Chapter 67 Musculoskeletal Care Modalities 1 Cast A
- Slides: 30
Chapter 67 Musculoskeletal Care Modalities 1
Cast A rigid, external immobilizing device n Uses n Immobilize a reduced fracture n Correct a deformity n Apply uniform pressure to soft tissues n Support to stabilize a joint n n Materials—nonplaster (fiberglass), plaster 2
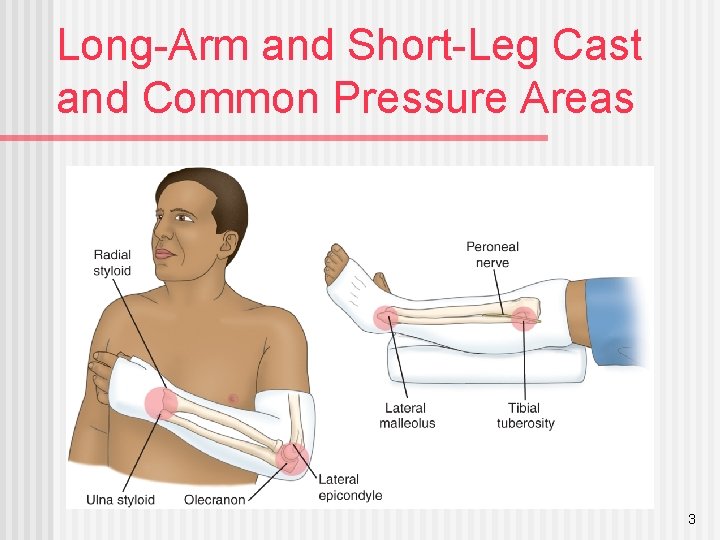
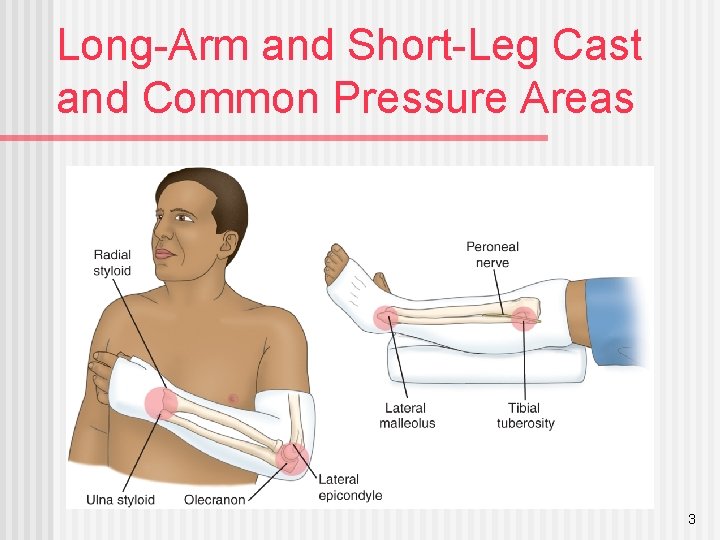
Long-Arm and Short-Leg Cast and Common Pressure Areas 3
Teaching Needs of the Patient with a Cast or Splint Exercises n Do not scratch or stick anything under cast n Cushion rough edges n Signs and symptoms to report: persistent pain or swelling, changes in sensation, movement, skin color or temperature, signs of infection or pressure areas n Required follow-up care n Cast removal n 4
Collaborative Problems/Potential Complications Compartment syndrome n Pressure ulcer n Disuse syndrome n Delayed union or nonunion of fracture(s) n 5
Interventions n n Relieving pain n Elevation to reduce edema n Intermittent application of ice or cold n Positioning changes n Administration of analgesics Note: Unrelieved pain may indicate compartment syndrome; discomfort due to pressure may require change of cast Muscle-setting exercises Patient teaching 6
