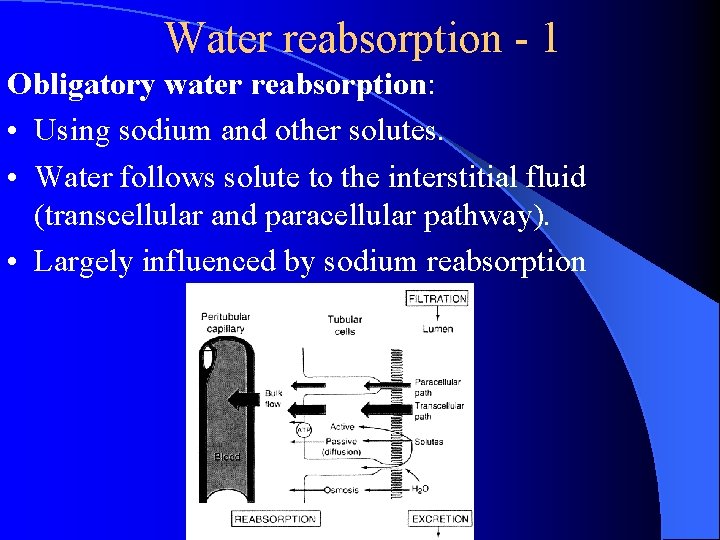
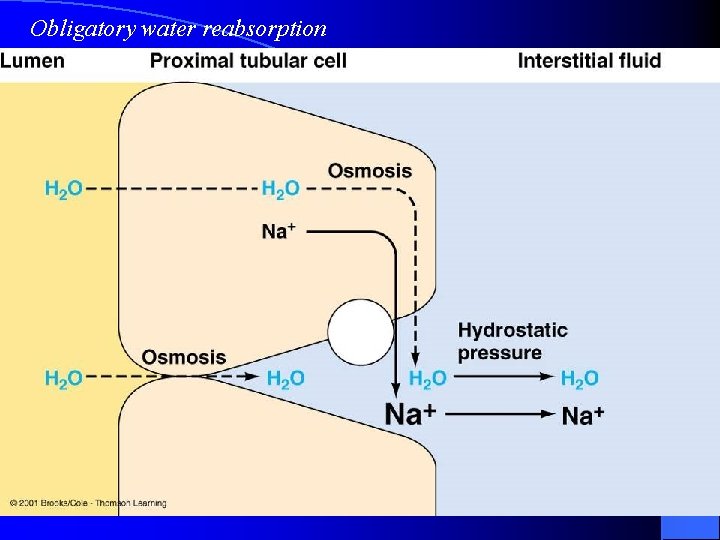
Water reabsorption - 1 Obligatory water reabsorption: • Using sodium and other solutes. • Water follows solute to the interstitial fluid (transcellular and paracellular pathway). • Largely influenced by sodium reabsorption
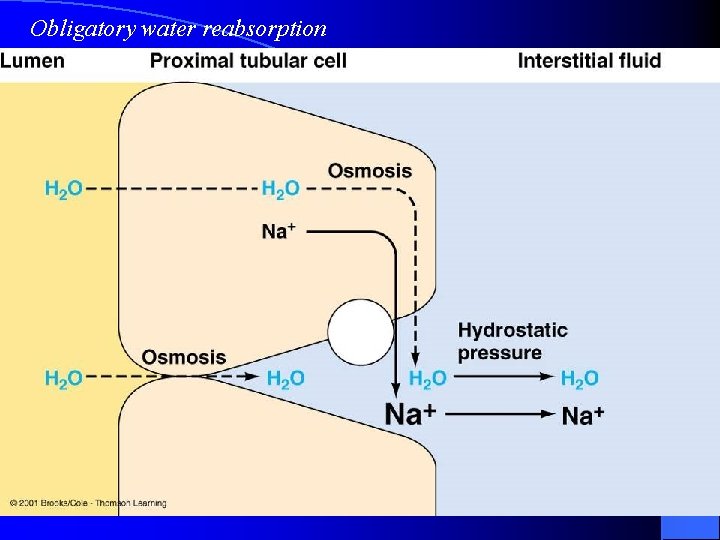
Obligatory water reabsorption
Water reabsorption - 2 Facultative (特许的) water reabsorption: • Occurs mostly in collecting ducts • Through the water poles (channel) • Regulated by the ADH
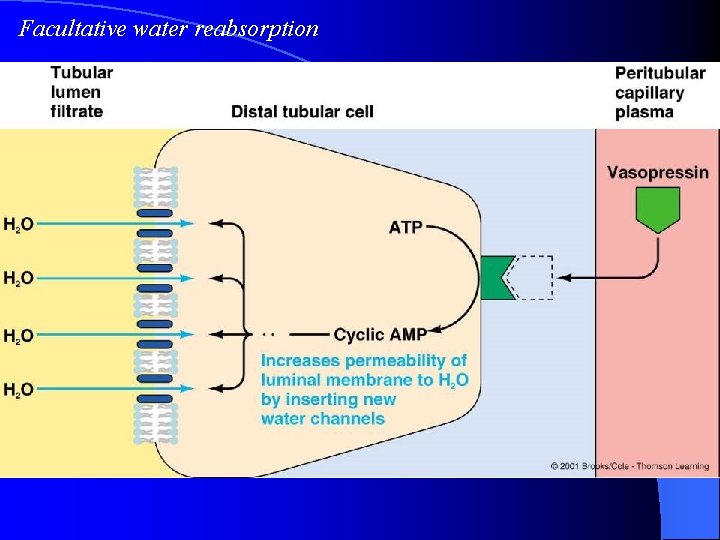
Facultative water reabsorption
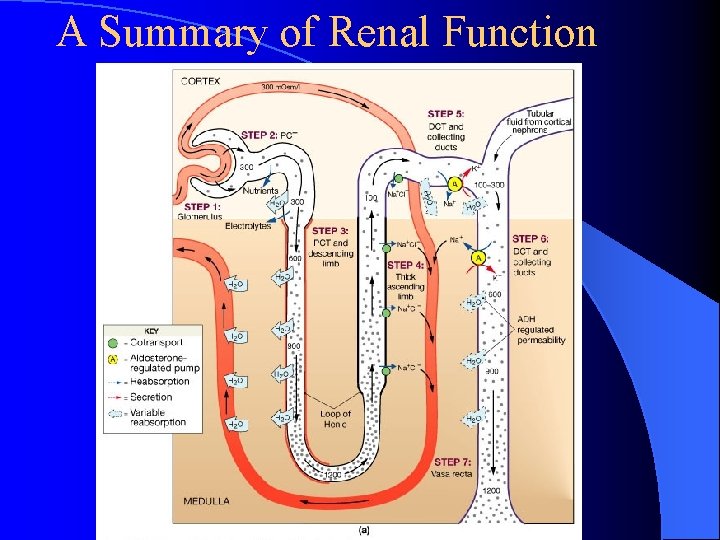
A Summary of Renal Function
Regulation of the Urine Formation I. Autoregulation of the renal reabsorption
