Chapter 5 PHYSICAL ASSESSMENT 1 HEALTH ASSESSMENT Physical















- Slides: 43

Chapter 5 PHYSICAL ASSESSMENT 1

HEALTH ASSESSMENT Physical Examination 2
Purposes • Ascertain client’s level of health & physiological function • Identify important factors • Confirm alterations, disease or inability to perform ADLs • Identify need for additional testing / examination • Aid in evaluating outcome of treatment / therapy 3
Subjective and Objective Data • Subjective Data. History – what the patient tells/communicates to you • Objective Data. Exam – what you discover through your physical assessment 4
Possible Client Position During an Examination 5
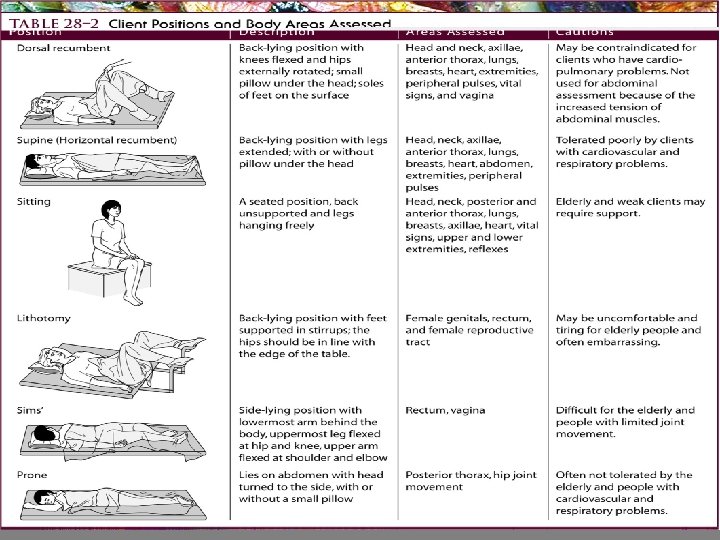
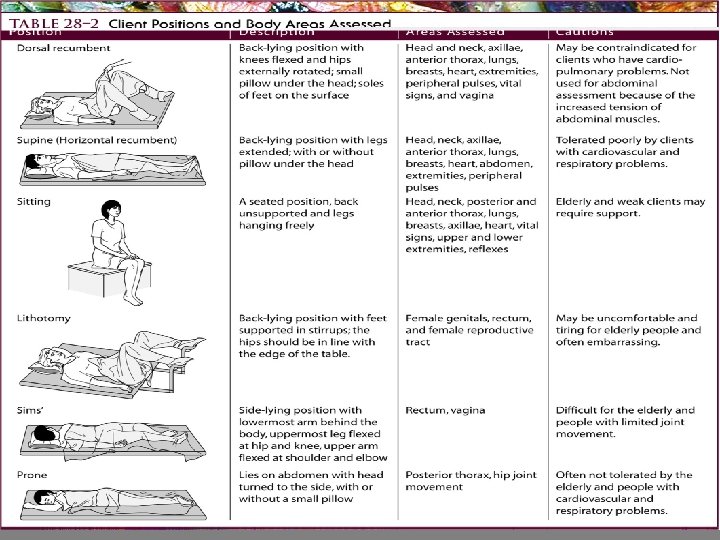
6

Positions for physical Examination • Assessment positions e. g. : (Standing position, Supine position, Sitting position, Dorsal recumbent position, Sims position, Prone position, Knee chest position, and Lithotomy position) • Each position has it's specialty for parts of examination 7
Sitting position • Areas Assessed: Head and neck, back, posterior thorax and lungs, anterior thorax , breasts, axillae, heart, vital signs, and upper extremities • Limitations: Physically weakened client may be unable to sit 8
Supine position • Most normally relaxed position • Areas Assessed: Head and neck anterior thorax and lungs, breasts, axillae, heart, abdomen, extremities, pulses • Limitations: Not use for client SOB, you may need to raise head of bed 9
Dorsal position • Areas Assessed: Head and neck, anterior thorax and lungs, breasts, axillae, heart. • Limitations: Not used for abdominal assessment because it promotes contracture of abdominal muscles 10
. Lithotomy Position • Areas Assessed: Female genitalia and genital tract. • * Limitations: • This position is embarrassing & uncomfortable, so examiner minimizes time that client spends in it. • Client is kept well draped. • This position not used for Client 11 with severe arthritis or other joint
Sims’ position • Areas Assessed: Rectum and vagina. • * Limitations: Joint deformities may prevent client’s ability to Bend hip and knee Prone position: • * Areas Assessed: Musculoskeletal system. • * Limitations: don’t use this position for client with 12 respiratory difficulties

