Chapter 4 Thermotherapy and Cryotherapy Infrared Modalities Most

- Slides: 61
Chapter 4: Thermotherapy and Cryotherapy
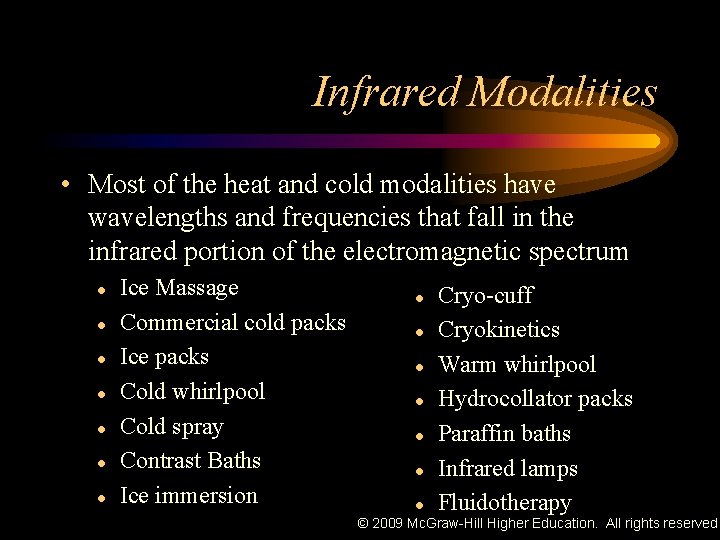
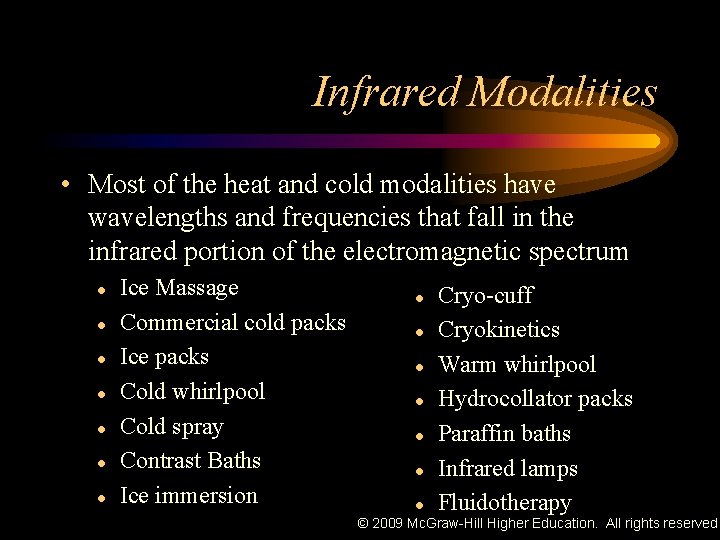
Infrared Modalities • Most of the heat and cold modalities have wavelengths and frequencies that fall in the infrared portion of the electromagnetic spectrum l l l l Ice Massage Commercial cold packs Ice packs Cold whirlpool Cold spray Contrast Baths Ice immersion l l l l Cryo-cuff Cryokinetics Warm whirlpool Hydrocollator packs Paraffin baths Infrared lamps Fluidotherapy © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
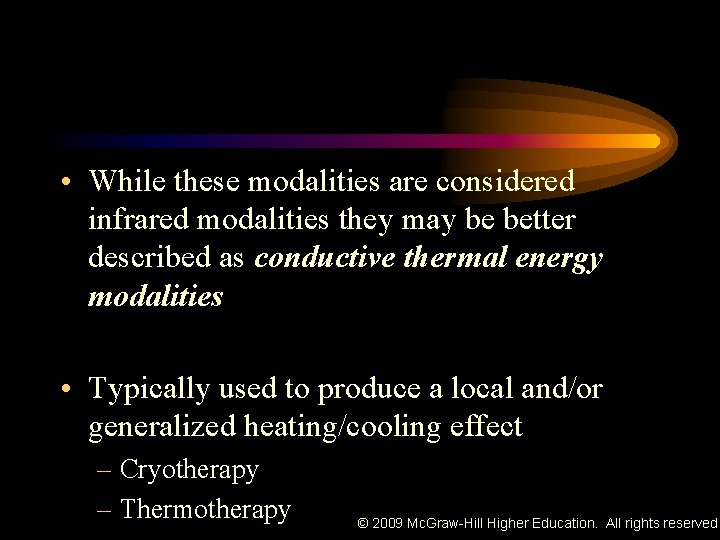
• While these modalities are considered infrared modalities they may be better described as conductive thermal energy modalities • Typically used to produce a local and/or generalized heating/cooling effect – Cryotherapy – Thermotherapy © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Mechanisms of Heat Transfer • Transmission of heat occurs by three mechanisms: Conduction n Convection n Radiation n *Conversion (involves change in one energy form to another) © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Appropriate Use of Infrared Modalities • Thermotherapy – Heating techniques used for therapeutic purposes – Used when a rise in tissue temperature is the goal of treatment • Cryotherapy – Used in the acute stages of the healing process immediately following injury when a loss of tissue temperature is the goal of therapy © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Appropriate Use of Infrared Modalities • Cold application is often continued throughout the rehabilitation and reconditioning process of an injury • Hydrotherapy is also included (hot or cold) as water can be used as the medium through which heat is transferred © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Appropriate Use of Infrared Modalities • Knowledge of the injury mechanism, pathology and healing process are critical when determining appropriate hot and cold application • Simple, efficient, and inexpensive means of patient care © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Clinical Use of Conductive Energy Modalities • Physiologic effects are rarely the result of direct absorption of infrared energy • No form of infrared energy can have a depth of penetration greater than 1 cm • Effects of infrared modalities are primarily superficial and directly affect cutaneous blood vessels and nerve receptors © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
• If significant amounts of energy are absorbed over time, temperature of circulating blood will increase – Hypothalamus reflexively increase blood flow to the area – The reverse is true with cold application – Deep heating modalities (US, diathermy) may be more beneficial when increased blood flow to deeper tissues is desired © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
• Most effective use of infrared modalities should be to provide analgesia or reduce sensation of pain associated with injury – Gate control theory of pain modulation • Pain reduction to facilitate therapeutic exercise is common practice • Continued research and investigation is necessary to provide athletic trainers with effective and efficient means of injury © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Effects of Tissue Temperature Change on Circulation • Main physiologic effect is on superficial circulation – Changes due to response of temperature receptors in skin and sympathetic nervous system • When cold is applied the skin vessels progressively constrict to a temperature of about 15° C (59° F) at which point they reach maximum constriction © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Effects of Tissue Temperature Change on Circulation • At temperatures below 15° C vessels begin to dilate – Caused by paralysis of contractile mechanism in vessel wall or blockage of nerve impulses • General exposure to cold causes sympathetic nerves to elicit cutaneous vasoconstriction, shivering, piloerection, and an increase in epinephrine secretion so vascular contraction occurs © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
• Simultaneously, metabolism and heat production increase – Aids in increasing core temperature • Increased blood flow will also result in increasing oxygen to the area – Results in analgesic and relaxation effects on muscle spasm – Increased proprioceptive reflex may explain © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
