Chapter 7 The Respiratory System Meet The Lungs
- Slides: 38
Chapter 7 The Respiratory System
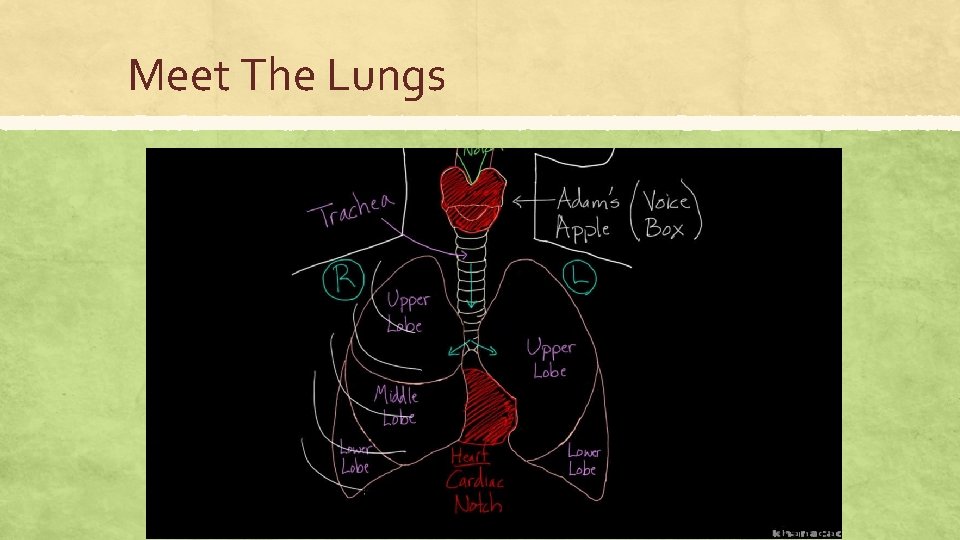
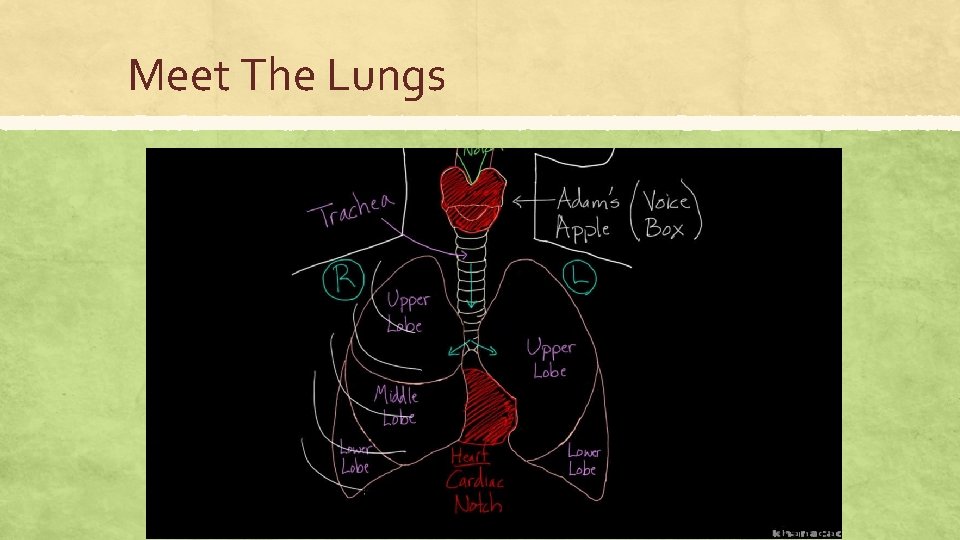
Meet The Lungs
The Respiratory System
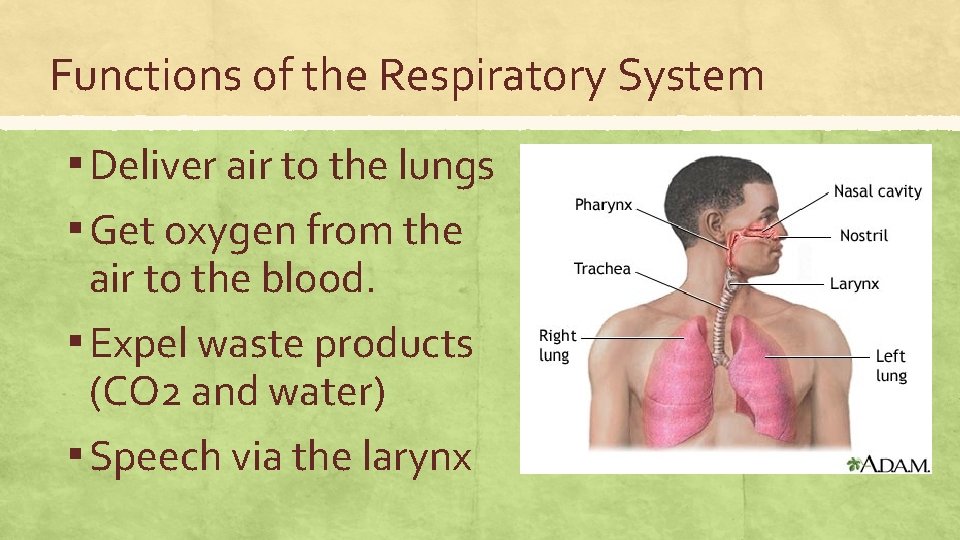
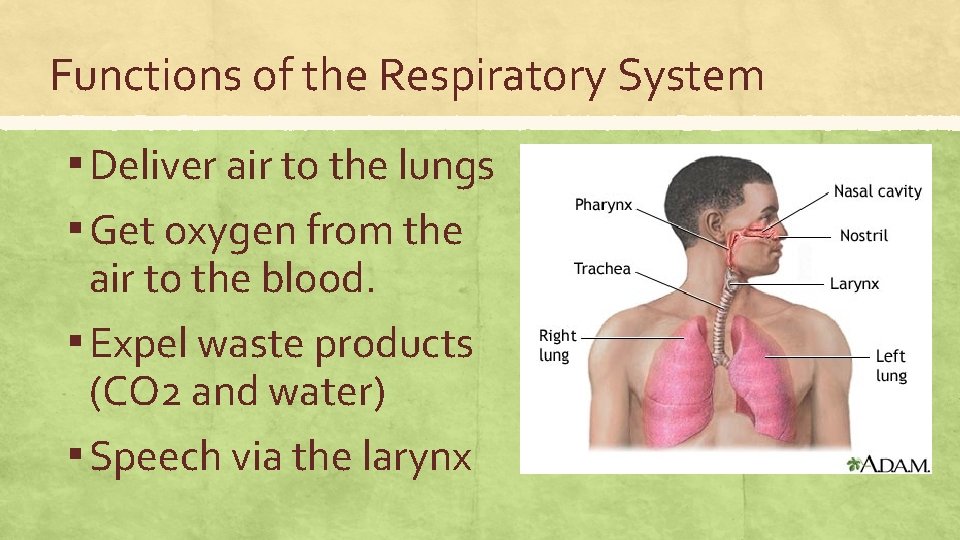
Functions of the Respiratory System ▪ Deliver air to the lungs ▪ Get oxygen from the air to the blood. ▪ Expel waste products (CO 2 and water) ▪ Speech via the larynx
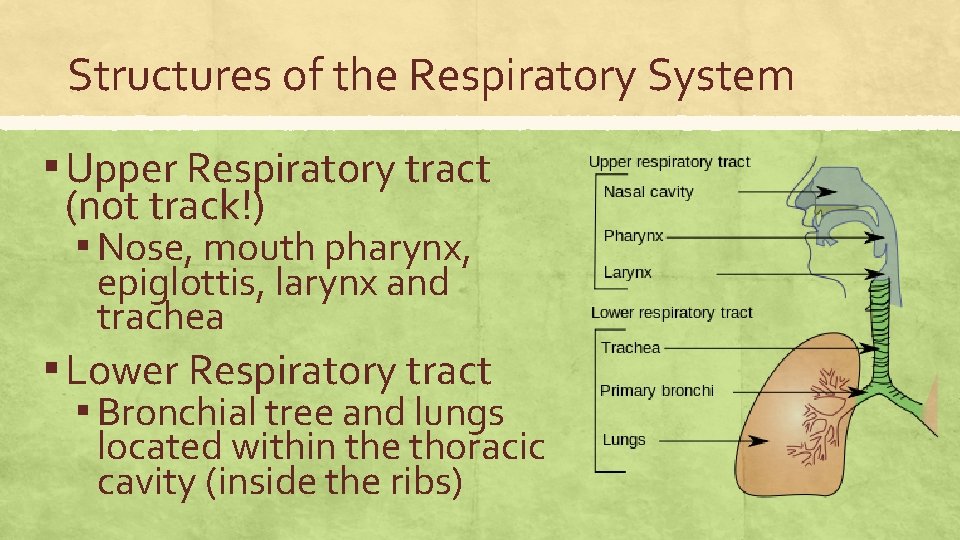
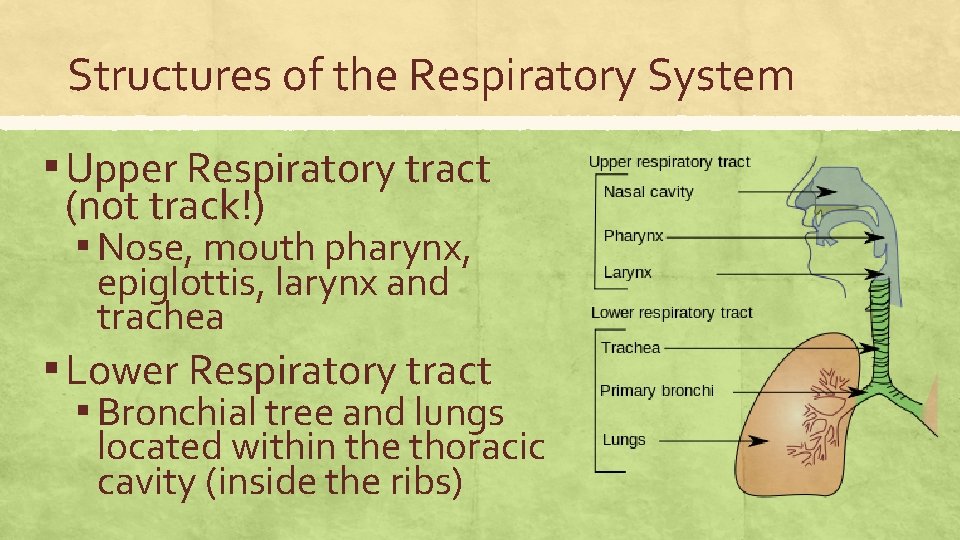
Structures of the Respiratory System ▪ Upper Respiratory tract (not track!) ▪ Nose, mouth pharynx, epiglottis, larynx and trachea ▪ Lower Respiratory tract ▪ Bronchial tree and lungs located within the thoracic cavity (inside the ribs)
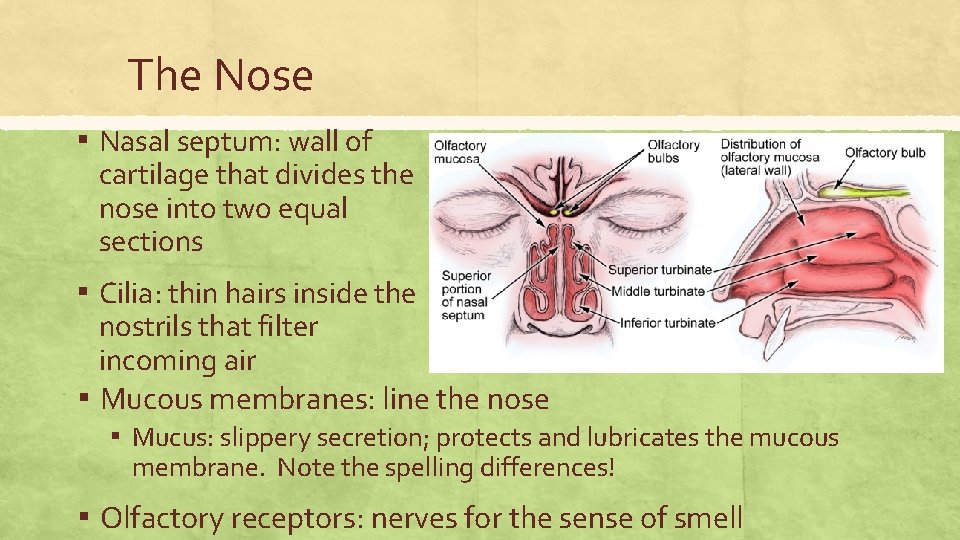
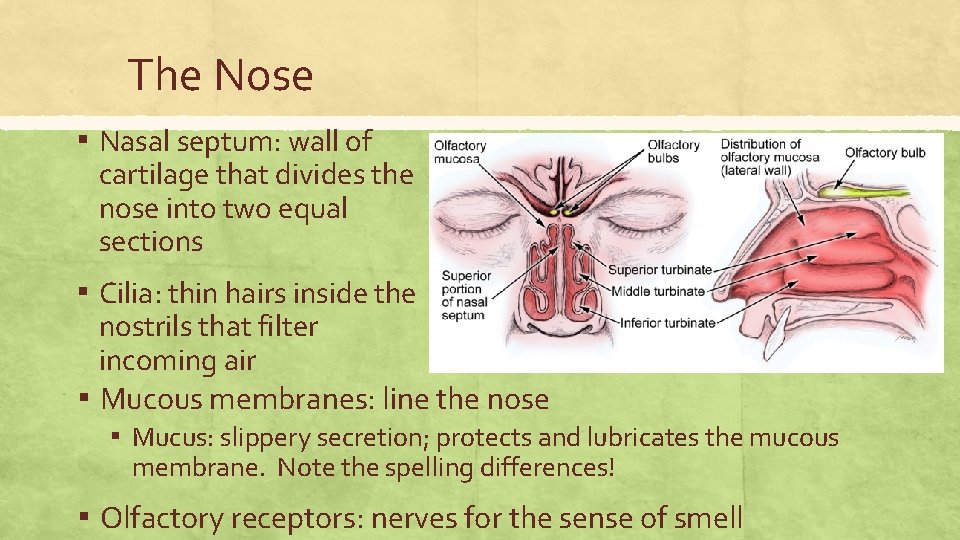
The Nose ▪ Nasal septum: wall of cartilage that divides the nose into two equal sections ▪ Cilia: thin hairs inside the nostrils that filter incoming air ▪ Mucous membranes: line the nose ▪ Mucus: slippery secretion; protects and lubricates the mucous membrane. Note the spelling differences! ▪ Olfactory receptors: nerves for the sense of smell
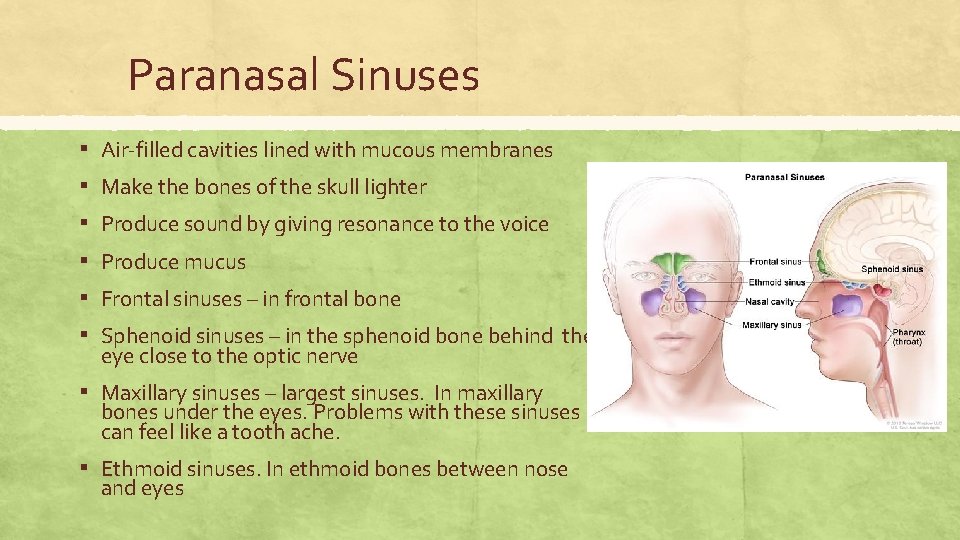
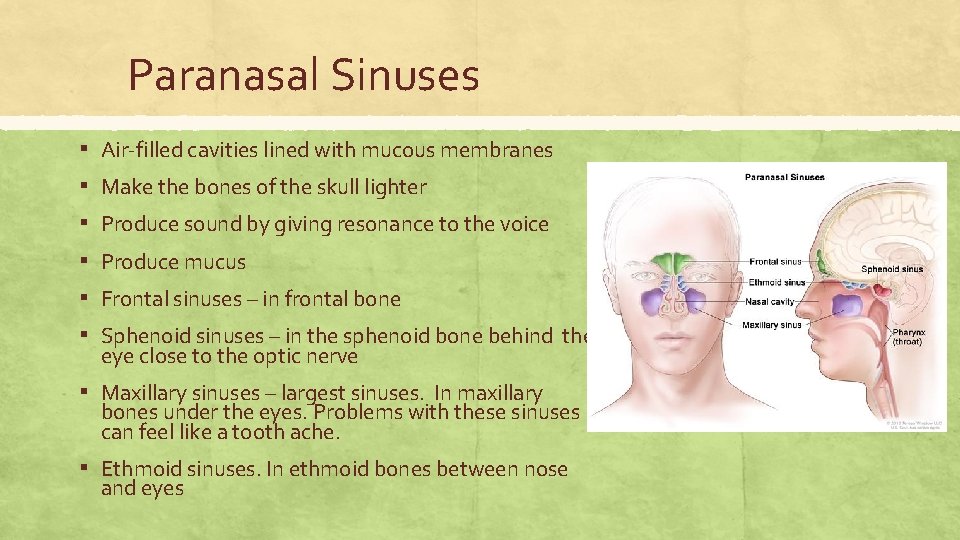
Paranasal Sinuses ▪ ▪ ▪ Air-filled cavities lined with mucous membranes Make the bones of the skull lighter Produce sound by giving resonance to the voice Produce mucus Frontal sinuses – in frontal bone Sphenoid sinuses – in the sphenoid bone behind the eye close to the optic nerve ▪ Maxillary sinuses – largest sinuses. In maxillary bones under the eyes. Problems with these sinuses can feel like a tooth ache. ▪ Ethmoid sinuses. In ethmoid bones between nose and eyes