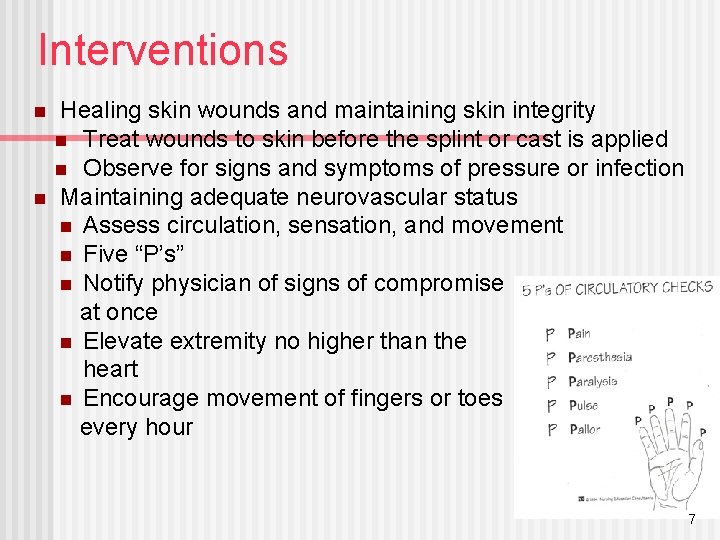
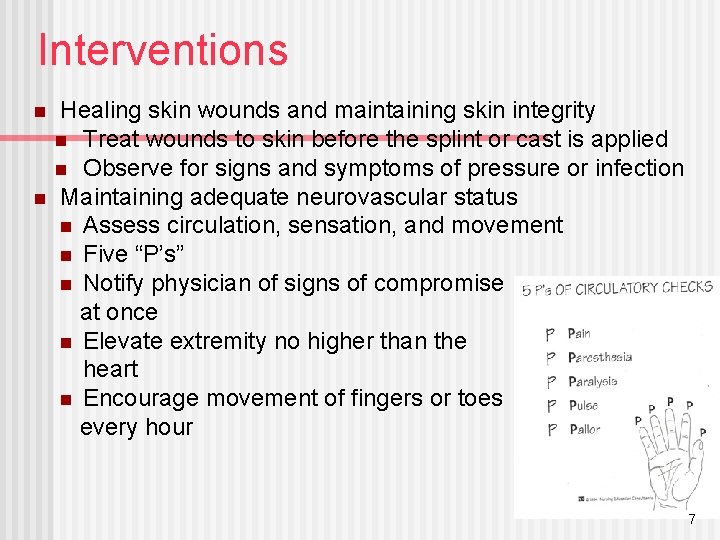
Interventions n n Healing skin wounds and maintaining skin integrity n Treat wounds to skin before the splint or cast is applied n Observe for signs and symptoms of pressure or infection Maintaining adequate neurovascular status n Assess circulation, sensation, and movement n Five “P’s” n Notify physician of signs of compromise at once n Elevate extremity no higher than the heart n Encourage movement of fingers or toes every hour 7
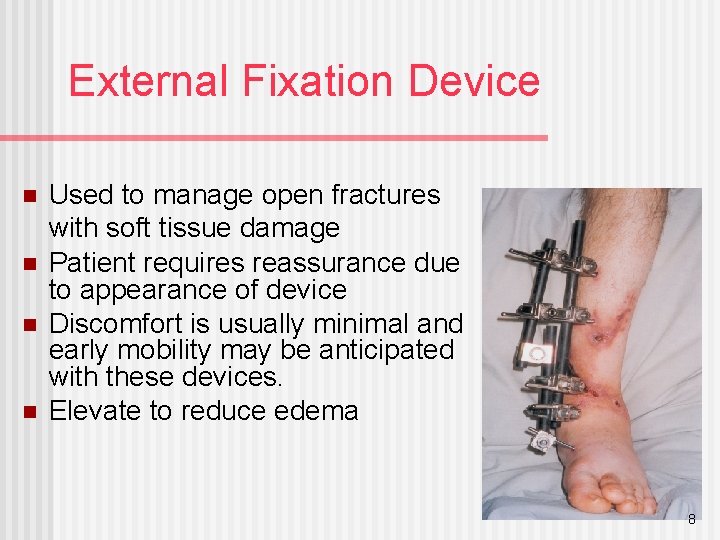
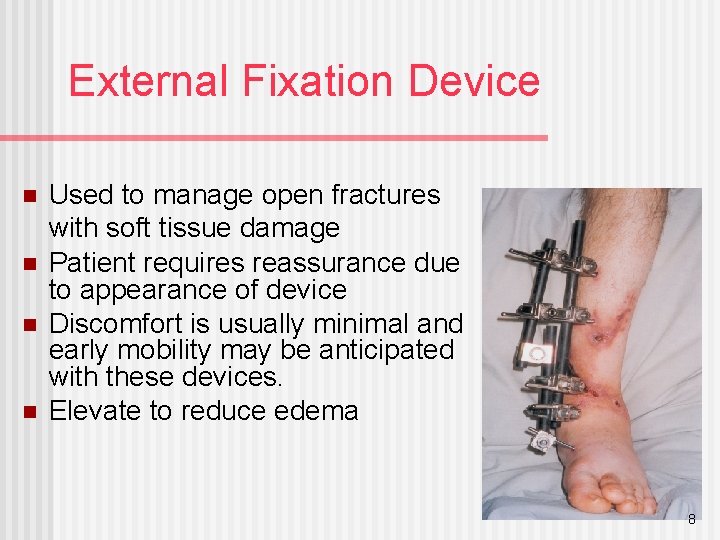
External Fixation Device n n Used to manage open fractures with soft tissue damage Patient requires reassurance due to appearance of device Discomfort is usually minimal and early mobility may be anticipated with these devices. Elevate to reduce edema 8
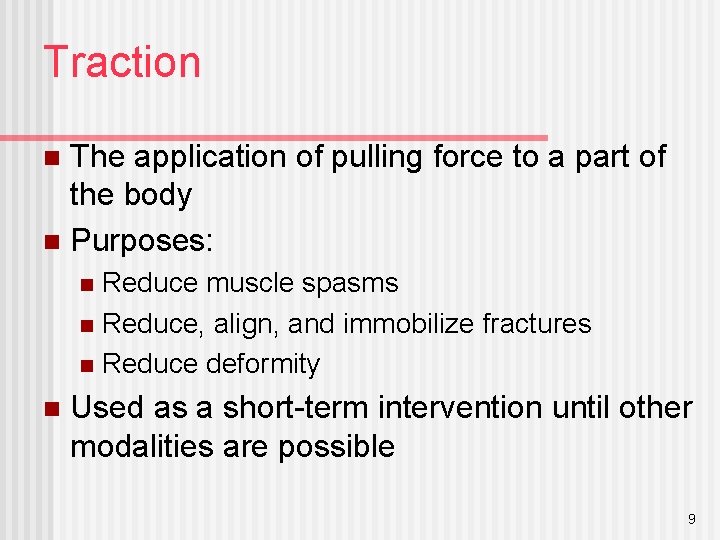
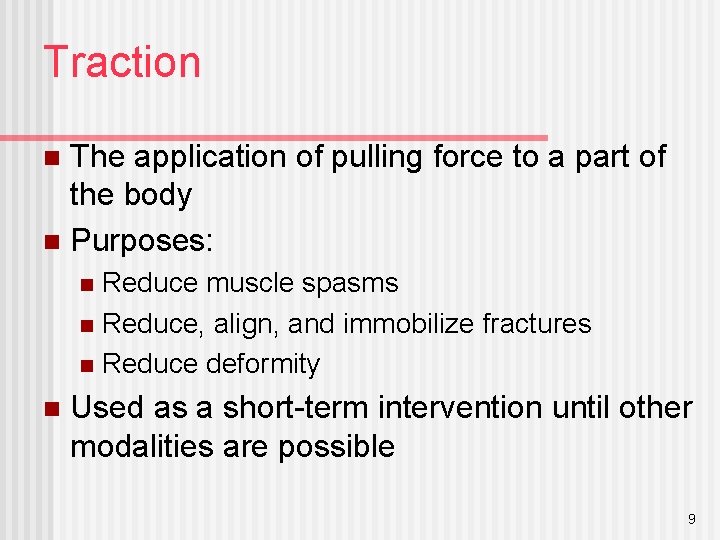
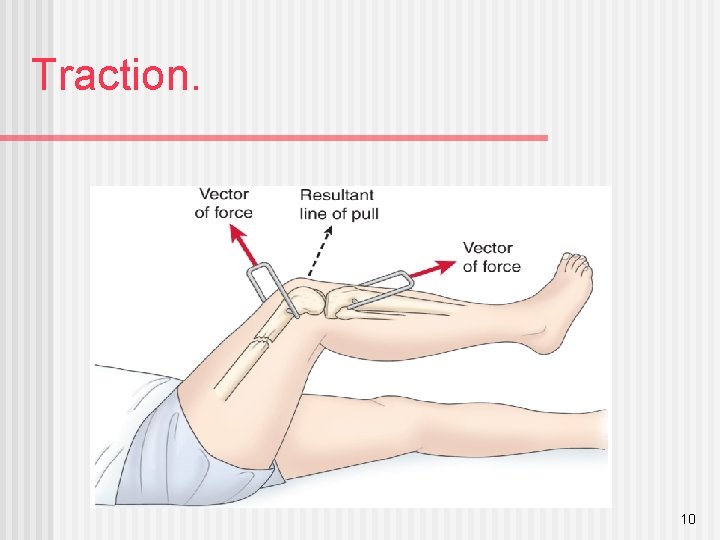
