Chapter 4 Epithelial tissue Tissues Cells work together
- Slides: 63
Chapter 4: Epithelial tissue
Tissues § § Cells work together in functionally related groups called tissues Types of tissues: 1. Epithelial – protection, secretions 2. Connective – support , protections 3. Muscle – movement 4. Nervous – control
Epithelial Tissue The Characteristics & Form §Epithelial membranes are avascular, deriving their nutrients by diffusion from blood vessels in the adjacent connective tissues. These membranes can: • cover a surface, • line a cavity, or • line a tube. §Closely aggregated polyhedral cells. § Very little extracellular matrix. § plenty of intercellular junctions and strong adhesion.
Epithelial Tissue The Characteristics & Form §Functions of epithelium: • Protection • Absorption • Secretion • Sensation • Contractility • Everything enter the body must cross the epithelium.
Epithelial Tissue The Characteristics & Form §The forms and dimensions of epithelial cells range from: high columnar to cuboidal to low squamous cells. §Their common polyhedral form results from their close juxtaposition in cellular layers or masses. §Cells nuclei form correspond roughly to the cell shape. Varying from spherical to elongated or elliptic. §The long axis of the nucleus is always parallel to the main axis of the cell
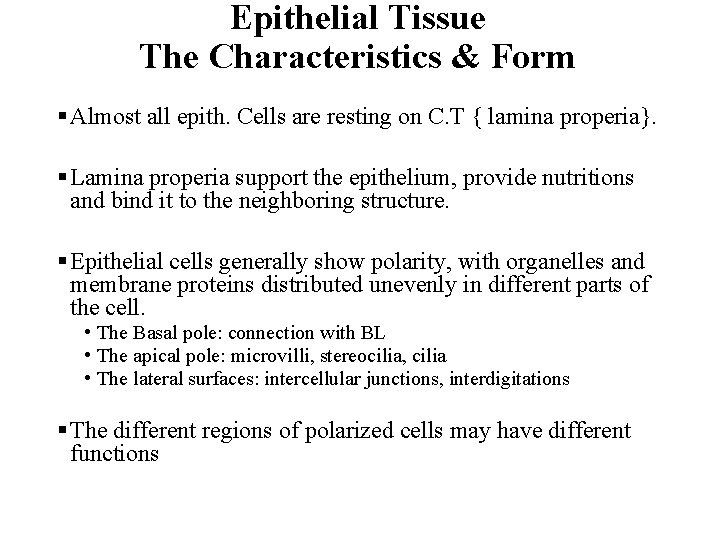
Epithelial Tissue The Characteristics & Form § Almost all epith. Cells are resting on C. T { lamina properia}. § Lamina properia support the epithelium, provide nutritions and bind it to the neighboring structure. § Epithelial cells generally show polarity, with organelles and membrane proteins distributed unevenly in different parts of the cell. • The Basal pole: connection with BL • The apical pole: microvilli, stereocilia, cilia • The lateral surfaces: intercellular junctions, interdigitations § The different regions of polarized cells may have different functions
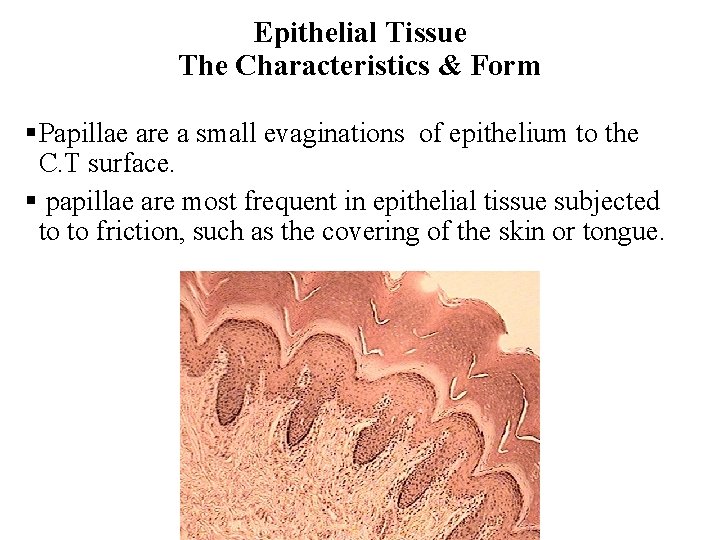
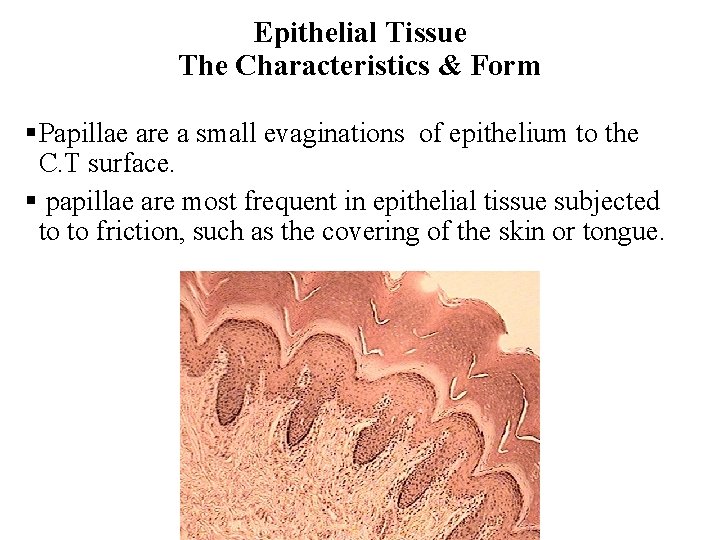
Epithelial Tissue The Characteristics & Form §Papillae are a small evaginations of epithelium to the C. T surface. § papillae are most frequent in epithelial tissue subjected to to friction, such as the covering of the skin or tongue.
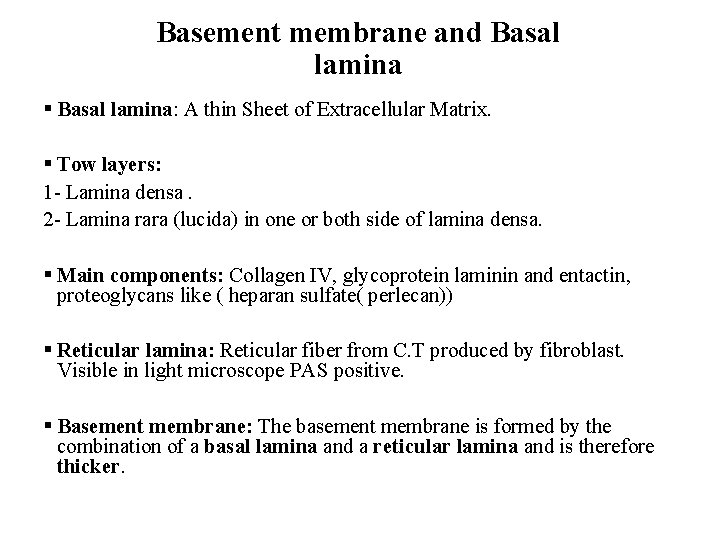
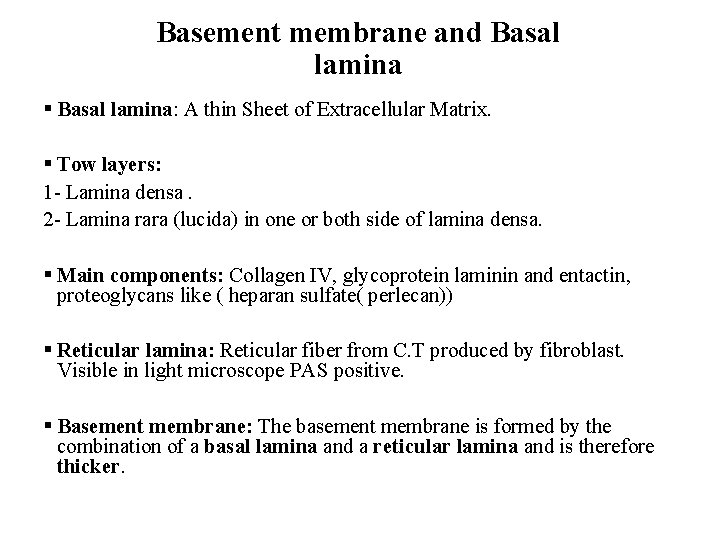
Basement membrane and Basal lamina § Basal lamina: A thin Sheet of Extracellular Matrix. § Tow layers: 1 - Lamina densa. 2 - Lamina rara (lucida) in one or both side of lamina densa. § Main components: Collagen IV, glycoprotein laminin and entactin, proteoglycans like ( heparan sulfate( perlecan)) § Reticular lamina: Reticular fiber from C. T produced by fibroblast. Visible in light microscope PAS positive. § Basement membrane: The basement membrane is formed by the combination of a basal lamina and a reticular lamina and is therefore thicker.
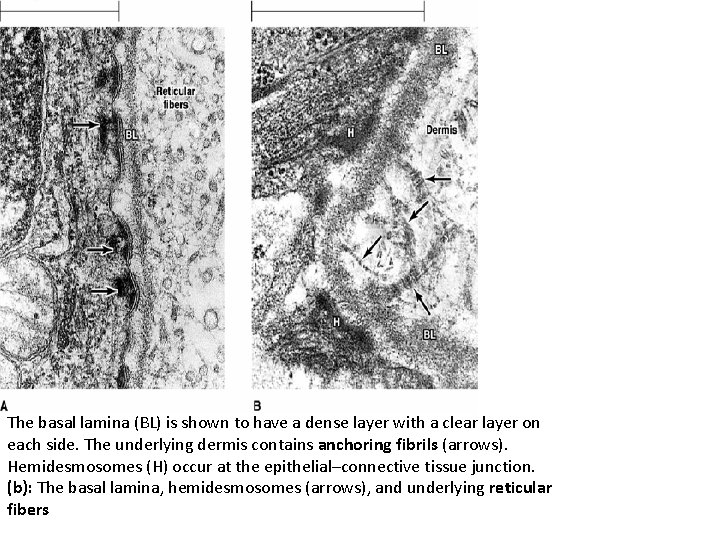
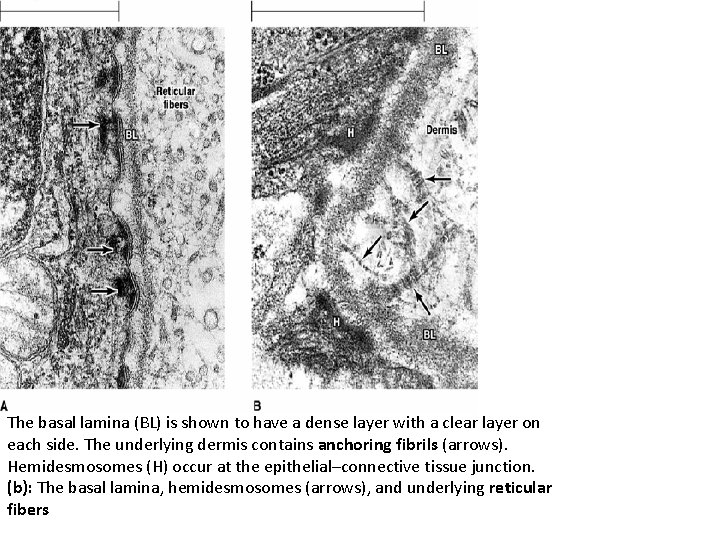
The basal lamina (BL) is shown to have a dense layer with a clear layer on each side. The underlying dermis contains anchoring fibrils (arrows). Hemidesmosomes (H) occur at the epithelial–connective tissue junction. (b): The basal lamina, hemidesmosomes (arrows), and underlying reticular fibers
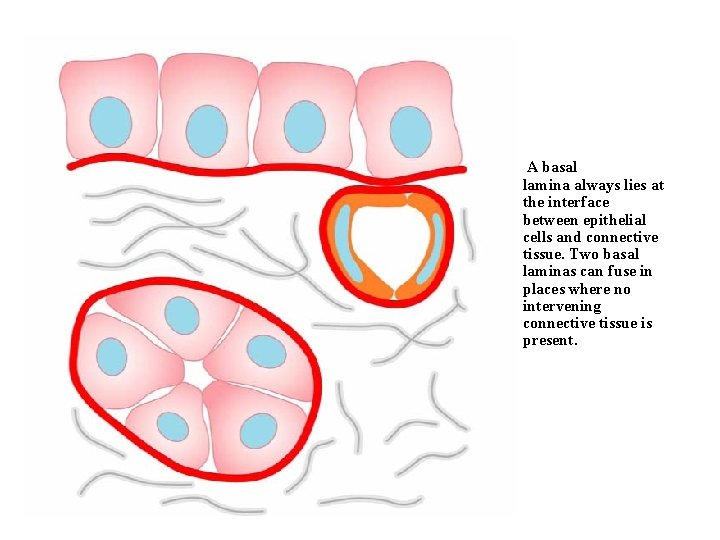
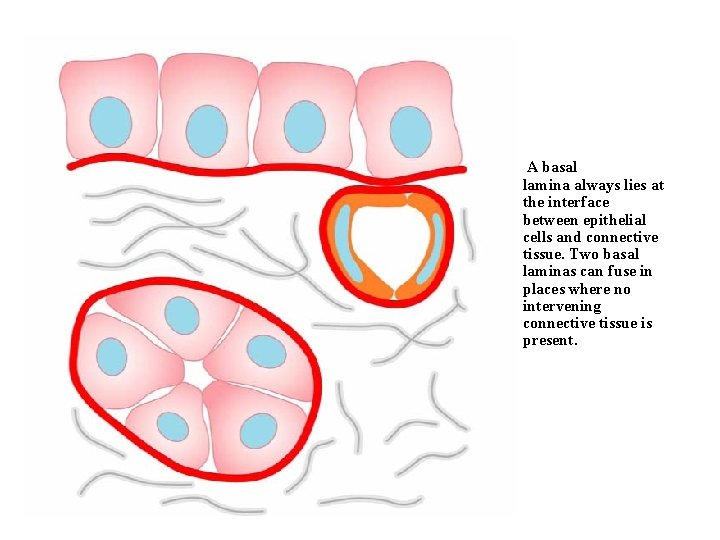
A basal lamina always lies at the interface between epithelial cells and connective tissue. Two basal laminas can fuse in places where no intervening connective tissue is present.