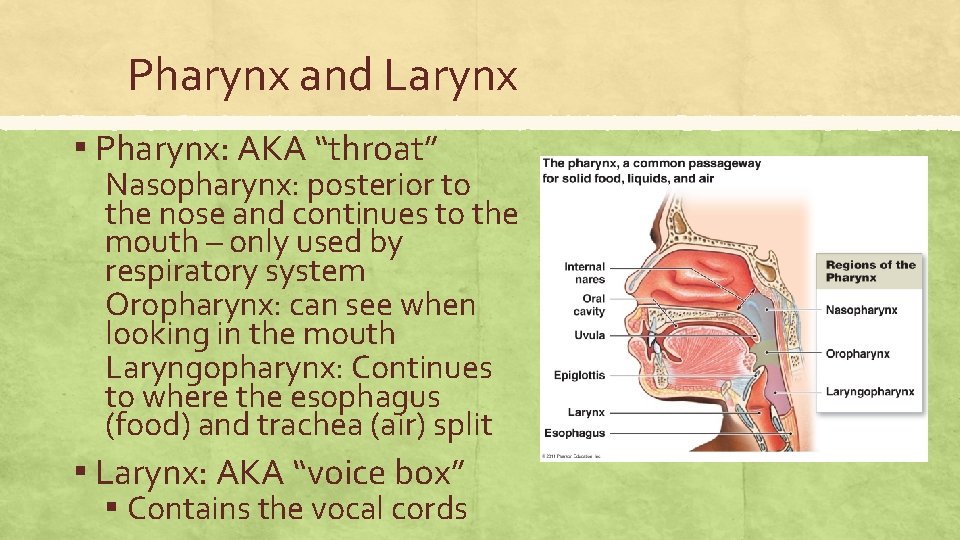
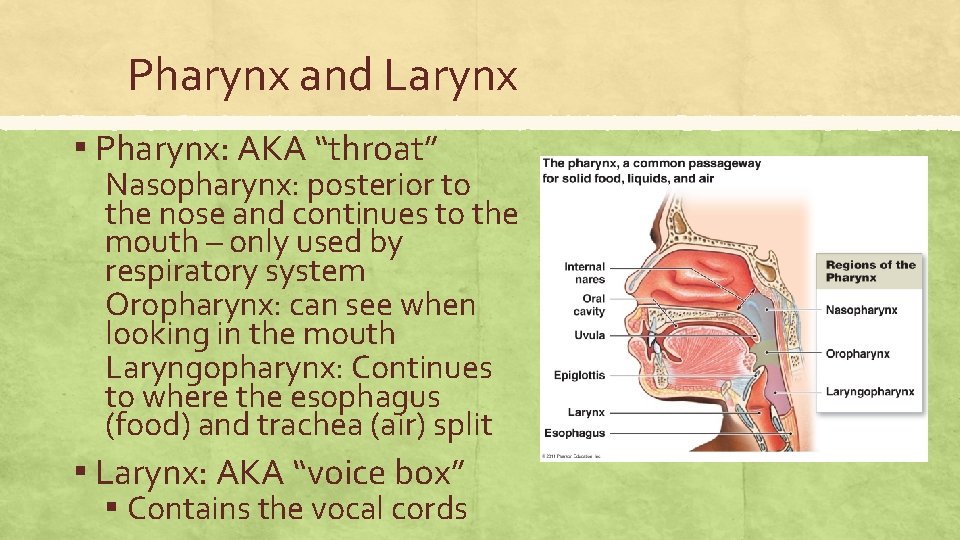
Pharynx and Larynx ▪ Pharynx: AKA “throat” Nasopharynx: posterior to the nose and continues to the mouth – only used by respiratory system Oropharynx: can see when looking in the mouth Laryngopharynx: Continues to where the esophagus (food) and trachea (air) split ▪ Larynx: AKA “voice box” ▪ Contains the vocal cords
Protective Swallowing ▪ Since respiratory and digestive share pharynx, there is a risk of aspiration into the lungs ▪ 1. Soft palate: moves up and backward during swallowing to close off the Nasopharynx so food does not go into the nose ▪ 2. Epiglottis: lid-like structure at the base of the tongue closes off the laryngopharynx so food does not enter the trachea.
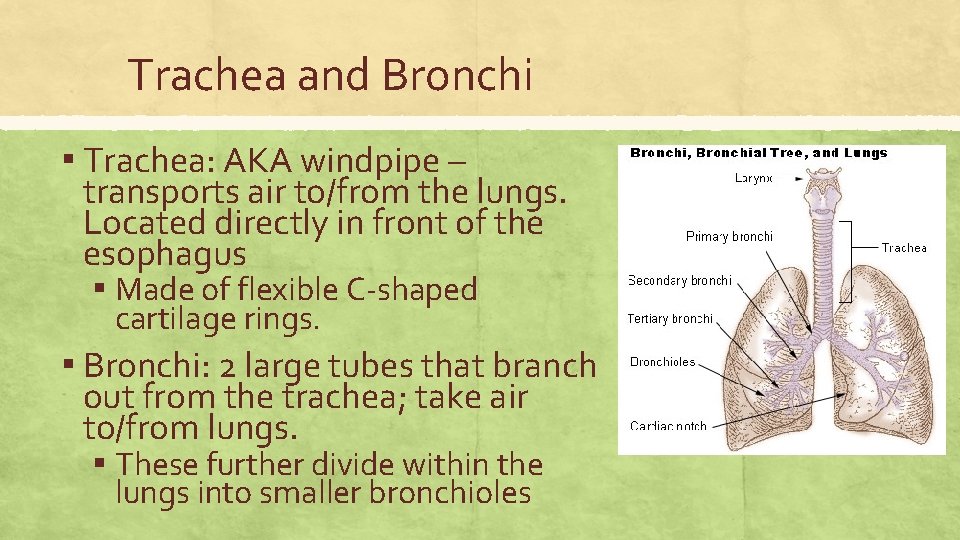
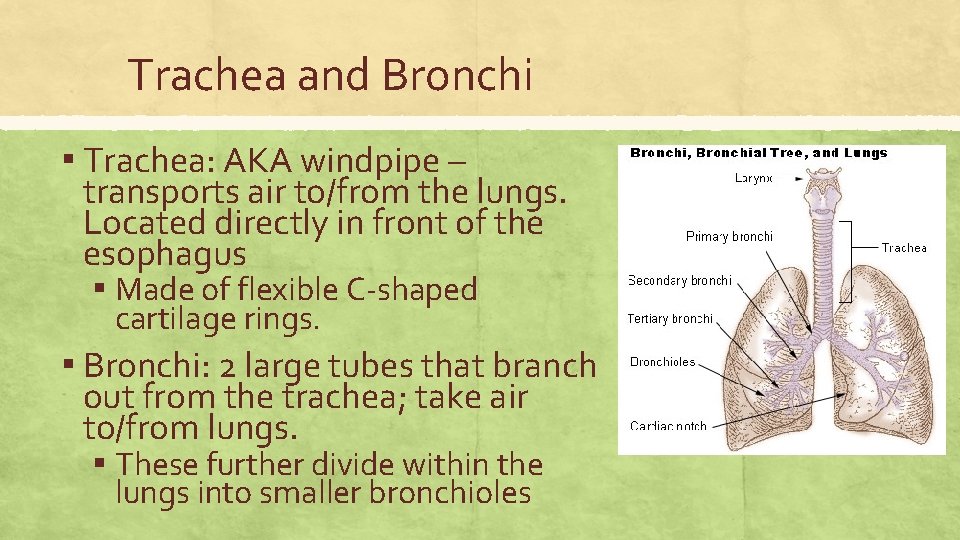
Trachea and Bronchi ▪ Trachea: AKA windpipe – transports air to/from the lungs. Located directly in front of the esophagus ▪ Made of flexible C-shaped cartilage rings. ▪ Bronchi: 2 large tubes that branch out from the trachea; take air to/from lungs. ▪ These further divide within the lungs into smaller bronchioles
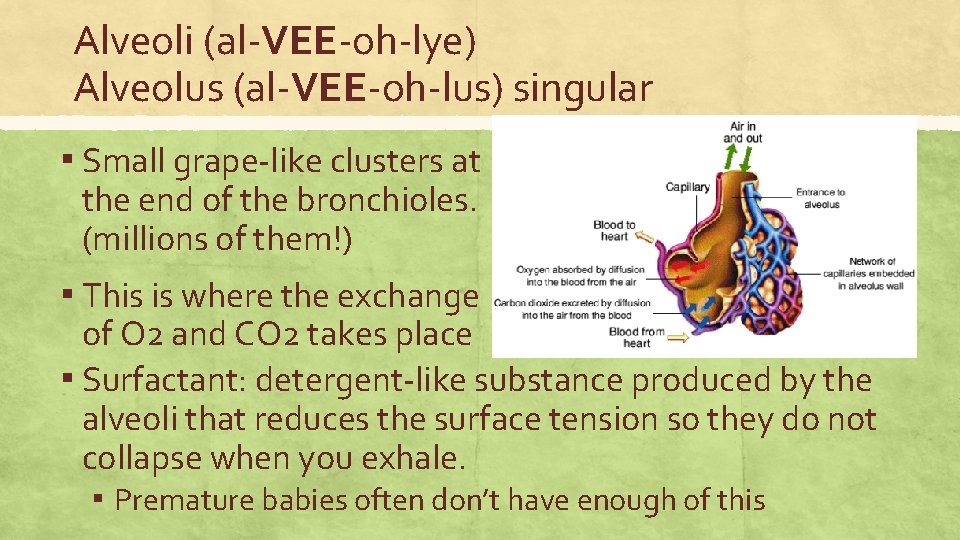
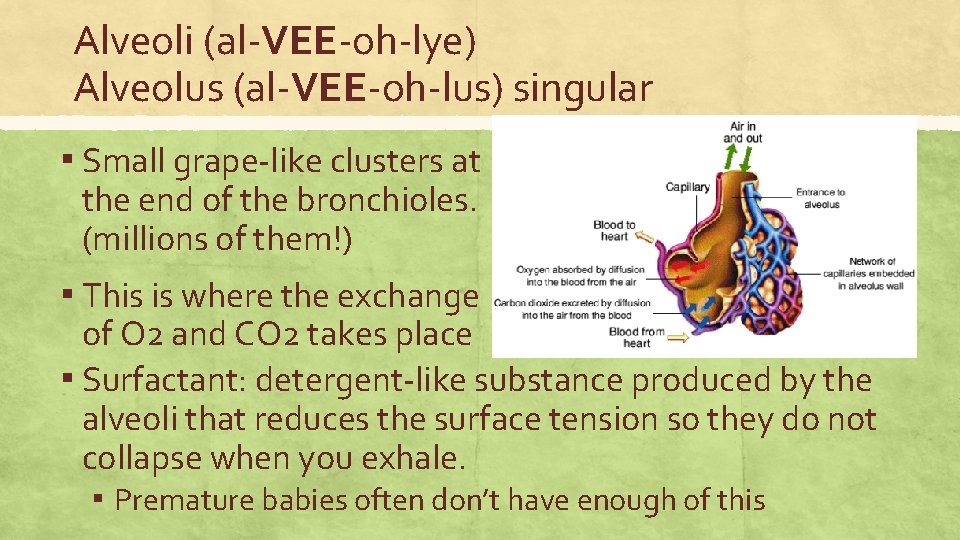
Alveoli (al-VEE-oh-lye) Alveolus (al-VEE-oh-lus) singular ▪ Small grape-like clusters at the end of the bronchioles. (millions of them!) ▪ This is where the exchange of O 2 and CO 2 takes place ▪ Surfactant: detergent-like substance produced by the alveoli that reduces the surface tension so they do not collapse when you exhale. ▪ Premature babies often don’t have enough of this