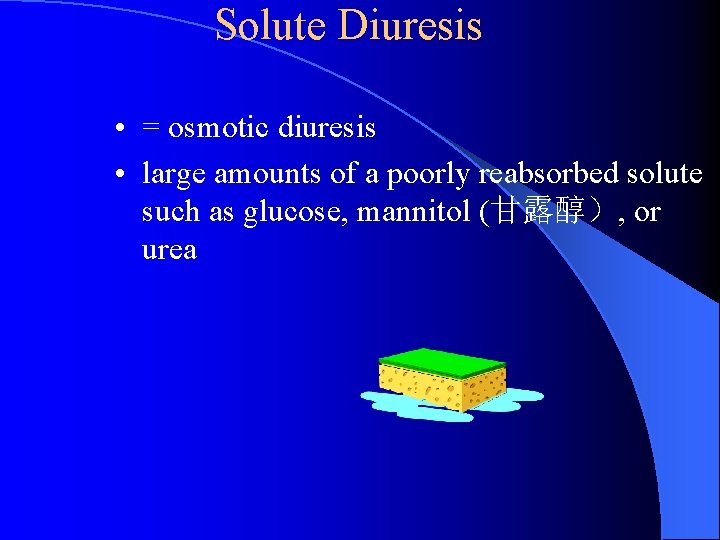
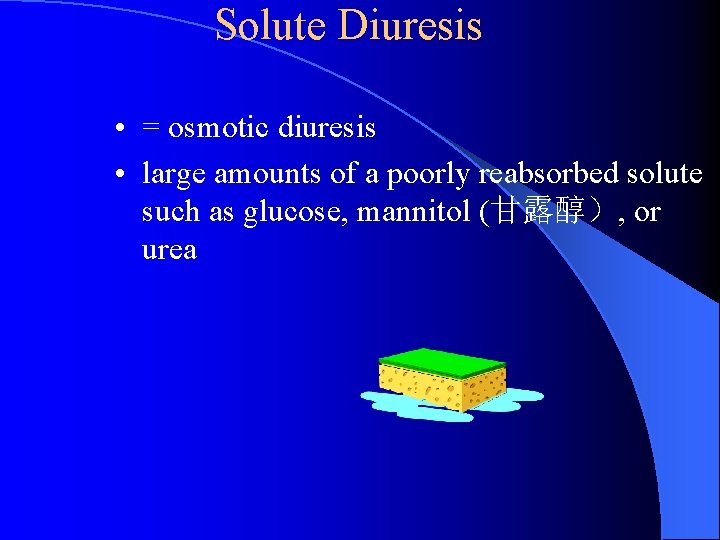
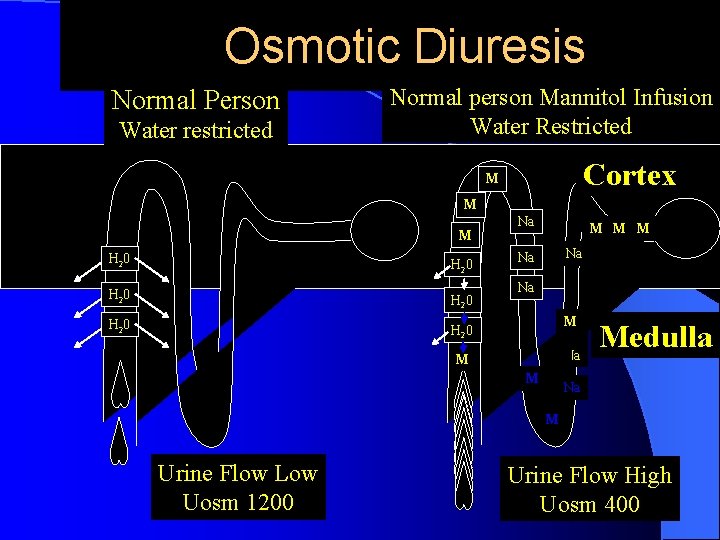
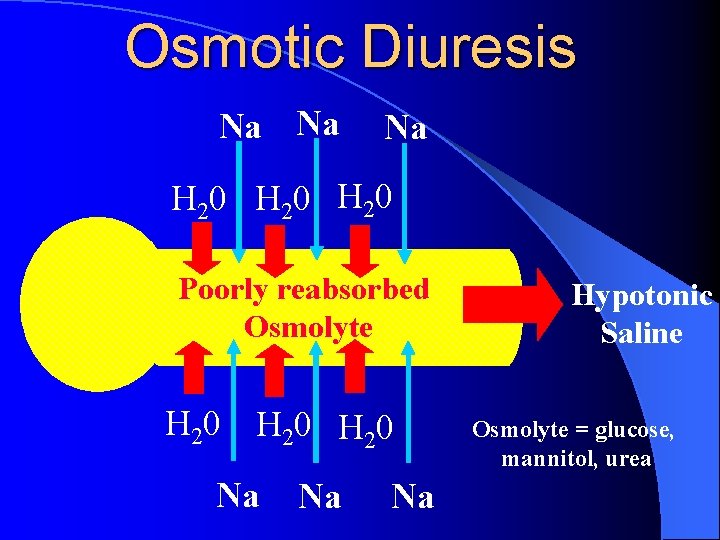
Solute Diuresis • = osmotic diuresis • large amounts of a poorly reabsorbed solute such as glucose, mannitol (甘露醇), or urea
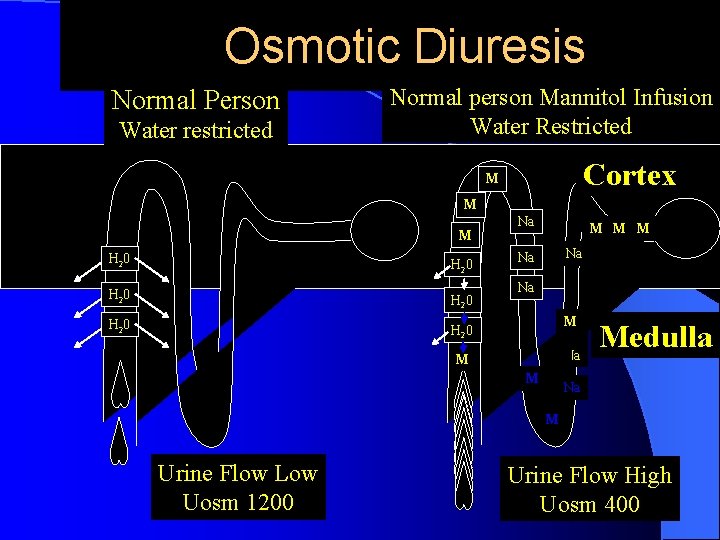
Osmotic Diuresis Normal Person Water restricted Normal person Mannitol Infusion Water Restricted Cortex M M M H 2 0 H 2 0 Na M M M Na Na Na M M Medulla Na M Urine Flow Low Uosm 1200 Urine Flow High Uosm 400
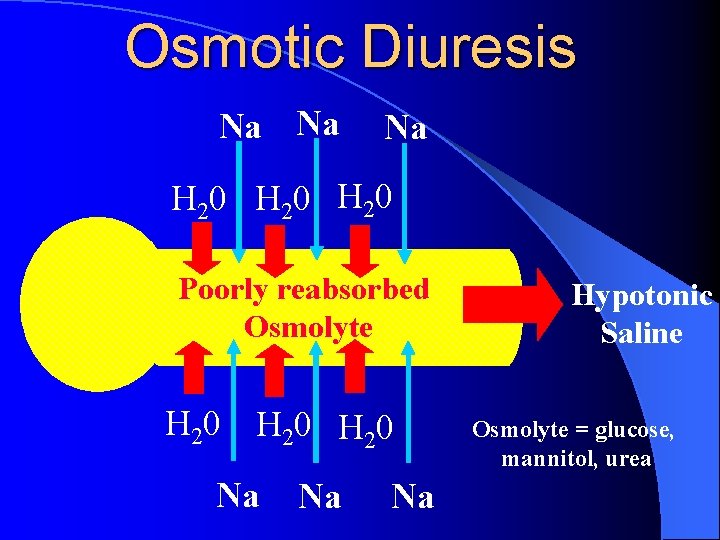
Osmotic Diuresis Na Na Na H 20 Poorly reabsorbed Osmolyte H 20 Na Na Na Hypotonic Saline Osmolyte = glucose, mannitol, urea
