Chapter 6 Innate Immunity Inflammation and Wound Healing


- Slides: 55
Chapter 6 Innate Immunity: Inflammation and Wound Healing Copyright © 2017, Elsevier Inc. All rights reserved.

Immunity First line of defense Ø Second line of defense Ø Innate (natural) (native) immunity • Physical, mechanical, biochemical barriers Inflammation Third line of defense Ø Adaptive (acquired) (specific) immunity Copyright © 2017, Elsevier Inc. All rights reserved. 2
First Line of Defense Physical barriers: Skin Ø Linings of the gastrointestinal, genitourinary, and respiratory tracts • Sloughing off of cells • Coughing and sneezing • Flushing—urine • Vomiting • Mucus and cilia Ø Copyright © 2017, Elsevier Inc. All rights reserved. 3
First Line of Defense (Cont. ) Epithelial cell-derived chemical barriers: Secrete saliva, tears, earwax, sweat, and mucus Ø Antimicrobial peptides • Cathelicidins, defensins, collectins, and mannose-binding Ø lectin Normal microbiome Ø Each surface colonized by bacteria and fungi that is unique to the particular location and individual Copyright © 2017, Elsevier Inc. All rights reserved. 4
Second Line of Defense Inflammatory response (first immune response to injury) Nonspecific Ø Caused by a variety of materials • Infection, tissue necrosis, trauma, physical or chemical Ø injury, foreign bodies, immune reaction, ischemia, etc. Ø Local manifestations • Redness, heat, swelling, pain, loss of function Copyright © 2017, Elsevier Inc. All rights reserved. 5
Second Line of Defense (Cont. ) Inflammatory response Ø Vascular responses: • Blood vessel dilation • Increased vascular permeability and leakage • White blood cell adherence to the inner walls of the vessels and migration through the vessels Copyright © 2017, Elsevier Inc. All rights reserved. 6
Inflammation Goals: Limit and control the inflammatory process Ø Prevent and limit infection and further damage Ø Initiate adaptive immune response Ø Initiate healing Ø Copyright © 2017, Elsevier Inc. All rights reserved. 7
Plasma Protein Systems Protein systems: Complement system Ø Clotting system Ø Kinin system Ø Copyright © 2017, Elsevier Inc. All rights reserved. 8
Plasma Protein Systems (Cont. ) All contain inactive enzymes (proenzymes) Ø Sequentially activated • First proenzyme is converted to an active enzyme • Substrate of the activated enzyme becomes the next component in the series (cascade) Copyright © 2017, Elsevier Inc. All rights reserved. 9
