CHAPTER 6 INFECTION CONTROL Roosevelt Health Science Clinical

- Slides: 29
CHAPTER 6: INFECTION CONTROL Roosevelt Health Science Clinical Rotations Successful Nursing Assistant Care, 2 nd Ed.
Chapter 6 Objectives • Define important words • • Define “infection control” and discuss types of infections Discuss the use of Personal Protective Equipment (PPE) • • Discuss terms related to infection control List guidelines for handling linen and equipment • Explain how to handle spills • Describe the chain of infection • Discuss Transmission-Based Precautions • Explain why the elderly are at high risk for infection • Describe care of the resident in an isolation unit • Describe the CDC and explain Standard Precautions • Explain OSHA’s Bloodborne Pathogen Standard • Define “hand hygiene” and identify when to wash hands. • Discuss two important bloodborne diseases • Discuss MRSA, VRE, and C. Difficile
Infection Control • Communities strive to maintain clean conditions in order to help prevent the spread of disease. • This is known as sanitation. • Infection Control- the set of methods used to control and prevent the spread of disease. • It is the responsibility of all members of the care team • Know the facility policies on infection control and follow them to protect you, patients, visitors, and other staff members. • By using proper infection control methods, you can prevent all people in your care, as well as other staff members and visitors, from acquiring an infection from someone else. • This is called cross-infection or cross-contamination • Also prevents residents from being infected a second time, called reinfection
Infections • Microorganism (MO) is a tiny living thing visible only by a microscope. • Also known as a microbe • They are always present in the environment, though many are not harmful. • Bacteria, viruses, fungi, protozoa are types of MOs • Pathogens are harmful microorganisms that can cause infections or infectious disease. • For infections to develop, pathogens must invade and grow within the human body. • Grow best in warm, dark, and moist places where food is present, and in hosts who have low resistance. • Some MOs need to survive, while others do not.
Types of Infections • A localized infection is limited to a specific part of the body. It has local symptoms, near the site of infection. • For example, eye infections could be red, swollen, painful, and warm to the touch. • S/Sx include redness, swelling, pain, heat, drainage (fluid from a wound or cavity). • A systemic infection occurs when pathogens enter the bloodstream and move throughout the body, causing generalized symptoms. • Acquired Immune Deficiency Syndrome (AIDS) is an example • S/Sx include fever, chills, headache, change in other vital signs, nausea, vomiting, diarrhea, mental confusion.
Types of Infections • As special type of infection that can be localized or systemic is a healthcare-associated infection (HAI), an infection associated with various healthcare setting, including long-term care facilities, hospitals, ambulatory settings and home care. • A second type of infection that can be localized or systemic is a nosocomial infection, which comes from a hospital. • Example: a resident gets a UTI from a urinary catheter after entering a facility. • Catheter- a tube inserted through the skin or into a body opening that is used to add or drain fluid. • HAIs and nosocomial infections can be mild or life-threatening • Report to nurse immediately
Infectious Disease • A communicable disease occurs when a pathogen is spread from one person to another. • Ex: Hepatitis, Influenza, Polio, TB, Malaria, etc. • A contagious disease is a communicable disease is spread easily from person to person. • Ex: STDs, MRSA, Varicella (Chicken Pox), etc. • A non-communicable disease is a disease not capable of being spread from one person to another. • Ex: Emphysema, Diabetes, Stroke, COPD, etc.