• Three types of sensory receptors in subepithelial tissue – Cold, warm, pain – Each responds differently at different temperatures – Adapt to changes in temperature, with rapid temperature change = more rapid adaptation • Stimulation of larger surface areas results in summation of thermal signals trigger vasomotor centers in hypothalamus © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Effects of Tissue Temperature Change on Muscle Spasm • Physiologic mechanisms underlying the effectiveness of heat and cold treatments in reducing muscle spasm lie at level of muscle spindle and Golgi tendon organs • Heat relaxes muscles simultaneously lessening stimulus threshold of muscle spindles and by decreasing gamma efferent firing rate – Thus muscle spindles are more easily excited © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Effects of Tissue Temperature Change on Muscle Spasm • Muscles may be electromyographically silent while at rest during application of heat, but the slightest amount of voluntary or passive movement may cause the efferents to fire • Local applications of cold decrease local neural activity © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Effects of Tissue Temperature Change on Muscle Spasm • Cold raises the threshold stimulus of muscle spindles, and heat tends to lower it • Local cooling results in a significant reduction of muscle spasm greater than with use of heat • Unclear if reduction of spasticity is caused by excitability of motor neurons or hyperactivity of gamma systems • Cold effective in modifying stretch-reflex mechanism © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Effects of Tissue Temperature Change on Muscle Spasm • Nerve conduction velocity reduction also occurs with cold application – Decreases afferent discharge from cutaneous receptors © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Effects of Tissue Temperature Change on Performance • Cryotherapy – Some disagreement on relative concentric and eccentric torque capabilities – May not increase torque but may improve endurance – Decreases vertical jump – No impact joint range of motion – Negatively impacts functional performance, which can be negated via an active warm-up – Minimal or no effect on joint position sense, proprioception, balance and agility © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Effects of Tissue Temperature Change on Performance • Thermotherapy – Minimal or no effect on joint position sense, proprioception, and balance © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Cryotherapy: Physiologic Effects of Tissue Cooling • General agreement that cold should be initial treatment for musculoskeletal injuries – Primary reason is to lower temperature in injured area reduces metabolic rate with a corresponding decrease in production of metabolites and metabolic heat (secondary hypoxic response) • More effective when combined with compression – Promotes vasoconstriction and helps to control hemorrhaging and edema © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Cryotherapy: Physiologic Effects of Tissue Cooling • Used immediately after injury to decrease pain and muscle spasm – Result of decreased nerve conduction velocity – Cold stimulus bombards sensory receptors resulting in pain modulation through gate control • Effective in treating myofascial pain • Effective in treating acute muscle pain as opposed to delayed onset muscle soreness © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Cryotherapy: Physiologic Effects of Tissue Cooling • Reduction in muscle guarding has been observed clinically • Initial reaction of body to cold is local vasoconstriction – Results in decreased nutrient and phagocyte delivery to area • Hunting Response – Periods of vasodilation and constriction following prolonged cold application to limit possible tissue injury due to cold use© 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Cryotherapy: Physiologic Effects of Tissue Cooling • Cooling for too long may be detrimental to healing • Ice application for 20 min. = decreased muscle blood flow – However, effects of ice application diminishes with increased tissue depth • Length of cooling required is dependent on subcutaneous tissue thickness – Recommended treatment times = 5 -45 minutes © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
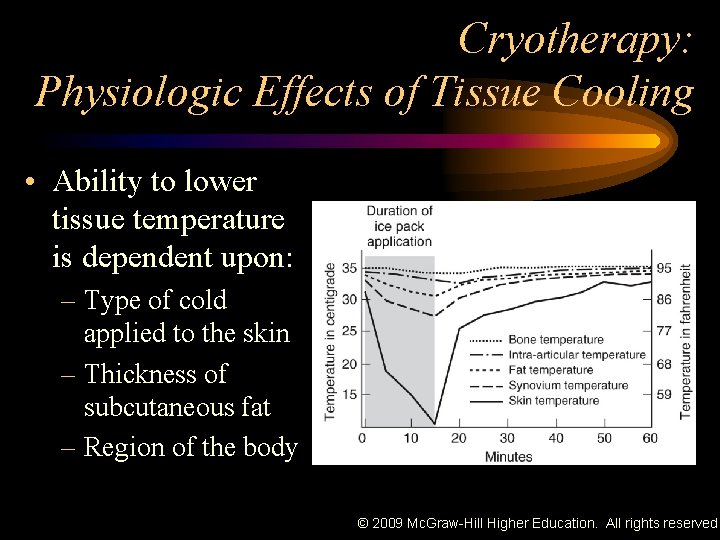
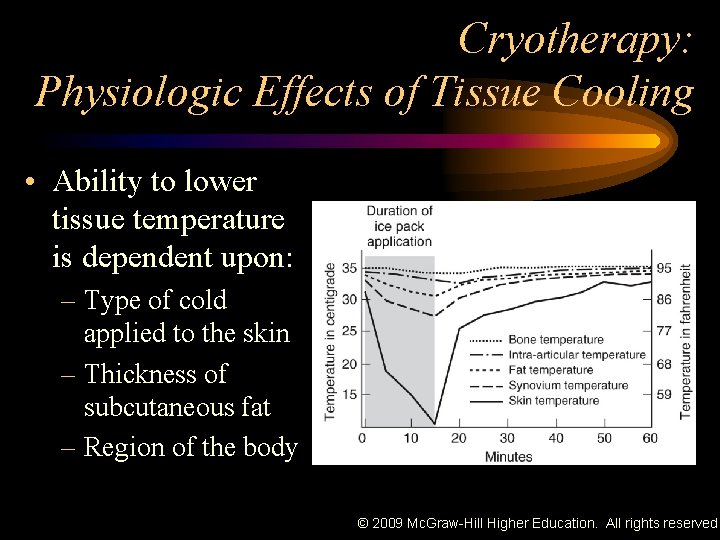
Cryotherapy: Physiologic Effects of Tissue Cooling • Ability to lower tissue temperature is dependent upon: – Type of cold applied to the skin – Thickness of subcutaneous fat – Region of the body © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Cryotherapy: Physiologic Effects of Tissue Cooling • Cold application results in: – Decreased cell permeability and metabolism – Decreased edema accumulation • Should be continued in 5 -45 minute applications for up to 72 hours initially © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
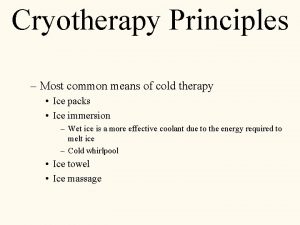
Cryotherapy Techniques • Cryotherapy techniques include – – – Ice massage Cold packs Ice packs Cold whirlpool Cold spray – – Contrast baths Ice immersion Cryo-cuff Cryokinetics © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Cryotherapy Techniques • Application of cryotherapy produces a three - to four-stage sensation – Uncomfortable sensation of cold – Stinging – Burning or aching feeling – Numbness • Caution should be exercised when applying intense cold directly to the skin © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
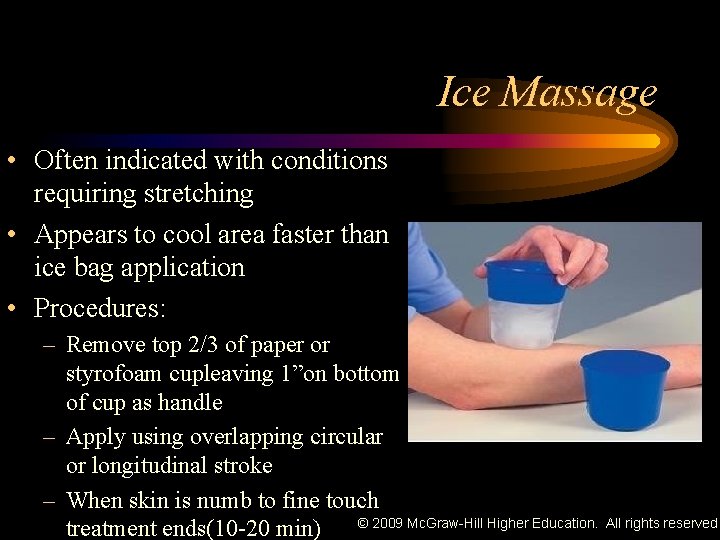
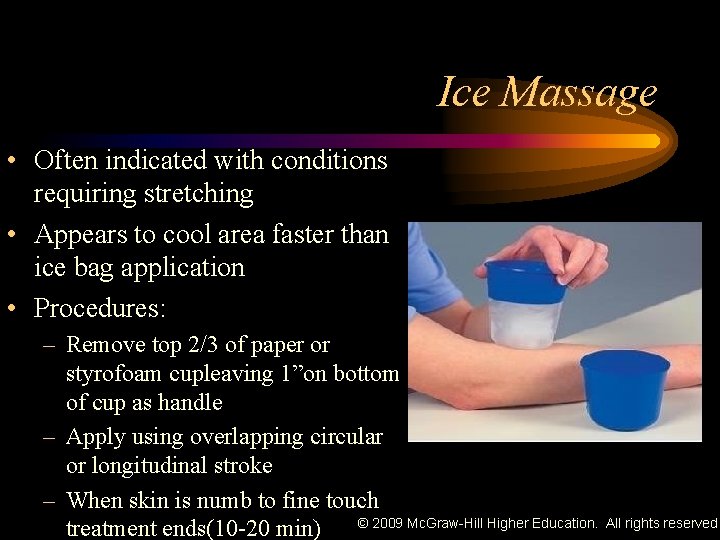
Ice Massage • Often indicated with conditions requiring stretching • Appears to cool area faster than ice bag application • Procedures: – Remove top 2/3 of paper or styrofoam cupleaving 1”on bottom of cup as handle – Apply using overlapping circular or longitudinal stroke – When skin is numb to fine touch © 2009 Mc. Graw-Hill Higher Education. treatment ends(10 -20 min) All rights reserved.
