Chapter 52 Assessment of the Musculoskeletal System Skeletal



- Slides: 44
Chapter 52 Assessment of the Musculoskeletal System
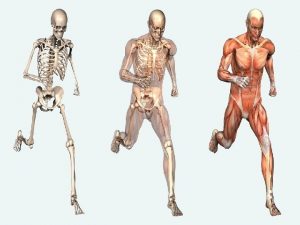
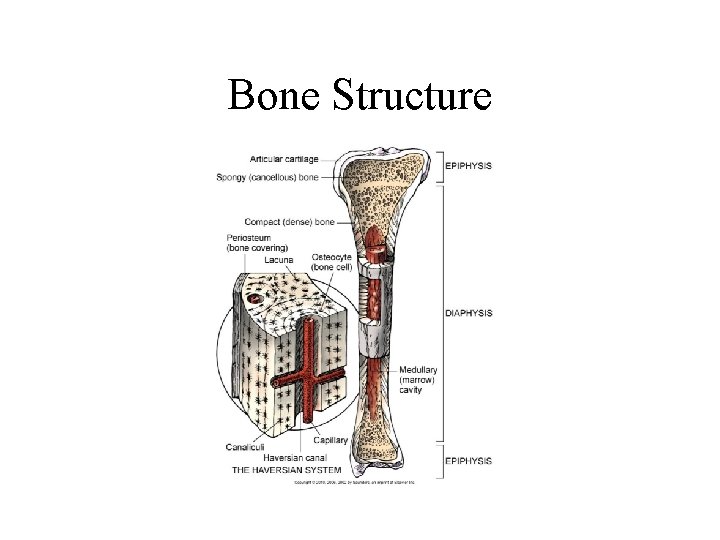
Skeletal System • • Bone types Bone structure Bone function Bone growth and metabolism affected by calcium and phosphorus, calcitonin, vitamin D, parathyroid hormone, growth hormone, glucocorticoids, estrogens androgens, thyroxine, and insulin
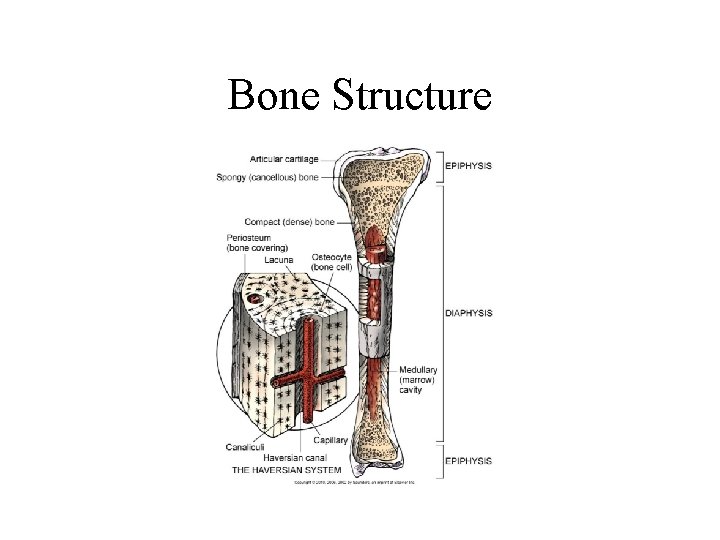
Bone Structure
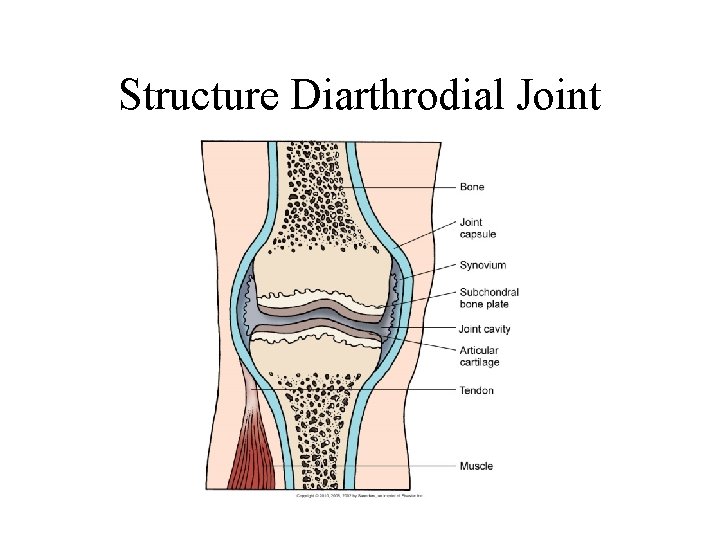
Joints • Types include synarthrodial, amphiarthrodial, diarthrodial. • Structure synovial joint. • Subtyped by anatomic structure: – Ball-and-socket – Hinge – Condylar – Biaxial – Pivot