Knee-chest position Areas Assessed: Rectum. Limitations: This position is embarrassing and uncomfortable. Don’t use this position for Clients with arthritis or other joint deformities. • When palpation assess for Crepitus (crackling sensation & noise caused by rubbing of bone fragments). • * If a joint appears swollen and inflamed, detect warmth in the 13 tissues.
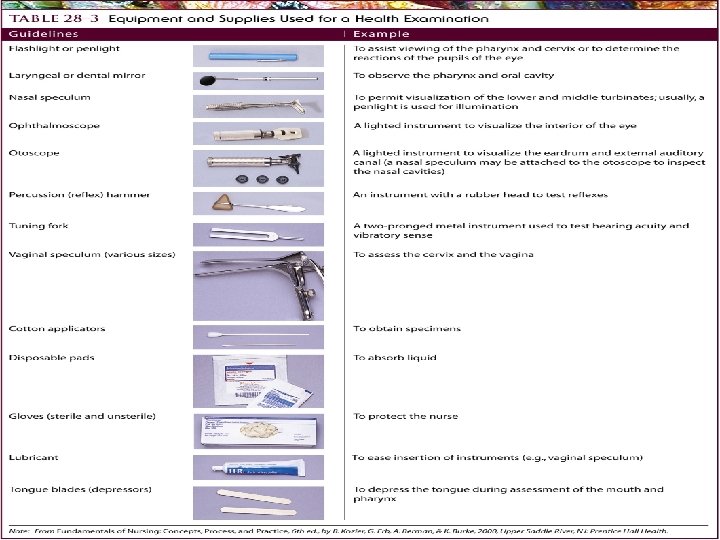
Equipment Preparation For a Health Assessment 14
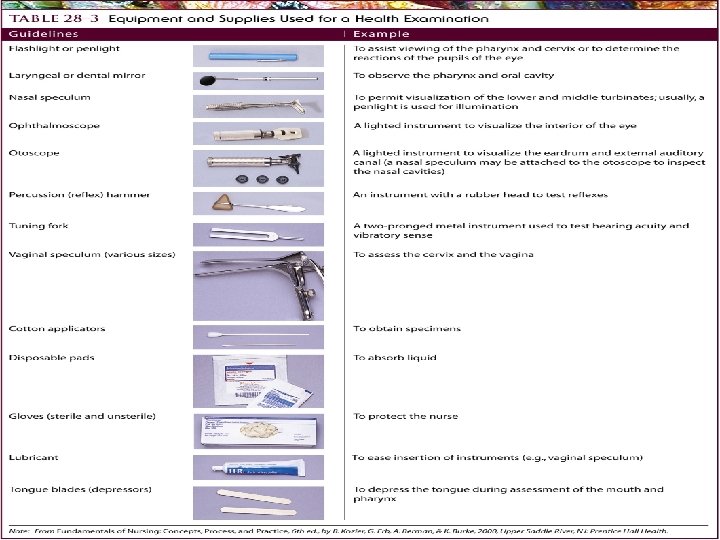
15
Indications for the Physical Exam • Routine screening • Eligibility prerequisite for health insurance, military service, job, sports, school • Admission to a hospital or long term care facility 16
STEPS OF ASSESSMENT • Think • Organize Don’t forget…Nutrition / Height & Weight • Environment: • Accommodate special needs (cultural sensitivity) • Equipment - clean surface & clean equipment Room - quiet, warm & well lit • Maintain privacy • Observe & Listen 17