Plasma Protein Systems (Cont. ) Complement system Produces biologically active fragments that recruit phagocytes, activate mast cells, and destroy pathogens Ø Activation of C 3 and C 5 • Opsonins • Chemotactic factors • Anaphylatoxins Ø Pathways: • Classical • Lectin • Alternative Ø Copyright © 2017, Elsevier Inc. All rights reserved. 10
Plasma Protein Systems (Cont. ) Coagulation (clotting) system Forms a fibrinous meshwork at an injured or inflamed site • Prevents the spread of infection • Localizes microorganisms and foreign bodies • Forms a clot that stops bleeding • Provides a framework for repair and healing Ø Main substance is an insoluble protein called fibrin Ø Extrinsic pathway Ø Intrinsic pathway Ø Copyright © 2017, Elsevier Inc. All rights reserved. 11
Plasma Protein Systems (Cont. ) Kinin system Functions to activate and assist inflammatory cells Ø Primary kinin is bradykinin Ø Causes dilation of blood vessels, pain, and smooth muscle contraction; increases vascular permeability Ø Copyright © 2017, Elsevier Inc. All rights reserved. 12
Plasma Protein Systems (Cont. ) Control and interaction of plasma protein systems Tight regulation is essential Ø Multiple mechanisms are available to either activate or inactivate (regulate) these plasma protein systems Ø Copyright © 2017, Elsevier Inc. All rights reserved. 13
Cellular Components of Inflammation Cellular components: Erythrocytes Ø Platelets Ø Leukocytes • Granulocytes • Monocytes • Lymphocytes Ø Copyright © 2017, Elsevier Inc. All rights reserved. 14
Cellular Components of Inflammation (Cont. ) Cellular receptors: Pattern recognition receptors (PRRs) Ø Pathogen-associated molecular patterns (PAMPs) Ø Damage-associated molecular patterns Ø Toll-like receptors Ø Complement receptors Ø Scavenger receptors Ø NOD-like receptors Ø Copyright © 2017, Elsevier Inc. All rights reserved. 15
Cytokines Responsible for activating other cells and regulating inflammatory response Ø Chemokines • Synthesized by many cells (macrophages, fibroblasts, endothelial cells) in response to proinflammatory cytokines • Induce chemotaxis to promote phagocytosis and wound healing • Examples: Monocyte/macrophage chemotactic proteins Macrophage inflammatory proteins Neutrophils Copyright © 2017, Elsevier Inc. All rights reserved. 16
Cytokines (Cont. ) Ø Interleukins (IL) • Produced primarily by macrophages and lymphocytes in response to stimulation of PRRs or by other cytokines • Many types • Examples: IL-1 is proinflammatory IL-10 is anti-inflammatory Copyright © 2017, Elsevier Inc. All rights reserved. 17
