Chapter 4 Tissues Copyright 2003 Pearson Education Inc

- Slides: 60
Chapter 4 Tissues Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings
Body Tissues · What are the characteristics of the different types of body tissues? Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide 3. 41
Body Tissues · Cells are specialized for particular functions · Tissues · Groups of cells with similar structure and function · Four primary types · Epithelium · Connective tissue · Nervous tissue · Muscle Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide 3. 41
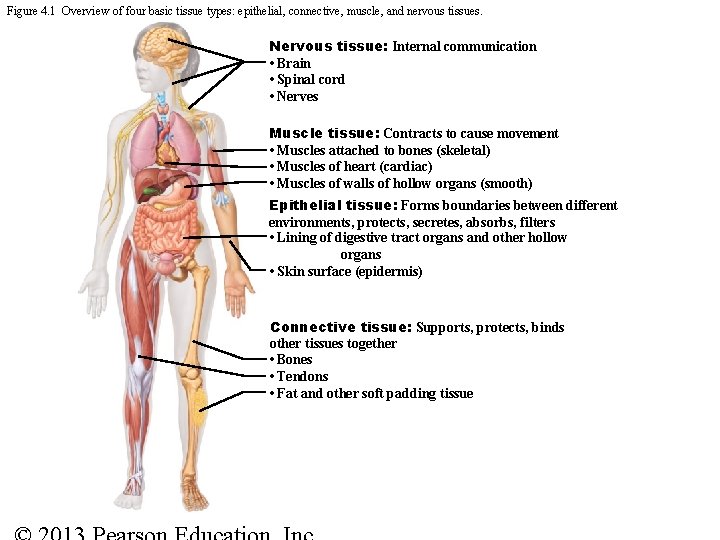
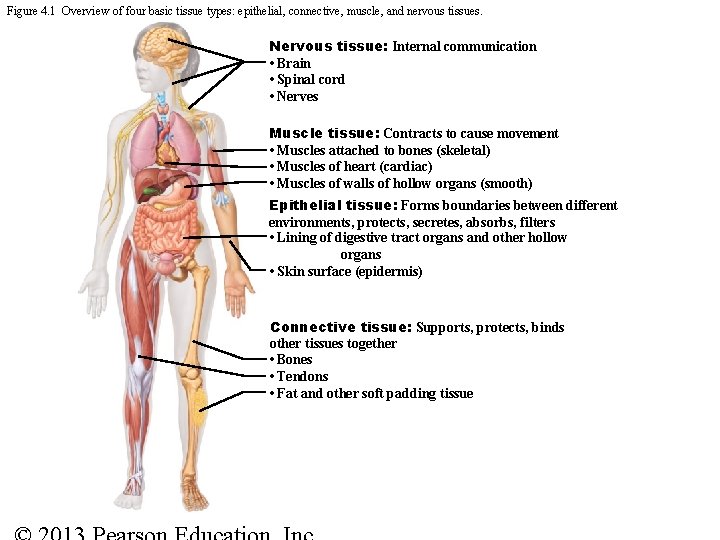
Figure 4. 1 Overview of four basic tissue types: epithelial, connective, muscle, and nervous tissues. Nervous tissue: Internal communication • Brain • Spinal cord • Nerves Muscle tissue: Contracts to cause movement • Muscles attached to bones (skeletal) • Muscles of heart (cardiac) • Muscles of walls of hollow organs (smooth) Epithelial tissue: Forms boundaries between different environments, protects, secretes, absorbs, filters • Lining of digestive tract organs and other hollow organs • Skin surface (epidermis) Connective tissue: Supports, protects, binds other tissues together • Bones • Tendons • Fat and other soft padding tissue
Studying Human Tissue: Microscopy • Tissue is fixed • Preserved • Cut • Sliced thin enough to transmit light or electrons • Stained • Enhances contrast
Epithelial Tissue (Epithelium) • Form boundaries • Two main types (by location) • Covering and lining epithelia • On external and internal surfaces • Glandular epithelia • Secretory tissue in glands
Epithelial Tissues · Found in different areas · Body coverings · Body linings · Glandular tissue · Functions · Protection · Absorption · Filtration · Secretion Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide 3. 42
Epithelium Characteristics · Cells fit closely together · Always has one free surface (apical surface) · Lower surface is bound by a basement membrane (basal surface) · Avascular (no blood supply) but innervated by nerve fibers · Regenerate easily if well nourished · Most have microvilli, some have cilia Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide 3. 43
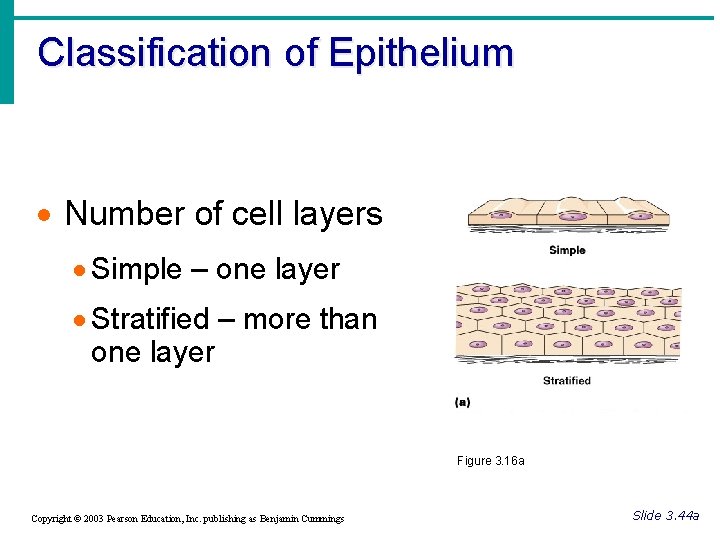
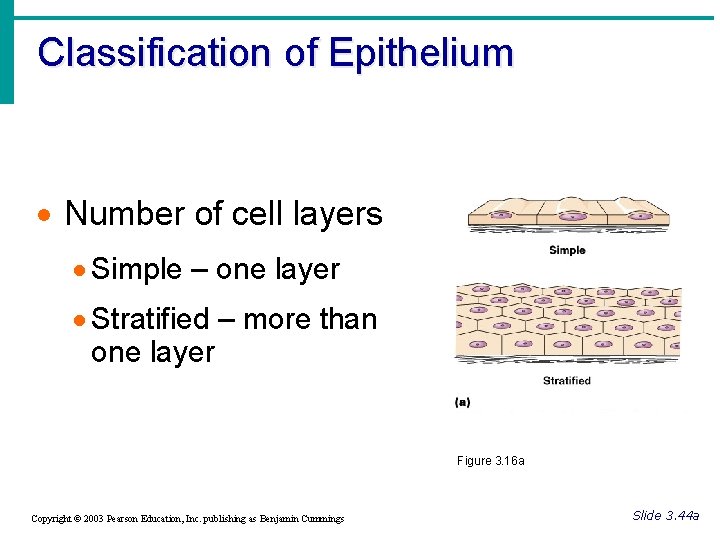
Classification of Epithelium · Number of cell layers · Simple – one layer · Stratified – more than one layer Figure 3. 16 a Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide 3. 44 a
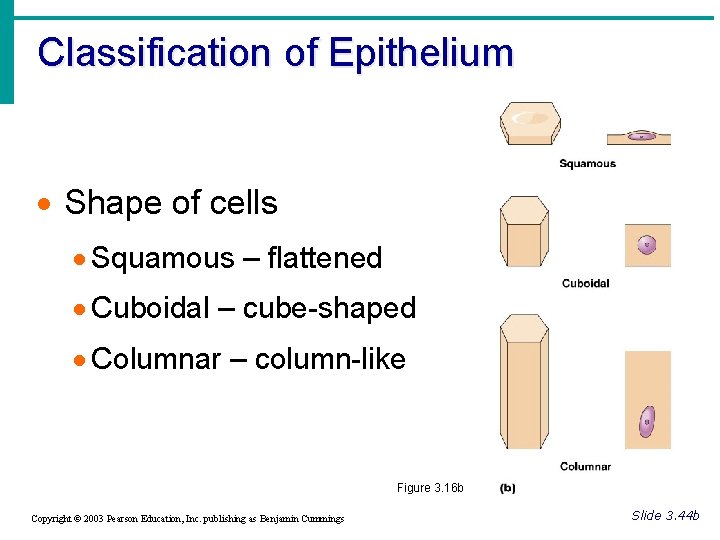
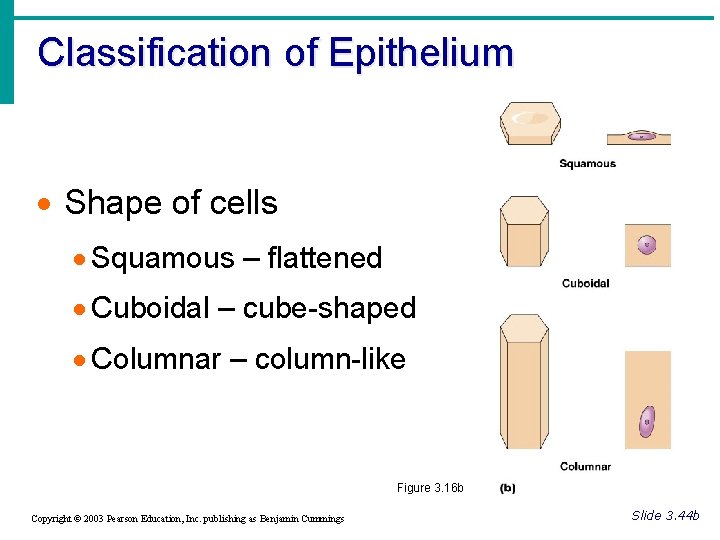
Classification of Epithelium · Shape of cells · Squamous – flattened · Cuboidal – cube-shaped · Columnar – column-like Figure 3. 16 b Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide 3. 44 b
Glandular Epithelia • Gland • One or more cells that makes and secretes an aqueous fluid called a secretion • Classified by • Site of product release—endocrine or exocrine • Relative number of cells forming the gland • unicellular (e. g. , goblet cells) or multicellular
Endocrine Glands • Ductless glands • Secretions not released into a duct • Secrete (by exocytosis) hormones that travel through lymph or blood to their specific target organs • Target organs respond in some characteristic way
Exocrine Glands • Secretions released onto body surfaces (skin) or into body cavities • More numerous than endocrine glands • Secrete products into ducts • Examples include mucous, sweat, oil, and salivary glands © 2013 Pearson Education, Inc.
