CHAPTER 8 Cardiorespiratory Responses to Acute Exercise Cardiovascular
- Slides: 44
CHAPTER 8 Cardiorespiratory Responses to Acute Exercise
Cardiovascular Responses to Acute Exercise • Increases blood flow to working muscle • Involves altered heart function, peripheral circulatory adaptations – – – Heart rate Stroke volume Cardiac output Blood pressure Blood flow Blood
Cardiovascular Responses: Resting Heart Rate (RHR) • Normal ranges – Untrained RHR: 60 to 80 beats/min – Trained RHR: as low as 30 to 40 beats/min – Affected by neural tone, temperature, altitude • Anticipatory response: HR above RHR just before start of exercise – Vagal tone – Norepinephrine, epinephrine
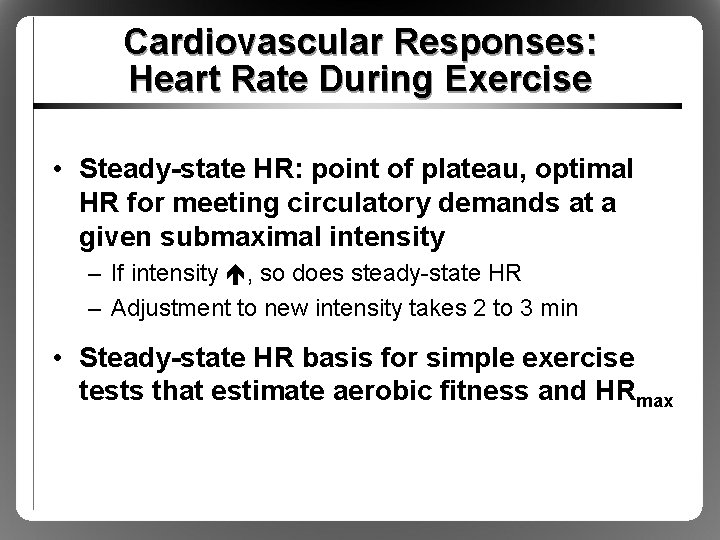
Cardiovascular Responses: Heart Rate During Exercise • Directly proportional to exercise intensity • Maximum HR (HRmax): highest HR achieved in all-out effort to volitional fatigue – – Highly reproducible Declines slightly with age Estimated HRmax = 220 – age in years Better estimated HRmax = 208 – (0. 7 x age in years)
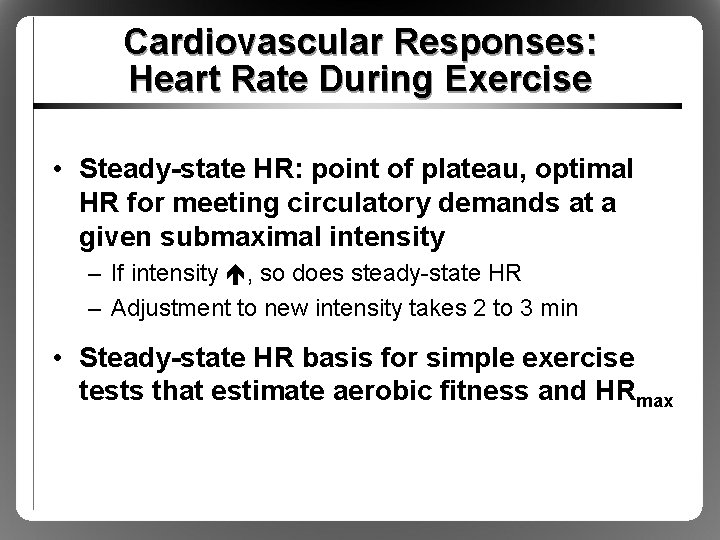
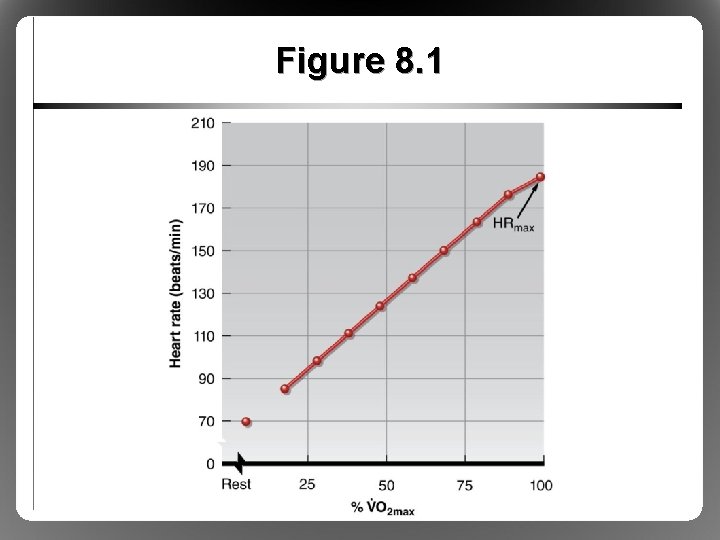
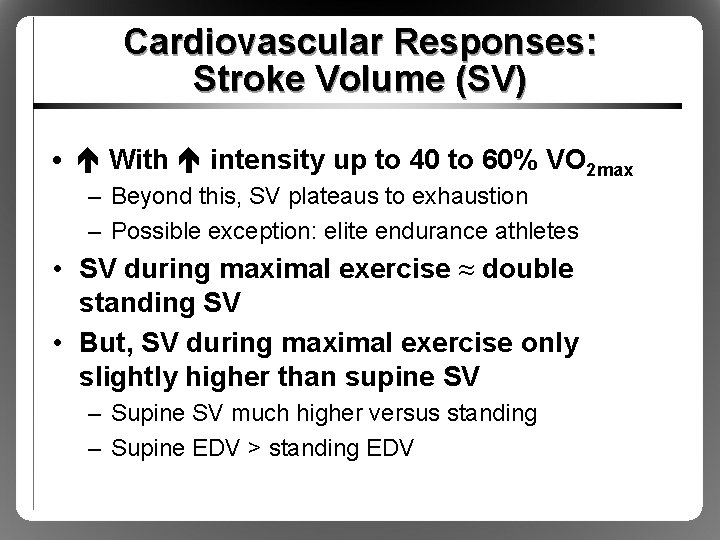
Cardiovascular Responses: Heart Rate During Exercise • Steady-state HR: point of plateau, optimal HR for meeting circulatory demands at a given submaximal intensity – If intensity , so does steady-state HR – Adjustment to new intensity takes 2 to 3 min • Steady-state HR basis for simple exercise tests that estimate aerobic fitness and HRmax
