Chapter 4 Life Cycle of an Insurance Claim
- Slides: 28
Chapter 4 Life Cycle of an Insurance Claim Copyright © 2008 Delmar Learning. All rights reserved.
Development of an Insurance Claim • CMS-1500 claim is used to report professional and technical services • Patient encounter form (or Superbill) is used to generate the provider’s claim for payment 2 Copyright © 2008 Delmar Learning. All rights reserved.
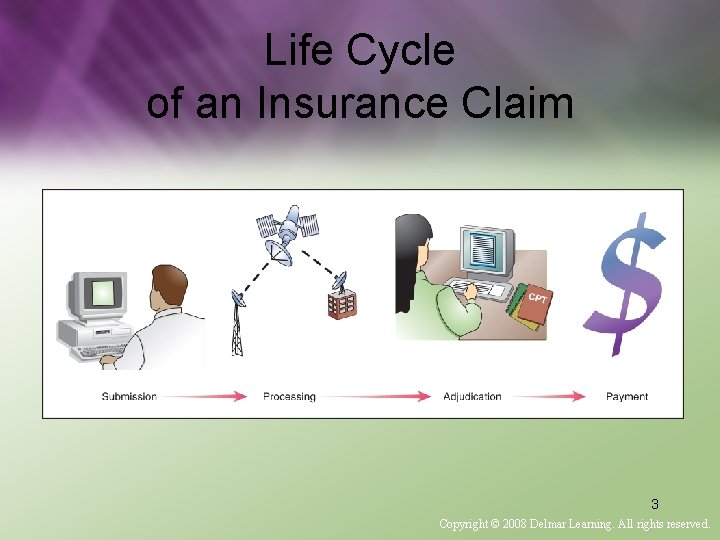
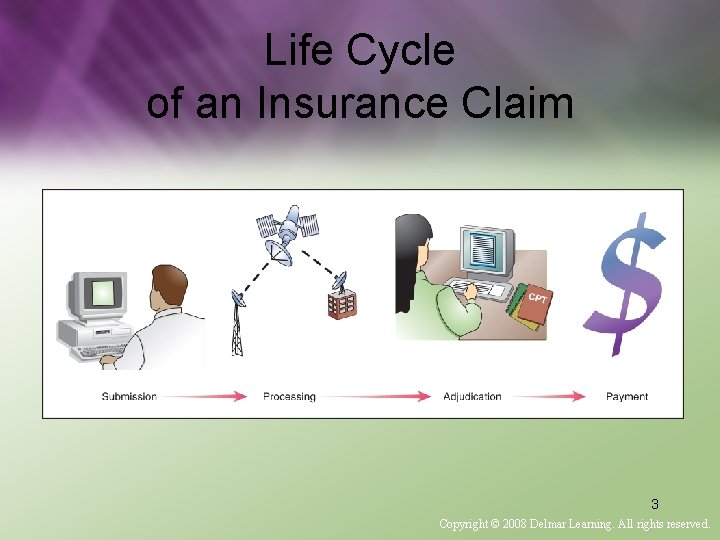
Life Cycle of an Insurance Claim 3 Copyright © 2008 Delmar Learning. All rights reserved.
Information to Claim • Information from the Superbill, patient record, or chart is then transferred to the CMS-1500 claim 4 Copyright © 2008 Delmar Learning. All rights reserved.
Accepting Assignment • When provider agrees to what the insurance company allows and or approves as payment 5 Copyright © 2008 Delmar Learning. All rights reserved.
Accepting Assignment • CMS-1500 claim: – Requires responses pertaining to patient’s condition and if related to employment, auto or any other accident, additional insurance coverage, or use of an outside laboratory. 6 Copyright © 2008 Delmar Learning. All rights reserved.
Accepting Assignment • Patient is responsible for co-payment and coinsurance amounts • “Signature on File” can be used as a substitute for patient’s signature, as long as real signature is on file. 7 Copyright © 2008 Delmar Learning. All rights reserved.
Accepting Assignment • Claim is proofread and double checked – Any supporting documents are copied from patient’s chart and attached to claim 8 Copyright © 2008 Delmar Learning. All rights reserved.
Managing New Patients • Office policy and procedures (paying copayments) – Should be explained and posted at receptionist desk • Determine whether appropriate office has been contacted – Then preregister new patients 9 Copyright © 2008 Delmar Learning. All rights reserved.
Managing New Patients • Patient must complete a patient registration form upon arrival • Make photocopy (front and back) of patient’s insurance card – File in patient’s financial record 10 Copyright © 2008 Delmar Learning. All rights reserved.
Managing New Patients • Contact payer – Confirm patient’s insurance information located on back of insurance card • Verify information with patient and/or subscriber – Make changes – Enter information using computer entry software 11 Copyright © 2008 Delmar Learning. All rights reserved.
Managing New Patients • Create a new medical record for the patient • Generate patient’s encounter form • Encounter form is a financial record that documents treated diagnoses and services 12 Copyright © 2008 Delmar Learning. All rights reserved.