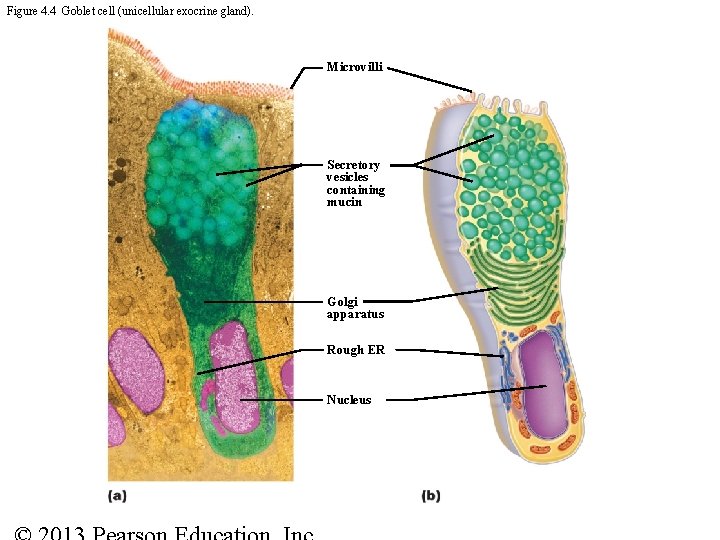
Unicellular Exocrine Glands • The only important unicellular glands are mucous cells and goblet cells • epithelial linings of intestinal and respiratory tracts • All produce mucin • Dissolves in water to form mucus • Slimy protective, lubricating coating
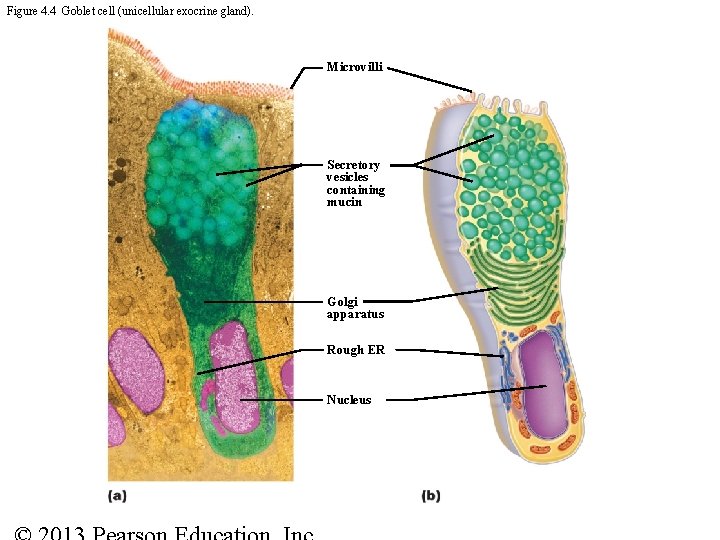
Figure 4. 4 Goblet cell (unicellular exocrine gland). Microvilli Secretory vesicles containing mucin Golgi apparatus Rough ER Nucleus
Multicellular Exocrine Glands • Multicellular exocrine glands are composed of a duct and a secretory unit • Usually surrounded by supportive connective tissue • Supplies blood and nerve fibers • Extends into and divides gland into lobes
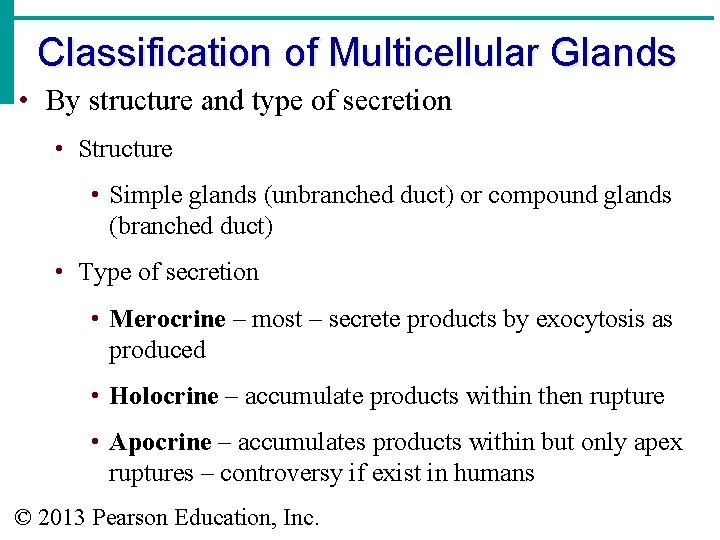
Classification of Multicellular Glands • By structure and type of secretion • Structure • Simple glands (unbranched duct) or compound glands (branched duct) • Type of secretion • Merocrine – most – secrete products by exocytosis as produced • Holocrine – accumulate products within then rupture • Apocrine – accumulates products within but only apex ruptures – controversy if exist in humans © 2013 Pearson Education, Inc.
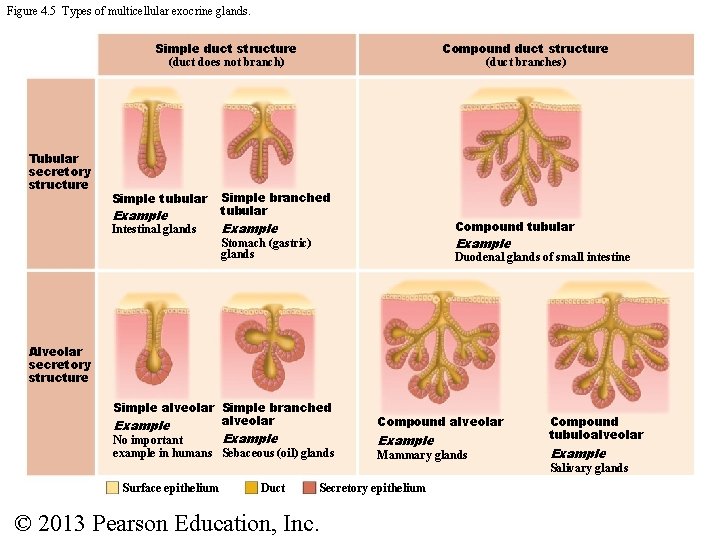
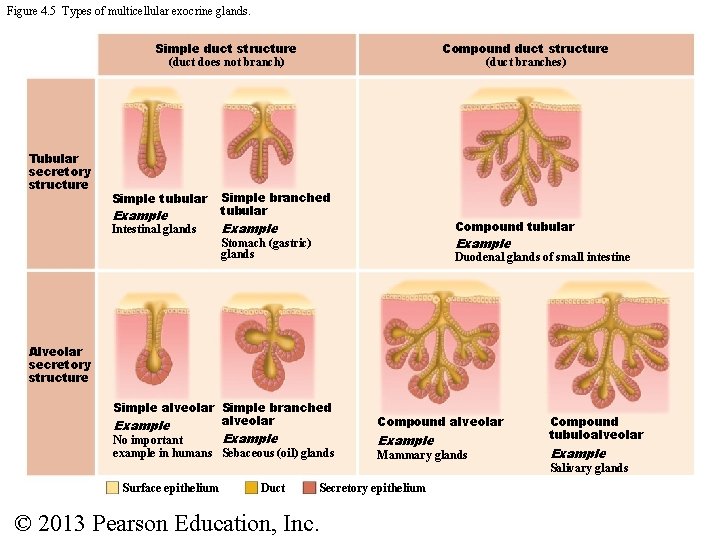
Figure 4. 5 Types of multicellular exocrine glands. Simple duct structure (duct does not branch) Tubular secretory structure Compound duct structure (duct branches) Simple tubular Simple branched tubular Intestinal glands Example Compound tubular Example Stomach (gastric) glands Duodenal glands of small intestine Alveolar secretory structure Simple alveolar Simple branched alveolar Example No important example in humans Sebaceous (oil) glands Surface epithelium Duct Compound alveolar Example Mammary glands Secretory epithelium © 2013 Pearson Education, Inc. Compound tubuloalveolar Example Salivary glands
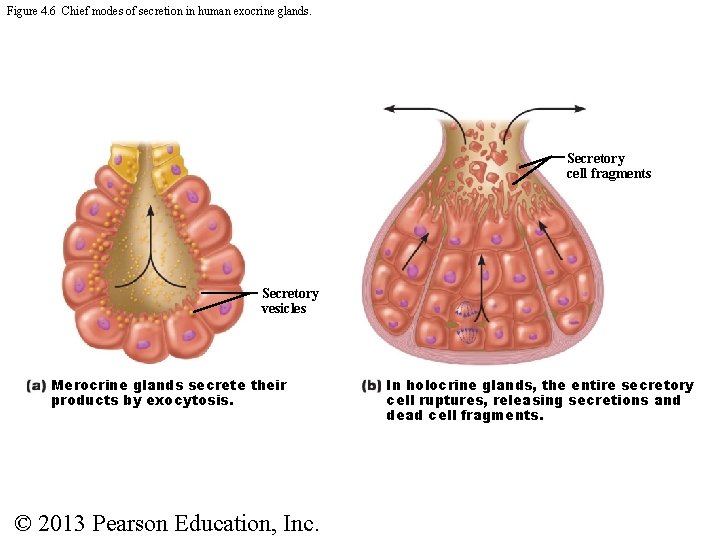
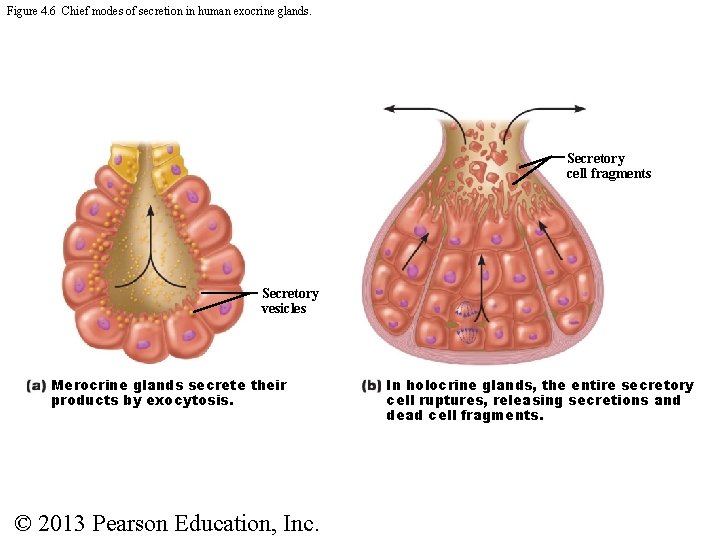
Figure 4. 6 Chief modes of secretion in human exocrine glands. Secretory cell fragments Secretory vesicles Merocrine glands secrete their products by exocytosis. © 2013 Pearson Education, Inc. In holocrine glands, the entire secretory cell ruptures, releasing secretions and dead cell fragments.
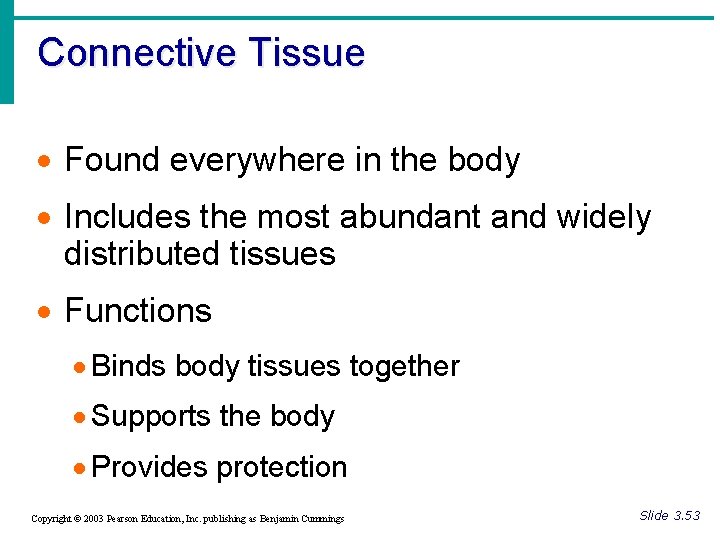
Connective Tissue · Found everywhere in the body · Includes the most abundant and widely distributed tissues · Functions · Binds body tissues together · Supports the body · Provides protection Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide 3. 53