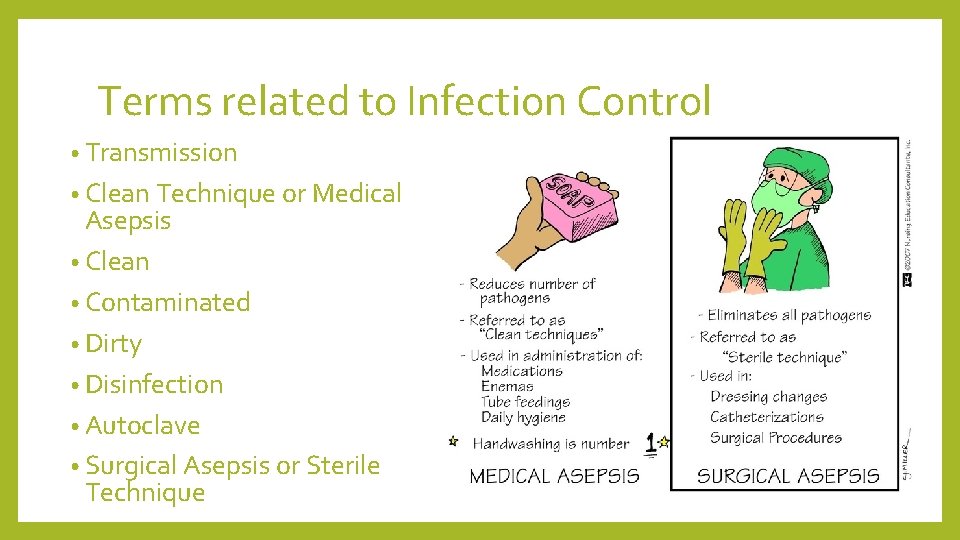
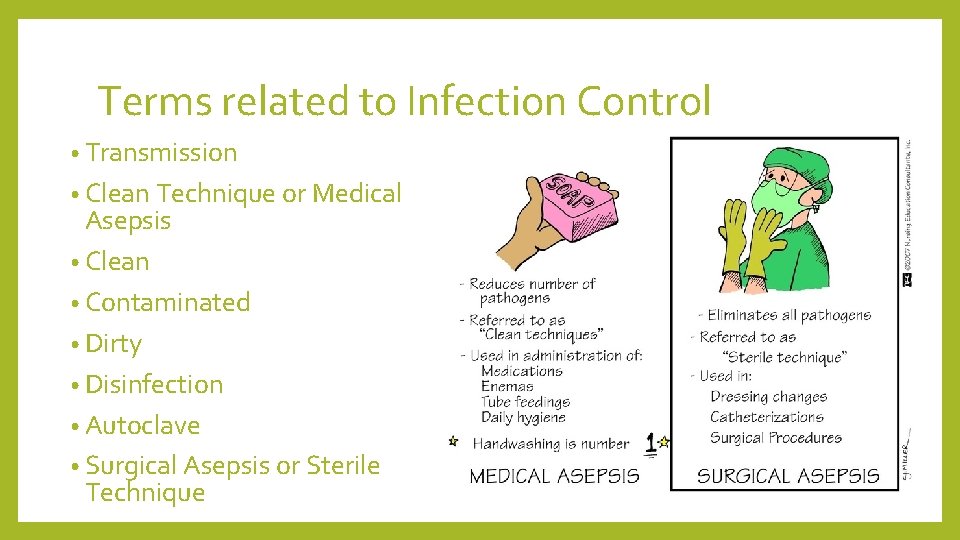
Terms related to Infection Control • Transmission • Clean Technique or Medical Asepsis • Clean • Contaminated • Dirty • Disinfection • Autoclave • Surgical Asepsis or Sterile Technique
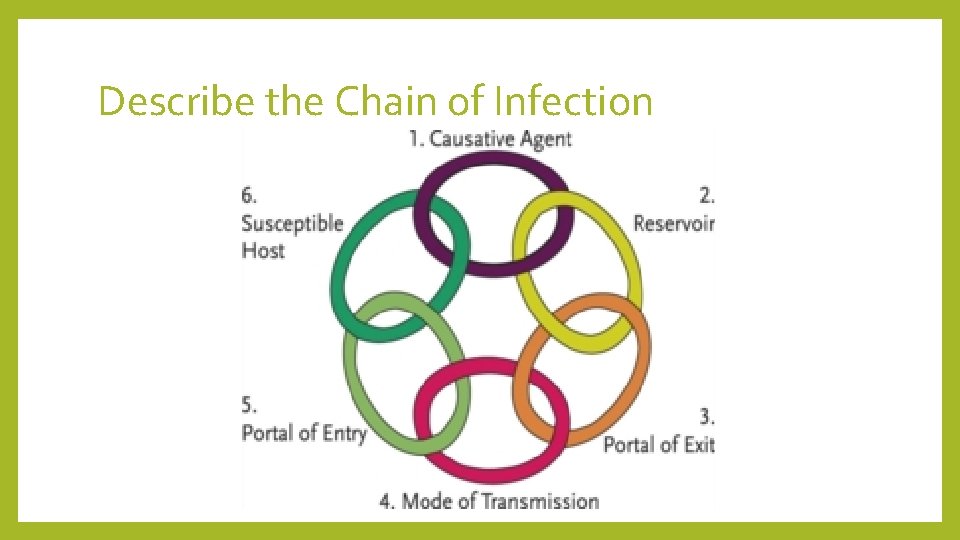
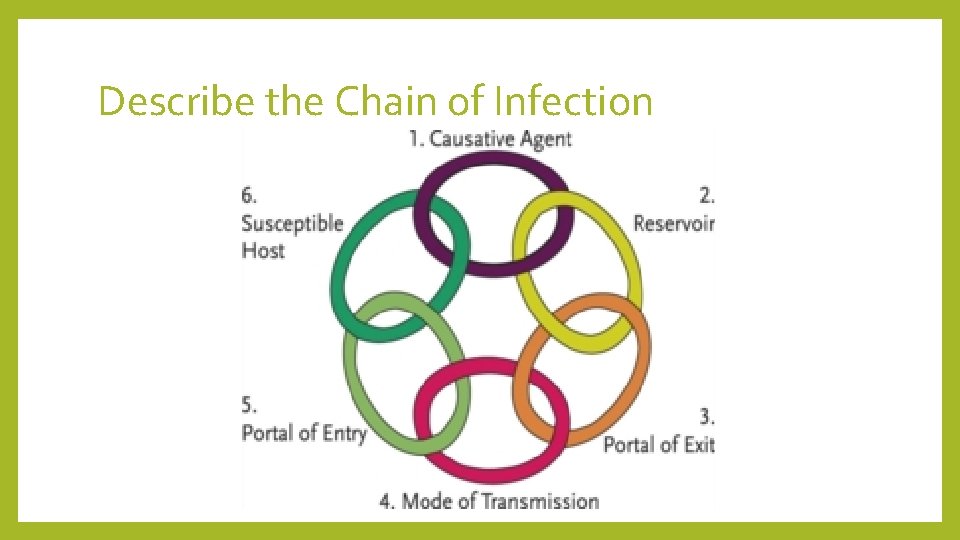
Describe the Chain of Infection
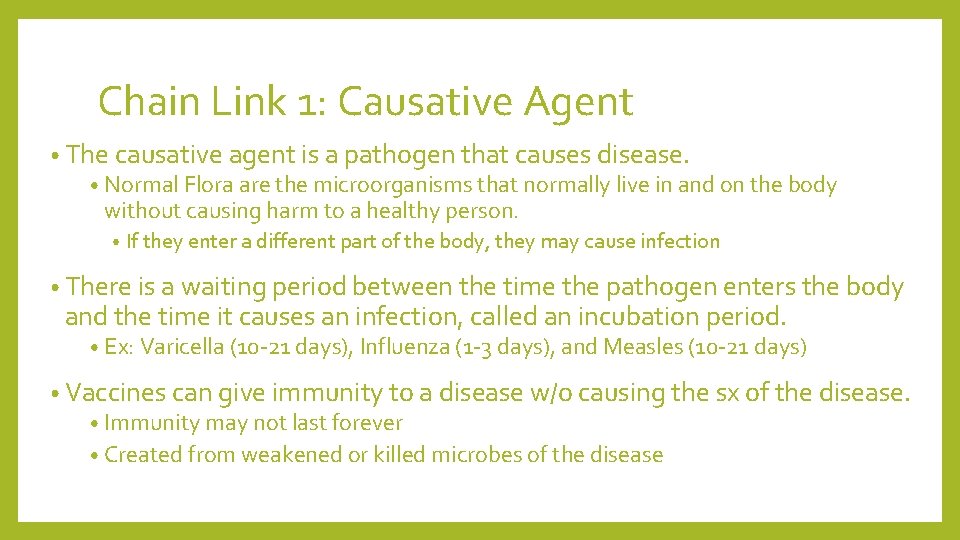
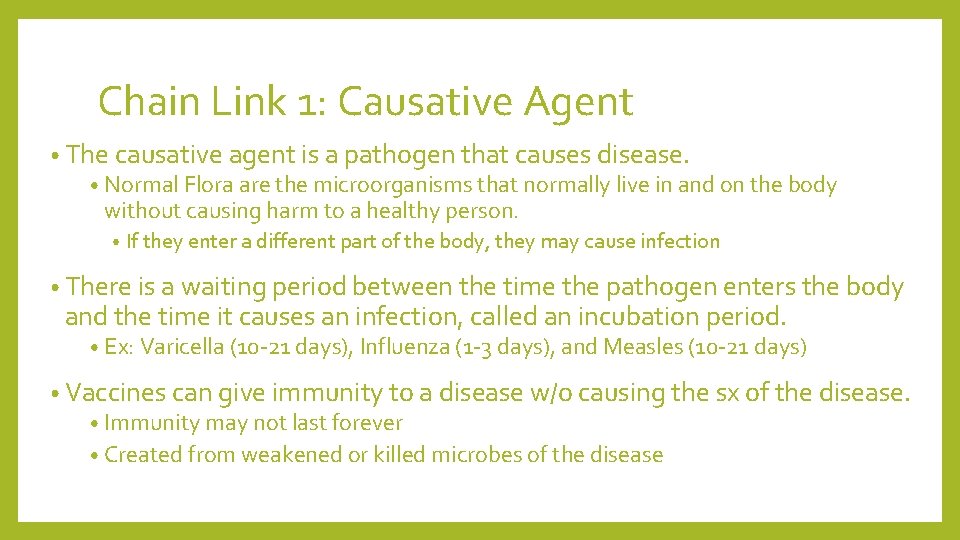
Chain Link 1: Causative Agent • The causative agent is a pathogen that causes disease. • Normal Flora are the microorganisms that normally live in and on the body without causing harm to a healthy person. • If they enter a different part of the body, they may cause infection • There is a waiting period between the time the pathogen enters the body and the time it causes an infection, called an incubation