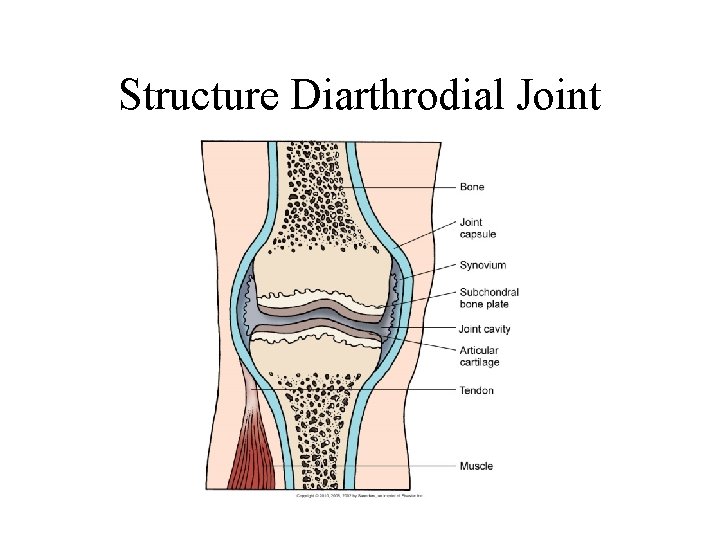
Structure Diarthrodial Joint
Muscular System Assessment • • Patient history Nutritional history Family history and genetic risk General inspection: – Posture and gait
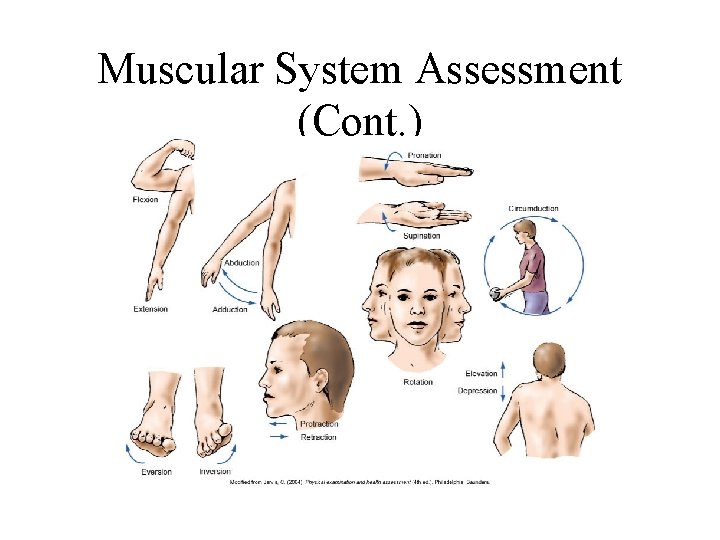
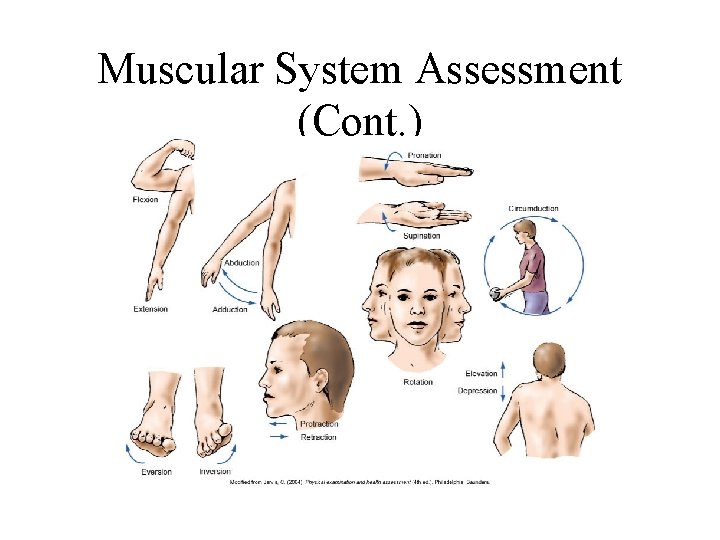
Muscular System Assessment (Cont. )
Specific Assessments • • Face and neck Spine Hand Hip Ankles, feet Neurovascular assessment Psychosocial assessment
Diagnostic Assessment • Laboratory tests—serum calcium and phosphorus, alkaline phosphatase, serum muscle enzymes • Radiographic examinations—standard radiography, bone density, tomography and xeroradiography, myelography, arthrography, and CT • Other diagnostic tests—bone and muscle biopsy
