Chapter 5 The Integumentary System 2012 Pearson Education
- Slides: 36
Chapter 5 The Integumentary System © 2012 Pearson Education, Inc. http: //farm 2. static. flickr. com/1231/534175495_73 a 6 d 12308. jpg
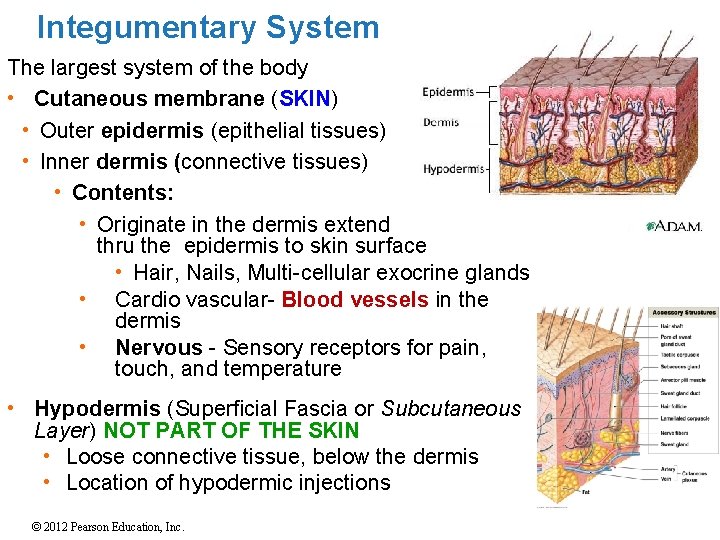
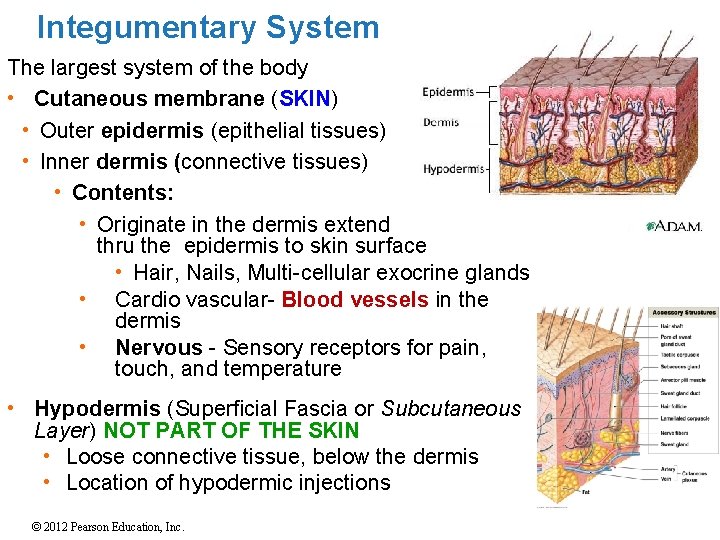
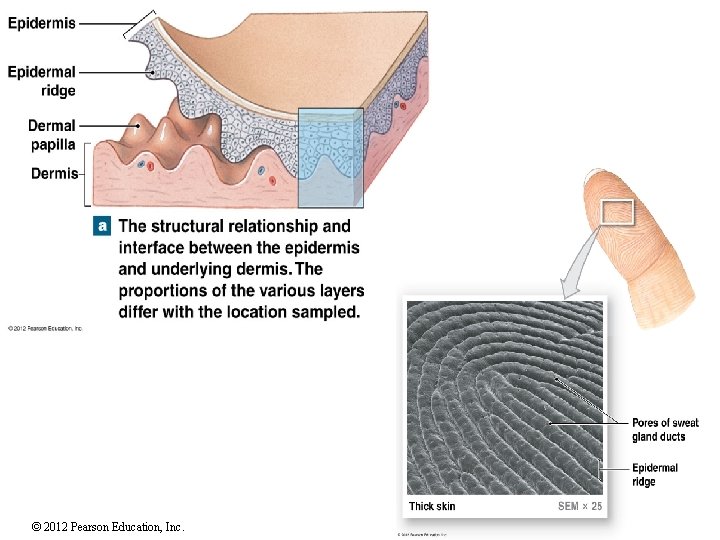
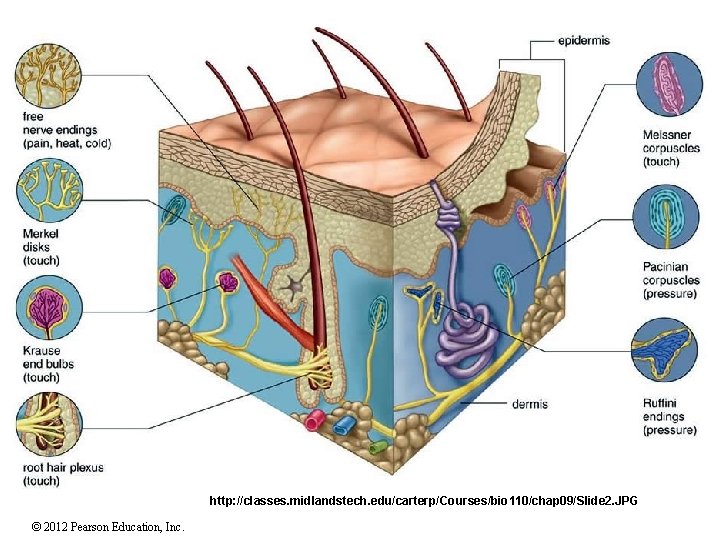
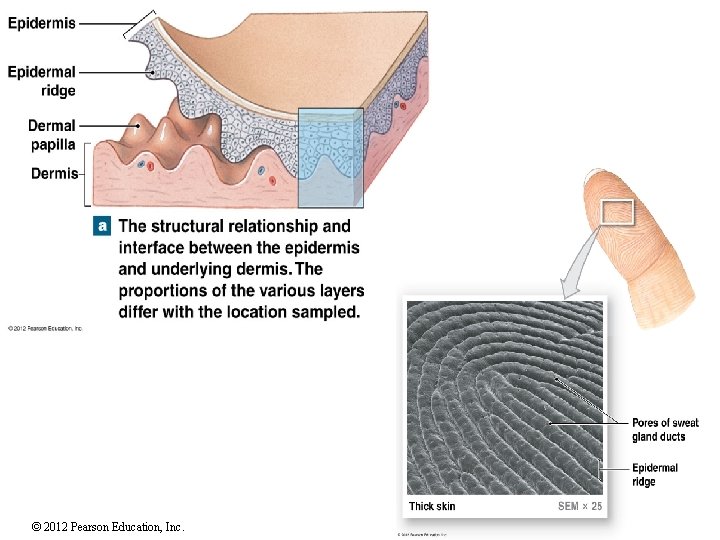
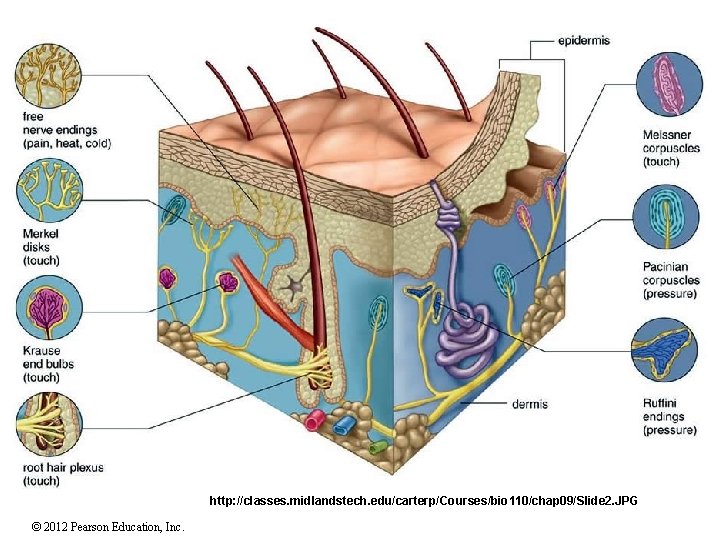
Integumentary System The largest system of the body • Cutaneous membrane (SKIN) • Outer epidermis (epithelial tissues) • Inner dermis (connective tissues) • Contents: • Originate in the dermis extend thru the epidermis to skin surface • Hair, Nails, Multi-cellular exocrine glands • Cardio vascular- Blood vessels in the dermis • Nervous - Sensory receptors for pain, touch, and temperature • Hypodermis (Superficial Fascia or Subcutaneous Layer) NOT PART OF THE SKIN • Loose connective tissue, below the dermis • Location of hypodermic injections © 2012 Pearson Education, Inc.
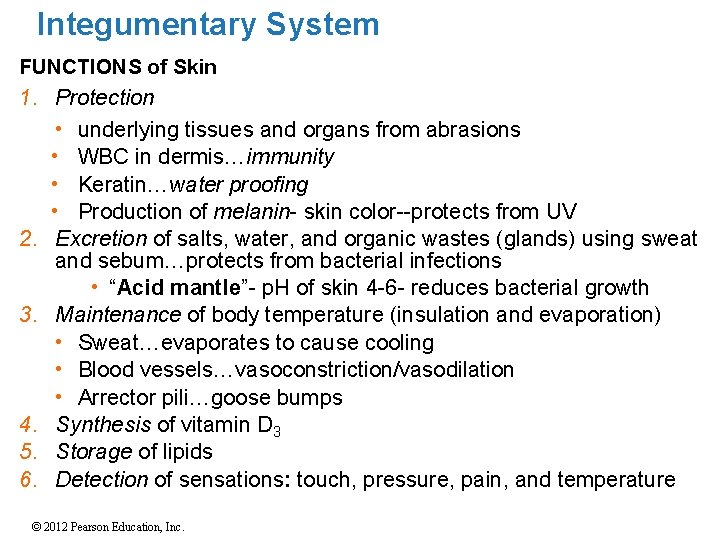
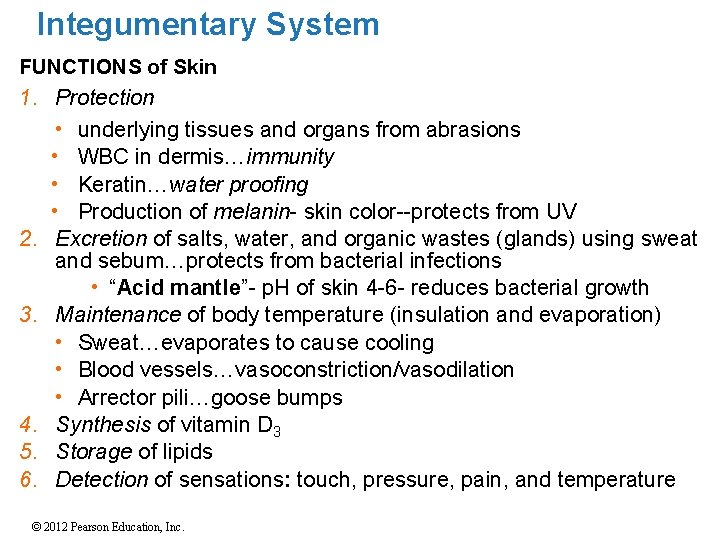
Integumentary System FUNCTIONS of Skin 1. Protection 2. 3. 4. 5. 6. • underlying tissues and organs from abrasions • WBC in dermis…immunity • Keratin…water proofing • Production of melanin- skin color--protects from UV Excretion of salts, water, and organic wastes (glands) using sweat and sebum…protects from bacterial infections • “Acid mantle”- p. H of skin 4 -6 - reduces bacterial growth Maintenance of body temperature (insulation and evaporation) • Sweat…evaporates to cause cooling • Blood vessels…vasoconstriction/vasodilation • Arrector pili…goose bumps Synthesis of vitamin D 3 Storage of lipids Detection of sensations: touch, pressure, pain, and temperature © 2012 Pearson Education, Inc.