period. • Ex: Varicella (10 -21 days), Influenza (1 -3 days), and Measles (10 -21 days) • Vaccines can give immunity to a disease w/o causing the sx of the disease. • Immunity may not last forever • Created from weakened or killed microbes of the disease
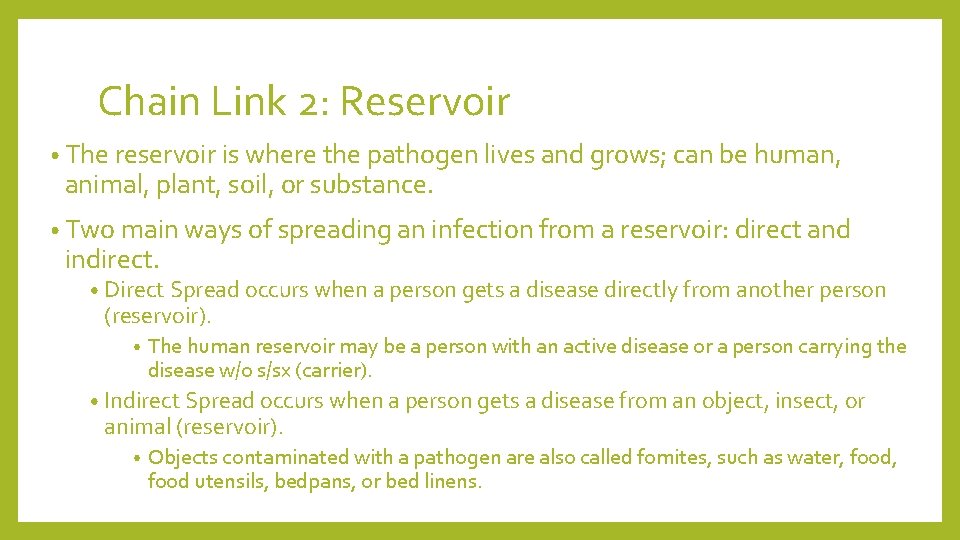
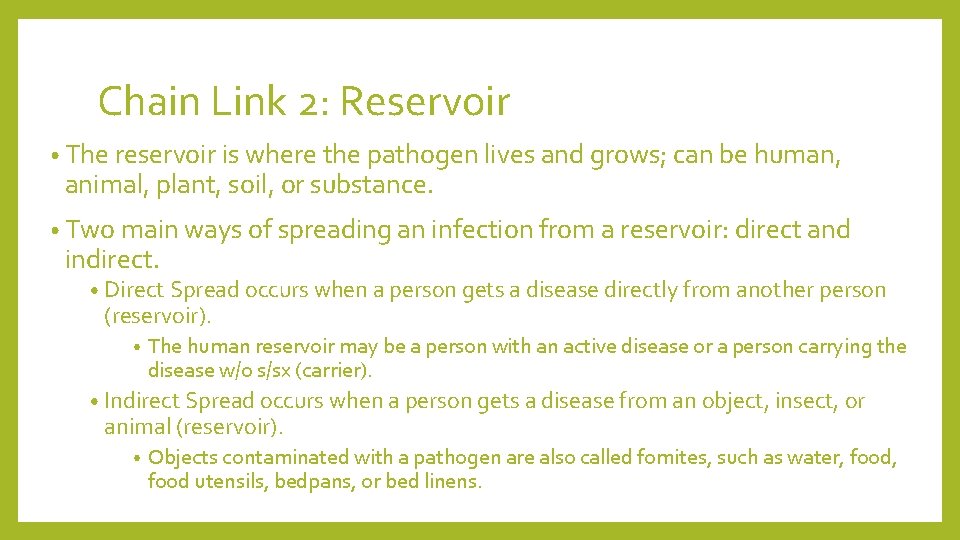
Chain Link 2: Reservoir • The reservoir is where the pathogen lives and grows; can be human, animal, plant, soil, or substance. • Two main ways of spreading an infection from a reservoir: direct and indirect. • Direct Spread occurs when a person gets a disease directly from another person (reservoir). • The human reservoir may be a person with an active disease or a person carrying the disease w/o s/sx (carrier). • Indirect Spread occurs when a person gets a disease from an object, insect, or animal (reservoir). • Objects contaminated with a pathogen are also called fomites, such as water, food utensils, bedpans, or bed linens.