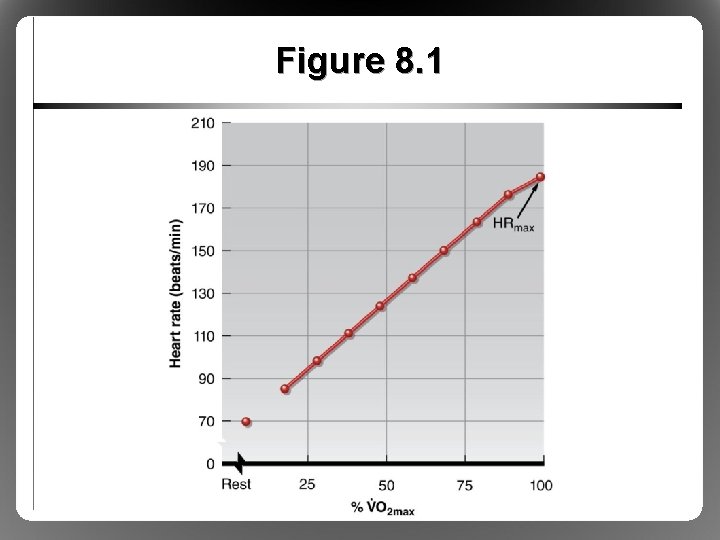
Figure 8. 1
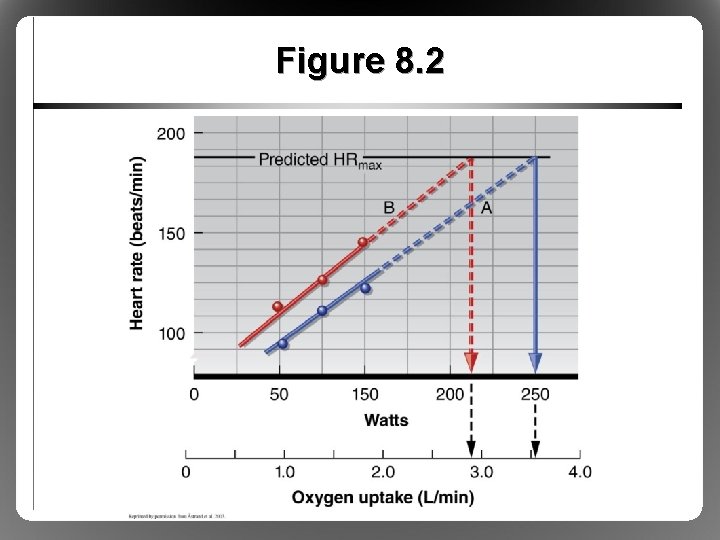
Figure 8. 2
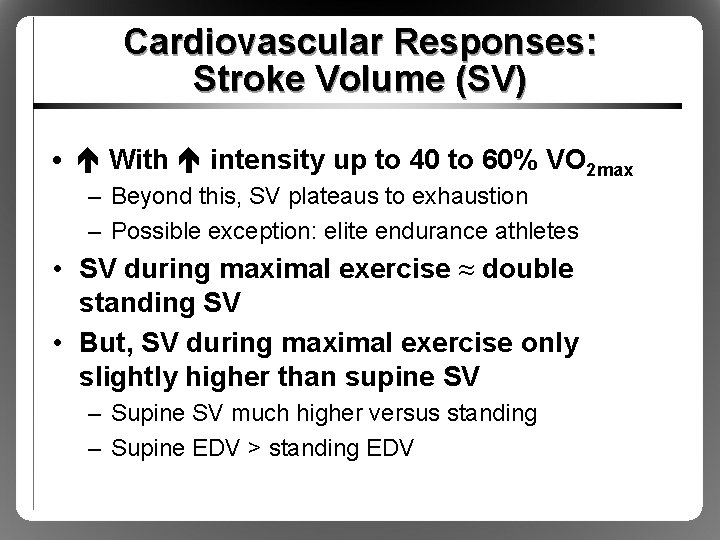
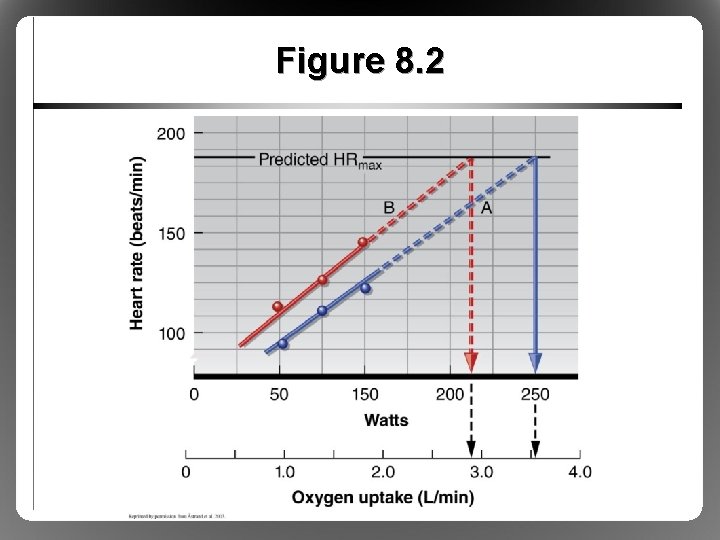
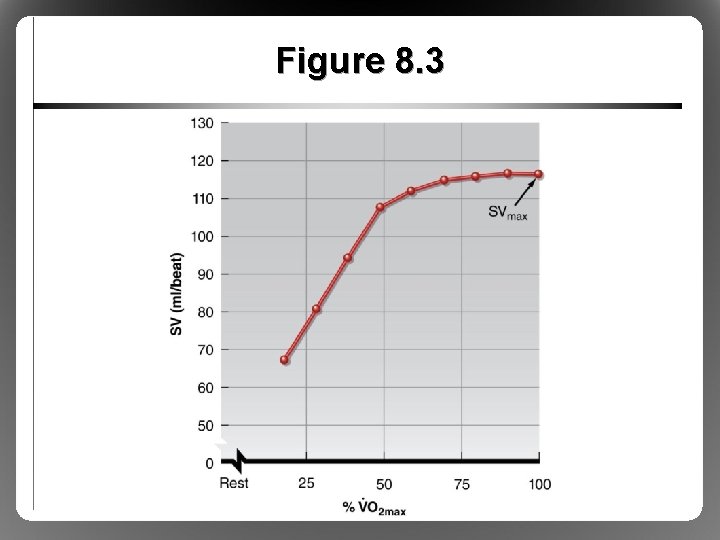
Cardiovascular Responses: Stroke Volume (SV) • With intensity up to 40 to 60% VO 2 max – Beyond this, SV plateaus to exhaustion – Possible exception: elite endurance athletes • SV during maximal exercise ≈ double standing SV • But, SV during maximal exercise only slightly higher than supine SV – Supine SV much higher versus standing – Supine EDV > standing EDV
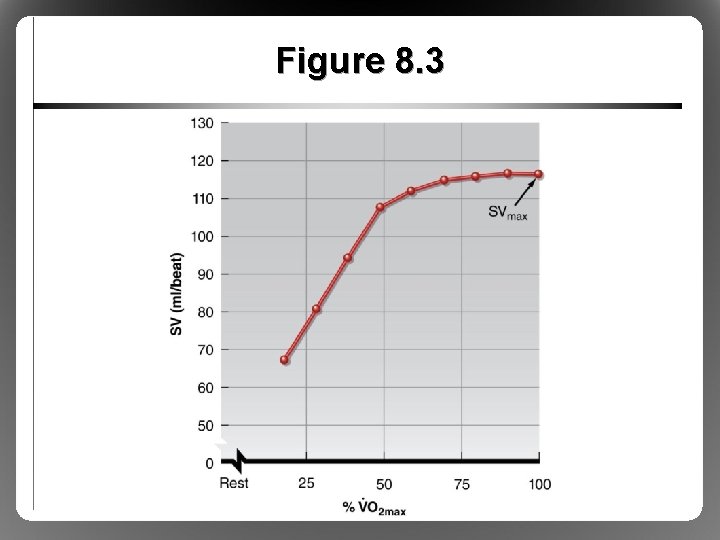
Figure 8. 3
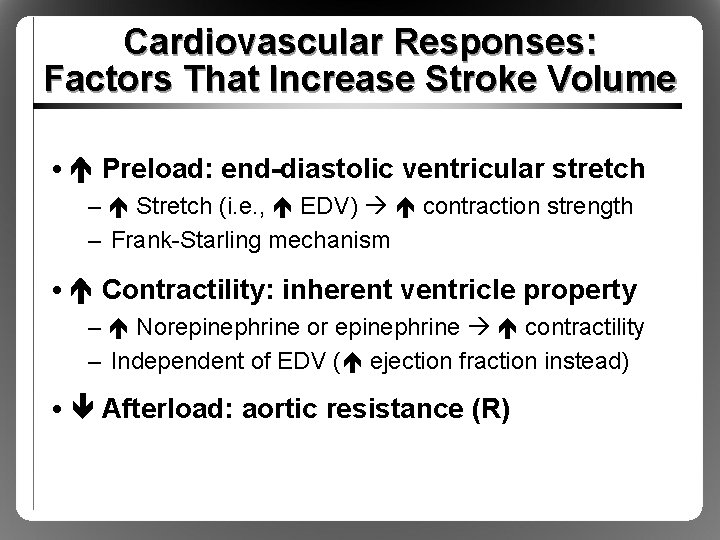
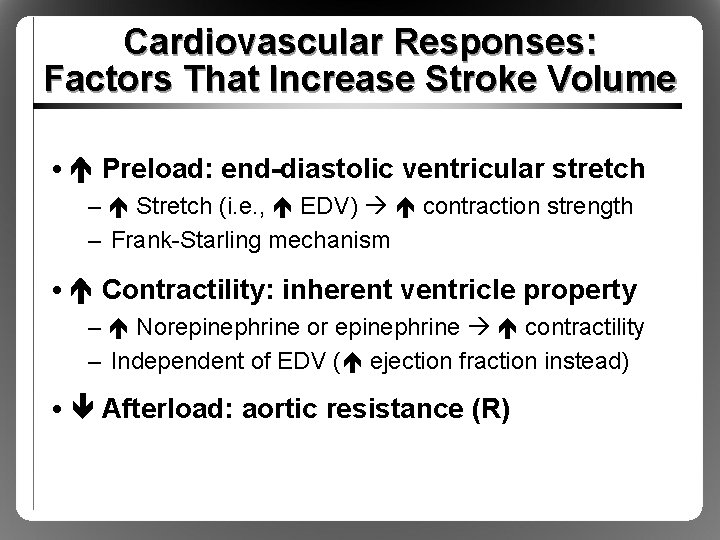
Cardiovascular Responses: Factors That Increase Stroke Volume • Preload: end-diastolic ventricular stretch – Stretch (i. e. , EDV) contraction strength – Frank-Starling mechanism • Contractility: inherent ventricle property – Norepinephrine or epinephrine contractility – Independent of EDV ( ejection fraction instead) • Afterload: aortic resistance (R)
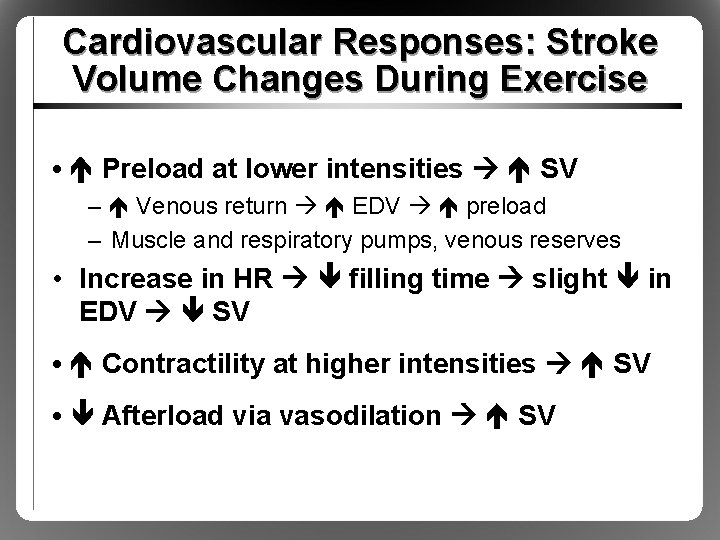
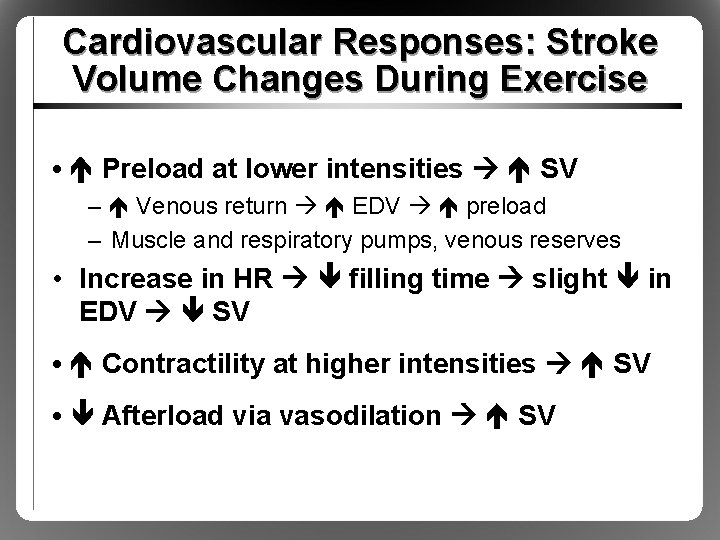