2. Glomerulotubular Balance l Concept: The constant fraction (about 65% - 70%) of the filtered Na+ and water are reabsorbed in the proximal tubule, despite variation of GFR. l Importance: To prevent overloading of the distal tubular segments when GFR increases.
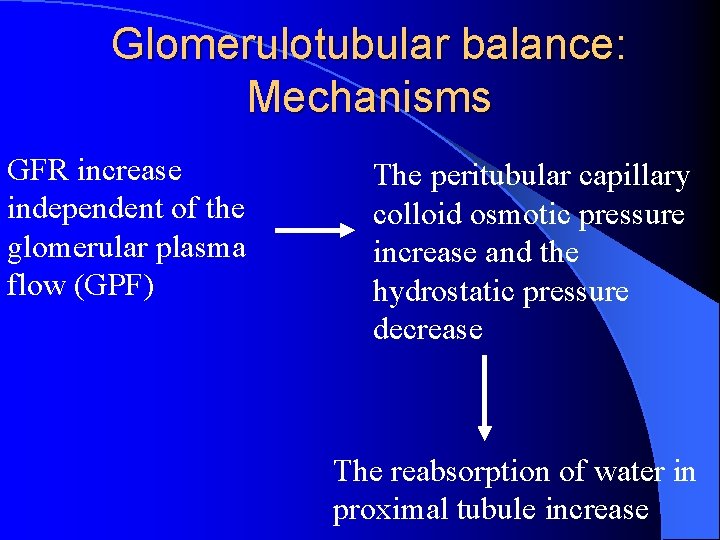
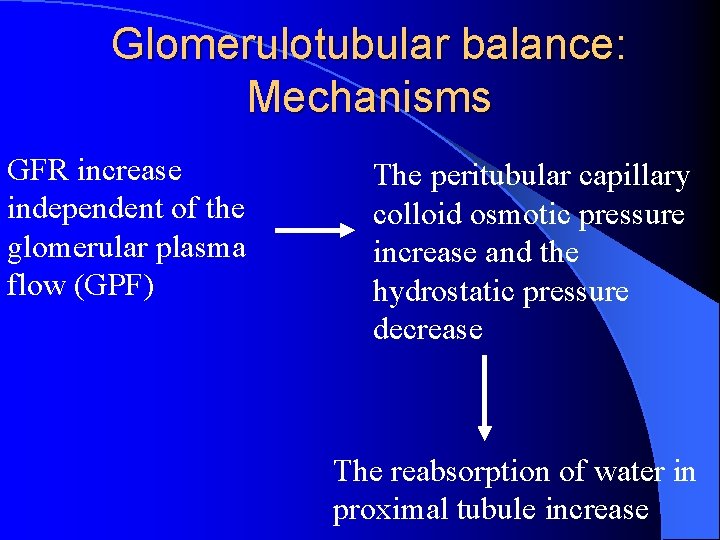
Glomerulotubular balance: Mechanisms GFR increase independent of the glomerular plasma flow (GPF) The peritubular capillary colloid osmotic pressure increase and the hydrostatic pressure decrease The reabsorption of water in proximal tubule increase

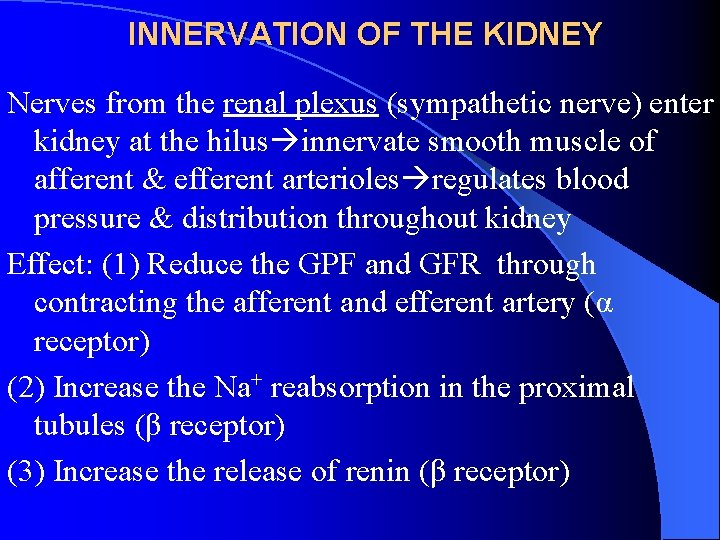
II Nervous Regulation
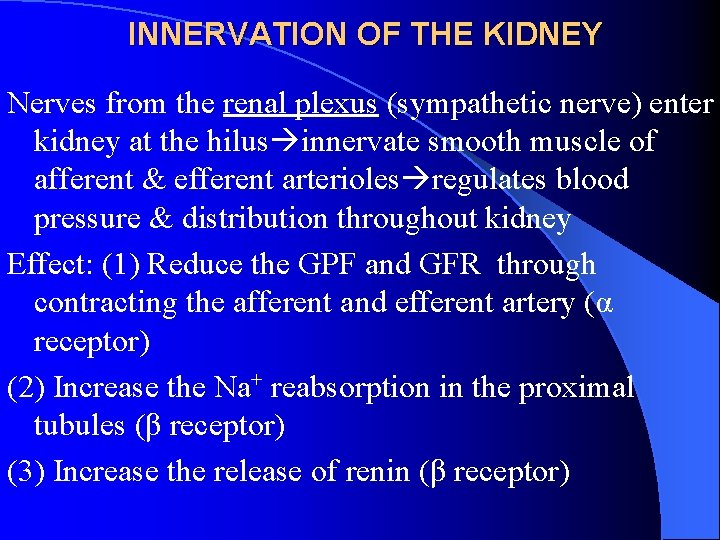