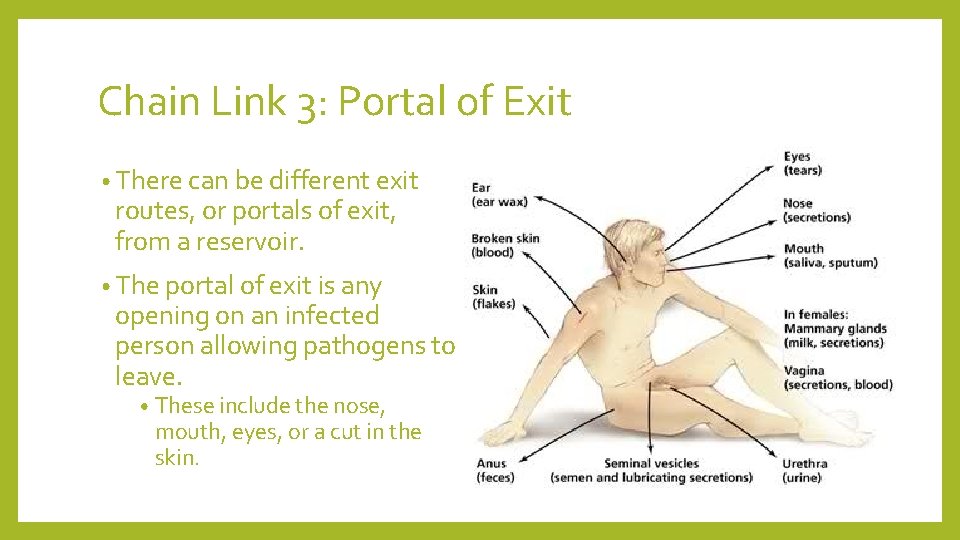
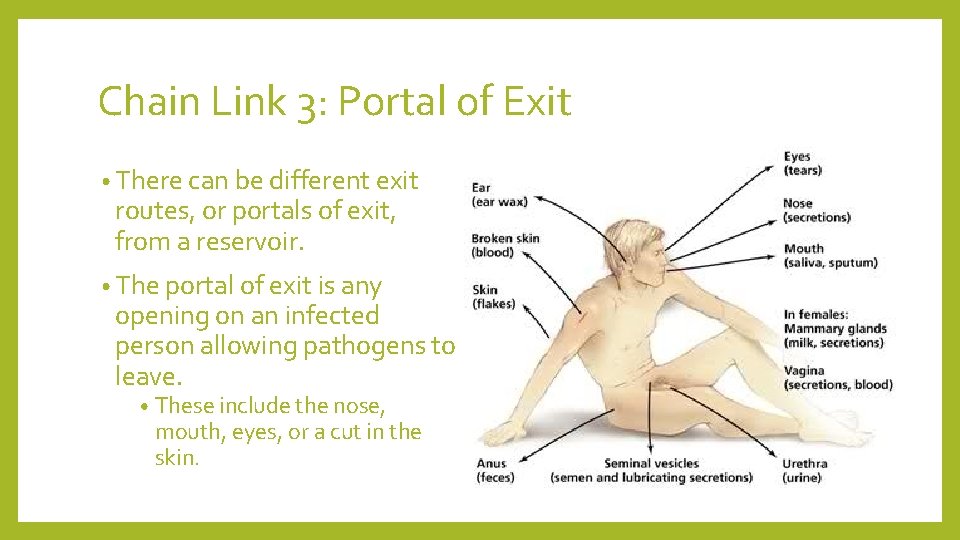
Chain Link 3: Portal of Exit • There can be different exit routes, or portals of exit, from a reservoir. • The portal of exit is any opening on an infected person allowing pathogens to leave. • These include the nose, mouth, eyes, or a cut in the skin.
Chain Link 4: Mode of Transmission • Mode of Transmission describes how the infectious disease travels. • This can include contact, droplet, and airborne transmission. • Contact with blood or body fluids (tears, saliva, sputum, urine, feces, semen, vaginal secretions, pus or other wound drainage) • Droplets come from coughing, sneezing, talking, laughing, suctioning, singing, and spitting • Less than 3 ft • Airborne travels in the air (more than 3 ft) through moisture and dust.