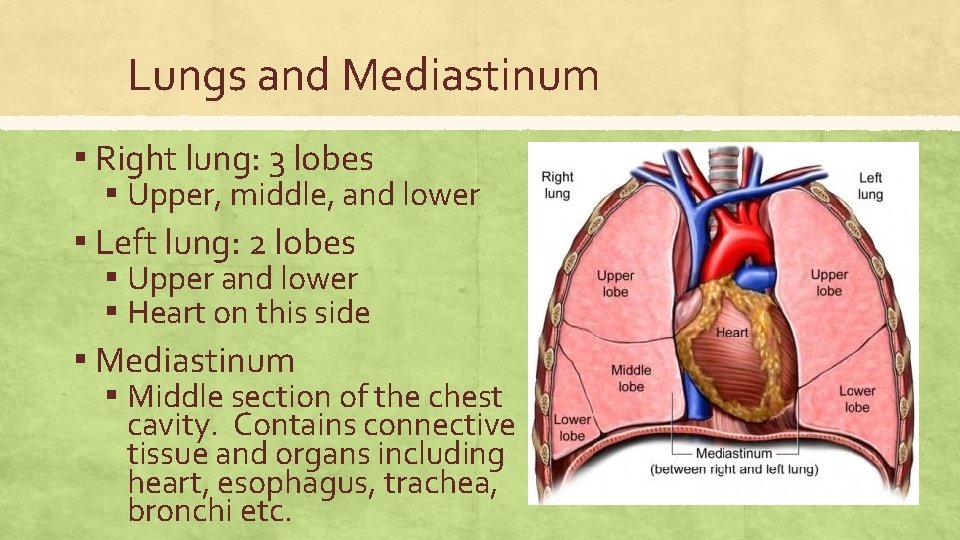
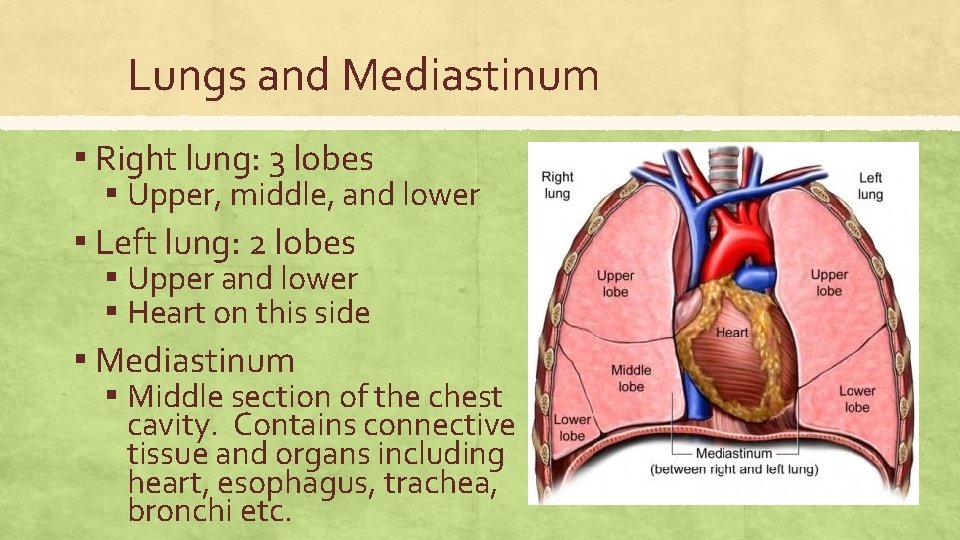
Lungs and Mediastinum ▪ Right lung: 3 lobes ▪ Upper, middle, and lower ▪ Left lung: 2 lobes ▪ Upper and lower ▪ Heart on this side ▪ Mediastinum ▪ Middle section of the chest cavity. Contains connective tissue and organs including heart, esophagus, trachea, bronchi etc.
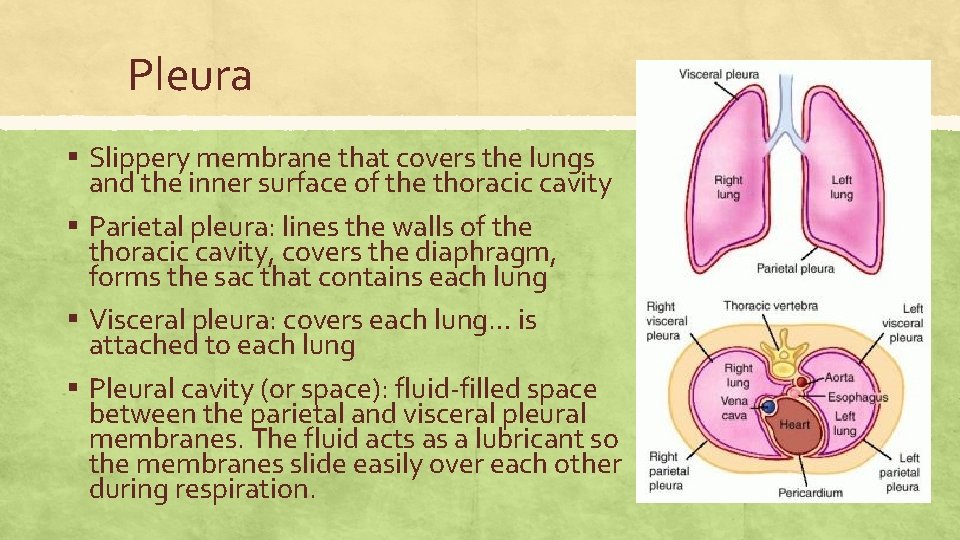
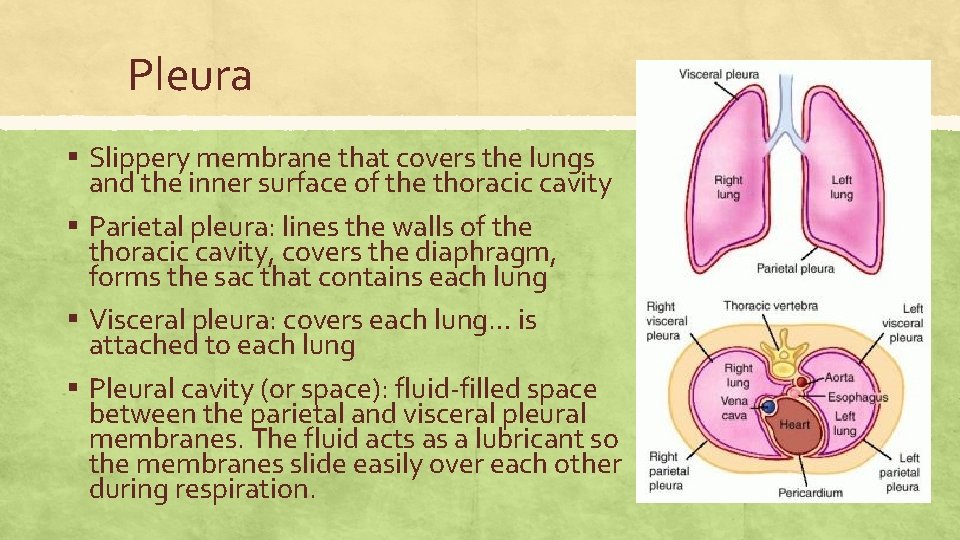
Pleura ▪ Slippery membrane that covers the lungs and the inner surface of the thoracic cavity ▪ Parietal pleura: lines the walls of the thoracic cavity, covers the diaphragm, forms the sac that contains each lung ▪ Visceral pleura: covers each lung… is attached to each lung ▪ Pleural cavity (or space): fluid-filled space between the parietal and visceral pleural membranes. The fluid acts as a lubricant so the membranes slide easily over each other during respiration.
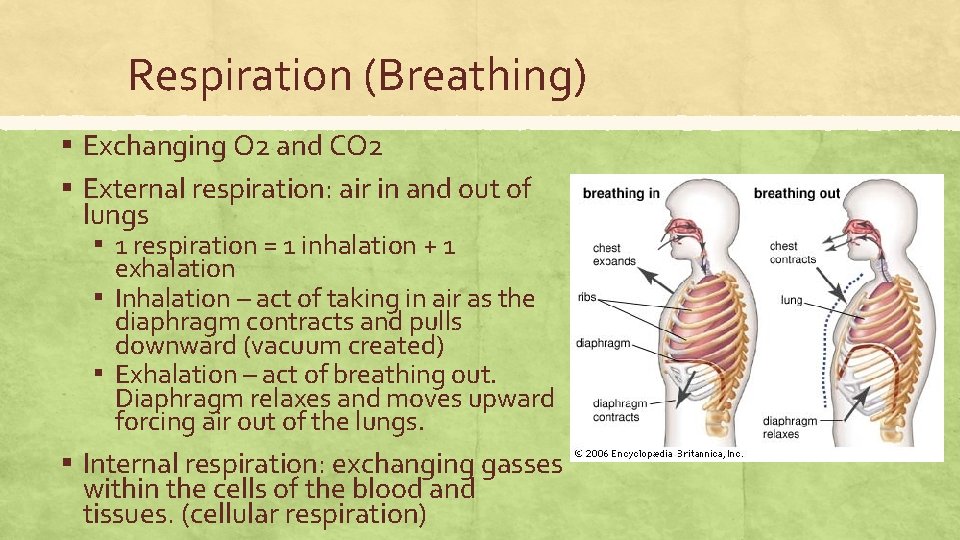
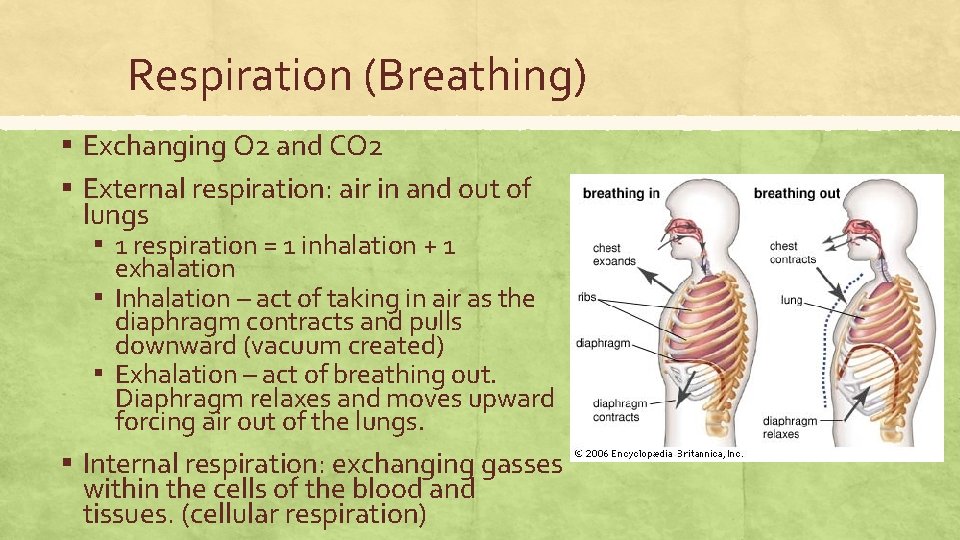
Respiration (Breathing) ▪ Exchanging O 2 and CO 2 ▪ External respiration: air in and out of lungs ▪ 1 respiration = 1 inhalation + 1 exhalation ▪ Inhalation – act of taking in air as the diaphragm contracts and pulls downward (vacuum created) ▪ Exhalation – act of breathing out. Diaphragm relaxes and moves upward forcing air out of the lungs. ▪ Internal respiration: exchanging gasses within the cells of the blood and tissues. (cellular respiration)
Medical Specialties ▪ Otolaryngologist: ENT (ear, nose, throat) – specializes in diseases of head and neck ▪ Pulmonologist: Specializes in diagnosing and treating diseases/disorders of the respiratory system.