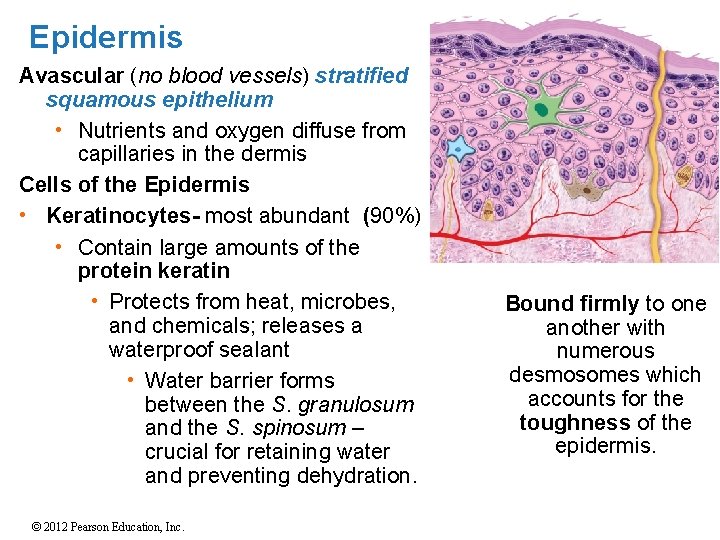
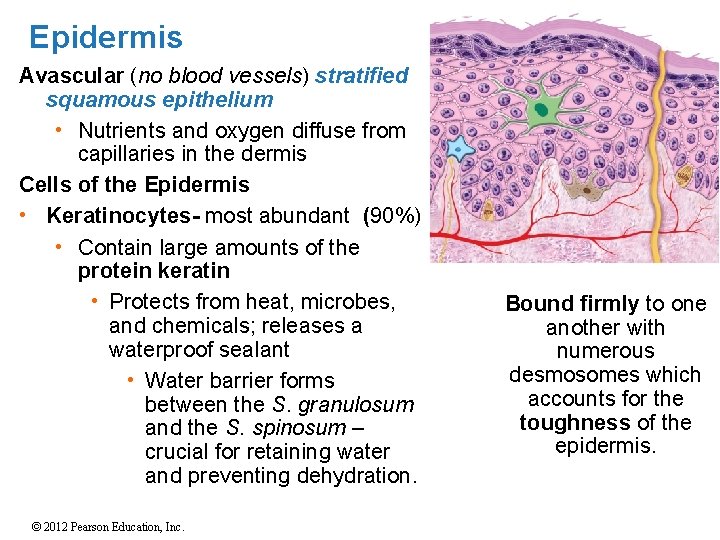
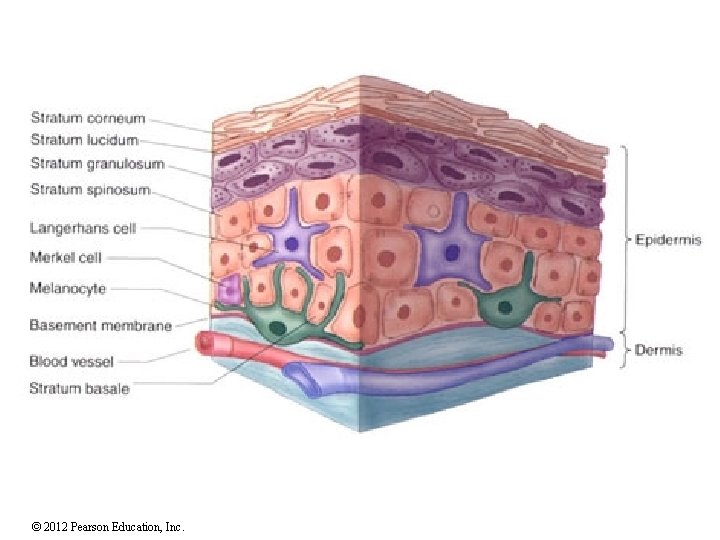
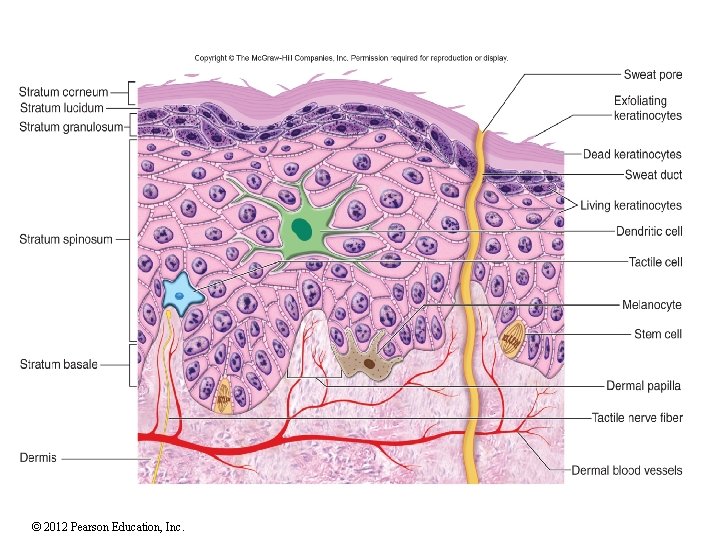
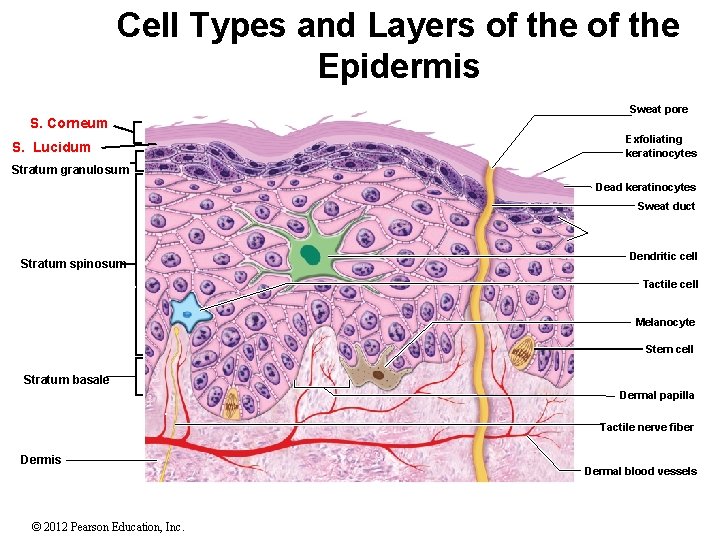
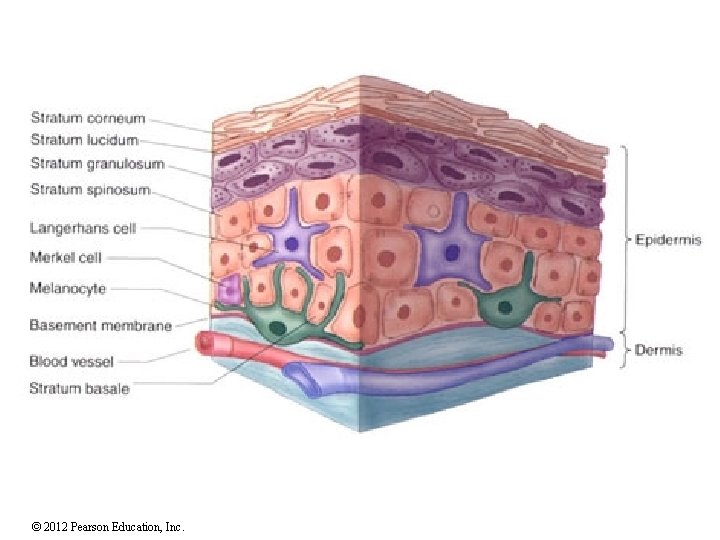
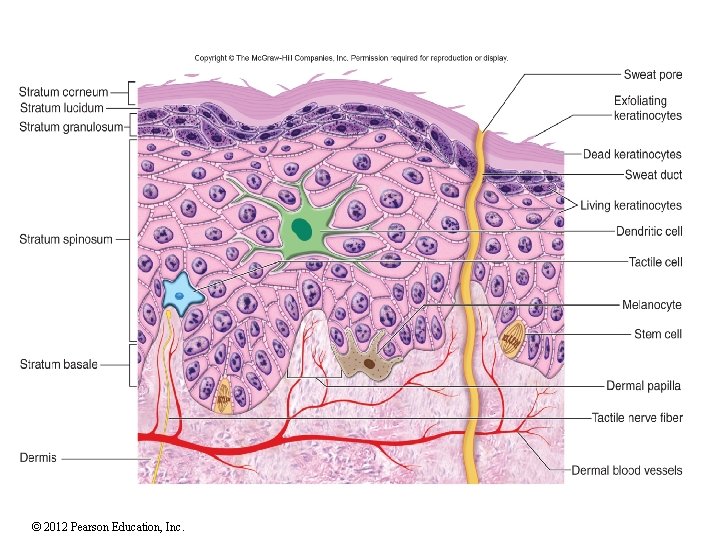
Epidermis Avascular (no blood vessels) stratified squamous epithelium • Nutrients and oxygen diffuse from capillaries in the dermis Cells of the Epidermis • Keratinocytes- most abundant (90%) • Contain large amounts of the protein keratin • Protects from heat, microbes, and chemicals; releases a waterproof sealant • Water barrier forms between the S. granulosum and the S. spinosum – crucial for retaining water and preventing dehydration. © 2012 Pearson Education, Inc. Bound firmly to one another with numerous desmosomes which accounts for the toughness of the epidermis.
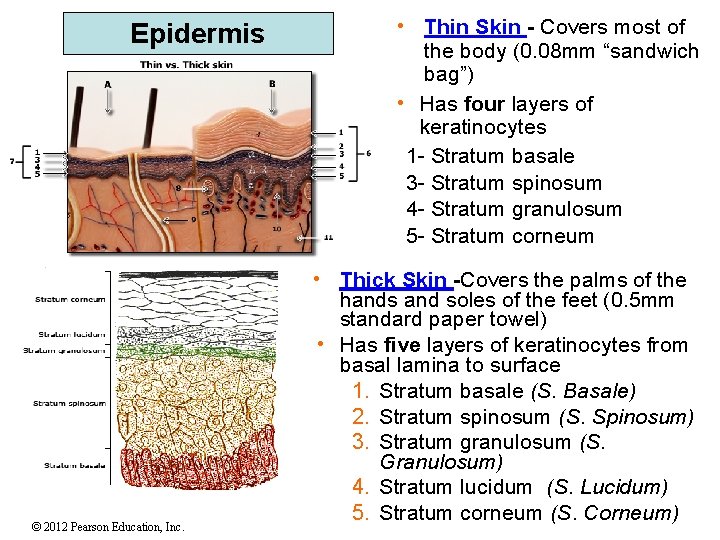
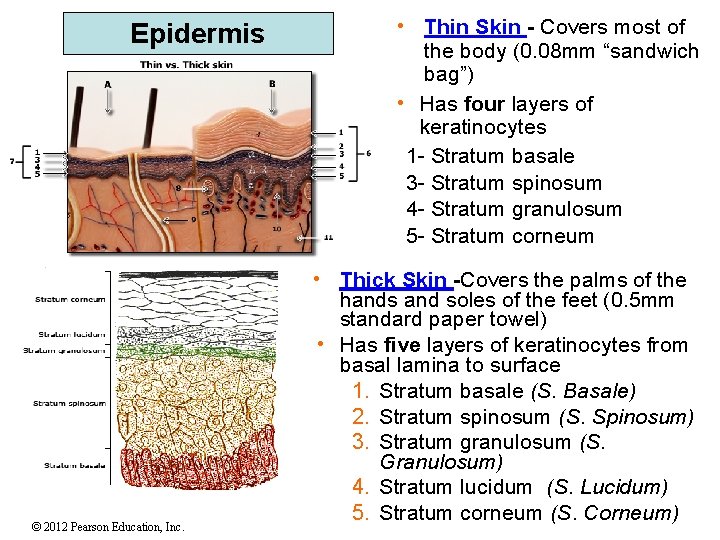
Epidermis © 2012 Pearson Education, Inc. • Thin Skin - Covers most of the body (0. 08 mm “sandwich bag”) • Has four layers of keratinocytes 1 - Stratum basale 3 - Stratum spinosum 4 - Stratum granulosum 5 - Stratum corneum • Thick Skin -Covers the palms of the hands and soles of the feet (0. 5 mm standard paper towel) • Has five layers of keratinocytes from basal lamina to surface 1. Stratum basale (S. Basale) 2. Stratum spinosum (S. Spinosum) 3. Stratum granulosum (S. Granulosum) 4. Stratum lucidum (S. Lucidum) 5. Stratum corneum (S. Corneum)
© 2012 Pearson Education, Inc.
