Chapter 43 The Immune System nonspecific specific immunity
- Slides: 44
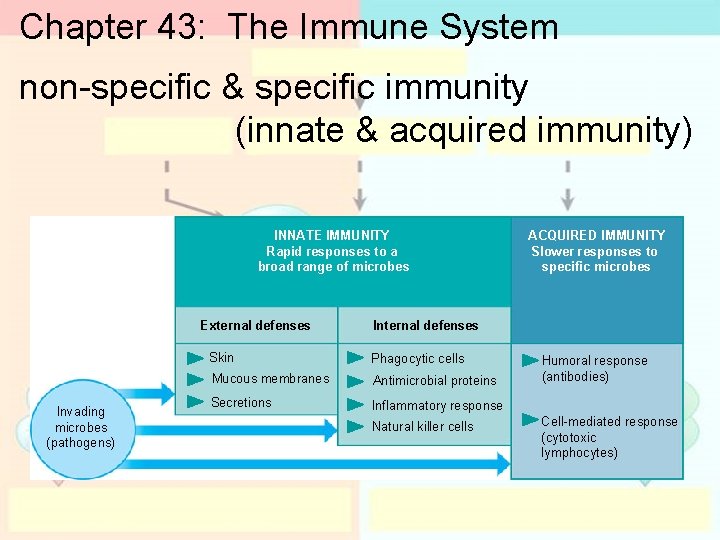
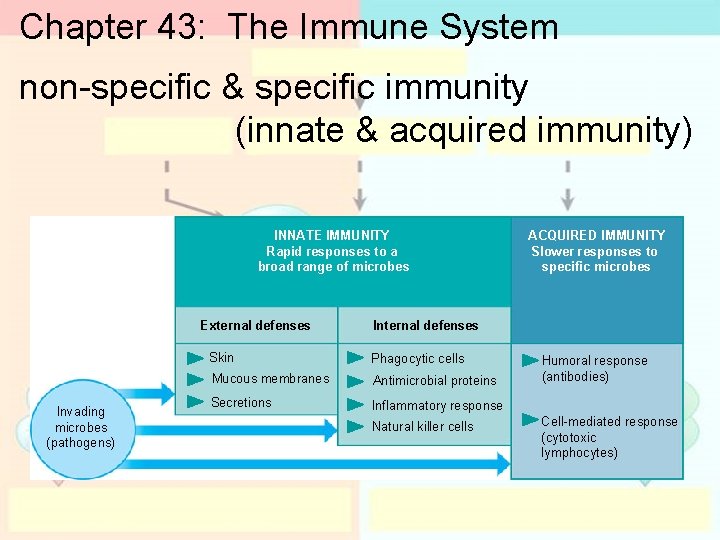
Chapter 43: The Immune System non-specific & specific immunity (innate & acquired immunity) INNATE IMMUNITY Rapid responses to a broad range of microbes External defenses Invading microbes (pathogens) ACQUIRED IMMUNITY Slower responses to specific microbes Internal defenses Skin Phagocytic cells Mucous membranes Antimicrobial proteins Secretions Inflammatory response Natural killer cells Humoral response (antibodies) Cell-mediated response (cytotoxic lymphocytes)
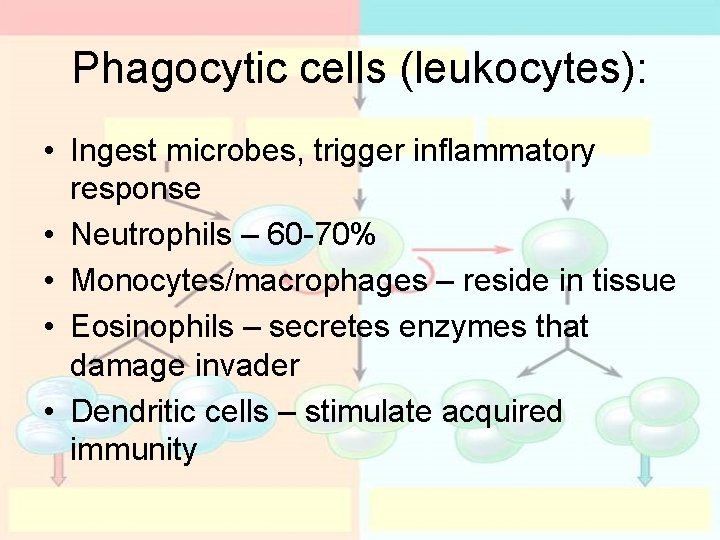
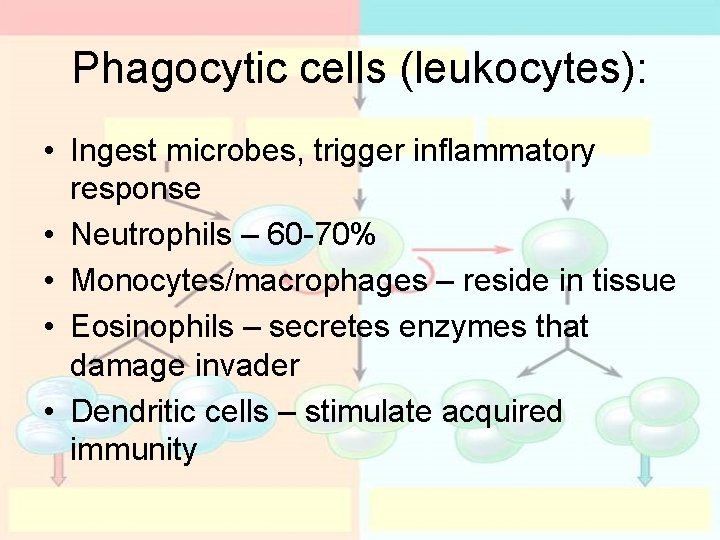
Phagocytic cells (leukocytes): • Ingest microbes, trigger inflammatory response • Neutrophils – 60 -70% • Monocytes/macrophages – reside in tissue • Eosinophils – secretes enzymes that damage invader • Dendritic cells – stimulate acquired immunity
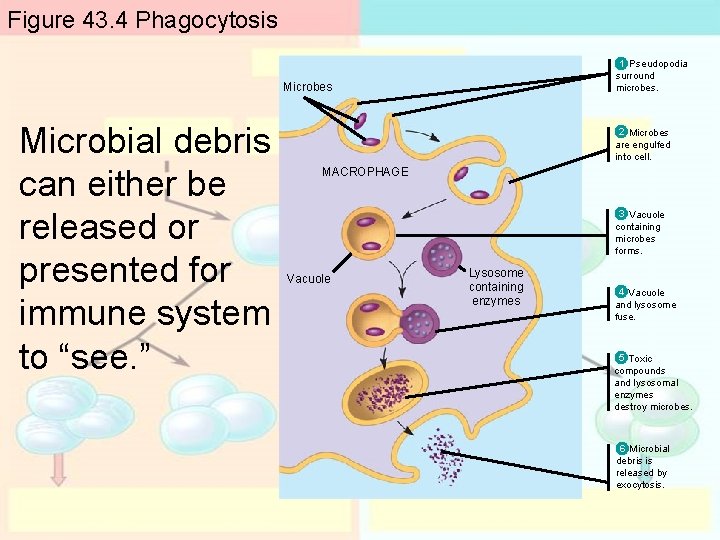
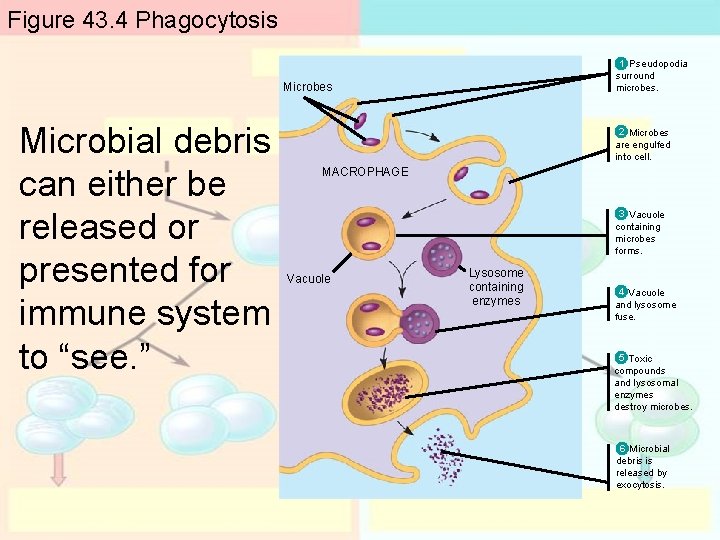
Figure 43. 4 Phagocytosis 1 Pseudopodia surround microbes. Microbes Microbial debris can either be released or presented for immune system to “see. ” 2 Microbes are engulfed into cell. MACROPHAGE 3 Vacuole containing microbes forms. Vacuole Lysosome containing enzymes 4 Vacuole and lysosome fuse. 5 Toxic compounds and lysosomal enzymes destroy microbes. 6 Microbial debris is released by exocytosis.
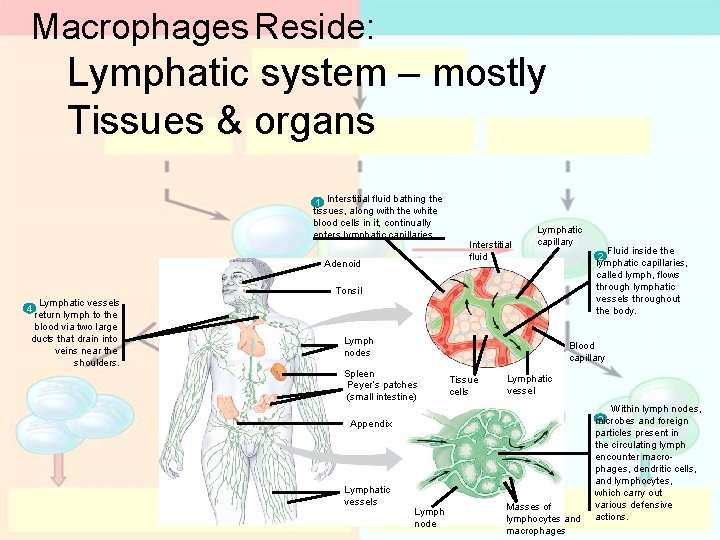
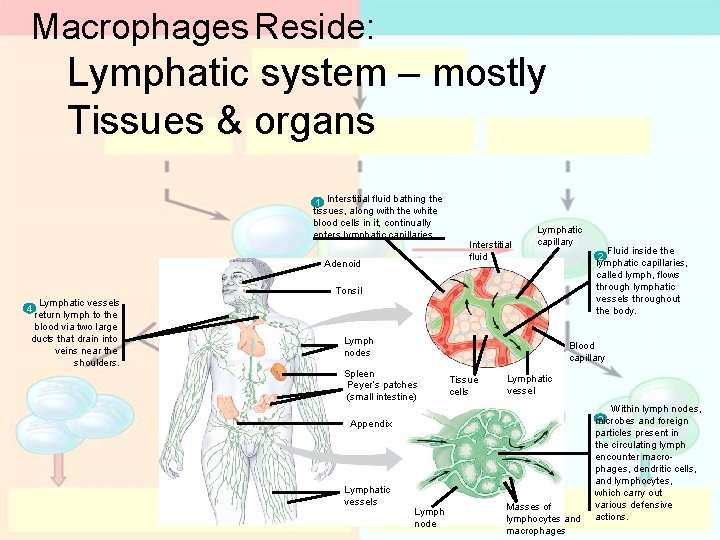
Macrophages Reside: Lymphatic system – mostly Tissues & organs 1 Interstitial fluid bathing the tissues, along with the white blood cells in it, continually enters lymphatic capillaries. Adenoid Interstitial fluid Lymphatic capillary Tonsil Lymphatic vessels 4 return lymph to the blood via two large ducts that drain into veins near the shoulders. Lymph nodes Blood capillary Spleen Peyer’s patches (small intestine) Tissue cells Lymphatic vessel Appendix Lymphatic vessels Fluid inside the 2 lymphatic capillaries, called lymph, flows through lymphatic vessels throughout the body. Lymph node Masses of lymphocytes and macrophages Within lymph nodes, 3 microbes and foreign particles present in the circulating lymph encounter macrophages, dendritic cells, and lymphocytes, which carry out various defensive actions.
