Chapter 38 Activity and Exercise Scientific Knowledge Base
Chapter 38 Activity and Exercise
Scientific Knowledge Base • Overview of exercise and activity: – Body alignment • Relationship of one body part to another – Body balance • Achieved by low center of gravity; enhanced by posture – Coordinated body movement • A result of weight, center of gravity, and balance
Scientific Knowledge Base (cont’d) • Overview of exercise and activity: – Friction • Force that occurs in a direction to oppose movement – Exercise and activity • A patient’s individualized exercise program depends on the patient’s activity tolerance or the type and amount of exercise or activity that the patient is able to perform. • Isotonic exercises • Isometric exercises
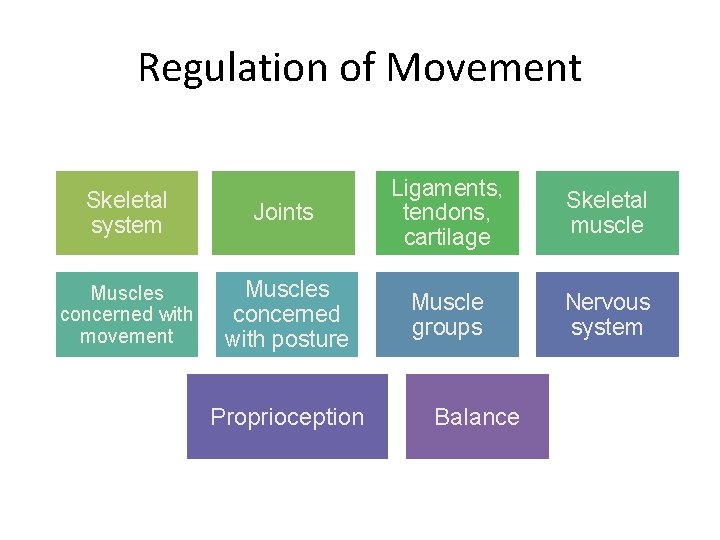
Regulation of Movement Skeletal system Muscles concerned with movement Joints Ligaments, tendons, cartilage Skeletal muscle Muscles concerned with posture Muscle groups Nervous system Proprioception Balance
Factors Influencing Activity and Exercise • Developmental changes – Infants through school-aged children – Adolescence – Young to middle adults – Older adults • Behavioral aspects – Patients are more likely to incorporate an exercise program if those around them are supportive.
Factors Influencing Activity and Exercise • Environmental issues – Work site – Schools – Community • Cultural and ethnic influences • Family and social support
Nursing Process Assessment Diagnosis Planning Implementation Evaluation
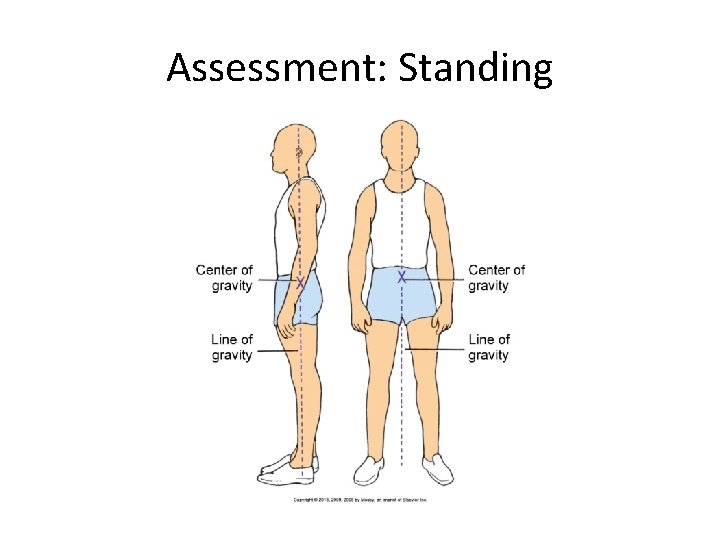
Assessment: Standing
Assessment: Sitting • Sitting – Head is erect. – Neck and vertebral column are in straight alignment. – Body weight is distributed on the buttocks and thighs. – Thighs are parallel and horizontal. – Feet are supported on the floor. – Forearms are supported on the armrest, in the lap, or on a table in front of the chair.