INNERVATION OF THE KIDNEY Nerves from the renal plexus (sympathetic nerve) enter kidney at the hilus innervate smooth muscle of afferent & efferent arterioles regulates blood pressure & distribution throughout kidney Effect: (1) Reduce the GPF and GFR through contracting the afferent and efferent artery (α receptor) (2) Increase the Na+ reabsorption in the proximal tubules (β receptor) (3) Increase the release of renin (β receptor)
III. Humoral Regulation 1. Antidiuretic Hormone (ADH)
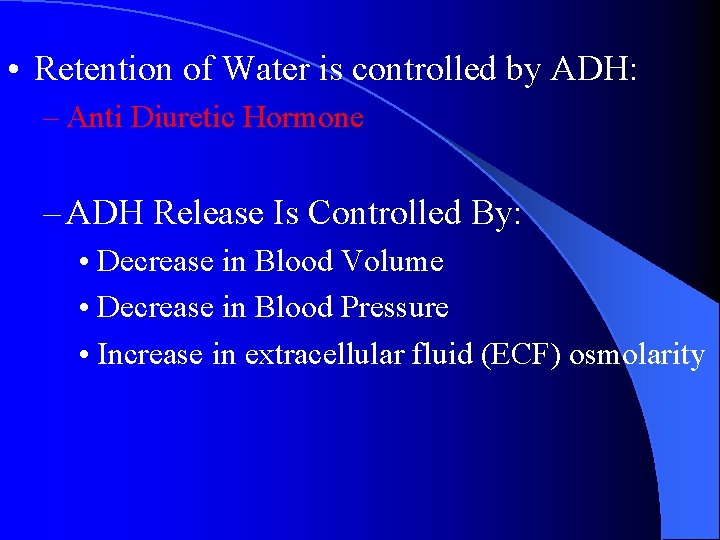
• Retention of Water is controlled by ADH: – Anti Diuretic Hormone – ADH Release Is Controlled By: • Decrease in Blood Volume • Decrease in Blood Pressure • Increase in extracellular fluid (ECF) osmolarity
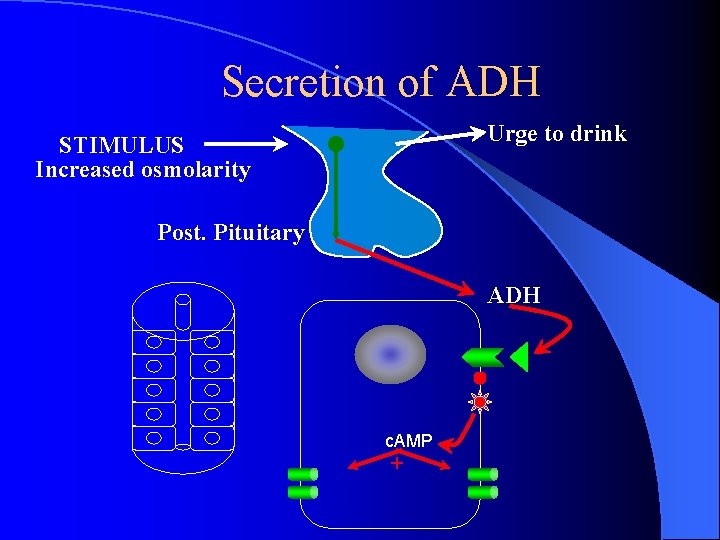
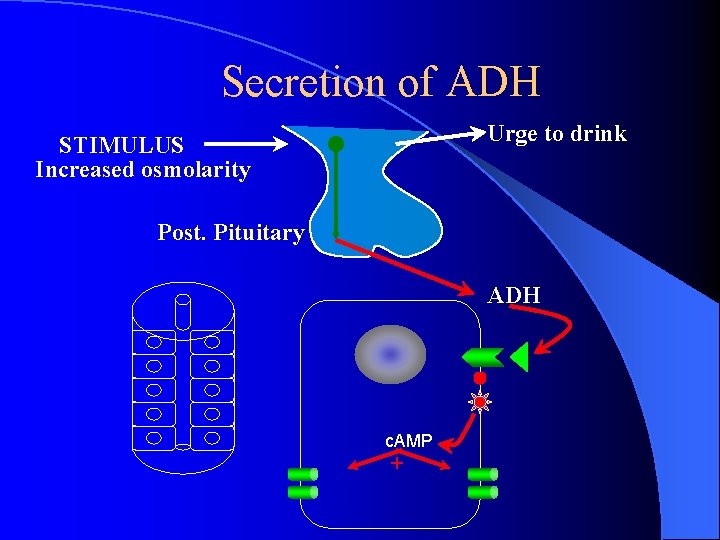