Connective Tissue Characteristics · Variations in blood supply · Some tissue types are well vascularized · Some have poor blood supply or are avascular · Extracellular matrix · Non-living material that surrounds living cells Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide 3. 54
Connective Tissue Characteristics · Three characteristics make connective tissues different from other primary tissues 1. Have mesenchyme (an embryonic tissue) as their common tissue of origin 2. Have varying degrees of vascularity (blood vessels) 3. Have extracellular matrix · Connective tissue not composed mainly of cells · Largely nonliving extracellular matrix separates cells · So can bear weight, withstand tension, endure abuse Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide 3. 54
Structural Elements of Connective Tissue • Three elements • Ground substance • Fibers • Cells • Composition and arrangement varies in different connective tissues
Ground Substance • Unstructured material that fills space between cells • Medium through which solutes diffuse between blood capillaries and cells • Components • Interstitial fluid • Cell adhesion proteins ("glue" for attachment) • Proteoglycans • Protein core + large polysaccharides • Trap water in varying amounts, affecting viscosity of ground substance
Connective Tissue Fibers • Three types of fibers provide support • Collagen • Strongest and most abundant type • Tough; provides high tensile strength • Elastic fibers • Networks of long, thin, elastin fibers that allow for stretch and recoil • Reticular • Short, fine, highly branched collagenous fibers (different chemistry and form than collagen fibers) • Branch, forming networks that offer more "give" © 2013 Pearson Education, Inc.
Cells • "Blast" cells-Immature form; mitotically active; secrete ground substance and fibers • Fibroblasts in connective tissue proper • Chondroblasts in cartilage • Osteoblasts in bone • Hematopoietic stem cells in bone marrow (hemocytoblast) • "Cyte" cells- Mature form; maintain matrix • Chondrocytes in cartilage • Osteocytes in bone
Other Cell Types: Connective Tissues • Fat cells • Store nutrients • White blood cells • Neutrophils, eosinophils, lymphocytes • Tissue response to injury • Mast cells • Initiate local inflammatory response against foreign microorganisms they detect • Macrophages • Phagocytic cells that "eat" dead cells, microorganisms; function in immune system
Types of Connective Tissues: Connective Tissue Proper • All connective tissues except bone, cartilage and blood • Two subclasses • Loose connective tissues • Areolar, Adipose, Reticular • Dense connective tissues (also called fibrous connective tissues) • Dense regular, Dense irregular, Elastic © 2013 Pearson Education, Inc.