Assessment • Recumbent position • Mobility – Range of motion – Gait – Exercise • Activity tolerance
Nursing Diagnosis Activity intolerance Ineffective coping Impaired gas exchange Risk for injury Impaired physical mobility Imbalanced nutrition: more than body requirements • Acute or chronic pain • • •
Planning • Goals and outcomes – Participates in prescribed physical activity while maintaining appropriate heart rate, blood pressure, and breathing rate – Verbalizes an understanding of the need to gradually increase activity based on tolerance and symptoms – Expresses understanding of balancing rest and activity • Setting priorities • Teamwork and collaboration
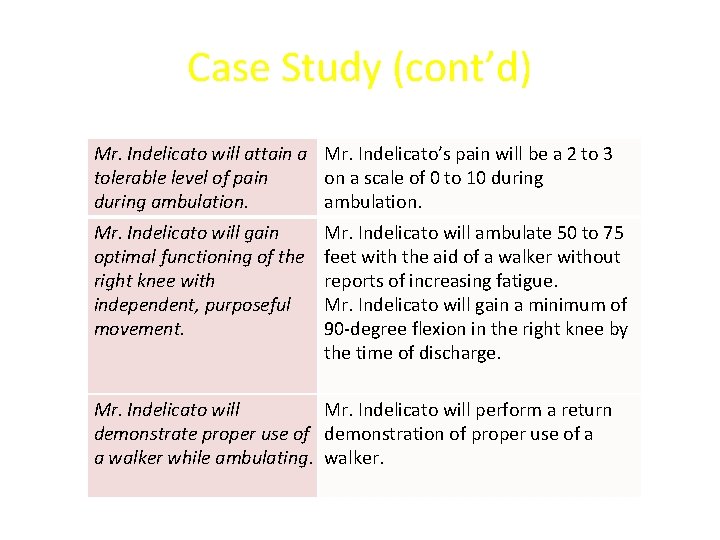
Case Study (cont’d) Mr. Indelicato will attain a Mr. Indelicato’s pain will be a 2 to 3 tolerable level of pain on a scale of 0 to 10 during ambulation. Mr. Indelicato will gain optimal functioning of the right knee with independent, purposeful movement. Mr. Indelicato will ambulate 50 to 75 feet with the aid of a walker without reports of increasing fatigue. Mr. Indelicato will gain a minimum of 90 -degree flexion in the right knee by the time of discharge. Mr. Indelicato will perform a return demonstrate proper use of demonstration of proper use of a a walker while ambulating. walker.
Implementation • Health promotion – Teach patients to calculate maximum heart rate. – Body mechanics • Acute care – Musculoskeletal system – Joint mobility – Walking • Restorative and continuing care
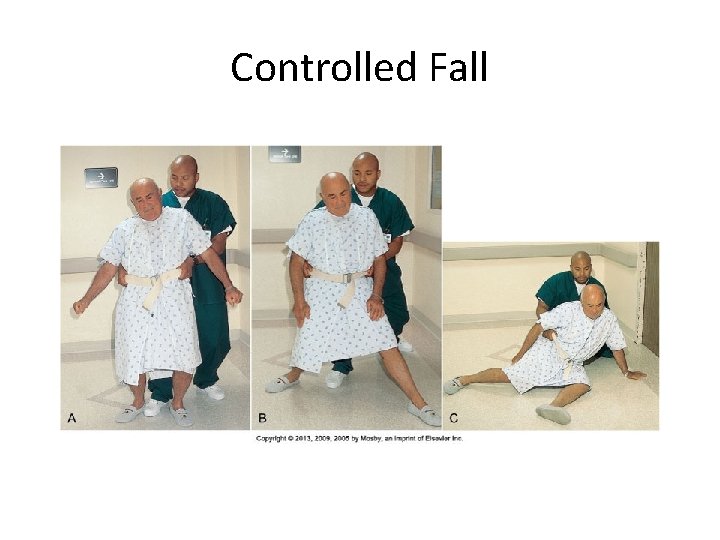
Controlled Fall