Secretion of ADH Urge to drink STIMULUS Increased osmolarity Post. Pituitary ADH c. AMP +
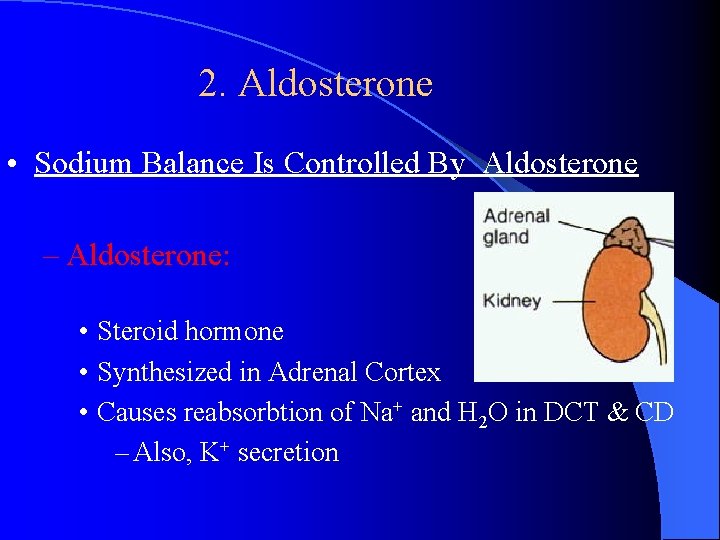
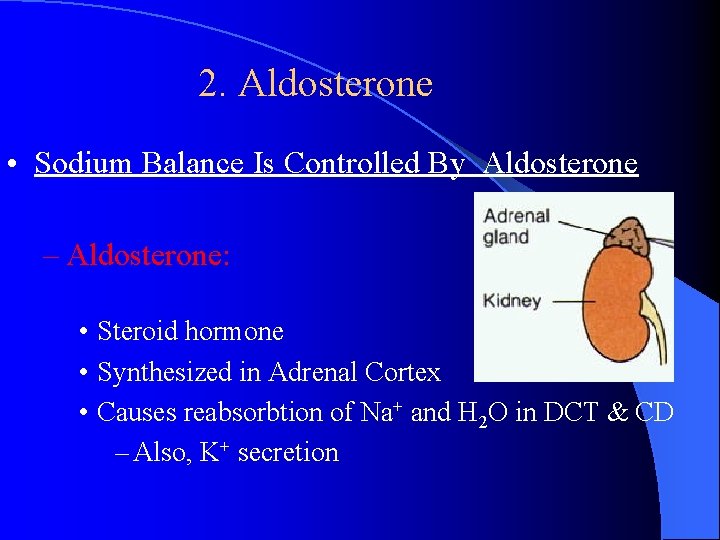
2. Aldosterone • Sodium Balance Is Controlled By Aldosterone – Aldosterone: • Steroid hormone • Synthesized in Adrenal Cortex • Causes reabsorbtion of Na+ and H 2 O in DCT & CD – Also, K+ secretion
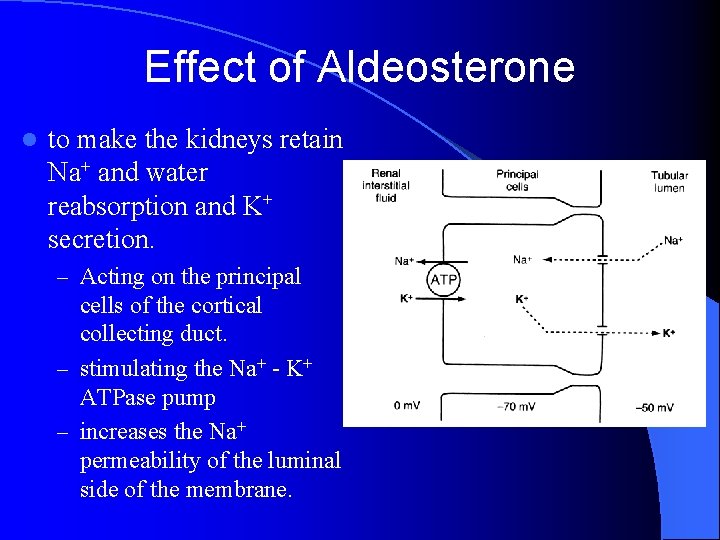
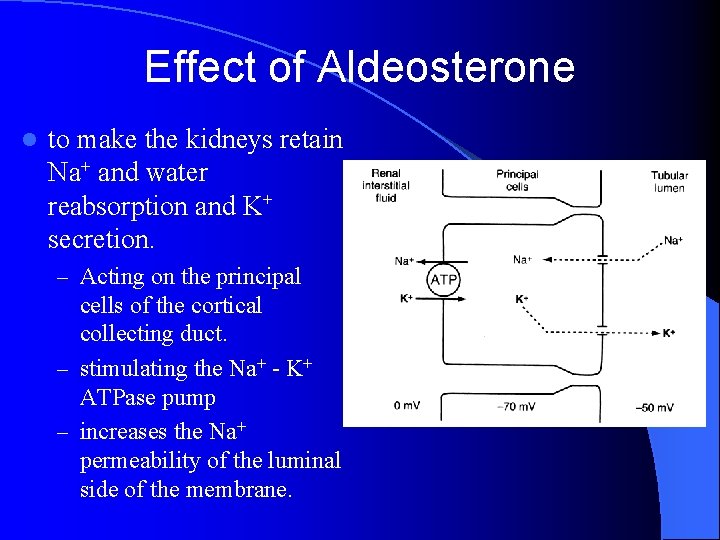
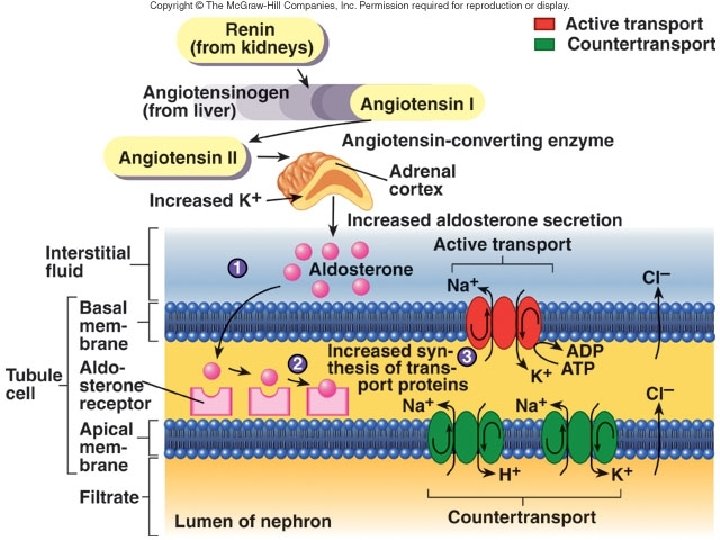
Effect of Aldeosterone l to make the kidneys retain Na+ and water reabsorption and K+ secretion. – Acting on the principal cells of the cortical collecting duct. – stimulating the Na+ - K+ ATPase pump – increases the Na+ permeability of the luminal side of the membrane.