Electromyography • EMG aids in the diagnosis of neuromuscular, lower motor neuron, and peripheral nerve disorders; usually with nerve conduction studies. • Low electrical currents are passed through flat electrodes placed along the nerve. • If needles are used, inspect needle sites for hematoma formation.
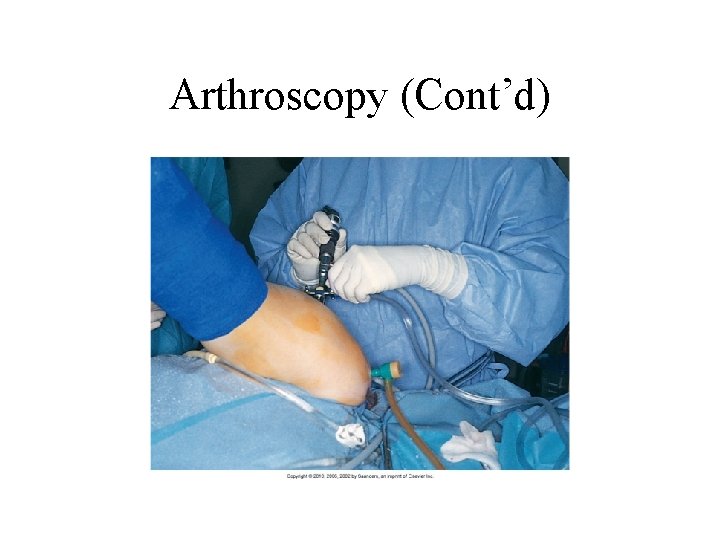
Arthroscopy • Fiberoptic tube is inserted into a joint for direct visualization. • Patient must be able to flex the knee; exercises are prescribed for ROM. • Evaluate the neurovascular status of the affected limb frequently. • Analgesics are prescribed. • Monitor for complications.