Case Study (cont’d) • Marilyn wants to help Mr. Indelicato with ambulation and strength training. To implement her plan of care, she: – Encourages Mr. Indelicato to use PCA pump before ambulation – Explains why he should sit in bed and dangle his legs before standing to ambulate – Establishes realistic increments for Mr. Indelicato to increase walking distance during ambulation – Talks with him about exercise tolerance
Principles of Transfer and Positioning Techniques • When moving a patient, knowledge of safe transfer and positioning is crucial. • Pathological influences on body alignment and mobility: – Congenital defects – Disorders of bones, joints, and muscles – Central nervous system damage – Musculoskeletal trauma
Assistive Devices for Walking • Walkers • Canes • Crutches – Measuring for crutches – Crutch gait – Sitting in a chair with crutches
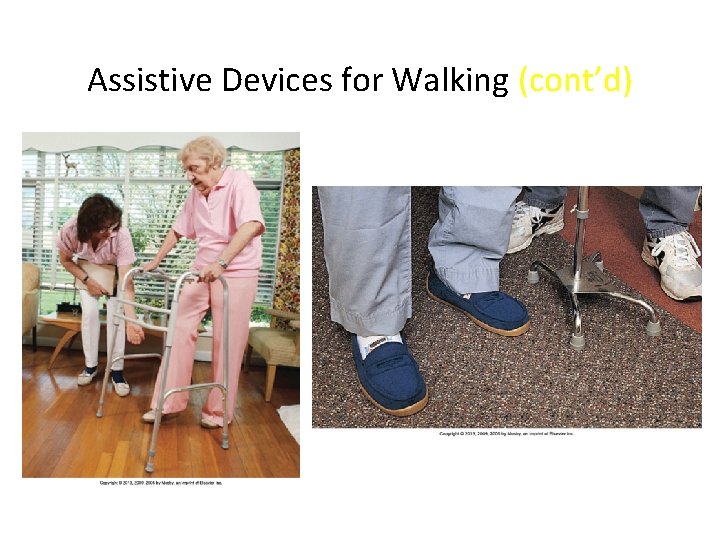
Assistive Devices for Walking (cont’d)
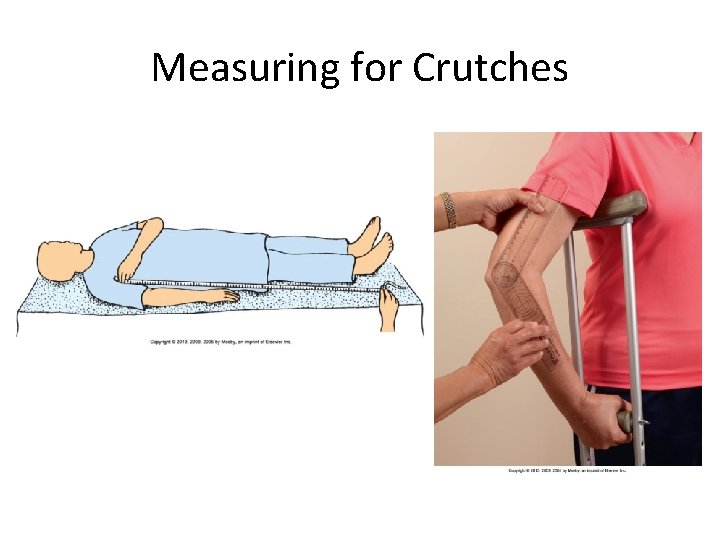
Measuring for Crutches
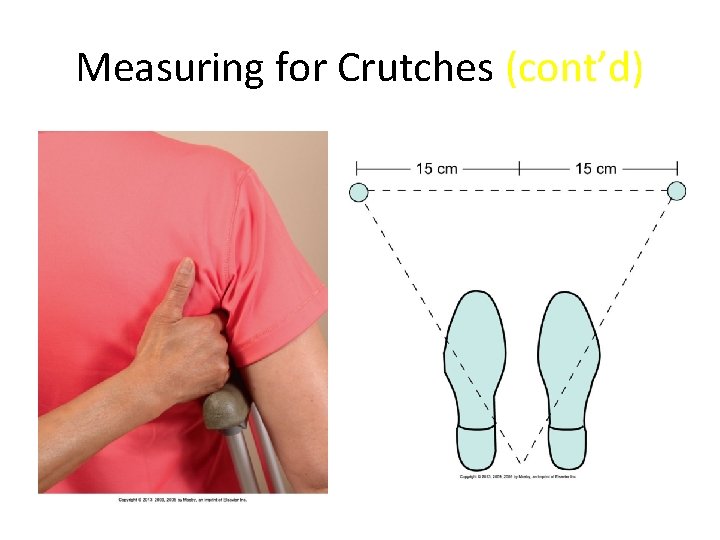
Measuring for Crutches (cont’d)
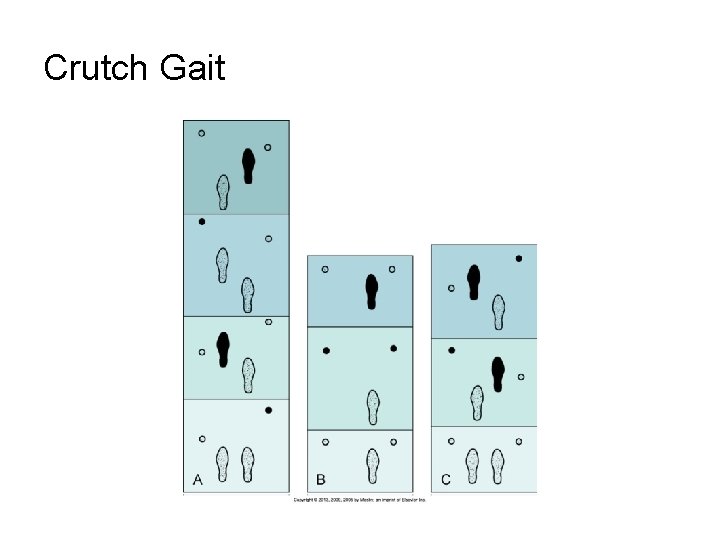
Crutch Gait
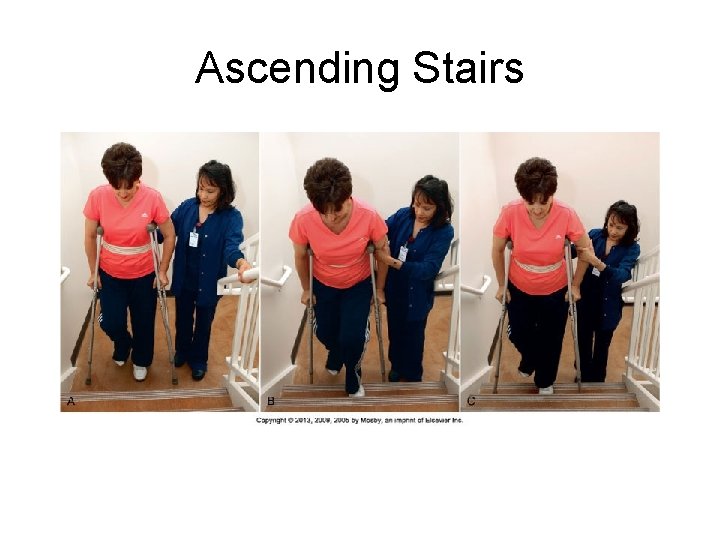
Ascending Stairs
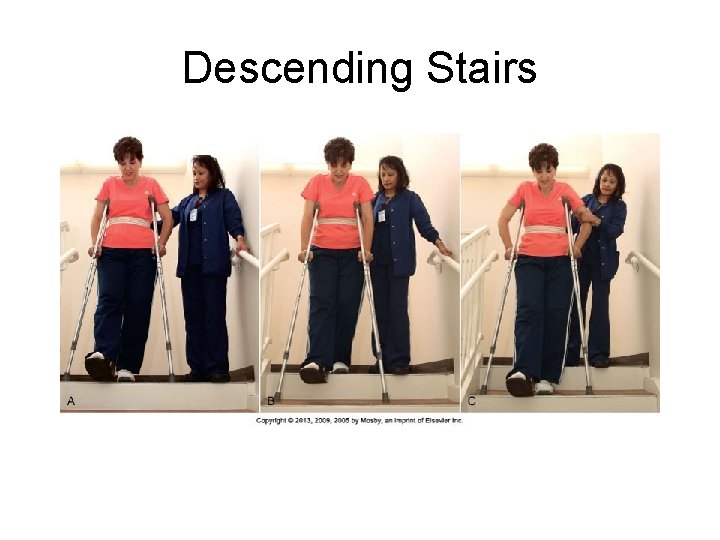
Descending Stairs

Sitting in a Chair
Implementation • Restoration of activity and chronic illness – Coronary heart disease – Hypertension – Chronic obstructive pulmonary disease – Diabetes mellitus
Evaluation • Patient outcomes – Reassess the patient for signs of improved activity and exercise tolerance. – Ask for the patient’s perception of activity and exercise status after interventions. – Ask if the patient’s expectations are being met.