Cardiovascular Responses: Stroke Volume Changes During Exercise • Preload at lower intensities SV – Venous return EDV preload – Muscle and respiratory pumps, venous reserves • Increase in HR filling time slight in EDV SV • Contractility at higher intensities SV • Afterload via vasodilation SV
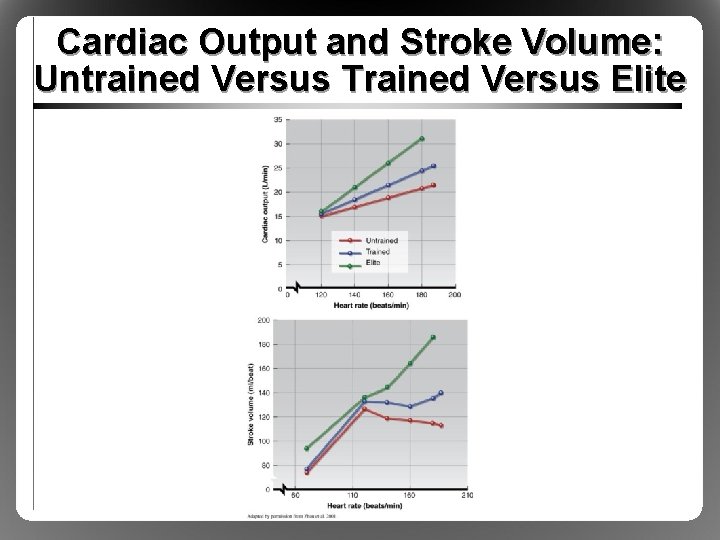
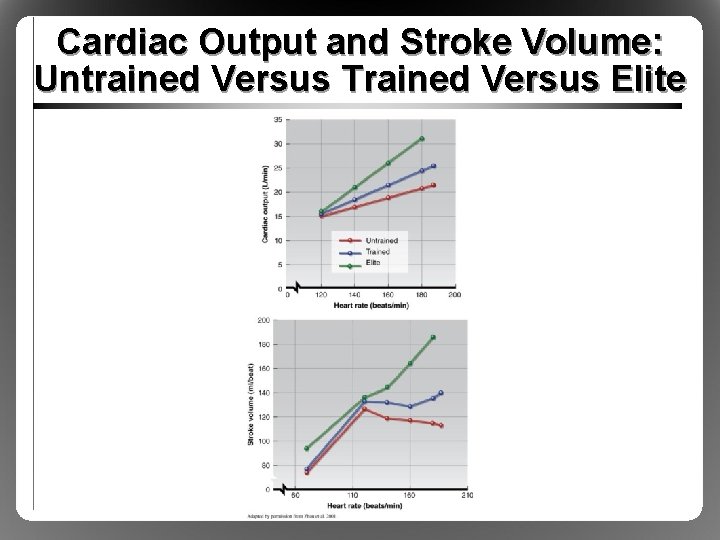
Cardiac Output and Stroke Volume: Untrained Versus Trained Versus Elite
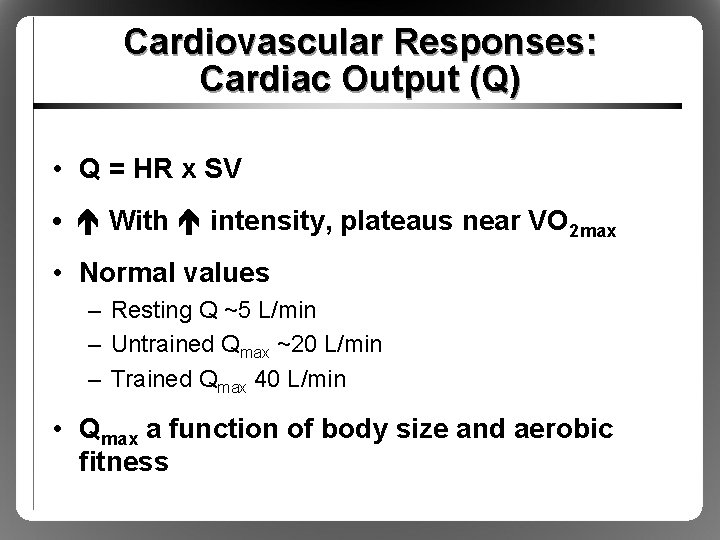
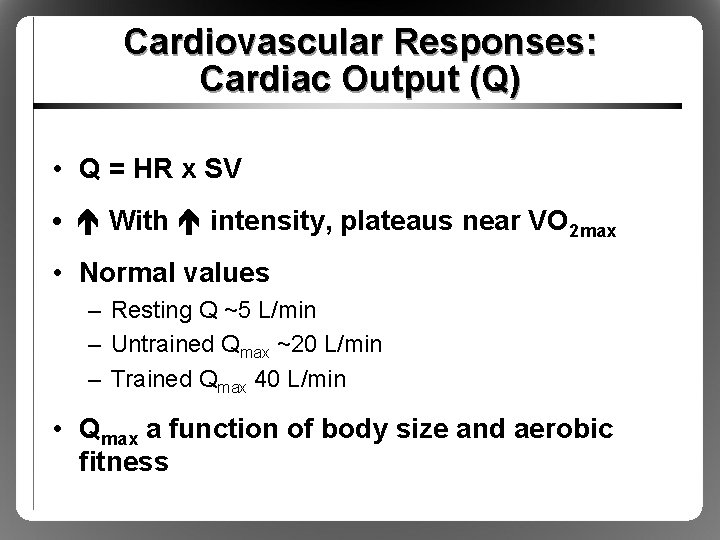
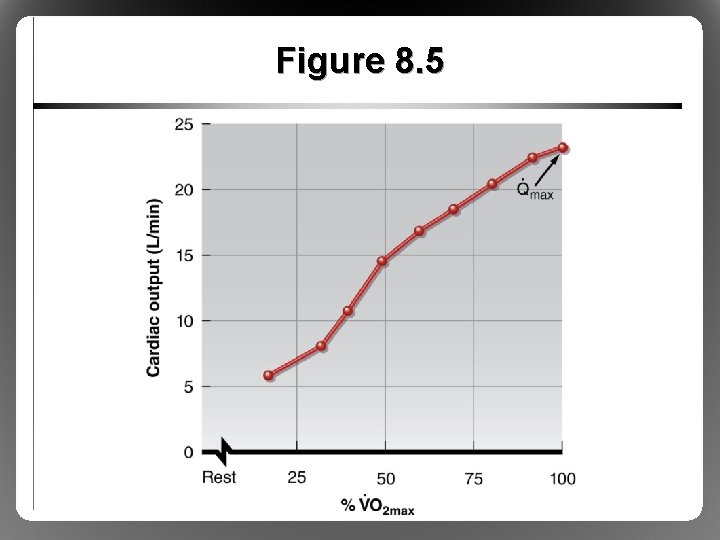
Cardiovascular Responses: Cardiac Output (Q) • Q = HR x SV • With intensity, plateaus near VO 2 max • Normal values – Resting Q ~5 L/min – Untrained Qmax ~20 L/min – Trained Qmax 40 L/min • Qmax a function of body size and aerobic fitness
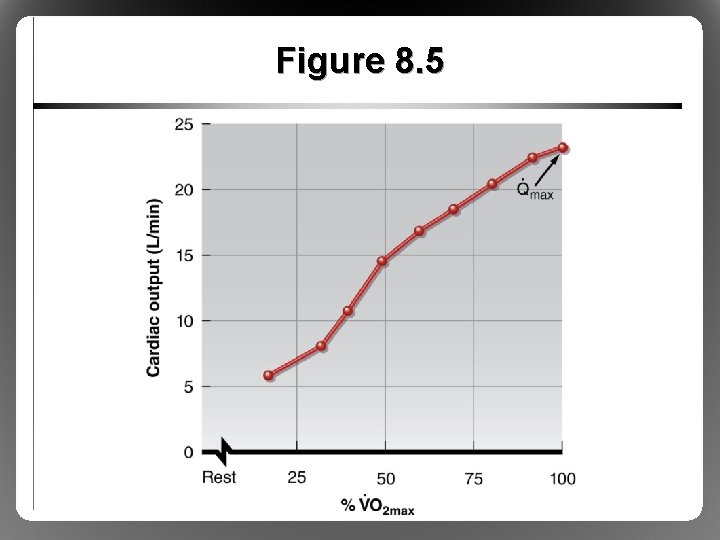
Figure 8. 5
Cardiovascular Responses: Fick Principle • Calculation of tissue O 2 consumption depends on blood flow, O 2 extraction • VO 2 = Q x (a-v)O 2 difference • VO 2 = HR x SV x (a-v)O 2 difference
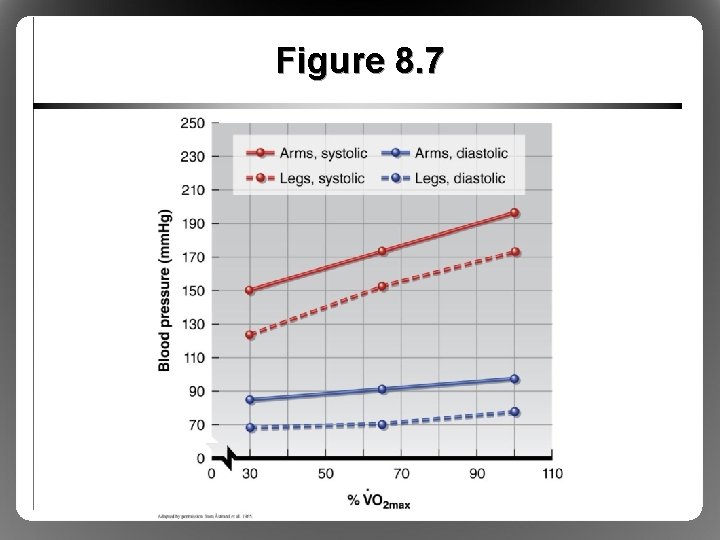
Cardiovascular Responses: Blood Pressure • During endurance exercise, mean arterial pressure (MAP) increases – Systolic BP proportional to exercise intensity – Diastolic BP slight or slight (at max exercise) • MAP = Q x total peripheral resistance (TPR) – Q , TPR slightly – Muscle vasodilation versus sympatholysis
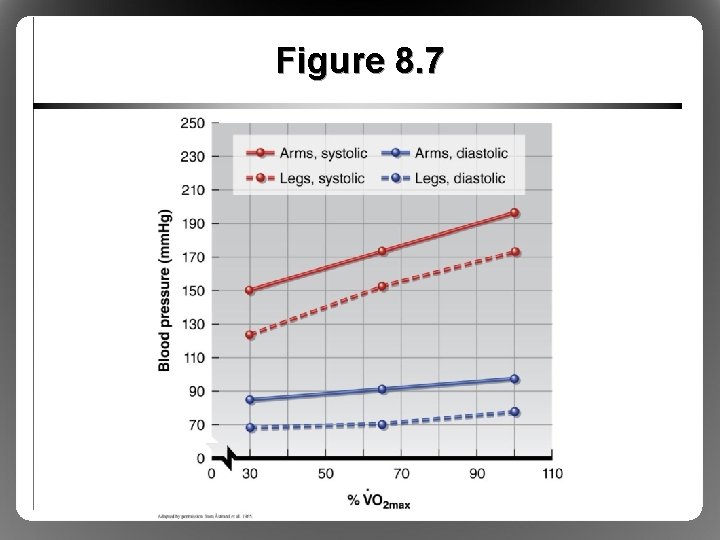
Figure 8. 7