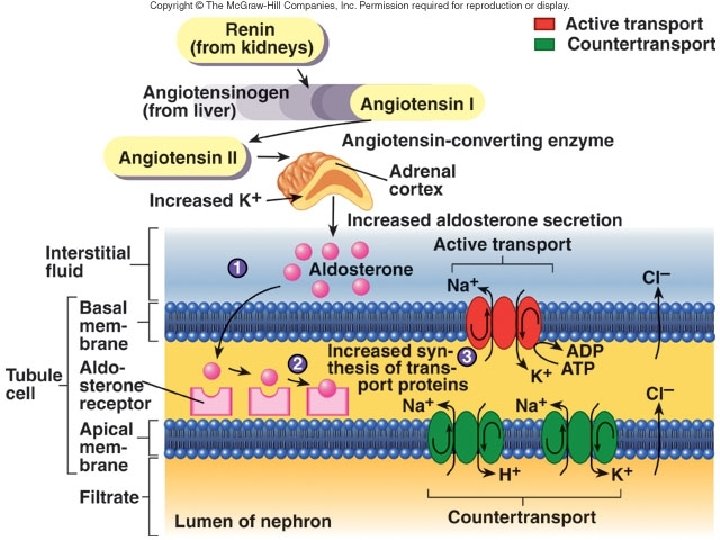
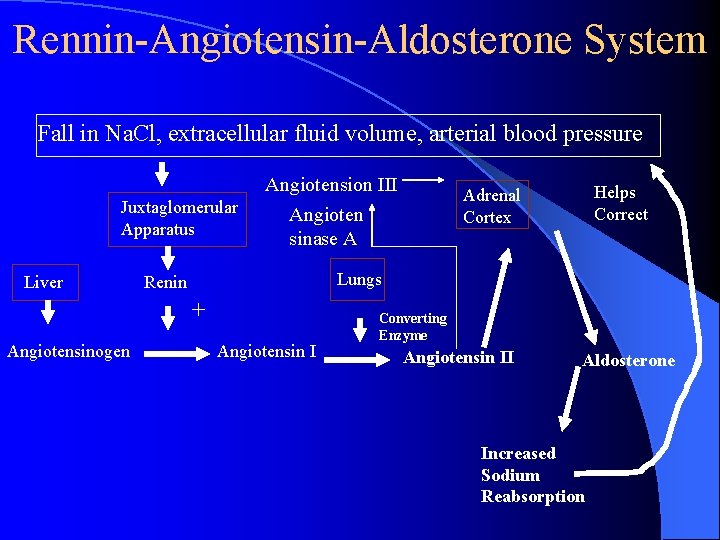
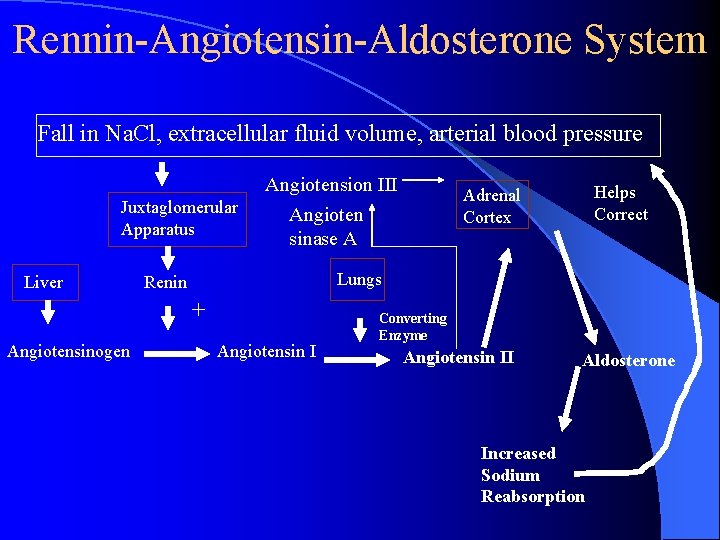
Rennin-Angiotensin-Aldosterone System Fall in Na. Cl, extracellular fluid volume, arterial blood pressure Juxtaglomerular Apparatus Liver Angiotension III Angioten sinase A Lungs Renin + Angiotensinogen Helps Correct Adrenal Cortex Angiotensin I Converting Enzyme Angiotensin II Aldosterone Increased Sodium Reabsorption
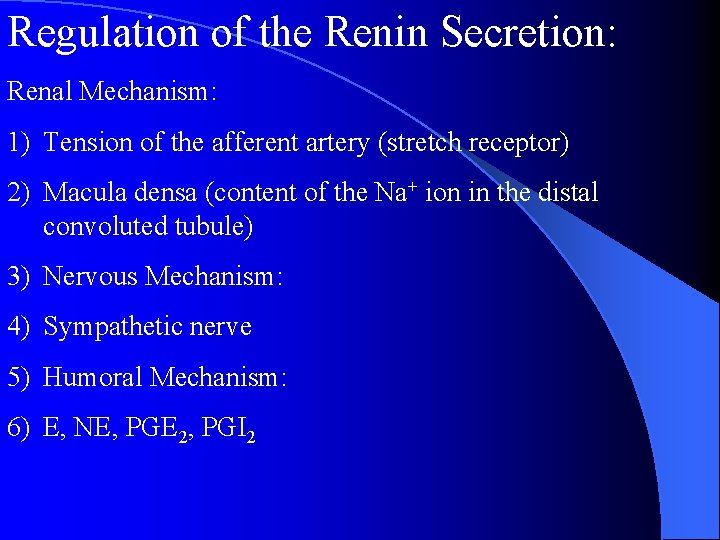
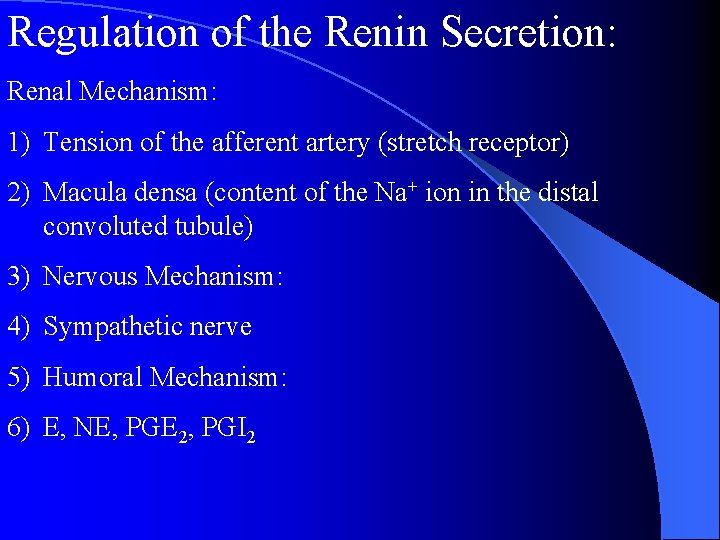
Regulation of the Renin Secretion: Renal Mechanism: 1) Tension of the afferent artery (stretch receptor) 2) Macula densa (content of the Na+ ion in the distal convoluted tubule) 3) Nervous Mechanism: 4) Sympathetic nerve 5) Humoral Mechanism: 6) E, NE, PGE 2, PGI 2