Muscle Tissue · Function is to produce movement · Either locomotion of body or substances within body · Highly cellular · Well vascularized · Possess myofilaments (allow for contraction) Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide 3. 64
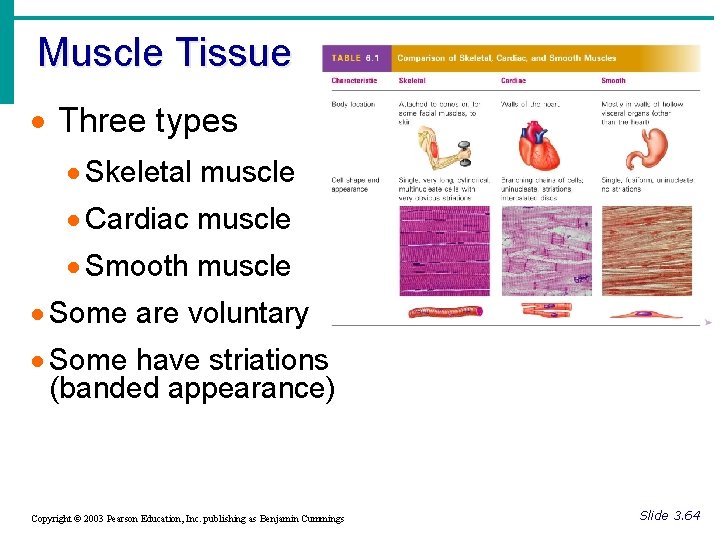
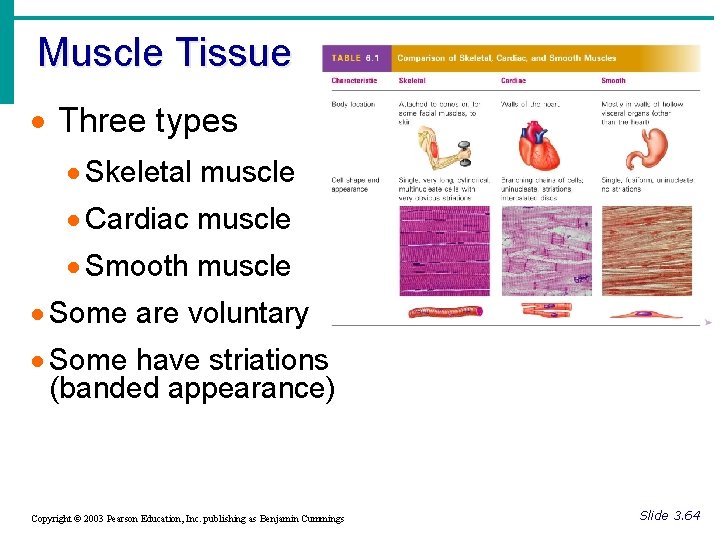
Muscle Tissue · Three types · Skeletal muscle · Cardiac muscle · Smooth muscle · Some are voluntary · Some have striations (banded appearance) Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide 3. 64
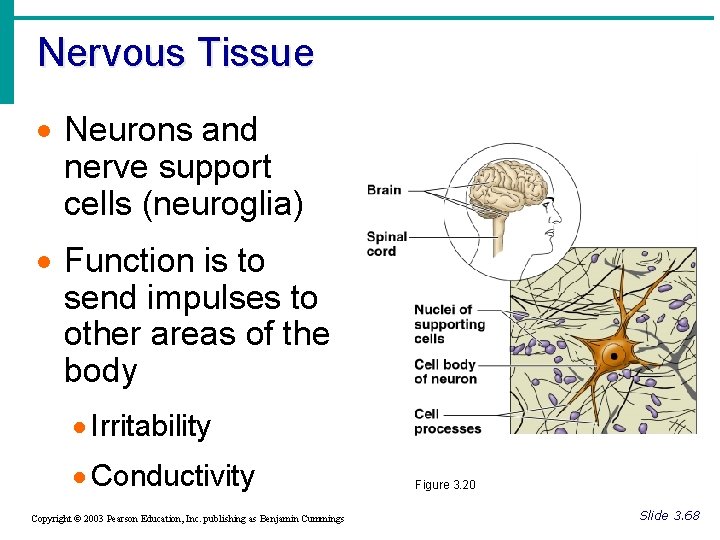
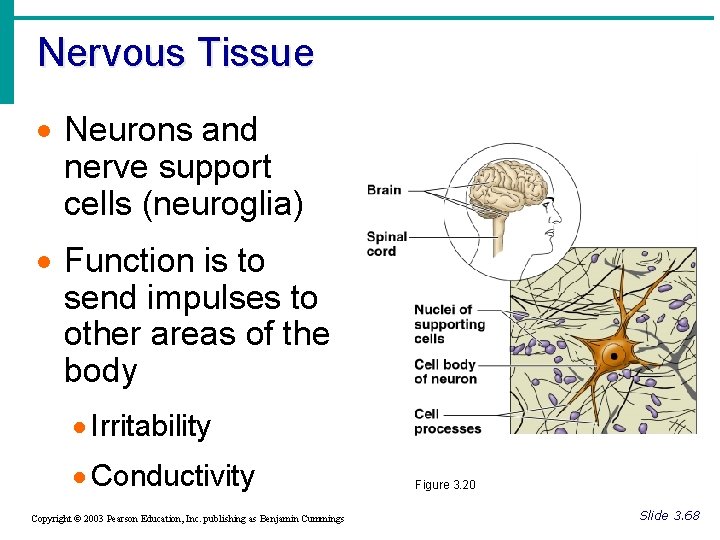
Nervous Tissue · Neurons and nerve support cells (neuroglia) · Function is to send impulses to other areas of the body · Irritability · Conductivity Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Figure 3. 20 Slide 3. 68
Cell Junctions • How do cells bind together to form tissues?
Factors that bind cells to form a tissue • Adhesive glycoproteins on plasma membrane surface • Wavy indention that “fit” together
Membrane Junctions Some cells "free" e. g. , blood cells, sperm cells Some bound into communities • Tight junction • Desmosome • Gap junction
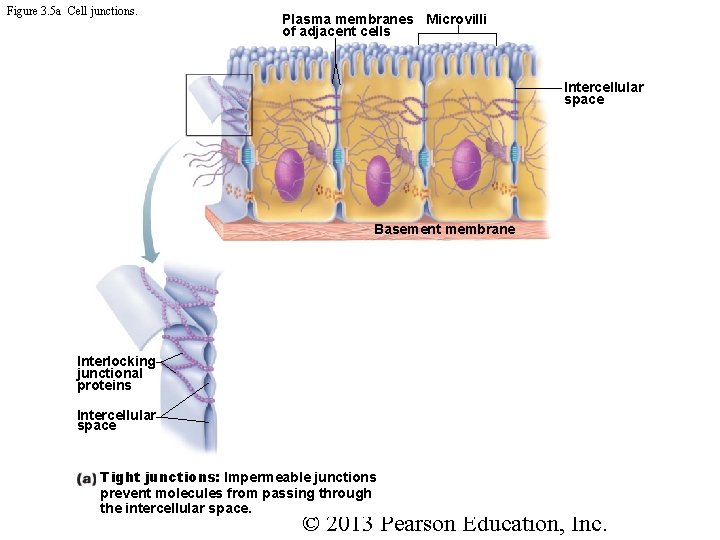
Tight junction • Plasma membranes touch • Protein molecules fuse together tightly • Like zipper • Prevent fluids and most molecules from moving between cells • Where might these be useful in body? • Small intestine
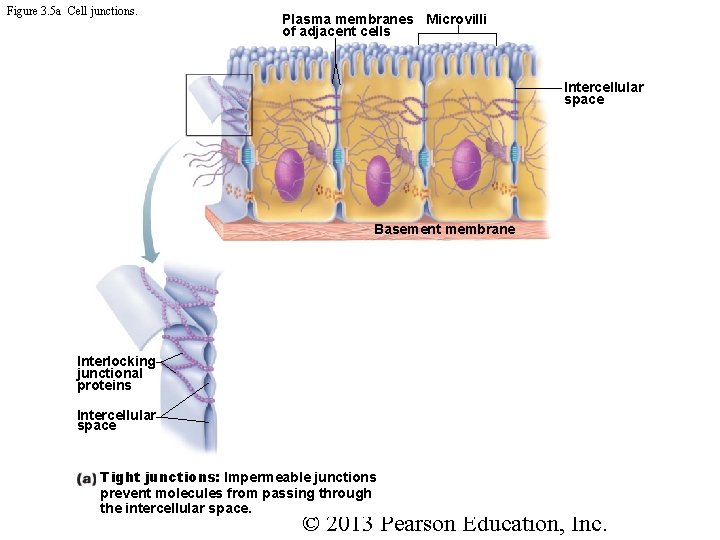
Figure 3. 5 a Cell junctions. Plasma membranes Microvilli of adjacent cells Intercellular space Basement membrane Interlocking junctional proteins Intercellular space Tight junctions: Impermeable junctions prevent molecules from passing through the intercellular space. © 2013 Pearson Education, Inc.