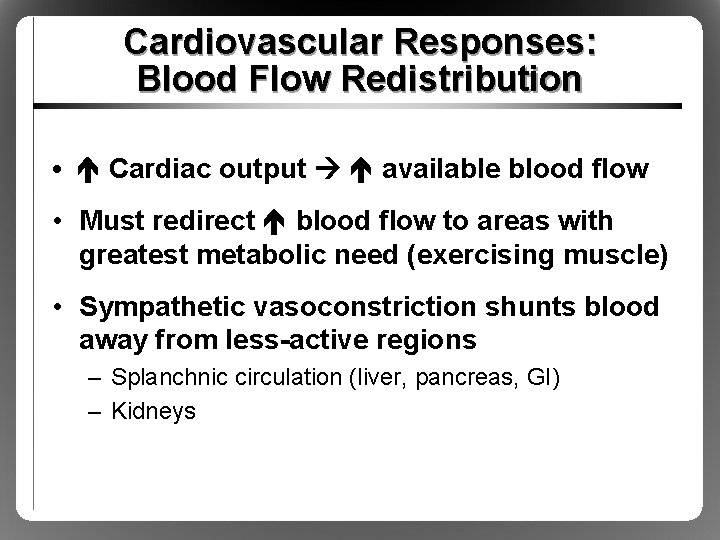
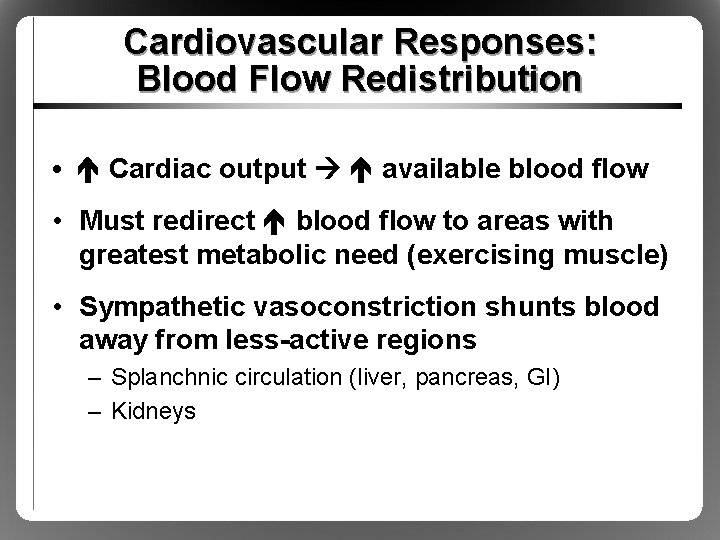
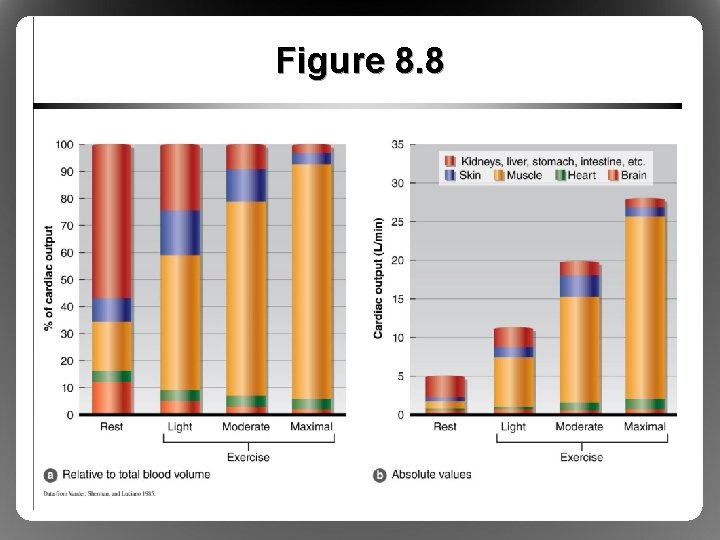
Cardiovascular Responses: Blood Flow Redistribution • Cardiac output available blood flow • Must redirect blood flow to areas with greatest metabolic need (exercising muscle) • Sympathetic vasoconstriction shunts blood away from less-active regions – Splanchnic circulation (liver, pancreas, GI) – Kidneys
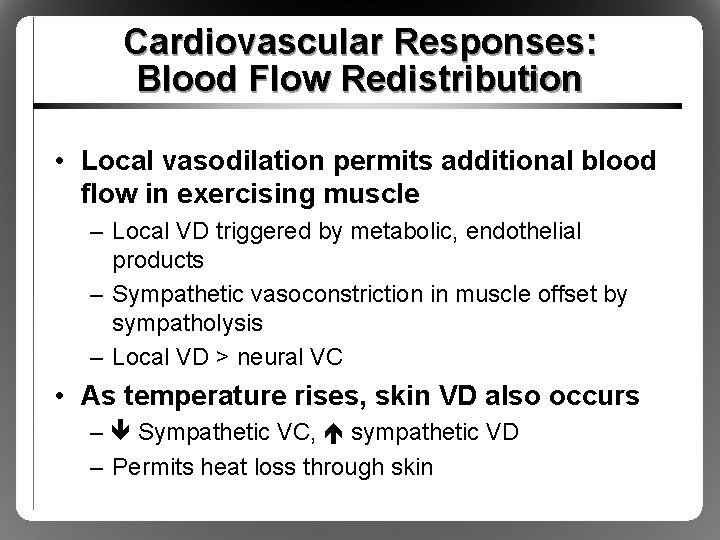
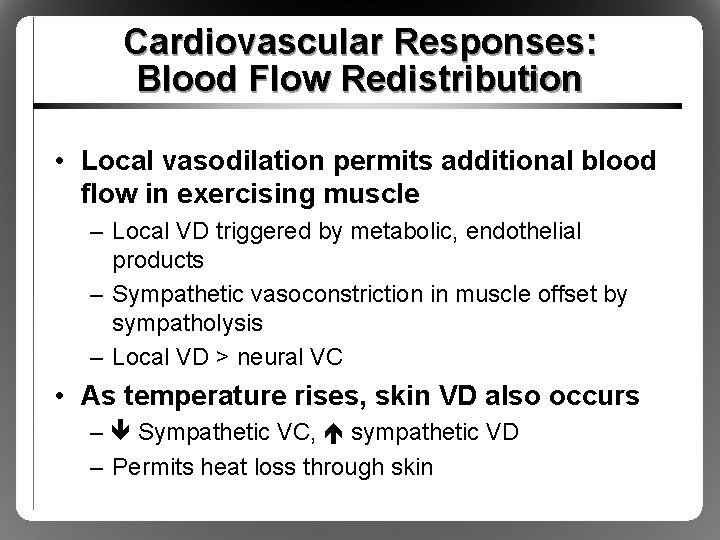
Cardiovascular Responses: Blood Flow Redistribution • Local vasodilation permits additional blood flow in exercising muscle – Local VD triggered by metabolic, endothelial products – Sympathetic vasoconstriction in muscle offset by sympatholysis – Local VD > neural VC • As temperature rises, skin VD also occurs – Sympathetic VC, sympathetic VD – Permits heat loss through skin
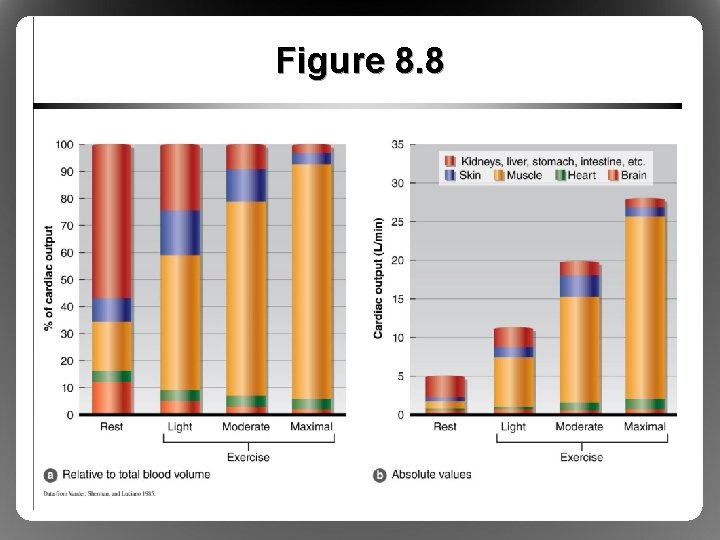
Figure 8. 8
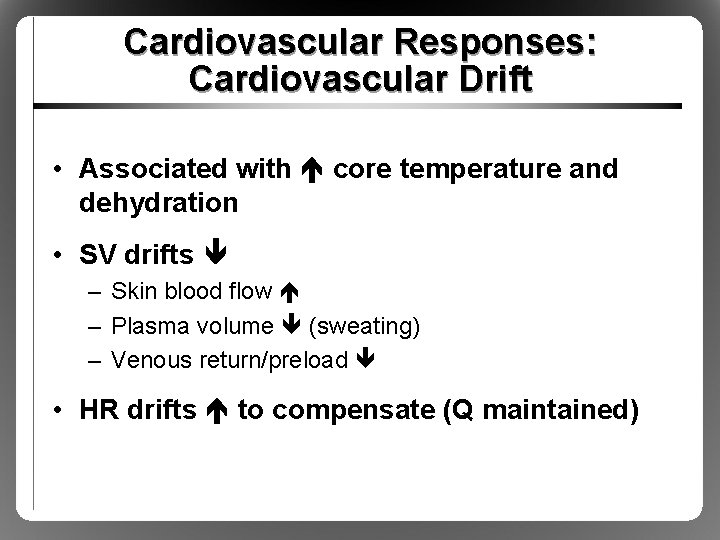
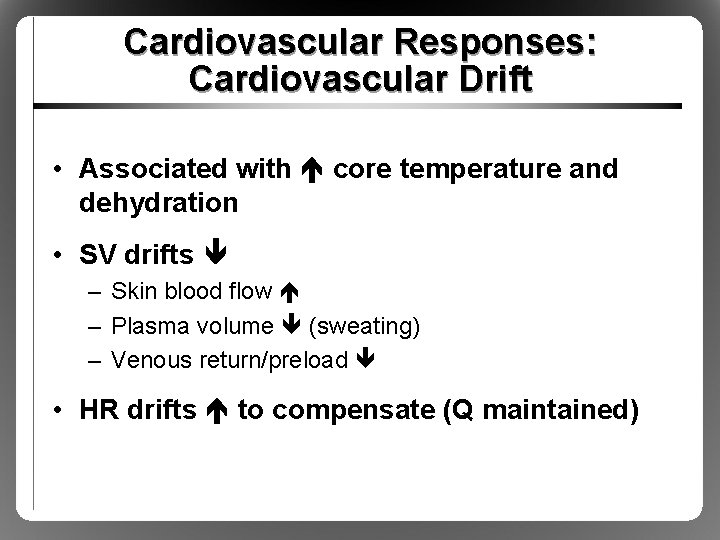
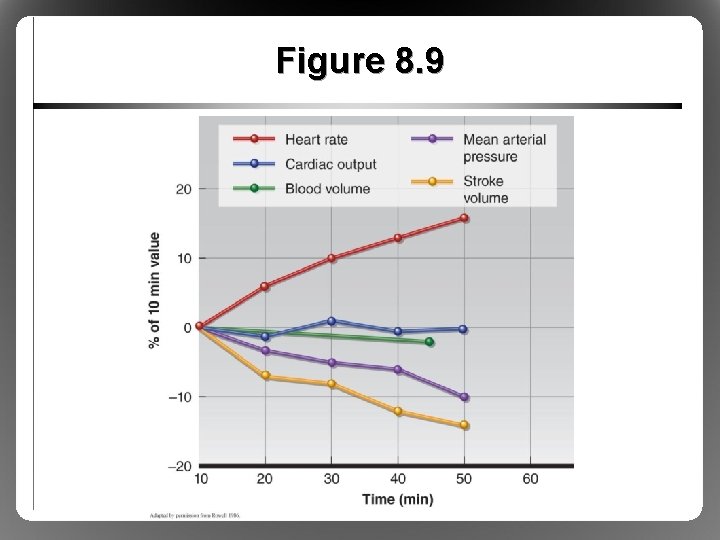
Cardiovascular Responses: Cardiovascular Drift • Associated with core temperature and dehydration • SV drifts – Skin blood flow – Plasma volume (sweating) – Venous return/preload • HR drifts to compensate (Q maintained)
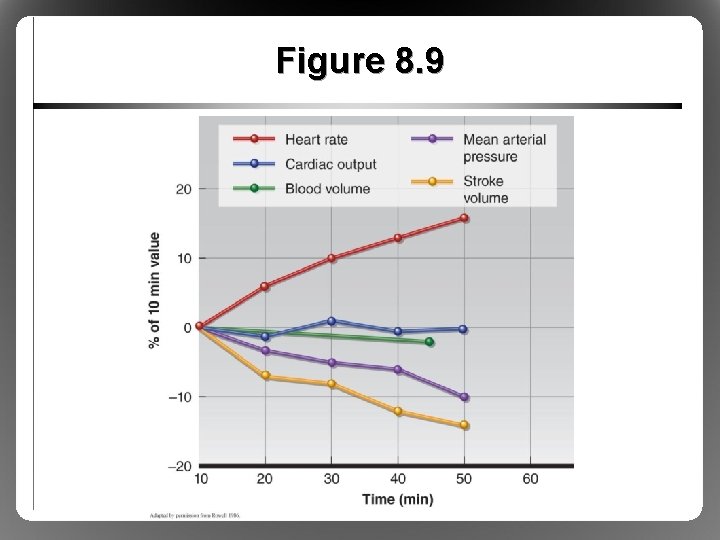
Figure 8. 9
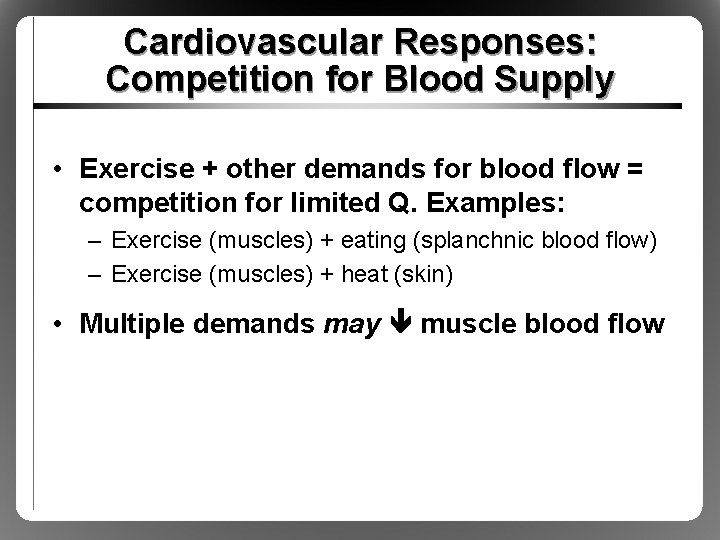