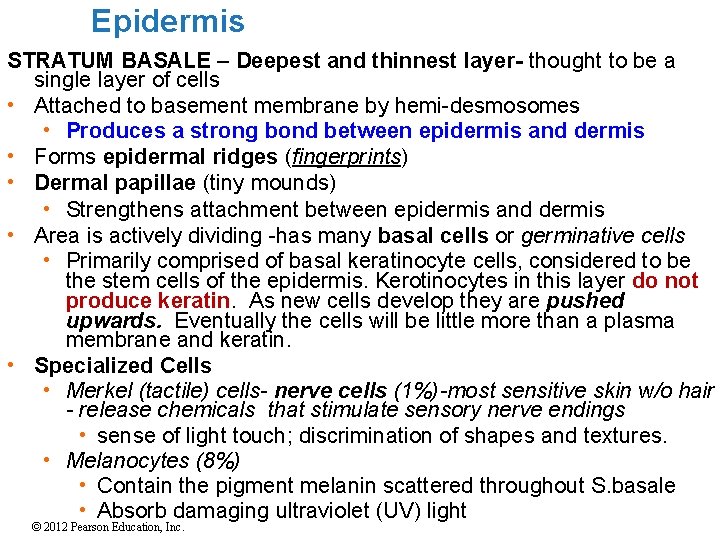
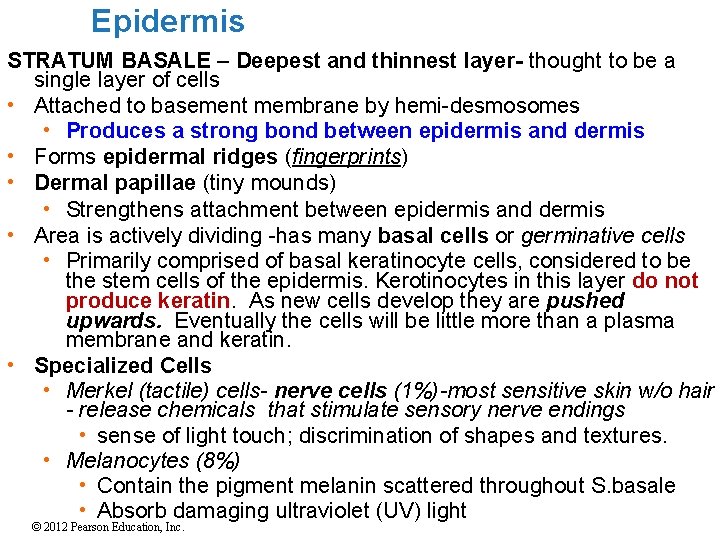
Epidermis STRATUM BASALE – Deepest and thinnest layer- thought to be a single layer of cells • Attached to basement membrane by hemi-desmosomes • Produces a strong bond between epidermis and dermis • Forms epidermal ridges (fingerprints) • Dermal papillae (tiny mounds) • Strengthens attachment between epidermis and dermis • Area is actively dividing -has many basal cells or germinative cells • Primarily comprised of basal keratinocyte cells, considered to be the stem cells of the epidermis. Kerotinocytes in this layer do not produce keratin. As new cells develop they are pushed upwards. Eventually the cells will be little more than a plasma membrane and keratin. • Specialized Cells • Merkel (tactile) cells- nerve cells (1%)-most sensitive skin w/o hair - release chemicals that stimulate sensory nerve endings • sense of light touch; discrimination of shapes and textures. • Melanocytes (8%) • Contain the pigment melanin scattered throughout S. basale • Absorb damaging ultraviolet (UV) light © 2012 Pearson Education, Inc.
© 2012 Pearson Education, Inc.
© 2012 Pearson Education, Inc.
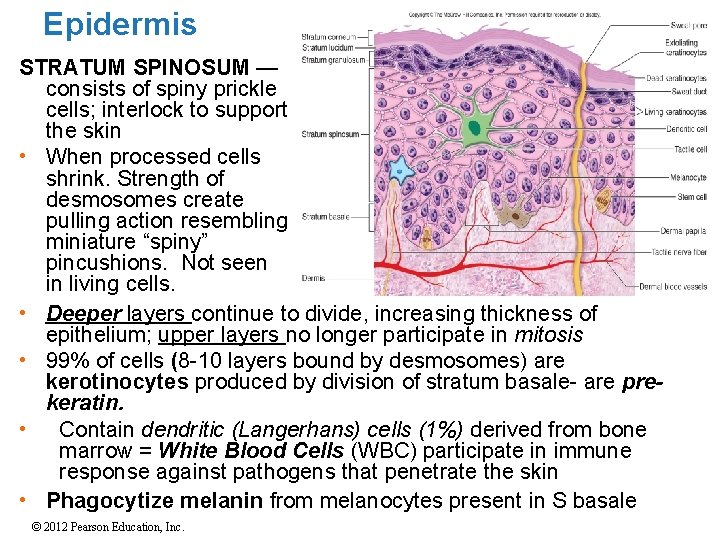
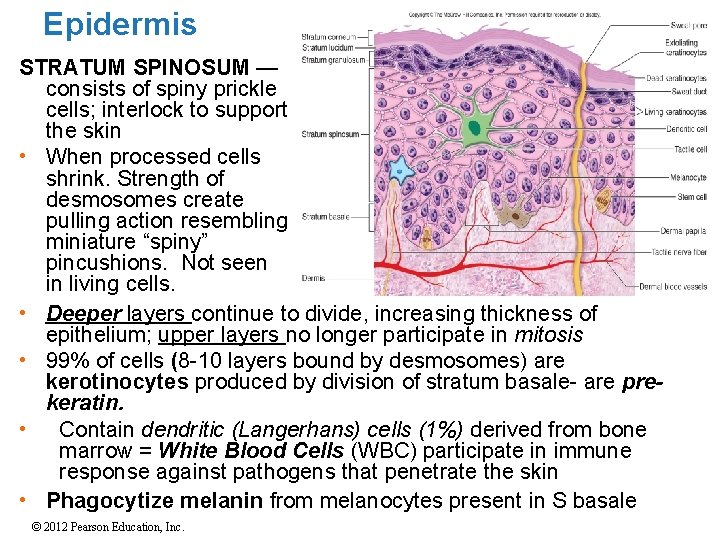
Epidermis STRATUM SPINOSUM — consists of spiny prickle cells; interlock to support the skin • When processed cells shrink. Strength of desmosomes create pulling action resembling miniature “spiny” pincushions. Not seen in living cells. • Deeper layers continue to divide, increasing thickness of epithelium; upper layers no longer participate in mitosis • 99% of cells (8 -10 layers bound by desmosomes) are kerotinocytes produced by division of stratum basale- are prekeratin. • Contain dendritic (Langerhans) cells (1%) derived from bone marrow = White Blood Cells (WBC) participate in immune response against pathogens that penetrate the skin • Phagocytize melanin from melanocytes present in S basale © 2012 Pearson Education, Inc.
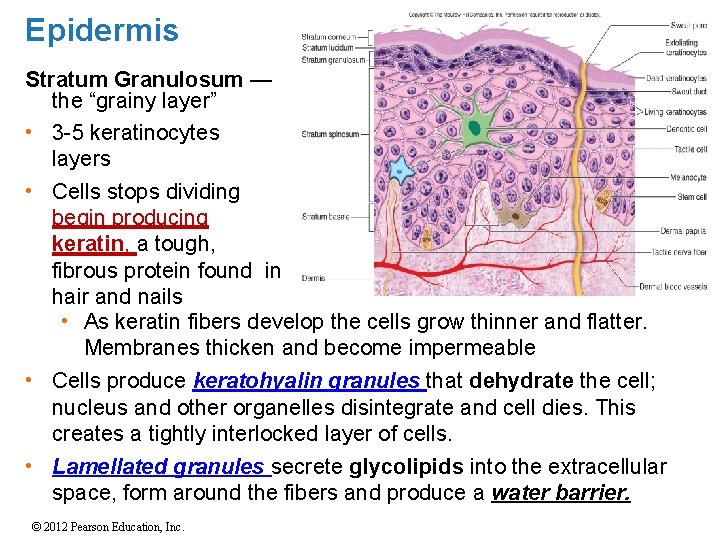
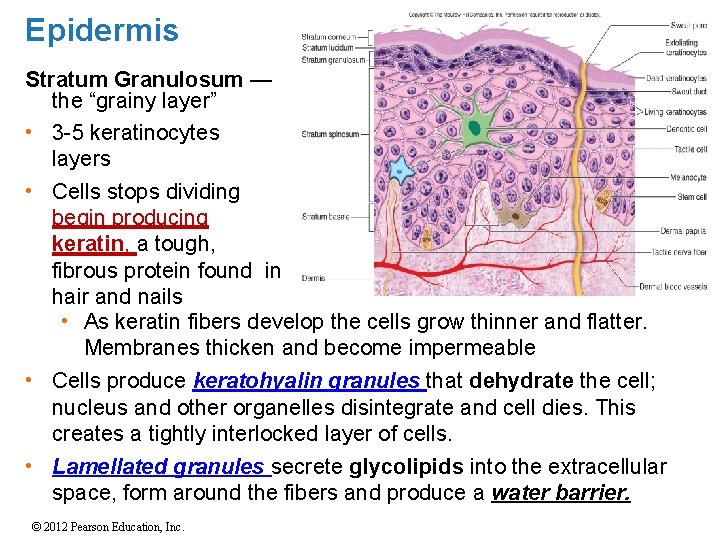
Epidermis Stratum Granulosum — the “grainy layer” • 3 -5 keratinocytes layers • Cells stops dividing begin producing keratin, a tough, fibrous protein found in hair and nails • As keratin fibers develop the cells grow thinner and flatter. Membranes thicken and become impermeable • Cells produce keratohyalin granules that dehydrate the cell; nucleus and other organelles disintegrate and cell dies. This creates a tightly interlocked layer of cells. • Lamellated granules secrete glycolipids into the extracellular space, form around the fibers and produce a water barrier. © 2012 Pearson Education, Inc.
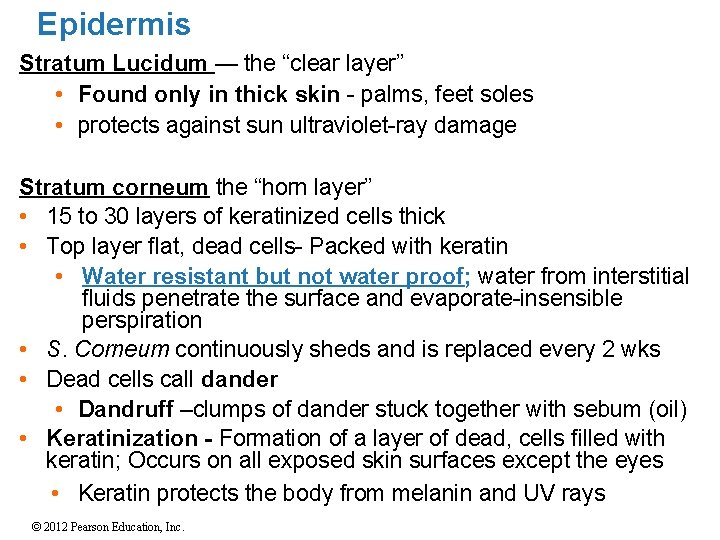
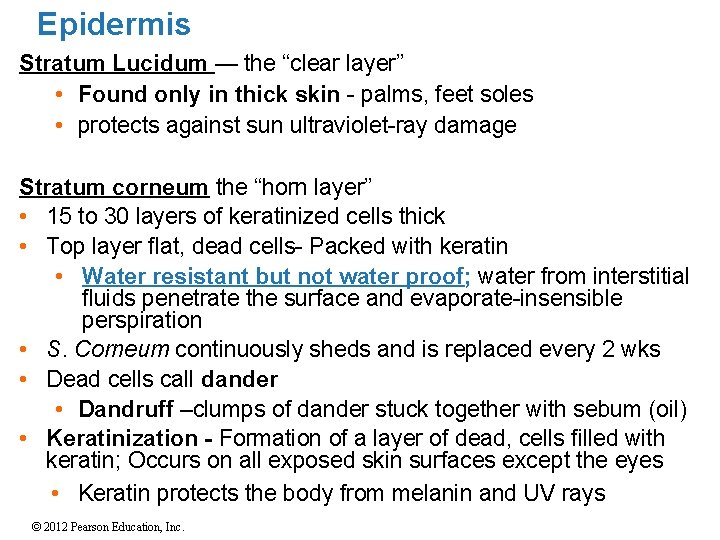
Epidermis Stratum Lucidum — the “clear layer” • Found only in thick skin - palms, feet soles • protects against sun ultraviolet-ray damage Stratum corneum the “horn layer” • 15 to 30 layers of keratinized cells thick • Top layer flat, dead cells- Packed with keratin • Water resistant but not water proof; water from interstitial fluids penetrate the surface and evaporate-insensible perspiration • S. Corneum continuously sheds and is replaced every 2 wks • Dead cells call dander • Dandruff –clumps of dander stuck together with sebum (oil) • Keratinization - Formation of a layer of dead, cells filled with keratin; Occurs on all exposed skin surfaces except the eyes • Keratin protects the body from melanin and UV rays © 2012 Pearson Education, Inc.