Cytokines (Cont. ) Tumor necrosis factor-alpha Ø Secreted by macrophages in response to PAMP and toll-like receptor recognition • Induces fever by acting as an endogenous pyrogen • Increases synthesis of inflammatory serum proteins • Causes muscle wasting (cachexia) and intravascular thrombosis Ø Very high levels can be lethal Copyright © 2017, Elsevier Inc. All rights reserved. 18
Cytokines (Cont. ) Interferon (IFN) Protects against viral infections Ø Produced and released by virally infected host cells in response to viral double-stranded RNA • Protects neighboring healthy cells Ø Types: • IFN-α and IFN-β Ø Induce production of antiviral proteins • IFN- Increases microbiocidal activity of macrophages Copyright © 2017, Elsevier Inc. All rights reserved. 19
Mast Cells and Basophils Mast cells are cellular bags of granules located in the loose connective tissues close to blood vessels Skin, digestive lining, and respiratory tract Ø Contain histamine, cytokines, and chemotaxic factors Ø Basophils are found in blood and probably function in same way as mast cells Copyright © 2017, Elsevier Inc. All rights reserved. 20
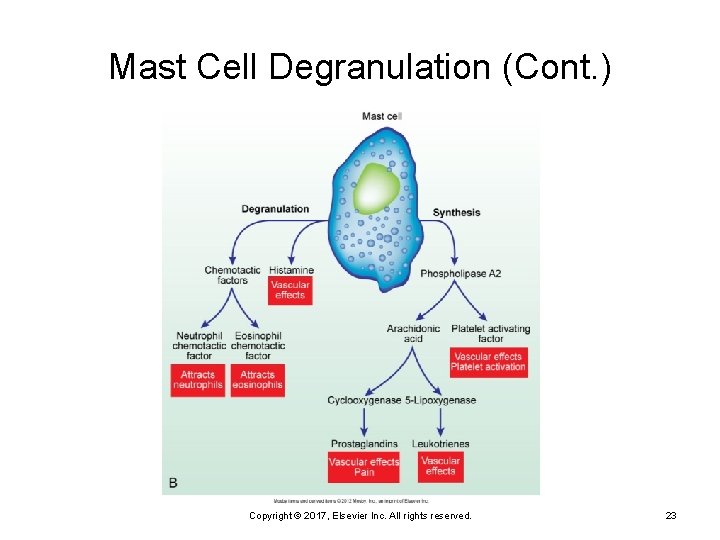
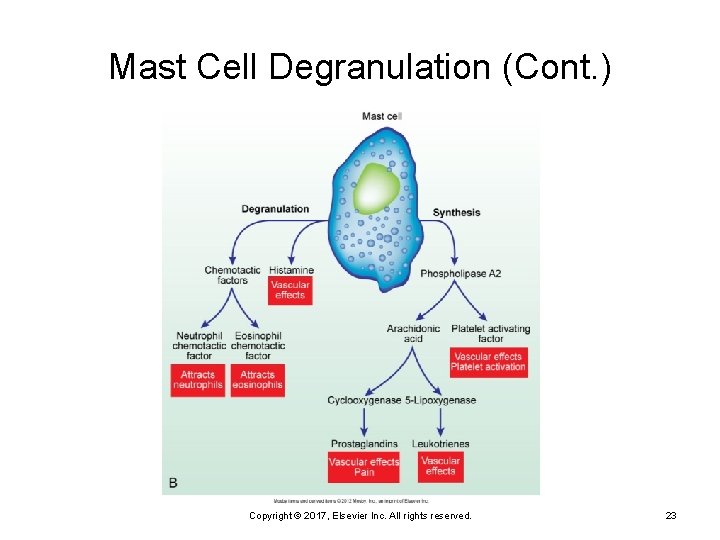
Mast Cells and Basophils (Cont. ) Chemical release in two ways Degranulation • The release of the contents of mast cell granules Ø Synthesis • The new production and release of mediators in Ø response to a stimulus Copyright © 2017, Elsevier Inc. All rights reserved. 21
Mast Cell Degranulation Histamine Vasoactive amine that causes temporary, rapid constriction of the large blood vessels and the dilation of the postcapillary venules Ø Retraction of endothelial cells lining the capillaries Ø Copyright © 2017, Elsevier Inc. All rights reserved. 22
Mast Cell Degranulation (Cont. ) Copyright © 2017, Elsevier Inc. All rights reserved. 23
Histamine Receptors: H 1 receptor • Proinflammatory • Present in smooth muscle cells of the bronchi Ø H 2 receptor • Anti-inflammatory • Present on parietal cells of the stomach mucosa Ø Induces the secretion of gastric acid Copyright © 2017, Elsevier Inc. All rights reserved. 24
Degranulation Chemotactic factors: Neutrophil chemotactic factor • Attracts neutrophils Ø Eosinophil chemotactic factor of anaphylaxis (ECF -A) • Attracts eosinophils Ø Copyright © 2017, Elsevier Inc. All rights reserved. 25