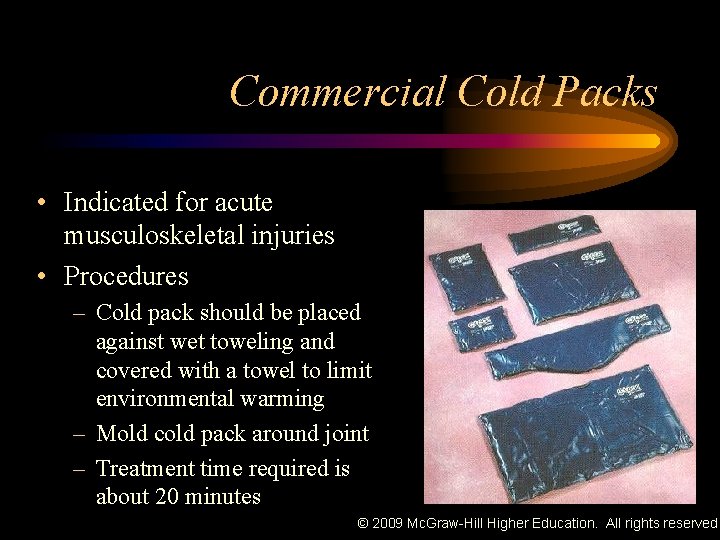
Commercial Cold Packs • Indicated for acute musculoskeletal injuries • Procedures – Cold pack should be placed against wet toweling and covered with a towel to limit environmental warming – Mold cold pack around joint – Treatment time required is about 20 minutes © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
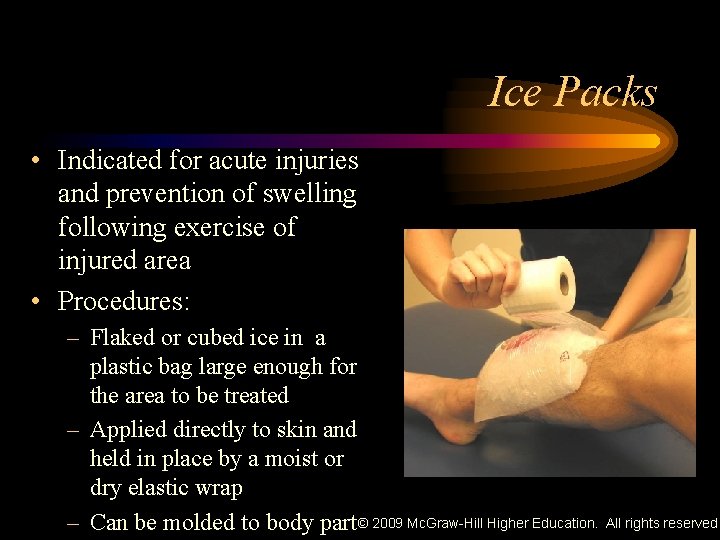
Ice Packs • Indicated for acute injuries and prevention of swelling following exercise of injured area • Procedures: – Flaked or cubed ice in a plastic bag large enough for the area to be treated – Applied directly to skin and held in place by a moist or dry elastic wrap – Can be molded to body part © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
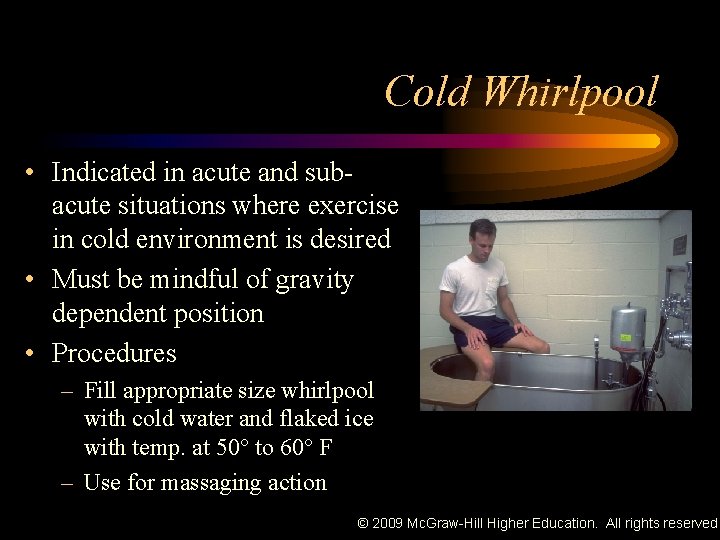
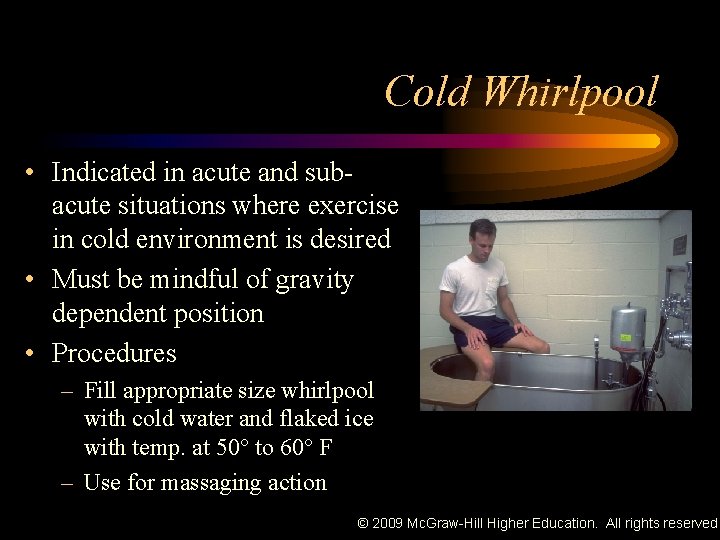
Cold Whirlpool • Indicated in acute and subacute situations where exercise in cold environment is desired • Must be mindful of gravity dependent position • Procedures – Fill appropriate size whirlpool with cold water and flaked ice with temp. at 50° to 60° F – Use for massaging action © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
– Most intense application of cryotherapy • Inability to develop thermopane (insulating layer of water) due to water turbulence • Convection provides for continuous circulation of cold water • Results in significantly longer periods of temp. reduction following treatment • Additional care must be used with total body immersion • With increased treatment area systemic effects are possible – Equipment maintenance and cleaning are critical © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
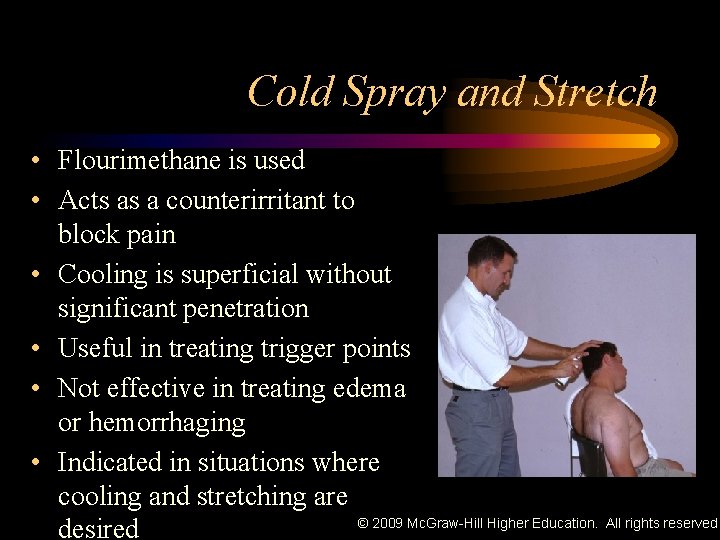
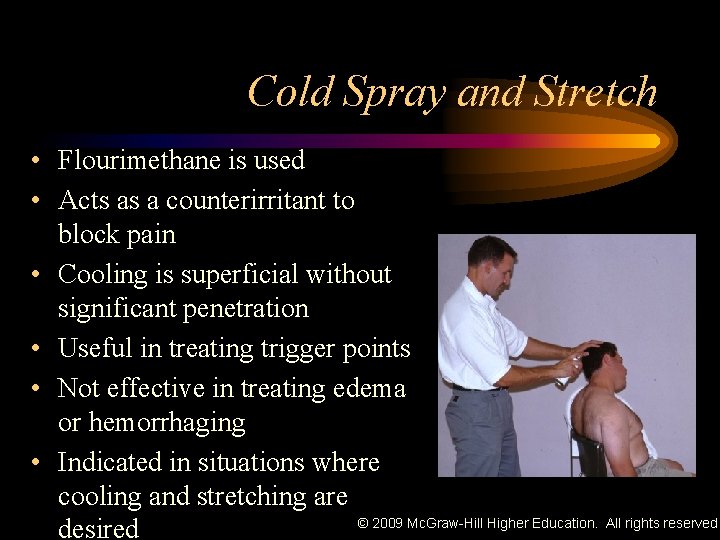
Cold Spray and Stretch • Flourimethane is used • Acts as a counterirritant to block pain • Cooling is superficial without significant penetration • Useful in treating trigger points • Not effective in treating edema or hemorrhaging • Indicated in situations where cooling and stretching are © 2009 Mc. Graw-Hill Higher Education. All rights reserved. desired
• Procedure – Spraying technique • Same direction, even sweeps • Work proximal to distal • For trigger points, work from point to referred pain area • Affected muscles should be sprayed from the affected area to the insertion • Static stretching can be incorporated as you spray © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
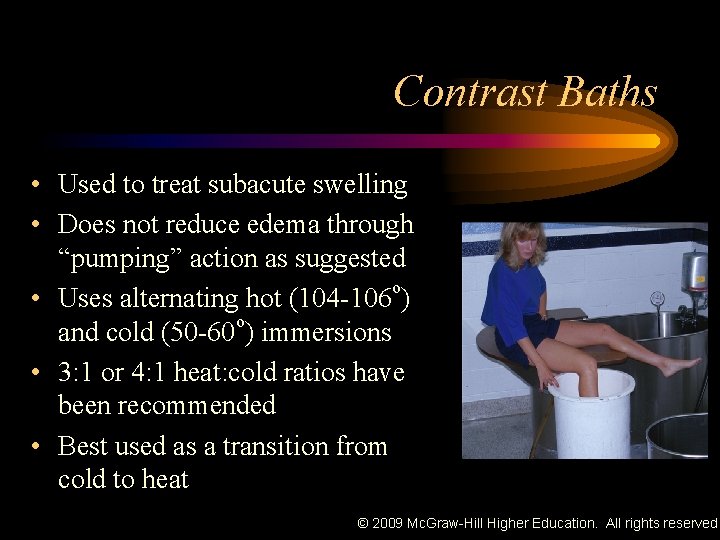
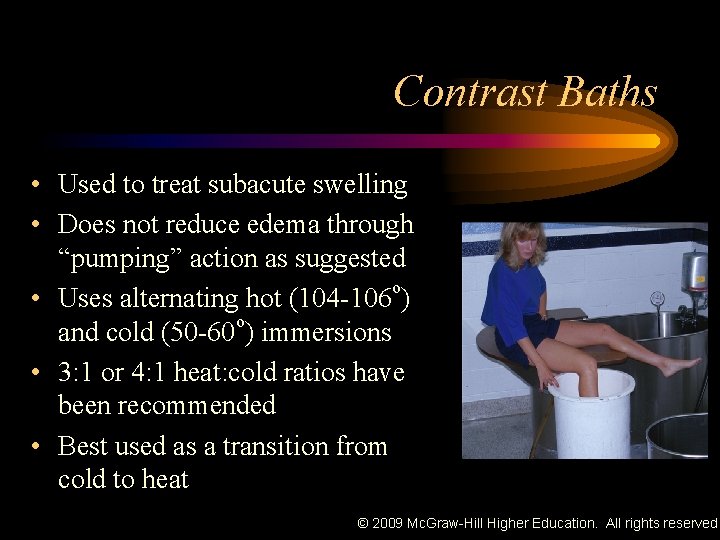