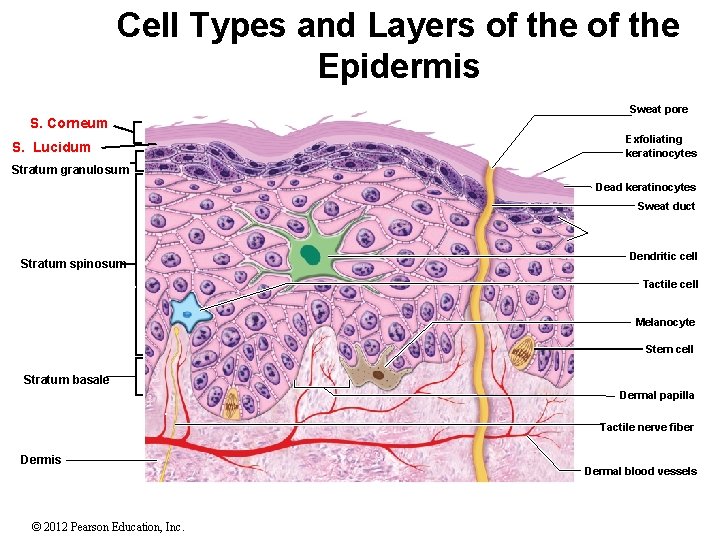
Cell Types and Layers of the Epidermis Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. S. Corneum Sweat pore Exfoliating keratinocytes S. Lucidum Stratum granulosum Dead keratinocytes Sweat duct Living keratinocytes Dendritic cell Stratum spinosum Tactile cell Melanocyte Stem cell Stratum basale Dermal papilla Tactile nerve fiber Dermis © 2012 Pearson Education, Inc. Dermal blood vessels Figure 6. 3
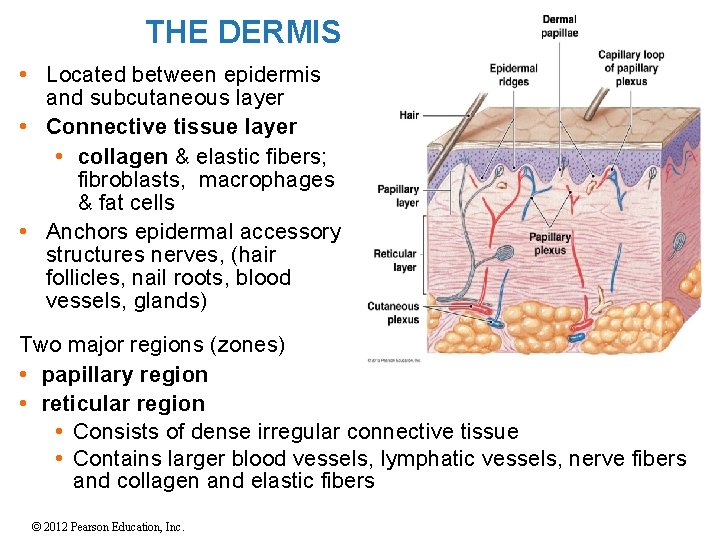
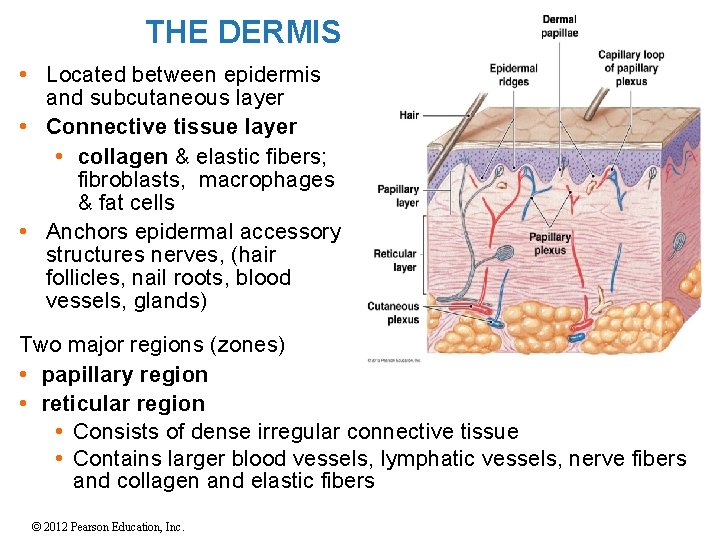
THE DERMIS • Located between epidermis and subcutaneous layer • Connective tissue layer • collagen & elastic fibers; fibroblasts, macrophages & fat cells • Anchors epidermal accessory structures nerves, (hair follicles, nail roots, blood vessels, glands) Two major regions (zones) • papillary region • reticular region • Consists of dense irregular connective tissue • Contains larger blood vessels, lymphatic vessels, nerve fibers and collagen and elastic fibers © 2012 Pearson Education, Inc.
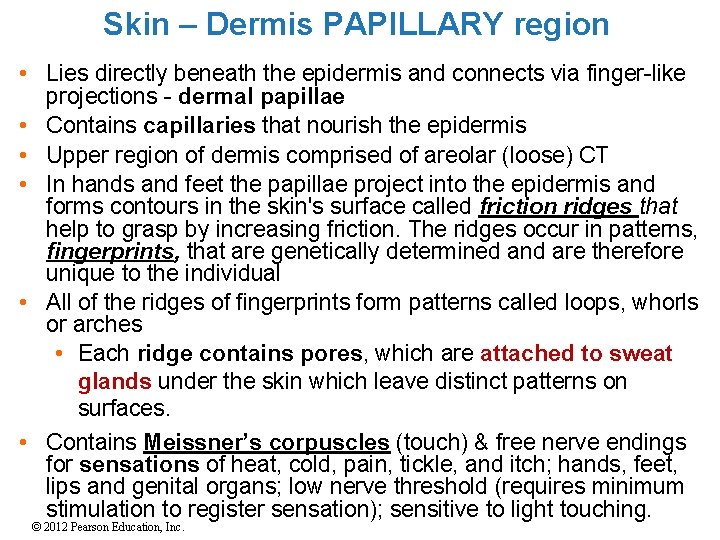
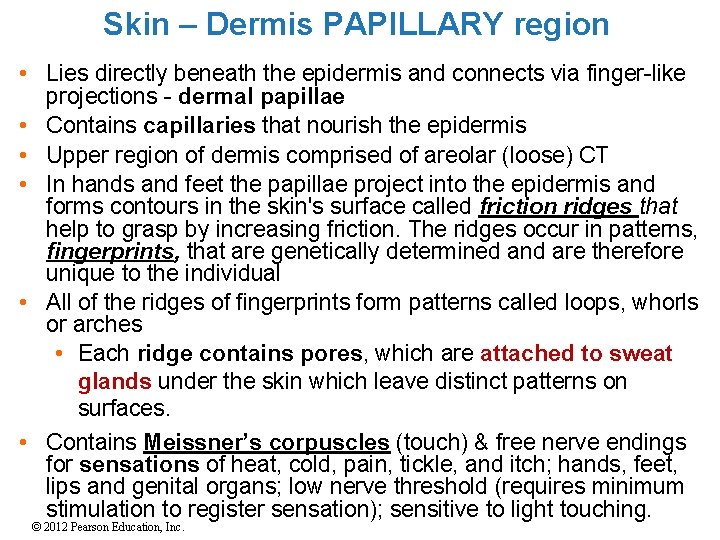
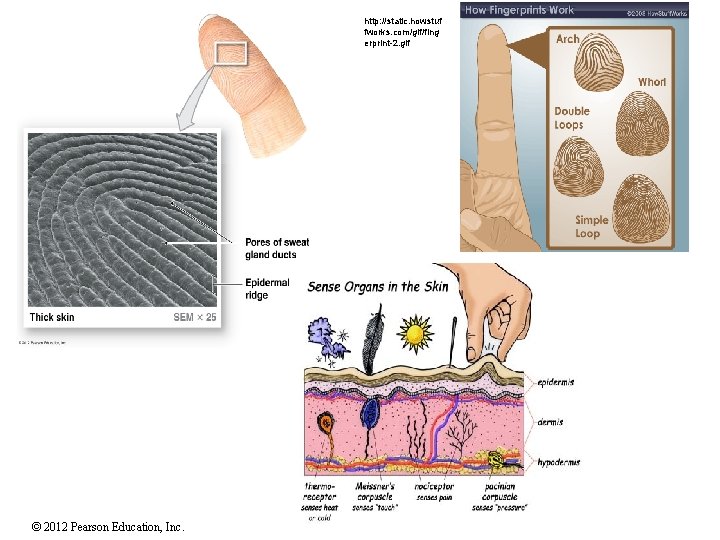
Skin – Dermis PAPILLARY region • Lies directly beneath the epidermis and connects via finger-like projections - dermal papillae • Contains capillaries that nourish the epidermis • Upper region of dermis comprised of areolar (loose) CT • In hands and feet the papillae project into the epidermis and forms contours in the skin's surface called friction ridges that help to grasp by increasing friction. The ridges occur in patterns, fingerprints, that are genetically determined and are therefore unique to the individual • All of the ridges of fingerprints form patterns called loops, whorls or arches • Each ridge contains pores, which are attached to sweat glands under the skin which leave distinct patterns on surfaces. • Contains Meissner’s corpuscles (touch) & free nerve endings for sensations of heat, cold, pain, tickle, and itch; hands, feet, lips and genital organs; low nerve threshold (requires minimum stimulation to register sensation); sensitive to light touching. © 2012 Pearson Education, Inc.
http: //classes. midlandstech. edu/carterp/Courses/bio 110/chap 09/Slide 2. JPG © 2012 Pearson Education, Inc.
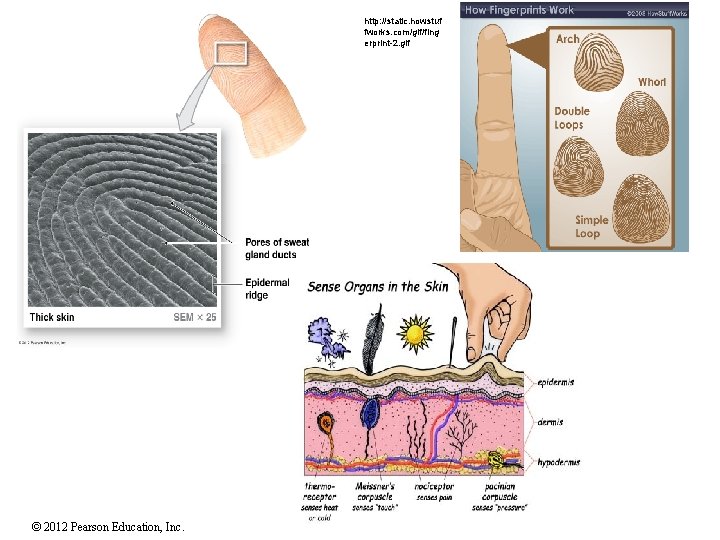
http: //static. howstuf fworks. com/gif/fing erprint-2. gif © 2012 Pearson Education, Inc.