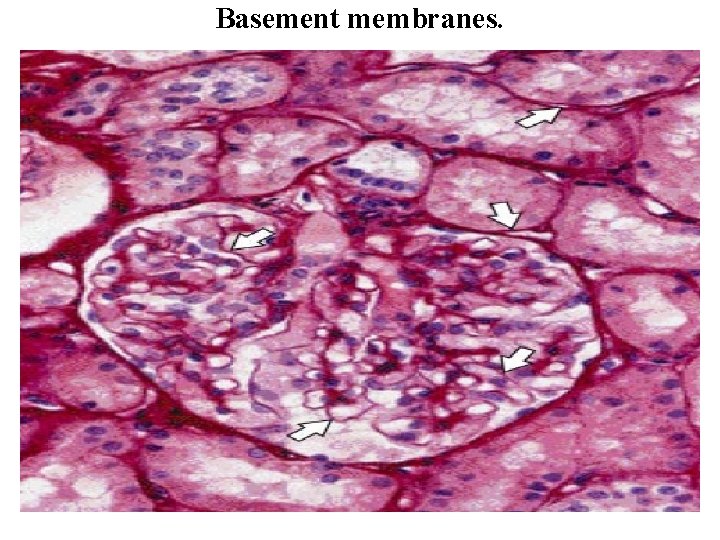
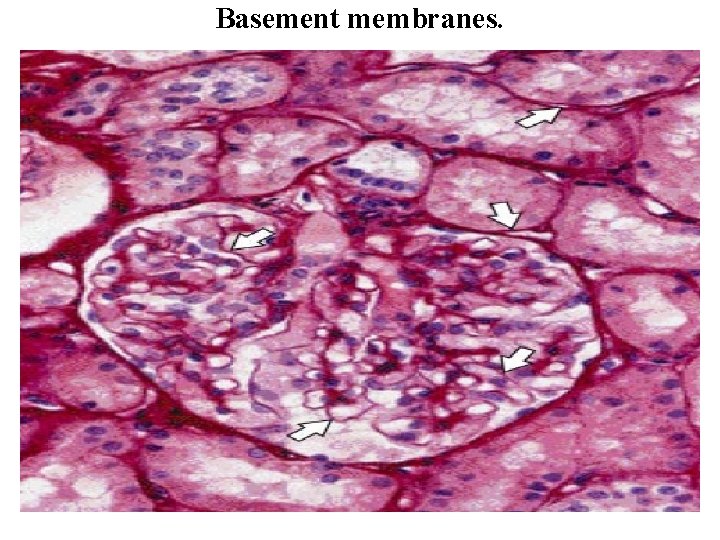
Basement membranes.
Function of basal lamina • Suporting • Barrier üregulate the exchange of macromolecules • Regulate cell proliferation and differentiation üby binding GF. • Influence cell polarity.
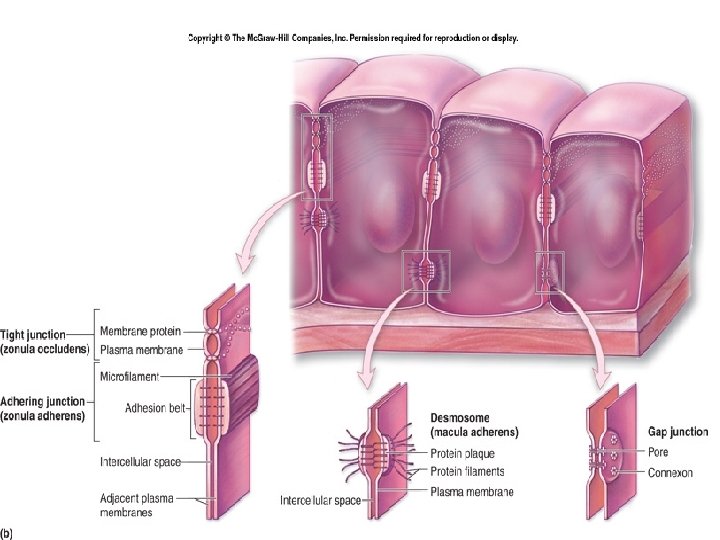
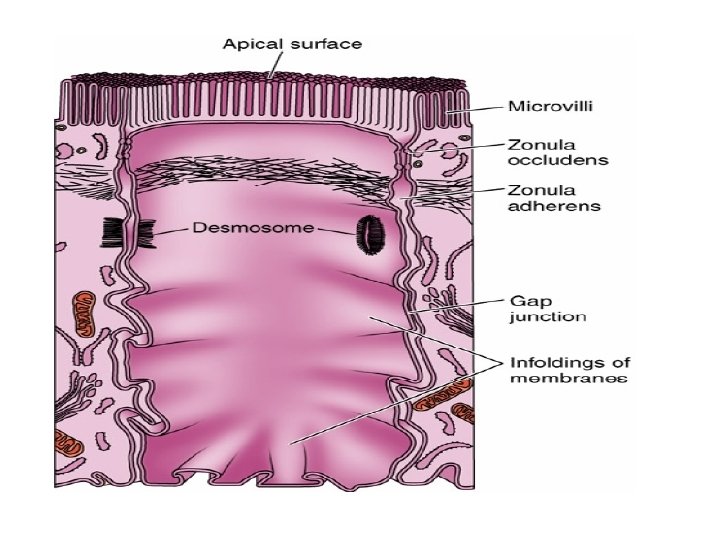
Intercellular Junctions § Several membrane-associated structures contribute to adhesion and communication between cells. § They are present in most tissues but are particularly numerous and prominent in epithelia. § Epithelial tissue strongly cohesive & strong mechanical forces necessary to separate them. § The lateral membranes of epithelial cells exhibit several specialized intercellular junctions. Various junctions serve to function as: • Seals to prevent the flow of materials between the cells (occluding junctions) • Sites of adhesion (adhesive or anchoring junctions) • Channels for communication between adjacent cells (gap junctions).
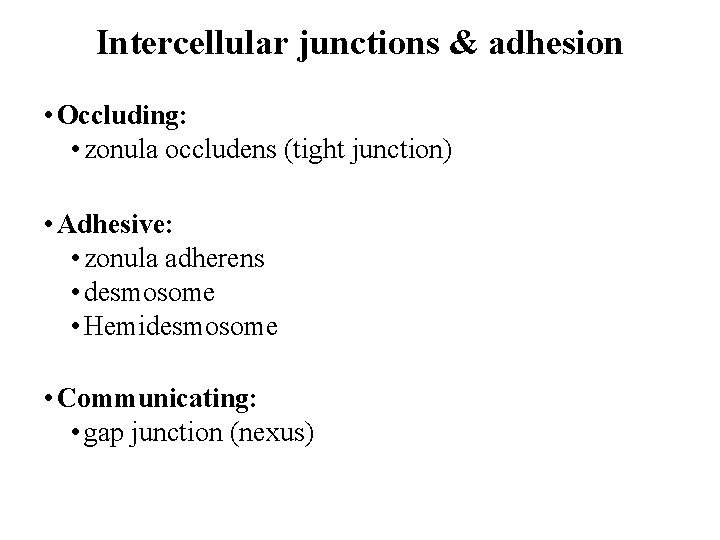
Intercellular junctions & adhesion • Occluding: • zonula occludens (tight junction) • Adhesive: • zonula adherens • desmosome • Hemidesmosome • Communicating: • gap junction (nexus)
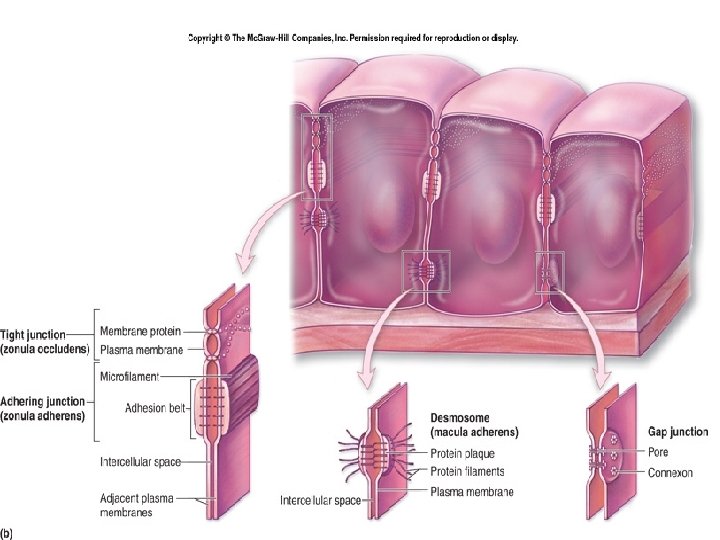
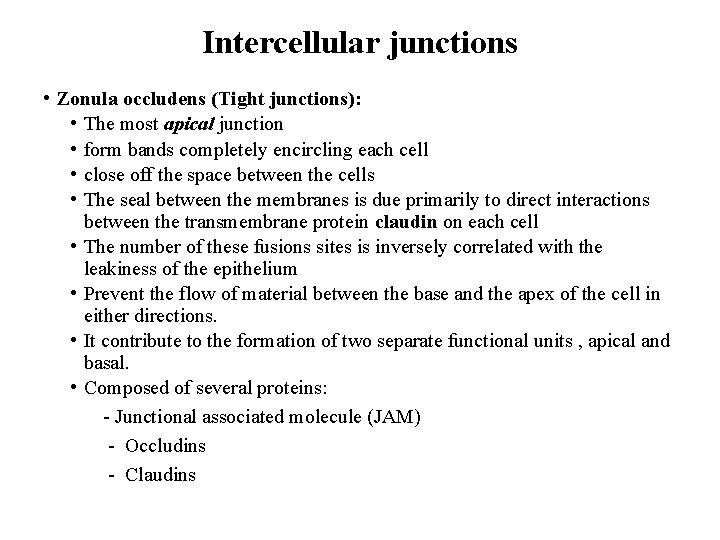
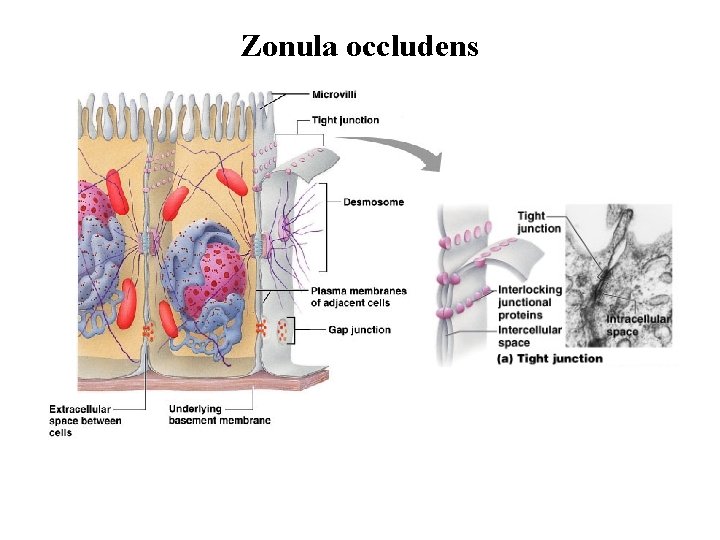
Intercellular junctions • Zonula occludens (Tight junctions): • The most apical junction • form bands completely encircling each cell • close off the space between the cells • The seal between the membranes is due primarily to direct interactions between the transmembrane protein claudin on each cell • The number of these fusions sites is inversely correlated with the leakiness of the epithelium • Prevent the flow of material between the base and the apex of the cell in either directions. • It contribute to the formation of two separate functional units , apical and basal. • Composed of several proteins: - Junctional associated molecule (JAM) - Occludins - Claudins