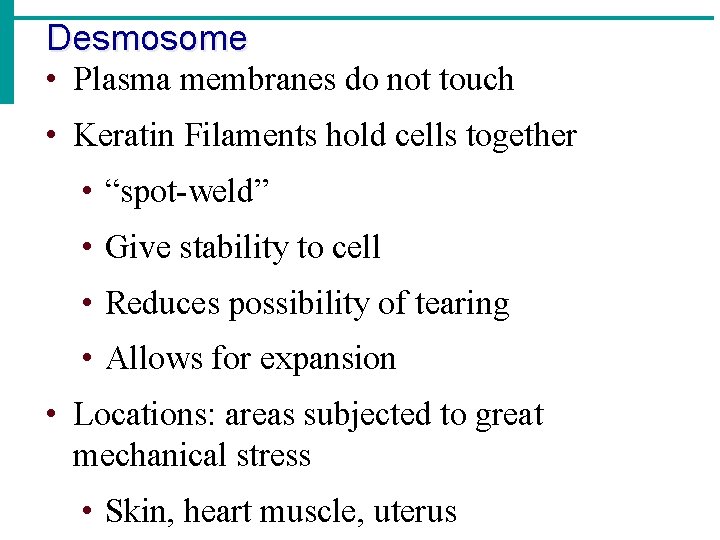
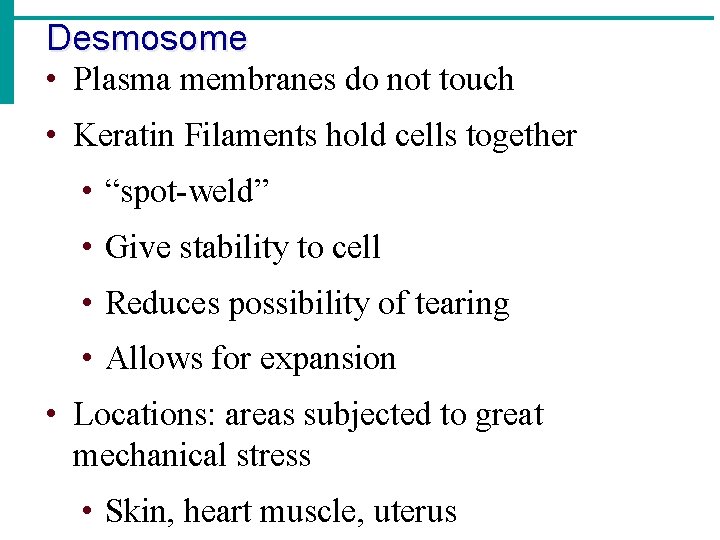
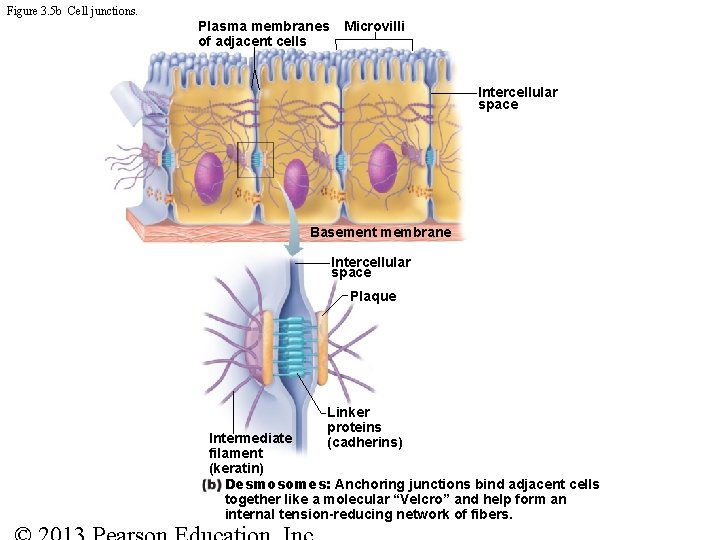
Desmosome • Plasma membranes do not touch • Keratin Filaments hold cells together • “spot-weld” • Give stability to cell • Reduces possibility of tearing • Allows for expansion • Locations: areas subjected to great mechanical stress • Skin, heart muscle, uterus
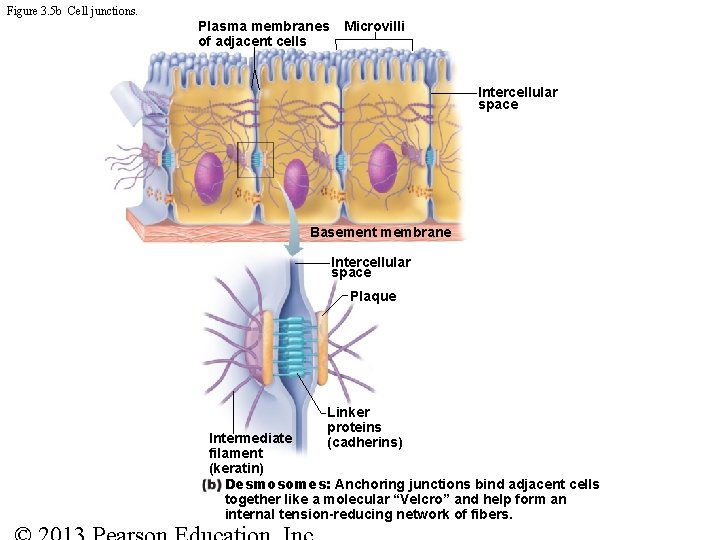
Figure 3. 5 b Cell junctions. Plasma membranes of adjacent cells Microvilli Intercellular space Basement membrane Intercellular space Plaque Linker proteins (cadherins) Intermediate filament (keratin) Desmosomes: Anchoring junctions bind adjacent cells together like a molecular “Velcro” and help form an internal tension-reducing network of fibers.
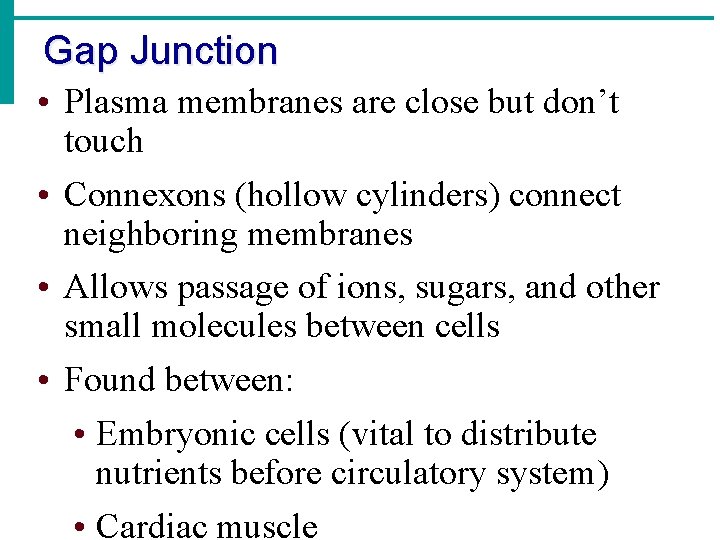
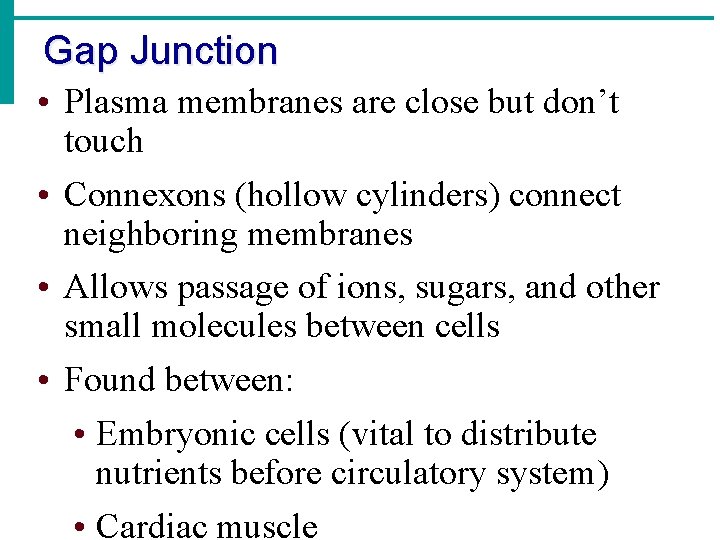
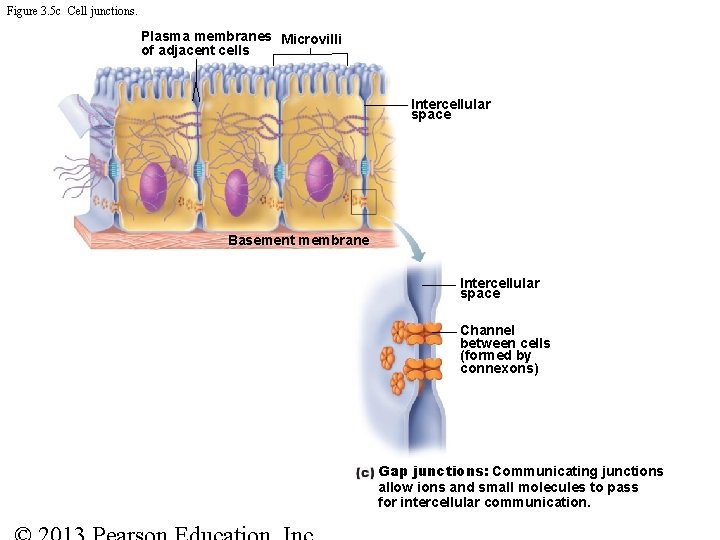
Gap Junction • Plasma membranes are close but don’t touch • Connexons (hollow cylinders) connect neighboring membranes • Allows passage of ions, sugars, and other small molecules between cells • Found between: • Embryonic cells (vital to distribute nutrients before circulatory system) • Cardiac muscle
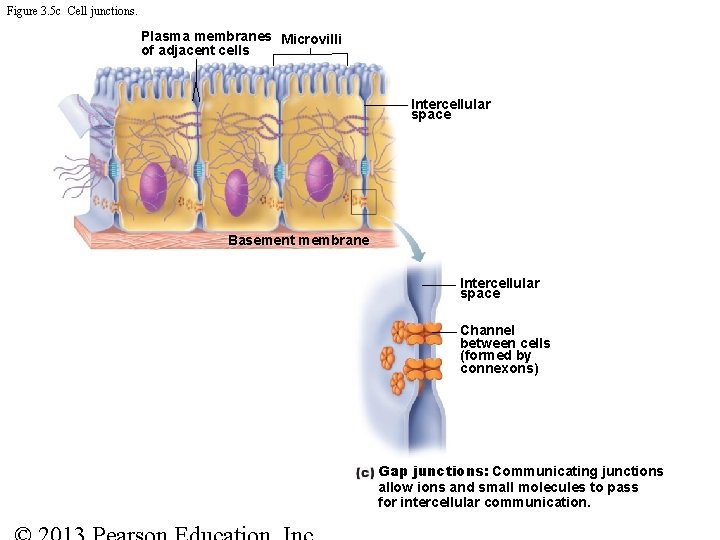
Figure 3. 5 c Cell junctions. Plasma membranes Microvilli of adjacent cells Intercellular space Basement membrane Intercellular space Channel between cells (formed by connexons) Gap junctions: Communicating junctions allow ions and small molecules to pass for intercellular communication.