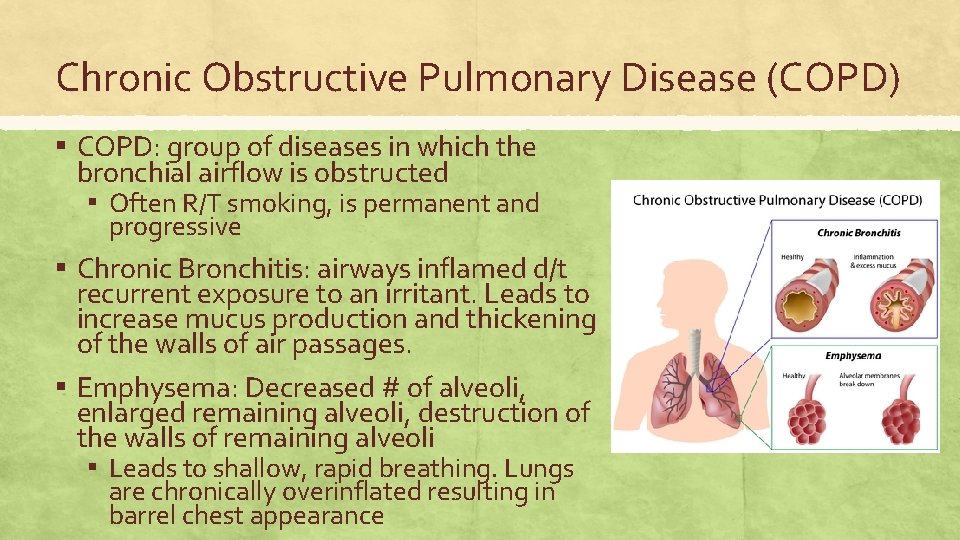
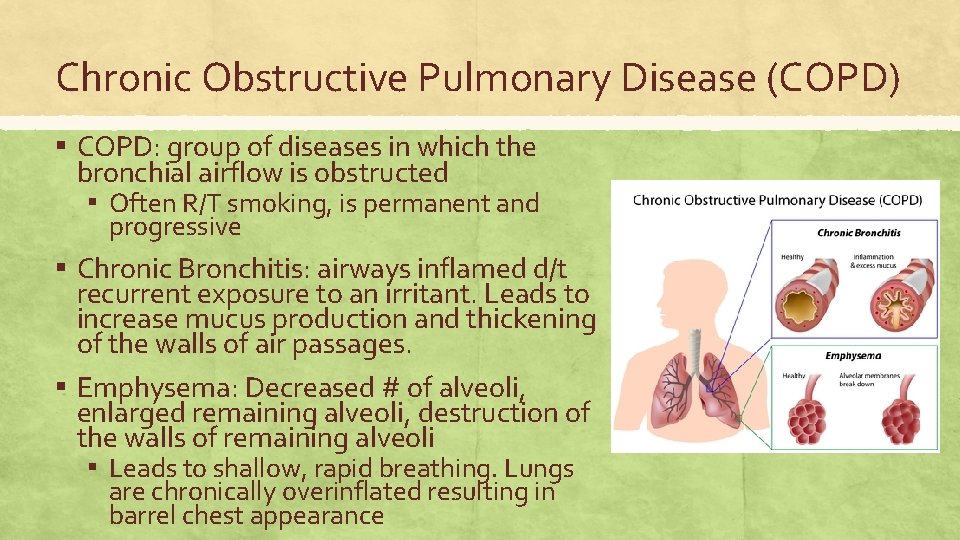
Chronic Obstructive Pulmonary Disease (COPD) ▪ COPD: group of diseases in which the bronchial airflow is obstructed ▪ Often R/T smoking, is permanent and progressive ▪ Chronic Bronchitis: airways inflamed d/t recurrent exposure to an irritant. Leads to increase mucus production and thickening of the walls of air passages. ▪ Emphysema: Decreased # of alveoli, enlarged remaining alveoli, destruction of the walls of remaining alveoli ▪ Leads to shallow, rapid breathing. Lungs are chronically overinflated resulting in barrel chest appearance
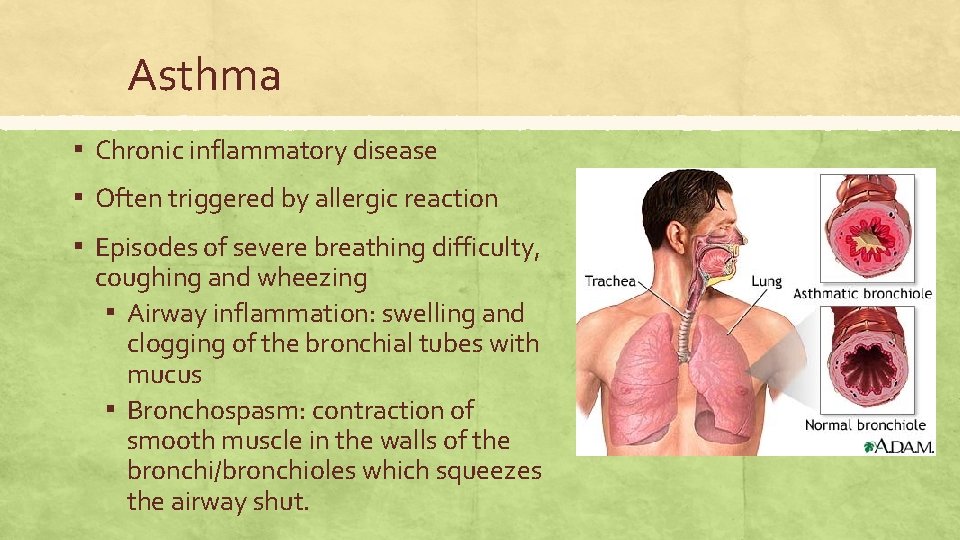
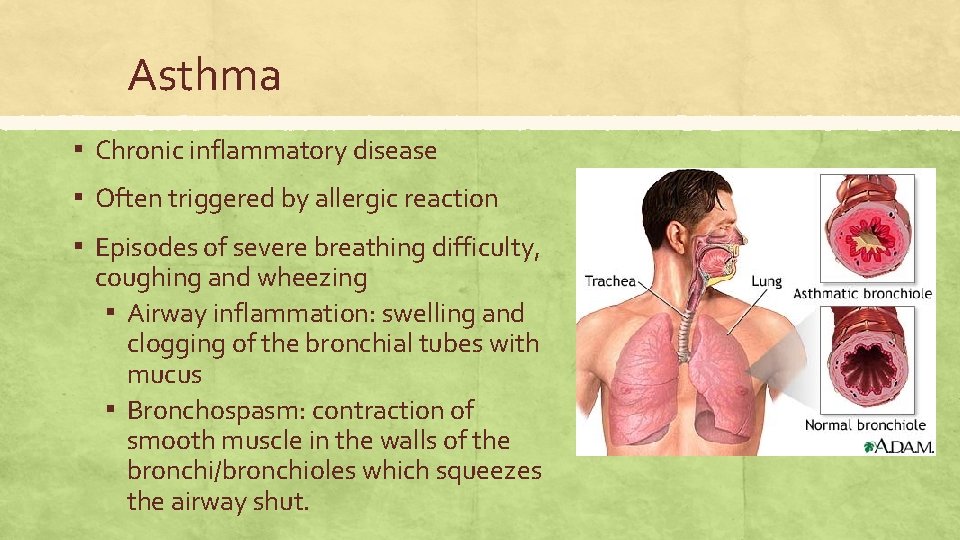
Asthma ▪ Chronic inflammatory disease ▪ Often triggered by allergic reaction ▪ Episodes of severe breathing difficulty, coughing and wheezing ▪ Airway inflammation: swelling and clogging of the bronchial tubes with mucus ▪ Bronchospasm: contraction of smooth muscle in the walls of the bronchi/bronchioles which squeezes the airway shut.
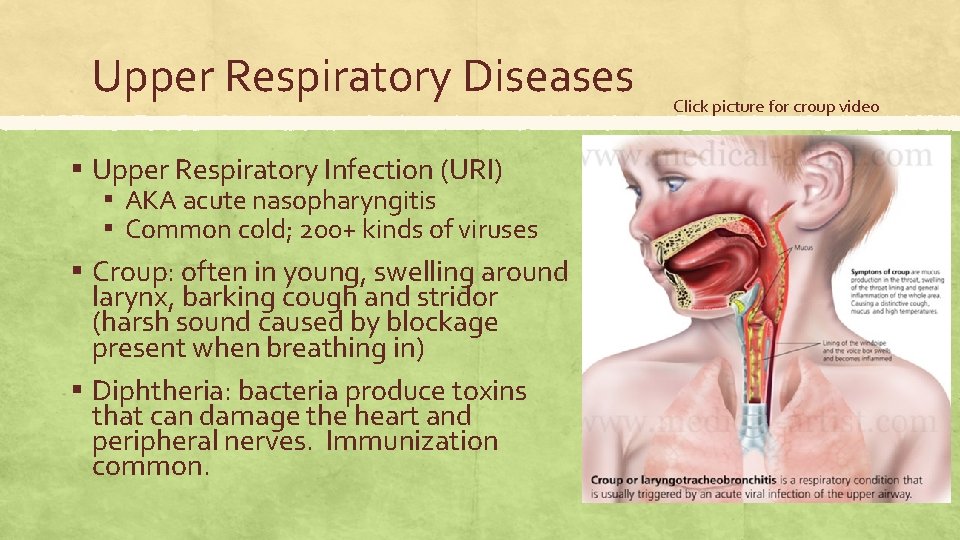
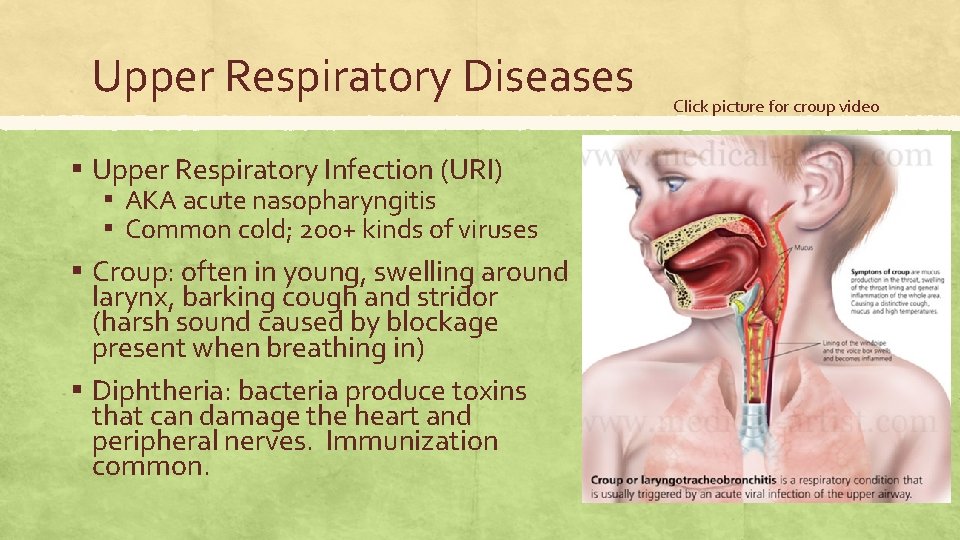
Upper Respiratory Diseases ▪ Upper Respiratory Infection (URI) ▪ AKA acute nasopharyngitis ▪ Common cold; 200+ kinds of viruses ▪ Croup: often in young, swelling around larynx, barking cough and stridor (harsh sound caused by blockage present when breathing in) ▪ Diphtheria: bacteria produce toxins that can damage the heart and peripheral nerves. Immunization common. Click picture for croup video
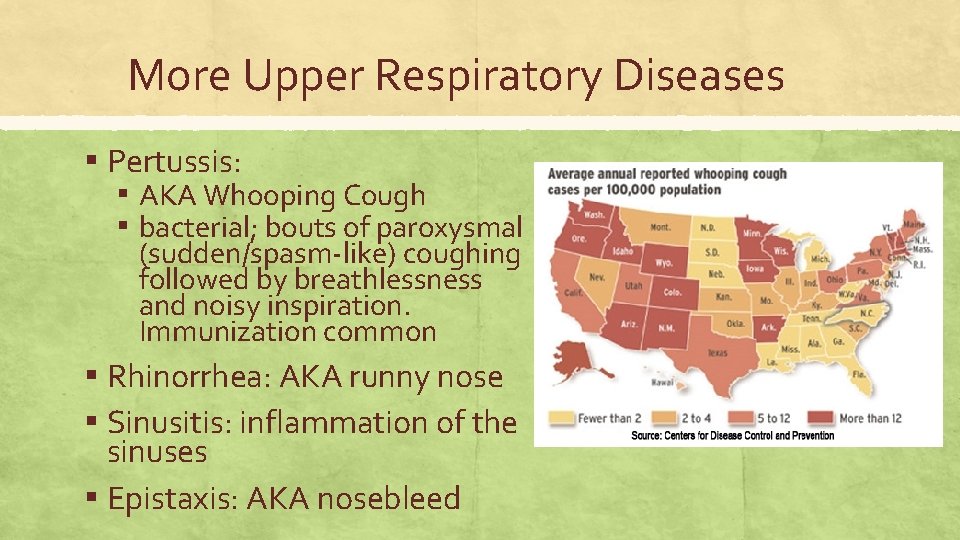
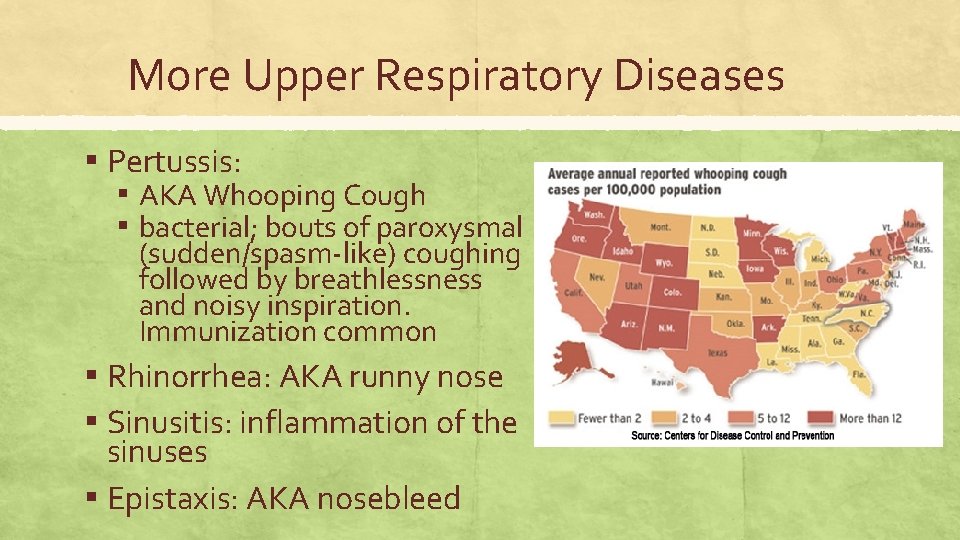
More Upper Respiratory Diseases ▪ Pertussis: ▪ AKA Whooping Cough ▪ bacterial; bouts of paroxysmal (sudden/spasm-like) coughing followed by breathlessness and noisy inspiration. Immunization common ▪ Rhinorrhea: AKA runny nose ▪ Sinusitis: inflammation of the sinuses ▪ Epistaxis: AKA nosebleed
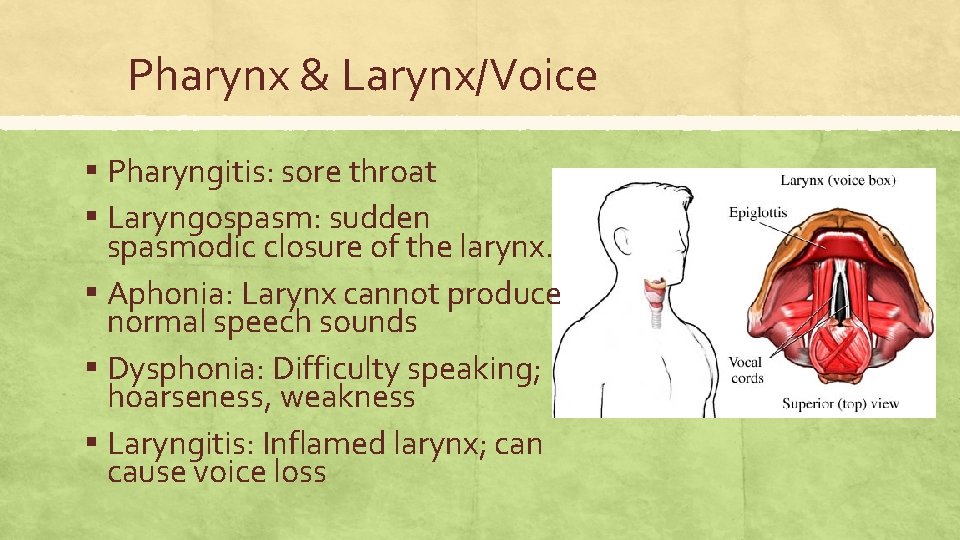
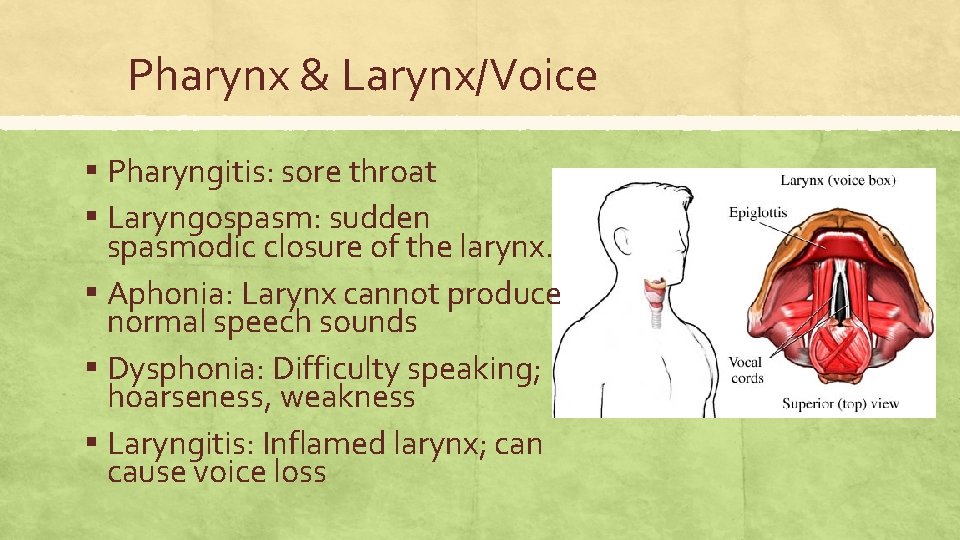
Pharynx & Larynx/Voice ▪ Pharyngitis: sore throat ▪ Laryngospasm: sudden spasmodic closure of the larynx. ▪ Aphonia: Larynx cannot produce normal speech sounds ▪ Dysphonia: Difficulty speaking; hoarseness, weakness ▪ Laryngitis: Inflamed larynx; can cause voice loss