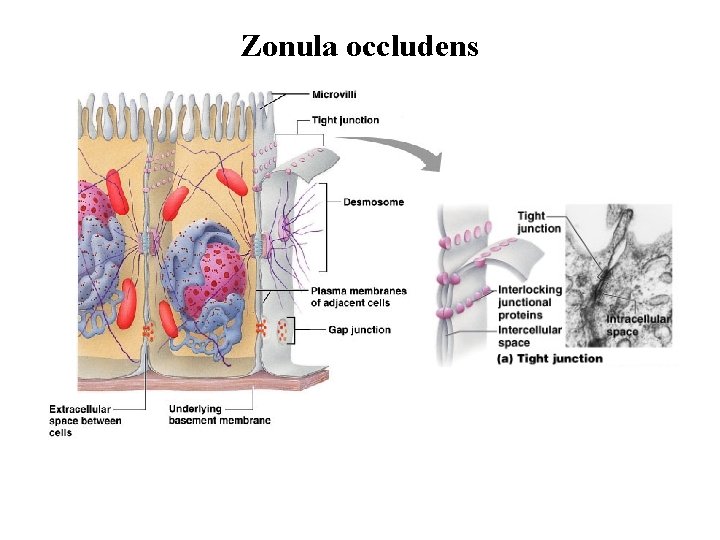
Zonula occludens
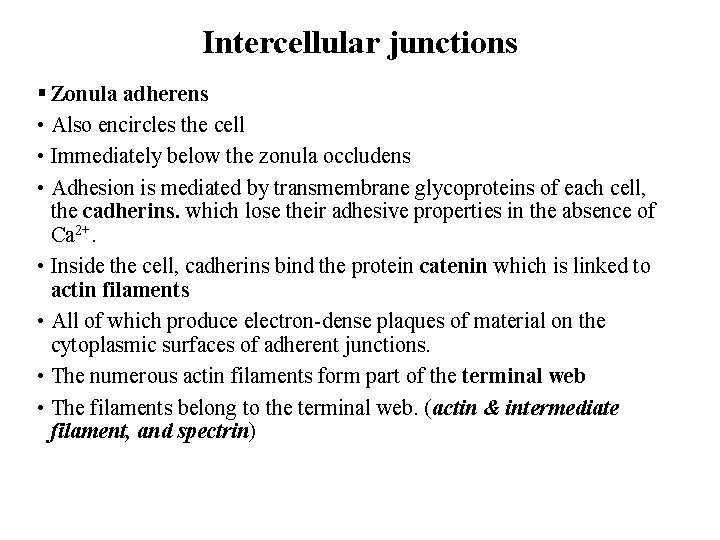
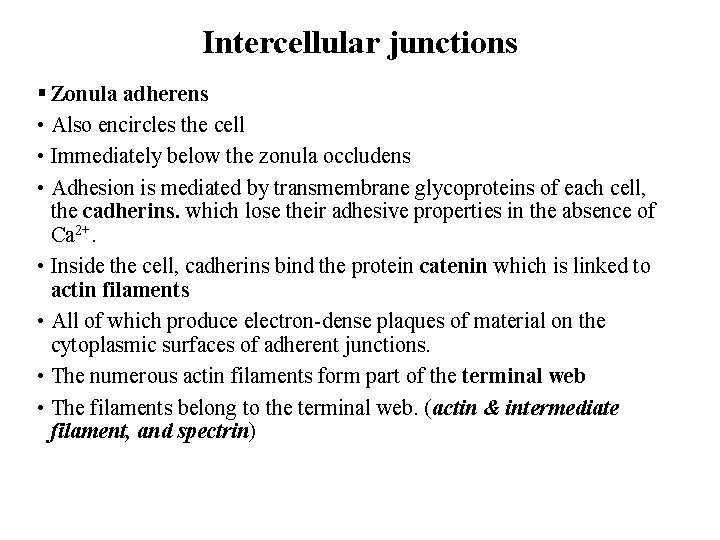
Intercellular junctions § Zonula adherens • Also encircles the cell • Immediately below the zonula occludens • Adhesion is mediated by transmembrane glycoproteins of each cell, the cadherins. which lose their adhesive properties in the absence of Ca 2+. • Inside the cell, cadherins bind the protein catenin which is linked to actin filaments • All of which produce electron-dense plaques of material on the cytoplasmic surfaces of adherent junctions. • The numerous actin filaments form part of the terminal web • The filaments belong to the terminal web. (actin & intermediate filament, and spectrin)
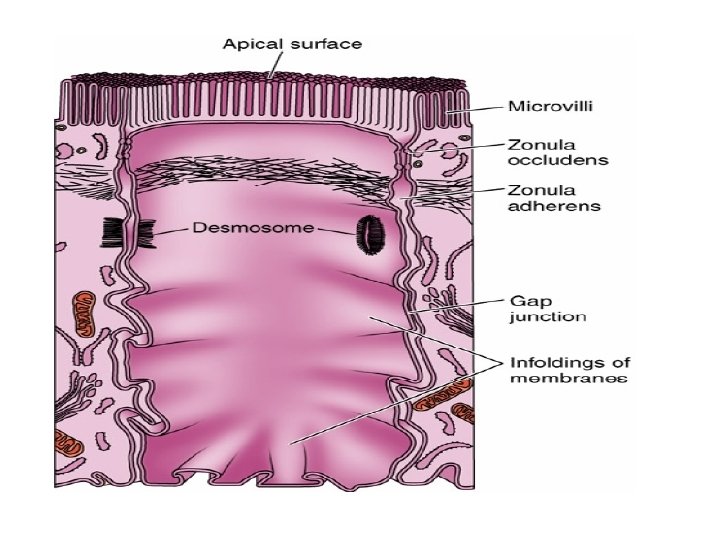
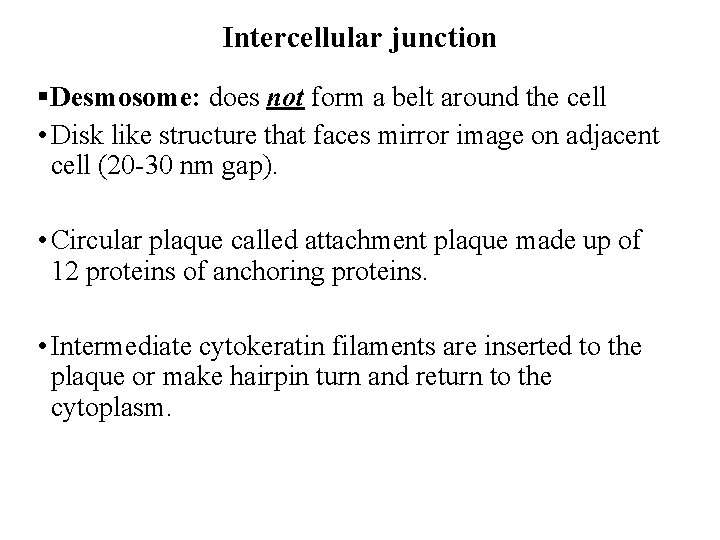
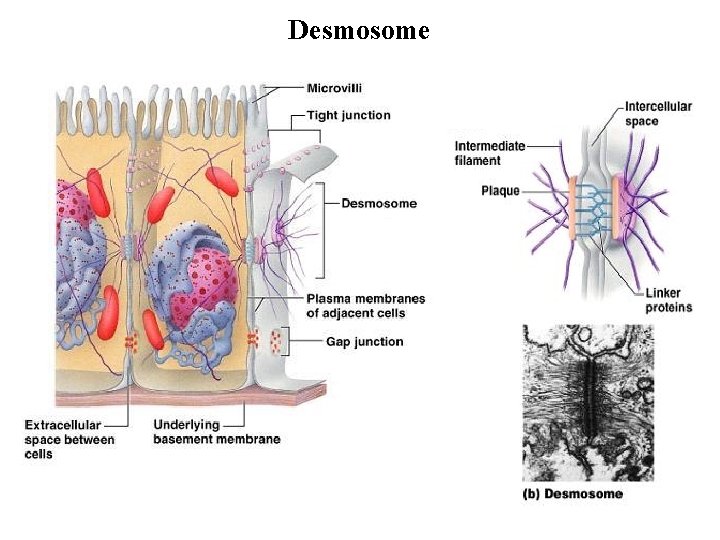
Intercellular junction §Desmosome: does not form a belt around the cell • Disk like structure that faces mirror image on adjacent cell (20 -30 nm gap). • Circular plaque called attachment plaque made up of 12 proteins of anchoring proteins. • Intermediate cytokeratin filaments are inserted to the plaque or make hairpin turn and return to the cytoplasm.
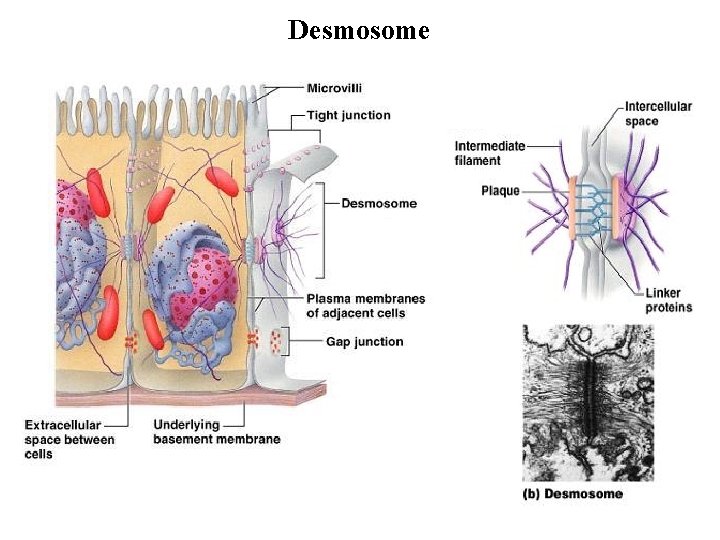
Desmosome
Intercellular junction § Hemidesmosome: • connection between cell and BL • Take the shape of half desmosome. • The attachment plaque contain mainly integrin not cadherin.
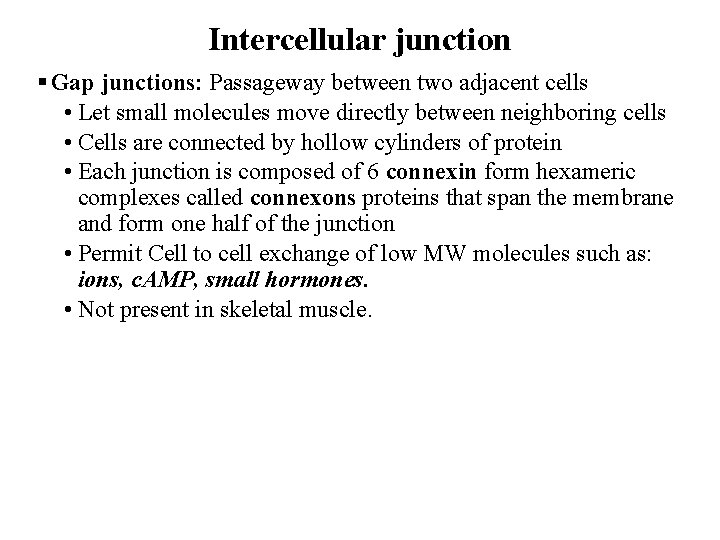
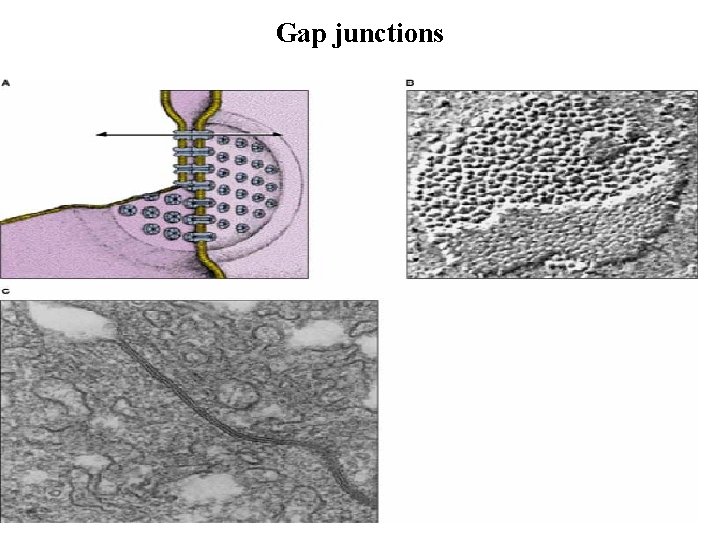
Intercellular junction § Gap junctions: Passageway between two adjacent cells • Let small molecules move directly between neighboring cells • Cells are connected by hollow cylinders of protein • Each junction is composed of 6 connexin form hexameric complexes called connexons proteins that span the membrane and form one half of the junction • Permit Cell to cell exchange of low MW molecules such as: ions, c. AMP, small hormones. • Not present in skeletal muscle.