Traction The application of pulling force to a part of the body n Purposes: n Reduce muscle spasms n Reduce, align, and immobilize fractures n Reduce deformity n n Used as a short-term intervention until other modalities are possible 9
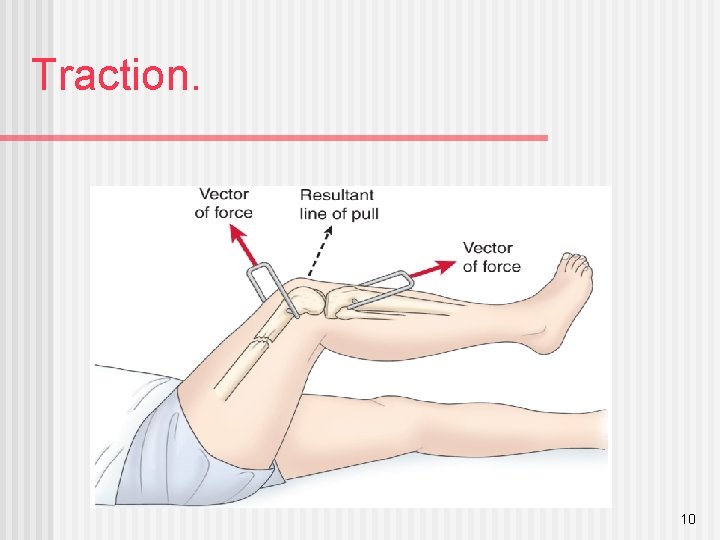
Traction. 10
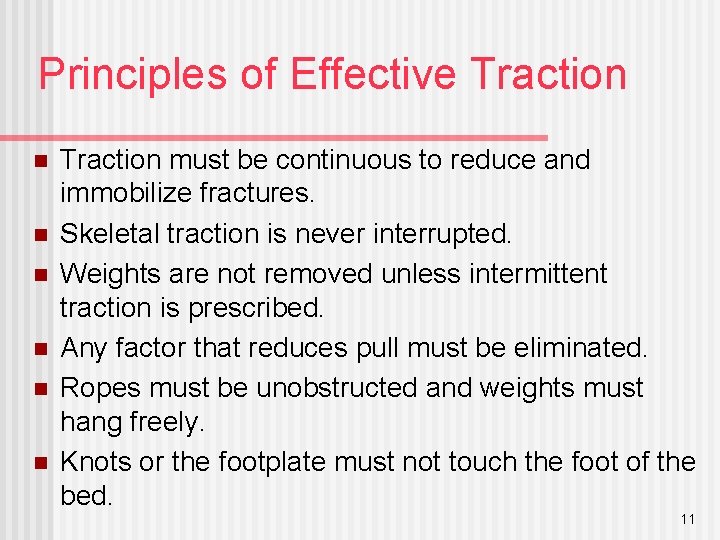
Principles of Effective Traction n n n Traction must be continuous to reduce and immobilize fractures. Skeletal traction is never interrupted. Weights are not removed unless intermittent traction is prescribed. Any factor that reduces pull must be eliminated. Ropes must be unobstructed and weights must hang freely. Knots or the footplate must not touch the foot of the bed. 11
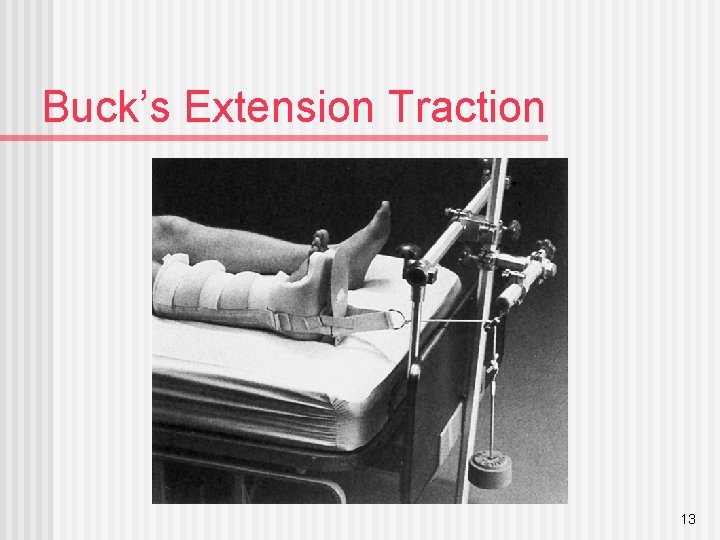
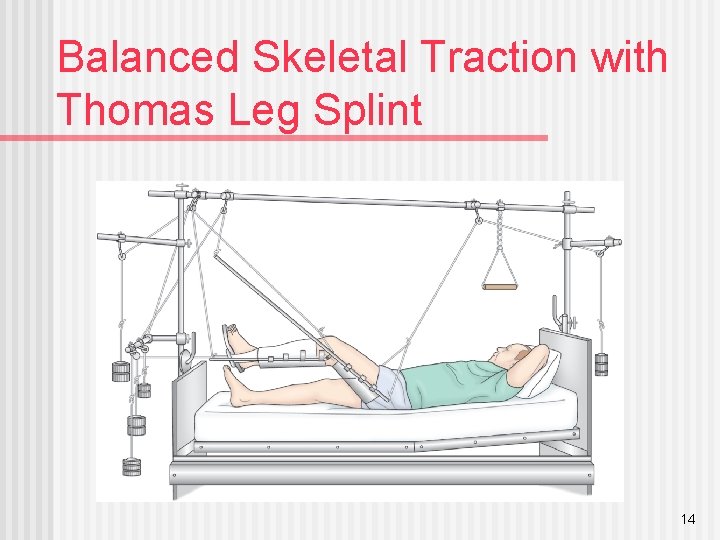
Types of Traction n Skin traction Buck’s extension traction n Cervical head halter n Pelvic traction n n Skeletal traction 12
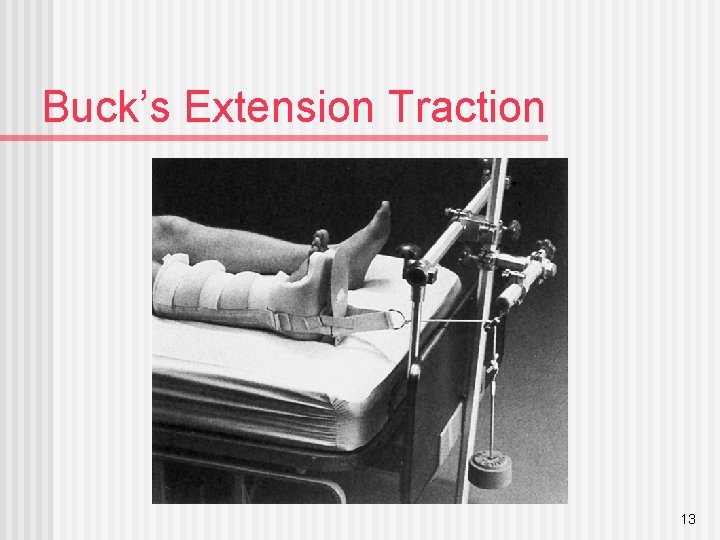
Buck’s Extension Traction 13
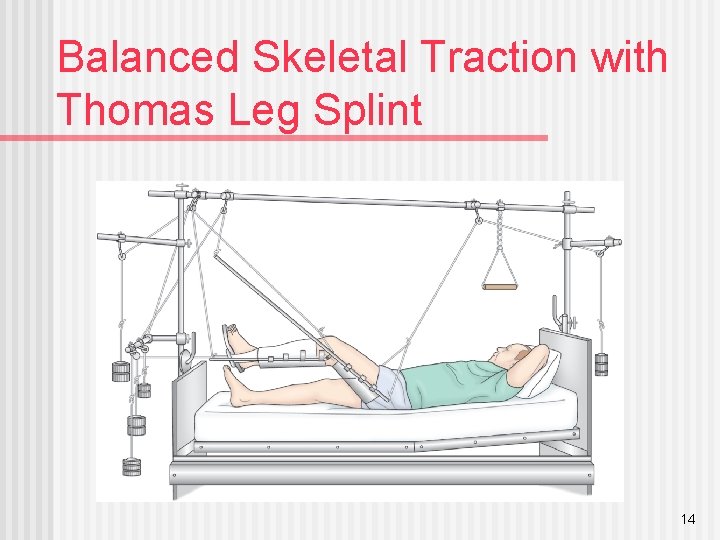
Balanced Skeletal Traction with Thomas Leg Splint 14
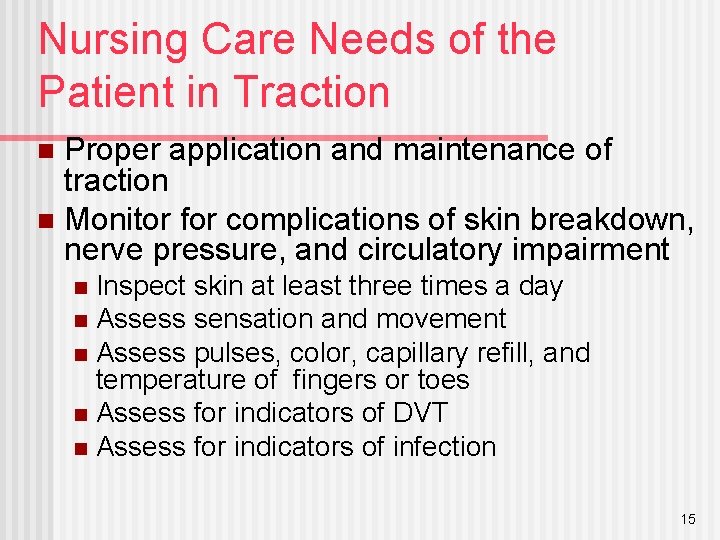
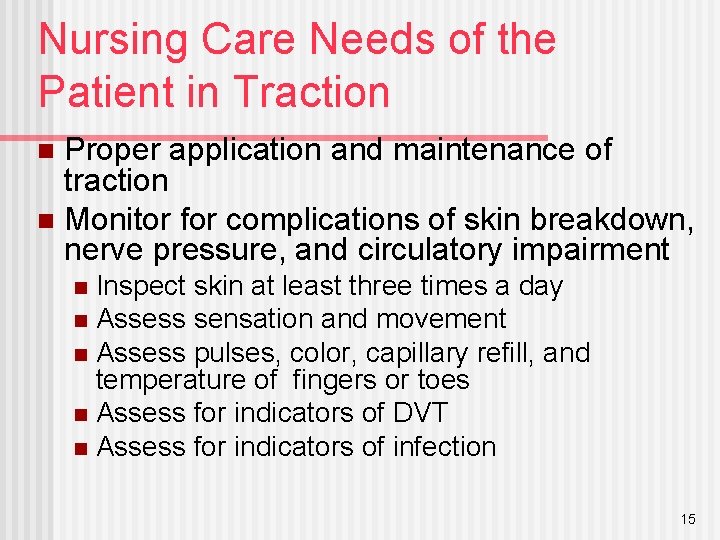