Cardiovascular Responses: Competition for Blood Supply • Exercise + other demands for blood flow = competition for limited Q. Examples: – Exercise (muscles) + eating (splanchnic blood flow) – Exercise (muscles) + heat (skin) • Multiple demands may muscle blood flow
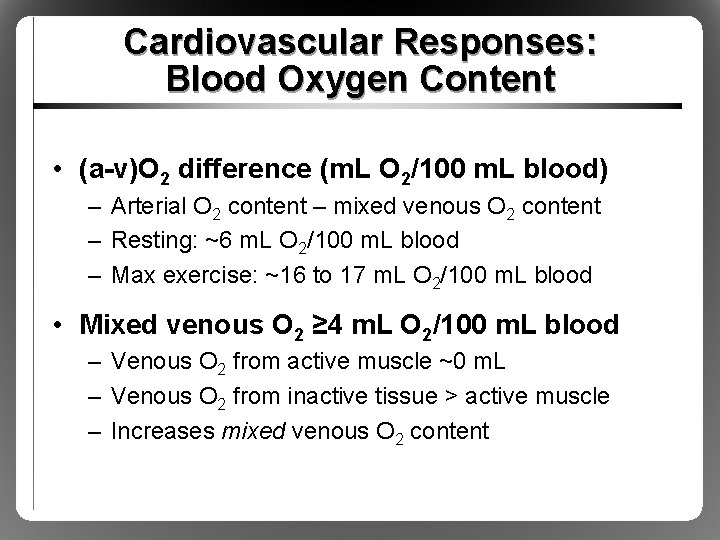
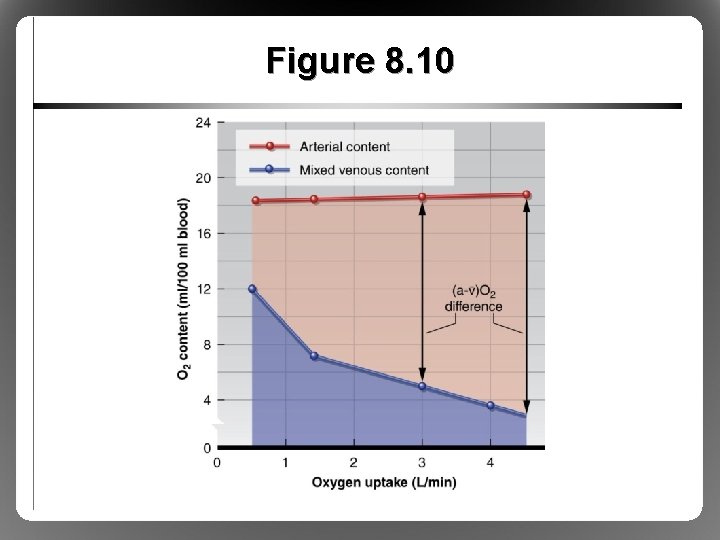
Cardiovascular Responses: Blood Oxygen Content • (a-v)O 2 difference (m. L O 2/100 m. L blood) – Arterial O 2 content – mixed venous O 2 content – Resting: ~6 m. L O 2/100 m. L blood – Max exercise: ~16 to 17 m. L O 2/100 m. L blood • Mixed venous O 2 ≥ 4 m. L O 2/100 m. L blood – Venous O 2 from active muscle ~0 m. L – Venous O 2 from inactive tissue > active muscle – Increases mixed venous O 2 content
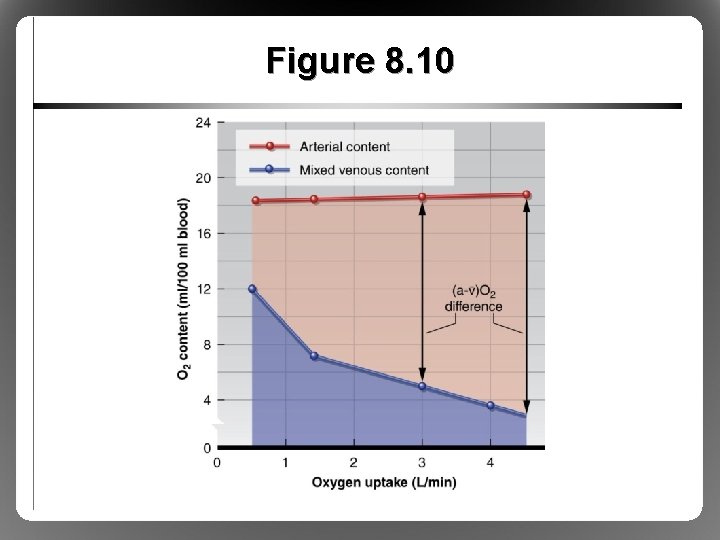
Figure 8. 10
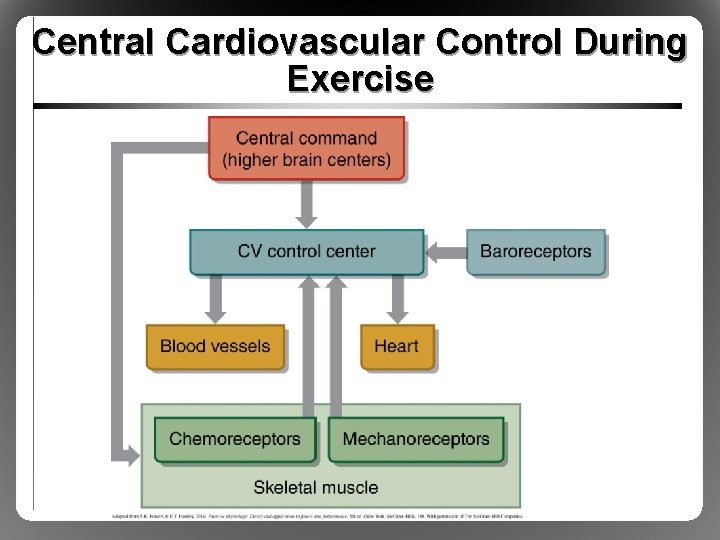
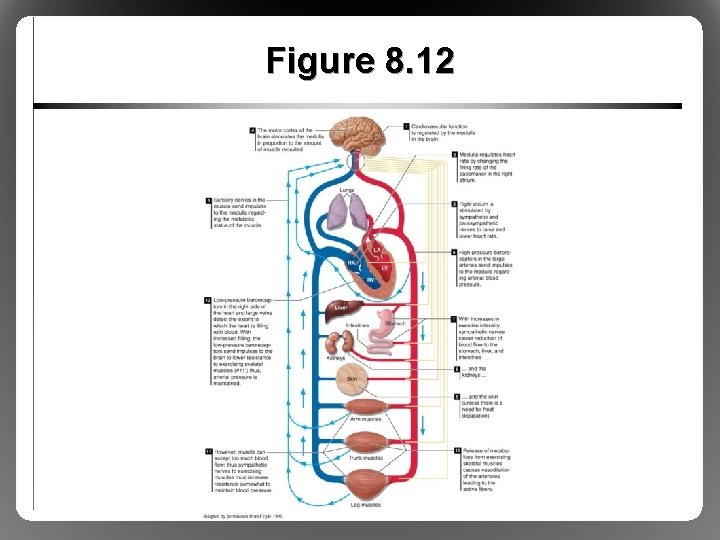
Central Regulation of Cardiovascular Responses • What stimulates rapid changes in HR, Q, and blood pressure during exercise? – Precede metabolite buildup in muscle – HR increases within 1 s of onset of exercise • Central command – Higher brain centers – Coactivates motor and cardiovascular centers
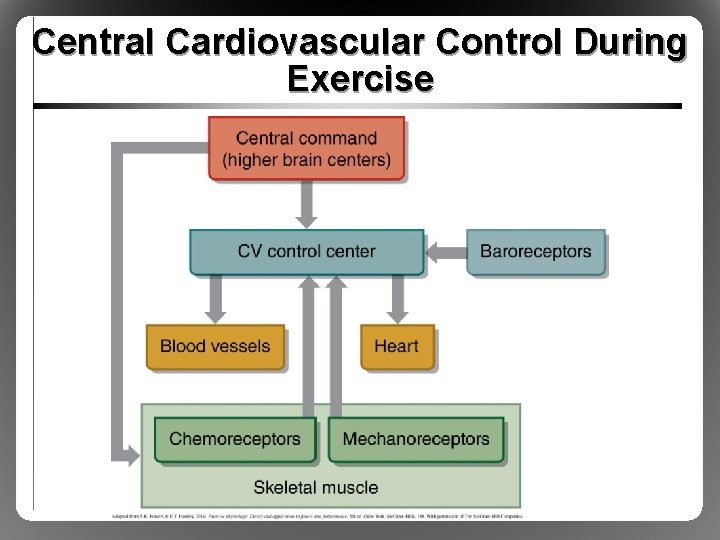
Central Cardiovascular Control During Exercise