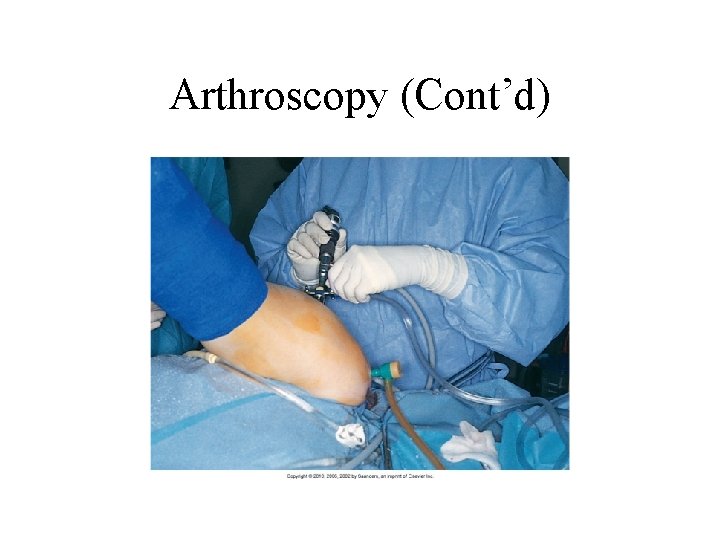
Arthroscopy (Cont’d)
Other Tests • • Bone scan Gallium or thallium scan Magnetic resonance imaging Ultrasonography
Chapter 53 Care of Patients with Musculoskeletal Problems
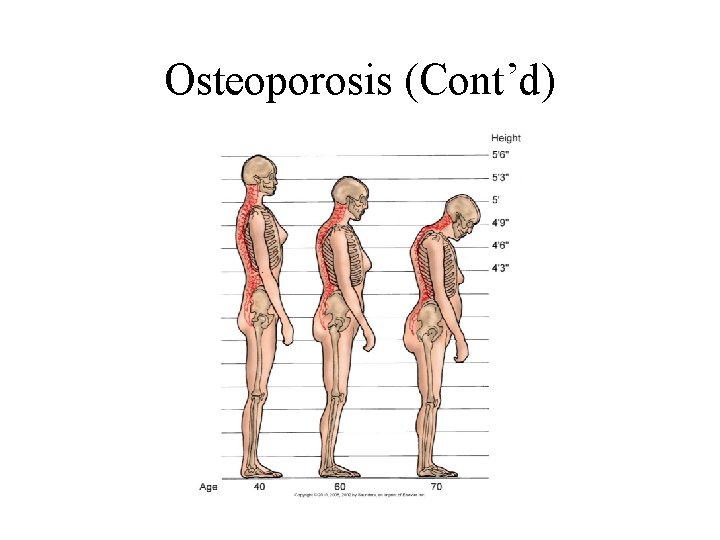
Osteoporosis • Chronic metabolic disease, in which bone loss causes decreased density and possible fracture • Osteopenia (low bone mass), which occurs when osteoclastic activity is greater than osteoblastic activity
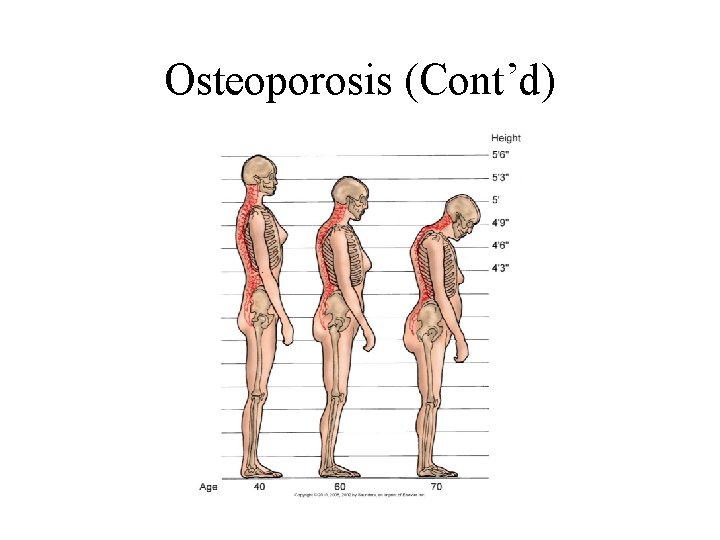
Osteoporosis (Cont’d)
Osteoporosis (Cont’d) • • Etiology and genetic risk Genetic considerations Incidence/prevalence Cultural considerations
Classification of Osteoporosis • Generalized osteoporosis occurs most commonly in postmenopausal women and men in their 60 s and 70 s. • Secondary osteoporosis results from an associated medical condition such as hyperparathyroidism, long-term drug therapy, long-term immobility. • Regional osteoporosis occurs when a limb is immobilized.