DON’T FORGET…… • REVIEWING GENERAL INFORMATION • INTRODUCTION TO CLIENT • OBTAINING THE HEALTH HISTORY • PAIN ASSESSMENT • THIS IS KEY TO HOLISTIC APPROACH 18
Five Assessment Techniques During A Physical Examination • Inspection • Palpation • Percussion • Auscultation • Olfaction 19

20
Inspection • • • Use vision& smell Always first Look for symmetry Use good lighting Use good exposure 21

22

Principles of Accurate Inspection • Good lightening either day light or artificial light is suitable. • Expose body parts being observed only. • look before touching. • warm room for examination of the client “not cold not hot". • Observe for color, size, location, texture, symmetry, odors, and sounds. • Compare each area inspected with the opposite side of body if possible. • Use pen light to inspect body cavities. 23
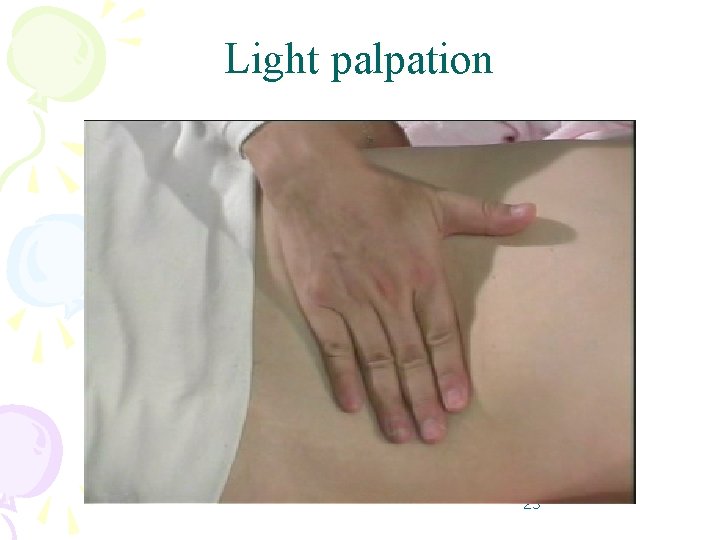
Palpation • Touch & feel with hands to determine: § Texture – use fingertips § Temperature – use back of hand § Moisture § Organ location and size • Slow and systematic • Light to deep • Light palpation (tenderness) • Deep palpation (abdominal organs/masses) 24
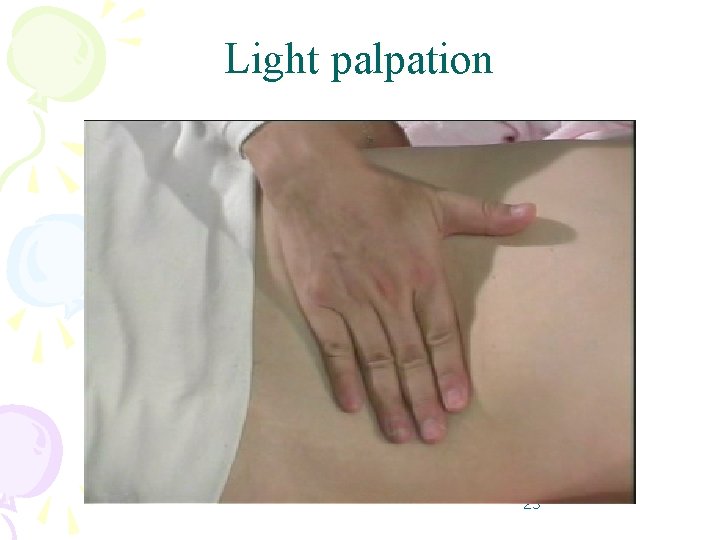
Light palpation 25