Synthesis of Mediators Leukotrienes Product of arachidonic acid from mast cell membranes Ø Similar effects to histamine in later stages Ø Prostaglandins Similar effects to leukotrienes; they also induce pain Ø Aspirin and some other nonsteroidal anti-inflammatory drugs (NSAIDs) block the synthesis of prostaglandins, thereby inhibiting inflammation and pain Ø Platelet-activating factor Ø Similar effect to leukotrienes and platelet activation Copyright © 2017, Elsevier Inc. All rights reserved. 26
Endothelium Endothelial cells adhere to underlying connective tissue matrix Interact with circulating cells, platelets, plasma proteins Ø Regulate circulating inflammatory components Ø Damage to these initiates platelet adherence Ø Copyright © 2017, Elsevier Inc. All rights reserved. 27
Platelets Activated by tissue destruction and inflammation Activation leads to interaction with coagulation cascade to stop bleeding Ø Degranulation with serotonin release (acts like histamine) Copyright © 2017, Elsevier Inc. All rights reserved. 28
Phagocytes Neutrophils Also referred to as polymorphonuclear neutrophils (PMNs) Ø Predominate in early inflammatory responses Ø Ingest bacteria, dead cells, and cellular debris Ø Cells are short lived and become a component of the purulent exudate Ø Copyright © 2017, Elsevier Inc. All rights reserved. 29
Phagocytes (Cont. ) Eosinophils Mildly phagocytic Ø Defense against parasites and regulation of vascular mediators Ø Basophils Least prevalent granulocytes Ø Primary role unknown Ø Copyright © 2017, Elsevier Inc. All rights reserved. 30
Phagocytes (Cont. ) Monocytes and macrophages Monocytes are produced in the bone marrow, enter the circulation, and migrate to the inflammatory site, where they develop into macrophages Ø Macrophages typically arrive at the inflammatory site 24 hours or later after neutrophils Ø Copyright © 2017, Elsevier Inc. All rights reserved. 31
Phagocytes (Cont. ) Dendritic cells In peripheral organs and skin Ø Migrate through lymph vessels to lymph tissue and interact with T lymphocytes to generate an acquired immune response Ø Copyright © 2017, Elsevier Inc. All rights reserved. 32
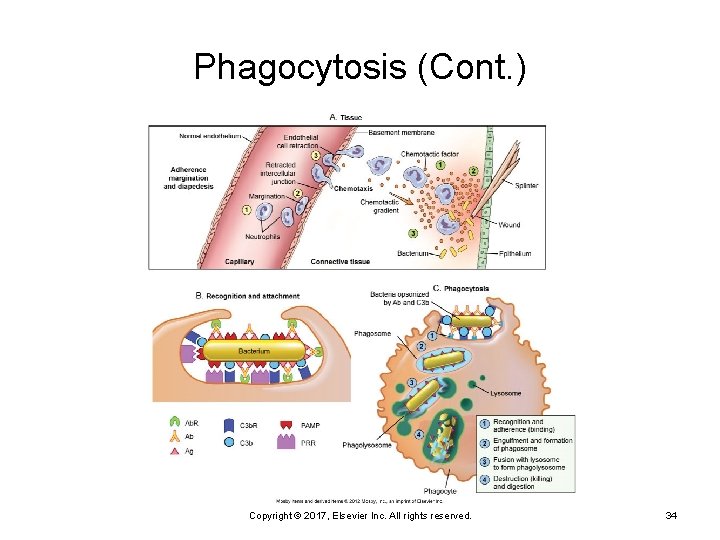
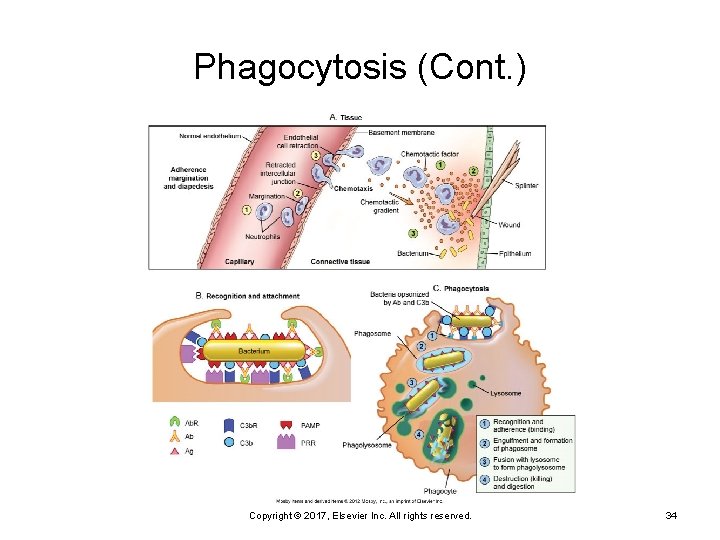
Phagocytosis Process by which a cell ingests and disposes of foreign material Production of adhesion molecules Margination (pavementing) Ø Adherence of leukocytes to endothelial cells Diapedesis Ø Emigration of cells through the endothelial junctions Copyright © 2017, Elsevier Inc. All rights reserved. 33
Phagocytosis (Cont. ) Copyright © 2017, Elsevier Inc. All rights reserved. 34
Phagocytosis (Cont. ) Steps: Adherence Ø Engulfment Ø Phagosome formation Ø Fusion with lysosomal granules Ø Destruction of the target Ø Copyright © 2017, Elsevier Inc. All rights reserved. 35