Managing Established Patients • Schedule a return appointment when patient is checking out or when patient calls office • Verify all registration information • Encounter form needs to be generated for patient’s current visit 13 Copyright © 2008 Delmar Learning. All rights reserved.
Managing Office Finances • CPT and HCPCS level 2 (national) codes are assigned to procedures • Enter charges for services and/or procedures • Post charges to patient’s account • Collect payment from patient 14 Copyright © 2008 Delmar Learning. All rights reserved.
Managing Office Finances • • Post payment to patient’s account Complete insurance claim Attach documents that support the claim Obtain provider’s signature on claim if processed manually 15 Copyright © 2008 Delmar Learning. All rights reserved.
Managing Office Finances • File copies of the claim and attachments in the practice’s insurance files • Log completed claims in an insurance registry • Send claims by mail or electronically 16 Copyright © 2008 Delmar Learning. All rights reserved.
Appealing Denied Claims • Remittance advice indicates that the payment was denied for reasons other than a processing error 17 Copyright © 2008 Delmar Learning. All rights reserved.
Steps to Appeal Denial 1. Procedure or services should be reviewed from original documents for diagnostic supporting documentation – Research procedure and patient documentation when denied for “medical necessity. ” 18 Copyright © 2008 Delmar Learning. All rights reserved.
Steps to Appeal Denial 2. Determine if condition is pre-existing – If incorrect diagnosis code was submitted on original claim • Correct claim and resubmit 19 Copyright © 2008 Delmar Learning. All rights reserved.
Steps to Appeal Denial 3. Noncovered benefit – Determine if treatment submitted was excluded – If incorrect procedure code was submitted • Correct claim, resubmit, and attach copy of medical record documentation to support code change 20 Copyright © 2008 Delmar Learning. All rights reserved.
Steps to Appeal Denial 4. Termination of coverage – Contact patient – Determine current coverage – Authorization should be performed prior to service – If this was performed, submit with authorization number 21 Copyright © 2008 Delmar Learning. All rights reserved.
Steps to Appeal Denial 5. Failure to obtain preauthorization requests is a costly error for practice – Retrospective review of claims are more difficult or sometimes impossible to obtain 22 Copyright © 2008 Delmar Learning. All rights reserved.
Steps to Appeal Denial 6. Out of network providers – Write letter of appeal explaining why treatment was sought outside the provider network 23 Copyright © 2008 Delmar Learning. All rights reserved.
Steps to Appeal Denial 7. Provide letter of appeal explaining why higher level of care was required – Copies of patient’s chart may be needed for review by insurance adjudicator. 24 Copyright © 2008 Delmar Learning. All rights reserved.
Credit and Collections • • Delinquent claims and prevention Verify health insurance cards Determine each patient’s coverage Electronically submit a clean claim 25 Copyright © 2008 Delmar Learning. All rights reserved.
Credit and Collections • Contact payer to verify received claim • Review records to determine if claim is paid, denied, or pending • Submit supporting documents 26 Copyright © 2008 Delmar Learning. All rights reserved.
Claim Submission Problems, Descriptions, and Resolutions • • Coding errors Delinquent Denied Lost 27 Copyright © 2008 Delmar Learning. All rights reserved.
Claim Submission Problems, Descriptions, and Resolutions • Overpayment • Payment errors • Pending – Suspense • Rejected 28 Copyright © 2008 Delmar Learning. All rights reserved.
 Claim processing life cycle
Claim processing life cycle Example claim of value
Example claim of value Features of fire insurance
Features of fire insurance Short sales formula in insurance claim
Short sales formula in insurance claim Interrogating frequency claims
Interrogating frequency claims Example of
Example of Counterclaim paragraph examples
Counterclaim paragraph examples Chapter 14 health disability and life insurance
Chapter 14 health disability and life insurance Chapter 10 financial planning with life insurance
Chapter 10 financial planning with life insurance Chapter 5 principles of engine operation
Chapter 5 principles of engine operation Chapter 17 the beginning of the life cycle
Chapter 17 the beginning of the life cycle Chapter 19 section 2 the life cycle of stars answer key
Chapter 19 section 2 the life cycle of stars answer key Ricb bhutan
Ricb bhutan Desjardins life insurance
Desjardins life insurance Gcu annuity
Gcu annuity Life insurance customer journey map
Life insurance customer journey map Climbs insurance logo
Climbs insurance logo Icuba benefits
Icuba benefits Bmo insurance auto
Bmo insurance auto Life insurance review letter
Life insurance review letter Cfglife login
Cfglife login Byu student alumni
Byu student alumni State life insurance table 03
State life insurance table 03 Life insurance contractual provisions
Life insurance contractual provisions Ethos life insurance bbb
Ethos life insurance bbb State life bonus rate 2020
State life bonus rate 2020 Loss assessor leicester
Loss assessor leicester Whole life insurance
Whole life insurance Jervey eye group patient portal
Jervey eye group patient portal