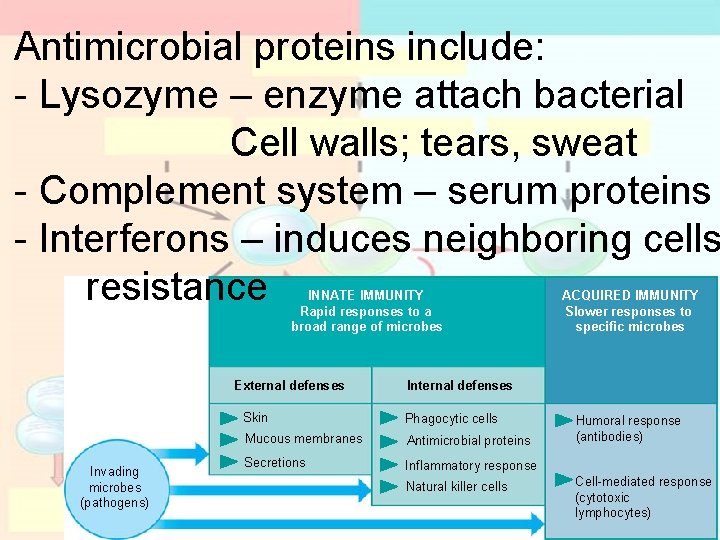
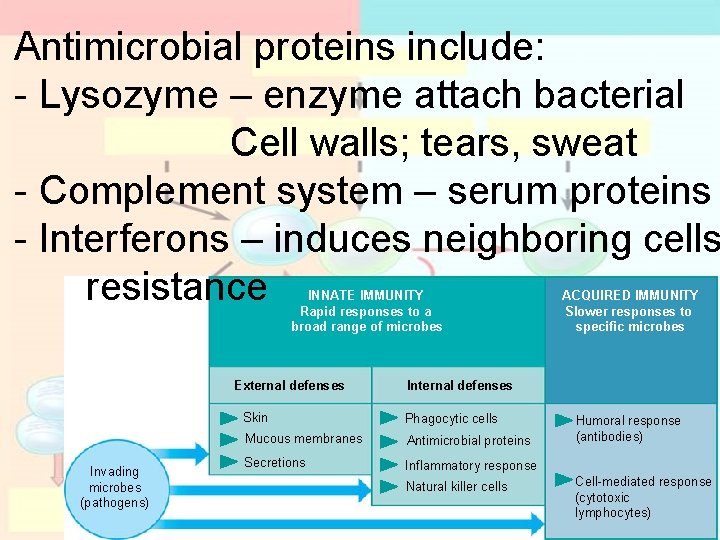
Antimicrobial proteins include: - Lysozyme – enzyme attach bacterial Cell walls; tears, sweat - Complement system – serum proteins - Interferons – induces neighboring cells resistance INNATE IMMUNITY Rapid responses to a broad range of microbes External defenses Invading microbes (pathogens) ACQUIRED IMMUNITY Slower responses to specific microbes Internal defenses Skin Phagocytic cells Mucous membranes Antimicrobial proteins Secretions Inflammatory response Natural killer cells Humoral response (antibodies) Cell-mediated response (cytotoxic lymphocytes)
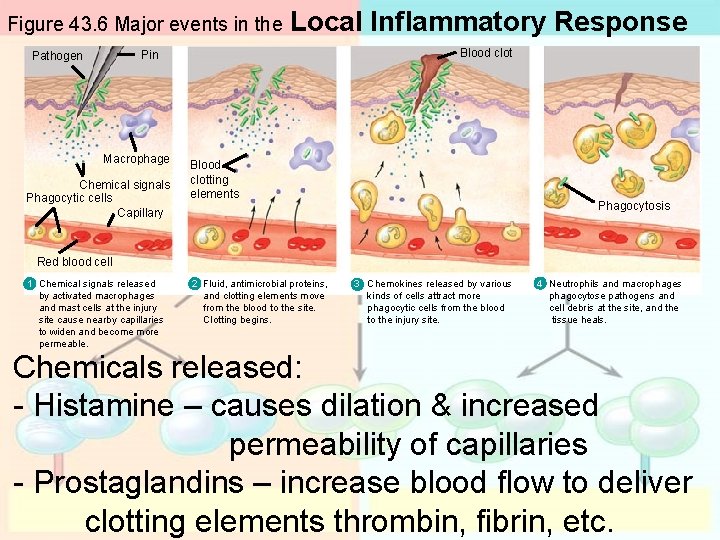
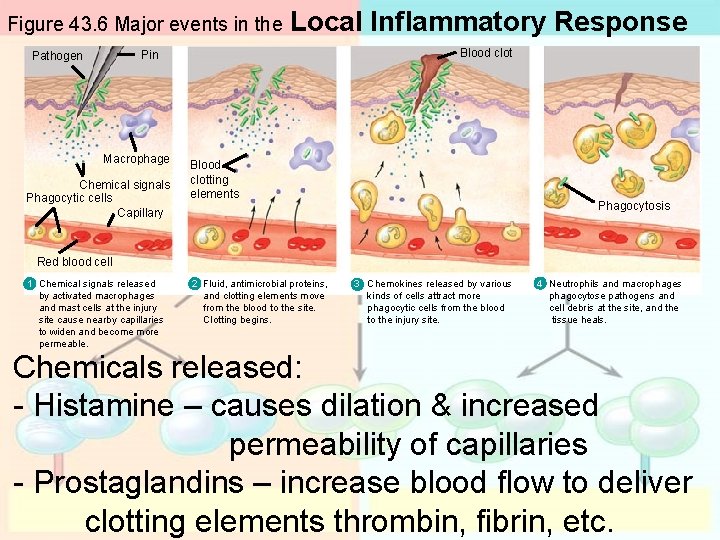
Figure 43. 6 Major events in the Local Inflammatory Response Blood clot Pin Pathogen Macrophage Chemical signals Phagocytic cells Capillary Blood clotting elements Phagocytosis Red blood cell 1 Chemical signals released by activated macrophages and mast cells at the injury site cause nearby capillaries to widen and become more permeable. 2 Fluid, antimicrobial proteins, and clotting elements move from the blood to the site. Clotting begins. 3 Chemokines released by various kinds of cells attract more phagocytic cells from the blood to the injury site. 4 Neutrophils and macrophages phagocytose pathogens and cell debris at the site, and the tissue heals. Chemicals released: - Histamine – causes dilation & increased permeability of capillaries - Prostaglandins – increase blood flow to deliver clotting elements thrombin, fibrin, etc.
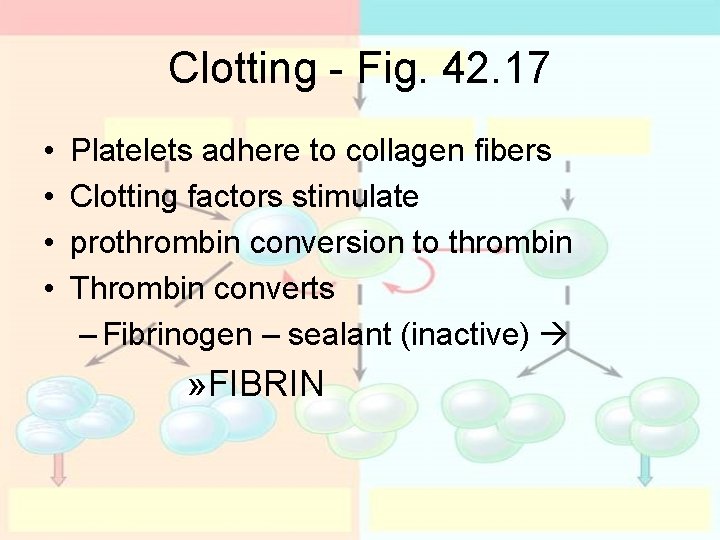
Clotting - Fig. 42. 17 • • Platelets adhere to collagen fibers Clotting factors stimulate prothrombin conversion to thrombin Thrombin converts – Fibrinogen – sealant (inactive) » FIBRIN
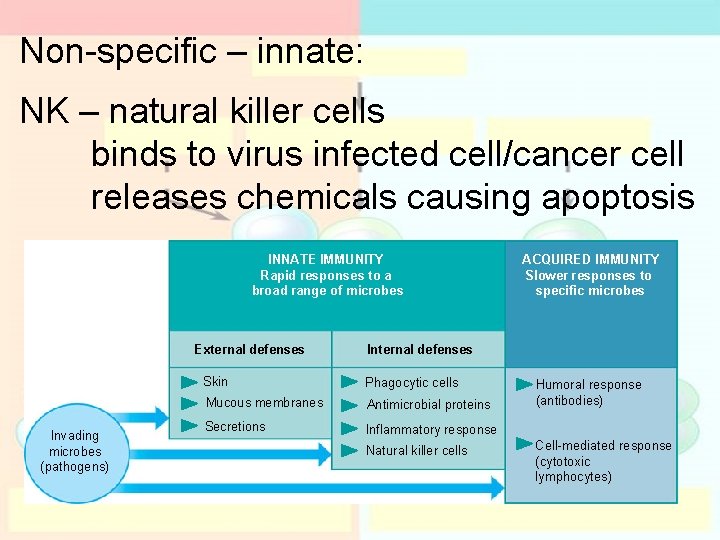
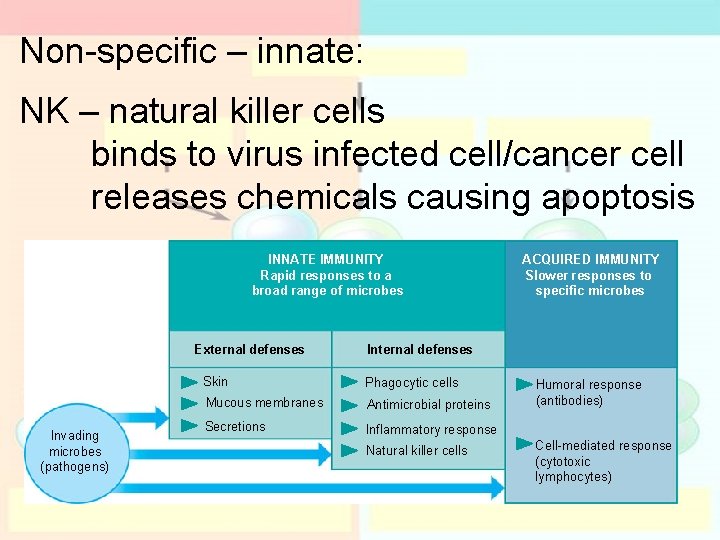
Non-specific – innate: NK – natural killer cells binds to virus infected cell/cancer cell releases chemicals causing apoptosis INNATE IMMUNITY Rapid responses to a broad range of microbes External defenses Invading microbes (pathogens) ACQUIRED IMMUNITY Slower responses to specific microbes Internal defenses Skin Phagocytic cells Mucous membranes Antimicrobial proteins Secretions Inflammatory response Natural killer cells Humoral response (antibodies) Cell-mediated response (cytotoxic lymphocytes)
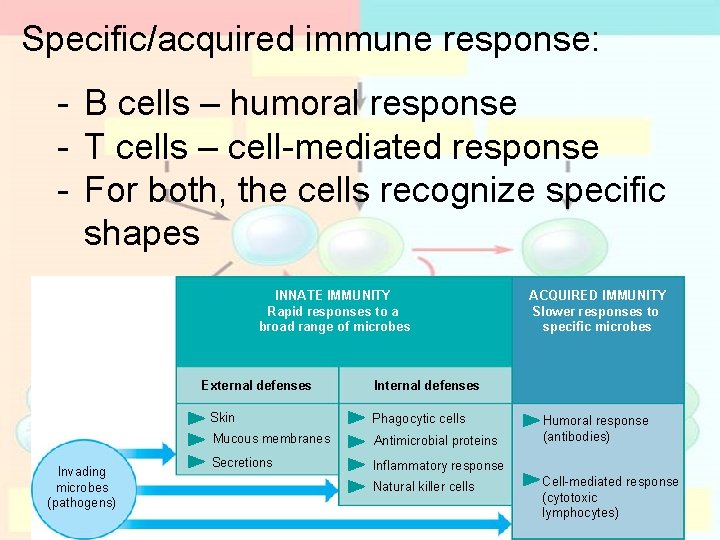
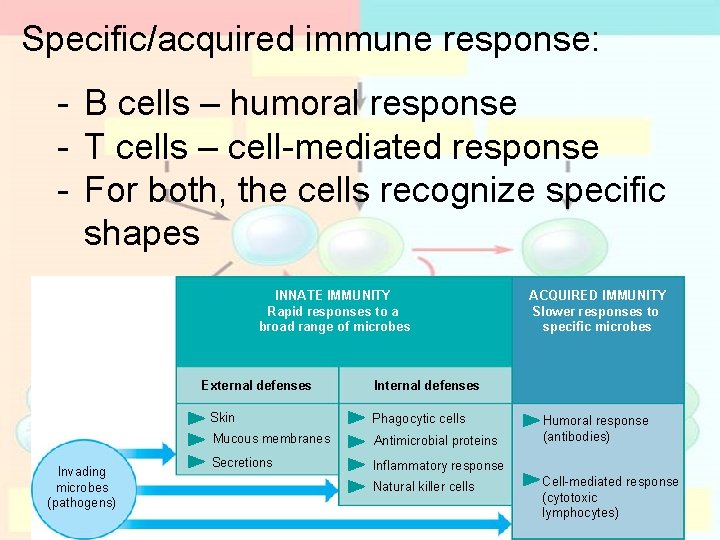