Deep palpation 26
Principles for Accurate Palpation • • • Examiner finger nails should be short. Use sensitive part your hand. Light Palpation precedes deep palpation. Start with light then deep palpation Tender area are palpated last Client must relax during palpation. Tell client to take slow deep breath to enhance muscle relaxation. Examine condition of the abdominal organs Depressed areas must be approximately “ 2 cm” Assess turger of skin measured by lightly grasping the body part with finger tips. 27
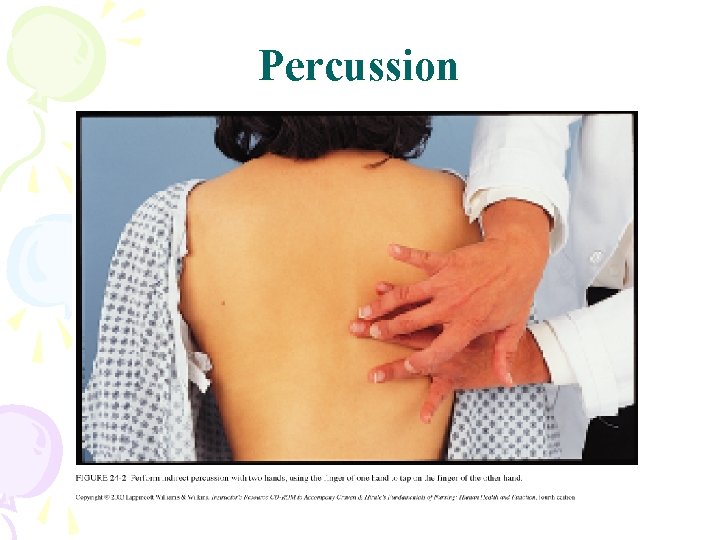
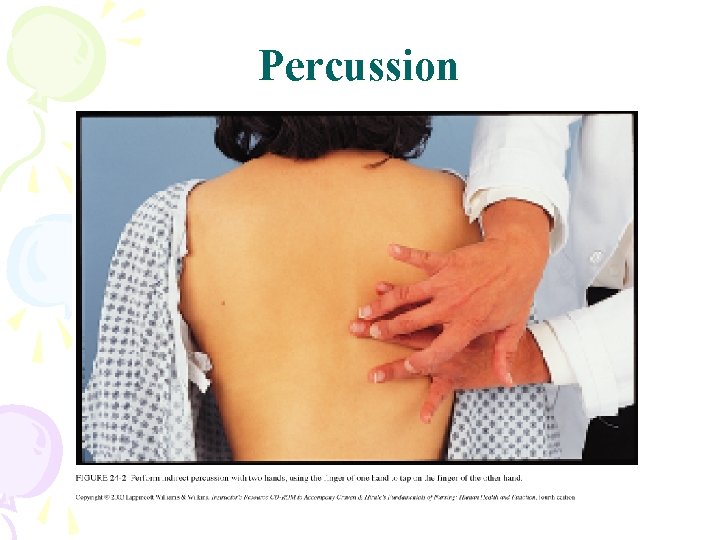
Percussion 28
Percussion • Tapping of body part to assess tenderness, Size, location, density • Direct: with one or two fingers e. g. Sinuses • Indirect: middle finger of left hand against the body surface with palm and fingers remaining off the skin, § and the tip of the middle finger of the right hand strikes the base of the distal joint. § Use a quick & sharp stroke 29

Five Percussion Sounds Produced in Different Body Regions • • Resonant – normal lung Hyper resonant – infant lung, emphysema Tympany – air filled (stomach) Dull – organ (liver, spleen) • Flat – no air (thigh muscle, bone, tumor) 30