Contrast Baths • Used to treat subacute swelling • Does not reduce edema through “pumping” action as suggested • Uses alternating hot (104 -106 o) o and cold (50 -60 ) immersions • 3: 1 or 4: 1 heat: cold ratios have been recommended • Best used as a transition from cold to heat © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
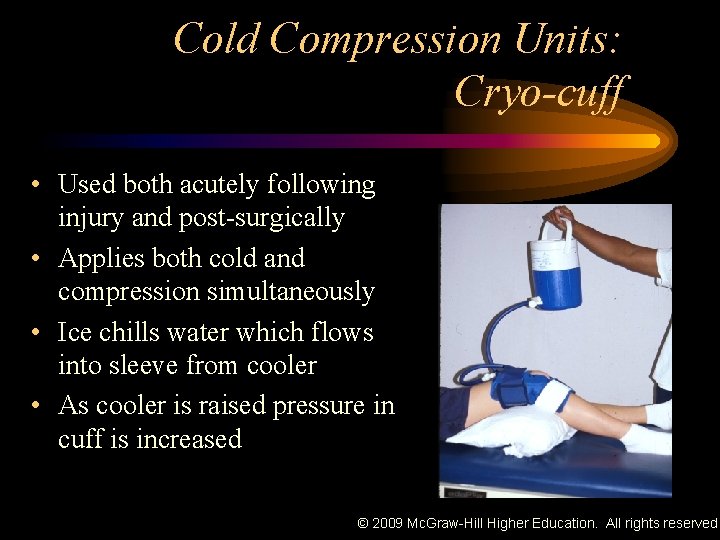
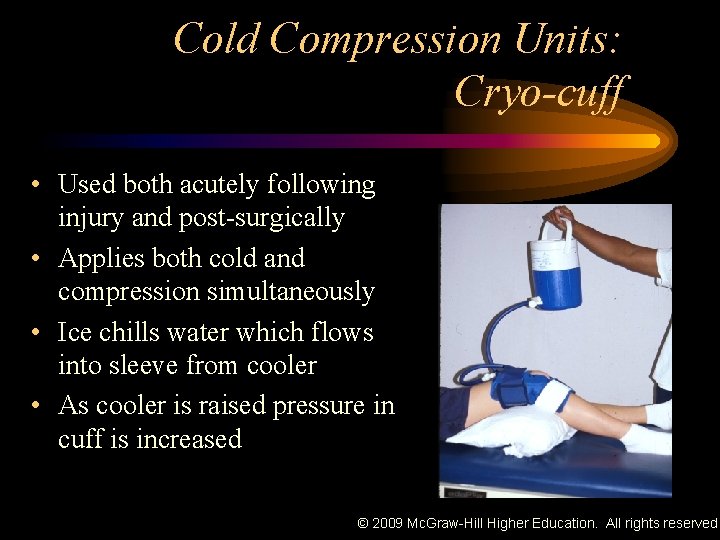
Cold Compression Units: Cryo-cuff • Used both acutely following injury and post-surgically • Applies both cold and compression simultaneously • Ice chills water which flows into sleeve from cooler • As cooler is raised pressure in cuff is increased © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Cryokinetics • Combines cryotherapy with exercise • Goal is to numb injured part (12 -20 min) then work toward achieving normal ROM through progressive active exercise • Numbness usually last for 3 -5 min. at which point ice is reapplied for 3 -5 minutes until numbness returns – Can be repeated five times • Exercises should be pain free and progressive in intensity concentrating on both flexibility and © 2009 Mc. Graw-Hill Higher Education. All rights reserved. strength
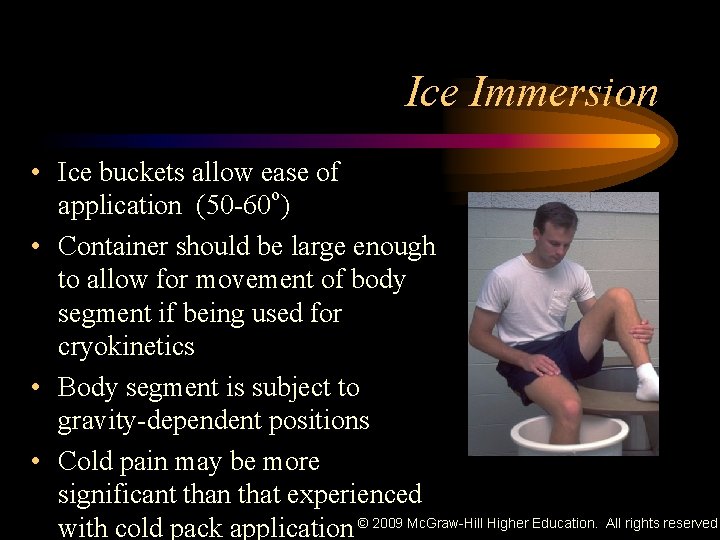
Ice Immersion • Ice buckets allow ease of application (50 -60 o) • Container should be large enough to allow for movement of body segment if being used for cryokinetics • Body segment is subject to gravity-dependent positions • Cold pain may be more significant than that experienced with cold pack application © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
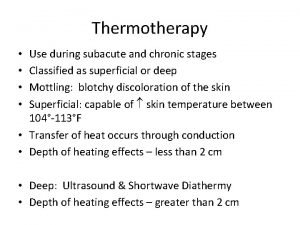
Thermotherapy: Physiologic Effects of Tissue Heating • Local superficial heating (infrared heat) is recommended in subacute conditions for reducing pain and inflammation through analgesic effects • During later stages of healing a deeper heating effect is desirable and should be achieved using the diathermies or ultrasound © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Thermotherapy Physiologic Effects of Tissue Heating • Increase in temperature increases metabolism – 13% increase in metabolism for each 1° C • Superficial heat vasodilates vessels, which increases capillary blood flow thus increasing tendency toward formation of edema – In mild or moderate inflammation increased capillary blood flow causes an increase in supply of oxygen, antibodies, leukocytes, and other nutrients and enzymes, along with clearing of metabolites © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Thermotherapy Physiologic Effects of Tissue Heating • Used to produce an analgesic effect through gate control – Most frequent indication for the use • Heat is applied in musculoskeletal and neuromuscular disorders • Increases the elasticity and decreases the viscosity