Specific/acquired immune response: - B cells – humoral response - T cells – cell-mediated response - For both, the cells recognize specific shapes INNATE IMMUNITY Rapid responses to a broad range of microbes External defenses Invading microbes (pathogens) ACQUIRED IMMUNITY Slower responses to specific microbes Internal defenses Skin Phagocytic cells Mucous membranes Antimicrobial proteins Secretions Inflammatory response Natural killer cells Humoral response (antibodies) Cell-mediated response (cytotoxic lymphocytes)
How microbes are detected
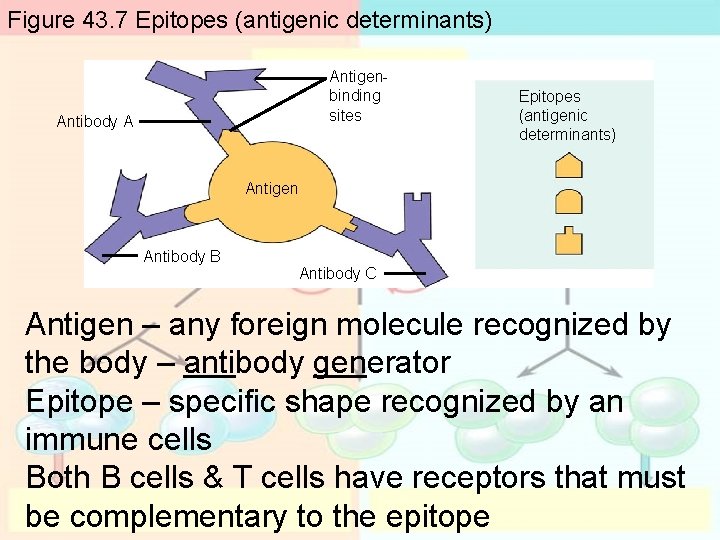
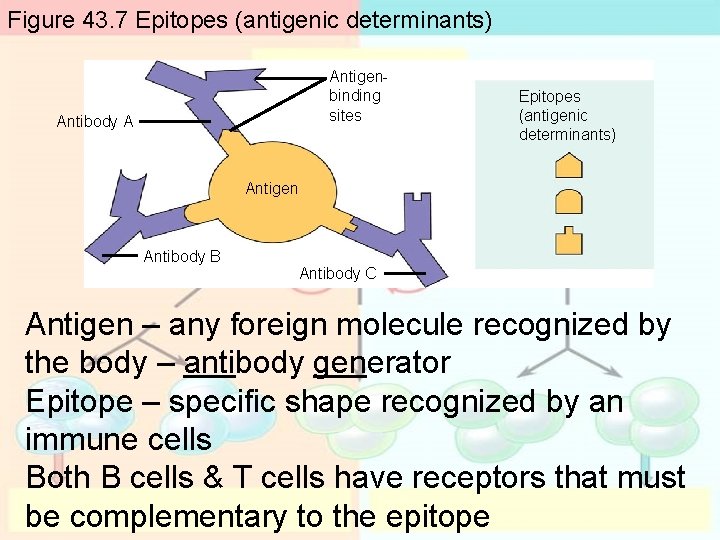
Figure 43. 7 Epitopes (antigenic determinants) Antigenbinding sites Antibody A Epitopes (antigenic determinants) Antigen Antibody B Antibody C Antigen – any foreign molecule recognized by the body – antibody generator Epitope – specific shape recognized by an immune cells Both B cells & T cells have receptors that must be complementary to the epitope
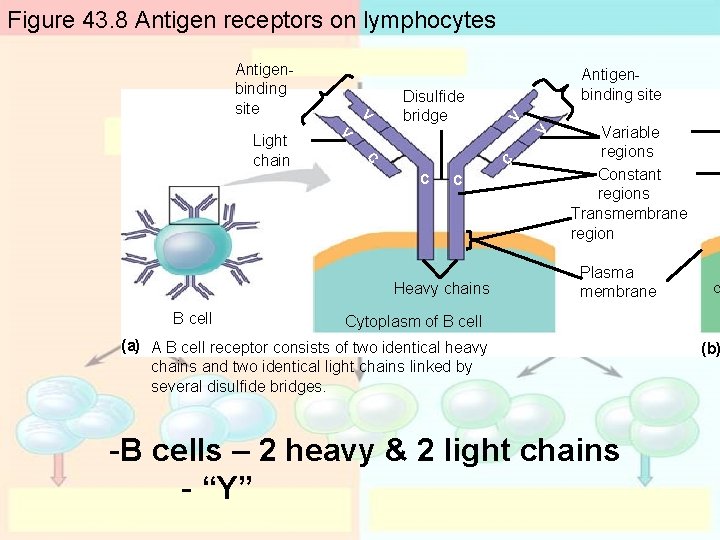
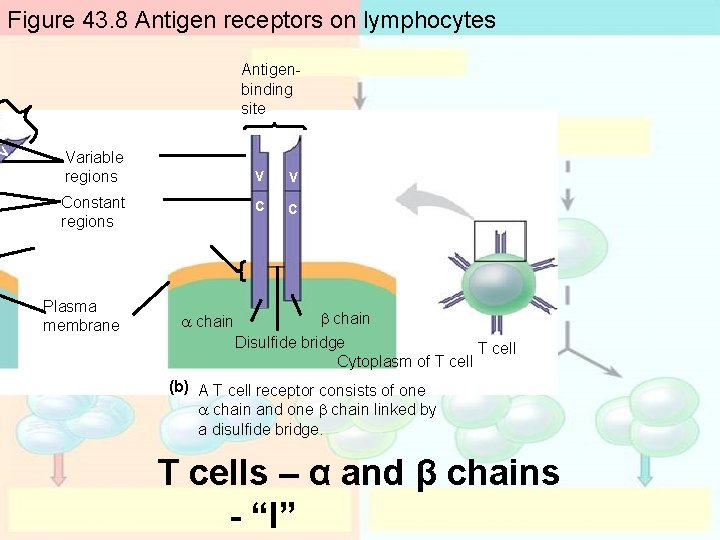
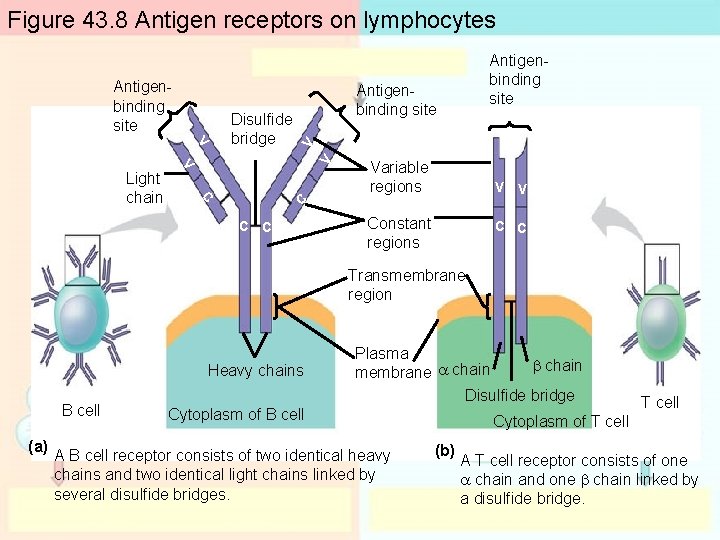
B cell & T cell receptors: Fig. 43. 8 Constant regions embedded in membrane Variable regions that bind to epitopes (vary) Quarternary proteins
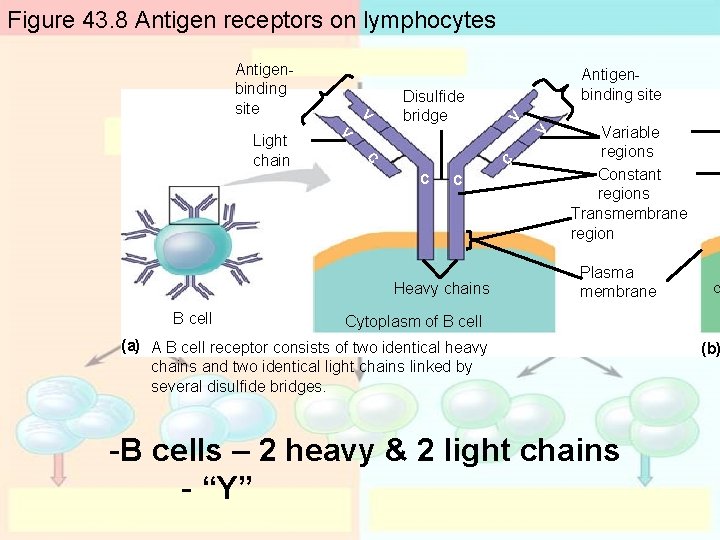
Figure 43. 8 Antigen receptors on lymphocytes V V C C Light chain V Disulfide bridge C C Heavy chains B cell Antigenbinding site Variable regions Constant regions Transmembrane region Plasma membrane a Cytoplasm of B cell (a) A B cell receptor consists of two identical heavy chains and two identical light chains linked by several disulfide bridges. -B cells – 2 heavy & 2 light chains - “Y” (b)
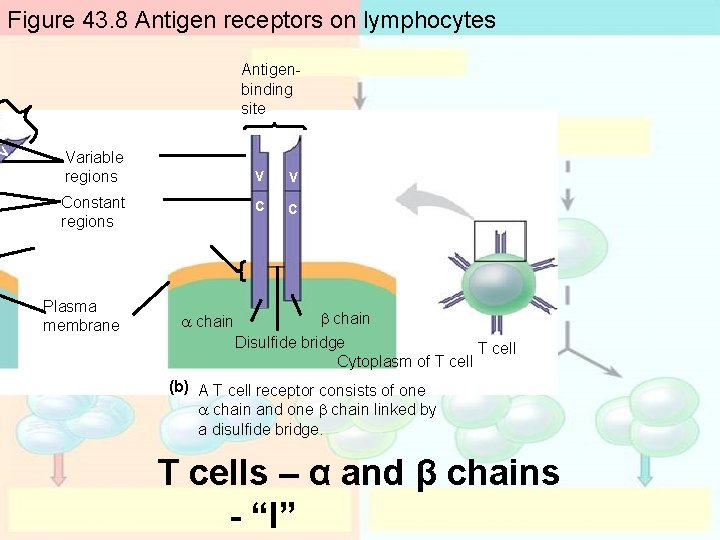
V Figure 43. 8 Antigen receptors on lymphocytes Antigenbinding site Variable regions Constant regions Plasma membrane a chain V V C C b chain Disulfide bridge T cell Cytoplasm of T cell (b) A T cell receptor consists of one a chain and one b chain linked by a disulfide bridge. T cells – α and β chains - “I”
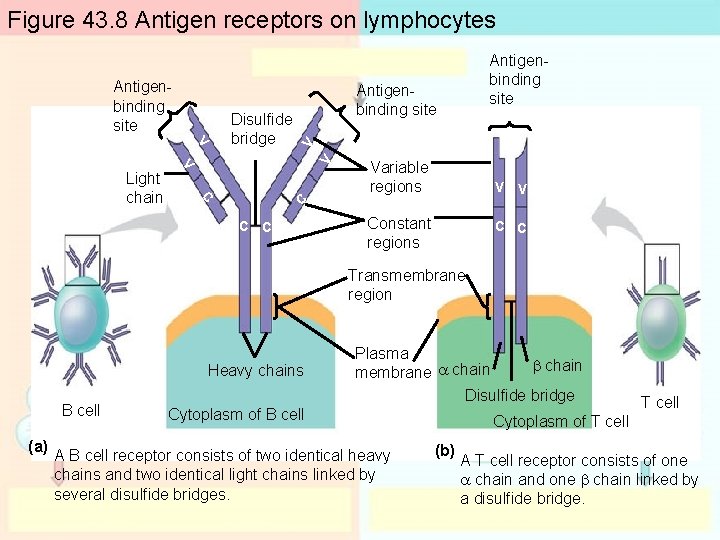
Figure 43. 8 Antigen receptors on lymphocytes V V V C C Light chain Disulfide bridge Antigenbinding site V Antigenbinding site C C Variable regions V V Constant regions C C Transmembrane region Heavy chains B cell (a) Plasma b chain membrane a chain Disulfide bridge Cytoplasm of B cell A B cell receptor consists of two identical heavy chains and two identical light chains linked by several disulfide bridges. T cell Cytoplasm of T cell (b) A T cell receptor consists of one a chain and one b chain linked by a disulfide bridge.