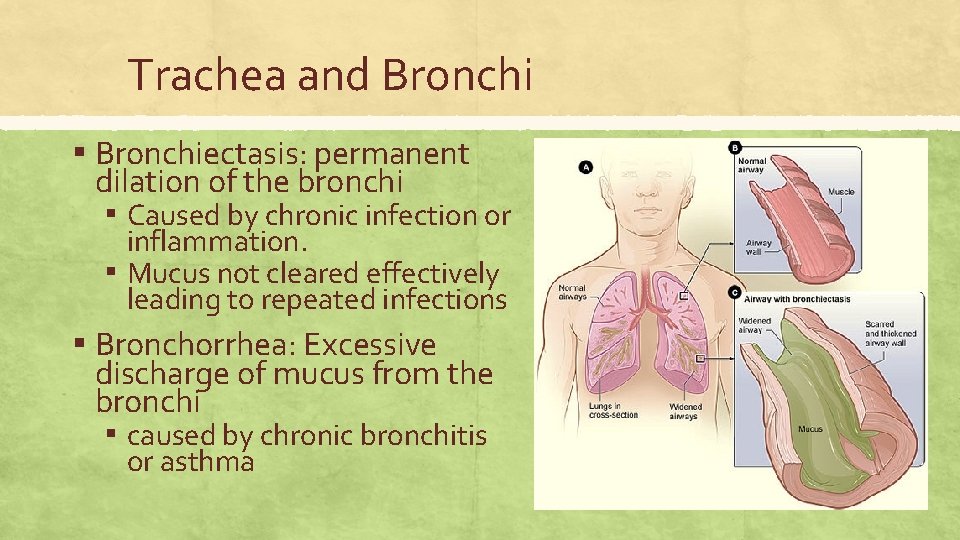
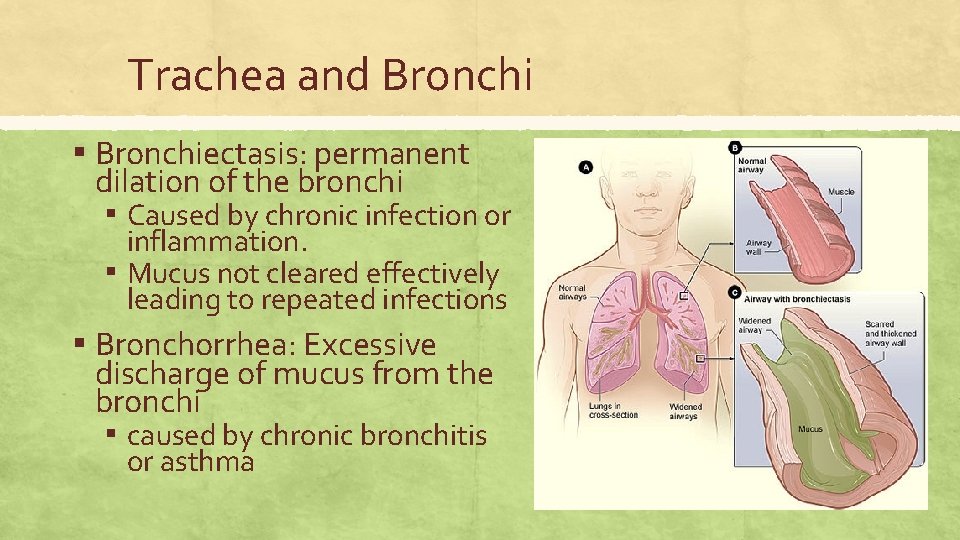
Trachea and Bronchi ▪ Bronchiectasis: permanent dilation of the bronchi ▪ Caused by chronic infection or inflammation. ▪ Mucus not cleared effectively leading to repeated infections ▪ Bronchorrhea: Excessive discharge of mucus from the bronchi ▪ caused by chronic bronchitis or asthma
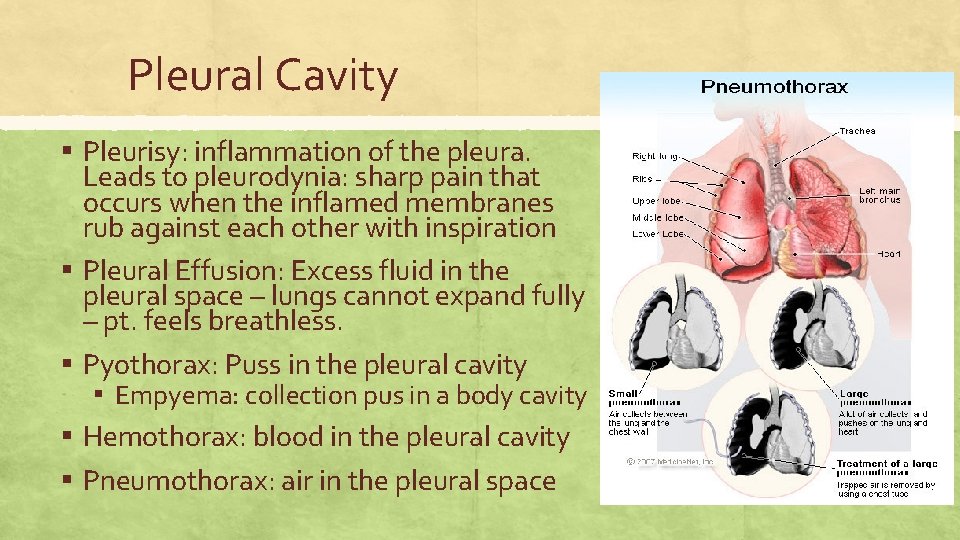
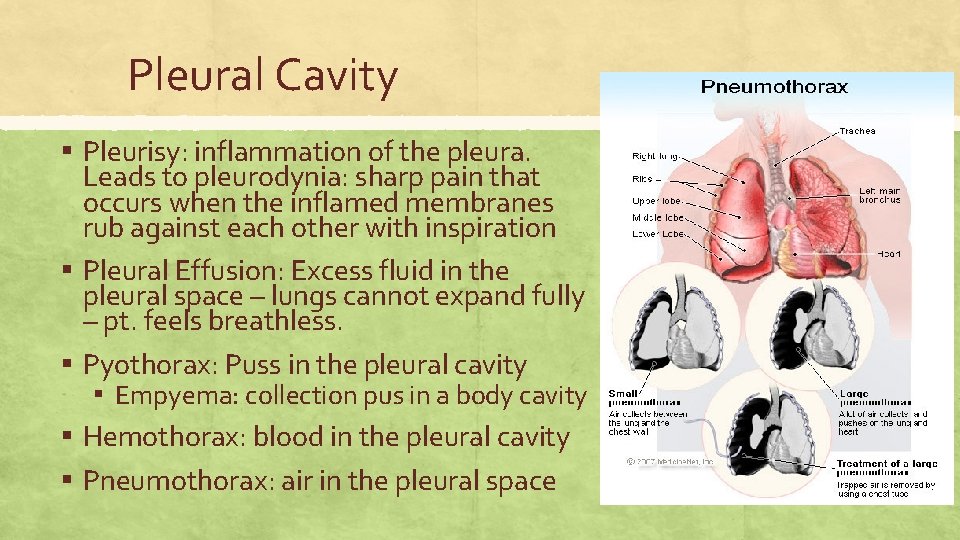
Pleural Cavity ▪ Pleurisy: inflammation of the pleura. ▪ ▪ Leads to pleurodynia: sharp pain that occurs when the inflamed membranes rub against each other with inspiration Pleural Effusion: Excess fluid in the pleural space – lungs cannot expand fully – pt. feels breathless. Pyothorax: Puss in the pleural cavity ▪ Empyema: collection pus in a body cavity Hemothorax: blood in the pleural cavity Pneumothorax: air in the pleural space
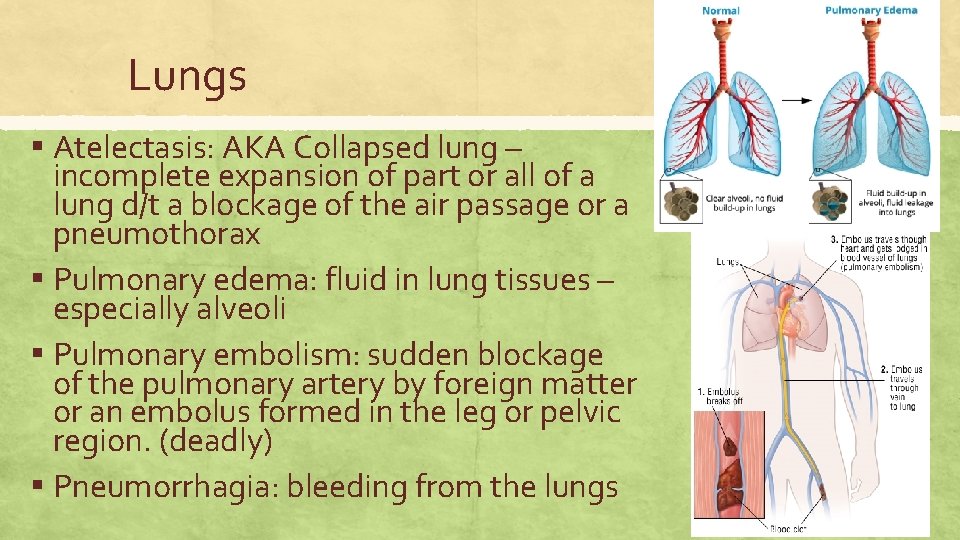
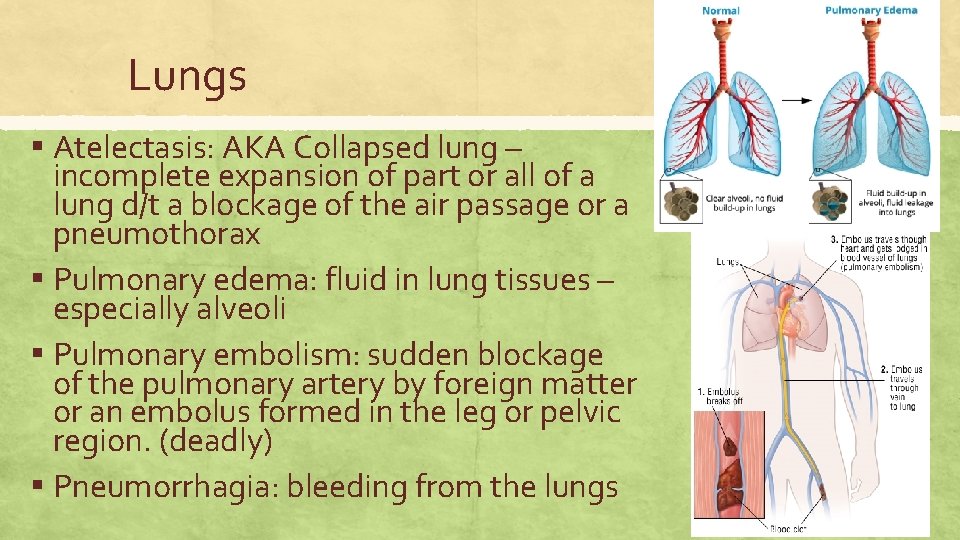
Lungs ▪ Atelectasis: AKA Collapsed lung – incomplete expansion of part or all of a lung d/t a blockage of the air passage or a pneumothorax ▪ Pulmonary edema: fluid in lung tissues – especially alveoli ▪ Pulmonary embolism: sudden blockage of the pulmonary artery by foreign matter or an embolus formed in the leg or pelvic region. (deadly) ▪ Pneumorrhagia: bleeding from the lungs
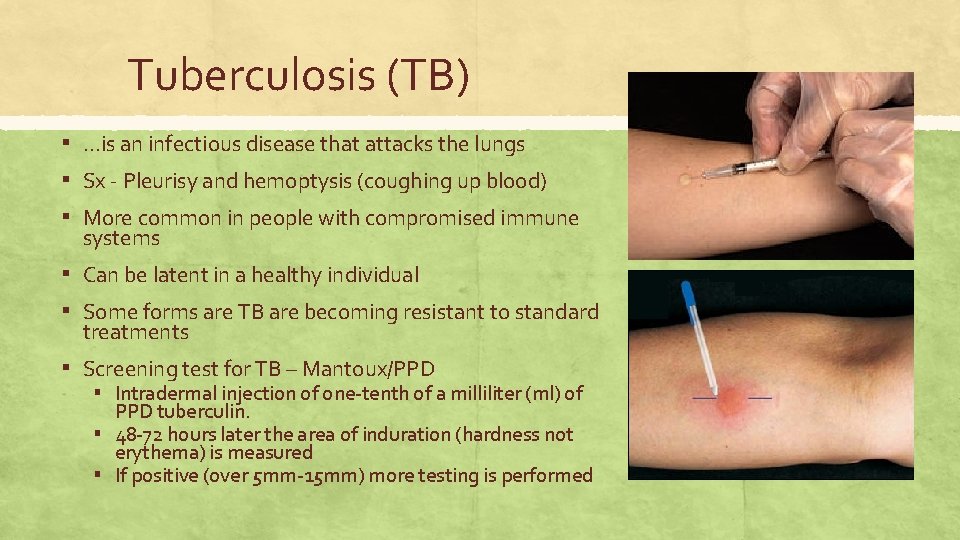
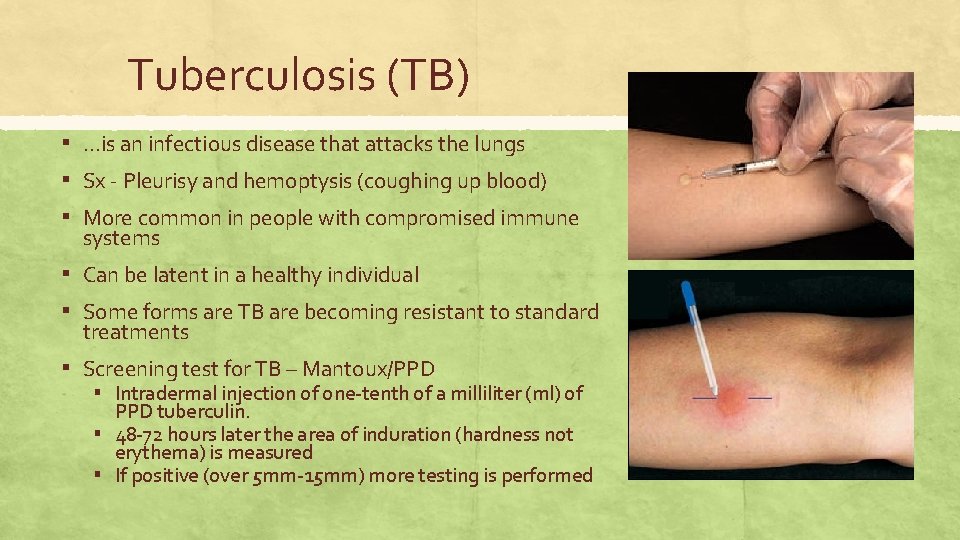
Tuberculosis (TB) ▪ …is an infectious disease that attacks the lungs ▪ Sx - Pleurisy and hemoptysis (coughing up blood) ▪ More common in people with compromised immune systems ▪ Can be latent in a healthy individual ▪ Some forms are TB are becoming resistant to standard treatments ▪ Screening test for TB – Mantoux/PPD ▪ Intradermal injection of one-tenth of a milliliter (ml) of PPD tuberculin. ▪ 48 -72 hours later the area of induration (hardness not erythema) is measured ▪ If positive (over 5 mm-15 mm) more testing is performed
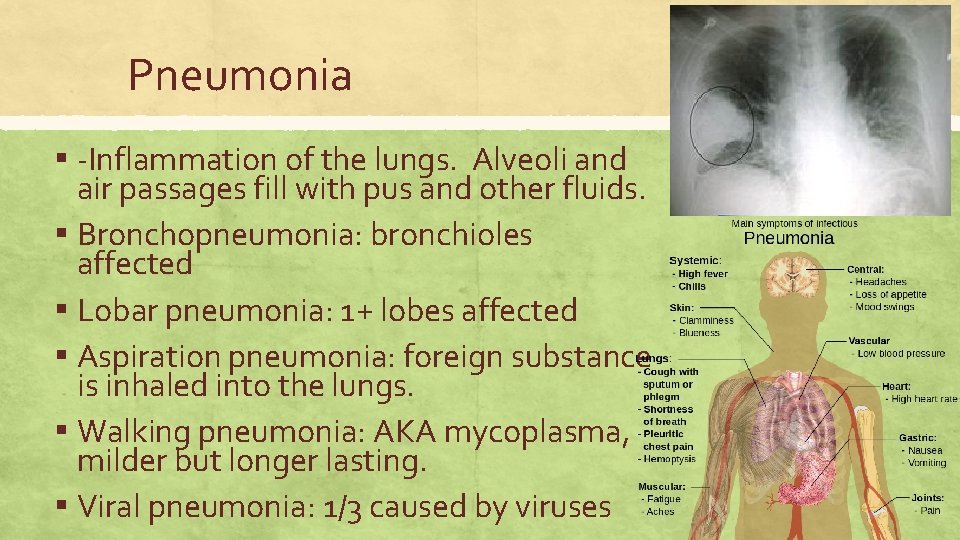
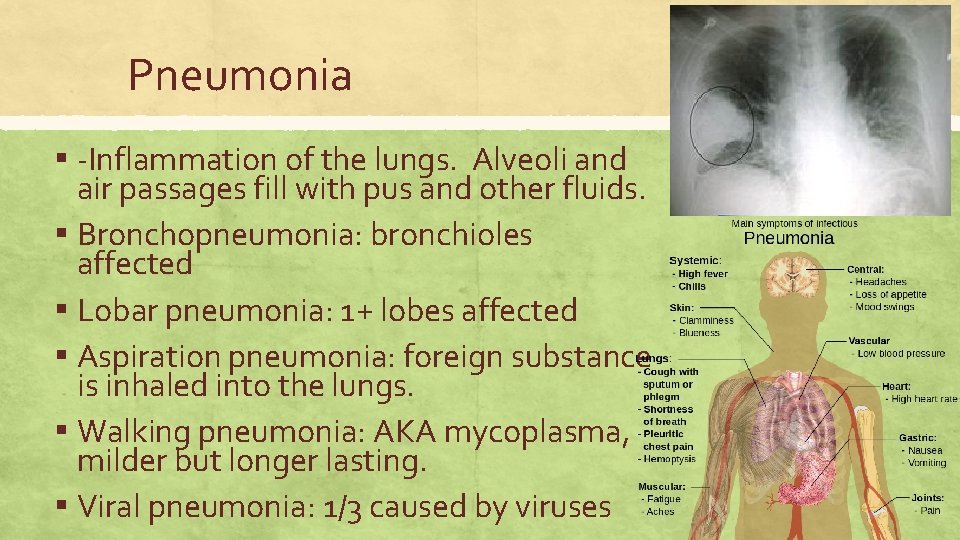
Pneumonia ▪ -Inflammation of the lungs. Alveoli and air passages fill with pus and other fluids. ▪ Bronchopneumonia: bronchioles affected ▪ Lobar pneumonia: 1+ lobes affected ▪ Aspiration pneumonia: foreign substance is inhaled into the lungs. ▪ Walking pneumonia: AKA mycoplasma, milder but longer lasting. ▪ Viral pneumonia: 1/3 caused by viruses