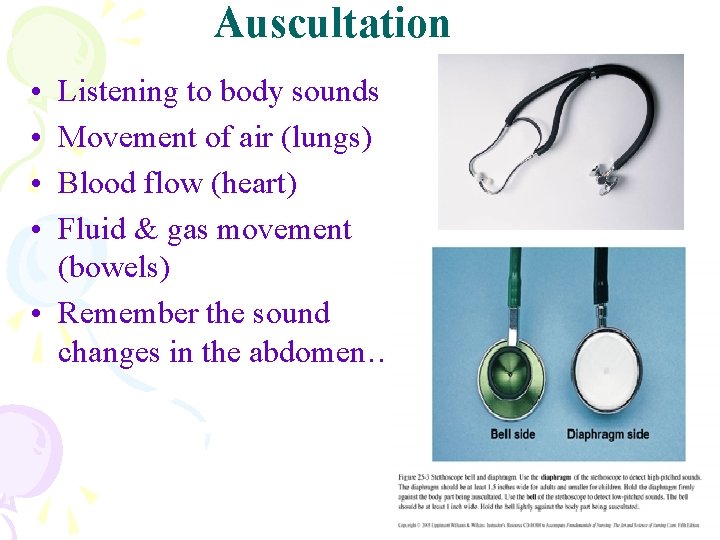
Auscultation 31
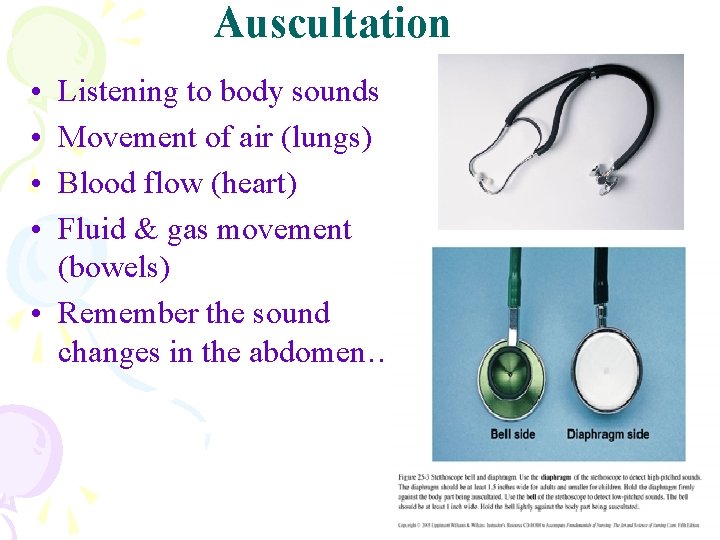
Auscultation • • Listening to body sounds Movement of air (lungs) Blood flow (heart) Fluid & gas movement (bowels) • Remember the sound changes in the abdomen… 32
HOW TO BEGIN… • • Positions for physical exam Using a stethoscope: longer the tube – more sound has to travel Hold diaphragm firmly against client’s skin (NOT THROUGH CLOTHING!!) If using bell – less pressure Warm in your hands first! Listen / Concentrate on the sounds 33
Olfaction Another skill that used during assessment. Certain alteration in body function creates characteristic body odors. Smelling can detect abnormalities that unrecognized by other means. 34
Assessment of Characteristic Odors • • • Alcohol odor from oral mouth ingestion of alcohol. Ammonia from urine means urinary tract infection. Bad odor from skin, (e. g. under arms and beneath breasts) means poor hygiene, excess perspiration (bromidrosis)(foul smelling perspiration). • Feces odor from wound site means wound abscess, but this odor from vomitus this means bowel obstruction, and if the odor from rectal area this means fecal incontinence. • Foul smelling stool in infant means mal absorption syndrome. 35
Assessment of Characteristic Odors…cont • Halitosis from oral cavity means poor dental hygiene. • Sweat, fruity ketenes from mouth DKA • Musty odor from organ with cast part means infection inside cast. • Fetid odor from tracheotomy or mucous secretions means infection 36

Basic Guidelines for Physical Assessment • Obtain a nursing history. • Maintain Privacy. • Explain the procedure and purpose of each examined part of the client. • Follow a planned order of examination for each body system. 37