Health Promotion/Illness Prevention • Teaching should begin with young women who begin to lose bone after 30 years of age. • The focus of osteoporosis prevention is to decrease modifiable risk factors. • Ensure adequate calcium intake. • Avoid sedentary lifestyle. • Continue program of weight-bearing exercises.
Assessment • • Physical assessment Psychosocial assessment Laboratory assessment Imaging assessment: – DXA – QCT – QUS
Osteoporosis: Interventions • Nutrition therapy • Exercise • Other lifestyle changes
Osteoporosis: Drug Therapy • • • Calcium and vitamin D supplements Estrogen or hormone therapy Bisphonates Selective estrogen receptor modulators Calcitonin Other agents used with varying results
Osteoporosis: Surgical Interventions • Vertebroplasty • Kyphoplasty
Osteomalacia • Loss of bone related to vitamin D deficiency • Bone softens because of inadequate deposits of calcium and phosphorus in the bone matrix • Rickets
Collaborative Care • Assessment • The major treatment for osteomalacia is vitamin D
Paget’s Disease of the Bone • Chronic metabolic disorder in which bone is excessively broken down and reformed • Genetic considerations • Collaborative care: – Physical assessment – Diagnostic assessment
Paget’s Disease: Nonsurgical Management • • Analgesics Decrease bone resorption Selected bisphonates Calcitonin Plicamycin Diet therapy Nonpharmacologic pain-relief measures
Paget’s Disease: Surgical Management • Tibial osteotomy • Partial or total joint replacement • Surgical decompression and stabilization of the spine
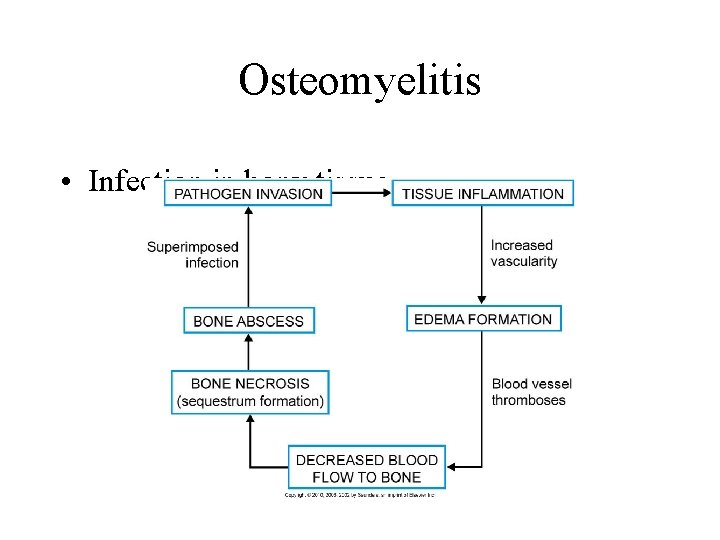
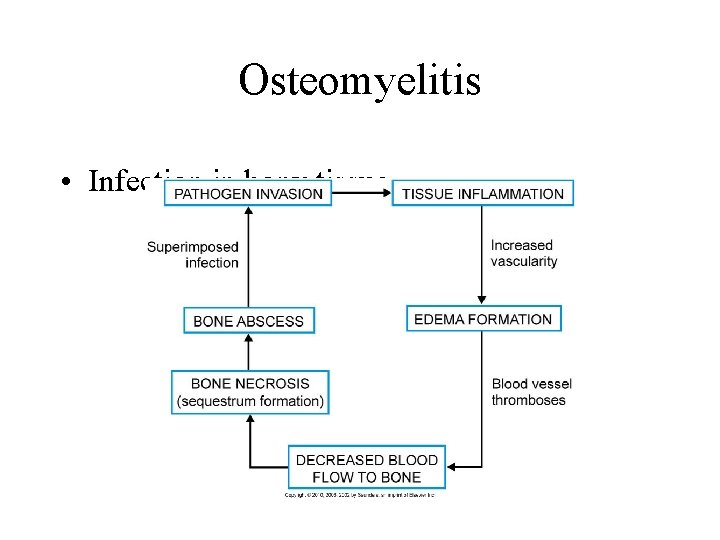
Osteomyelitis • Infection in bony tissue
Osteomyelitis: Collaborative Care • • Assessment Antibiotic therapy Hyperbaric oxygen therapy Surgical management: – Sequestrectomy – Microvascular bone transfers
Benign Bone Tumors • Often asymptomatic and may be discovered on routine x-ray or as a cause of pathologic fracture: – Chrondrogenic tumors—from cartilage – Osteogenic tumors—from bone – Fibrogenic tumors—from fibrous tissue; most commonly found in children