Nursing Care Needs of the Patient in Traction Proper application and maintenance of traction n Monitor for complications of skin breakdown, nerve pressure, and circulatory impairment n Inspect skin at least three times a day n Assess sensation and movement n Assess pulses, color, capillary refill, and temperature of fingers or toes n Assess for indicators of DVT n Assess for indicators of infection n 15
Preventative Interventions n n n n n Promptly report any alteration in sensation or circulation Frequent back care and skin care Regular shifting of position Special mattresses or other pressure reduction devices Perform active foot exercises and leg exercises every hour Elastic hose, pneumatic compression hose, or anticoagulant therapy may be prescribed Trapeze to help with movement for patients in skeletal traction Pin care Exercises to maintain muscle tone and strength 16
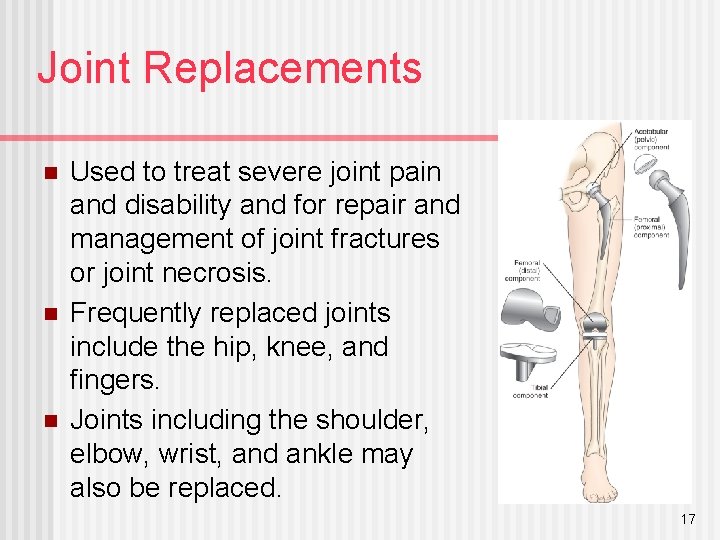
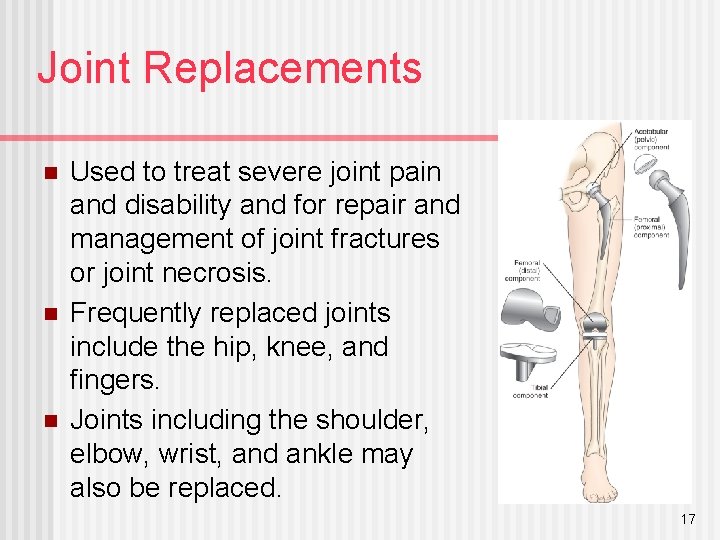
Joint Replacements n n n Used to treat severe joint pain and disability and for repair and management of joint fractures or joint necrosis. Frequently replaced joints include the hip, knee, and fingers. Joints including the shoulder, elbow, wrist, and ankle may also be replaced. 17