Natural Killer Cells Recognize and eliminate cells infected with viruses Inhibitory and activating receptors to allow differentiation between normal and abnormal cells Produce cytokines and toxic molecules Copyright © 2017, Elsevier Inc. All rights reserved. 36
Acute and Chronic Inflammation Acute Self-limiting Ø Local manifestations—result from vascular changes and corresponding leakage of circulating components into the tissue • Heat, swelling, redness, pain • Exudative fluids Ø Copyright © 2017, Elsevier Inc. All rights reserved. 37
Exudative Fluids Serous exudate Ø Fibrinous exudate Ø Thick, clotted exudate: indicates more advanced inflammation Purulent exudate (suppurative) Ø Watery exudate: indicates early inflammation Pus: indicates a bacterial infection Hemorrhagic exudate Ø Exudate contains blood: indicates bleeding Copyright © 2017, Elsevier Inc. All rights reserved. 38
Systemic Manifestations of Acute Inflammation Fever Ø Caused by exogenous and endogenous pyrogens • Act directly on the hypothalamus Leukocytosis Ø Increased numbers of circulating leukocytes Copyright © 2017, Elsevier Inc. All rights reserved. 39
Systemic Manifestations of Acute Inflammation (Cont. ) Increased plasma protein synthesis Ø Acute-phase reactants: • C-reactive protein • Fibrinogen • Haptoglobin • Amyloid • Ceruloplasmin, etc. Copyright © 2017, Elsevier Inc. All rights reserved. 40
1. An injury to a vascularized tissue has occurred and activated an acute inflammatory response. Which of the following is TRUE regarding this response? It: A. B. C. D. Is nonspecific Is activated slowly Is the third line of defense Relies on cellular components only Copyright © 2017, Elsevier Inc. All rights reserved. 41
Chronic Inflammation lasting 2 weeks or longer Often related to an unsuccessful acute inflammatory response Ø Characterized by pus formation, suppuration, and incomplete wound healing Copyright © 2017, Elsevier Inc. All rights reserved. 42
Chronic Inflammation (Cont. ) Other causes of chronic inflammation: High lipid and wax content of a microorganism Ø Ability to survive inside the macrophage Ø Toxins Ø Chemicals, particulate matter, or physical irritants Ø Copyright © 2017, Elsevier Inc. All rights reserved. 43
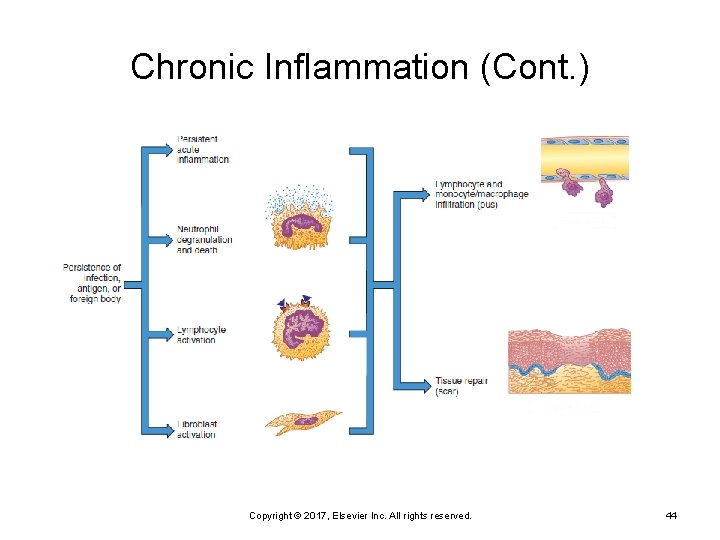
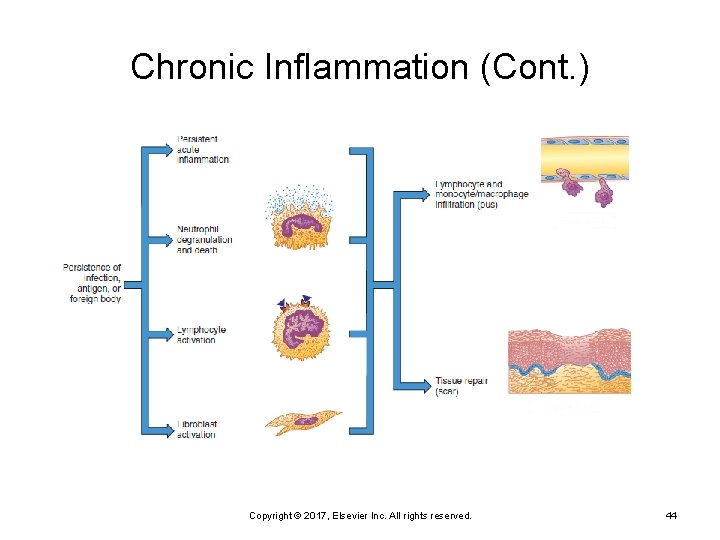
Chronic Inflammation (Cont. ) Copyright © 2017, Elsevier Inc. All rights reserved. 44