Interventions • Non-drug pain-relief measures • Drug therapy—analgesics, NSAIDs • Surgical therapy—curettage (simple excision of the tumor tissue), joint replacement, or arthrodesis

Bone Cancer • • • Primary tumors Metastatic lesions Pathophysiology Assessment Nonsurgical management: – Drug therapy – Radiation therapy
Bone Cancer: Surgical Management • Preoperative care • Operative procedure • Postoperative care
Bone Cancer: Community. Based Care • Home care management • Health teaching • Health care resources
Disorders of the Hand • Dupuytren's contracture—slowly progressive contracture of the palmar fascia resulting in flexion of the fourth or fifth digit of the hand
Ganglion • Round, benign cyst often found on a wrist or foot joint or tendon

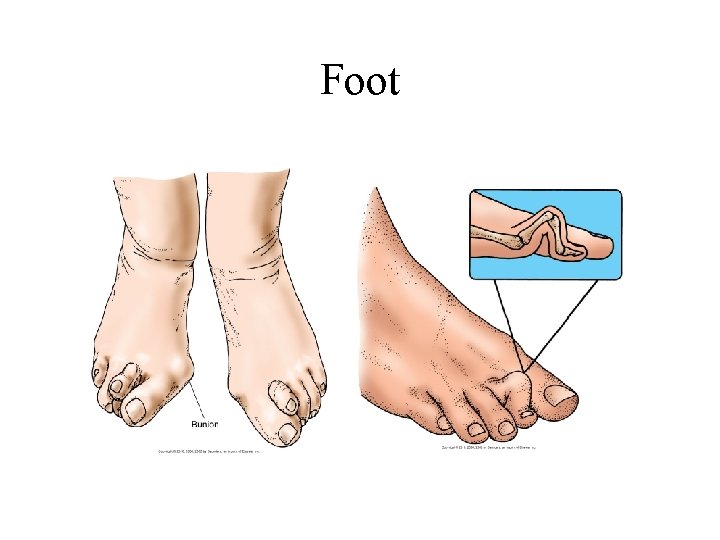
Disorders of the Foot • • • Hallux valgus Hammertoe Morton’s neuroma Tarsal tunnel syndrome Plantar fasciitis Other problems of the foot
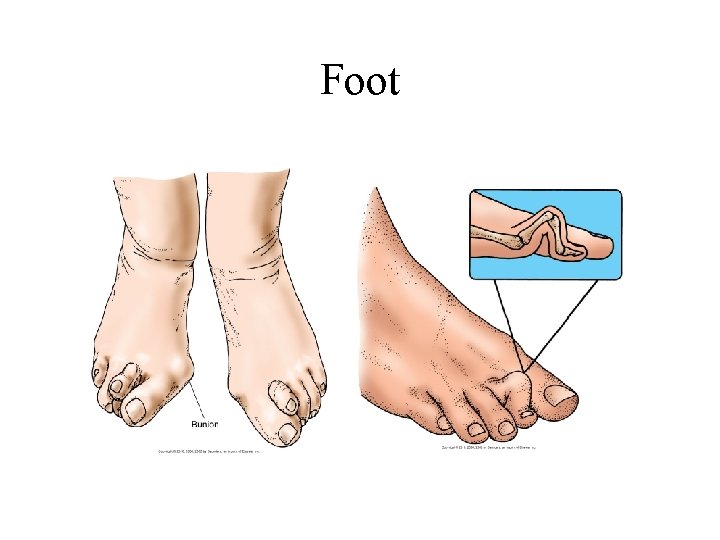
Foot
Scoliosis • Changes in muscles and ligaments on the concave side of the spinal column

Scoliosis (Cont’d) • • Pathophysiology History Treatment of children Treatment of adults
Progressive Muscular Dystrophies • • • Pathophysiology Genetic considerations Diagnosis Management Nursing interventions
 Assessment of the musculoskeletal system
Assessment of the musculoskeletal system Muscle strength scale
Muscle strength scale The musculoskeletal system chapter 21
The musculoskeletal system chapter 21 Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Chapter 15 musculoskeletal system practical
Chapter 15 musculoskeletal system practical Musculoskeletal fitness
Musculoskeletal fitness Musculoskeletal system
Musculoskeletal system Unit 41 musculoskeletal system
Unit 41 musculoskeletal system Musculoskeletal system
Musculoskeletal system Medical term for top of foot
Medical term for top of foot Diseases of the musculoskeletal system
Diseases of the musculoskeletal system Musculoskeletal system
Musculoskeletal system Objective data for musculoskeletal system
Objective data for musculoskeletal system Chapter 41 musculoskeletal care modalities