of connective tissue © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Thermotherapy Physiologic Effects of Tissue Heating • Produces a relaxation effect and a reduction in muscle guarding by: – Relieving pain – Lessening hypertonicity of muscles – Producing sedation – Decreasing spasticity, tenderness, and spasm – Decreasing tightness in muscles and related structures © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Thermotherapy Physiologic Effects of Tissue Heating • Primary goals of thermotherapy include – Increased blood flow – Increased muscle temperature to stimulate analgesia – Increased nutrition to the damaged cells – Reduction of edema – Removal of metabolites and other products of inflammatory process © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Thermotherapy Techniques • • • Warm Whirlpool Hydrocollator Packs Paraffin Bath Infrared Lamps Fluidotherapy © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
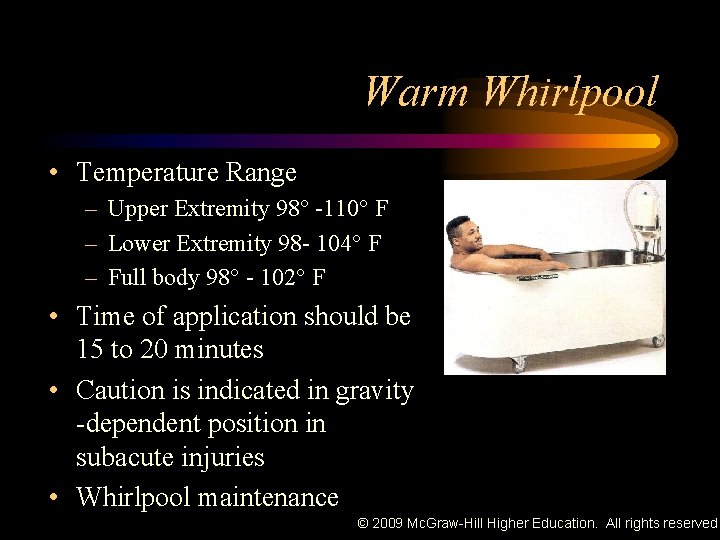
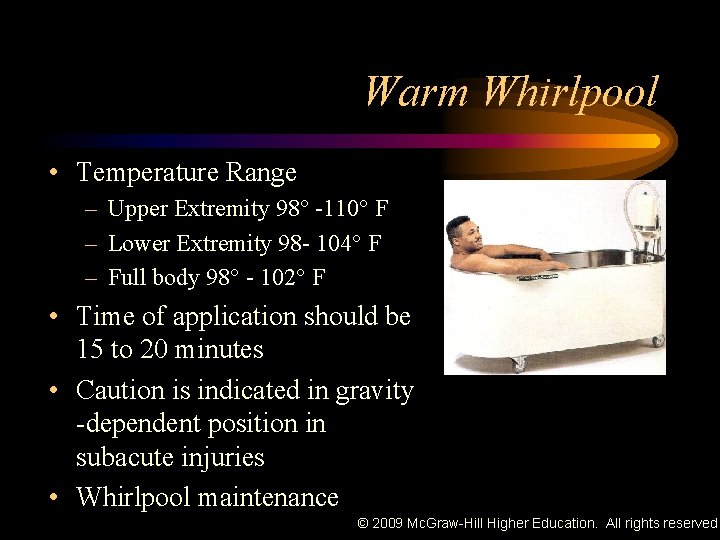
Warm Whirlpool • Temperature Range – Upper Extremity 98° -110° F – Lower Extremity 98 - 104° F – Full body 98° - 102° F • Time of application should be 15 to 20 minutes • Caution is indicated in gravity -dependent position in subacute injuries • Whirlpool maintenance © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Warm Whirlpool • Provides massaging effect and will stimulate circulation – Monitor for changes in edema • Excellent post-surgical modality – Increases systemic blood flow and mobilization of body part • Also noted to be one of the most abused clinical modalities © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
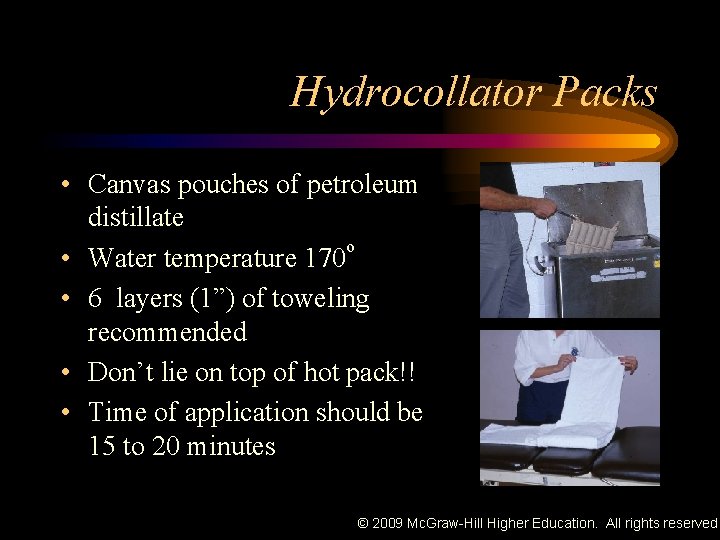
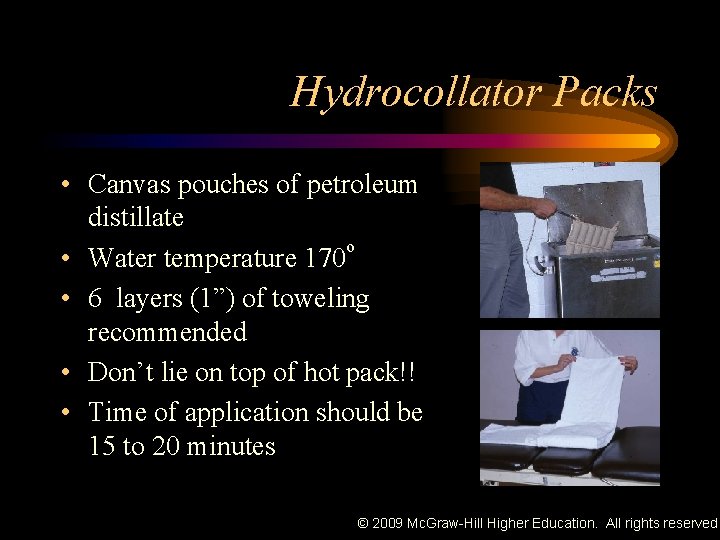
Hydrocollator Packs • Canvas pouches of petroleum distillate o • Water temperature 170 • 6 layers (1”) of toweling recommended • Don’t lie on top of hot pack!! • Time of application should be 15 to 20 minutes © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Paraffin Baths • Mixture ratio of paraffin to mineral oil (2 lbs : 1 gallon) • Mineral oil reduces temp of the paraffin to 126° F • Extremity dipped into paraffin for a couple of seconds then removed to allow paraffin to harden © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Paraffin Bath • Repeat until 6 layers have accumulated • Wrap in a plastic bag with several layers of toweling • Must exercise caution with use to reduce chance of burning patient © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
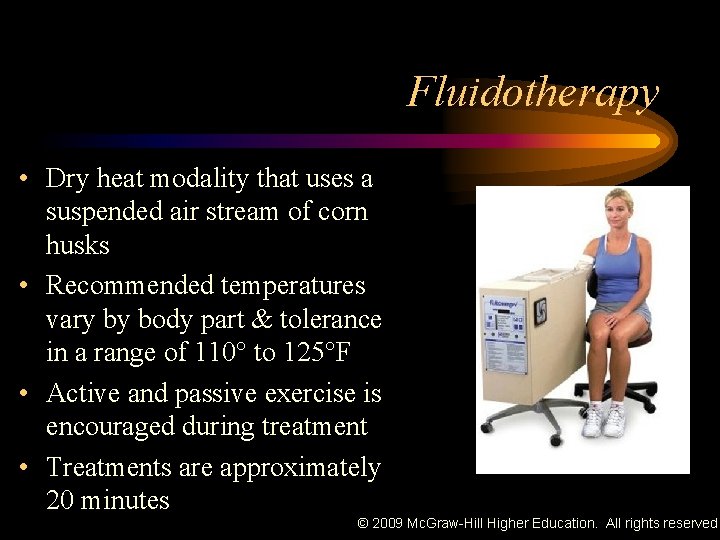