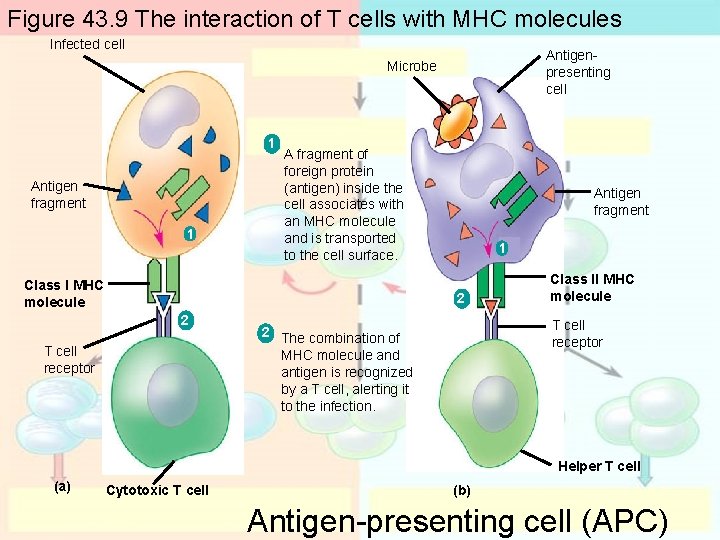
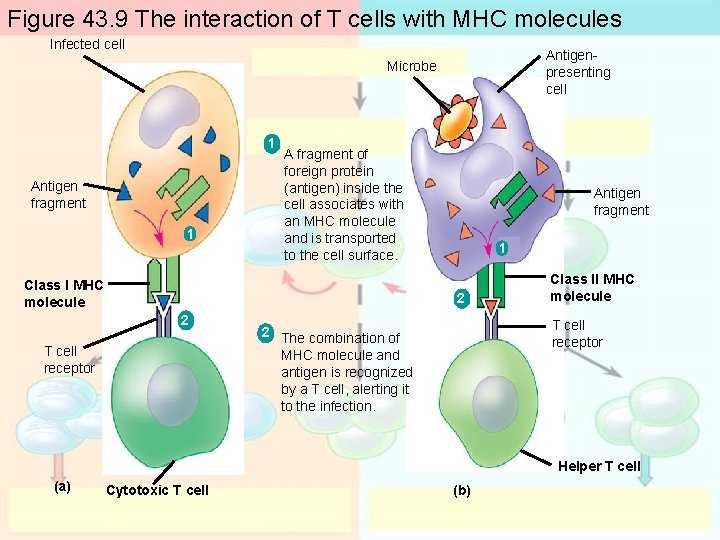
T cell receptors recognize antigens: Figure 43. 9
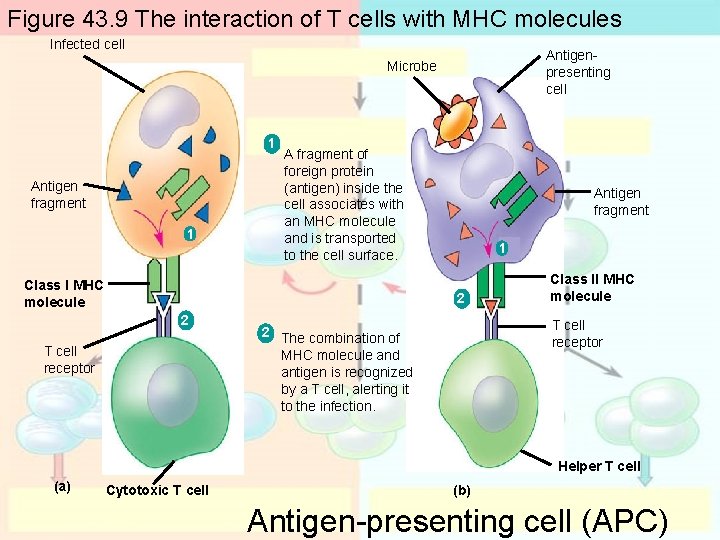
Figure 43. 9 The interaction of T cells with MHC molecules Infected cell Antigenpresenting cell Microbe 1 Antigen fragment 1 A fragment of foreign protein (antigen) inside the cell associates with an MHC molecule and is transported to the cell surface. Class I MHC molecule Antigen fragment 1 2 2 T cell receptor Class II MHC molecule T cell receptor 2 The combination of MHC molecule and antigen is recognized by a T cell, alerting it to the infection. Helper T cell (a) Cytotoxic T cell (b) Antigen-presenting cell (APC)
T cell receptors recognize antigens: Figure 43. 9 Class I MHC molecule of an infected cell fills with an antigen fragment TC recognizes filled MHC forms complementary receptor Class II MHC of a phagocytic cell Helper T binds
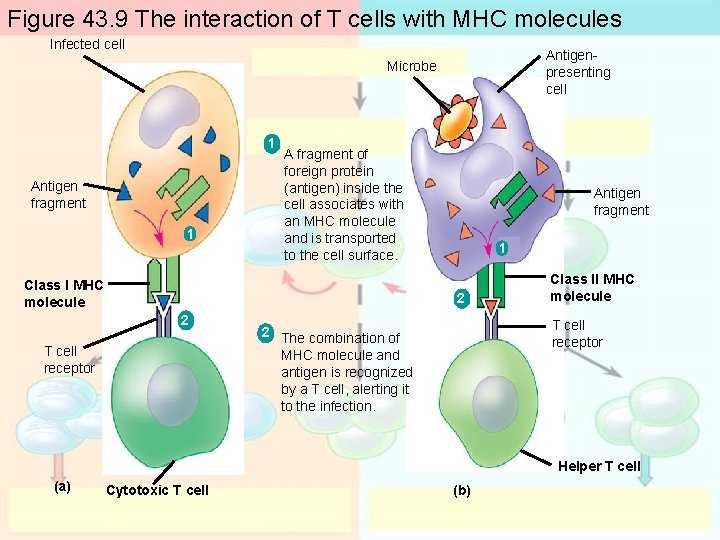
Figure 43. 9 The interaction of T cells with MHC molecules Infected cell Antigenpresenting cell Microbe 1 Antigen fragment 1 A fragment of foreign protein (antigen) inside the cell associates with an MHC molecule and is transported to the cell surface. Class I MHC molecule Antigen fragment 1 2 2 T cell receptor Class II MHC molecule T cell receptor 2 The combination of MHC molecule and antigen is recognized by a T cell, alerting it to the infection. Helper T cell (a) Cytotoxic T cell (b)
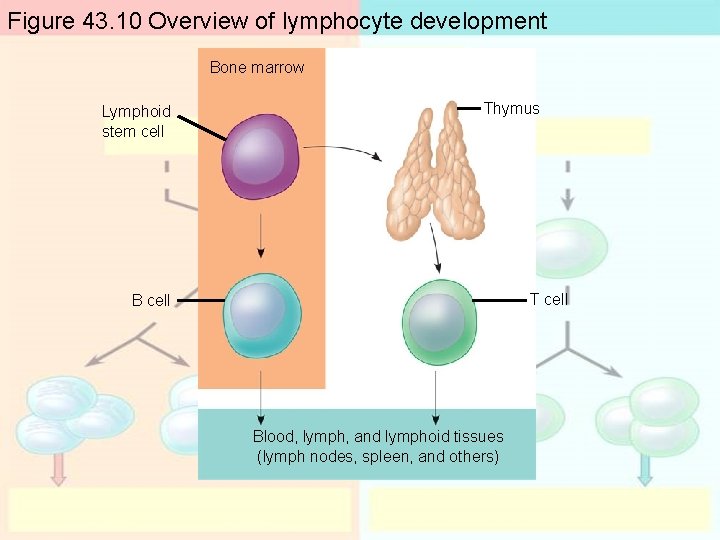
Naming B & T cells: - Where they mature - B cells – bone - T cells – thymus
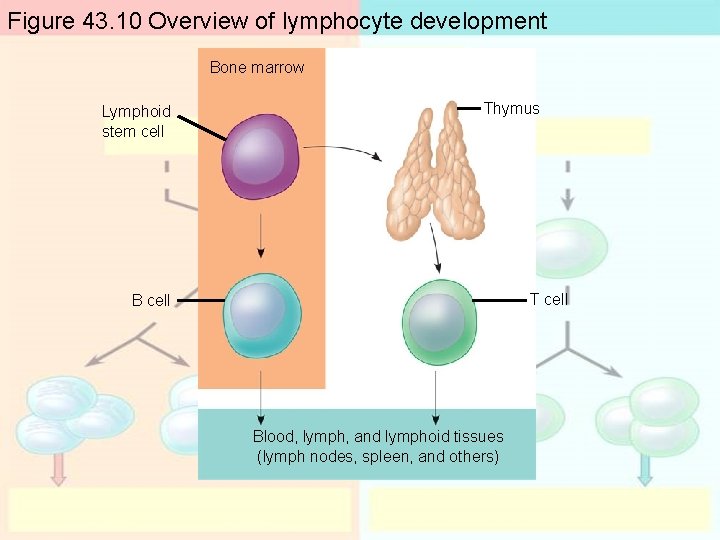
Figure 43. 10 Overview of lymphocyte development Bone marrow Lymphoid stem cell Thymus T cell Blood, lymph, and lymphoid tissues (lymph nodes, spleen, and others)
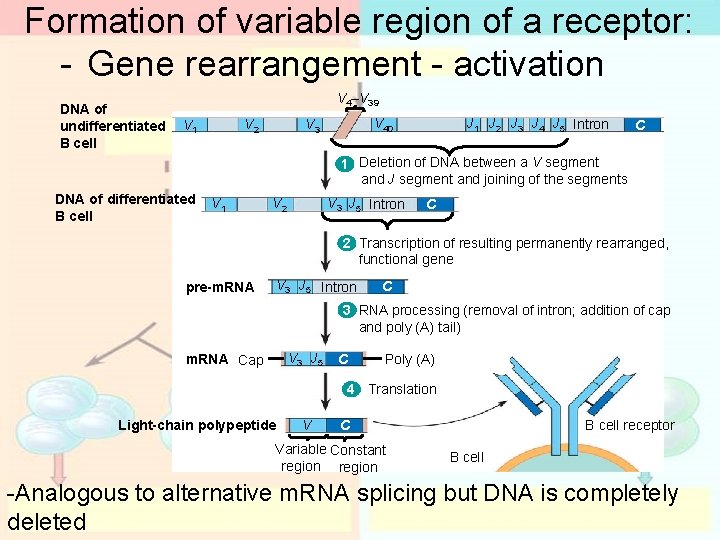
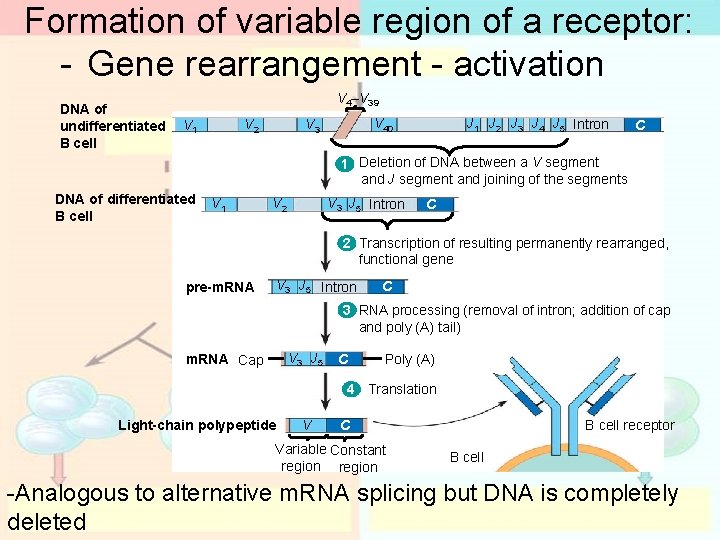