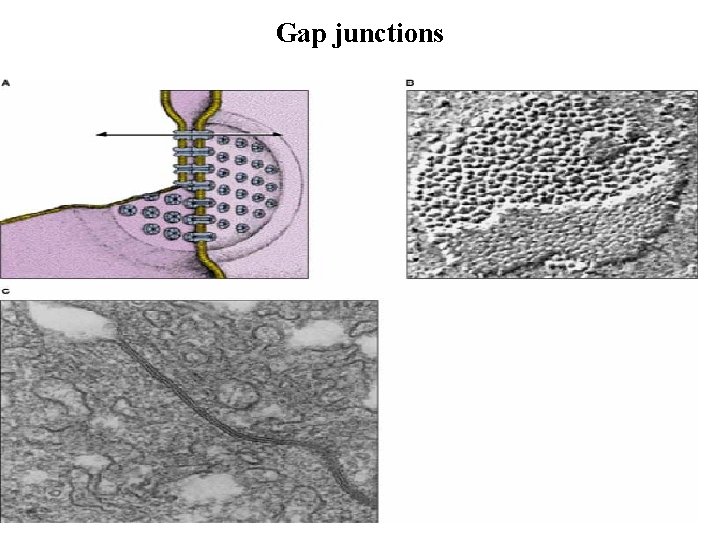
Gap junctions
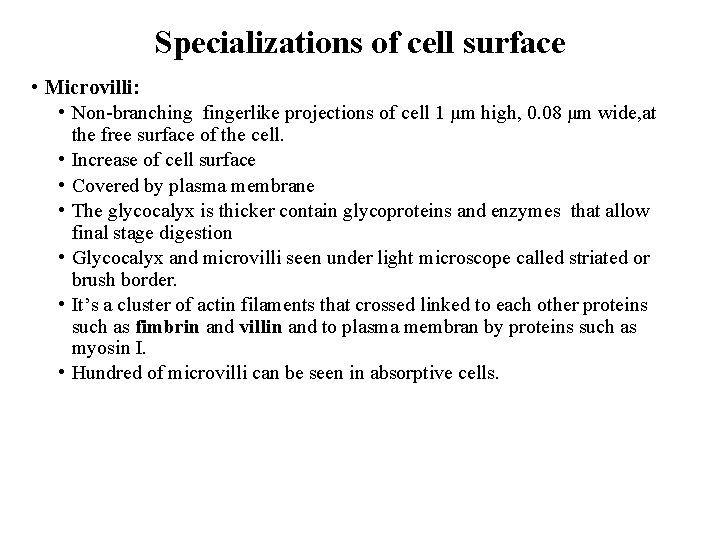
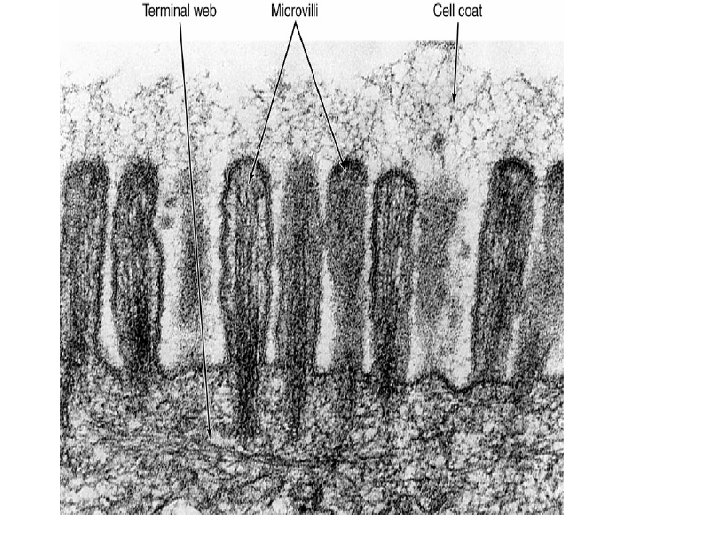
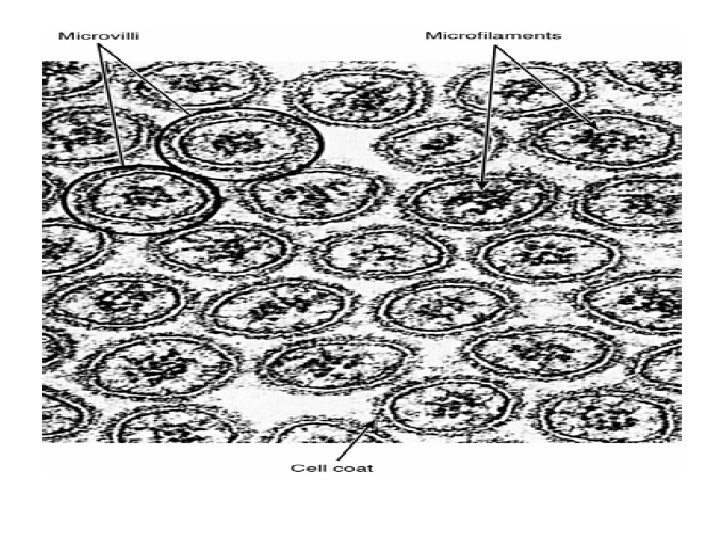
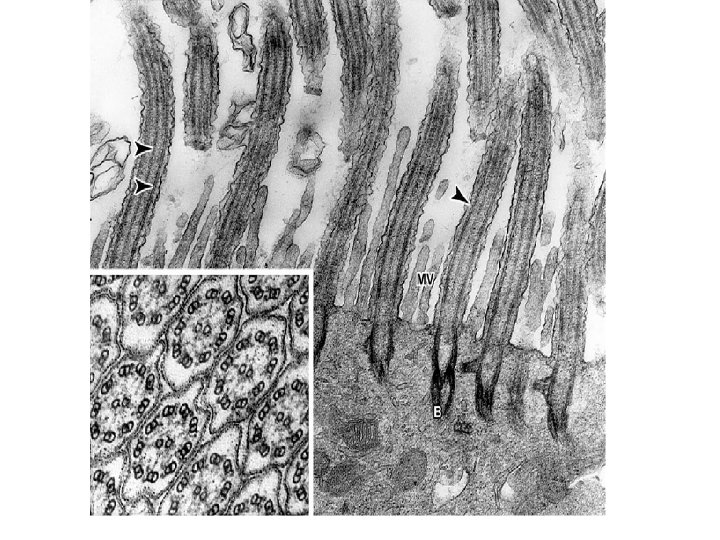
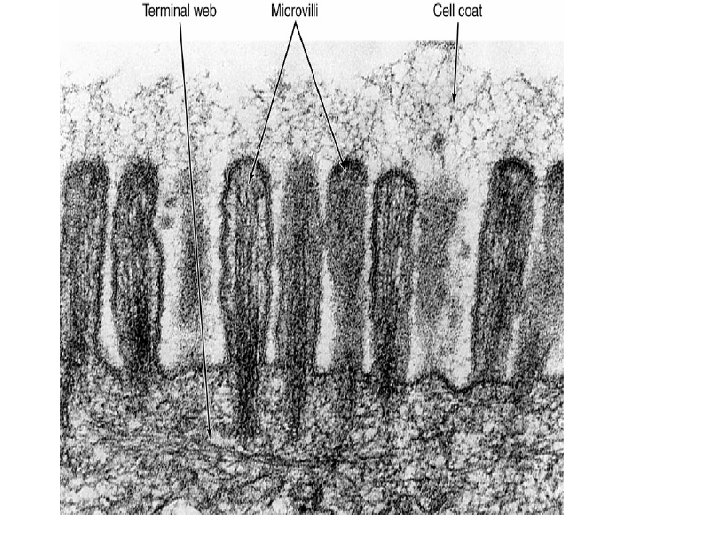
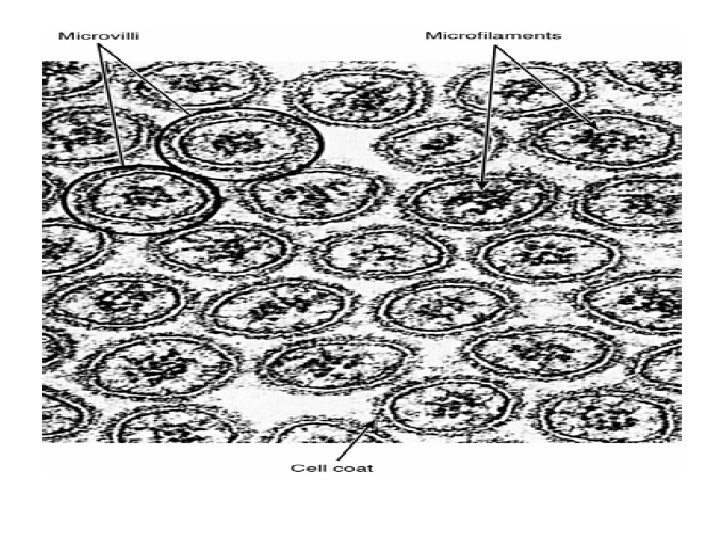
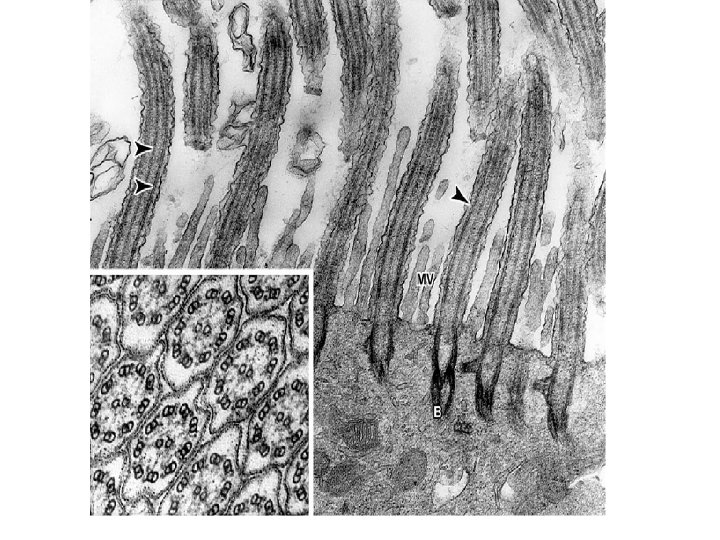
Specializations of cell surface • Microvilli: • Non-branching fingerlike projections of cell 1 μm high, 0. 08 μm wide, at • • • the free surface of the cell. Increase of cell surface Covered by plasma membrane The glycocalyx is thicker contain glycoproteins and enzymes that allow final stage digestion Glycocalyx and microvilli seen under light microscope called striated or brush border. It’s a cluster of actin filaments that crossed linked to each other proteins such as fimbrin and villin and to plasma membran by proteins such as myosin I. Hundred of microvilli can be seen in absorptive cells.
Specializations of cell surface • stereocilia • Branched non – motile microvilli of cells of epididymis and ductus deference • Its function to increase the surface area • Cilia • Non-branching motile projections • Transport of extracellular mass • May be numerous • 270 per cell in trachea • 5 -10 μm tall , 0. 2 μm wide • Composed of central pair of microtubules doublets surrounded by nine pair of microtubules = axoneme • Attached to basal bodies ( analogus to the centrioles) at the apical area • Flagella very long cillia 100 μm , only in spermatozoa
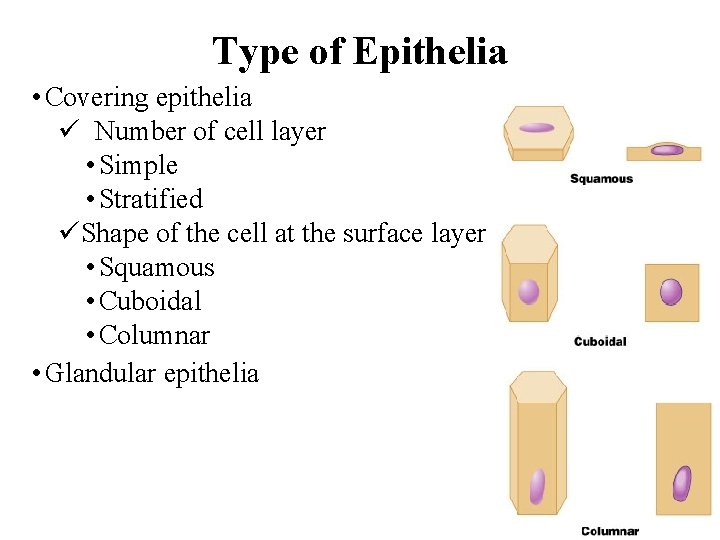
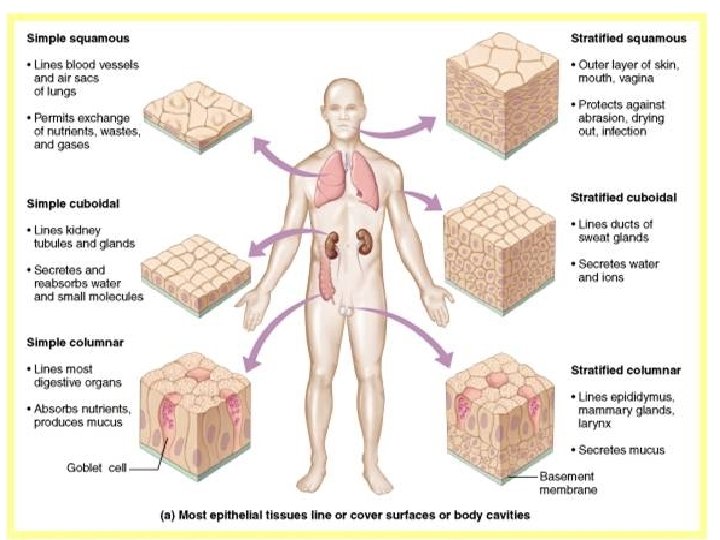
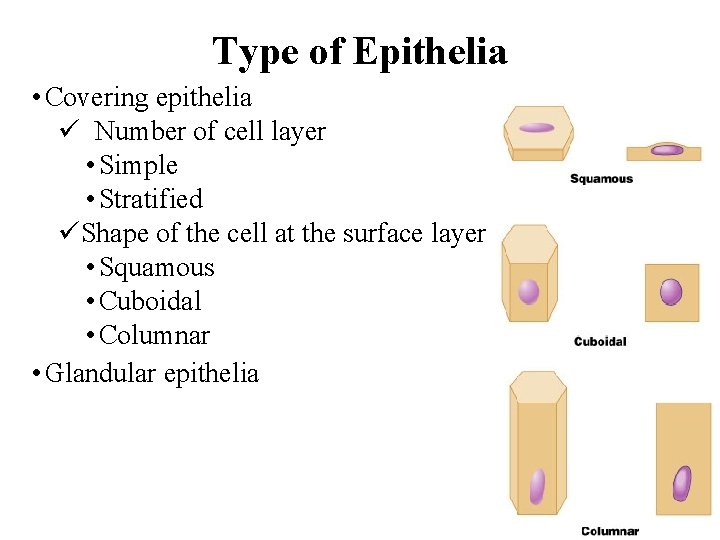
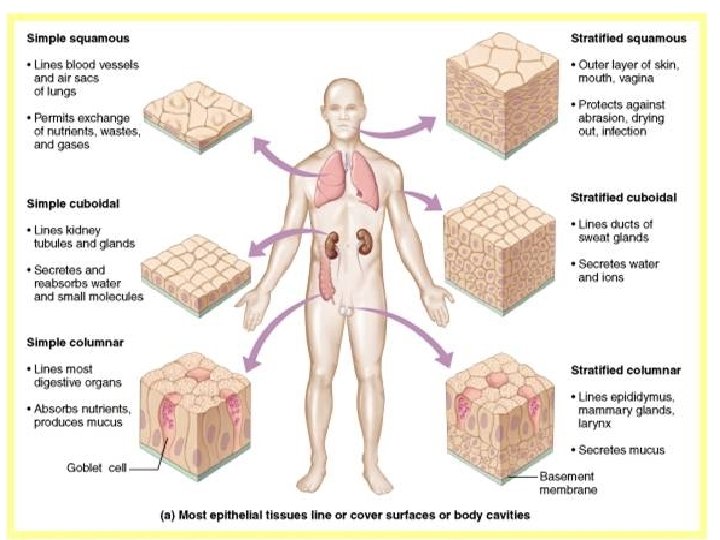
Type of Epithelia • Covering epithelia ü Number of cell layer • Simple • Stratified üShape of the cell at the surface layer • Squamous • Cuboidal • Columnar • Glandular epithelia
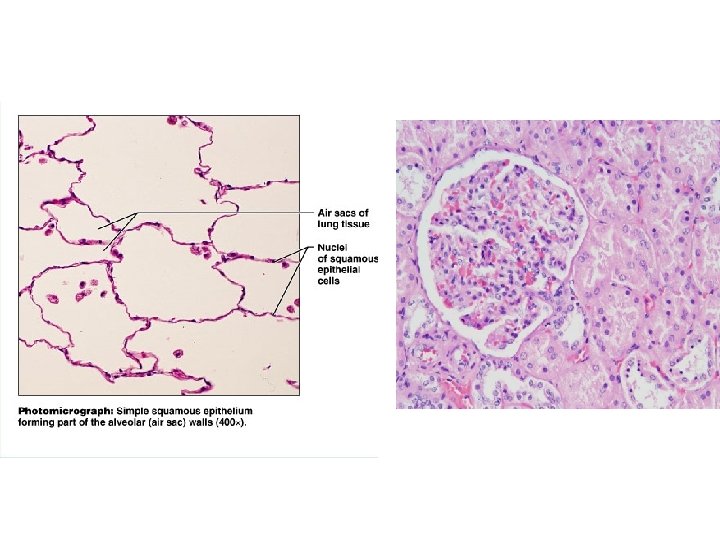