Fluidotherapy • Dry heat modality that uses a suspended air stream of corn husks • Recommended temperatures vary by body part & tolerance in a range of 110° to 125°F • Active and passive exercise is encouraged during treatment • Treatments are approximately 20 minutes © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Fluidotherapy • Medium allows for much higher treatment temperatures – Skin irritation and thermal shock limited as well – Mechano- and thermoreceptor stimulation reduces pain sensitivity (counterirritation) • Pressure may assist with edema reduction • Increases blood flow, sedates blood pressure, accelerates © 2009 Mc. Graw-Hill Higher Education. All rights reserved. biochemical reactions
Therma. Care Wraps • Cloth like material that conforms to body • Contains iron, charcoal, table salt and water that heat up when exposed to oxygen • Shown to be effective in increasing tissue temp. up to 2 cm © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Infrared Lamps • Superficial tissue temperature can be increased even though unit does not touch patient • Seldom used because of limited depth of skin penetration (<1 mm) • Moist towels should cover the area to be treated • Distance from treatment area to lamp should be adjusted according to treatment time • 20 inches = 20 minutes © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
Infrared Lamps • Luminous and non-luminous infrared lamps are classified as electromagnetic energy modalities – Effects on tissue temperature are not related to conduction • Non-luminous – Metal coil wrapped around core of non-conducting material • No longer used • Luminous – Tungsten filament and quartz red lamps © 2009 Mc. Graw-Hill Higher Education. All rights reserved.

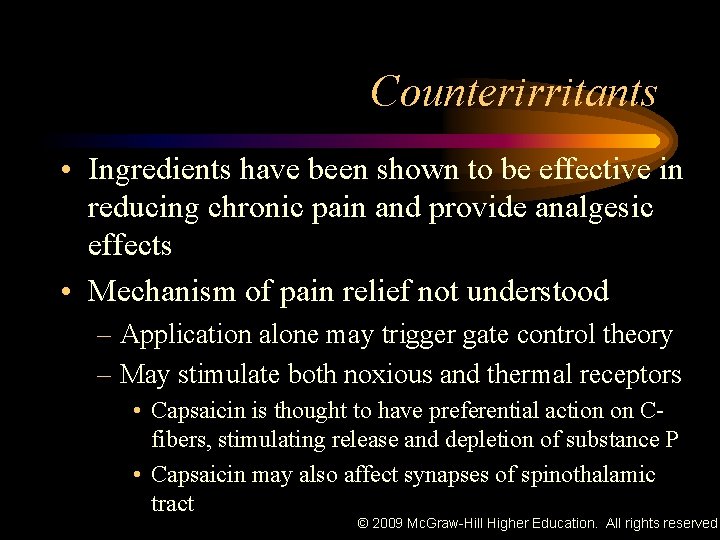
Counterirritants • Not classified as infrared modalities • Topically applied ointments that chemically stimulate sensory receptors of the skin • Contains – Menthol – Methyl salicylate – Camphor – Capsaicin © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
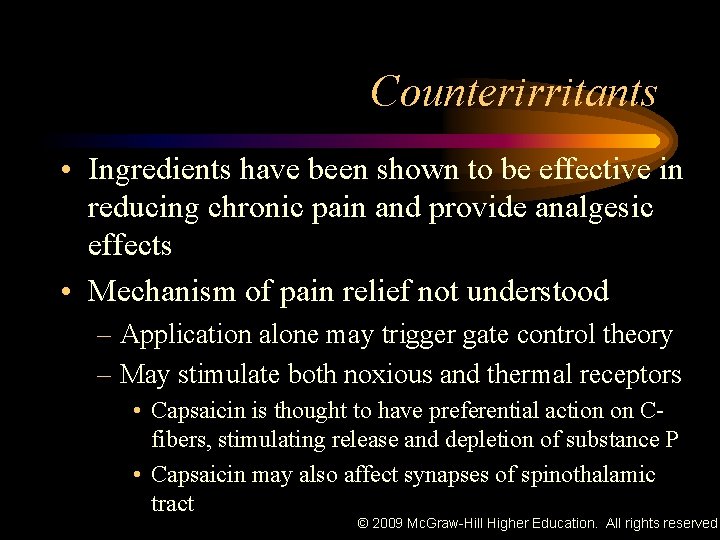
Counterirritants • Ingredients have been shown to be effective in reducing chronic pain and provide analgesic effects • Mechanism of pain relief not understood – Application alone may trigger gate control theory – May stimulate both noxious and thermal receptors • Capsaicin is thought to have preferential action on Cfibers, stimulating release and depletion of substance P • Capsaicin may also affect synapses of spinothalamic tract © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
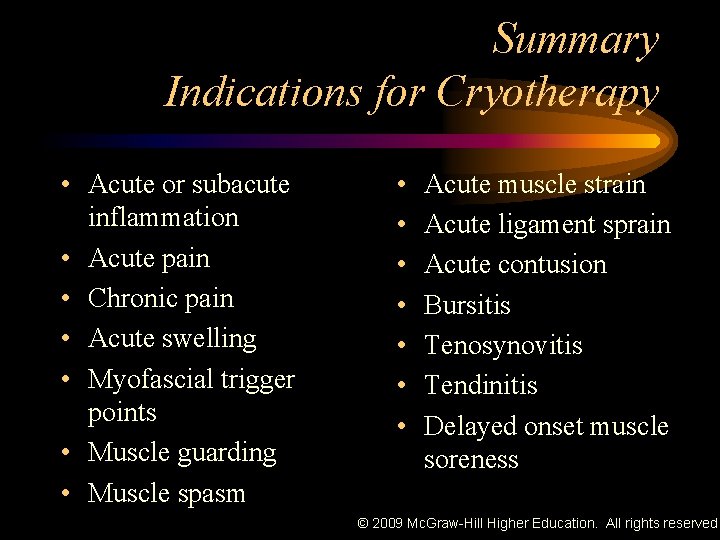
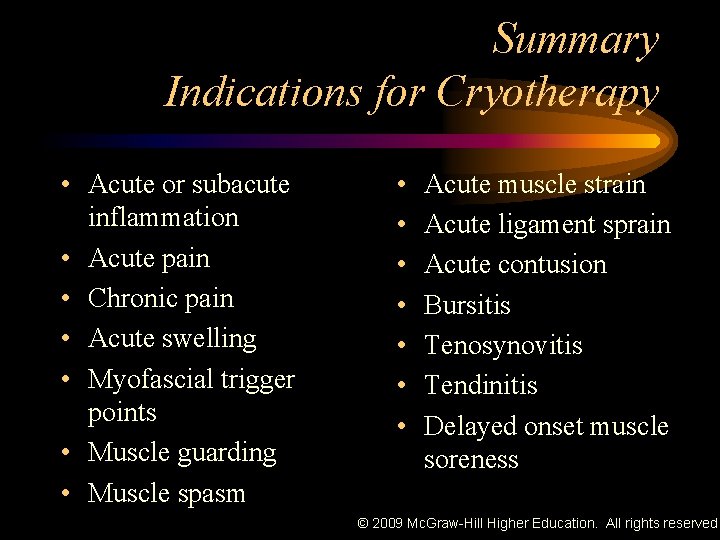