Cardiovascular Responses: Integration of Exercise Response • Cardiovascular responses to exercise complex, fast, and finely tuned • First priority: maintenance of blood pressure – Blood flow can be maintained only as long as BP remains stable – Prioritized before other needs (exercise, thermoregulatory, etc. )
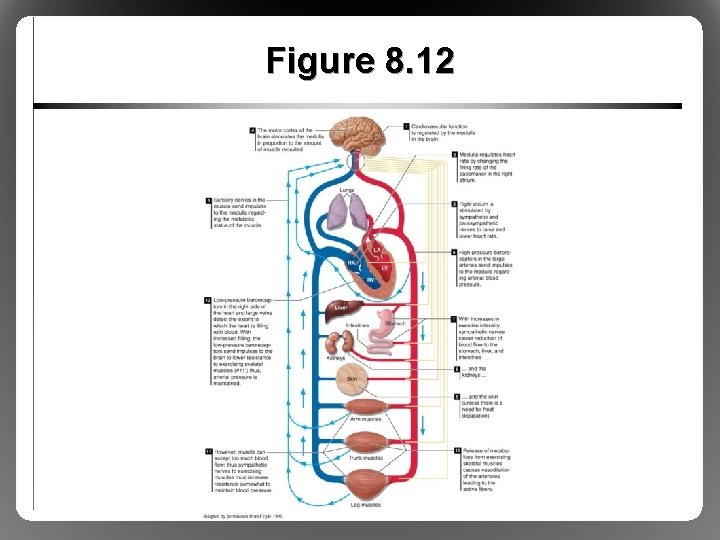
Figure 8. 12
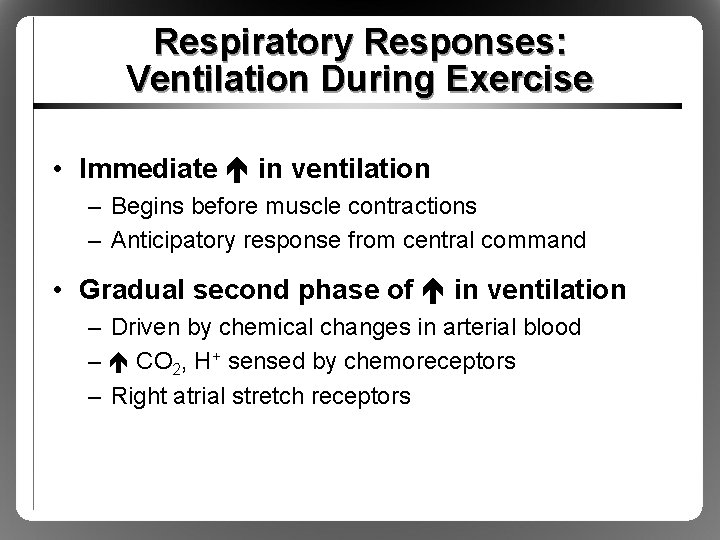
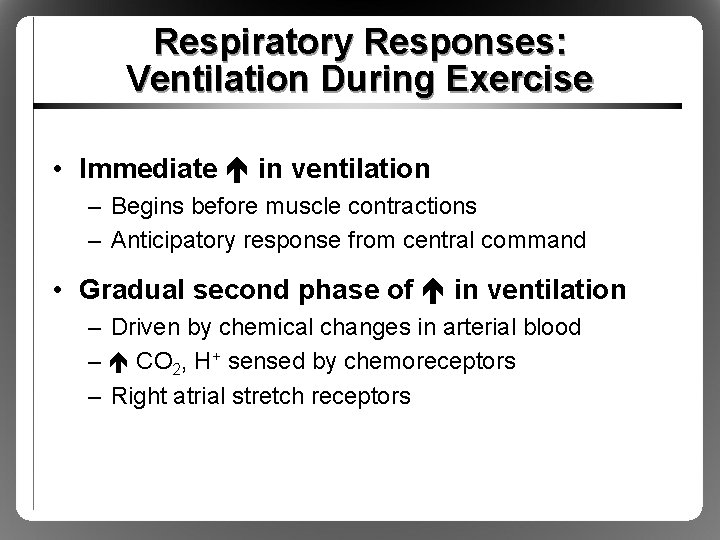
Respiratory Responses: Ventilation During Exercise • Immediate in ventilation – Begins before muscle contractions – Anticipatory response from central command • Gradual second phase of in ventilation – Driven by chemical changes in arterial blood – CO 2, H+ sensed by chemoreceptors – Right atrial stretch receptors
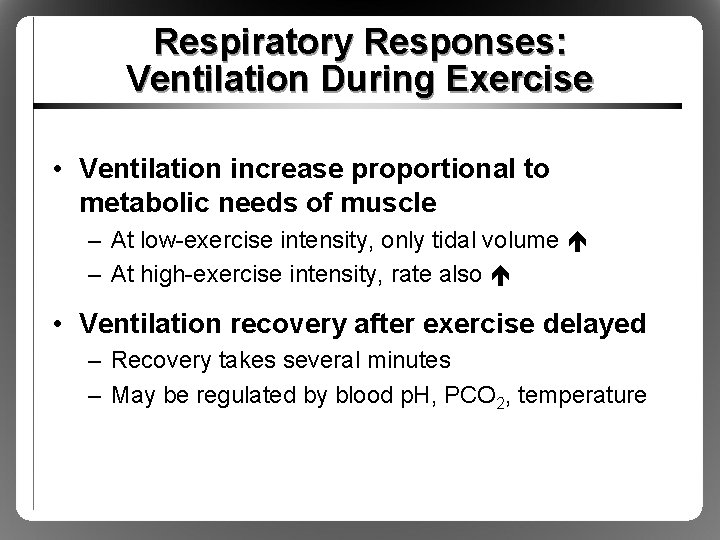
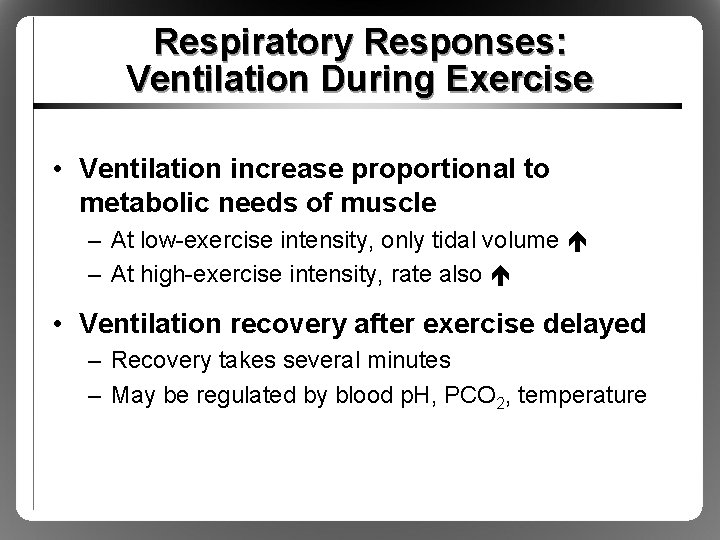
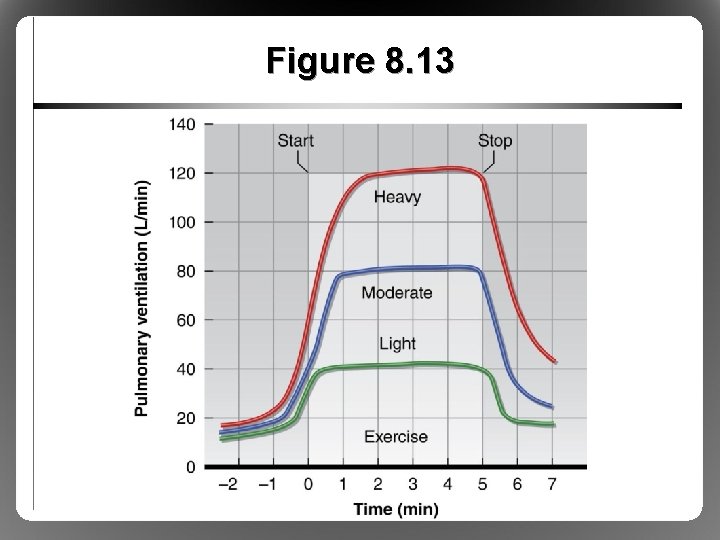
Respiratory Responses: Ventilation During Exercise • Ventilation increase proportional to metabolic needs of muscle – At low-exercise intensity, only tidal volume – At high-exercise intensity, rate also • Ventilation recovery after exercise delayed – Recovery takes several minutes – May be regulated by blood p. H, PCO 2, temperature
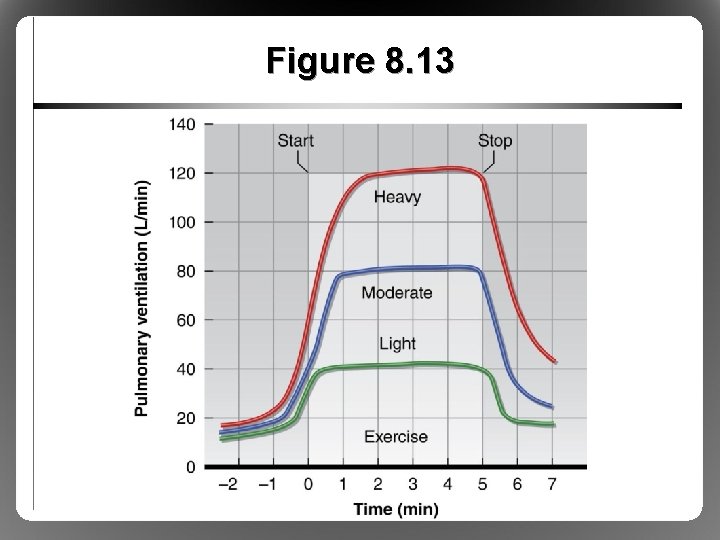
Figure 8. 13
Respiratory Responses: Breathing Irregularities • Valsalva maneuver: potentially dangerous but accompanies certain types of exercise – Close glottis – Intra-abdominal P (bearing down) – Intrathoracic P (contracting breathing muscles) • High pressures collapse great veins venous return Q arterial blood pressure