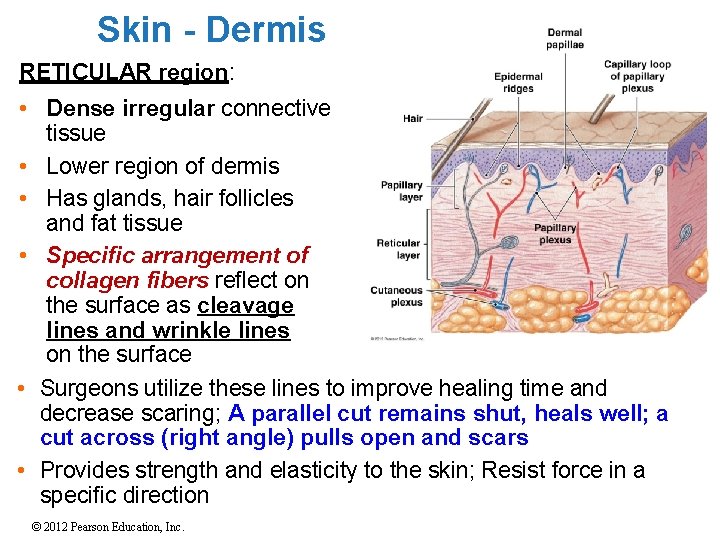
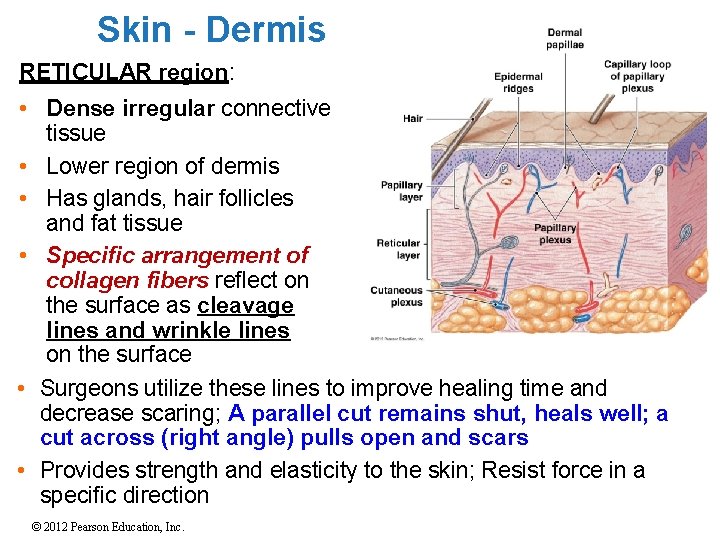
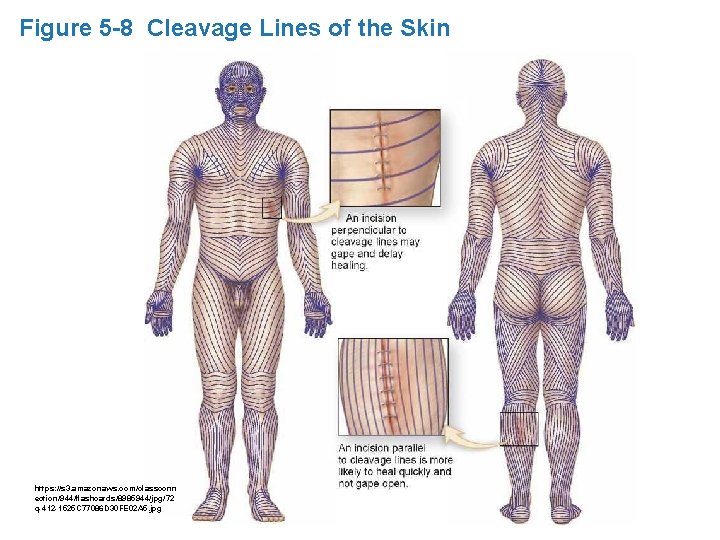
Skin - Dermis RETICULAR region: • Dense irregular connective tissue • Lower region of dermis • Has glands, hair follicles and fat tissue • Specific arrangement of collagen fibers reflect on the surface as cleavage lines and wrinkle lines on the surface • Surgeons utilize these lines to improve healing time and decrease scaring; A parallel cut remains shut, heals well; a cut across (right angle) pulls open and scars • Provides strength and elasticity to the skin; Resist force in a specific direction © 2012 Pearson Education, Inc.
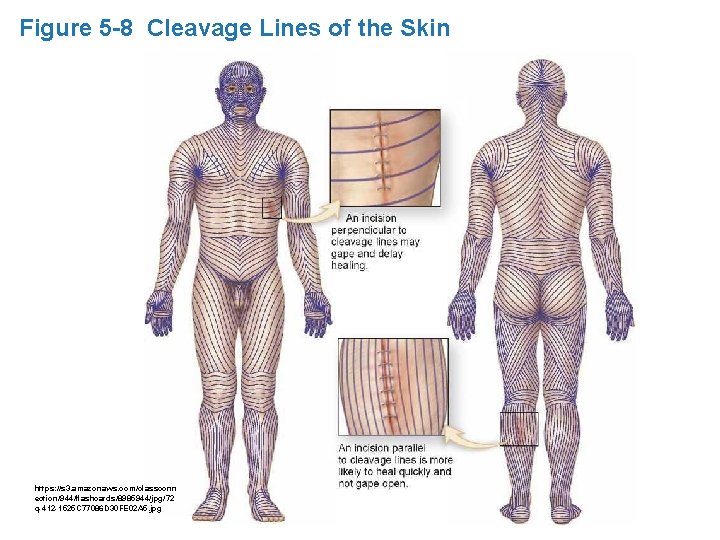
Figure 5 -8 Cleavage Lines of the Skin https: //s 3. amazonaws. com/classconn ection/944/flashcards/8985944/jpg/72 q-412 -1525 C 77086 D 30 FE 02 A 5. jpg © 2012 Pearson Education, Inc.
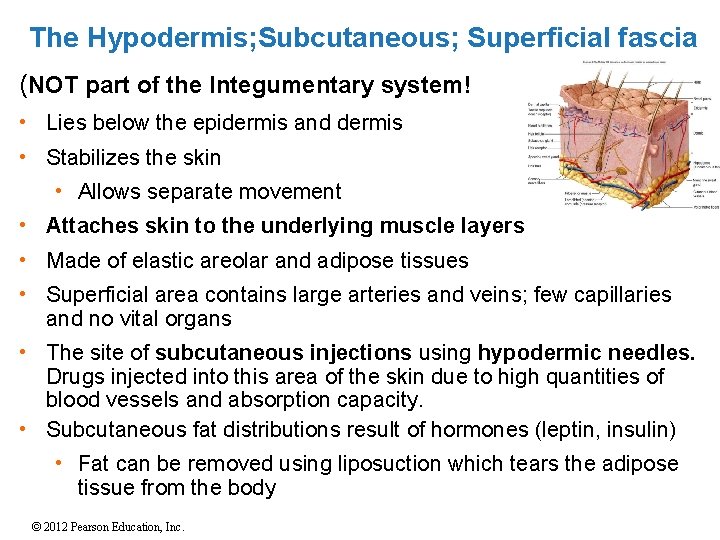
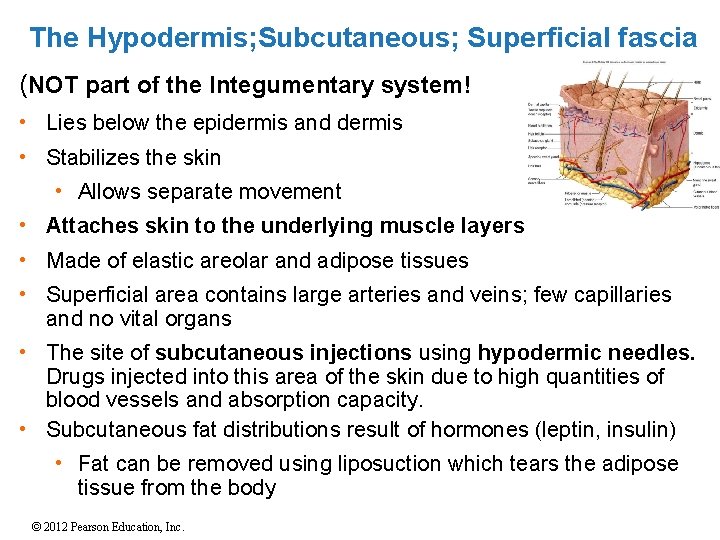
The Hypodermis; Subcutaneous; Superficial fascia (NOT part of the Integumentary system! • Lies below the epidermis and dermis • Stabilizes the skin • Allows separate movement • Attaches skin to the underlying muscle layers • Made of elastic areolar and adipose tissues • Superficial area contains large arteries and veins; few capillaries and no vital organs • The site of subcutaneous injections using hypodermic needles. Drugs injected into this area of the skin due to high quantities of blood vessels and absorption capacity. • Subcutaneous fat distributions result of hormones (leptin, insulin) • Fat can be removed using liposuction which tears the adipose tissue from the body © 2012 Pearson Education, Inc.
Accessory Structures: HAIR • Located in dermis • Project through the skin surface • 2. 5 million hairs; 75% on general body surface and not the head • Body covered with hair, except: • Palms; Soles; Lips; Portions of external genitalia • Functions of Hair • Protects and insulates • Guards openings against particles and insects • Sensitivity to very touch • Types of Hair • Vellus Hair: Soft, fine; covers body surface • Terminal hairs: Heavy, pigmented • Head, eyebrows, eyelashes, and pubic area • Other parts of body after puberty © 2012 Pearson Education, Inc.
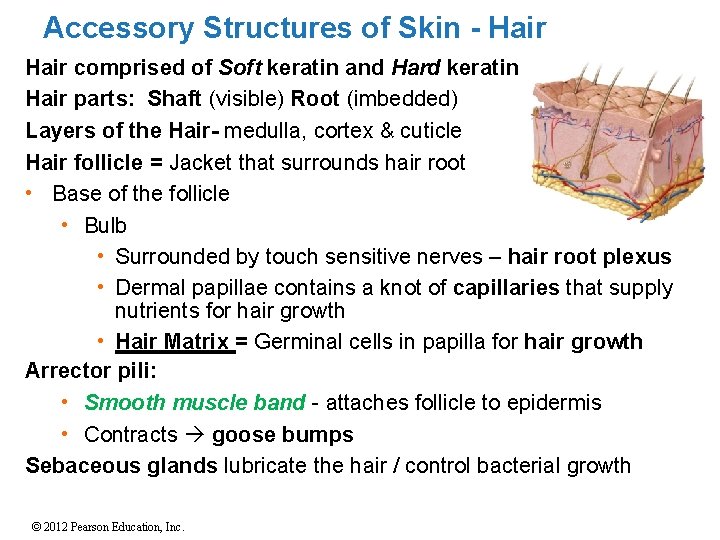
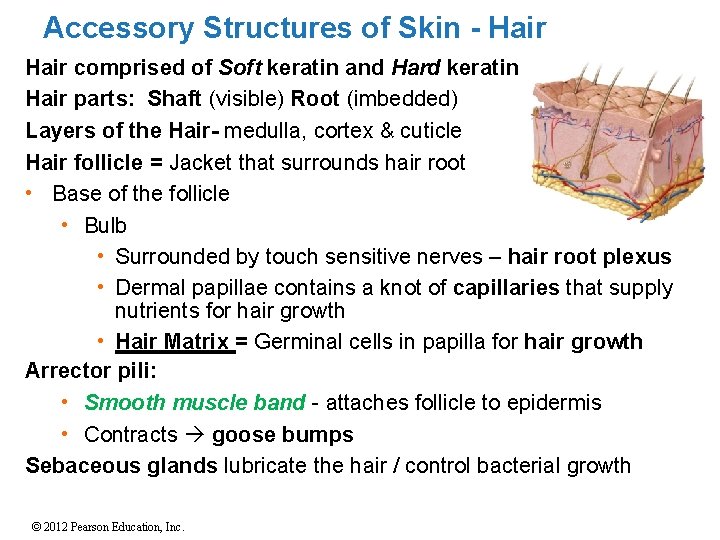
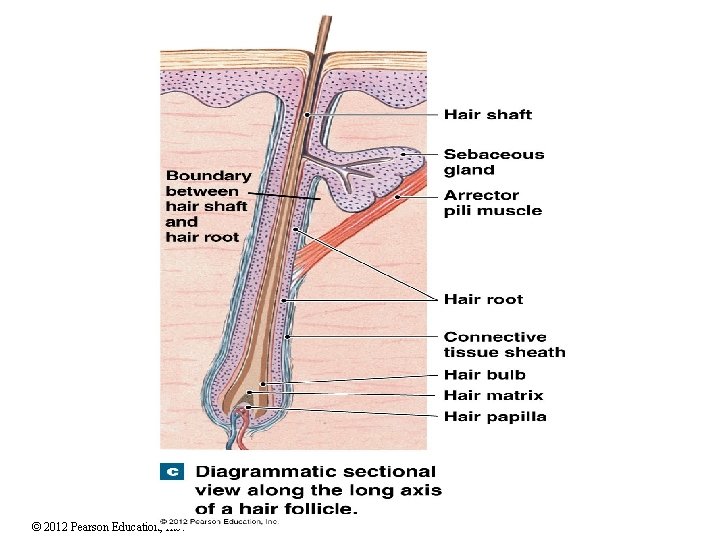
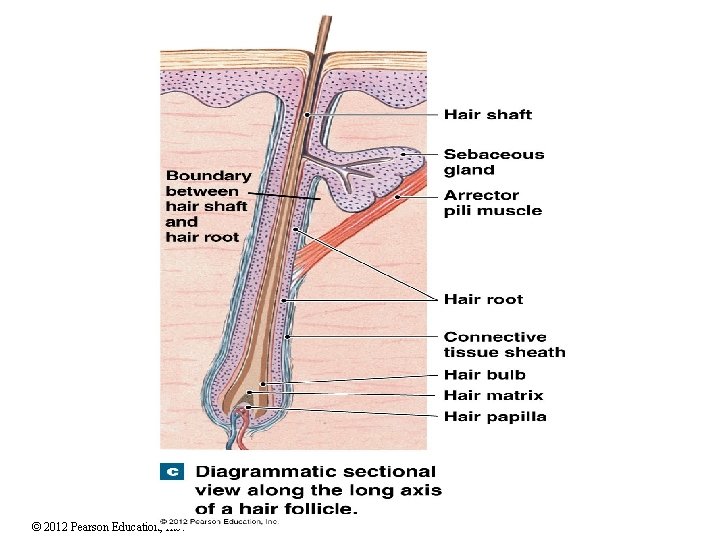
Accessory Structures of Skin - Hair comprised of Soft keratin and Hard keratin Hair parts: Shaft (visible) Root (imbedded) Layers of the Hair- medulla, cortex & cuticle Hair follicle = Jacket that surrounds hair root • Base of the follicle • Bulb • Surrounded by touch sensitive nerves – hair root plexus • Dermal papillae contains a knot of capillaries that supply nutrients for hair growth • Hair Matrix = Germinal cells in papilla for hair growth Arrector pili: • Smooth muscle band - attaches follicle to epidermis • Contracts goose bumps Sebaceous glands lubricate the hair / control bacterial growth © 2012 Pearson Education, Inc.