Formation of variable region of a receptor: - Gene rearrangement - activation DNA of undifferentiated B cell V 4–V 39 V 2 V 1 V 40 V 3 J 1 J 2 J 3 J 4 J 5 Intron C 1 Deletion of DNA between a V segment and J segment and joining of the segments DNA of differentiated B cell V 1 V 3 J 5 Intron V 2 C 2 Transcription of resulting permanently rearranged, functional gene pre-m. RNA V 3 J 5 Intron C 3 RNA processing (removal of intron; addition of cap and poly (A) tail) V 3 J 5 m. RNA Cap C Poly (A) 4 Translation Light-chain polypeptide V C Variable Constant region B cell receptor B cell -Analogous to alternative m. RNA splicing but DNA is completely deleted
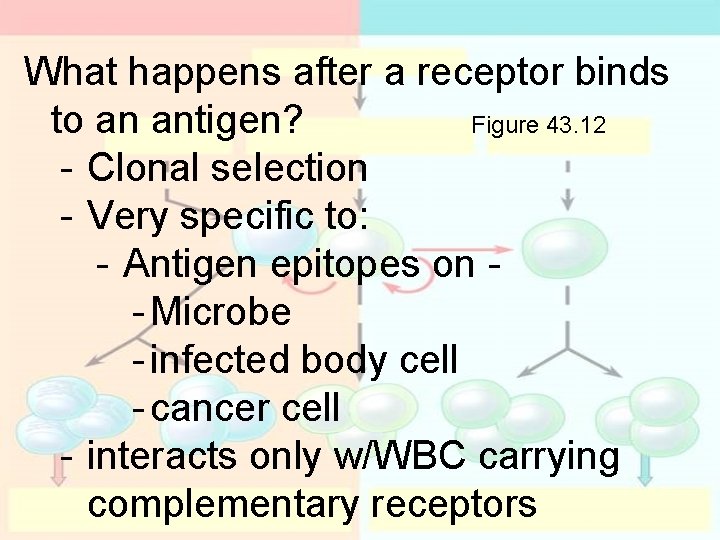
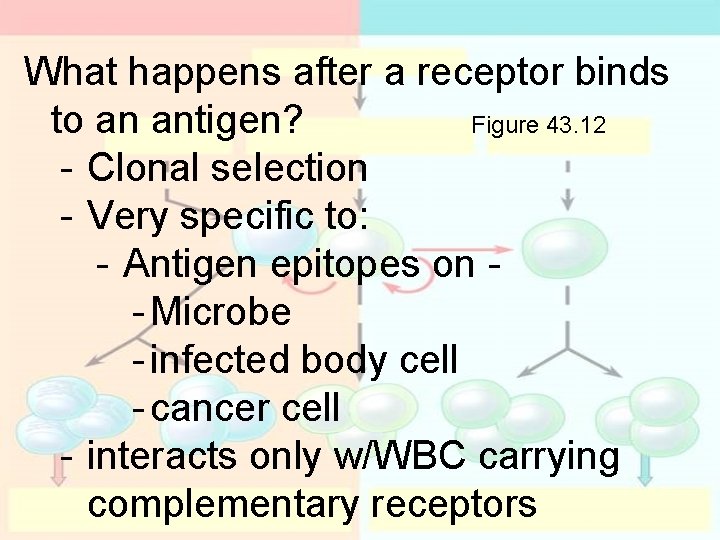
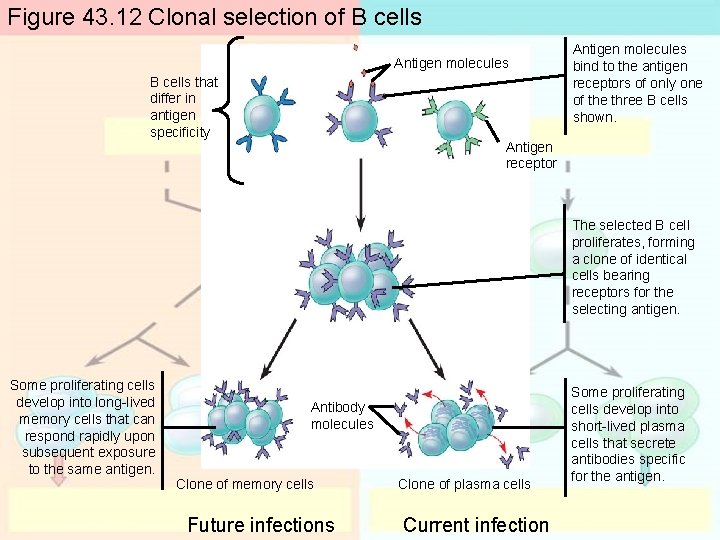
What happens after a receptor binds to an antigen? Figure 43. 12 - Clonal selection - Very specific to: - Antigen epitopes on - Microbe - infected body cell - cancer cell - interacts only w/WBC carrying complementary receptors
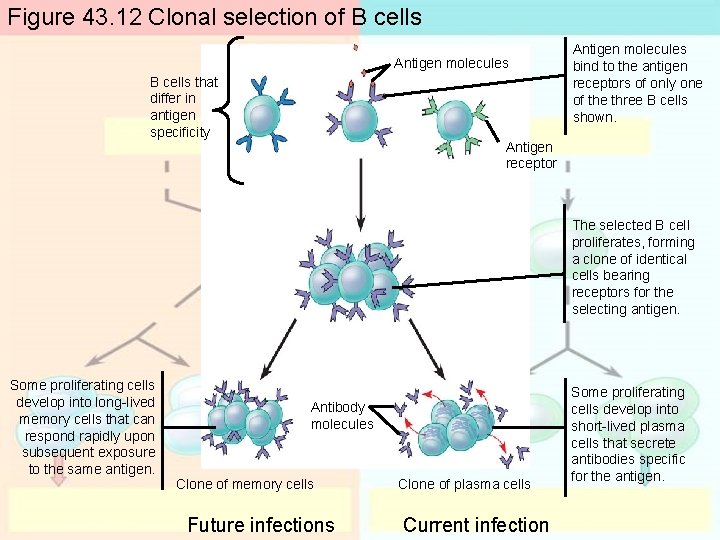
Figure 43. 12 Clonal selection of B cells Antigen molecules B cells that differ in antigen specificity Antigen molecules bind to the antigen receptors of only one of the three B cells shown. Antigen receptor The selected B cell proliferates, forming a clone of identical cells bearing receptors for the selecting antigen. Some proliferating cells develop into long-lived memory cells that can respond rapidly upon subsequent exposure to the same antigen. Antibody molecules Clone of memory cells Future infections Clone of plasma cells Current infection Some proliferating cells develop into short-lived plasma cells that secrete antibodies specific for the antigen.
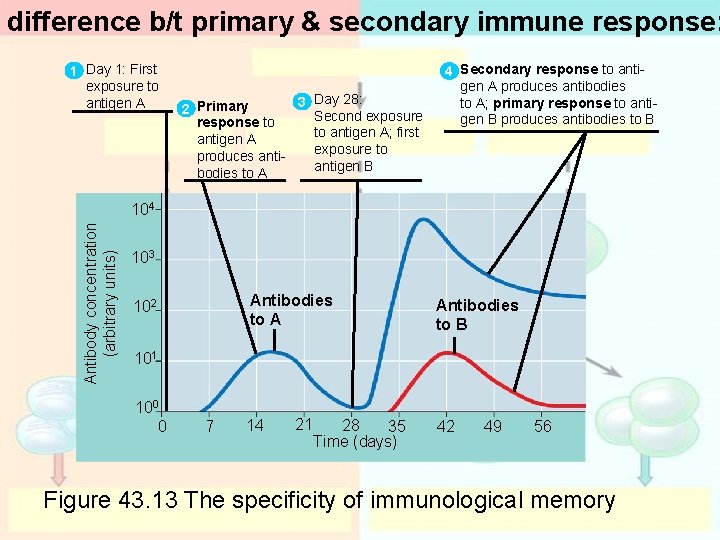
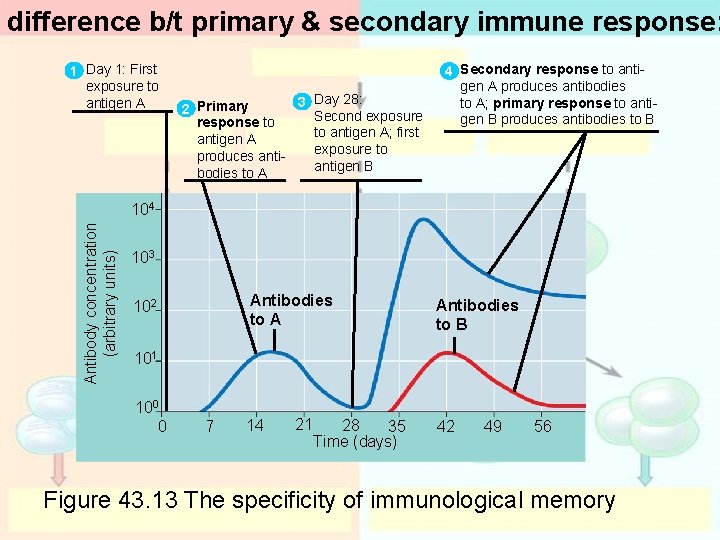
difference b/t primary & secondary immune response: 1 Day 1: First exposure to antigen A 3 Day 28: 2 Primary Second exposure response to to antigen A; first antigen A exposure to produces antigen B bodies to A 4 Secondary response to antigen A produces antibodies to A; primary response to antigen B produces antibodies to B Antibody concentration (arbitrary units) 104 103 Antibodies to A 102 Antibodies to B 101 100 0 7 14 21 28 35 Time (days) 42 49 56 Figure 43. 13 The specificity of immunological memory
The Immune Response….