Quick Quiz! 1. A patient with a long history of arthritis complains of sensitivity and warmth in the knees. To determine the degree of limitation, the nurse should assess A. Posture. B. Activity tolerance. C. Body mechanics. D. Range of joint motion. 37 - 28
Chapter 47 Mobility and Immobility
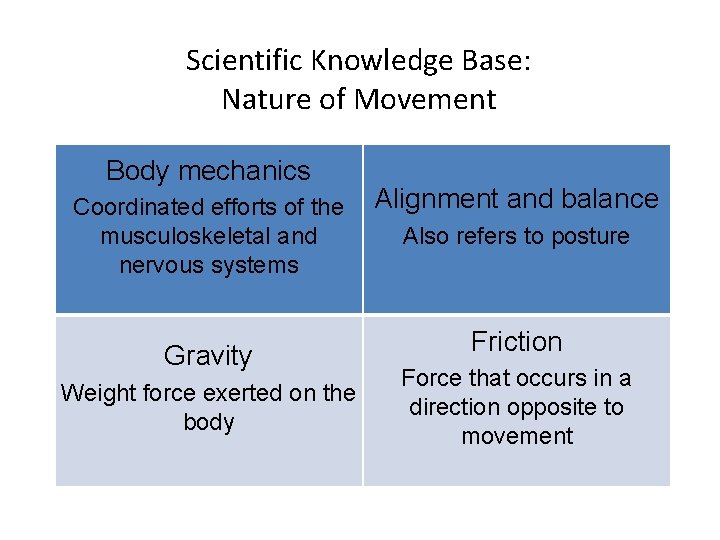
Scientific Knowledge Base: Nature of Movement Body mechanics Coordinated efforts of the musculoskeletal and nervous systems Gravity Weight force exerted on the body Alignment and balance Also refers to posture Friction Force that occurs in a direction opposite to movement
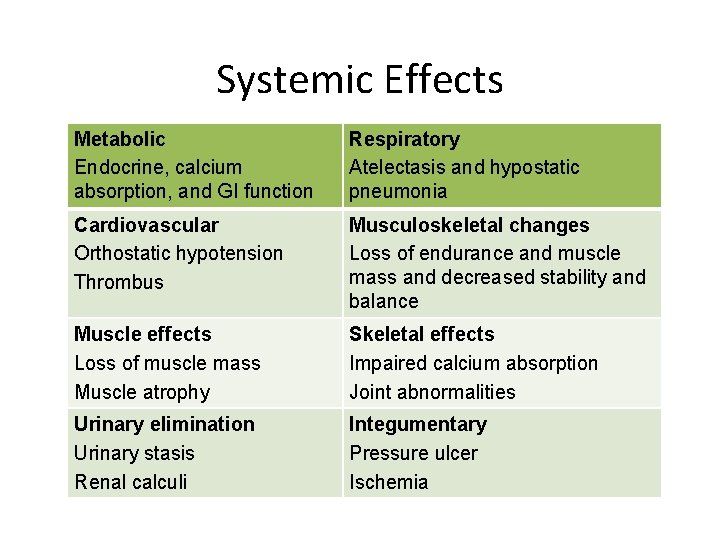
Systemic Effects Metabolic Endocrine, calcium absorption, and GI function Respiratory Atelectasis and hypostatic pneumonia Cardiovascular Orthostatic hypotension Thrombus Musculoskeletal changes Loss of endurance and muscle mass and decreased stability and balance Muscle effects Loss of muscle mass Muscle atrophy Skeletal effects Impaired calcium absorption Joint abnormalities Urinary elimination Urinary stasis Renal calculi Integumentary Pressure ulcer Ischemia