© 2012 Pearson Education, Inc.
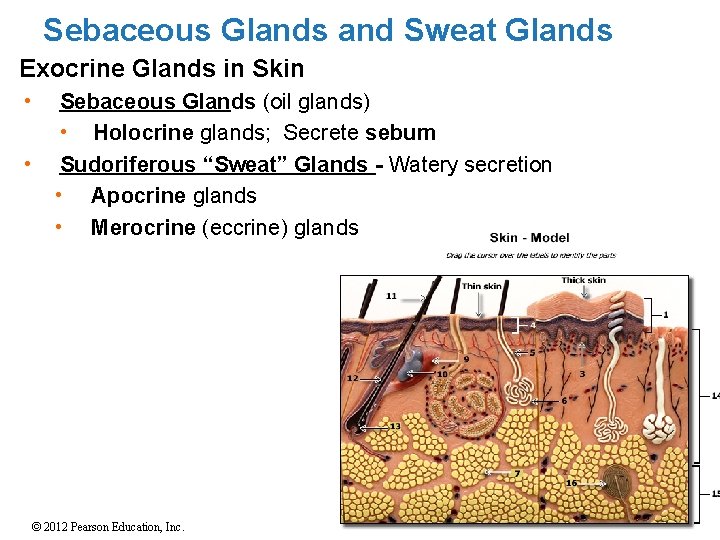
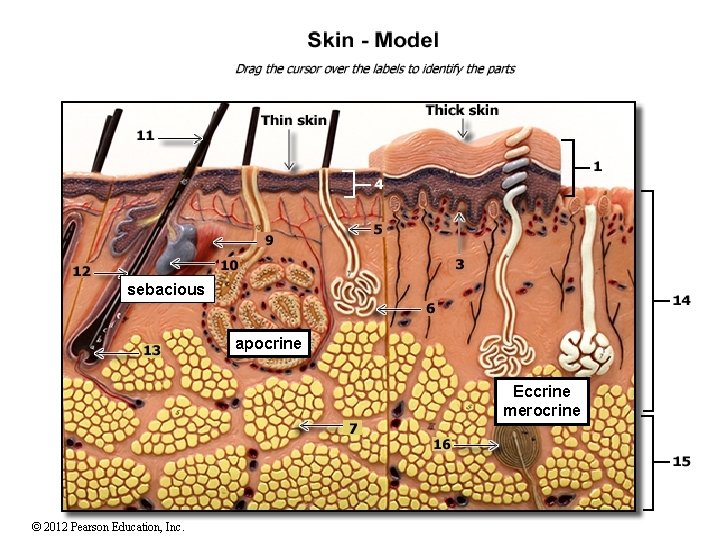
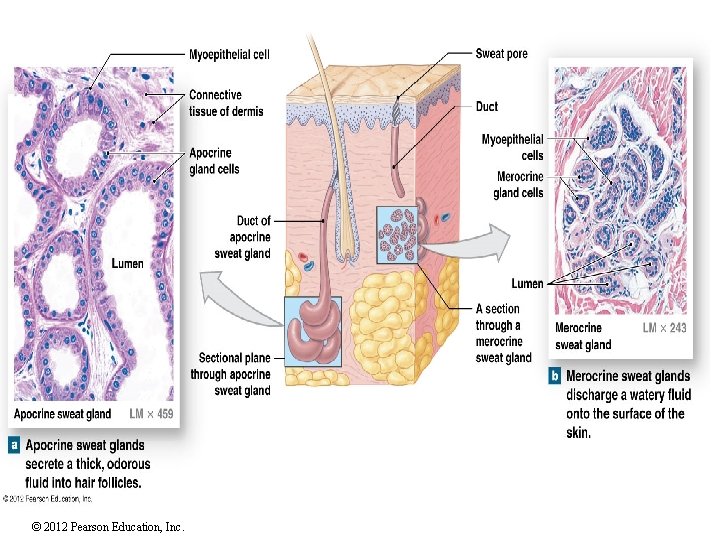
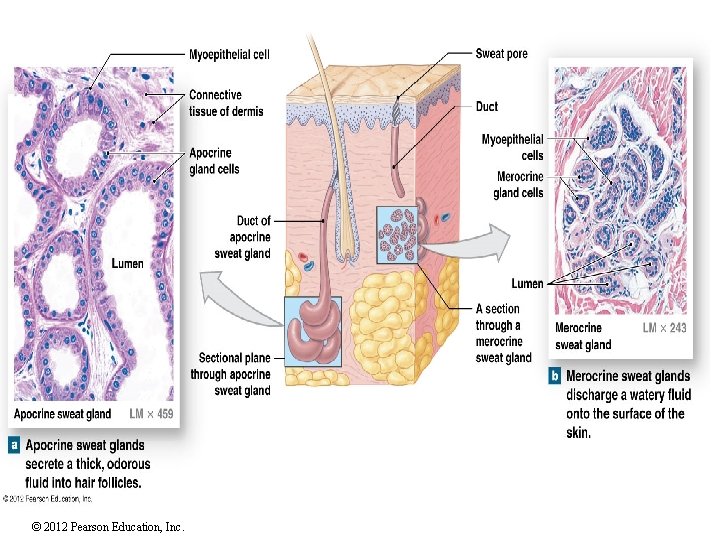
Sebaceous Glands and Sweat Glands Exocrine Glands in Skin • • Sebaceous Glands (oil glands) • Holocrine glands; Secrete sebum Sudoriferous “Sweat” Glands - Watery secretion • Apocrine glands • Merocrine (eccrine) glands © 2012 Pearson Education, Inc.
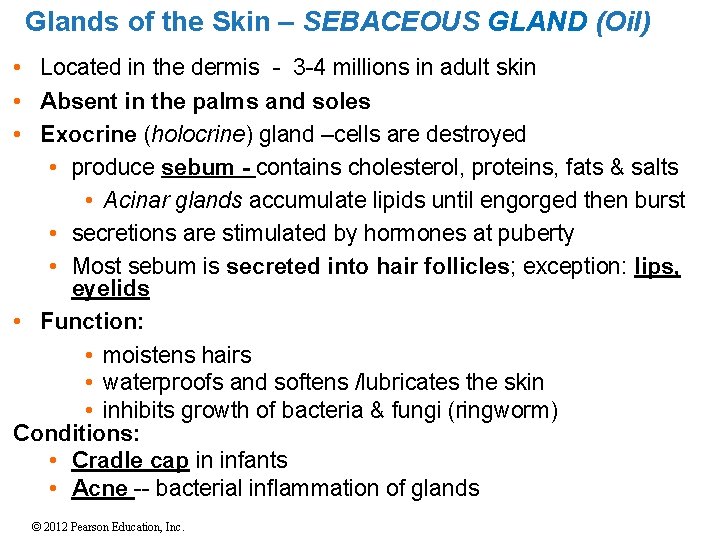
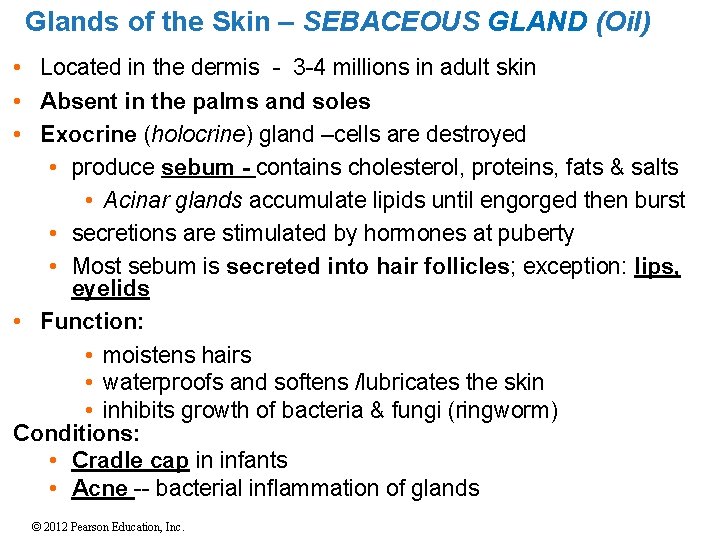
Glands of the Skin – SEBACEOUS GLAND (Oil) • Located in the dermis - 3 -4 millions in adult skin • Absent in the palms and soles • Exocrine (holocrine) gland –cells are destroyed • produce sebum - contains cholesterol, proteins, fats & salts • Acinar glands accumulate lipids until engorged then burst • secretions are stimulated by hormones at puberty • Most sebum is secreted into hair follicles; exception: lips, eyelids • Function: • moistens hairs • waterproofs and softens /lubricates the skin • inhibits growth of bacteria & fungi (ringworm) Conditions: • Cradle cap in infants • Acne -- bacterial inflammation of glands © 2012 Pearson Education, Inc.
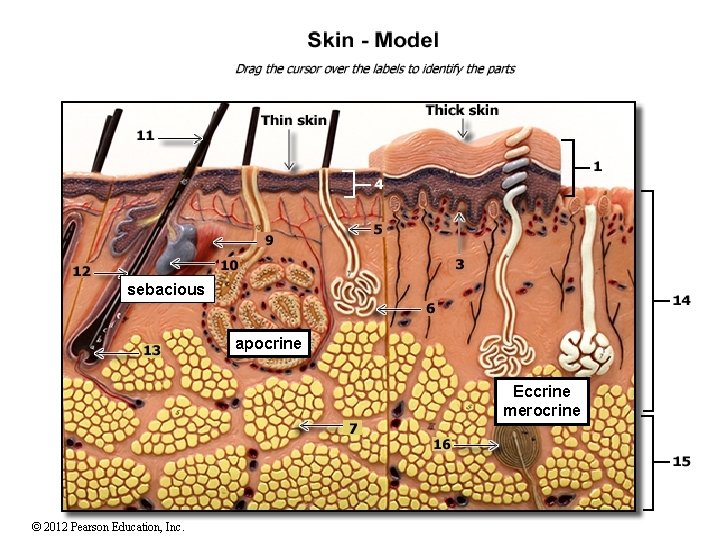
sebacious apocrine Eccrine merocrine © 2012 Pearson Education, Inc.