Interstitial Lung Disease ▪ Interstitial: relating to the spaces within or around a tissue or organ. ▪ Interstitial lung disease: 200+ disordersinflammation and scarring of the alveoli and their supporting structures. ▪ Many have an environmental basis ▪ Pulmonary fibrosis: formation of scar tissue in the lung ▪ Leads to decreased lung capacity and difficulty breathing.
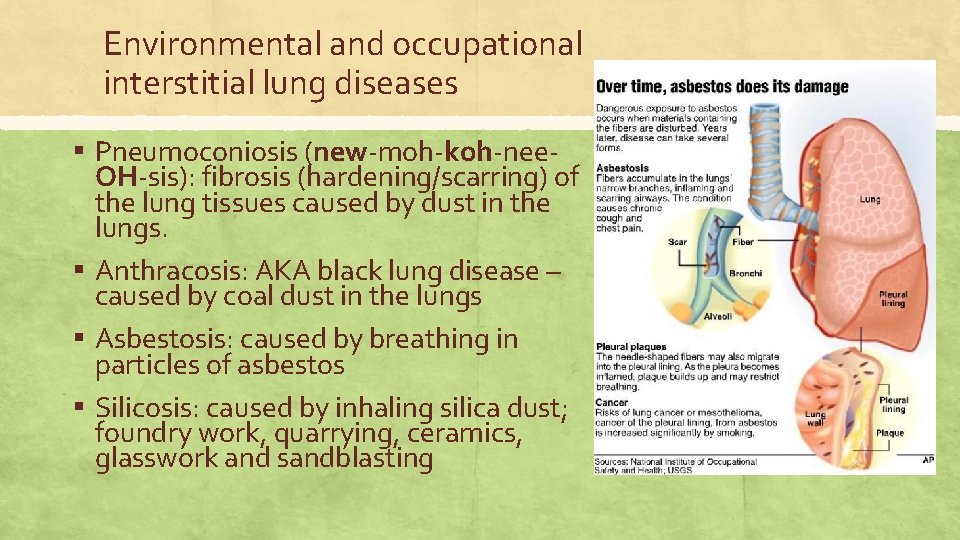
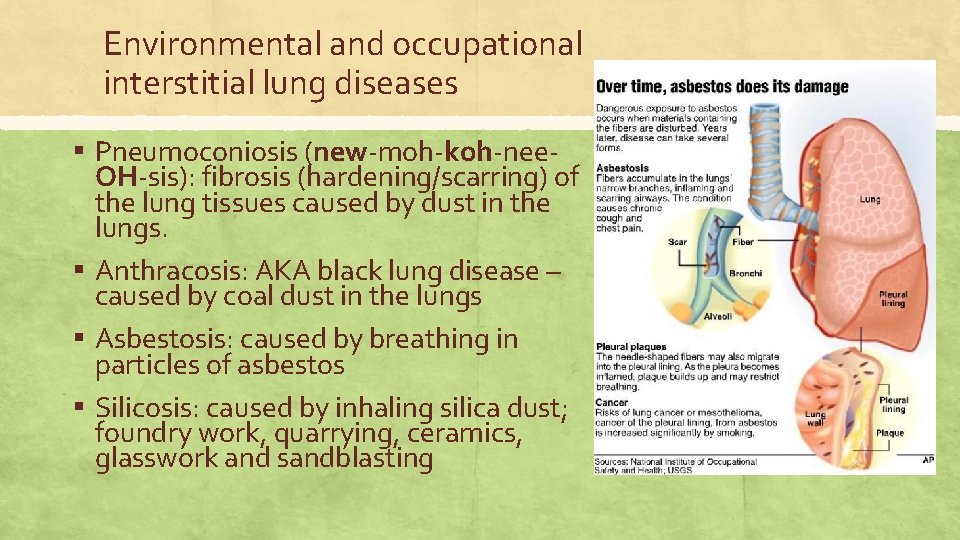
Environmental and occupational interstitial lung diseases ▪ Pneumoconiosis (new-moh-koh-nee- OH-sis): fibrosis (hardening/scarring) of the lung tissues caused by dust in the lungs. ▪ Anthracosis: AKA black lung disease – caused by coal dust in the lungs ▪ Asbestosis: caused by breathing in particles of asbestos ▪ Silicosis: caused by inhaling silica dust; foundry work, quarrying, ceramics, glasswork and sandblasting
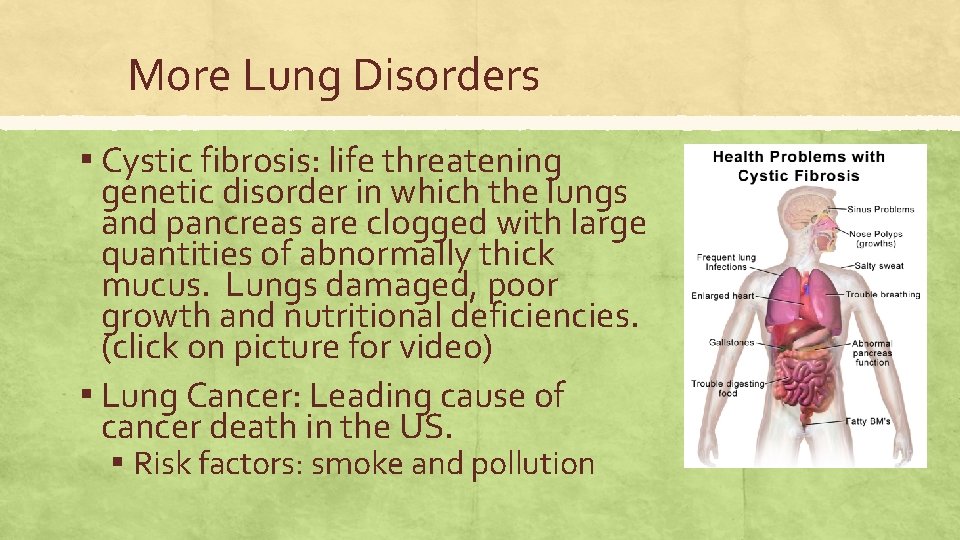
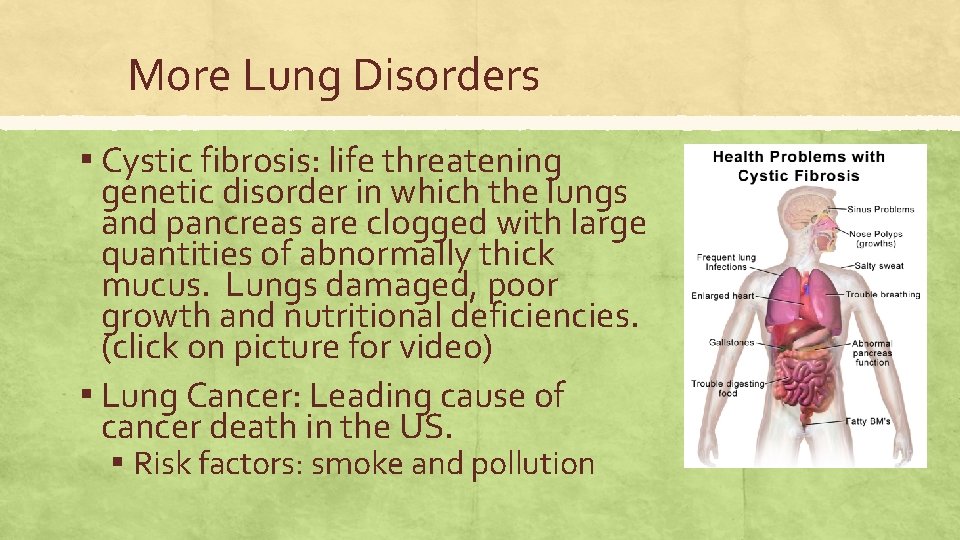
More Lung Disorders ▪ Cystic fibrosis: life threatening genetic disorder in which the lungs and pancreas are clogged with large quantities of abnormally thick mucus. Lungs damaged, poor growth and nutritional deficiencies. (click on picture for video) ▪ Lung Cancer: Leading cause of cancer death in the US. ▪ Risk factors: smoke and pollution
Breathing Disorders ▪ Apnea (AP-nee-ah): temporary absence of spontaneous respiration. (premature infants) ▪ Sleep apnea: breathing repeatedly stops and starts during sleep. Lowers O 2 levels. ▪ Dyspnea: AKA shortness of breath (SOB) difficult or labored breathing. ▪ ▪ ▪ Can be a sign of heart failure or lung damage Bradypnea: (brad-ihp-NEE-ah)slow respiration usually <10/min Hypopnea: (high-poh-NEE-ah): slow shallow breathing. Tachypnea: (tack-ihp-NEE-ah) Rapid respiration. Usually >20/min Hyperpnea: (high-per(p)-NEE-ah): R/T exertion, breathing is deeper and more rapid Cheyne-Stokes respiration: Irregular pattern of breathing characterized by alternating rapid or shallow respiration followed by slower respiration or apnea. Seen in comatose patients or those nearing death.