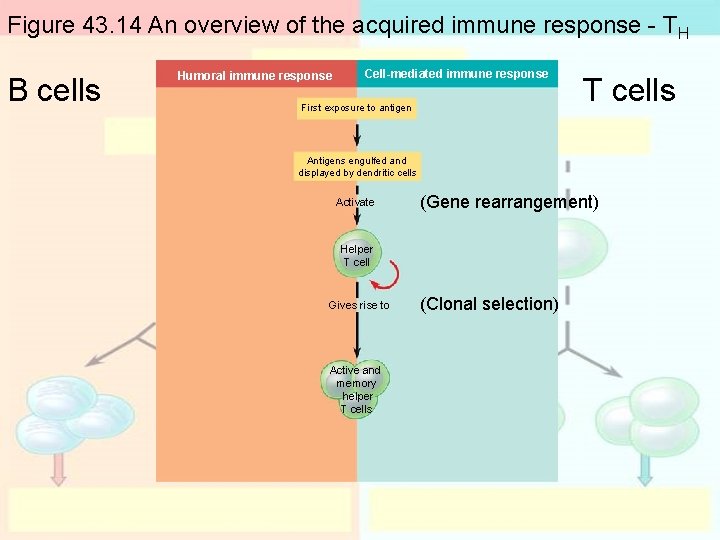
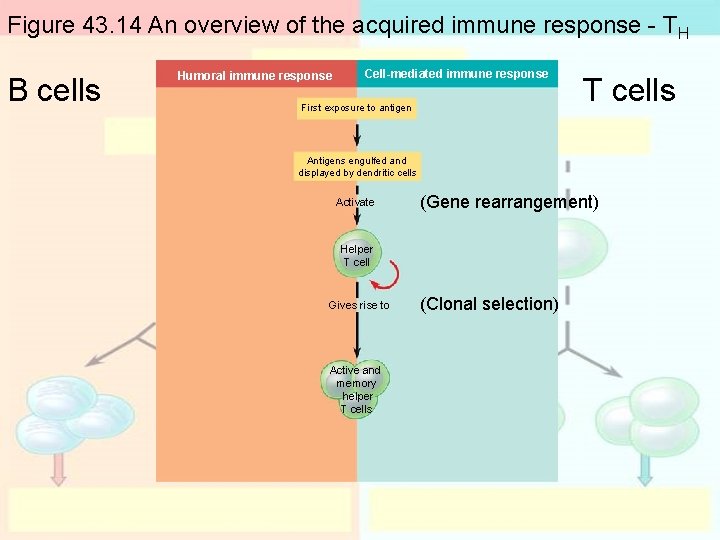
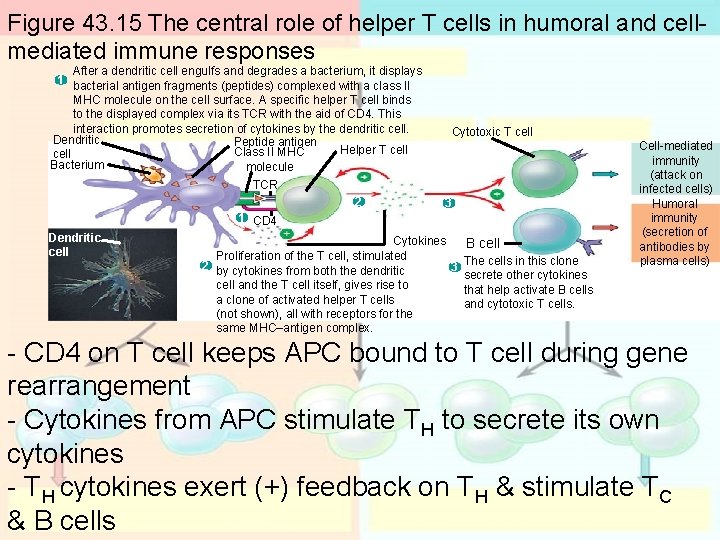
Figure 43. 14 An overview of the acquired immune response - TH B cells Humoral immune response Cell-mediated immune response First exposure to antigen T cells Antigens engulfed and displayed by dendritic cells Activate (Gene rearrangement) Helper T cell Gives rise to Active and memory helper T cells (Clonal selection)
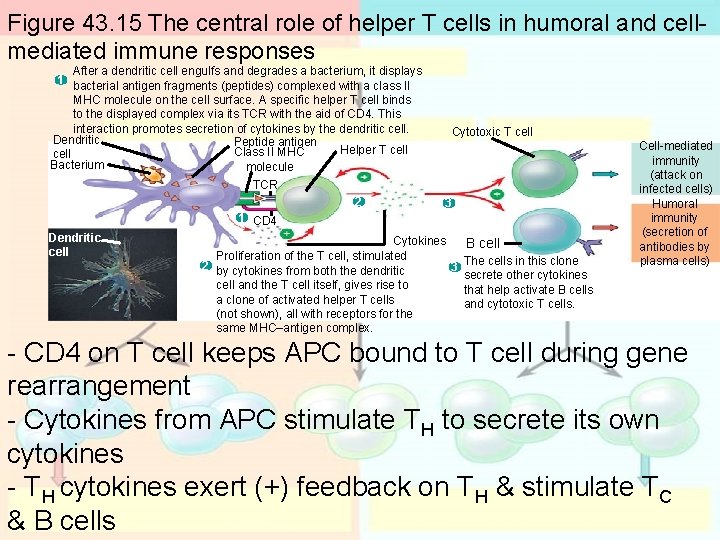
Figure 43. 15 The central role of helper T cells in humoral and cellmediated immune responses After a dendritic cell engulfs and degrades a bacterium, it displays 1 bacterial antigen fragments (peptides) complexed with a class II MHC molecule on the cell surface. A specific helper T cell binds to the displayed complex via its TCR with the aid of CD 4. This interaction promotes secretion of cytokines by the dendritic cell. Dendritic Peptide antigen Helper T cell Class II MHC cell Bacterium molecule Cytotoxic T cell TCR 2 3 1 CD 4 Dendritic cell Cytokines B cell Proliferation of the T cell, stimulated The cells in this clone 2 by cytokines from both the dendritic 3 secrete other cytokines cell and the T cell itself, gives rise to that help activate B cells a clone of activated helper T cells and cytotoxic T cells. (not shown), all with receptors for the same MHC–antigen complex. Cell-mediated immunity (attack on infected cells) Humoral immunity (secretion of antibodies by plasma cells) - CD 4 on T cell keeps APC bound to T cell during gene rearrangement - Cytokines from APC stimulate TH to secrete its own cytokines - TH cytokines exert (+) feedback on TH & stimulate TC & B cells
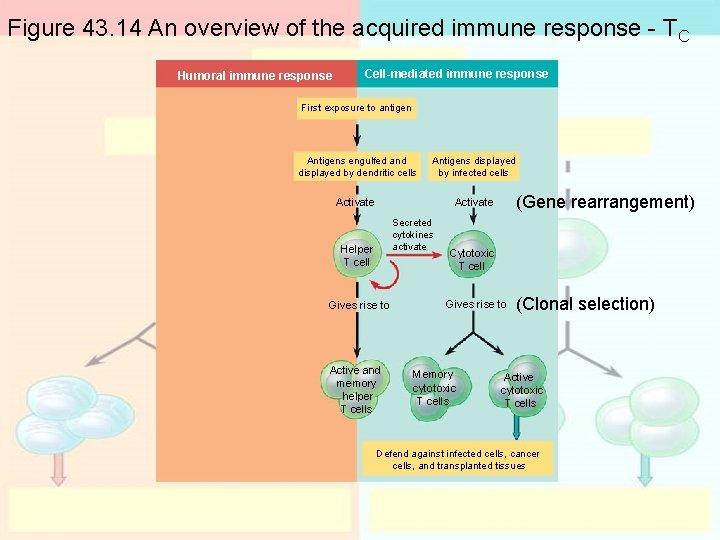
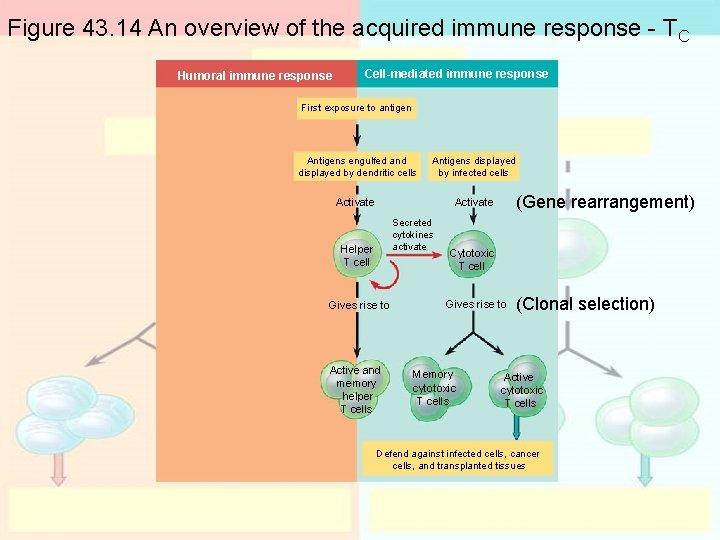
Figure 43. 14 An overview of the acquired immune response - TC Humoral immune response Cell-mediated immune response First exposure to antigen Antigens engulfed and displayed by dendritic cells Antigens displayed by infected cells Activate Secreted cytokines activate Helper T cell Gives rise to Active and memory helper T cells (Gene rearrangement) Cytotoxic T cell Gives rise to Memory cytotoxic T cells (Clonal selection) Active cytotoxic T cells Defend against infected cells, cancer cells, and transplanted tissues
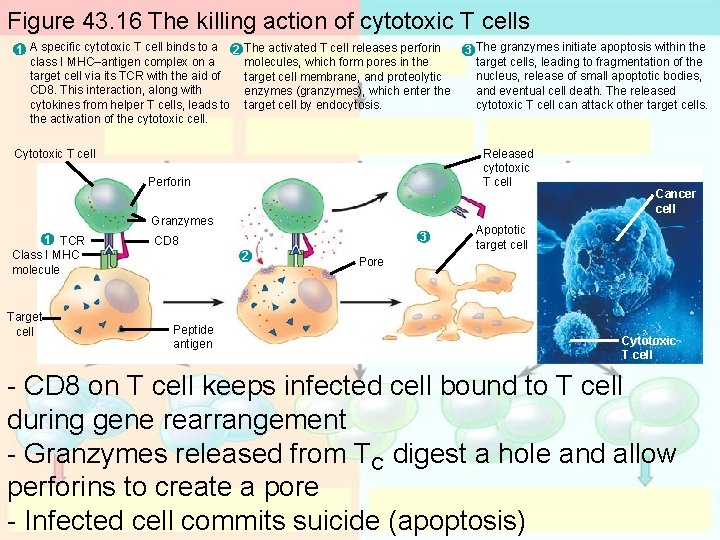
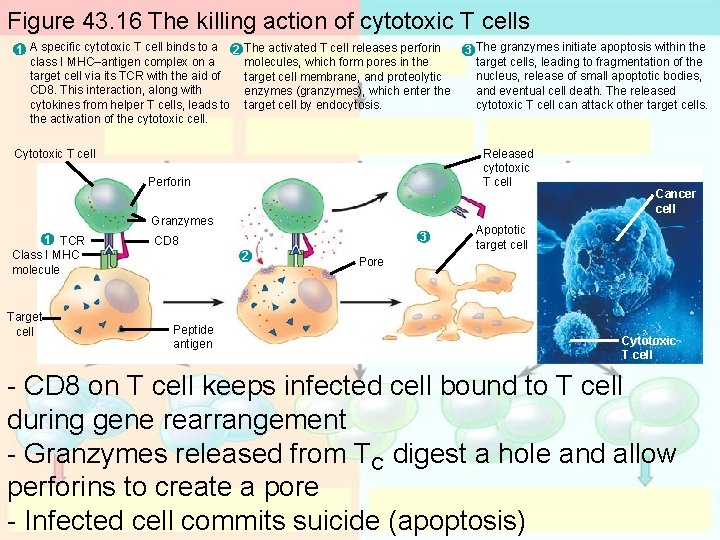
Figure 43. 16 The killing action of cytotoxic T cells 1 A specific cytotoxic T cell binds to a 2 class I MHC–antigen complex on a target cell via its TCR with the aid of CD 8. This interaction, along with cytokines from helper T cells, leads to the activation of the cytotoxic cell. The activated T cell releases perforin molecules, which form pores in the target cell membrane, and proteolytic enzymes (granzymes), which enter the target cell by endocytosis. Released cytotoxic T cell Cytotoxic T cell Perforin