3. Atrial natriuretic peptide (ANP) • released by atrium in response to atrial stretching due to increased blood volume • promotes increased sodium excretion (natriuresis) and water excretion (diuresis) in urine by • inhibiting Na+ and water reabsorption • inhibitiing ADH secretion
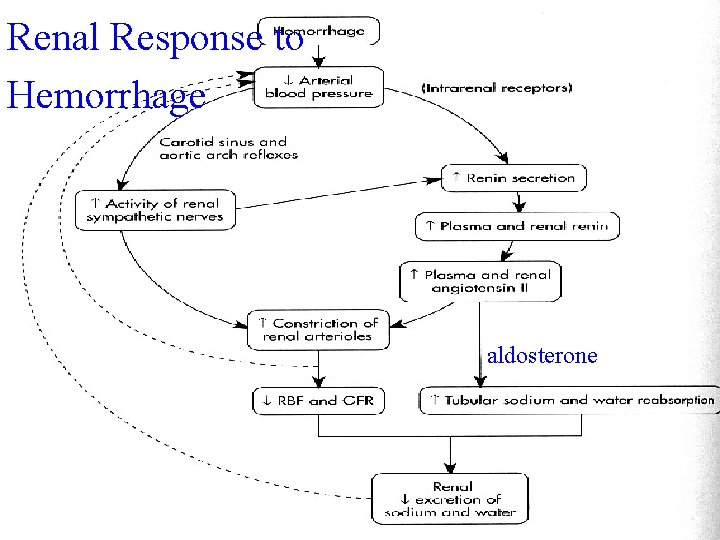
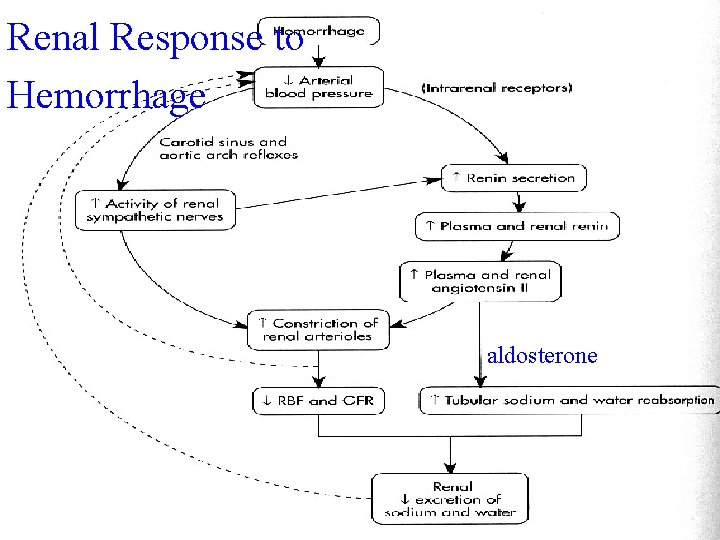
Renal Response to Hemorrhage aldosterone 2934
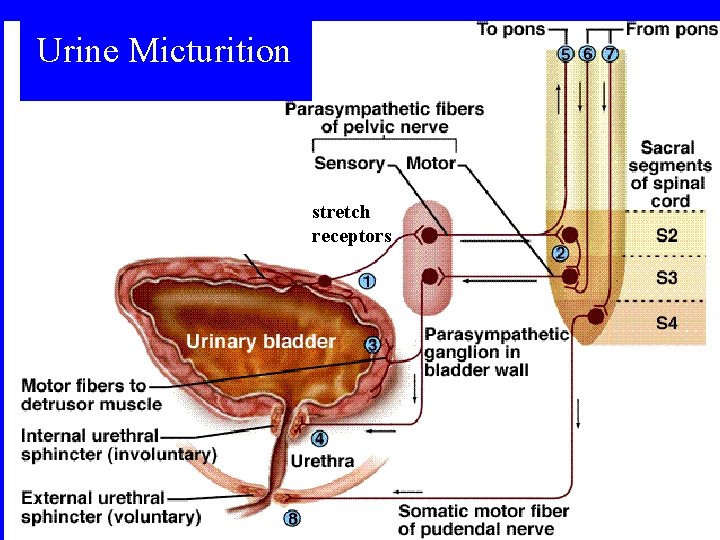
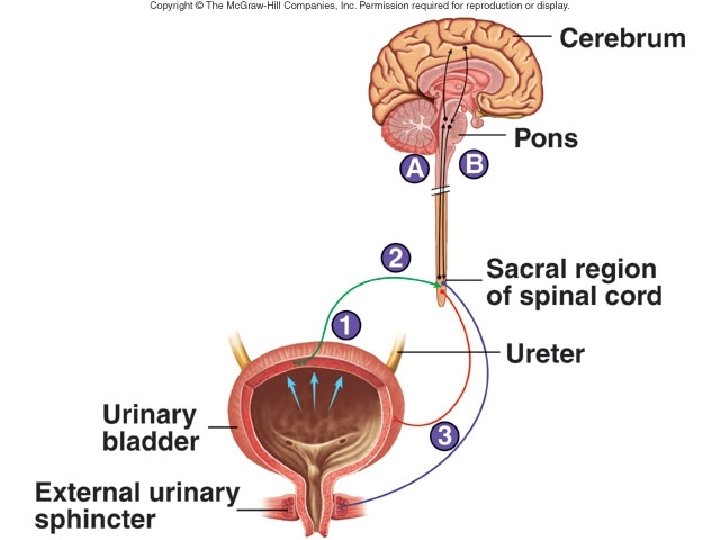
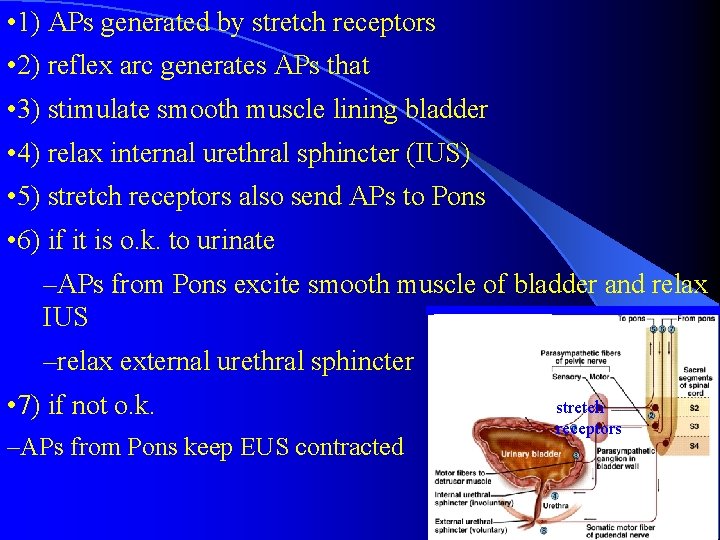
IV Micturition Once urine enters the renal pelvis, it flows through the ureters and enters the bladder, where urine is stored. Micturition is the process of emptying the urinary bladder. Two processes are involved: (1) The bladder fills progressively until the tension in its wall rises above a threshold level, and then (2) A nervous reflex called the micturition reflex occurs that empties the bladder. (3) The