Summary Indications for Cryotherapy • Acute or subacute inflammation • Acute pain • Chronic pain • Acute swelling • Myofascial trigger points • Muscle guarding • Muscle spasm • • Acute muscle strain Acute ligament sprain Acute contusion Bursitis Tenosynovitis Tendinitis Delayed onset muscle soreness © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
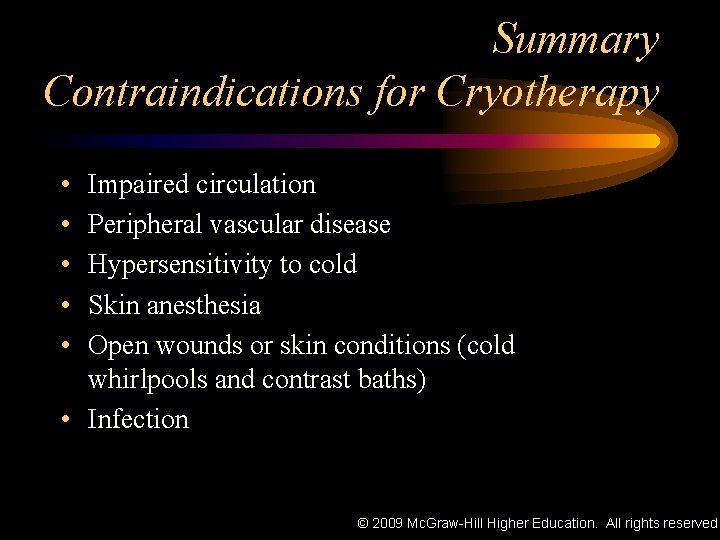
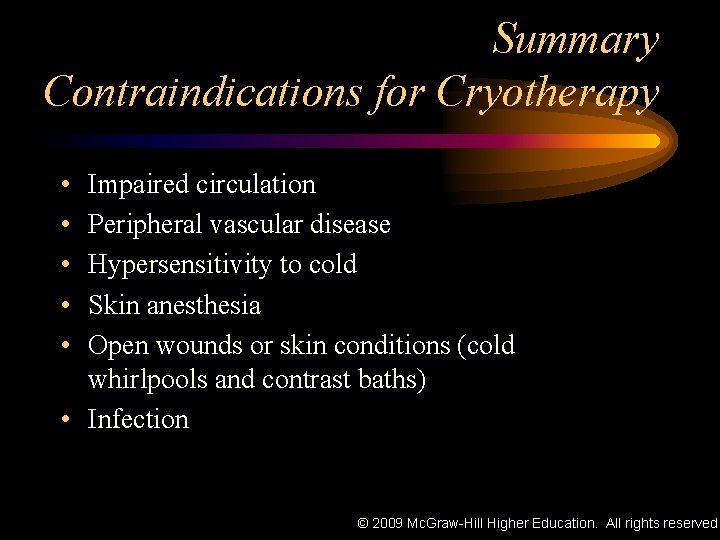
Summary Contraindications for Cryotherapy • • • Impaired circulation • Peripheral vascular disease Hypersensitivity to cold Skin anesthesia Open wounds or skin conditions (cold whirlpools and contrast baths) • Infection © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
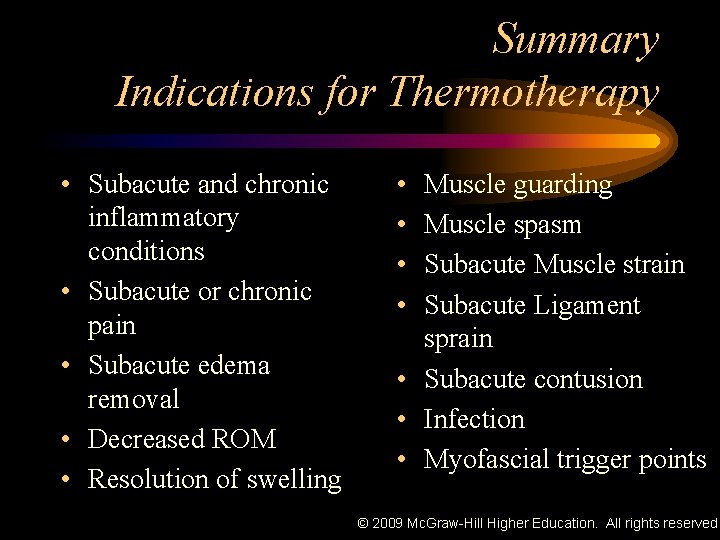
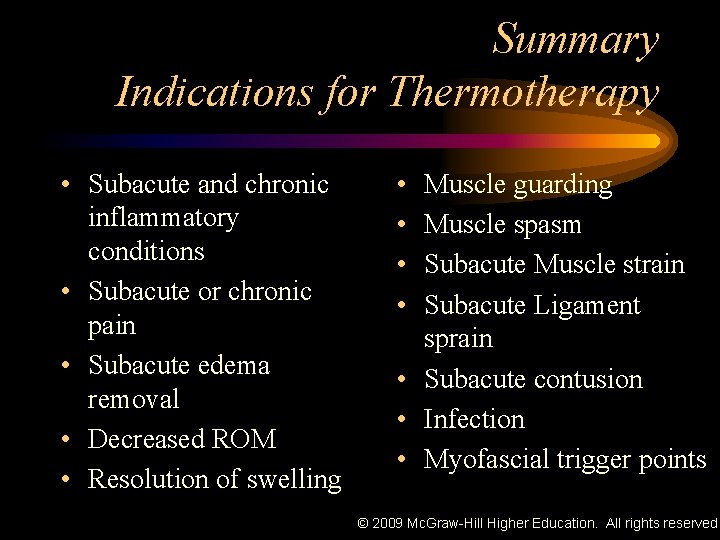
Summary Indications for Thermotherapy • Subacute and chronic inflammatory conditions • Subacute or chronic pain • Subacute edema removal • Decreased ROM • Resolution of swelling • • Muscle guarding Muscle spasm Subacute Muscle strain Subacute Ligament sprain • Subacute contusion • Infection • Myofascial trigger points © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
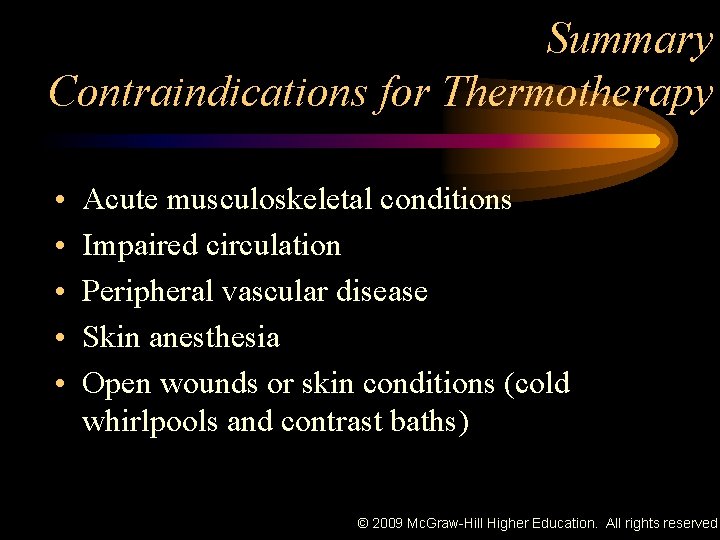
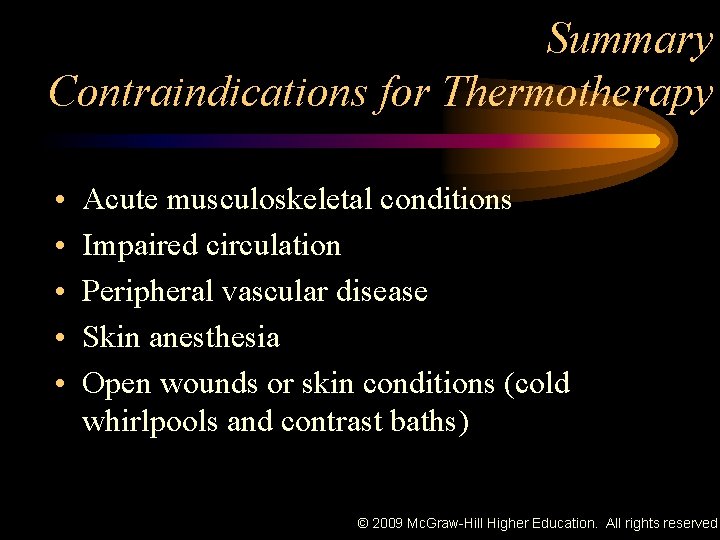
Summary Contraindications for Thermotherapy • • • Acute musculoskeletal conditions • Impaired circulation Peripheral vascular disease Skin anesthesia Open wounds or skin conditions (cold whirlpools and contrast baths) © 2009 Mc. Graw-Hill Higher Education. All rights reserved.
 Rich stanek bio
Rich stanek bio Chapter 41 musculoskeletal care modalities
Chapter 41 musculoskeletal care modalities Thermotherapy indications
Thermotherapy indications Vidian nerve cryotherapy
Vidian nerve cryotherapy Cryotherapy fisioterapi
Cryotherapy fisioterapi Thermotherapy types
Thermotherapy types Superficial and deep heating modalities
Superficial and deep heating modalities Cervical strain
Cervical strain Thermal modalities
Thermal modalities Mechanical modalities
Mechanical modalities Tatiana yugay
Tatiana yugay Infrared touch screen advantages and disadvantages
Infrared touch screen advantages and disadvantages Infrared vs bluetooth
Infrared vs bluetooth Infrared vs bluetooth
Infrared vs bluetooth Pengertian infrared
Pengertian infrared Nir spectroscopy instrumentation
Nir spectroscopy instrumentation Bill nye light
Bill nye light Infrared spektroskopisi
Infrared spektroskopisi Ethyl benzoate ir
Ethyl benzoate ir What is an infrared thermometer best used for servsafe
What is an infrared thermometer best used for servsafe Shortwave infrared camera
Shortwave infrared camera Bluetooth vs infrared
Bluetooth vs infrared Kuas infrared panel
Kuas infrared panel Infrared radiation discovery
Infrared radiation discovery Infrared spectroscopy theory