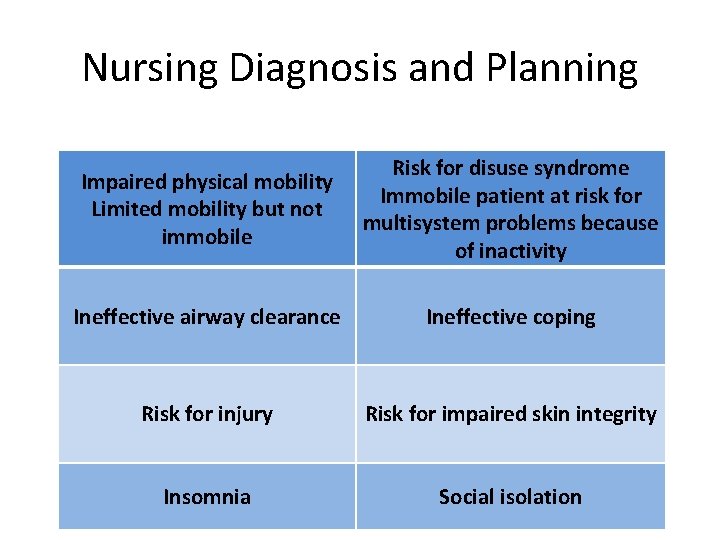
Nursing Diagnosis and Planning Impaired physical mobility Limited mobility but not immobile Risk for disuse syndrome Immobile patient at risk for multisystem problems because of inactivity Ineffective airway clearance Ineffective coping Risk for injury Risk for impaired skin integrity Insomnia Social isolation
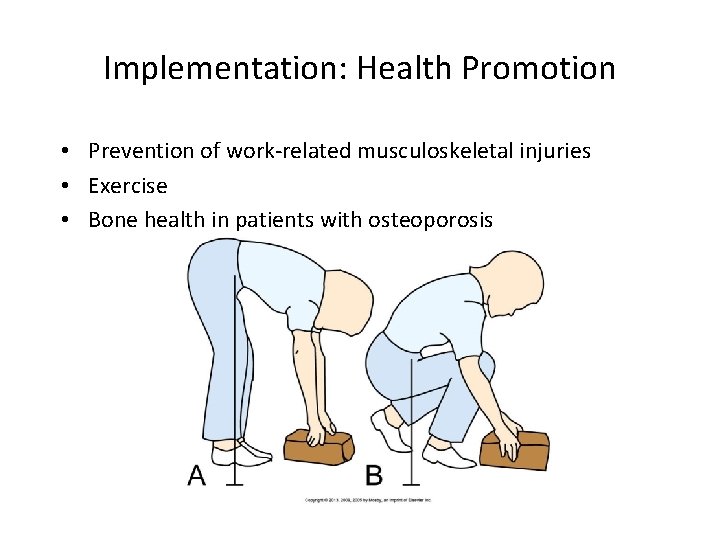
Implementation: Health Promotion • Prevention of work-related musculoskeletal injuries • Exercise • Bone health in patients with osteoporosis
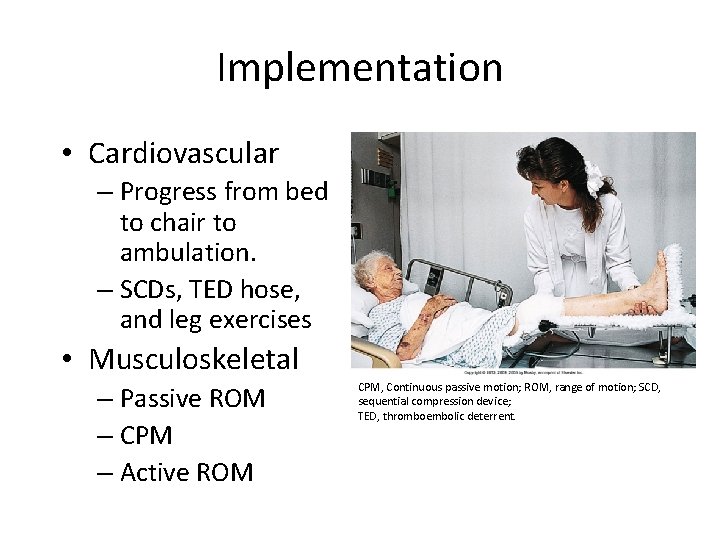
Implementation • Cardiovascular – Progress from bed to chair to ambulation. – SCDs, TED hose, and leg exercises • Musculoskeletal – Passive ROM – CPM – Active ROM CPM, Continuous passive motion; ROM, range of motion; SCD, sequential compression device; TED, thromboembolic deterrent.