micturition reflex is an automatic spinal cord reflex; however, it can be inhibited or facilitated by centers in the brainstem and cerebral cortex.
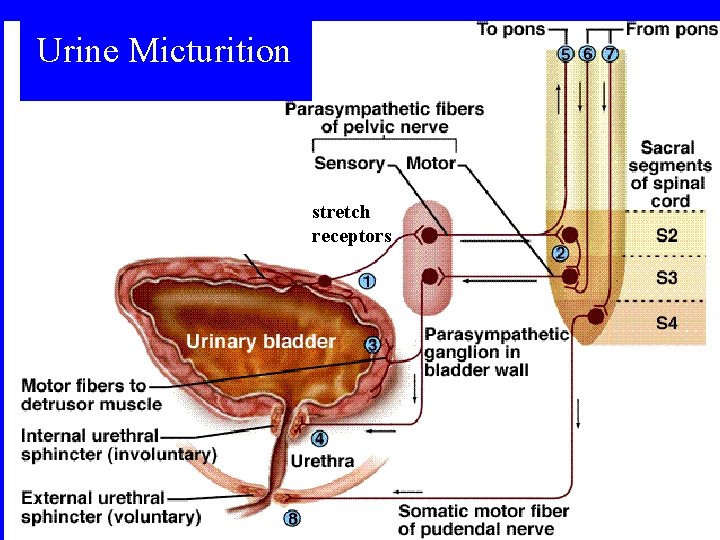
Urine Micturition stretch receptors
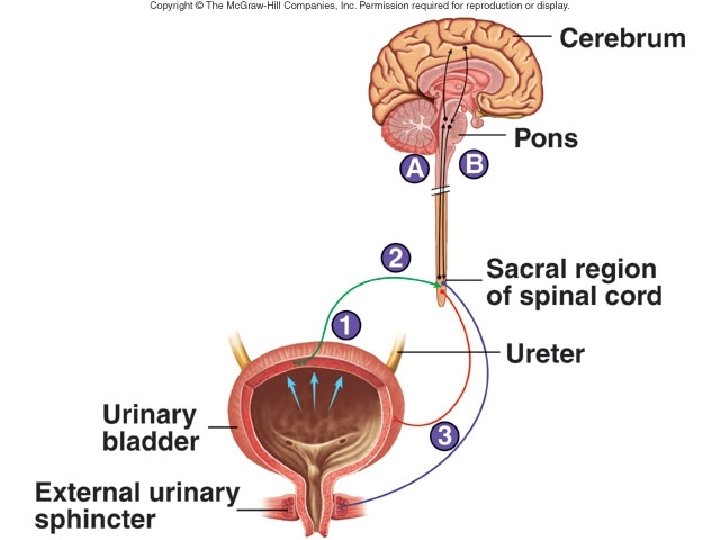
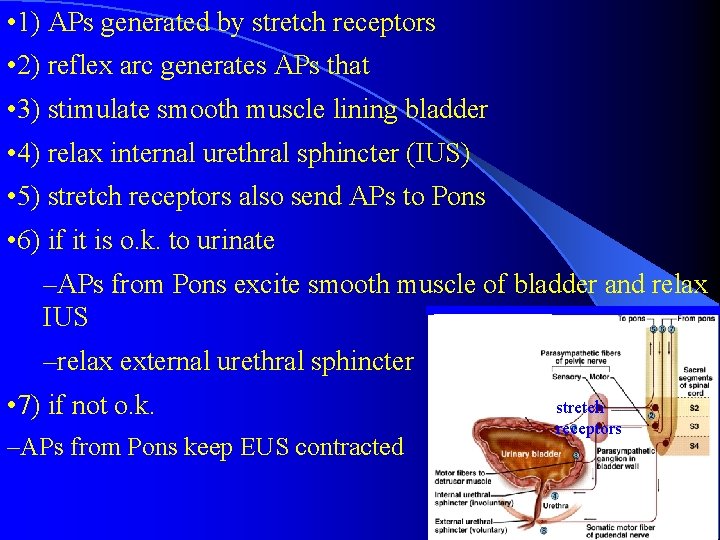
• 1) APs generated by stretch receptors • 2) reflex arc generates APs that • 3) stimulate smooth muscle lining bladder • 4) relax internal urethral sphincter (IUS) • 5) stretch receptors also send APs to Pons • 6) if it is o. k. to urinate –APs from Pons excite smooth muscle of bladder and relax IUS –relax external urethral sphincter • 7) if not o. k. –APs from Pons keep EUS contracted stretch receptors
V Changes with aging include: • • Decline in the number of functional nephrons Reduction of GFR Reduced sensitivity to ADH Problems with the micturition reflex