Chronic Inflammation (Cont. ) Characteristics: Dense infiltration of lymphocytes and macrophages Ø Granuloma formation Ø Epithelioid cell formation Ø Giant cell formation Ø Copyright © 2017, Elsevier Inc. All rights reserved. 45
Wound Healing Regeneration Resolution Ø Returning injured tissue to the original structure and function Repair Replacement of destroyed tissue with scar tissue Ø Scar tissue • Composed primarily of collagen to restore the strength of Ø the tissue but not its function Copyright © 2017, Elsevier Inc. All rights reserved. 46
Wound Healing (Cont. ) Healing Filling in the wound Ø Sealing the wound (epithelialization) Ø Shrinking the wound (contraction) Ø Copyright © 2017, Elsevier Inc. All rights reserved. 47
Wound Healing (Cont. ) Primary intention Ø Wounds that heal under conditions of minimal tissue loss Secondary intention Ø Wounds that require a great deal more tissue replacement • Open wound Copyright © 2017, Elsevier Inc. All rights reserved. 48
Wound Healing (Cont. ) Inflammation phase Coagulation Ø Infiltration of wound-healing cells Ø Angiogenesis Ø Copyright © 2017, Elsevier Inc. All rights reserved. 49
Wound Healing (Cont. ) Proliferative phase Granulation Ø Epithelialization Ø Requires fibroblast proliferation, collagen formation, wound contraction Ø Copyright © 2017, Elsevier Inc. All rights reserved. 50
Wound Healing (Cont. ) Remodeling and maturation phase Continuation of cellular differentiation Ø Scar tissue formation Ø Scar remodeling Ø Copyright © 2017, Elsevier Inc. All rights reserved. 51

Wound Healing (Cont. ) From Roberts JR, Custalow CB: Roberts and Hedges’ clinical procedures in emergency medicine, ed 6, Philadelphia, 2013, Saunders. Copyright © 2017, Elsevier Inc. All rights reserved. 52
Dysfunctional Wound Healing May occur during any phase of wound healing Ischemia Ø Excessive bleeding Ø Excessive fibrin deposition Ø Predisposing disorders • Diabetes • Obesity • Wound infection • Inadequate nutrients • Numerous drugs • Tobacco smoke Ø Copyright © 2017, Elsevier Inc. All rights reserved. 53
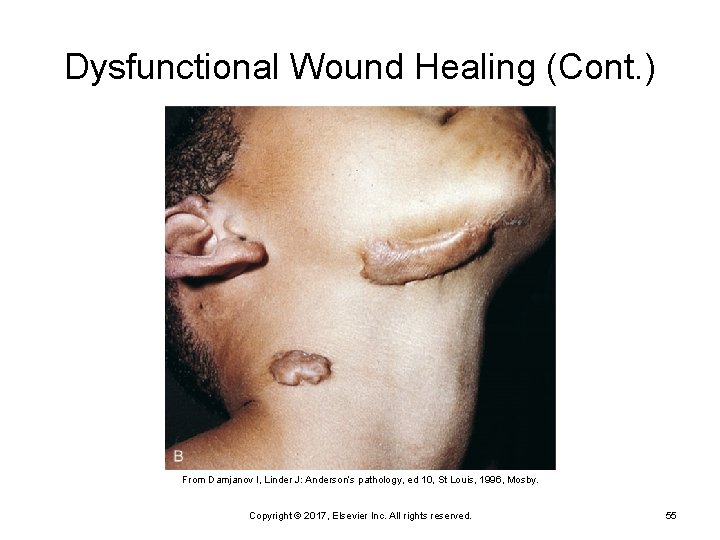
Dysfunctional Wound Healing (Cont. ) Dysfunction during reconstructive phase Dysfunctional collagen synthesis • Keloid scar • Hypertrophic scar Ø Wound disruption • Dehiscence (increases risk of infection) Ø Impaired contraction • Contracture Ø Copyright © 2017, Elsevier Inc. All rights reserved. 54
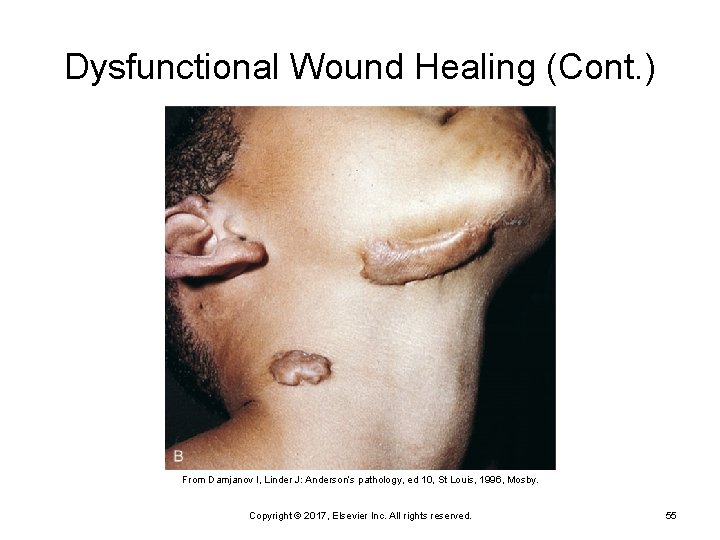
Dysfunctional Wound Healing (Cont. ) From Damjanov I, Linder J: Anderson’s pathology, ed 10, St Louis, 1996, Mosby. Copyright © 2017, Elsevier Inc. All rights reserved. 55