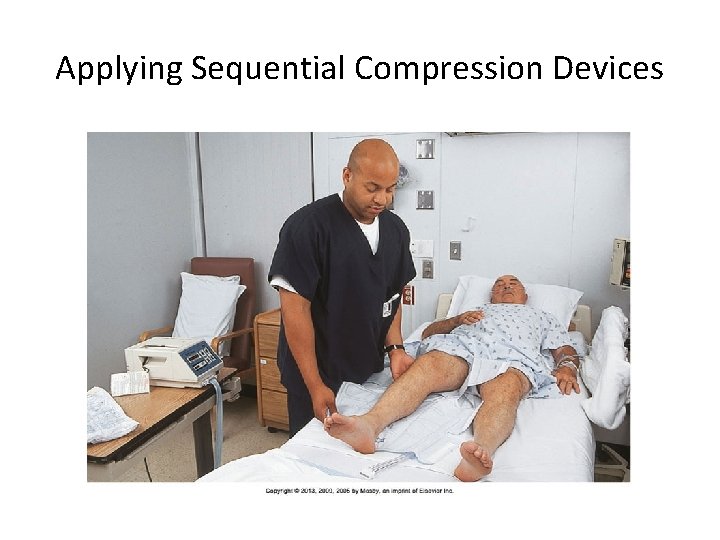
Applying Sequential Compression Devices
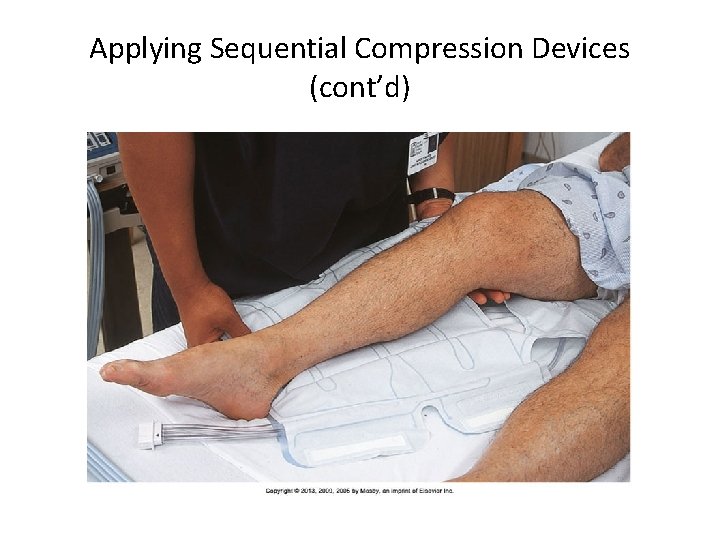
Applying Sequential Compression Devices (cont’d)
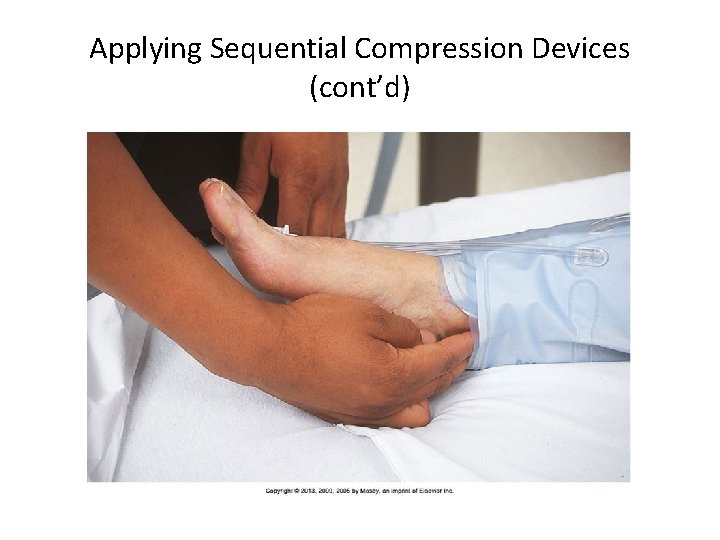
Applying Sequential Compression Devices (cont’d)
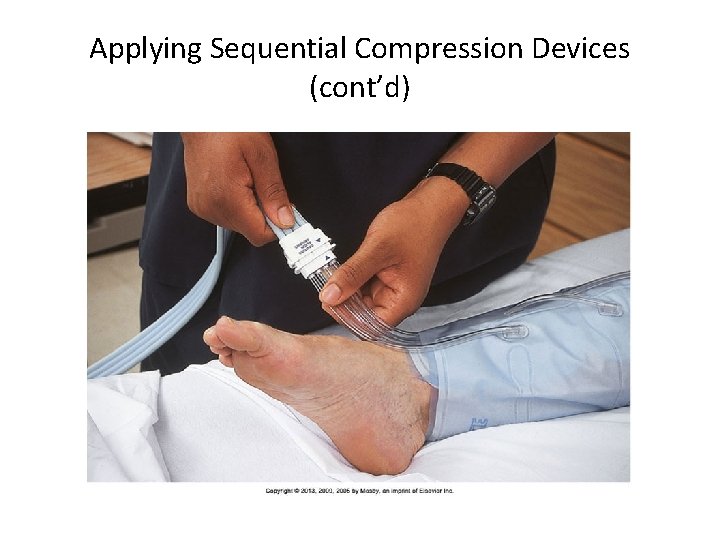
Applying Sequential Compression Devices (cont’d)
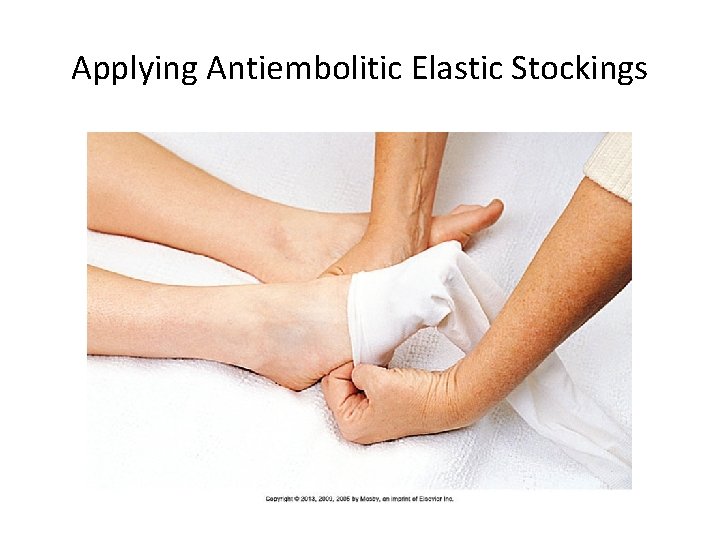
Applying Antiembolitic Elastic Stockings
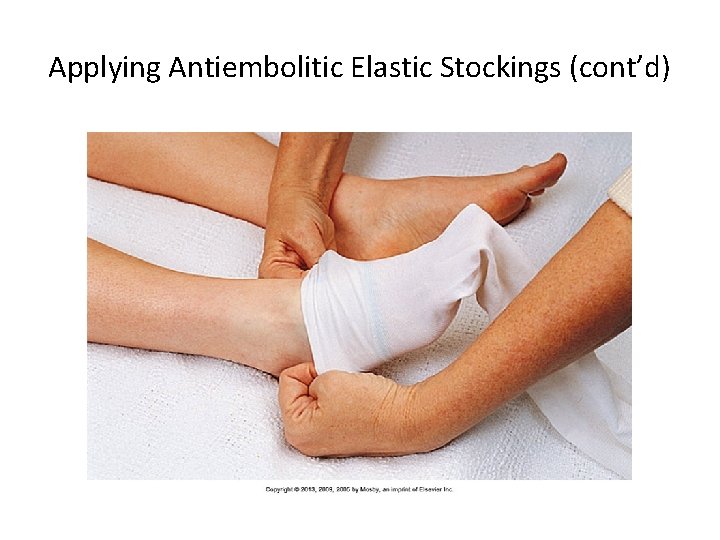
Applying Antiembolitic Elastic Stockings (cont’d)
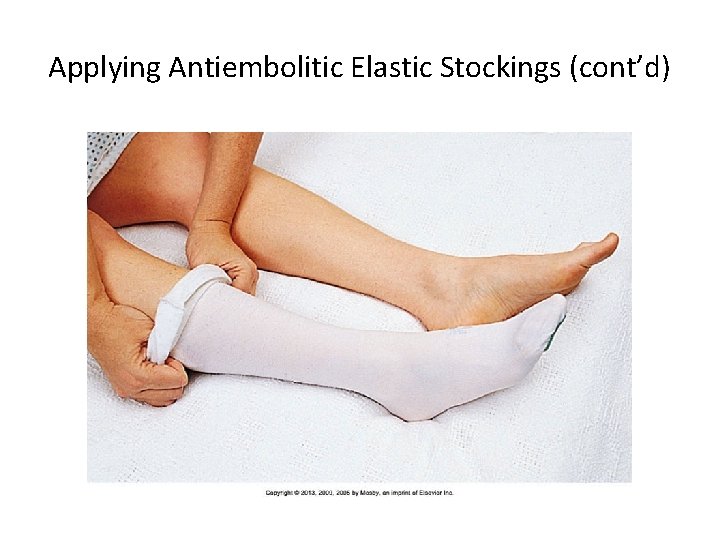
Applying Antiembolitic Elastic Stockings (cont’d)
Quick Quiz! 2. After completing preoperative teaching for a surgical patient, you can evaluate the patient’s understanding of the use of elastic stockings when the patient states A. “I can remove them at night. ” B. “I can roll them no lower than my calf muscle. ” C. “I wear them no longer than 4 hours at a time. ” D. “I can remove them for 30 minutes every 8 hours. ”
Implementation • Integumentary system – Reposition every 1 to 2 hours. – Provide skin care. • Elimination system – Provide adequate hydration. – Serve a diet rich in fluids, fruits, vegetables, and fiber.