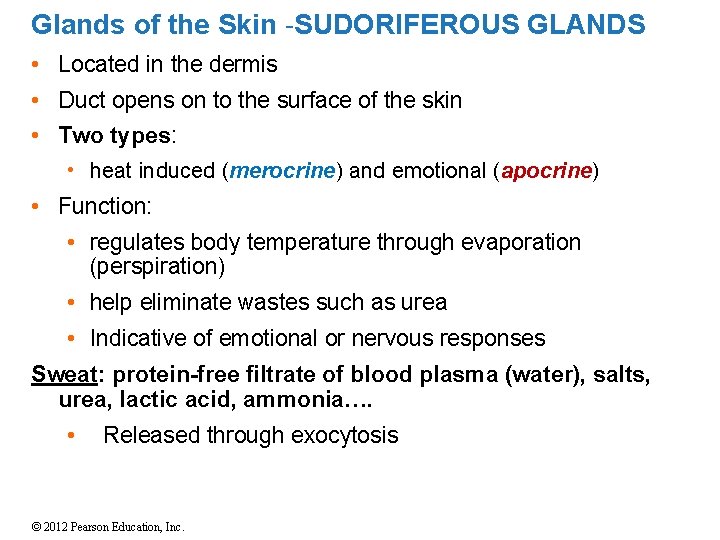
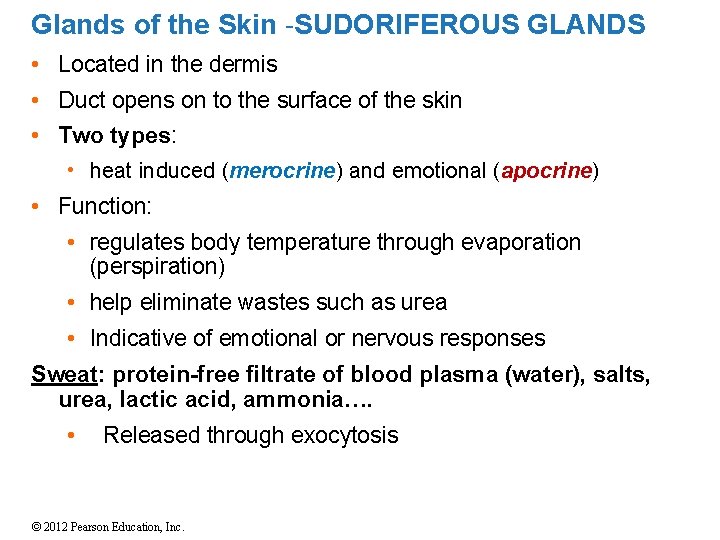
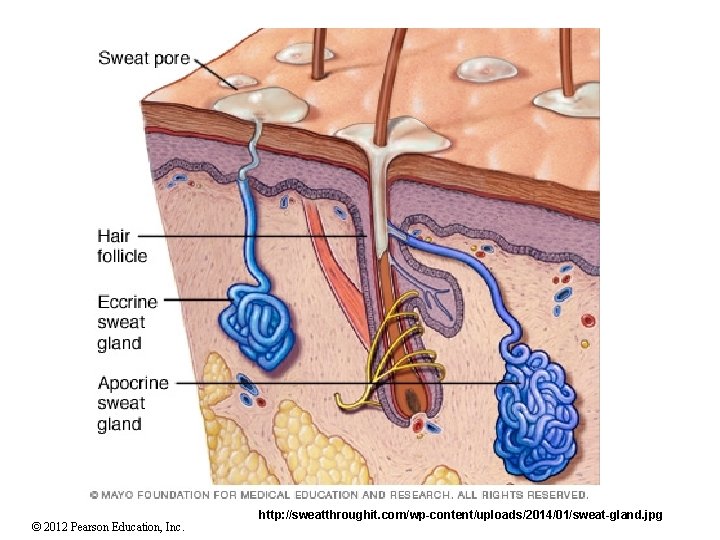
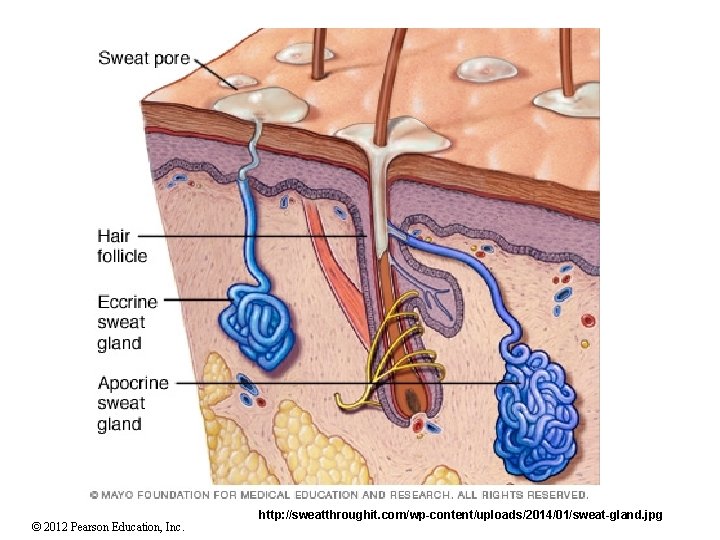
Glands of the Skin -SUDORIFEROUS GLANDS • Located in the dermis • Duct opens on to the surface of the skin • Two types: • heat induced (merocrine) and emotional (apocrine) • Function: • regulates body temperature through evaporation (perspiration) • help eliminate wastes such as urea • Indicative of emotional or nervous responses Sweat: protein-free filtrate of blood plasma (water), salts, urea, lactic acid, ammonia…. • Released through exocytosis © 2012 Pearson Education, Inc.
© 2012 Pearson Education, Inc. http: //sweatthroughit. com/wp-content/uploads/2014/01/sweat-gland. jpg
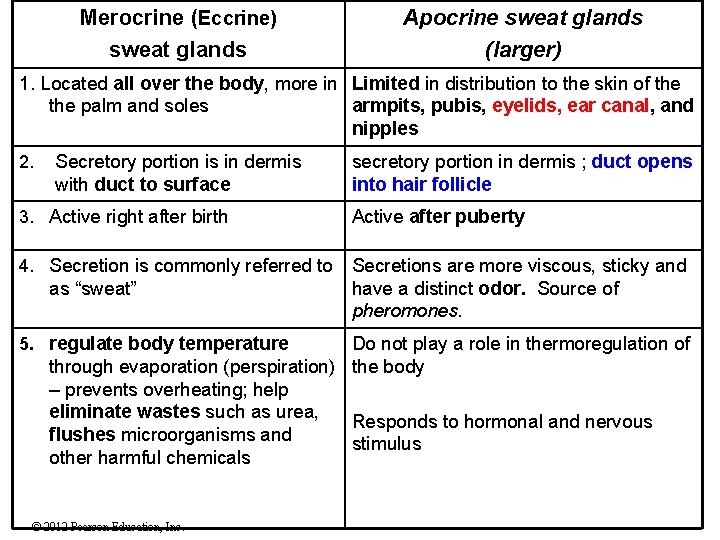
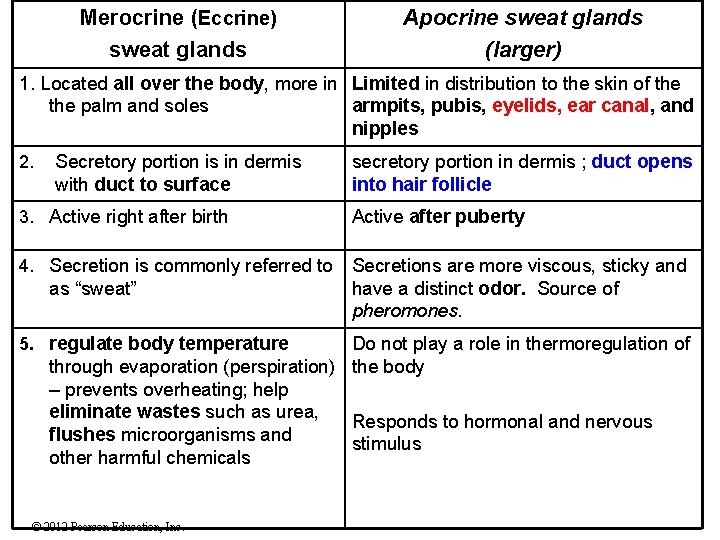
Merocrine (Eccrine) sweat glands Apocrine sweat glands (larger) 1. Located all over the body, more in Limited in distribution to the skin of the palm and soles armpits, pubis, eyelids, ear canal, and nipples 2. Secretory portion is in dermis with duct to surface secretory portion in dermis ; duct opens into hair follicle 3. Active right after birth Active after puberty 4. Secretion is commonly referred to Secretions are more viscous, sticky and have a distinct odor. Source of pheromones. as “sweat” 5. regulate body temperature Do not play a role in thermoregulation of through evaporation (perspiration) the body – prevents overheating; help eliminate wastes such as urea, Responds to hormonal and nervous flushes microorganisms and stimulus other harmful chemicals © 2012 Pearson Education, Inc.
© 2012 Pearson Education, Inc.
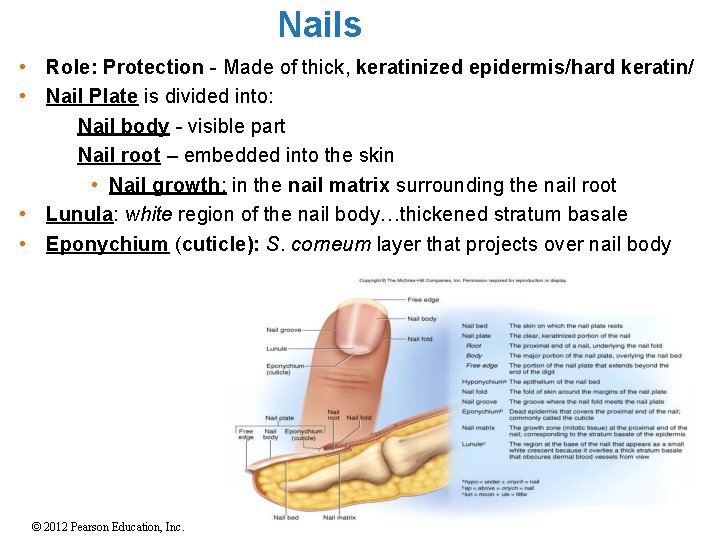
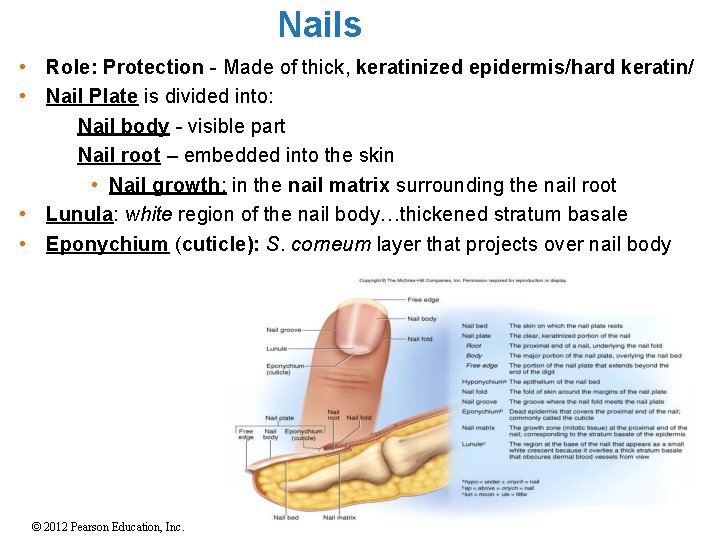
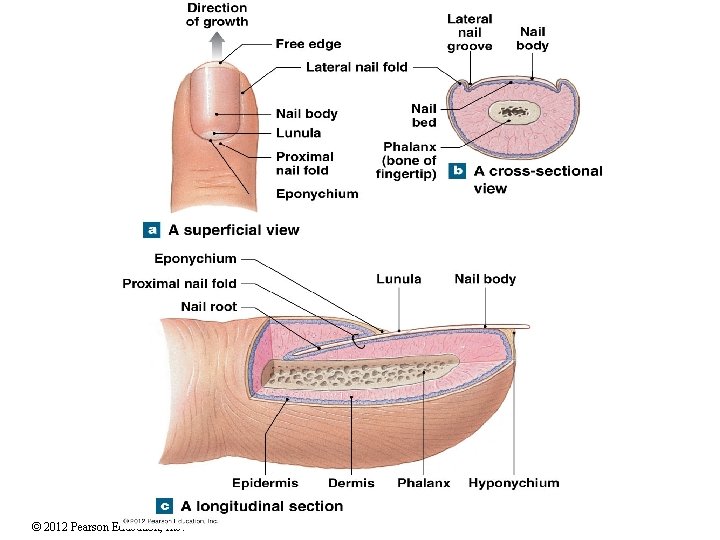
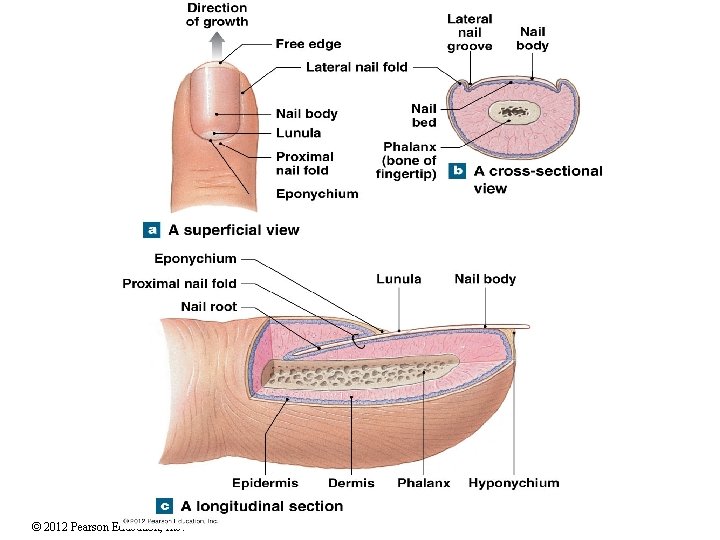
Nails • Role: Protection - Made of thick, keratinized epidermis/hard keratin/ • Nail Plate is divided into: • Nail body - visible part • Nail root – embedded into the skin • Nail growth: in the nail matrix surrounding the nail root • Lunula: white region of the nail body…thickened stratum basale • Eponychium (cuticle): S. corneum layer that projects over nail body © 2012 Pearson Education, Inc.