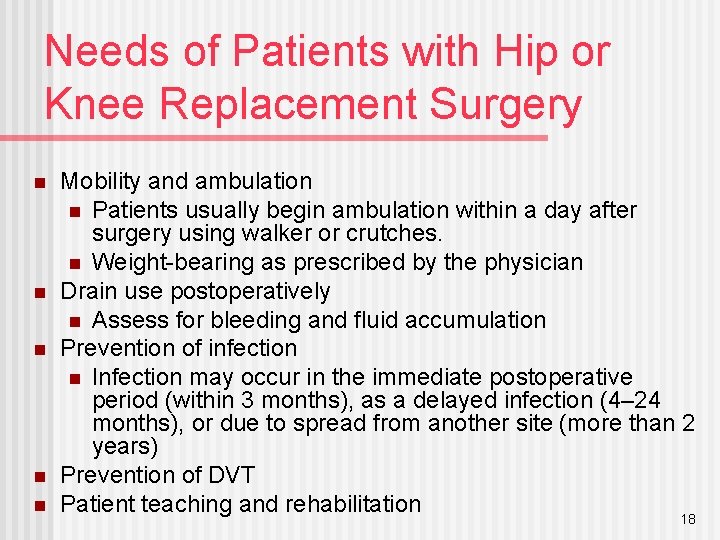
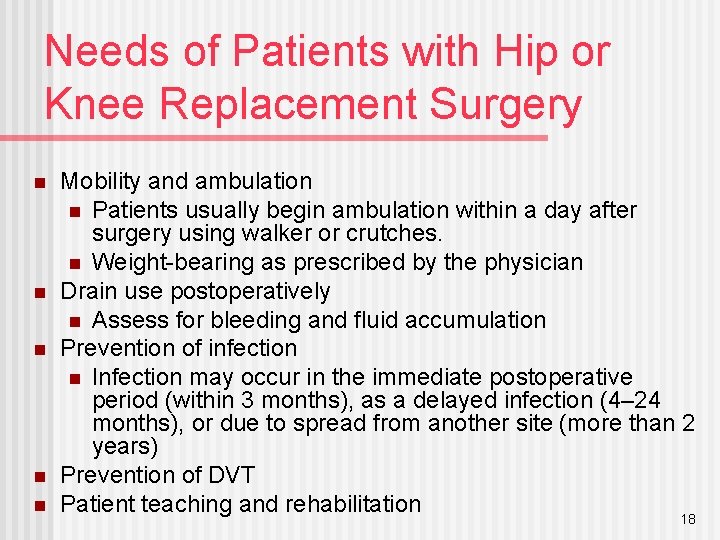
Needs of Patients with Hip or Knee Replacement Surgery n n n Mobility and ambulation n Patients usually begin ambulation within a day after surgery using walker or crutches. n Weight-bearing as prescribed by the physician Drain use postoperatively n Assess for bleeding and fluid accumulation Prevention of infection n Infection may occur in the immediate postoperative period (within 3 months), as a delayed infection (4– 24 months), or due to spread from another site (more than 2 years) Prevention of DVT Patient teaching and rehabilitation 18
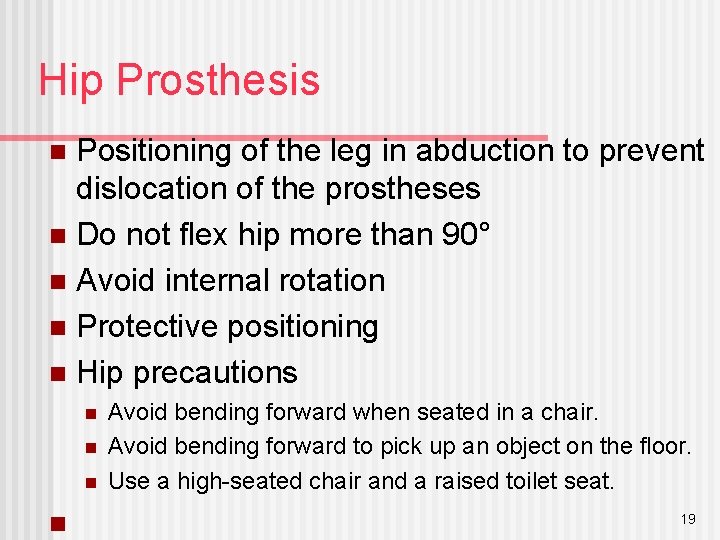
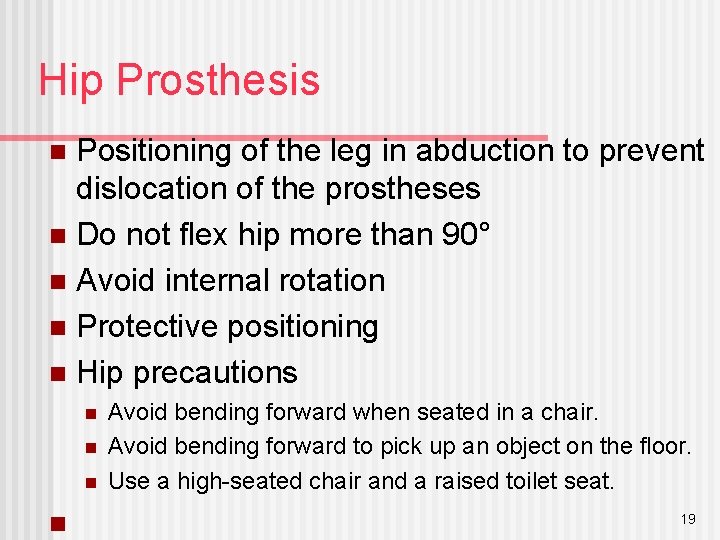
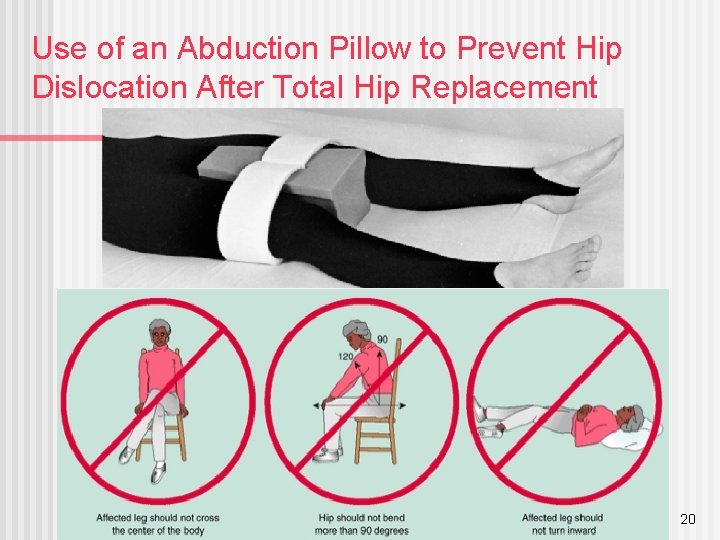
Hip Prosthesis Positioning of the leg in abduction to prevent dislocation of the prostheses n Do not flex hip more than 90° n Avoid internal rotation n Protective positioning n Hip precautions n n n Avoid bending forward when seated in a chair. Avoid bending forward to pick up an object on the floor. Use a high-seated chair and a raised toilet seat. 19