Simple Squamous Epithelium • Description • single layer of flat cells with disc-shaped nuclei • Special types • Endothelium (inner covering) • slick lining of hollow organs • Mesothelium (middle covering) • Lines peritoneal, pleural, and pericardial cavities • Covers visceral organs of those cavities
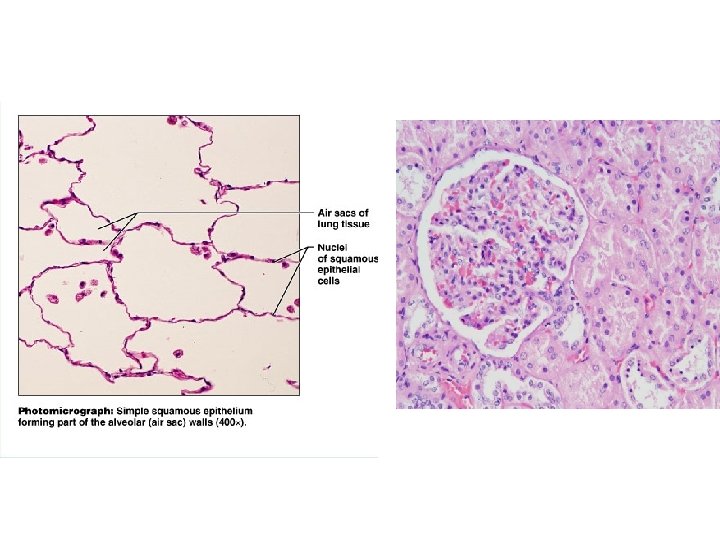
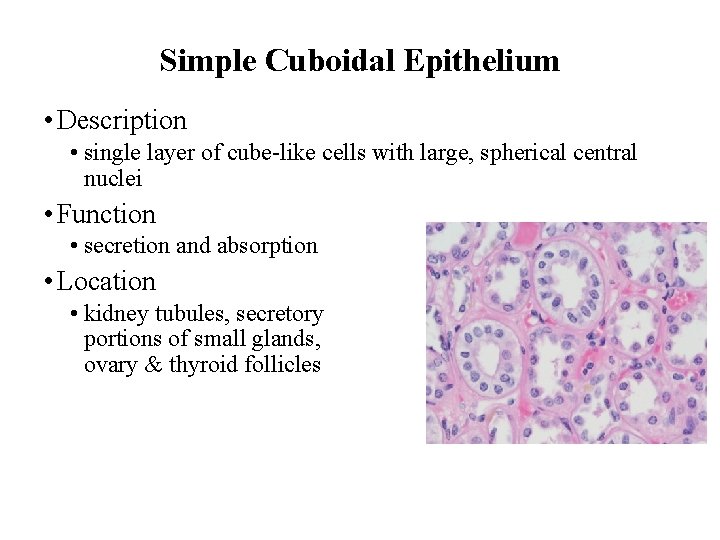
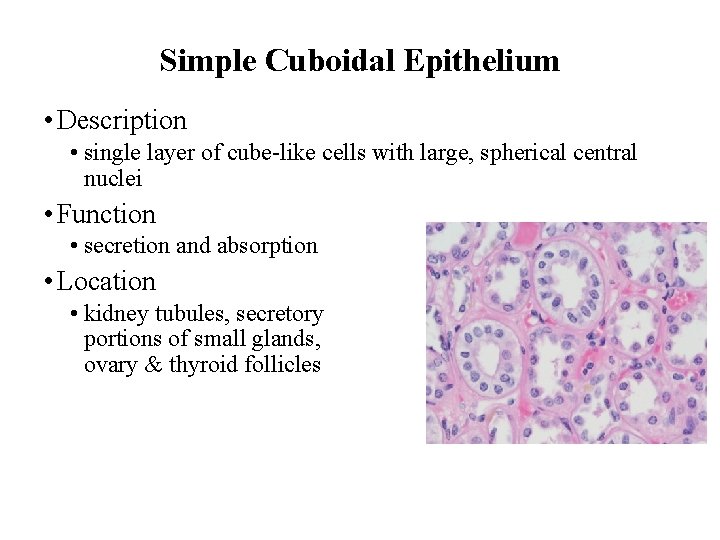
Simple Cuboidal Epithelium • Description • single layer of cube-like cells with large, spherical central nuclei • Function • secretion and absorption • Location • kidney tubules, secretory portions of small glands, ovary & thyroid follicles
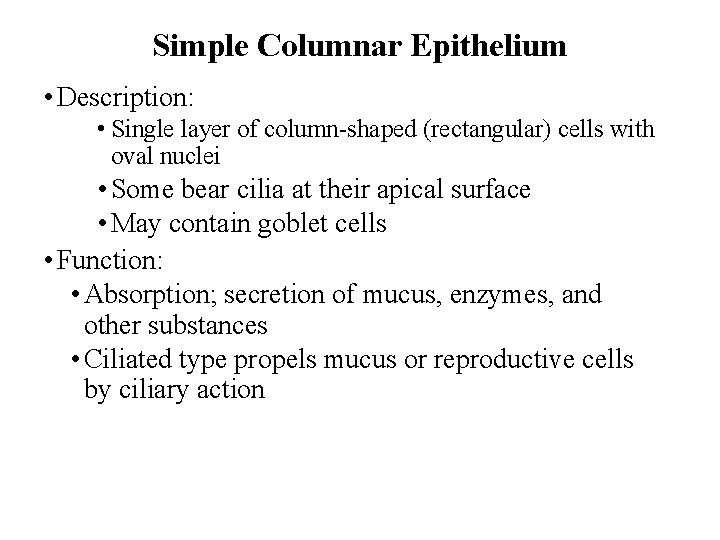
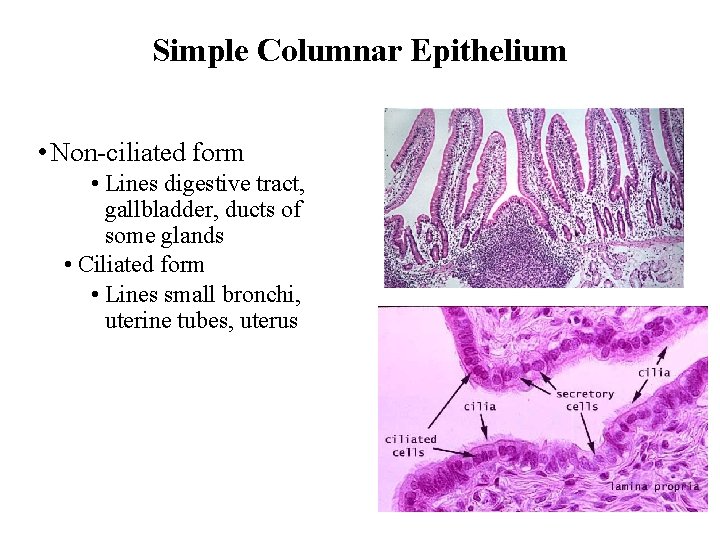
Simple Columnar Epithelium • Description: • Single layer of column-shaped (rectangular) cells with oval nuclei • Some bear cilia at their apical surface • May contain goblet cells • Function: • Absorption; secretion of mucus, enzymes, and other substances • Ciliated type propels mucus or reproductive cells by ciliary action
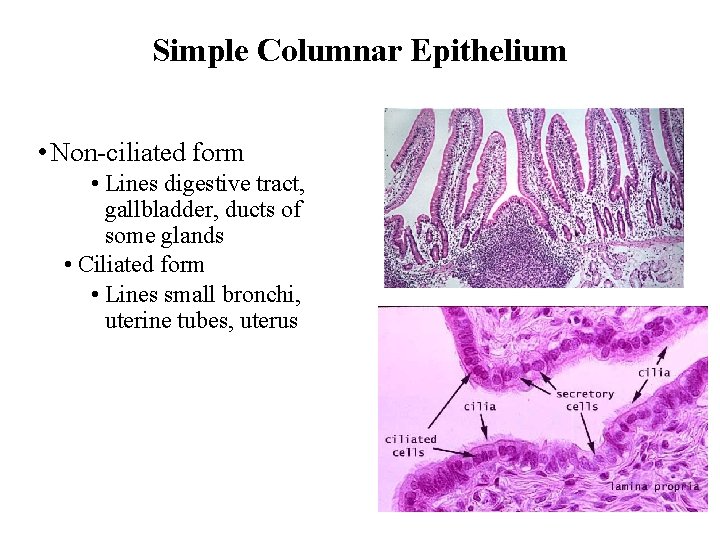
Simple Columnar Epithelium • Non-ciliated form • Lines digestive tract, gallbladder, ducts of some glands • Ciliated form • Lines small bronchi, uterine tubes, uterus
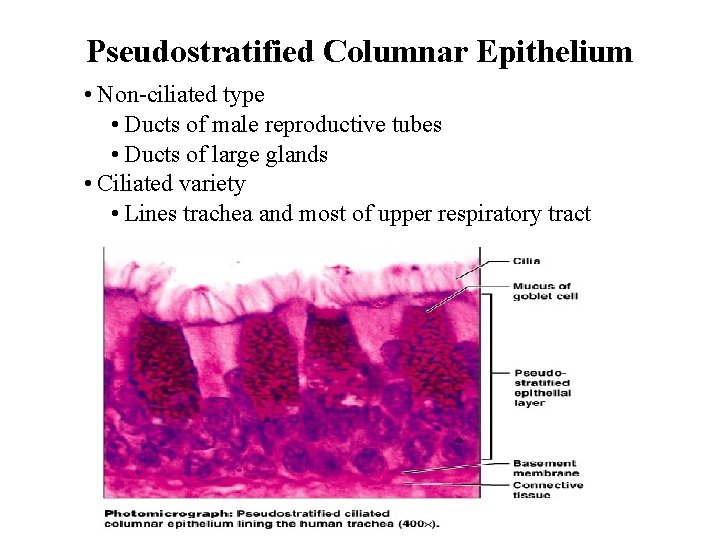
Pseudostratified Columnar Epithelium • Description: • All cells originate at basement membrane • Only tall cells reach the apical surface • May contain goblet cells and bear cilia • Nuclei lie at varying heights within cells • Gives false impression of stratification • Function: • secretion of mucus; propulsion of mucus by cilia
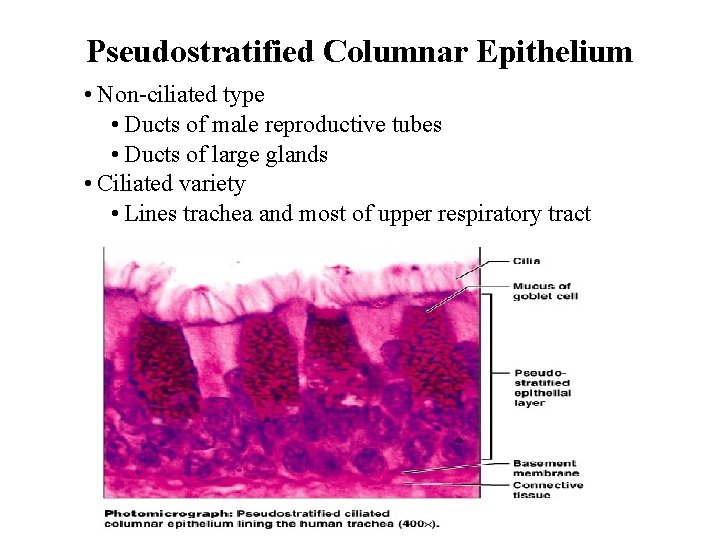
Pseudostratified Columnar Epithelium • Non-ciliated type • Ducts of male reproductive tubes • Ducts of large glands • Ciliated variety • Lines trachea and most of upper respiratory tract
Stratified Epithelia • Contain two or more layers of cells • Regenerate from below • Major role is protection • Are named according to the shape of cells at apical layer
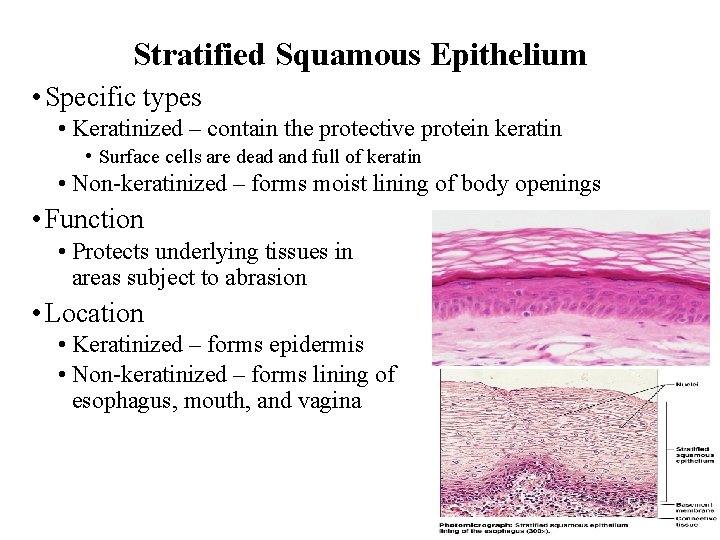