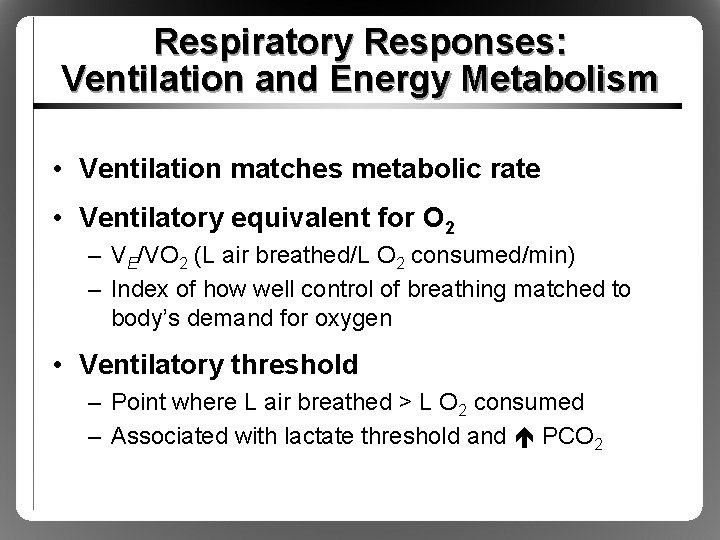
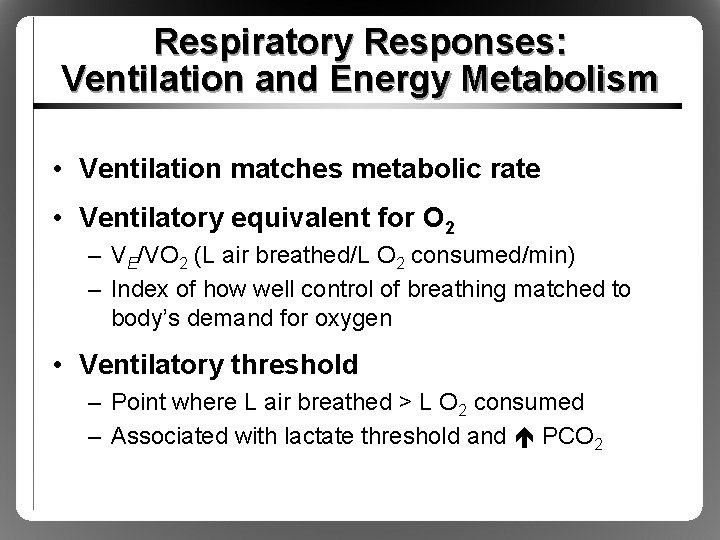
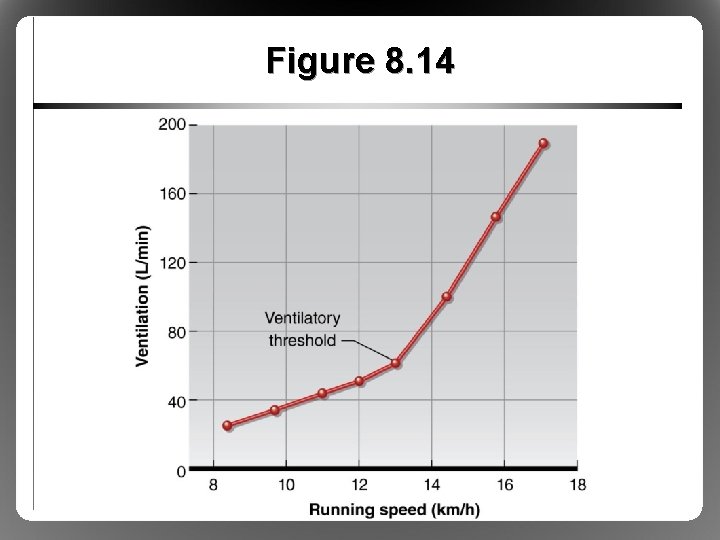
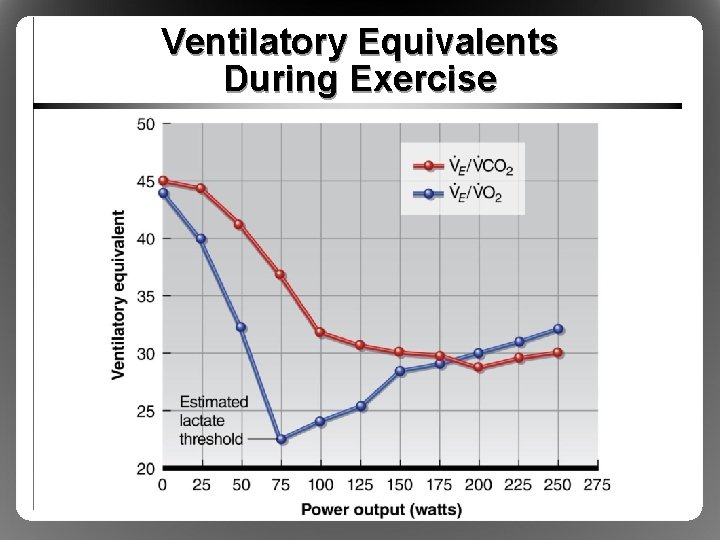
Respiratory Responses: Ventilation and Energy Metabolism • Ventilation matches metabolic rate • Ventilatory equivalent for O 2 – VE/VO 2 (L air breathed/L O 2 consumed/min) – Index of how well control of breathing matched to body’s demand for oxygen • Ventilatory threshold – Point where L air breathed > L O 2 consumed – Associated with lactate threshold and PCO 2
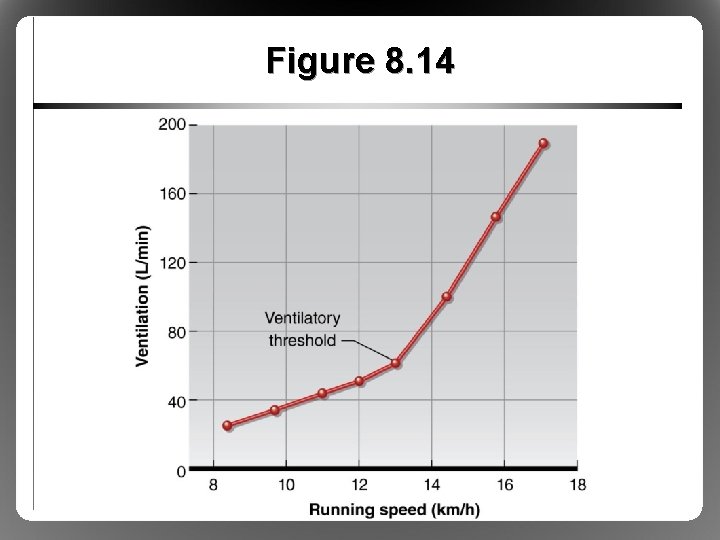
Figure 8. 14
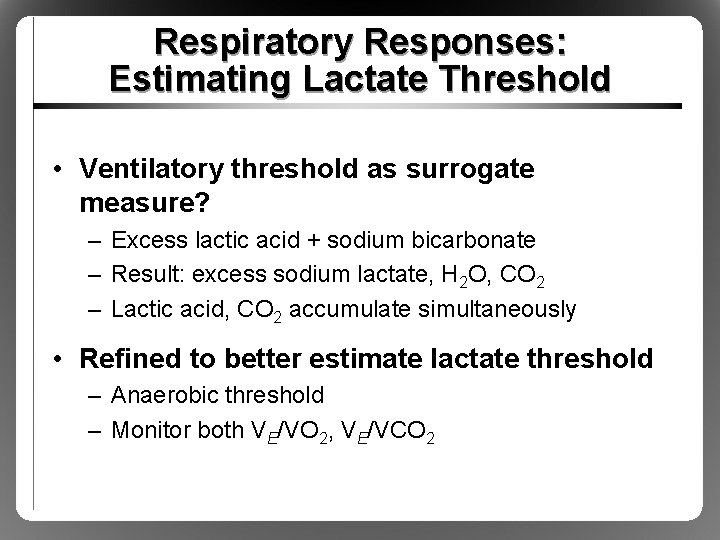
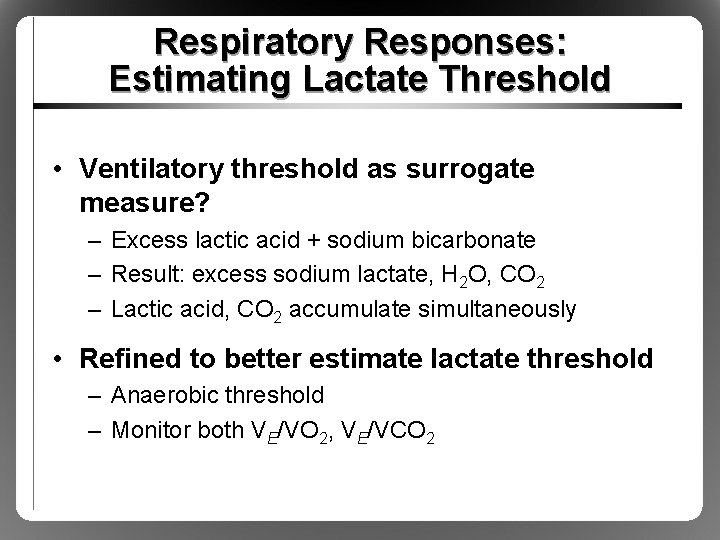
Respiratory Responses: Estimating Lactate Threshold • Ventilatory threshold as surrogate measure? – Excess lactic acid + sodium bicarbonate – Result: excess sodium lactate, H 2 O, CO 2 – Lactic acid, CO 2 accumulate simultaneously • Refined to better estimate lactate threshold – Anaerobic threshold – Monitor both VE/VO 2, VE/VCO 2
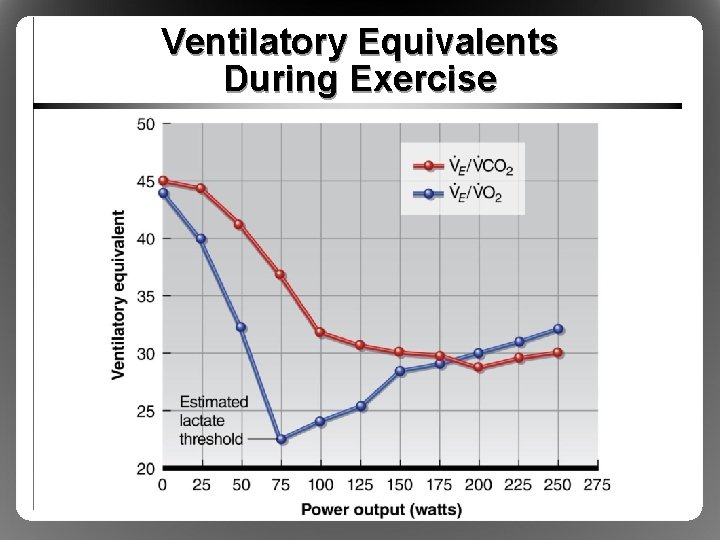
Ventilatory Equivalents During Exercise
Respiratory Responses: Limitations to Performance • Ventilation normally not limiting factor – Respiratory muscles account for 10% of VO 2, 15% of Q during heavy exercise – Respiratory muscles very fatigue resistant • Airway resistance and gas diffusion normally not limiting factors at sea level • Restrictive or obstructive respiratory disorders can be limiting