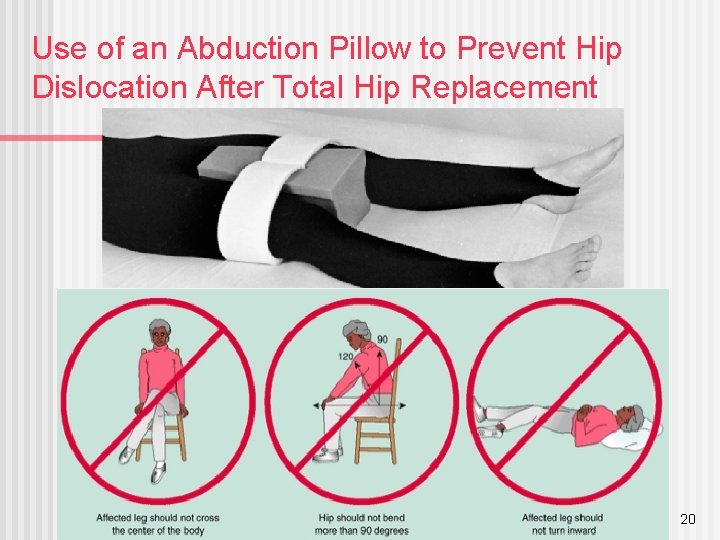
Use of an Abduction Pillow to Prevent Hip Dislocation After Total Hip Replacement 20
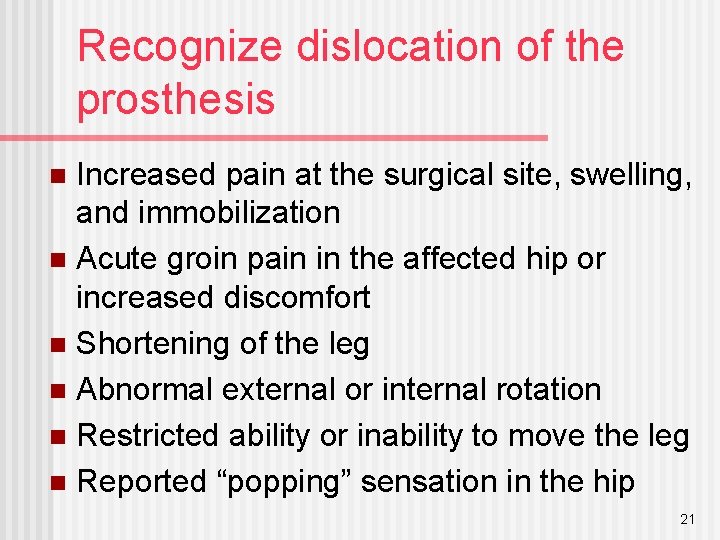
Recognize dislocation of the prosthesis Increased pain at the surgical site, swelling, and immobilization n Acute groin pain in the affected hip or increased discomfort n Shortening of the leg n Abnormal external or internal rotation n Restricted ability or inability to move the leg n Reported “popping” sensation in the hip n 21
Knee Prostheses The knee is dressed with a compression bandage. n Ice may be applied to control edema and bleeding. n Encourage active flexion exercises n Use of continuous passive motion (CPM) device n 22
Nursing Process: The Care of the Patient Undergoing Orthopedic Surgery— Assessment, Preoperative Routine preoperative assessment n Hydration status n Medication history n Possible infection n n Ask specifically about colds, dental problems, urinary tract infections, infections within 2 weeks Knowledge n Support and coping n 23