Stratified Squamous Epithelium • Description: • Many layers of cells – squamous in shape • Deeper layers of cells appear cuboidal or columnar • Thickest epithelial tissue – adapted for protection
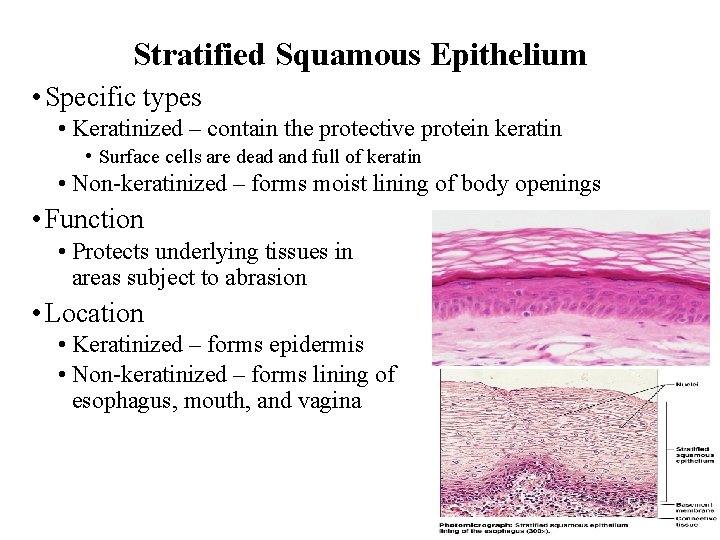
Stratified Squamous Epithelium • Specific types • Keratinized – contain the protective protein keratin • Surface cells are dead and full of keratin • Non-keratinized – forms moist lining of body openings • Function • Protects underlying tissues in areas subject to abrasion • Location • Keratinized – forms epidermis • Non-keratinized – forms lining of esophagus, mouth, and vagina
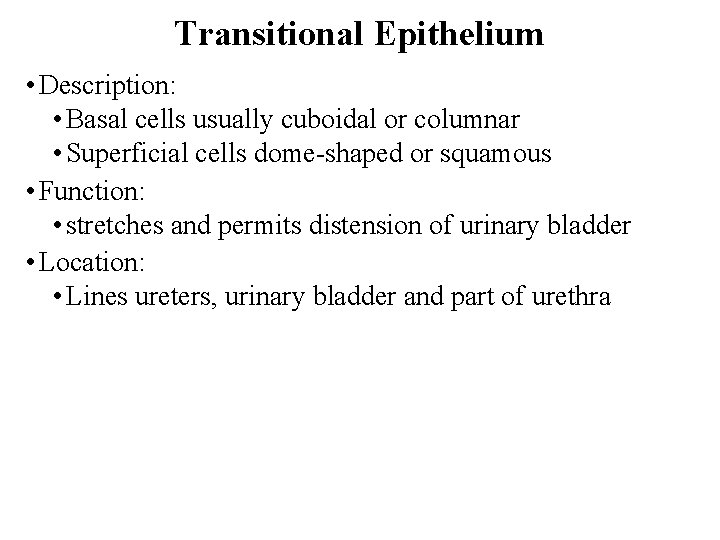
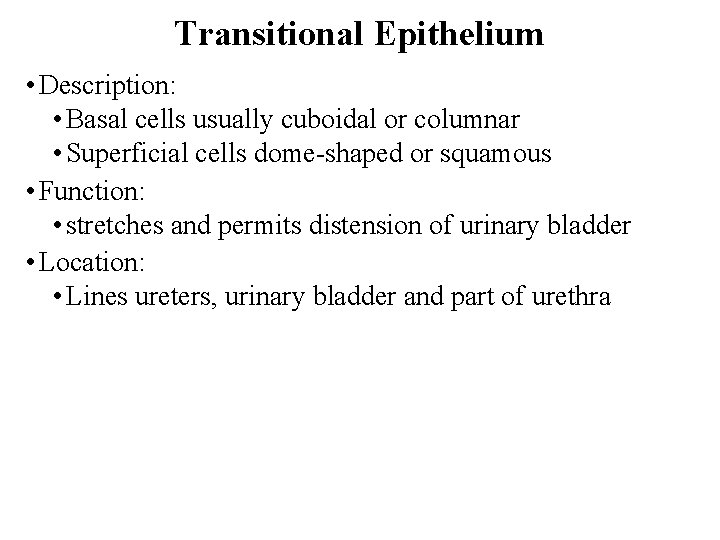
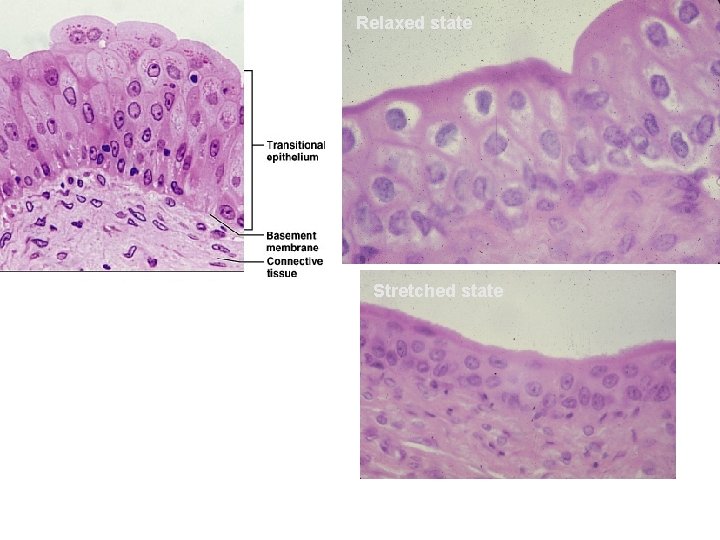
Transitional Epithelium • Description: • Basal cells usually cuboidal or columnar • Superficial cells dome-shaped or squamous • Function: • stretches and permits distension of urinary bladder • Location: • Lines ureters, urinary bladder and part of urethra
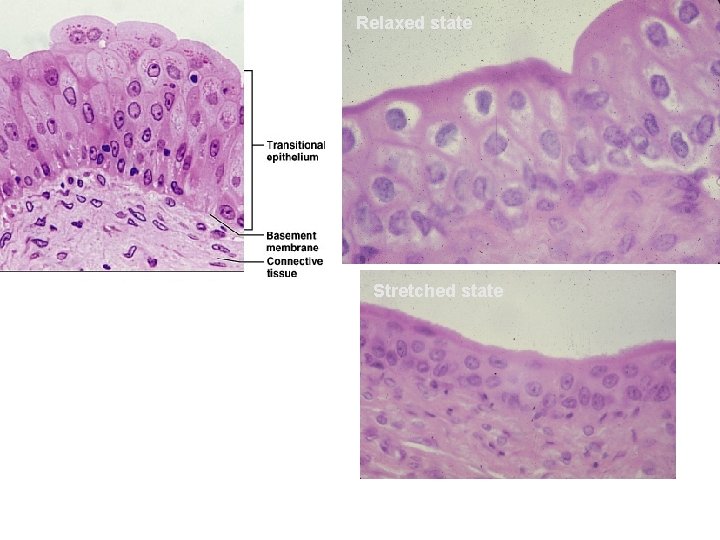
Relaxed state Stretched state
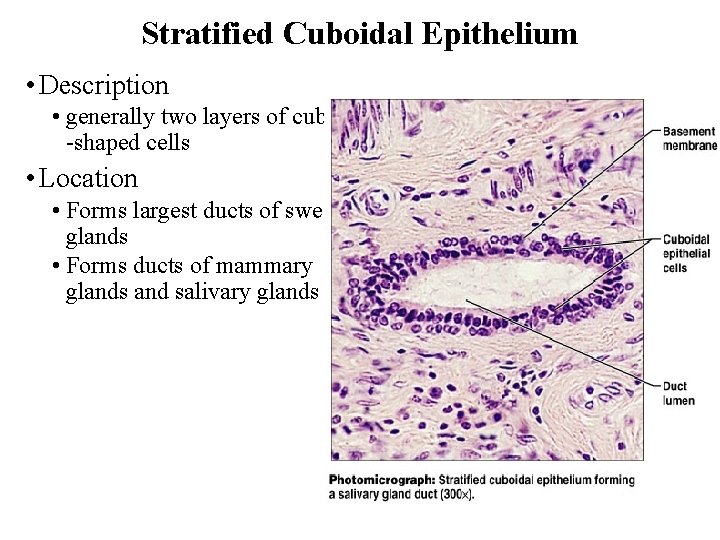
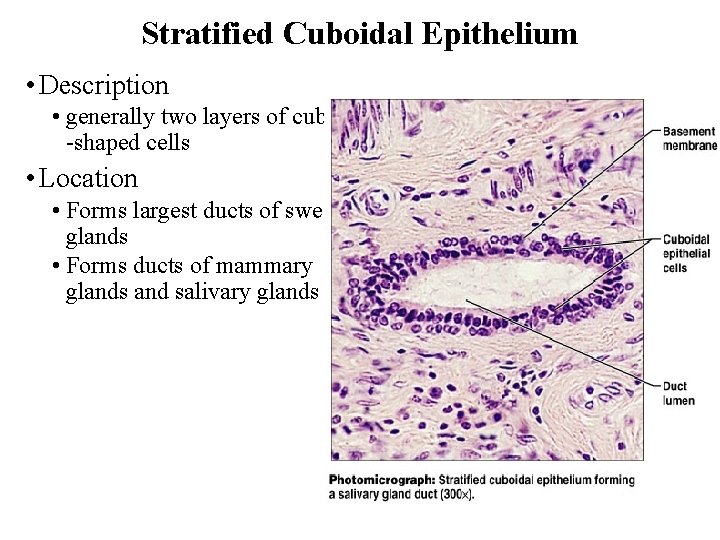
Stratified Cuboidal Epithelium • Description • generally two layers of cube -shaped cells • Location • Forms largest ducts of sweat glands • Forms ducts of mammary glands and salivary glands
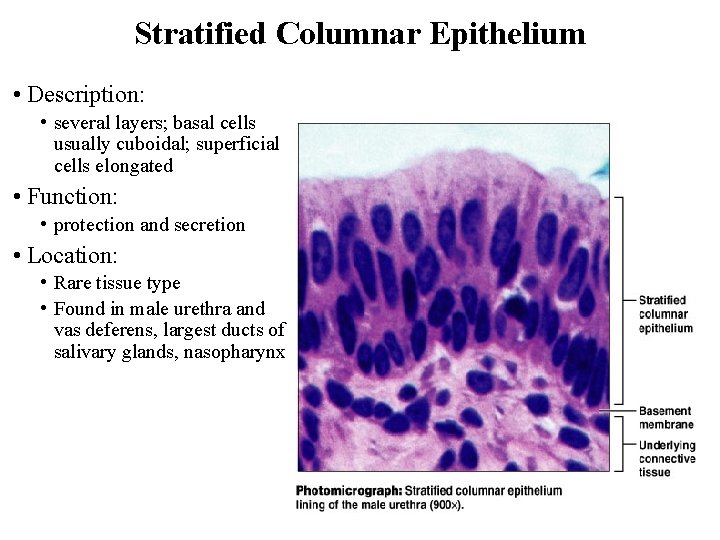
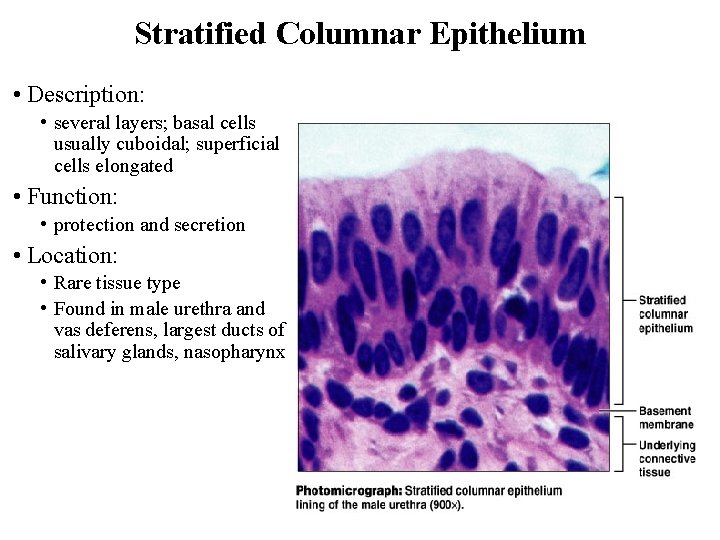
Stratified Columnar Epithelium • Description: • several layers; basal cells usually cuboidal; superficial cells elongated • Function: • protection and secretion • Location: • Rare tissue type • Found in male urethra and vas deferens, largest ducts of salivary glands, nasopharynx
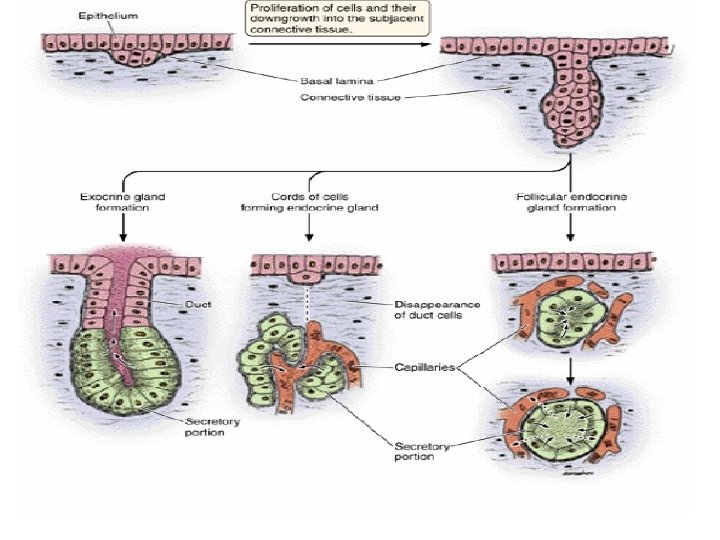
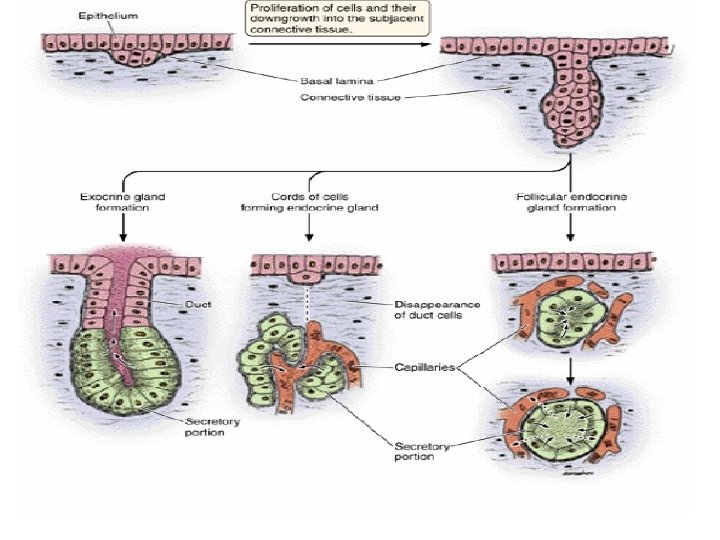
Glandular epithelium • Cells that are specialized to produce and secrete substances into ducts or into body fluids. • Gland = 1 or more cuboidal or columnar cell. • Secretion (lipid, proteins, &carbohydrate complex ). • Salivary glands, sweat glands, endocrine glands.