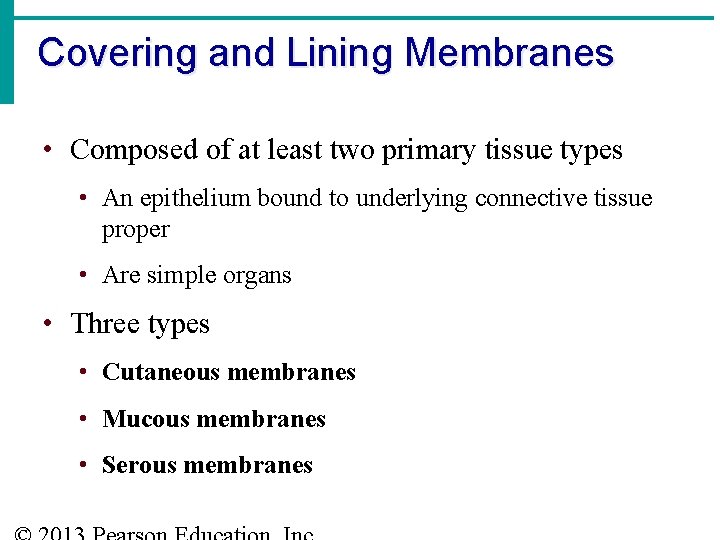
Covering and Lining Membranes • Composed of at least two primary tissue types • An epithelium bound to underlying connective tissue proper • Are simple organs • Three types • Cutaneous membranes • Mucous membranes • Serous membranes
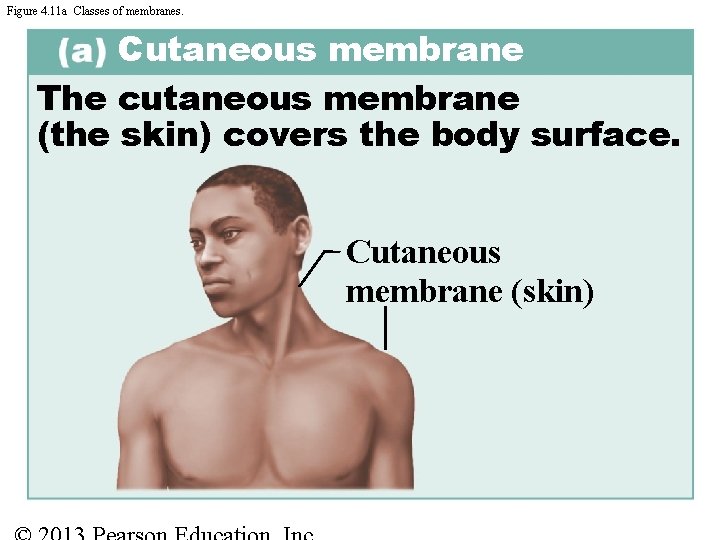
Cutaneous Membranes • Skin • Keratinized stratified squamous epithelium (epidermis) attached to a thick layer of connective tissue (dermis) • Dry membrane
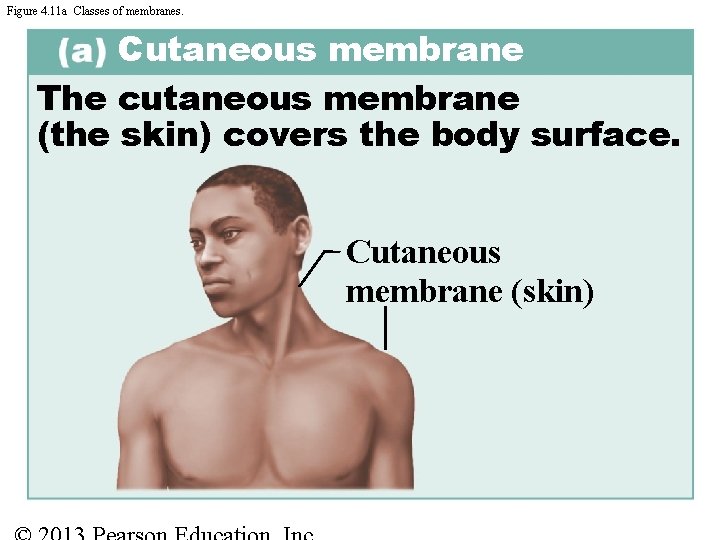
Figure 4. 11 a Classes of membranes. Cutaneous membrane The cutaneous membrane (the skin) covers the body surface. Cutaneous membrane (skin)
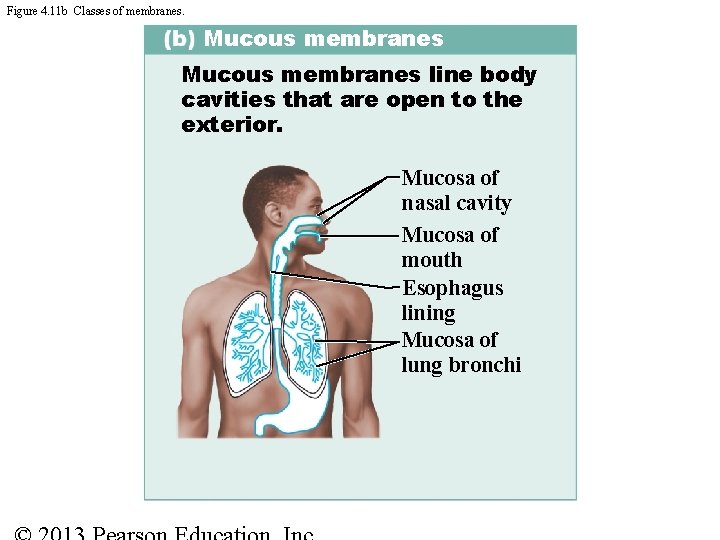
Mucous Membranes • Mucosa indicates location not cell composition • All called mucosae • Line body cavities open to the exterior (e. g. , Digestive, respiratory, urogenital tracts) • Moist membranes bathed by secretions (or urine) • Epithelial sheet lies over layer of connective tissue called lamina propria • May secrete mucus
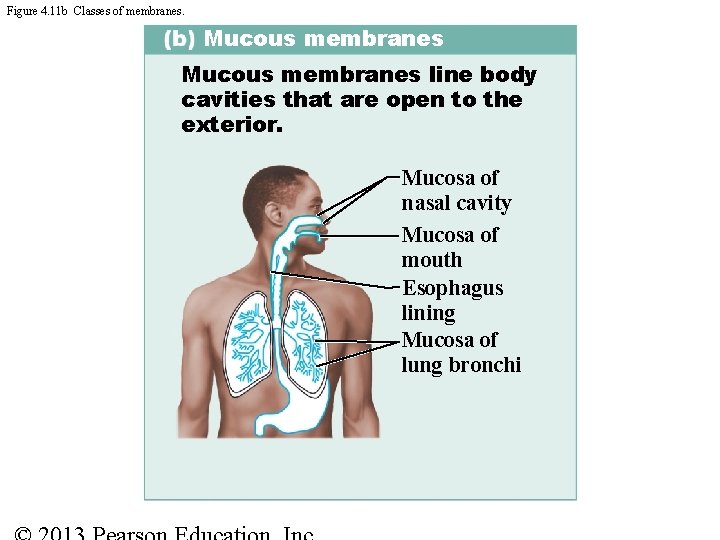
Figure 4. 11 b Classes of membranes. Mucous membranes line body cavities that are open to the exterior. Mucosa of nasal cavity Mucosa of mouth Esophagus lining Mucosa of lung bronchi
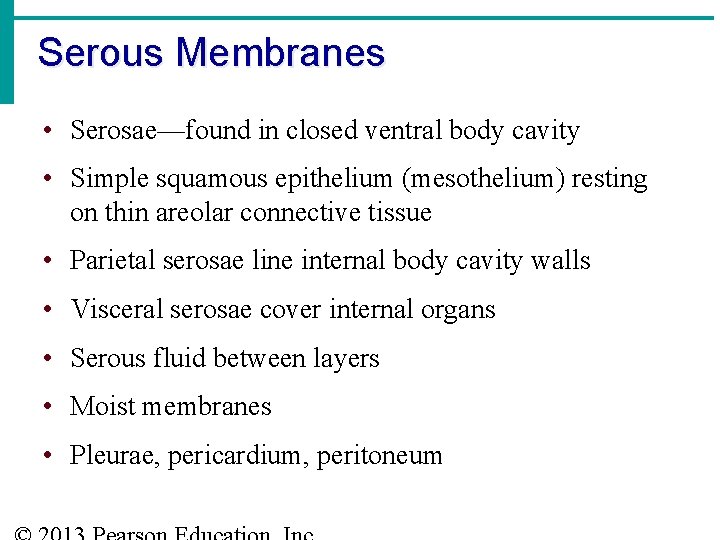
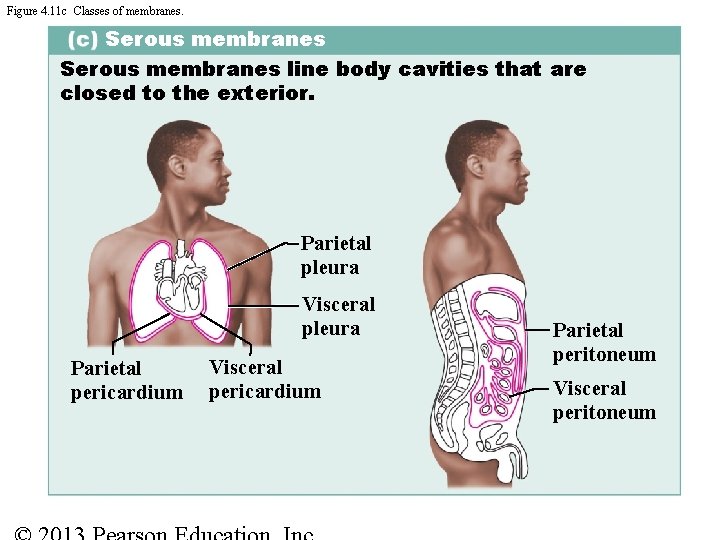
Serous Membranes • Serosae—found in closed ventral body cavity • Simple squamous epithelium (mesothelium) resting on thin areolar connective tissue • Parietal serosae line internal body cavity walls • Visceral serosae cover internal organs • Serous fluid between layers • Moist membranes • Pleurae, pericardium, peritoneum
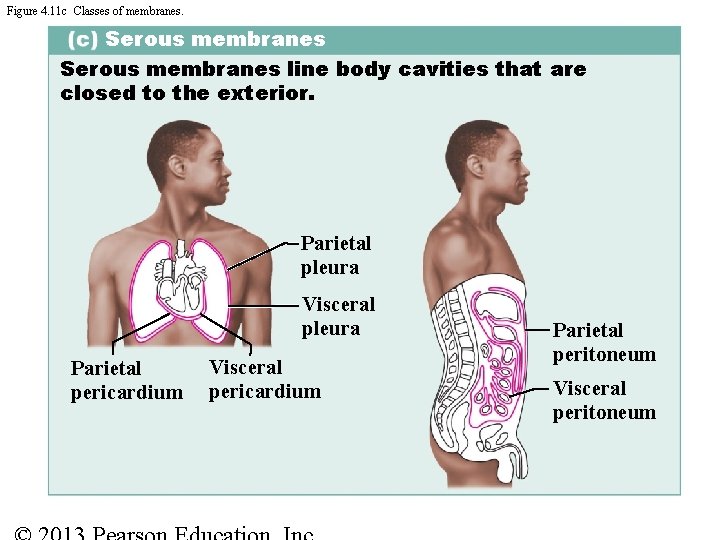
Figure 4. 11 c Classes of membranes. Serous membranes line body cavities that are closed to the exterior. Parietal pleura Visceral pleura Parietal pericardium Visceral pericardium Parietal peritoneum Visceral peritoneum
Tissue Repair · How are tissues repaired when injured? Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide 3. 69