Chapter 41 musculoskeletal care modalities Chapter 24 the child with a musculoskeletal condition
Chapter 24 the child with a musculoskeletal condition Chapter 5 the skeletal system
Chapter 5 the skeletal system The skeletal system learning exercises chapter 3
The skeletal system learning exercises chapter 3 Chapter 7:4 skeletal system
Chapter 7:4 skeletal system Chapter 5 the skeletal system figure 5-13
Chapter 5 the skeletal system figure 5-13 Chapter 6 skeletal system
Chapter 6 skeletal system 7 12 5 spine
7 12 5 spine Chapter 32 section 2 the skeletal system answer key
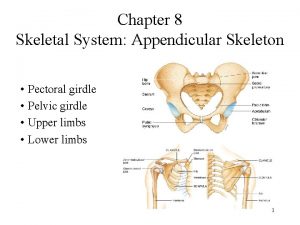
Chapter 32 section 2 the skeletal system answer key Chapter 8 skeletal system
Chapter 8 skeletal system Chapter 7:4 skeletal system
Chapter 7:4 skeletal system Chapter 5 axial skeleton worksheet answers
Chapter 5 axial skeleton worksheet answers Figure 5-13 is a diagram of the articulated skeleton
Figure 5-13 is a diagram of the articulated skeleton Chapter 5 the skeletal system figure 5-13
Chapter 5 the skeletal system figure 5-13 Chapter 5 the skeletal system figure 5-10
Chapter 5 the skeletal system figure 5-10 Chapter 5 the skeletal system
Chapter 5 the skeletal system Axial skeleton
Axial skeleton Chapter 3 the skeletal system labeling exercises
Chapter 3 the skeletal system labeling exercises Hollow portions of bones surrounding the nasal cavity
Hollow portions of bones surrounding the nasal cavity Chapter 5 the skeletal system figure 5-10
Chapter 5 the skeletal system figure 5-10 Chapter 8 skeletal system
Chapter 8 skeletal system Male vs female skeleton pelvis
Male vs female skeleton pelvis All about bones
All about bones Soal uas sistem muskuloskeletal
Soal uas sistem muskuloskeletal Kode icd 10 osteoarthritis genu
Kode icd 10 osteoarthritis genu Work related musculoskeletal disorders definition
Work related musculoskeletal disorders definition Musculoskeletal pronounce
Musculoskeletal pronounce West coast musculoskeletal
West coast musculoskeletal Mpsq
Mpsq Subcostal retractions
Subcostal retractions Musculoskeletal integrity
Musculoskeletal integrity Musculoskeletal injury
Musculoskeletal injury