Respiratory Responses: Limitations to Performance • Exception: elite endurance-trained athletes exercising at high intensities – Ventilation may be limiting – Ventilation-perfusion mismatch – Exercise-induced arterial hypoxemia (EIAH)
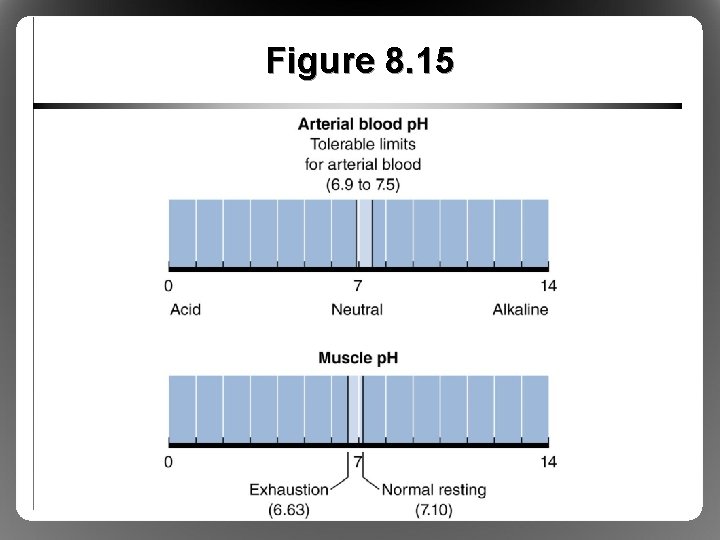
Respiratory Responses: Acid-Base Balance • Metabolic processes produce H+ p. H • H+ + buffer H-buffer • At rest, body slightly alkaline – 7. 1 to 7. 4 – Higher p. H = Alkalosis • During exercise, body slightly acidic – 6. 6 to 6. 9 – Lower p. H = Acidosis
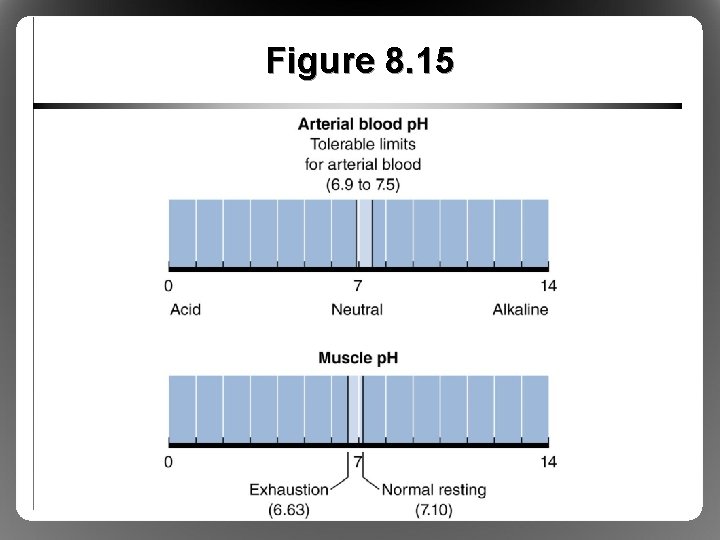
Figure 8. 15
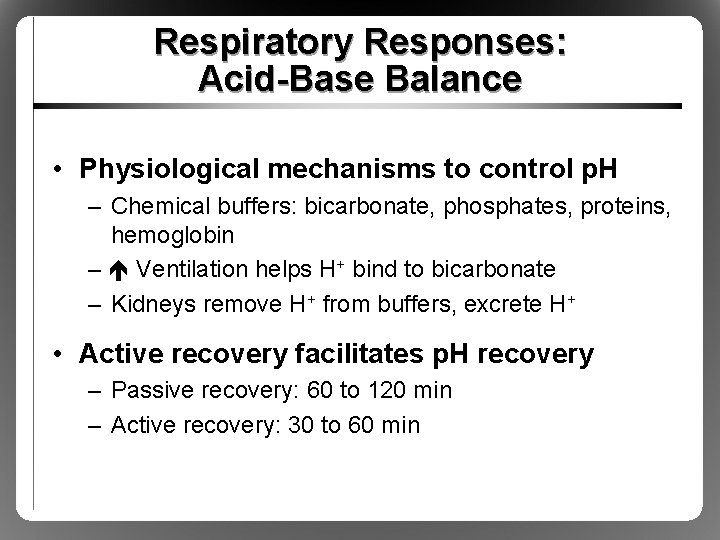
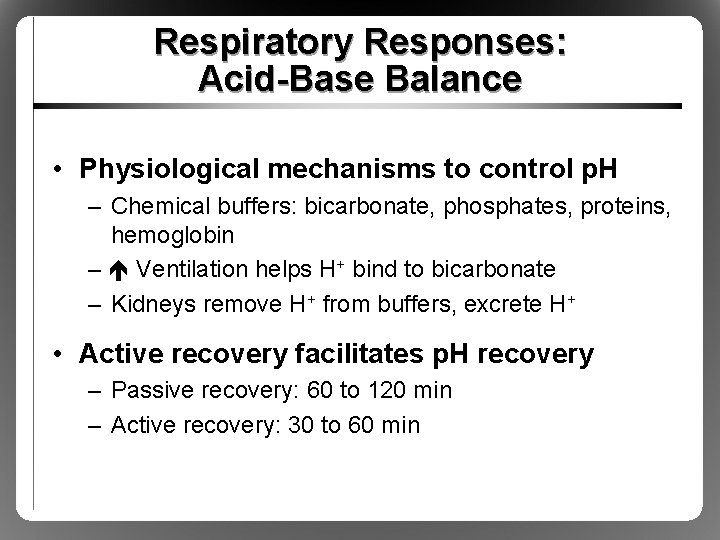
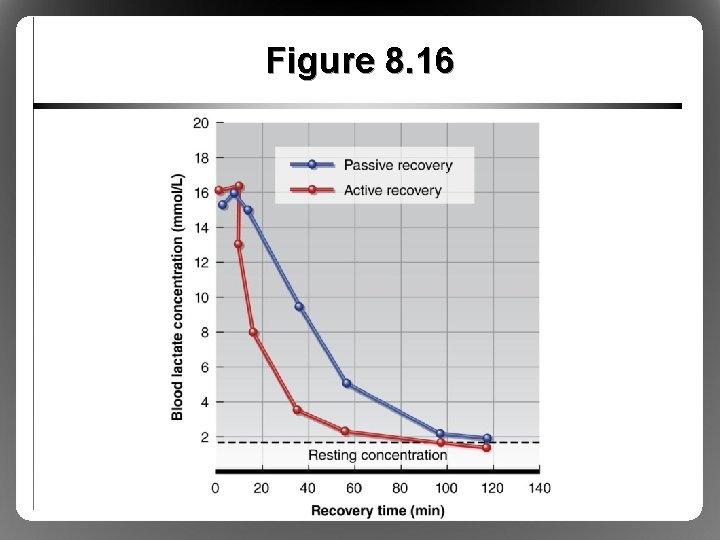
Respiratory Responses: Acid-Base Balance • Physiological mechanisms to control p. H – Chemical buffers: bicarbonate, phosphates, proteins, hemoglobin – Ventilation helps H+ bind to bicarbonate – Kidneys remove H+ from buffers, excrete H+ • Active recovery facilitates p. H recovery – Passive recovery: 60 to 120 min – Active recovery: 30 to 60 min
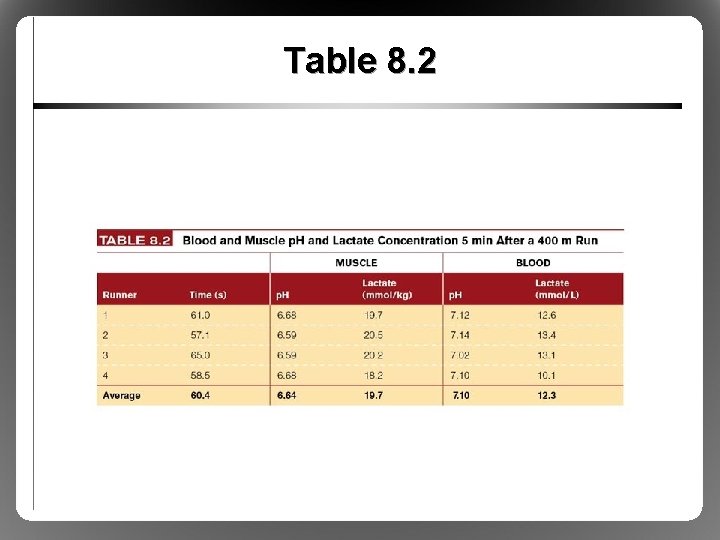
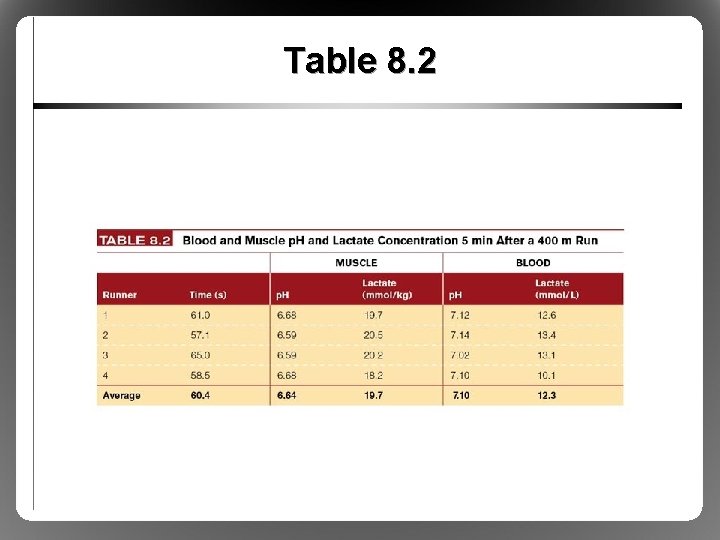
Table 8. 2
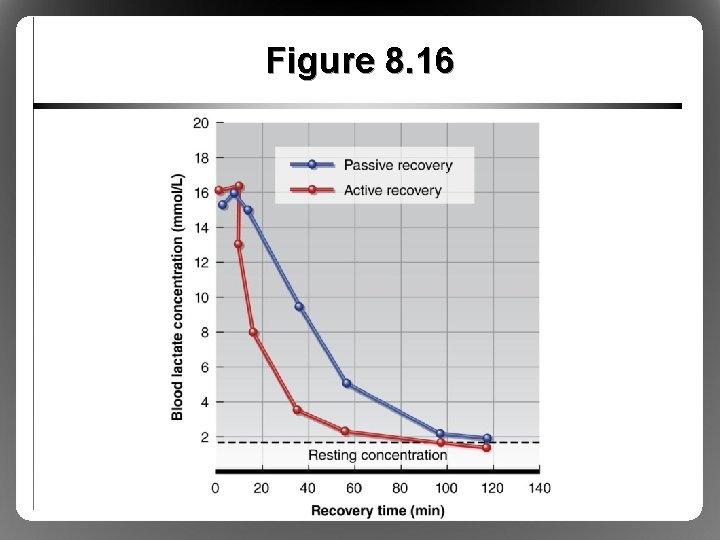
Figure 8. 16