Exocrine vs. Endocrine • Exocrine = secrete sub. into ducts that open onto surfaces • skin or linings of digestive tract • Endocrine = secrete sub. into tissue fluid or blood • hormones
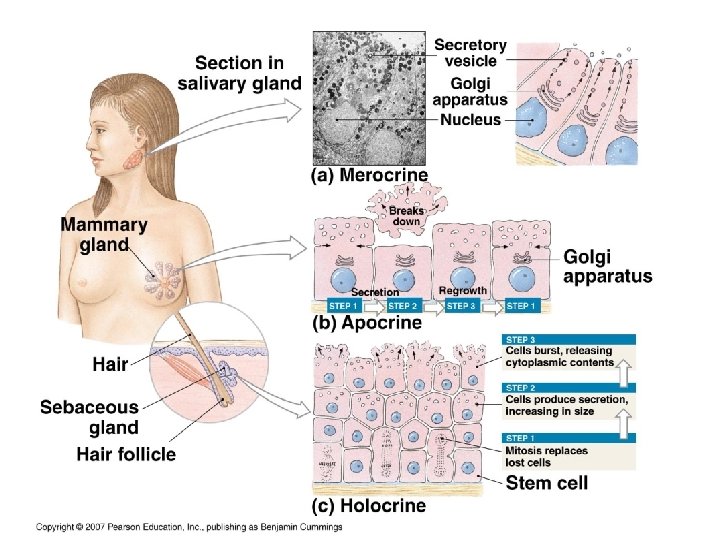
Exocrine glands • Merocrine = Secretory material is released with little or no loss of cytoplasm. Release watery, protein-rich fluid by exocytosis E. g. salivary glands, sweat glands • Apocrine = Secretory material is concentrated in apical end of Cell Apical plasma membrane is lost during secretion E. g. mammary glands, ear wax • Holocrine = entire cell lysis (breaks apart) during secretion, Cell membrane disintegrates and contents shed into duct or lumen E. g. sebaceous gland
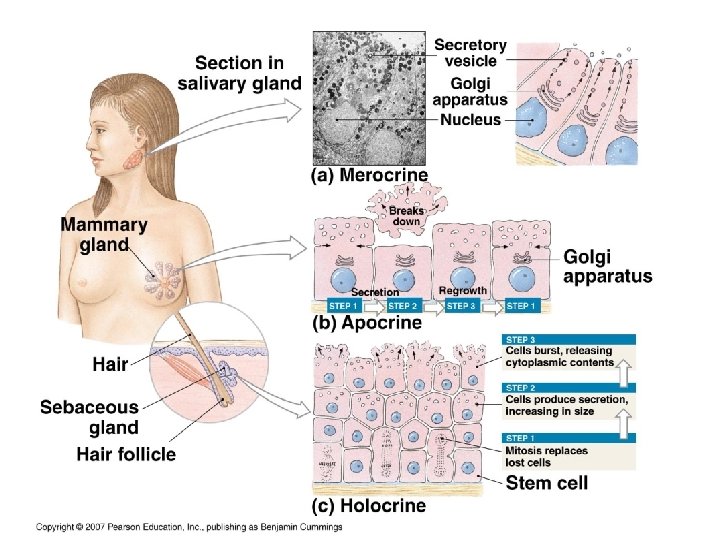
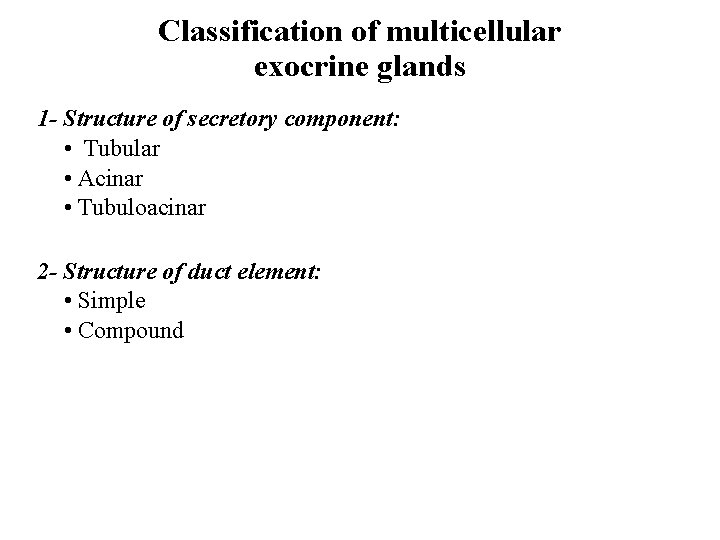
Classification of multicellular exocrine glands 1 - Structure of secretory component: • Tubular • Acinar • Tubuloacinar 2 - Structure of duct element: • Simple • Compound
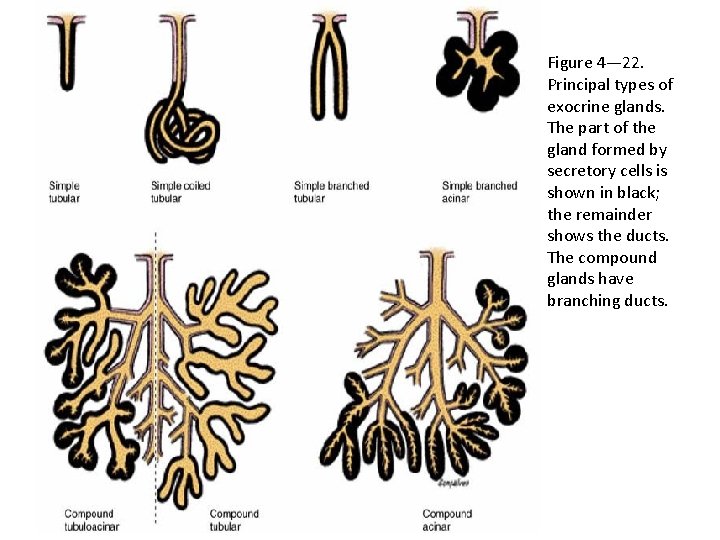
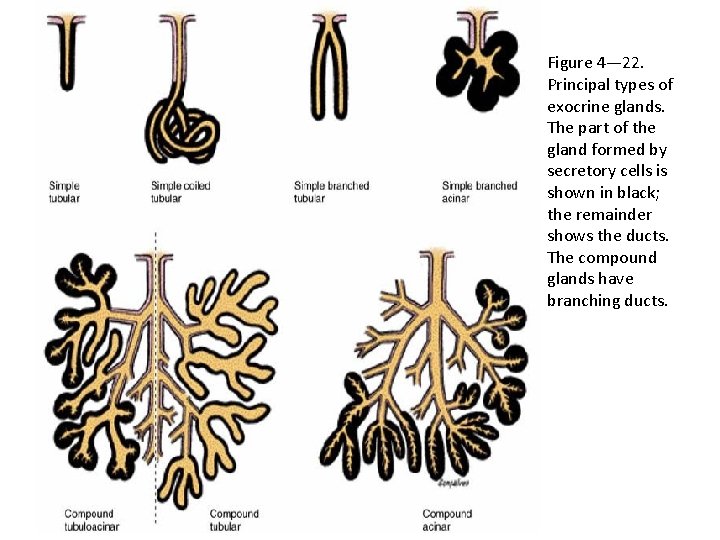
Figure 4— 22. Principal types of exocrine glands. The part of the gland formed by secretory cells is shown in black; the remainder shows the ducts. The compound glands have branching ducts.
Unicellular vs Multicellular glands • Unicellular glands: • Mucous (goblet) cells are the only unicellular exocrine glands • Scattered among epithelia • For example, in intestinal lining • Multicellular glands: 1. Structure of the duct • Simple (undivided) • Compound (divided) 2. Shape of secretory portion of the gland • Tubular (tube shaped) • Alveolar or acinar (blind pockets) 3. Relationship between ducts and glandular areas • Branched (several secretory areas sharing one duct)
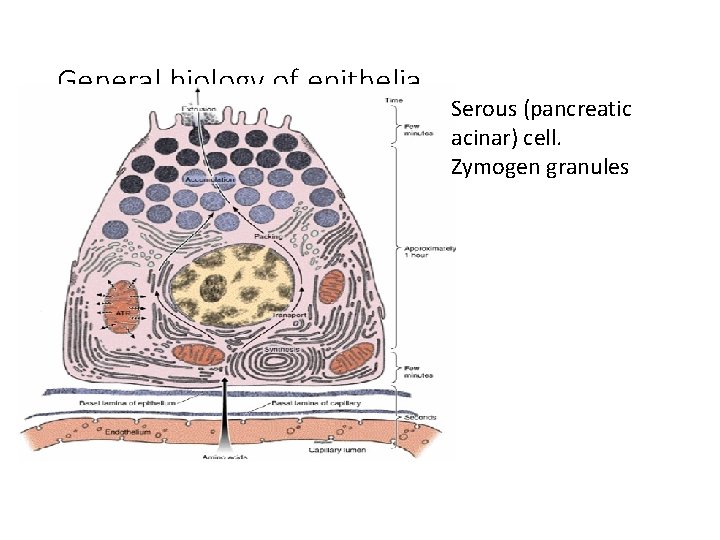
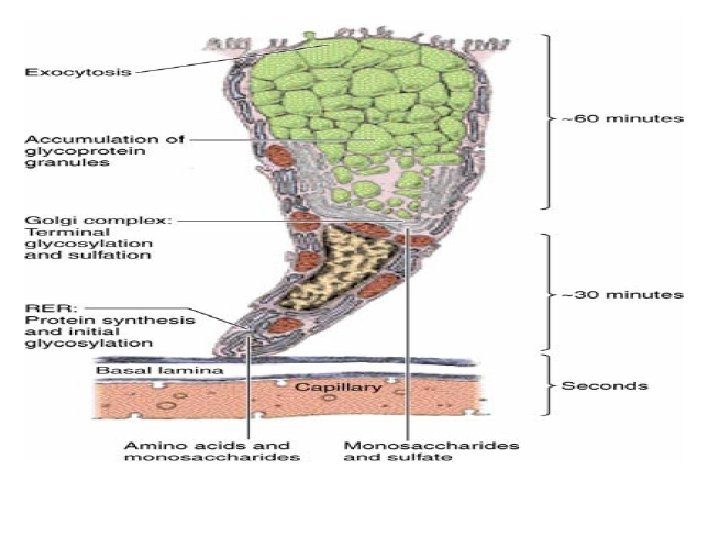
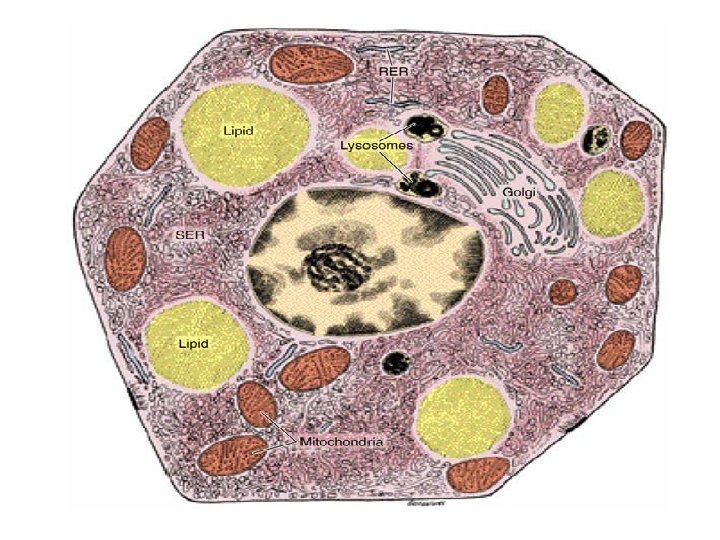
Serous cell • Example: acinar cell of pancreas and parotid salivary gland which secrete digestive enzymes • Polyhedral or pyramidal with central round nucleus • Abundant RER & polyribosome in the base. • Well developed golgi between nucleus and the apex • Mature sec. granule accumulate in the apical area which can seen under L. M as light staining granule • These granule called zymogen • Secretion by exocytosis.