Infrared spectroscopy theory Infrared spectroscopy ppt
Infrared spectroscopy ppt Thermal infrared
Thermal infrared Thermal infrared
Thermal infrared National infrared operations
National infrared operations Ir spectroscopy instrumentation
Ir spectroscopy instrumentation Wide field infrared survey explorer
Wide field infrared survey explorer Electromagnetic wave carry
Electromagnetic wave carry Infrared radiation hazards
Infrared radiation hazards Infrared sensor principle
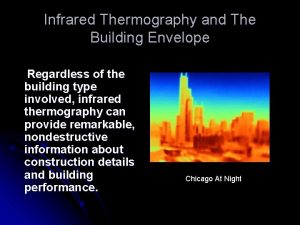
Infrared sensor principle Infrared building envelope
Infrared building envelope Made up school
Made up school Catalytic heater oil and gas
Catalytic heater oil and gas Most general to most specific classification
Most general to most specific classification Most general to most specific classification
Most general to most specific classification What is the world record for reading words per minute
What is the world record for reading words per minute The most
The most Beneficent pronunciation
Beneficent pronunciation Guddi baji
Guddi baji This is the study of grouping and naming organisms
This is the study of grouping and naming organisms Arrangement of organisms
Arrangement of organisms In the name of god most gracious prayer
In the name of god most gracious prayer In the name of allah the most gracious the most merciful
In the name of allah the most gracious the most merciful In the name of allah most gracious most merciful in arabic
In the name of allah most gracious most merciful in arabic The most gracious
The most gracious Aqaid e islam
Aqaid e islam In the name of god the most gracious the most merciful
In the name of god the most gracious the most merciful In the name of allah the most beneficent
In the name of allah the most beneficent Most new-product ideas come from chapter 14
Most new-product ideas come from chapter 14 7 ionic and metallic bonding
7 ionic and metallic bonding Chapter 7 ionic and metallic bonding answer key
Chapter 7 ionic and metallic bonding answer key Properties of ionic bonds
Properties of ionic bonds Chapter 7 chapter assessment ionic compounds and metals
Chapter 7 chapter assessment ionic compounds and metals Chemical names and formulas chapter 9
Chemical names and formulas chapter 9 The simplest and most basic aerobic activity is
The simplest and most basic aerobic activity is Which profession do you like and why
Which profession do you like and why What is at the root of most arguments and many fights?
What is at the root of most arguments and many fights? Words are like leaves and where they most abound
Words are like leaves and where they most abound