Granzymes 1 TCR Class I MHC molecule Target cell 3 CD 8 2 Peptide antigen 3 The granzymes initiate apoptosis within the target cells, leading to fragmentation of the nucleus, release of small apoptotic bodies, and eventual cell death. The released cytotoxic T cell can attack other target cells. Cancer cell Apoptotic target cell Pore Cytotoxic T cell - CD 8 on T cell keeps infected cell bound to T cell during gene rearrangement - Granzymes released from TC digest a hole and allow perforins to create a pore - Infected cell commits suicide (apoptosis)
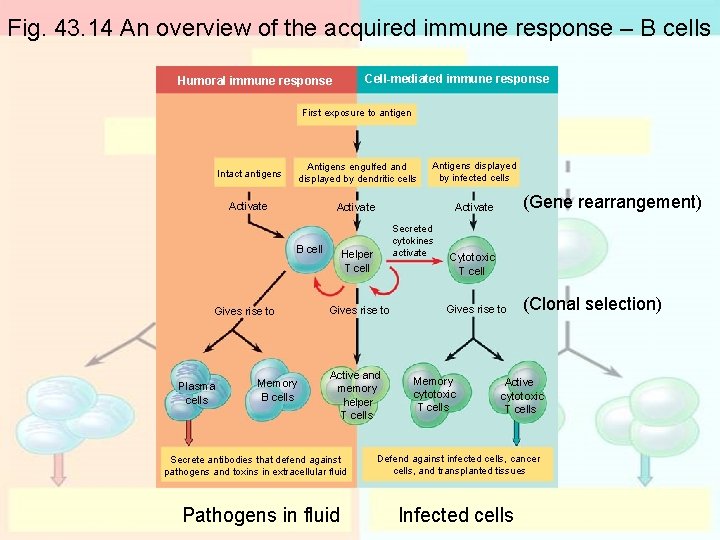
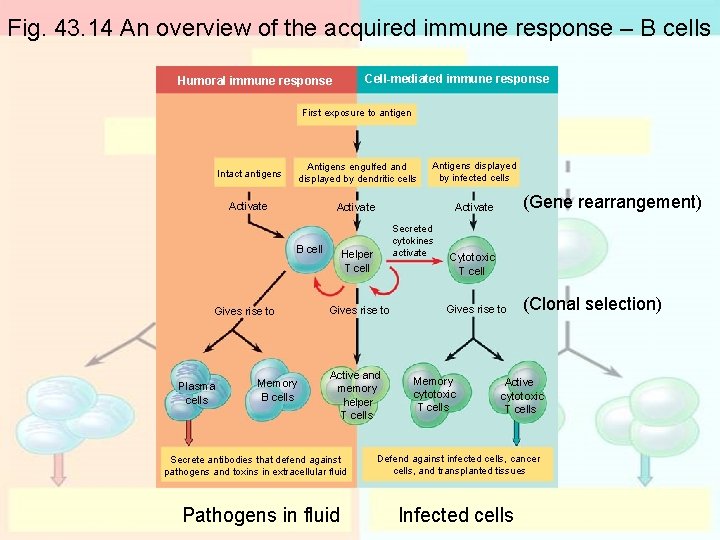
Fig. 43. 14 An overview of the acquired immune response – B cells Cell-mediated immune response Humoral immune response First exposure to antigen Intact antigens Antigens engulfed and displayed by dendritic cells Antigens displayed by infected cells Activate B cell Gives rise to Plasma cells Memory B cells Secreted cytokines activate Helper T cell Gives rise to Active and memory helper T cells Secrete antibodies that defend against pathogens and toxins in extracellular fluid Pathogens in fluid (Gene rearrangement) Cytotoxic T cell Gives rise to Memory cytotoxic T cells (Clonal selection) Active cytotoxic T cells Defend against infected cells, cancer cells, and transplanted tissues Infected cells
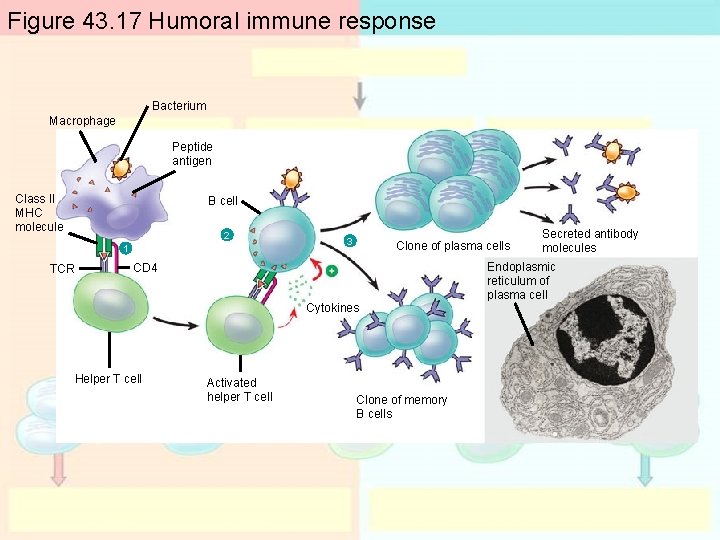
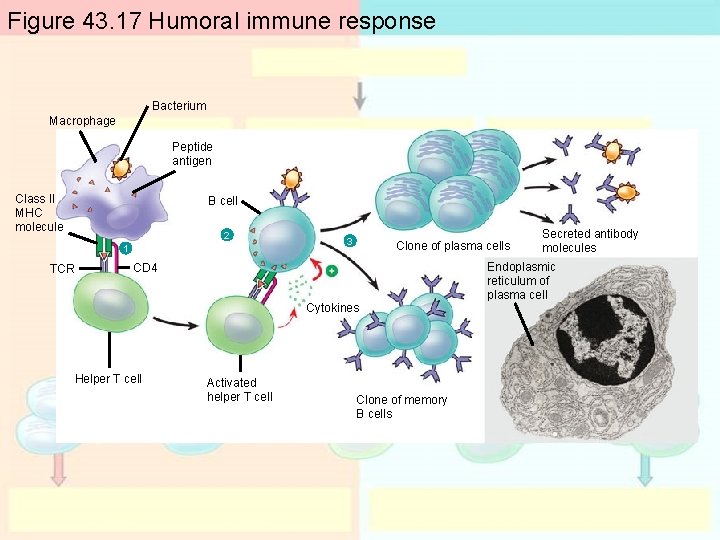
Figure 43. 17 Humoral immune response Bacterium Macrophage Peptide antigen Class II MHC molecule B cell 2 1 TCR 3 Clone of plasma cells CD 4 Cytokines Helper T cell Activated helper T cell Clone of memory B cells Secreted antibody molecules Endoplasmic reticulum of plasma cell
5 classes of antibodies: - GAMED - immunoglobulins
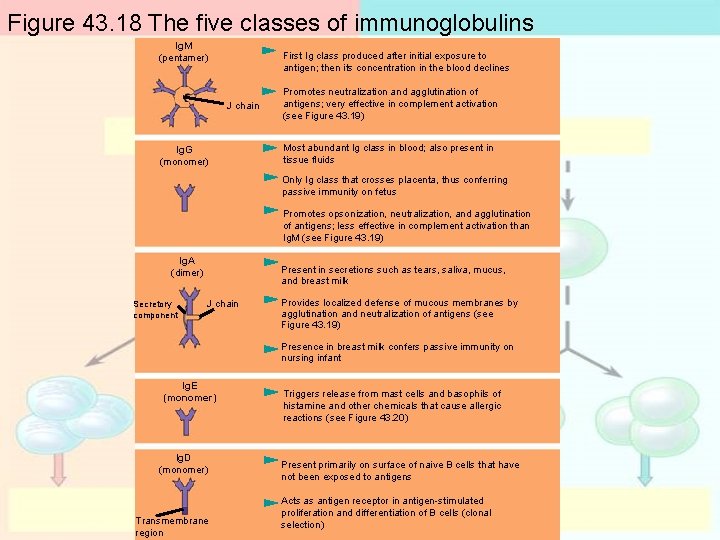
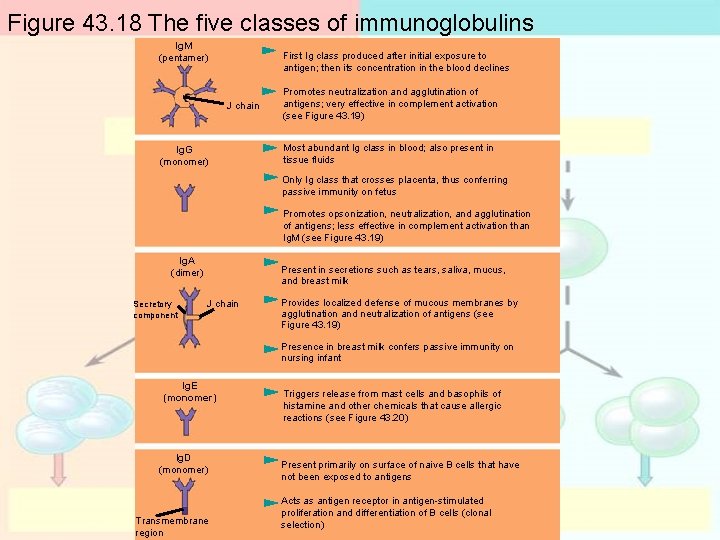
Figure 43. 18 The five classes of immunoglobulins Ig. M (pentamer) First Ig class produced after initial exposure to antigen; then its concentration in the blood declines J chain Ig. G (monomer) Promotes neutralization and agglutination of antigens; very effective in complement activation (see Figure 43. 19) Most abundant Ig class in blood; also present in tissue fluids Only Ig class that crosses placenta, thus conferring passive immunity on fetus Promotes opsonization, neutralization, and agglutination of antigens; less effective in complement activation than Ig. M (see Figure 43. 19) Ig. A (dimer) Secretory component Present in secretions such as tears, saliva, mucus, and breast milk J chain Provides localized defense of mucous membranes by agglutination and neutralization of antigens (see Figure 43. 19) Presence in breast milk confers passive immunity on nursing infant Ig. E (monomer) Ig. D (monomer) Transmembrane region Triggers release from mast cells and basophils of histamine and other chemicals that cause allergic reactions (see Figure 43. 20) Present primarily on surface of naive B cells that have not been exposed to antigens Acts as antigen receptor in antigen-stimulated proliferation and differentiation of B cells (clonal selection)