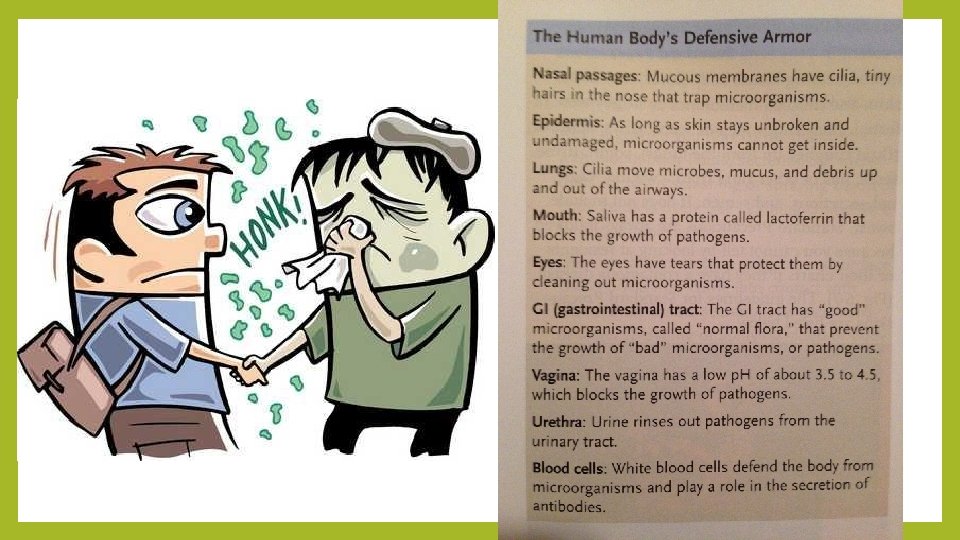
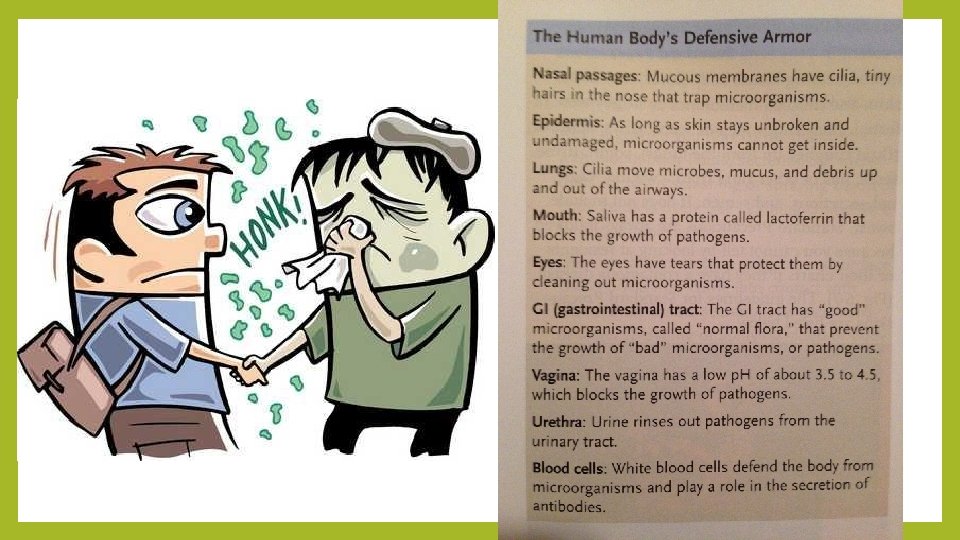
Chain Link 5: Portal of Entry • Pathogens enter the human host through different portals of entry. • The portal of entry is any body opening on an uninfected person that allows pathogens to enter. • Includes nose, mouth, eyes, and other mucous membranes, cuts in the skin, and cracked skin. • Mucous membranes are membranes that line body cavities that open to the outside of the body such as the mouth, nose, eyes, rectum, and genitals. • Many areas of the body are protected from invading pathogens, sort of like an “armor. ”
Chain Link 6: Susceptible Host • A susceptible host is an uninfected person who could get sick. • A person becomes susceptible when his/her resistance decreases due to age, existing illness, fatigue, and/or stress. • When a pathogen invades the body, it will start reproducing itself. • As pathogens grow, they damage healthy tissue.