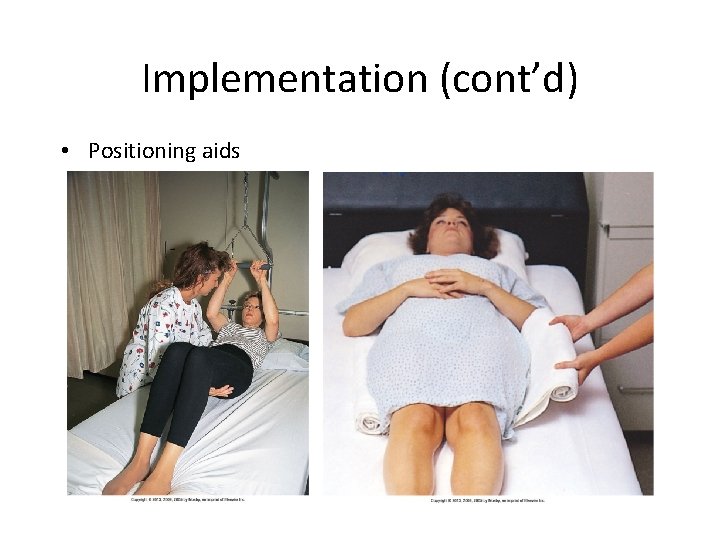
Implementation (cont’d) • Positioning aids
Implementation (cont’d) • Positioning techniques – Supported Fowler’s – Supine – Prone – Side-lying – Sims’
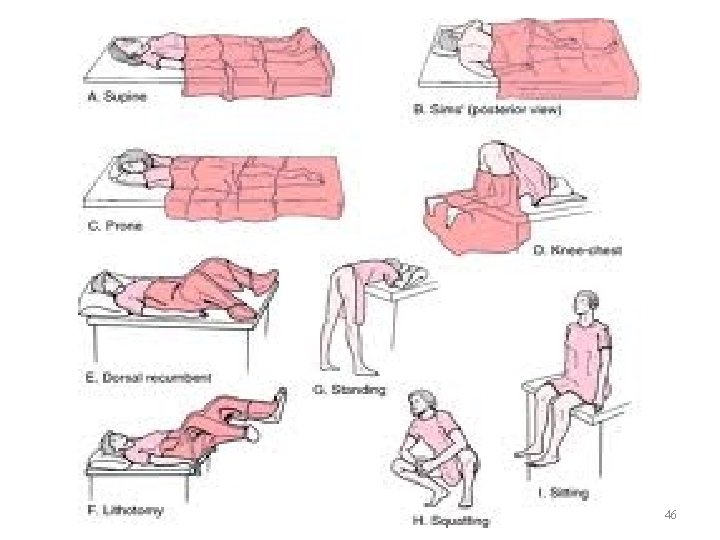
46
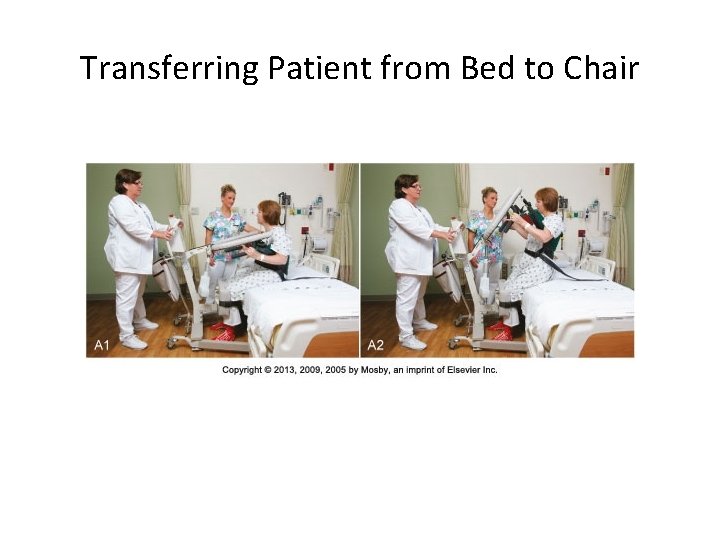
Transferring Patient from Bed to Chair

Transferring Patient from Bed to Chair (cont’d)

Transferring Patient from Bed to Chair (cont’d)

Transferring Patient from Bed to Chair (cont’d)
Transferring Patient from Bed to Stretcher • Determine patient’s ability to assist. • Communicate actions to patient. • Use appropriate resources.
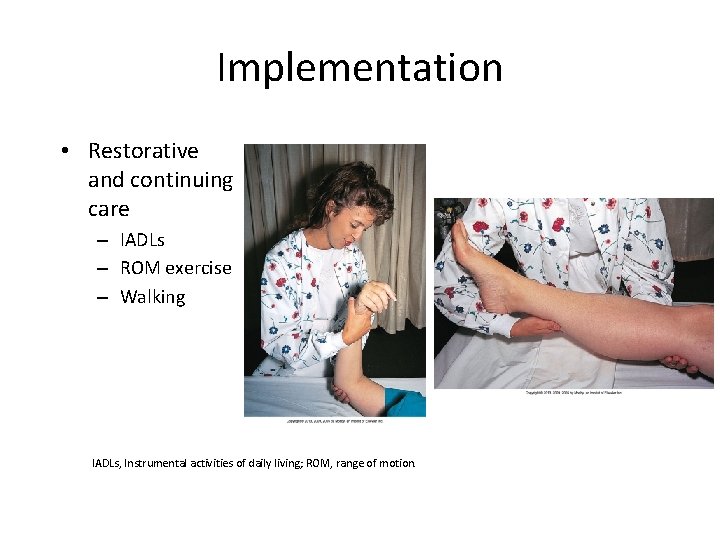
Implementation • Restorative and continuing care – IADLs – ROM exercise – Walking IADLs, Instrumental activities of daily living; ROM, range of motion.
Safety Guidelines • • • Communicate clearly. Mentally review transfer steps. Assess patient mobility and strength. Determine assistance needed. Raise side rail on opposite side of bed. Arrange equipment. Evaluate body alignment. Understand use of equipment. Educate patient.
This work is licensed under a Creative Commons Attribution 4. 0 International License. Except where otherwise noted, this content by Southern Regional Technical College is licensed under the Creative Commons Attribution 4. 0 International License. To view a copy of this license, click https: //creativecommons. org/licenses/by/4. 0/ Healthcare Careers Work!(HCW) is sponsored by a $2. 3 million grant from the U. S. Department of Labor, Employment & Training Administration. TAACCCT Grant #TC- 26488 -14 -60 -A-13. Southern Regional Technical College is an equal opportunity employer and will make adaptive equipment available to persons with disabilities upon request. This workforce product was funded by a grant awarded by the U. S. Department of Labor’s Employment and Training Administration. The product was created by the grantee and does not necessarily reflect the official position of the U. S. Department of Labor. The U. S. Department of Labor makes no guarantees, warranties, or assurances of any kind, express or implied, with respect to such information, including any information on linked sites and including, but not limited to, accuracy of the information or its completeness, timeliness, usefulness, adequacy, continued availability, or ownership.
- Slides: 54