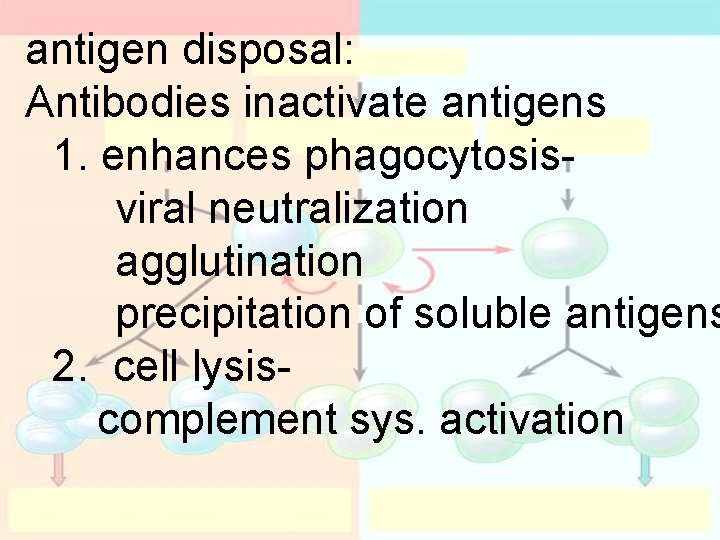
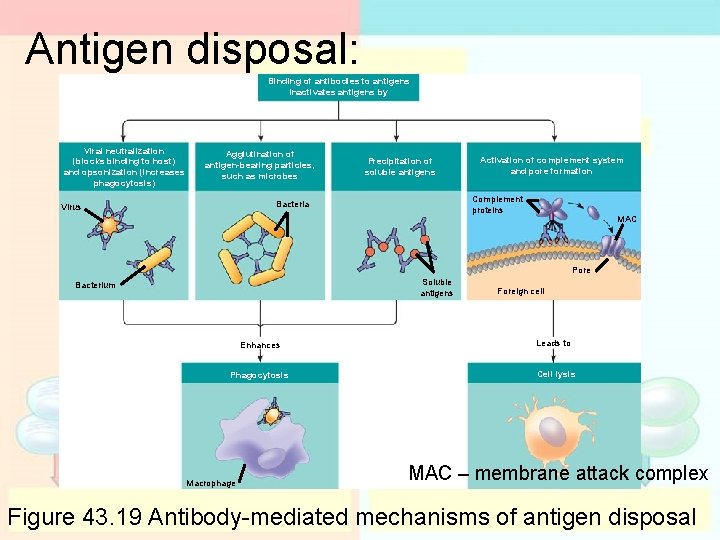
antigen disposal: Antibodies inactivate antigens 1. enhances phagocytosisviral neutralization agglutination precipitation of soluble antigens 2. cell lysiscomplement sys. activation
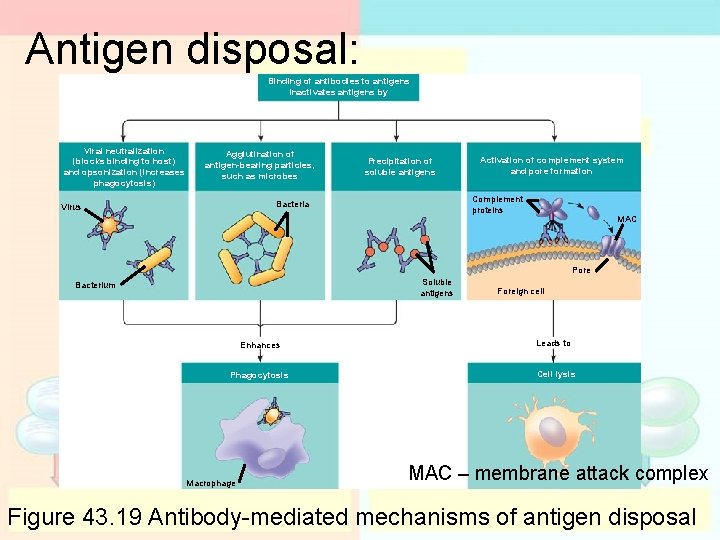
Antigen disposal: Binding of antibodies to antigens inactivates antigens by Viral neutralization (blocks binding to host) and opsonization (increases phagocytosis) Agglutination of antigen-bearing particles, such as microbes Precipitation of soluble antigens Complement proteins Bacteria Virus Activation of complement system and pore formation MAC Pore Soluble antigens Bacterium Enhances Phagocytosis Macrophage Foreign cell Leads to Cell lysis MAC – membrane attack complex Figure 43. 19 Antibody-mediated mechanisms of antigen disposal
passive vs. active immunity: Passive – - transfer of antibodies breastfeeding, injection (rabies) Active – - body creates its own antibodies during an infection – vaccine
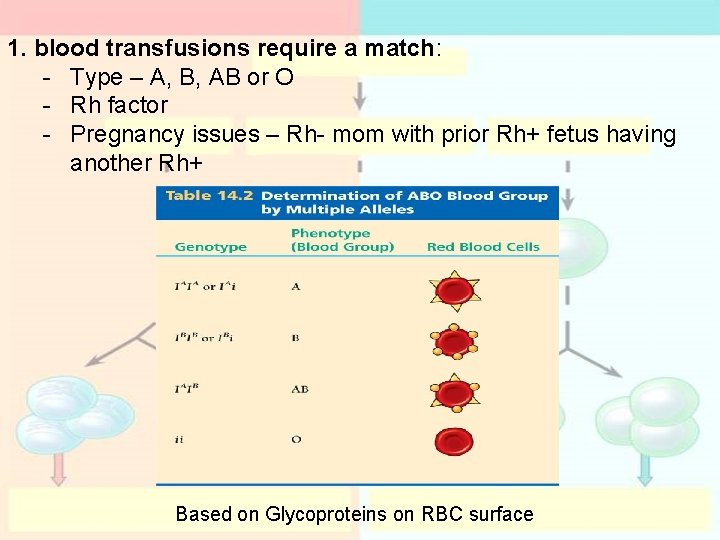
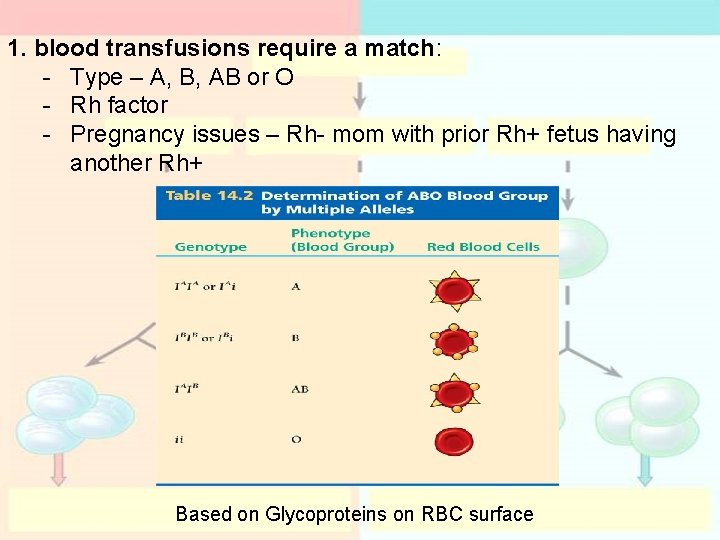
1. blood transfusions require a match: - Type – A, B, AB or O - Rh factor - Pregnancy issues – Rh- mom with prior Rh+ fetus having another Rh+ Based on Glycoproteins on RBC surface
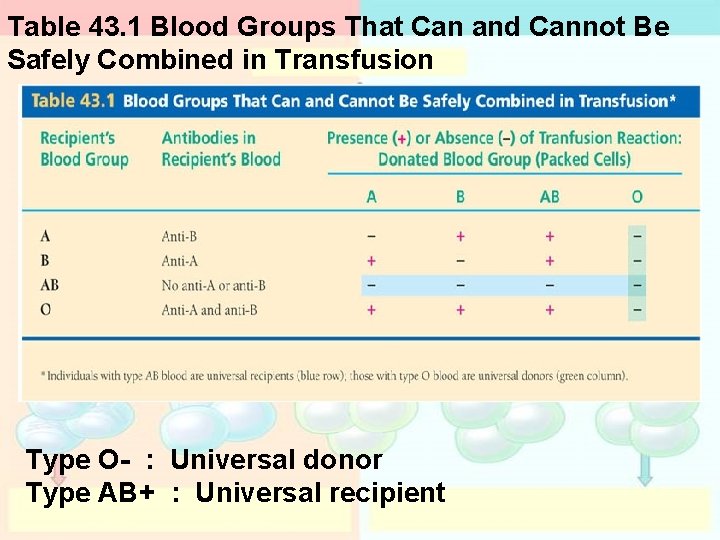
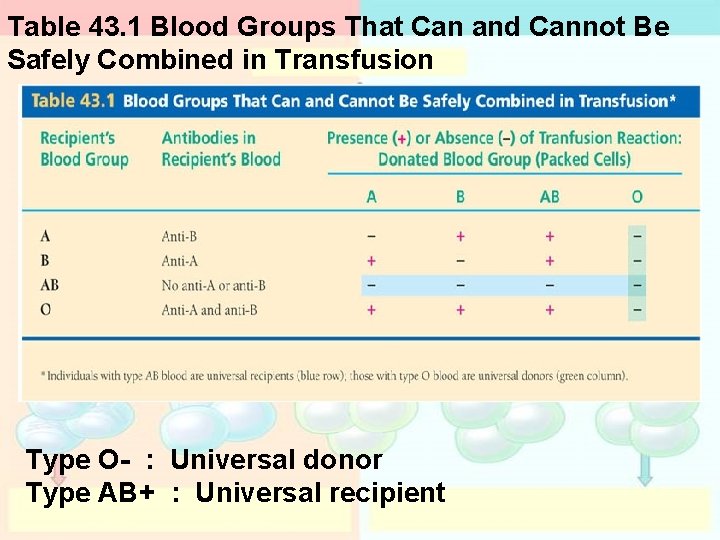
Table 43. 1 Blood Groups That Can and Cannot Be Safely Combined in Transfusion Type O- : Universal donor Type AB+ : Universal recipient
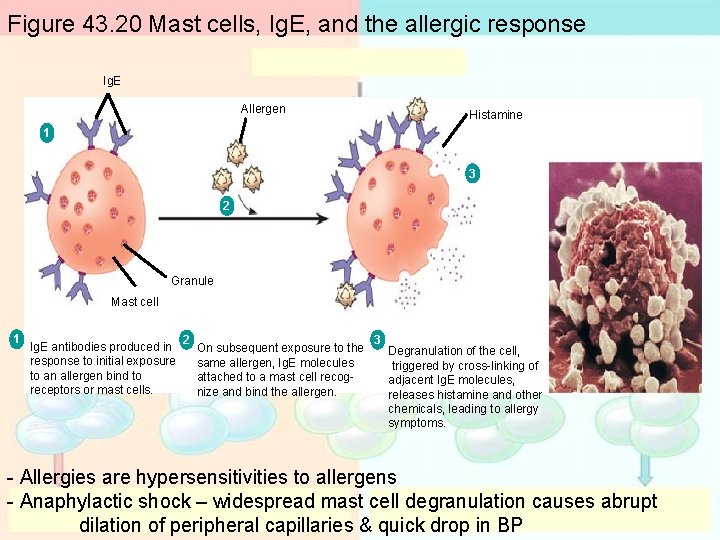
allergic response Allergies are hypersensitivities to allergens Anaphylactic shock – widespread mast cell degranulation causes abrupt dilation of peripheral capillaries & quick drop in BP
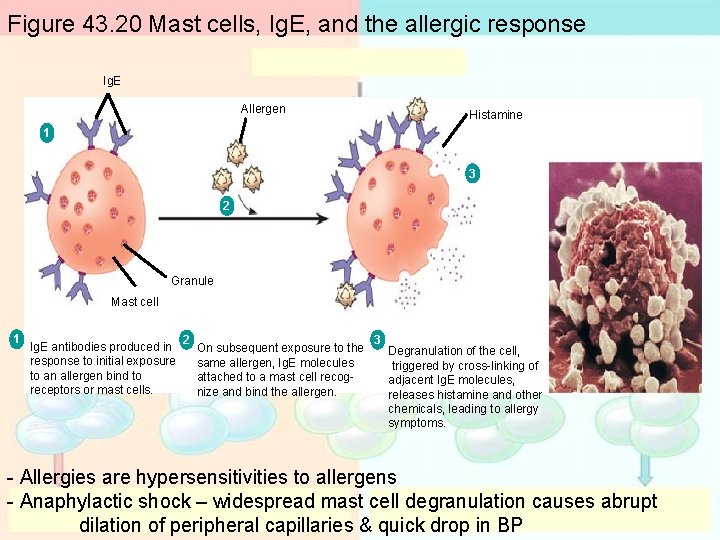
Figure 43. 20 Mast cells, Ig. E, and the allergic response Ig. E Allergen Histamine 1 3 2 Granule Mast cell 1 Ig. E antibodies produced in response to initial exposure to an allergen bind to receptors or mast cells. 2 On subsequent exposure to the same allergen, Ig. E molecules attached to a mast cell recognize and bind the allergen. 3 Degranulation of the cell, triggered by cross-linking of adjacent Ig. E molecules, releases histamine and other chemicals, leading to allergy symptoms. - Allergies are hypersensitivities to allergens - Anaphylactic shock – widespread mast cell degranulation causes abrupt dilation of peripheral capillaries & quick drop in BP
autoimmune diseases: - Lupus - Rheumatoid arthritis - Insulin-dependent diabetes - MS – multiple sclerosis
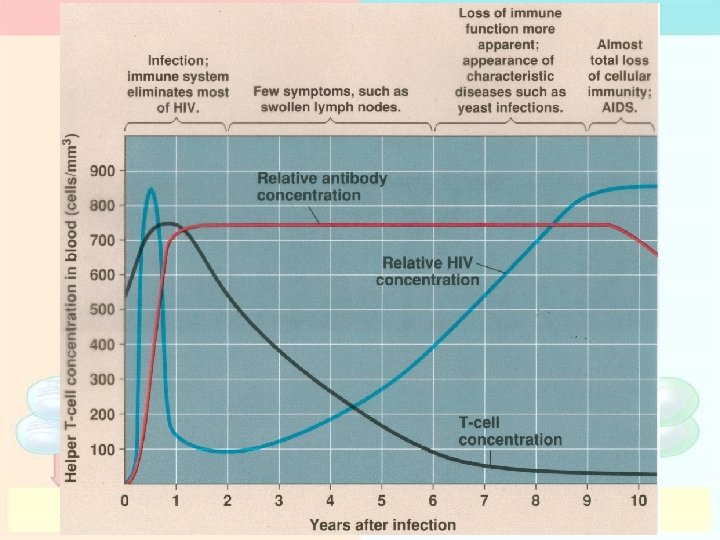
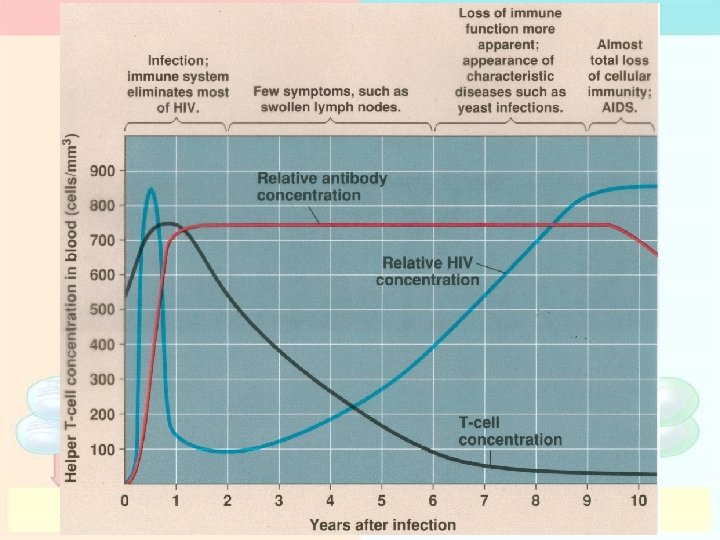
1. AIDS: - Acquired Immune Deficiency Syndrome