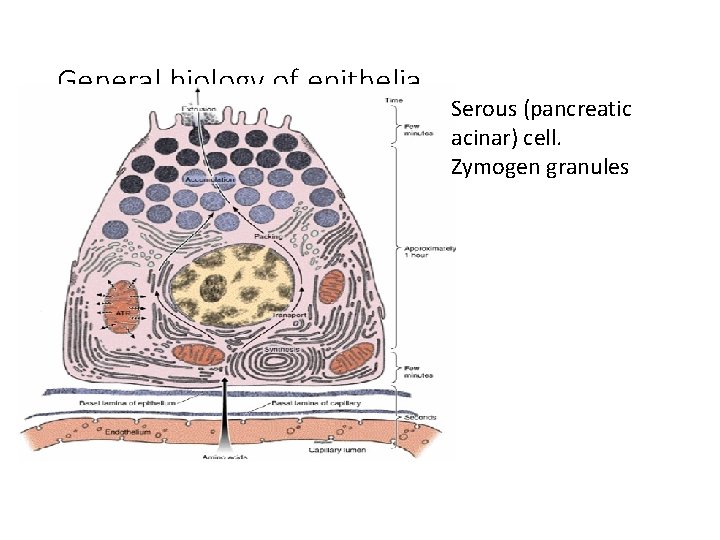
General biology of epithelia Serous (pancreatic acinar) cell. Zymogen granules
Regeneration of epithelium (renewal) • Its rate is variable: • Fast small intestine – 3 days • Slow liver and pancreas, skin - 27 days • Mitosis in stem cells ( germinal layer )
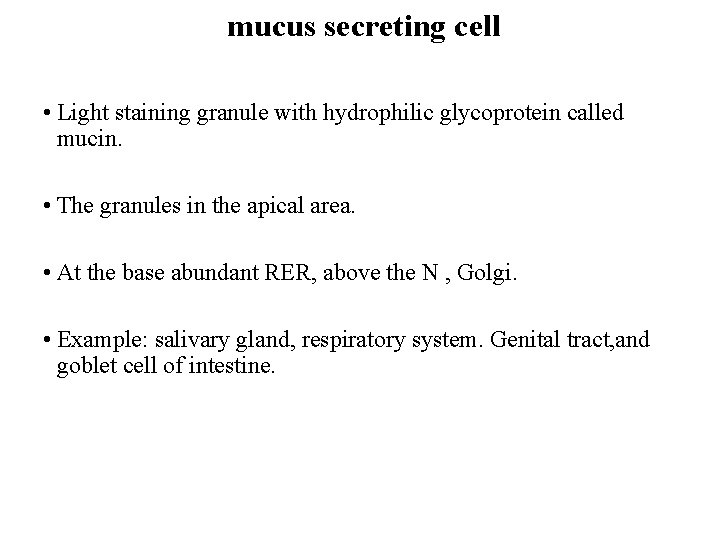
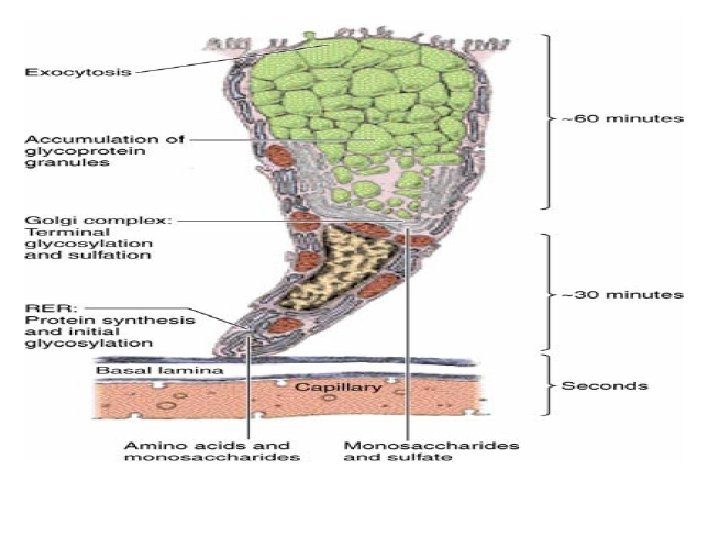
mucus secreting cell • Light staining granule with hydrophilic glycoprotein called mucin. • The granules in the apical area. • At the base abundant RER, above the N , Golgi. • Example: salivary gland, respiratory system. Genital tract, and goblet cell of intestine.
General biology of epithelia
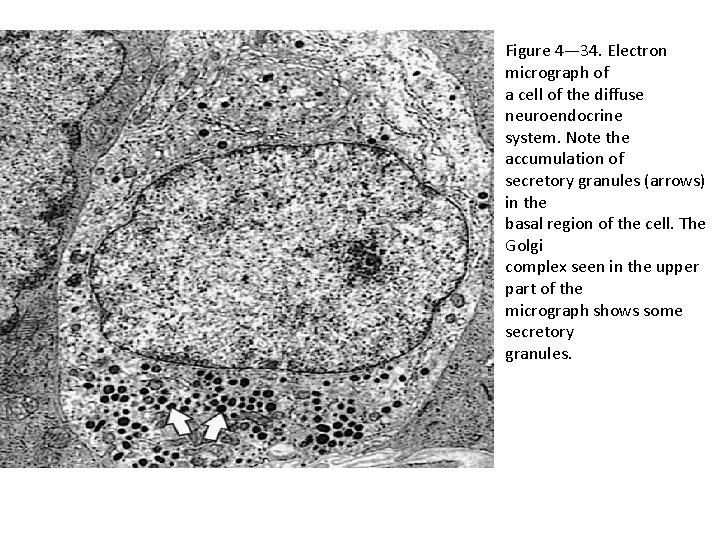
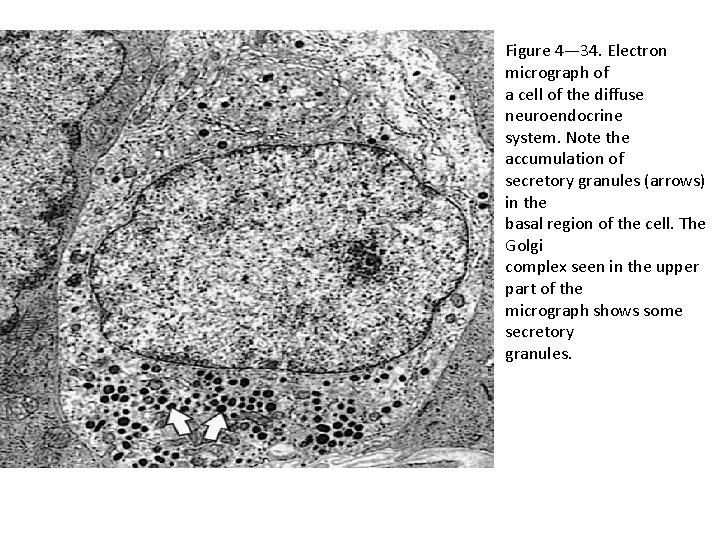
Figure 4— 34. Electron micrograph of a cell of the diffuse neuroendocrine system. Note the accumulation of secretory granules (arrows) in the basal region of the cell. The Golgi complex seen in the upper part of the micrograph shows some secretory granules.
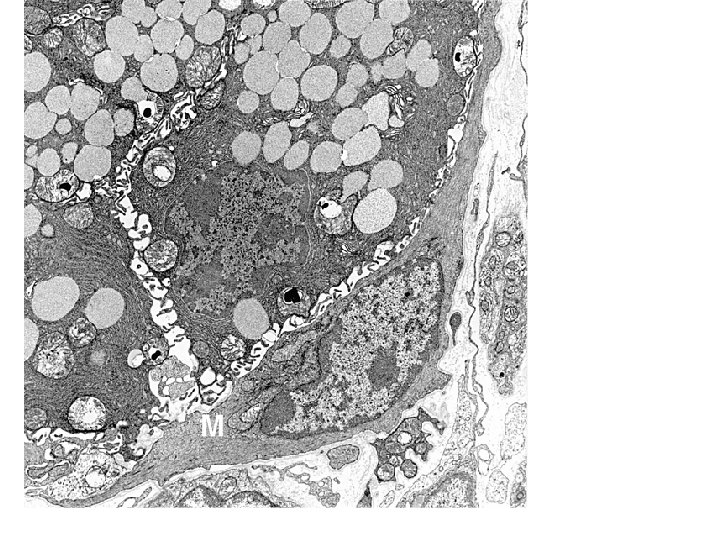
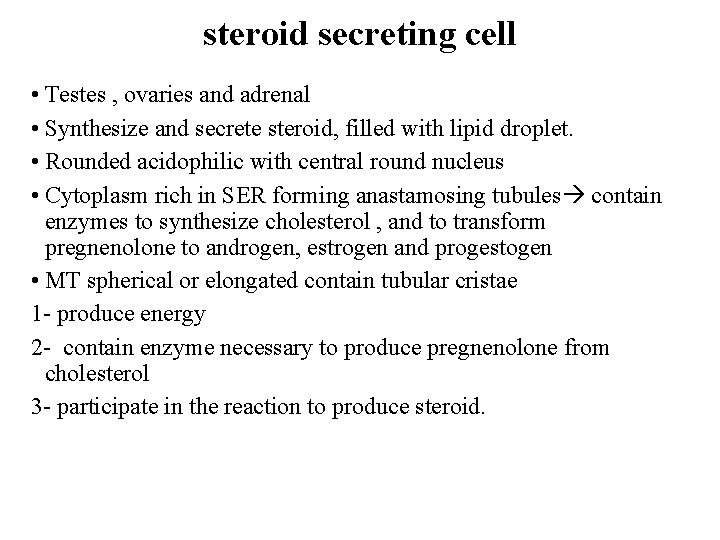
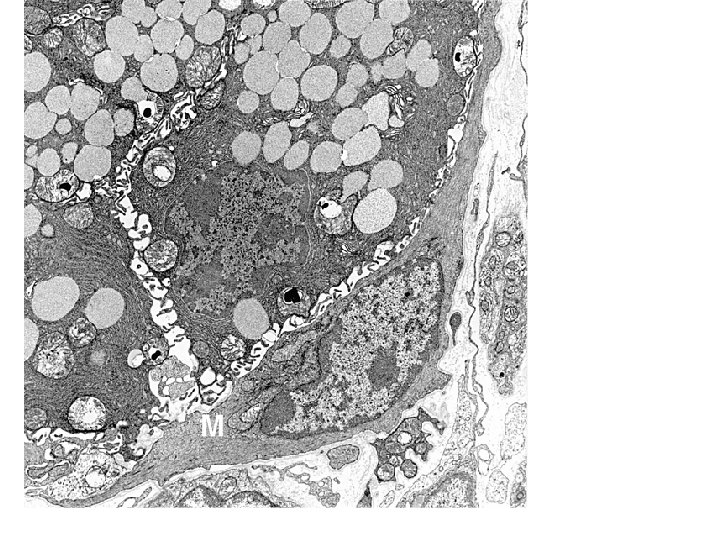
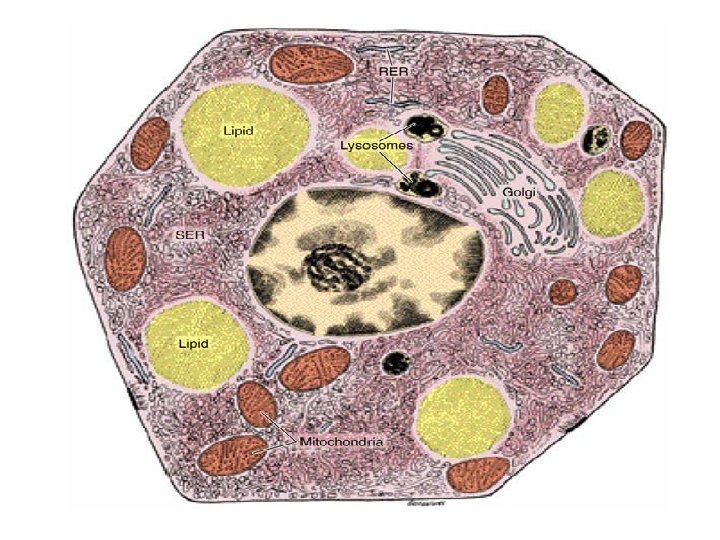
steroid secreting cell • Testes , ovaries and adrenal • Synthesize and secrete steroid, filled with lipid droplet. • Rounded acidophilic with central round nucleus • Cytoplasm rich in SER forming anastamosing tubules contain enzymes to synthesize cholesterol , and to transform pregnenolone to androgen, estrogen and progestogen • MT spherical or elongated contain tubular cristae 1 - produce energy 2 - contain enzyme necessary to produce pregnenolone from cholesterol 3 - participate in the reaction to produce steroid.
THANK YOU