Reasons for Increased Risk of Infection for Elderly • Immune systems become weaker • Hospitalized more frequently (nosocomial) • Longer recovery • Thinner skin • Limited mobility • Bones become more brittle • Decreased circulation • Slow wound healing • Frequent use of catheters • Dehydration • Malnutrition
Center for Disease Control • CDC is a federal government agency that issues guidelines to protect and improve health. • It promotes public health and safety through education and tries to control and prevent disease. • In 1996, the CDC created new guidelines to protect people in health care from contracting infectious diseases. • It was updated 2007 • There are two levels of precautions in the infection control system recommended by the CDC. • Standard Precautions and Isolation Precautions
Standard Precautions • Standard Precautions means treating blood, body fluids, non- intact skin, and mucous membranes as if they were infected. • They are always followed because you cannot tell by looking at a patient or his/her chart if they have a contagious disease. • Assume everyone has something!!!! • For guidelines, please view the chapter provided.
Hand Hygiene • Hand hygiene is defined by the CDC as any method that removes or destroys microorganisms on hands, including handwashing and hand sanitizer. • Alcohol-based hand rubs ARE NOT a substitute for frequent and proper handwashing! • As you move between patients’ rooms, always wash your hands. • Taking care of patients means you will get microorganisms on your hands. • Wash your hands before giving care. • It will help prevent the spread of disease.