Coughing ▪ Expectoration: coughing up and spitting out fluids ▪ Hemoptysis: Expectoration of blood or bloodstained sputum. ▪ Phlegm: thick mucus secreted by the respiratory system ▪ Sputum: Phlegm ejected through the mouth that can be examined for diagnostic purposes.
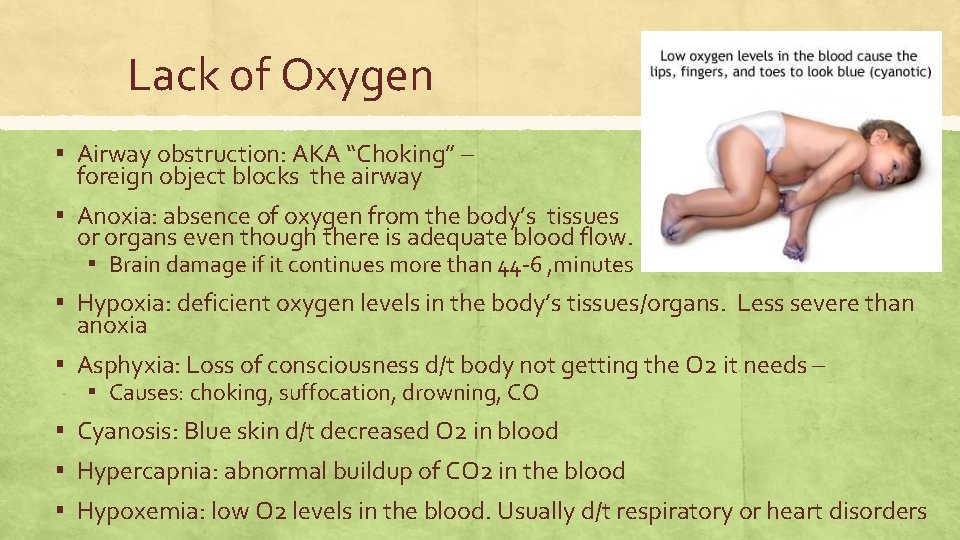
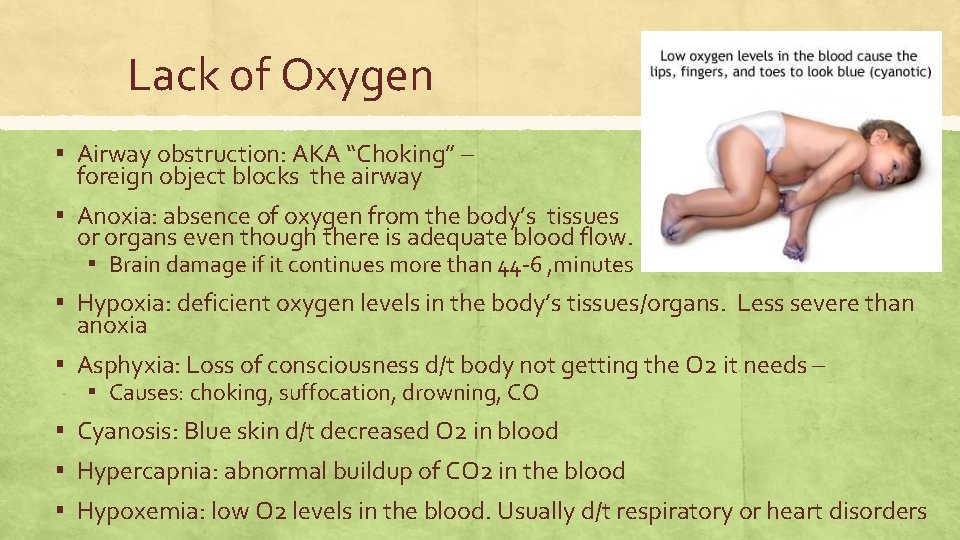
Lack of Oxygen ▪ Airway obstruction: AKA “Choking” – foreign object blocks the airway ▪ Anoxia: absence of oxygen from the body’s tissues or organs even though there is adequate blood flow. ▪ Brain damage if it continues more than 44 -6 , minutes ▪ Hypoxia: deficient oxygen levels in the body’s tissues/organs. Less severe than anoxia ▪ Asphyxia: Loss of consciousness d/t body not getting the O 2 it needs – ▪ Causes: choking, suffocation, drowning, CO ▪ Cyanosis: Blue skin d/t decreased O 2 in blood ▪ Hypercapnia: abnormal buildup of CO 2 in the blood ▪ Hypoxemia: low O 2 levels in the blood. Usually d/t respiratory or heart disorders
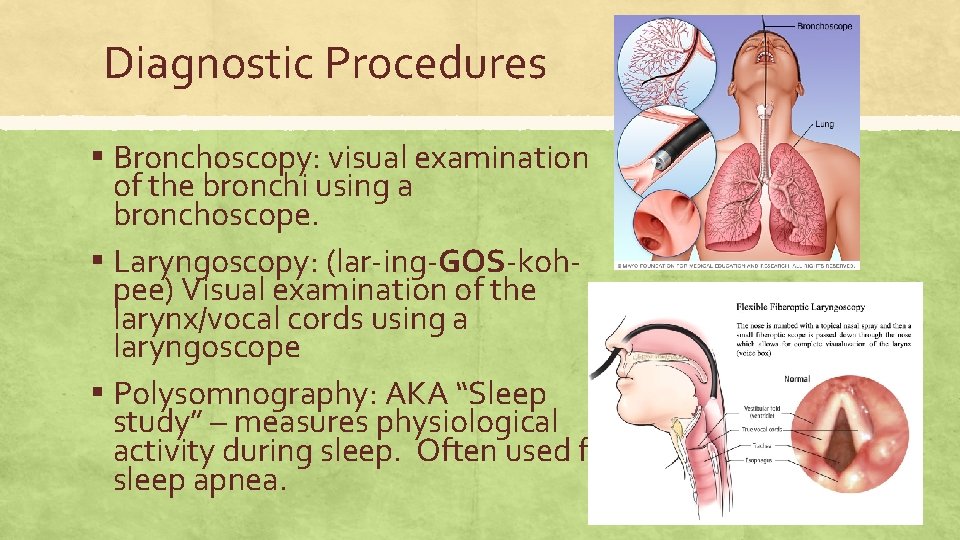
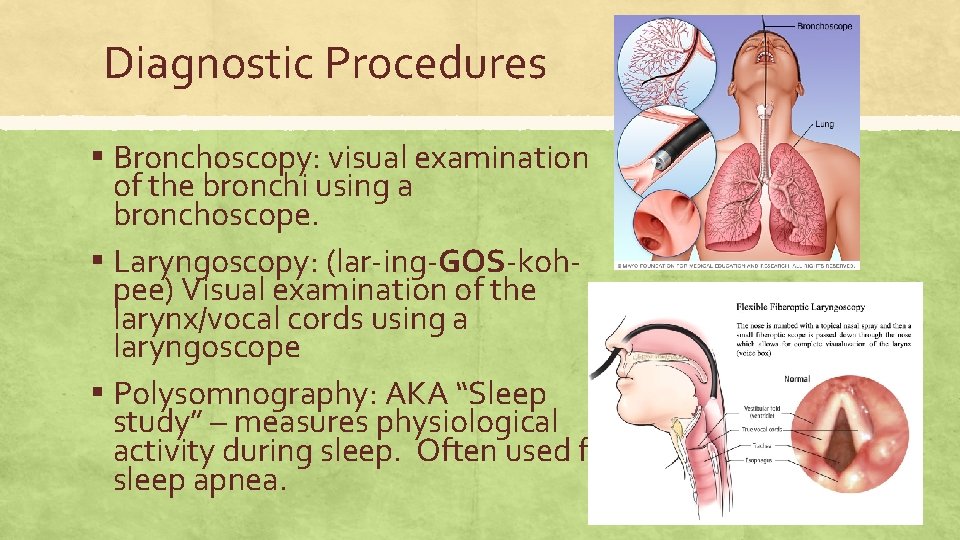
Diagnostic Procedures ▪ Bronchoscopy: visual examination of the bronchi using a bronchoscope. ▪ Laryngoscopy: (lar-ing-GOS-kohpee) Visual examination of the larynx/vocal cords using a laryngoscope ▪ Polysomnography: AKA “Sleep study” – measures physiological activity during sleep. Often used for sleep apnea.