Nursing Process: The Care of the Patient Undergoing Orthopedic Surgery— Assessment, Postoperative n n n n n Pain Vital signs, including respirations and breath sounds LOC Neurovascular status and tissue perfusion Signs and symptoms of bleeding—wound drainage Mobility and understanding of mobility restrictions Bowel sounds and bowel elimination Urinary output Signs and symptoms of complications—DVT or infection 24
Nursing Process: The Care of the Patient Undergoing Orthopedic Surgery—Diagnoses Acute pain n Risk for peripheral neurovascular dysfunction n Risk for ineffective therapeutic regimen management n Impaired physical mobility n Risk for situational low self-esteem and/or disturbed body image n 25
Collaborative Problems/Potential Complications—Postoperative Hypovolemic shock n Atelectasis n Pneumonia n Urinary retention n Infection n Thromboembolism—DVT or PE n Constipation or fecal impaction n 26
Nursing Process: The Care of the Patient Undergoing Orthopedic Surgery—Planning Major goals preoperatively and postoperatively may include the relief of pain, adequate neurovascular function, health promotion, improved mobility, and positive self-esteem. n Postoperative goals include the absence of complications. n 27
Relief of Pain n Administration of medications Patient-controlled analgesia (PCA) n Other medications n Medicate before planned activity and ambulation n n Use alternative methods of pain relief n n Repositioning, distraction, guided imagery. etc. Specific individualized strategies to control pain Use of ice or cold n Elevation n Immobilization n 28
Interventions n n n Muscle setting, ankle and calf-pumping exercises Measures to ensure adequate nutrition and hydration Note: Large amounts of milk should not be given to orthopedic patients on bed rest Skin care measures including frequent turning and positioning Follow physical therapy and rehabilitation programs Encourage the patient to set realistic goals and perform self-care within limits of therapeutic regimen 29
Interventions n Preventing atelectasis and pneumonia Encourage coughing and deep breathing exercises n Use of incentive spirometry n n Constipation Monitoring of bowel function n Hydration n Early mobilization n Stool softeners n n Patient teaching 30