© 2012 Pearson Education, Inc.
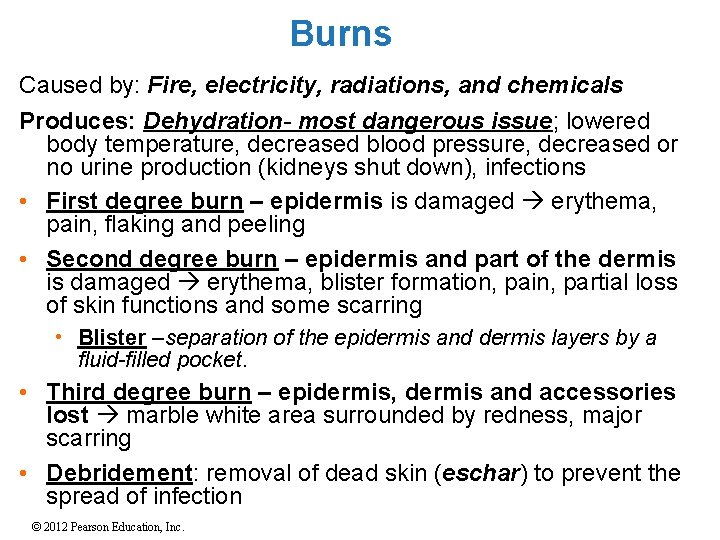
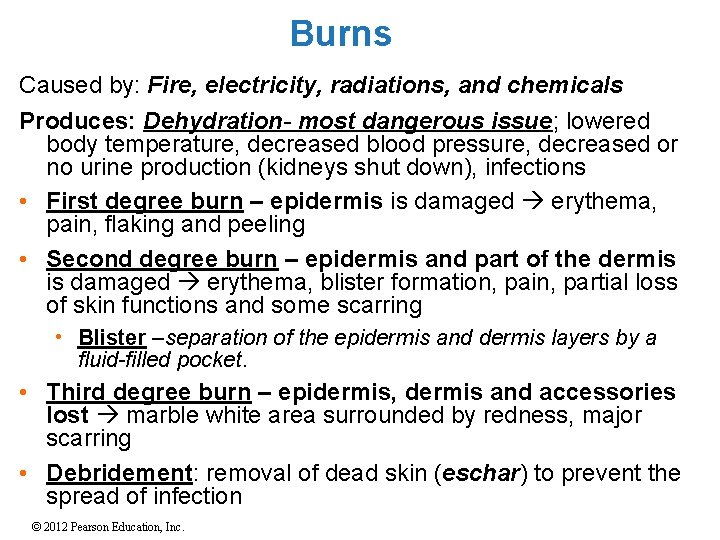
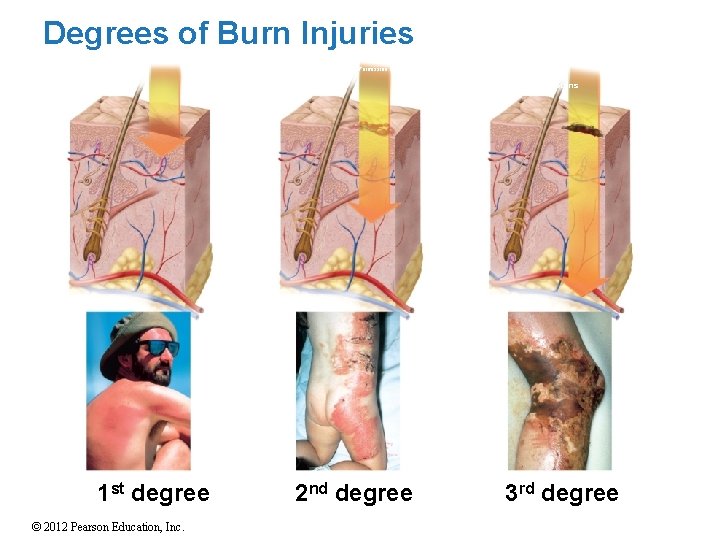
Burns Caused by: Fire, electricity, radiations, and chemicals Produces: Dehydration- most dangerous issue; lowered body temperature, decreased blood pressure, decreased or no urine production (kidneys shut down), infections • First degree burn – epidermis is damaged erythema, pain, flaking and peeling • Second degree burn – epidermis and part of the dermis is damaged erythema, blister formation, pain, partial loss of skin functions and some scarring • Blister –separation of the epidermis and dermis layers by a fluid-filled pocket. • Third degree burn – epidermis, dermis and accessories lost marble white area surrounded by redness, major scarring • Debridement: removal of dead skin (eschar) to prevent the spread of infection © 2012 Pearson Education, Inc.
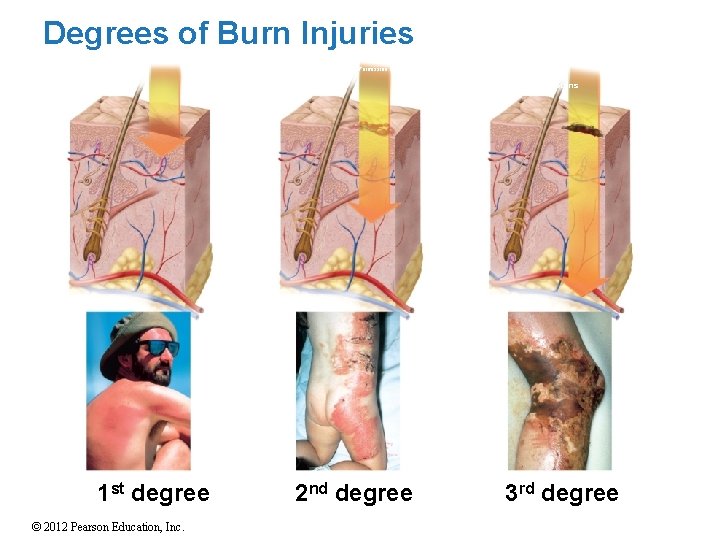
Degrees of Burn Injuries Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Full-thickness burns (a) First degree 1 st degree © 2012 Pearson Education, Inc. (b) Second degree 2 nd degree (c) Third degree 3 rd degree
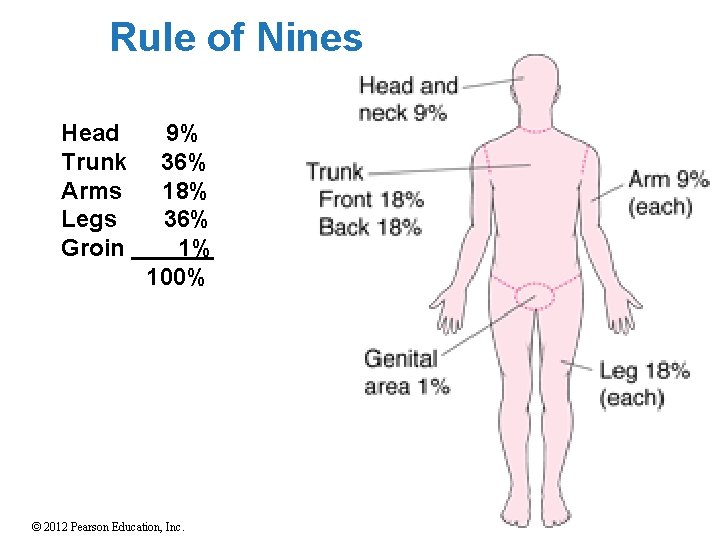
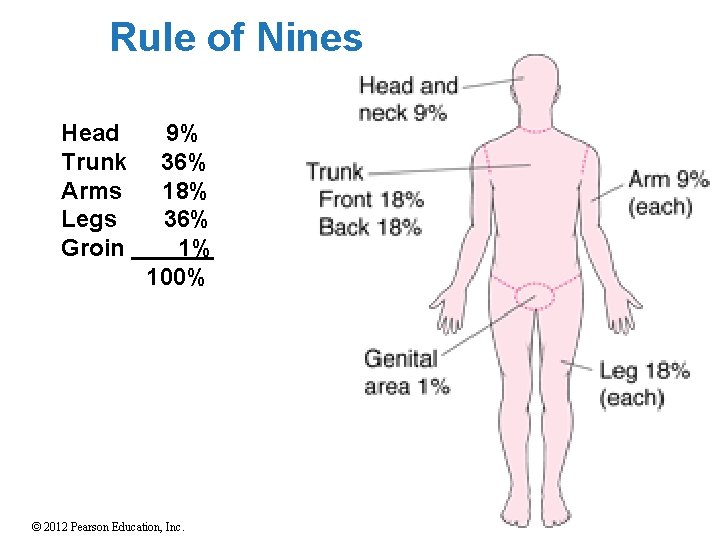
Rule of Nines Head Trunk Arms Legs Groin 9% 36% 18% 36% 1% 100% © 2012 Pearson Education, Inc.
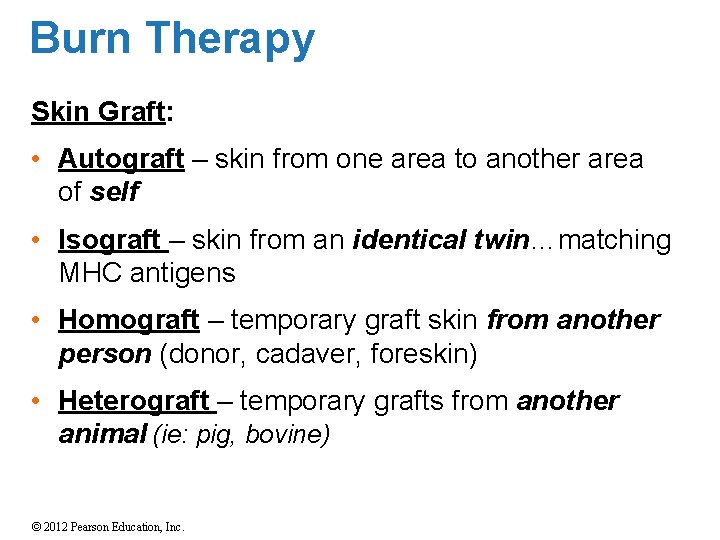
Burn Therapy Skin Graft: • Autograft – skin from one area to another area of self • Isograft – skin from an identical twin…matching MHC antigens • Homograft – temporary graft skin from another person (donor, cadaver, foreskin) • Heterograft – temporary grafts from another animal (ie: pig, bovine) © 2012 Pearson Education, Inc.