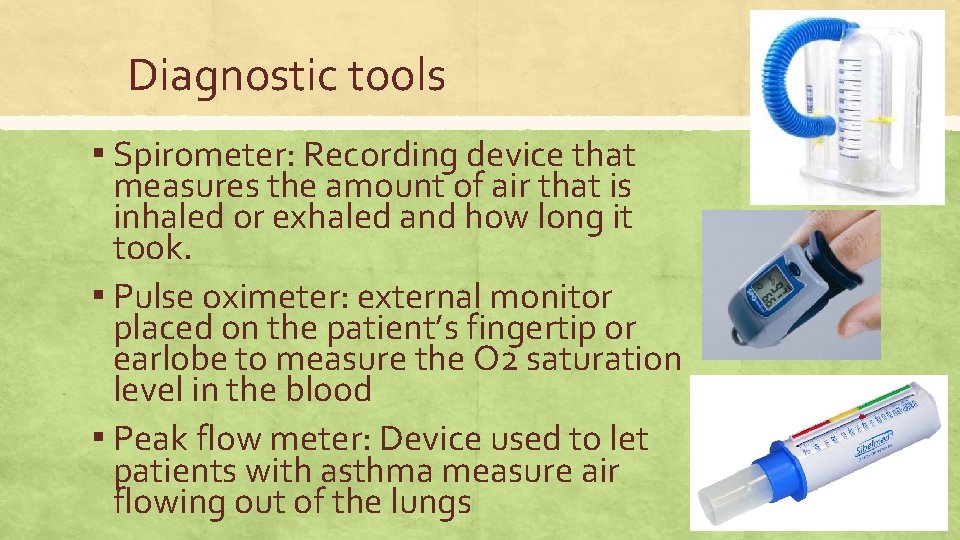
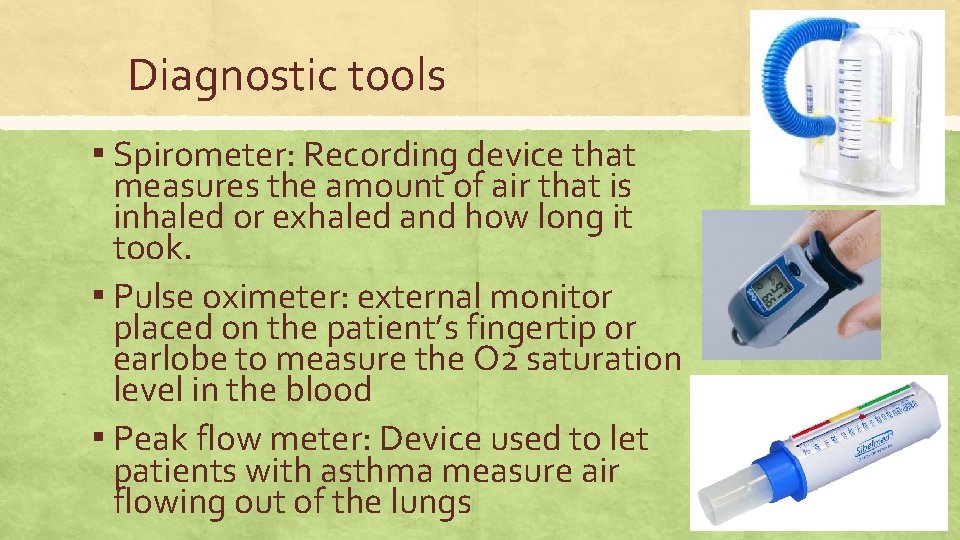
Diagnostic tools ▪ Spirometer: Recording device that measures the amount of air that is inhaled or exhaled and how long it took. ▪ Pulse oximeter: external monitor placed on the patient’s fingertip or earlobe to measure the O 2 saturation level in the blood ▪ Peak flow meter: Device used to let patients with asthma measure air flowing out of the lungs
Medications ▪ Antitussive: AKA “Cough medicine” ▪ Bronchodilator: relaxes and expands the bronchial passages into the lungs. Come in longacting and short-acting forms. Used for persons with asthma ▪ Nebulizer: Electronic – pumps air or oxygen through a liquid medicine to turn it into a mist to be inhaled.
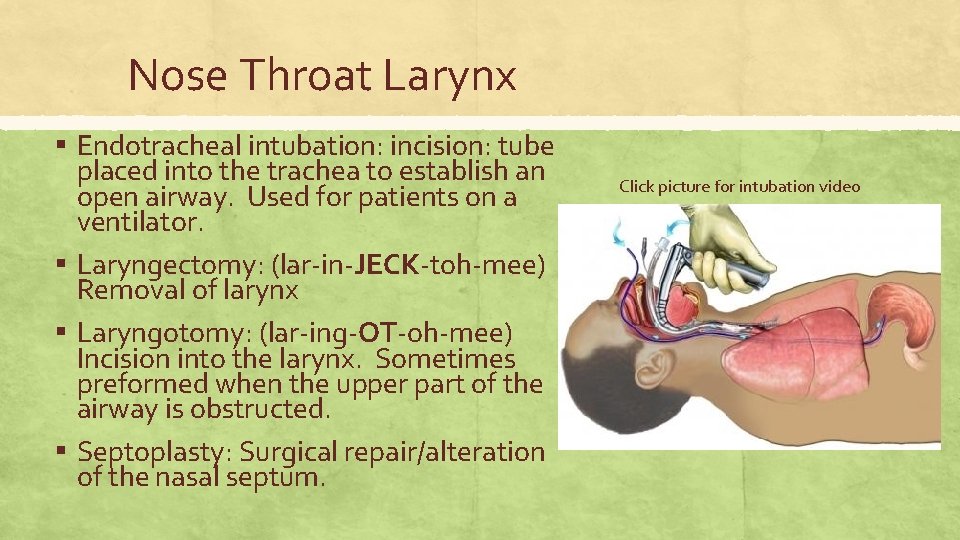
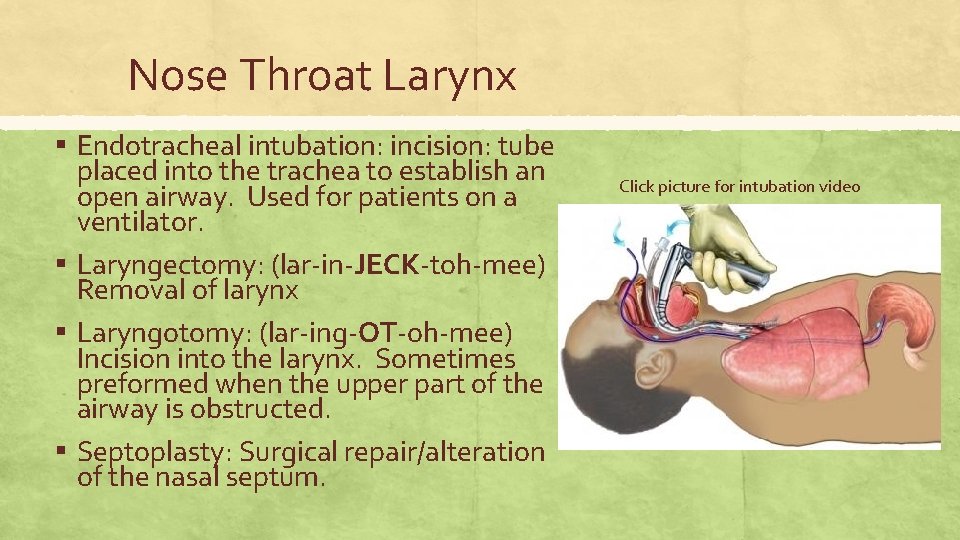
Nose Throat Larynx ▪ Endotracheal intubation: incision: tube placed into the trachea to establish an open airway. Used for patients on a ventilator. ▪ Laryngectomy: (lar-in-JECK-toh-mee) Removal of larynx ▪ Laryngotomy: (lar-ing-OT-oh-mee) Incision into the larynx. Sometimes preformed when the upper part of the airway is obstructed. ▪ Septoplasty: Surgical repair/alteration of the nasal septum. Click picture for intubation video
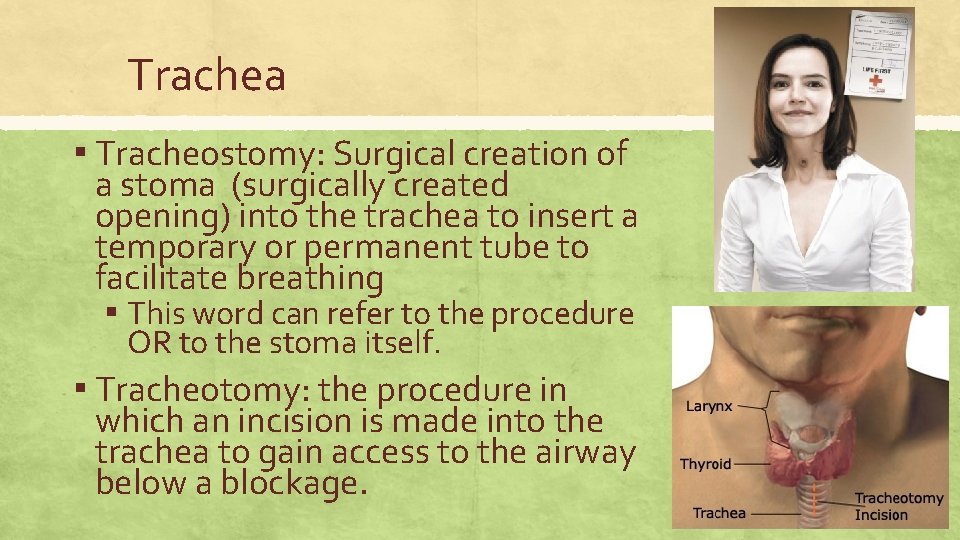
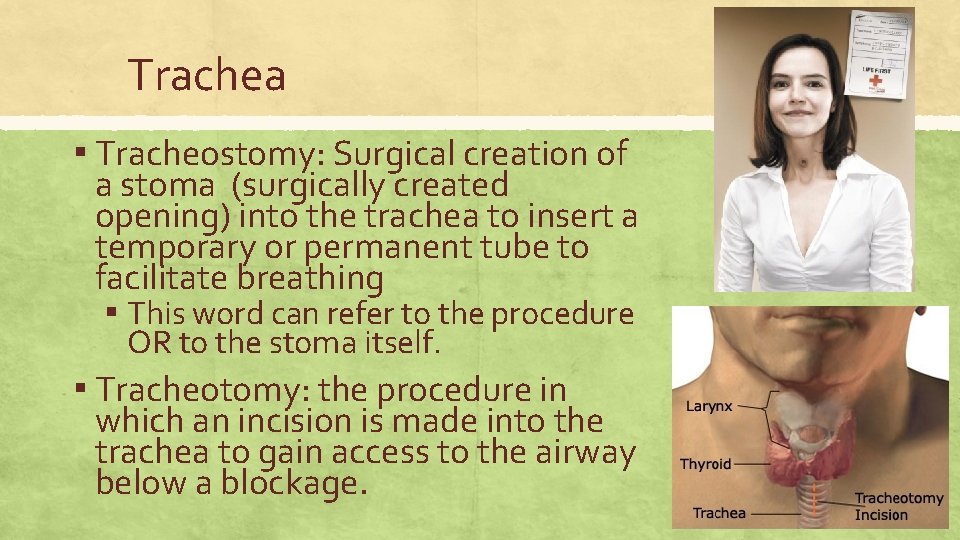
Trachea ▪ Tracheostomy: Surgical creation of a stoma (surgically created opening) into the trachea to insert a temporary or permanent tube to facilitate breathing ▪ This word can refer to the procedure OR to the stoma itself. ▪ Tracheotomy: the procedure in which an incision is made into the trachea to gain access to the airway below a blockage.
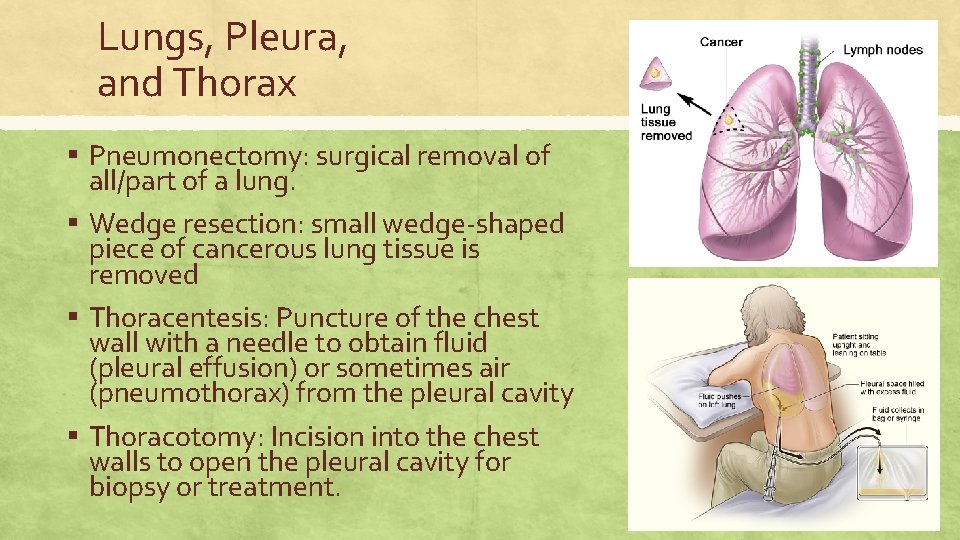
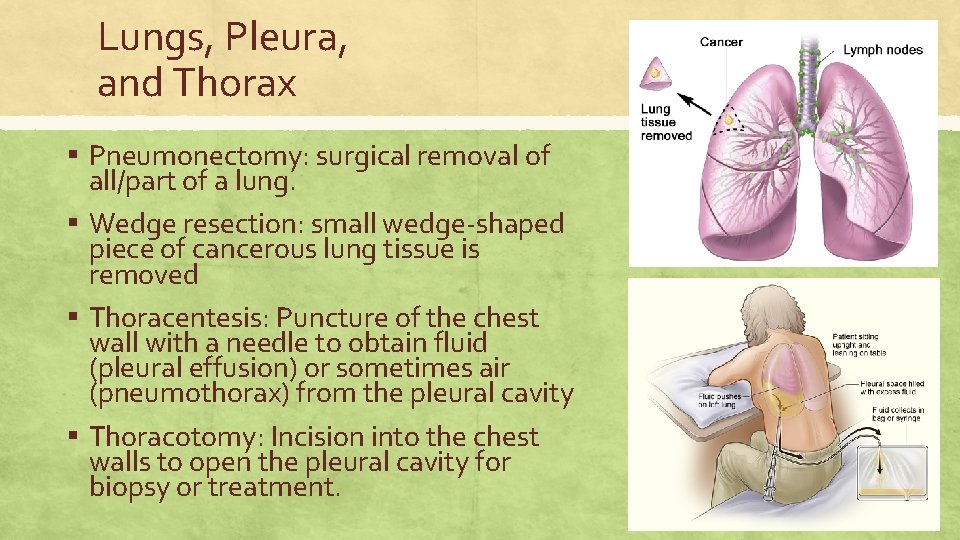
Lungs, Pleura, and Thorax ▪ Pneumonectomy: surgical removal of all/part of a lung. ▪ Wedge resection: small wedge-shaped piece of cancerous lung tissue is removed ▪ Thoracentesis: Puncture of the chest wall with a needle to obtain fluid (pleural effusion) or sometimes air (pneumothorax) from the pleural cavity ▪ Thoracotomy: Incision into the chest walls to open the pleural cavity for biopsy or treatment.
Respiratory Therapy ▪ Diaphragmatic breathing: AKA abdominal breathing. Relaxation technique (click for link to video) ▪ CPAP: Continuous Positive Airway Pressure; tx sleep apnea ▪ Ventilator: AKA “Respirator” mechanical device for artificial respiration. ▪ Hyperbaric oxygen therapy: breathing pure O 2 in a high pressure chamber. Promotes healing and fights infection. Also for scuba divers with decompression sickness