Basic Guidelines for Physical Assessment cont. . • Inspect, palpate, percuss, and then auscultate, except in the abdomen auscultate then percuss to avoid alteration in the bowel sounds • Compare symmetrical sides of the body and organs. • Assess both structure and function of each body part and organ e. g. (the appearance and condition of the ear as well as its hearing function) 38
Basic Guidelines for Physical Assessment cont. . • If there is abnormality assess for further data. e. g. radiation of pain, effect on eating? bowels? ADLs? • Assess self physical assessment (e. g. exam of the breast, testicular exam, foot care for the diabetic) • Allow time for client questions • “Remember: the most important guideline for adequate physical assessment is, continuous practice of physical assessment skills” 39

Variation in Physical Assessment of the Pediatric Client • Sequence of physical assessment depends on the development level of the client. • Establishment of rapport with the child and significant others is the most essential step in physical assessment data. • Reduce fearing of child prior to beginning the examination. • You may require physical restraint of the client with help of another adult. 40
Variation in Physical Assessment of the Pediatric Client…cont • Assistance from the child’s significant caregiver may facilitate examination. • Assessment approach of the child based on child's response. • Uncooperative attitude toward the examiner is a normal finding in children from birth to early adolescence. 41
Variations for Physical Assessment of the Geriatric Client • Remember normal variation related to aging. • Divide the physical assessment into parts in order to avoid fatigue. • Provide room with comfortable temperature. • Allow sufficient time for client to respond to directions. • If possible assess the elderly clients in a setting position. • Give him/her fulltime to understand you. 42

THANK YOU 43
 Chapter 3 health wellness and health disparities
Chapter 3 health wellness and health disparities Glencoe health chapter 1 understanding health and wellness
Glencoe health chapter 1 understanding health and wellness Chapter 1 health and wellness fundamentals
Chapter 1 health and wellness fundamentals Glencoe health chapter 9
Glencoe health chapter 9 Copyright
Copyright Chapter 10 chemical reactions answer key
Chapter 10 chemical reactions answer key Chapter 11 stoichiometry answer key
Chapter 11 stoichiometry answer key Chapter 9 chemical reactions study guide
Chapter 9 chemical reactions study guide Chapter 9 surface water chapter assessment answer key
Chapter 9 surface water chapter assessment answer key Chapter 2 assessment physics answers
Chapter 2 assessment physics answers Chemistry the central science 14th edition
Chemistry the central science 14th edition Chapter 2 chapter assessment
Chapter 2 chapter assessment Ionic compound properties
Ionic compound properties Chapter 7 chapter assessment ionic compounds and metals
Chapter 7 chapter assessment ionic compounds and metals Role and responsibility of occupational health nurse
Role and responsibility of occupational health nurse National program related to children
National program related to children Louisiana department of health and hospitals licensing
Louisiana department of health and hospitals licensing Similarities between health education and health promotion
Similarities between health education and health promotion Whole health circle of health
Whole health circle of health Health and social care component 3
Health and social care component 3 Health promotion world health organization
Health promotion world health organization Pet 3351 ucf
Pet 3351 ucf Health education and health propaganda
Health education and health propaganda Optimal health in each of the six components of health
Optimal health in each of the six components of health Victorian curriculum health and physical education
Victorian curriculum health and physical education Health triangle project
Health triangle project Who global strategy on diet, physical activity and health
Who global strategy on diet, physical activity and health Health education aims
Health education aims Physical disorders and health psychology
Physical disorders and health psychology Section physical fitness and your health
Section physical fitness and your health Chapter 3 benefits of physical activity
Chapter 3 benefits of physical activity Victorian curriculum physical education
Victorian curriculum physical education Whats the health triangle
Whats the health triangle Social health triangle
Social health triangle Hltaap002 confirm physical health status
Hltaap002 confirm physical health status Physical environment determinants of health
Physical environment determinants of health Health related physical fitness definition
Health related physical fitness definition Physical health
Physical health A state of complete physical mental and social well-being
A state of complete physical mental and social well-being Health is state of complete physical
Health is state of complete physical 3 parts of health triangle
3 parts of health triangle Health enhancing physical activity definition
Health enhancing physical activity definition Assessment skills
Assessment skills Health assessment
Health assessment