Personal Protective Equipment (PPE) • PPE is a barrier between a person and disease. It is what you wear to prevent the transmission of disease. • PPE includes gloves, gowns, masks, goggles, and face shields. • See chapter provided for proper steps to putting on and removing PPEs.
Handling Linen and Equipment • Facilities handle storage and disposal of linen and equipment by following guidelines set by the CDC. • Facilities have separate areas for clean and dirty items called clean and dirty utility rooms. • Linen and equipment will be placed in separate containers to be cleaned or discarded. • There will be disposal containers for linen, trash, equipment, and special infectious waste disposal. • Guidelines can be found in the chapter provided.
Handling Spills • Spills happen when blood, body fluids, or other fluids get on any person, object, or area in a facility. • Spills pose a serious risk of infection and fall risk for patients. • Clean spills using proper equipment and procedures. • Wear gloves and wipe up immediately for the outside moving in. • Use a cleaning solution of 1 part bleach to 10 parts water. There may be ready-touse spray bottles at the facility. • Be careful if any glass or other sharp objects are in a spill. Get help when picking up and disposing of sharps. • NEVER PICK UP GLASS EVEN WITH GLOVED HANDS • For large spills, call the nurse and follow your facility policy for large spills. • If you spill on your body, wash it off immediately. Report the exposure. • Wash your hands after cleaning spills
Transmission-Based Precautions • Precautions beyond Standard Precautions. • These guidelines were for persons who are infected or may be infected with diseases. • Also known as Isolation Precautions, consisting of three categories. • Airborne • Droplet • Contact • Refer to chapter provided
Isolation Unit • Patients who require Transmission-Based Precautions are referred to as being in “isolation. ” • A sign should be on the door indicating “isolation” or alerting people to see the nurse before entering the room. • Patients in isolation cannot move about freely, and are separated from everyone else. • May cause resident loneliness, be empathetic • They may be allowed visitors, but all visitors must be trained in PPEs • Follow the guidelines in the chapter provided.
OSHA’s Bloodborne Pathogen Standard • Bloodborne pathogens are MOs found in human blood that can cause infection and disease. • They may also be found in body fluids, draining wounds, and mucous membranes • Occupational Safety and Health Administration (OSHA) is a federal government agency that is responsible for the safety of workers in the U. S. • By law, employers must follow these rules to reduce the risk of acquiring infectious disease. The Standard also guides employer and employees through the steps to follow if exposed to infectious material. • Refer to the chapter provided for specific guidelines
HIV/AIDS • Bloodborne pathogen, HIV, can lead to AIDs. • Over time, HIV damages the immune system so that the body cannot fight infections • HIV is transmitted by blood, infected needles, and from mother to fetus. • Also transmitted sexually!
Hepatitis • Hepatitis is an inflammation of the liver caused by infection. Liver function can be permanently damaged by hepatitis. • There are several types of hepatitis, including A, B, C, D, and E • Most common are A, B, C • Hepatitis B and C are Bloodborne Pathogens, and can cause death. • More people have Hepatitis B (HBV) than HIV. • For more facts about Hepatitis see chapter provided.
Multidrug-Resistant Organisms (MDROs) • MDROs are microorganisms, mostly bacteria, that are resistant to one or more antimicrobial agents. • Two common types of MDROs are MRSA and VRE • Methicillin-resistant Staphylococcus aureus (MRSA) is a strain of staph bacteria that can cause disease and is resistant to powerful antibiotics in the methicillin family. Spreads by direct contact and indirect contact • Sx of MRSA include drainage, fever, chills, and redness • • Vancomycin-resistant enterococcus (VRE) is a bacterium that is resistant to the antibiotic Vancomycin. Very dangerous because it cannot be treated with antibiotics at all, causes life-threatening infections. • Spreads by direct contact and indirect contact • Sx of VRE include fever, fatigue, chills, and drainage. • • For more information on MDROs and how to handle them, see chapter provided