Tissue Repair · Regeneration · Replacement of destroyed tissue by the same kind of cells · Fibrosis · Repair by dense fibrous connective tissue (scar tissue) · Determination of method · Type of tissue damaged · Severity of the injury Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide 3. 69
Tissue Repair • Necessary when barriers are penetrated • Cells must divide and migrate • Occurs in two major ways • Regeneration • Same kind of tissue replaces destroyed tissue • Original function restored • Fibrosis • Connective tissue replaces destroyed tissue • Original function lost
Tissue Repair: Step 1 • Inflammation sets stage • Release of inflammatory chemicals • Dilation of blood vessels • Increase in vessel permeability • Clotting occurs

Figure 4. 12. Tissue repair of a nonextensive skin wound: regeneration and fibrosis. Slide 1 Scab Epider mis Vein Blood clot in incised wound Inflammato ry chemicals Migrating white Arteryblood cell 1 Inflammation sets the stage: • Severed blood vessels bleed. • Inflammatory chemicals are released. • Local blood vessels become more permeable, allowing white blood cells, fluid, clotting proteins, and other plasma proteins to seep into the injured area. • Clotting occurs; surface dries and forms a scab.
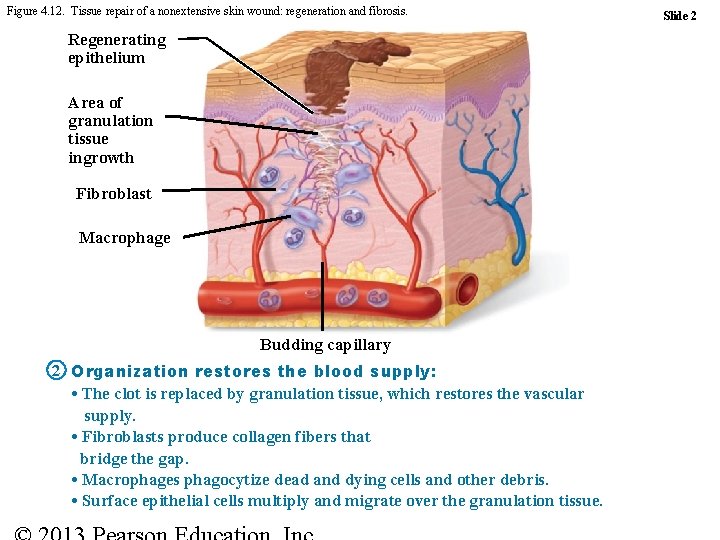
Tissue Repair: Step 2 • Organization restores blood supply • The blood clot is replaced with granulation tissue • Epithelium begins to regenerate • Fibroblasts produce collagen fibers to bridge the gap • Debris is phagocytized
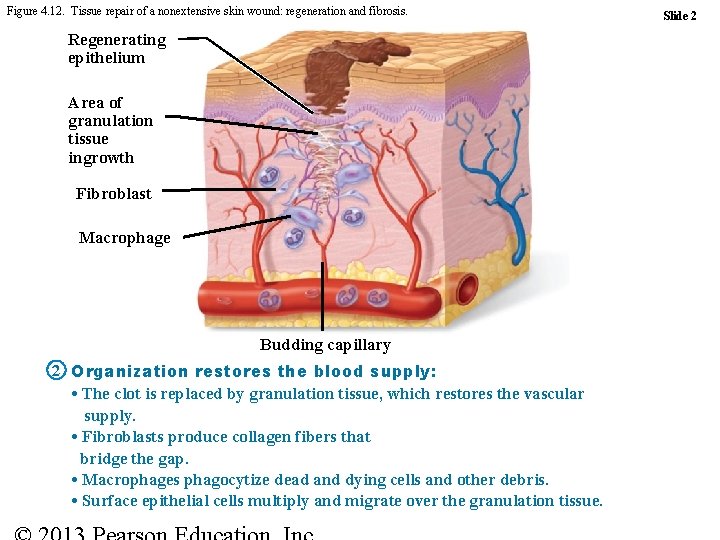
Figure 4. 12. Tissue repair of a nonextensive skin wound: regeneration and fibrosis. Regenerating epithelium Area of granulation tissue ingrowth Fibroblast Macrophage Budding capillary 2 Organization restores the blood supply: • The clot is replaced by granulation tissue, which restores the vascular supply. • Fibroblasts produce collagen fibers that bridge the gap. • Macrophages phagocytize dead and dying cells and other debris. • Surface epithelial cells multiply and migrate over the granulation tissue. Slide 2
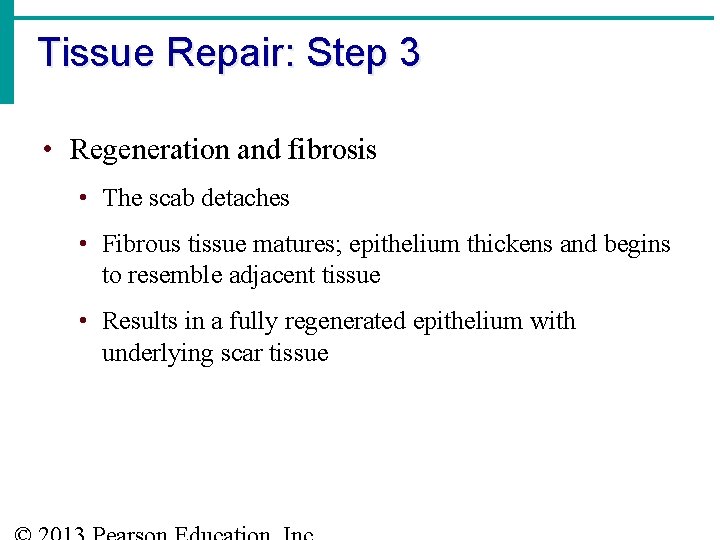
Tissue Repair: Step 3 • Regeneration and fibrosis • The scab detaches • Fibrous tissue matures; epithelium thickens and begins to resemble adjacent tissue • Results in a fully regenerated epithelium with underlying scar tissue
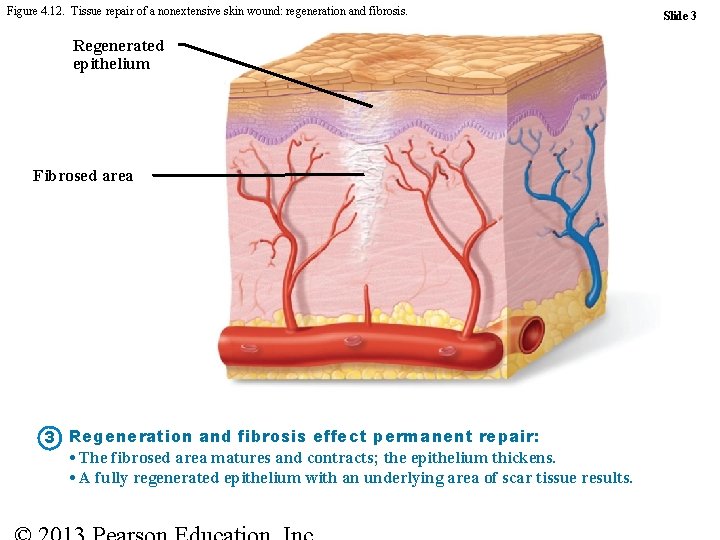
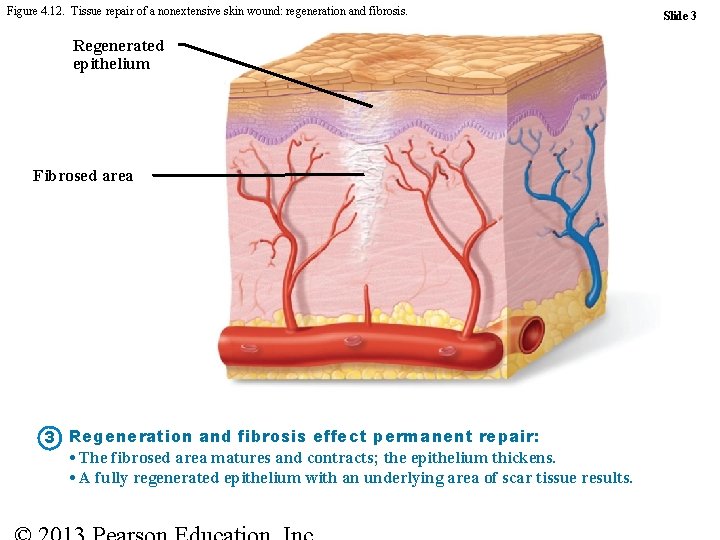
Figure 4. 12. Tissue repair of a nonextensive skin wound: regeneration and fibrosis. Regenerated epithelium Fibrosed area 3 Regeneration and fibrosis effect permanent repair: • The fibrosed area matures and contracts; the epithelium thickens. • A fully regenerated epithelium with an underlying area of scar tissue results. Slide 3
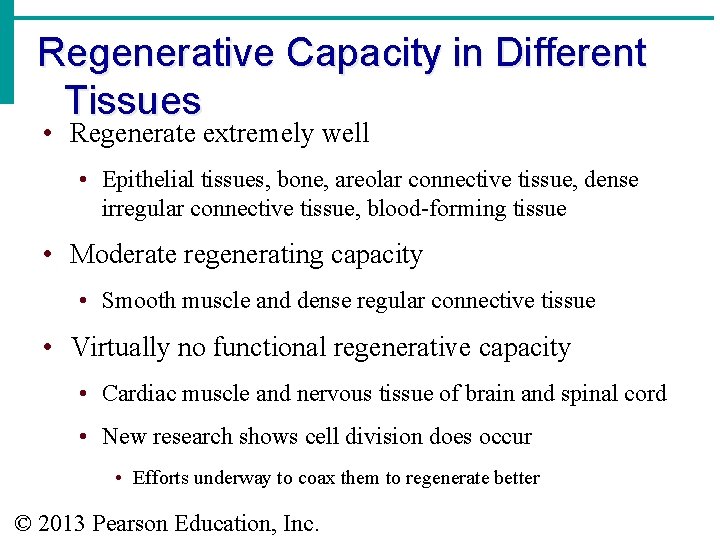
Regenerative Capacity in Different Tissues • Regenerate extremely well • Epithelial tissues, bone, areolar connective tissue, dense irregular connective tissue, blood-forming tissue • Moderate regenerating capacity • Smooth muscle and dense regular connective tissue • Virtually no functional regenerative capacity • Cardiac muscle and nervous tissue of brain and spinal cord • New research shows cell division does occur • Efforts underway to coax them to regenerate better © 2013 Pearson Education, Inc.
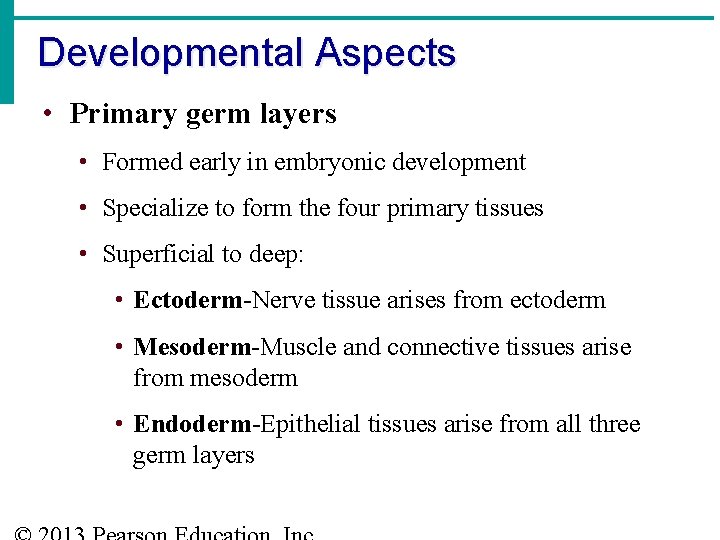
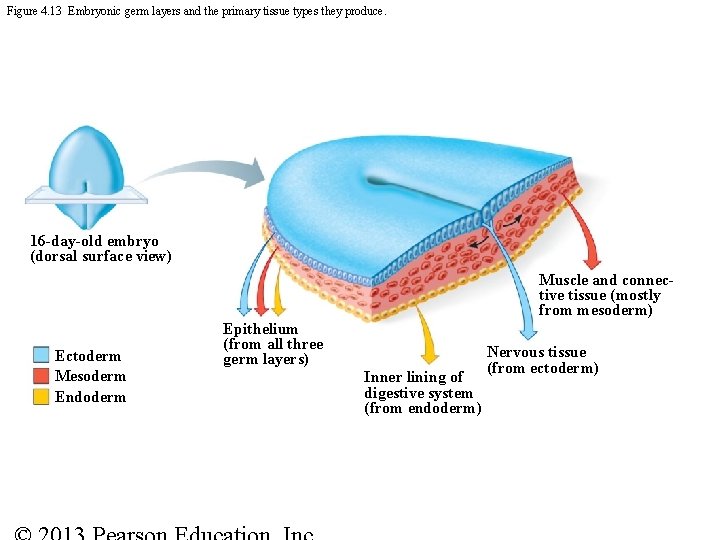
Developmental Aspects • Primary germ layers • Formed early in embryonic development • Specialize to form the four primary tissues • Superficial to deep: • Ectoderm-Nerve tissue arises from ectoderm • Mesoderm-Muscle and connective tissues arise from mesoderm • Endoderm-Epithelial tissues arise from all three germ layers
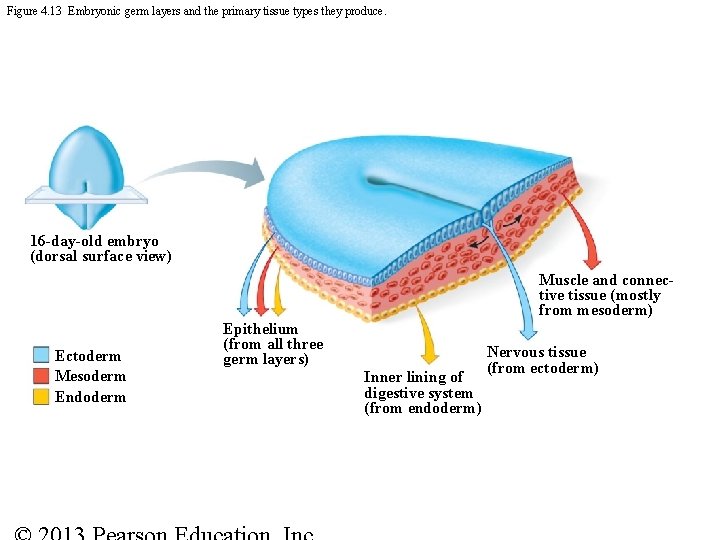
Figure 4. 13 Embryonic germ layers and the primary tissue types they produce. 16 -day-old embryo (dorsal surface view) Muscle and connective tissue (mostly from mesoderm) Ectoderm Mesoderm Endoderm Epithelium (from all three germ layers) Inner lining of digestive system (from endoderm) Nervous tissue (from ectoderm)
Aging Tissues • Normally function well through youth and middle age if adequate diet, circulation, and infrequent wounds and infections • Epithelia thin with increasing age so more easily breached • Tissue repair less efficient • Bone, muscle and nervous tissues begin to atrophy • DNA mutations possible increased cancer risk © 2013 Pearson Education, Inc.